Proteinuria Plasma proteins essential components of any living



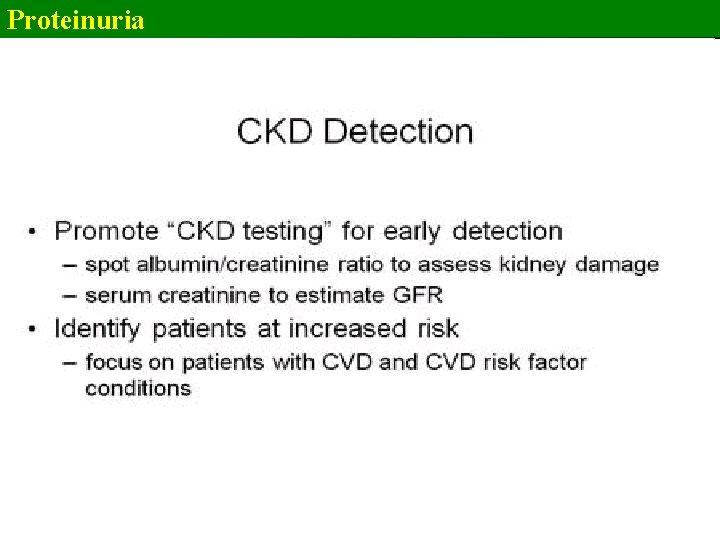
- Slides: 68
Proteinuria Plasma proteins - essential components of any living being The kidneys play a major role in the retention of plasma proteins glomerular filtration barrier renal tubules reabsorption of the passing through glomerular filtration barrier proteins
Proteinuria The glomerular capillary wall - charge and size-selective properties high-molecular-weight (HMW) plasma proteins can not enter the urinary space only a tiny fraction of albumin, globulin, and other large plasma proteins cross LMW proteins (<20, 000 Da) cross capillary wall they are normally reabsorbed by the proximal tubule
Proteinuria Most healthy individuals excrete 30 and 130 mg/day of protein the upper limit of normal total urine protein excretion - 150 to 200 mg/day for adults the upper limit of normal albumin excretion - 30 mg/day
Proteinuria Normal tubular protein secretion a very small amount of protein that normally appears in the urine Tamm-Horsfall protein (uromodulin) HMW glycoprotein (23 × 106 Da) formed on the epithelial surface of the thick ascending limb of the loop of Henle and early distal convoluted tubule binds and inactivates the cytokines interleukin-1 and tumor necrosis factor Immunoglobulin A (Ig. A) Urokinase
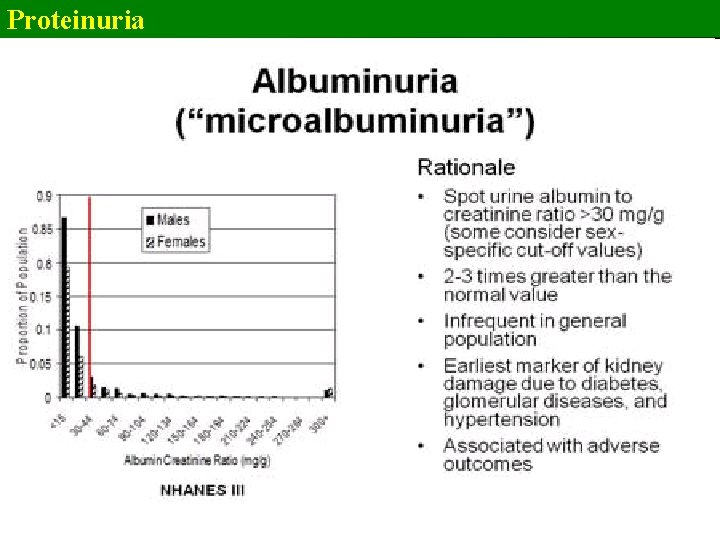
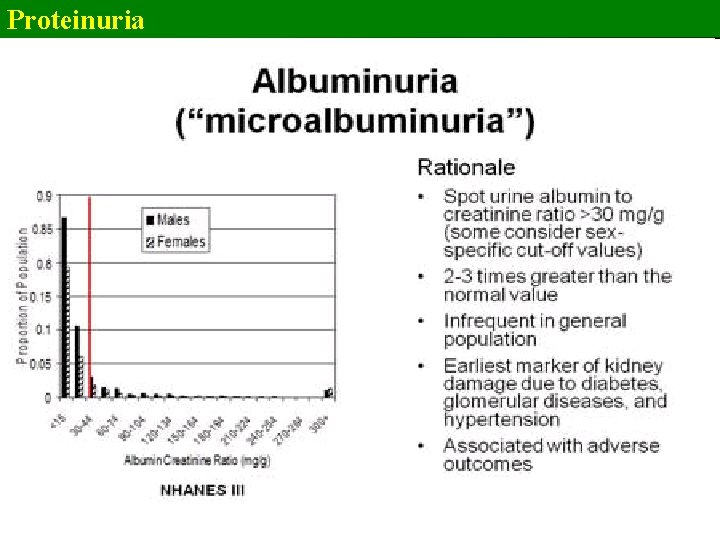
Proteinuria Normal urine protein excretion up to 150 mg/d the detection of abnormal quantities or types of protein in the urine - an early sign of significant renal or systemic disease Normal urine albumin excretion less than 5 mg/L low levels of albumin excretion = microalbuminuria linked to the identification of the early stages of diabetic kidney disease Microalbuminuria excretion of 30 -300 mg/d or 20 -200 µg/min too small to be detected by routine dipstick screening
Proteinuria Abnormal amounts of protein in the urine – three/four mechanisms glomerular proteinuria üdisruption of the capillary wall barrier a large amount of HMW plasma proteins that overwhelm the limited capacity of tubular reabsorption and cause protein to appear in the urine tubular proteinuria ütubular damage or dysfunction inhibit the normal resorptive capacity of the proximal tubule increased amounts of mostly LMW proteins appear in the urine increased production of normal or abnormal plasma proteins can be filtered at the glomerulus and overwhelms the resorptive capacity of the proximal tubule (!!) –rarely - increased urine protein due to increased tubular production of protein
Proteinuria β 2 -Microglobulin üan LMW (11. 8 -k. Da) protein üidentified as the light chain of class I major histocompatibility antigens (e. g. , human leukocyte antigens [HLAs] A, B, and C) üfreely filtered at the glomerulus avidly taken up and catabolized by the proximal tubule üdetectable urinary levels of β 2 -microglobulin - associated with many pathologic conditions involving the proximal tubule • aminoglycoside • Balkan endemic nephropathy • heavy metal nephropathies • radiocontrast nephropathy • kidney transplant rejection • useful in distinguishing upper from lower urinary tract infection.
Proteinuria Bence Jones protein üimmunoglobulin light chains filtered at the glomerulus üplasma cell dyscrasias may produce monoclonal proteins, immunoglobulin, free light chains, and a combination of these üthe detection of urine immunoglobulin light chains can be the first clue to a number of important clinical syndromes associated with plasma cell dyscrasias that involve the kidney üplasma cell dyscrasias may also manifest as proteinuria or albuminuria when the glomerular deposition of light chains causes disruption of the normally impermeable capillary wall (!!)
Proteinuria Selective or nonselective proteinuria üglomerular proteinuria can be further characterized as selective or nonselective üa clearance ratio of immunoglublin G (Ig. G; an HMW protein)–to-albumin that is less than 0. 10 = selective proteinuria ümore often seen in patients with minimal change disease üpredicts a good response to treatment with corticosteroids üIg. G-to-albumin clearance ratios greater than 0. 50 = nonselective pattern üthe cost of the protein separation procedures has limited their widespread clinical use
Proteinuria Glomerular proteinuria / tubular proteinuria ühigher amounts of albumin and HMW proteins suggest glomerular proteinuria ünephrotic range >3 g/24 hr certain glomerular source üisolated increases in LMW protein fractions are more suggestive of tubular proteinuria üit is unusual for tubular proteinuria to exceed 1 to 2 g/day üonly a small fraction of protein excretion due to tubular damage should be albumin ütubular proteins are heterogeneous; α 2 -microglobulin is often a major constituent
Proteinuria Techniques to Measure Urine Protein in random samples in timed or untimed overnight samples in 24 -hour collections üsource of error - inaccurate urine collection particularly 24 -hour collections
Proteinuria Techniques to Measure Urine Protein Tests to accurately quantitate total protein concentration in urine rely on precipitation(sulfosalicylic acid is added to a sample of urine, and the turbidity is measured with a photometer or a nephelometer ) Tests to estimate total protein concentration in urine chemically impregnated plastic strips (dipstick)
Proteinuria Techniques to Measure Urine Protein Tests to accurately quantitate total protein concentration in urine (precipitation) üproteins detected: γ-globulin light chains, albumin üthe method is more sensitive to albumin than to globulins ütrichloroacetic acid can be used in place of sulfosalicylic acid to increase the sensitivity to γ-globulin (eg for Bence Jones protein) Tests to estimate total protein concentration in urine(dipstick) üp. H-sensitive colorimetric indicator that changes color when negatively charged proteins bind to it üpositively charged proteins are less detected immunoglobulin light chains may escape urine dipstick detection even when present in large amounts in the urine üsensitive to very small urine protein concentrations -the lower limit of detection 1020 mg/d. L (could be Tamm-Horsfall protein )
Proteinuria Techniques to Measure Urine Protein quantitative determinations of albuminas gold standards üRadioimmunoassay üImmunoturbimetric technique üEnzyme-linked immunosorbent assay (ELISA)
Proteinuria Techniques to Measure Urine Protein Screening methods dipstick = qualitative or semiquantitative for total protein excretion and microalbuminuria üsensitivity and specificity - markedly influenced by fluid intake, state of diuresis, and the resulting urine concentration protein-to-creatinine or albumin-to-creatinine ratio in random, or timed urine collections üthere is a high degree of correlation between 24 -hour urine protein excretion and protein-to-creatinine ratios in random, single-voided urine samples in patients with a variety of kidney diseases
Proteinuria Techniques to Measure Urine Protein Screening methods - protein-to-creatinine or albumin-to-creatinine ratio ümore quantitative than a simple dipstick screening procedure üa protein-to-creatinine ratio of greater than 3. 0 or 3. 5 mg/mg or less than 0. 2 mg/mg indicates protein excretion rates of greater than 3. 0 or 3. 5 g/24 hr or less than 0. 2 g/24 hr
Proteinuria Analytic tools - to separate and identify individual urinary proteins üagarose gel electrophoresis ücolumn gel chromatography üpolyacrylamide gel electrophoresis üimmunoelectrophoresis üisoelectric focusing üproteomic techniques employing mass spectrometry üpeptide mass fingerprinting have been used in clinical laboratories üto determine the selectivity of urine protein üto identify monoclonal immunoglobulin heavy and light chains
Proteinuria β 2 -Microglobulin ücommonly measured in urine using radioimmunoassay or ELISA Bence Jones protein üimmunoglobulin light chains may not be detected by dipstick üa proteinuria or albuminuria may also exists when the glomerular deposition of light chains causes disruption of the normally impermeable capillary wall ümonoclonal proteins are best detected using serum and urine immunoelectrophoresis üthe diagnosis of a plasma cell dyscrasia can be suspected when a tall, narrow band on electrophoresis suggests the presence of a monoclonal γ-globulin or immunoglobulin light chain
Proteinuria Screening methods established diagnosis of kidney disease Measuring the amount of urine protein (usefull in Ig. A nephropathy, membranous nephropathy, type I membranoproliferative glomerulonephritis, nephrotic syndrome, mild renal insufficiency ) additional prognostic information can be used to monitor the response to immunosuppressive therapy
Proteinuria There are variations of concentration of albumin in the urine with: physical activity level, acute illnesses or fevers, menstruation, pregnancy, vaginal discharge, diet, blood pressure, volume status, degree of glycemic control, and urine collection method (eg, 24 h, overnight or timed, short-term) Albumin excretion - 25% higher during the day than overnight, with a day-to-day variation of 40% before a patient is classified as having microalbuminuria - at least 3 urine samples over a 6 -month period that satisfy the above range criterion are recommended
Proteinuria The presence of abnormal amounts or types of protein in the urine reflects : A defective glomerular barrier abnormal amounts of proteins of intermediate molecular weight enter the Bowman space Tubular diseases inability of the kidneys to normally reabsorb the proteins through the renal tubules Overproduction of plasma proteins pass through the normal glomerular basement membrane (GBM) enter the tubular fluid in amounts that exceed the capacity of the normal proximal tubule to reabsorb them
Proteinuria Symptoms in most patients - asymptomatic proteinuria detected upon screening in patients with hypertension, diabetes frequently in the absence of serious underlying renal disease
Proteinuria The more common and benign causes of proteinuria transient proteinuria associated with physical exertion and fever orthostatic proteinuria (albuminuria < 1 g/d, normal renal function) typically - in tall thin adolescents or adults younger than 30 years, +/severe lordosis overnight urine collection shows normal protein excretion (ie, <50 mg during 8 -h period) nonrenal disease (proteinuria < 1 g/d, normal renal function) severe cardiac failure, sleep apnea
Proteinuria Microalbuminuria (30 -300 mg/d or 20 -200 µg/min) frequently observed in association with: Hypertension Early stages of diabetic nephropathy
Proteinuria in significant glomerular disease in excess of 500 mg/d particularly associated with: Changes in urine appearance: red/smoky, frothy Edema: ankle, periorbital, labial, scrotal Elevated blood pressure Elevated cholesterol, lipiduria, hypoalbuminemia Active urine sediment (dysmorphic red blood cells, +/-red cell casts) Abnormal renal function
Proteinuria in significant glomerular disease Joint discomfort, skin rash, eye symptoms, or symptoms of Raynaud syndrome Multisystem disease : systemic lupus erythematosus, rheumatoid arthritis History of kidney disease (including pregnancy related) Medication, including over-the-counter or herbal remedies Past health problems, such as jaundice, tuberculosis, malaria, syphilis, endocarditis Systemic symptoms, such as fever, night sweats, weight loss, or bone pain Risk factors for HIV or hepatitis Symptoms that suggest complication(s) of nephrotic syndrome Loin pain, abdominal pain, breathlessness, pleuritic chest pain, rigors Associated upper respiratory tract infection
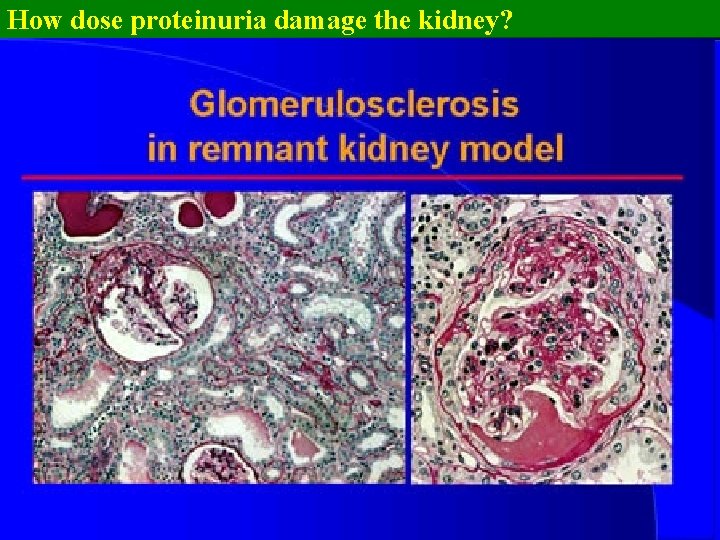
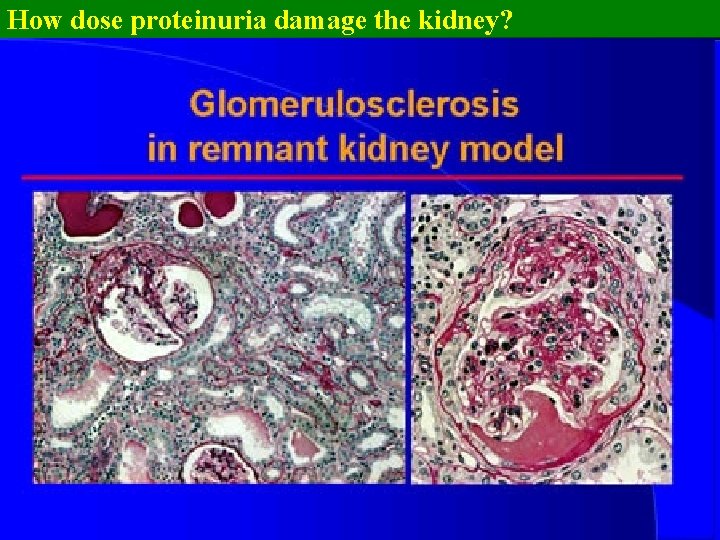
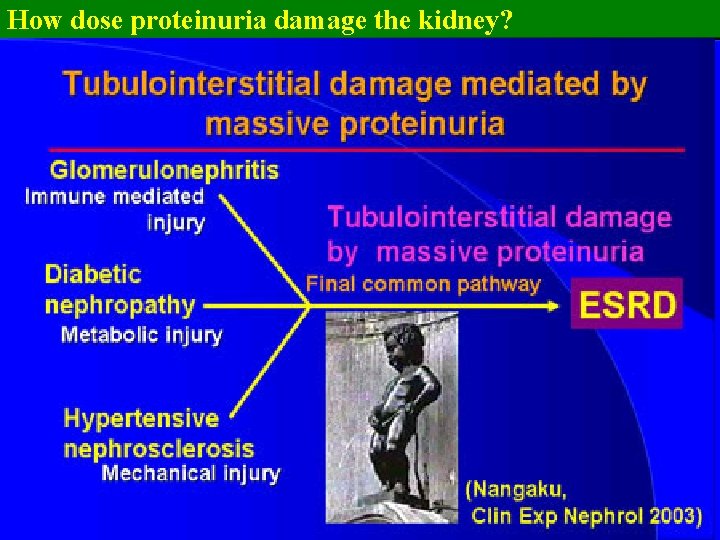
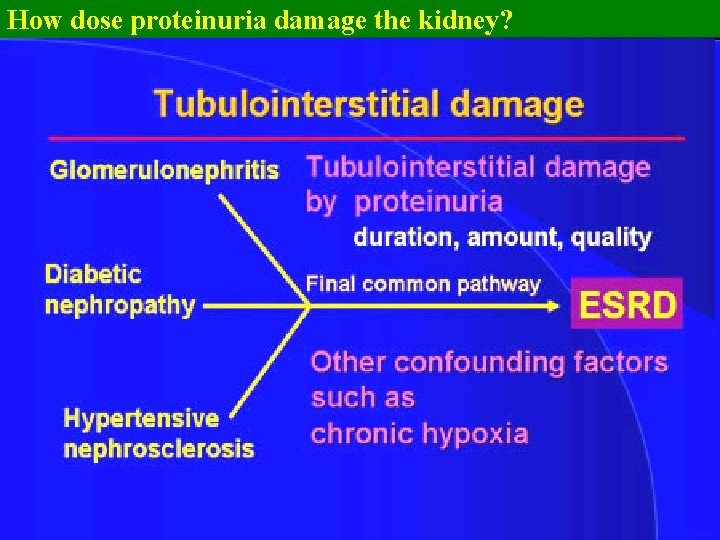
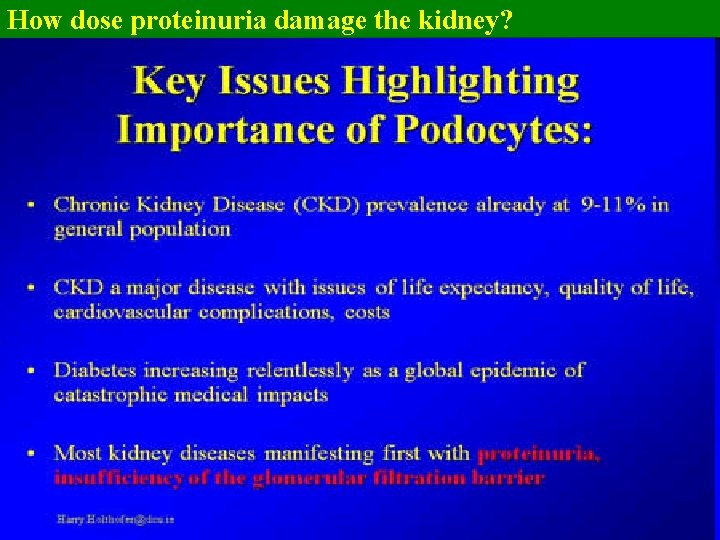
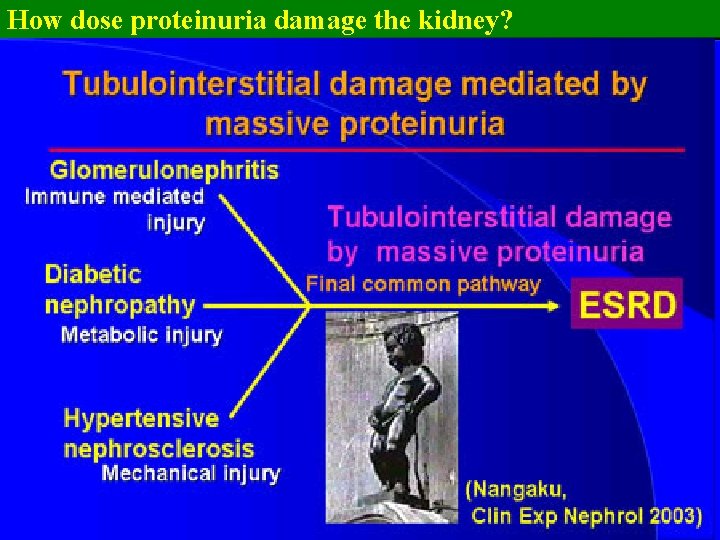
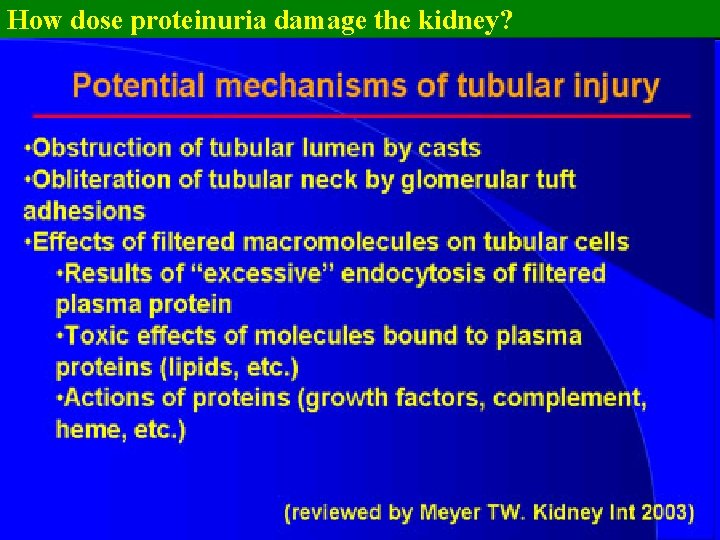
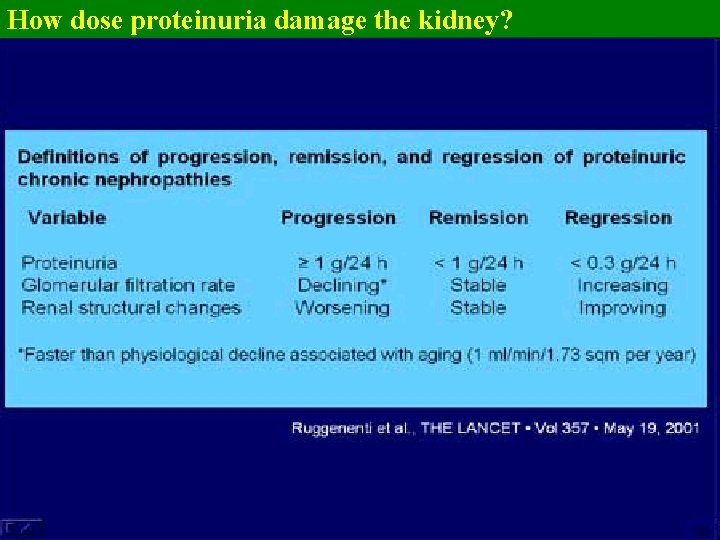
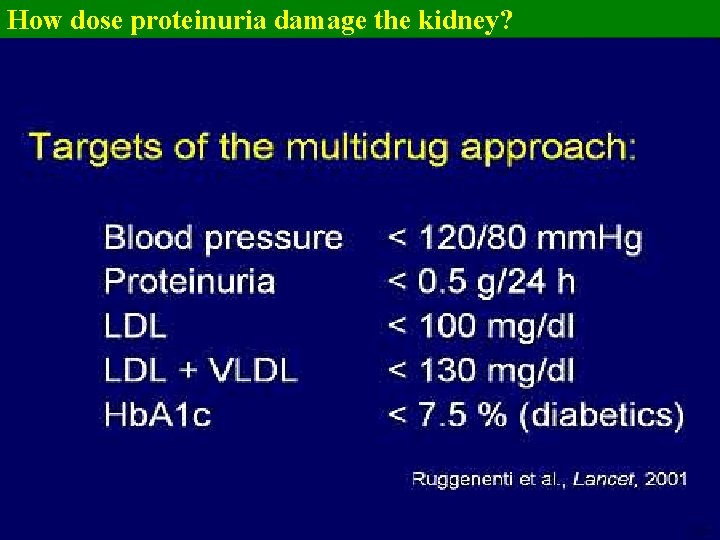
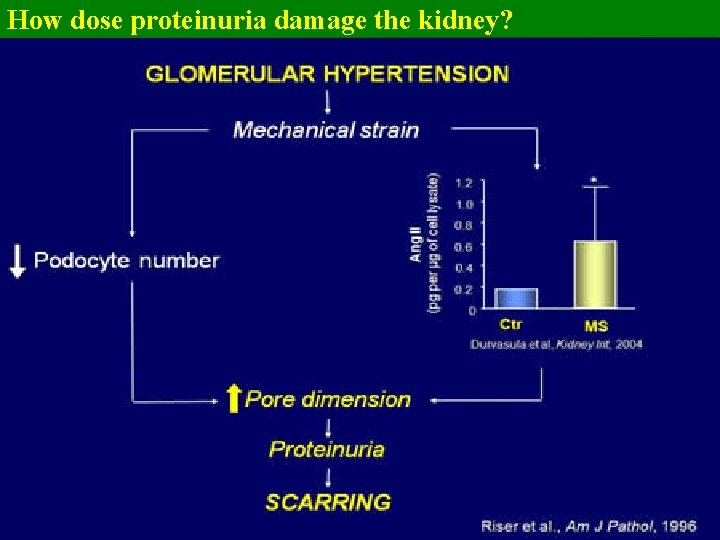
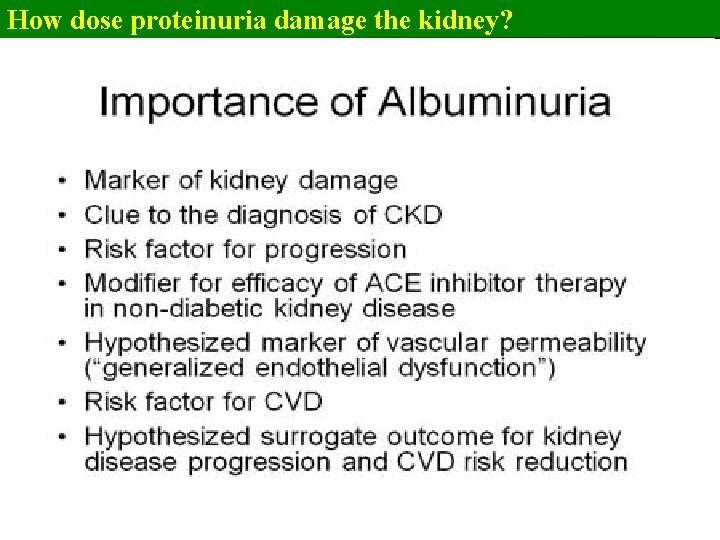
How dose proteinuria damage the kidney?
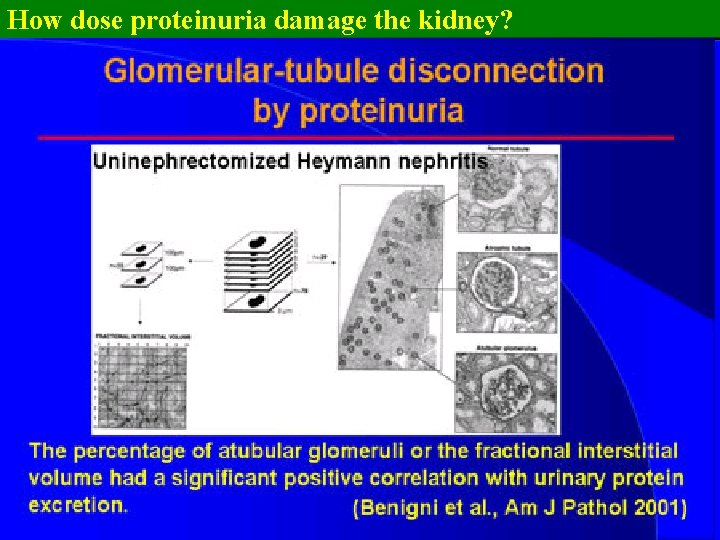
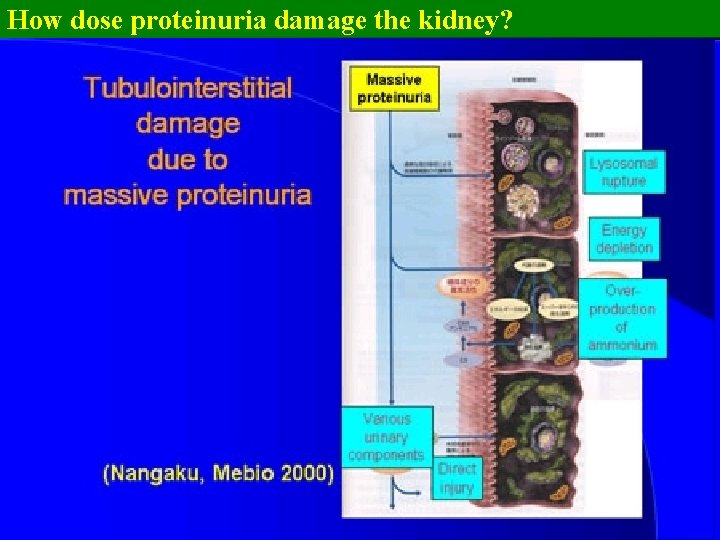
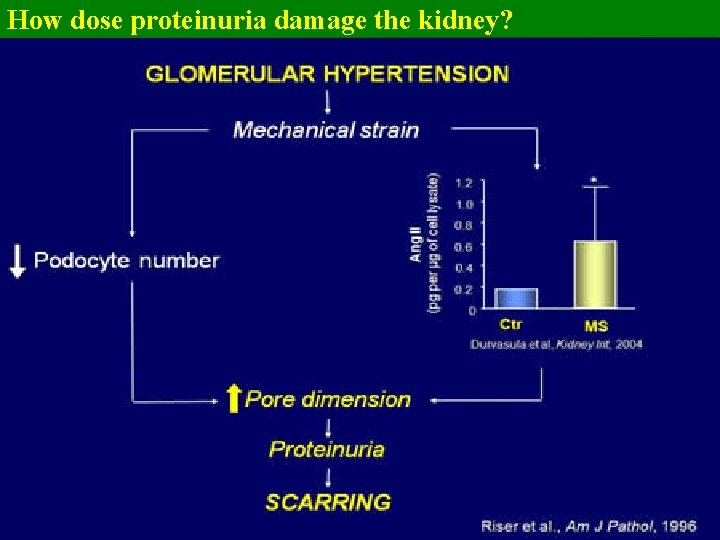
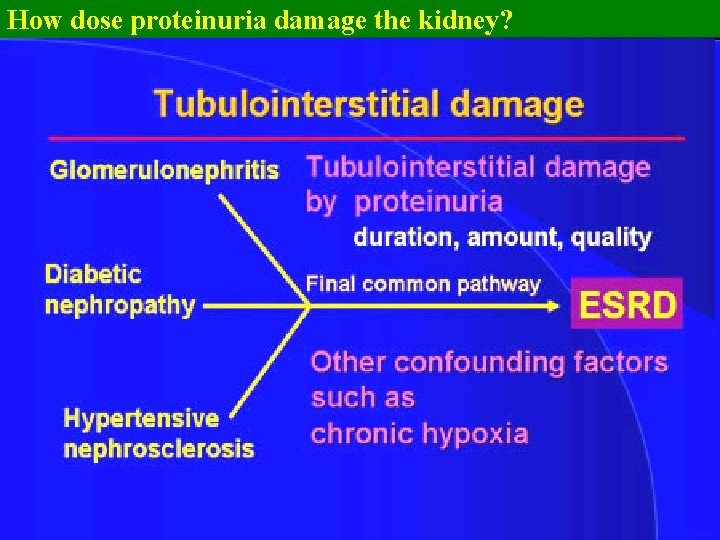
How dose proteinuria damage the kidney? 1. glomerulosclerosis is explained by the hyperfiltration theory 2. tubulointerstitial injury is olso induced by proteinuria; this is a final common pathway to eventual kidney failure
How dose proteinuria damage the kidney?
How dose proteinuria damage the kidney?
How dose proteinuria damage the kidney?
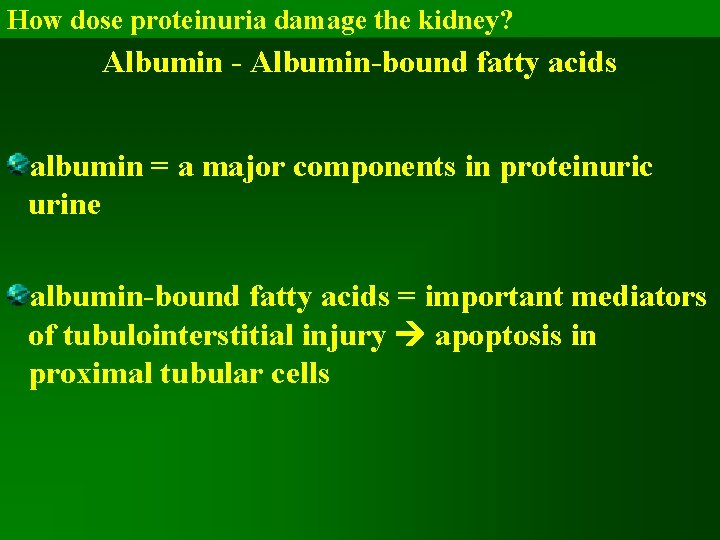
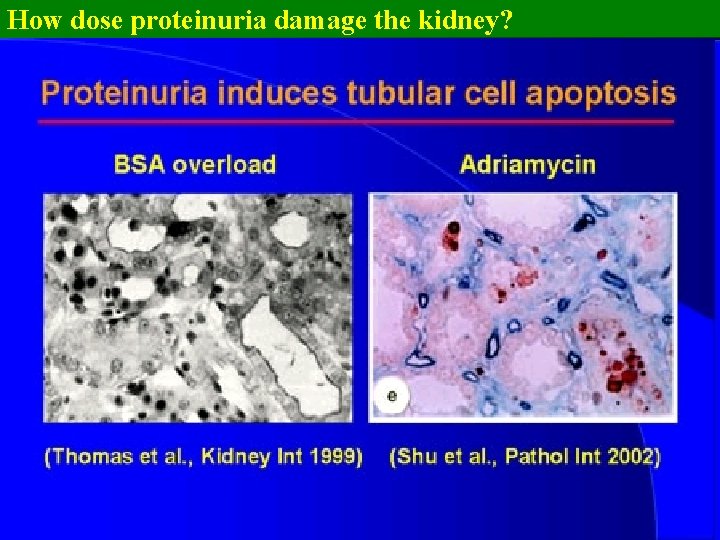
How dose proteinuria damage the kidney? Albumin - Albumin-bound fatty acids albumin = a major components in proteinuric urine albumin-bound fatty acids = important mediators of tubulointerstitial injury apoptosis in proximal tubular cells
How dose proteinuria damage the kidney?
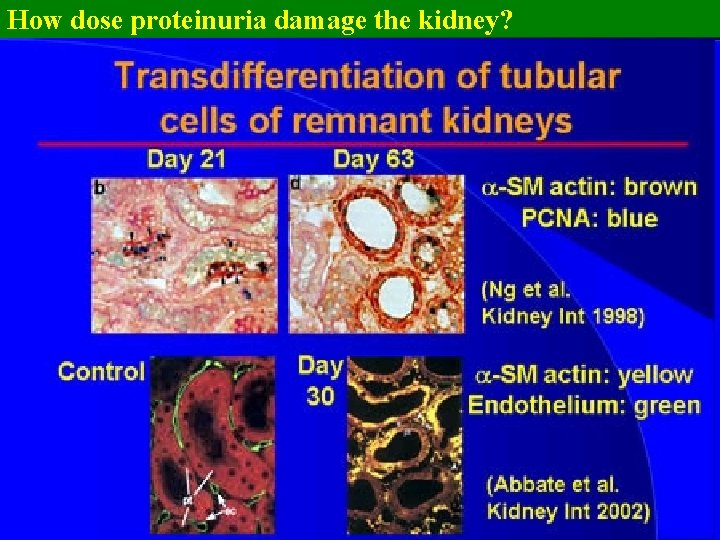
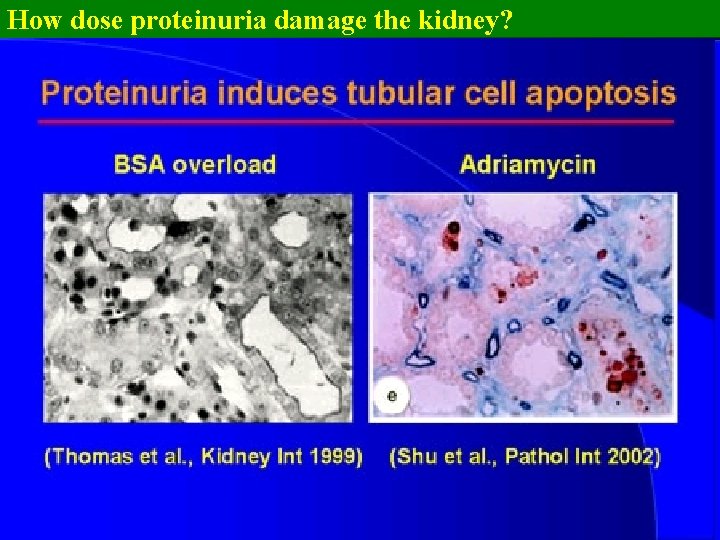
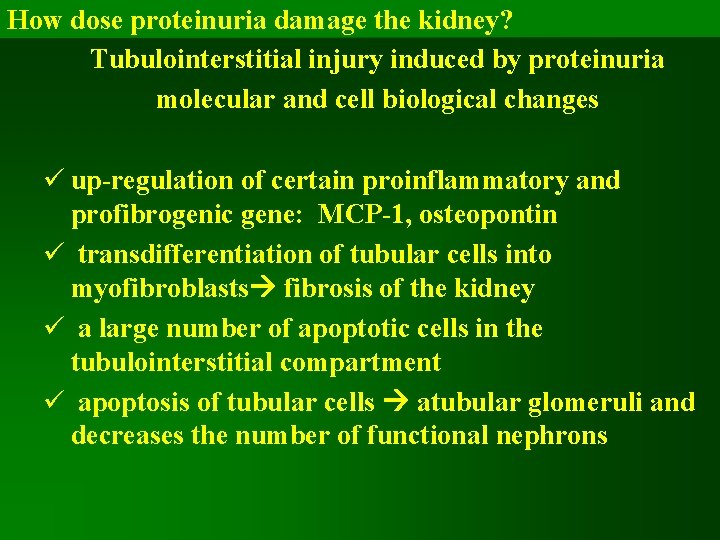
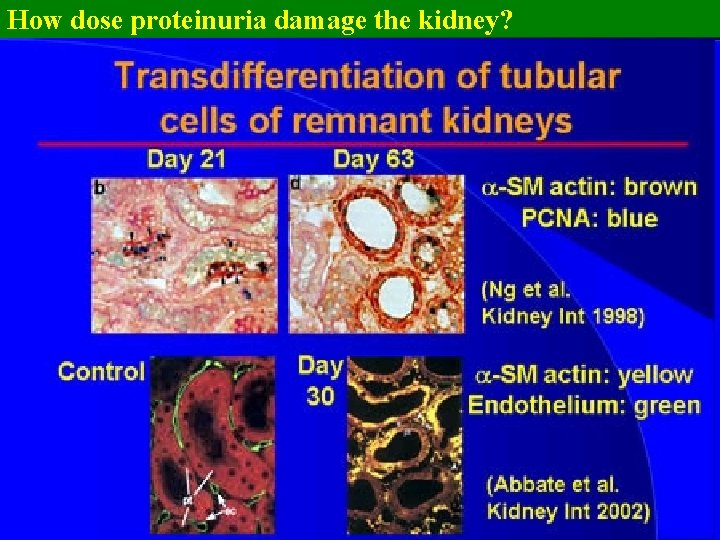
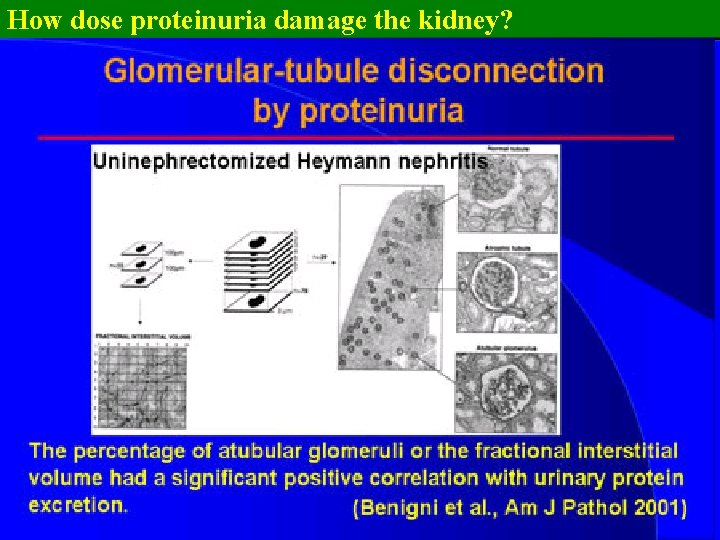
How dose proteinuria damage the kidney? Tubulointerstitial injury induced by proteinuria molecular and cell biological changes ü up-regulation of certain proinflammatory and profibrogenic gene: MCP-1, osteopontin ü transdifferentiation of tubular cells into myofibroblasts fibrosis of the kidney ü a large number of apoptotic cells in the tubulointerstitial compartment ü apoptosis of tubular cells atubular glomeruli and decreases the number of functional nephrons
How dose proteinuria damage the kidney? Tubulointerstitial injury induced by proteinuria = atubular glomeruli and interstitial fibrosis

How dose proteinuria damage the kidney? What mediates tubular and interstitial damage induced by proteinuria?
How dose proteinuria damage the kidney?
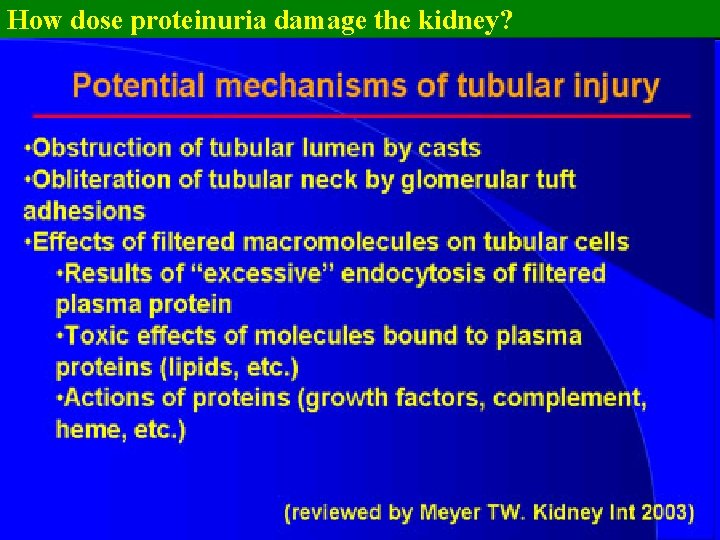
How dose proteinuria damage the kidney? Effects of filtered macromolecules on tubular cells
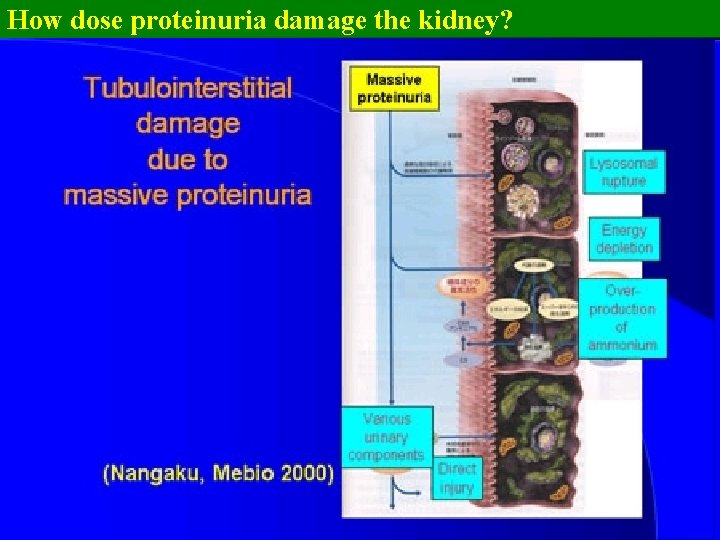
How dose proteinuria damage the kidney?
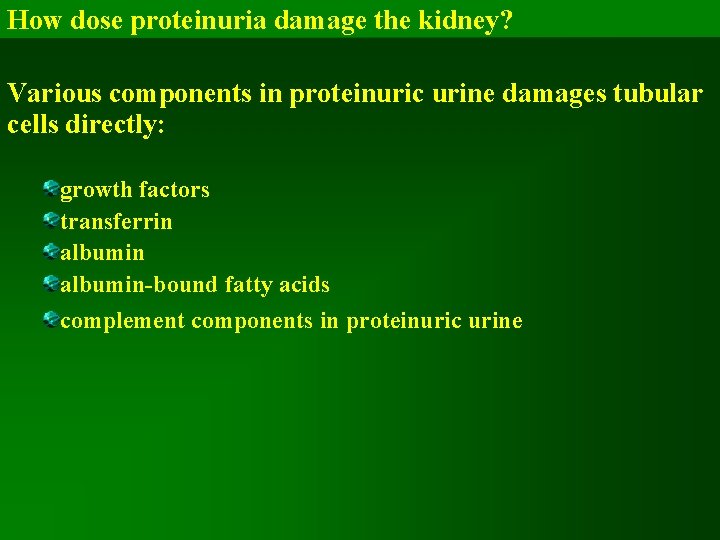
How dose proteinuria damage the kidney? Various components in proteinuric urine damages tubular cells directly: growth factors transferrin albumin-bound fatty acids complement components in proteinuric urine
How dose proteinuria damage the kidney? Protein overload in tubular cells is also associated with ammonium production Complement component C 3 modified by ammonia = amidated C 3 forms the alternative pathway convertase of the complement cascade Preferential secretion of ammonia into the tubular lumen inappropriate activation of the alternative pathway at the brush border in proteinuric conditions
How dose proteinuria damage the kidney? Complement components in proteinuric urine = crucial mediator of tubulointerstitial damage complement is activated in urine of patients with various glomerular diseases the degree of intratubular complement activation correlated with the level of non-selective proteinuria
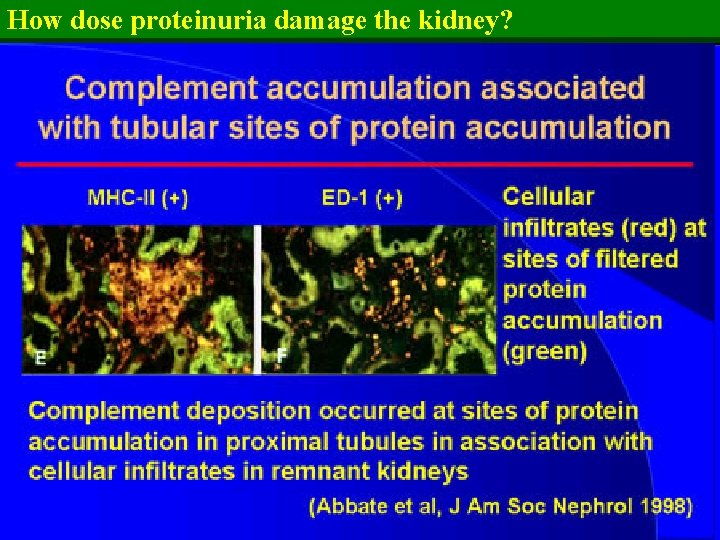
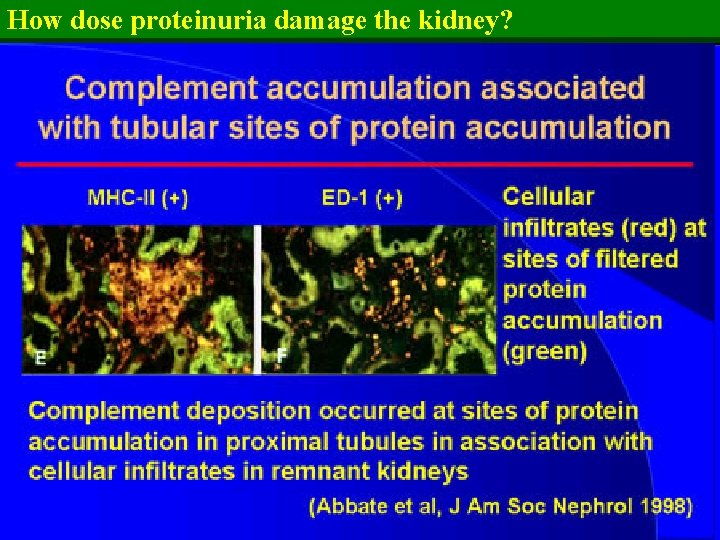
How dose proteinuria damage the kidney?
How dose proteinuria damage the kidney? accumulation of inflammatory cells around tubules of high filtered protein load C 3 staining in the brush border or within the cytoplasm at sites of high protein reabsorption !! renoprotective effects of ACE inhibitor by limiting tubular activation of complement
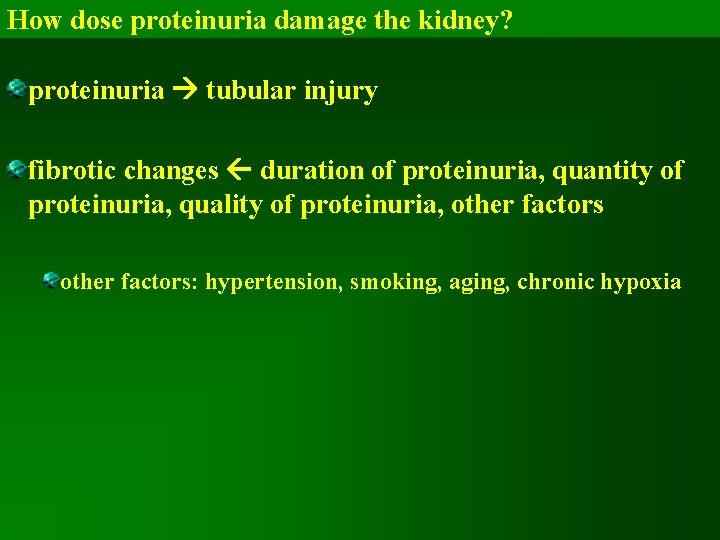
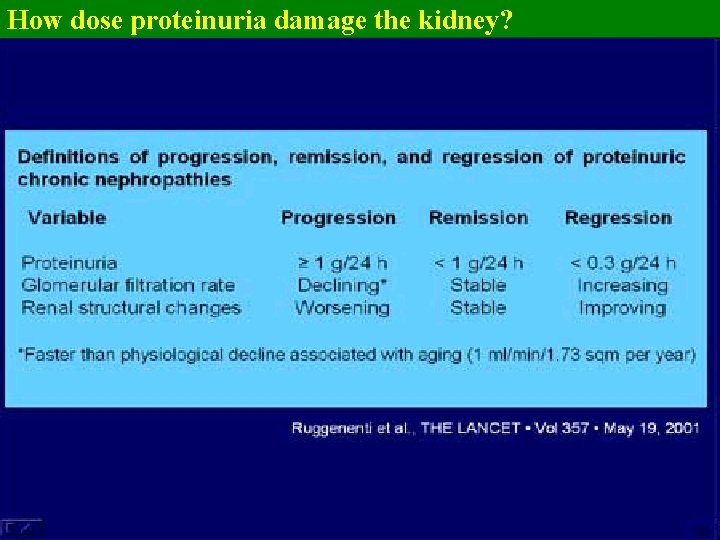
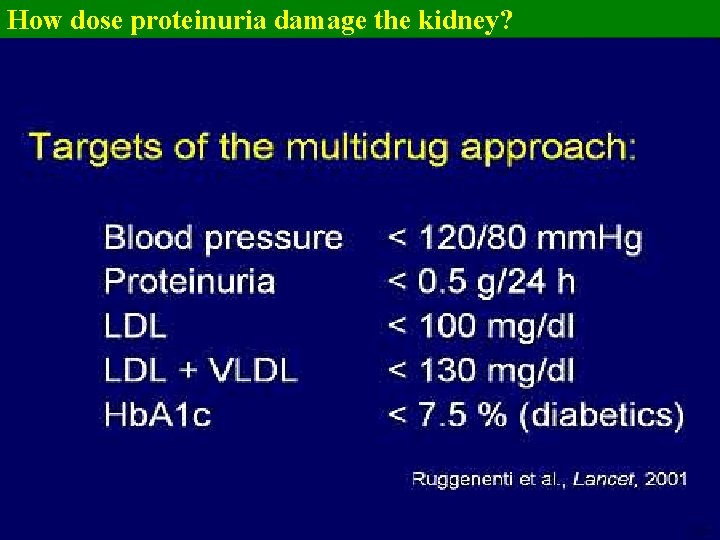
How dose proteinuria damage the kidney? proteinuria tubular injury fibrotic changes duration of proteinuria, quantity of proteinuria, quality of proteinuria, other factors: hypertension, smoking, aging, chronic hypoxia
How dose proteinuria damage the kidney? ?

How dose proteinuria damage the kidney?
How dose proteinuria damage the kidney? ?
How dose proteinuria damage the kidney?

How dose proteinuria damage the kidney?
How dose proteinuria damage the kidney?
How dose proteinuria damage the kidney?
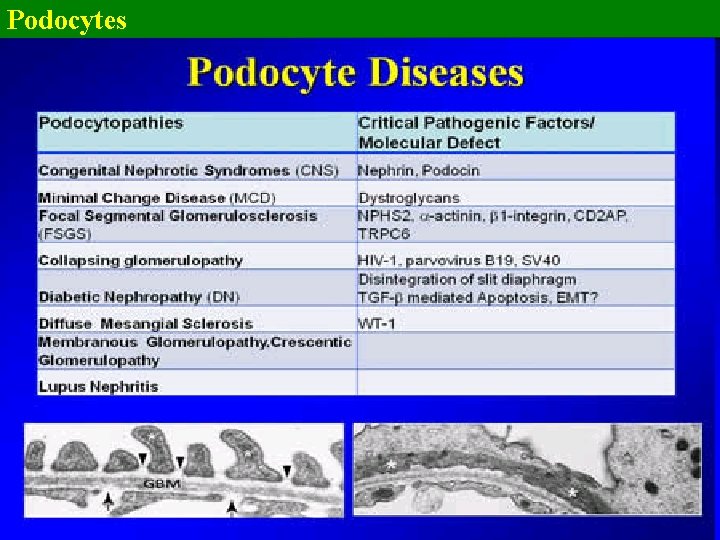
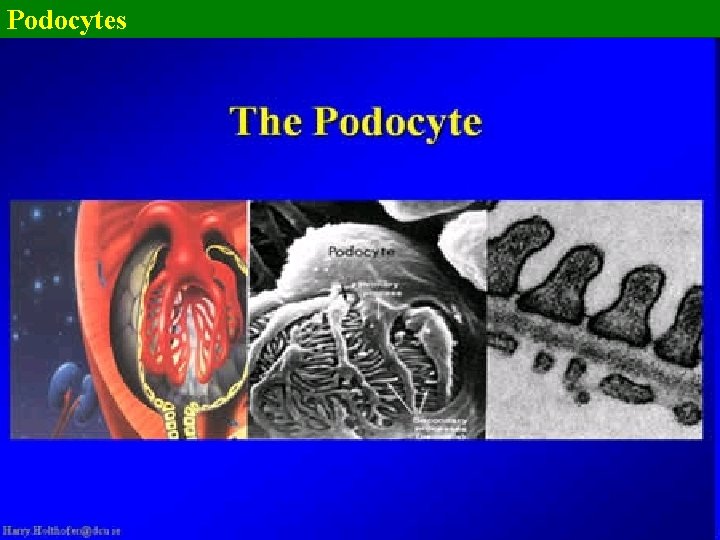
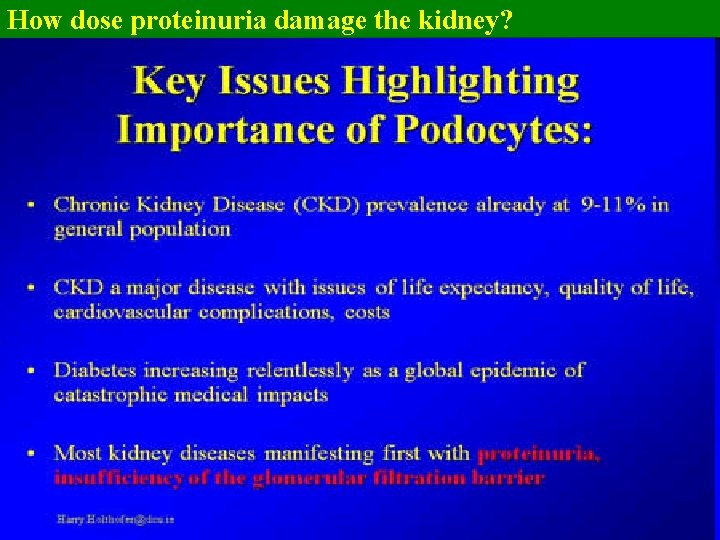
Podocytes
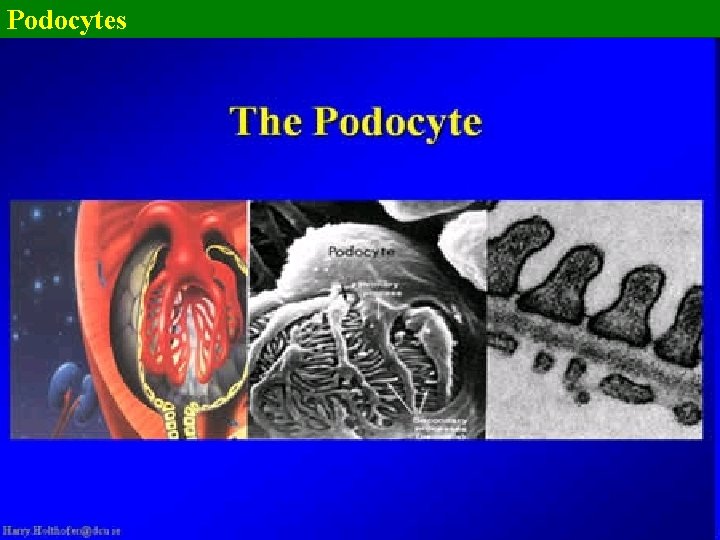
Podocytes
Podocytes
Podocytes
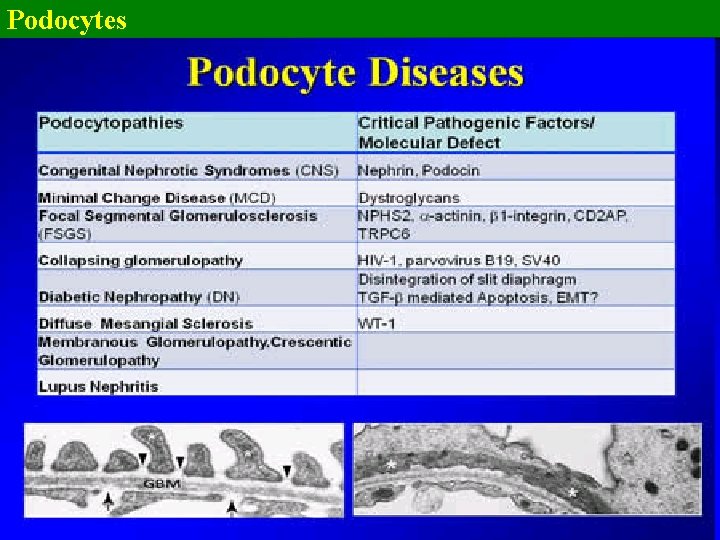
Podocytes there are quite a number of podocyte diseases = podocytopathies in the podocytopathies the orderly structure of the podocytes and the foot processes interlinked by the slit diaphragms is lost (effacement of the podocytes
Podocytes the filtration barrier = an amazing structure filtering something like 200 -500 l plasma per day and producing something like 200 l of primary urine the podocyte which is really standing or sitting on top of the capillaries is one of the key players there in the final regulation of the passage of the proteins or actually preventing the leakage of the proteins
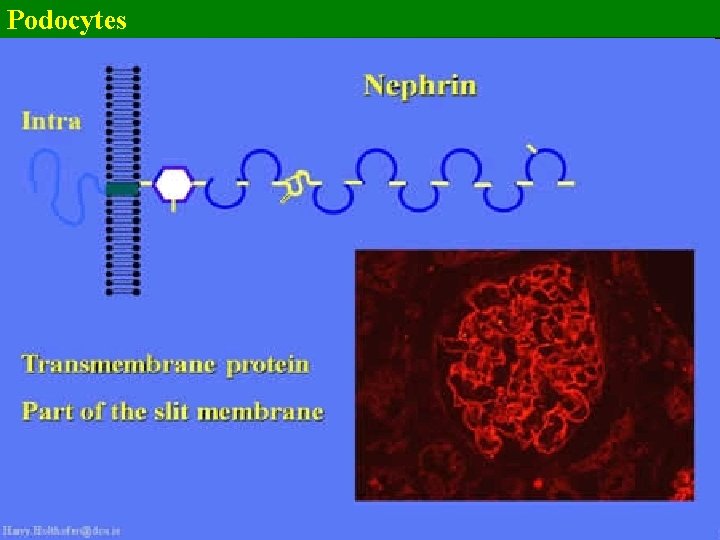
Podocytes there is a number of molecules located in the slit diaphragm domain transmembrane or intracellular these molecules adjust the shape of the podocyte foot processes
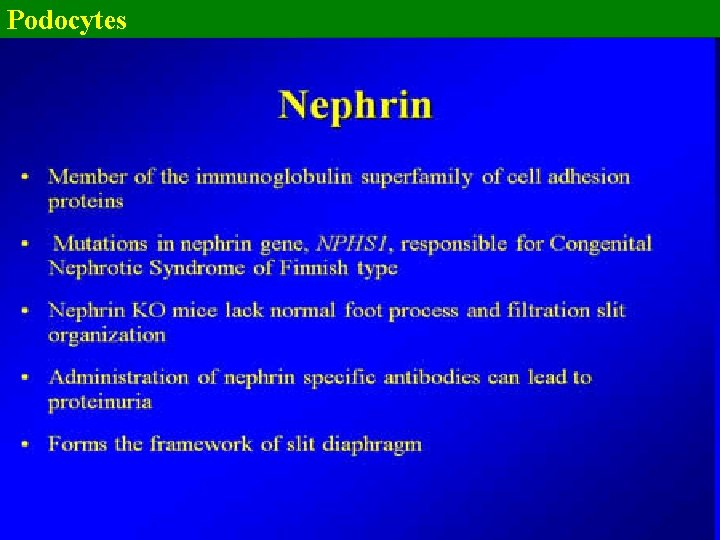
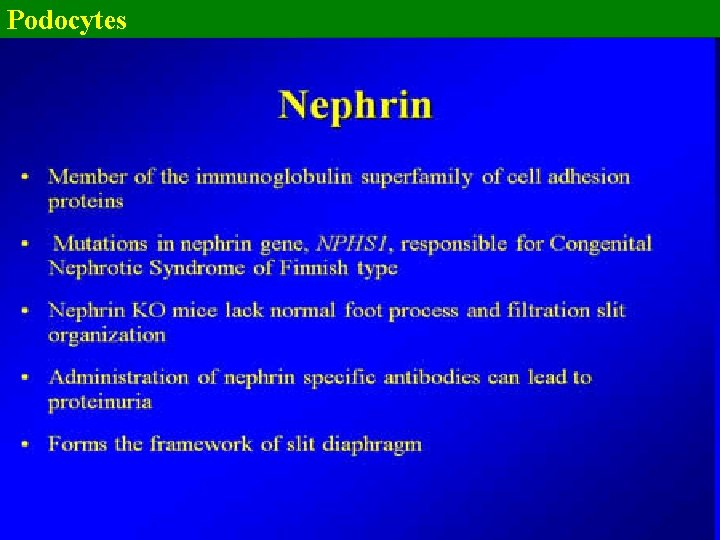
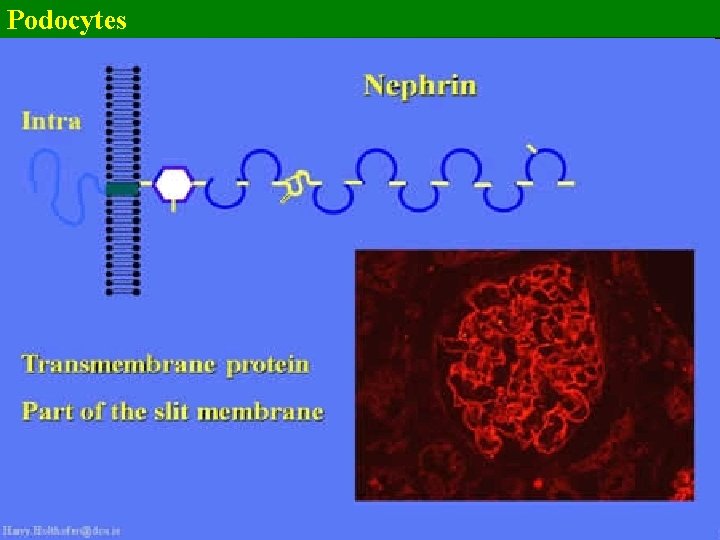
Podocytes Nephrin - neph-1, neph-2, filtrin, hemoglobulin group of molecules, an immunoglobulin family of cell adhesion proteins They are clustering together with podocin for the functionality of the slit diaphragm The nephrin molecules extend from neighbouring podocytes and foot processes and induce the interaction between the different podocyte foot processes Nephrin really forms the framework of the slit diaphragm
Podocytes The nephrin damage determines lack of normal foot processes and the filtration slit organisation Specific administration or generation of specific nephrin antibodies lead to proteinuria In diabetes and diabetic nephropathy there are found circulating anti-nephrin antibodies many months before the actual attack to the kidney
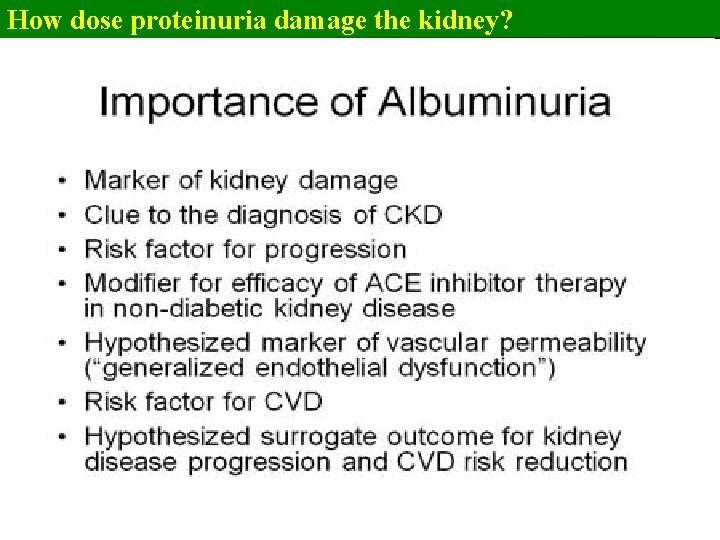
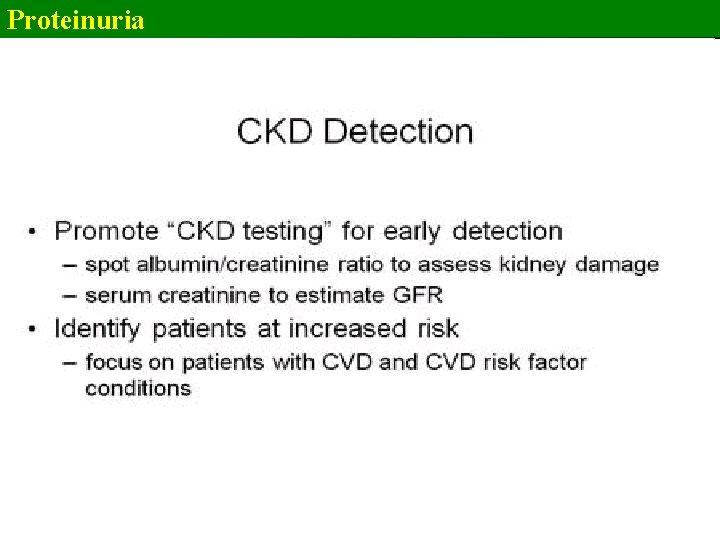
Proteinuria Microalbuminuria üan independent predictor of cardiovascular disease üan independent predictor all-cause mortality in both diabetic and ünondiabetic men and women üa stronger indicator future cardiovascular events than systolic BP or serum cholesterol Detecting microalbuminuria is an important screening tool to identify people üwho are at high risk for cardiovascular events and progression of kidney disease üwho need more intensive therapy compared with subjects with normal albumin excretion rates
Proteinuria According to the American Diabetes Association (ADA), the gold standard for measuring urine albumin excretion is a 24 -h urine collection A more convenient method to detect microalbuminuriais the albumin (g)/creatinine (mg) ratio (ACR) measured in a random urine specimen Currently, the National Kidney Foundation recommends the use of spot urine ACR obtained under standardized conditions (first voided, morning, midstream specimen) to detect microalbuminuria The ACR is a more convenient test for patients and may be less prone to errors due to improper collection methods and variations in 24 -h protein excretion compared with a random urine specimen
Proteinuria The ADA and the National Kidney Foundation define microalbuminuria as an ACR between 30 to 300 g/mg in both men and women
Proteinuria
Proteinuria
How dose proteinuria damage the kidney?
Proteinuria
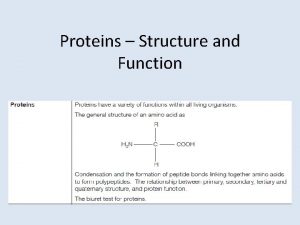
 Is defined as
Is defined as Function of plasma protein
Function of plasma protein Functions of plasma proteins
Functions of plasma proteins Upc idexx instructions
Upc idexx instructions Proteinuria overflow
Proteinuria overflow Reabsorbcia
Reabsorbcia Prerenal proteinuria
Prerenal proteinuria Proteinuria
Proteinuria Proteinuria
Proteinuria Blood plasma contents
Blood plasma contents Characteristics of lipids
Characteristics of lipids No there aren't
No there aren't Any to any connectivity
Any to any connectivity Seknder
Seknder Any living thing is called
Any living thing is called Venn diagram living and non living
Venn diagram living and non living Is a candle living or nonliving
Is a candle living or nonliving Living non living dead
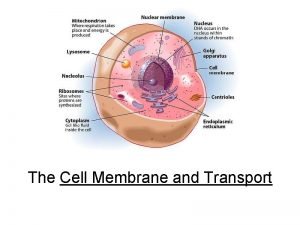
Living non living dead What is the smallest living unit in the body
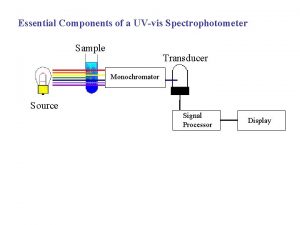
What is the smallest living unit in the body Components of spectrophotometer
Components of spectrophotometer 4 components of healthy active living
4 components of healthy active living Protein pump vs protein channel
Protein pump vs protein channel Globular vs fibrous proteins
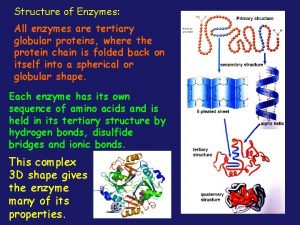
Globular vs fibrous proteins All enzymes are globular proteins
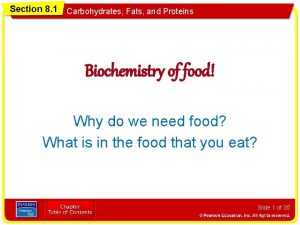
All enzymes are globular proteins Section 8-1 carbohydrates fats and proteins answer key
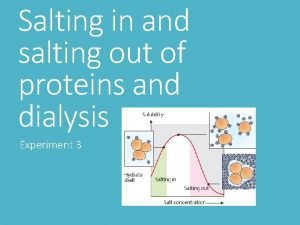
Section 8-1 carbohydrates fats and proteins answer key Salting in salting out
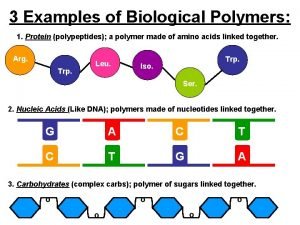
Salting in salting out Building blocks of protein
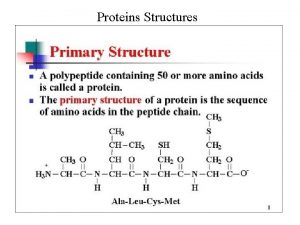
Building blocks of protein Qualitative test for protein
Qualitative test for protein What are derived proteins
What are derived proteins Protein monomers
Protein monomers Function of protein
Function of protein Protein metabolism notes
Protein metabolism notes Protein folding
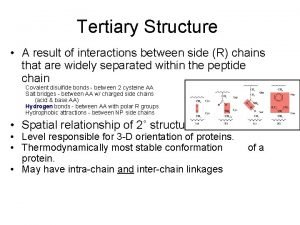
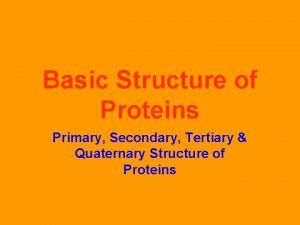
Protein folding Structure database in bioinformatics
Structure database in bioinformatics Quantitative determination of proteins
Quantitative determination of proteins Elementary composition of proteins
Elementary composition of proteins Glycoprotein vs glycolipid
Glycoprotein vs glycolipid Protein domains and motifs
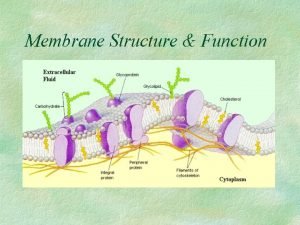
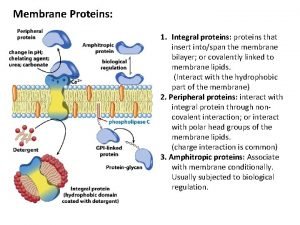
Protein domains and motifs Functions of membrane proteins
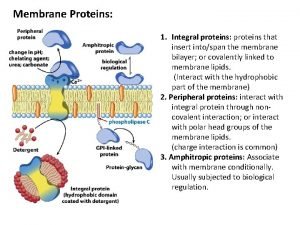
Functions of membrane proteins Integral proteins
Integral proteins Exocytosis definition biology
Exocytosis definition biology Precipitation of proteins by strong mineral acids
Precipitation of proteins by strong mineral acids Edman degradation
Edman degradation Fibrous protein collagen
Fibrous protein collagen Not all enzymes are proteins
Not all enzymes are proteins Electrophoretic mobility shift assay
Electrophoretic mobility shift assay Salt bridge amino acids
Salt bridge amino acids Higher order structure of proteins
Higher order structure of proteins Role of cholesterol in cell membrane
Role of cholesterol in cell membrane Membrane proteins functions
Membrane proteins functions Salting out proteins
Salting out proteins Biomedical importance of proteins
Biomedical importance of proteins Organic compounds such as proteins and starches are too
Organic compounds such as proteins and starches are too Primary secondary tertiary quaternary
Primary secondary tertiary quaternary Lbv foods
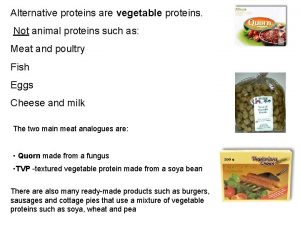
Lbv foods Three main types of rna
Three main types of rna Steroid hormones lipids
Steroid hormones lipids Section 8-1 summary carbohydrates fats and proteins
Section 8-1 summary carbohydrates fats and proteins Protein elements
Protein elements Integral proteins hydrophobic
Integral proteins hydrophobic Dna rna and proteins study guide answers
Dna rna and proteins study guide answers Functions and importance of proteins
Functions and importance of proteins Biological polymers examples
Biological polymers examples Which organelle prepares proteins for specific jobs
Which organelle prepares proteins for specific jobs Translation refers to:
Translation refers to: Protein hydrolysis
Protein hydrolysis Quantitative test for proteins
Quantitative test for proteins Amphoteric proteins
Amphoteric proteins Amphoteric proteins
Amphoteric proteins