Informed Consent And The Right To Know Medical

- Slides: 13
Informed Consent And The Right To Know: Medical Professionals’ Conversations About Care At the End of Life Joanna K. Weinberg, JD, LLM UC San Francisco UC Hastings College of the Law

AMERICAN MEDICAL ASSOCIATION 2010 The patient’s right of self-decision can be effectively exercised only if the patient possesses enough information to enable an informed choice. The patient should make his or her own determination about treatment. The physician’s obligation is to present the medical facts accurately to the patient or to the individual responsible for the patient’s care and to make recommendations for management in accordance with good medical practice. The physician has an ethical obligation to help the patient make choices from among therapeutic alternatives consistent with good medical practice. . .
Informed Consent and the Right of Patients to be Informed �At common law, treatment without informing patients of the risks of treatment is a denial of informed consent, and constitutes criminal battery. �Theoretically, then, under common law, treating a patient without giving the patient adequate information about available alternatives and their risks and benefits, should also constitute a denial of informed consent.
• What about giving the patient information about alternatives – and the risks and benefits – of not treating? • Shouldn’t this be considered a denial of informed consent? • The issue becomes extremely sensitive when the conversation touches upon care at the edges of life.
Within the Space of Two Years, How Doctors Communicate With Patients has Become a Hot Topic
§ Oct. 21, 2008 “The Right to Know, Then to Say ‘No’: CA Terminal Patients’ Right to Know End of Life Options Act, ” Jane Gross, New York Times § August 24, 2009 Death Panels Smite Journalism, Howard Kurtz, Washington Post § August 23, 2010 “New York Law Encourages Frank Talk on Palliative Care, ” Jane E. Brody, The New York Times
The New York Palliative Care Act Effective 2 -2011: “physicians and nurse practitioners are required to provide a patient who has less than 6 months to live with information and counseling on palliative care and end-of-life options, including, ‘the range of options appropriate to the patient, the prognosis, risks and benefits of the various options, and the patient’s legal rights to comprehensive pain and symptom management at the end of life. ’ “
California Right to Know End-of-Life Options Act When a healthcare provider diagnoses a patient with a terminal illness, the healthcare provider shall, upon the patient’s request, provide the patient with “comprehensive information and counseling” regarding legal end-of-life options.
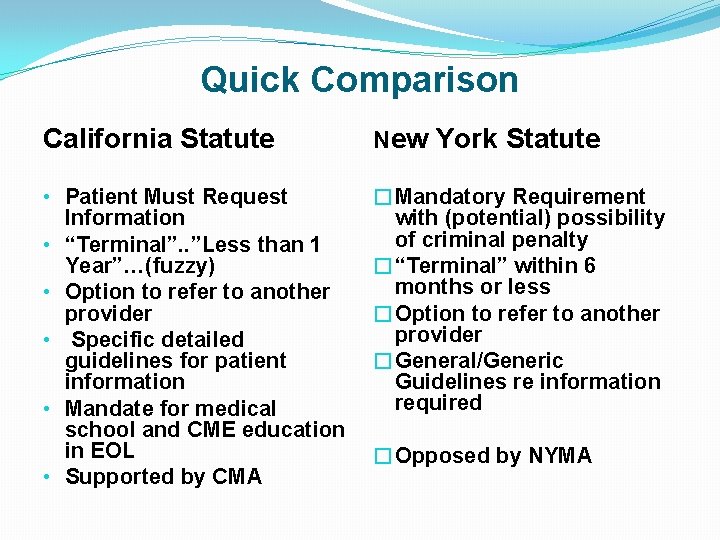
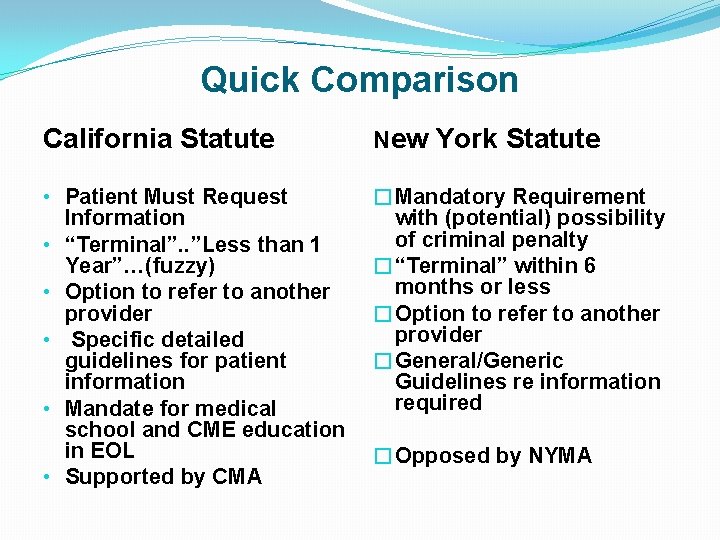
Quick Comparison California Statute New York Statute • Patient Must Request Information • “Terminal”. . ”Less than 1 Year”…(fuzzy) • Option to refer to another provider • Specific detailed guidelines for patient information • Mandate for medical school and CME education in EOL • Supported by CMA �Mandatory Requirement with (potential) possibility of criminal penalty �“Terminal” within 6 months or less �Option to refer to another provider �General/Generic Guidelines re information required �Opposed by NYMA
Some Final Thoughts • The discussion about the Right to Know legislation highlights a not-so-hidden defect in the 25+ years or so that we have been talking about Advance Directives, and the 20 years since the PSDA became federal law: • The low use of advance care directives and problems with implementing those that exist have made it clear that emphasizing patient’s rights and patient control over decision making are not necessarily the most effective ways to improve care for dying patients.
More Thoughts Without abandoning the idea of advance directives, an evolving perspective views direct communication about options for end-of-life care as a component of a much larger process that looks at what a “good death” means and tries to define the various domains that are necessary for optimal end-of-life care –the physical, psychological and social supports that are critical to the care of patients at the end of life. These views also provide the basis for training physicians and other health professionals in end-of-life care. The California law mandates this (with respect to physicians). While the NY law doesn’t, its mandated communication seems to point in that direction.
Thank you
 Free prior and informed consent
Free prior and informed consent Right product right place right time right price
Right product right place right time right price Right time right place right quantity right quality
Right time right place right quantity right quality Dasar hukum informed consent adalah
Dasar hukum informed consent adalah Http informed delivery usps
Http informed delivery usps Ethical principles governing informed consent process
Ethical principles governing informed consent process Advantages of informed consent
Advantages of informed consent Broad informed consent
Broad informed consent Informed consent brochure
Informed consent brochure Essential elements of informed consent
Essential elements of informed consent The right man on the right place at the right time
The right man on the right place at the right time Dfps medical consent training
Dfps medical consent training Right to be informed
Right to be informed Know history know self
Know history know self