PERIPHERAL ARTERIAL DISEASE Sadie T Velsquez M D



















- Slides: 56

PERIPHERAL ARTERIAL DISEASE Sadie T. Velásquez, M. D.
A 68 -year-old man is evaluated for left calf pain that occurs after walking 2 -3 blocks, relieved with rest; he has had the pain for 6 months. He has a history of CAD with left ventricular systolic function of 30% treated with CABG 2 years ago and implanted cardiac defibrillator placement for primary prevention purposes. PMH: HTN, HLP Social: prior tobacco Meds: atorvastatin, aspirin, metoprolol, lisinopril
A 72 -year-old man is evaluated in the emergency department for acute severe pain during rest in the LLE that began 3 days ago. The patient has repeatedly used vicodin that he had at home for relief of pain. His pain is now much better, but he finds that he is having difficulty walking. + progressive exertional pain in the LLE x 1 year. PMH: HTN, HLP PSH: L fem-pop bypass for occlusive PAD with distal ulceration (5 yrs ago) Social: 50 pack-year tobacco Meds: aspirin, lisinopril, hydrochlorothiazide, simvastatin.
ACC/AHA 2005 GUIDELINES FOR THE MANAGEMENT OF PATIENTS WITH PERIPHERAL ARTERIAL DISEASE (with 2011 Update In Press)
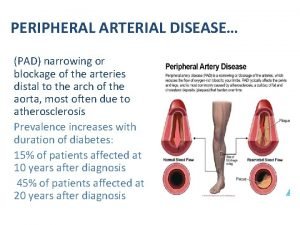
Definitions “Peripheral arterial disease” - vascular diseases caused primarily by atherosclerosis and thromboembolic pathophysiological processes altering normal structure and function of the aorta, its visceral arterial branches, and the arteries of the lower extremity, exclusive of the coronary arteries
Today, we are just going to focus on lower extremity PAD…

Objectives 1. 2. 3. 4. Risks for lower extremity PAD Natural history of atherosclerosis Causes of PAD Clinical presentation of lower extremity PAD 5. Diagnose lower extremity PAD 6. Treatment of PAD

Objectives 1. 2. 3. 4. Risks for lower extremity PAD Natural history of atherosclerosis Causes of PAD Clinical presentation of lower extremity PAD 5. Diagnose lower extremity PAD 6. Treatment of PAD
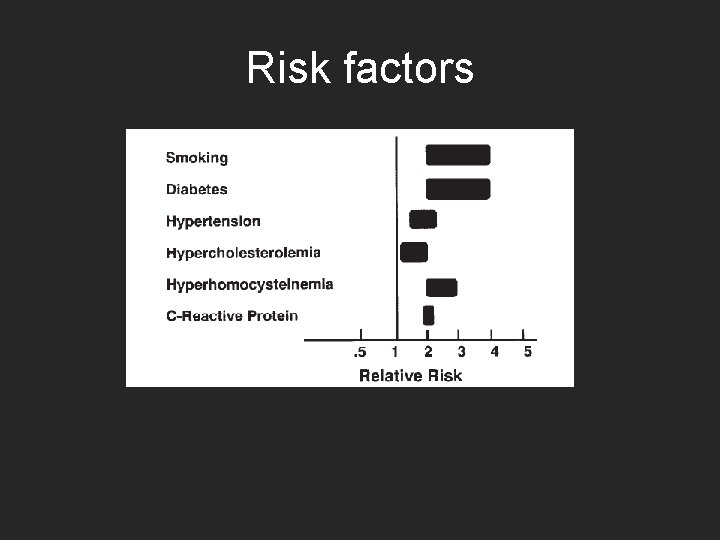
Risk factors • Age < 50 with DM and one other atherosclerosis risk factor • Age >50 years and h/o smoking or DM • Age >65 years • Leg symptoms • Abnormal pulse exam • Known atherosclerotic coronary, carotid or renal artery disease
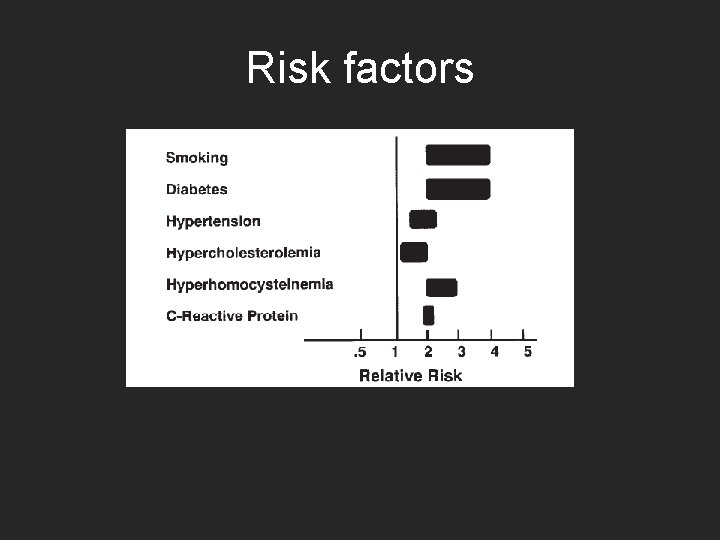
Risk factors

History and physical Individuals at risk for lower extremity PAD: • Vascular review of symptoms – Exertional limitation of pain – Leg or foot wounds – Rest pain in LE/association with upright or recumbent positions – Postprandial pain provoked by eating and reproducible, weight loss – FH of AAA
Physical exam Vascular physical examination: • Bilateral UE blood pressure • Carotid pulses • Auscultation of the abdomen and flank • Aortic pulsation and its maximal diameter • Palpation of pulses at the brachial, radial, ulnar, femoral, popliteal, dorsalis pedis, and posterior tibial sites
• • • Allen’s test Auscultation of both femoral arteries Pulse intensity Foot inspection Distal hair loss, trophic skin changes, and hypertrophic nails
Why do we even care?
Other causes of PAD • • • Thromboembolic Inflammatory Aneurysmal disease Trauma Entrapment syndromes Congenital abnormalities

Objectives 1. 2. 3. 4. Risks for lower extremity PAD Natural history of atherosclerosis Causes of PAD Clinical presentation of lower extremity PAD 5. Diagnose lower extremity PAD 6. Treatment of PAD
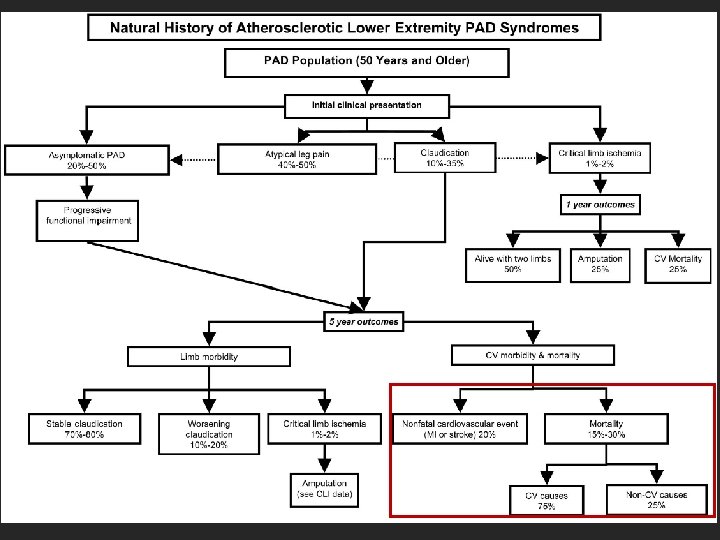
Clinical presentation 1. 2. 3. 4. 5. Asymptomatic Claudication Critical Limb Ischemia Acute Limb Ischemia Prior Limb Arterial Revascularization

Risk factors • Age < 50 with DM and one other atherosclerosis risk factor • Age >50 years and h/o smoking or DM • Age >65 years • Leg symptoms • Abnormal pulse exam • Known atherosclerotic coronary, carotid or renal artery disease

Asymptomatic • Vascular review of systems for those at risk – May have subtle impairments of LE function • Examination and ABI to identify PAD • Exercise ABI if ABI is normal
Claudication • Consistently produced by exercise => relieved by rest • Distinguish from ‘pseudoclaudication’ • Vascular physical exam, ABI measurement • Exercise ABI • Comprehensive medical approach


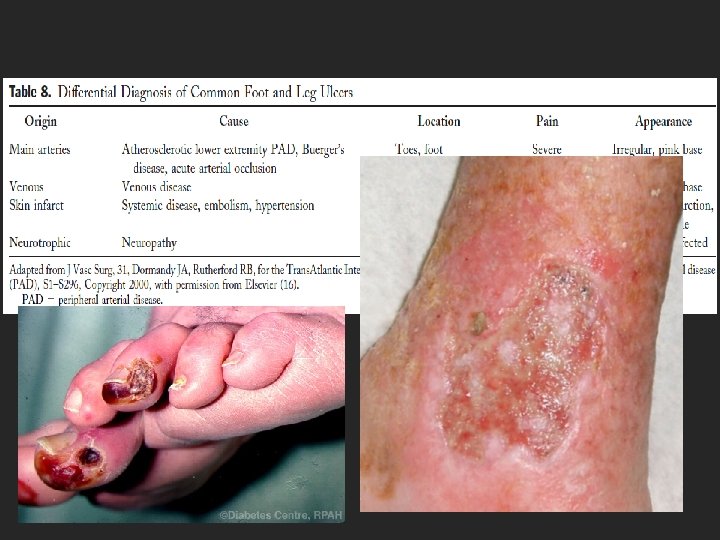
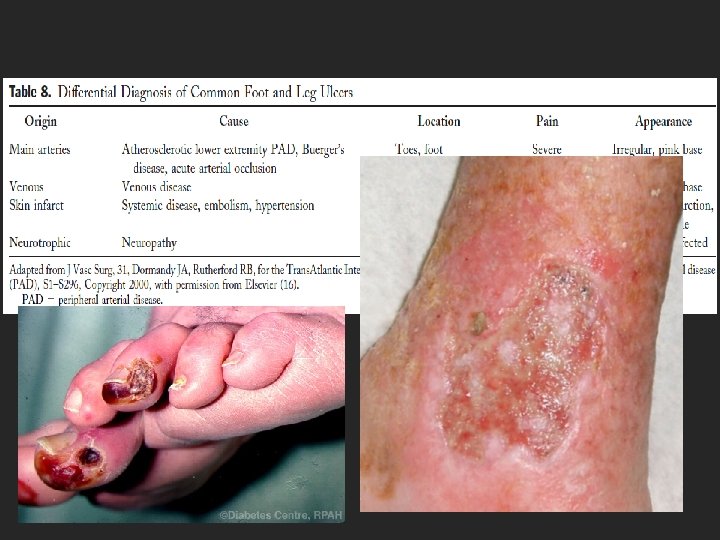
Critical Limb Ischemia • Limb pain at rest +/- trophic skin changes or tissue loss • Discomfort worse supine; less in the dependent position • Require narcotics for pain • Distinguish arterial vs venous or neurotrophic ulcers • CBC, chemistry, EKG and ABI for evaluation
Critical Limb Ischemia • CV risk assessment • Evaluate for aneurysmal disease if suspicious • Systemic antibiotics • Refer to wound specialist Without revascularization, CLI requires amputation within 6 months

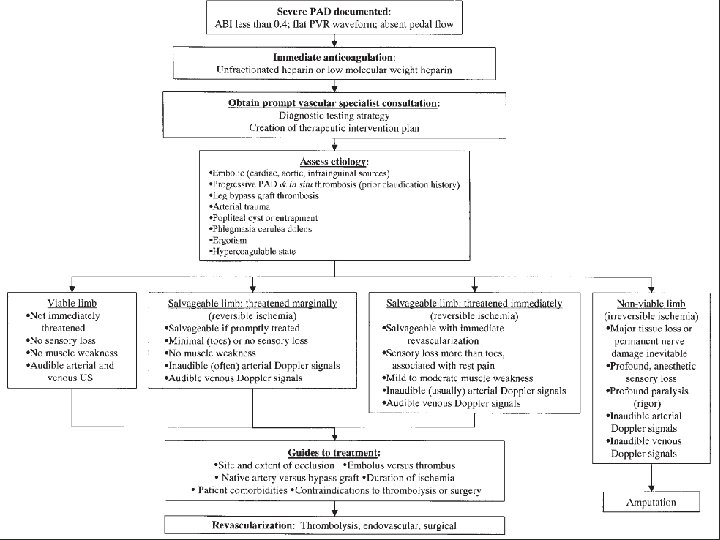
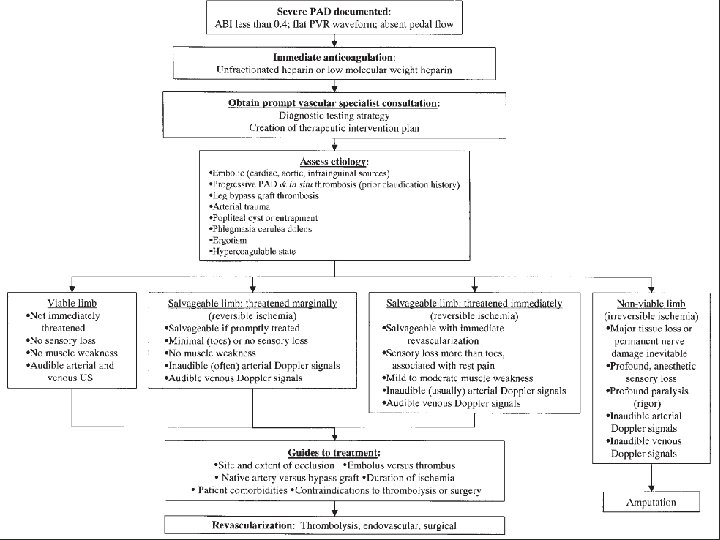
Acute Limb Ischemia • Rapid or sudden decrease in limb perfusion threatening tissue viability • 5 “P’s” – Pain – Paralysis – Paresthesias – Pulselessness – Pallor • 6 th “P”? Polar

Prior Limb Arterial Revascularization • Surveillance program for 2 years: – Interval vascular history – Resting ABIs – PE – Duplex ultrasound if venous conduit used • Timeframe by specialist or bypass type • Angiography if noninvasive methods suggest hemodynamically significant lesions J Vasc Surg, 31, Dormandy JA, Rutherford RB, for the Trans. Atlantic Inter-Society Consensus (TASC) Working Group, Management of peripheral arterial disease (PAD), S 1–S 296, Copyright 2000
Objectives 1. 2. 3. 4. Risks for lower extremity PAD Natural history of atherosclerosis Causes of PAD Clinical presentation of lower extremity PAD 5. Diagnose lower extremity PAD 6. Treatment of PAD
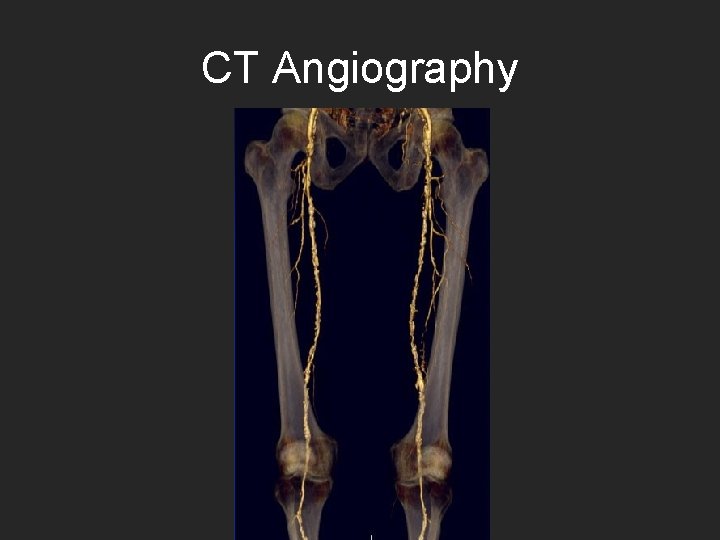
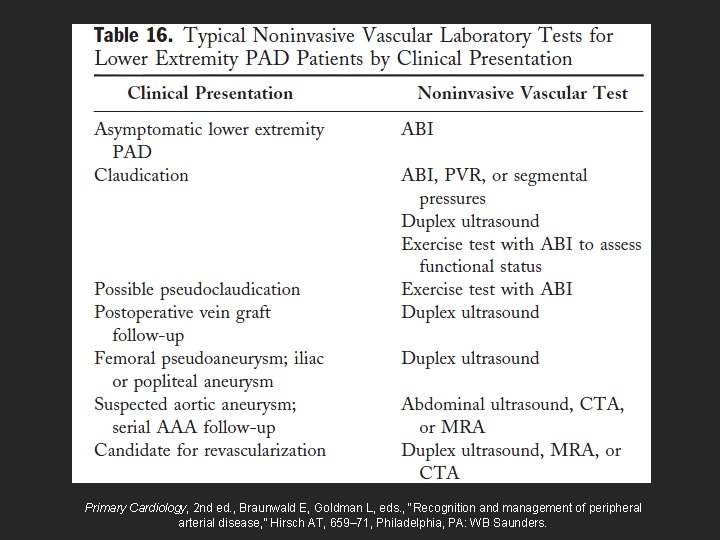
Diagnostic Methods 1. Ankle-Brachial and Toe-Brachial Indices 2. Treadmill Exercise Testing with and without ABI Assessments and 6 -Minute Walk Test 3. Duplex Ultrasound 4. CT Angiography 5. MRI Angiography
6. 7. 8. 9. Contrast Angiography Pulse Volume Recording Segmental pressure examination Continuous-wave Doppler ultrasound

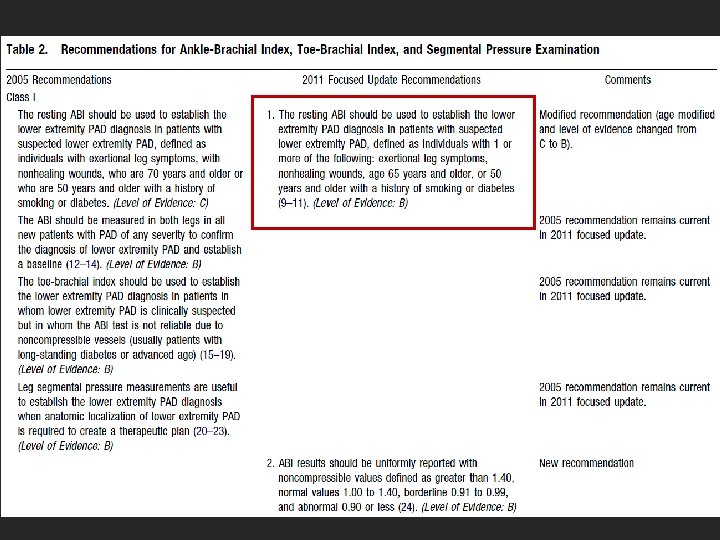
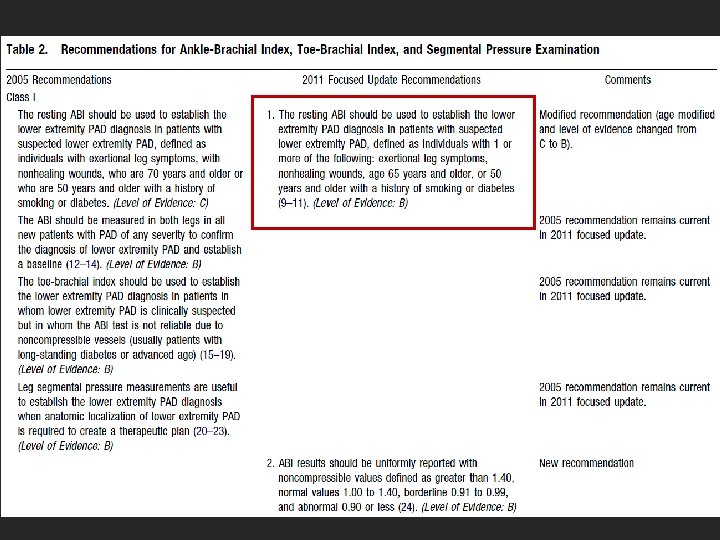
Ankle-Brachial Index • >1. 40: noncompressible • 1. 00 -1. 40: normal • 0. 91 to 0. 99: borderline • < 0. 90: abnormal Mayo Foundation
Ankle-Brachial Index • Patients at risk and those suspected of LE PAD • Bilateral LE • TBI if ABI is not reliable • Leg segmental pressure measurements useful for anatomic localization
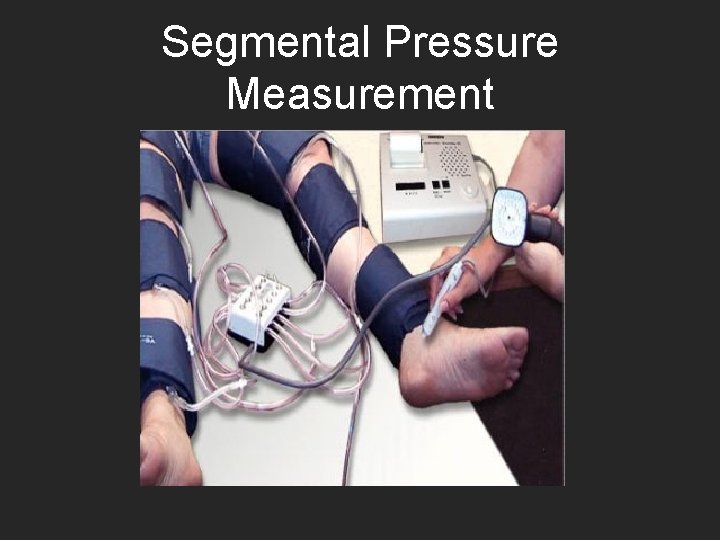
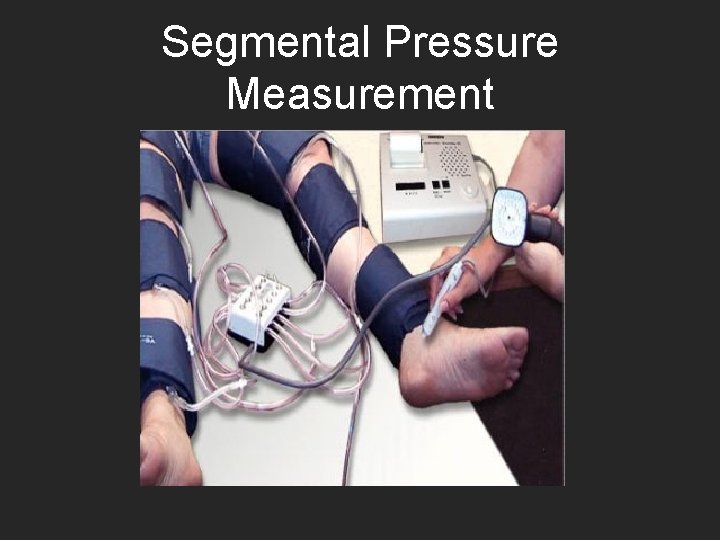
Segmental Pressure Measurement
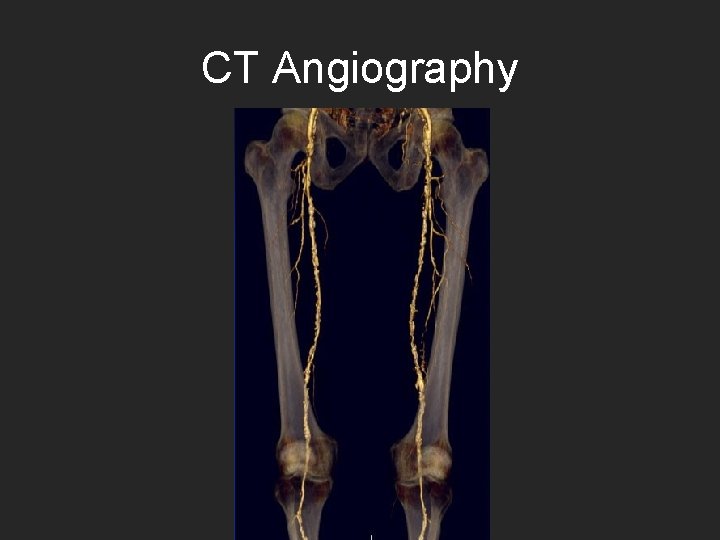
CT Angiography

Owen A R , Roditi G H Postgrad Med J doi: 10. 1136/pgmj. 2009. 082040 Copyright © The Fellowship of Postgraduate Medicine. All rights reserved.

MR angiograms show severe bilateral occlusive PAD below the knee Hodnett P A et al. Radiology 2011; 260: 282 -293 © 2011 by Radiological Society of North America
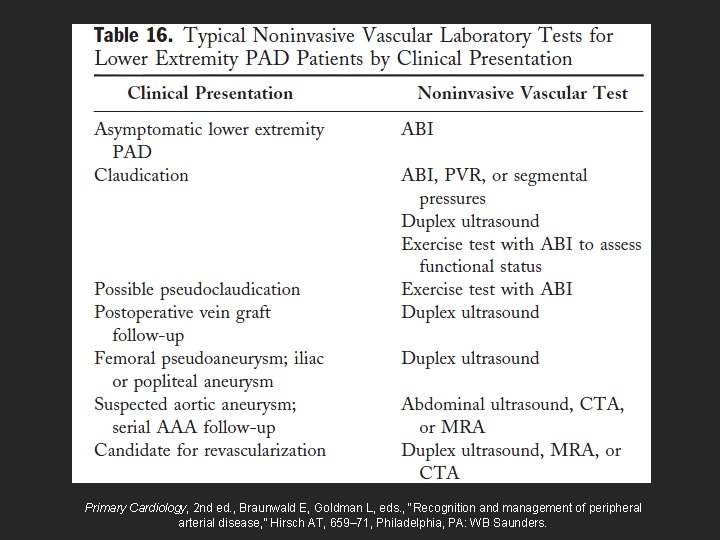
Primary Cardiology, 2 nd ed. , Braunwald E, Goldman L, eds. , “Recognition and management of peripheral arterial disease, ” Hirsch AT, 659– 71, Philadelphia, PA: WB Saunders.
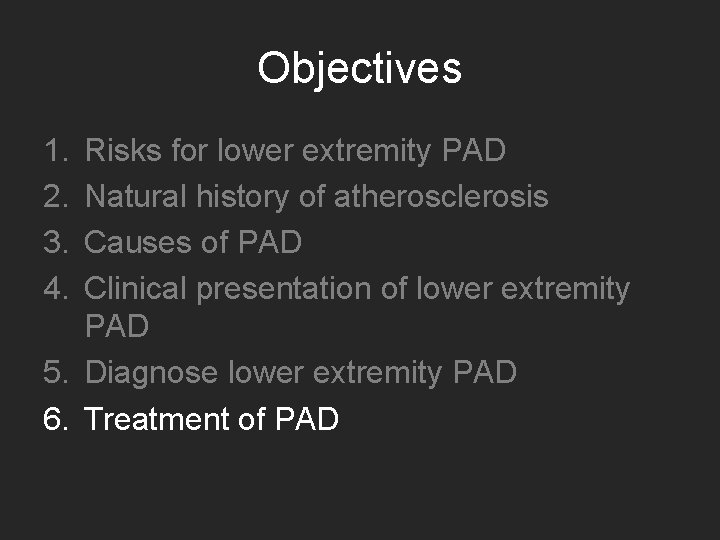
Objectives 1. 2. 3. 4. Risks for lower extremity PAD Natural history of atherosclerosis Causes of PAD Clinical presentation of lower extremity PAD 5. Diagnose lower extremity PAD 6. Treatment of PAD
Treatment • Cardiovascular Risk Reduction • Claudication • Critical Limb Ischemia and Treatment for Limb Salvage
CV Risk Reduction • • • Lipid-lowering Drugs Antihypertensive Drugs DM Therapies Smoking Cessation * Homocysteine-Lowering Drugs Antiplatelet and Antithrombotic Drugs
Smoking Cessation • Ask about smoking status at every visit • Provide counseling and development smoking cessation plan • Pharmacotherapy should be offered to all smokers
Claudication • Exercise and LE PAD Rehabilitation • Medical and Pharmacologic Treatment for Claudication – Cilostazol – Pentoxifylline • Endovascular Treatment for Claudication • Surgery
Critical Limb Ischemia and Treatment for Limb Salvage • Prostaglandins may be considered • Endovascular treatment • Thrombolysis for acute and chronic limb ischemia • Surgery



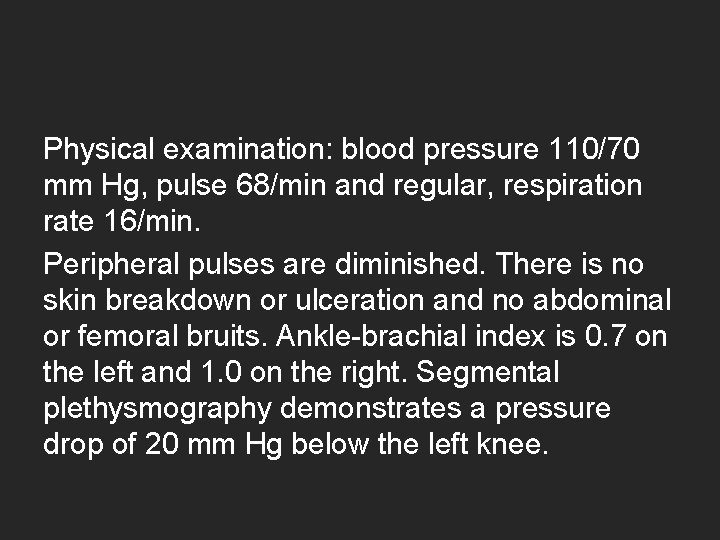
Questions A 68 -year-old man is evaluated for left calf pain that occurs after walking 2 -3 blocks, relieved with rest; he has had the pain for 6 months. He has a history of CAD with left ventricular systolic function of 30% treated with CABG 2 years ago and implanted cardiac defibrillator placement for primary prevention purposes. PMH: HTN, HLP Social: prior tobacco Meds: atorvastatin, aspirin, metoprolol, lisinopril.
Physical examination: blood pressure 110/70 mm Hg, pulse 68/min and regular, respiration rate 16/min. Peripheral pulses are diminished. There is no skin breakdown or ulceration and no abdominal or femoral bruits. Ankle-brachial index is 0. 7 on the left and 1. 0 on the right. Segmental plethysmography demonstrates a pressure drop of 20 mm Hg below the left knee.
Which of the following is the most appropriate treatment for this patient? A. Femoral-popliteal bypass B. Medical treatment with cilostazol C. Percutaneous intervention D. Supervised exercise program

A 72 -year-old man is evaluated in the emergency department for acute severe pain during rest in the LLE that began 3 days ago. The patient has repeatedly used vicodin that he had at home for relief of pain. His pain is now much better, but he finds that he is having difficulty walking. + progressive exertional pain in the LLE x 1 year. PMH: HTN, HLP PSH: L fem-pop bypass for occlusive PAD with distal ulceration (5 yrs ago) Social: 50 pack-year tobacco Meds: aspirin, lisinopril, hydrochlorothiazide, simvastatin.

Physical examination: temperature is 37. 8 °C (100. 1 °F), blood pressure 106/60 mm Hg, pulse 100/min, respiration rate is 20/min. Left lower extremity is pale and cool from the toes to the mid shin, and there is a small ulceration on the ball of the left foot. The left posterior tibialis and dorsalis pedis pulses are not palpable and cannot be identified by Doppler ultrasonography. Venous Doppler signals are audible. The left foot and calf feel stiff, and the patient can only weakly flex the foot. Toe movement on the left side is minimal, and sensation to light touch is absent.
Which of the following is the most appropriate treatment for this patient? A. Emergent surgical revascularization B. Intravenous heparin C. Intra-arterial thrombolytic therapy D. Prompt amputation
References • MKSAP • ACC/AHA 2005 Guidelines for the Management of Patients With Peripheral Arterial Disease (Lower Extremity, Renal, Mesenteric, and Abdominal Aortic): Executive Summary. • Rooke et al. 2011 ACCF/AHA Focused Update of the Guideline for the Management of Patients With Peripheral Artery Disease (Updating the 2005 Guideline). J. Am. Coll. Cardiol. published online Sep 29, 2011. In Press.
 Peripheral arterial disease
Peripheral arterial disease Peripheral arterial pulse sites
Peripheral arterial pulse sites Realistic drama
Realistic drama Sadie is so fearful of being overwhelmed
Sadie is so fearful of being overwhelmed Sadie is so fearful of being overwhelmed by anxiety
Sadie is so fearful of being overwhelmed by anxiety Phloem rays
Phloem rays Communicable disease and non communicable disease
Communicable disease and non communicable disease Passive stains definition
Passive stains definition Arterial arcades of jejunum and ileum
Arterial arcades of jejunum and ileum Continuous capillaries
Continuous capillaries Mean pulmonary arterial pressure
Mean pulmonary arterial pressure Alcalose metabolica
Alcalose metabolica Arterial blood vs venous blood
Arterial blood vs venous blood Arterial gushing definition
Arterial gushing definition Route of administration of drugs definition
Route of administration of drugs definition Rias en salud
Rias en salud Clasificacion fontaine
Clasificacion fontaine Gasometria arterial valores normales
Gasometria arterial valores normales Angle of impact
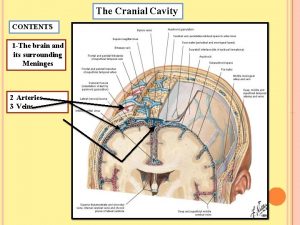
Angle of impact Brain arterial supply
Brain arterial supply Classificação de rutherford para oclusão arterial aguda
Classificação de rutherford para oclusão arterial aguda Arterial underfilling
Arterial underfilling Presión arterial
Presión arterial Tabla presion arterial niños
Tabla presion arterial niños Macrodrip vs microdrip
Macrodrip vs microdrip Pons vascular supply
Pons vascular supply Corniculate
Corniculate Arterial gush
Arterial gush Alcalosis respiratoria
Alcalosis respiratoria Pressão arterial normal
Pressão arterial normal Twin reversed arterial perfusion
Twin reversed arterial perfusion Normal arterial blood gas
Normal arterial blood gas How to measure jvp
How to measure jvp Arterial thrombosis vs embolism
Arterial thrombosis vs embolism Label the major systemic arteries
Label the major systemic arteries Veia pulmonar sangue arterial
Veia pulmonar sangue arterial Adrenaline
Adrenaline Zona de penumbra isquemica
Zona de penumbra isquemica Enfermedad arterial periferica
Enfermedad arterial periferica Central venous pressure range
Central venous pressure range Low velocity impact splatter
Low velocity impact splatter Cushing's reflex
Cushing's reflex Qon ketganda birinchi yordam
Qon ketganda birinchi yordam Mapa de tensão arterial
Mapa de tensão arterial Venous vs arterial blood
Venous vs arterial blood Stomach vascular anatomy
Stomach vascular anatomy Valor normal de gasometria
Valor normal de gasometria Arterial line whip
Arterial line whip Brain
Brain Lateral venous lacunae
Lateral venous lacunae Presion arterial
Presion arterial Posterior thorax lecture
Posterior thorax lecture Maniobra de millis
Maniobra de millis Femoral approach
Femoral approach Objetivo de la hipertensión arterial
Objetivo de la hipertensión arterial Twin reversed arterial perfusion
Twin reversed arterial perfusion Ampa y mapa
Ampa y mapa