PERIPHERAL NERVOUS SYSTEM PERIPHERAL NERVOUS SYSTEM The peripheral

- Slides: 61
PERIPHERAL NERVOUS SYSTEM
PERIPHERAL NERVOUS SYSTEM The peripheral nervous system refers to parts of the nervous system outside the brain and spinal cord. It includes the cranial nerves, spinal nerves and their roots and branches, peripheral nerves, and neuromuscular junctions. The anterior horn cells, although technically part of the central nervous system (CNS), are sometimes discussed with the peripheral nervous system because they are part of the motor unit. In the peripheral nervous system, bundles of nerve fibers or axons conduct information to and from the central nervous system. The autonomic nervous system is the part of the nervous system concerned with the innervation of involuntary structures, such as the heart, smooth muscle, and glands within the body. It is distributed throughout the central and peripheral nervous systems.
Nerve cells are called neurones. A neurone consists of a cell body (with a nucleus and cytoplasm), dendrites that carry electrical impulses to the cell, and a long axon that carries the impulses away from the cell. The axon of one neurone and the dendrites of the next neurone do not actually touch. The gap between neurones is called the synapse. Neuronal function is complex and involves numerous processes in nerve transmission. Generation of a nerve impulse (action potential) of a sensory neurone occurs as a result of a stimulus such as light, a particular chemical, or stretching of a cell membrane by sound. Conduction of an impulse along a neurone occurs from the dendrites to the cell body to the axon. Transmission of a signal to another neuron across a synapse occurs via chemical transmitter. This substance causes the next neurone to be electrically stimulated and keeps the signal going along a nerve.
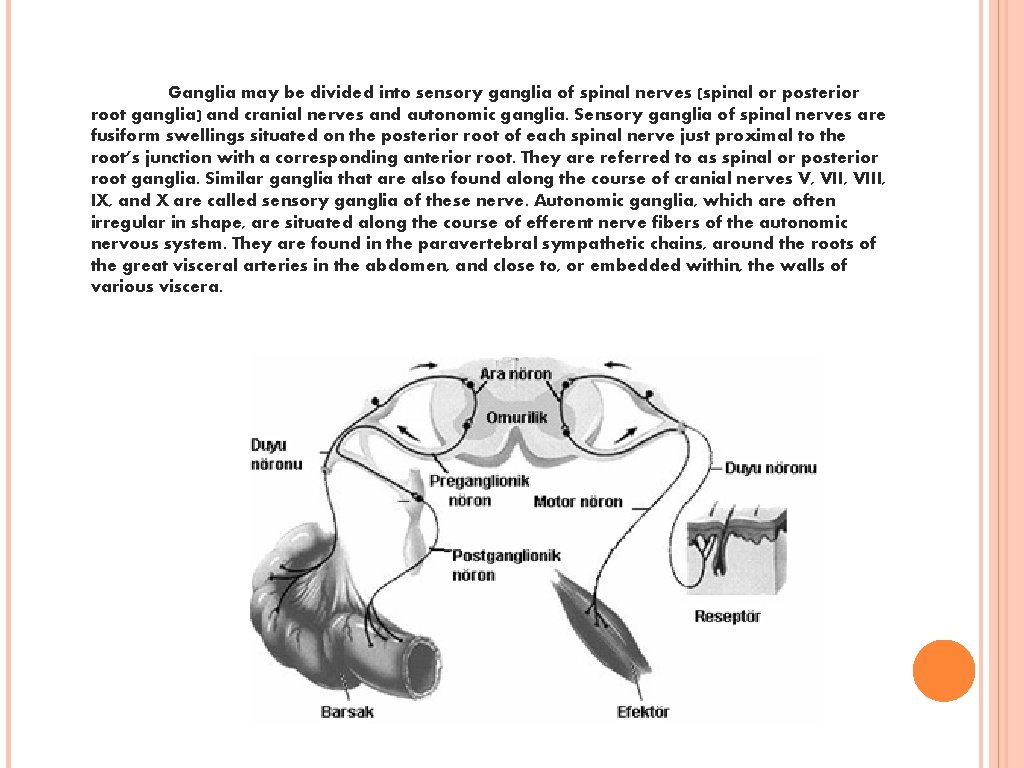
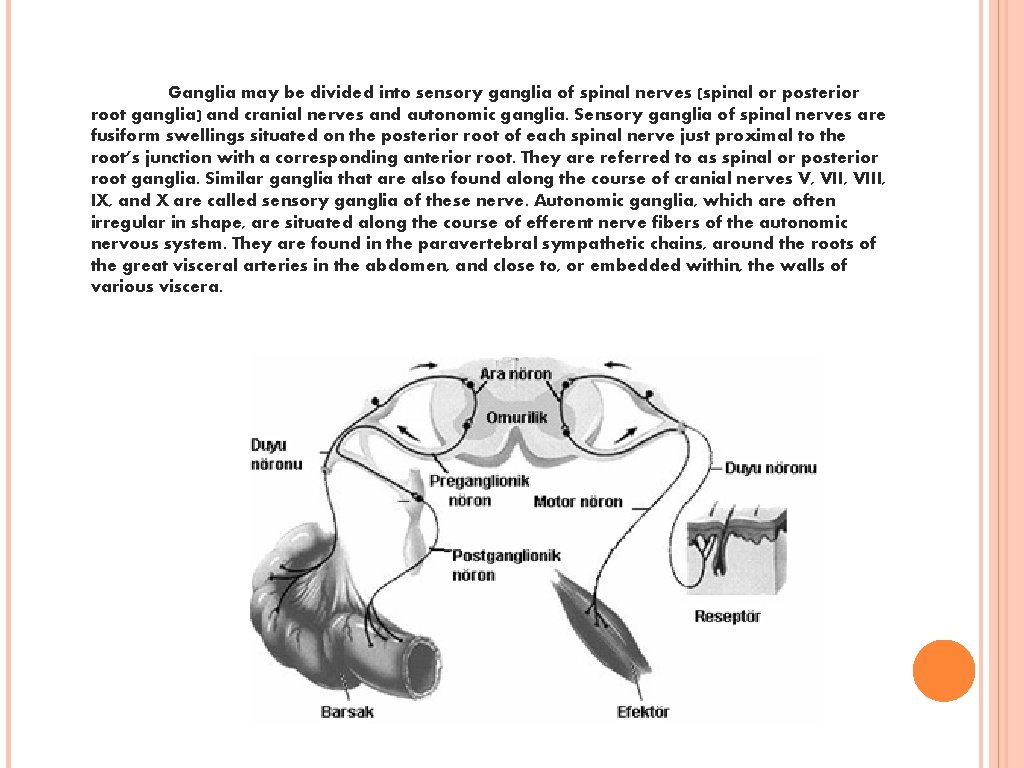
Ganglia may be divided into sensory ganglia of spinal nerves (spinal or posterior root ganglia) and cranial nerves and autonomic ganglia. Sensory ganglia of spinal nerves are fusiform swellings situated on the posterior root of each spinal nerve just proximal to the root’s junction with a corresponding anterior root. They are referred to as spinal or posterior root ganglia. Similar ganglia that are also found along the course of cranial nerves V, VIII, IX, and X are called sensory ganglia of these nerve. Autonomic ganglia, which are often irregular in shape, are situated along the course of efferent nerve fibers of the autonomic nervous system. They are found in the paravertebral sympathetic chains, around the roots of the great visceral arteries in the abdomen, and close to, or embedded within, the walls of various viscera.
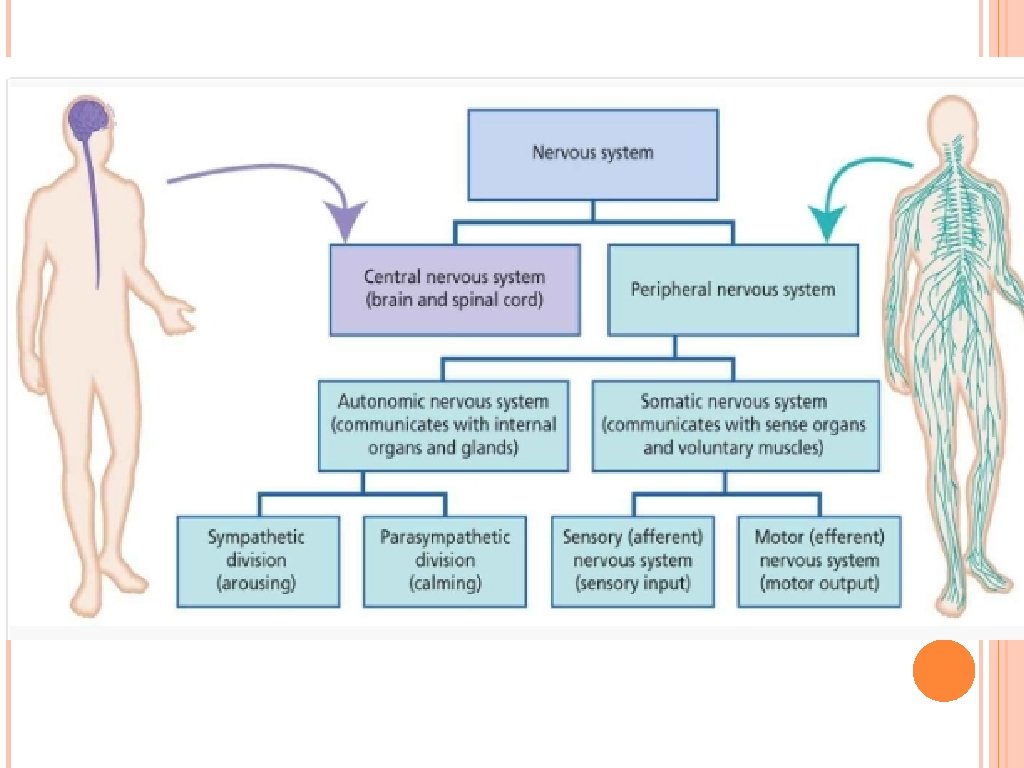
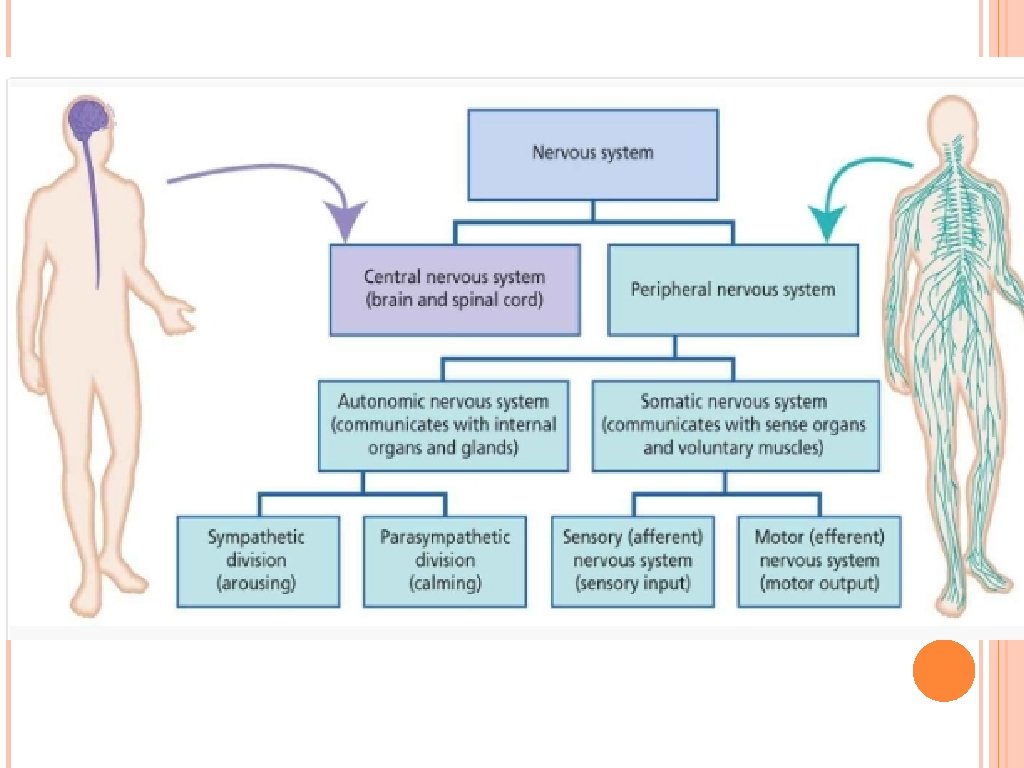
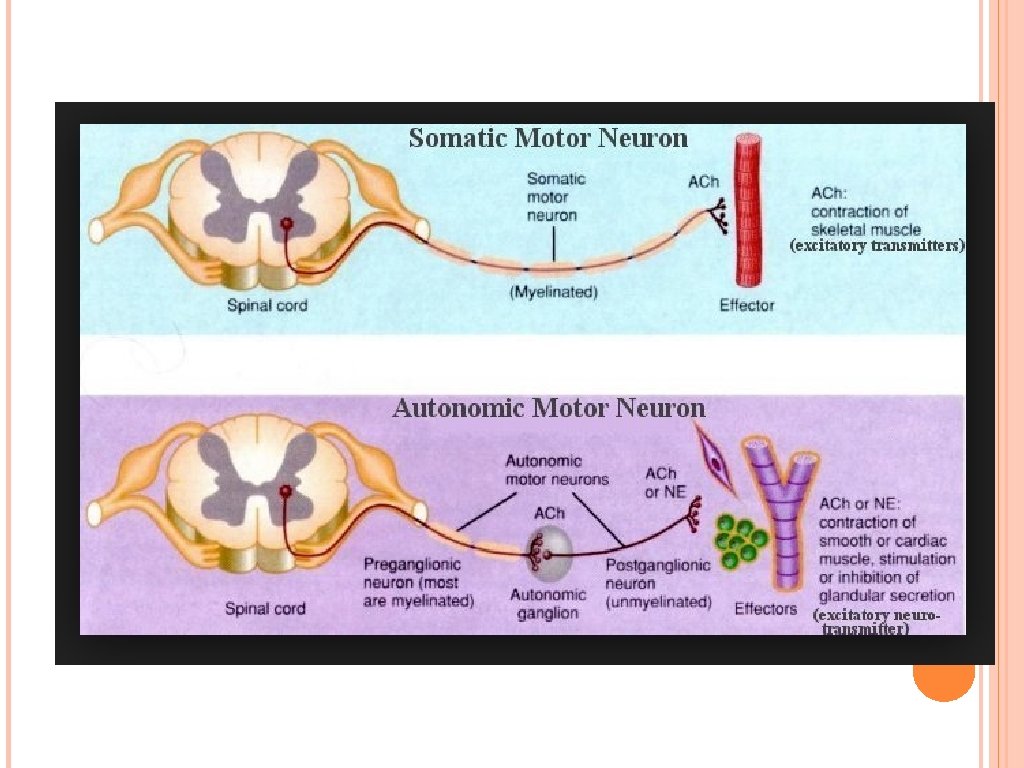
The sensory (afferent) division carries sensory signals by way of afferent nerve fibers from receptors in the central nervous system (CNS). It can be further subdivided into somatic and visceral divisions. The somatic sensory division carries signals from receptors in the skin, muscles, bones and joints. The visceral sensory division carries signals mainly from the viscera of the thoracic and abdominal cavities. The motor (efferent) division carries motor signals by way of efferent nerve fibers from the CNS to effectors (mainly glands and muscles). It can be further subdivided into somatic and visceral divisions. The somatic motor division carries signals to the skeletal muscles. The visceral motor division, also known as the autonomic nervous system, carries signals to glands, cardiac muscle, and smooth muscle. It can be further divided into the sympathetic and parasympathetic divisions. The sympathetic division tends to arouse the body to action. The parasympathetic divisions tend to have a calming effect. Nerve fibers of the PNS are classified according to their involvement in motor or sensory, somatic or visceral pathways. Mixed nerves contain both motor and sensory fibers. Sensory nerves contain mostly sensory fibers; they are less common and include the optic and olfactory nerves. Motor nerves contain motor fibers.
Sensory-somatic nervous system The somatosensory nervous system consists of sensory nerves and somatic nerves, and many nerves which hold both functions. In the head and neck, cranial nerves carry somatosensory data. There are twelve cranial nerves, ten of which originate from the brainstem, and mainly control the functions of the anatomic structures of the head with some exceptions. The nuclei of the olfactory nerve and the optic nerves lie in the forebrain and thalamus, respectively, and are thus not considered to be true cranial nerves. One unique cranial nerve is the vagus nerve, which receives sensory information from organs in the thorax and abdomen. The accessory nerve is responsible for innervating the sternocleidomastoid and trapezius muscles, neither of which being exclusively in the head.
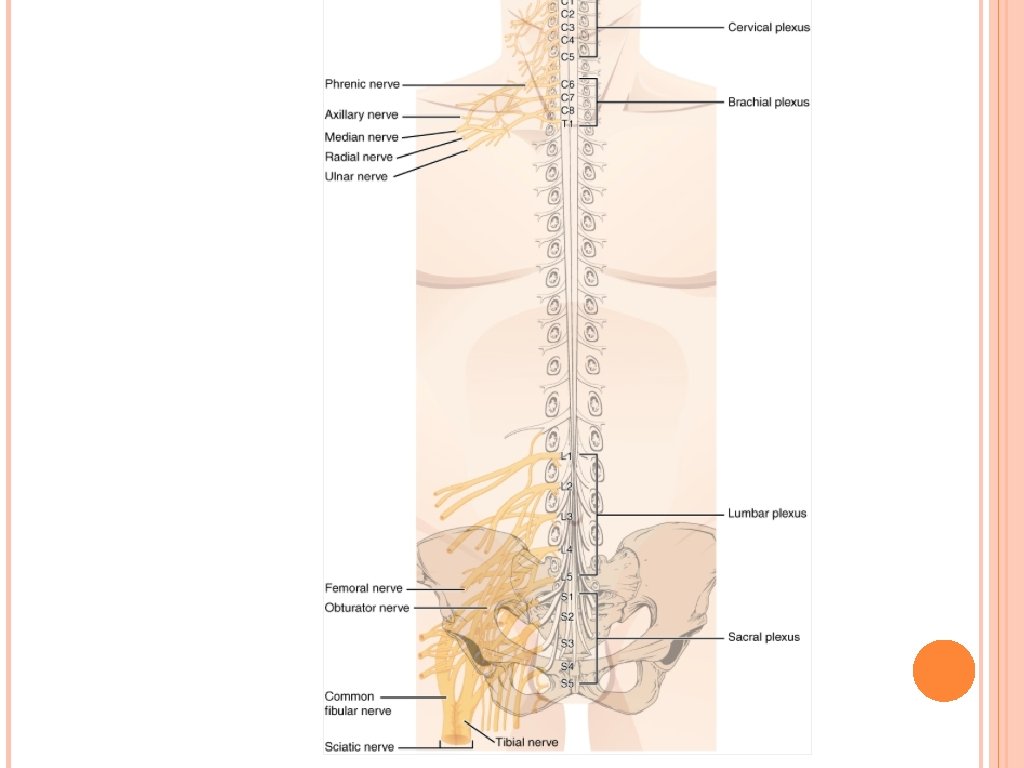
For the rest of the body, spinal nerves are responsible for somatosensory information. The nerves connected to the spinal cord are the spinal nerves. The arrangement of these nerves is much more regular than that of the cranial nerves. All of the spinal nerves are combined sensory and motor axons that separate into two nerve roots. The sensory axons enter the spinal cord as the dorsal nerve root. The motor fibers, both somatic and autonomic, emerge as the ventral nerve root. The dorsal root ganglion for each nerve is an enlargement of the spinal nerve. There are 31 spinal nerves, named for the level of the spinal cord at which each one emerges. There are eight pairs of cervical nerves designated C 1 to C 8, twelve thoracic nerves designated T 1 to T 12, five pairs of lumbar nerves designated L 1 to L 5, five pairs of sacral nerves designated S 1 to S 5, and one pair of coccygeal nerves.
The first nerve, C 1, emerges between the first cervical vertebra and the occipital bone. The second nerve, C 2, emerges between the first and second cervical vertebrae. The same occurs for C 3 to C 7, but C 8 emerges between the seventh cervical vertebra and the first thoracic vertebra. For the thoracic and lumbar nerves, each one emerges between the vertebra that has the same designation and the next vertebra in the column. The sacral nerves emerge from the sacral foramina along the length of that unique vertebra.
Spinal nerves extend outward from the vertebral column to enervate the periphery. The nerves in the periphery are not straight continuations of the spinal nerves, but rather the reorganization of the axons in those nerves to follow different courses. Axons from different spinal nerves will come together into a systemic nerve. This occurs at four places along the length of the vertebral column, each identified as a nerve plexus, whereas the other spinal nerves directly correspond to nerves at their respective levels. In this instance, the word plexus is used to describe networks of nerve fibers with no associated cell bodies.
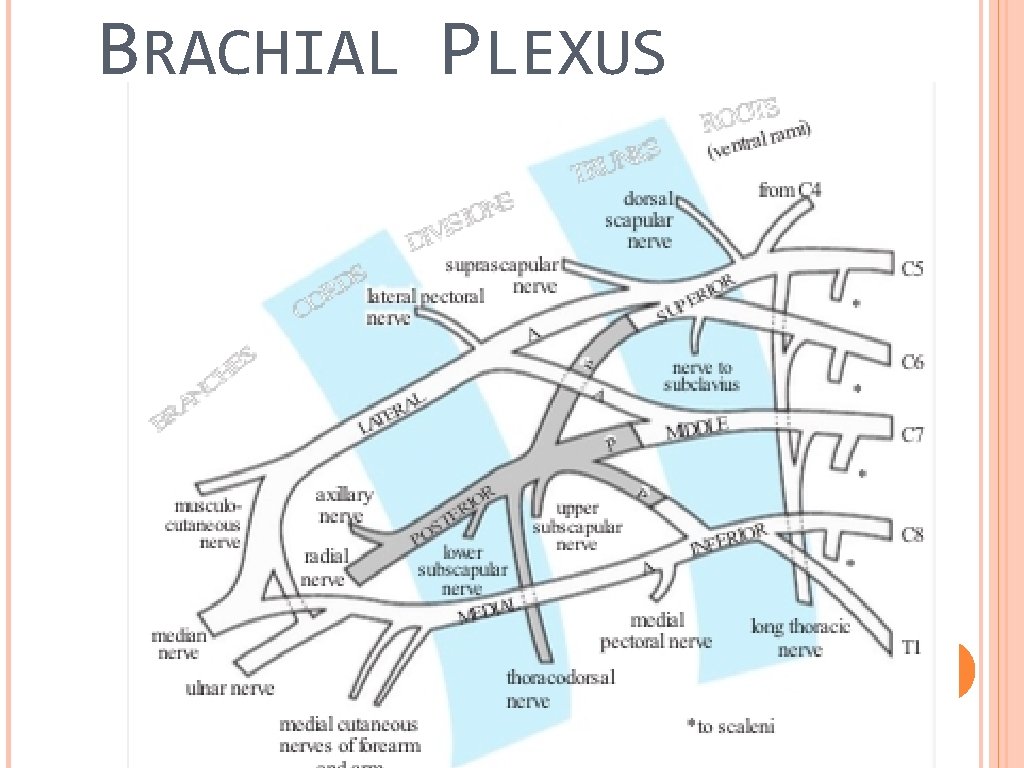
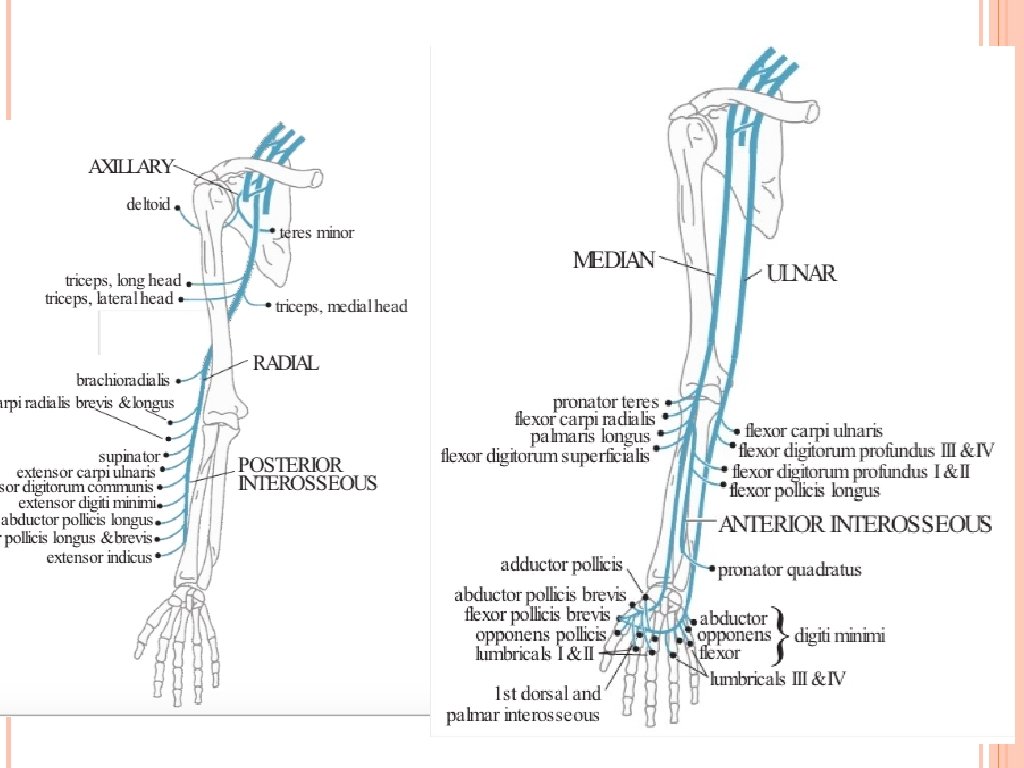
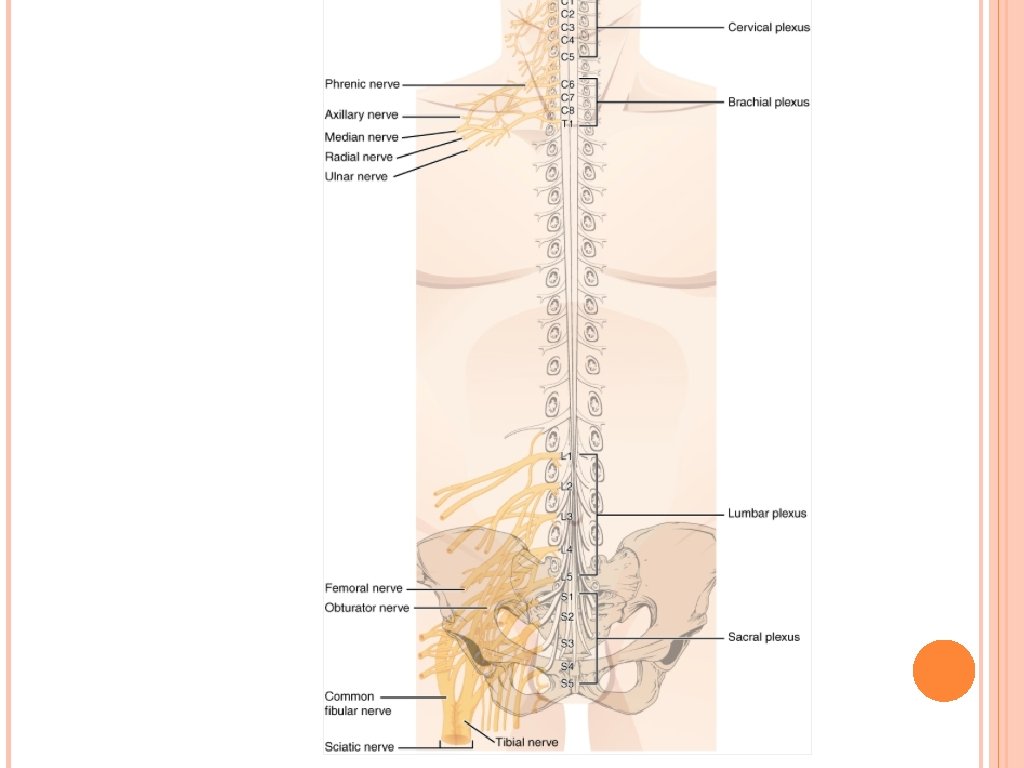
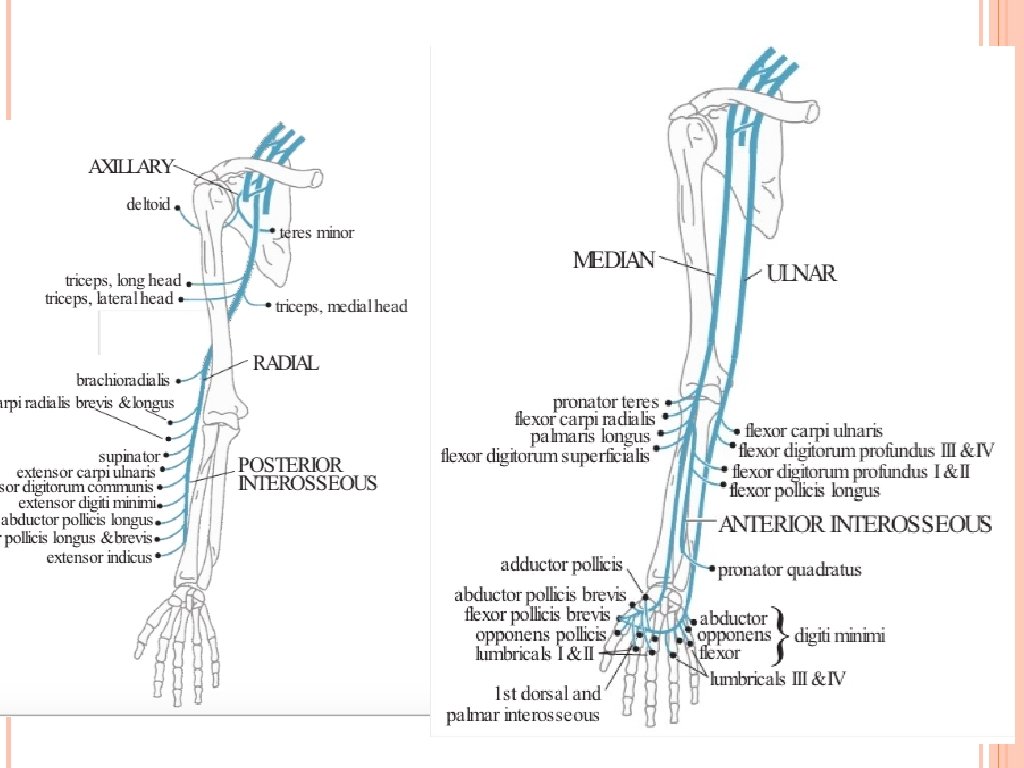
Of the four nerve plexuses, two are found at the cervical level, one at the lumbar level, and one at the sacral level. The cervical plexus is composed of axons from spinal nerves C 1 through C 5 and branches into nerves in the posterior neck and head, as well as the phrenic nerve, which connects to the diaphragm at the base of the thoracic cavity. The other plexus from the cervical level is the brachial plexus. Spinal nerves C 4 through T 1 reorganize through this plexus to give rise to the nerves of the arms, as the name brachial suggests. A large nerve from this plexus is the radial nerve from which the axillary nerve branches to go to the armpit region. The radial nerve continues through the arm and is paralleled by the ulnar nerve and the median nerve.
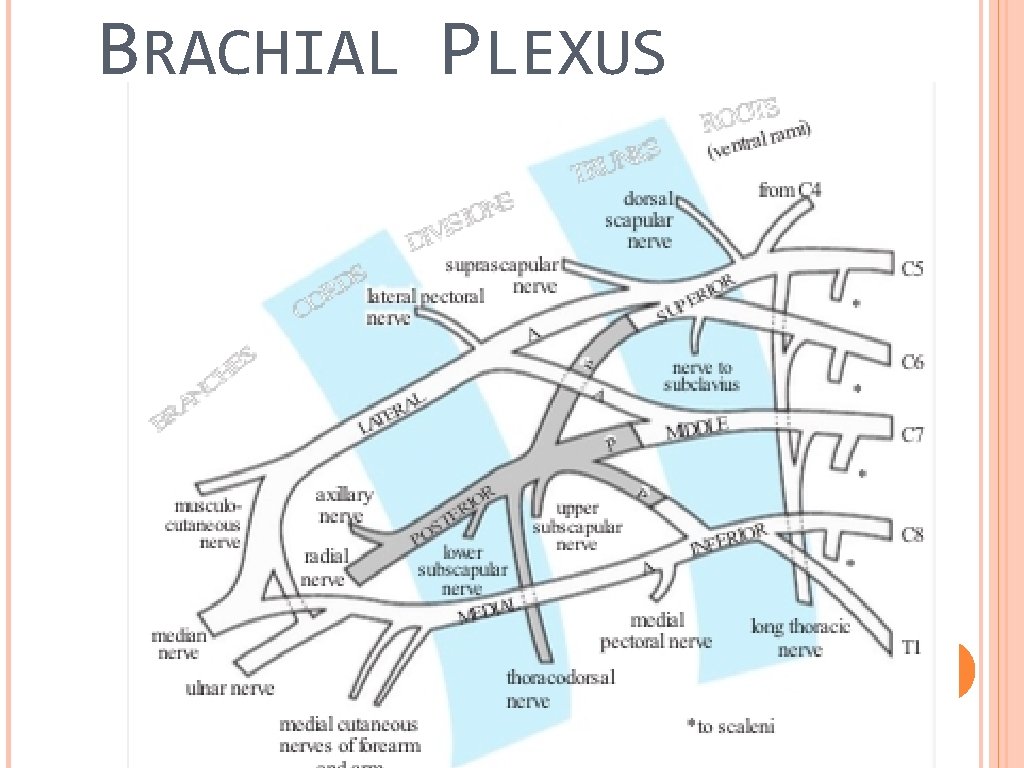
BRACHIAL PLEXUS
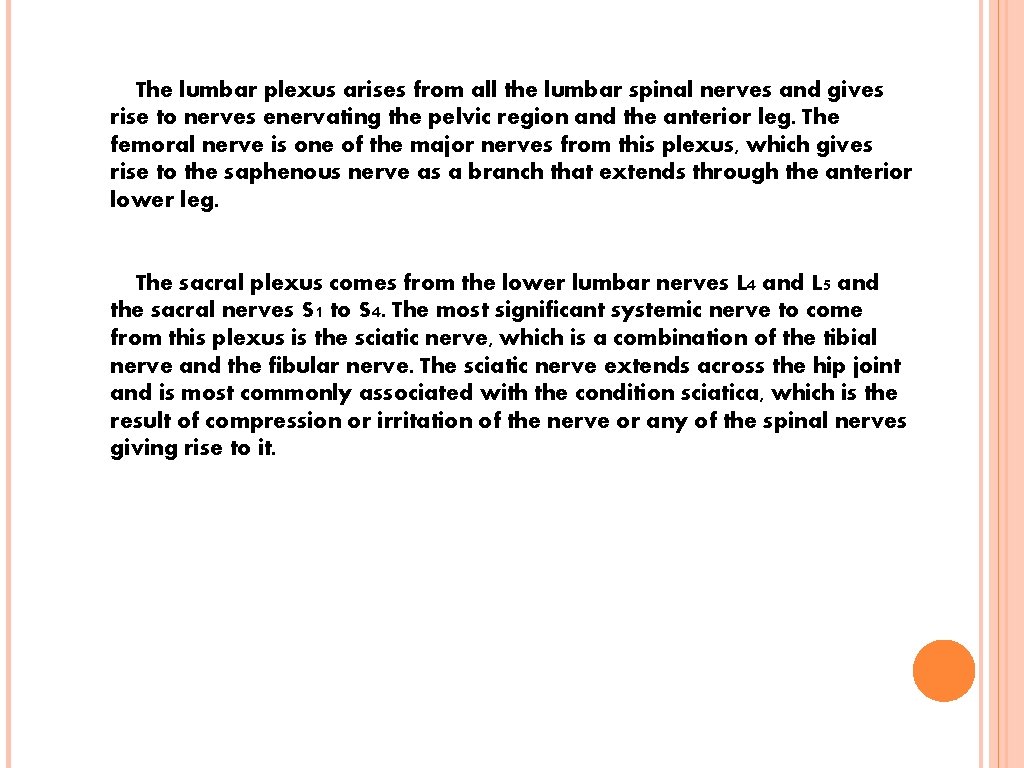
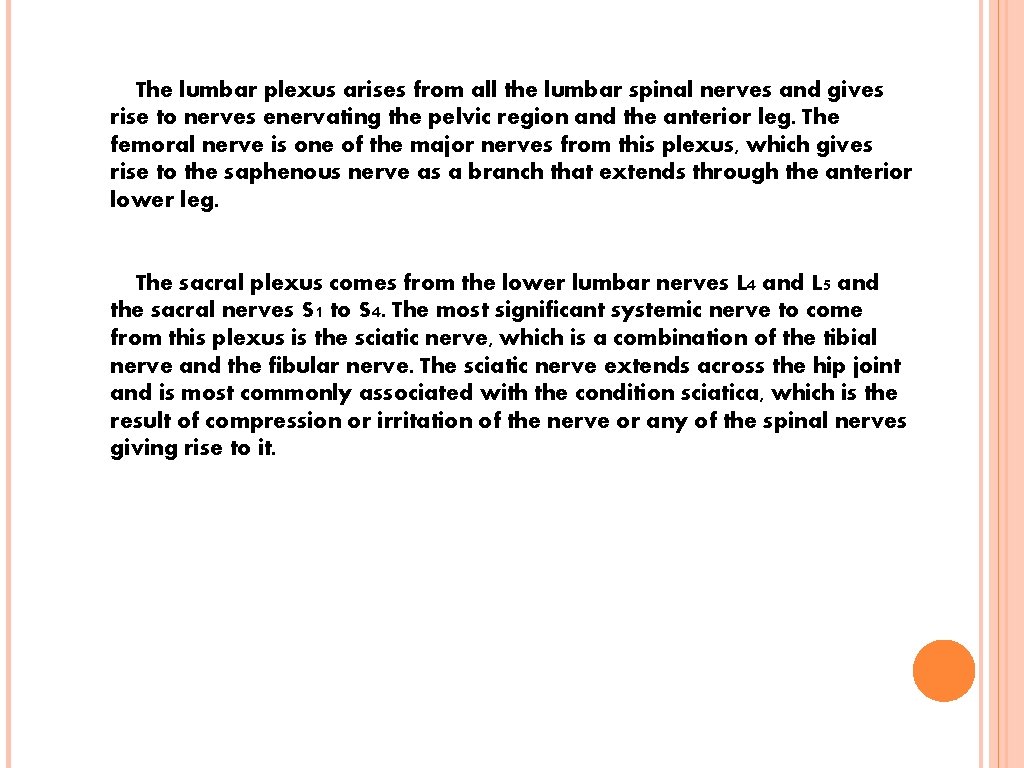
The lumbar plexus arises from all the lumbar spinal nerves and gives rise to nerves enervating the pelvic region and the anterior leg. The femoral nerve is one of the major nerves from this plexus, which gives rise to the saphenous nerve as a branch that extends through the anterior lower leg. The sacral plexus comes from the lower lumbar nerves L 4 and L 5 and the sacral nerves S 1 to S 4. The most significant systemic nerve to come from this plexus is the sciatic nerve, which is a combination of the tibial nerve and the fibular nerve. The sciatic nerve extends across the hip joint and is most commonly associated with the condition sciatica, which is the result of compression or irritation of the nerve or any of the spinal nerves giving rise to it.
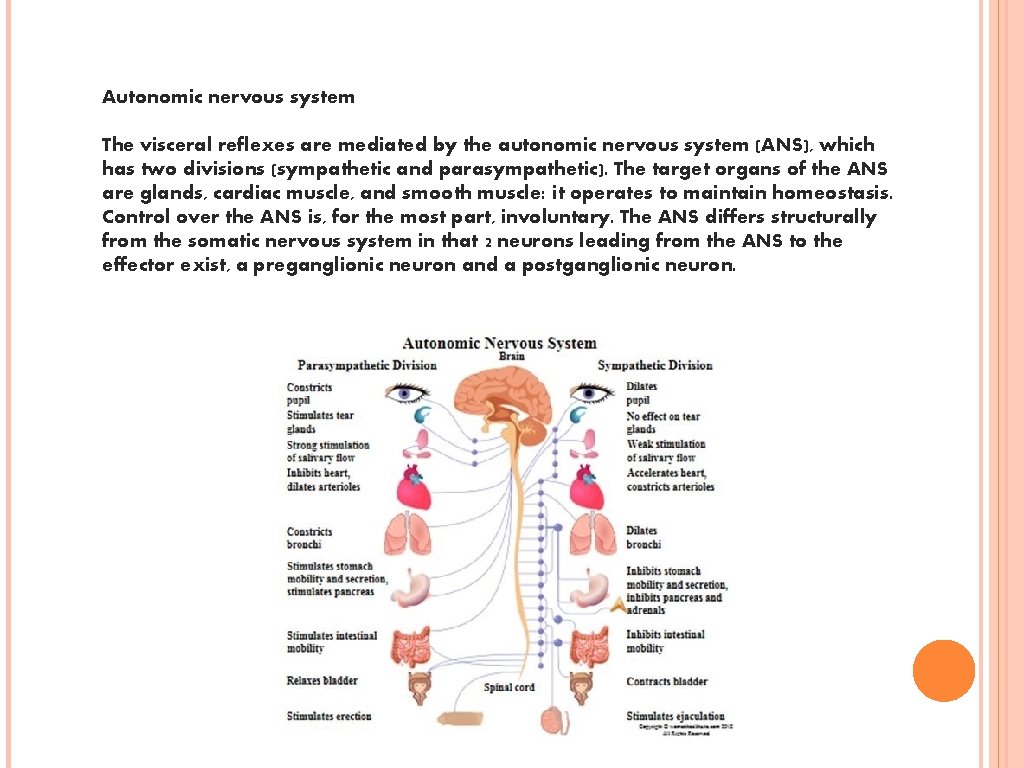
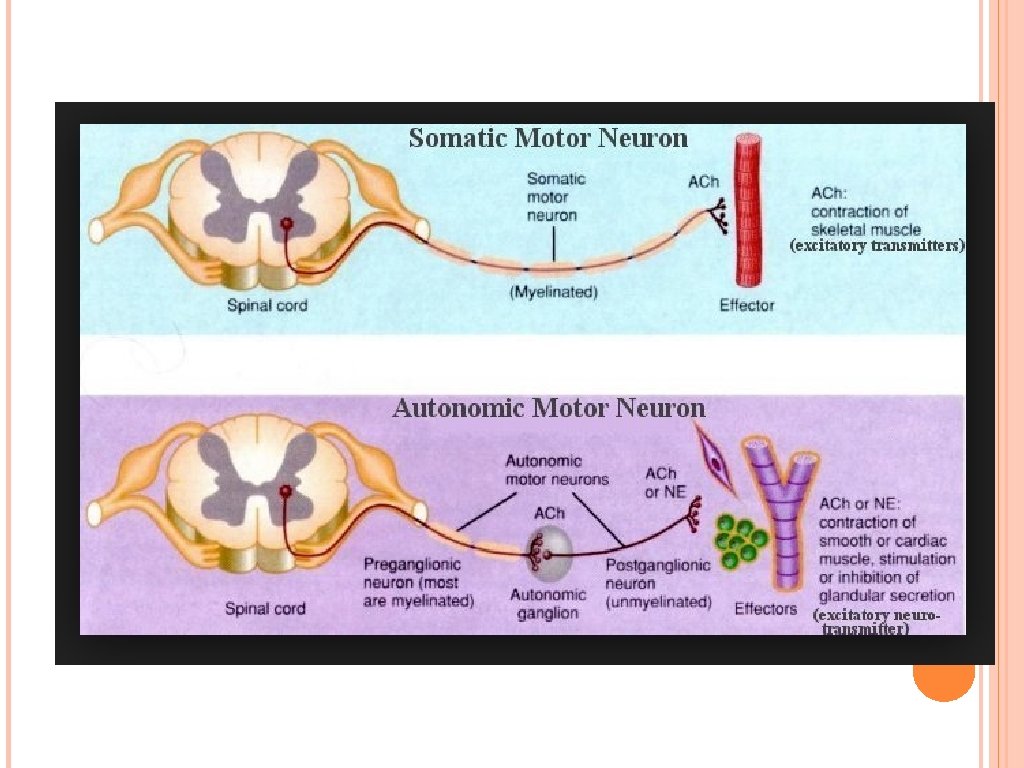
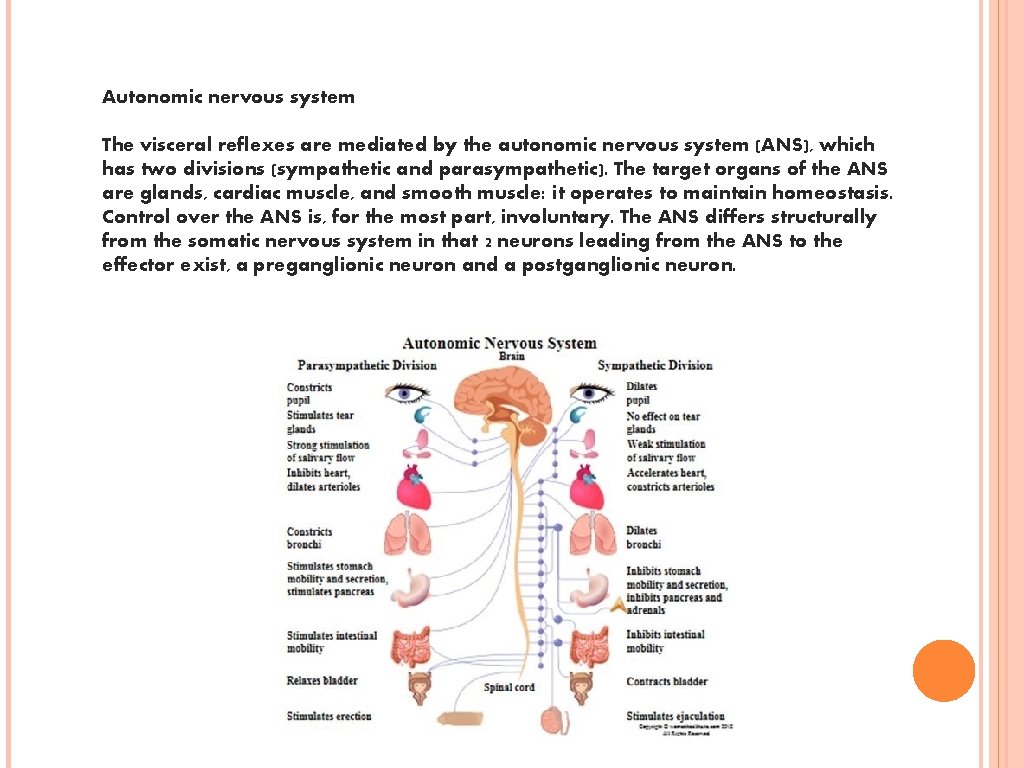
Autonomic nervous system The visceral reflexes are mediated by the autonomic nervous system (ANS), which has two divisions (sympathetic and parasympathetic). The target organs of the ANS are glands, cardiac muscle, and smooth muscle: it operates to maintain homeostasis. Control over the ANS is, for the most part, involuntary. The ANS differs structurally from the somatic nervous system in that 2 neurons leading from the ANS to the effector exist, a preganglionic neuron and a postganglionic neuron.
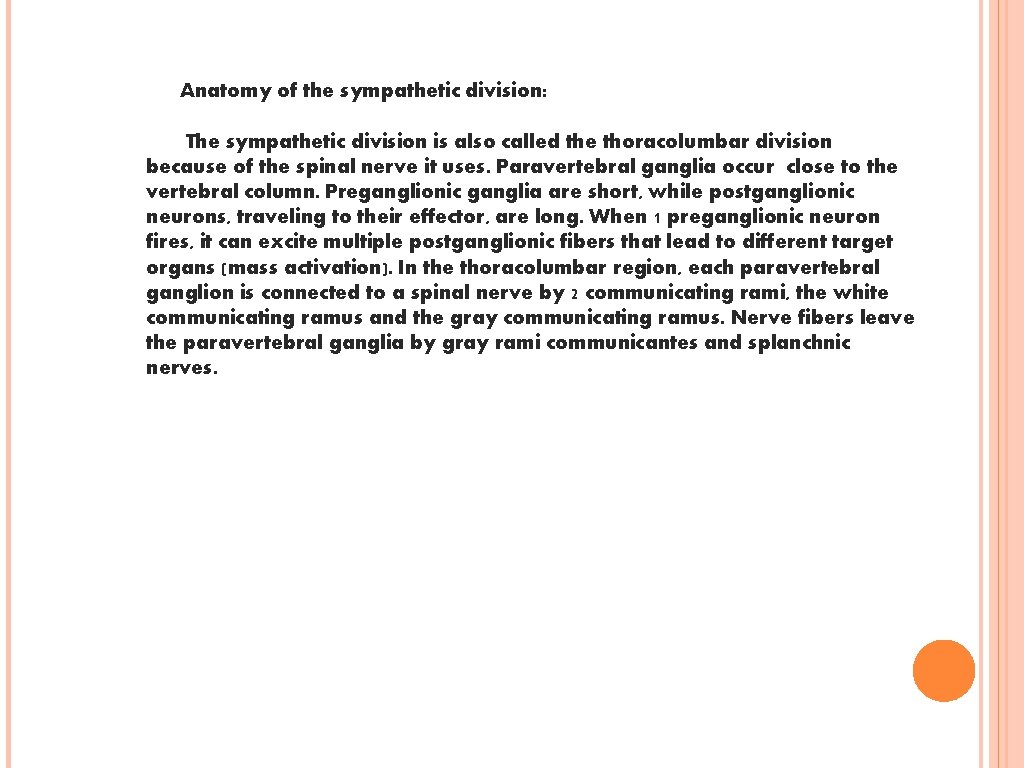
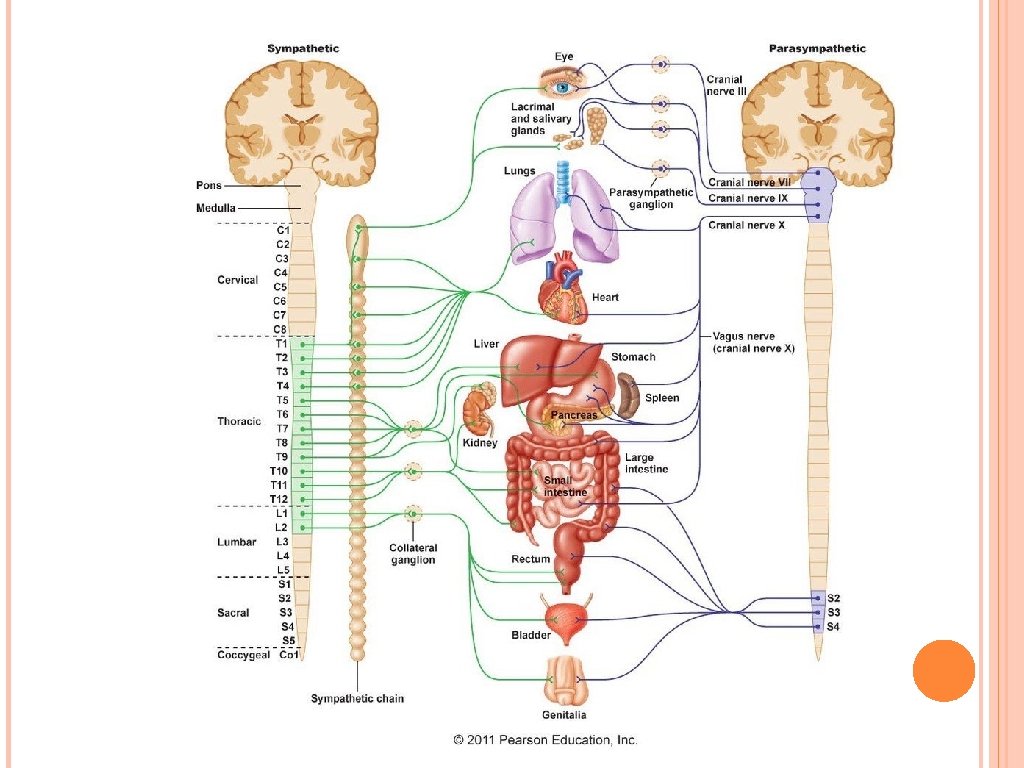
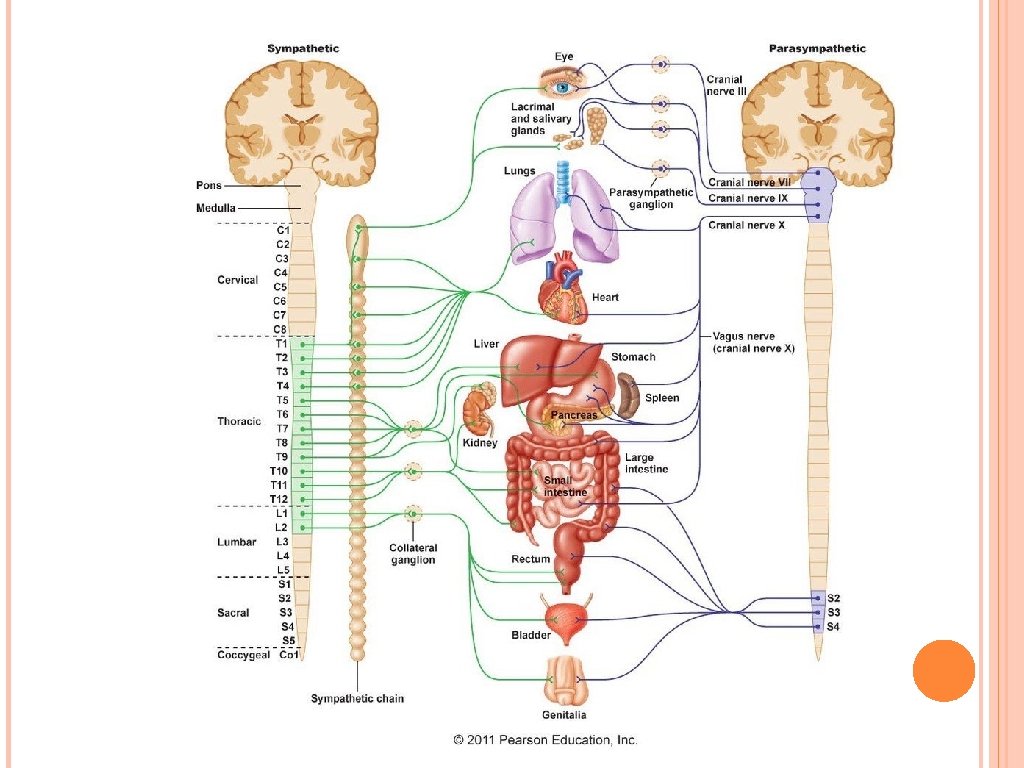
Anatomy of the sympathetic division: The sympathetic division is also called the thoracolumbar division because of the spinal nerve it uses. Paravertebral ganglia occur close to the vertebral column. Preganglionic ganglia are short, while postganglionic neurons, traveling to their effector, are long. When 1 preganglionic neuron fires, it can excite multiple postganglionic fibers that lead to different target organs (mass activation). In the thoracolumbar region, each paravertebral ganglion is connected to a spinal nerve by 2 communicating rami, the white communicating ramus and the gray communicating ramus. Nerve fibers leave the paravertebral ganglia by gray rami communicantes and splanchnic nerves.
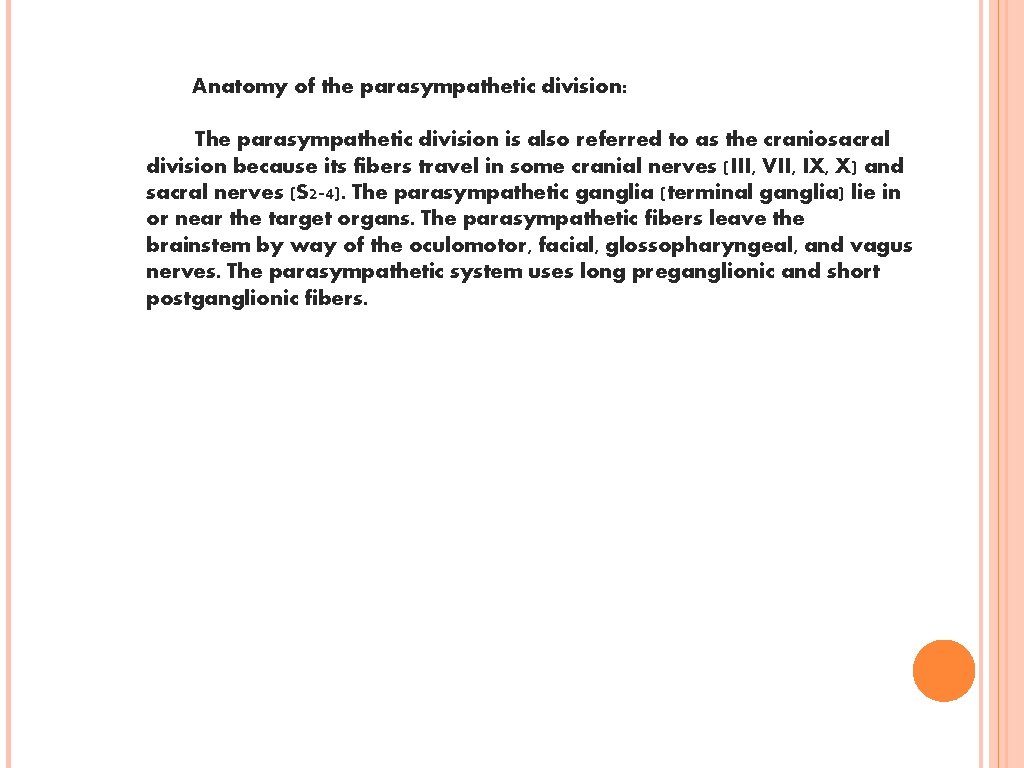
Anatomy of the parasympathetic division: The parasympathetic division is also referred to as the craniosacral division because its fibers travel in some cranial nerves (III, VII, IX, X) and sacral nerves (S 2 -4). The parasympathetic ganglia (terminal ganglia) lie in or near the target organs. The parasympathetic fibers leave the brainstem by way of the oculomotor, facial, glossopharyngeal, and vagus nerves. The parasympathetic system uses long preganglionic and short postganglionic fibers.
Entrapment Neuropathies Entrapment neuropathy is a peripheral nerve injury resulting from compression either by external forces or from nearby anatomic structures. Mechanism can vary from one or two significant compressive insults to many localized, repetitive mild compressions of a nerve. The most common symptom is pain (frequently at rest, more severe at night, often with retrograde radiation causing more proximal lesion to be suspected) with tenderness at the point of entrapment. Referred pain is so common.
Always consider the possibility of a systemic cause. Entrapment neuropathies may be associated with: 1. diabetes mellitus 2. hypothyroidism: due to glycogen deposition in Schwann cells 3. acromegaly 4. amyloidosis: primary or secondary (as in multiple myeloma) 5. carcinomatosis 6. polymyalgia rheumatica 7. RA 8. gout
Carpal Tunnel Syndrome Carpal tunnel syndrome (CTS) is the most common entrapment neuropathy in the upper extremity at the level of transverse carpal ligament. Carpal tunnel syndrome (CTS) is a collection of characteristic symptoms and signs that occurs following compression of the median nerve within the carpal tunnel. Usual symptoms include numbness, paresthesias, and pain in the median nerve distribution. Usually occurs in middle aged patients. Ratio of female: male =4: 1
Etiology Age Female gender Menopause Local trauma(Colles fr. ) systemic conditions: RA, diabetes obesity pregnancy and breastfeeding tuberculous tenosynovitis amyloidosis multiple myeloma pts with a-v dialysis shunt in forearm acute CTS: -median artery thrombosis -hemorrhage or hematom in the tr. carpal lig.
History Numbness and tingling Pain Autonomic Symptoms that temperature and skin color changes Weakness and clumsiness loss of power n the hand
Physical Examination Sensory examination: Abnormalities in sensory modalities may be present on the palmar aspect of the first 3 digits and radial one half of the fourth digit. Sensory examination is most useful in confirming that areas outside the distal median nerve territory are normal (eg, thenar eminence, hypothenar eminence, dorsum of first web space).
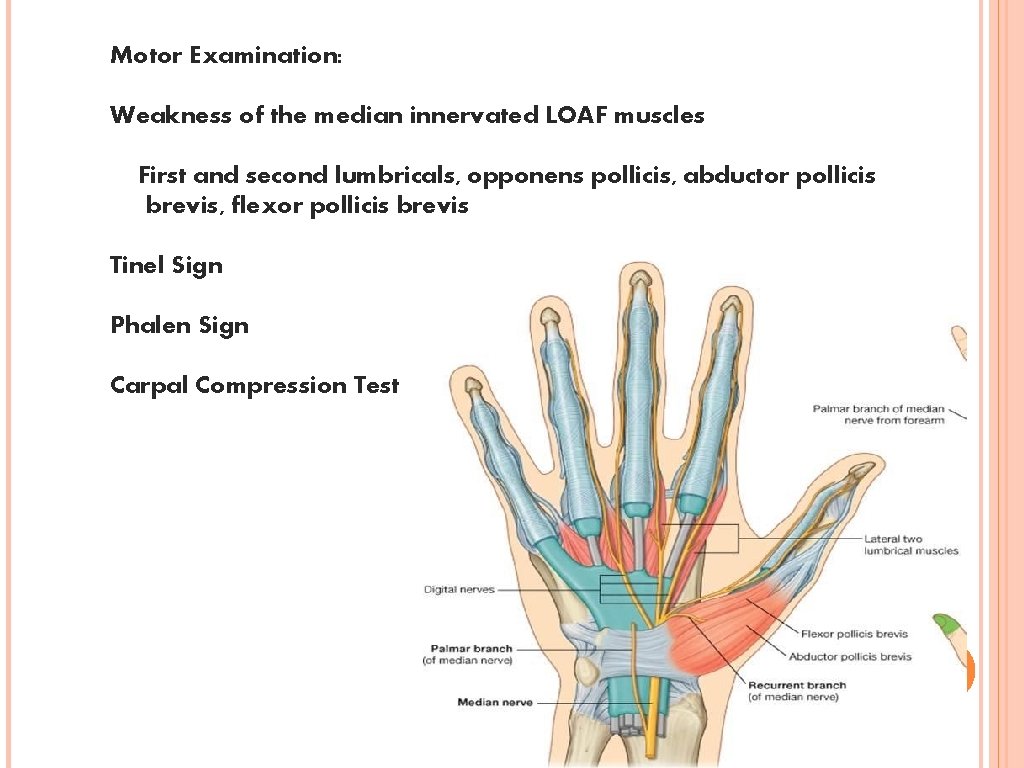
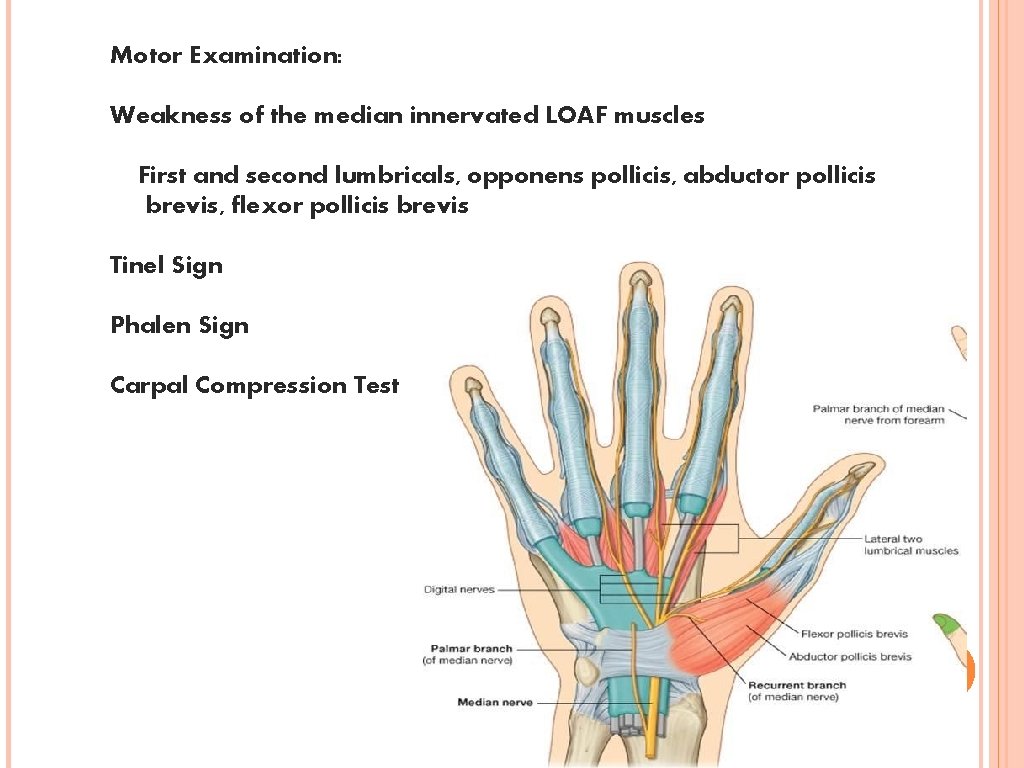
Motor Examination: Weakness of the median innervated LOAF muscles First and second lumbricals, opponens pollicis, abductor pollicis brevis, flexor pollicis brevis Tinel Sign Phalen Sign Carpal Compression Test
Laboratory tests Recommended in cases where an underlying peripheral neuropathy is suspected (e. g. unclear etiol- ogy in a young individual with no risk factors such as repetitive hand use). This same protocol is a useful initial workup for any case of peripheral neuropathy: 1. thyroid hormone levels (T 4 (total or free) &TSH): to R/O myxedema 2. CBC: anemia is common in multiple myeloma, also to R/O amyloidosis 3. electrolytes: 4. MM investigation:
Electrophysiologic studies, including electromyography (EMG) and nerve conductions studies (NCS), are the first-line investigations in suggested carpal tunnel syndrome (CTS). Abnormalities on electrophysiologic testing, in association with specific symptoms and signs, are considered the criterion standard for CTS diagnosis. In addition, other neurologic diagnoses can be excluded with these test results. CTS is predominantly a demyelinating injury although it can progress to axonal loss. No imaging studies are considered routine in diagnosis of CTS.
Treatment Physical Therapy Wrist splints with the wrist joint in neutral or slight extension (to be worn at nighttime for a minimum of 3 -4 wk) Steroid injection into the carpal tunnel The anticonvulsants gabapentin and pregabalin for the neuropathic pain Nonsteroidal anti-inflammatory drugs (NSAIDs) and/or diuretics Oral drugs are not effective
Surgical Treatment Indications Surgical intervention is recommended for: constant numbness, symptoms >1 year duration, sensory loss, or thenar weakness/atrophy. Surgical treatment of cases due to amyloidosis from multiple myeloma is also effective. Surgical release of the transverse ligament Neuroplasty of the median nerve at wrist Outcome: %75 -90
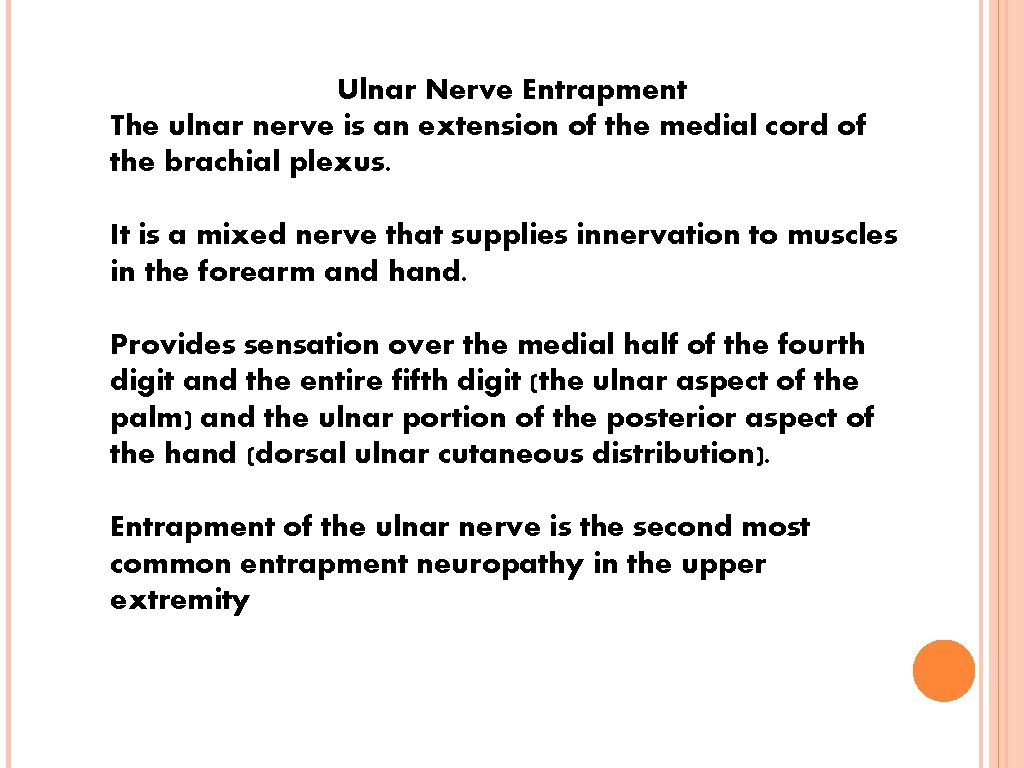
Ulnar Nerve Entrapment The ulnar nerve is an extension of the medial cord of the brachial plexus. It is a mixed nerve that supplies innervation to muscles in the forearm and hand. Provides sensation over the medial half of the fourth digit and the entire fifth digit (the ulnar aspect of the palm) and the ulnar portion of the posterior aspect of the hand (dorsal ulnar cutaneous distribution). Entrapment of the ulnar nerve is the second most common entrapment neuropathy in the upper extremity
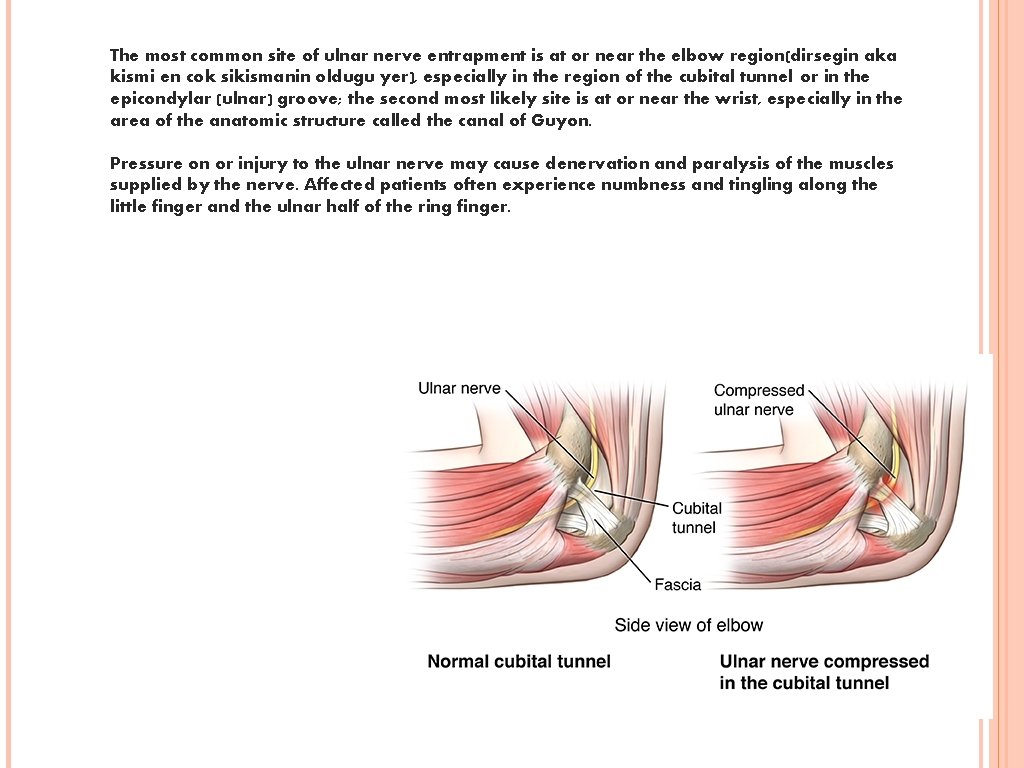
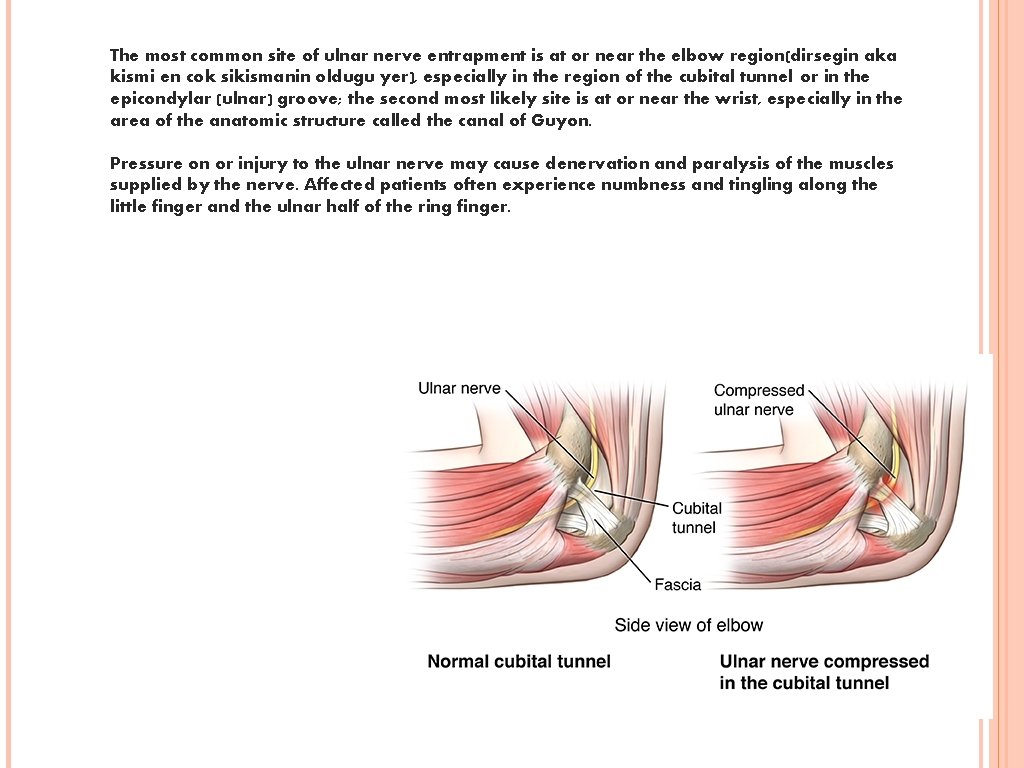
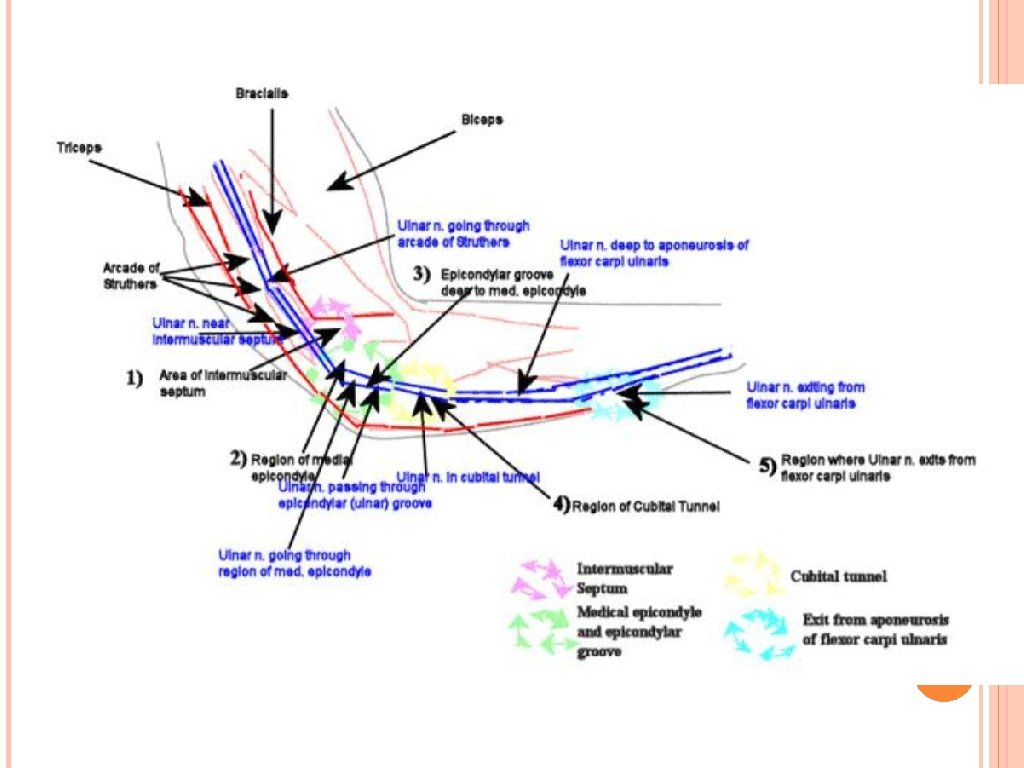
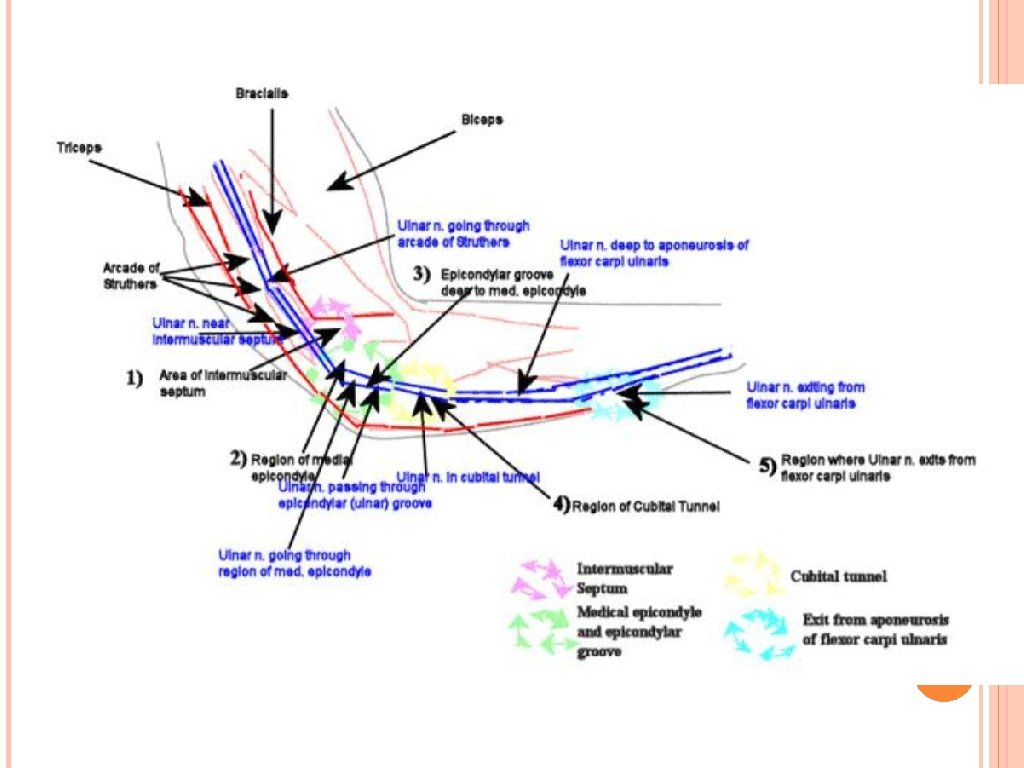
The most common site of ulnar nerve entrapment is at or near the elbow region(dirsegin aka kismi en cok sikismanin oldugu yer), especially in the region of the cubital tunnel or in the epicondylar (ulnar) groove; the second most likely site is at or near the wrist, especially in the area of the anatomic structure called the canal of Guyon. Pressure on or injury to the ulnar nerve may cause denervation and paralysis of the muscles supplied by the nerve. Affected patients often experience numbness and tingling along the little finger and the ulnar half of the ring finger.
Factors that may cause ulnar neuropathy Compression during general anesthesia Trauma, fractures Deformities like RA Diabetes Subdermal contraceptive implants Venipuncture Hemophilia Cigarette smoking Tumors
Clinic Many patients complain of sensory changes in the fourth and fifth digits. Pain rarely occurs in the hand. Complaints of pain tend to be more common in the arm, up to and including the elbow area. Indeed, the elbow is probably the most common site of pain in an ulnar neuropathy. Claw deformity of the hand Wartenberg’s sign: one of the earliest findings of ulnar nerve entrapment (abducted little finger due to weakness of the third palmar interosseous muscle–patient may complain that the little finger doesn’t make it in when they reach into their pocket) kucuk parmagın kapanamaması Muscle atrophy (it looks older) Weakness (my grip is weak) because mostly the grip muscles are innervated by ulnar nerves
Physical Examination Check elbow range of motion, and examine the carrying angle; look for areas of tenderness or ulnar nerve subluxation Check for the Tinel sign - This sign is typically present in individuals with cubital tunnel syndrome; positive tinel sign at elbow Perform an elbow flexion test - This test, generally considered the best diagnostic test for cubital tunnel syndrome Palpate the cubital tunnel region to exclude mass lesions Check grip and pinch strength Check 2 -point discrimination Evaluate sensation, especially the area on the ulnar dorsum of the hand supplied by the dorsal ulnar sensory nerve - Hypoesthesia in this area suggests a lesion proximal to the canal of Guyon
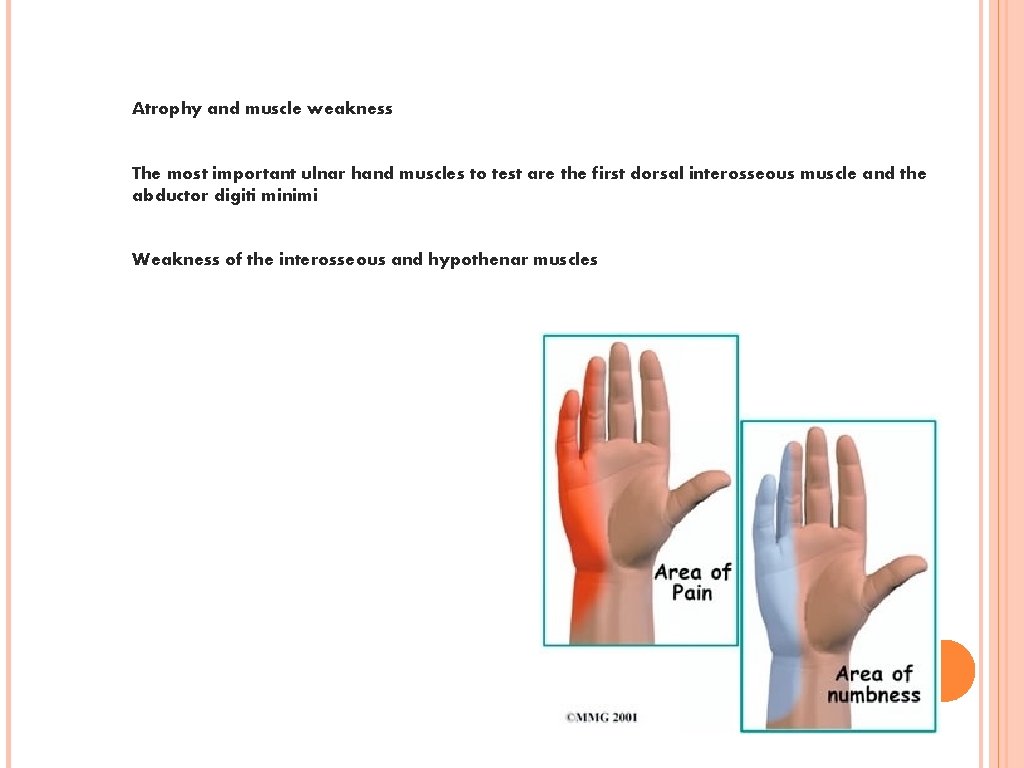
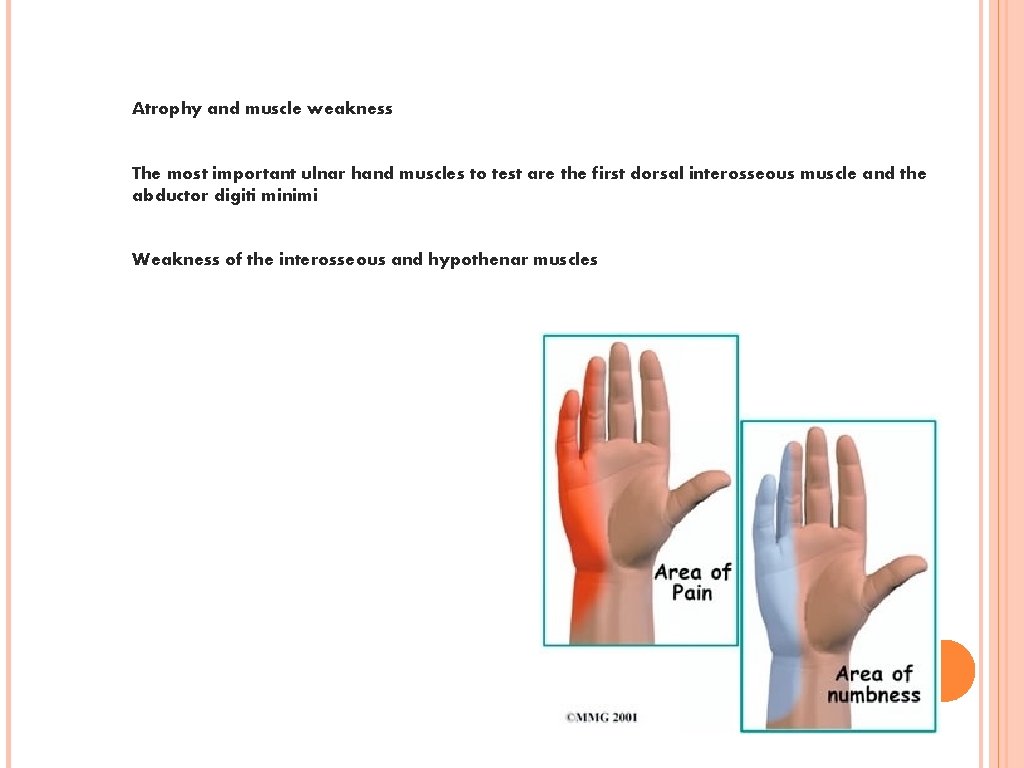
Atrophy and muscle weakness The most important ulnar hand muscles to test are the first dorsal interosseous muscle and the abductor digiti minimi Weakness of the interosseous and hypothenar muscles
Evaluation Lab Studies CBC, Urinanalysis, fasting glucose level, ANA, ESR, thyroid function tests, VIT B 12 B 6, … to rule out systemic diseases US Unlike computed tomography (CT) or magnetic resonance imaging (MRI), ultrasonography provides real time evaluation of nerve displacement or compression during movements of adjacent joints
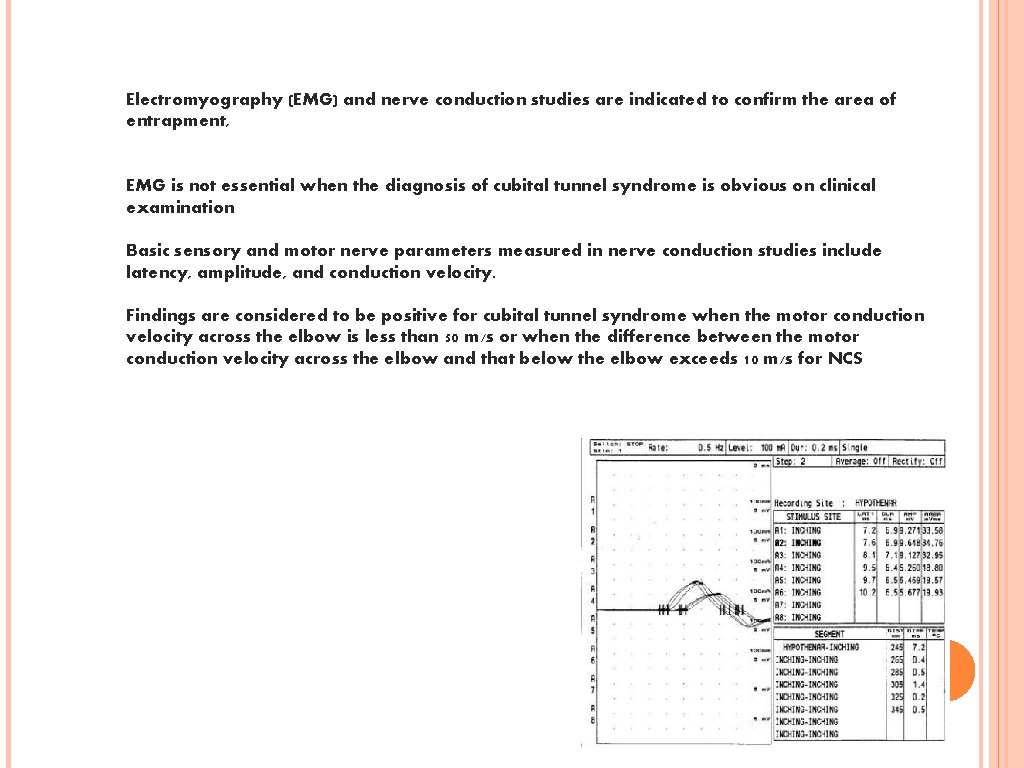
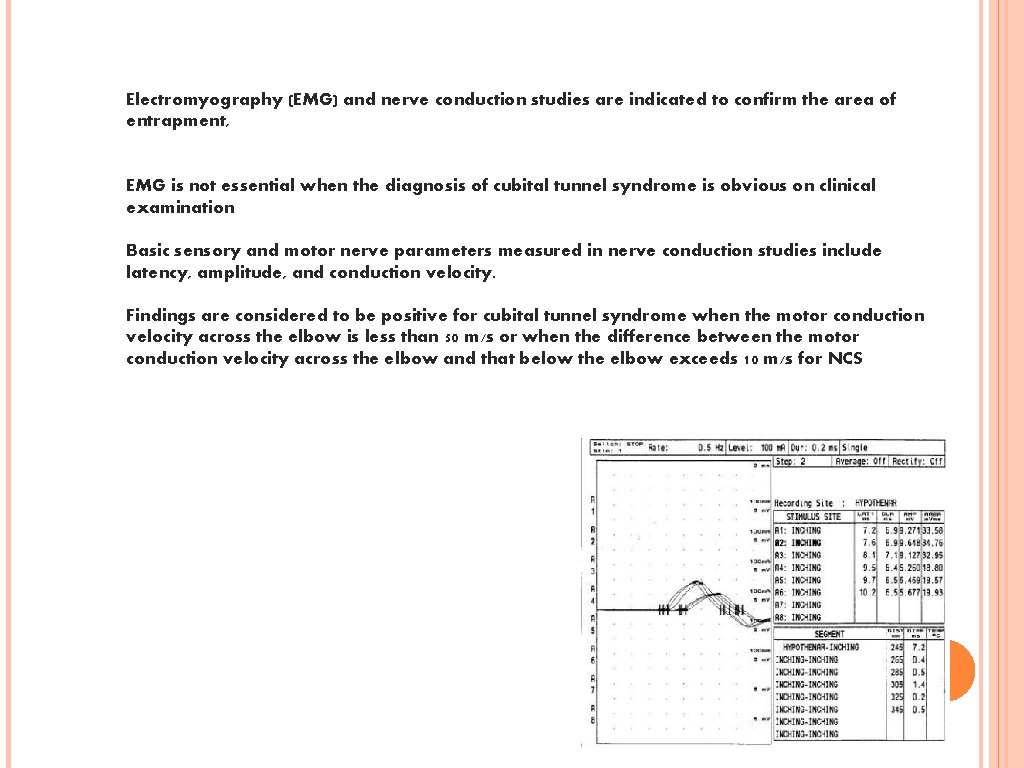
Electromyography (EMG) and nerve conduction studies are indicated to confirm the area of entrapment, EMG is not essential when the diagnosis of cubital tunnel syndrome is obvious on clinical examination Basic sensory and motor nerve parameters measured in nerve conduction studies include latency, amplitude, and conduction velocity. Findings are considered to be positive for cubital tunnel syndrome when the motor conduction velocity across the elbow is less than 50 m/s or when the difference between the motor conduction velocity across the elbow and that below the elbow exceeds 10 m/s for NCS
Nonsurgical therapy(NSAID, TCA, antiarrythmics class 1 b, opioids, pregabalin gabapentin…) may be helpful in many cases of ulnar neuropathy. If conservative therapy fails, surgical treatment is warranted, typically involving one of the following procedures Decompression in situ Decompression with anterior transposition Medial Epicondylectomy Endoscopic Cubital Tunnel Release Indications for surgery for ulnar nerve entrapment: No improvement in presenting symptoms after 6 -12 weeks of conservative treatment Progressive palsy or paralysis Clinical evidence of a long-standing lesion (eg, muscle wasting or clawing of the fourth and fifth digits)
Radial Nerve Entrapment Radial nerve compression or injury may occur at any point along the anatomic course of the nerve and may have varied etiologies. Compression or scarring of the radial nerve at different points along its course may cause denervation of extensor or supinator muscles and numbness or paresthesias in the distribution of the radial sensory nerve (RSN)
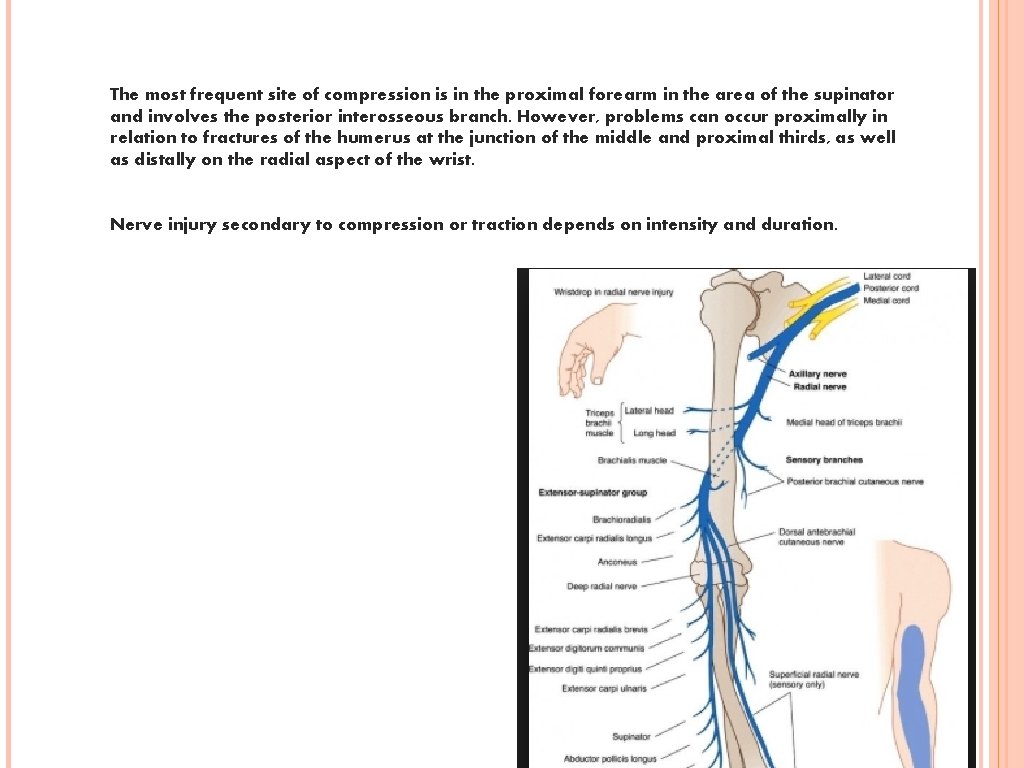
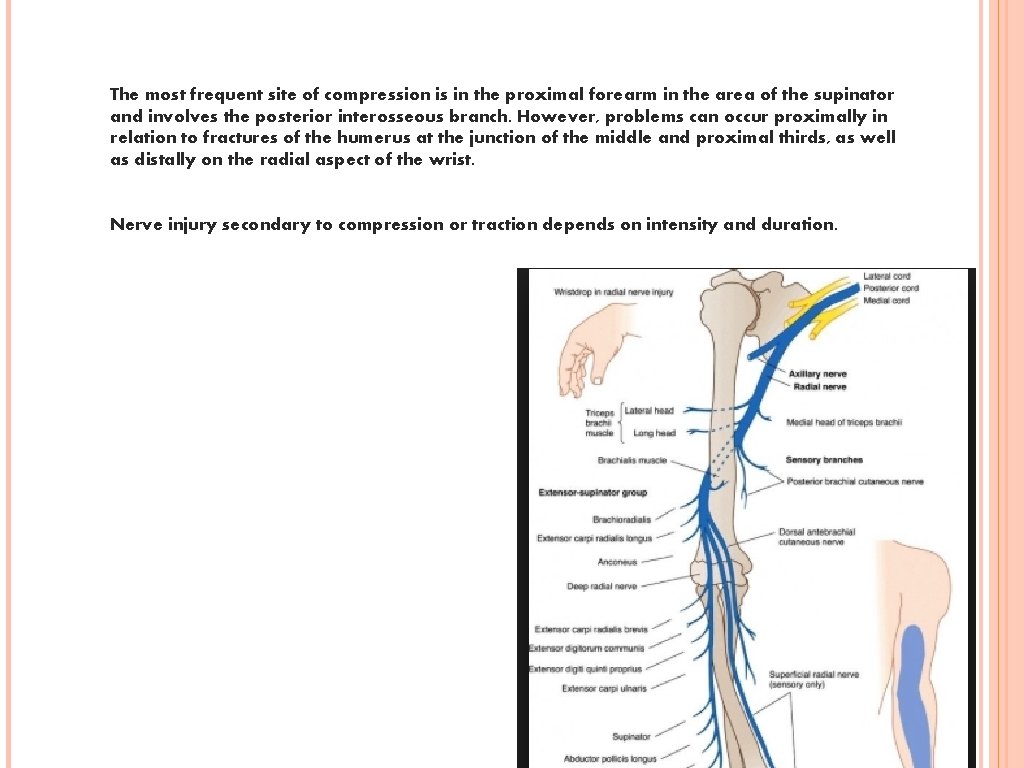
The most frequent site of compression is in the proximal forearm in the area of the supinator and involves the posterior interosseous branch. However, problems can occur proximally in relation to fractures of the humerus at the junction of the middle and proximal thirds, as well as distally on the radial aspect of the wrist. Nerve injury secondary to compression or traction depends on intensity and duration.

Etiology Radial nerve palsy in the arm most commonly is caused by fracture of the humerus, especially in the middle third (Holstein-Lewis fracture) or at the junction of the middle and distal thirds. Radial tunnel syndrome: result of overuse synovitis(rheumatoid) tumors iatrogenic injuries axillary and mid upper arm compression (saturday night palsy) positioning under general anesthesia The anatomic site of compression corresponds to the transit of the nerve from its submuscular position beneath the brachioradialis to its subcutaneous position on the extensor carpi radialis longus. Especially with pronation, these two muscles can create a scissorlike effect, compressing the RSN. Sites of compression include the fibrous bands attached to the radiocapitellar joint, radial recurrent vessels, the tendinous origin of the extensor carpi radialis brevis, the tendinous origin of the supinator (ie, arcade of Frohse), and fibrous thickenings within and at the distal margin of the supinator.
Presentation Radial Nerve Palsy Radial nerve palsy in the middle third of the arm is characterized by palsy or paralysis of all extensors of the wrist and digits, as well as the forearm supinators. Numbness occurs on the dorsoradial aspect of the hand the dorsal aspect of the radial three-and-ahalf digits.
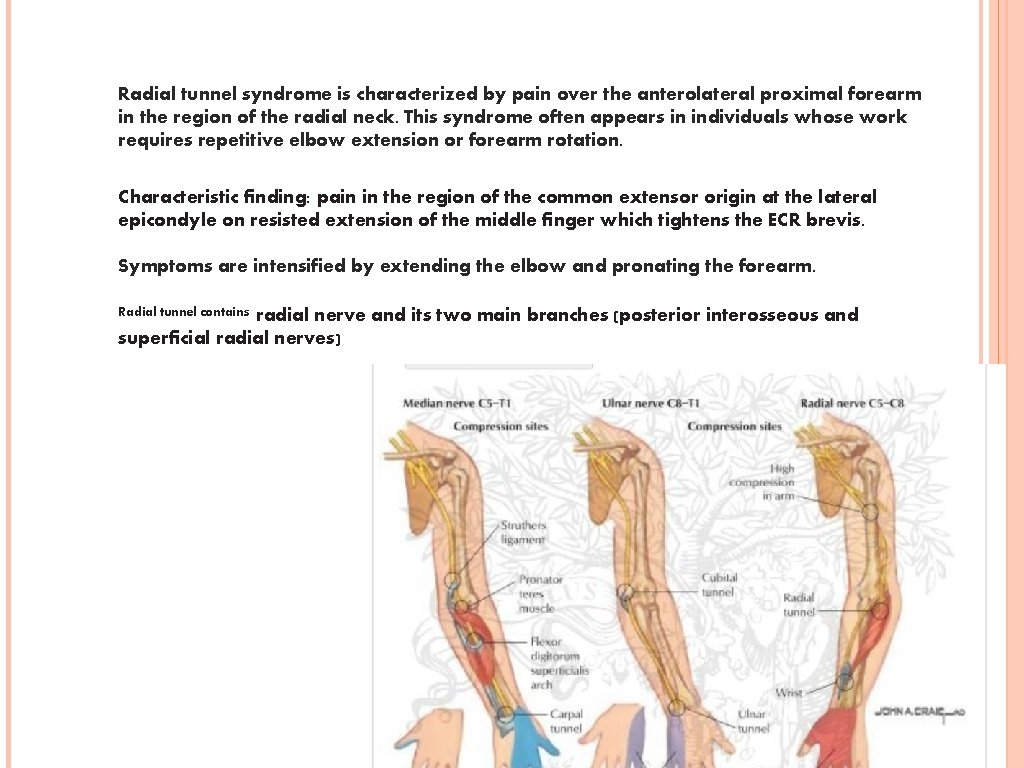
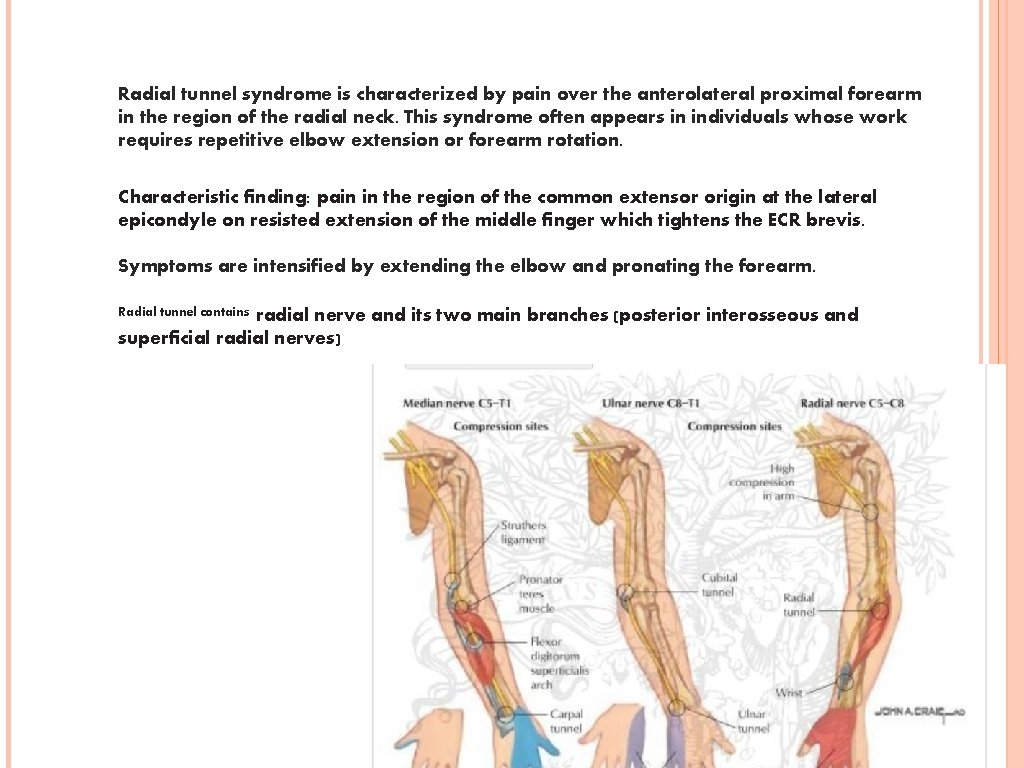
Radial tunnel syndrome is characterized by pain over the anterolateral proximal forearm in the region of the radial neck. This syndrome often appears in individuals whose work requires repetitive elbow extension or forearm rotation. Characteristic finding: pain in the region of the common extensor origin at the lateral epicondyle on resisted extension of the middle finger which tightens the ECR brevis. Symptoms are intensified by extending the elbow and pronating the forearm. Radial tunnel contains radial nerve and its two main branches (posterior interosseous and superficial radial nerves)
Evaluation Radiography for fractures MRI for tumors High resolution US Electromyography (EMG) and nerve conduction studies show abnormal results in radial nerve injuries in the middle and distal third of the humerus.
Axillary nerve injuries Isolated neuropathy of the axillary nerve may occur in the following situations: shoulder dislocation: the nerve is tethered to the joint capsule sleeping in the prone position with the arms abducted above the head injection injury in the high posterior aspect of the shoulder entrapment of the nerve in the quadrilateral space (bounded by the teres major and minor muscles, long head of triceps, and neck of humerus) which contains the axillary nerve and the posterior humeral circumflex artery. Arteriogram may show loss of filling of the artery with the arm abducted and externally rotated
Tarsal Tunnel Syndrome Entrapment of (posterior) tibial nerve may occur in the tarsal tunnel, posterior and inferior to medial malleolus. There is often (but not necessarily) a history of old ankle dislocation or fracture. The nerve may be trapped at the retinacular ligament. This results in pain and paresthesias in the toes and sole of foot (often sparing the heel because the sensory branches often originate proximal to the tunnel), typically worse at night. May cause clawing of toes secondary to weakness of intrinsic foot muscles. Often caused by fracture or dislocation, also rheumatoid arthritis, rarely tumors.
Dorsiflexion-eversion test: examiner maximally everts and dorsiflexes the ankle while dorsiflexing the toes at the MTP joints for 5– 10 seconds. Positive test reproduces the pain. EMGand NCVstudies may help. Surgical decompression is indicated for confirmed cases
TEŞEKKÜRLER… MUSTAFA BEYKAN İSTANBULLU