Arterial Pressure Monitoring Components of an Arterial Pressure





- Slides: 62
Arterial Pressure Monitoring
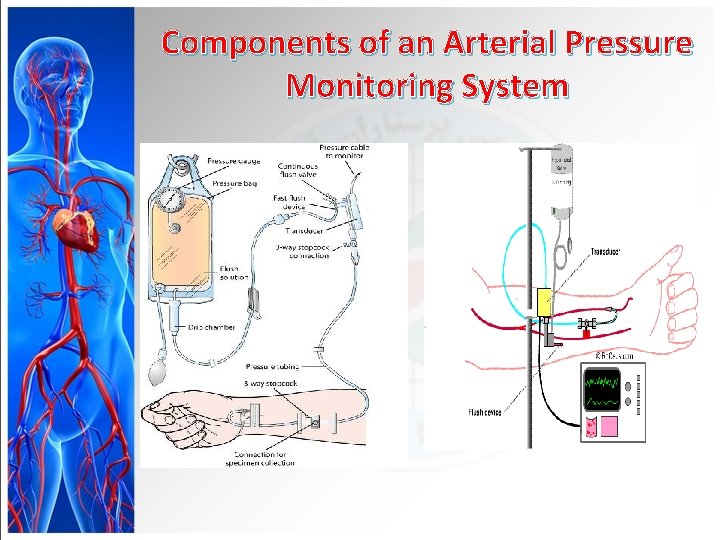
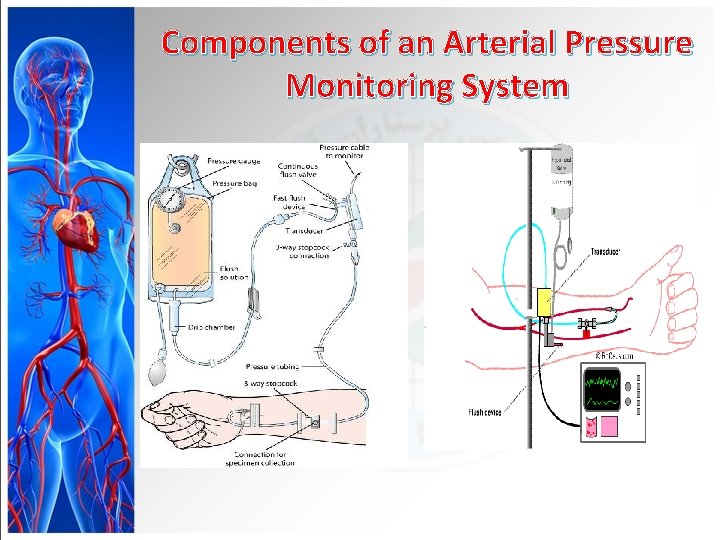
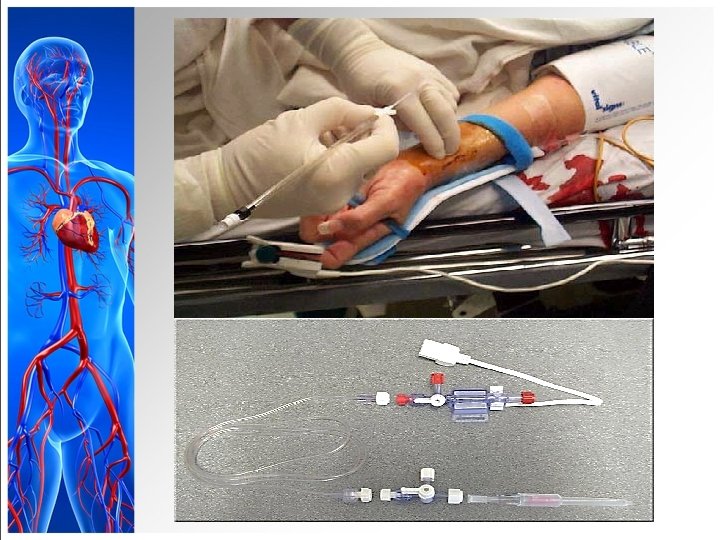
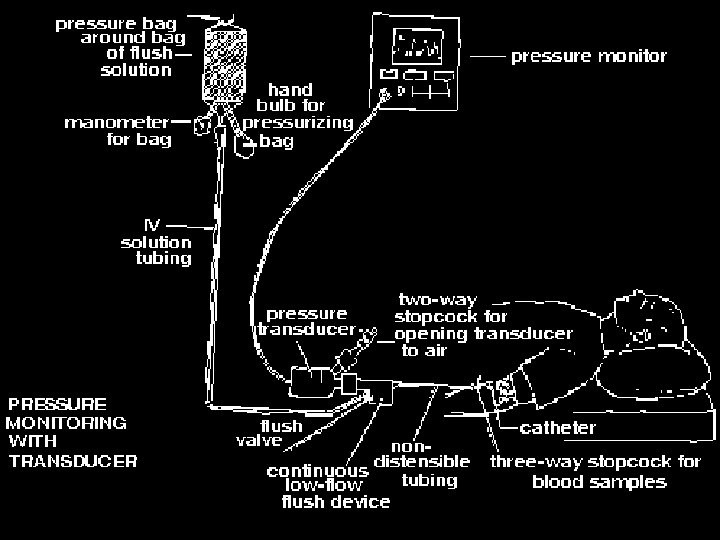
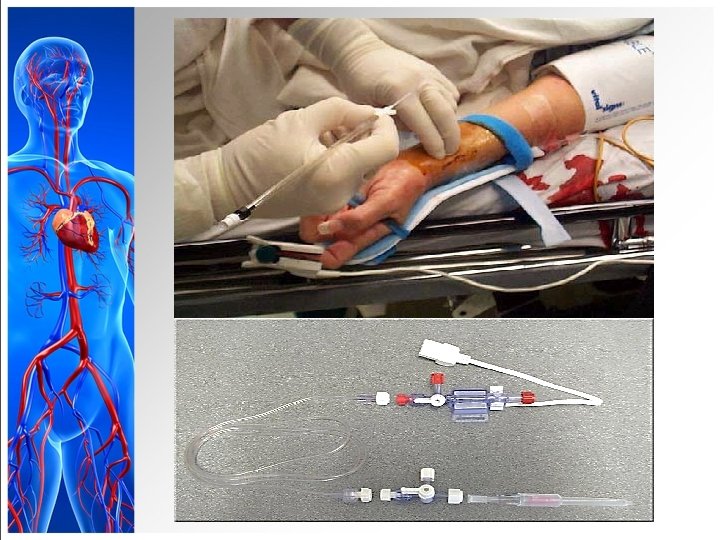
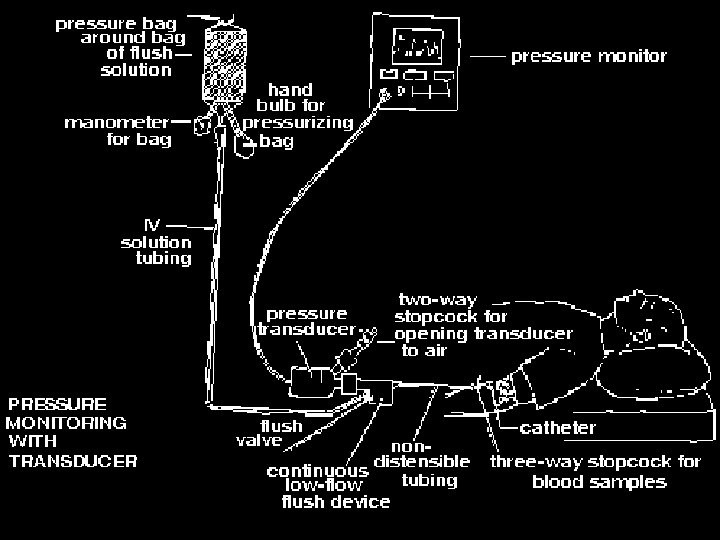
Components of an Arterial Pressure Monitoring System
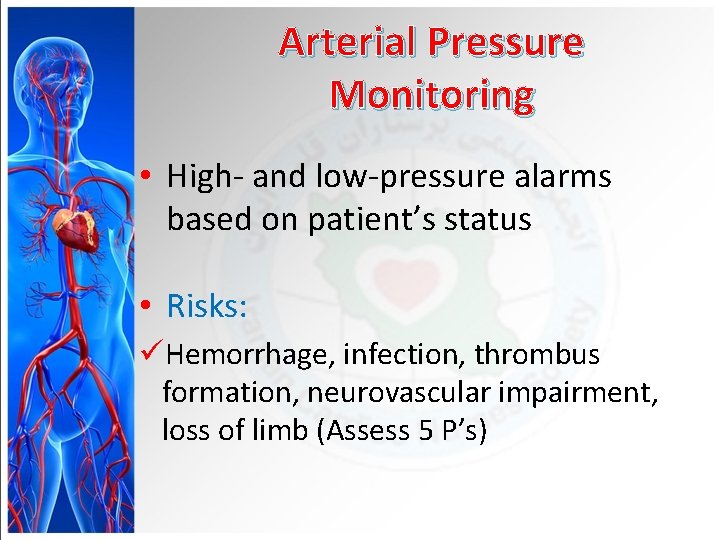
Arterial Pressure Monitoring • High- and low-pressure alarms based on patient’s status • Risks: üHemorrhage, infection, thrombus formation, neurovascular impairment, loss of limb (Assess 5 P’s)
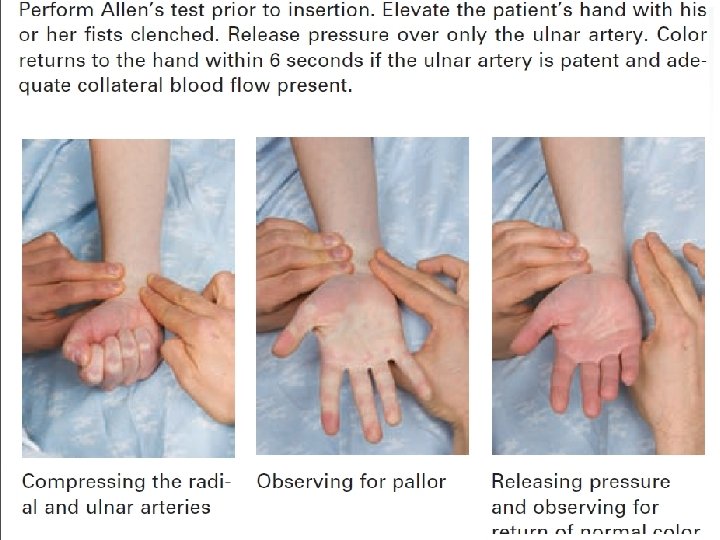
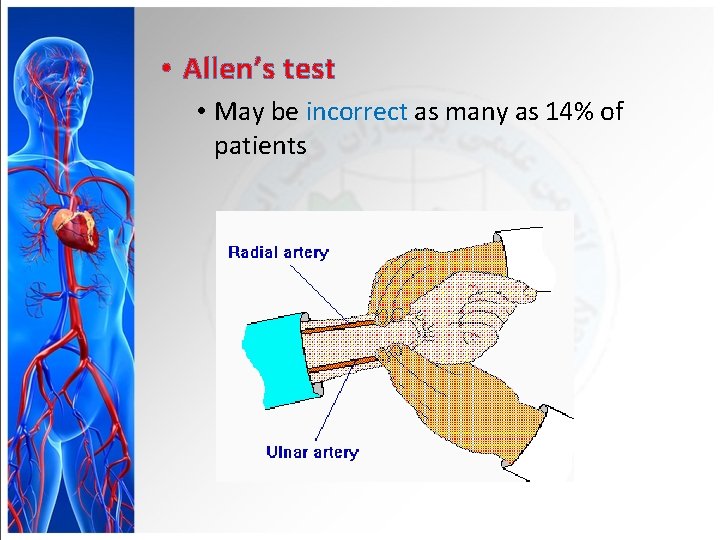
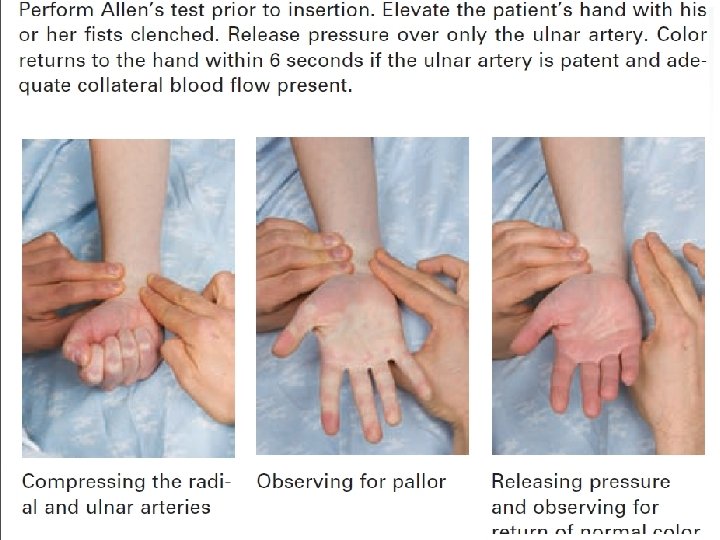
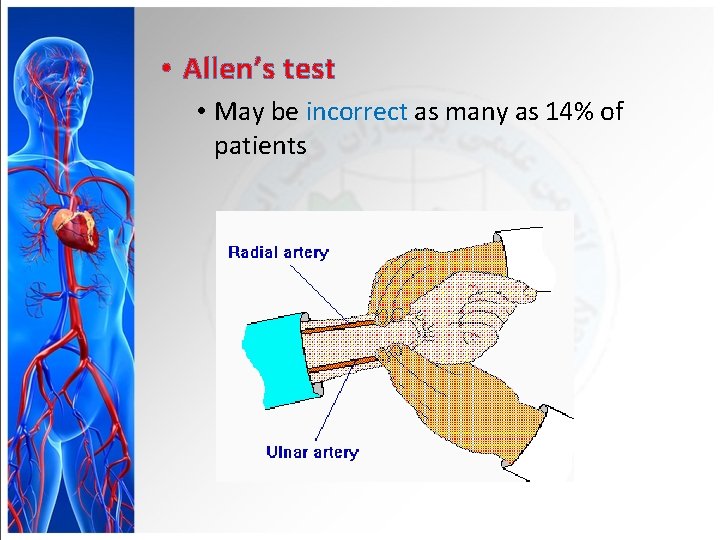
• Allen’s test • May be incorrect as many as 14% of patients


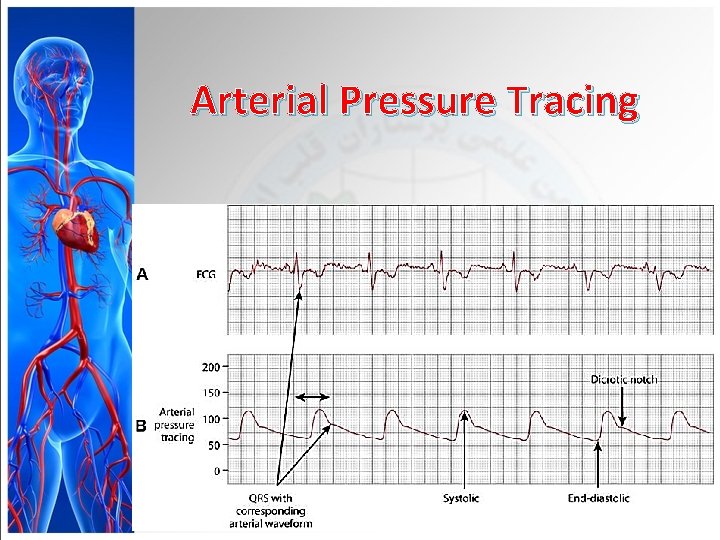
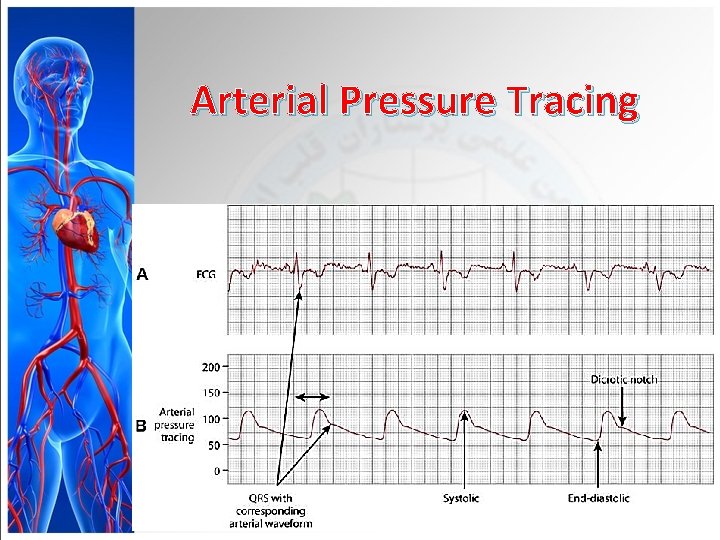
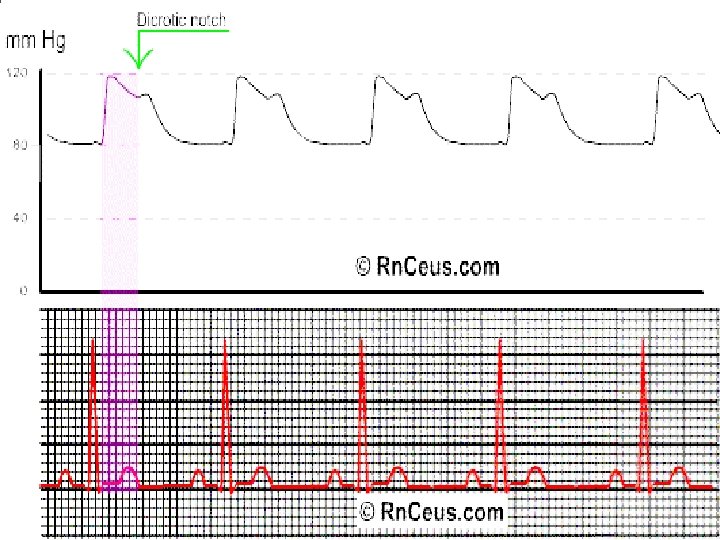
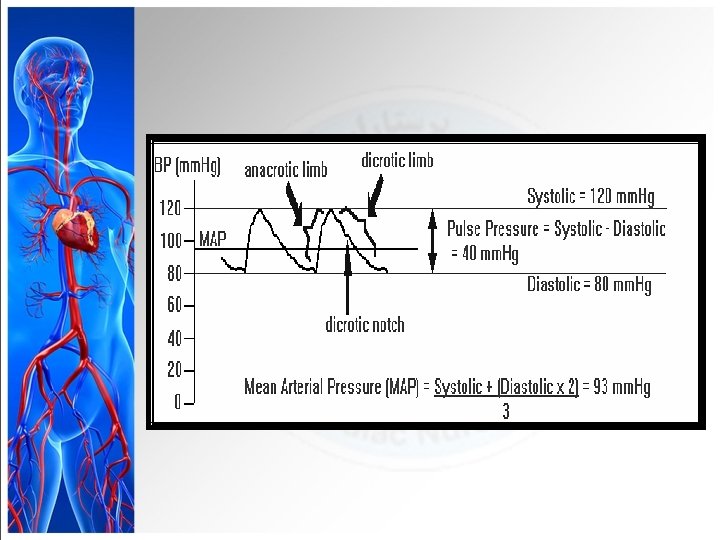
Arterial Pressure Tracing
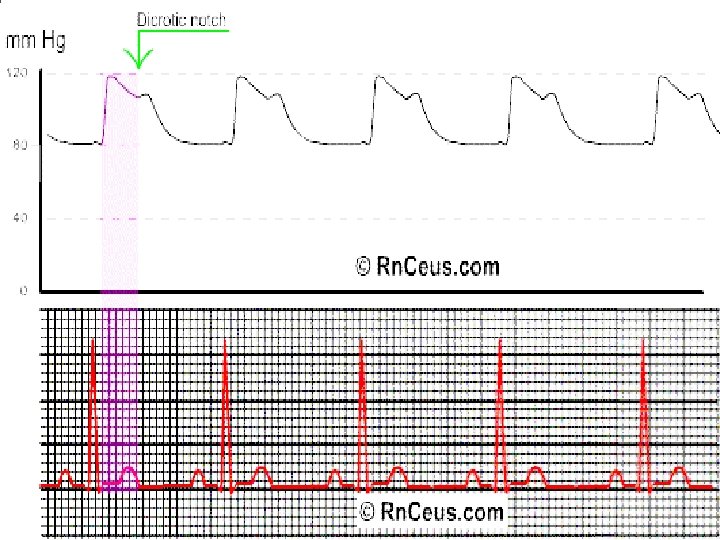

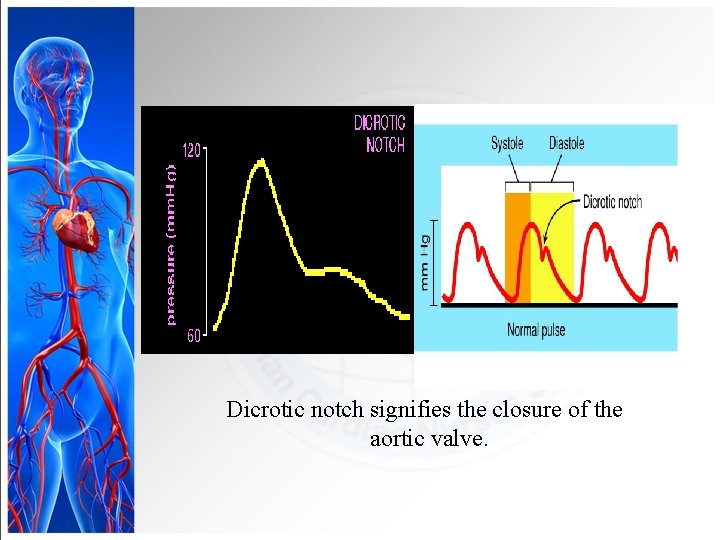
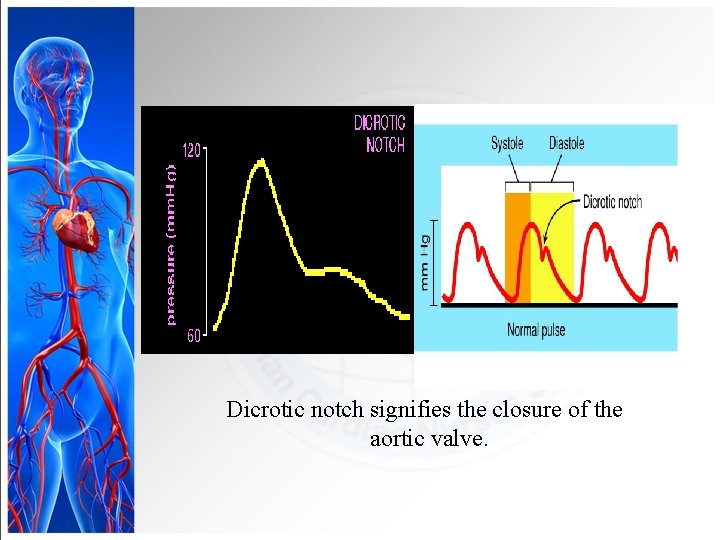
Dicrotic notch signifies the closure of the aortic valve.

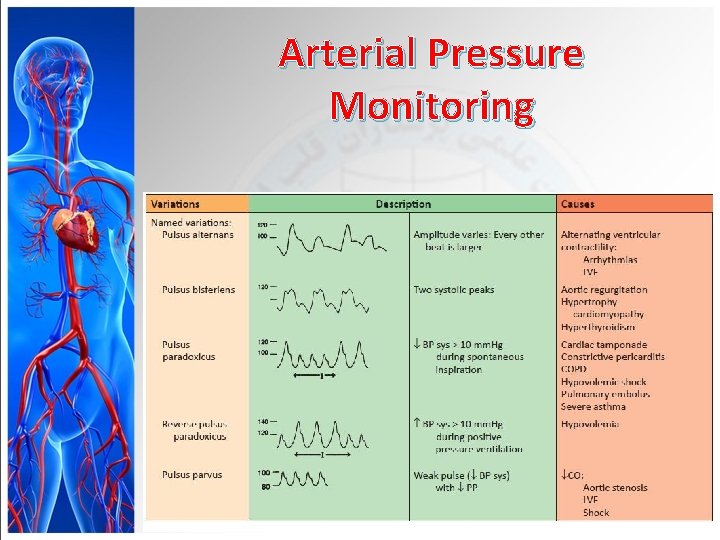
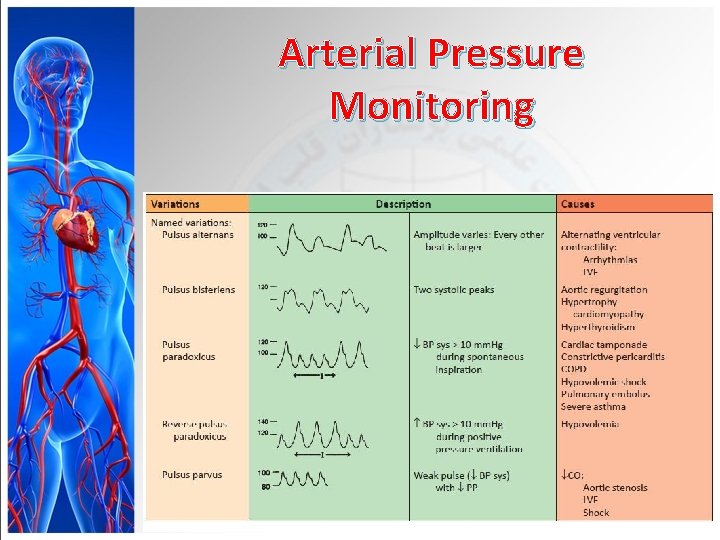
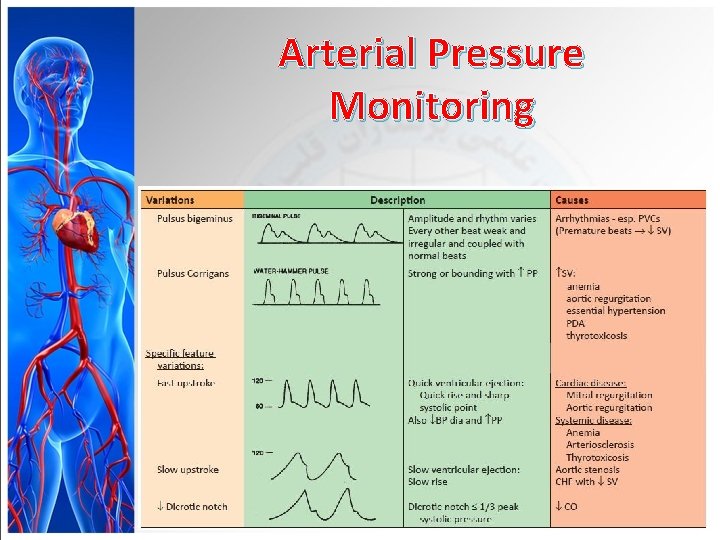
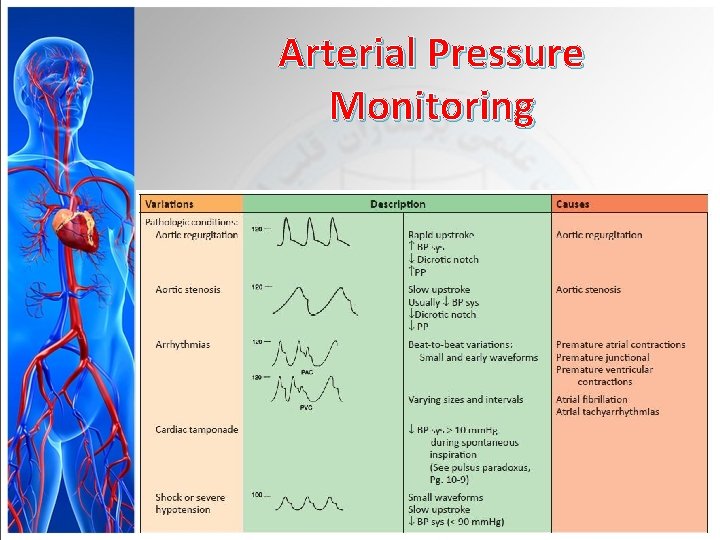
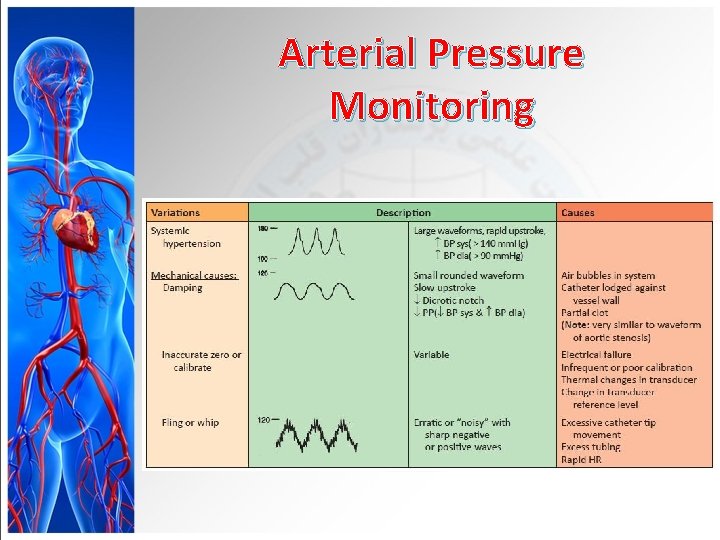
Arterial Pressure Monitoring
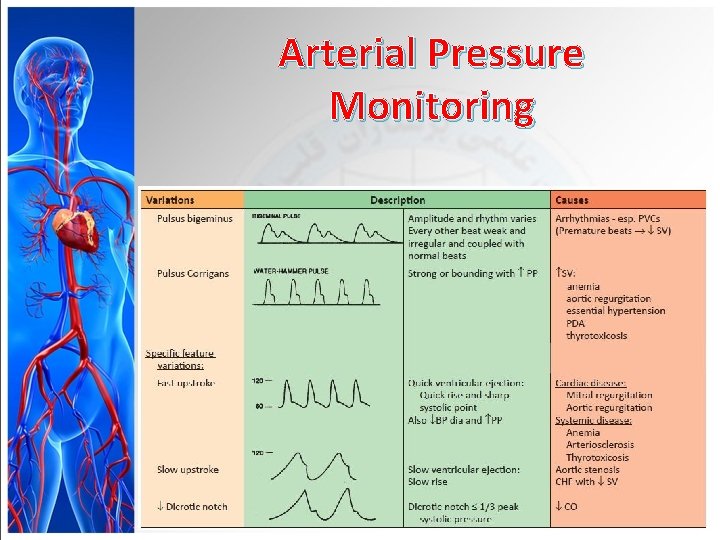
Arterial Pressure Monitoring
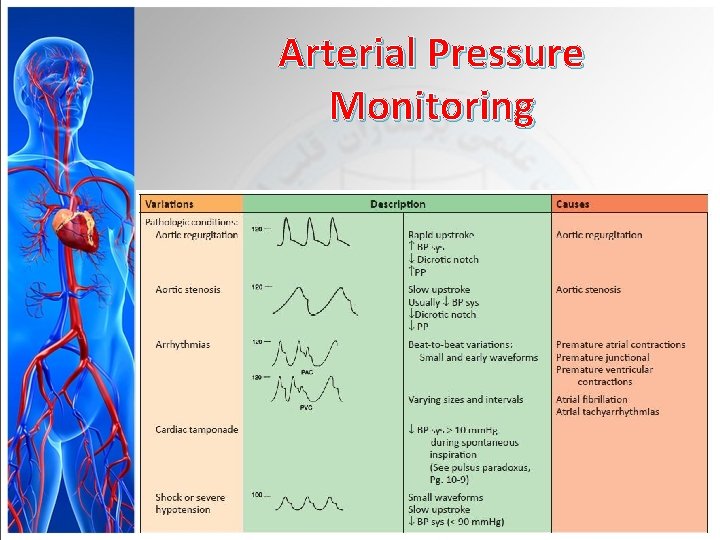
Arterial Pressure Monitoring
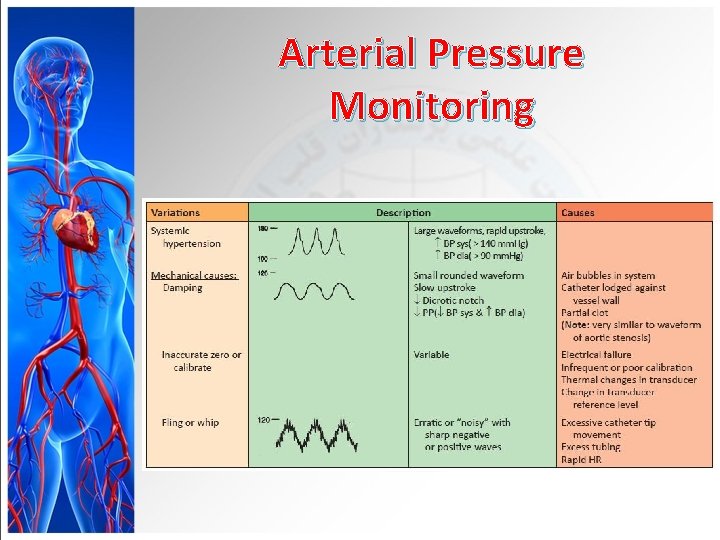
Arterial Pressure Monitoring
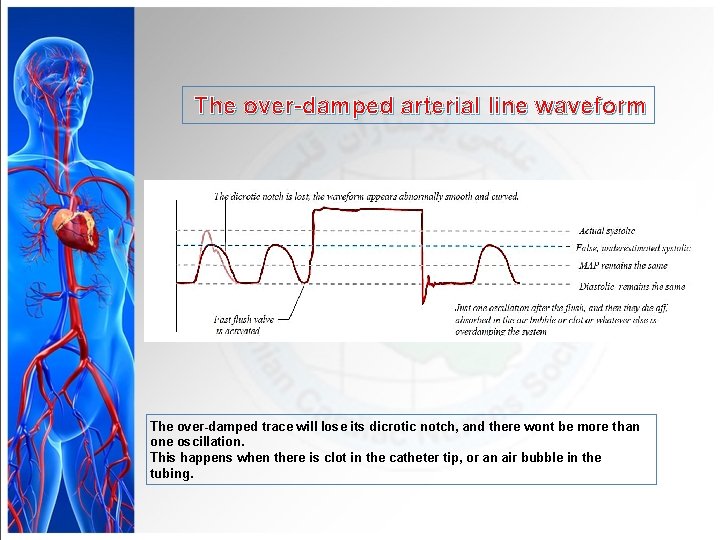
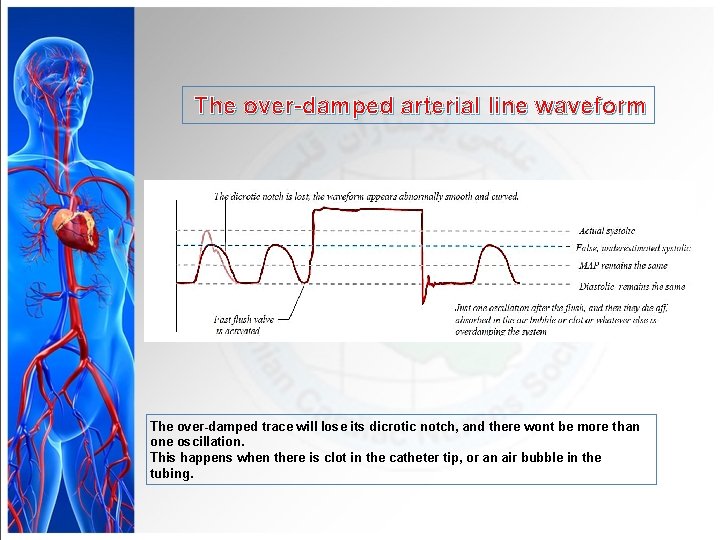
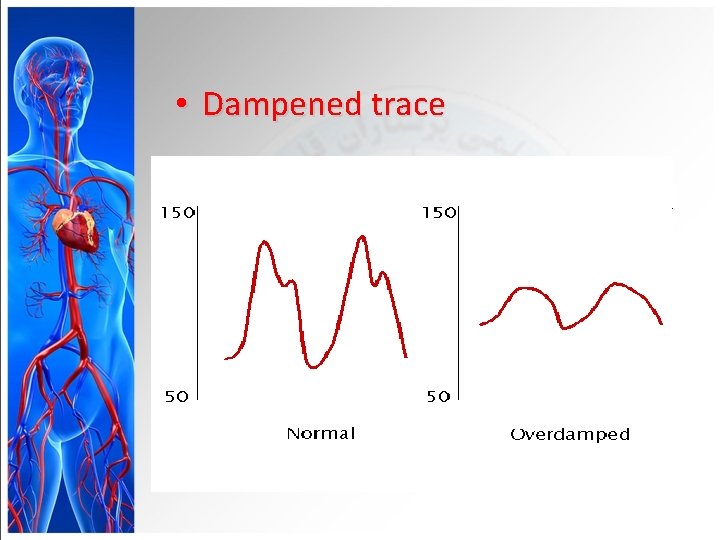
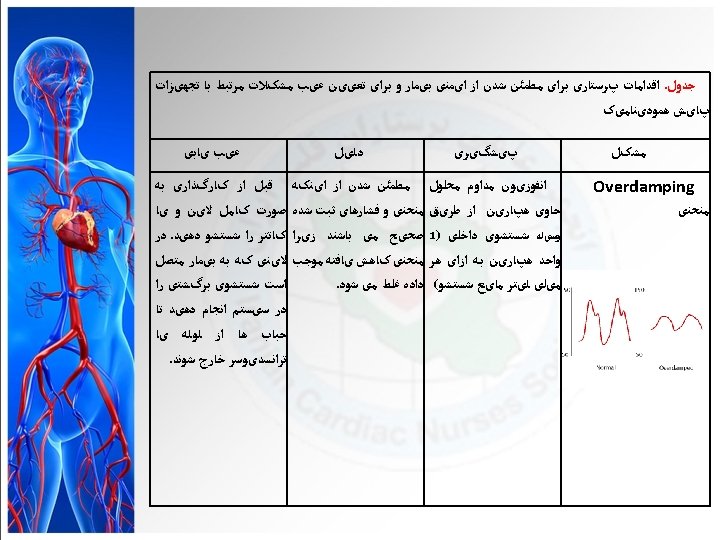
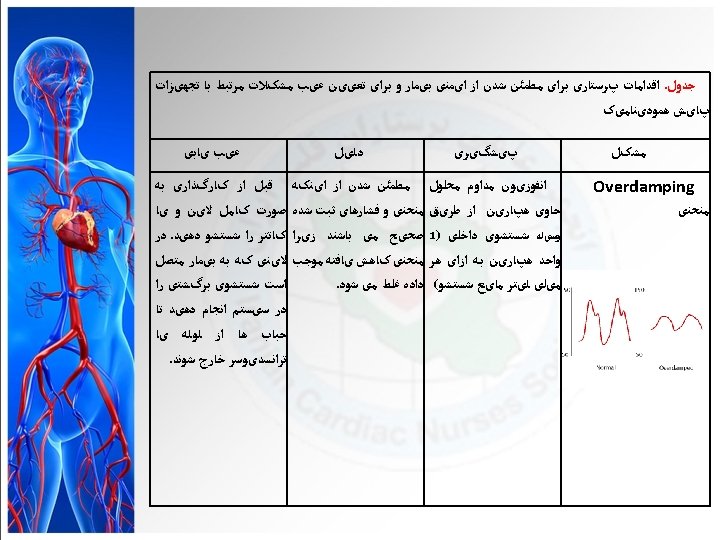
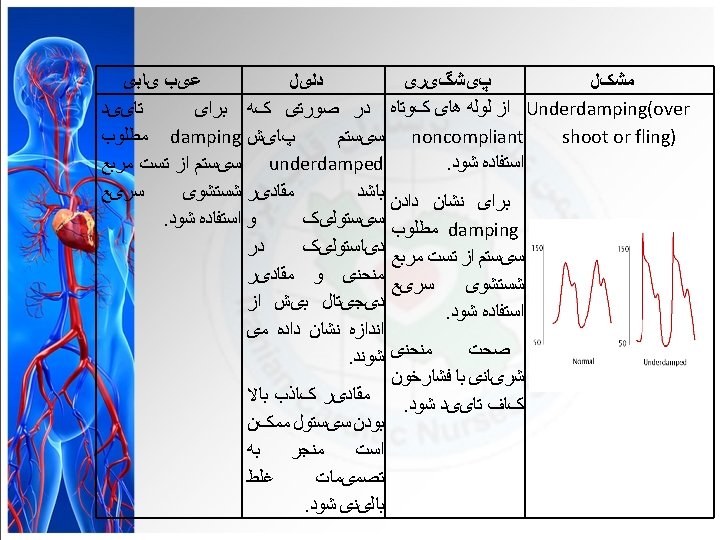
The over-damped arterial line waveform The over-damped trace will lose its dicrotic notch, and there wont be more than one oscillation. This happens when there is clot in the catheter tip, or an air bubble in the tubing.
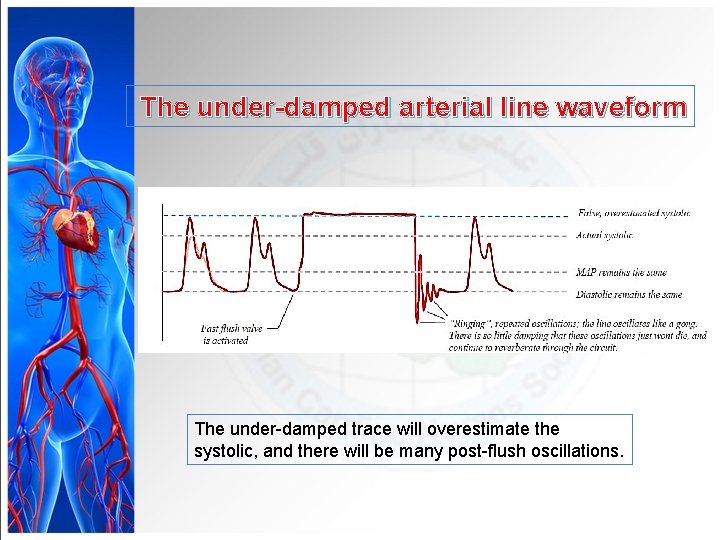
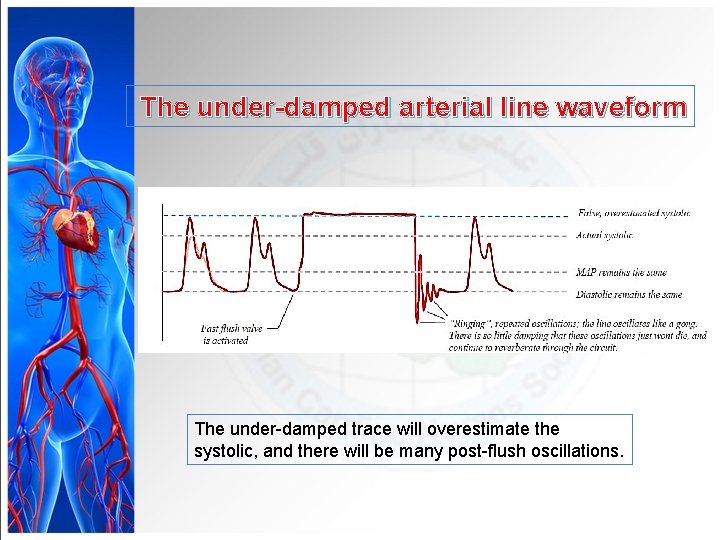
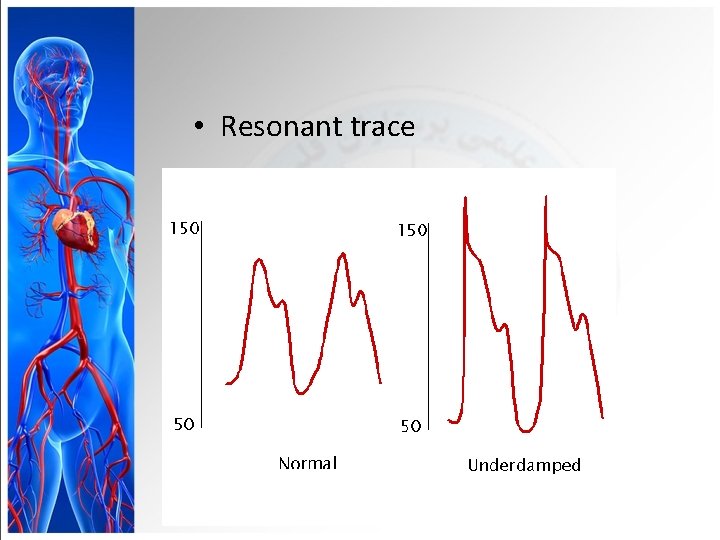
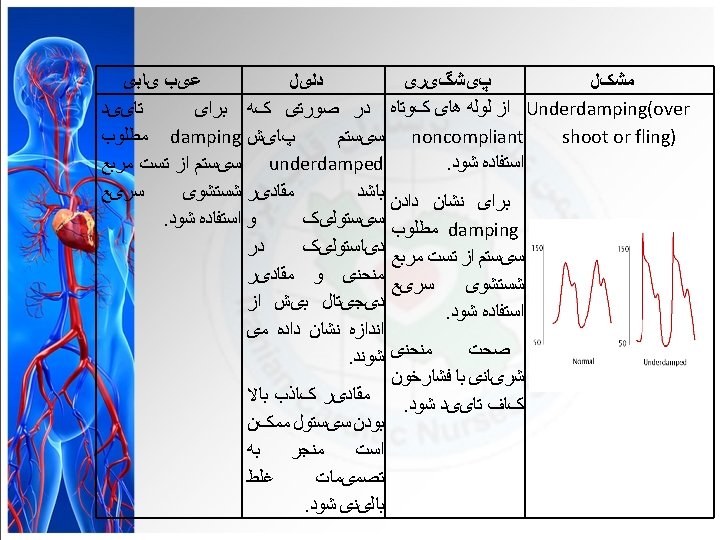
The under-damped arterial line waveform The under-damped trace will overestimate the systolic, and there will be many post-flush oscillations.
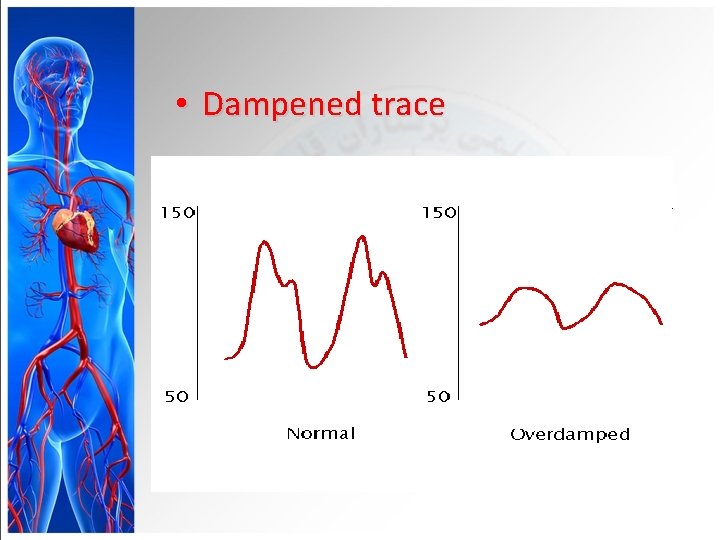
• Dampened trace
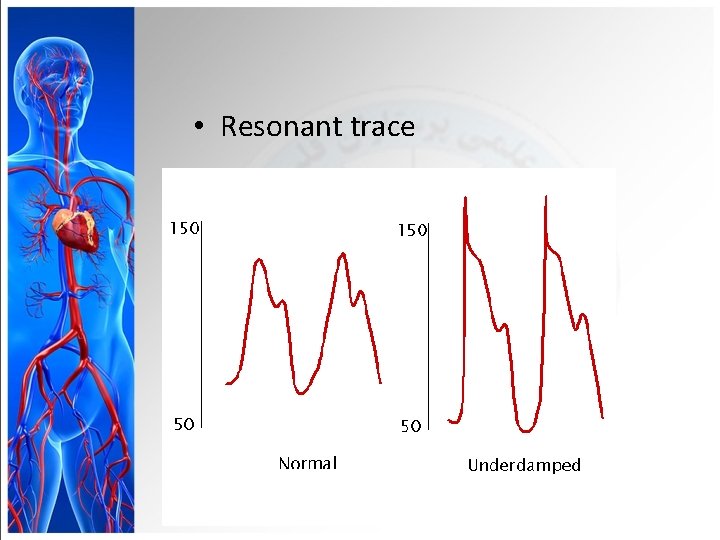
• Resonant trace
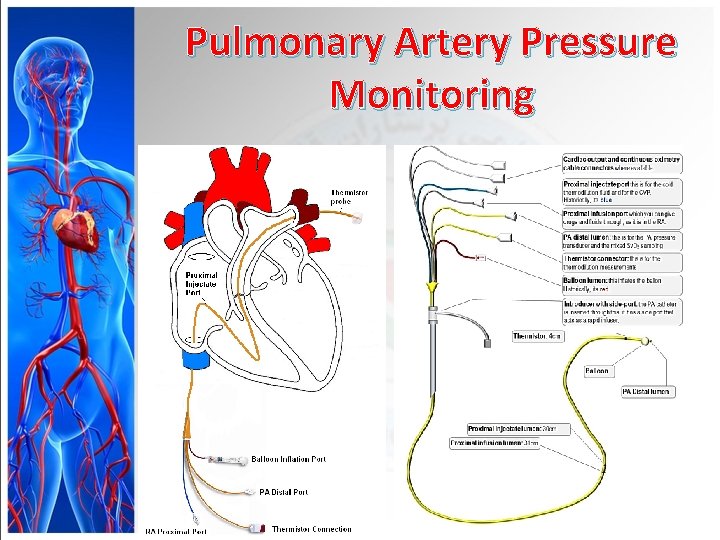
Pulmonary Artery Pressure Monitoring
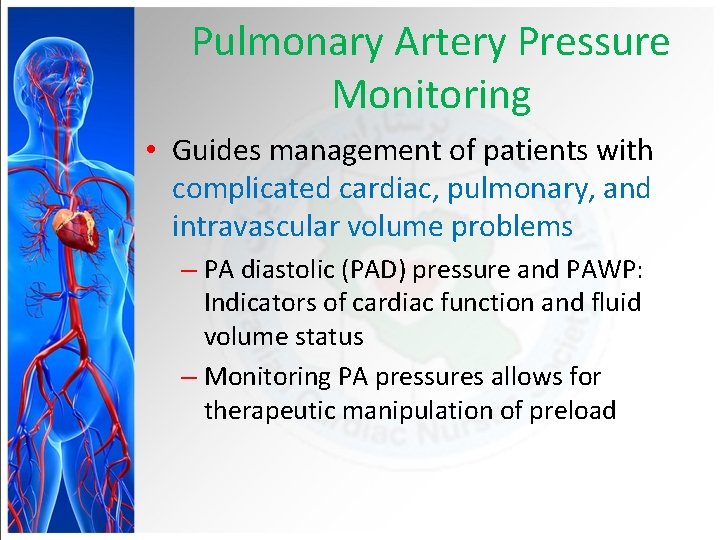
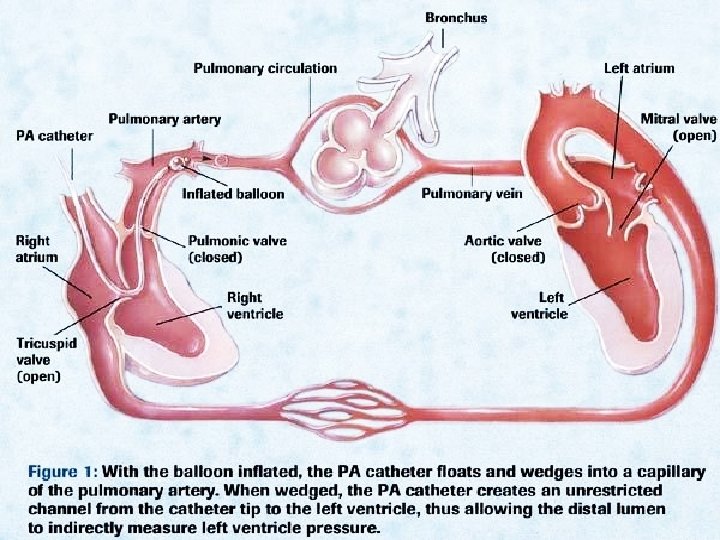
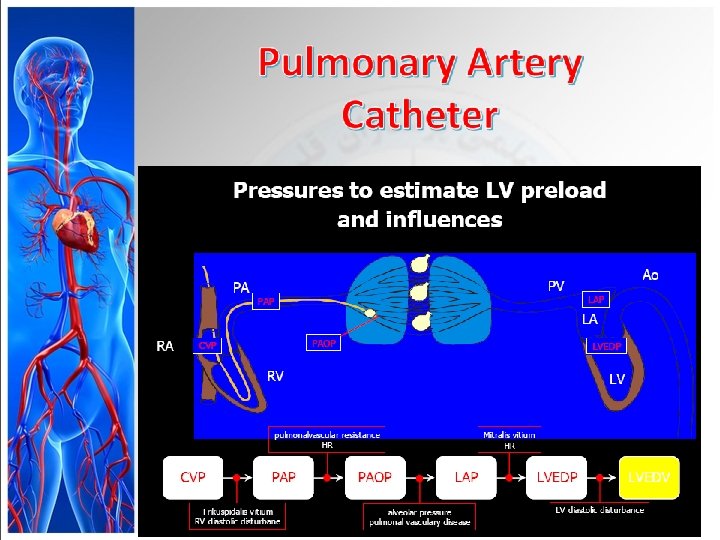
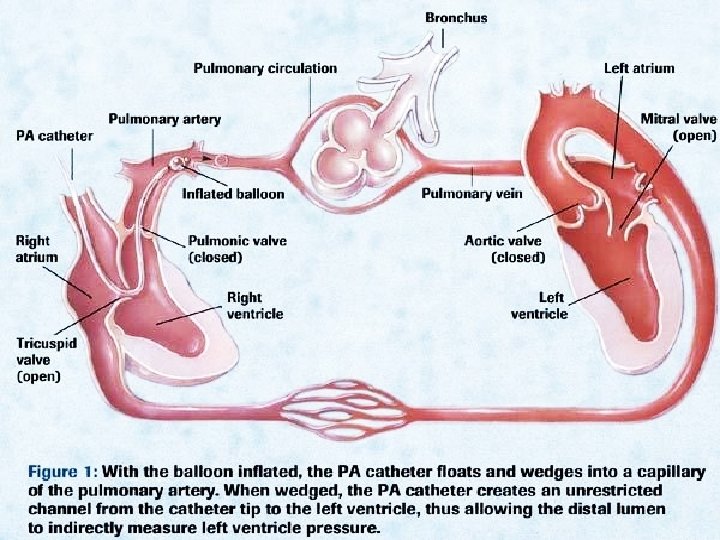
Pulmonary Artery Pressure Monitoring • Guides management of patients with complicated cardiac, pulmonary, and intravascular volume problems – PA diastolic (PAD) pressure and PAWP: Indicators of cardiac function and fluid volume status – Monitoring PA pressures allows for therapeutic manipulation of preload
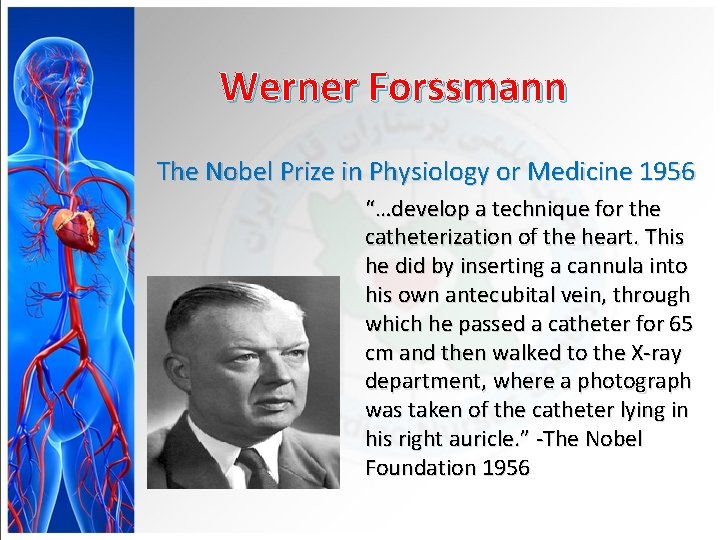
Werner Forssmann The Nobel Prize in Physiology or Medicine 1956 “…develop a technique for the catheterization of the heart. This he did by inserting a cannula into his own antecubital vein, through which he passed a catheter for 65 cm and then walked to the X-ray department, where a photograph was taken of the catheter lying in his right auricle. ” -The Nobel Foundation 1956
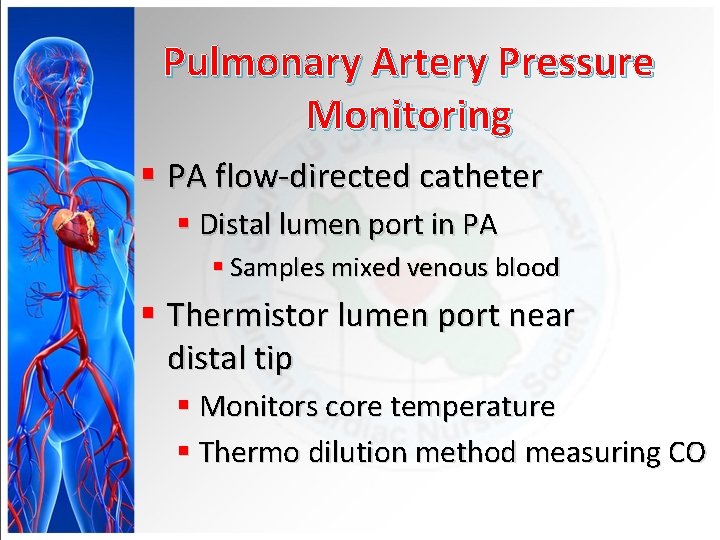
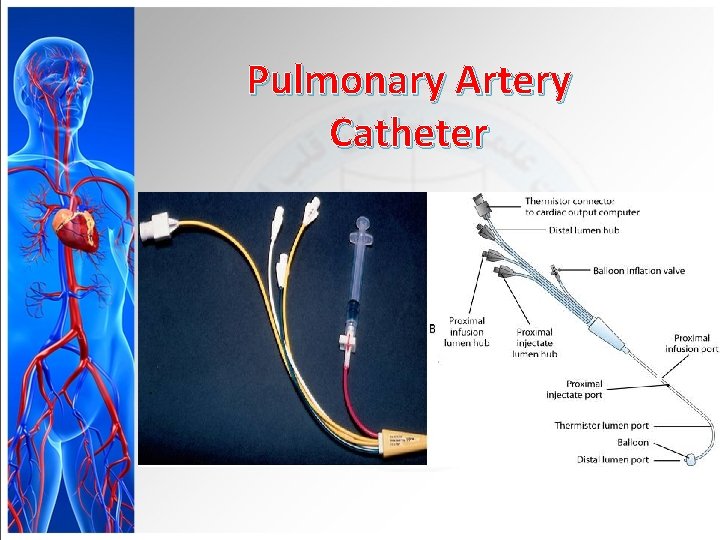
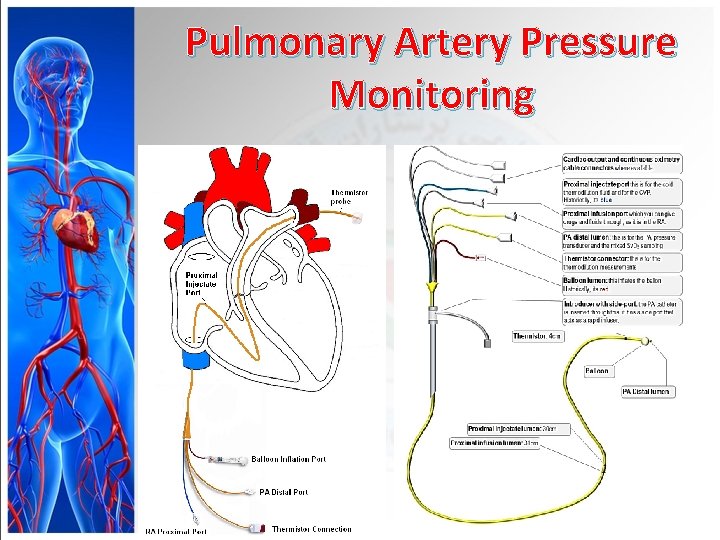
Pulmonary Artery Pressure Monitoring § PA flow-directed catheter § Distal lumen port in PA § Samples mixed venous blood § Thermistor lumen port near distal tip § Monitors core temperature § Thermo dilution method measuring CO
Pulmonary Artery Pressure Monitoring
Pulmonary Artery Pressure Monitoring § Proximal -Right atrium port Measurement of CVP, Injection of fluid, for CO measurement, Blood sampling, Administer medications
Purpose Measuring of pulmonary artery pressure § § § § Measuring of right atrium pressure. Measuring of right ventricle pressure. Measuring of cardiac out put. indirect measurement of the pressure in the left atrium heart atrium Assessing the status of the mitral valve.
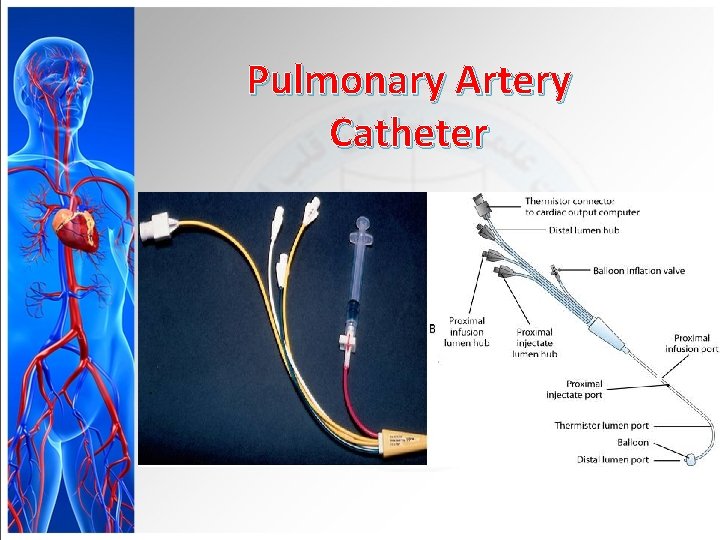
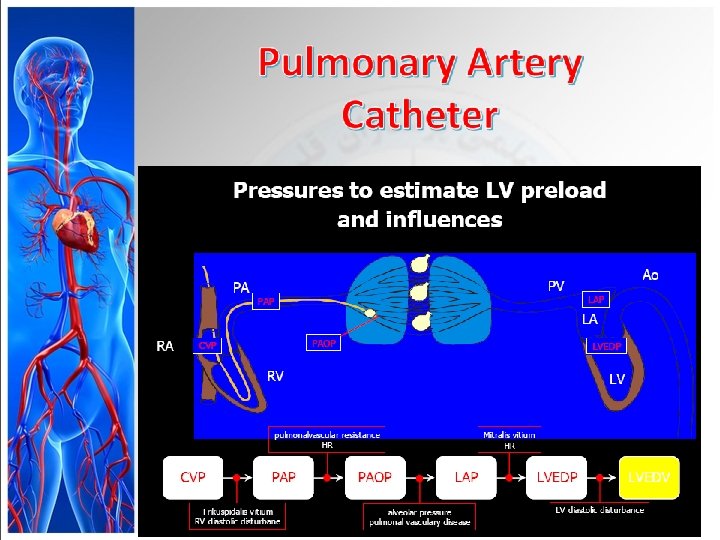
Pulmonary Artery Catheter
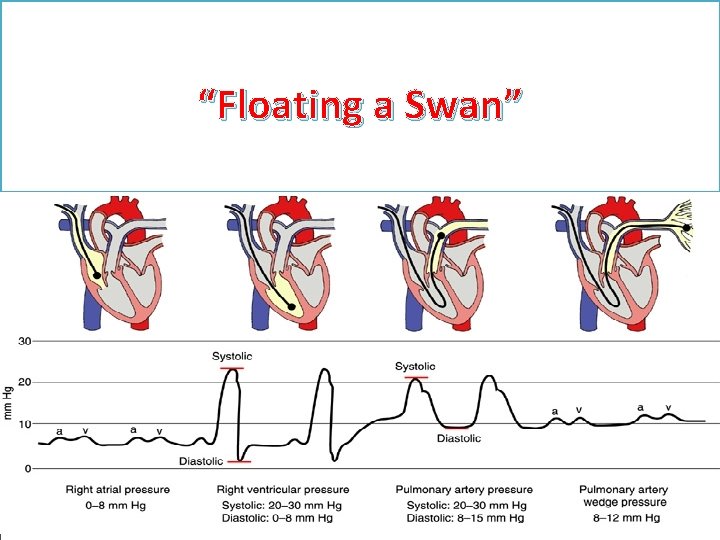
“Floating a Swan”
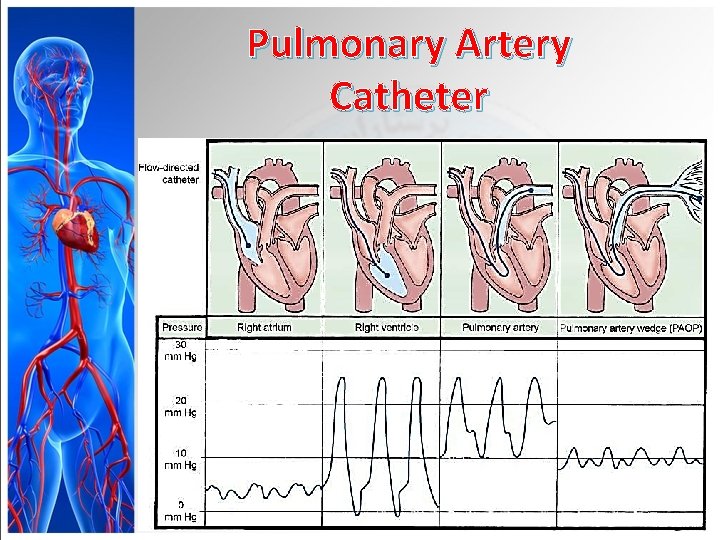
Pulmonary Artery Catheter
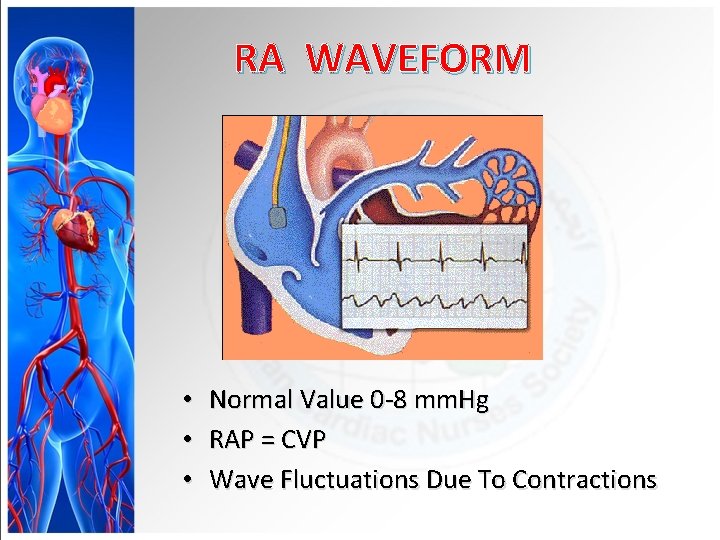
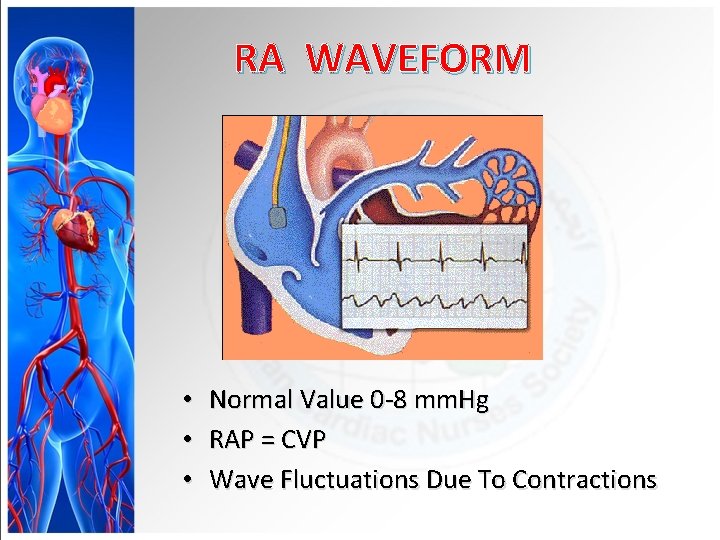
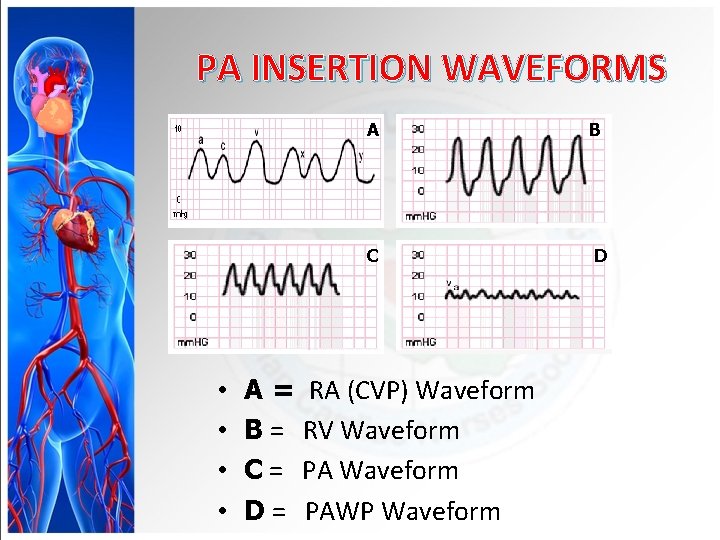
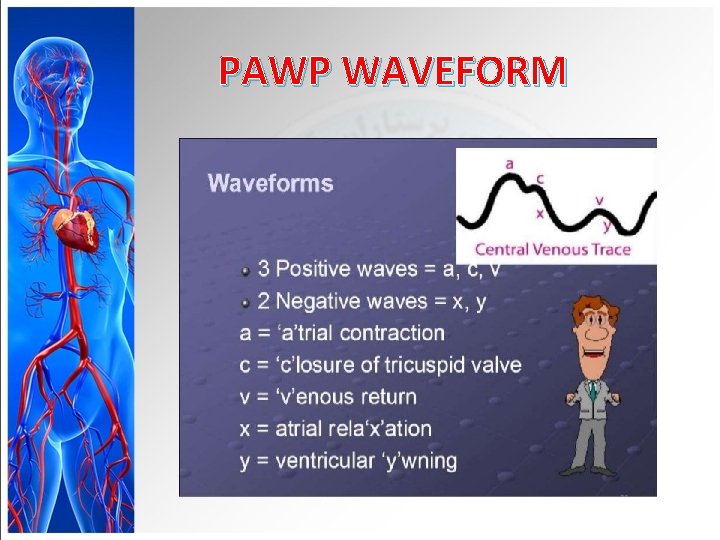
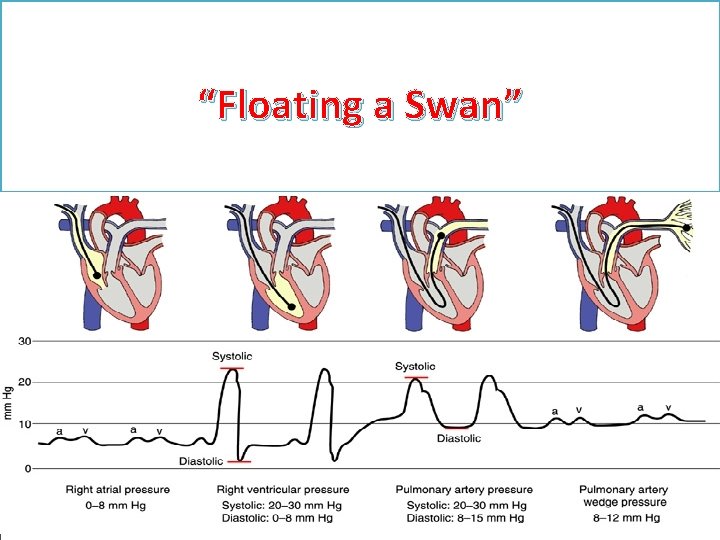
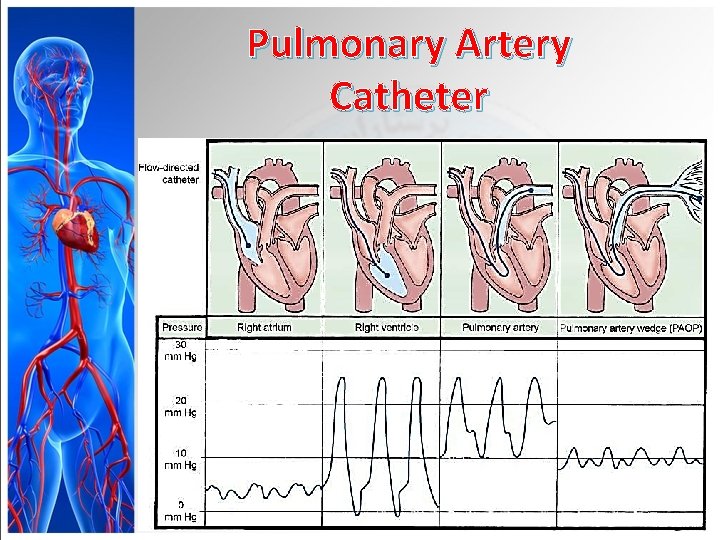
RA WAVEFORM • • • Normal Value 0 -8 mm. Hg RAP = CVP Wave Fluctuations Due To Contractions
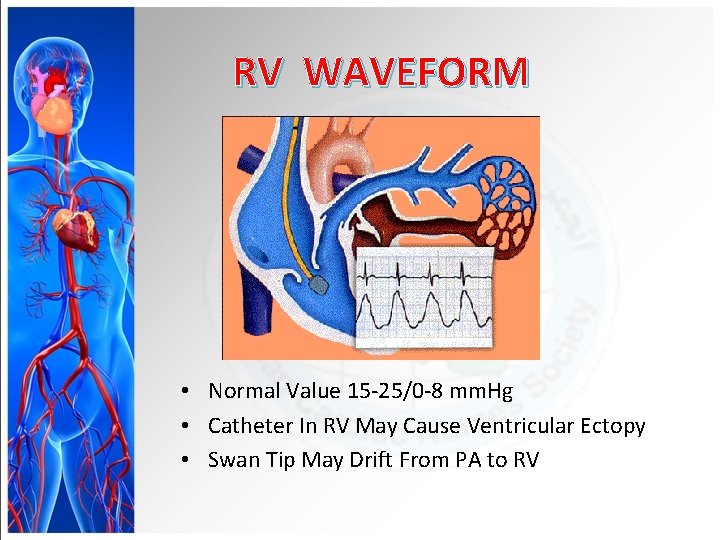
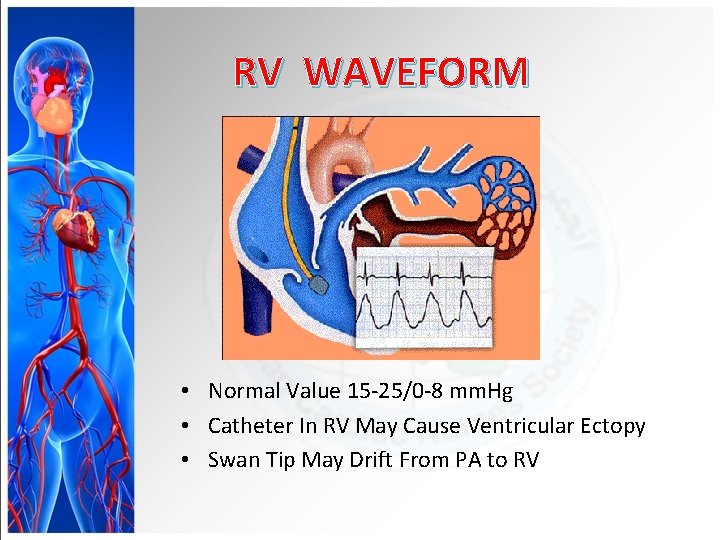
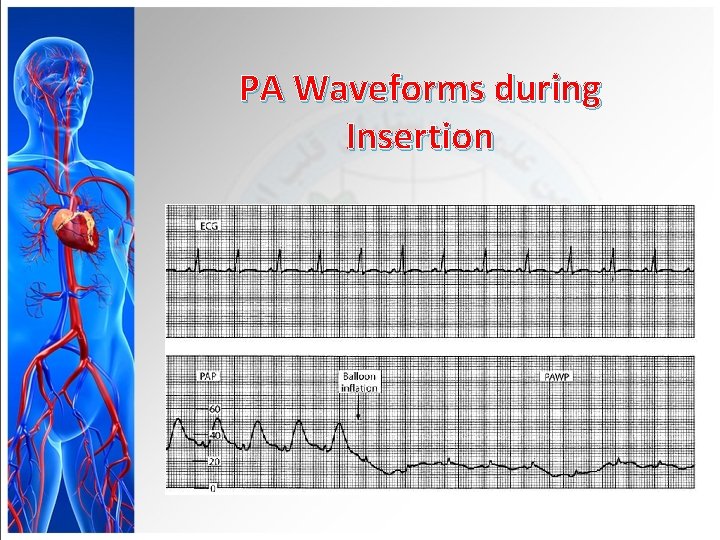
RV WAVEFORM • Normal Value 15 -25/0 -8 mm. Hg • Catheter In RV May Cause Ventricular Ectopy • Swan Tip May Drift From PA to RV
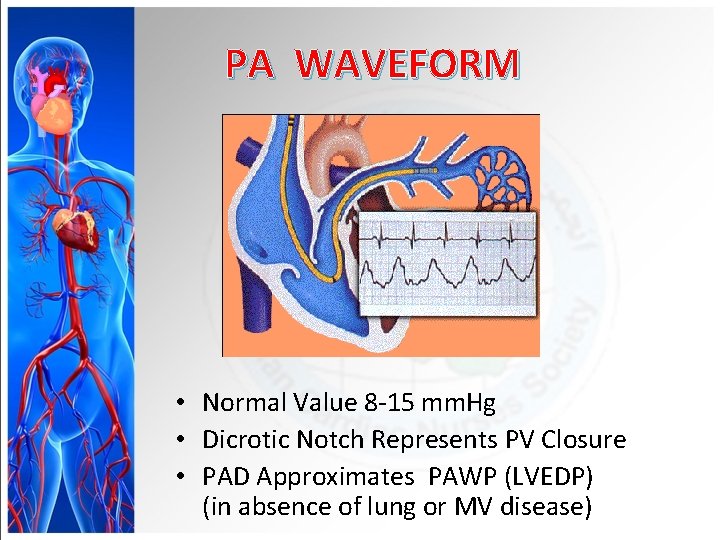
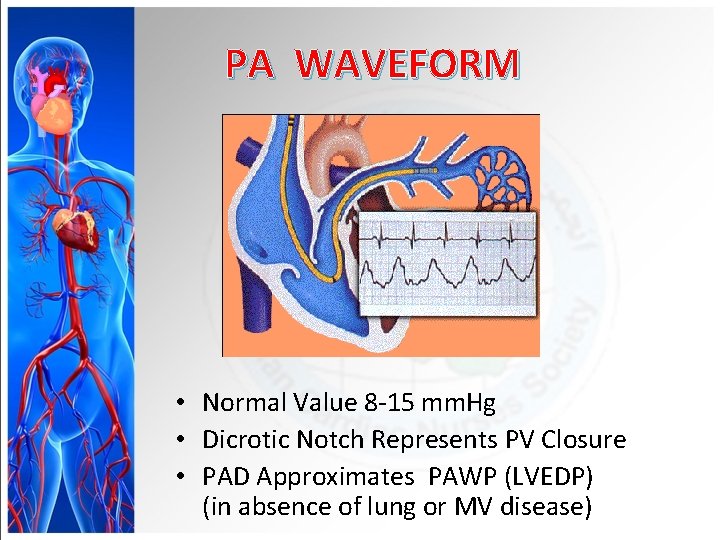
PA WAVEFORM • Normal Value 8 -15 mm. Hg • Dicrotic Notch Represents PV Closure • PAD Approximates PAWP (LVEDP) (in absence of lung or MV disease)
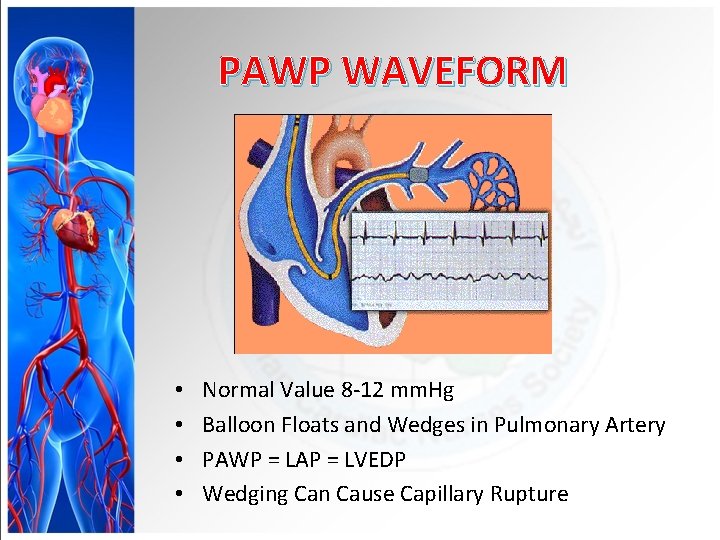
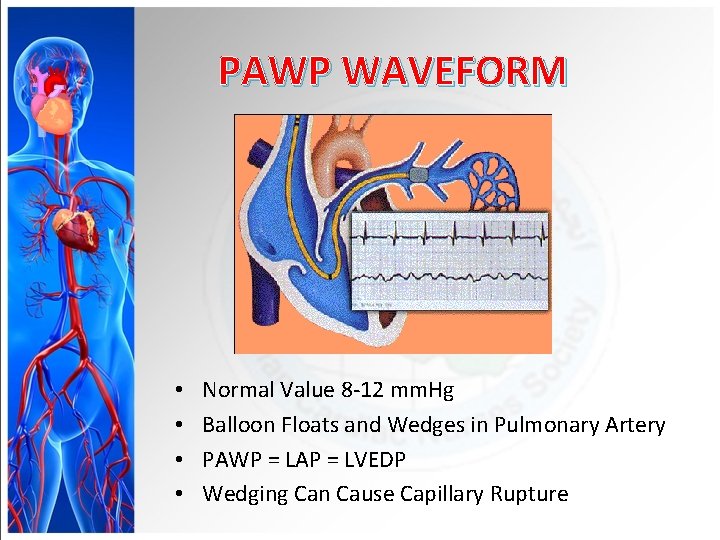
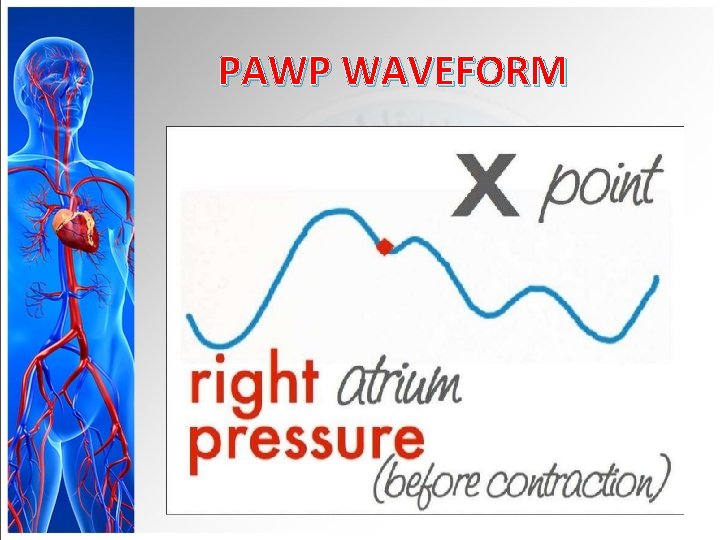
PAWP WAVEFORM • • Normal Value 8 -12 mm. Hg Balloon Floats and Wedges in Pulmonary Artery PAWP = LAP = LVEDP Wedging Can Cause Capillary Rupture
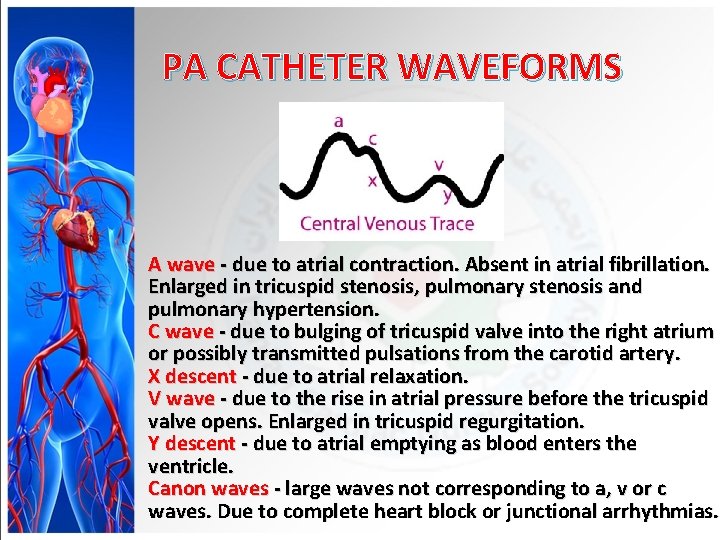
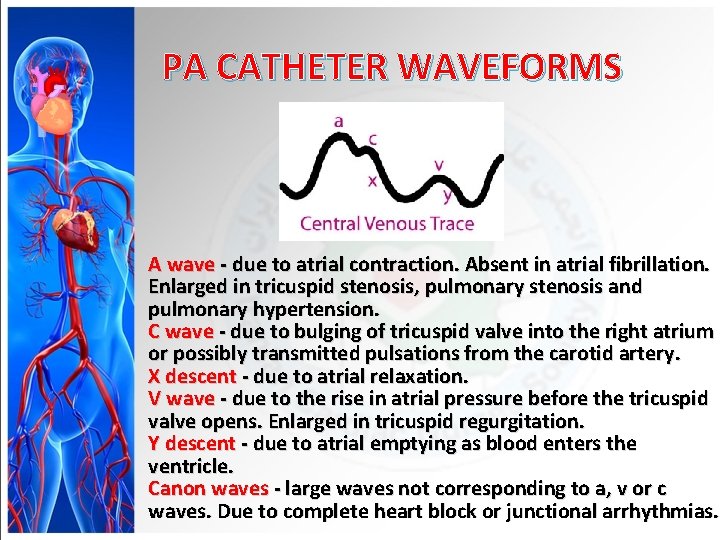
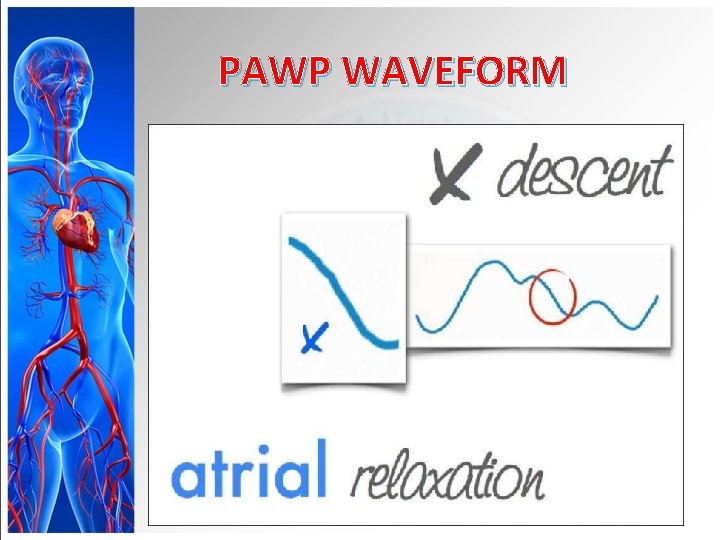
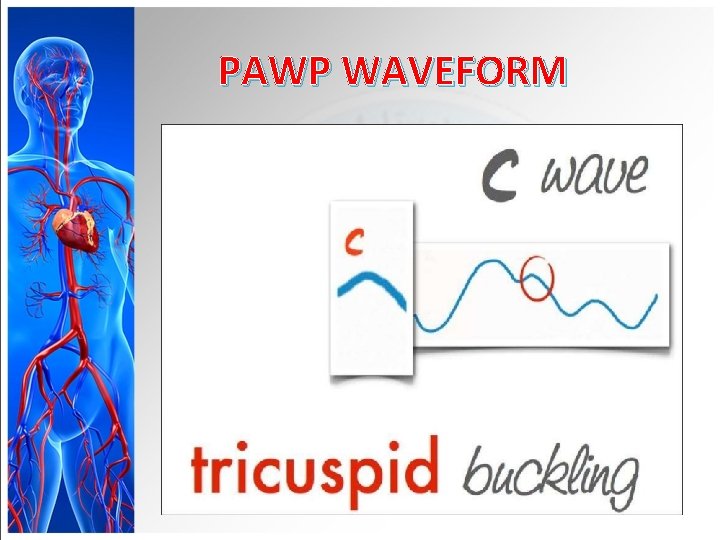
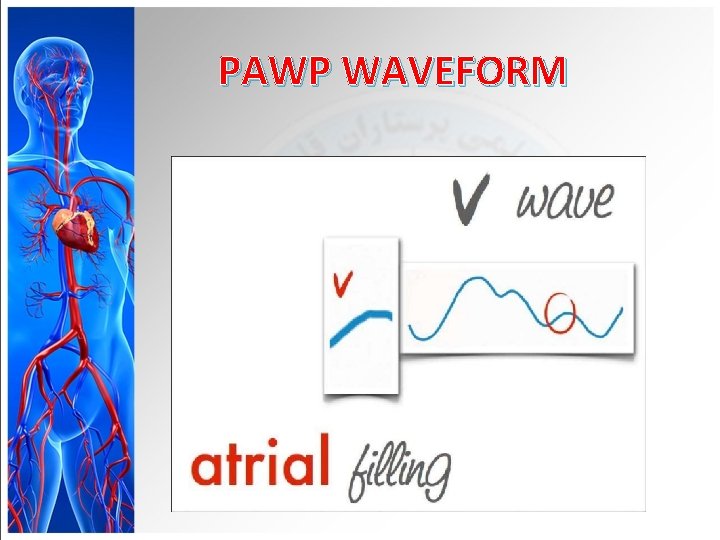
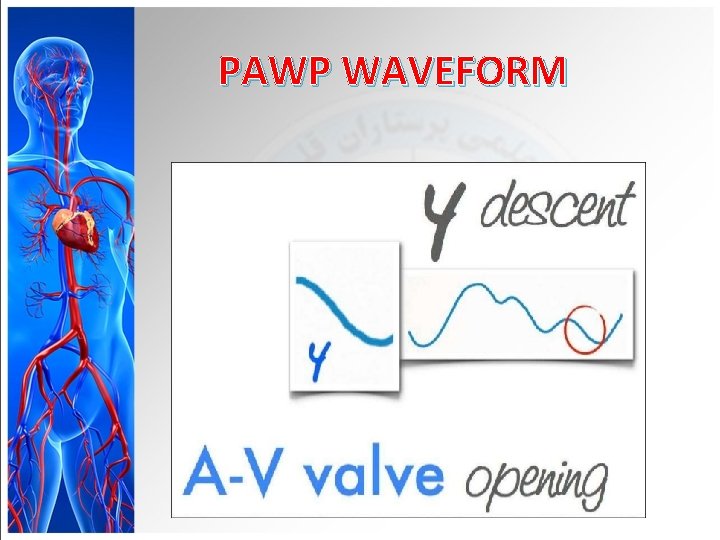
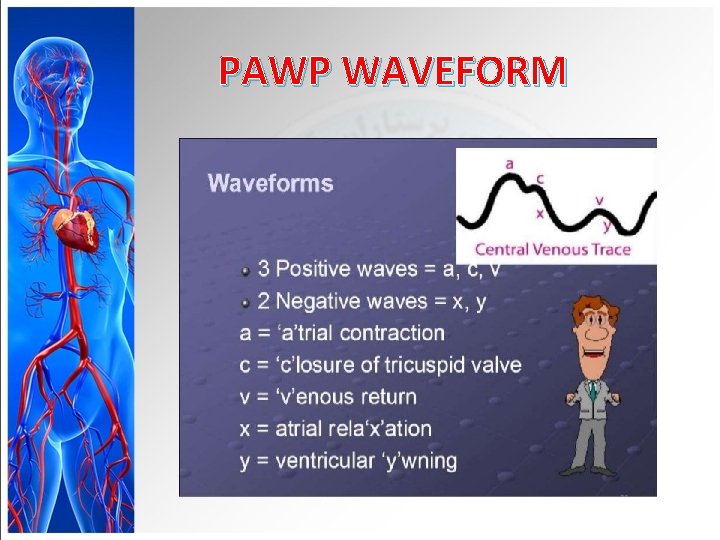
PA CATHETER WAVEFORMS A wave - due to atrial contraction. Absent in atrial fibrillation. Enlarged in tricuspid stenosis, pulmonary stenosis and pulmonary hypertension. C wave - due to bulging of tricuspid valve into the right atrium or possibly transmitted pulsations from the carotid artery. X descent - due to atrial relaxation. V wave - due to the rise in atrial pressure before the tricuspid valve opens. Enlarged in tricuspid regurgitation. Y descent - due to atrial emptying as blood enters the ventricle. Canon waves - large waves not corresponding to a, v or c waves. Due to complete heart block or junctional arrhythmias.
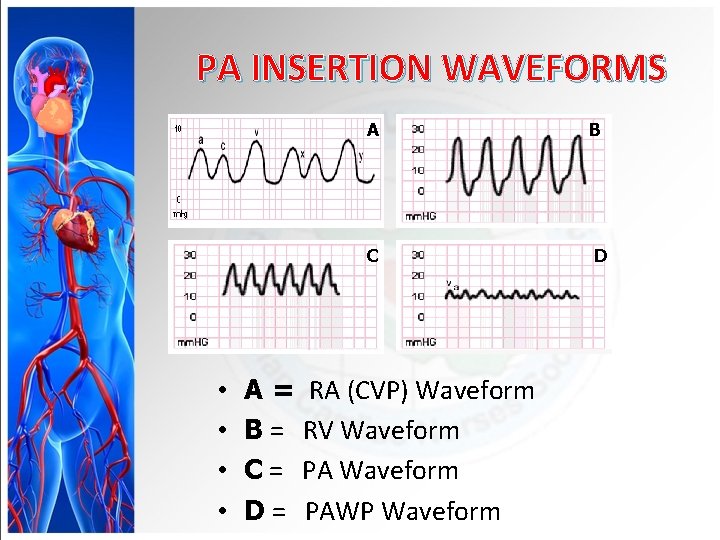
PA INSERTION WAVEFORMS • • A B C D A = RA (CVP) Waveform B = RV Waveform C = PA Waveform D = PAWP Waveform
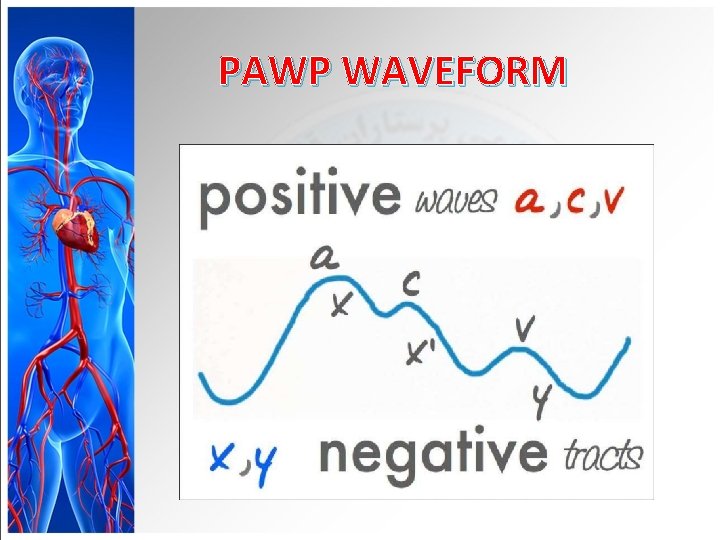
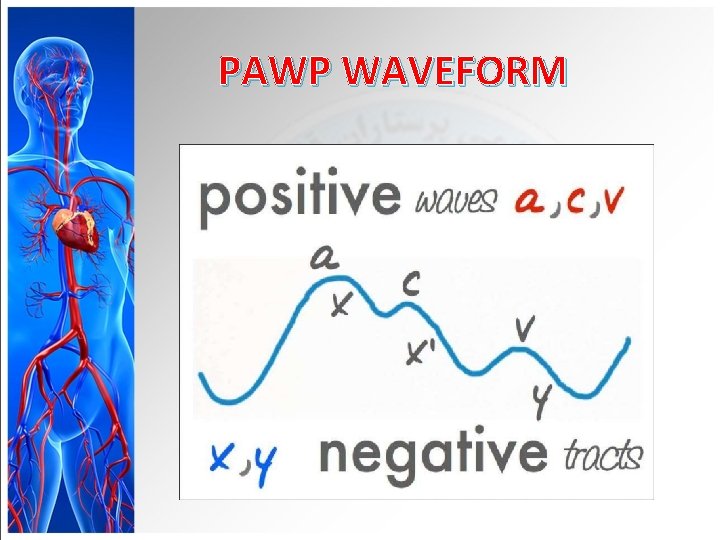
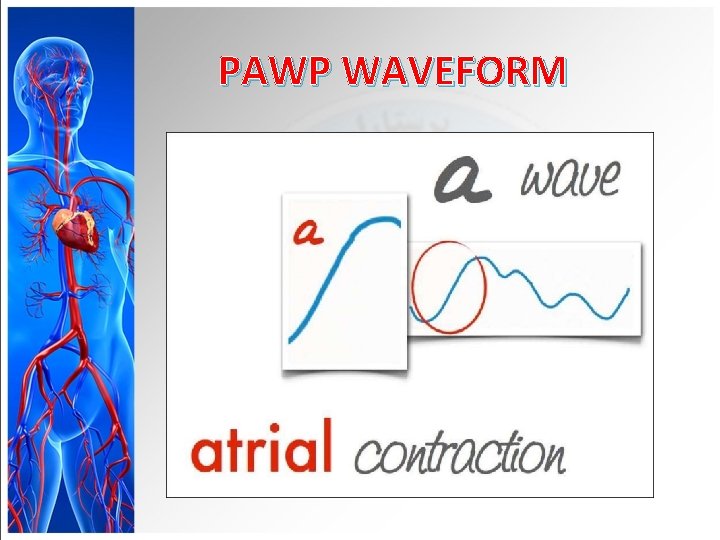
PAWP WAVEFORM
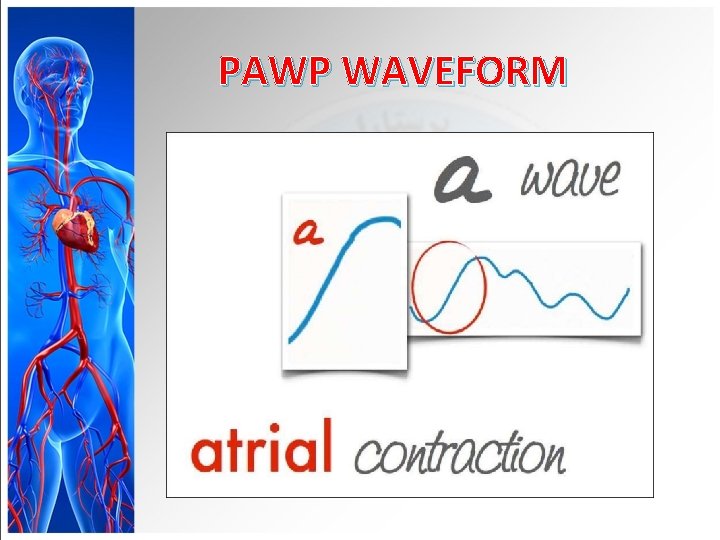
PAWP WAVEFORM
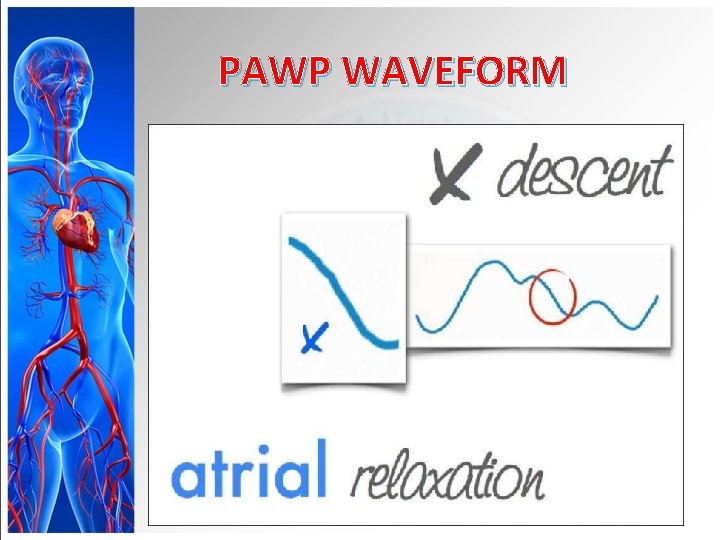
PAWP WAVEFORM
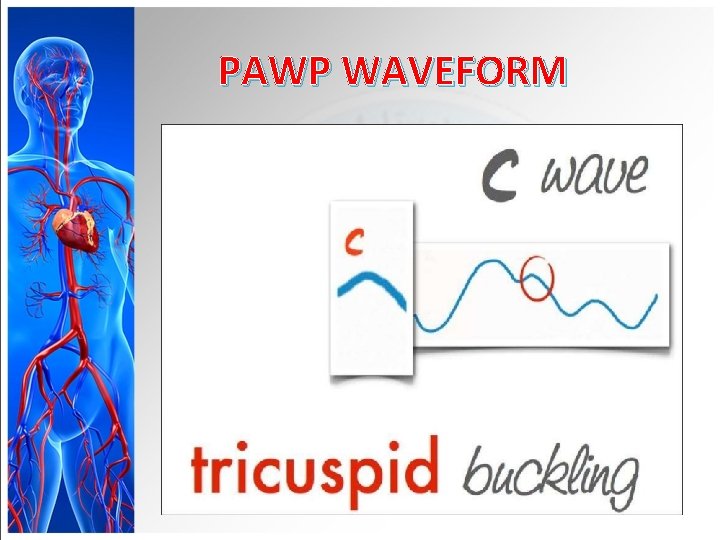
PAWP WAVEFORM
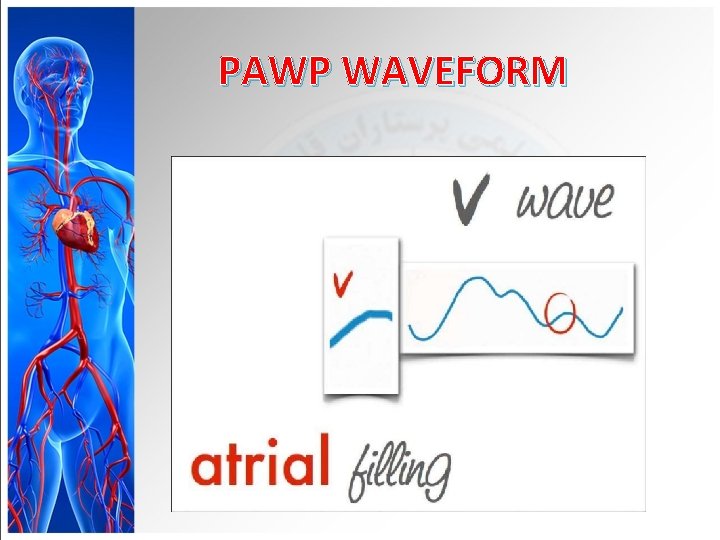
PAWP WAVEFORM
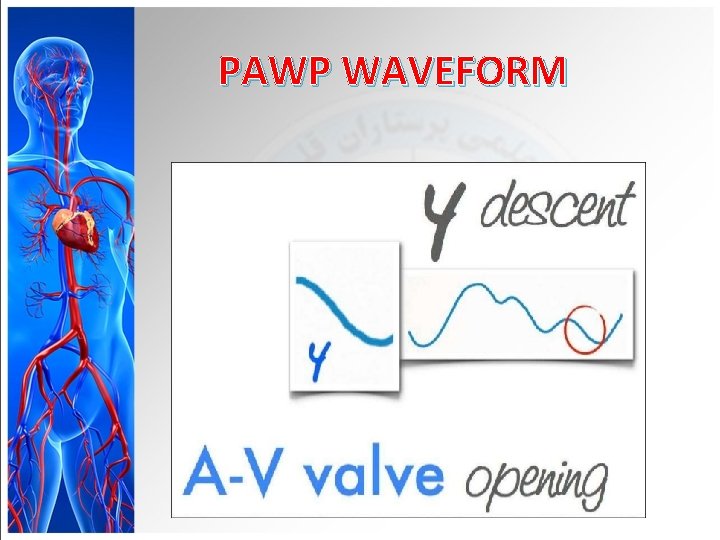
PAWP WAVEFORM
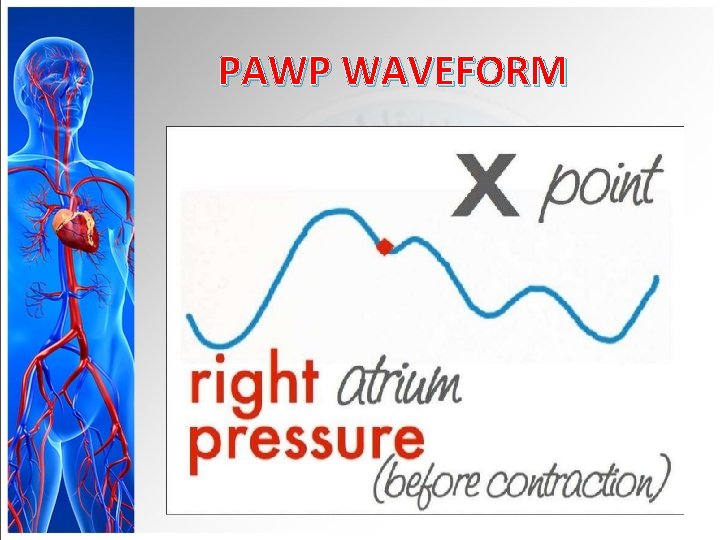
PAWP WAVEFORM
PAWP WAVEFORM
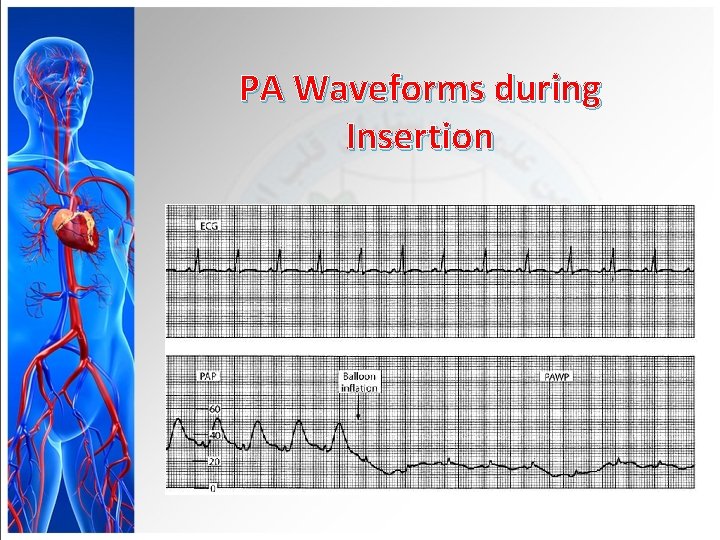
PA Waveforms during Insertion
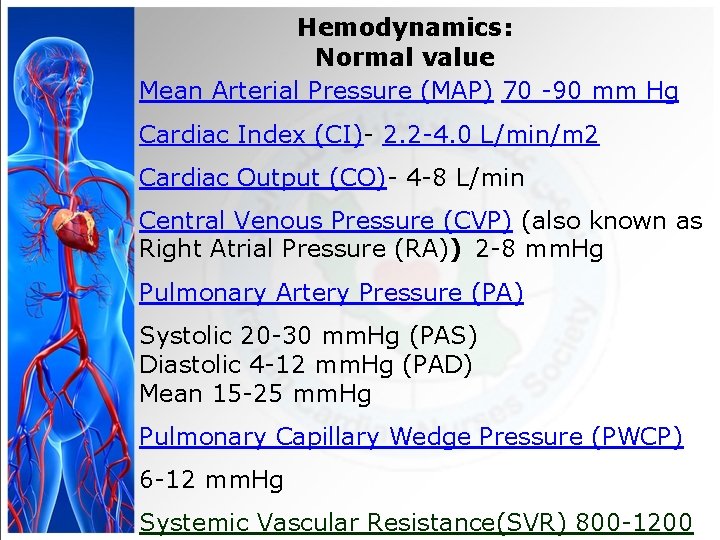
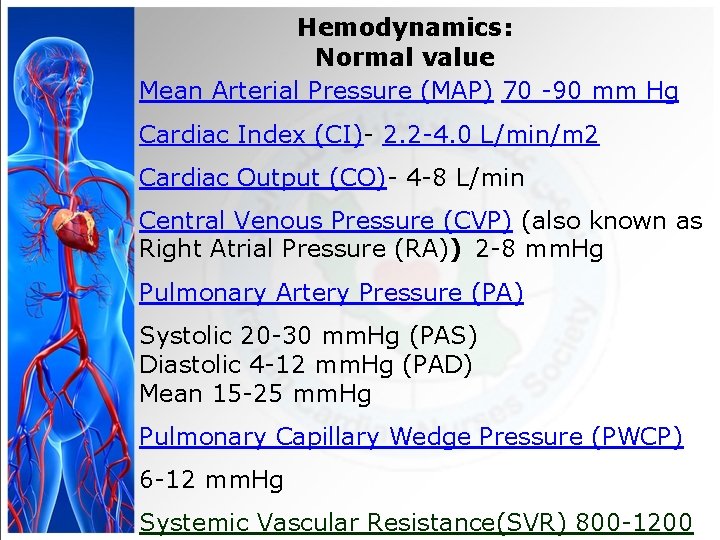
Hemodynamics: Normal value Mean Arterial Pressure (MAP) 70 -90 mm Hg Cardiac Index (CI)- 2. 2 -4. 0 L/min/m 2 Cardiac Output (CO)- 4 -8 L/min Central Venous Pressure (CVP) (also known as Right Atrial Pressure (RA)) 2 -8 mm. Hg Pulmonary Artery Pressure (PA) Systolic 20 -30 mm. Hg (PAS) Diastolic 4 -12 mm. Hg (PAD) Mean 15 -25 mm. Hg Pulmonary Capillary Wedge Pressure (PWCP) 6 -12 mm. Hg Systemic Vascular Resistance(SVR) 800 -1200
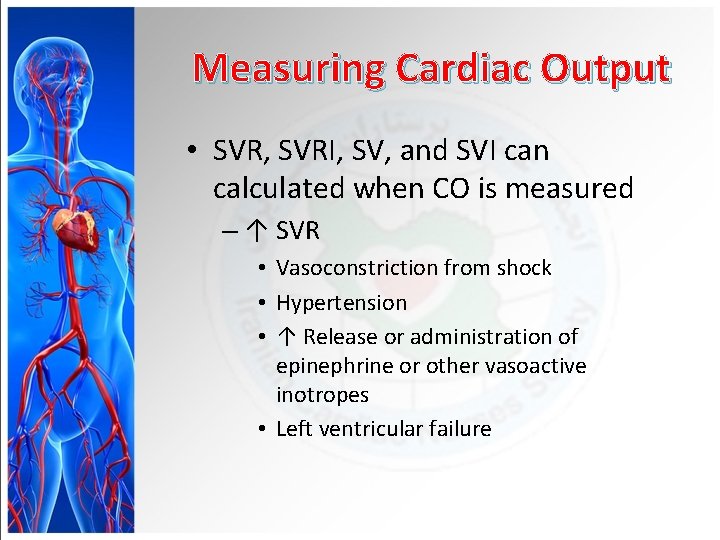
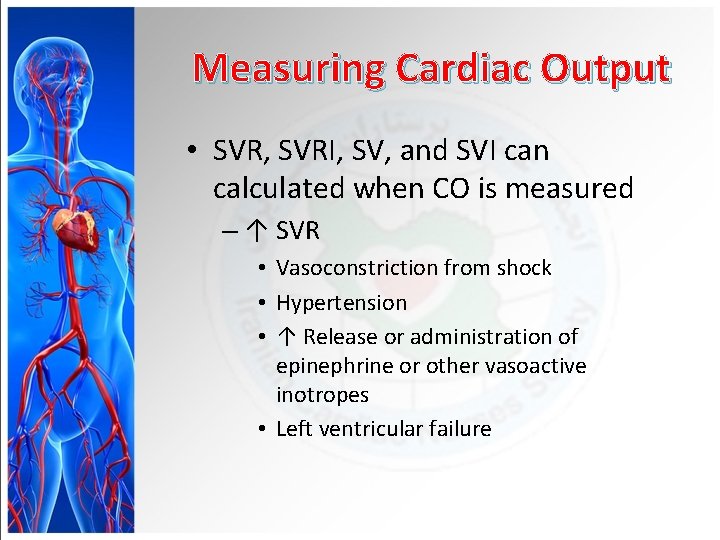
Measuring Cardiac Output • SVR, SVRI, SV, and SVI can calculated when CO is measured – ↑ SVR • Vasoconstriction from shock • Hypertension • ↑ Release or administration of epinephrine or other vasoactive inotropes • Left ventricular failure
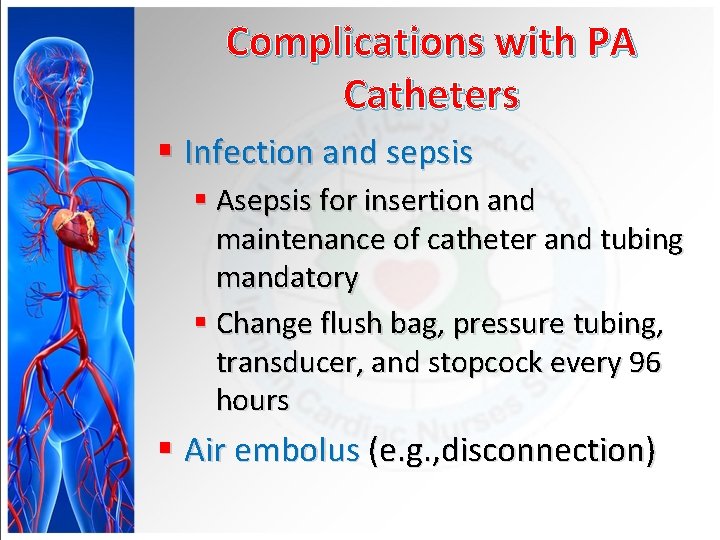
Complications with PA Catheters § Infection and sepsis § Asepsis for insertion and maintenance of catheter and tubing mandatory § Change flush bag, pressure tubing, transducer, and stopcock every 96 hours § Air embolus (e. g. , disconnection)
Complications with PA Catheters § Ventricular dysrhythmias § During PA catheter insertion or removal § If tip migrates back from PA to right ventricle § PA catheter cannot be wedged § May need repositioning
Complications with PA Catheters § Pulmonary infarction or PA rupture § Balloon rupture (e. g. , overinflation) § Prolonged inflation § Spontaneous wedging § Thrombus/embolus formation
Noninvasive Hemodynamic Monitoring § Major indications • Early signs and symptoms of pulmonary or cardiac dysfunction • Differentiation of cardiac or pulmonary cause of shortness of breath • Evaluation of etiology and management of hypotension
Noninvasive Hemodynamic Monitoring § Major indications(cont’d) • Monitoring after discontinuing a PA catheter or justification for insertion of a PA catheter • Evaluation of pharmacotherapy • Diagnosis of rejection following cardiac transplantation

QUESTION?
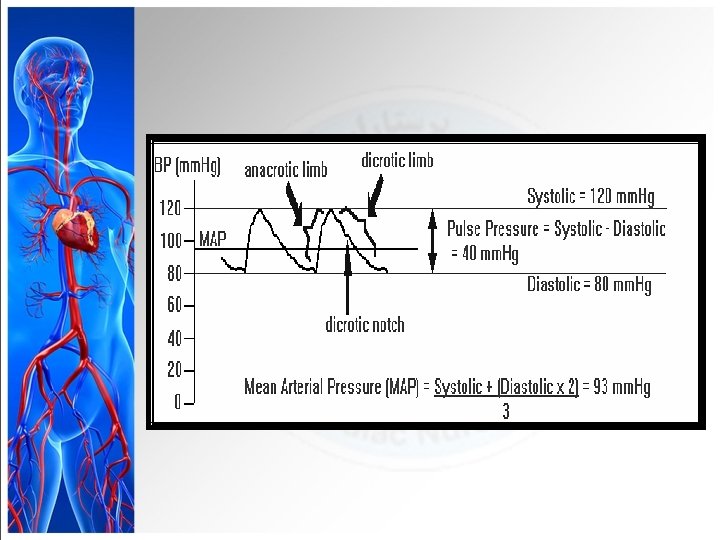
 How to calculate mean arterial pressure
How to calculate mean arterial pressure Map formula bp
Map formula bp Arterial blood pressure definition
Arterial blood pressure definition Mean pulmonary arterial pressure
Mean pulmonary arterial pressure Vasoreflexes
Vasoreflexes Systolic and diastolic pressure
Systolic and diastolic pressure Vasodilatos
Vasodilatos Cns ischemic response flow chart
Cns ischemic response flow chart Cvp normal range
Cvp normal range Normal cvp
Normal cvp Intra abdominal pressure monitoring
Intra abdominal pressure monitoring Downhole pressure monitoring
Downhole pressure monitoring Decorticate
Decorticate Insall salvati ratio
Insall salvati ratio Pressure support vs pressure control
Pressure support vs pressure control Pressure mapping for pressure ulcers
Pressure mapping for pressure ulcers Intrapulmonary pressure
Intrapulmonary pressure Describing edema
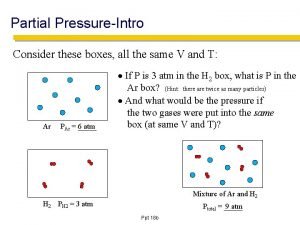
Describing edema Partial pressure formula
Partial pressure formula Clubbing fingers
Clubbing fingers How are metamorphic rocks classified
How are metamorphic rocks classified Pressure support vs pressure control
Pressure support vs pressure control Bernoulli equation mass flow rate
Bernoulli equation mass flow rate Oncotic pressure vs hydrostatic
Oncotic pressure vs hydrostatic Oncotic pressure
Oncotic pressure Oncotic vs osmotic pressure
Oncotic vs osmotic pressure Hydrostatic oncotic pressure
Hydrostatic oncotic pressure Metamorphism
Metamorphism How to find partial pressure
How to find partial pressure P support in ventilator
P support in ventilator High pressure and low pressure
High pressure and low pressure High pressure and low pressure
High pressure and low pressure Blood supply to thoracic wall
Blood supply to thoracic wall Peripheral arterial pulse sites
Peripheral arterial pulse sites Macrodrip vs microdrip
Macrodrip vs microdrip Tentorium cerebelli cranial nerve
Tentorium cerebelli cranial nerve Puntos anatomicos para tomar la presion arterial
Puntos anatomicos para tomar la presion arterial Arterial arcades of jejunum and ileum
Arterial arcades of jejunum and ileum Veia pulmonar sangue arterial
Veia pulmonar sangue arterial Valores da tensão arterial
Valores da tensão arterial Sinais vitais criança
Sinais vitais criança O que é hipocondrio
O que é hipocondrio Rutas integrales de atencion en salud
Rutas integrales de atencion en salud Qon ketishda birinchi tibbiy yordam
Qon ketishda birinchi tibbiy yordam Veia pulmonar sangue arterial
Veia pulmonar sangue arterial Arterial wave form
Arterial wave form Gush blood spatter
Gush blood spatter Twin anaemia polycythaemia sequence
Twin anaemia polycythaemia sequence Aeromesenterie
Aeromesenterie Arterial blood vs venous blood
Arterial blood vs venous blood Gasometra
Gasometra Normal blood gas levels
Normal blood gas levels Percentiles de presión arterial en niños oms
Percentiles de presión arterial en niños oms Puntos anatomicos para tomar la presion arterial
Puntos anatomicos para tomar la presion arterial Arteriografia taça invertida
Arteriografia taça invertida Arterial underfilling
Arterial underfilling Presion arterial
Presion arterial Arterial spray spatter
Arterial spray spatter Arterial vs venous end of capillary
Arterial vs venous end of capillary Gas exchange between tissues and capillaries
Gas exchange between tissues and capillaries Arterial spurting pattern
Arterial spurting pattern Classificação de rutherford para oclusão arterial aguda
Classificação de rutherford para oclusão arterial aguda Arterial line whip
Arterial line whip