Peripheral Arterial Disease Simulation Training Curriculum 1 Peripheral
- Slides: 97
Peripheral Arterial Disease: Simulation Training Curriculum 1
Peripheral Arterial Disease üEtiology Epidemiology Physical examination Clinical Manifestations Diagnosis Indications Treatment Options Prognosis 2
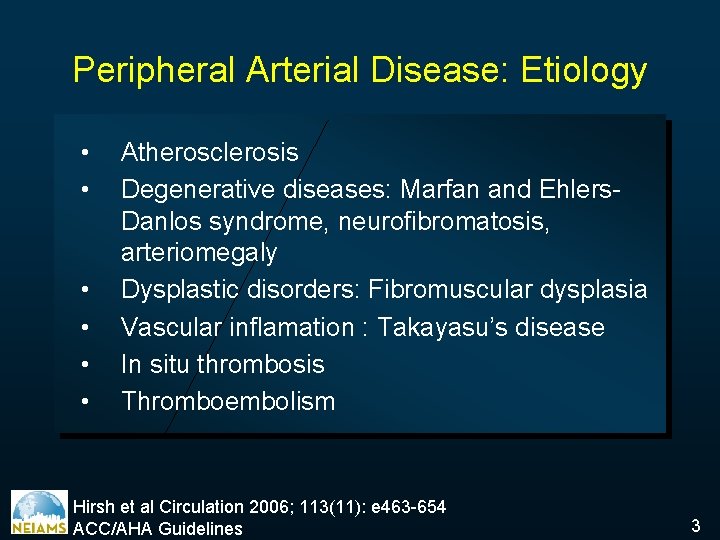
Peripheral Arterial Disease: Etiology • • • Atherosclerosis Degenerative diseases: Marfan and Ehlers. Danlos syndrome, neurofibromatosis, arteriomegaly Dysplastic disorders: Fibromuscular dysplasia Vascular inflamation : Takayasu’s disease In situ thrombosis Thromboembolism Hirsh et al Circulation 2006; 113(11): e 463 -654 ACC/AHA Guidelines 3
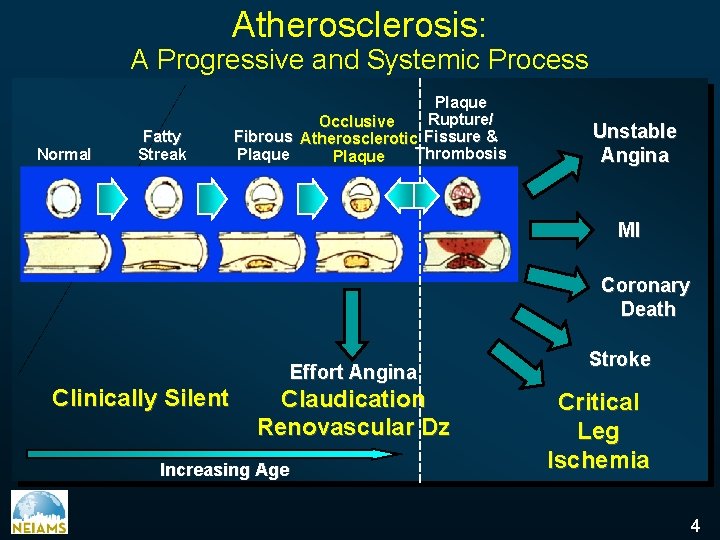
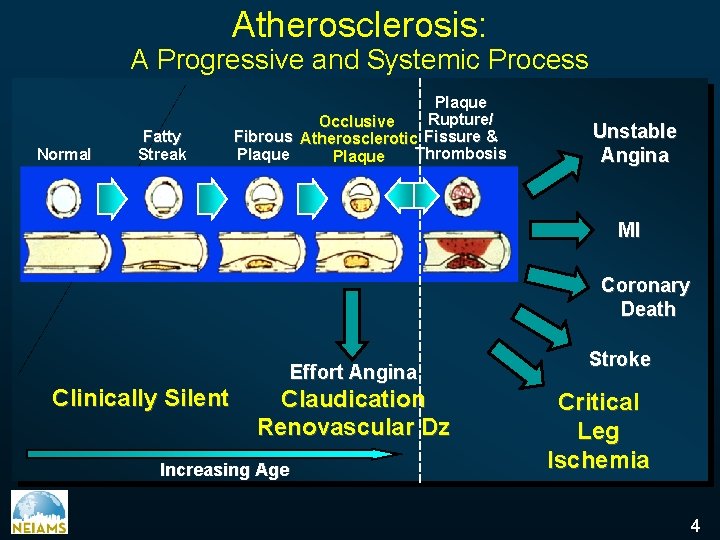
Atherosclerosis: A Progressive and Systemic Process Normal Fatty Streak Plaque Rupture/ Occlusive Fibrous Atherosclerotic Fissure & Thrombosis Plaque Unstable Angina MI Coronary Death Effort Angina Clinically Silent Claudication Renovascular Dz Increasing Age Stroke Critical Leg Ischemia 4
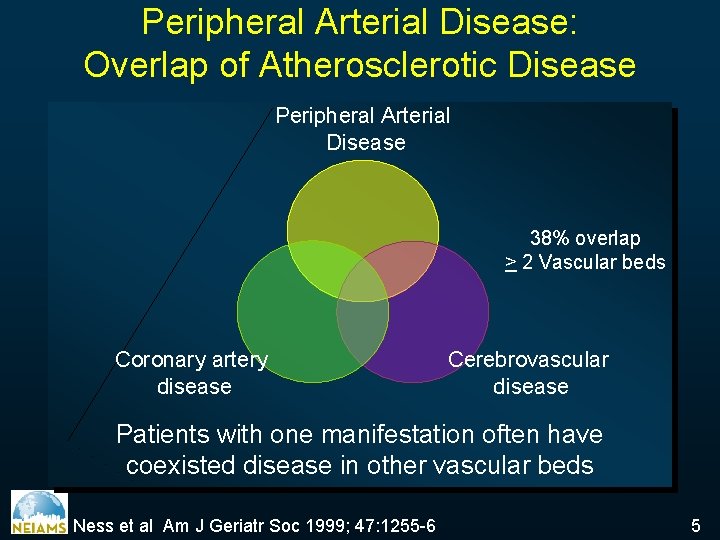
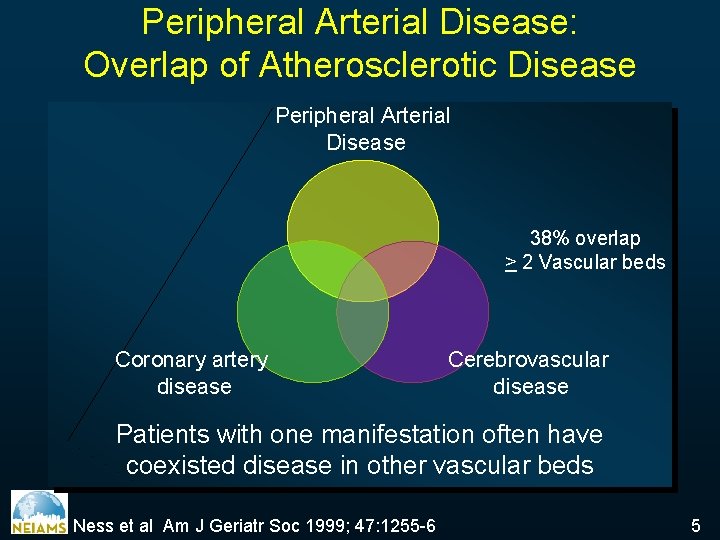
Peripheral Arterial Disease: Overlap of Atherosclerotic Disease Peripheral Arterial Disease 38% overlap > 2 Vascular beds Coronary artery disease Cerebrovascular disease Patients with one manifestation often have coexisted disease in other vascular beds Ness et al Am J Geriatr Soc 1999; 47: 1255 -6 5
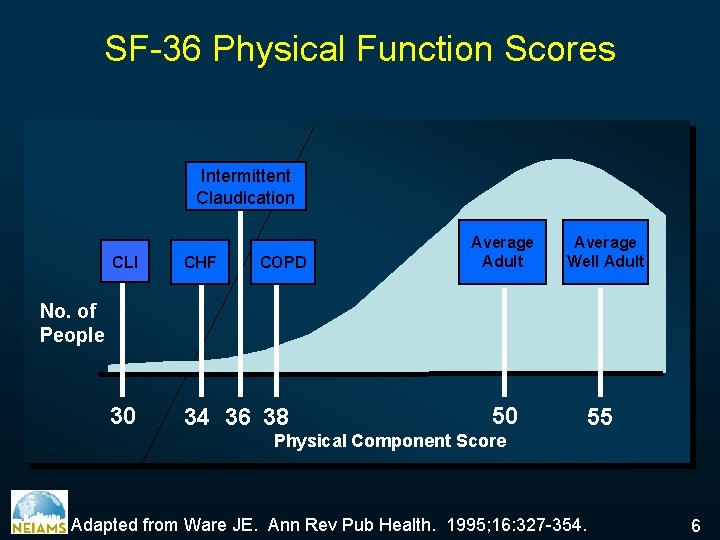
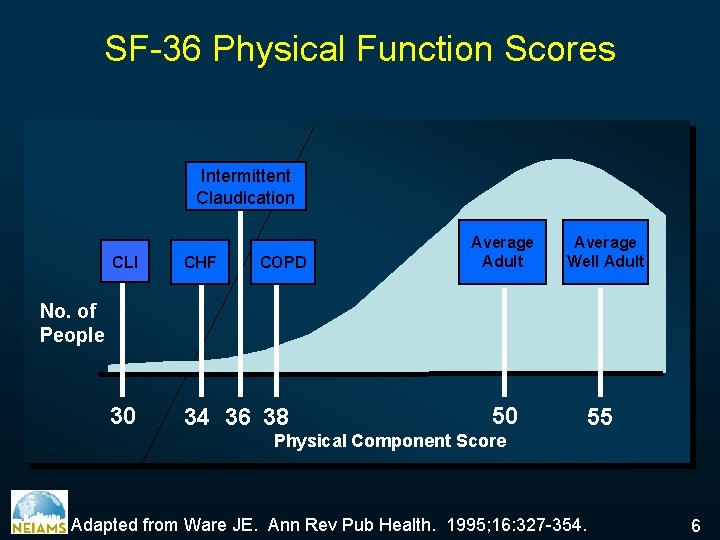
SF-36 Physical Function Scores Intermittent Claudication CLI CHF 30 34 36 38 COPD Average Adult Average Well Adult No. of People 50 55 Physical Component Score Adapted from Ware JE. Ann Rev Pub Health. 1995; 16: 327 -354. 6
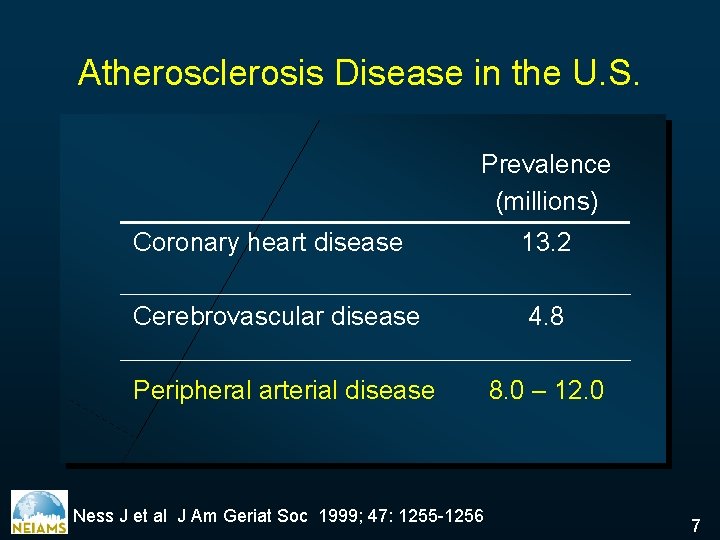
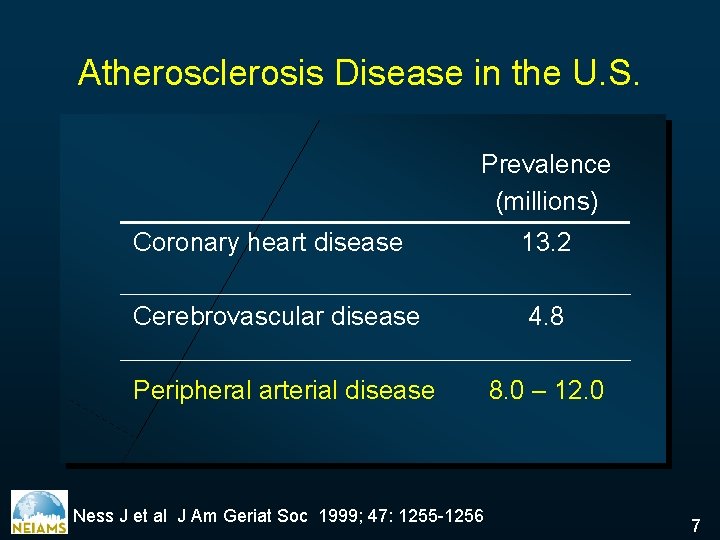
Atherosclerosis Disease in the U. S. Prevalence (millions) Coronary heart disease 13. 2 Cerebrovascular disease 4. 8 Peripheral arterial disease 8. 0 – 12. 0 Ness J et al J Am Geriat Soc 1999; 47: 1255 -1256 7
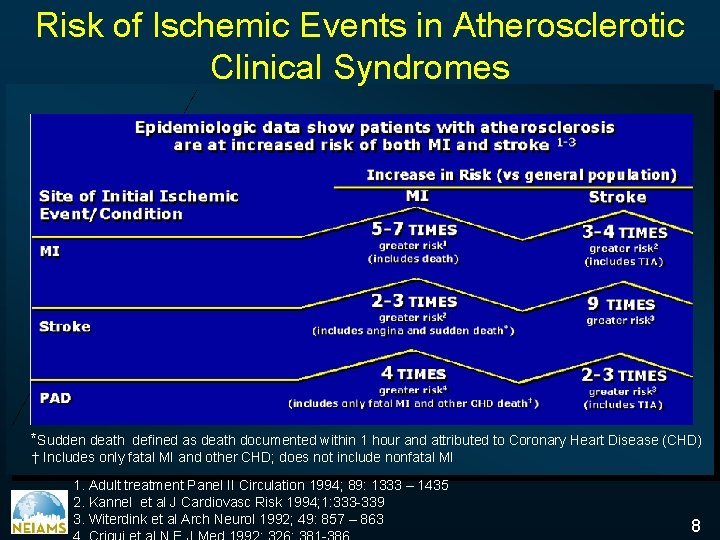
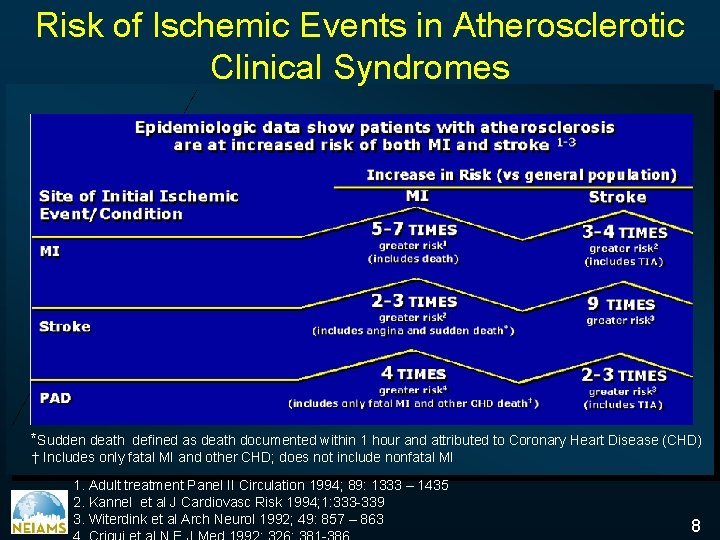
Risk of Ischemic Events in Atherosclerotic Clinical Syndromes *Sudden death defined as death documented within 1 hour and attributed to Coronary Heart Disease (CHD) † Includes only fatal MI and other CHD; does not include nonfatal MI 1. Adult treatment Panel II Circulation 1994; 89: 1333 – 1435 2. Kannel et al J Cardiovasc Risk 1994; 1: 333 -339 3. Witerdink et al Arch Neurol 1992; 49: 857 – 863 8
Peripheral Arterial Disease Etiology üEpidemiology Physical examination Clinical Manifestations Diagnosis Indications Treatment Options Prognosis 9
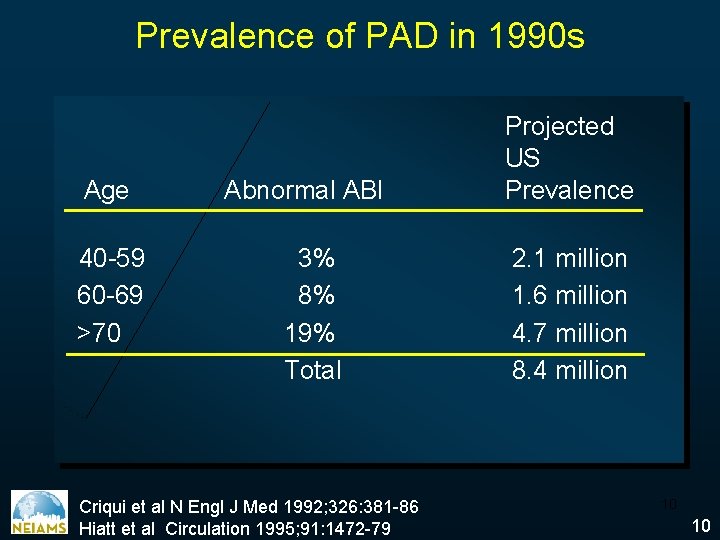
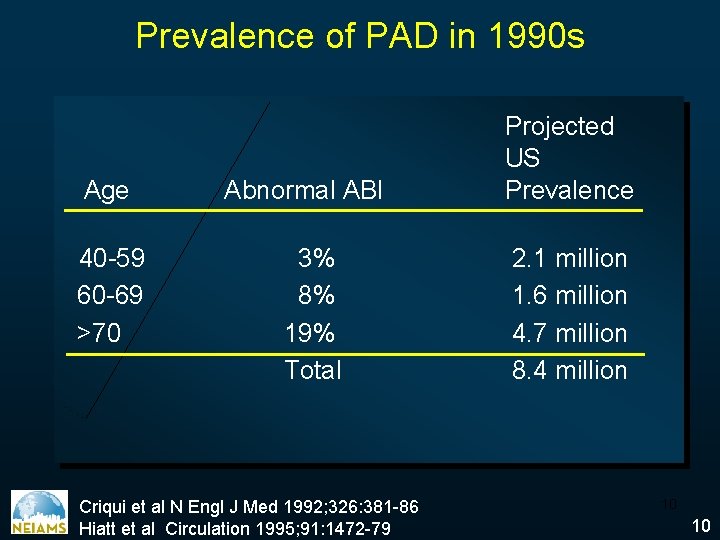
Prevalence of PAD in 1990 s Age 40 -59 60 -69 >70 Abnormal ABI 3% 8% 19% Total Criqui et al N Engl J Med 1992; 326: 381 -86 Hiatt et al Circulation 1995; 91: 1472 -79 Projected US Prevalence 2. 1 million 1. 6 million 4. 7 million 8. 4 million 10 10
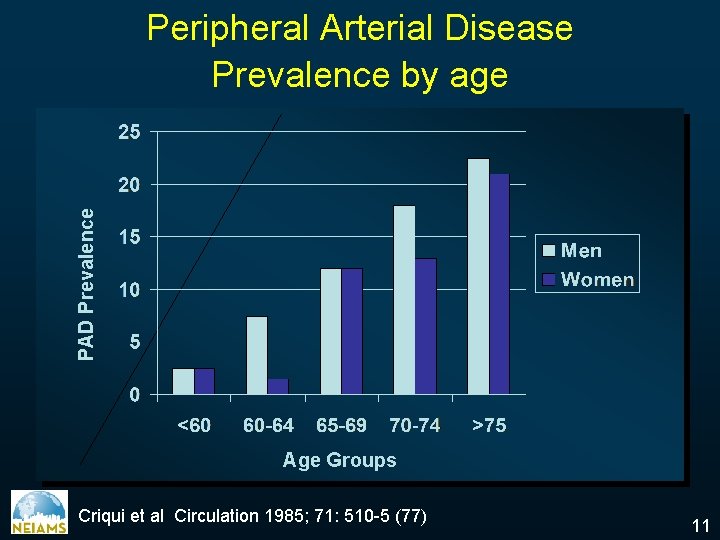
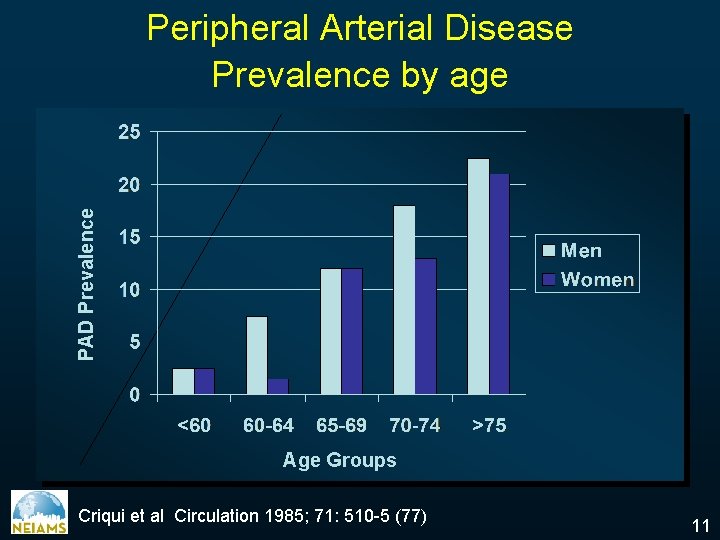
PAD Prevalence Peripheral Arterial Disease Prevalence by age Age Groups Criqui et al Circulation 1985; 71: 510 -5 (77) 11
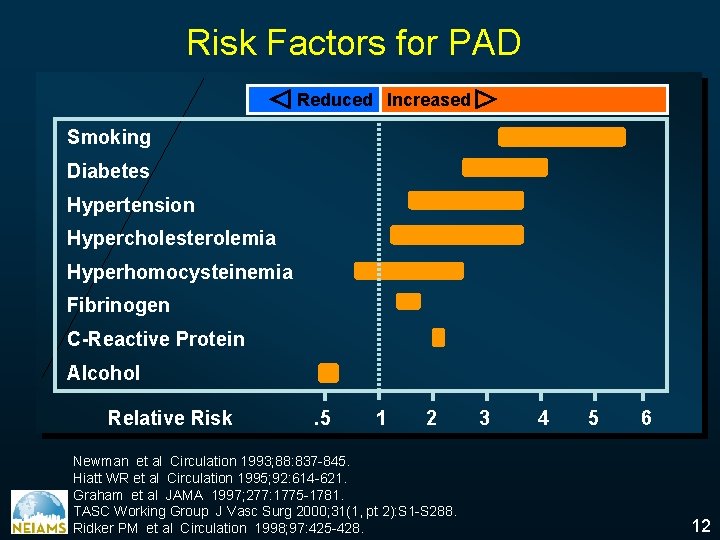
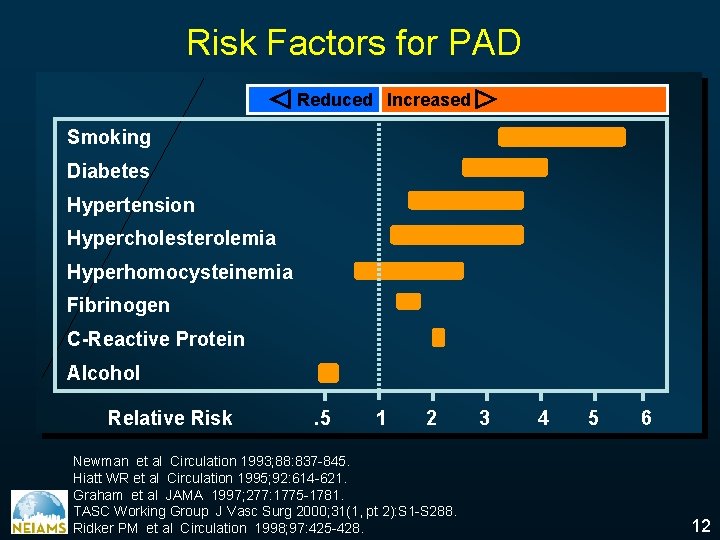
Risk Factors for PAD Reduced Increased Smoking Diabetes Hypertension Hypercholesterolemia Hyperhomocysteinemia Fibrinogen C-Reactive Protein Alcohol Relative Risk . 5 1 2 Newman et al Circulation 1993; 88: 837 -845. Hiatt WR et al Circulation 1995; 92: 614 -621. Graham et al JAMA 1997; 277: 1775 -1781. TASC Working Group J Vasc Surg 2000; 31(1, pt 2): S 1 -S 288. Ridker PM et al Circulation 1998; 97: 425 -428. 3 4 5 6 12
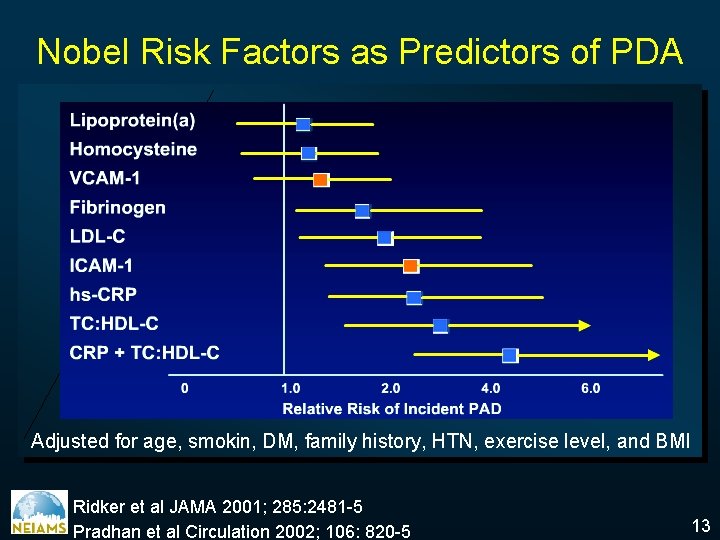
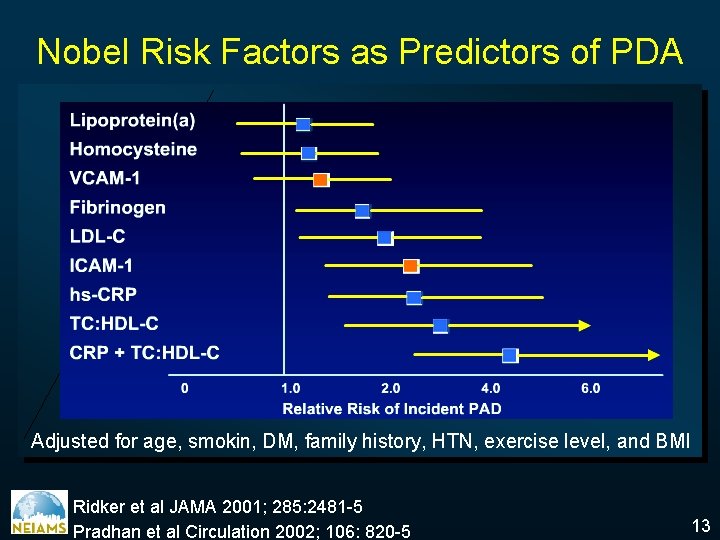
Nobel Risk Factors as Predictors of PDA Adjusted for age, smokin, DM, family history, HTN, exercise level, and BMI Ridker et al JAMA 2001; 285: 2481 -5 Pradhan et al Circulation 2002; 106: 820 -5 13
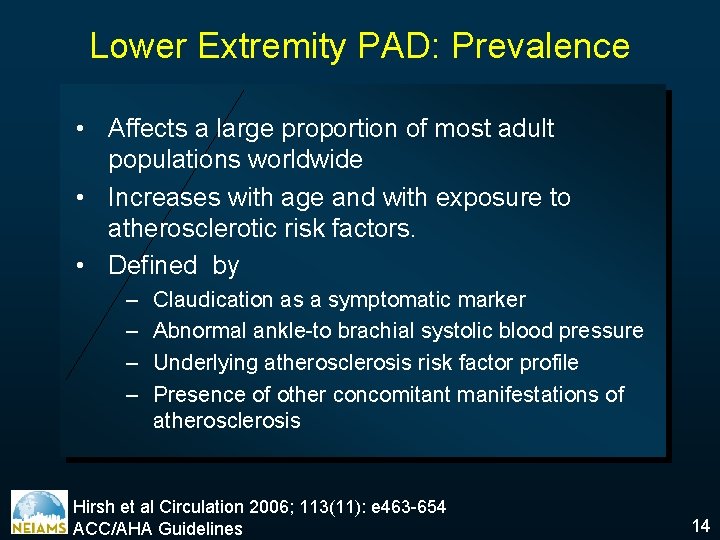
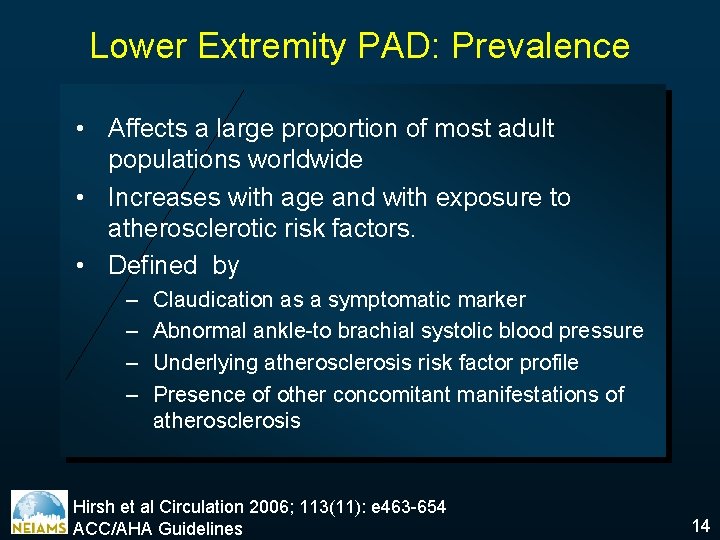
Lower Extremity PAD: Prevalence • Affects a large proportion of most adult populations worldwide • Increases with age and with exposure to atherosclerotic risk factors. • Defined by – – Claudication as a symptomatic marker Abnormal ankle-to brachial systolic blood pressure Underlying atherosclerosis risk factor profile Presence of other concomitant manifestations of atherosclerosis Hirsh et al Circulation 2006; 113(11): e 463 -654 ACC/AHA Guidelines 14
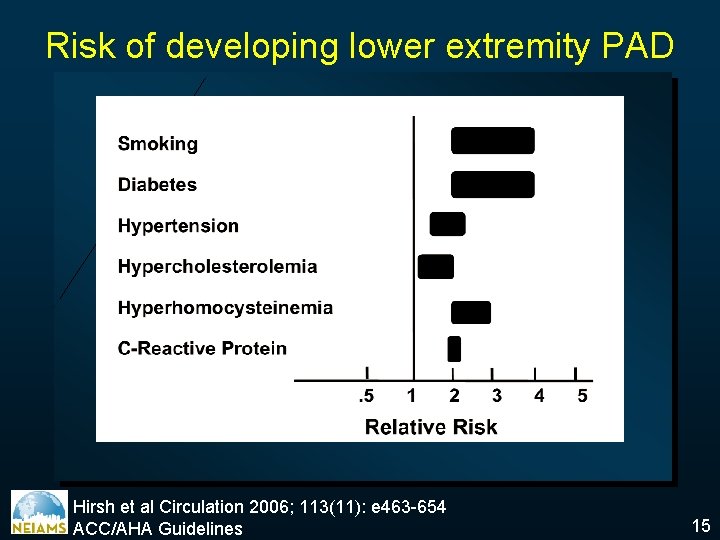
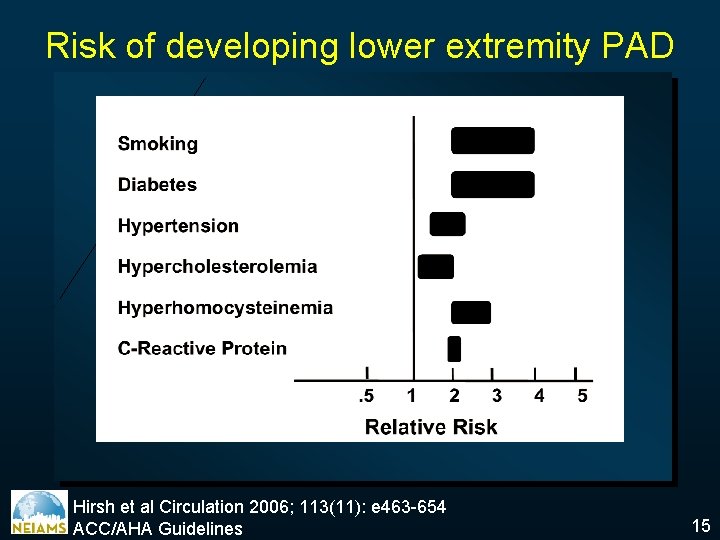
Risk of developing lower extremity PAD Hirsh et al Circulation 2006; 113(11): e 463 -654 ACC/AHA Guidelines 15
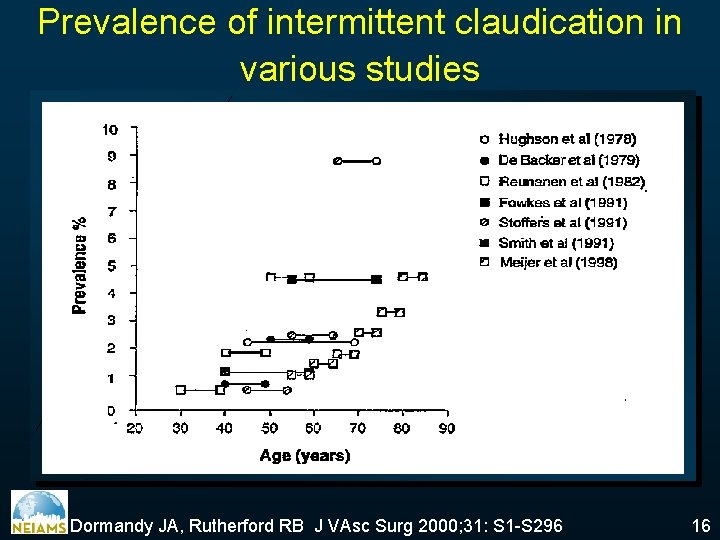
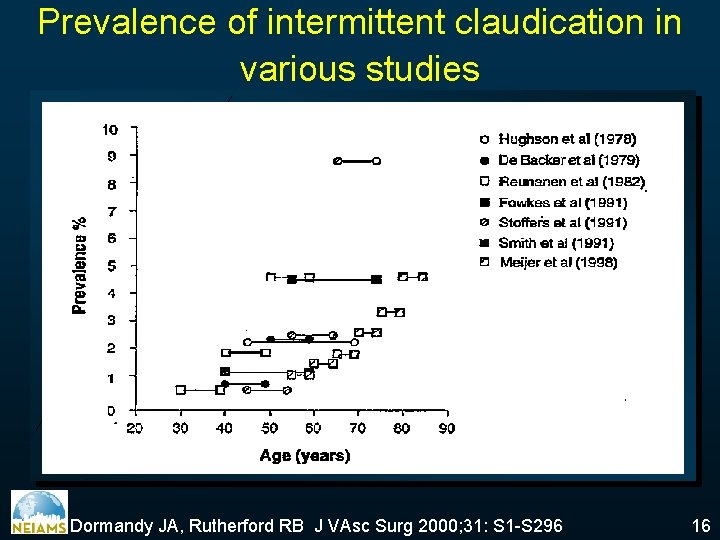
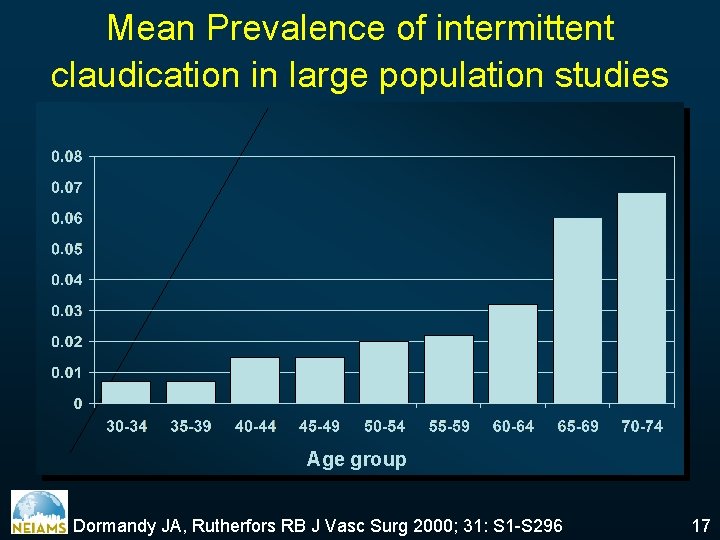
Prevalence of intermittent claudication in various studies Dormandy JA, Rutherford RB J VAsc Surg 2000; 31: S 1 -S 296 16
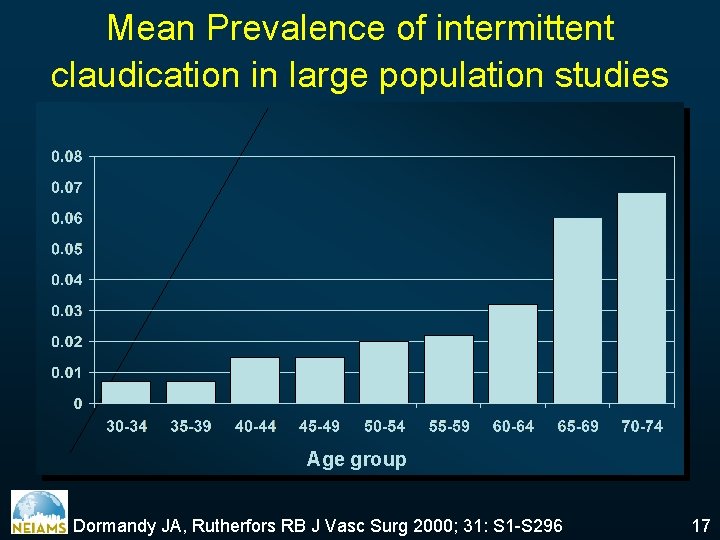
Mean Prevalence of intermittent claudication in large population studies Age group Dormandy JA, Rutherfors RB J Vasc Surg 2000; 31: S 1 -S 296 17
Peripheral Arterial Disease Etiology Epidemiology üPhysical examination Clinical Manifestations Diagnosis Indications Treatment Options Prognosis 18
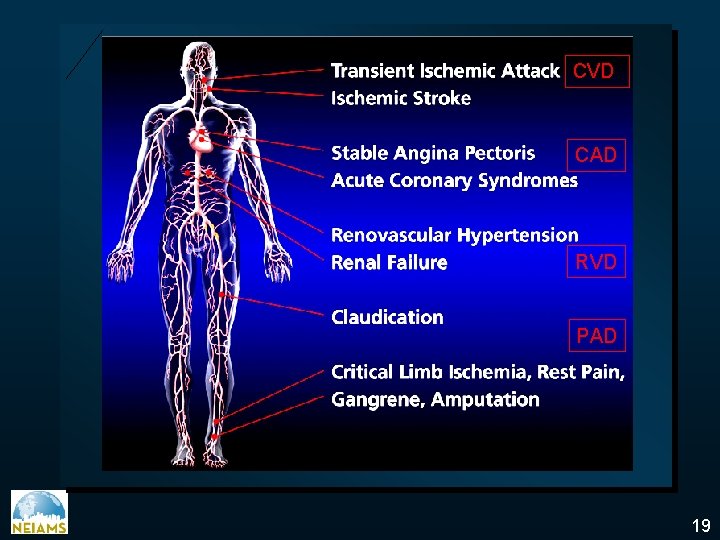
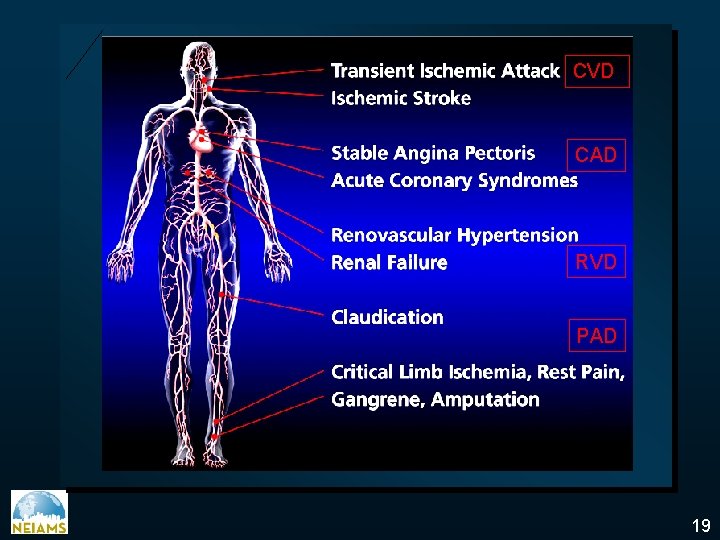
CVD CAD RVD PAD 19
Peripheral Arterial Disease: Clinical Diagnosis • Must have a high index of suspicion • Must perform a thorough physicial examination • Determine the global atherosclerotic burden • Utilize the vascular diagnostic laboratory • Magnetic resonance angiography is rapidly replacing invasive testing • Reserve arteriography for cases requiring intervention TCT 2005 20
Vascular Review of Systems • Any exertional limitation of the lower extremity muscles or any history of walking impairment (fatigue, numbness, aching, or pain • Any poorly healing or non healing of the legs or feet • Any pain at rest localized at the lower leg or foot and its association with the upright or recumbent positions • Postprandial abdominal pain that reproducibly is provoked by eating and is associated with weight loss • Family history of a first-degree relative with Abdominal Aortic Aneurysm ACC/AHA Guidelines 21
Vascular Physical Examination • Measurement of blood pressure in both arm and notation of any interarm assymetry • Palpation of the carotid pulses and notation of the carotid upstroke and amplitude and presence of bruits • Auscultation of the abdomen and flank for bruits • Palpation of the pulses at the brachial, radial ulnar, femoral, popliteal, dorsalis pedis, and posterior tibial sites. Performance of Allen’s test when knowledge of hand perfusion is needed • Auscultation of both femoral ateries for the presence of bruits • Pulse intensity should be recorded numerically: 0, absent; 1, diminished; 2, normal; 3, bounding • Additional findings: distal hair loss, trophic sin changes hypertrophic nails ACC/AHA Guidelines 22
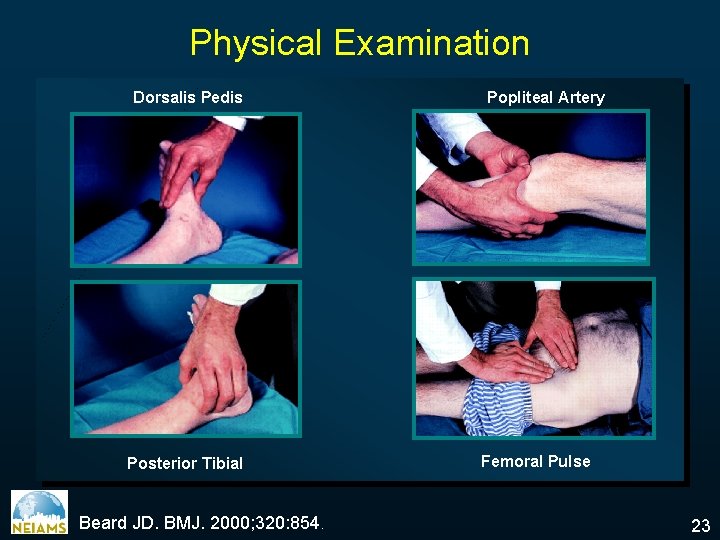
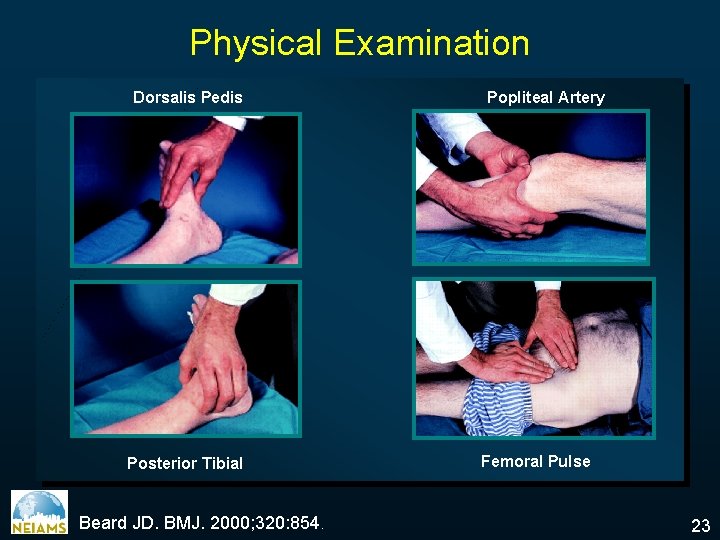
Physical Examination Dorsalis Pedis Posterior Tibial Beard JD. BMJ. 2000; 320: 854. Popliteal Artery Femoral Pulse 23
Signs of PAD • Decreased or absent pulses • Bruits • Muscle atrophy • Pallor of feet with elevation • Dependent rubor • Signs of chronic ischemia: Hair loss, thickened nails, smooth & shiny skin, coolness, pallor or cyanosis 24
Peripheral Arterial Disease Etiology Epidemiology Physical examination ü Clinical Manifestations Diagnosis Indications Treatment Options Prognosis 25
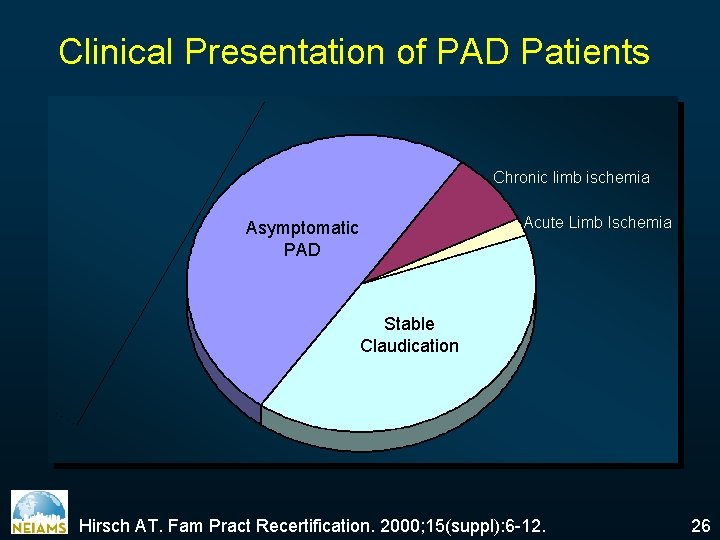
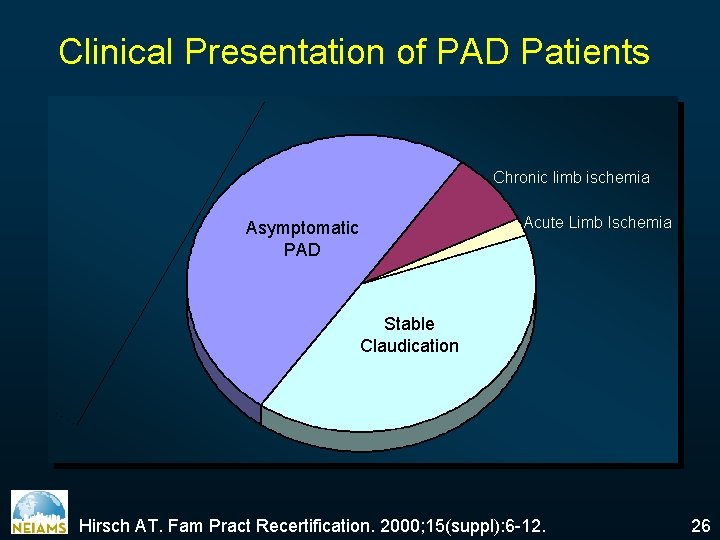
Clinical Presentation of PAD Patients Chronic limb ischemia Acute Limb Ischemia Asymptomatic PAD Stable Claudication Hirsch AT. Fam Pract Recertification. 2000; 15(suppl): 6 -12. 26
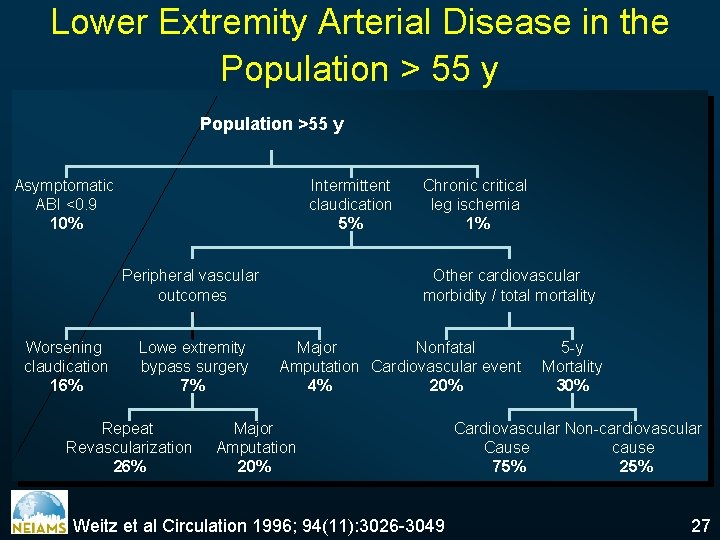
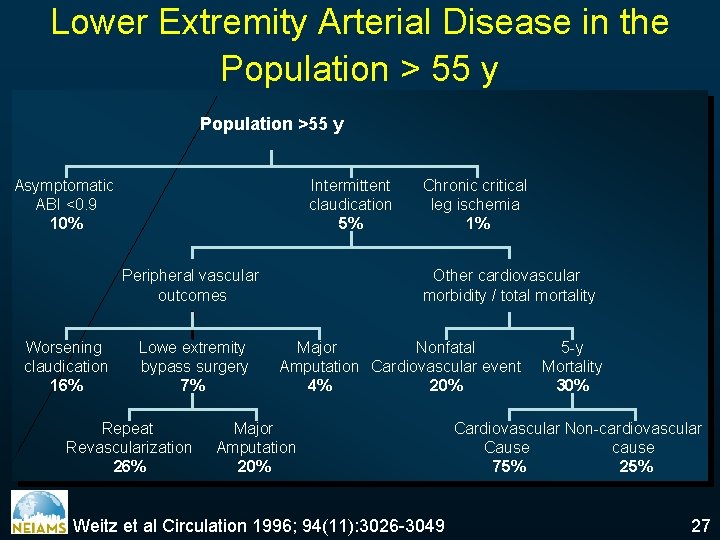
Lower Extremity Arterial Disease in the Population > 55 y Population >55 y Asymptomatic ABI <0. 9 10% Intermittent claudication 5% Peripheral vascular outcomes Worsening claudication 16% Lowe extremity bypass surgery 7% Repeat Revascularization 26% Chronic critical leg ischemia 1% Other cardiovascular morbidity / total mortality Major Nonfatal Amputation Cardiovascular event 4% 20% Major Amputation 20% Weitz et al Circulation 1996; 94(11): 3026 -3049 5 -y Mortality 30% Cardiovascular Non-cardiovascular Cause cause 75% 27
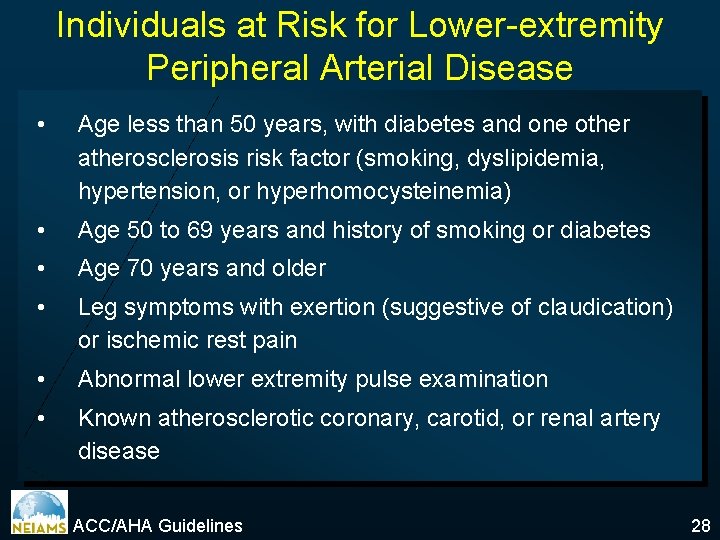
Individuals at Risk for Lower-extremity Peripheral Arterial Disease • Age less than 50 years, with diabetes and one other atherosclerosis risk factor (smoking, dyslipidemia, hypertension, or hyperhomocysteinemia) • Age 50 to 69 years and history of smoking or diabetes • Age 70 years and older • Leg symptoms with exertion (suggestive of claudication) or ischemic rest pain • Abnormal lower extremity pulse examination • Known atherosclerotic coronary, carotid, or renal artery disease ACC/AHA Guidelines 28
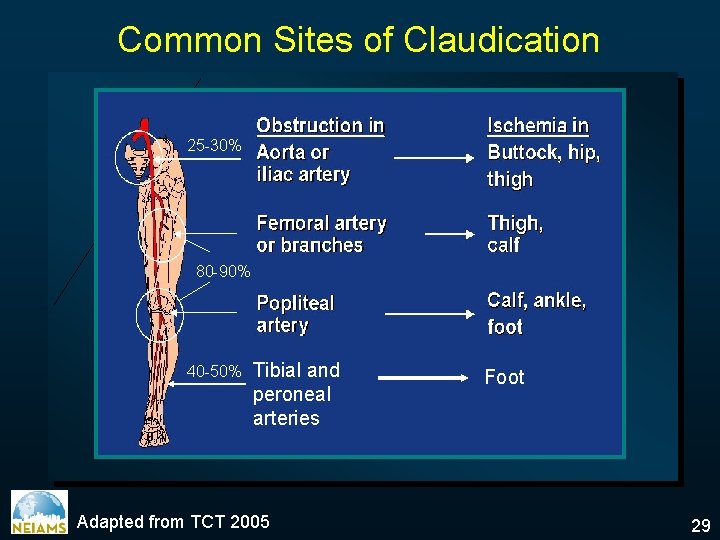
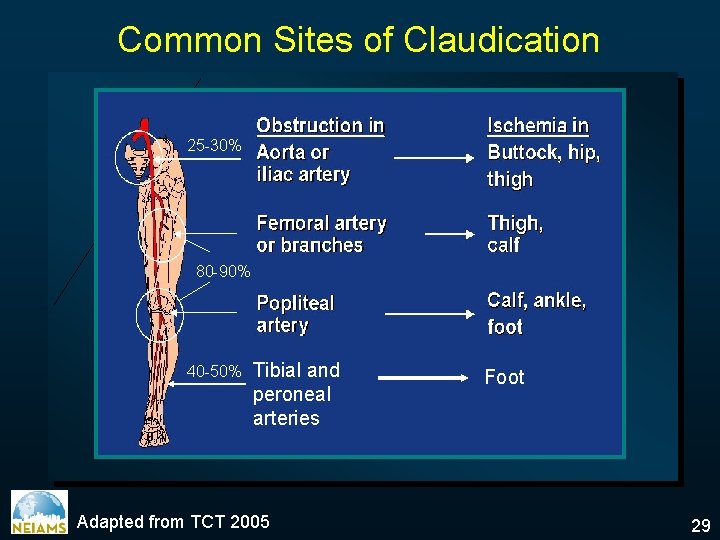
Common Sites of Claudication 25 -30% 80 -90% 40 -50% Tibial and peroneal arteries Adapted from TCT 2005 Foot 29
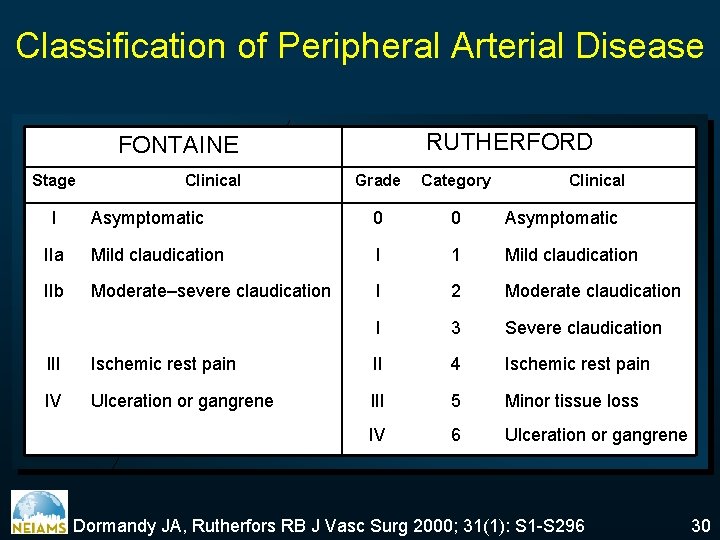
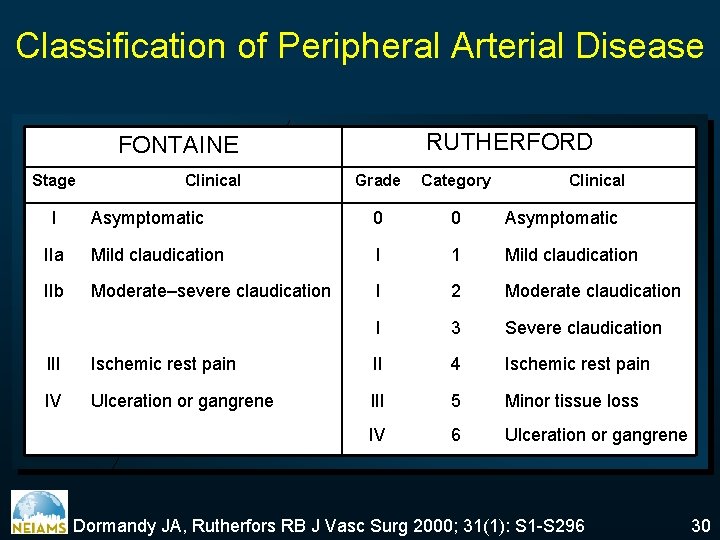
Classification of Peripheral Arterial Disease RUTHERFORD FONTAINE Stage Grade Category Asymptomatic 0 0 Asymptomatic IIa Mild claudication I 1 Mild claudication IIb Moderate–severe claudication I 2 Moderate claudication I 3 Severe claudication I Clinical III Ischemic rest pain II 4 Ischemic rest pain IV Ulceration or gangrene III 5 Minor tissue loss IV 6 Ulceration or gangrene Dormandy JA, Rutherfors RB J Vasc Surg 2000; 31(1): S 1 -S 296 30
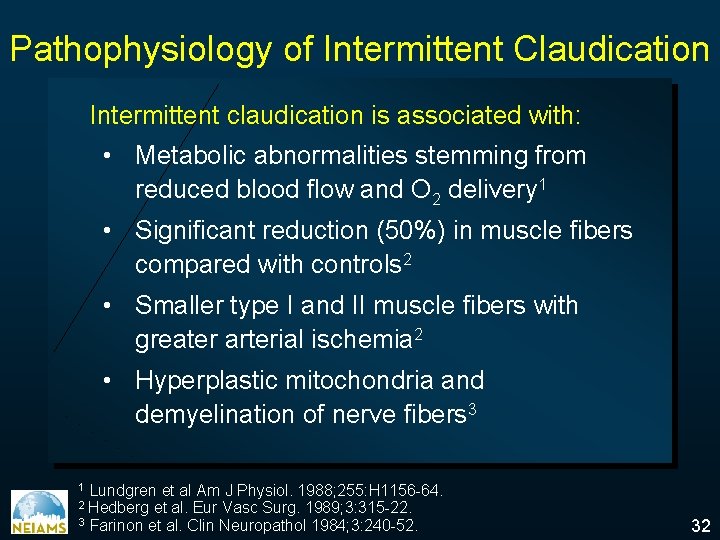
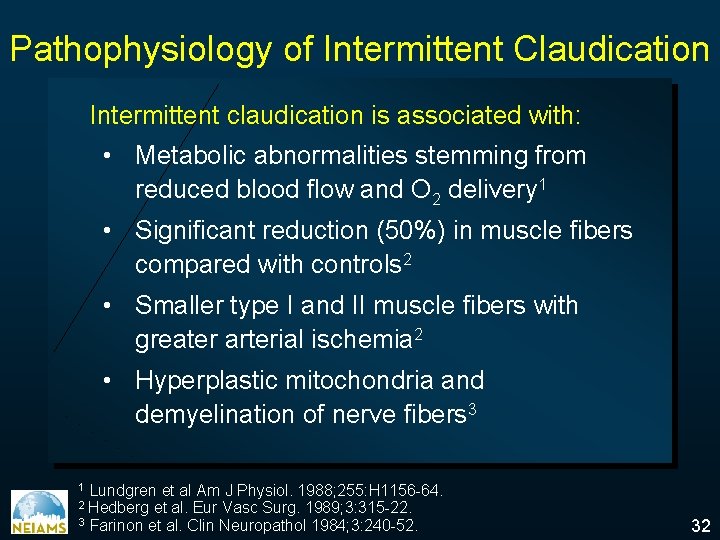
Pathophysiology of Intermittent Claudication Intermittent claudication is associated with: • Metabolic abnormalities stemming from reduced blood flow and O 2 delivery 1 • Significant reduction (50%) in muscle fibers compared with controls 2 • Smaller type I and II muscle fibers with greater arterial ischemia 2 • Hyperplastic mitochondria and demyelination of nerve fibers 3 Lundgren et al Am J Physiol. 1988; 255: H 1156 -64. et al. Eur Vasc Surg. 1989; 3: 315 -22. 3 Farinon et al. Clin Neuropathol 1984; 3: 240 -52. 1 2 Hedberg 32
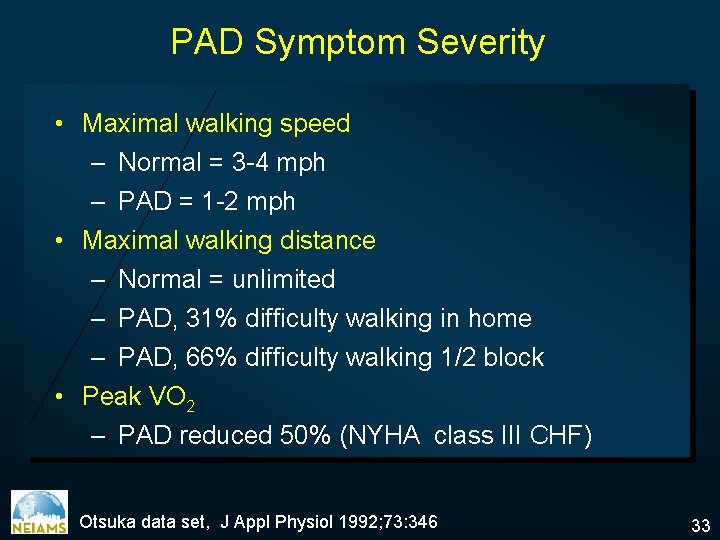
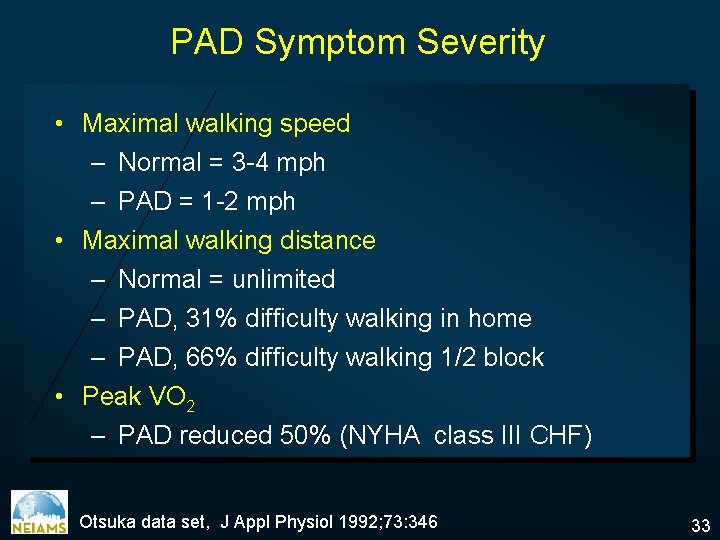
PAD Symptom Severity • Maximal walking speed – Normal = 3 -4 mph – PAD = 1 -2 mph • Maximal walking distance – Normal = unlimited – PAD, 31% difficulty walking in home – PAD, 66% difficulty walking 1/2 block • Peak VO 2 – PAD reduced 50% (NYHA class III CHF) Otsuka data set, J Appl Physiol 1992; 73: 346 33
Peripheral Arterial Disease Etiology Epidemiology Physical examination Clinical Manifestations ü Diagnosis Indications Treatment Options Prognosis 34
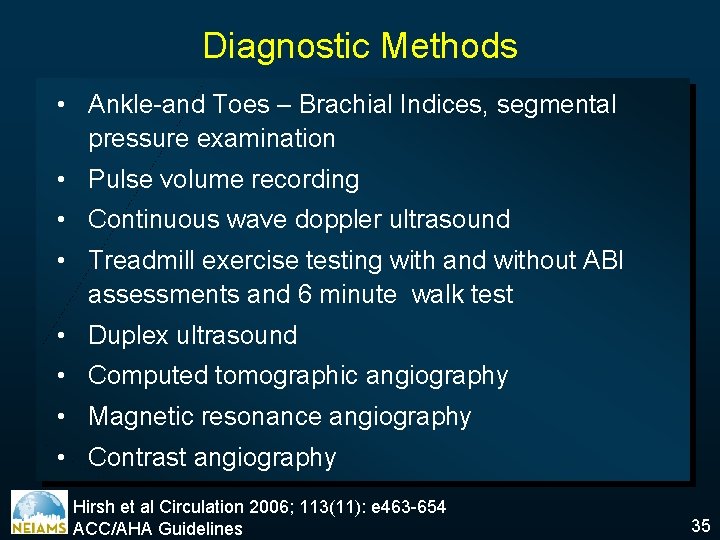
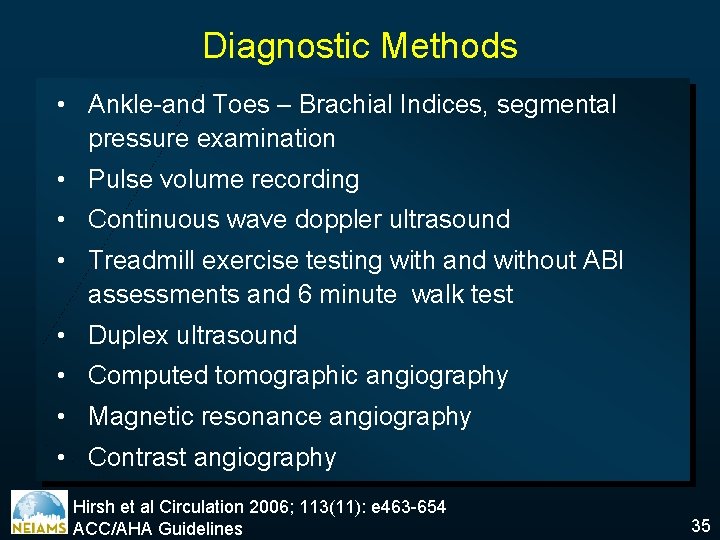
Diagnostic Methods • Ankle-and Toes – Brachial Indices, segmental pressure examination • Pulse volume recording • Continuous wave doppler ultrasound • Treadmill exercise testing with and without ABI assessments and 6 minute walk test • Duplex ultrasound • Computed tomographic angiography • Magnetic resonance angiography • Contrast angiography Hirsh et al Circulation 2006; 113(11): e 463 -654 ACC/AHA Guidelines 35
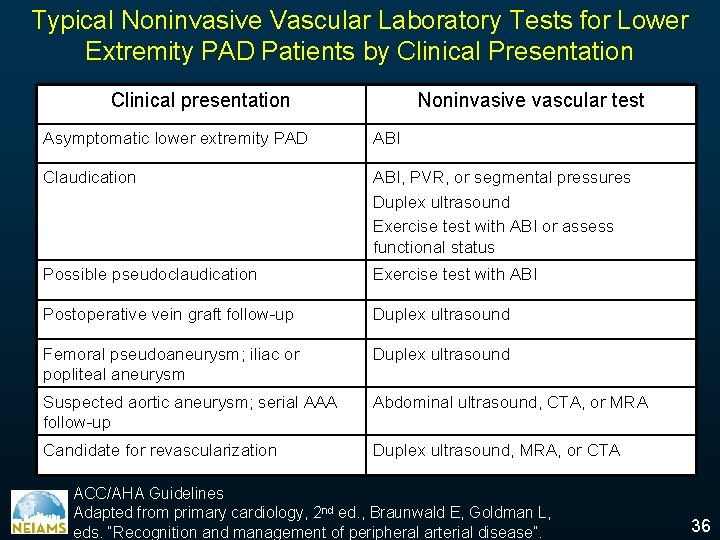
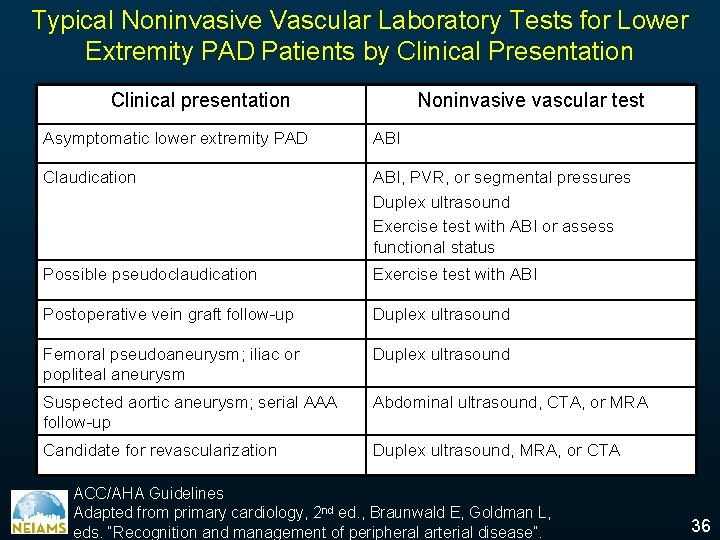
Typical Noninvasive Vascular Laboratory Tests for Lower Extremity PAD Patients by Clinical Presentation Clinical presentation Noninvasive vascular test Asymptomatic lower extremity PAD ABI Claudication ABI, PVR, or segmental pressures Duplex ultrasound Exercise test with ABI or assess functional status Possible pseudoclaudication Exercise test with ABI Postoperative vein graft follow-up Duplex ultrasound Femoral pseudoaneurysm; iliac or popliteal aneurysm Duplex ultrasound Suspected aortic aneurysm; serial AAA follow-up Abdominal ultrasound, CTA, or MRA Candidate for revascularization Duplex ultrasound, MRA, or CTA ACC/AHA Guidelines Adapted from primary cardiology, 2 nd ed. , Braunwald E, Goldman L, eds. “Recognition and management of peripheral arterial disease”. 36
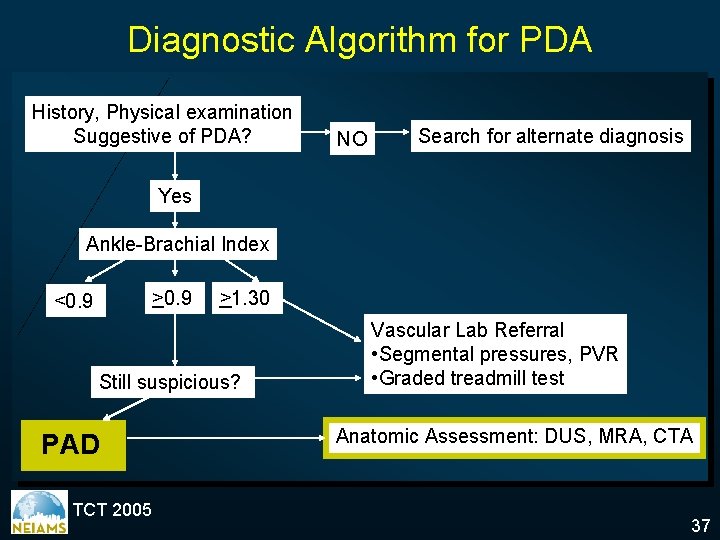
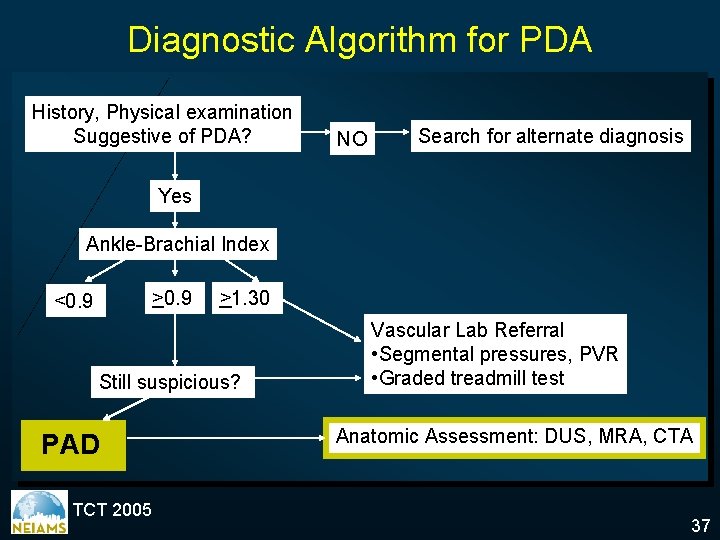
Diagnostic Algorithm for PDA History, Physical examination Suggestive of PDA? NO Search for alternate diagnosis Yes Ankle-Brachial Index >0. 9 <0. 9 >1. 30 Still suspicious? PAD TCT 2005 Vascular Lab Referral • Segmental pressures, PVR • Graded treadmill test Anatomic Assessment: DUS, MRA, CTA 37
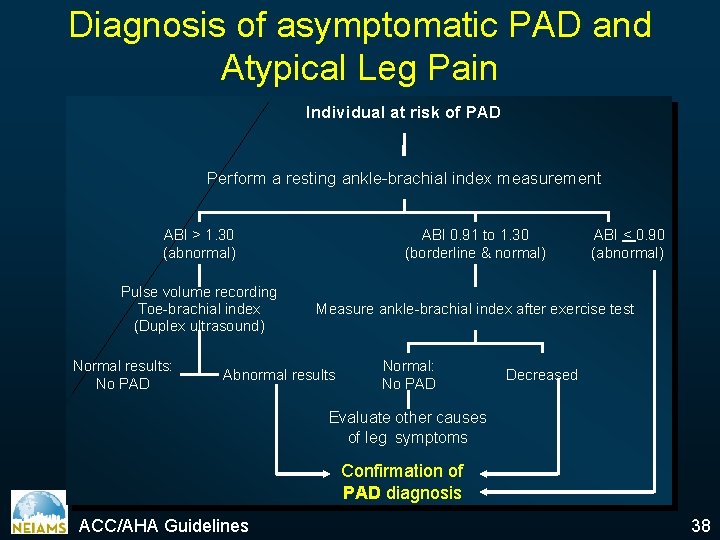
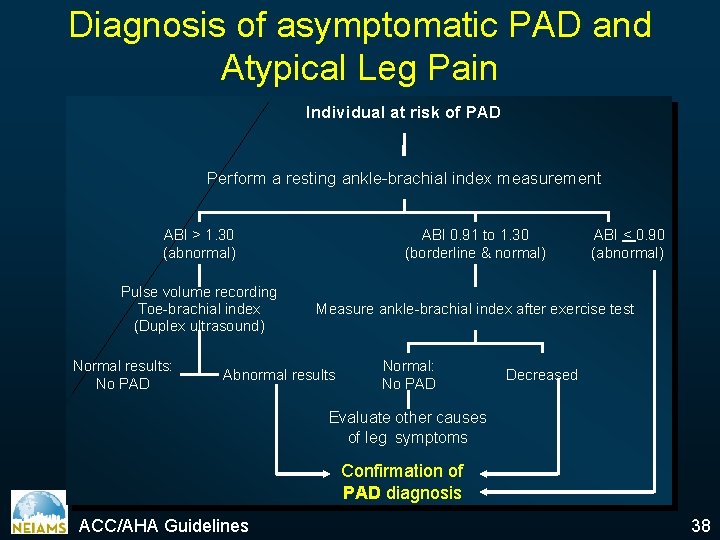
Diagnosis of asymptomatic PAD and Atypical Leg Pain Individual at risk of PAD Perform a resting ankle-brachial index measurement ABI > 1. 30 (abnormal) ABI 0. 91 to 1. 30 (borderline & normal) Pulse volume recording Toe-brachial index (Duplex ultrasound) Measure ankle-brachial index after exercise test Normal results: No PAD Abnormal results Normal: No PAD ABI < 0. 90 (abnormal) Decreased Evaluate other causes of leg symptoms Confirmation of PAD diagnosis ACC/AHA Guidelines 38
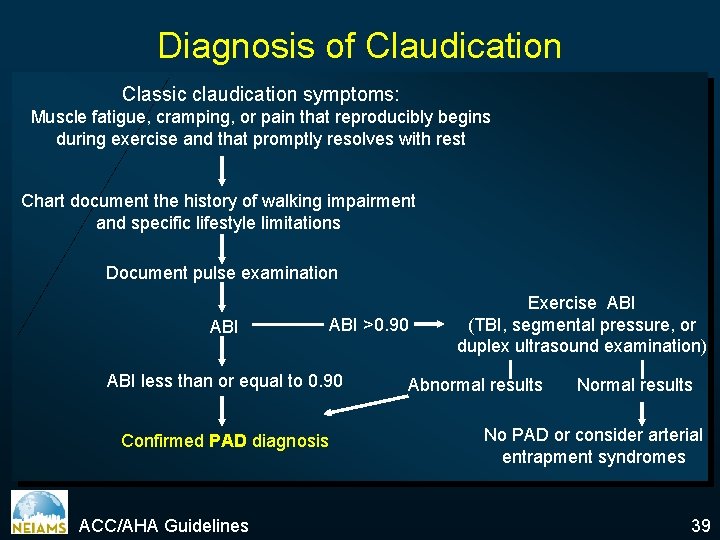
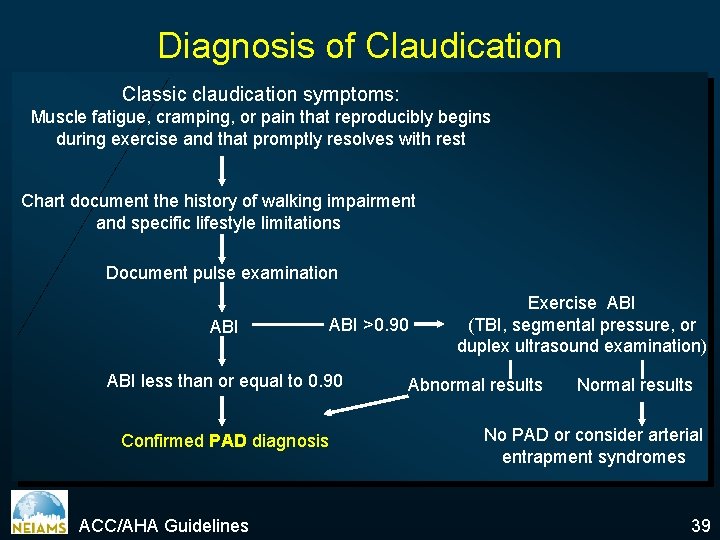
Diagnosis of Claudication Classic claudication symptoms: Muscle fatigue, cramping, or pain that reproducibly begins during exercise and that promptly resolves with rest Chart document the history of walking impairment and specific lifestyle limitations Document pulse examination ABI >0. 90 ABI less than or equal to 0. 90 Confirmed PAD diagnosis ACC/AHA Guidelines Exercise ABI (TBI, segmental pressure, or duplex ultrasound examination) Abnormal results No PAD or consider arterial entrapment syndromes 39
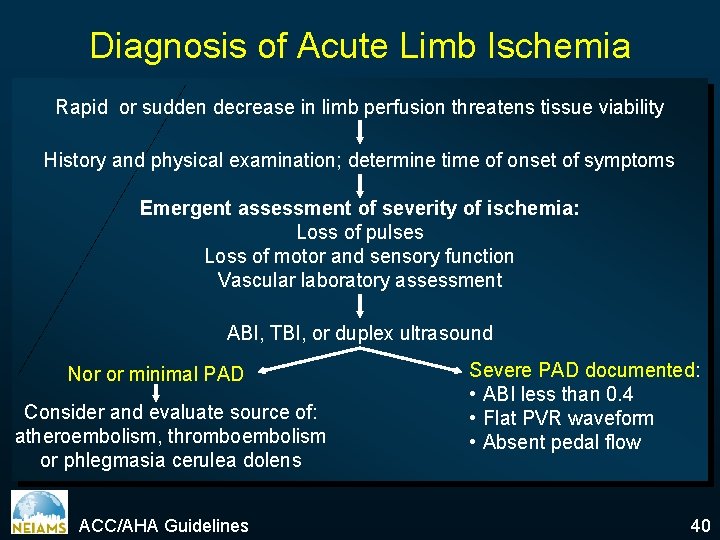
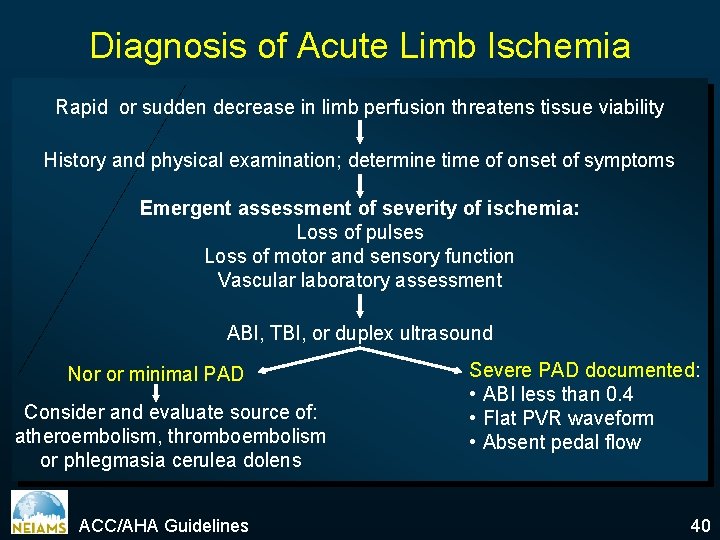
Diagnosis of Acute Limb Ischemia Rapid or sudden decrease in limb perfusion threatens tissue viability History and physical examination; determine time of onset of symptoms Emergent assessment of severity of ischemia: Loss of pulses Loss of motor and sensory function Vascular laboratory assessment ABI, TBI, or duplex ultrasound Nor or minimal PAD Consider and evaluate source of: atheroembolism, thromboembolism or phlegmasia cerulea dolens ACC/AHA Guidelines Severe PAD documented: • ABI less than 0. 4 • Flat PVR waveform • Absent pedal flow 40
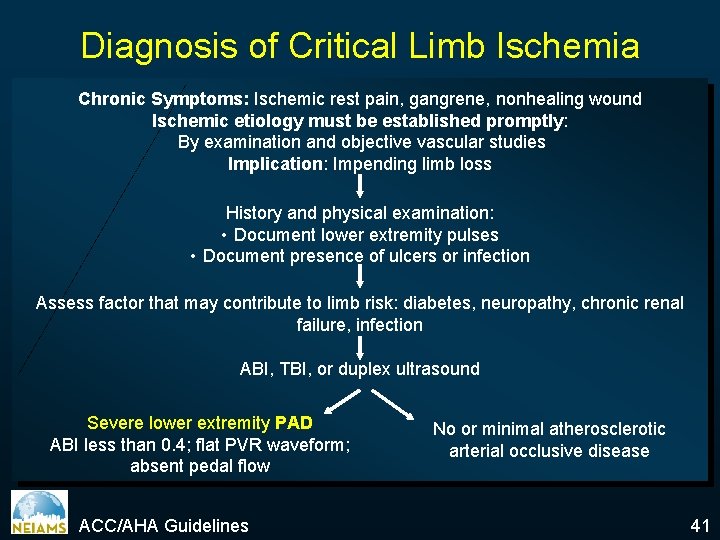
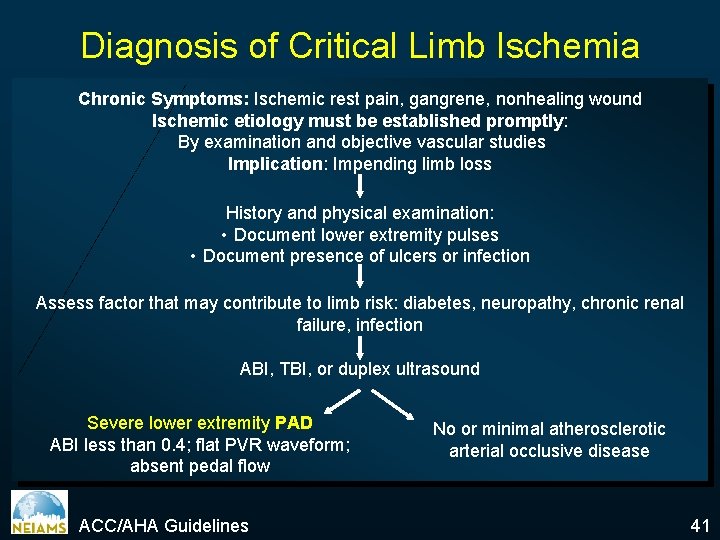
Diagnosis of Critical Limb Ischemia Chronic Symptoms: Ischemic rest pain, gangrene, nonhealing wound Ischemic etiology must be established promptly: By examination and objective vascular studies Implication: Impending limb loss History and physical examination: • Document lower extremity pulses • Document presence of ulcers or infection Assess factor that may contribute to limb risk: diabetes, neuropathy, chronic renal failure, infection ABI, TBI, or duplex ultrasound Severe lower extremity PAD ABI less than 0. 4; flat PVR waveform; absent pedal flow ACC/AHA Guidelines No or minimal atherosclerotic arterial occlusive disease 41
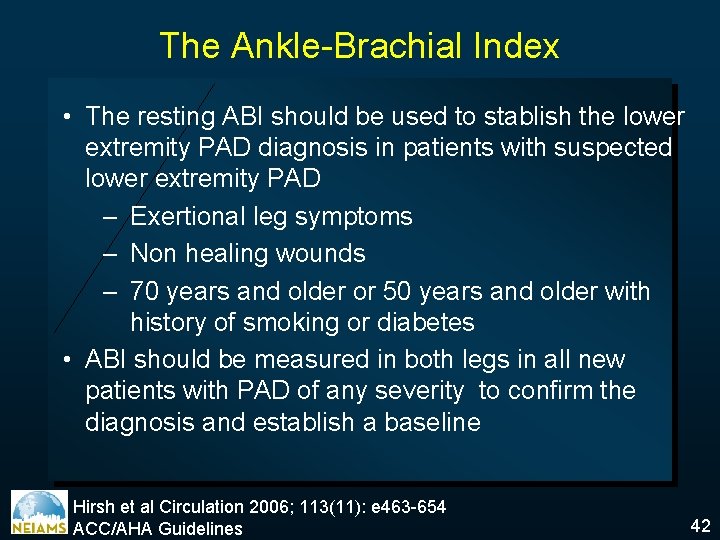
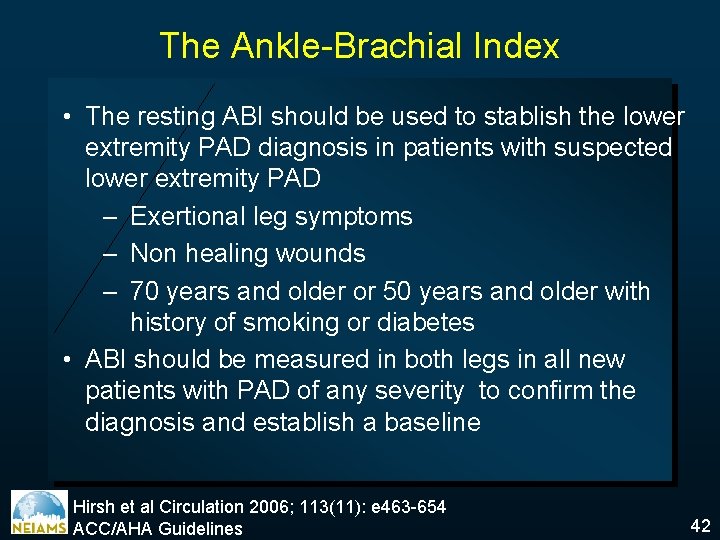
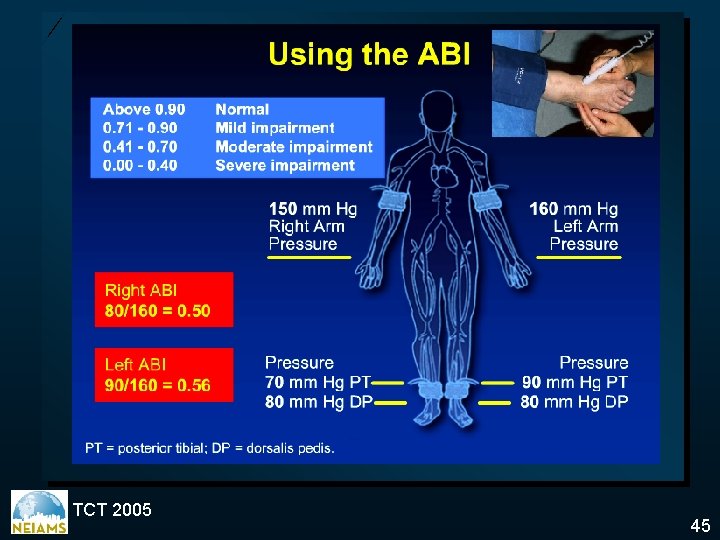
The Ankle-Brachial Index • The resting ABI should be used to stablish the lower extremity PAD diagnosis in patients with suspected lower extremity PAD – Exertional leg symptoms – Non healing wounds – 70 years and older or 50 years and older with history of smoking or diabetes • ABI should be measured in both legs in all new patients with PAD of any severity to confirm the diagnosis and establish a baseline Hirsh et al Circulation 2006; 113(11): e 463 -654 ACC/AHA Guidelines 42
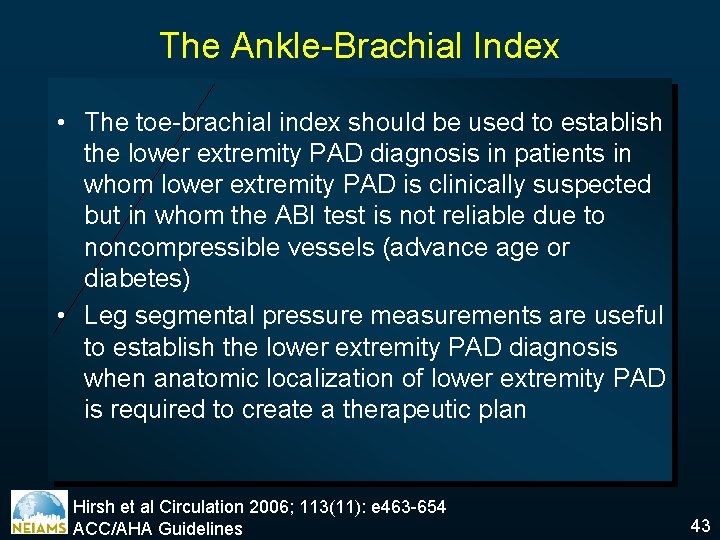
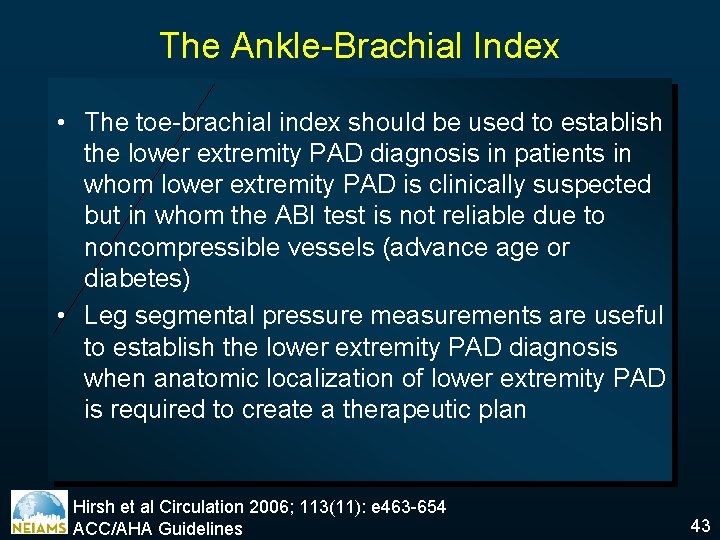
The Ankle-Brachial Index • The toe-brachial index should be used to establish the lower extremity PAD diagnosis in patients in whom lower extremity PAD is clinically suspected but in whom the ABI test is not reliable due to noncompressible vessels (advance age or diabetes) • Leg segmental pressure measurements are useful to establish the lower extremity PAD diagnosis when anatomic localization of lower extremity PAD is required to create a therapeutic plan Hirsh et al Circulation 2006; 113(11): e 463 -654 ACC/AHA Guidelines 43
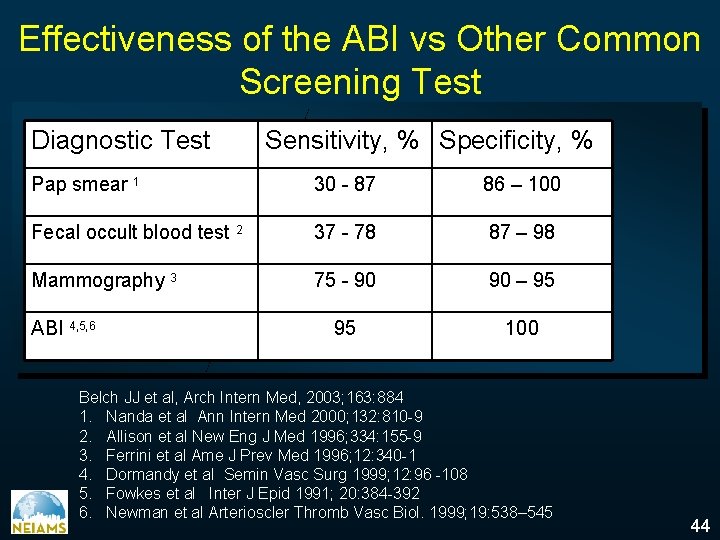
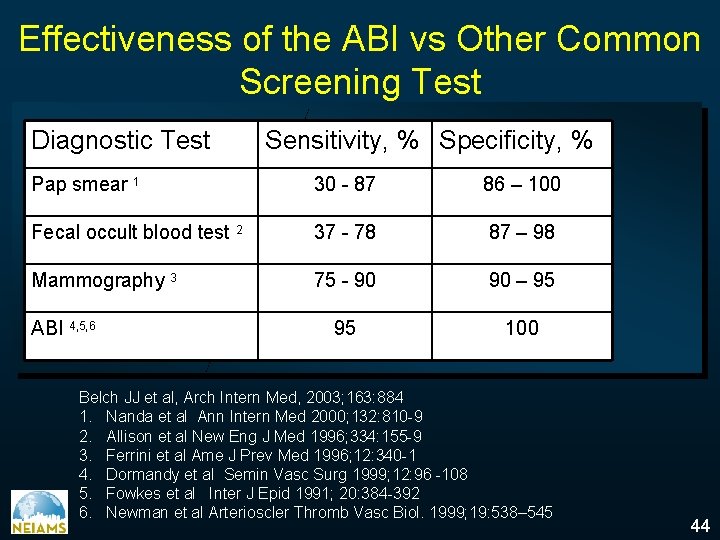
Effectiveness of the ABI vs Other Common Screening Test Diagnostic Test Sensitivity, % Specificity, % Pap smear 1 30 - 87 86 – 100 Fecal occult blood test 2 37 - 78 87 – 98 Mammography 3 75 - 90 90 – 95 95 100 ABI 4, 5, 6 Belch JJ et al, Arch Intern Med, 2003; 163: 884 1. Nanda et al Ann Intern Med 2000; 132: 810 -9 2. Allison et al New Eng J Med 1996; 334: 155 -9 3. Ferrini et al Ame J Prev Med 1996; 12: 340 -1 4. Dormandy et al Semin Vasc Surg 1999; 12: 96 -108 5. Fowkes et al Inter J Epid 1991; 20: 384 -392 6. Newman et al Arterioscler Thromb Vasc Biol. 1999; 19: 538– 545 44
TCT 2005 45
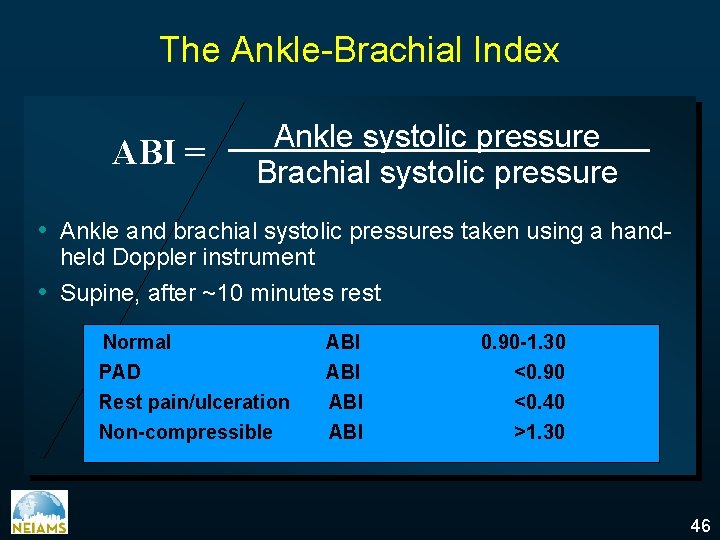
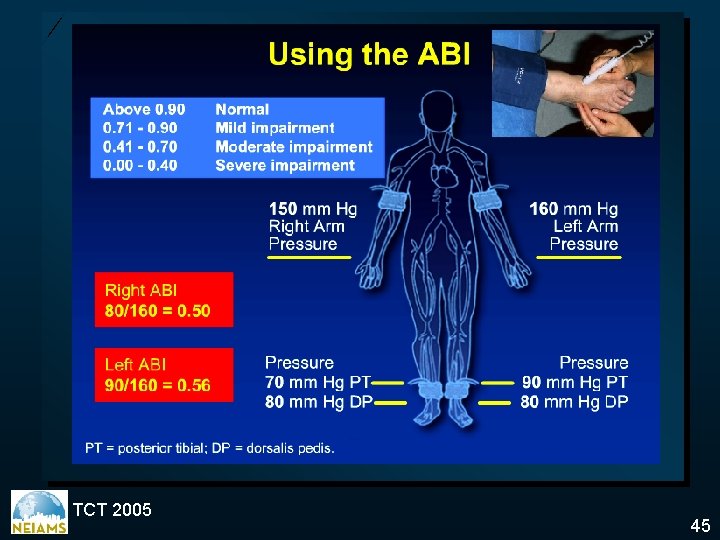
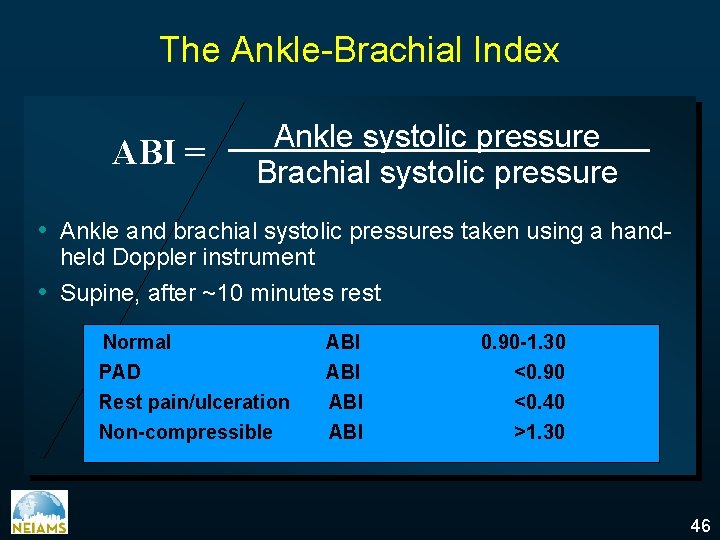
The Ankle-Brachial Index ABI = Ankle systolic pressure Brachial systolic pressure • Ankle and brachial systolic pressures taken using a handheld Doppler instrument • Supine, after ~10 minutes rest Normal ABI 0. 90 -1. 30 PAD Rest pain/ulceration Non-compressible ABI ABI <0. 90 <0. 40 >1. 30 46
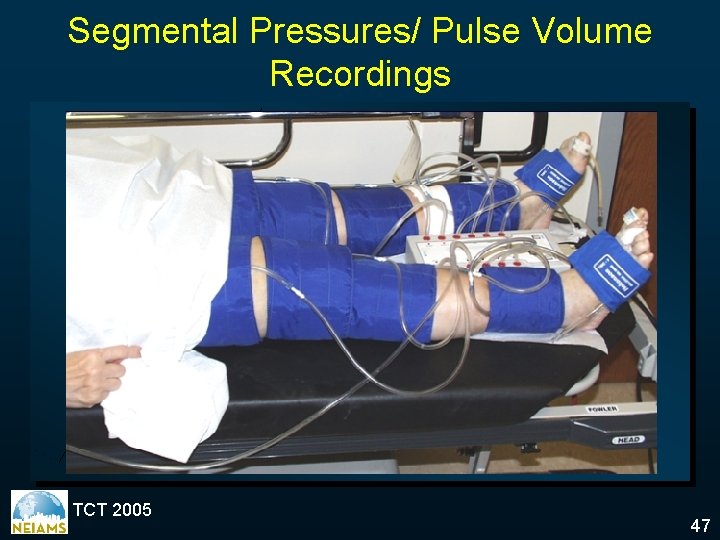
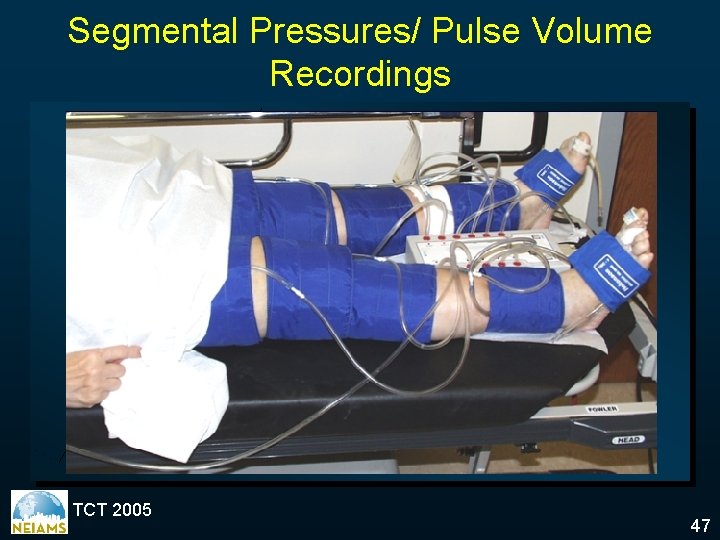
Segmental Pressures/ Pulse Volume Recordings TCT 2005 47
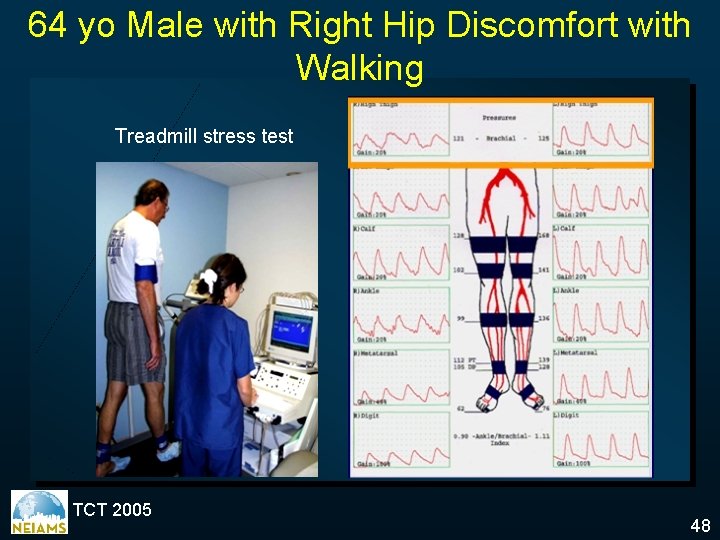
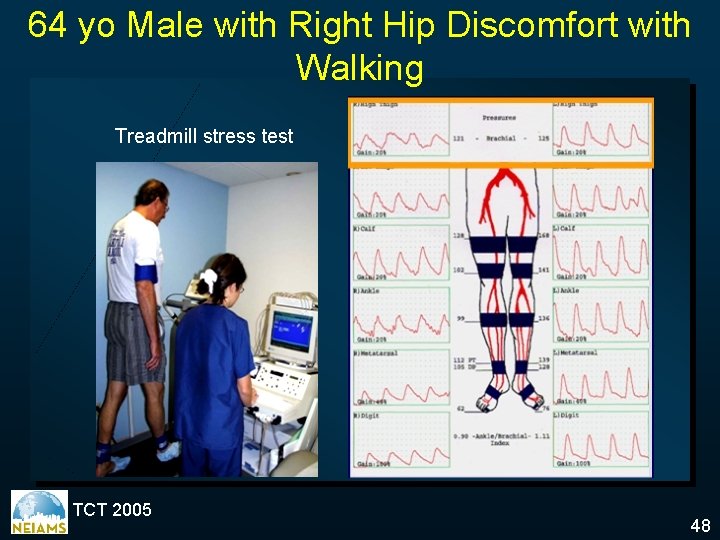
64 yo Male with Right Hip Discomfort with Walking Treadmill stress test TCT 2005 48
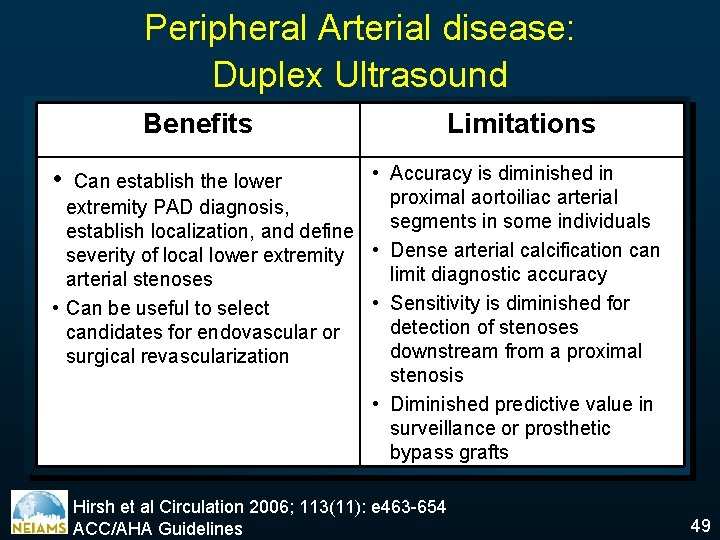
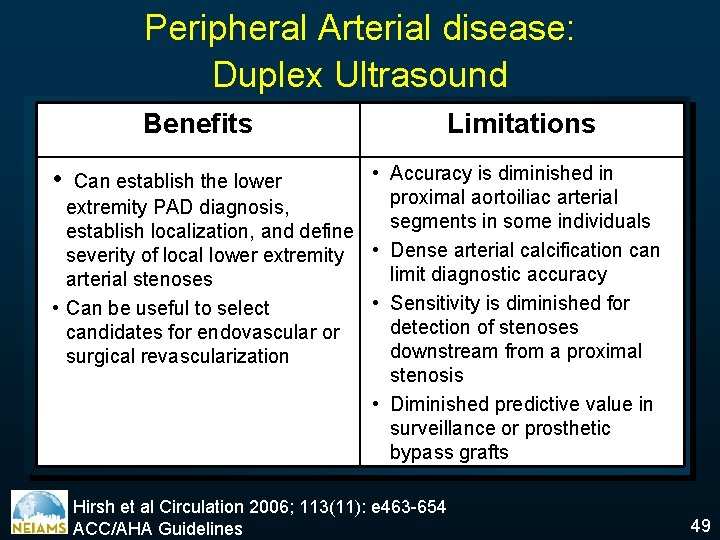
Peripheral Arterial disease: Duplex Ultrasound Benefits Limitations • Accuracy is diminished in Can establish the lower proximal aortoiliac arterial extremity PAD diagnosis, segments in some individuals establish localization, and define severity of local lower extremity • Dense arterial calcification can limit diagnostic accuracy arterial stenoses • Sensitivity is diminished for • Can be useful to select detection of stenoses candidates for endovascular or downstream from a proximal surgical revascularization stenosis • Diminished predictive value in surveillance or prosthetic bypass grafts • Hirsh et al Circulation 2006; 113(11): e 463 -654 ACC/AHA Guidelines 49
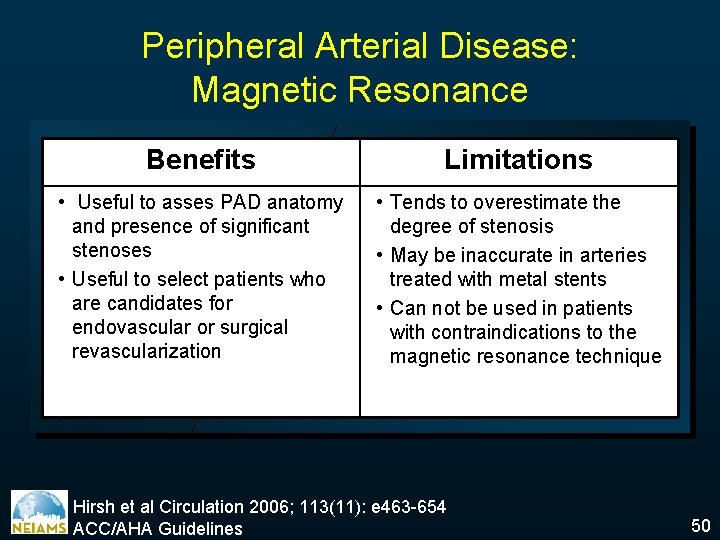
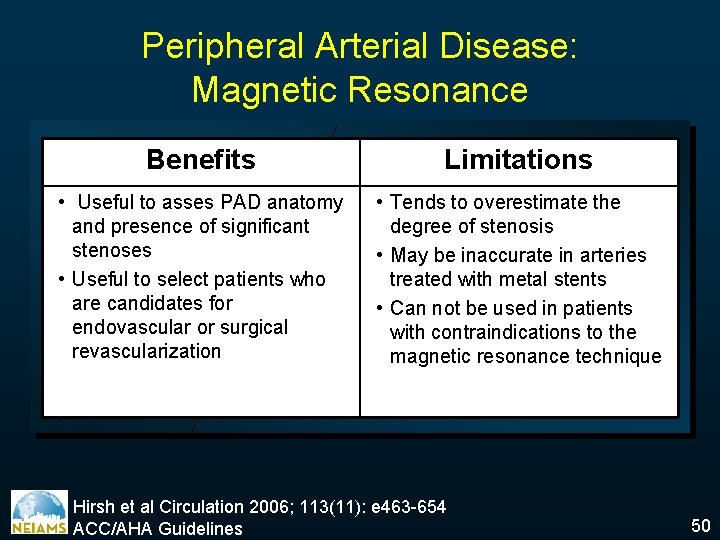
Peripheral Arterial Disease: Magnetic Resonance Benefits Limitations • Useful to asses PAD anatomy and presence of significant stenoses • Useful to select patients who are candidates for endovascular or surgical revascularization • Tends to overestimate the degree of stenosis • May be inaccurate in arteries treated with metal stents • Can not be used in patients with contraindications to the magnetic resonance technique Hirsh et al Circulation 2006; 113(11): e 463 -654 ACC/AHA Guidelines 50
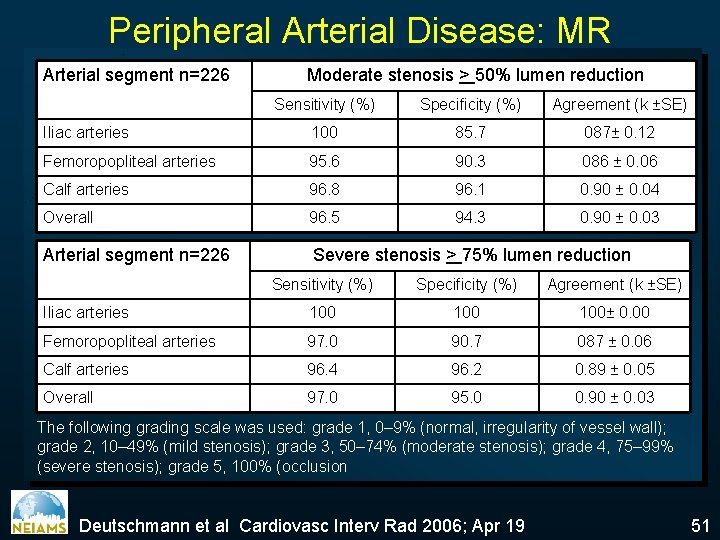
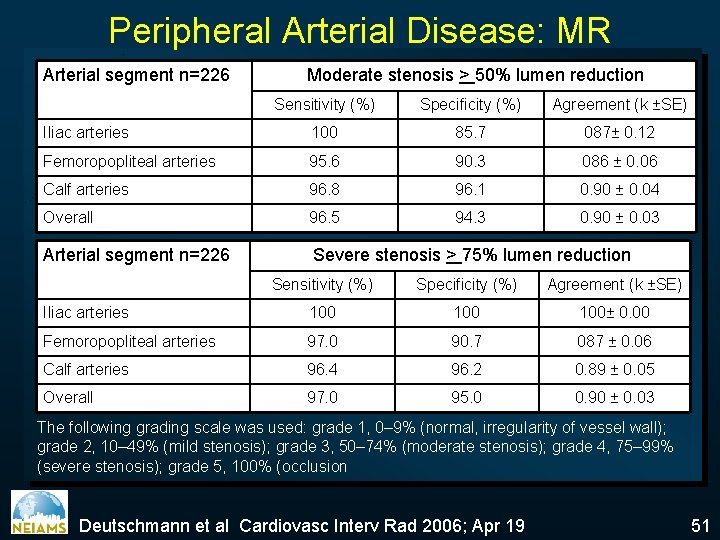
Peripheral Arterial Disease: MR Arterial segment n=226 Moderate stenosis > 50% lumen reduction Sensitivity (%) Specificity (%) Agreement (k ±SE) Iliac arteries 100 85. 7 087± 0. 12 Femoropopliteal arteries 95. 6 90. 3 086 ± 0. 06 Calf arteries 96. 8 96. 1 0. 90 ± 0. 04 Overall 96. 5 94. 3 0. 90 ± 0. 03 Arterial segment n=226 Severe stenosis > 75% lumen reduction Sensitivity (%) Specificity (%) Agreement (k ±SE) Iliac arteries 100 100± 0. 00 Femoropopliteal arteries 97. 0 90. 7 087 ± 0. 06 Calf arteries 96. 4 96. 2 0. 89 ± 0. 05 Overall 97. 0 95. 0 0. 90 ± 0. 03 The following grading scale was used: grade 1, 0– 9% (normal, irregularity of vessel wall); grade 2, 10– 49% (mild stenosis); grade 3, 50– 74% (moderate stenosis); grade 4, 75– 99% (severe stenosis); grade 5, 100% (occlusion Deutschmann et al Cardiovasc Interv Rad 2006; Apr 19 51
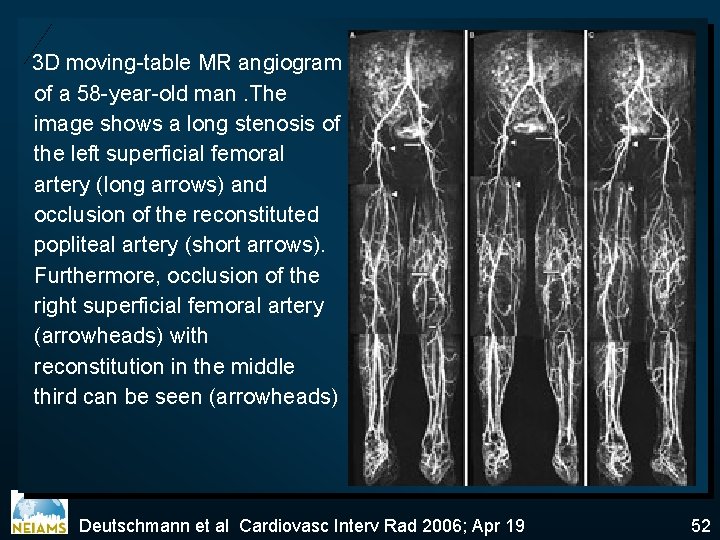
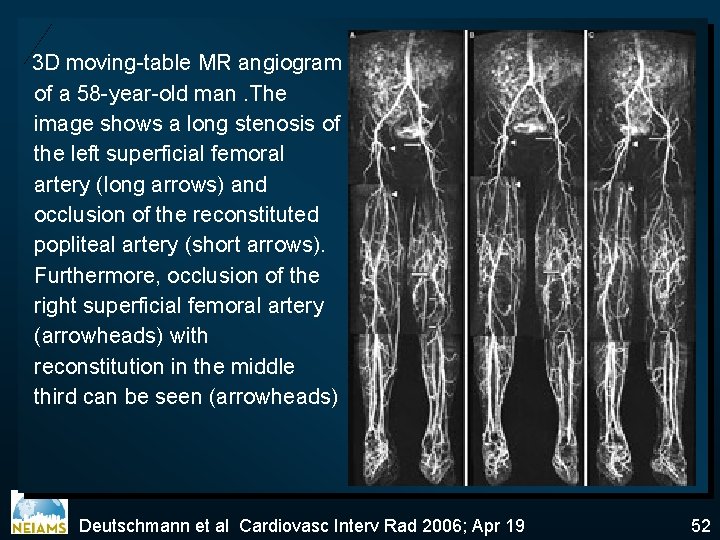
3 D moving-table MR angiogram of a 58 -year-old man. The image shows a long stenosis of the left superficial femoral artery (long arrows) and occlusion of the reconstituted popliteal artery (short arrows). Furthermore, occlusion of the right superficial femoral artery (arrowheads) with reconstitution in the middle third can be seen (arrowheads) Deutschmann et al Cardiovasc Interv Rad 2006; Apr 19 52
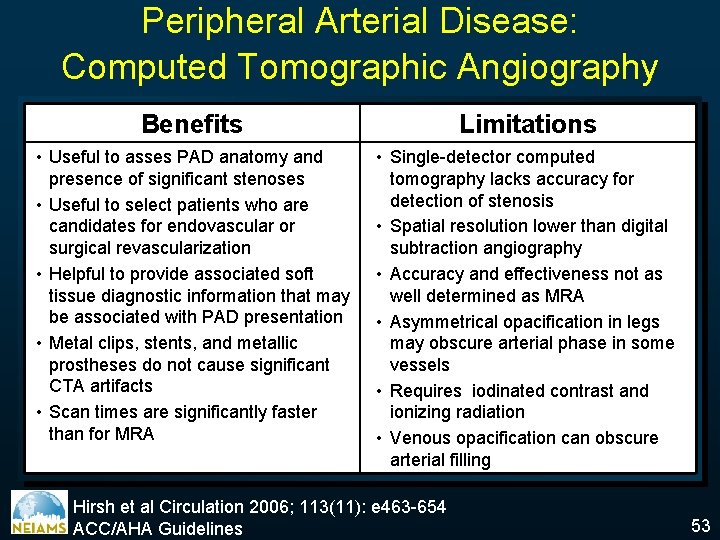
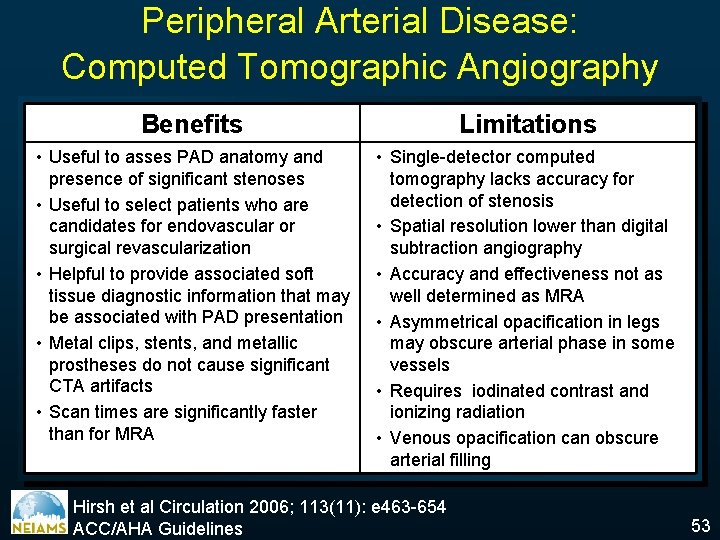
Peripheral Arterial Disease: Computed Tomographic Angiography Benefits Limitations • Useful to asses PAD anatomy and presence of significant stenoses • Useful to select patients who are candidates for endovascular or surgical revascularization • Helpful to provide associated soft tissue diagnostic information that may be associated with PAD presentation • Metal clips, stents, and metallic prostheses do not cause significant CTA artifacts • Scan times are significantly faster than for MRA • Single-detector computed tomography lacks accuracy for detection of stenosis • Spatial resolution lower than digital subtraction angiography • Accuracy and effectiveness not as well determined as MRA • Asymmetrical opacification in legs may obscure arterial phase in some vessels • Requires iodinated contrast and ionizing radiation • Venous opacification can obscure arterial filling Hirsh et al Circulation 2006; 113(11): e 463 -654 ACC/AHA Guidelines 53
Peripheral Arterial Disease Etiology Epidemiology Physical examination Clinical Manifestations Diagnosis ü Indications Treatment Options Prognosis 54
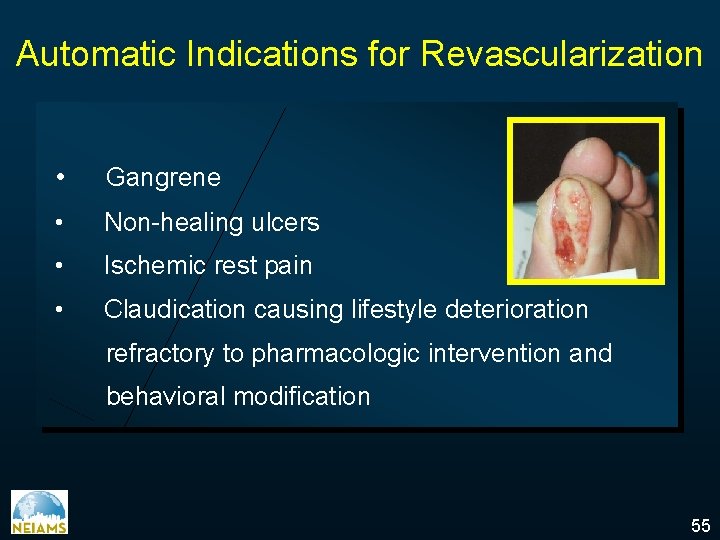
Automatic Indications for Revascularization • Gangrene • Non-healing ulcers • Ischemic rest pain • Claudication causing lifestyle deterioration refractory to pharmacologic intervention and behavioral modification 55
Peripheral Arterial Disease Etiology Epidemiology Physical examination Clinical Manifestations Diagnosis Indications ü Treatment Options Prognosis 56
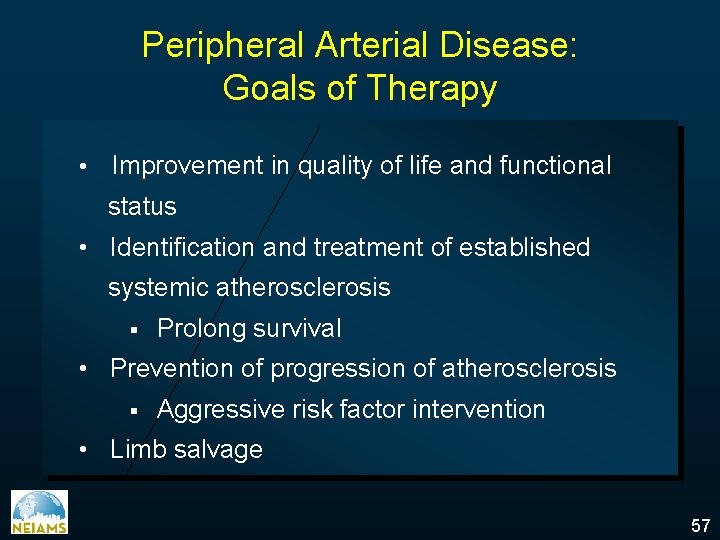
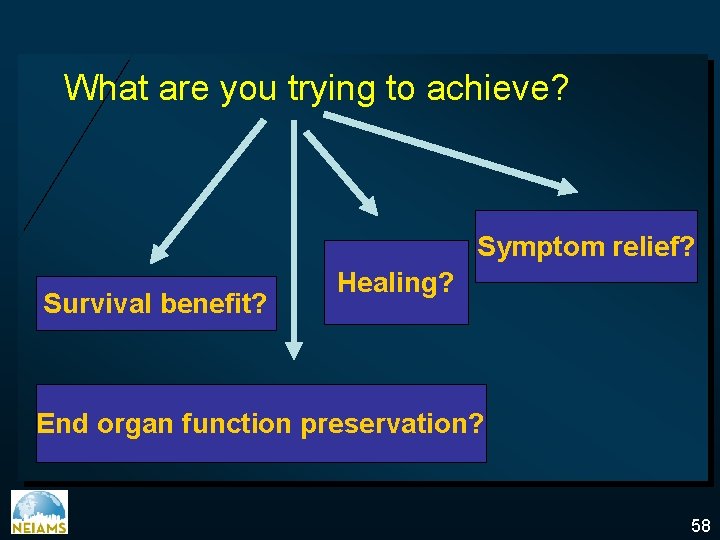
Peripheral Arterial Disease: Goals of Therapy • Improvement in quality of life and functional status • Identification and treatment of established systemic atherosclerosis § Prolong survival • Prevention of progression of atherosclerosis § Aggressive risk factor intervention • Limb salvage 57
What are you trying to achieve? Symptom relief? Survival benefit? Healing? End organ function preservation? 58
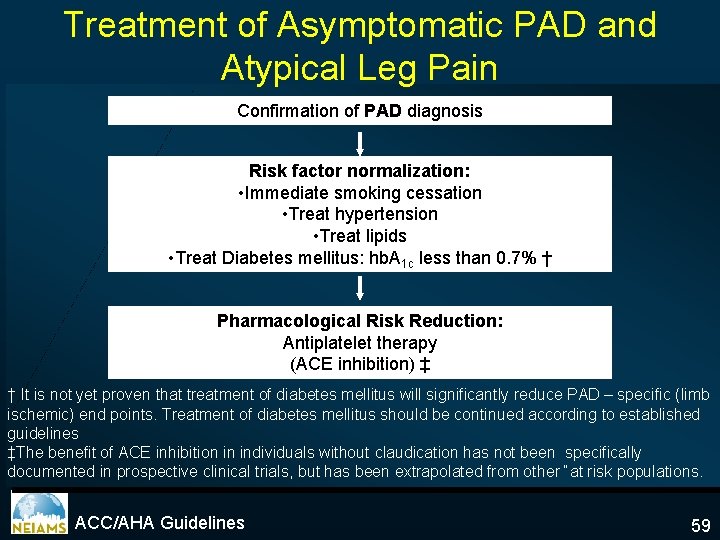
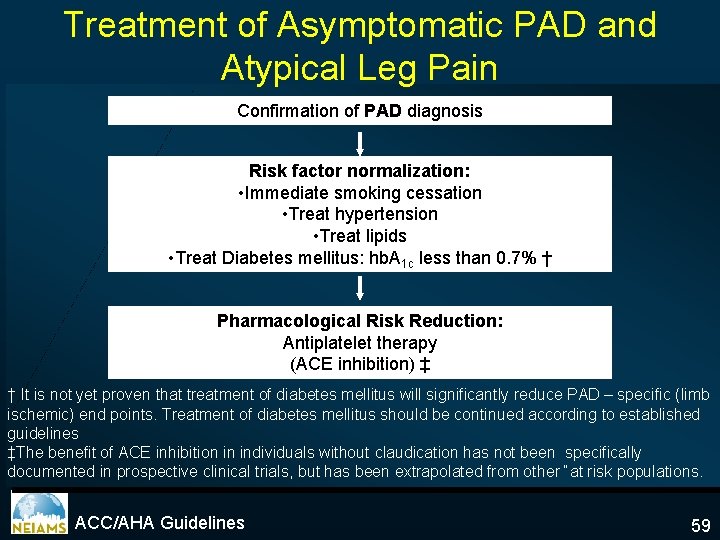
Treatment of Asymptomatic PAD and Atypical Leg Pain Confirmation of PAD diagnosis Risk factor normalization: • Immediate smoking cessation • Treat hypertension • Treat lipids • Treat Diabetes mellitus: hb. A 1 c less than 0. 7% † Pharmacological Risk Reduction: Antiplatelet therapy (ACE inhibition) ‡ † It is not yet proven that treatment of diabetes mellitus will significantly reduce PAD – specific (limb ischemic) end points. Treatment of diabetes mellitus should be continued according to established guidelines ‡The benefit of ACE inhibition in individuals without claudication has not been specifically documented in prospective clinical trials, but has been extrapolated from other “at risk populations. ACC/AHA Guidelines 59
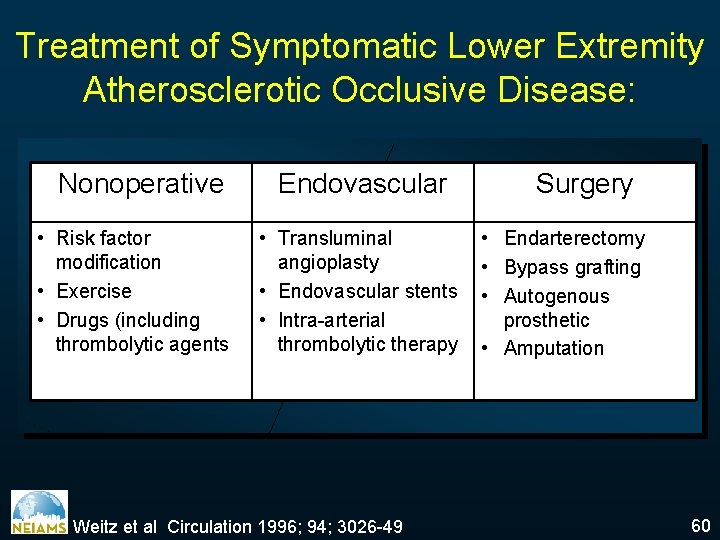
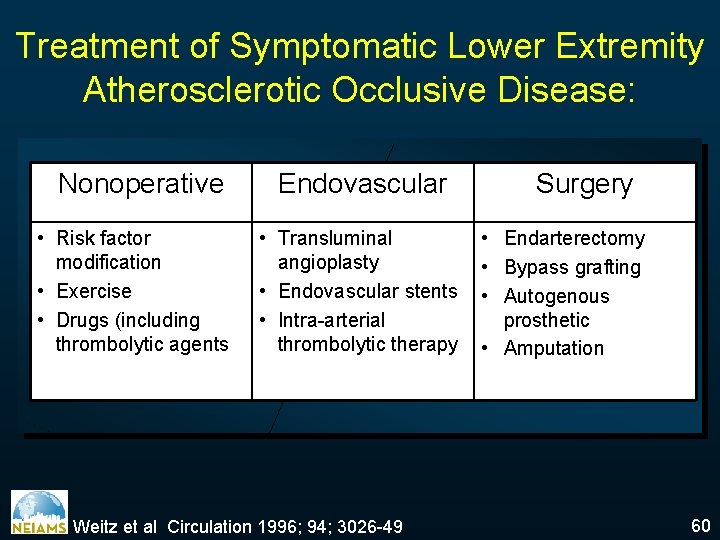
Treatment of Symptomatic Lower Extremity Atherosclerotic Occlusive Disease: Nonoperative • Risk factor modification • Exercise • Drugs (including thrombolytic agents Endovascular • Transluminal angioplasty • Endovascular stents • Intra-arterial thrombolytic therapy Weitz et al Circulation 1996; 94; 3026 -49 Surgery • Endarterectomy • Bypass grafting • Autogenous prosthetic • Amputation 60
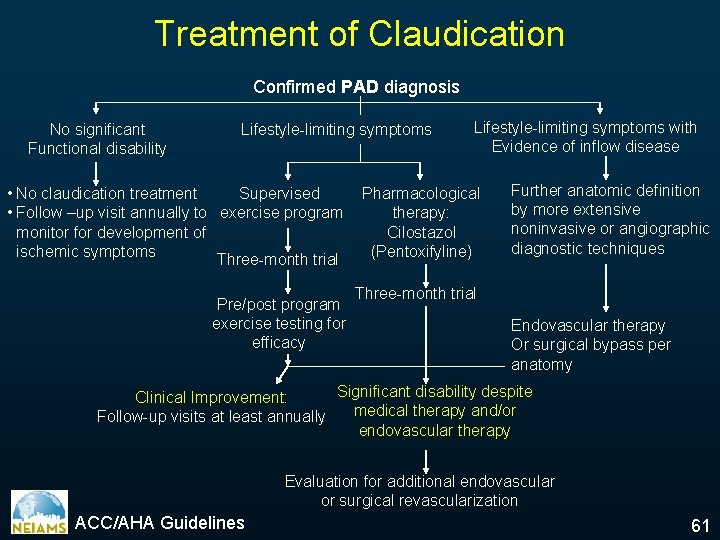
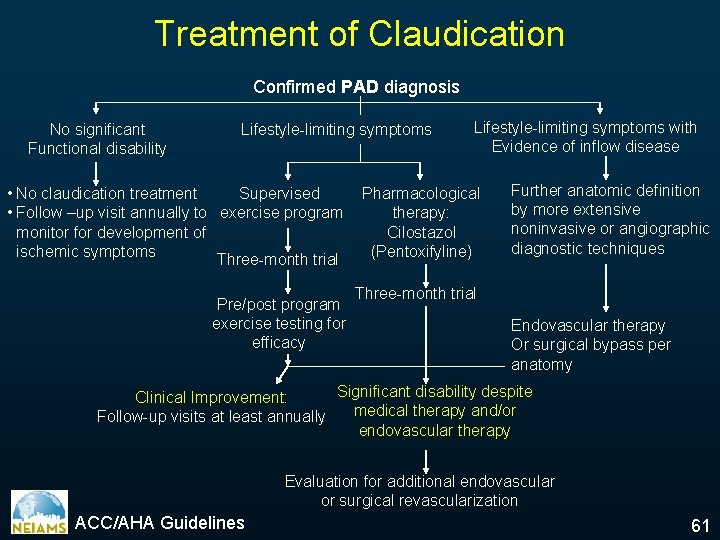
Treatment of Claudication Confirmed PAD diagnosis No significant Functional disability Lifestyle-limiting symptoms • No claudication treatment Supervised • Follow –up visit annually to exercise program monitor for development of ischemic symptoms Three-month trial Pre/post program exercise testing for efficacy Lifestyle-limiting symptoms with Evidence of inflow disease Pharmacological therapy: Cilostazol (Pentoxifyline) Further anatomic definition by more extensive noninvasive or angiographic diagnostic techniques Three-month trial Endovascular therapy Or surgical bypass per anatomy Significant disability despite Clinical Improvement: medical therapy and/or Follow-up visits at least annually endovascular therapy Evaluation for additional endovascular or surgical revascularization ACC/AHA Guidelines 61
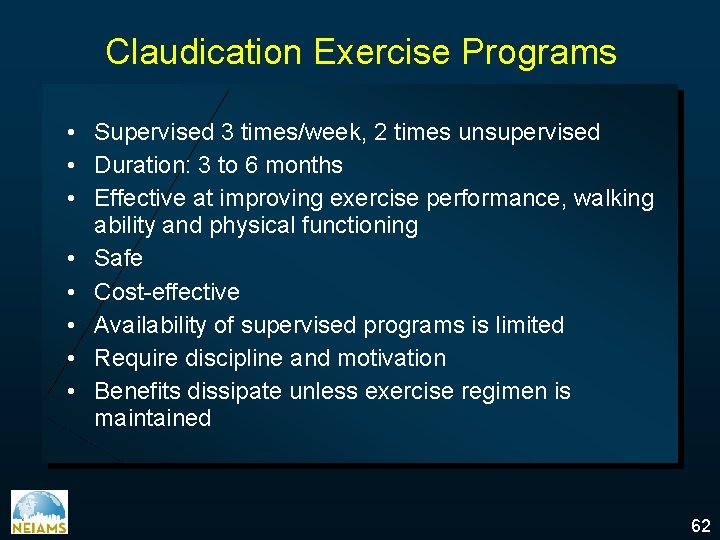
Claudication Exercise Programs • Supervised 3 times/week, 2 times unsupervised • Duration: 3 to 6 months • Effective at improving exercise performance, walking ability and physical functioning • Safe • Cost-effective • Availability of supervised programs is limited • Require discipline and motivation • Benefits dissipate unless exercise regimen is maintained 62
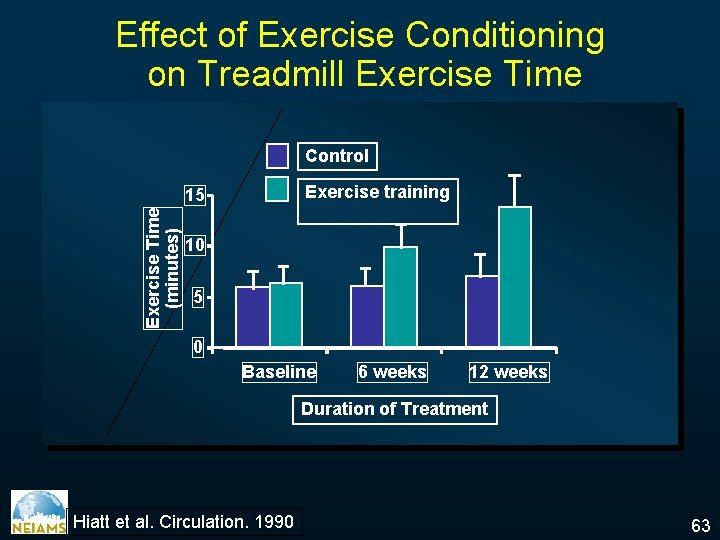
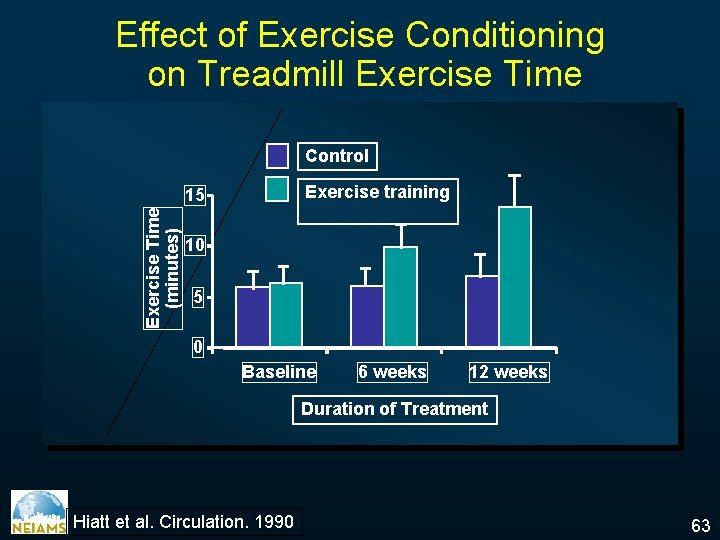
Effect of Exercise Conditioning on Treadmill Exercise Time Control Exercise training Exercise Time (minutes) 15 10 5 0 Baseline 6 weeks 12 weeks Duration of Treatment Hiatt et al. Circulation. 1990 63
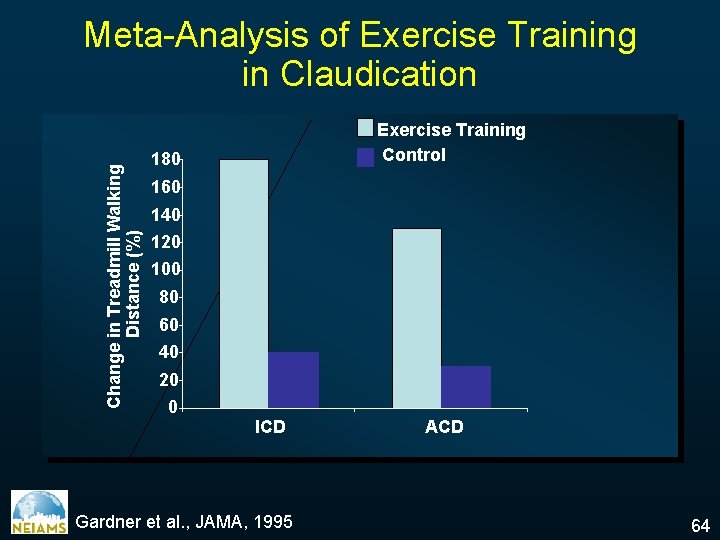
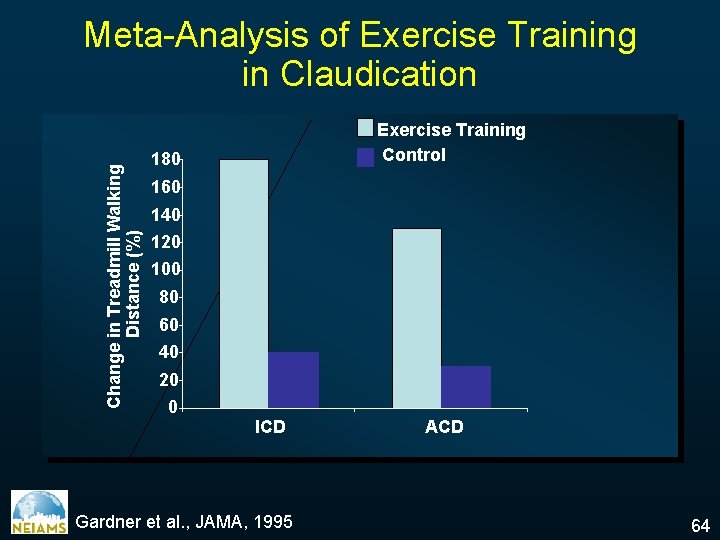
Change in Treadmill Walking Distance (%) Meta-Analysis of Exercise Training in Claudication Exercise Training Control 180 160 140 120 100 80 60 40 20 0 ICD Gardner et al. , JAMA, 1995 ACD 64
Mechanisms of Action of Exercise Therapy in Peripheral Arterial Disease • • Enlarging the radius of the supply vessel Enhance collateral growth (unlikely) Increase pressure gradient across stenosis Increase oxidative capacity of muscle cells Increase in Type I muscle fibers Higher ‘fluidity’ of arterial blood flow Enhanced oxygen affinity of hemoglobin Improved endothelial function 66
67 Statins Smoking cessation Cilostazol Ace Inhibitors Cornerstones of Medical Therapies in PAD
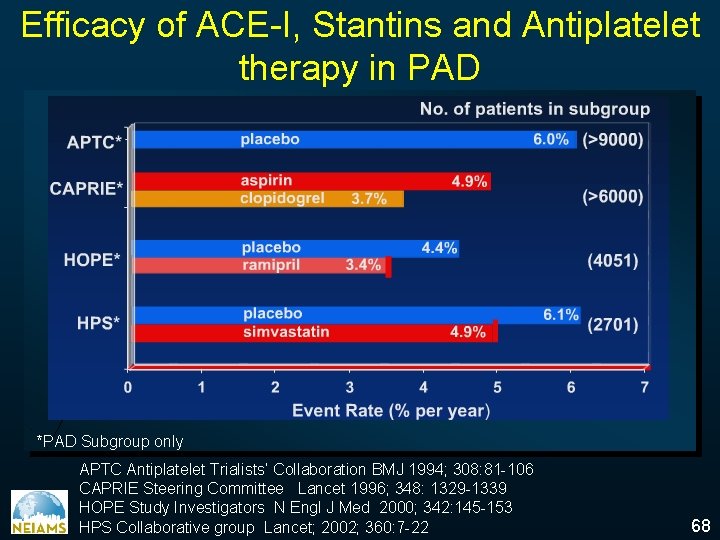
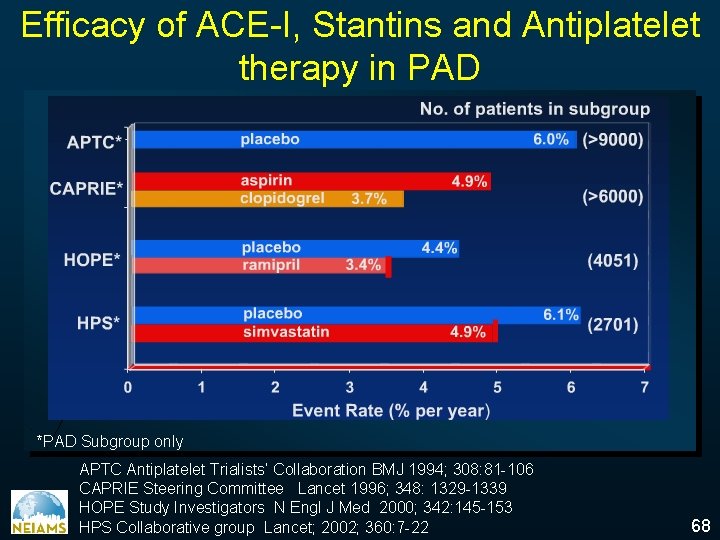
Efficacy of ACE-I, Stantins and Antiplatelet therapy in PAD *PAD Subgroup only APTC Antiplatelet Trialists’ Collaboration BMJ 1994; 308: 81 -106 CAPRIE Steering Committee Lancet 1996; 348: 1329 -1339 HOPE Study Investigators N Engl J Med 2000; 342: 145 -153 HPS Collaborative group Lancet; 2002; 360: 7 -22 68
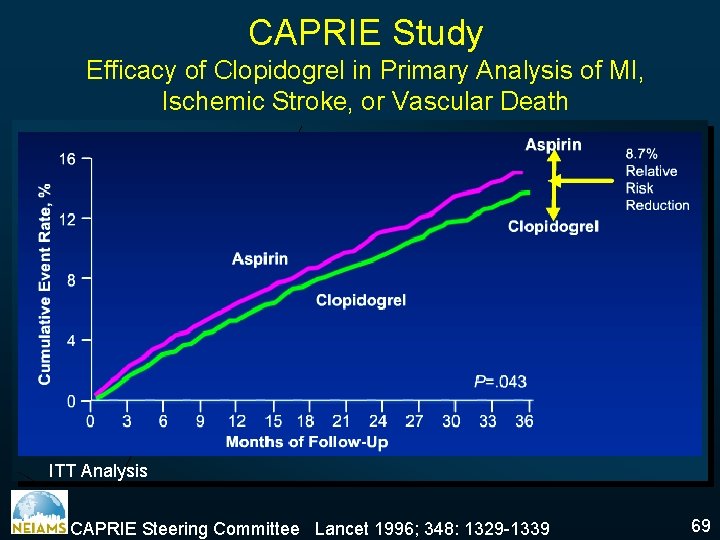
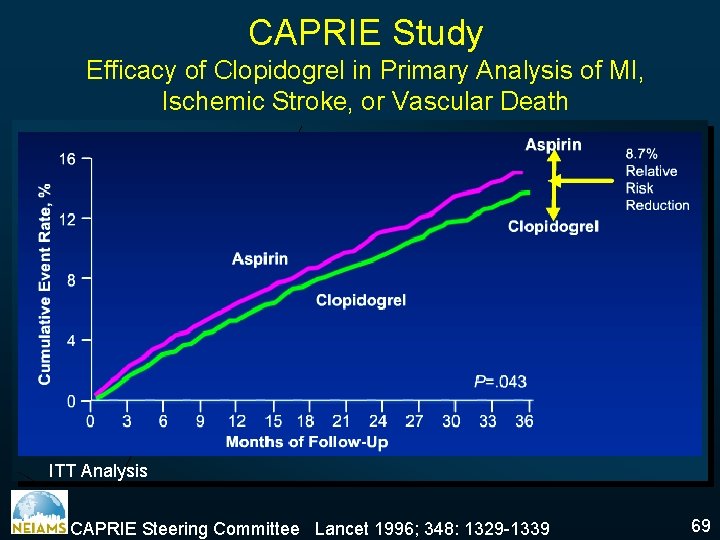
CAPRIE Study Efficacy of Clopidogrel in Primary Analysis of MI, Ischemic Stroke, or Vascular Death ITT Analysis CAPRIE Steering Committee Lancet 1996; 348: 1329 -1339 69
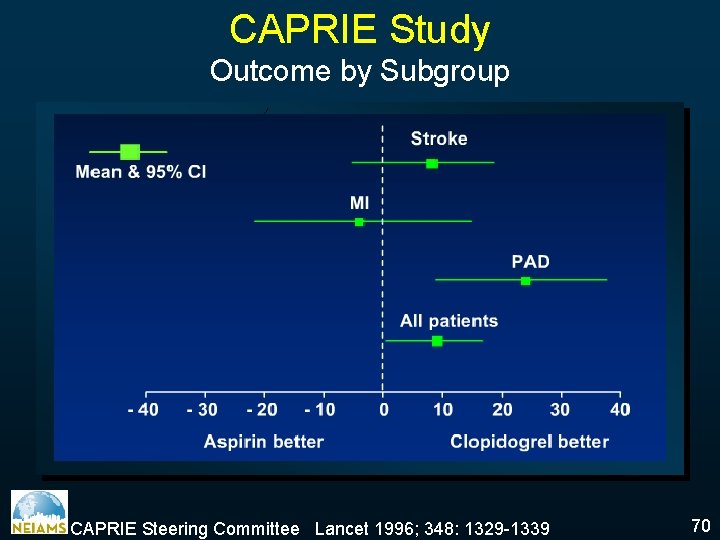
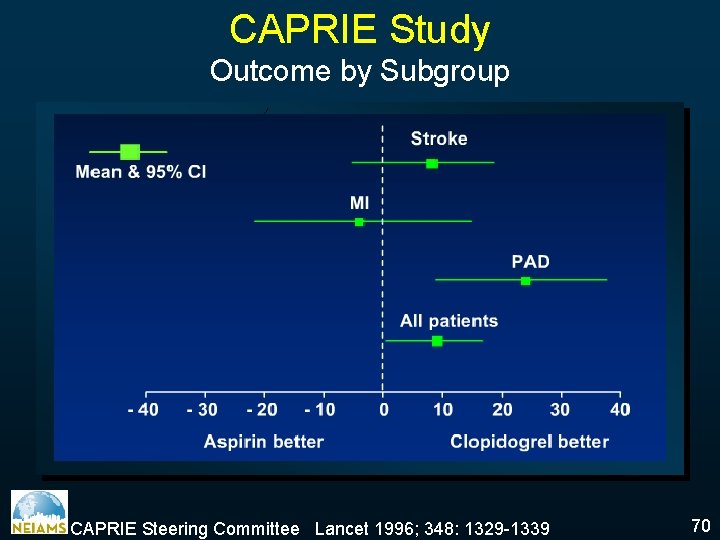
CAPRIE Study Outcome by Subgroup CAPRIE Steering Committee Lancet 1996; 348: 1329 -1339 70
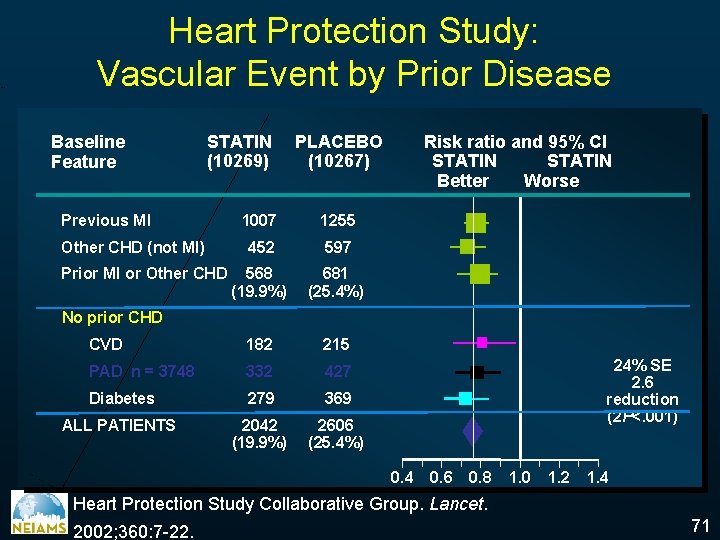
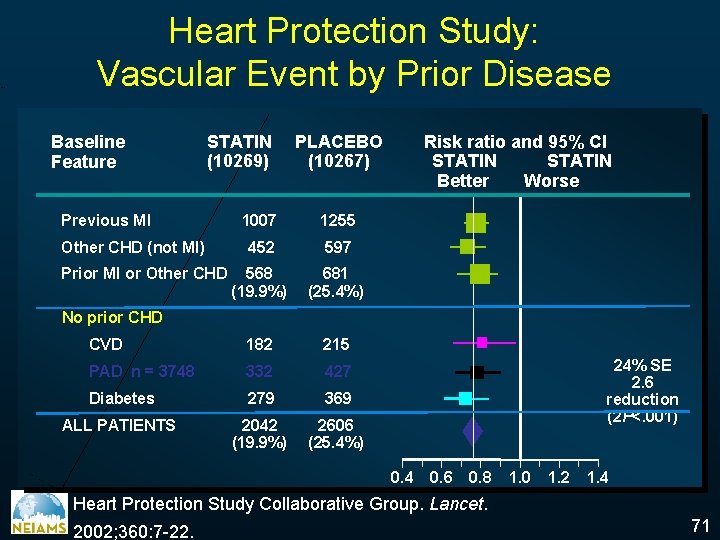
STATIN worse Heart Protection Study: Vascular Event by Prior Disease Baseline Feature STATIN (10269) Previous MI PLACEBO (10267) 1007 1255 452 597 568 (19. 9%) 681 (25. 4%) CVD 182 215 PAD n = 3748 332 427 Diabetes 279 369 ALL PATIENTS 2042 (19. 9%) 2606 (25. 4%) Other CHD (not MI) Prior MI or Other CHD Risk ratio and 95% CI STATIN Better Worse No prior CHD 24% SE 2. 6 reduction (2 P<. 001) 0. 4 0. 6 0. 8 1. 0 1. 2 1. 4 Heart Protection Study Collaborative Group. Lancet. 2002; 360: 7 -22. 71
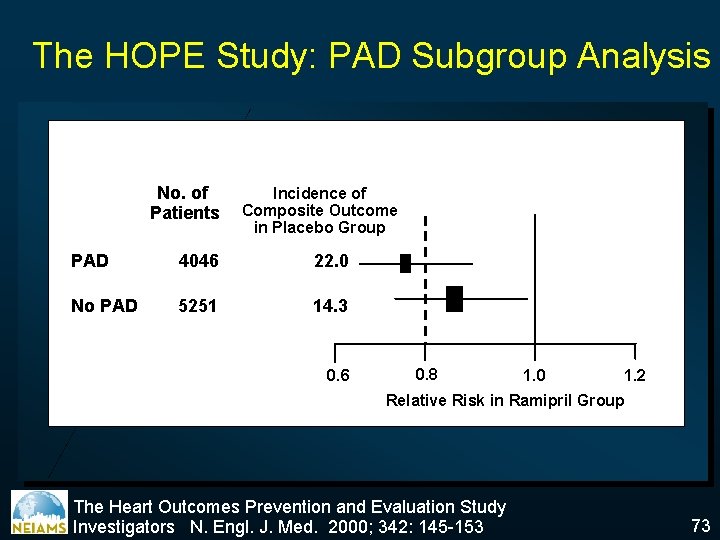
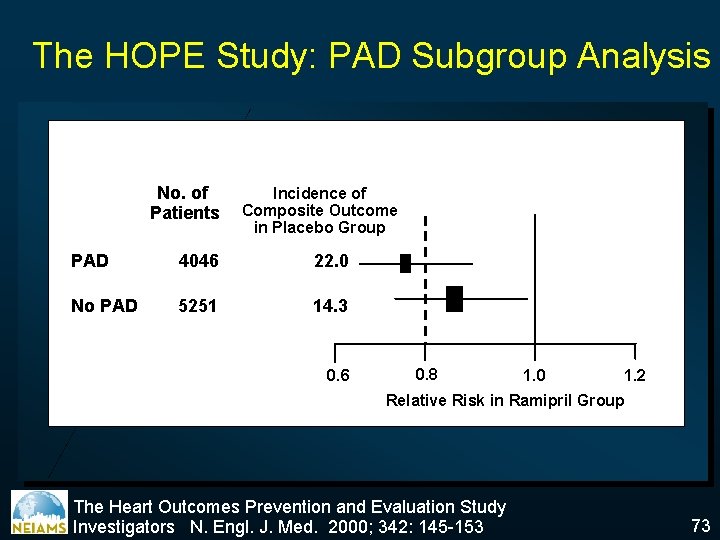
The HOPE Study: PAD Subgroup Analysis No. of Patients Incidence of Composite Outcome in Placebo Group PAD 4046 22. 0 No PAD 5251 14. 3 0. 6 0. 8 1. 0 1. 2 Relative Risk in Ramipril Group The Heart Outcomes Prevention and Evaluation Study Investigators N. Engl. J. Med. 2000; 342: 145 -153 73
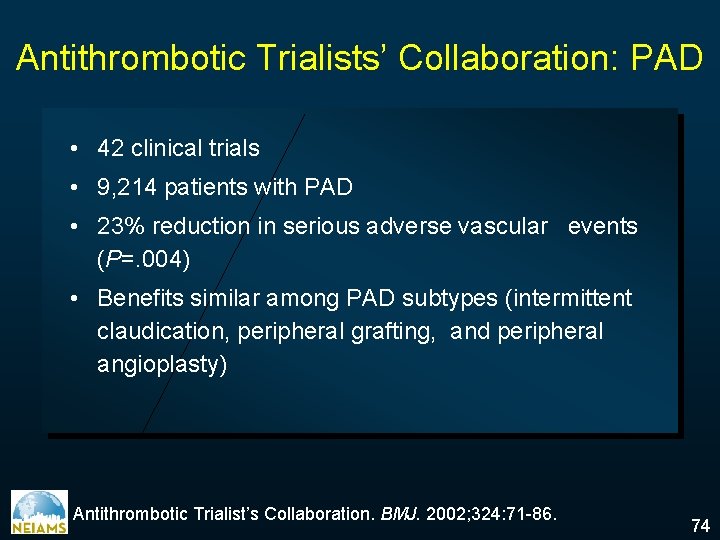
Antithrombotic Trialists’ Collaboration: PAD • 42 clinical trials • 9, 214 patients with PAD • 23% reduction in serious adverse vascular events (P=. 004) • Benefits similar among PAD subtypes (intermittent claudication, peripheral grafting, and peripheral angioplasty) Antithrombotic Trialist’s Collaboration. BMJ. 2002; 324: 71 -86. 74
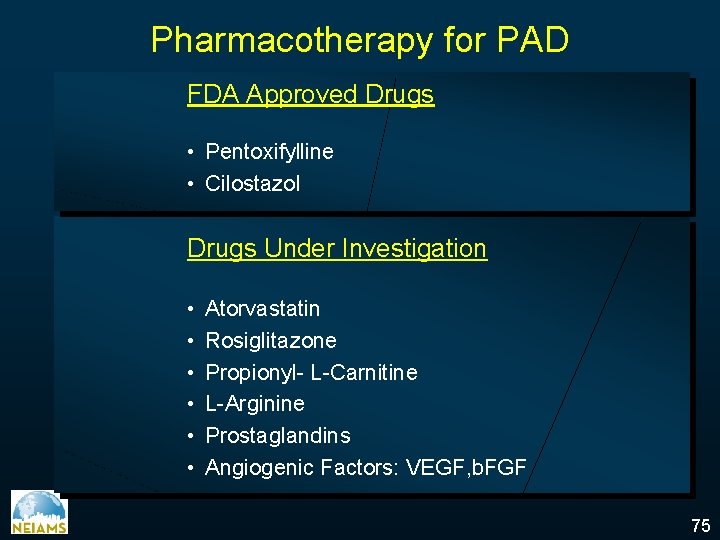
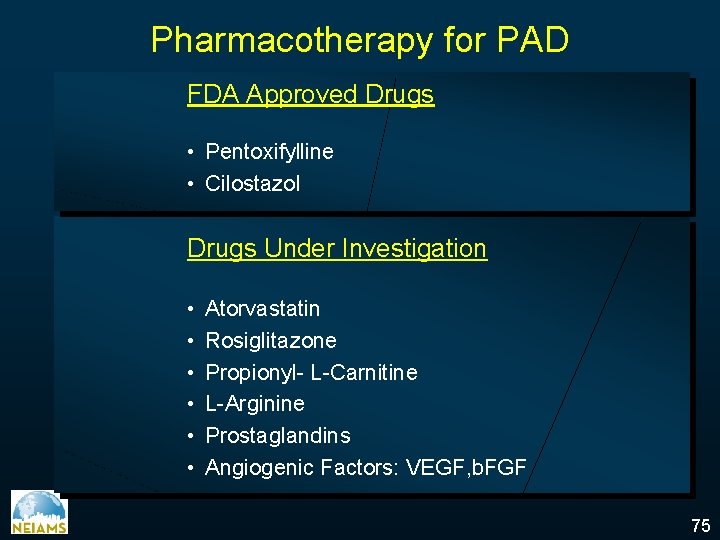
Pharmacotherapy for PAD FDA Approved Drugs • Pentoxifylline • Cilostazol Drugs Under Investigation • • • Atorvastatin Rosiglitazone Propionyl- L-Carnitine L-Arginine Prostaglandins Angiogenic Factors: VEGF, b. FGF 75
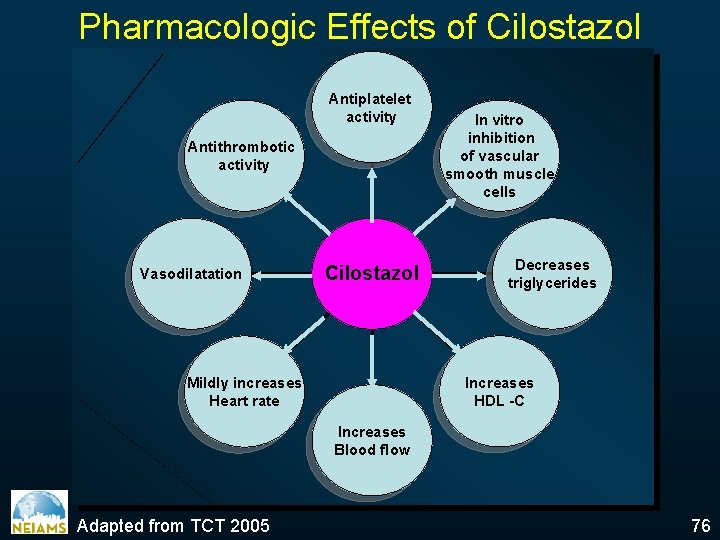
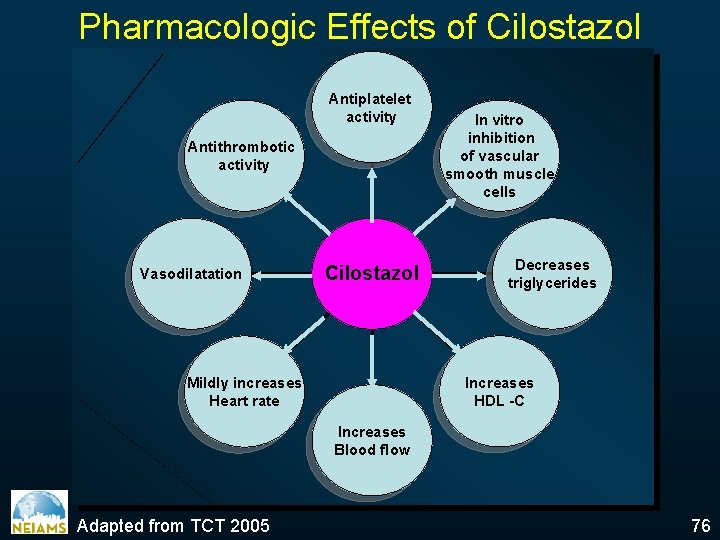
Pharmacologic Effects of Cilostazol Antiplatelet activity Antithrombotic activity Vasodilatation Cilostazol In vitro inhibition of vascular smooth muscle cells Decreases triglycerides Increases HDL -C Mildly increases Heart rate Increases Blood flow Adapted from TCT 2005 76
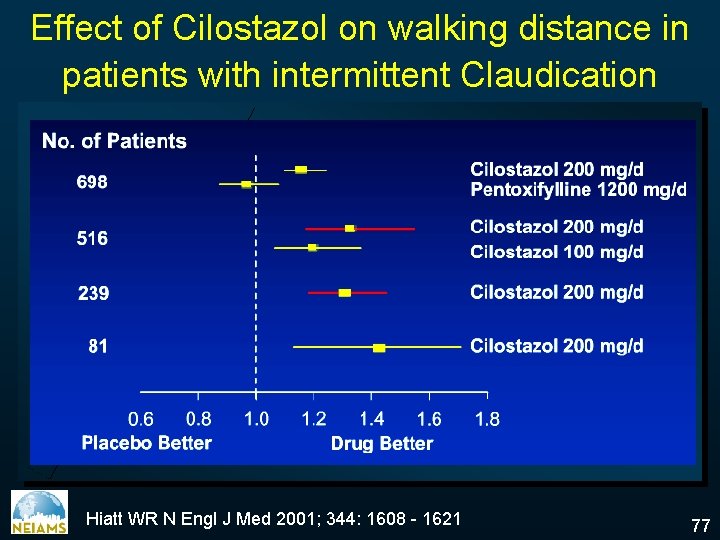
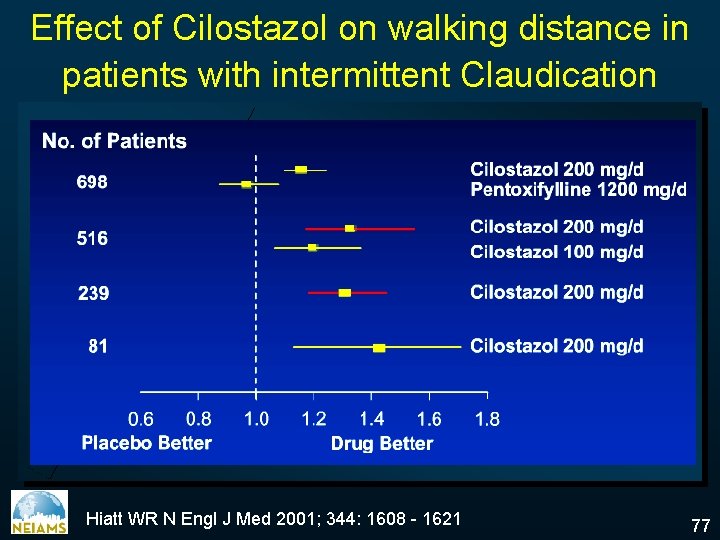
Effect of Cilostazol on walking distance in patients with intermittent Claudication Hiatt WR N Engl J Med 2001; 344: 1608 - 1621 77
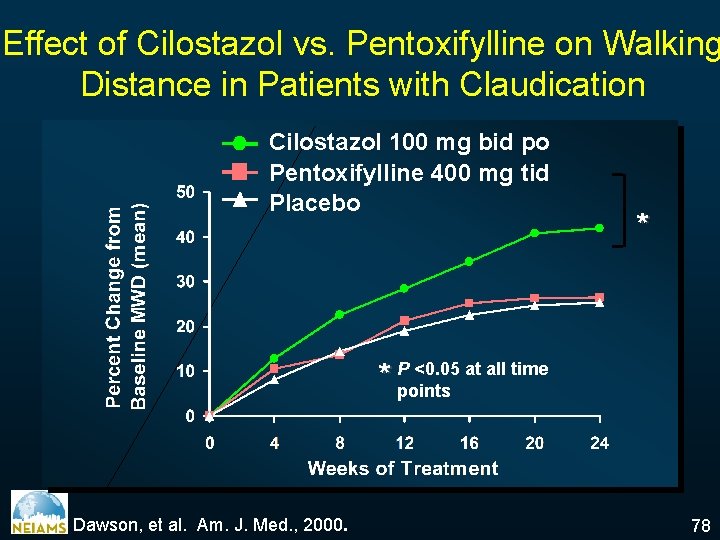
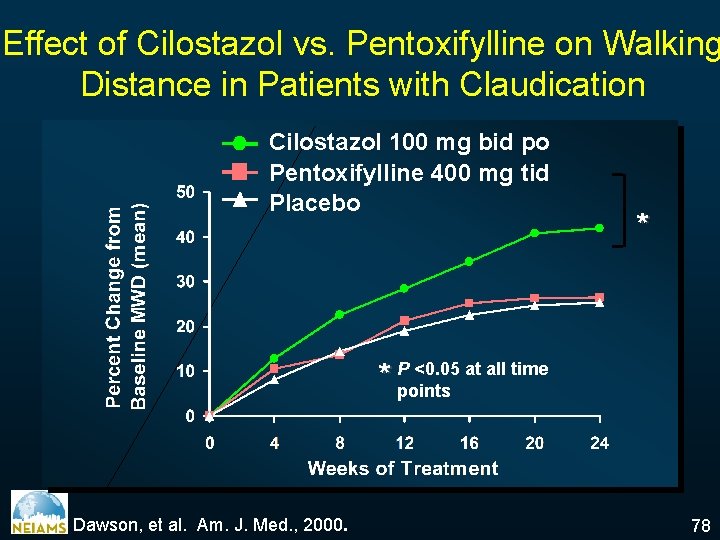
Effect of Cilostazol vs. Pentoxifylline on Walking Distance in Patients with Claudication Cilostazol 100 mg bid po Pentoxifylline 400 mg tid Placebo * <0. 05 at all time * Ppoints Dawson, et al. Am. J. Med. , 2000. 78
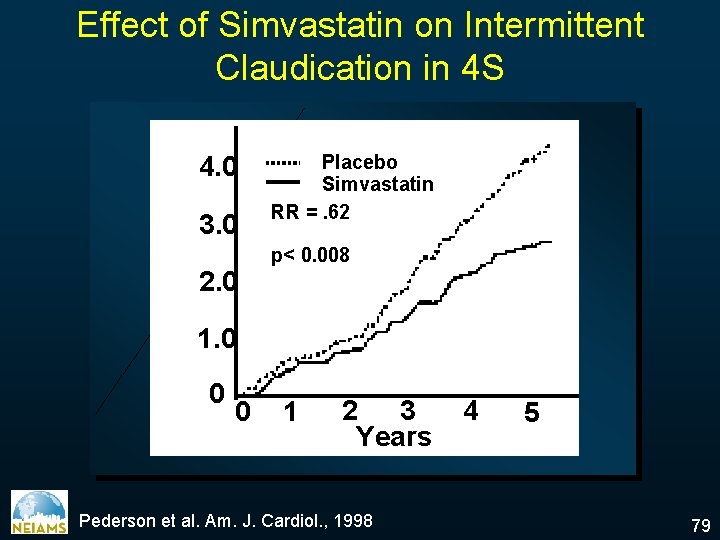
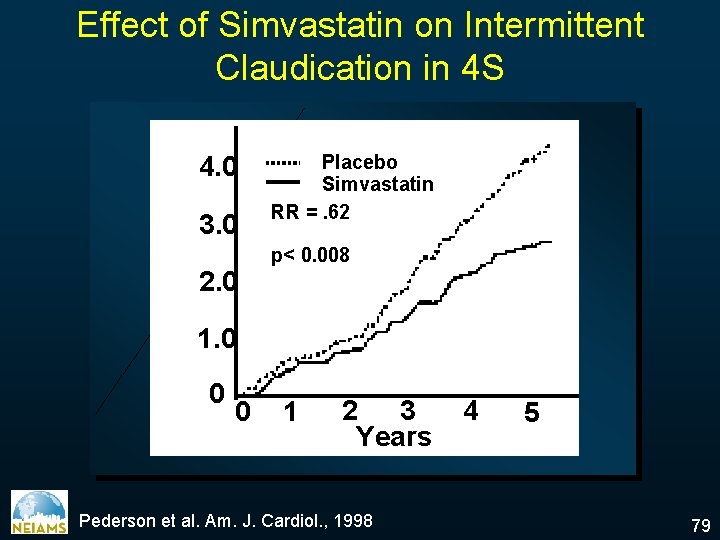
Effect of Simvastatin on Intermittent Claudication in 4 S 4. 0 3. 0 % 2. 0 Placebo Simvastatin RR =. 62 p< 0. 008 1. 0 0 0 1 2 3 Years Pederson et al. Am. J. Cardiol. , 1998 4 5 79
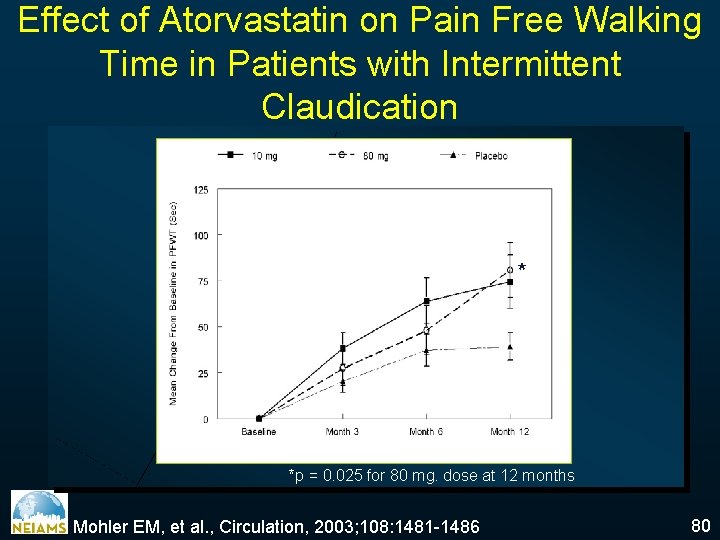
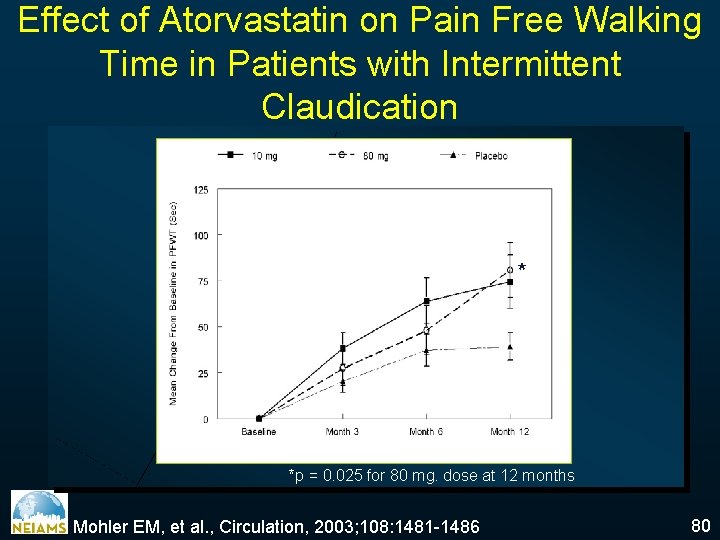
Effect of Atorvastatin on Pain Free Walking Time in Patients with Intermittent Claudication * *p = 0. 025 for 80 mg. dose at 12 months Mohler EM, et al. , Circulation, 2003; 108: 1481 -1486 80
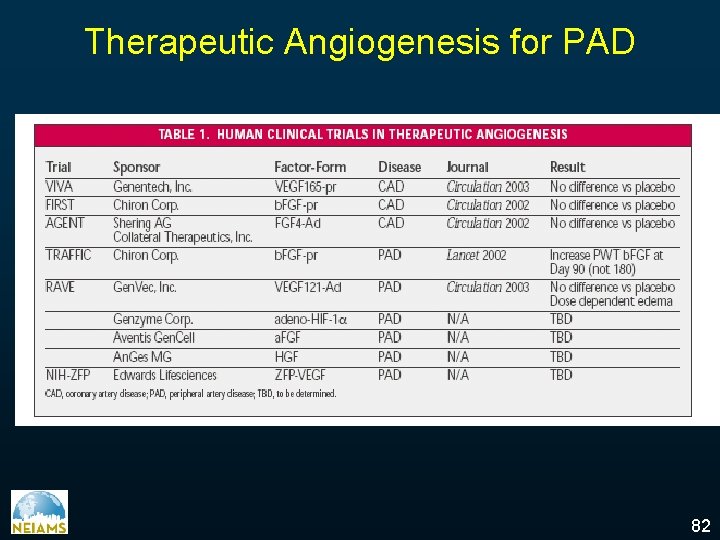
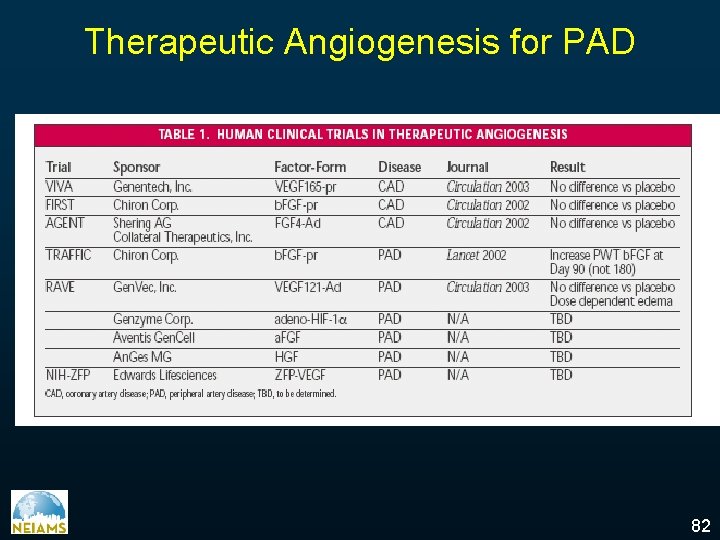
Therapeutic Angiogenesis for PAD 82
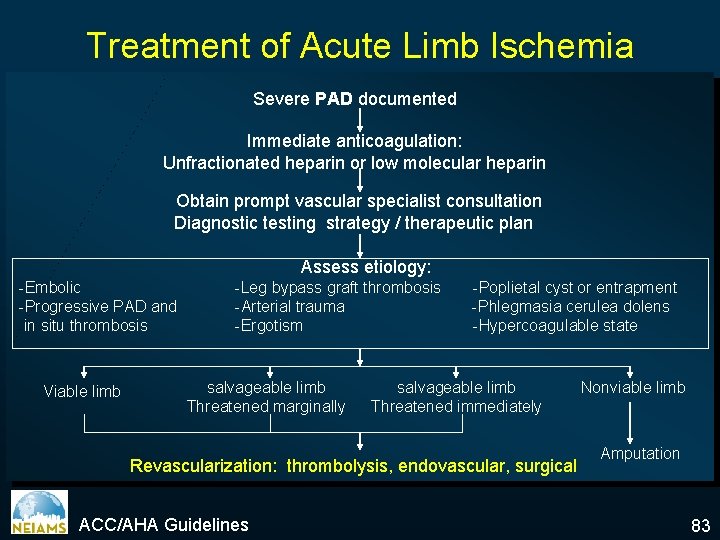
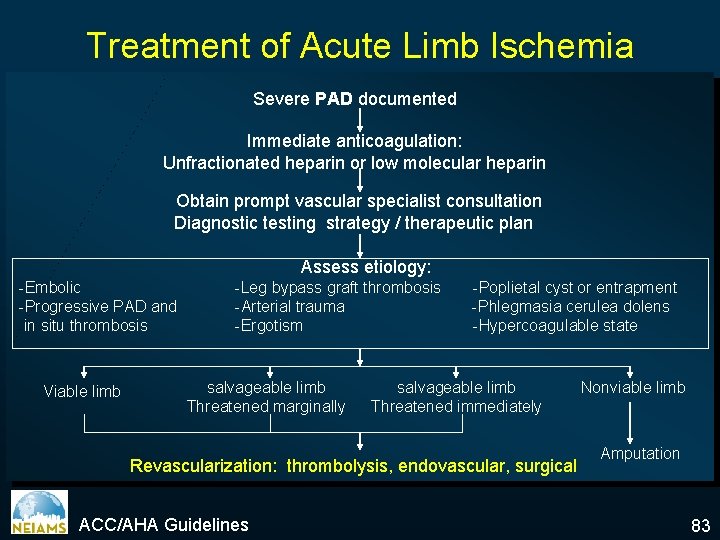
Treatment of Acute Limb Ischemia Severe PAD documented Immediate anticoagulation: Unfractionated heparin or low molecular heparin Obtain prompt vascular specialist consultation Diagnostic testing strategy / therapeutic plan Assess etiology: -Embolic -Progressive PAD and in situ thrombosis Viable limb -Leg bypass graft thrombosis -Arterial trauma -Ergotism salvageable limb Threatened marginally -Poplietal cyst or entrapment -Phlegmasia cerulea dolens -Hypercoagulable state salvageable limb Threatened immediately Revascularization: thrombolysis, endovascular, surgical ACC/AHA Guidelines Nonviable limb Amputation 83
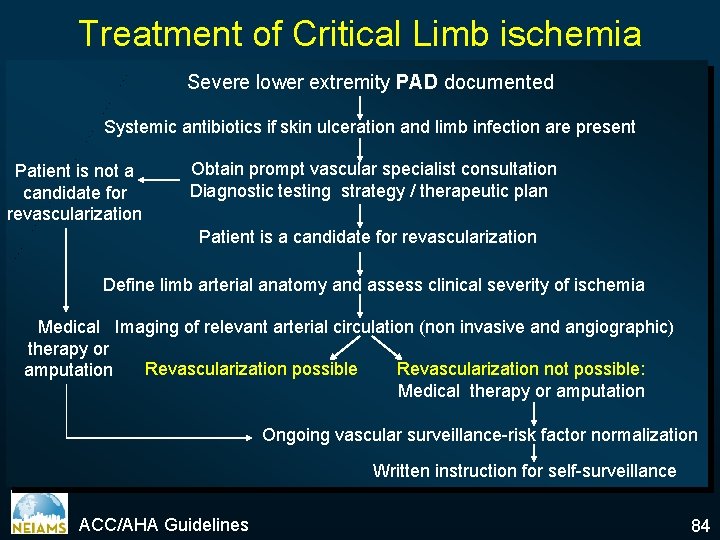
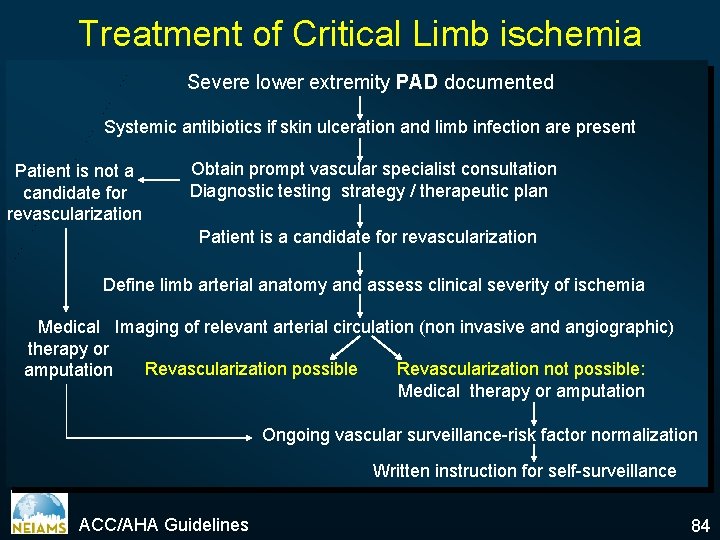
Treatment of Critical Limb ischemia Severe lower extremity PAD documented Systemic antibiotics if skin ulceration and limb infection are present Patient is not a candidate for revascularization Obtain prompt vascular specialist consultation Diagnostic testing strategy / therapeutic plan Patient is a candidate for revascularization Define limb arterial anatomy and assess clinical severity of ischemia Medical Imaging of relevant arterial circulation (non invasive and angiographic) therapy or Revascularization possible Revascularization not possible: amputation Medical therapy or amputation Ongoing vascular surveillance-risk factor normalization Written instruction for self-surveillance ACC/AHA Guidelines 84
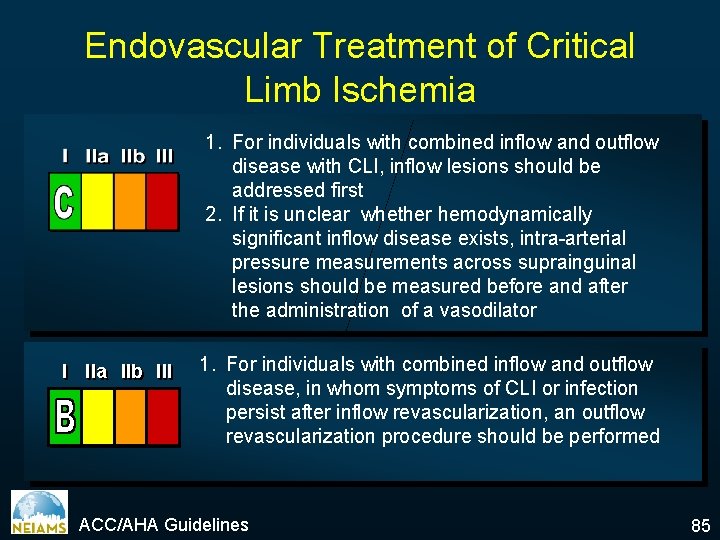
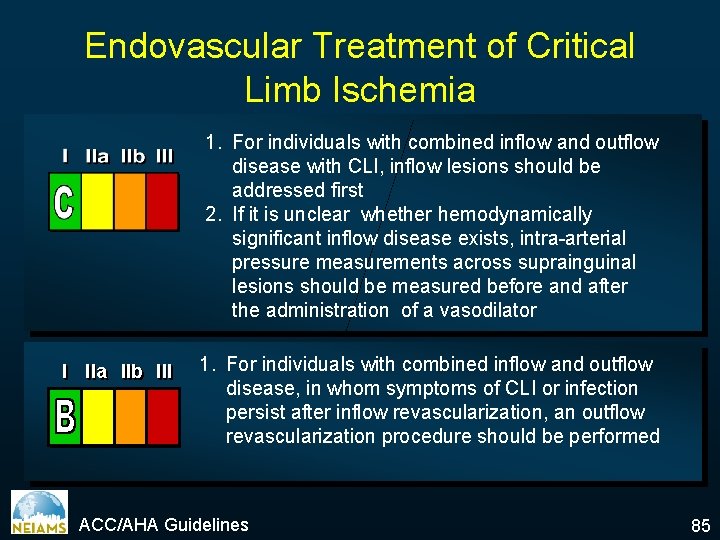
Endovascular Treatment of Critical Limb Ischemia 1. For individuals with combined inflow and outflow disease with CLI, inflow lesions should be addressed first 2. If it is unclear whether hemodynamically significant inflow disease exists, intra-arterial pressure measurements across suprainguinal lesions should be measured before and after the administration of a vasodilator I IIa IIb III 1. For individuals with combined inflow and outflow disease, in whom symptoms of CLI or infection persist after inflow revascularization, an outflow revascularization procedure should be performed ACC/AHA Guidelines 85
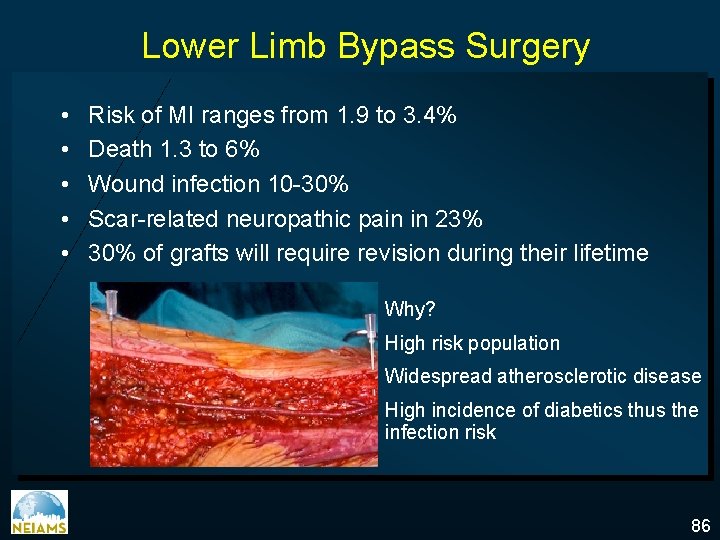
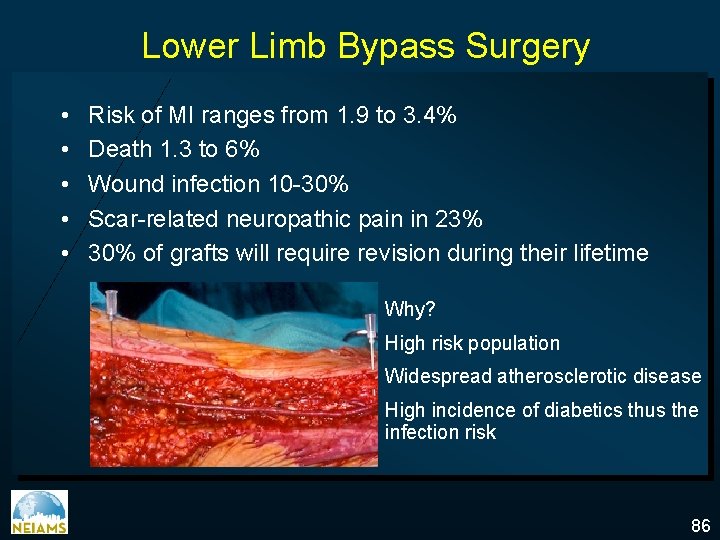
Lower Limb Bypass Surgery • • • Risk of MI ranges from 1. 9 to 3. 4% Death 1. 3 to 6% Wound infection 10 -30% Scar-related neuropathic pain in 23% 30% of grafts will require revision during their lifetime Why? High risk population Widespread atherosclerotic disease High incidence of diabetics thus the infection risk 86
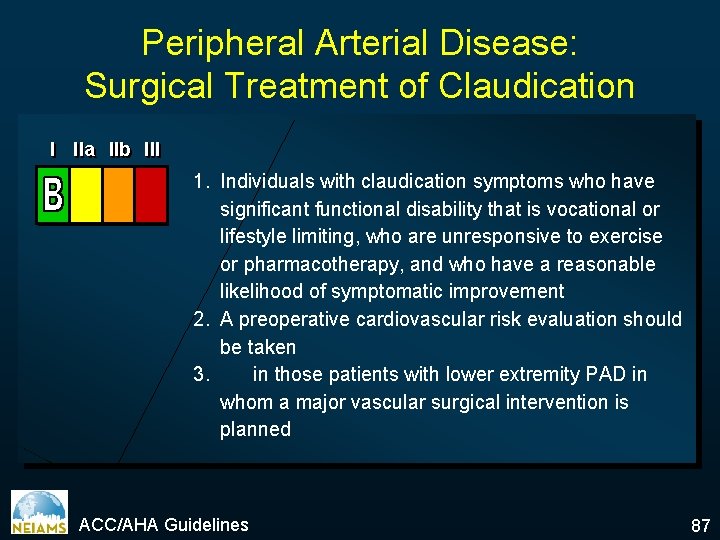
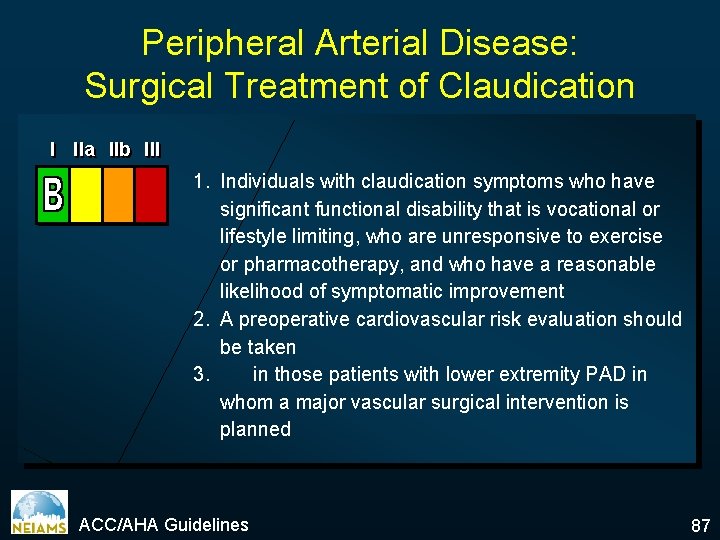
Peripheral Arterial Disease: Surgical Treatment of Claudication I IIa IIb III 1. Individuals with claudication symptoms who have significant functional disability that is vocational or lifestyle limiting, who are unresponsive to exercise or pharmacotherapy, and who have a reasonable likelihood of symptomatic improvement 2. A preoperative cardiovascular risk evaluation should be taken 3. in those patients with lower extremity PAD in whom a major vascular surgical intervention is planned ACC/AHA Guidelines 87
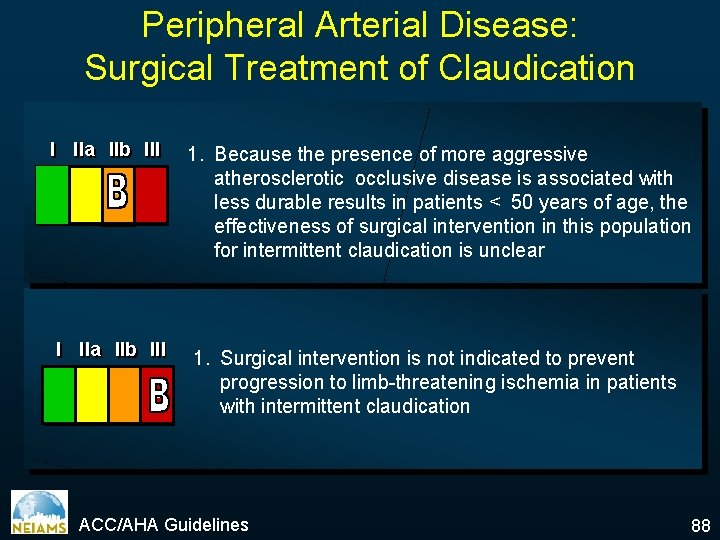
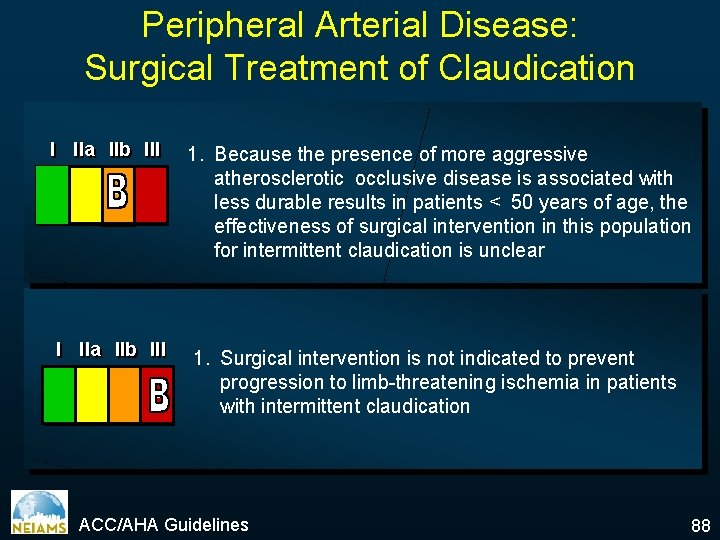
Peripheral Arterial Disease: Surgical Treatment of Claudication I IIa IIb III 1. Because the presence of more aggressive atherosclerotic occlusive disease is associated with less durable results in patients < 50 years of age, the effectiveness of surgical intervention in this population for intermittent claudication is unclear 1. Surgical intervention is not indicated to prevent progression to limb-threatening ischemia in patients with intermittent claudication ACC/AHA Guidelines 88
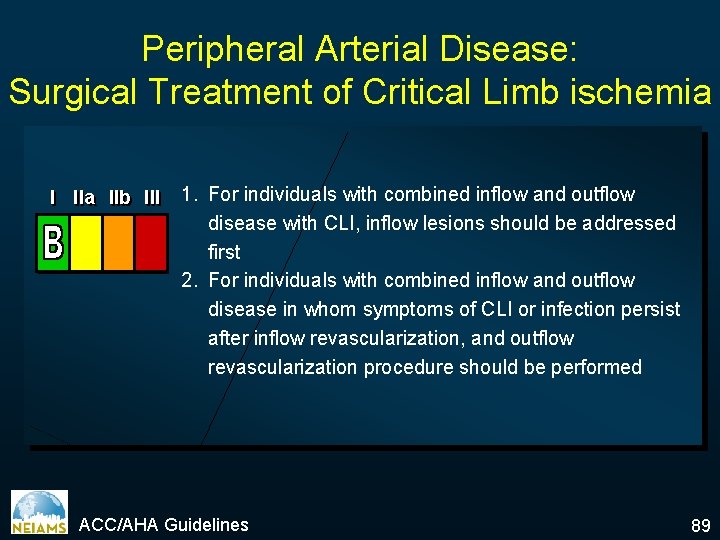
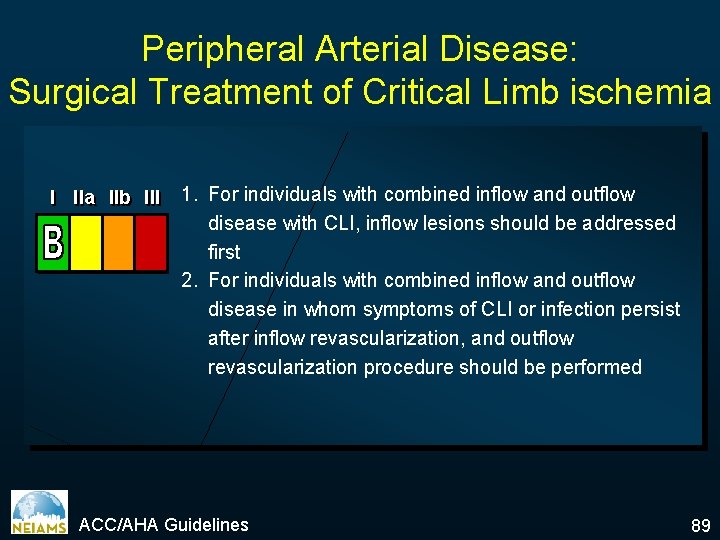
Peripheral Arterial Disease: Surgical Treatment of Critical Limb ischemia I IIa IIb III 1. For individuals with combined inflow and outflow disease with CLI, inflow lesions should be addressed first 2. For individuals with combined inflow and outflow disease in whom symptoms of CLI or infection persist after inflow revascularization, and outflow revascularization procedure should be performed ACC/AHA Guidelines 89
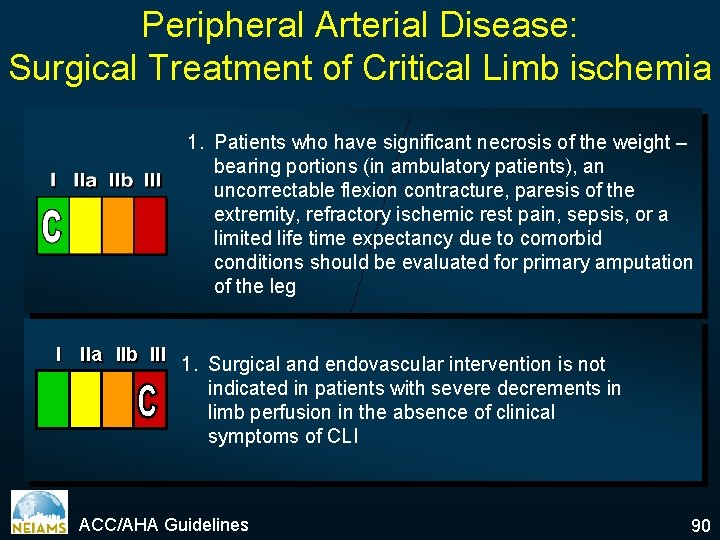
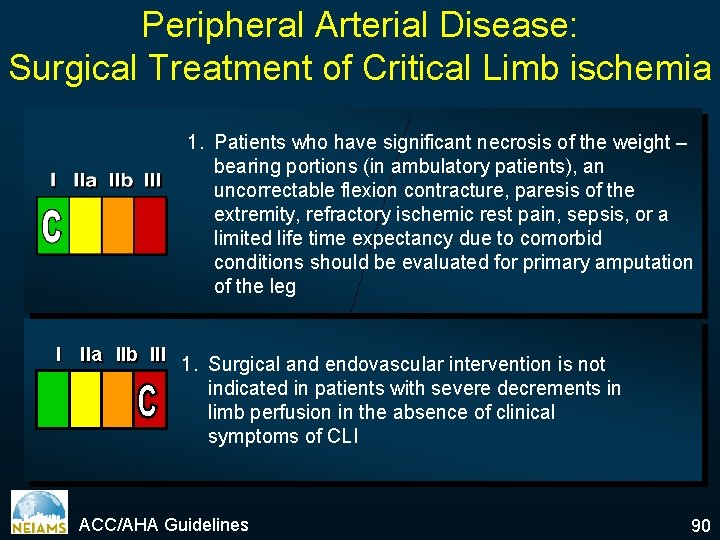
Peripheral Arterial Disease: Surgical Treatment of Critical Limb ischemia 1. Patients who have significant necrosis of the weight – bearing portions (in ambulatory patients), an uncorrectable flexion contracture, paresis of the extremity, refractory ischemic rest pain, sepsis, or a limited life time expectancy due to comorbid conditions should be evaluated for primary amputation of the leg I IIa IIb III 1. Surgical and endovascular intervention is not indicated in patients with severe decrements in limb perfusion in the absence of clinical symptoms of CLI ACC/AHA Guidelines 90
Peripheral Arterial Disease Etiology Epidemiology Physical examination Clinical Manifestations Diagnosis Indications Treatment Options ü Prognosis 91
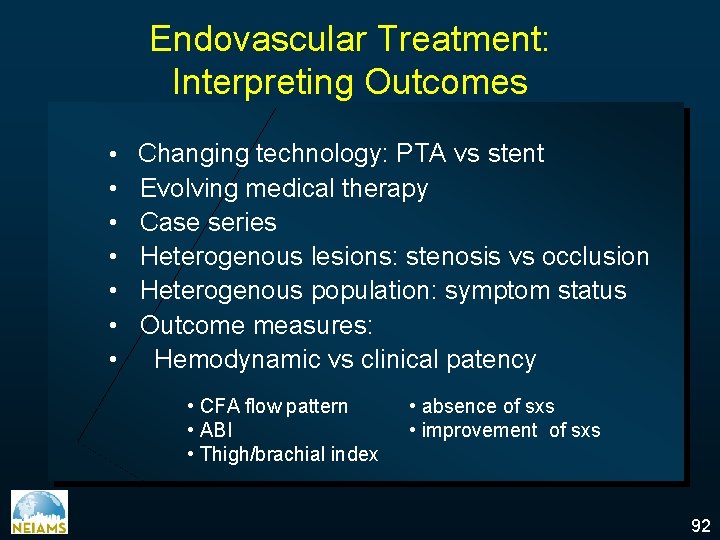
Endovascular Treatment: Interpreting Outcomes • Changing technology: PTA vs stent • • • Evolving medical therapy Case series Heterogenous lesions: stenosis vs occlusion Heterogenous population: symptom status Outcome measures: Hemodynamic vs clinical patency • CFA flow pattern • ABI • Thigh/brachial index • absence of sxs • improvement of sxs 92
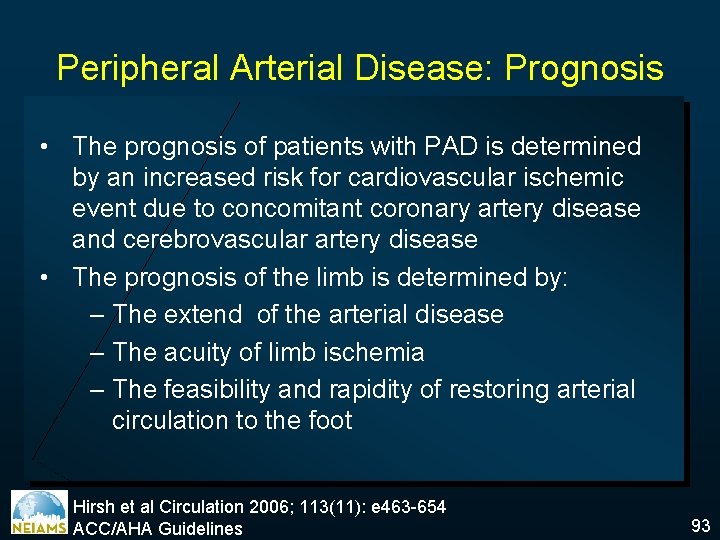
Peripheral Arterial Disease: Prognosis • The prognosis of patients with PAD is determined by an increased risk for cardiovascular ischemic event due to concomitant coronary artery disease and cerebrovascular artery disease • The prognosis of the limb is determined by: – The extend of the arterial disease – The acuity of limb ischemia – The feasibility and rapidity of restoring arterial circulation to the foot Hirsh et al Circulation 2006; 113(11): e 463 -654 ACC/AHA Guidelines 93
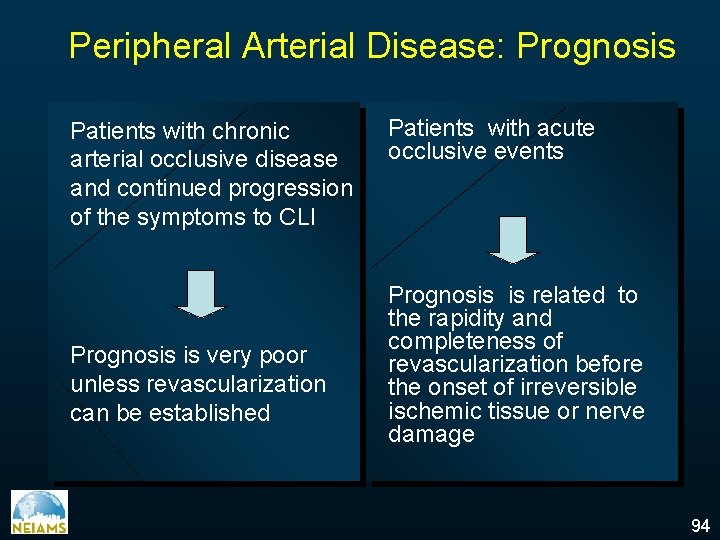
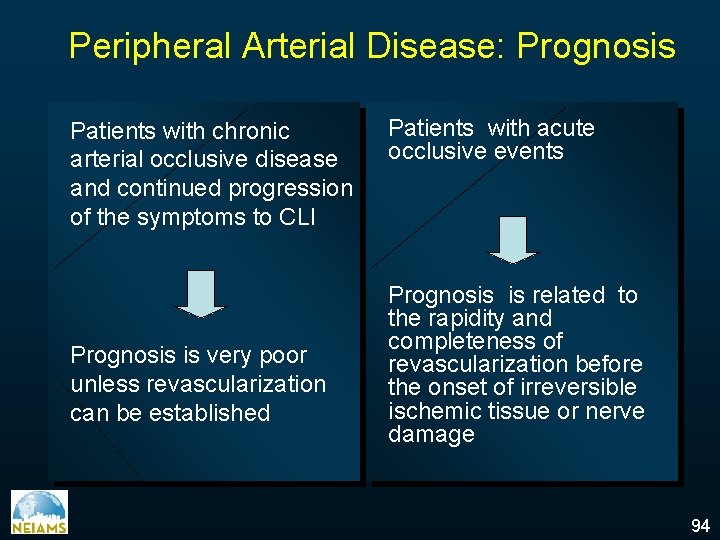
Peripheral Arterial Disease: Prognosis Patients with chronic arterial occlusive disease and continued progression of the symptoms to CLI Prognosis is very poor unless revascularization can be established Patients with acute occlusive events Prognosis is related to the rapidity and completeness of revascularization before the onset of irreversible ischemic tissue or nerve damage 94
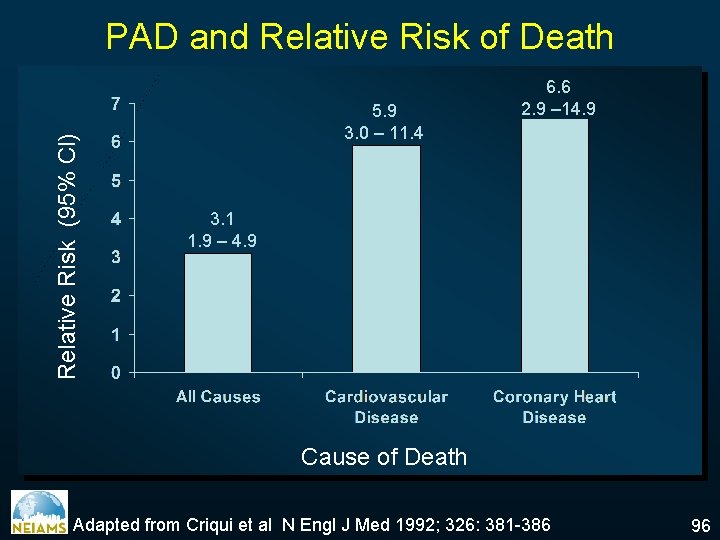
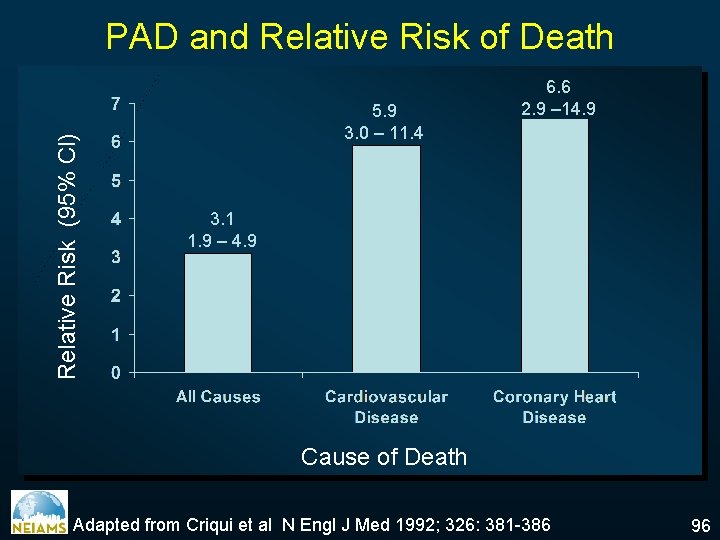
Relative Risk (95% Cl) PAD and Relative Risk of Death 5. 9 3. 0 – 11. 4 6. 6 2. 9 – 14. 9 3. 1 1. 9 – 4. 9 Cause of Death Adapted from Criqui et al N Engl J Med 1992; 326: 381 -386 96
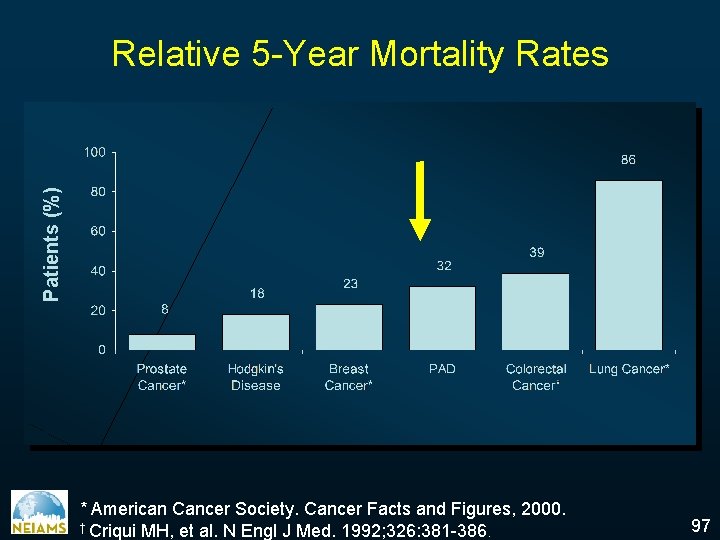
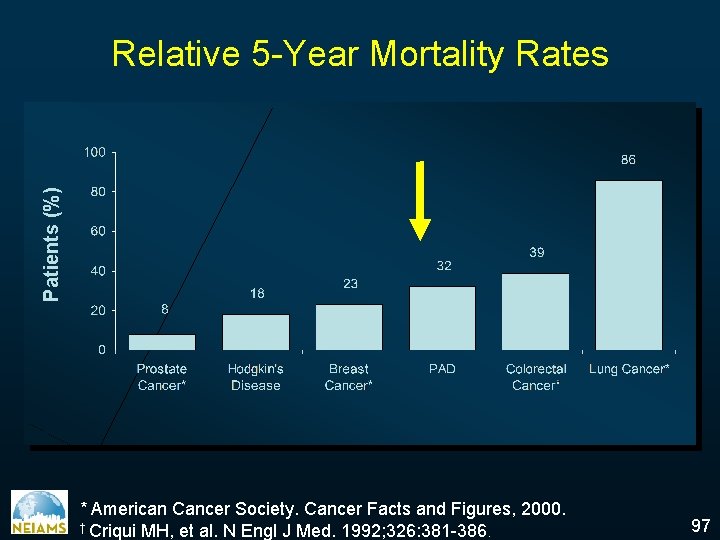
Patients (%) Relative 5 -Year Mortality Rates * American Cancer Society. Cancer Facts and Figures, 2000. † Criqui MH, et al. N Engl J Med. 1992; 326: 381 -386. 97
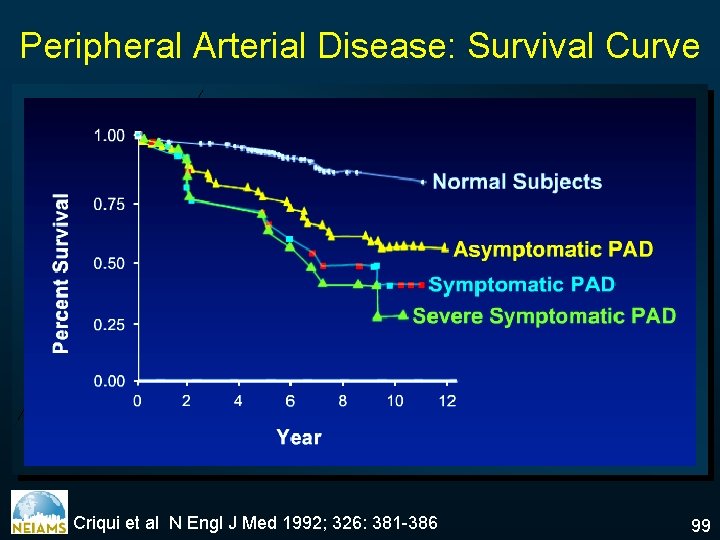
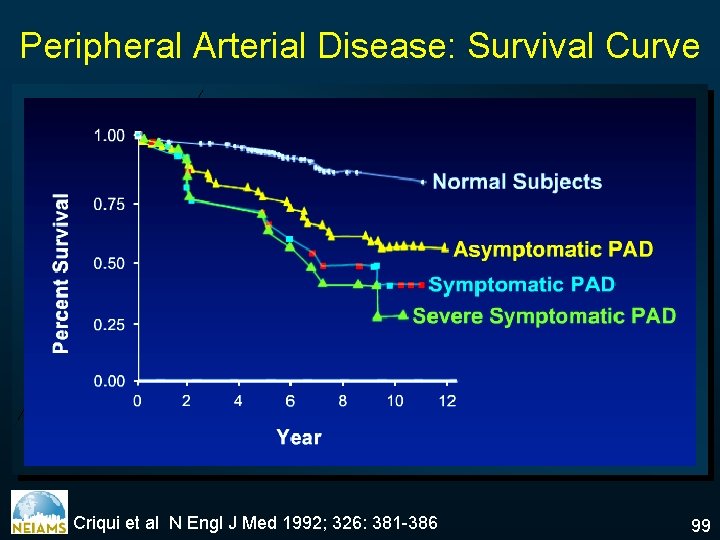
Peripheral Arterial Disease: Survival Curve Criqui et al N Engl J Med 1992; 326: 381 -386 99
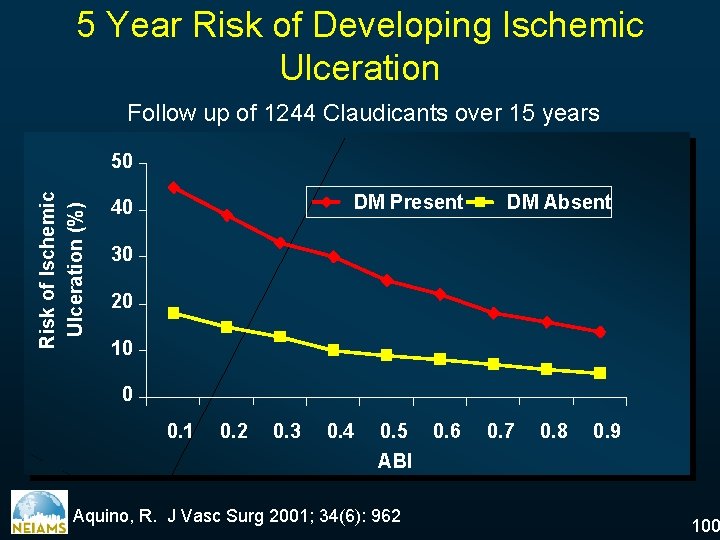
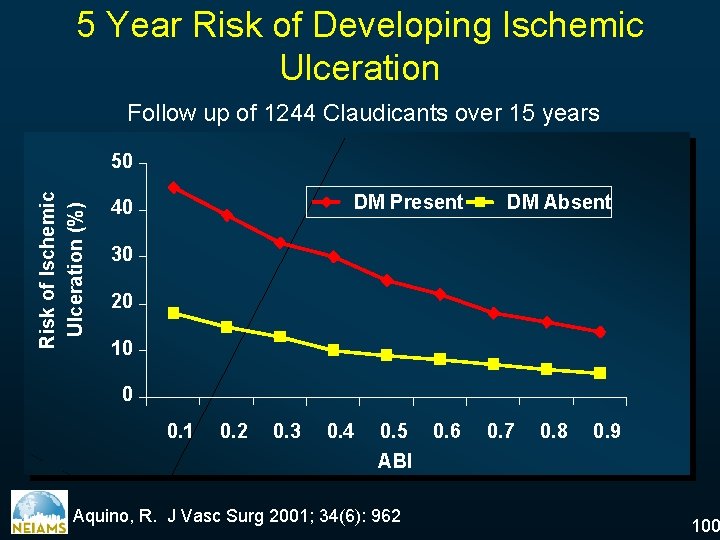
5 Year Risk of Developing Ischemic Ulceration Follow up of 1244 Claudicants over 15 years Risk of Ischemic Ulceration (%) 50 DM Present 40 DM Absent 30 20 10 0 0. 1 0. 2 0. 3 0. 4 0. 5 ABI Aquino, R. J Vasc Surg 2001; 34(6): 962 0. 6 0. 7 0. 8 0. 9 100
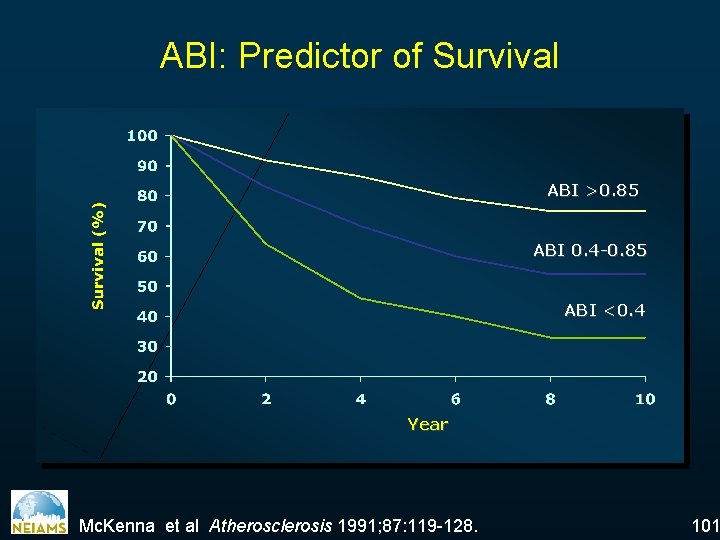
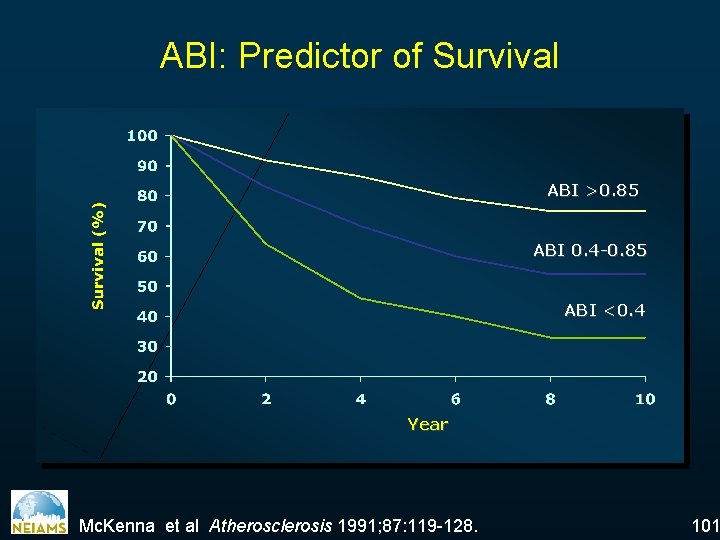
ABI: Predictor of Survival ABI >0. 85 ABI 0. 4 -0. 85 ABI <0. 4 Year Mc. Kenna et al Atherosclerosis 1991; 87: 119 -128. 101
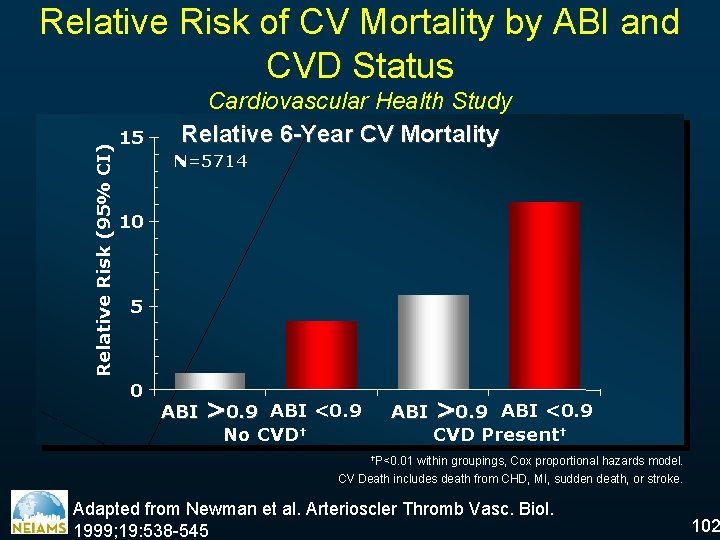
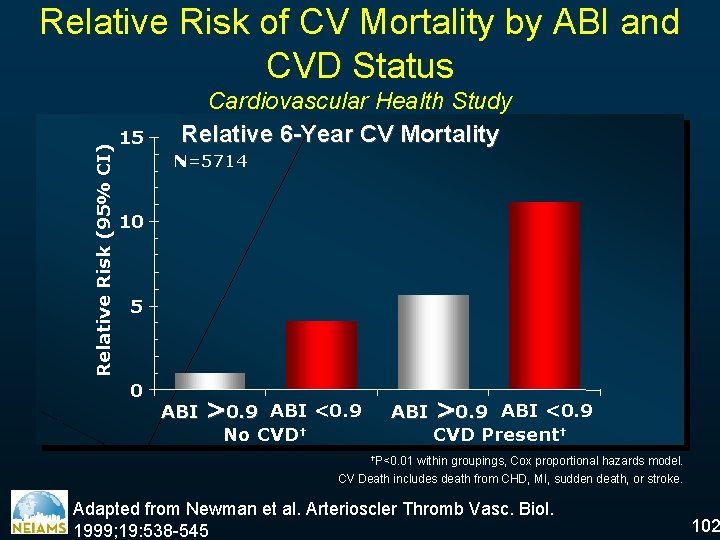
Relative Risk (95% CI) Relative Risk of CV Mortality by ABI and CVD Status 15 Cardiovascular Health Study Relative 6 -Year CV Mortality N=5714 10 5 0 ABI >0. 9 ABI <0. 9 No CVD† ABI >0. 9 ABI <0. 9 CVD Present† †P<0. 01 within groupings, Cox proportional hazards model. CV Death includes death from CHD, MI, sudden death, or stroke. Adapted from Newman et al. Arterioscler Thromb Vasc. Biol. 1999; 19: 538 -545 102
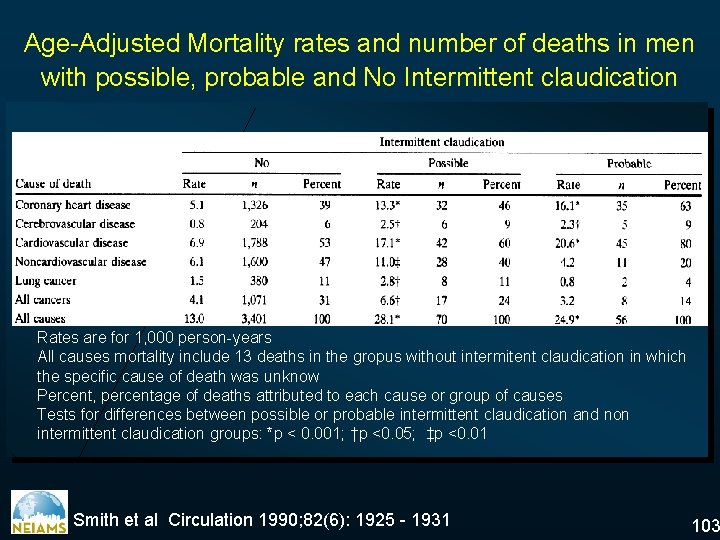
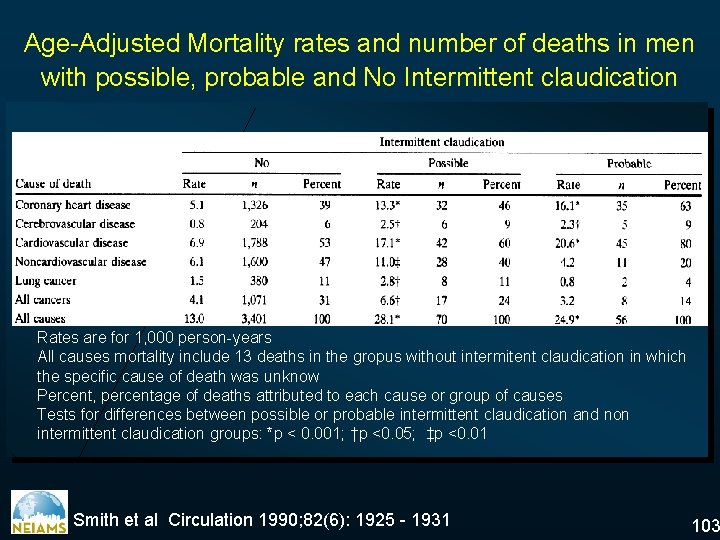
Age-Adjusted Mortality rates and number of deaths in men with possible, probable and No Intermittent claudication Rates are for 1, 000 person-years All causes mortality include 13 deaths in the gropus without intermitent claudication in which the specific cause of death was unknow Percent, percentage of deaths attributed to each cause or group of causes Tests for differences between possible or probable intermittent claudication and non intermittent claudication groups: *p < 0. 001; †p <0. 05; ‡p <0. 01 Smith et al Circulation 1990; 82(6): 1925 - 1931 103