Preparing for life events Advance Care Planning Options

- Slides: 60
Preparing for life events: Advance Care Planning Options in South Dakota National Active and Retired Federal Employees Karen Jensen, NARFE Chapter 0201 Membership Chair, South Dakota Federation Service Officer, Retired RN
What is Advance Care Planning? Making decisions about the care you want to receive if you are unable to speak for yourself Your decisions to make, decisions based on your personal values, preferences, and discussions with your loved ones
Why is Advanced Care Planning important? Helps people to make their wishes known upfront about any future medical treatment and care, should they become unable to voice their needs at that point. It involves appointing a substitute decision-maker Particularly important for those people who are older, are frail, or who have a chronic illness, multiple diseases, an early cognitive impairment, or are approaching their end of life.
What is an Advance Directive? Advance medical directives are legal forms that allow you to state your health care wishes, in the event you are unable to do so. The two most common types of advance directives are: o the durable power of attorney for health care o the living will.
Durable Power of Attorney for Health Care and Living Will Durable Power of Attorney for Health Care- Appoints someone to speak for you when you are no longer able to direct your care. If you improve and are able to speak for yourself, then you resume the ability to direct your care. A Living Will-Directs what treatment to provide or withhold when you are terminally ill or death is imminent, or if you are permanently unconscious. It only becomes effective when you are no longer able to speak for yourself. If you signed a durable power of attorney for health care before July 1, 1990, or if you signed a living will before July 1, 1991, you should have your document reviewed to make certain that it meets current requirements.
Differences in DPOA for Health care and Living Will • According to SDCL 34 -12 D Living Will-A competent adult can execute declaration regarding withholding or withdrawing life-sustaining treatment. The living will declaration becomes operative when the declarant is determined by the attending physician to be in a terminal condition, death is imminent, and the declarant is no longer able to communicate decisions about medical care
SDCL 34 -12 D Living Will • Document can be completed with 2 witnesses and optional notary public. • States preferences on receiving artificial nutrition and hydration. If not stated, provision of these is governed by law of the state. • Can be revoked any time by person who executed document, but cannot be overridden by surrogate • Doesn’t require mental capacity to revoke • Doesn’t need written documentation with patient signature • Medical provider documentation needed
Differences in DPOA for Health Care and Living Will According to SDCL 59 -7 A Durable Power of Attorney for Health Care that is established by a competent person, does not become operative until incapacity in decision making is determined by a physician.
SDCL 59 -7 A Durable Power of Attorney for Health Care • The attorney in fact or agent may NOT make a health care decision if attending physician has determined in good faith that the principal has decision making capacity. Attending physician may also proceed as if the agent or attorney in fact is unavailable or refuses to make a health care decision. • To execute the form, it must be signed by the principal or in the principal’s conscious presence by another individual directed by the principal to sign the principal’s name on the Power of Attorney. The signature MUST be witnessed by two other adult individuals or by a notary public.
Competency versus Capacity is a person’s ability to make an informed decision Competency determination is a judicial finding made by the court A physician can declare (state as one’s opinion) as to patient capacity, but cannot determine competency Adults are presumed to have capacity, unless determined by the court
Addressing Artificial Nutrition and Hydration under POA SDCL-59 -7 -2. 7 Comfort care required--Conditions for withdrawal of artificial nutrition or hydration. The attorney-in-fact or agent may not authorize the withholding or withdrawal of comfort care from the principal. The attorney-in-fact or agent may authorize that artificial nutrition or hydration be withheld or withdrawn if one or more of the following exist:
Conditions for withdrawal of artificial nutrition or hydration (1) Artificial nutrition or hydration is not needed for comfort care or the relief of pain and the attending physician reasonably believes that the principal's death is imminent; or (2) Artificial nutrition or hydration cannot be physically assimilated (taken in) by the principal; or (3) The burden of providing artificial nutrition or hydration outweighs its benefit, provided that the determination of burden refers to the provision of artificial nutrition or hydration itself and not to the quality of the continued life of the principal;
Conditions for withdrawal of artificial nutrition or hydration (4) There is clear and convincing evidence that the principal expressed the desire that artificial nutrition or hydration be withheld, or refused artificial nutrition or hydration prior to the loss of decisional capacity; or (5) The principal expressed in the document creating the power of attorney that artificial nutrition or hydration be withheld; or (6) The principal expressly authorized, in the writing creating the power of attorney, the attorney-in-fact or agent to direct the withholding of artificial nutrition or hydration
Palliative Care or Hospice? They are not the same Palliative care-A specialized medical care that focuses on providing patients relief from pain and other symptoms of a serious illness, no matter the diagnosis or stage of the disease. Hospice care- A specialized medical care for people who are nearing the end of life. Services provided by a team who maximize comfort for a person who is terminally ill, by reducing pain and addressing physical, psychological, social and spiritual needs.
Palliative Care or Hospice (continued) Hospice Individual with life expectancy of 6 months or less (Medicare definition) Requires individual have a terminal prognosis Curative treatment no longer beneficial Provided in most care settings (i. e. hospital inpatient levels of care only, no Long Term Care Acute or Clinic facility) All costs related to terminal diagnosis covered by Medicare/Medicaid Hospice Benefit. Some may not be covered under Benefit
Palliative Care or Hospice (continued) Palliative Care Not time limited re: life expectancy Any individual with a serious illness Often still pursuing curative treatment Provided in any care setting Covered through Medicare Part B/Medicaid (some treatments/meds may not be covered, or have co-pay from private insurance)
What Would You Want? Most People With A Serious Life-limiting Illness Want To Be: At Home With Loved Ones Free From Pain and Suffering In Control of Their Care
The Reality Is… § Many People in The Last Year of Life Experience Unwanted and Often Unnecessary Hospitalizations § Many People are Only Referred to Hospice Services in The Final Hours or Days of Life, if Ever. § The Majority of People, Even Those Who are Seriously Ill, Haven’t Talked About or Documented Their Wishes
Why this Happens End of Life Is Treated as A Medical Moment Instead of A Human Experience People Avoid Talking About End of Life Even if They Do Talk About It, Very Few People Write Down Their Wishes
Various Options to Express What YOU Want Five Wishes Comfort One SD MOST
FIVE WISHES Easy To Use, Written in Everyday Language Promotes Peace of Mind for Your Family Lets People Know What You Want Lets You Express Personal, Emotional, and Spiritual Needs Along with Medical Wishes
Wish 1 The Person You Want To Make Health Care Decisions For You When You Can’t Known as the Health Care Agent Allows for up to 2 Alternates if Your Agent is Unable or Unwilling
Wish 2 The Kind Of Medical Treatment You Want Or Don’t Want Instructions for Pain Control and Life Support Allows for Different Wishes in Different Situations Examples of Life Support are Provided Space for You To Write Instructions Based on Your Personal Beliefs
Wish 3 How Comfortable You Want To Be Expresses Your Choices for Types of Comfort Care Allows You To Cross Out or Keep Items Based on Your Choices
Wish 4 How You Want People To Treat You Things Your Caregivers and Family Should Know About How To Support You, Including if You wish To Die at Home Types of Things People Can Do for You, Including Prayers, Visits, Placing Pictures of Family in Your Room, and Holding Your Hand
Wish 5 What You Want Your Loved Ones To Know Share Your Thoughts with Family Offer Love and Forgiveness to Those Who Have Hurt You Ask Forgiveness for Times You Have Hurt Others Communicate Practical Matters Such As Preferences for Memorial or Burial, or Arrangements For Donating Your Body to Science
Five Wishes Booklet https: //agingwithdignity. org
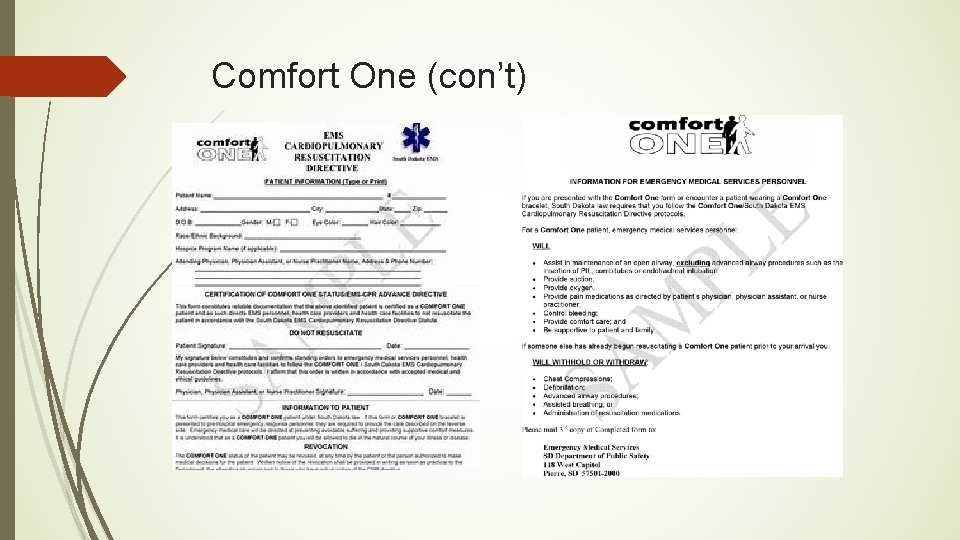
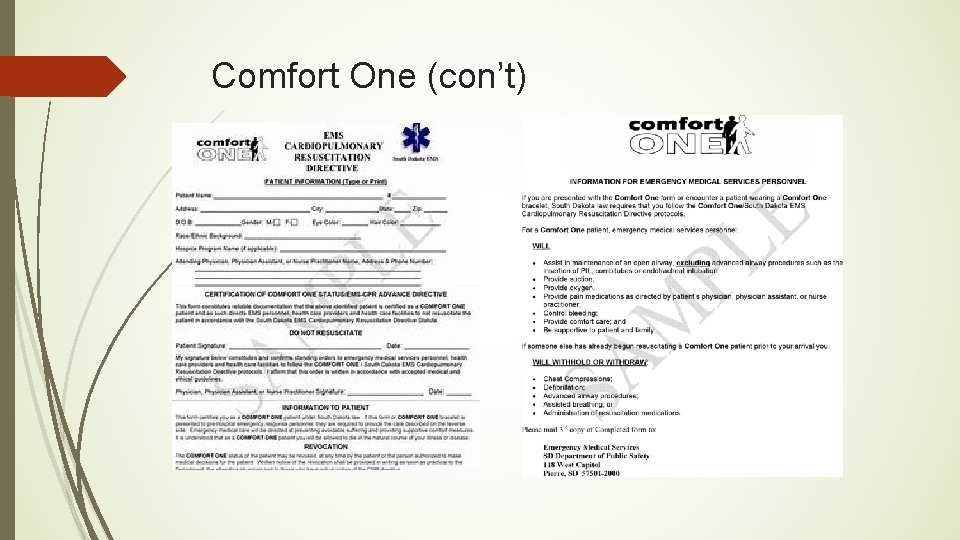
Comfort One In South Dakota it provides quick identification of patients who choose not to receive life-prolonging treatment (chest compressions, breathing tubes, shock, and so on) Patients have a special document and/or wear a special bracelet that states their requests, which indicates emergency personnel should only provide comfort measures. The Comfort One form must be signed by your physician, nurse practitioner, or physician assistant.
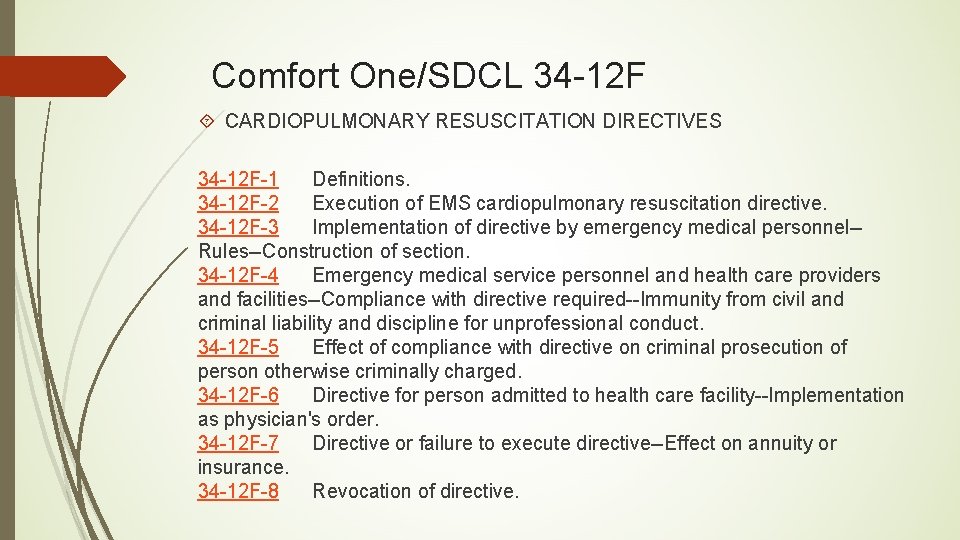
Comfort One/SDCL 34 -12 F CARDIOPULMONARY RESUSCITATION DIRECTIVES 34 -12 F-1 Definitions. 34 -12 F-2 Execution of EMS cardiopulmonary resuscitation directive. 34 -12 F-3 Implementation of directive by emergency medical personnel-Rules--Construction of section. 34 -12 F-4 Emergency medical service personnel and health care providers and facilities--Compliance with directive required--Immunity from civil and criminal liability and discipline for unprofessional conduct. 34 -12 F-5 Effect of compliance with directive on criminal prosecution of person otherwise criminally charged. 34 -12 F-6 Directive for person admitted to health care facility--Implementation as physician's order. 34 -12 F-7 Directive or failure to execute directive--Effect on annuity or insurance. 34 -12 F-8 Revocation of directive.

Comfort One (con’t) Comfort One can be put into effect by patient or person acting as their surrogate decision maker It becomes operative when necessary in the future Done with the informed consent of the patient or surrogate decision maker Executed process includes signature of the patient and Physician (or Physician’s Assistant or Nurse Practitioner, who are acting as agents of supervising physician as needed. Nurse practitioners in South Dakota are not required to practice under the supervision of a licensed physician once they have completed 1040 hours of clinical experience of supervised practice. ) It can be revoked by the patient, POA agent or authorized surrogate
Comfort One (con’t) Comfort One has the option to purchase a bracelet, cost is $36. 25, to signify that Comfort One form has been completed. Is a “portable” document that Emergency Medical Personnel and health care providers and facilities can utilize as a cardiopulmonary resuscitation directive which should be complied with as such. Comfort One is useful for the home care patient who desires no resuscitation at the end of life. The only intervention, would be to provide only comfort measures by Emergency Medical Personnel. These interventions would include to maintain open airway, suction, oxygen, pain medication as directed by medical personnel, or control bleeding. Be Supportive to the patient and the family
Comfort One (con’t)
Many Names for POLST/MOST Document Nebraska-NETO-Nebraska Emergency Treatment Orders North Dakota- POLST-Physician Orders for Life-Sustaining Treatment Minnesota-POLST-Provider Orders For Life Sustaining Treatment Iowa- IPOST- Iowa Physician Orders for Scope of Treatment Wyoming-Wyo. POLST-Provider Orders For Life-Sustaining Treatment South Dakota-MOST-Medical Orders for Scope of Treatment- South Dakota Department of Health recently made available on July 1, 2019. https: //www. sdaho. org/MOST
POLST SD MOST POLST –Portable Orders for Life-Sustaining Treatment SD MOST- South Dakota Medical Orders for Scope of Treatment South Dakota’s Work of POLST • Life. Circle. SD • Inter‐institutional, inter‐professional • Health Systems • Religious organizations • Government • State organizations • Anyone who is interested In 2019 the work was presented to the South Dakota Legislature resulting in Senate Bill 118. It passed through committee, Senate, and the House. On March 27, 2019, it was signed by Governor Noem
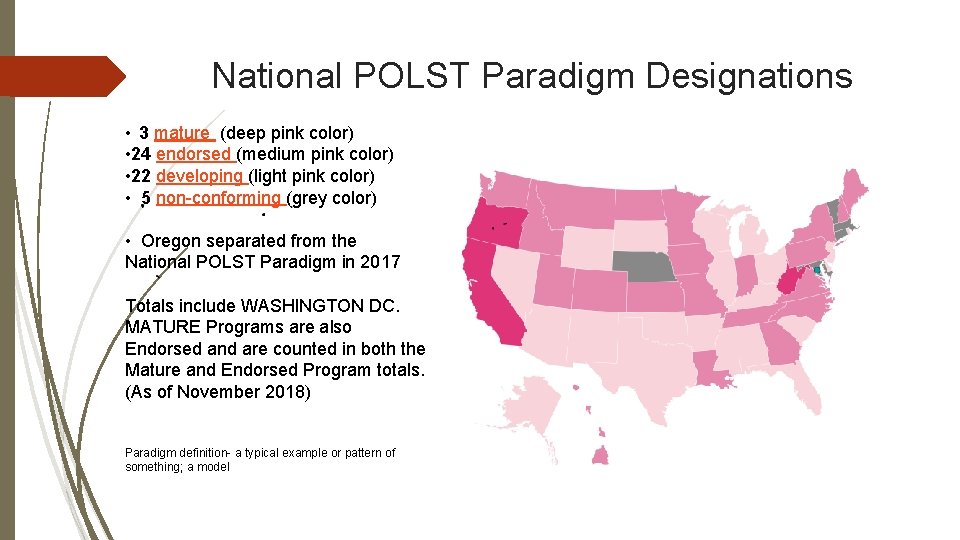
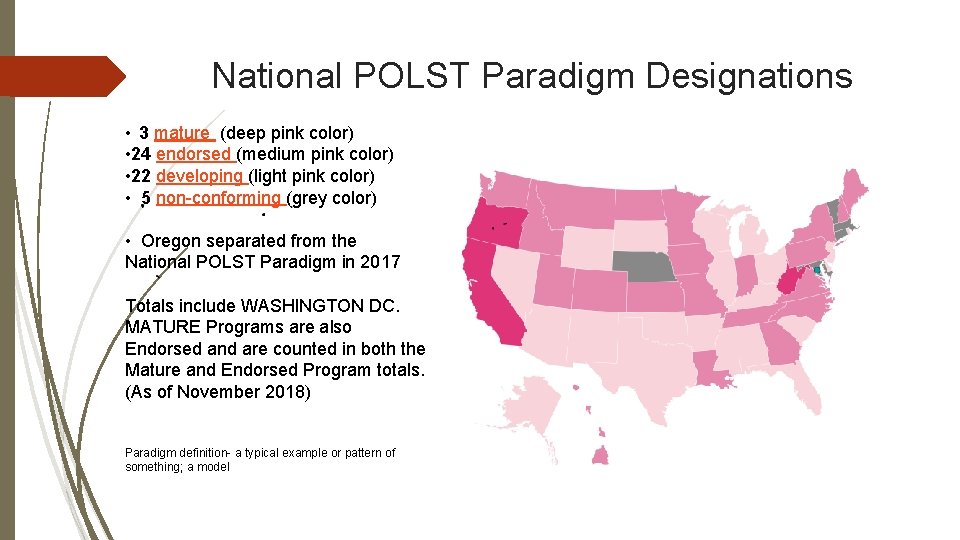
National POLST Paradigm Designations • 3 mature (deep pink color) • 24 endorsed (medium pink color) • 22 developing (light pink color) • 5 non-conforming (grey color) • Oregon separated from the National POLST Paradigm in 2017 Totals include WASHINGTON DC. MATURE Programs are also Endorsed and are counted in both the Mature and Endorsed Program totals. (As of November 2018) Paradigm definition- a typical example or pattern of something; a model
Twelve National POLST Paradigm Fundamentals used in SD MOST 1. A POLST Paradigm Form is not an Advance Directive, but an advanced Care planning tool. It is a portable, actionable medical order that helps ensure patient treatment wishes are known and honored. Helps to prevent initiation of unwanted, disproportionaly burdensome extraordinary treatment. 2. A POLST Paradigm Form is voluntary-it should never be mandatory to complete a POLST Paradigm Form. 3. Imperative that in completing a POLST Paradigm Form it involves informed, shared decision-making between patients and health care professionals. The conversation involves the patient discussing his/her values, beliefs, and goals for care, with the health care professional presenting the diagnosis, prognosis, and treatment alternatives, including the benefits and burdens of life-sustaining treatments. Together an informed decision is reached.
4. The POLST Paradigm is not for everyone; only patients with serious illnesses. Twelve or frailty for whom their. POLST health care. Paradigm professionals would not be National surprised if they died within a year should have a POLST Paradigm Form. For Fundamentals usedstatus in SD MOST these patients, their current health indicates the need for standing medical orders for emergent or future medical care. For healthy patients, an advance directive is an appropriate tool for making future end-of-life care wishes known to loved ones. 5. A POLST Paradigm Form allows patients to have their religious values respected. For example, the POLST Paradigm Form allows Catholics to make decisions consistent with the United States Conference of Catholic Bishops Ethical and Religious Directives for Catholic Health Care Services, 5 ed. (2009) and ensures that those decisions will be honored in an emergency and across care transitions. .
Twelve National POLST Paradigm Fundamentals used in SD MOST 6. A POLST Paradigm Form enables health care professionals to order treatments patients would want during a medical crisis, helping avoid the provision of treatments patients would not want, such as those that the patient considers “extraordinary” and excessively burdensome. 7. A POLST Paradigm Form requires that “ordinary” measures to improve the patient’s comfort, and food and fluid by mouth as tolerated, always be provided. 8. State law authorizes certain health care professionals to sign medical orders; the POLST Form is signed by those health care professionals who are accountable for the medical orders.
Twelve National POLST Paradigm Fundamentals used in SD MOST 9. A POLST Paradigm requires health care professionals be trained to conduct informed shared decision-making discussions with patients and families so that POLST Paradigm Forms are completed properly. 10. A POLST Paradigm Form may be signed by the patient or designated decision-maker (HCA*, DPOA for Healthcare, or surrogate), but this is not required in all states. The National POLST Paradigm Task Force encourages patient or surrogate signatures (or witnessed verbal consent) be required on POLST Paradigm Forms. *HCA=Health Care Agent
Twelve National POLST Paradigm Fundamentals used in SD MOST 11. The POLST Paradigm is not about how you want to die, it is about how you want to live with the time you have left. 12. The National POLST Paradigm recognizes that allowing natural death to occur is not the same as killing. (Death with Dignity = certain legislation that is about deliberately ending life, also called Physician Aid in Dying or Physician Assisted Suicide. This is when MD orders lethal dose of medication that patient self ingests) (https: //polst. org/wp-content/uploads/2016/09/POLST-Paradigm. Fundamentals. pdf)
South Dakota MOST Developed after several years long thoughtful discussion to develop draft form of document and legislative proposal Respect for autonomy (the ability of a person to make his/her own decisions, in this case regarding health care) Respect for religious beliefs Input was received from many professionals and organizations( Doctors, nurses, lawyers, legal experts, university instructors in Nursing, social workers, seminary professors and chaplains) Passed 2019 Legislative session and signed by Governor Form and other information found at https: //sdaho. org/most
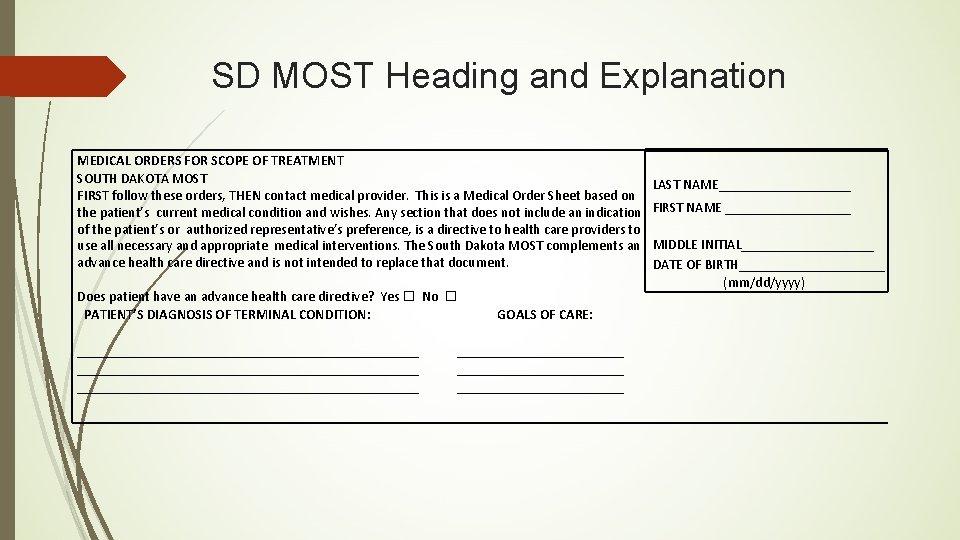
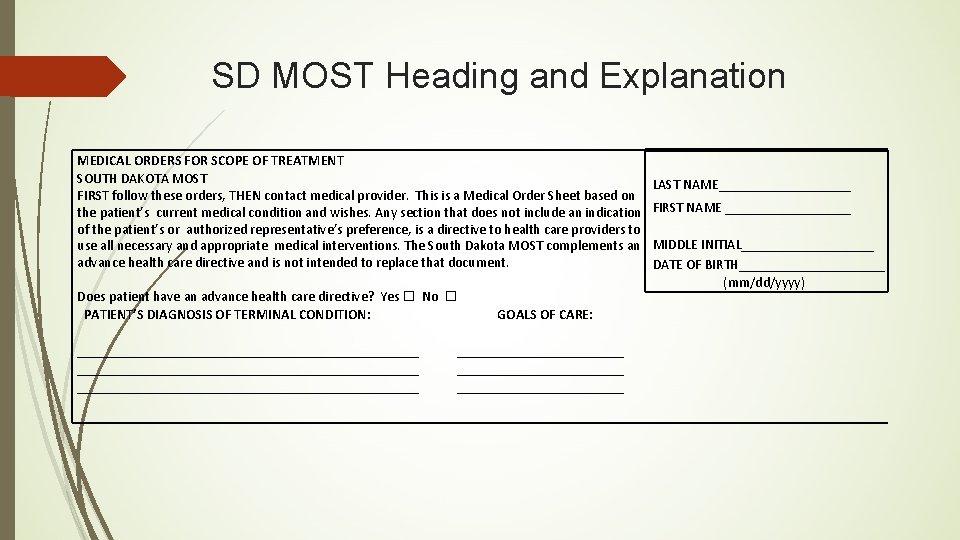
SD MOST Heading and Explanation MEDICAL ORDERS FOR SCOPE OF TREATMENT SOUTH DAKOTA MOST FIRST follow these orders, THEN contact medical provider. This is a Medical Order Sheet based on the patient’s current medical condition and wishes. Any section that does not include an indication of the patient’s or authorized representative’s preference, is a directive to health care providers to use all necessary and appropriate medical interventions. The South Dakota MOST complements an advance health care directive and is not intended to replace that document. Does patient have an advance health care directive? Yes No PATIENT’S DIAGNOSIS OF TERMINAL CONDITION: _________________________________________________ GOALS OF CARE: ________________________ LAST NAME__________ FIRST NAME _________ MIDDLE INITIAL__________ DATE OF BIRTH___________ (mm/dd/yyyy)
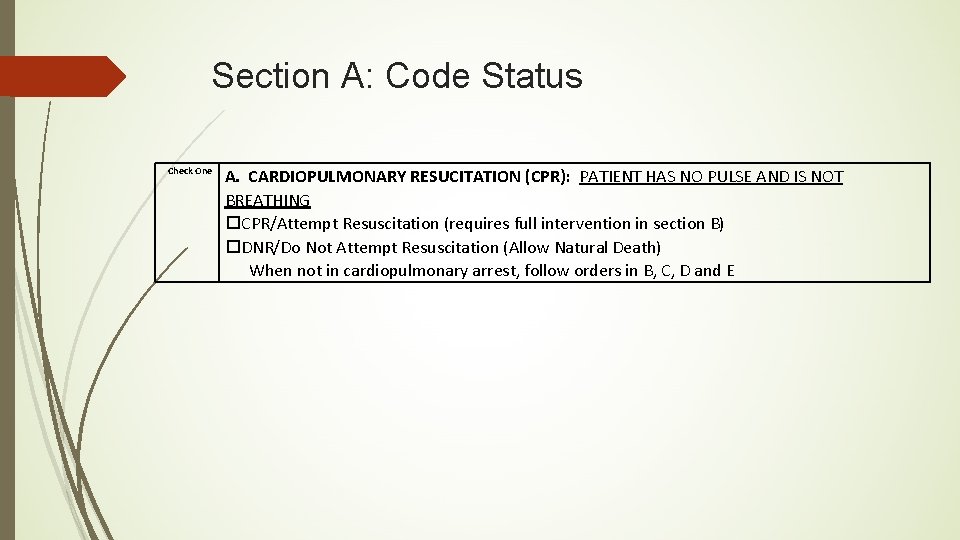
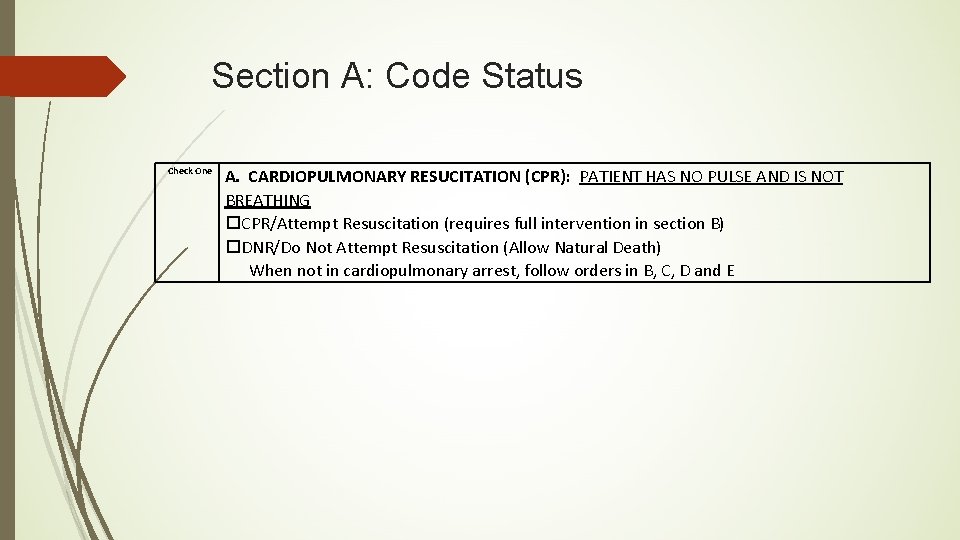
Section A: Code Status Check One A. CARDIOPULMONARY RESUCITATION (CPR): PATIENT HAS NO PULSE AND IS NOT BREATHING CPR/Attempt Resuscitation (requires full intervention in section B) DNR/Do Not Attempt Resuscitation (Allow Natural Death) When not in cardiopulmonary arrest, follow orders in B, C, D and E
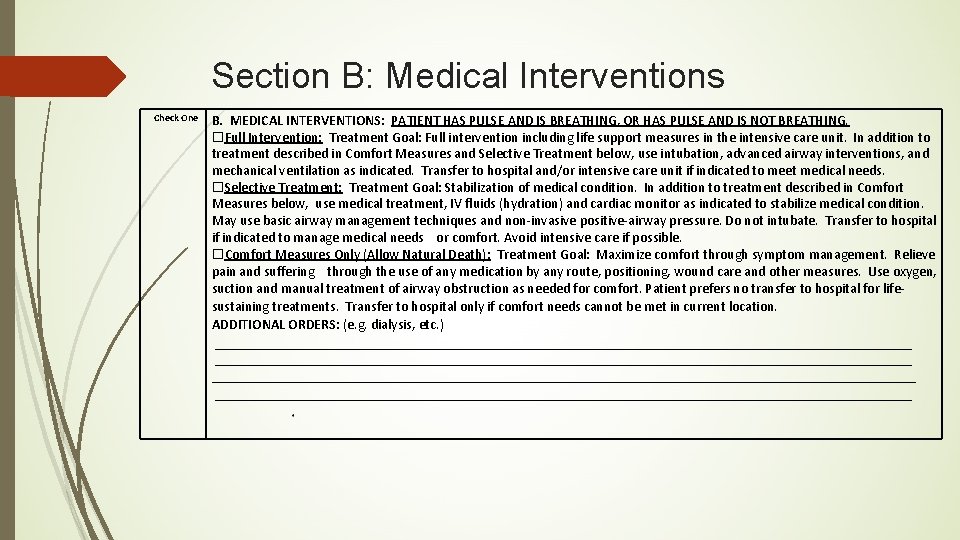
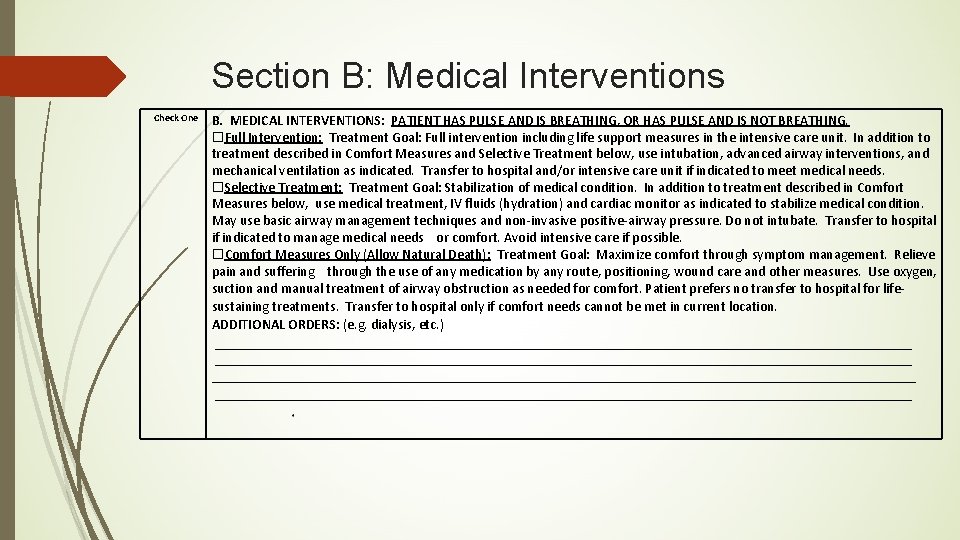
Section B: Medical Interventions Check One B. MEDICAL INTERVENTIONS: PATIENT HAS PULSE AND IS BREATHING, OR HAS PULSE AND IS NOT BREATHING. Full Intervention: Treatment Goal: Full intervention including life support measures in the intensive care unit. In addition to treatment described in Comfort Measures and Selective Treatment below, use intubation, advanced airway interventions, and mechanical ventilation as indicated. Transfer to hospital and/or intensive care unit if indicated to meet medical needs. Selective Treatment: Treatment Goal: Stabilization of medical condition. In addition to treatment described in Comfort Measures below, use medical treatment, IV fluids (hydration) and cardiac monitor as indicated to stabilize medical condition. May use basic airway management techniques and non-invasive positive-airway pressure. Do not intubate. Transfer to hospital if indicated to manage medical needs or comfort. Avoid intensive care if possible. Comfort Measures Only (Allow Natural Death): Treatment Goal: Maximize comfort through symptom management. Relieve pain and suffering through the use of any medication by any route, positioning, wound care and other measures. Use oxygen, suction and manual treatment of airway obstruction as needed for comfort. Patient prefers no transfer to hospital for lifesustaining treatments. Transfer to hospital only if comfort needs cannot be met in current location. ADDITIONAL ORDERS: (e. g. dialysis, etc. ) ____________________________________________________________________________________________________ __________________________________________________
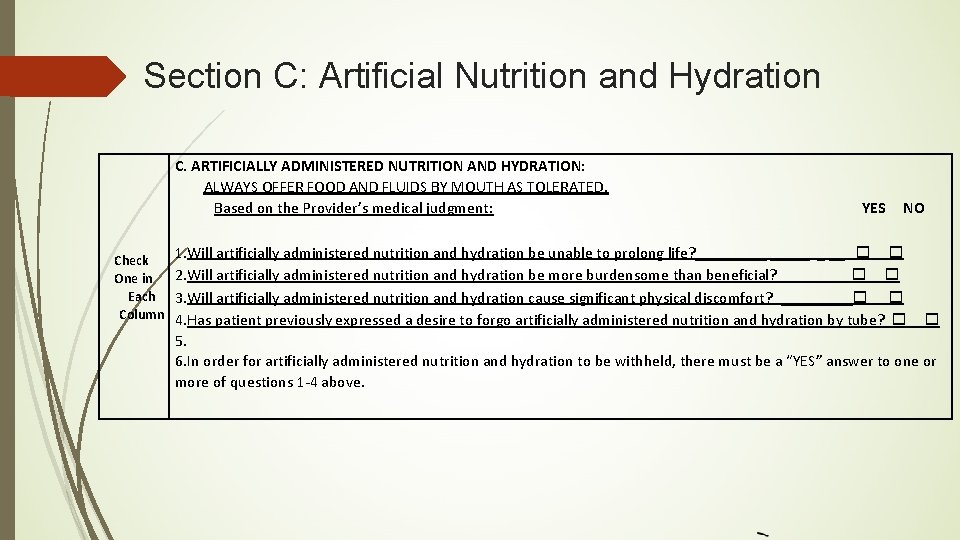
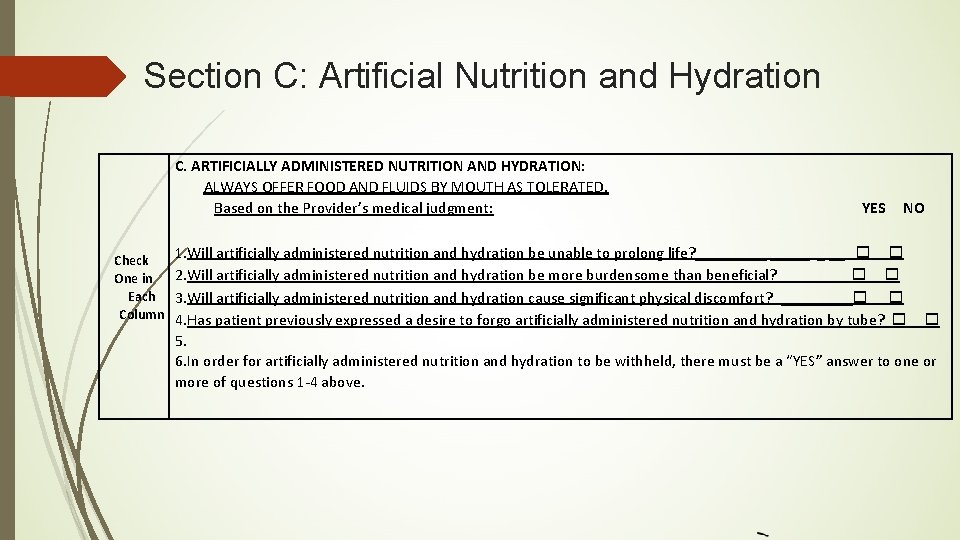
Section C: Artificial Nutrition and Hydration C. ARTIFICIALLY ADMINISTERED NUTRITION AND HYDRATION: ALWAYS OFFER FOOD AND FLUIDS BY MOUTH AS TOLERATED. Based on the Provider’s medical judgment: YES 1. Will artificially administered nutrition and hydration be unable to prolong life? _____ _ __ NO Check 2. Will artificially administered nutrition and hydration be more burdensome than beneficial? _______ __ One in Each 3. Will artificially administered nutrition and hydration cause significant physical discomfort? _____ Column 4. Has patient previously expressed a desire to forgo artificially administered nutrition and hydration by tube? 5. 6. In order for artificially administered nutrition and hydration to be withheld, there must be a “YES” answer to one or more of questions 1 -4 above.
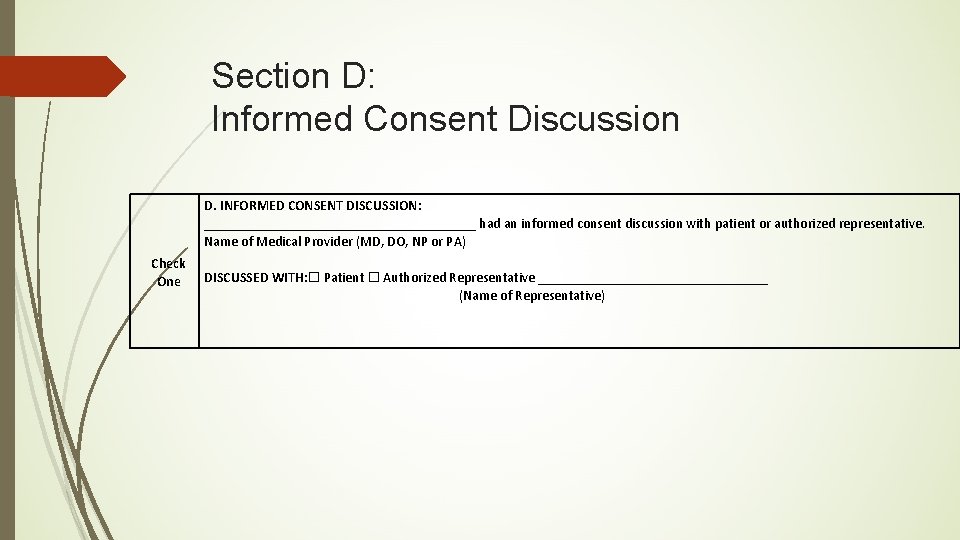
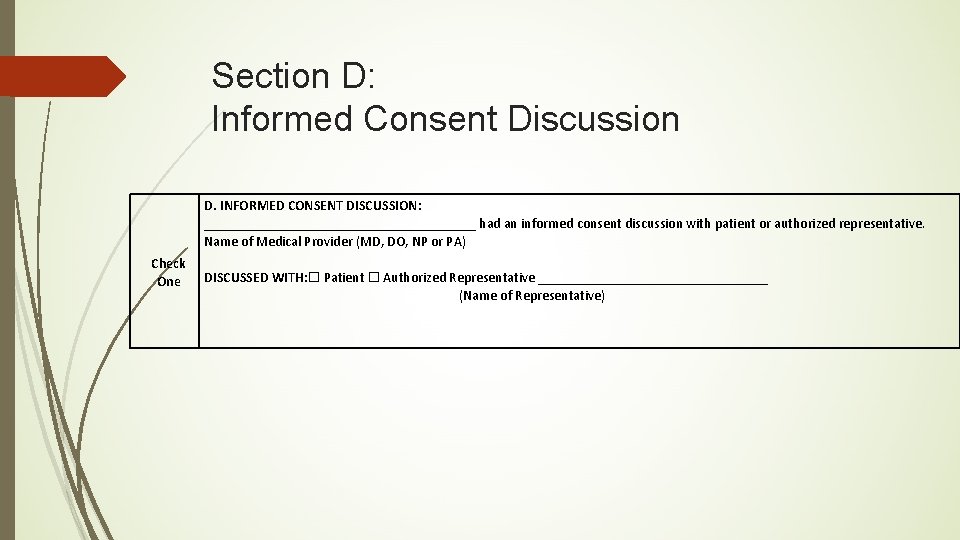
Section D: Informed Consent Discussion D. INFORMED CONSENT DISCUSSION: ____________________ had an informed consent discussion with patient or authorized representative. Name of Medical Provider (MD, DO, NP or PA) Check One DISCUSSED WITH: Patient Authorized Representative _________________ (Name of Representative)
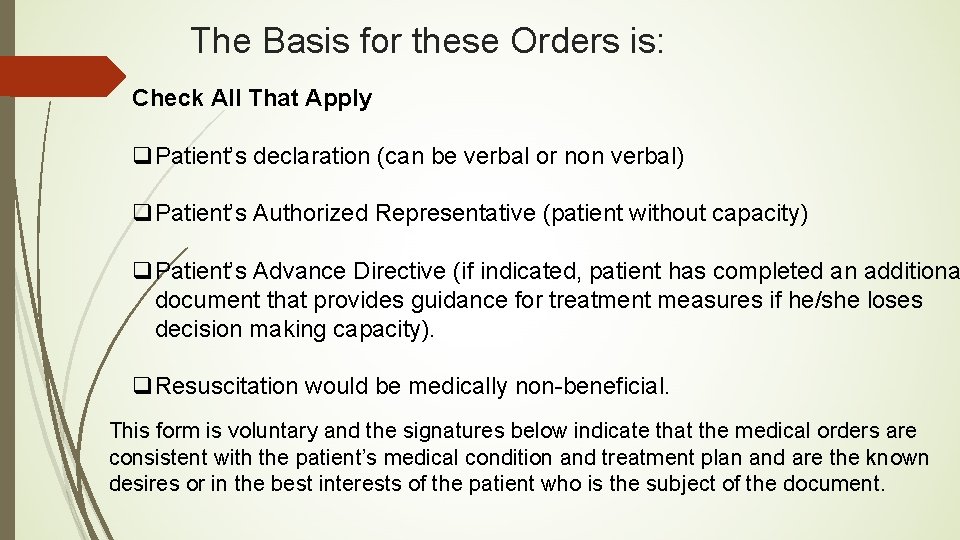
The Basis for these Orders is: Check All That Apply q. Patient’s declaration (can be verbal or non verbal) q. Patient’s Authorized Representative (patient without capacity) q. Patient’s Advance Directive (if indicated, patient has completed an additiona document that provides guidance for treatment measures if he/she loses decision making capacity). q. Resuscitation would be medically non-beneficial. This form is voluntary and the signatures below indicate that the medical orders are consistent with the patient’s medical condition and treatment plan and are the known desires or in the best interests of the patient who is the subject of the document.
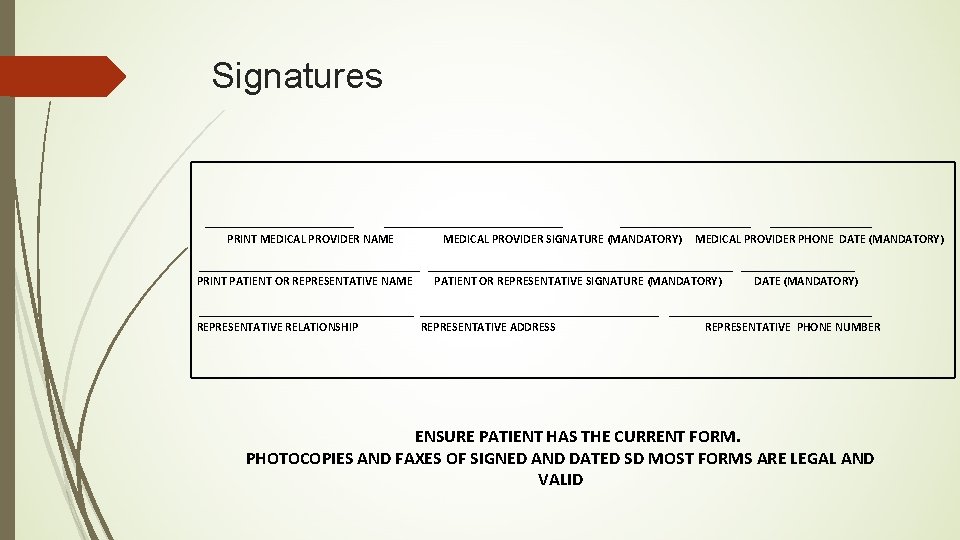
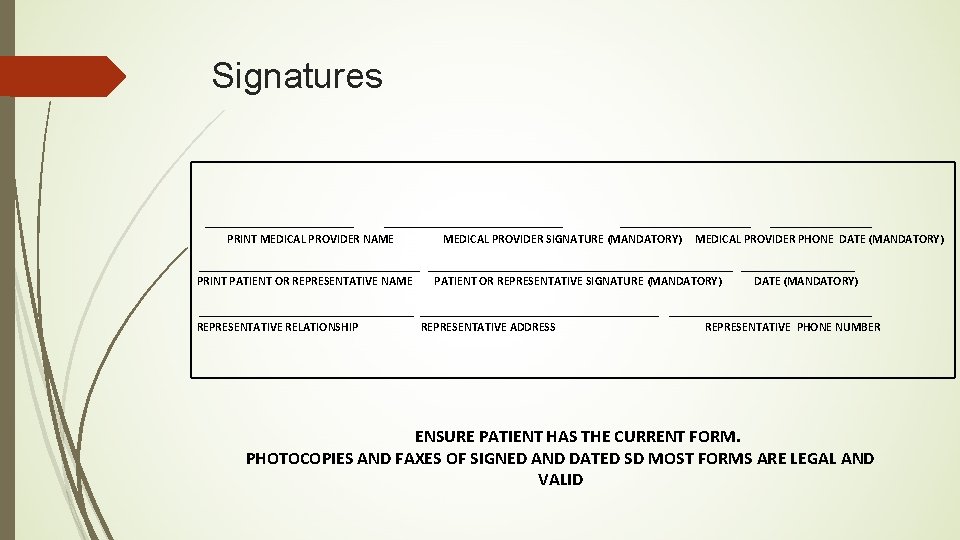
Signatures ______________________________ PRINT MEDICAL PROVIDER NAME MEDICAL PROVIDER SIGNATURE (MANDATORY) MEDICAL PROVIDER PHONE DATE (MANDATORY) ____________________________________________ PRINT PATIENT OR REPRESENTATIVE NAME PATIENT OR REPRESENTATIVE SIGNATURE (MANDATORY) DATE (MANDATORY) ________________________________________ REPRESENTATIVE RELATIONSHIP REPRESENTATIVE ADDRESS REPRESENTATIVE PHONE NUMBER ENSURE PATIENT HAS THE CURRENT FORM. PHOTOCOPIES AND FAXES OF SIGNED AND DATED SD MOST FORMS ARE LEGAL AND VALID
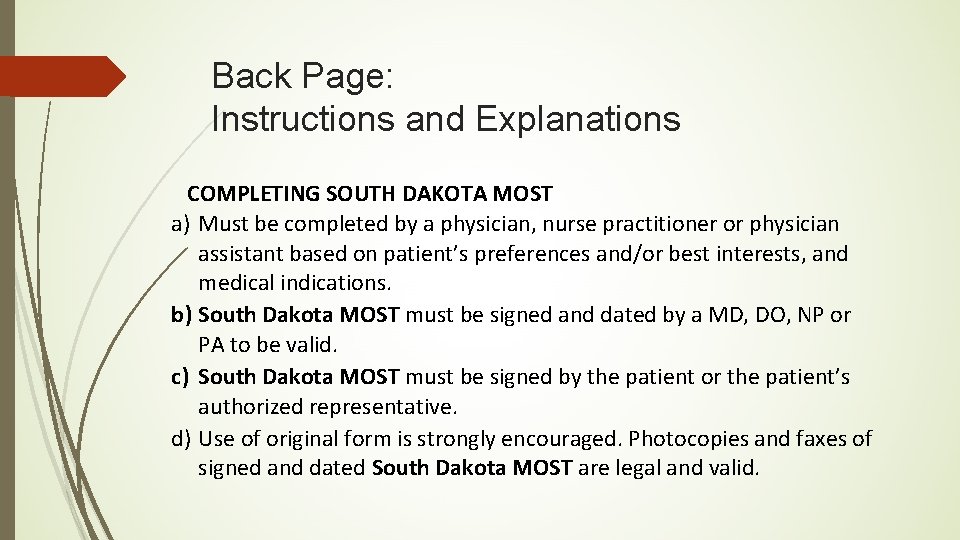
Back Page: Instructions and Explanations COMPLETING SOUTH DAKOTA MOST a) Must be completed by a physician, nurse practitioner or physician assistant based on patient’s preferences and/or best interests, and medical indications. b) South Dakota MOST must be signed and dated by a MD, DO, NP or PA to be valid. c) South Dakota MOST must be signed by the patient or the patient’s authorized representative. d) Use of original form is strongly encouraged. Photocopies and faxes of signed and dated South Dakota MOST are legal and valid.
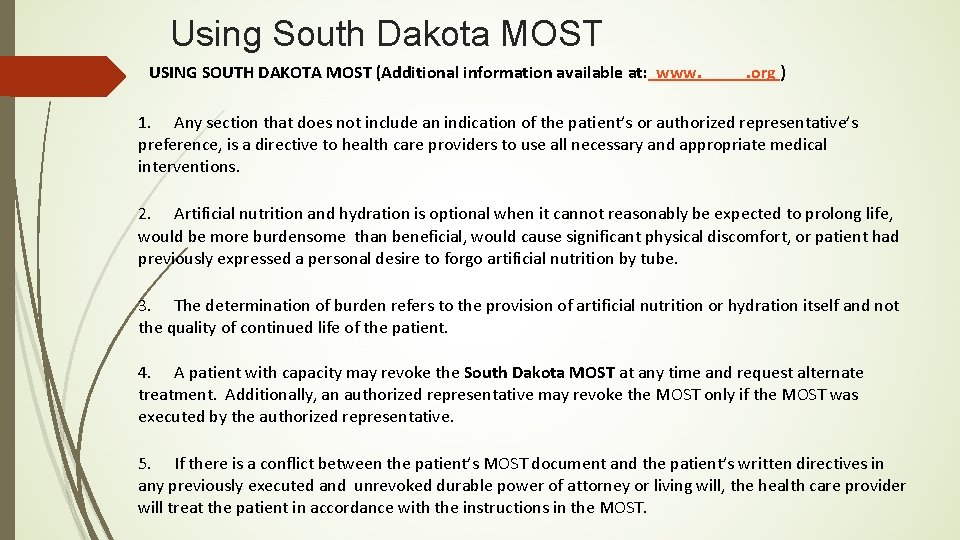
Using South Dakota MOST USING SOUTH DAKOTA MOST (Additional information available at: www. _____. org ) 1. Any section that does not include an indication of the patient’s or authorized representative’s preference, is a directive to health care providers to use all necessary and appropriate medical interventions. 2. Artificial nutrition and hydration is optional when it cannot reasonably be expected to prolong life, would be more burdensome than beneficial, would cause significant physical discomfort, or patient had previously expressed a personal desire to forgo artificial nutrition by tube. 3. The determination of burden refers to the provision of artificial nutrition or hydration itself and not the quality of continued life of the patient. 4. A patient with capacity may revoke the South Dakota MOST at any time and request alternate treatment. Additionally, an authorized representative may revoke the MOST only if the MOST was executed by the authorized representative. 5. If there is a conflict between the patient’s MOST document and the patient’s written directives in any previously executed and unrevoked durable power of attorney or living will, the health care provider will treat the patient in accordance with the instructions in the MOST.
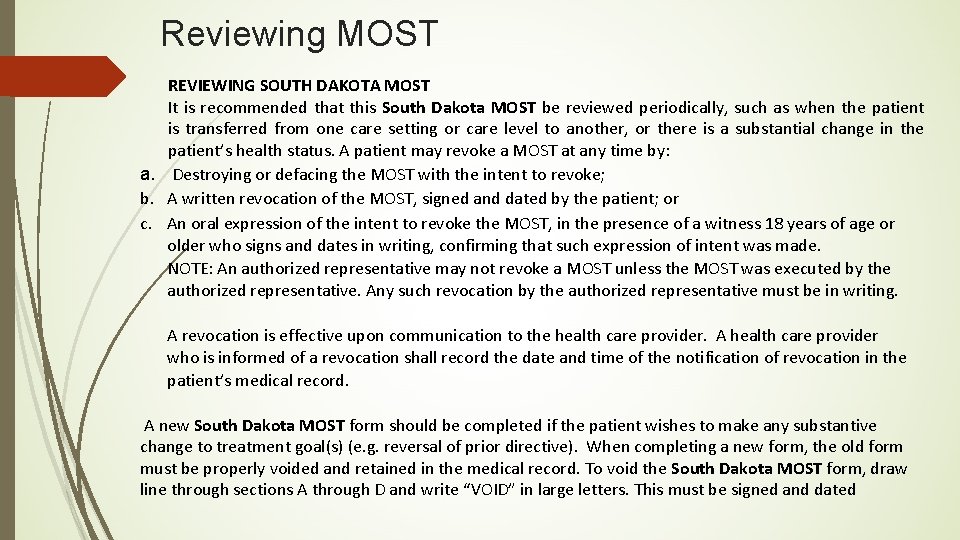
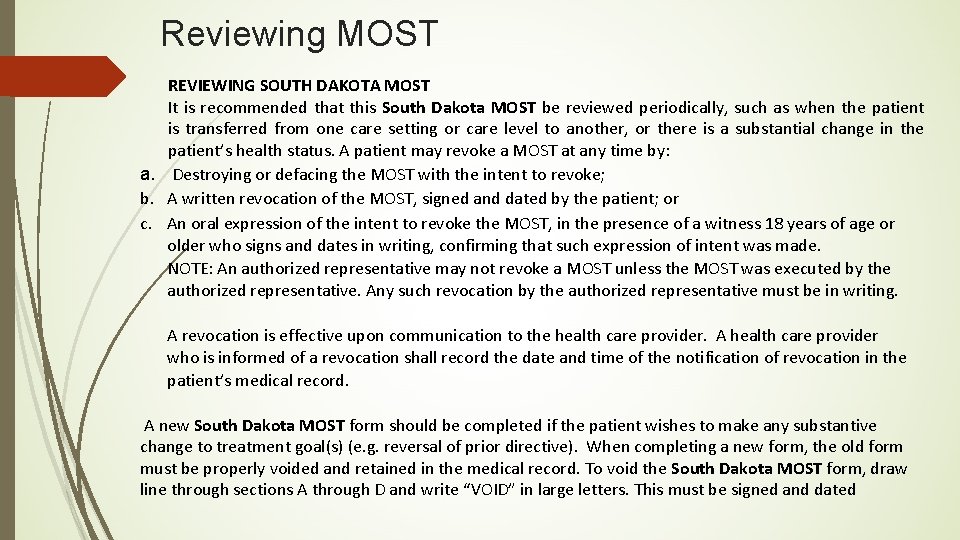
Reviewing MOST REVIEWING SOUTH DAKOTA MOST It is recommended that this South Dakota MOST be reviewed periodically, such as when the patient is transferred from one care setting or care level to another, or there is a substantial change in the patient’s health status. A patient may revoke a MOST at any time by: a. Destroying or defacing the MOST with the intent to revoke; b. A written revocation of the MOST, signed and dated by the patient; or c. An oral expression of the intent to revoke the MOST, in the presence of a witness 18 years of age or older who signs and dates in writing, confirming that such expression of intent was made. NOTE: An authorized representative may not revoke a MOST unless the MOST was executed by the authorized representative. Any such revocation by the authorized representative must be in writing. A revocation is effective upon communication to the health care provider. A health care provider who is informed of a revocation shall record the date and time of the notification of revocation in the patient’s medical record. A new South Dakota MOST form should be completed if the patient wishes to make any substantive change to treatment goal(s) (e. g. reversal of prior directive). When completing a new form, the old form must be properly voided and retained in the medical record. To void the South Dakota MOST form, draw line through sections A through D and write “VOID” in large letters. This must be signed and dated
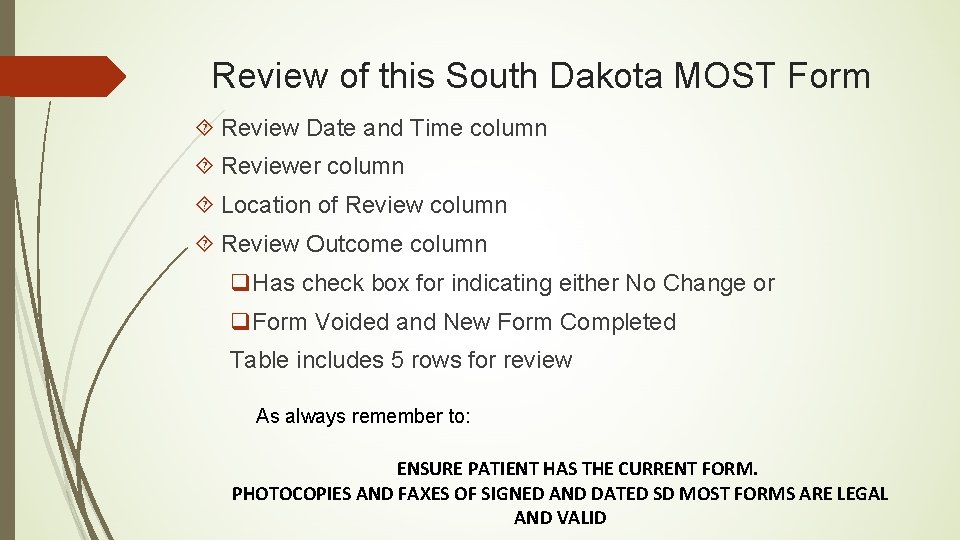
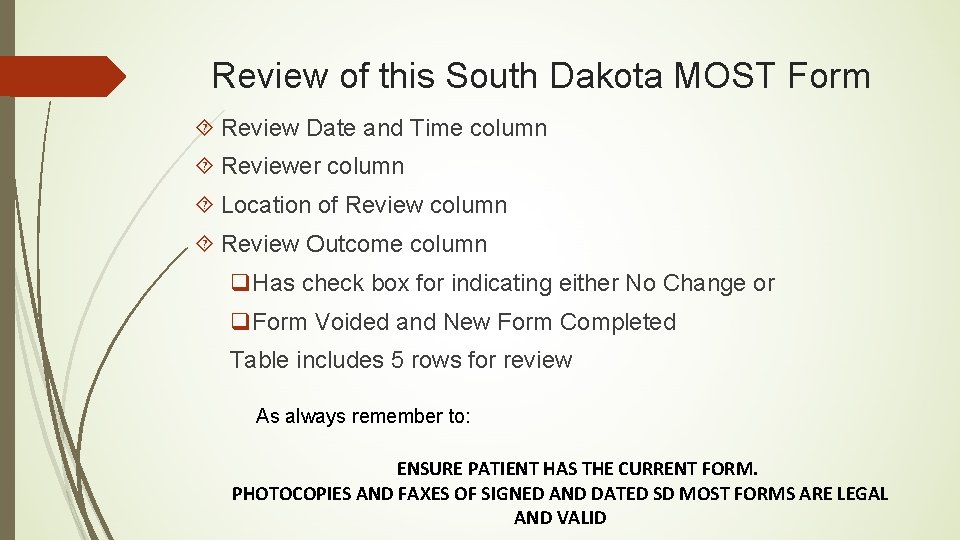
Review of this South Dakota MOST Form Review Date and Time column Reviewer column Location of Review column Review Outcome column q. Has check box for indicating either No Change or q. Form Voided and New Form Completed Table includes 5 rows for review As always remember to: ENSURE PATIENT HAS THE CURRENT FORM. PHOTOCOPIES AND FAXES OF SIGNED AND DATED SD MOST FORMS ARE LEGAL AND VALID
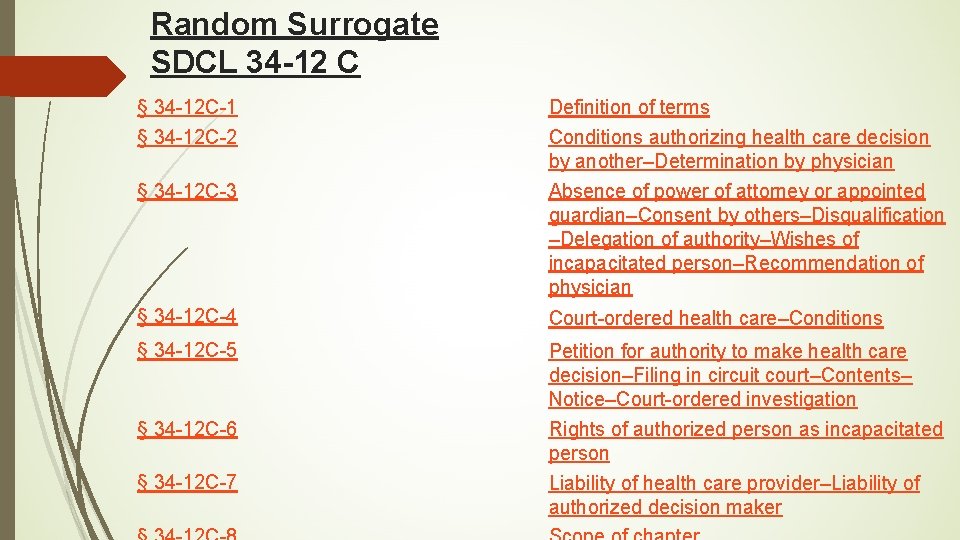
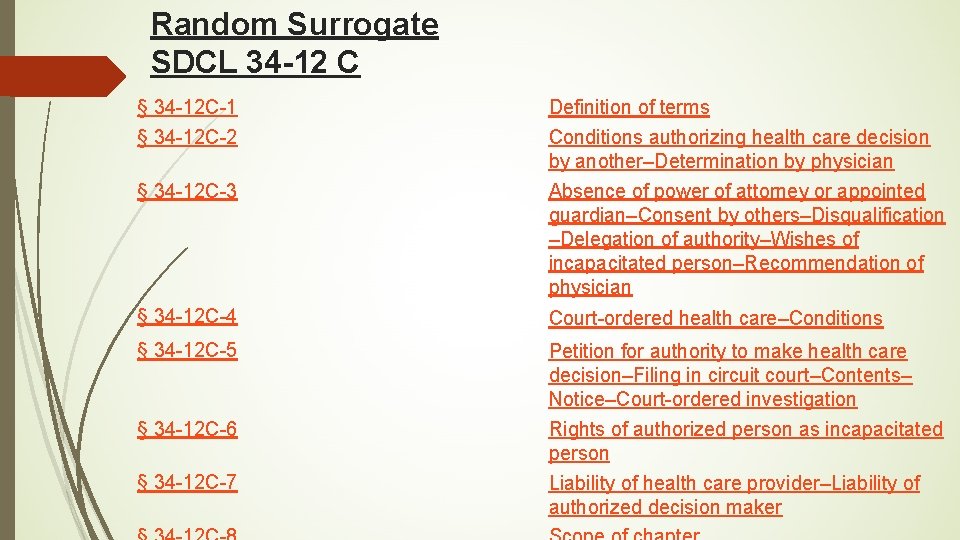
Random Surrogate SDCL 34 -12 C § 34 -12 C-1 § 34 -12 C-2 § 34 -12 C-3 Definition of terms Conditions authorizing health care decision by another–Determination by physician Absence of power of attorney or appointed guardian–Consent by others–Disqualification –Delegation of authority–Wishes of incapacitated person–Recommendation of physician § 34 -12 C-4 Court-ordered health care–Conditions § 34 -12 C-5 Petition for authority to make health care decision–Filing in circuit court–Contents– Notice–Court-ordered investigation Rights of authorized person as incapacitated person Liability of health care provider–Liability of authorized decision maker § 34 -12 C-6 § 34 -12 C-7
Random Surrogate (con’t) Occurs when patient has not designated a surrogate decision maker regarding health care directives for their care Becomes operative when physician or court determines incapacity/ incompetency (MD/Court, respectively) Health care interventions are done at the consent of designated random surrogate ( there is a “pecking order” for how this is done) Revocation of the random surrogate is done by the physician or court determining capacity or competency Patient is no longer in control of his/her health care decisions, which if were able to speak for self, the interventions done may not concur with beliefs or desires they would have wanted
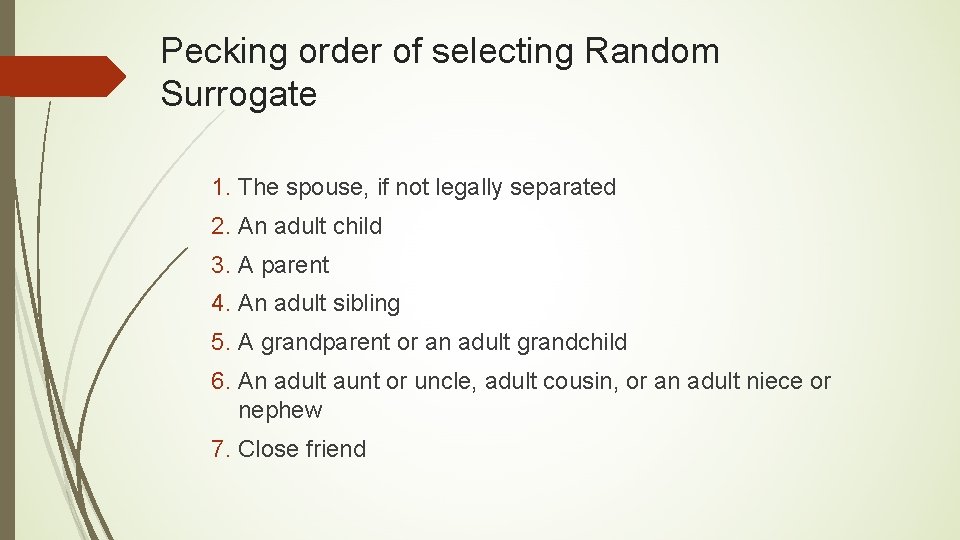
Pecking order of selecting Random Surrogate 1. The spouse, if not legally separated 2. An adult child 3. A parent 4. An adult sibling 5. A grandparent or an adult grandchild 6. An adult aunt or uncle, adult cousin, or an adult niece or nephew 7. Close friend
The Duty of Medicine The duty of medicine is to care for patients even when they cannot be cured. Physicians, nurse practitioners and physician assistants, and their patients must evaluate the use of technology at their disposal based on available information. Judgments about the use of technology to maintain life must reflect the inherent dignity of the patient and the purpose of medical care. Everyone is to be treated with dignity and respect.
Helpful guides for someone who is experiencing the end of life of a loved one
Summary Comments Ø SD MOST forms are medical orders and must be signed by a health care professional to be valid. Ø SD MOST form completion is always voluntary and should never be mandated. Ø Completion of a SD MOST form without a patient or surrogate knowledge is contrary to the purpose and intent of the POLST Paradigm and violates informed consent and principles of person and family-centered care.
Summary Comments (continued) Ø The SD MOST form is designated to document treatment decisions made after shared-decision making conversations between a patient and his/her health care professional. Ø The National POLST Paradigm strongly encourages training of all health care professionals who complete POLST forms.
QUESTIONS