PROTEINURIA IN CHILDREN HOW COMMON IS PROTEINURIA 5







































- Slides: 88
PROTEINURIA IN CHILDREN




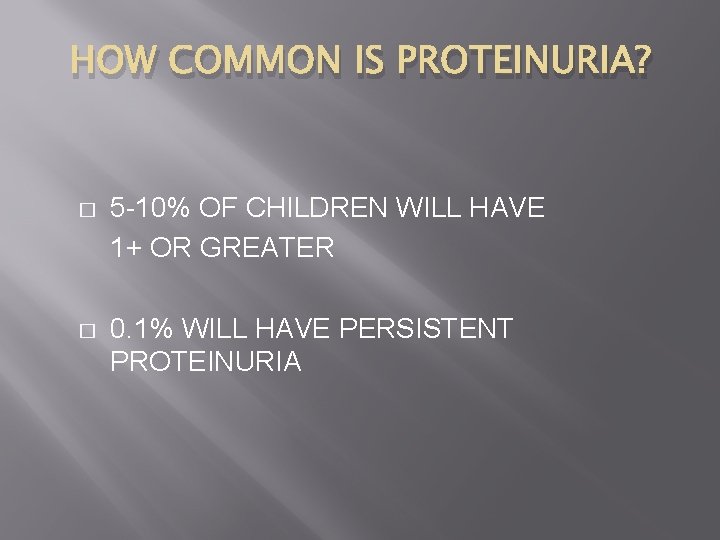
HOW COMMON IS PROTEINURIA? � 5 -10% OF CHILDREN WILL HAVE 1+ OR GREATER � 0. 1% WILL HAVE PERSISTENT PROTEINURIA
IS THE PROTEINURIA DANGEROUS? If the proteinuria is transient or orthostatic, it is benign.

MECHANISMS OF PROTEIN HANDLING BY KIDNEY � Glomerular capillary wall permits passage of small molecules while restricting macromolecules






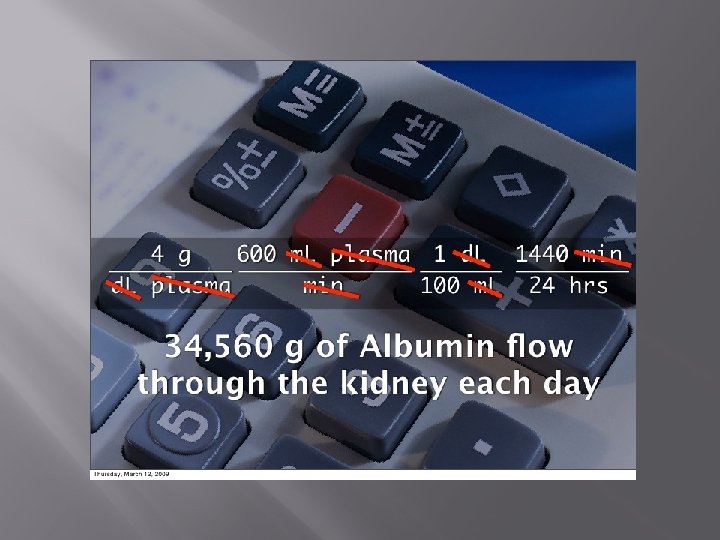


MECHANISMS OF PROTEIN HANDLING BY KIDNEY � � � Normal protein excretion affected by interplay of glomerular and tubular mechanisms Glomerular injury: abnormal losses of intermediate MW proteins like albumin Tubular damage: increased losses of low MW proteins

NORMAL PROTEIN EXCRETION � Normal protein excretion � Child: < 100 mg/m 2/day or 150 mg/day � Neonates: up to 300 mg/m 2
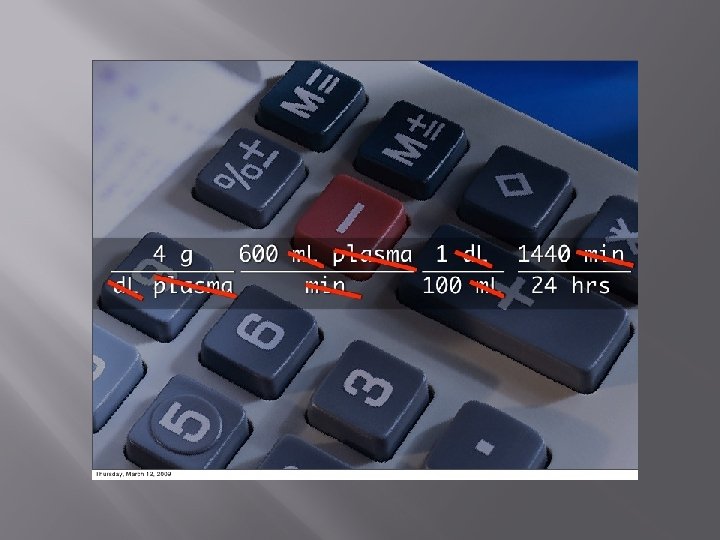
ABNORMAL PROTEIN EXCRETION � Urinary protein excretion in excess of 100 mg/m 2 per day or 4 mg/m 2 per hour � Nephrotic range proteinuria (heavy proteinuria) is defined as ≥ 1000 mg/m 2 per day or 40 mg/m 2 per hour.
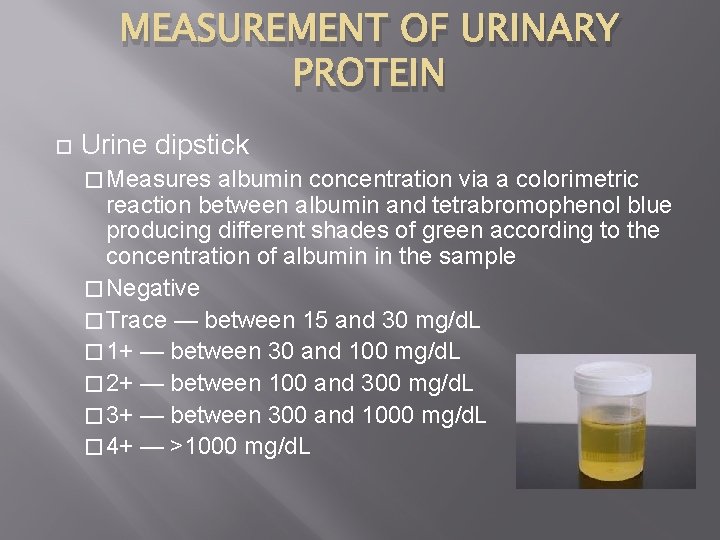
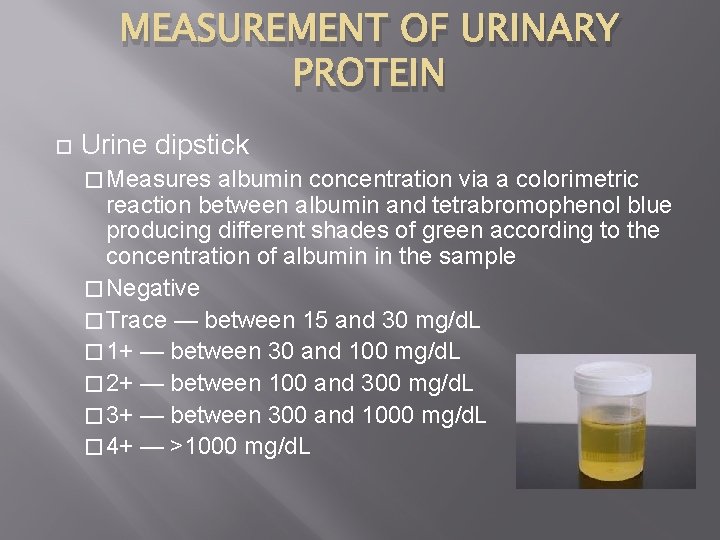
MEASUREMENT OF URINARY PROTEIN Urine dipstick � Measures albumin concentration via a colorimetric reaction between albumin and tetrabromophenol blue producing different shades of green according to the concentration of albumin in the sample � Negative � Trace — between 15 and 30 mg/d. L � 1+ — between 30 and 100 mg/d. L � 2+ — between 100 and 300 mg/d. L � 3+ — between 300 and 1000 mg/d. L � 4+ — >1000 mg/d. L
IS THE PROTEINURIA REAL? � Remember that the urine dipsticks only measure concentration. � Evaluate urine protein/Cr ratio on a spot urine sample (normal <0. 2) � 24 hour urine collection
MEASUREMENT OF URINARY PROTEIN � Quantitative assessment � Children with persistent dipstick-positive proteinuria must undergo a quantitative measurement of protein excretion, most commonly on a timed 24 -hour urine collection � In children: levels >100 mg/m 2 per day (or 4 mg/m 2 per hour) are abnormal � Proteinuria of greater than 40 mg/m 2 per hour is considered heavy or in the nephrotic range

ABNORMAL PROTEIN EXCRETION � Tubular proteinuria � Results from increased excretion of low molecular weight proteins such as beta-2 -microglobulin, alpha 1 -microglobulin, and retinol-binding protein � Tubulointerstitial diseases, can lead to increased excretion of these smaller proteins
ABNORMAL PROTEIN EXCRETION � Glomerular proteinuria � Due to increased filtration of macromolecules � May result from glomerular disease (most often minimal change disease) or from nonpathologic conditions such as fever, intensive exercise, and orthostatic (or postural) proteinuria

ABNORMAL PROTEIN EXCRETION � Overflow Proteinuria � Results from increased excretion of low molecular weight proteins due to marked overproduction of a particular protein to a level that exceeds tubular reabsorptive capacity

Classification of Proteinuria: Nonpathological Postural ( orthostatic) Febrile & Exercise-induced
TRANSIENT PROTEINURIA � � � Most common cause Can occur in association with fever, seizures, strenuous exercise, emotional stress, hypovolemia, extreme cold, epinephrine administration, abdominal surgery, or congestive heart failure Believed to be glomerular in origin, related to hemodynamic changes (decreased renal plasma flow) rather than altered permeability of capillary wall
ORTHOSTATIC PROTEINURIA � � Increase in protein excretion in the erect position compared with levels measured during recumbency Proteinuria usually does not exceed 1 -1. 5 gm/day Mechanism postulated to involve an increased permeability of the glomerular capillary wall and a decrease in renal plasma flow Long-term studies have documented the benign nature of this condition, with recorded normal renal function up to 50 years later
ORTHOSTATIC PROTEINURIA � � � Perform Orthostatic Test CBC BUN Creatinine Electrolytes 24 -hr urine excretion �< 1. 5 g/day repeat UA and blood work in 1 year � > 1. 5 g/day refer to Pediatric Nephrologist

Instructions for Testing for Orthostatic Proteinuria 1. 2. 3. 4. 5. 6. 7. Patient voids at bedtime. Discard urine. No food or fluids after dinner until the next morning. When patient awakes in the morning, urine specimen is collected prior to arising, or after as little ambulation as possible. Label specimen #1. Child should ambulate for the next 2 to 3 hours. Then collect specimen. Label specimen #2. Both specimens should be tested by dipstick or sulfosalicylic acid. Specimen #1 should be concentrated with a specific gravity of at least 1. 018. If specimen #1 is free of protein and specimen #2 has protein, then the test is positive for orthostatic proteinuria. If both specimens have protein, orthostatic proteinuria is unlikely and further evaluation is necessary. This protocol should be repeated on at least 2 occasions to confirm the diagnosis.
MANAGEMENT � � � Avoid excessive restrictions in child’s lifestyle Dietary protein supplementation is of no benefit Salt restriction unnecessary and potentially dangerous No indication for limitation of activity Importance of compliance with regular followup should be stressed
ASYMPTOMATIC PROTEINURIA � Levels of protein excretion above the upper limits of normal for age � No clinical manifestations such as edema, hematuria, oliguria, and hypertension
ASYMPTOMATIC PROTEINURIA: WHAT IT IS NOT. � It is absolutely not Minimal Change Nephrotic Syndrome � There is no indication for a steroid trial.
CAUSES OF ASYMPTOMATIC PROTEINURIA

DIFFERENTIAL DIAGNOSIS OF ASYMPTOMATIC PROTEINURIA � Focal Segmental Glomerulosclerosis � FSGS � � � Reflux Nephropathy Glomerulonephritis Systemic Lupus Erythematosis
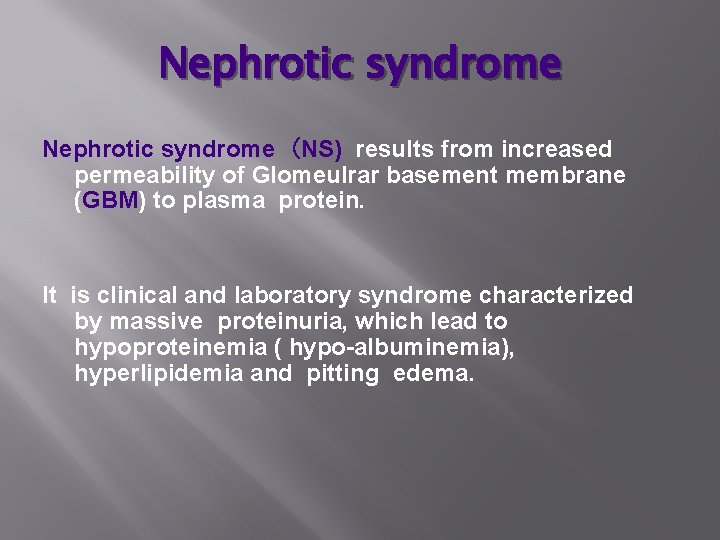
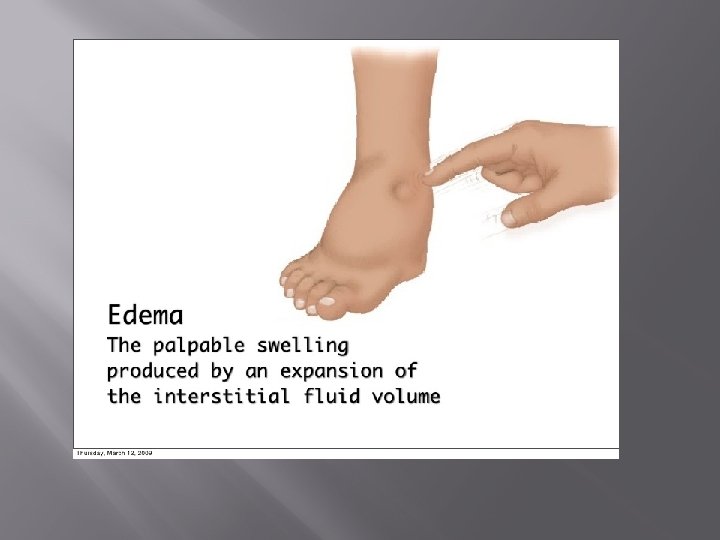
Nephrotic syndrome (NS) results from increased permeability of Glomeulrar basement membrane (GBM) to plasma protein. It is clinical and laboratory syndrome characterized by massive proteinuria, which lead to hypoproteinemia ( hypo-albuminemia), hyperlipidemia and pitting edema.

Nephrotic Criteria: *Massive proteinuria: qualitative proteinuria: 3+ or 4+, quantitative proteinuria : more than 40 mg/m 2/hr in children (selective). *Hypo-proteinemia : total plasma proteins < 5. 5 g/dl and serum albumin : < 2. 5 g/dl. *Hyperlipidemia: serum cholesterol : > 5. 7 mmol/L *Edema: pitting edema in different degree


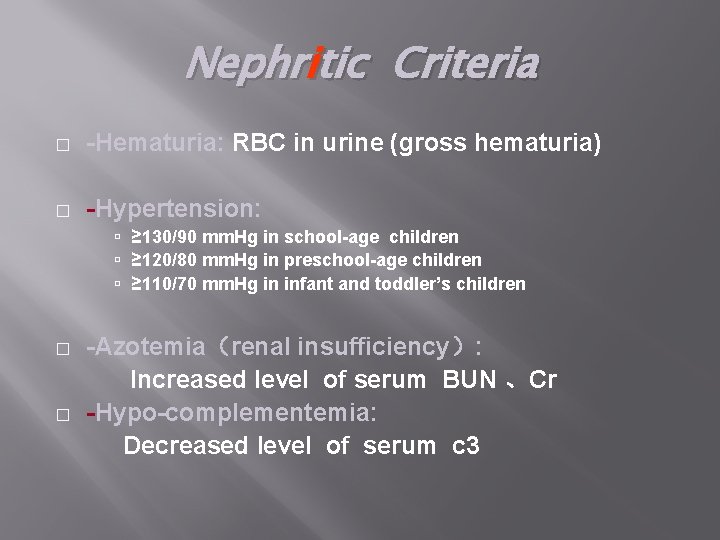
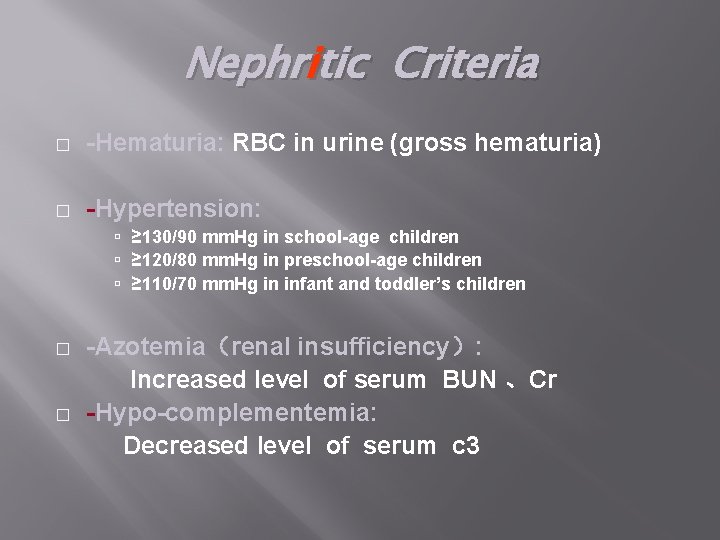
Nephritic Criteria � -Hematuria: RBC in urine (gross hematuria) � -Hypertension: ≥ 130/90 mm. Hg in school-age children ≥ 120/80 mm. Hg in preschool-age children ≥ 110/70 mm. Hg in infant and toddler’s children � � -Azotemia(renal insufficiency): Increased level of serum BUN 、Cr -Hypo-complementemia: Decreased level of serum c 3

� � Nephritis Frank haematuria Hypertension Low complement Non-nephrotic range proteinuria � � Nephrotic None or microscopic haematuria (20%) Normal BP Normal complement Nephrotic range proteinuria

Classification: � A-Primary Idiopathic NS (INS): majority The cause is still unclear up to now. Recent 10 years , increasing evidence has suggested that INS may result from a primary disorder of T– cell function. Accounting for 90% of NS in child. mainly discussed. B-Secondary NS: NS resulted from systemic diseases, such as anaphylactoid purpura , systemic lupus erythematosus, HBV infection. � C-Congenital NS: rare *1 st 3 monthe of life , only treatment renal transplantation �
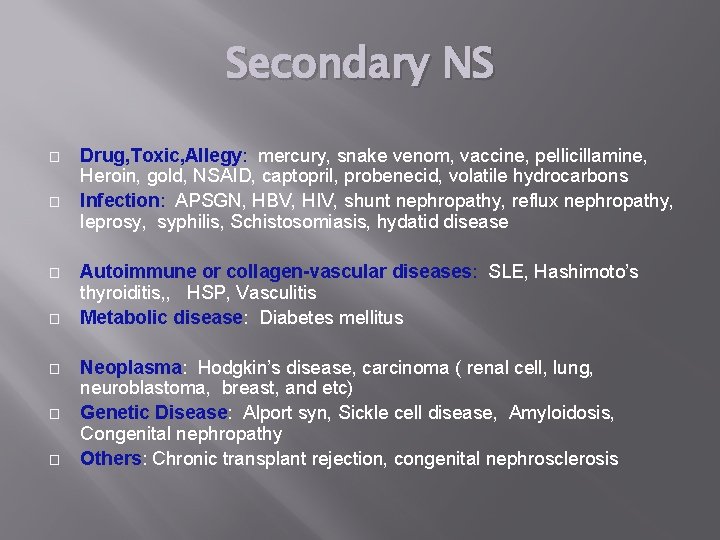
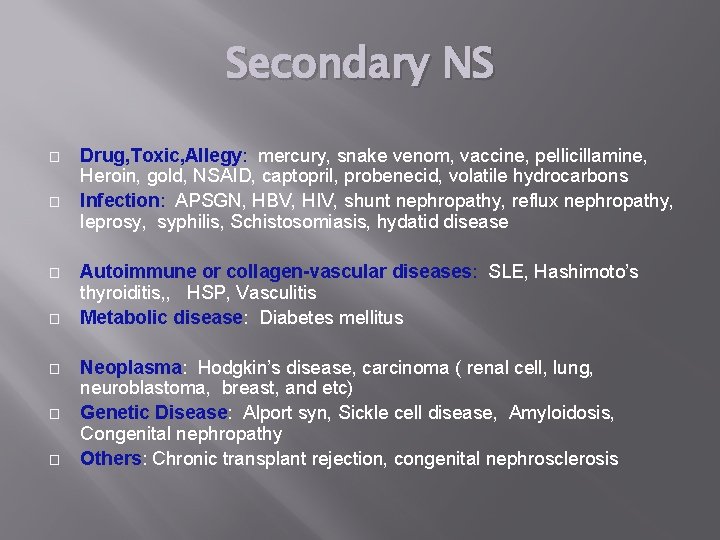
Secondary NS � � � � Drug, Toxic, Allegy: mercury, snake venom, vaccine, pellicillamine, Heroin, gold, NSAID, captopril, probenecid, volatile hydrocarbons Infection: APSGN, HBV, HIV, shunt nephropathy, reflux nephropathy, leprosy, syphilis, Schistosomiasis, hydatid disease Autoimmune or collagen-vascular diseases: SLE, Hashimoto’s thyroiditis, , HSP, Vasculitis Metabolic disease: Diabetes mellitus Neoplasma: Hodgkin’s disease, carcinoma ( renal cell, lung, neuroblastoma, breast, and etc) Genetic Disease: Alport syn, Sickle cell disease, Amyloidosis, Congenital nephropathy Others: Chronic transplant rejection, congenital nephrosclerosis
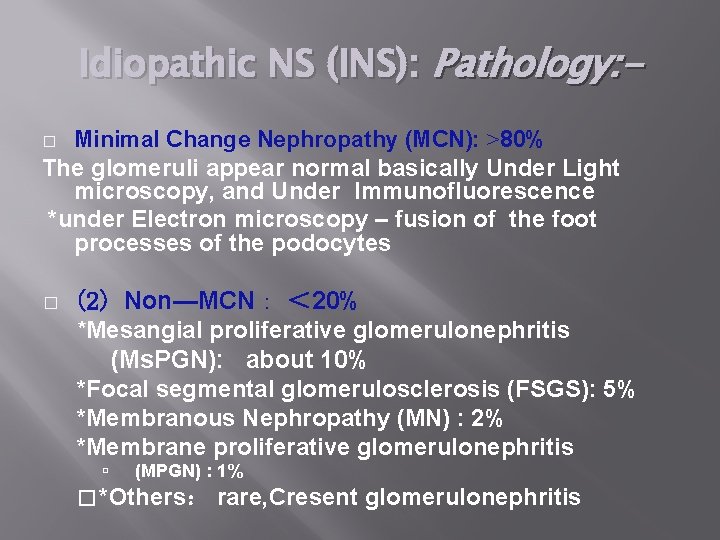
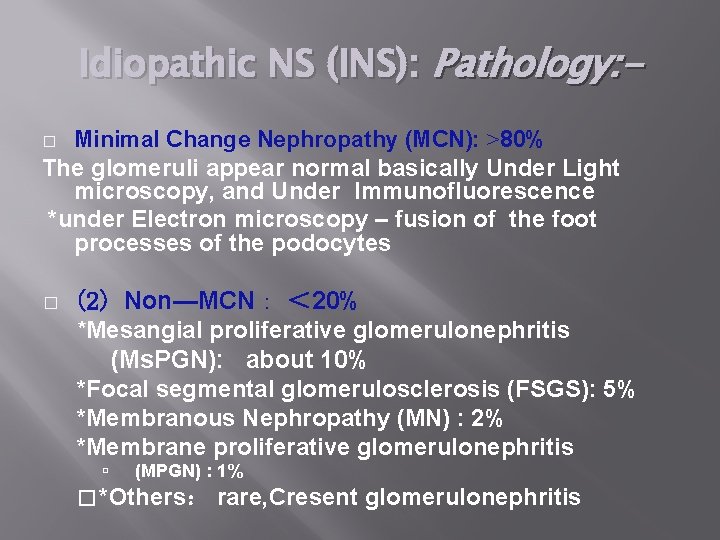
Idiopathic NS (INS): Pathology: Minimal Change Nephropathy (MCN): >80% The glomeruli appear normal basically Under Light microscopy, and Under Immunofluorescence *under Electron microscopy – fusion of the foot processes of the podocytes � � (2) Non—MCN: < 20% *Mesangial proliferative glomerulonephritis (Ms. PGN): about 10% *Focal segmental glomerulosclerosis (FSGS): 5% *Membranous Nephropathy (MN) : 2% *Membrane proliferative glomerulonephritis (MPGN) : 1% � *Others: rare, Cresent glomerulonephritis

� � � NB: - *Nephrotic syndrome is 15 times more common in children than in adults. *Most cases of primary nephrotic syndrome are in children and are due to minimal-change disease. The age at onset varies with the type of nephrotic syndrome.
WHAT GIVES YOU NEPHROTIC SYNDROME IN A TODDLER? � � � Minimal Change Disease Focal Segmental Glomerulosclerosis Membranous Membranoproliferative GN
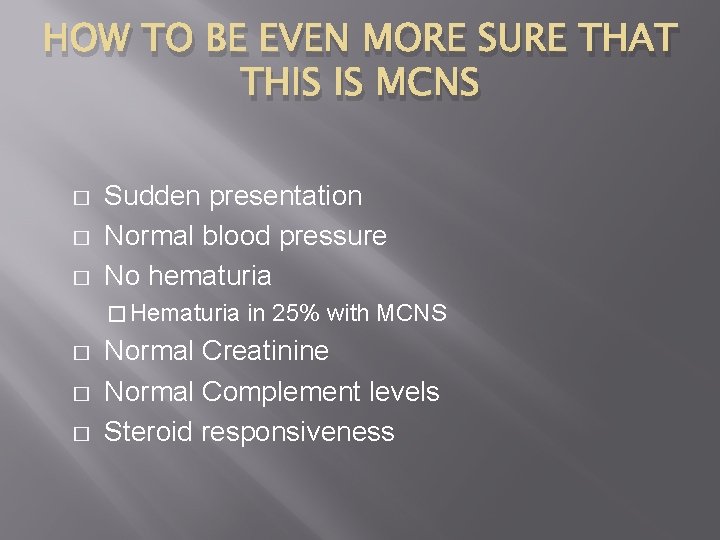
HOW TO BE EVEN MORE SURE THAT THIS IS MCNS � � � Sudden presentation Normal blood pressure No hematuria � Hematuria � � � in 25% with MCNS Normal Creatinine Normal Complement levels Steroid responsiveness
OTHER BLOOD WORK TO BE DONE AT PRESENTATION � � Complement levels ANA
IT IS NOT MINIMAL CHANGE DISEASE WHEN: � � Presentation as an infant Asymptomatic proteinuria Low complement levels Be suspicious in teenagers
SO WHAT IS MCNS? � � � Minimally altered glomerular structure Fusion of podocytes Profound proteinuria Steroid responsiveness Relapsing course Can be outgrown

Clinical Manifestation: IN MCNS , The male preponderance of 2: 1 : 1. Main manifestations: Edema (varying degrees) is the common symptom Local edema: edema in face , around eyes( Periorbital swelling) , in lower extremities. Generalized edema (anasarca), edema in penis and scrotum. 2 -Non-specific symptoms: Fatigue and lethargy loss of appetite, nausea and vomiting , abdominal pain , diarrhea body weight increase, urine output decrease pleural effusion (respiratory distress)

How many pathological types causes nephrotic syndrome?

Complications � � � Hypovalaemia Infection: peritonitis (pneumococci) Thrombosis
Complications of NS: 1 -Infections: Infections is a major complication in children with NS. It frequently trigger relapses. Nephrotic pt are liable to infection because : A-loss of immunoglobins in urine. B-the edema fluid act as a culture medium. C-use immunosuppressive agents. D- malnutrition The common infection : URI, peritonitis, cellulitis and UTI may be seen. Organisms: encapsulated (Pneumococci, H. influenzae), Gram negative (e. g E. coli

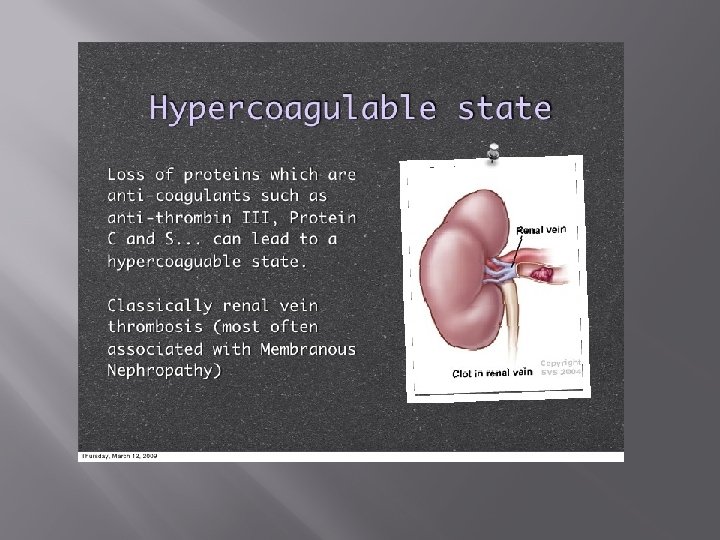
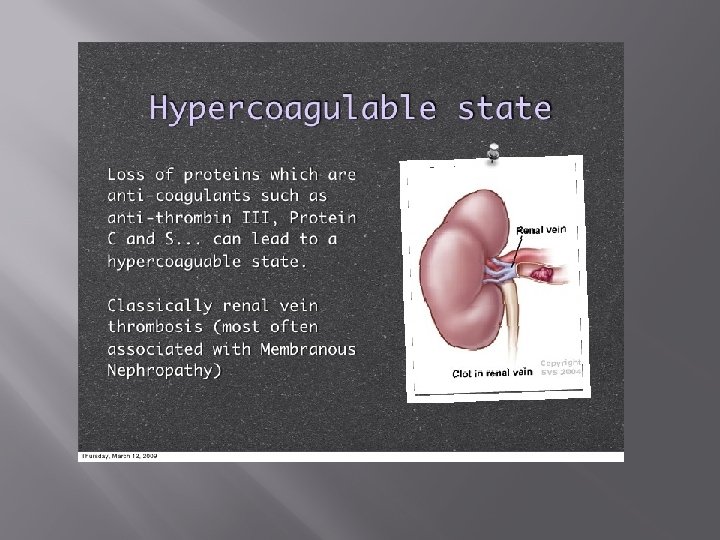
� 2 -Hypercoagulability (Thrombosis). Hypercoagulability …. . � � leading to venous or arterial thrombosis: Hypercoagulability in Nephrotic syndrome caused by: � 1 -Higher concentration of I, II, V, VIII, X and fibrinogen � 2 - Lower level of anticoagulant substance: antithrombin III � 3 -decrease fibrinolysis. � 4 -Higher blood viscosity � 5 - Increased platelet aggregation � 6 - Overaggressive diuresis
Management of NS: � General (non-specific ) � *Corticosteroid therapy
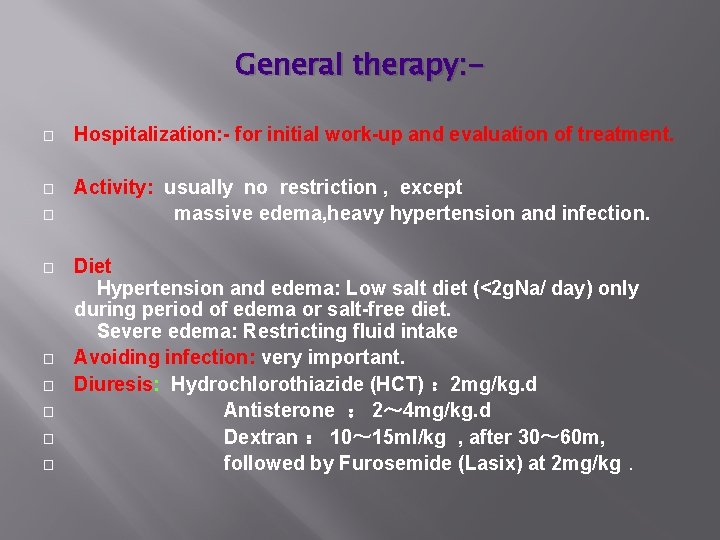
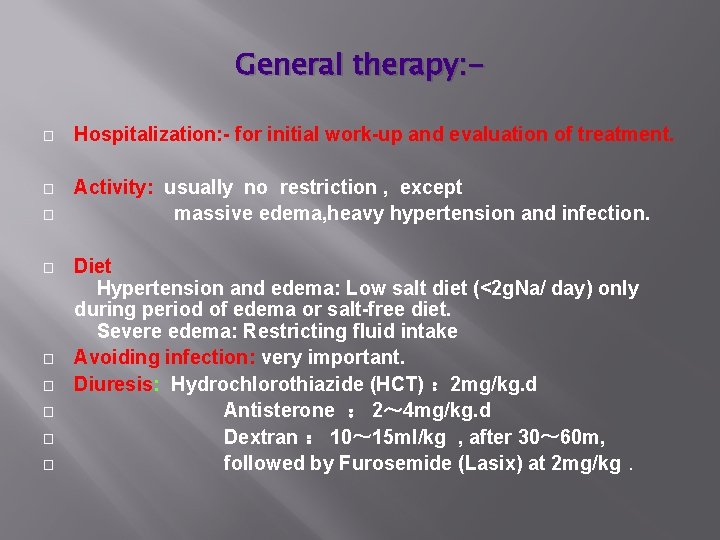
General therapy: � Hospitalization: - for initial work-up and evaluation of treatment. � Activity: usually no restriction , except massive edema, heavy hypertension and infection. � � � � Diet Hypertension and edema: Low salt diet (<2 g. Na/ day) only during period of edema or salt-free diet. Severe edema: Restricting fluid intake Avoiding infection: very important. Diuresis: Hydrochlorothiazide (HCT) : 2 mg/kg. d Antisterone : 2~ 4 mg/kg. d Dextran : 10~ 15 ml/kg , after 30~ 60 m, followed by Furosemide (Lasix) at 2 mg/kg.
NUTRITIONAL ADVICE � � � No added salt No fast food No food in little plastic packets

DIURETICS � Very tempting but potentially dangerous � Potentiates intravascular depletion � Increases risk of ATN � Increases risk of thrombosis
WHEN TO GIVE ALBUMIN AND LASIX � � � Peritonitis Pleural effusions Severe edema with skin breakdown/cellulitis
WHEN NOT TO GIVE ALUMIN AND LASIX � AESTHETIC PURPOSES
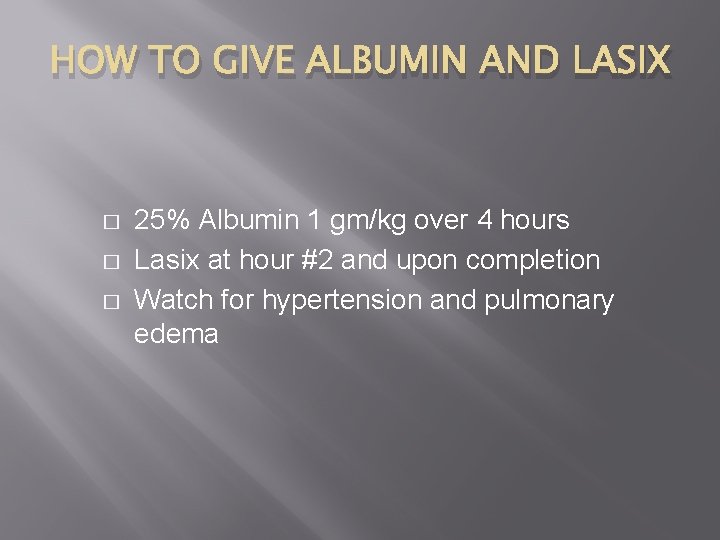
HOW TO GIVE ALBUMIN AND LASIX � � � 25% Albumin 1 gm/kg over 4 hours Lasix at hour #2 and upon completion Watch for hypertension and pulmonary edema
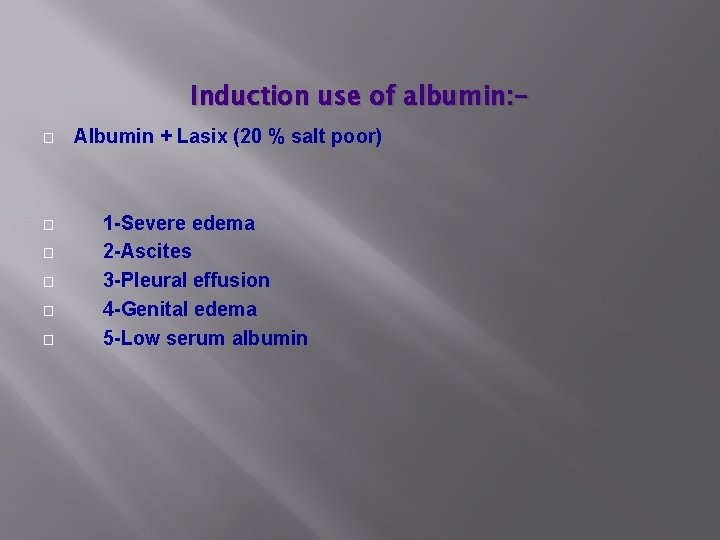
Induction use of albumin: � � � Albumin + Lasix (20 % salt poor) 1 -Severe edema 2 -Ascites 3 -Pleural effusion 4 -Genital edema 5 -Low serum albumin
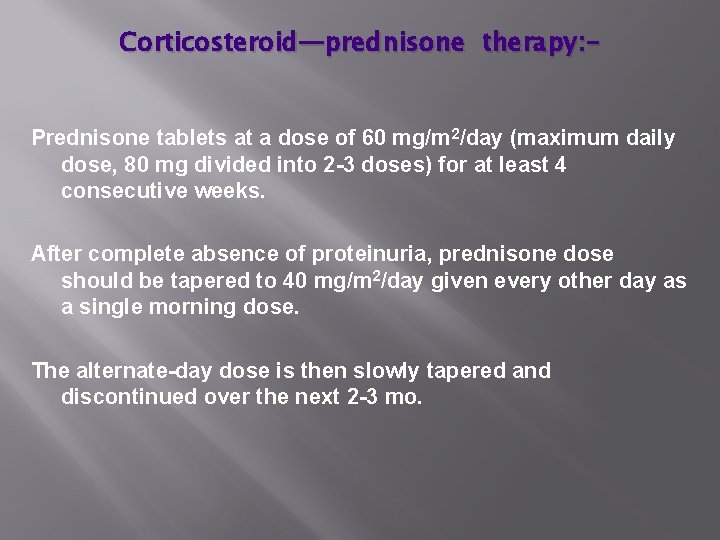
Corticosteroid—prednisone therapy: Prednisone tablets at a dose of 60 mg/m 2/day (maximum daily dose, 80 mg divided into 2 -3 doses) for at least 4 consecutive weeks. After complete absence of proteinuria, prednisone dose should be tapered to 40 mg/m 2/day given every other day as a single morning dose. The alternate-day dose is then slowly tapered and discontinued over the next 2 -3 mo.
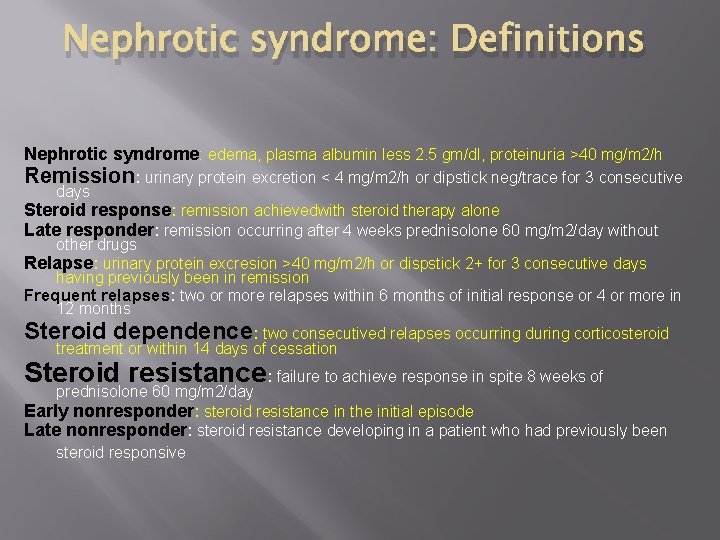
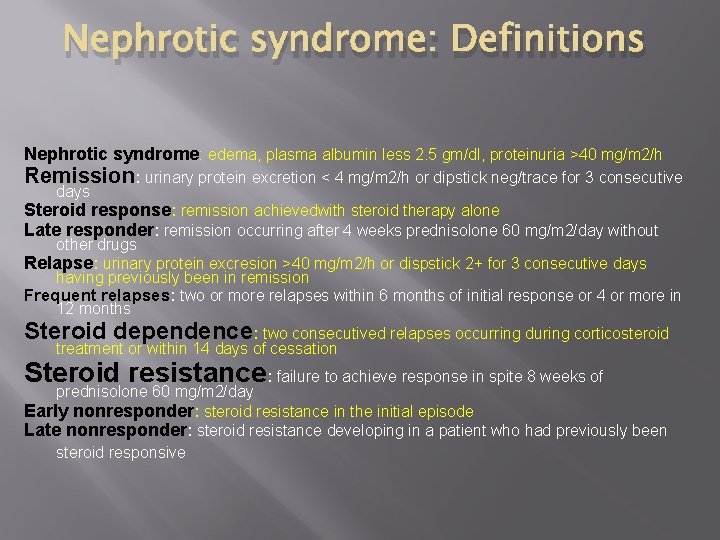
Nephrotic syndrome: Definitions Nephrotic syndrome: edema, plasma albumin less 2. 5 gm/dl, proteinuria >40 mg/m 2/h Remission: urinary protein excretion < 4 mg/m 2/h or dipstick neg/trace for 3 consecutive days Steroid response: remission achievedwith steroid therapy alone Late responder: remission occurring after 4 weeks prednisolone 60 mg/m 2/day without other drugs Relapse: urinary protein excresion >40 mg/m 2/h or dispstick 2+ for 3 consecutive days having previously been in remission Frequent relapses: two or more relapses within 6 months of initial response or 4 or more in 12 months Steroid dependence: two consecutived relapses occurring during corticosteroid treatment or within 14 days of cessation Steroid resistance: failure to achieve response in spite 8 weeks of prednisolone 60 mg/m 2/day Early nonresponder: steroid resistance in the initial episode Late nonresponder: steroid resistance developing in a patient who had previously been steroid responsive

Treatment of relapse in NS: Many children with nephrotic syndrome will experience at least 1 relapse (3 -4+proteinuria plus edema). daily divided-dose prednisone at the doses noted earlier (where he has the relapse) until the child enters remission (urine trace or negative for protein for 3 consecutive days). The pred-nisone dose is then changed to alternate-day dosing and tapered over 1 -2 mo.
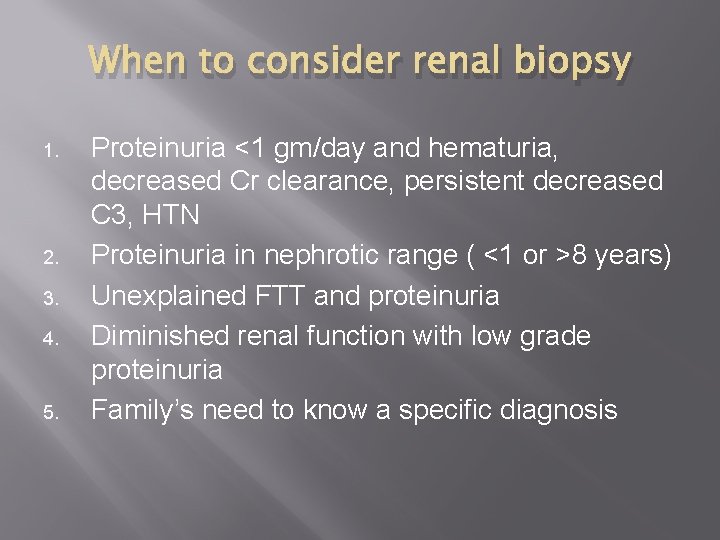
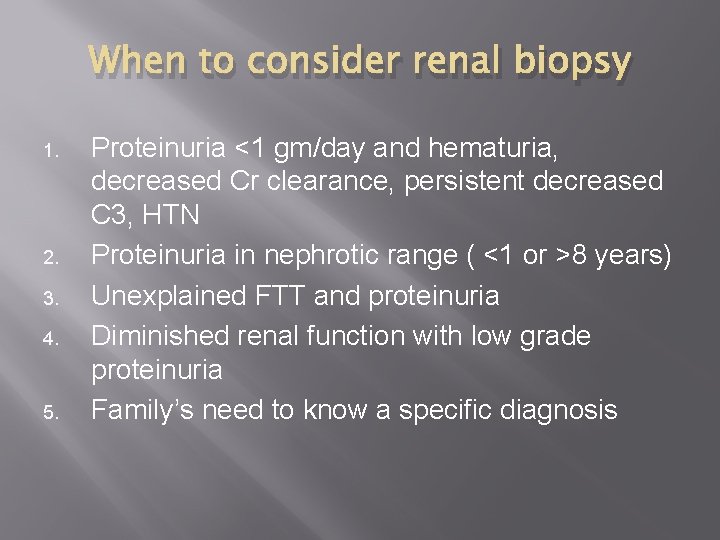
When to consider renal biopsy 1. 2. 3. 4. 5. Proteinuria <1 gm/day and hematuria, decreased Cr clearance, persistent decreased C 3, HTN Proteinuria in nephrotic range ( <1 or >8 years) Unexplained FTT and proteinuria Diminished renal function with low grade proteinuria Family’s need to know a specific diagnosis
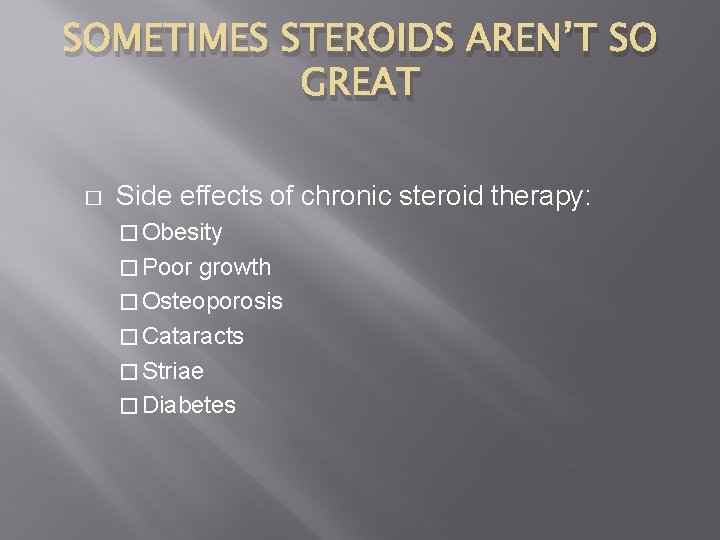
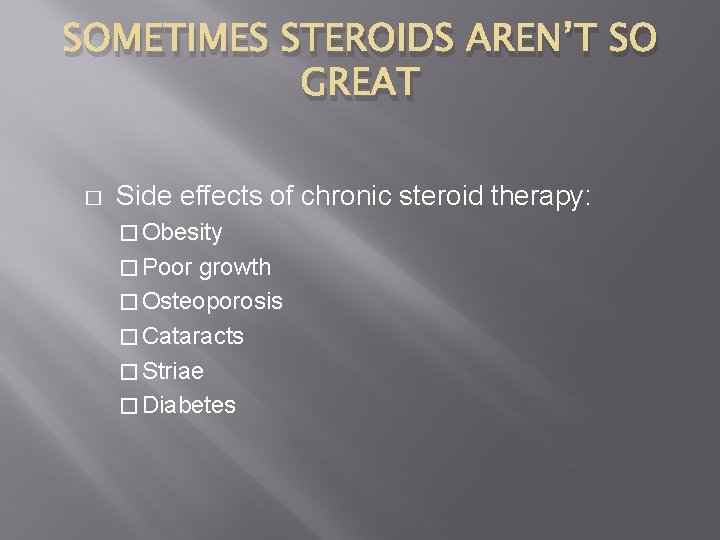
SOMETIMES STEROIDS AREN’T SO GREAT � Side effects of chronic steroid therapy: � Obesity � Poor growth � Osteoporosis � Cataracts � Striae � Diabetes
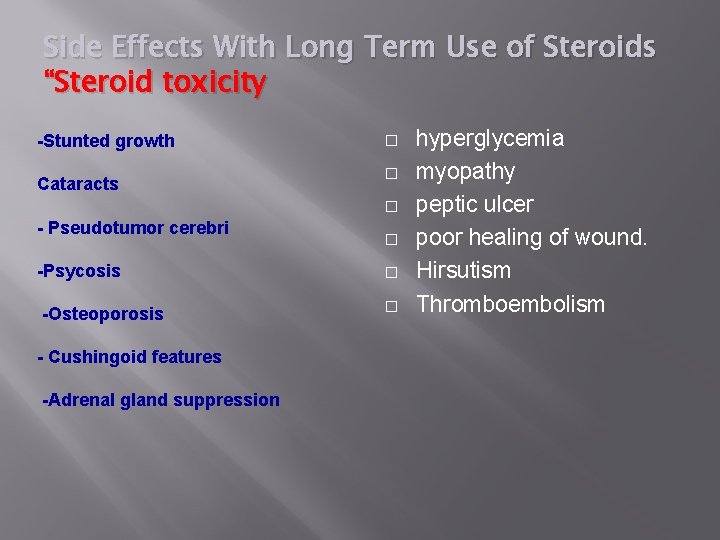
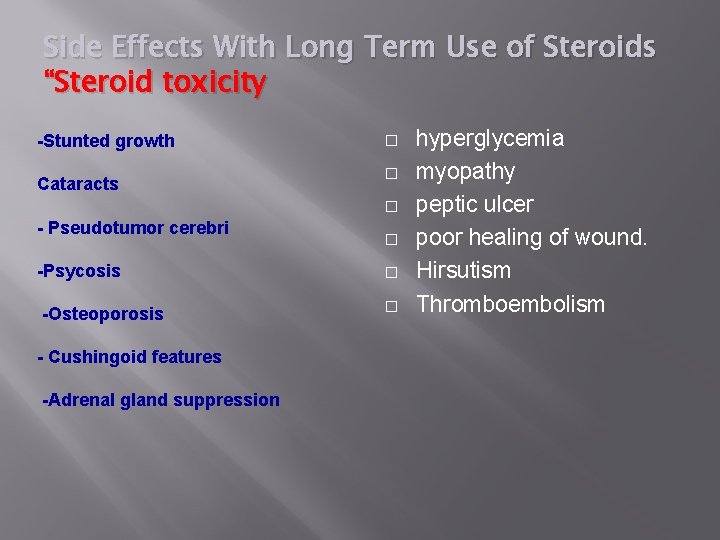
Side Effects With Long Term Use of Steroids “Steroid toxicity -Stunted growth Cataracts � � � - Pseudotumor cerebri -Psycosis -Osteoporosis - Cushingoid features -Adrenal gland suppression � � � hyperglycemia myopathy peptic ulcer poor healing of wound. Hirsutism Thromboembolism

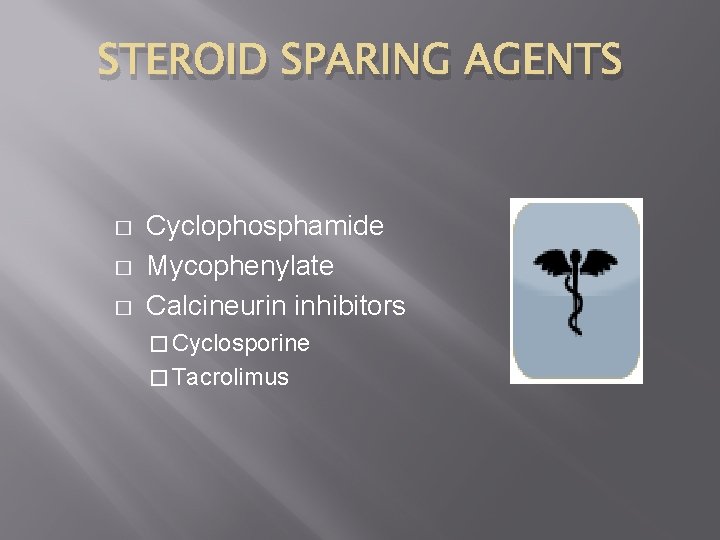
WHEN GOOD STEROIDS GO BAD � When excessive steroids are required to control nephrosis, consider a steroid sparing agent. � Don’t need to wait for development of steroid side effects.

STEROID SPARING AGENTS � � � Cyclophosphamide Mycophenylate Calcineurin inhibitors � Cyclosporine � Tacrolimus
Alternative agent: � � When can be used: Steroid-dependent patients, frequent relapsers, and steroid-resistant patients. � Cyclophosphamide Pulse steroids � Cyclosporin A � Tacrolimus � Microphenolate

NEPHROTIC SYNDROME IN CHILDREN IS CHANGING � � � Incidence of FSGS is on the rise Dramatic increase of around 300% since the 1960’s FSGS is much more prevalent in African Americans

FOCAL SEGMENTAL GLOMERULOSCLEROSIS � � Histologic Diagnosis More likely to be steroid resistant May present as asymptomatic proteinuria Higher chance of progression to renal failure

INCREASED INCIDENCE OF FSGS ? ? Related to the obesity epidemic? ? Obesity induced FSGS Hypertension induced FSGS



 Proteinuria overflow
Proteinuria overflow Fenestras
Fenestras Reabsorbcia
Reabsorbcia Prerenal proteinuria
Prerenal proteinuria Idexx upc
Idexx upc Proteinuria
Proteinuria Factors of 72
Factors of 72 What are the factors for 54
What are the factors for 54 Factors and multiples of 42
Factors and multiples of 42 Multiples of 18 and 24
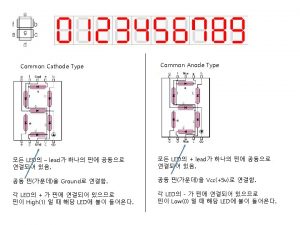
Multiples of 18 and 24 Common anode and common cathode
Common anode and common cathode Highest common factors and lowest common multiples
Highest common factors and lowest common multiples 2 chronicles 34 children's lesson
2 chronicles 34 children's lesson Kabc-ii
Kabc-ii Sos village multan
Sos village multan Happy children images
Happy children images Woodview children's home nottingham
Woodview children's home nottingham Children groups
Children groups Unit 10 caring for children and young people
Unit 10 caring for children and young people Adam and eve genealogy tree
Adam and eve genealogy tree Who is this
Who is this How to make your child mind without losing yours
How to make your child mind without losing yours Glory glory hallelujah he reigns
Glory glory hallelujah he reigns Basic life support sequence
Basic life support sequence Gordon lightfoot ethnicity
Gordon lightfoot ethnicity Council for the welfare of children
Council for the welfare of children Eris goddess family tree
Eris goddess family tree Children playing
Children playing National children's science congress projects ideas
National children's science congress projects ideas Vital signs normal range pediatrics
Vital signs normal range pediatrics Children's dyslexia center
Children's dyslexia center Alkaline phosphatase: normal range by age
Alkaline phosphatase: normal range by age International accepted rights of the child
International accepted rights of the child Lorain county cps
Lorain county cps Eatwell guide children
Eatwell guide children Jasmine toguchi mochi queen vocabulary
Jasmine toguchi mochi queen vocabulary Street children in latin america
Street children in latin america Children tend to learn english
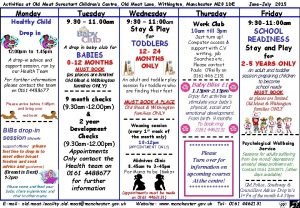
Children tend to learn english Old moat sure start
Old moat sure start National agencies related to child welfare
National agencies related to child welfare Children are made readers on the laps of their parents
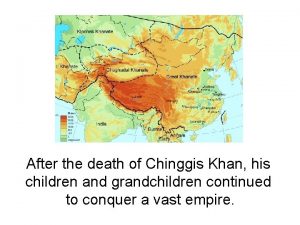
Children are made readers on the laps of their parents Genghis khan grandchildren
Genghis khan grandchildren Brand internalization
Brand internalization 4 sons
4 sons Nikola tesla brother
Nikola tesla brother Persepolis discussion questions by chapter
Persepolis discussion questions by chapter Teaching children joy
Teaching children joy Colorado childrens book award
Colorado childrens book award Act for children with autism and emotional challenges
Act for children with autism and emotional challenges Oh my children
Oh my children Working with young children/answer key chapter 1
Working with young children/answer key chapter 1 Exceptional children 10th edition
Exceptional children 10th edition Genitiv artikel
Genitiv artikel Section 47 children's act 1989
Section 47 children's act 1989 Joe tinning today
Joe tinning today Jacob's children's names in order
Jacob's children's names in order Eph 6:1-2
Eph 6:1-2 Macbeth children's book project
Macbeth children's book project Muddy children puzzle
Muddy children puzzle Children's mental health
Children's mental health My dearest children
My dearest children Socially maladjusted vs emotional disturbance
Socially maladjusted vs emotional disturbance Lisa arthey children's services
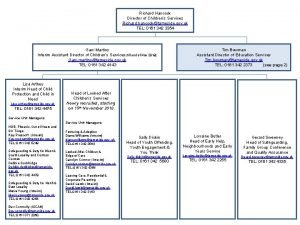
Lisa arthey children's services Sino ang di sakop sa republic act 10666
Sino ang di sakop sa republic act 10666 Dear children
Dear children Do children learn through correction and reinforcement?
Do children learn through correction and reinforcement? Beverly cleary awards
Beverly cleary awards Cycle safety for children
Cycle safety for children Welcome dear children
Welcome dear children Rct children's services
Rct children's services Causes of abdominal pain in children
Causes of abdominal pain in children Where did the children go to play every afternoon?
Where did the children go to play every afternoon? Week by week plans for documenting children's development
Week by week plans for documenting children's development According to jean piaget children cease to exhibit
According to jean piaget children cease to exhibit Arthur davison
Arthur davison To its plans children
To its plans children Colonial children's games
Colonial children's games Unlike b.f. skinner, noam chomsky believes that children
Unlike b.f. skinner, noam chomsky believes that children I grow strong by eating
I grow strong by eating Pictograms for children
Pictograms for children Vital sign ped
Vital sign ped Nj children's system of care
Nj children's system of care Charlie and the chocolate factory chapter 14
Charlie and the chocolate factory chapter 14 He is the child prodigy and composer of requime
He is the child prodigy and composer of requime Infants, children, and adolescents 8th edition
Infants, children, and adolescents 8th edition Internationally accepted rights of the child
Internationally accepted rights of the child Jesus said let the little ones come to me
Jesus said let the little ones come to me Signs of schizophrenia in children
Signs of schizophrenia in children I stand here ironing theme
I stand here ironing theme