Multiple Gestations Complications Maternal complications During pregnancy physiological









- Slides: 26
Multiple Gestations Complications
Maternal complications (During pregnancy) ↑↑ physiological changes of pregnancy • ↑ cardiac output • ↑ volume expansion • ↑ haemodilution • ↑ diaphragmatic splinting • ↑ weight gain • ↑ lordosis. ↑ ↑ Minor symptoms of (nausea , vomiting and heartburn)
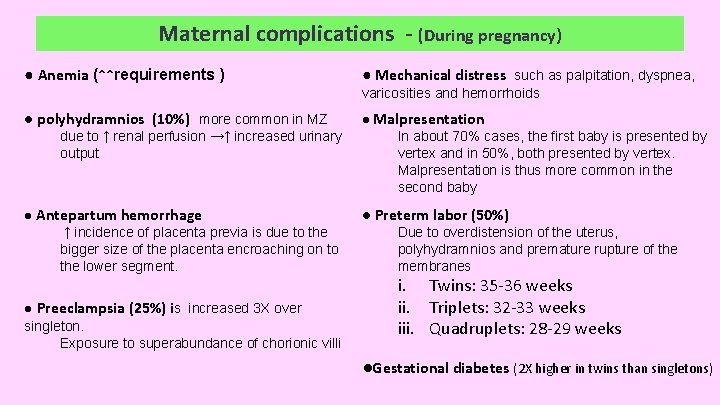
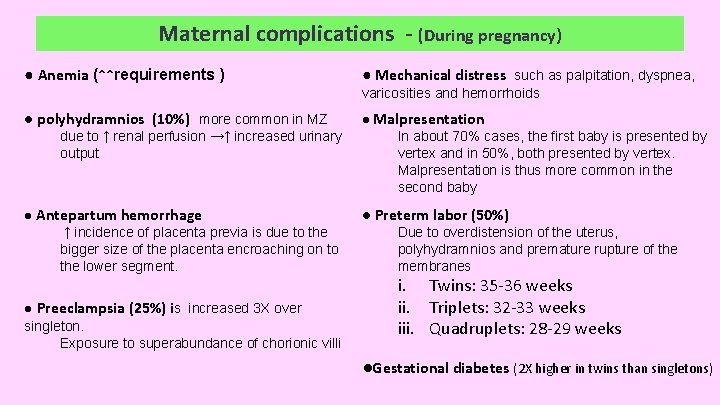
Maternal complications - (During pregnancy) ● Anemia (↑↑requirements ) ● Mechanical distress such as palpitation, dyspnea, varicosities and hemorrhoids ● polyhydramnios (10%) more common in MZ due to ↑ renal perfusion →↑ increased urinary output ● Antepartum hemorrhage ↑ incidence of placenta previa is due to the bigger size of the placenta encroaching on to the lower segment. ● Preeclampsia (25%) is increased 3 X over singleton. Exposure to superabundance of chorionic villi ● Malpresentation In about 70% cases, the first baby is presented by vertex and in 50%, both presented by vertex. Malpresentation is thus more common in the second baby ● Preterm labor (50%) Due to overdistension of the uterus, polyhydramnios and premature rupture of the membranes i. Twins: 35 -36 weeks ii. Triplets: 32 -33 weeks iii. Quadruplets: 28 -29 weeks ●Gestational diabetes (2 X higher in twins than singletons)
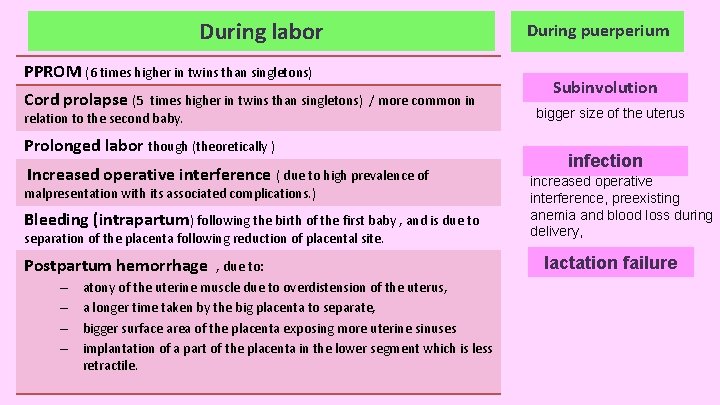
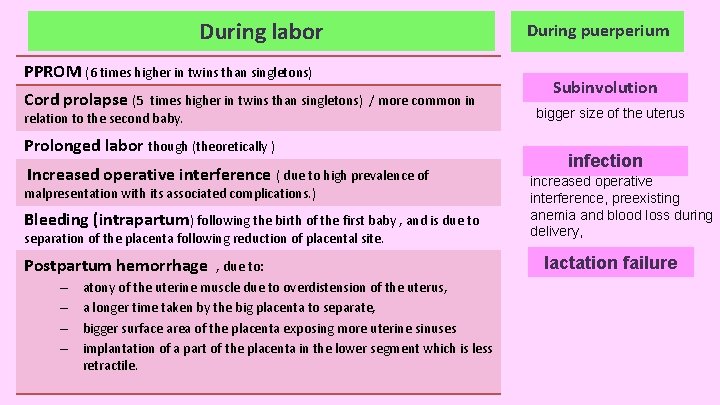
During labor PPROM (6 times higher in twins than singletons) Cord prolapse (5 times higher in twins than singletons) / more common in relation to the second baby. Prolonged labor though (theoretically ) Increased operative interference ( due to high prevalence of malpresentation with its associated complications. ) Bleeding (intrapartum) following the birth of the first baby , and is due to separation of the placenta following reduction of placental site. Postpartum hemorrhage – – , due to: atony of the uterine muscle due to overdistension of the uterus, a longer time taken by the big placenta to separate, bigger surface area of the placenta exposing more uterine sinuses implantation of a part of the placenta in the lower segment which is less retractile. During puerperium Subinvolution bigger size of the uterus infection increased operative interference, preexisting anemia and blood loss during delivery, lactation failure
Fetal complications • • Preterm Miscacrriage , (2 times higher in twins) , MZ IUGR Discordant twin growth Asphyxia Fetal anomaies Intrauterine death of one fetus COMPLICATIONS OF MONOCHORIONIC TWINS – Twin-twin transfusion syndrome (TTTS) – Twin reversed arterial perfusion (TRAP) – Conjoined twin – Monoamniocity
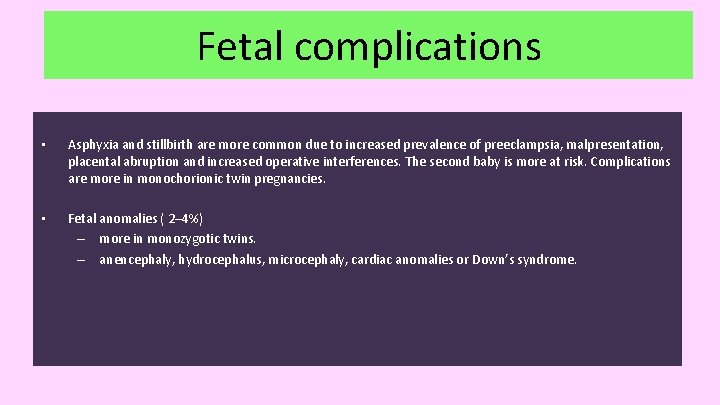
Fetal complications • Asphyxia and stillbirth are more common due to increased prevalence of preeclampsia, malpresentation, placental abruption and increased operative interferences. The second baby is more at risk. Complications are more in monochorionic twin pregnancies. • Fetal anomalies ( 2– 4%) – more in monozygotic twins. – anencephaly, hydrocephalus, microcephaly, cardiac anomalies or Down’s syndrome.
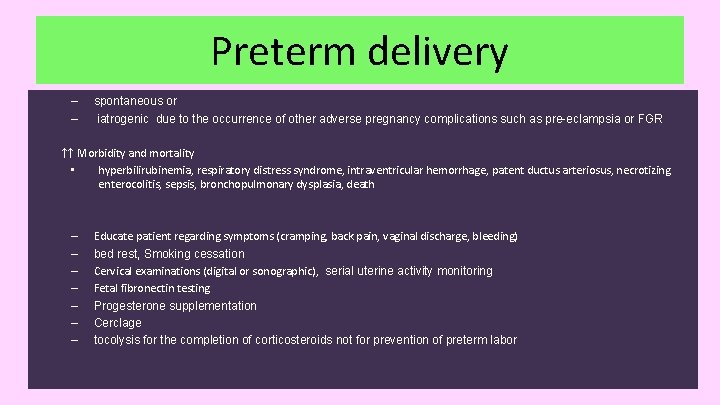
Preterm delivery – – spontaneous or iatrogenic due to the occurrence of other adverse pregnancy complications such as pre-eclampsia or FGR ↑↑ Morbidity and mortality • hyperbilirubinemia, respiratory distress syndrome, intraventricular hemorrhage, patent ductus arteriosus, necrotizing enterocolitis, sepsis, bronchopulmonary dysplasia, death – – – – Educate patient regarding symptoms (cramping, back pain, vaginal discharge, bleeding) bed rest, Smoking cessation Cervical examinations (digital or sonographic), serial uterine activity monitoring Fetal fibronectin testing Progesterone supplementation Cerclage tocolysis for the completion of corticosteroids not for prevention of preterm labor
IUGR – dichorionic pregnancy ــــ 25% chance that at least one of the fetuses will be small for gestational age. – monochorionic twins pregnancy ــــ 50% – in dichorionic twin pregnancies • delivery should be avoided before 28– 30 weeks’ gestation, even if there is evidence of imminent intrauterine death of the smaller twin – in monochorionic twins. • Below 30 weeks gestation, the aim is to prolong the pregnancy as far as possible without risking the death of the growth-restricted twin.

Discordant twin growth • • • size inequality of twin fetuses true pathological discordance involve estimated weight difference of 25% or more If >20% discordance, more frequent ultrasounds – due to • twin–twin transfusion syndrome • placental insufficiency • IUGR in one fetus • structural anomalies occurring in one fetus
Intrauterine death of one fetus • The deaths are due to cord compression, competition for nourishment or congenital malformation. • Neurological damage of the survivor (cerebral palsy, microcephaly, renal cortical necrosis) results from – Transfer of thromboplastin from dead twin causing thrombotic arterial occlusion in second twin – Acute hypotensive episode Maternal DIC (rare) If a loss occurs in first trimester (most common)→ the affected fetus Vanishes by resorption. With no developmental consequence in surviving twin If loss occur in the second or third trimester – In dichorionic twins → may be associated with the onset of labour, although in some cases the pregnancy may continue uneventfully and even result in delivery at term. – in monochorionic twins → immediate complications in the survivor • • •
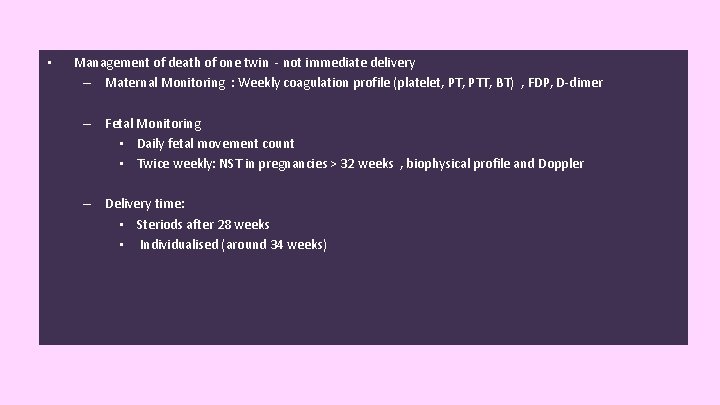
• Management of death of one twin - not immediate delivery – Maternal Monitoring : Weekly coagulation profile (platelet, PTT, BT) , FDP, D-dimer – Fetal Monitoring • Daily fetal movement count • Twice weekly: NST in pregnancies > 32 weeks , biophysical profile and Doppler – Delivery time: • Steriods after 28 weeks • Individualised (around 34 weeks)

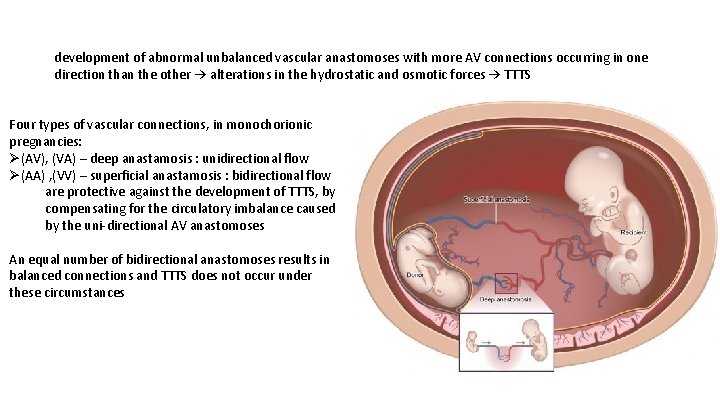
Twin-twin transfusion syndrome (TTTS) • Results from imbalance of vascular anastomoses of placental vessels between fetuses leading to “loss” of volume/blood from 1 twin (donor) to other (recipient) – 10% -15%of monochorionic diamniotic pregnancies and 5% of monoamniotic – Diagnosis by assessing monochorionic pregnancies every 2 weeks from 16 weeks’ gestation to at least 24 weeks’ gestation
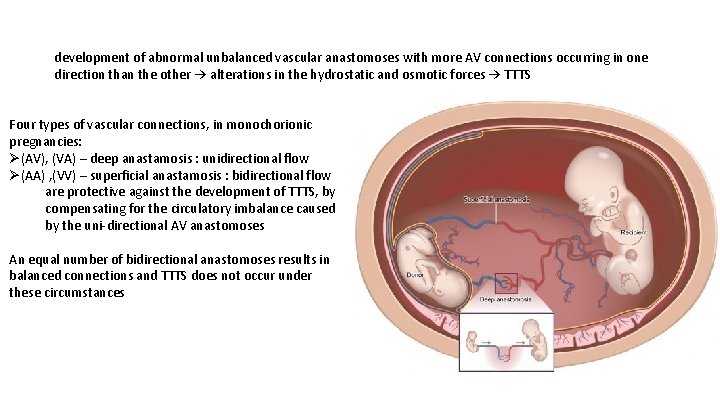
development of abnormal unbalanced vascular anastomoses with more AV connections occurring in one direction than the other → alterations in the hydrostatic and osmotic forces → TTTS Four types of vascular connections, in monochorionic pregnancies: Ø(AV), (VA) – deep anastamosis : unidirectional flow Ø(AA) , (VV) – superficial anastamosis : bidirectional flow are protective against the development of TTTS, by compensating for the circulatory imbalance caused by the uni-directional AV anastomoses An equal number of bidirectional anastomoses results in balanced connections and TTTS does not occur under these circumstances

donor twin : becomes smaller , Oligohydramnios, hypotensive , hypovolemic.

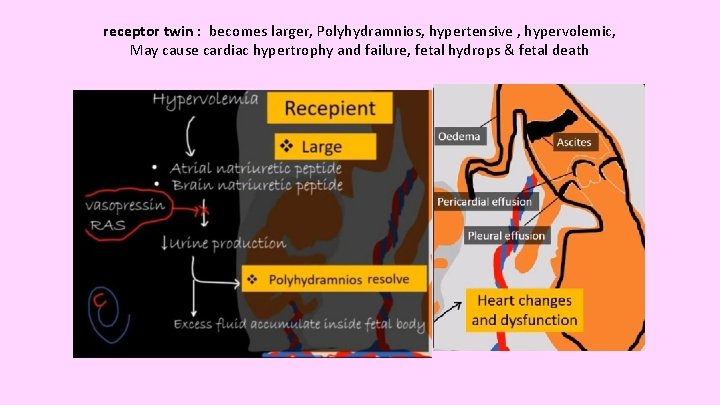
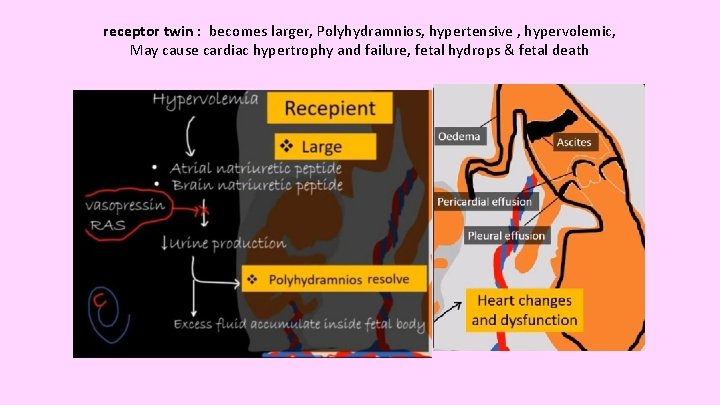
receptor twin : becomes larger, Polyhydramnios, hypertensive , hypervolemic, May cause cardiac hypertrophy and failure, fetal hydrops & fetal death
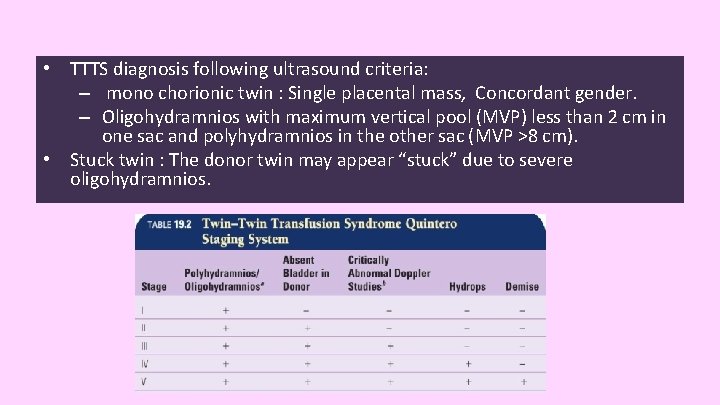
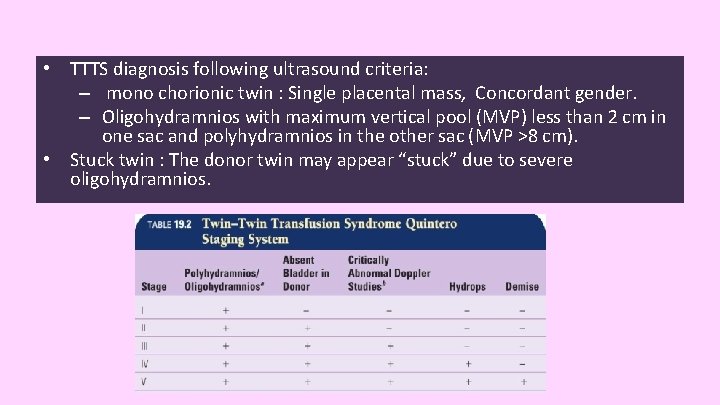
• TTTS diagnosis following ultrasound criteria: – mono chorionic twin : Single placental mass, Concordant gender. – Oligohydramnios with maximum vertical pool (MVP) less than 2 cm in one sac and polyhydramnios in the other sac (MVP >8 cm). • Stuck twin : The donor twin may appear “stuck” due to severe oligohydramnios.

Management: TTTS • Suspected patients should be referred for a tertiary referral 1. amnioreduction: (serial) amniocentesis to control polyhydramnios in the recipient twin is done 2. Septostomy (making a hole in the dividing amniotic membrane 3. Fetoscopic laser ablation : Better outcome compared with amnio-reduction – (the definitive treatment) for severe (defined as Quintero stage II or above) TTTS between 16 and 26 weeks’ gestation. (2 nd trimester) – Above 26 weeks, delivery may be considered. 4. Selective reduction (feticide) of one twin is done when survival of both the fetuses is at risk
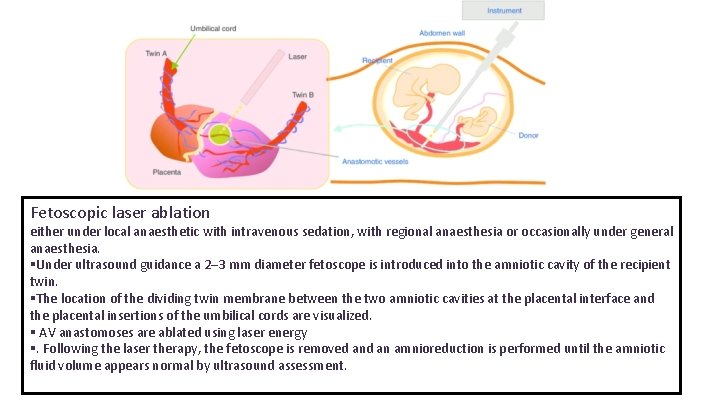
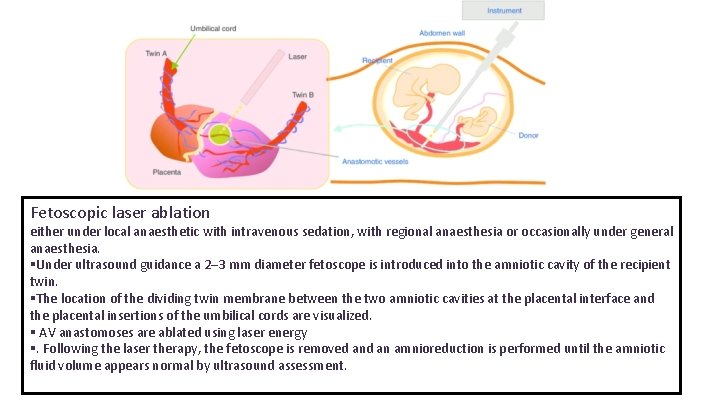
Fetoscopic laser ablation either under local anaesthetic with intravenous sedation, with regional anaesthesia or occasionally under general anaesthesia. §Under ultrasound guidance a 2– 3 mm diameter fetoscope is introduced into the amniotic cavity of the recipient twin. §The location of the dividing twin membrane between the two amniotic cavities at the placental interface and the placental insertions of the umbilical cords are visualized. § AV anastomoses are ablated using laser energy §. Following the laser therapy, the fetoscope is removed an amnioreduction is performed until the amniotic fluid volume appears normal by ultrasound assessment.

• TAPS (Twin anemia polycythemia sequence) – is a rarer chronic form of TTTS – a large haemoglobin difference – No oligohydramnios polyhydramnios sequence. residual small (<1 mm) unidirectional AV anastomoses the gradual development of anaemia in one twin and polycythaemia in the other twin. haemodynamic compensation No oligohydramnios polyhydramnios pattern. Severe polycythaemia can occur, leading to fetal and placental thrombosis and hydrops fetalis in the anaemic twin

Twin reversed arterial perfusion (TRAP) – “acardiac perfused twin” having blood supply from a normal co-twin via large arterio-arterial or vein to vein anastomosis. – The arterial pressure of the donor twin being high, the recipient twin receives the “used” blood from the donor. – The perfused twin is often chromosomally abnormal , may appear as an amorphous mass. – In majority the co-twin dies (in the perinatal period) due to high output cardiac failure. – Management of TRAP is controversial. • Ligation of the umbilical cord of the acardiac twin under fetoscopic guidance.
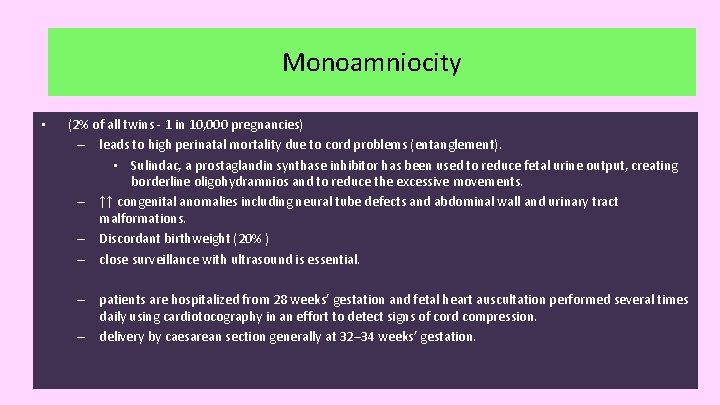
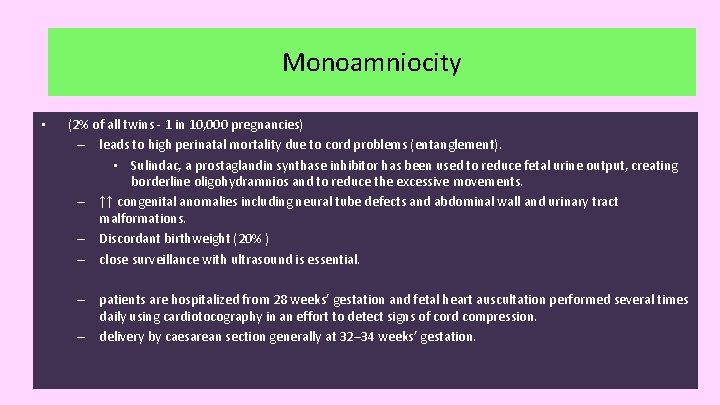
trap Monoamniocity • (2% of all twins - 1 in 10, 000 pregnancies) – leads to high perinatal mortality due to cord problems (entanglement). • Sulindac, a prostaglandin synthase inhibitor has been used to reduce fetal urine output, creating borderline oligohydramnios and to reduce the excessive movements. – ↑↑ congenital anomalies including neural tube defects and abdominal wall and urinary tract malformations. – Discordant birthweight (20% ) – close surveillance with ultrasound is essential. – patients are hospitalized from 28 weeks’ gestation and fetal heart auscultation performed several times daily using cardiotocography in an effort to detect signs of cord compression. – delivery by caesarean section generally at 32– 34 weeks’ gestation.
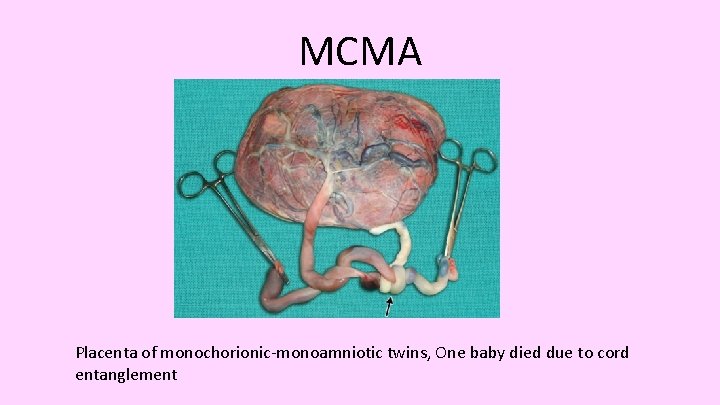
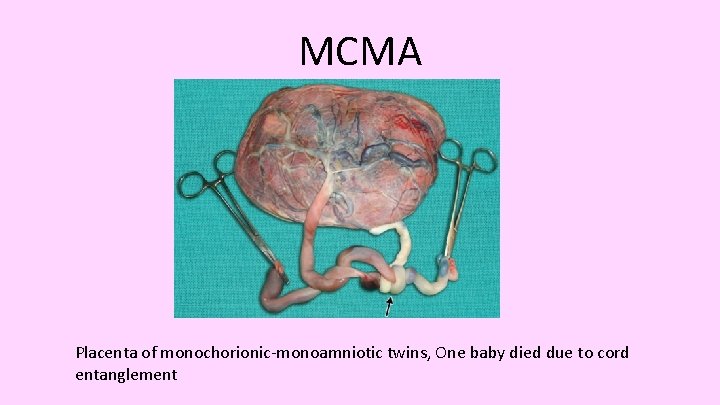
MCMA Placenta of monochorionic-monoamniotic twins, One baby died due to cord entanglement

Conjoined twin • Conjoined twin is rare (1. 3 per 100, 000 births). – Diagnosis: • often diagnosed during delivery – when there is obstruction in the second stage , failure of traction to deliver the first twin in the second stage – inability to move one twin without moving the other – Presence of a bridge of tissue between the fetuses on vaginal examination confirms the diagnosis. – Antenatal diagnosis is important. Benefits are: • Reduces maternal trauma and morbidity and to Improves fetal survival • Helps to plan the method of delivery , Allows time to organize the pediatric surgical team. – The survival of conjoined twins depends on the severity of malformations both at the site of union and distant from the site of union. – Management depends on : Extent and site of union , Possibility of surgical separation and Size of the fetuses and possibility of survival

Thank you