Peripheral Arterial Disease Faculty of Medicine University of










- Slides: 70
Peripheral Arterial Disease Faculty of Medicine University of Brawijaya Malang
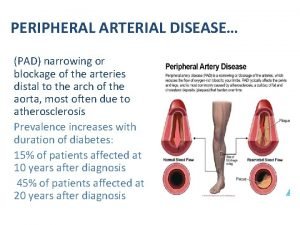
PAD is a common disorder n Occurs in approximately 1/3 of patients n n n Strong association with CAD n n n Over age 70 Over age 50 who smoke or have DM Obvious associated risk of stroke, MI, cardiovascular death Progressive disease in 25% with progressive intermittent claudication/limb threatening ischemia Outcomes n n n Impaired Qo. L (quality of life) Limb Loss Premature Mortality
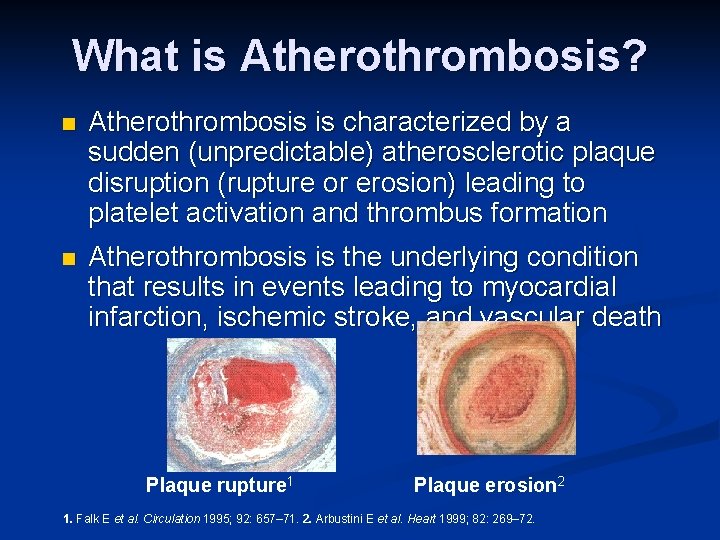
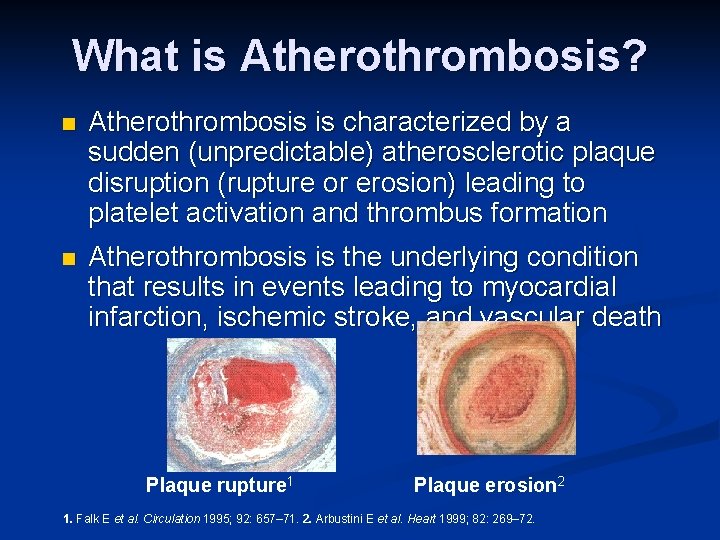
What is Atherothrombosis? n Atherothrombosis is characterized by a sudden (unpredictable) atherosclerotic plaque disruption (rupture or erosion) leading to platelet activation and thrombus formation n Atherothrombosis is the underlying condition that results in events leading to myocardial infarction, ischemic stroke, and vascular death Plaque rupture 1 Plaque erosion 2 1. Falk E et al. Circulation 1995; 92: 657– 71. 2. Arbustini E et al. Heart 1999; 82: 269– 72.
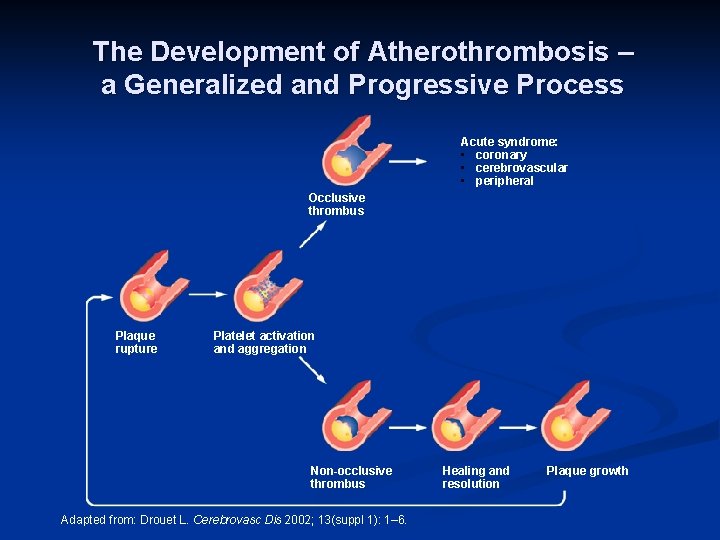
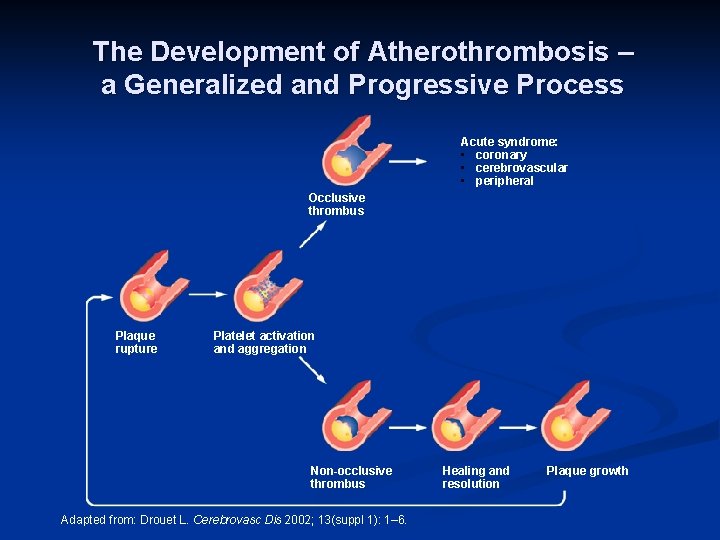
The Development of Atherothrombosis – a Generalized and Progressive Process Acute syndrome: • coronary • cerebrovascular • peripheral Occlusive thrombus Plaque rupture Platelet activation and aggregation Non-occlusive thrombus Adapted from: Drouet L. Cerebrovasc Dis 2002; 13(suppl 1): 1– 6. Healing and resolution Plaque growth
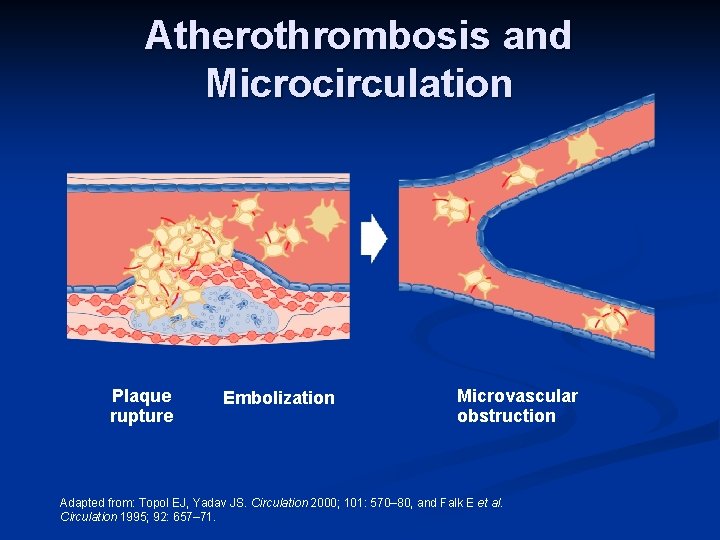
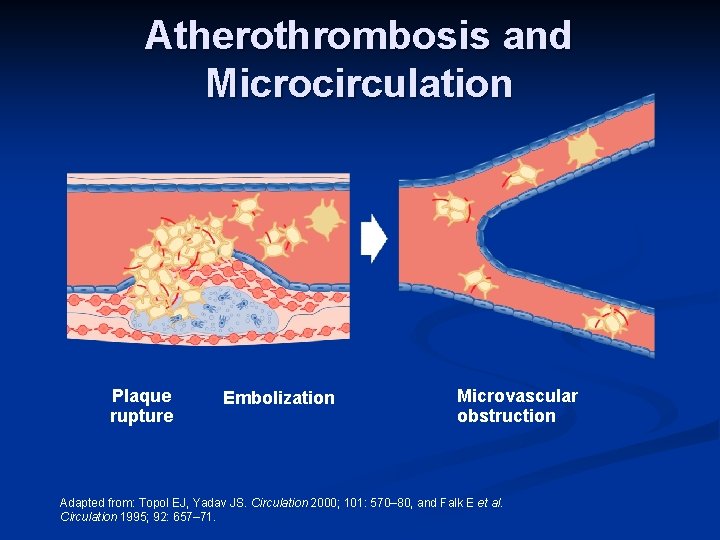
Atherothrombosis and Microcirculation Plaque rupture Embolization Microvascular obstruction Adapted from: Topol EJ, Yadav JS. Circulation 2000; 101: 570– 80, and Falk E et al. Circulation 1995; 92: 657– 71.
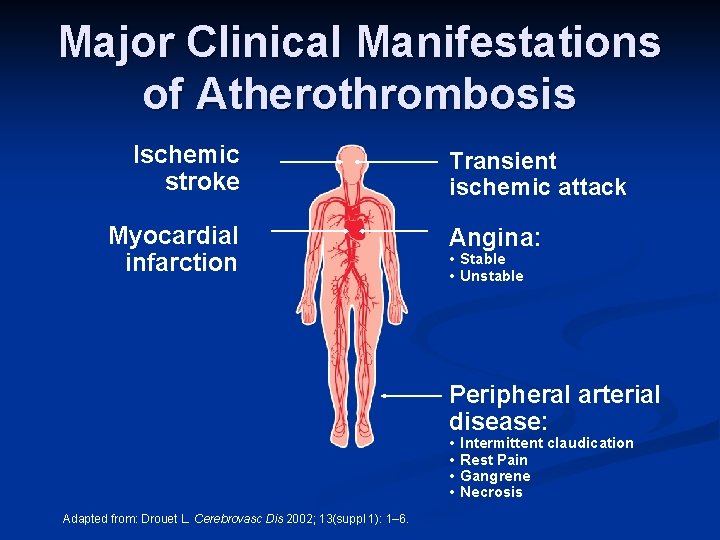
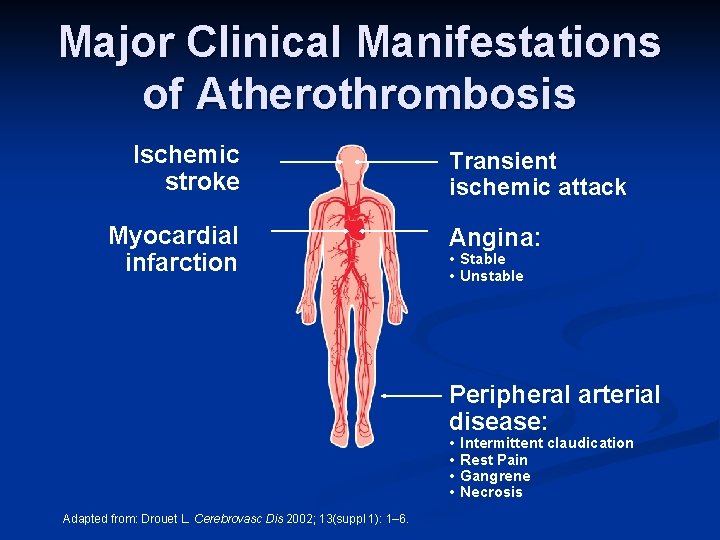
Major Clinical Manifestations of Atherothrombosis Ischemic stroke Myocardial infarction Transient ischemic attack Angina: • Stable • Unstable Peripheral arterial disease: • • Adapted from: Drouet L. Cerebrovasc Dis 2002; 13(suppl 1): 1– 6. Intermittent claudication Rest Pain Gangrene Necrosis
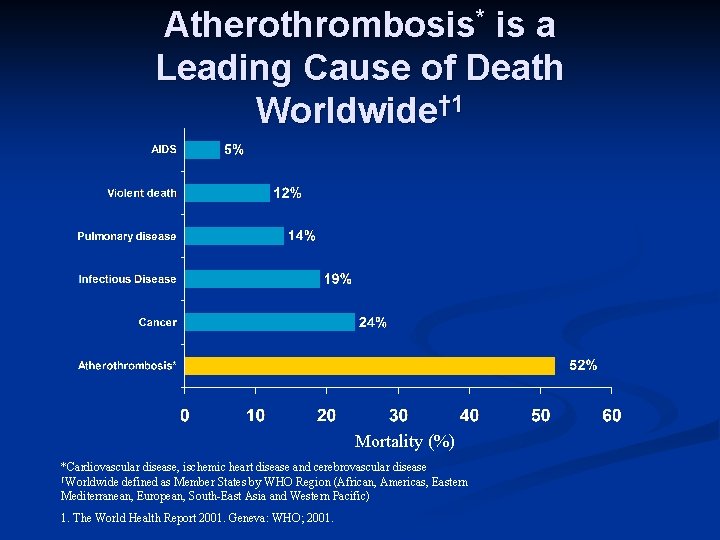
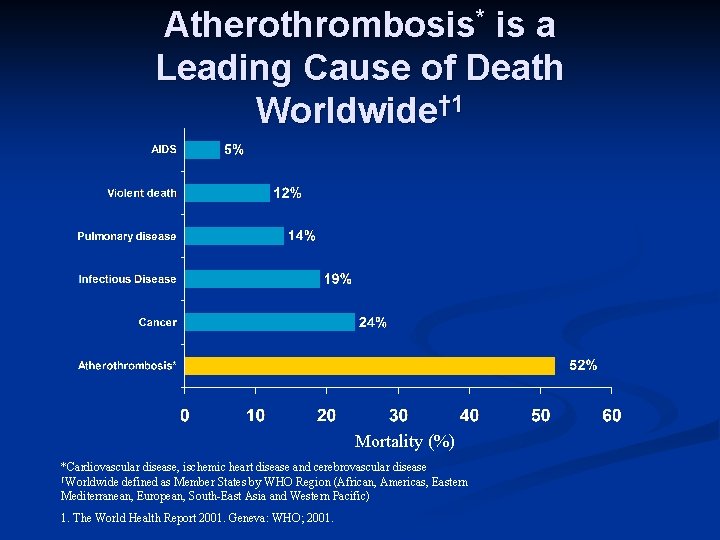
Atherothrombosis* is a Leading Cause of Death Worldwide† 1 Mortality (%) *Cardiovascular disease, ischemic heart disease and cerebrovascular disease †Worldwide defined as Member States by WHO Region (African, Americas, Eastern Mediterranean, European, South-East Asia and Western Pacific) 1. The World Health Report 2001. Geneva: WHO; 2001.
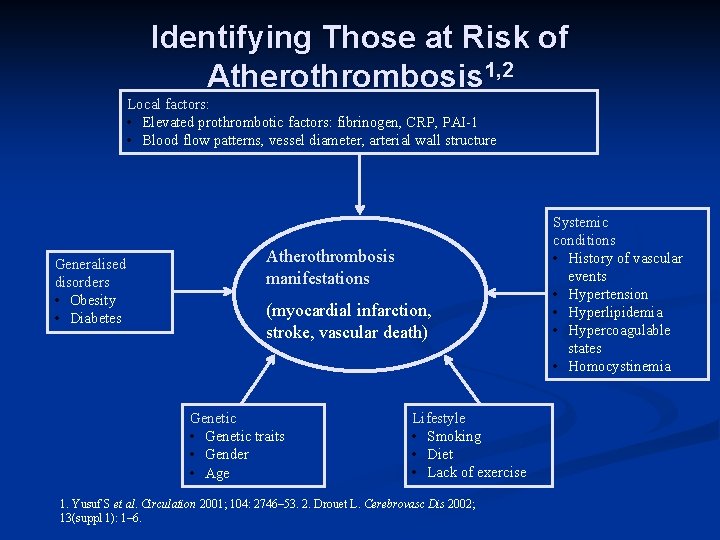
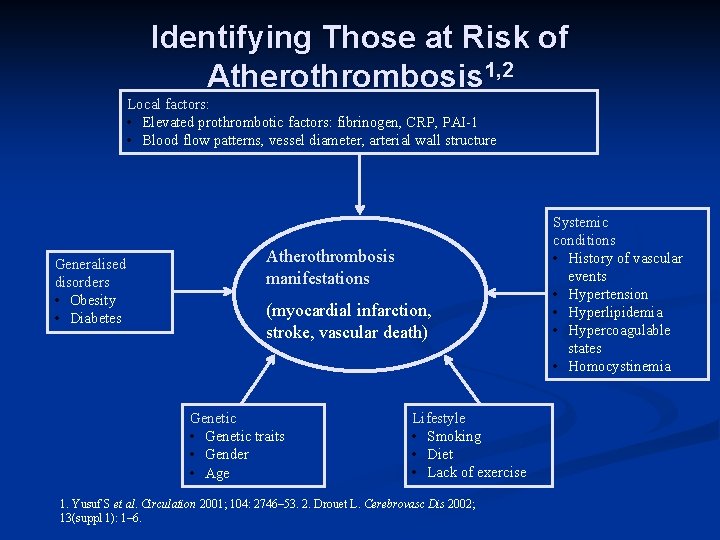
Identifying Those at Risk of Atherothrombosis 1, 2 Local factors: • Elevated prothrombotic factors: fibrinogen, CRP, PAI-1 • Blood flow patterns, vessel diameter, arterial wall structure Generalised disorders • Obesity • Diabetes Atherothrombosis manifestations (myocardial infarction, stroke, vascular death) Genetic • Genetic traits • Gender • Age Lifestyle • Smoking • Diet • Lack of exercise 1. Yusuf S et al. Circulation 2001; 104: 2746– 53. 2. Drouet L. Cerebrovasc Dis 2002; 13(suppl 1): 1– 6. Systemic conditions • History of vascular events • Hypertension • Hyperlipidemia • Hypercoagulable states • Homocystinemia
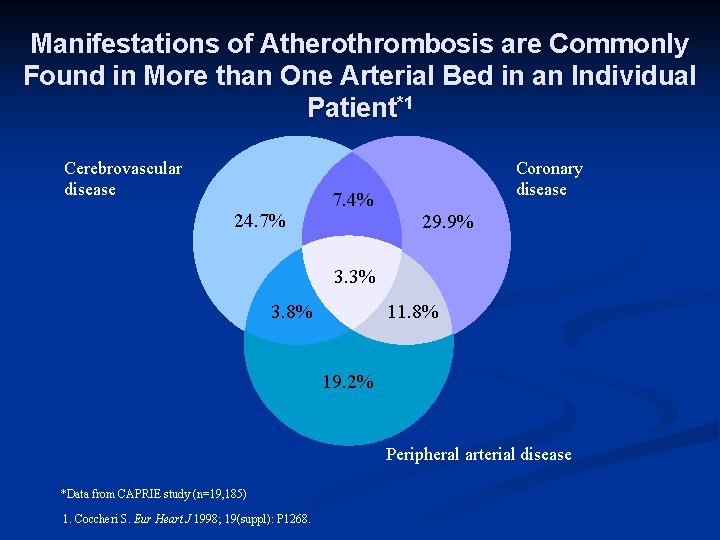
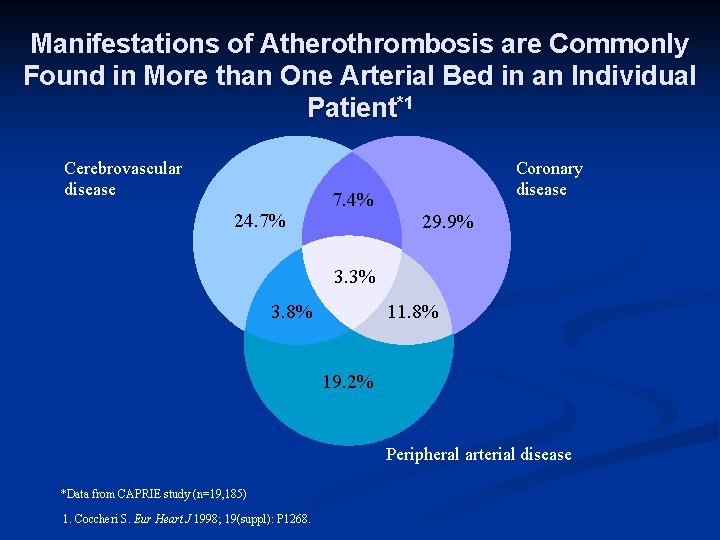
Manifestations of Atherothrombosis are Commonly Found in More than One Arterial Bed in an Individual Patient*1 Cerebrovascular disease 24. 7% 7. 4% Coronary disease 29. 9% 3. 3% 11. 8% 3. 8% 19. 2% Peripheral arterial disease *Data from CAPRIE study (n=19, 185) 1. Coccheri S. Eur Heart J 1998; 19(suppl): P 1268.
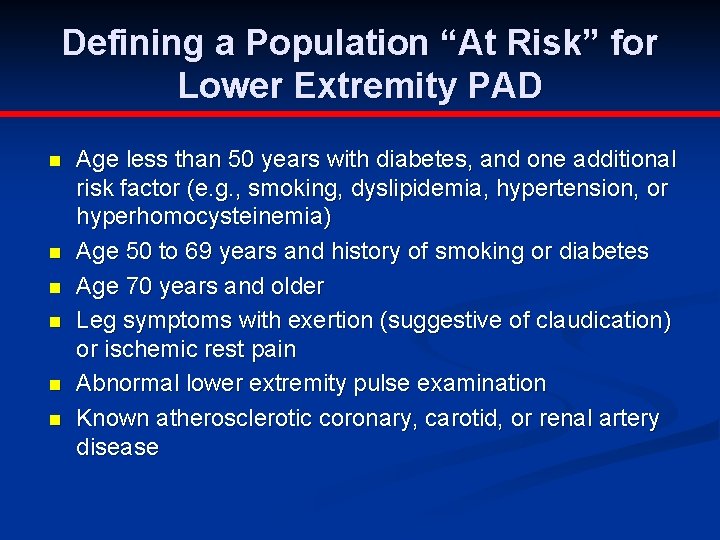
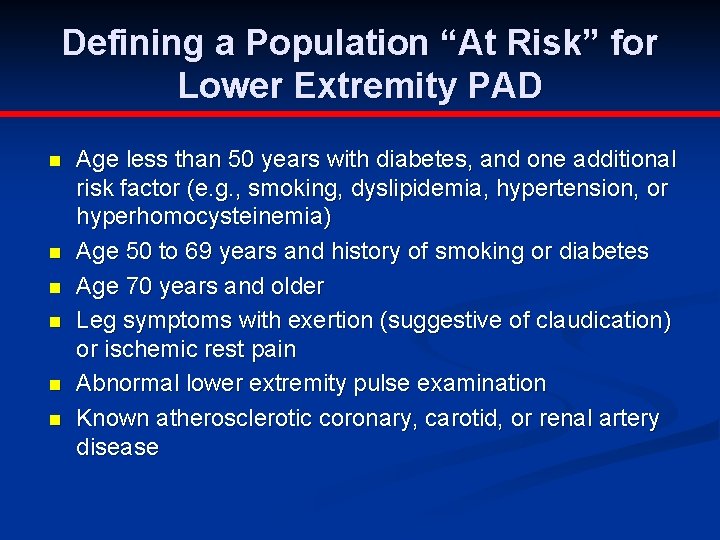
Defining a Population “At Risk” for Lower Extremity PAD n n n Age less than 50 years with diabetes, and one additional risk factor (e. g. , smoking, dyslipidemia, hypertension, or hyperhomocysteinemia) Age 50 to 69 years and history of smoking or diabetes Age 70 years and older Leg symptoms with exertion (suggestive of claudication) or ischemic rest pain Abnormal lower extremity pulse examination Known atherosclerotic coronary, carotid, or renal artery disease
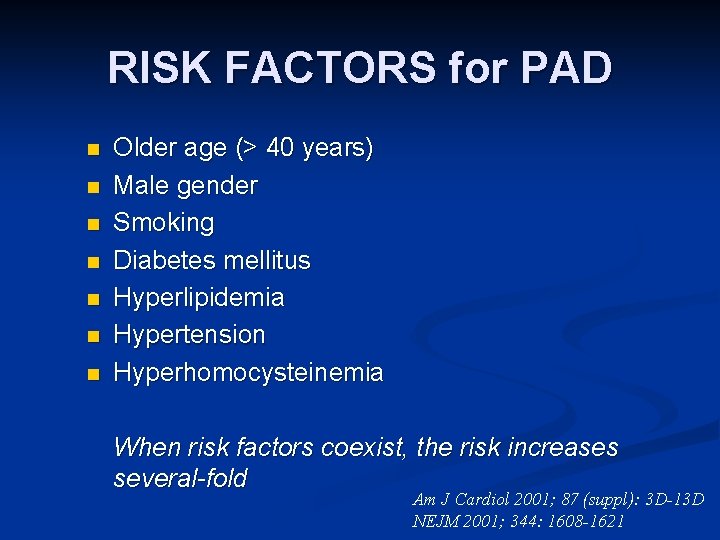
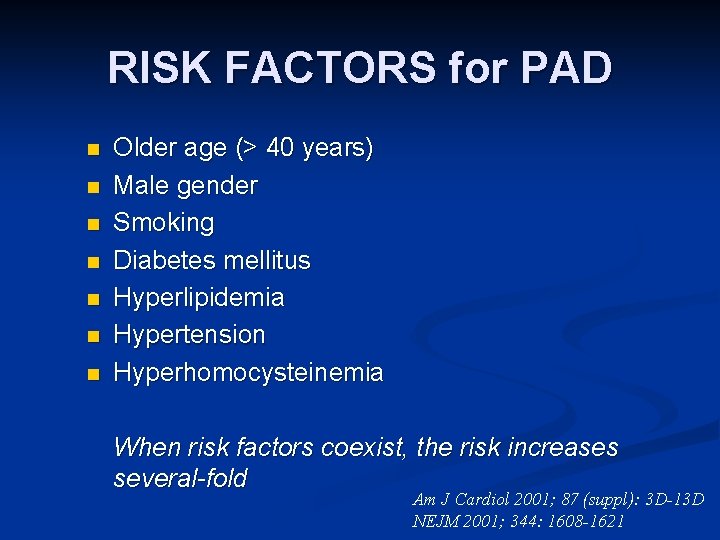
RISK FACTORS for PAD n n n n Older age (> 40 years) Male gender Smoking Diabetes mellitus Hyperlipidemia Hypertension Hyperhomocysteinemia When risk factors coexist, the risk increases several-fold Am J Cardiol 2001; 87 (suppl): 3 D-13 D NEJM 2001; 344: 1608 -1621

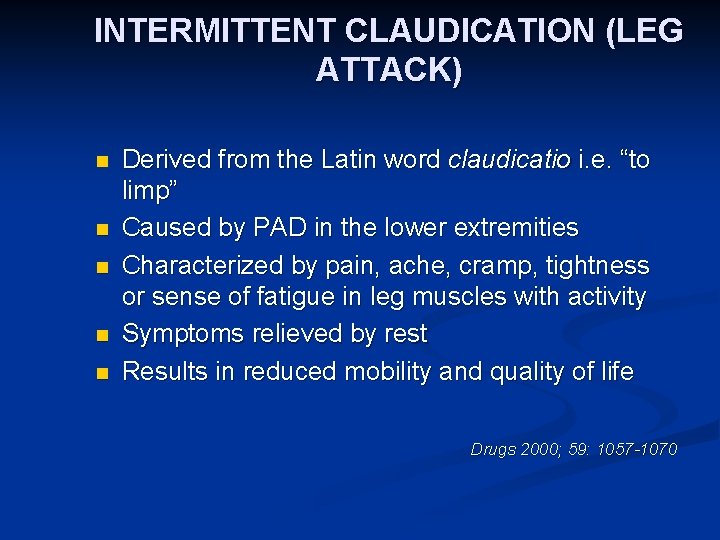
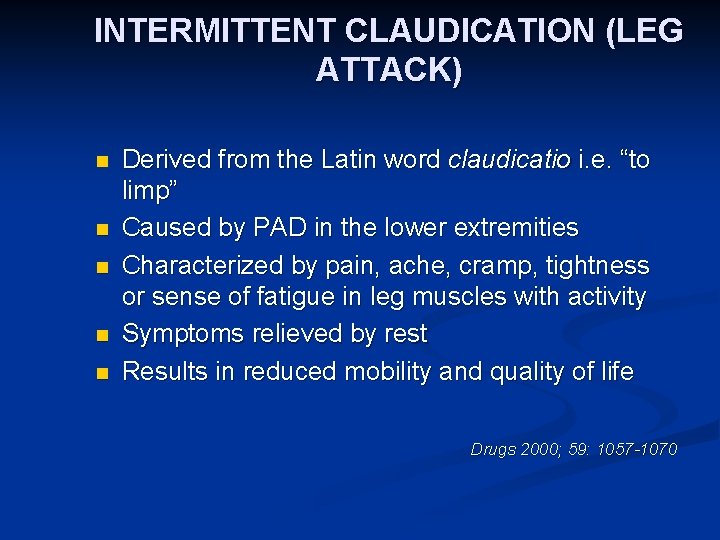
INTERMITTENT CLAUDICATION (LEG ATTACK) n n n Derived from the Latin word claudicatio i. e. “to limp” Caused by PAD in the lower extremities Characterized by pain, ache, cramp, tightness or sense of fatigue in leg muscles with activity Symptoms relieved by rest Results in reduced mobility and quality of life Drugs 2000; 59: 1057 -1070
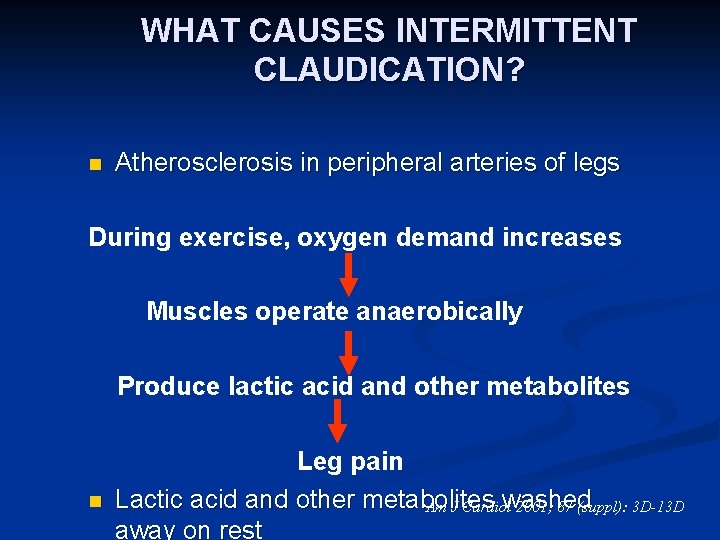
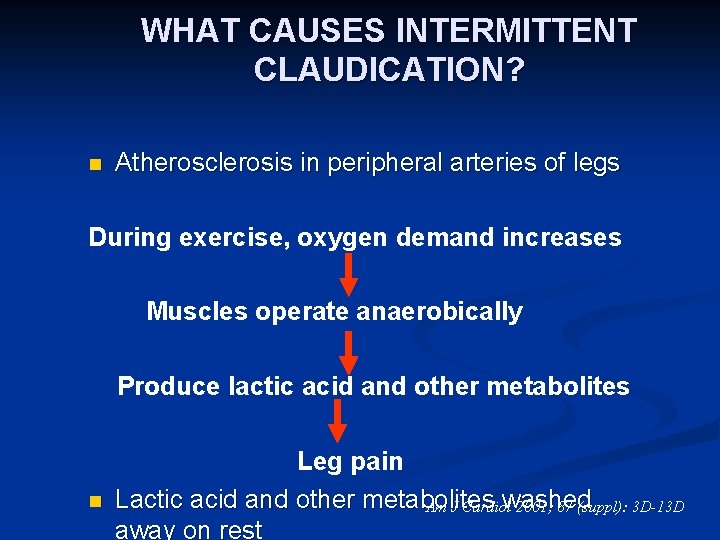
WHAT CAUSES INTERMITTENT CLAUDICATION? n Atherosclerosis in peripheral arteries of legs During exercise, oxygen demand increases Muscles operate anaerobically Produce lactic acid and other metabolites n Leg pain Lactic acid and other metabolites washed Am J Cardiol 2001; 87 (suppl): 3 D-13 D away on rest
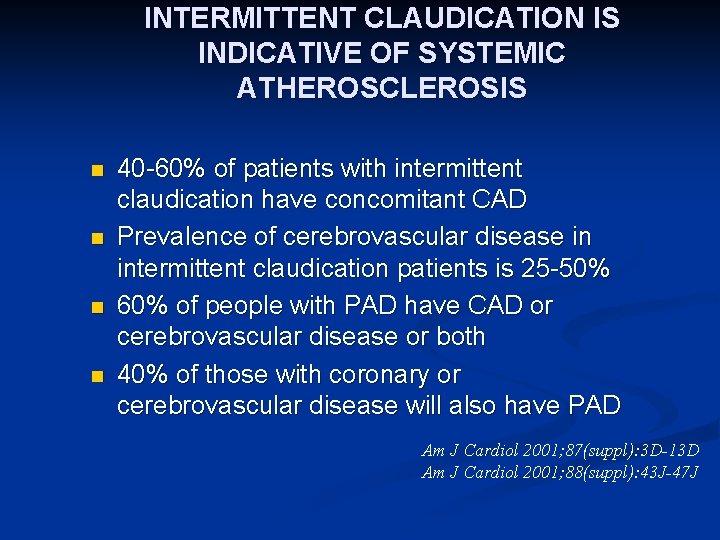
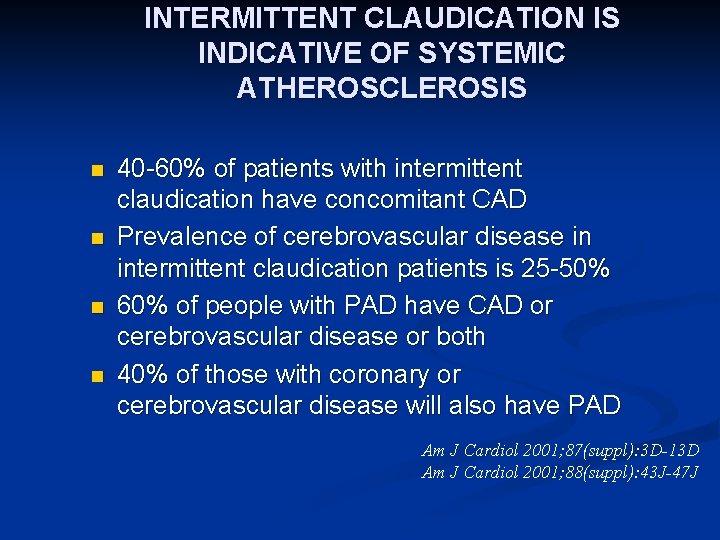
INTERMITTENT CLAUDICATION IS INDICATIVE OF SYSTEMIC ATHEROSCLEROSIS n n 40 -60% of patients with intermittent claudication have concomitant CAD Prevalence of cerebrovascular disease in intermittent claudication patients is 25 -50% 60% of people with PAD have CAD or cerebrovascular disease or both 40% of those with coronary or cerebrovascular disease will also have PAD Am J Cardiol 2001; 87(suppl): 3 D-13 D Am J Cardiol 2001; 88(suppl): 43 J-47 J


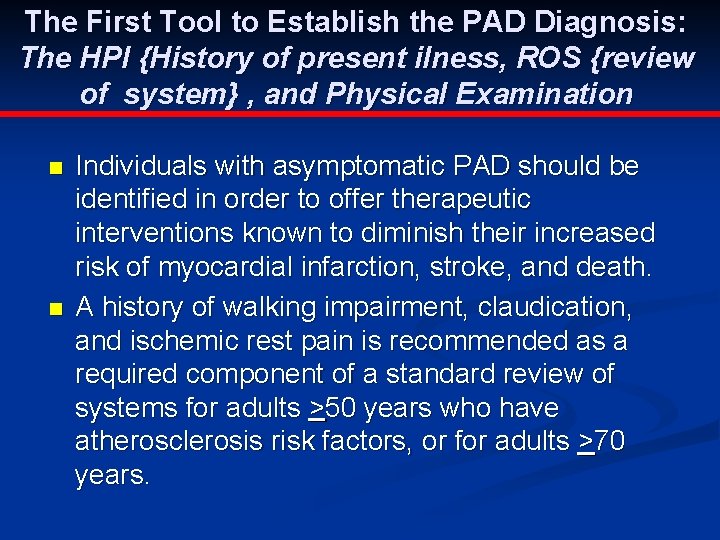
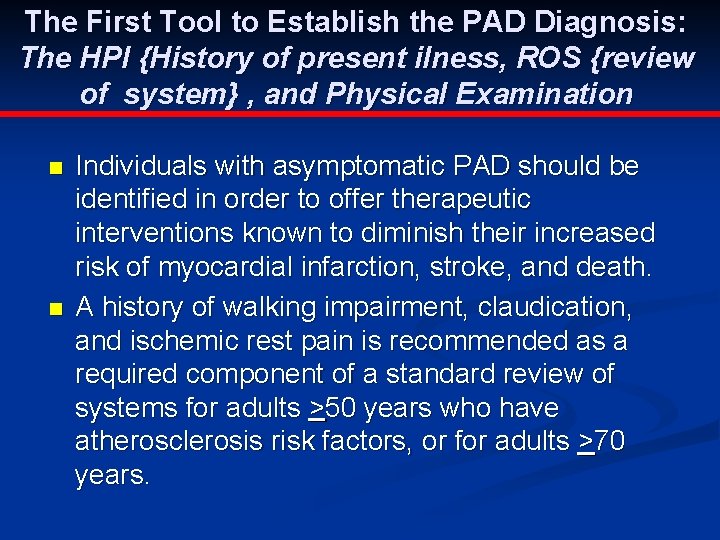
The First Tool to Establish the PAD Diagnosis: The HPI {History of present ilness, ROS {review of system} , and Physical Examination n n Individuals with asymptomatic PAD should be identified in order to offer therapeutic interventions known to diminish their increased risk of myocardial infarction, stroke, and death. A history of walking impairment, claudication, and ischemic rest pain is recommended as a required component of a standard review of systems for adults >50 years who have atherosclerosis risk factors, or for adults >70 years.
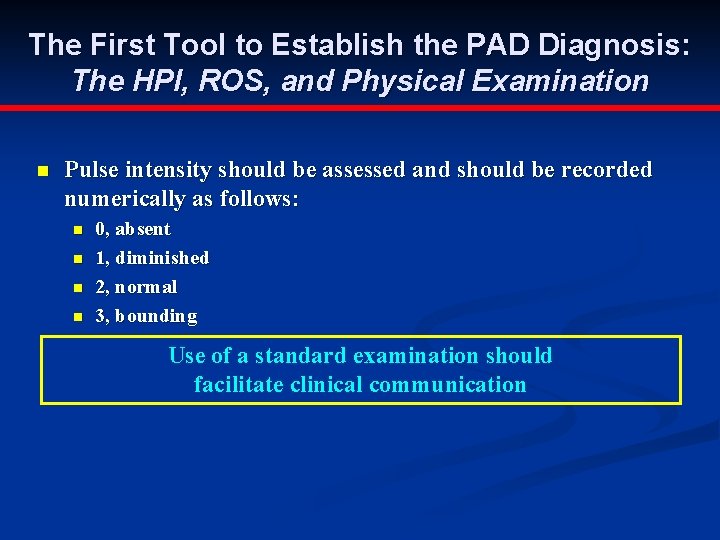
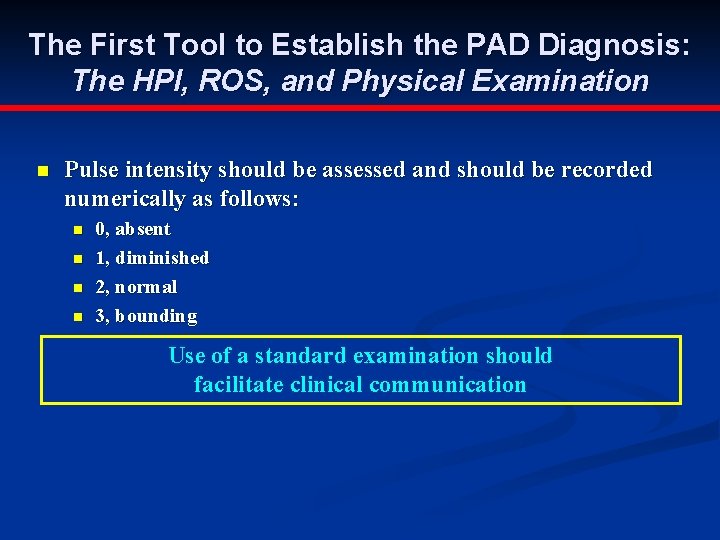
The First Tool to Establish the PAD Diagnosis: The HPI, ROS, and Physical Examination n Pulse intensity should be assessed and should be recorded numerically as follows: n n 0, absent 1, diminished 2, normal 3, bounding Use of a standard examination should facilitate clinical communication
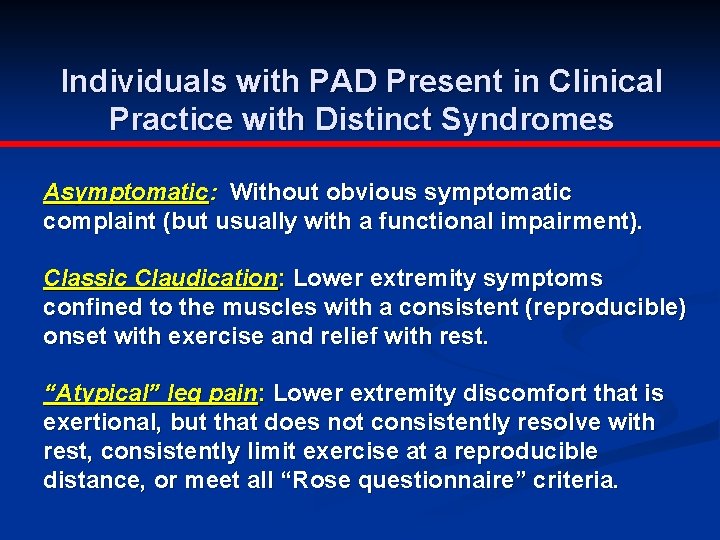
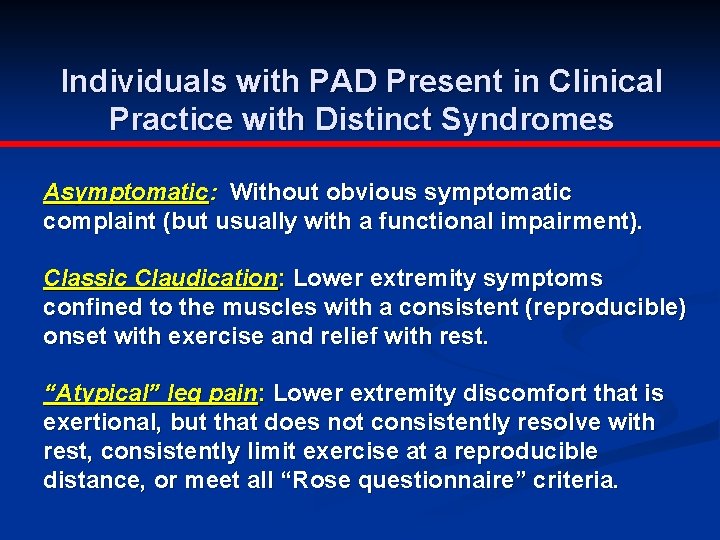
Individuals with PAD Present in Clinical Practice with Distinct Syndromes Asymptomatic: Without obvious symptomatic complaint (but usually with a functional impairment). Classic Claudication: Lower extremity symptoms confined to the muscles with a consistent (reproducible) onset with exercise and relief with rest. “Atypical” leg pain: Lower extremity discomfort that is exertional, but that does not consistently resolve with rest, consistently limit exercise at a reproducible distance, or meet all “Rose questionnaire” criteria.
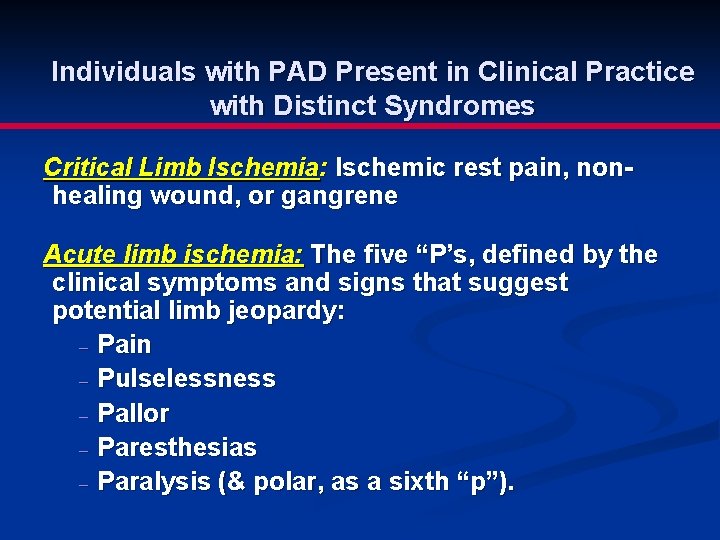
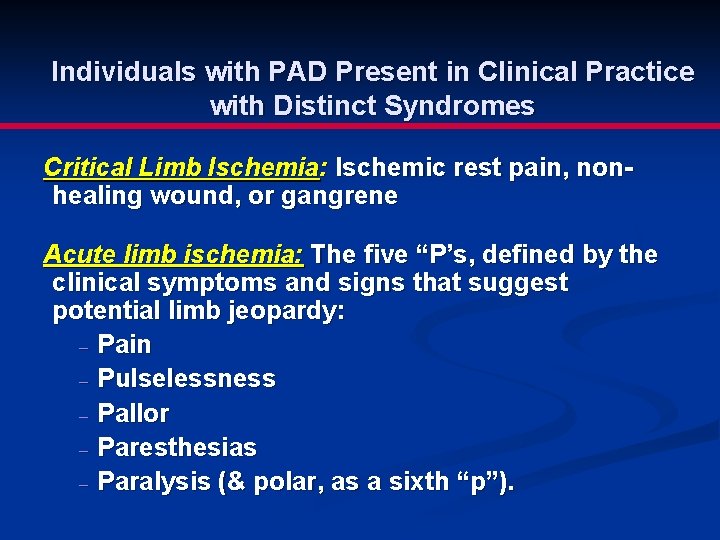
Individuals with PAD Present in Clinical Practice with Distinct Syndromes Critical Limb Ischemia: Ischemic rest pain, nonhealing wound, or gangrene Acute limb ischemia: The five “P’s, defined by the clinical symptoms and signs that suggest potential limb jeopardy: - Pain - Pulselessness - Pallor - Paresthesias - Paralysis (& polar, as a sixth “p”).

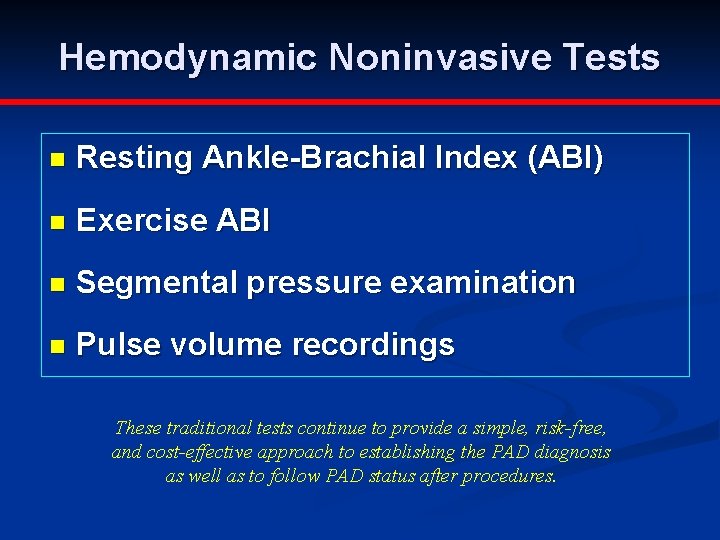
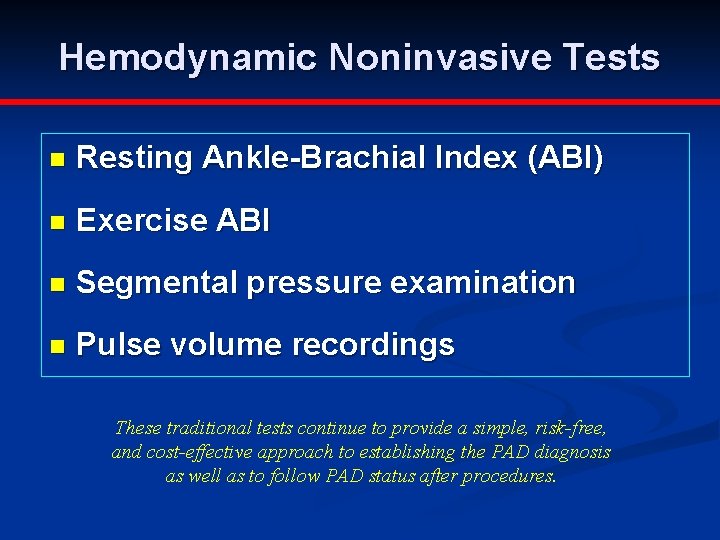
Hemodynamic Noninvasive Tests n Resting Ankle-Brachial Index (ABI) n Exercise ABI n Segmental pressure examination n Pulse volume recordings These traditional tests continue to provide a simple, risk-free, and cost-effective approach to establishing the PAD diagnosis as well as to follow PAD status after procedures.
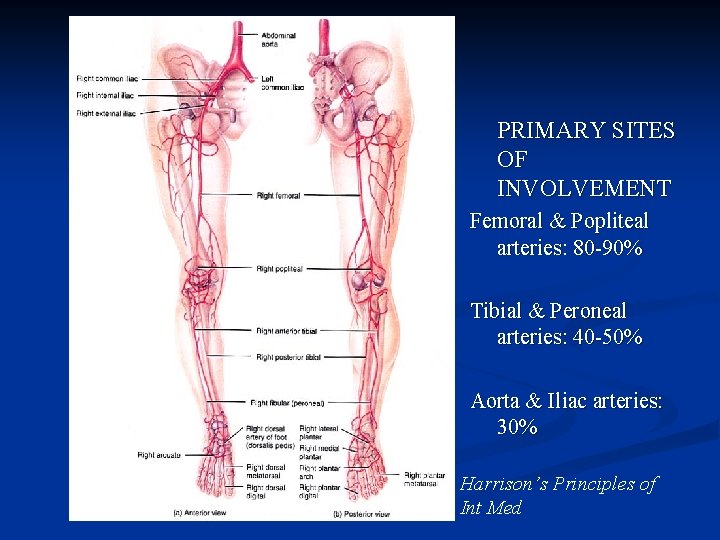
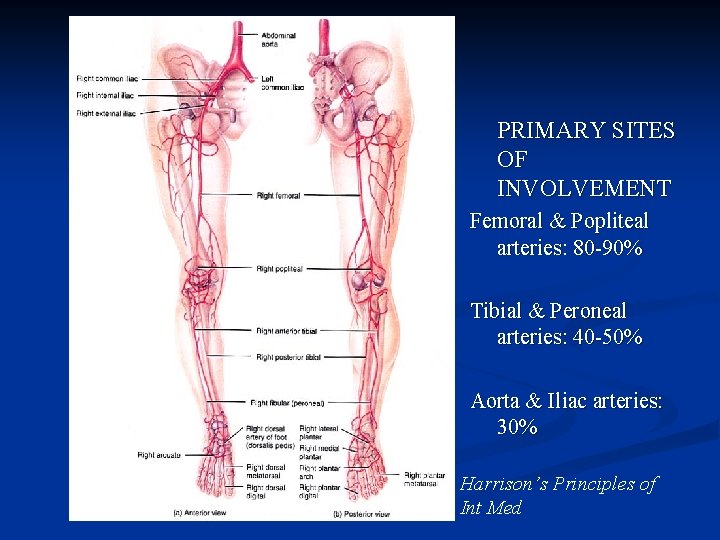
PRIMARY SITES OF INVOLVEMENT Femoral & Popliteal arteries: 80 -90% Tibial & Peroneal arteries: 40 -50% Aorta & Iliac arteries: 30% Harrison’s Principles of Int Med
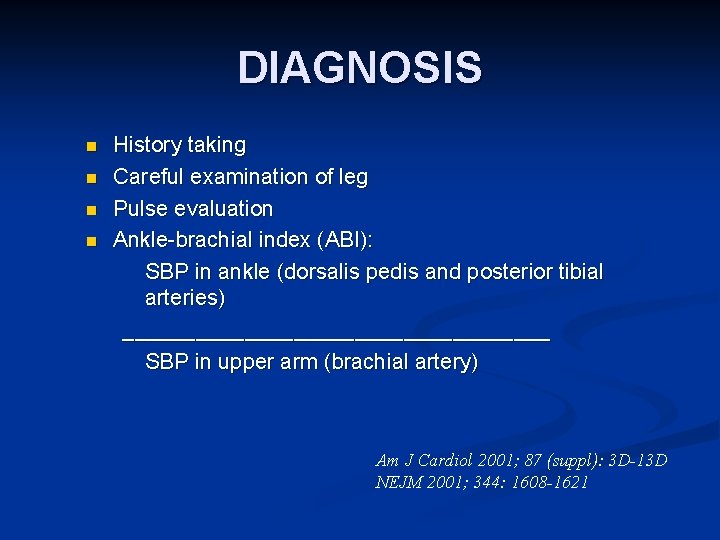
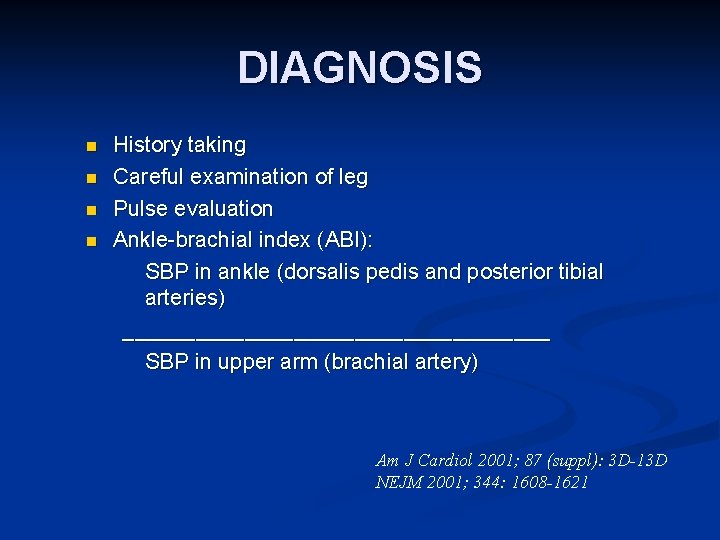
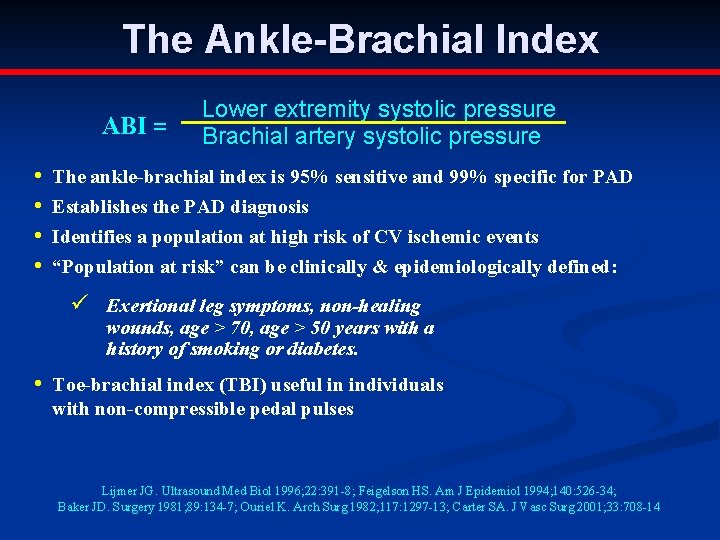
DIAGNOSIS n n History taking Careful examination of leg Pulse evaluation Ankle-brachial index (ABI): SBP in ankle (dorsalis pedis and posterior tibial arteries) __________________ SBP in upper arm (brachial artery) Am J Cardiol 2001; 87 (suppl): 3 D-13 D NEJM 2001; 344: 1608 -1621

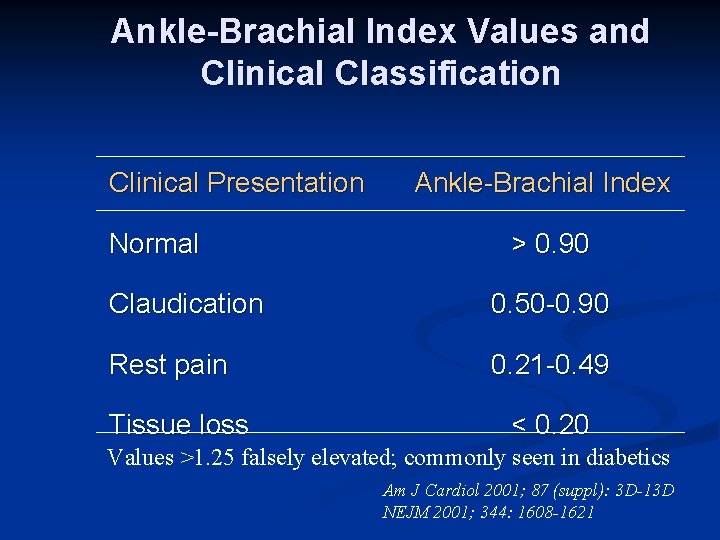
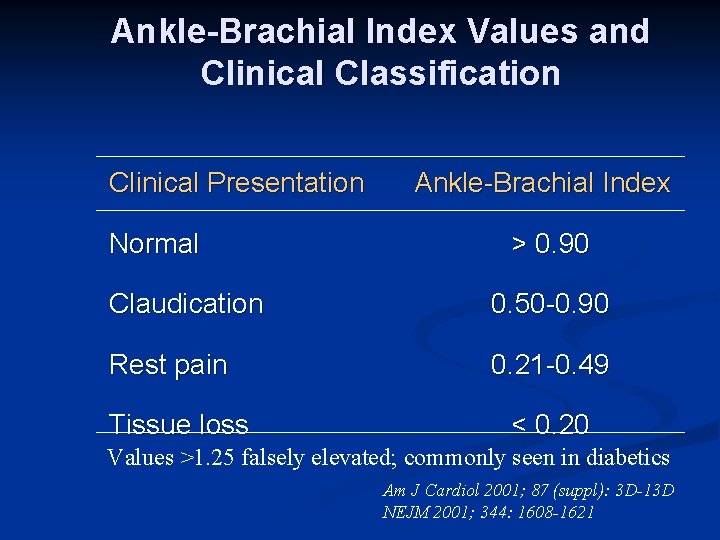
Ankle-Brachial Index Values and Clinical Classification Clinical Presentation Normal Ankle-Brachial Index > 0. 90 Claudication 0. 50 -0. 90 Rest pain 0. 21 -0. 49 Tissue loss < 0. 20 Values >1. 25 falsely elevated; commonly seen in diabetics Am J Cardiol 2001; 87 (suppl): 3 D-13 D NEJM 2001; 344: 1608 -1621
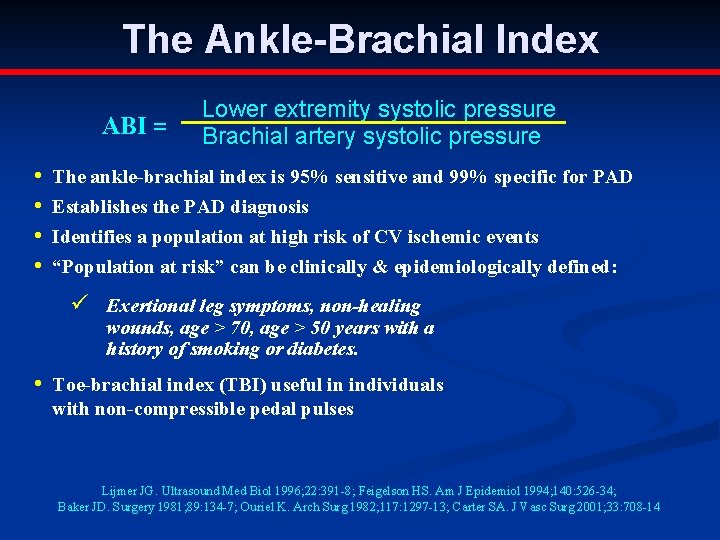
The Ankle-Brachial Index ABI = • • Lower extremity systolic pressure Brachial artery systolic pressure The ankle-brachial index is 95% sensitive and 99% specific for PAD Establishes the PAD diagnosis Identifies a population at high risk of CV ischemic events “Population at risk” can be clinically & epidemiologically defined: ü Exertional leg symptoms, non-healing wounds, age > 70, age > 50 years with a history of smoking or diabetes. • Toe-brachial index (TBI) useful in individuals with non-compressible pedal pulses Lijmer JG. Ultrasound Med Biol 1996; 22: 391 -8; Feigelson HS. Am J Epidemiol 1994; 140: 526 -34; Baker JD. Surgery 1981; 89: 134 -7; Ouriel K. Arch Surg 1982; 117: 1297 -13; Carter SA. J Vasc Surg 2001; 33: 708 -14
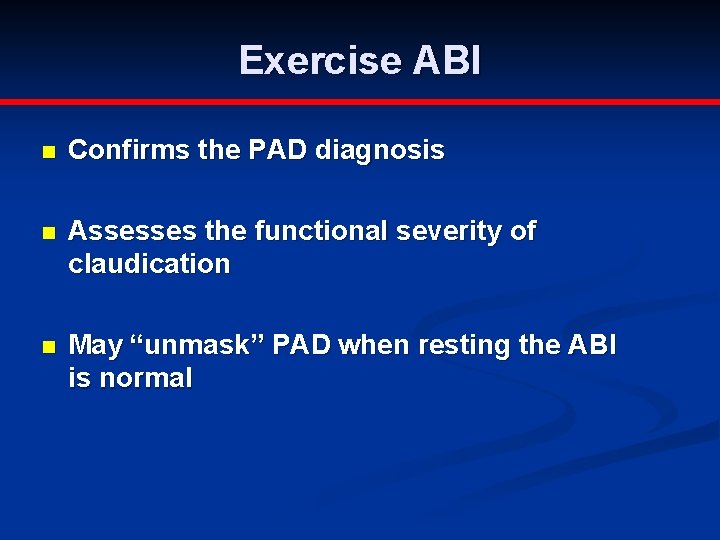
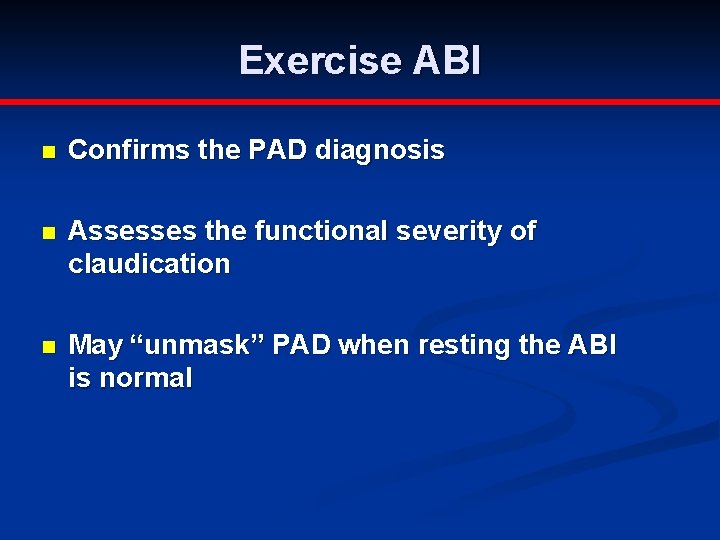
Exercise ABI n Confirms the PAD diagnosis n Assesses the functional severity of claudication n May “unmask” PAD when resting the ABI is normal
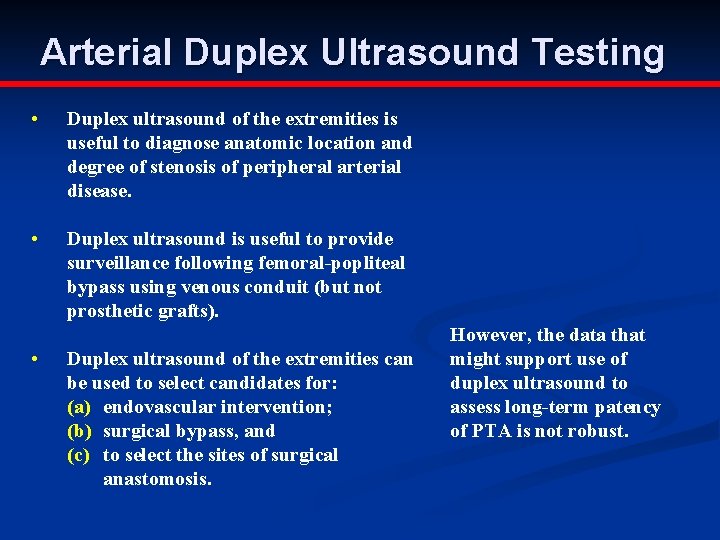
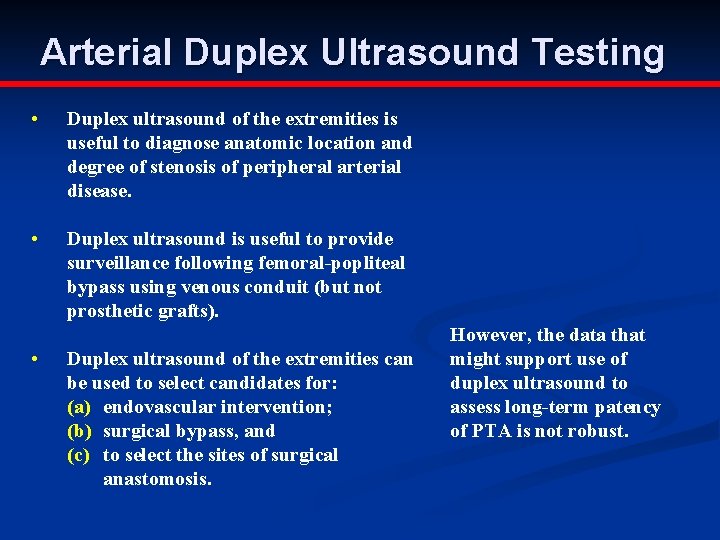
Arterial Duplex Ultrasound Testing • Duplex ultrasound of the extremities is useful to diagnose anatomic location and degree of stenosis of peripheral arterial disease. • Duplex ultrasound is useful to provide surveillance following femoral-popliteal bypass using venous conduit (but not prosthetic grafts). • Duplex ultrasound of the extremities can be used to select candidates for: (a) endovascular intervention; (b) surgical bypass, and (c) to select the sites of surgical anastomosis. However, the data that might support use of duplex ultrasound to assess long-term patency of PTA is not robust.
Noninvasive Imaging Tests Duplex Ultrasound Duplex ultrasound of the extremities is useful to diagnose the anatomic location and degree of stenosis of PAD. Duplex ultrasound is recommended for routine surveillance after femoral-popliteal or femoraltibial-pedal bypass with a venous conduit. minimum surveillance intervals are approximately 3, 6, and 12 months, and then yearly after graft placement.
Noninvasive Imaging Tests Magnetic Resonance Angiography (MRA) MRA of the extremities is useful to diagnose anatomic location and degree of stenosis of PAD. MRA of the extremities should be performed with a gadolinium enhancement. MRA of the extremities is useful in selecting patients with lower extremity PAD as candidates for endovascular intervention.
Noninvasive Imaging Tests Computed Tomographic Angiography (CTA) CTA of the extremities may be considered to diagnose anatomic location and presence of significant stenosis in patients with lower extremity PAD. CTA of the extremities may be considered as a substitute for MRA for those patients with contraindications to MRA.



The history and physical examination (pulse evaluation and careful examination of the leg) are usually sufficient to establish the diagnosis
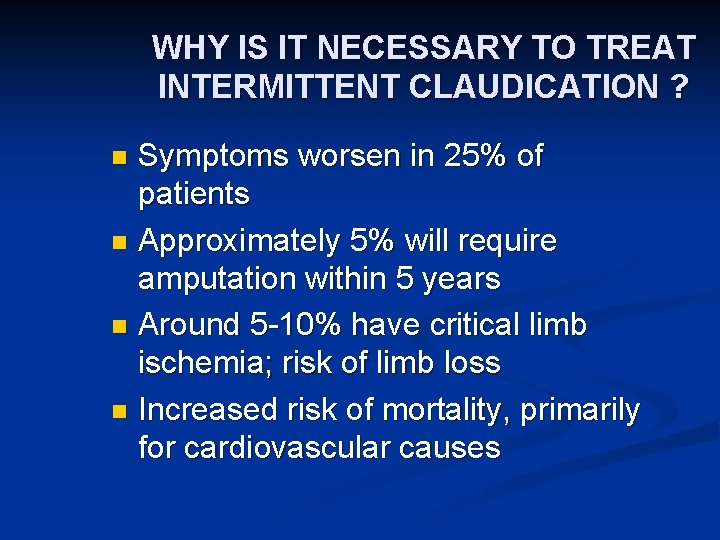
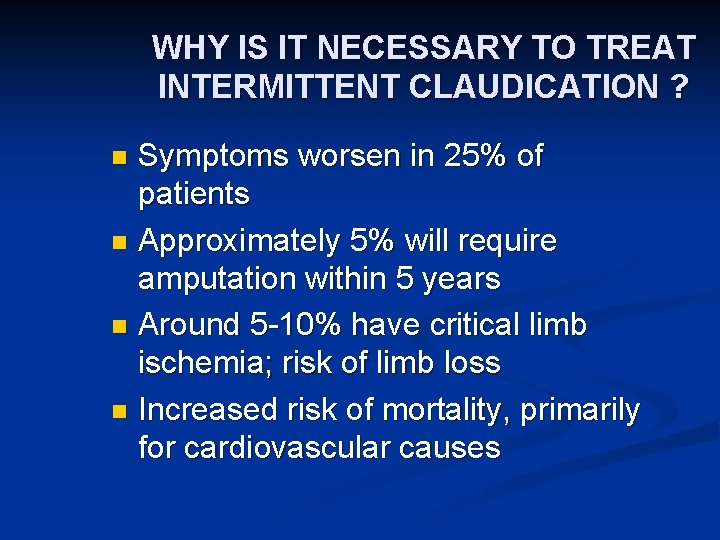
WHY IS IT NECESSARY TO TREAT INTERMITTENT CLAUDICATION ? Symptoms worsen in 25% of patients n Approximately 5% will require amputation within 5 years n Around 5 -10% have critical limb ischemia; risk of limb loss n Increased risk of mortality, primarily for cardiovascular causes n
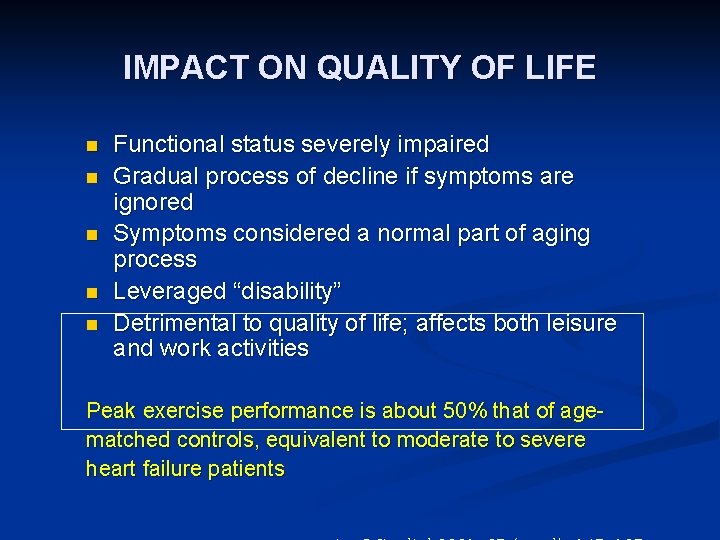
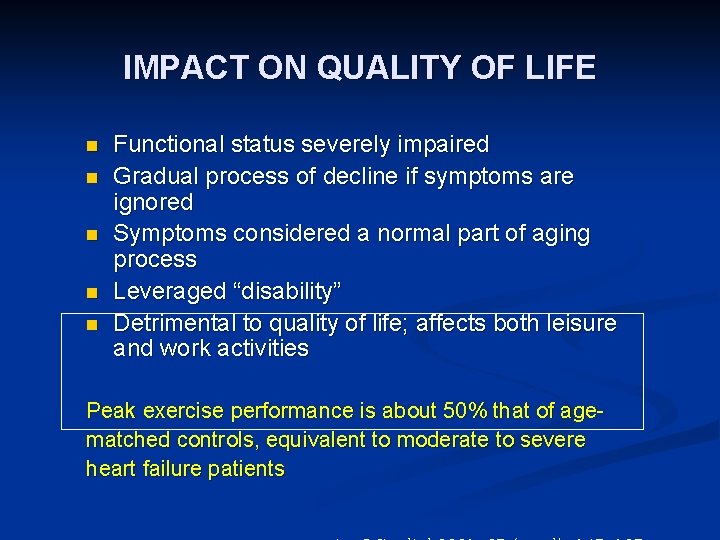
IMPACT ON QUALITY OF LIFE n n n Functional status severely impaired Gradual process of decline if symptoms are ignored Symptoms considered a normal part of aging process Leveraged “disability” Detrimental to quality of life; affects both leisure and work activities Peak exercise performance is about 50% that of agematched controls, equivalent to moderate to severe heart failure patients
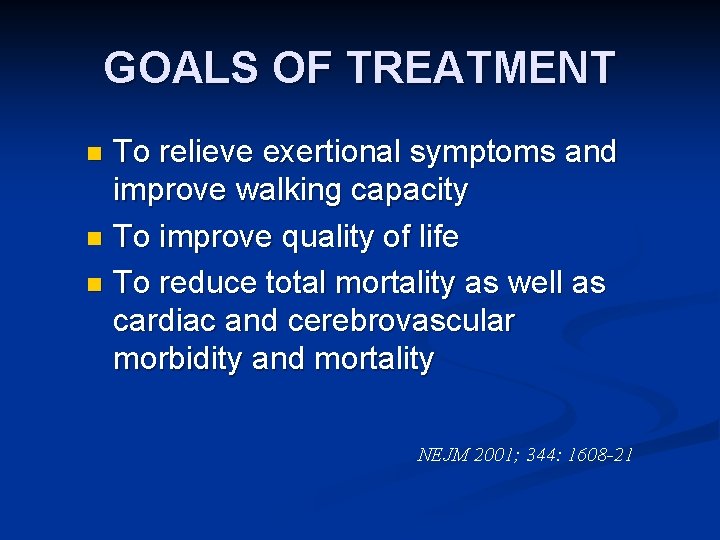
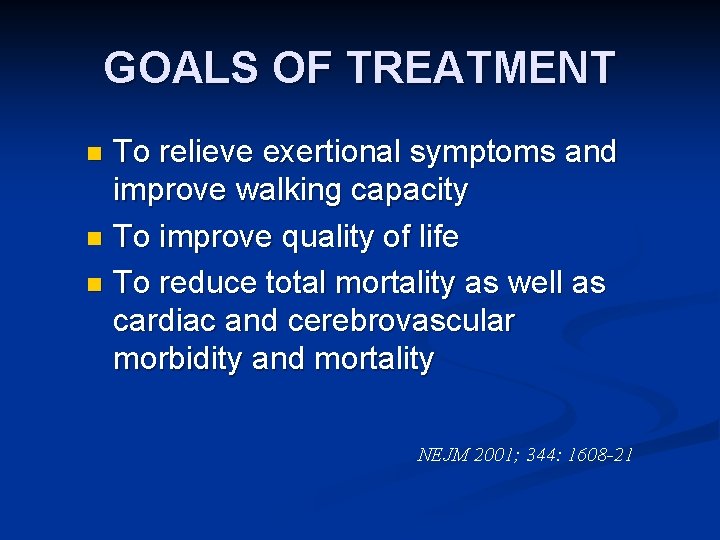
GOALS OF TREATMENT To relieve exertional symptoms and improve walking capacity n To improve quality of life n To reduce total mortality as well as cardiac and cerebrovascular morbidity and mortality n NEJM 2001; 344: 1608 -21
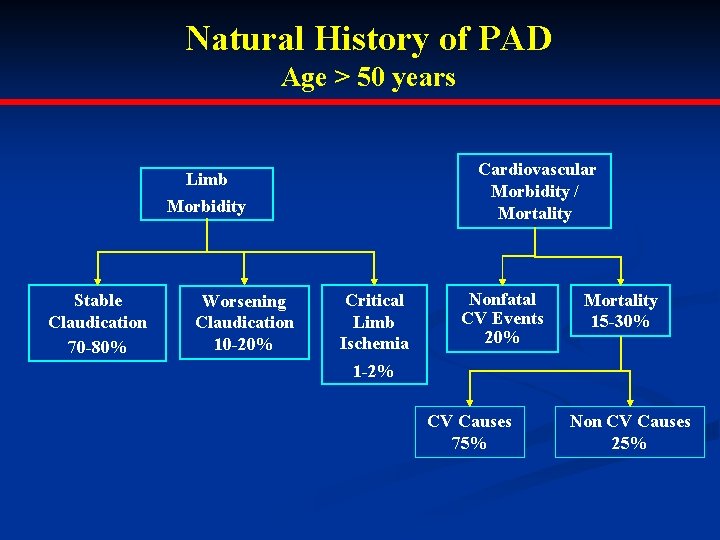
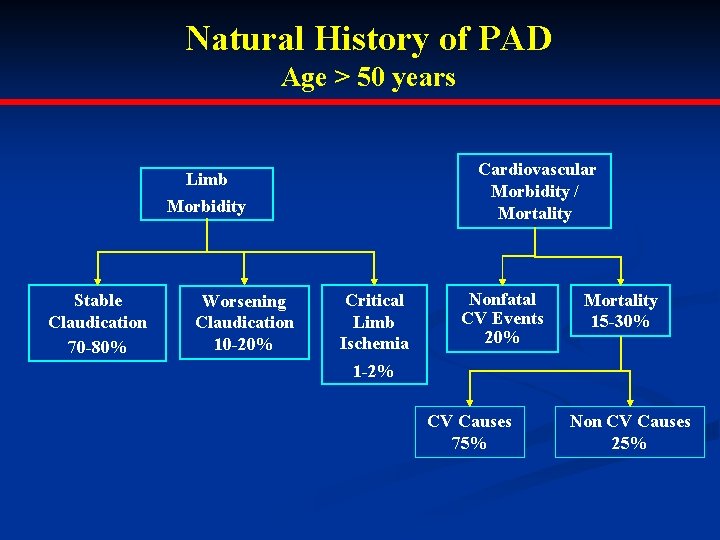
Natural History of PAD Age > 50 years Cardiovascular Morbidity / Mortality Limb Morbidity Stable Claudication 70 -80% Worsening Claudication 10 -20% Critical Limb Ischemia Nonfatal CV Events 20% Mortality 15 -30% 1 -2% CV Causes 75% Non CV Causes 25%
MANAGEMENT Risk factor modification n Exercise therapy n Antiplatelet therapy n Medical therapy targeted at symptoms n Revascularisation procedures n
Lipid Lowering and Antihypertensive Therapy Treatment with an HMG coenzyme-A reductase inhibitor (statin) medication is indicated for all patients with peripheral arterial disease to achieve a target LDL cholesterol of less than 100 mg/dl. Antihypertensive therapy should be administered to hypertensive patients with lower extremity PAD to a goal of less than 140/90 mm. Hg (non-diabetics) or less than 130/80 mm/Hg (diabetics and individuals with chronic renal disease) to reduce the risk of myocardial infarction, stroke, congestive heart failure, and cardiovascular death.
Antiplatelet Therapy Antiplatelet therapy is indicated to reduce the risk of myocardial infarction, stroke, or vascular death in individuals with atherosclerotic lower extremity PAD. Aspirin, in daily doses of 75 to 325 mg, is recommended as safe and effective antiplatelet therapy to reduce the risk of myocardial infarction, stroke, or vascular death in individuals with atherosclerotic lower extremity PAD. Clopidogrel (75 mg per day) is recommended as an effective alternative antiplatelet therapy to aspirin to reduce the risk of myocardial infarction, stroke, or vascular death in individuals with atherosclerotic lower extremity PAD.
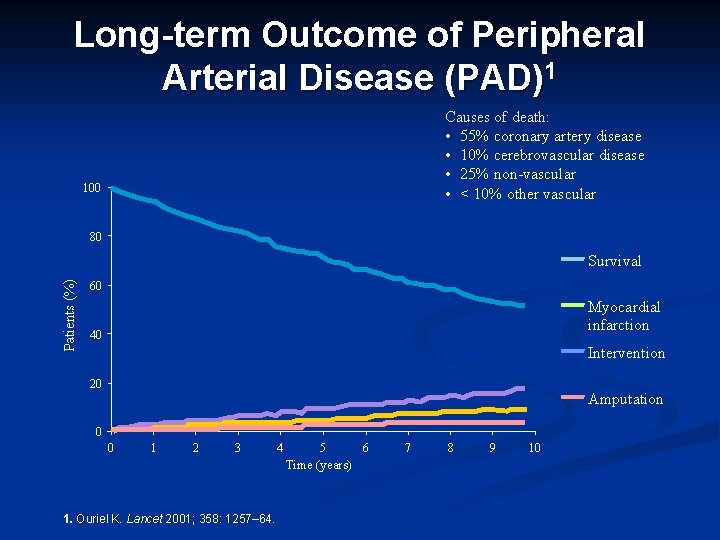
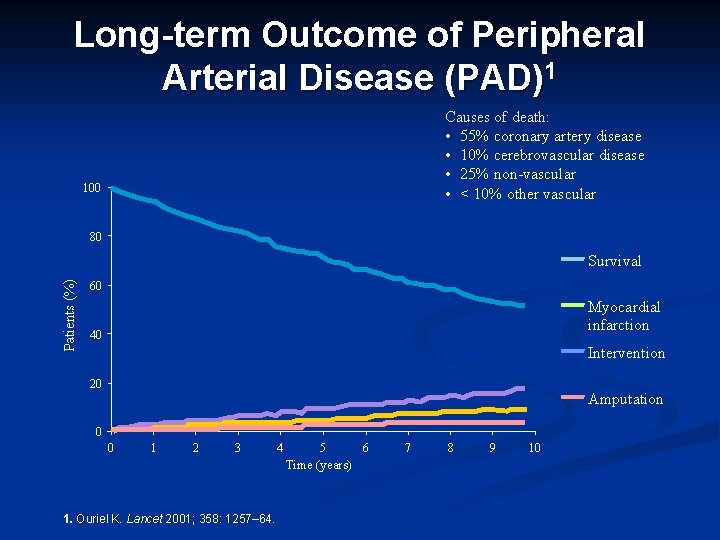
Long-term Outcome of Peripheral Arterial Disease (PAD)1 Causes of death: • 55% coronary artery disease • 10% cerebrovascular disease • 25% non-vascular • < 10% other vascular 100 80 Patients (%) Survival 60 Myocardial infarction 40 Intervention 20 Amputation 0 0 1 2 3 4 5 Time (years) 1. Ouriel K. Lancet 2001; 358: 1257– 64. 6 7 8 9 10
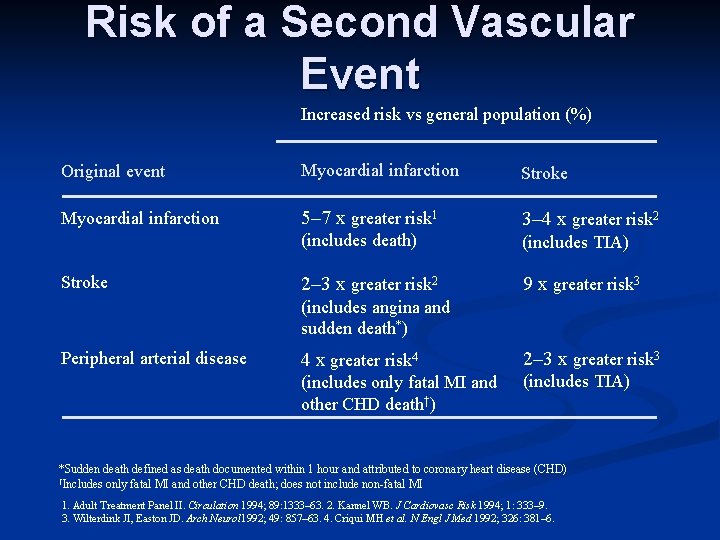
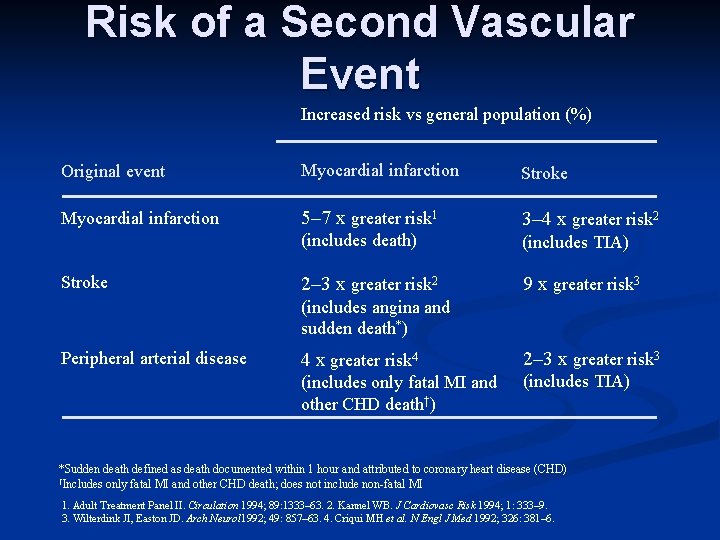
Risk of a Second Vascular Event Increased risk vs general population (%) Original event Myocardial infarction Stroke Myocardial infarction 5– 7 x greater risk 1 3– 4 x greater risk 2 (includes death) (includes TIA) 2– 3 x greater risk 2 9 x greater risk 3 Stroke (includes angina and sudden death*) Peripheral arterial disease 4 x greater risk 4 2– 3 x greater risk 3 (includes only fatal MI and other CHD death†) (includes TIA) *Sudden death defined as death documented within 1 hour and attributed to coronary heart disease (CHD) †Includes only fatal MI and other CHD death; does not include non-fatal MI 1. Adult Treatment Panel II. Circulation 1994; 89: 1333– 63. 2. Kannel WB. J Cardiovasc Risk 1994; 1: 333– 9. 3. Wilterdink JI, Easton JD. Arch Neurol 1992; 49: 857– 63. 4. Criqui MH et al. N Engl J Med 1992; 326: 381– 6.

Acute Limb Ischemia Definition, Etiology & Patophysiology Management
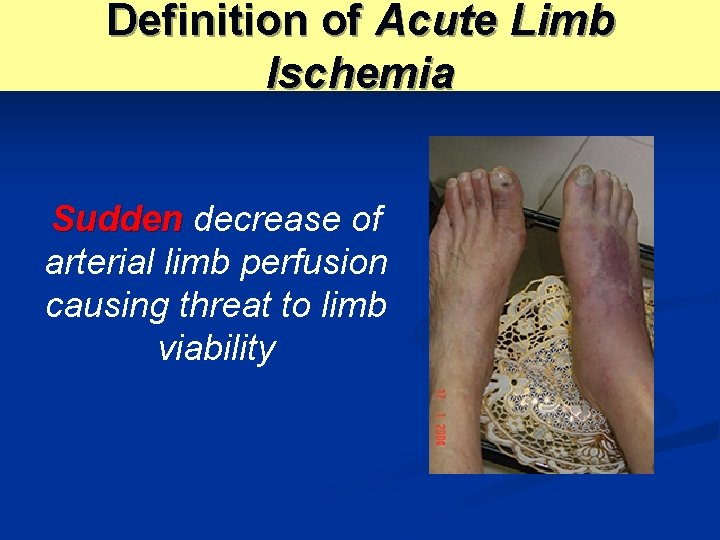
Definition of Acute Limb Ischemia Sudden decrease of arterial limb perfusion causing threat to limb viability
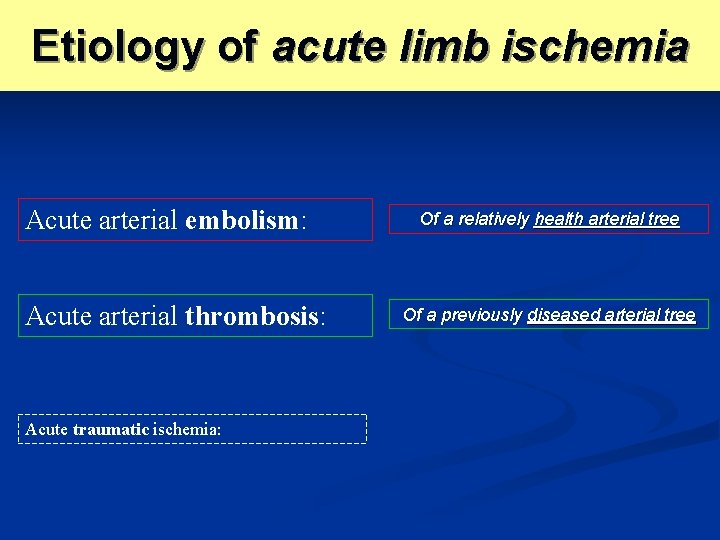
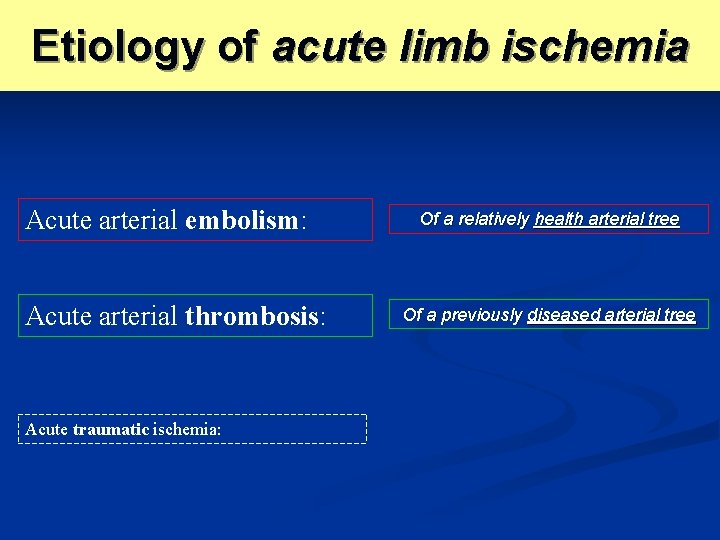
Etiology of acute limb ischemia Acute arterial embolism: Acute arterial thrombosis: Acute traumatic ischemia: Of a relatively health arterial tree Of a previously diseased arterial tree
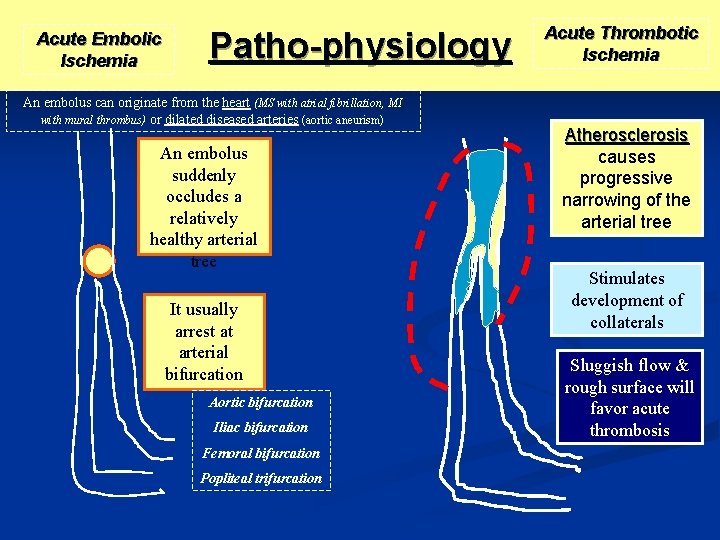
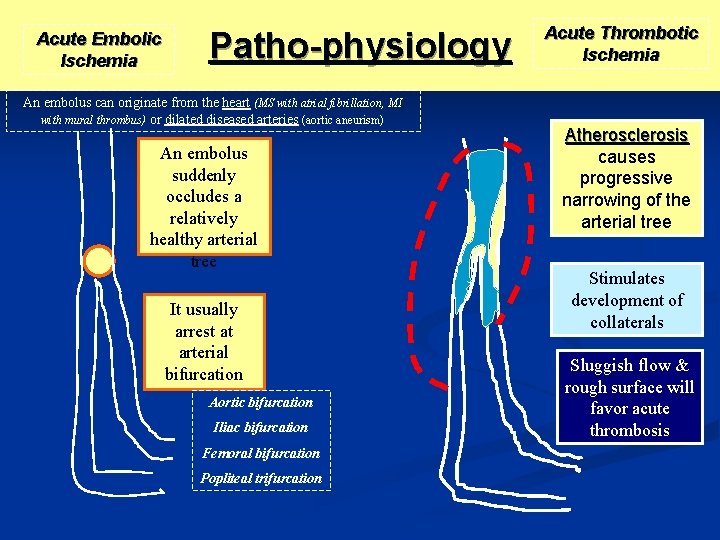
Acute Embolic Ischemia Patho-physiology An embolus can originate from the heart (MS with atrial fibrillation, MI with mural thrombus) or dilated diseased arteries (aortic aneurism) An embolus suddenly occludes a relatively healthy arterial tree It usually arrest at arterial bifurcation Aortic bifurcation Iliac bifurcation Femoral bifurcation Popliteal trifurcation Acute Thrombotic Ischemia Atherosclerosis causes progressive narrowing of the arterial tree Stimulates development of collaterals Sluggish flow & rough surface will favor acute thrombosis
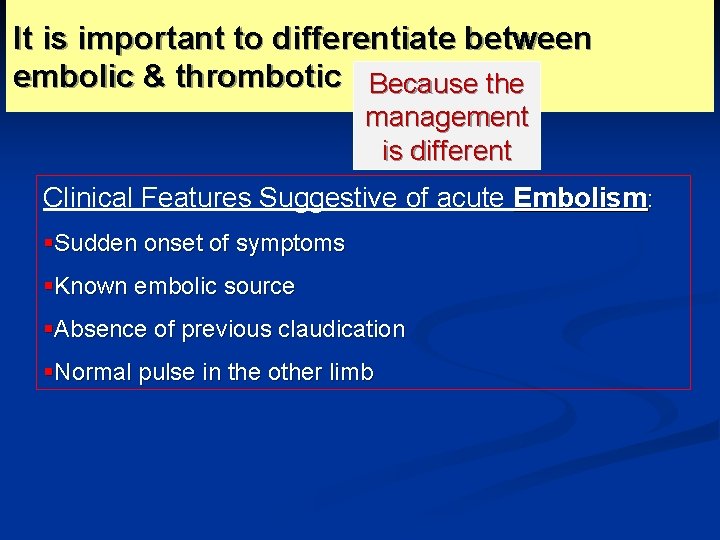
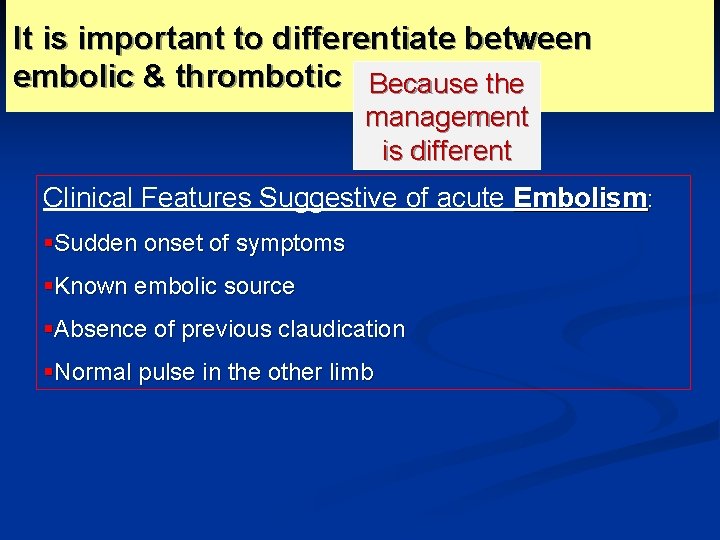
It is important to differentiate between embolic & thrombotic ischemia: Because the management is different Clinical Features Suggestive of acute Embolism: §Sudden onset of symptoms §Known embolic source §Absence of previous claudication §Normal pulse in the other limb
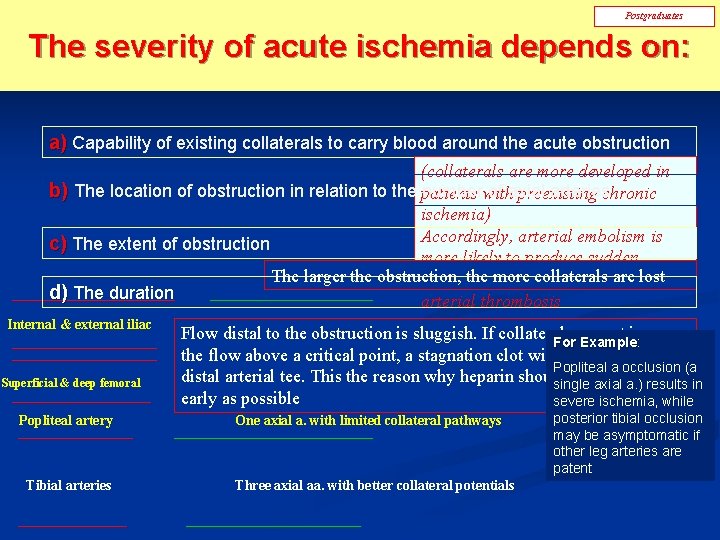
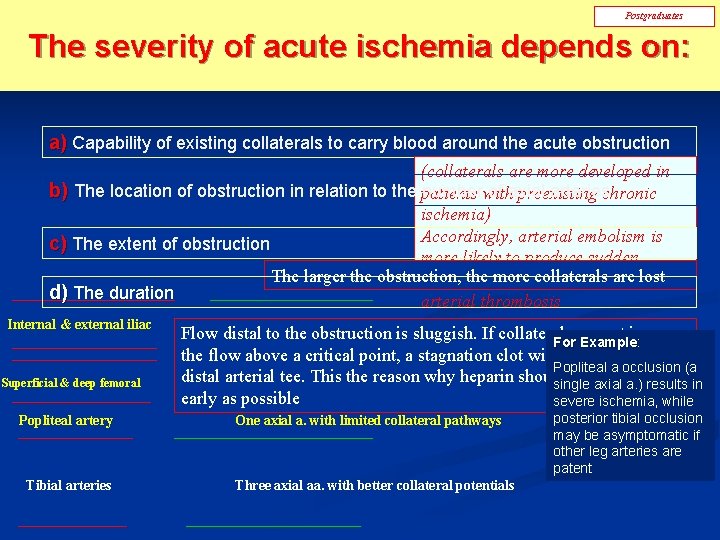
Postgraduates The severity of acute ischemia depends on: a) Capability of existing collaterals to carry blood around the acute obstruction (collaterals are more developed in b) The location of obstruction in relation to the patients numberwith of axial arterieschronic preexisting ischemia) Accordingly, arterial embolism is c) The extent of obstruction more likely to produce sudden One axial a. with limited collateral pathways Aorta & common iliac The larger the obstruction, the more collaterals arethen lost symptoms & severe ischemia d) The duration arterial thrombosis Internal & external iliac Superficial & deep femoral Popliteal artery Tibial arteries Two axial aa. With better collateral potentials Flow distal to the obstruction is sluggish. If collaterals cannot increase For Example: Example the flow above a critical point, a stagnation clot will develop in the Popliteal a occlusion (a distal arterial tee. aa. This reason whypotentials heparin should be given as Two axial Withthe better collateral single axial a. ) results in early as possible severe ischemia, while One axial a. with limited collateral pathways Three axial aa. with better collateral potentials posterior tibial occlusion may be asymptomatic if other leg arteries are patent
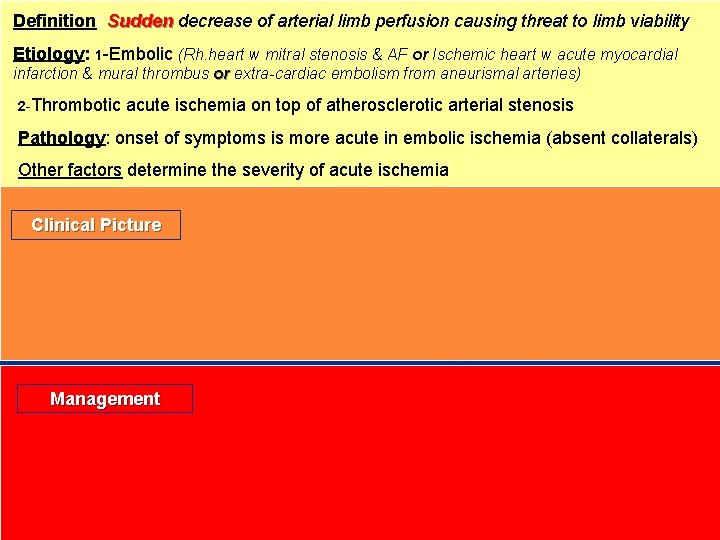
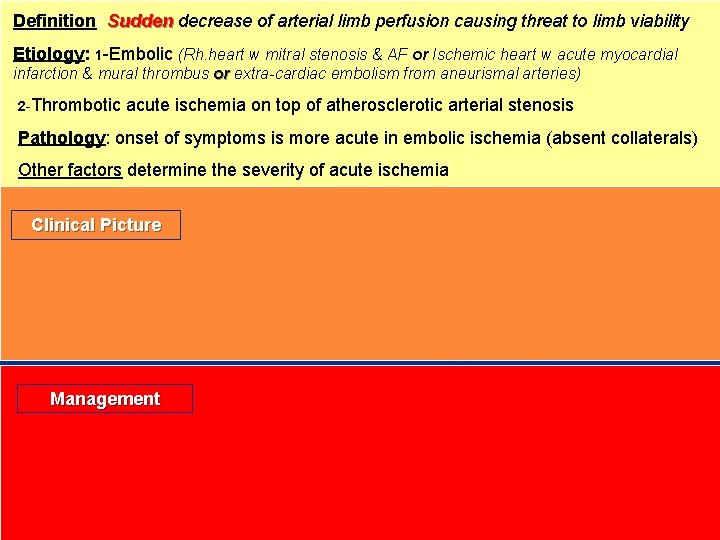
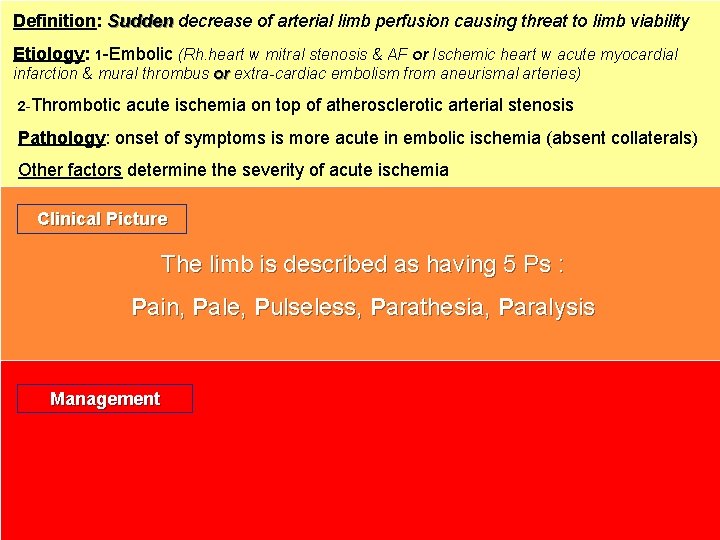
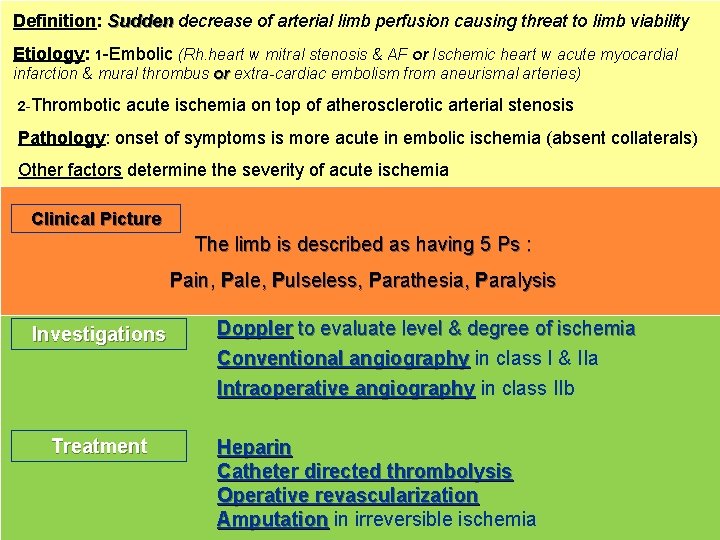
Definition: Sudden decrease of arterial limb perfusion causing threat to limb viability Etiology: 1 -Embolic (Rh. heart w mitral stenosis & AF or Ischemic heart w acute myocardial infarction & mural thrombus or extra-cardiac embolism from aneurismal arteries) 2 -Thrombotic acute ischemia on top of atherosclerotic arterial stenosis Pathology: onset of symptoms is more acute in embolic ischemia (absent collaterals) Other factors determine the severity of acute ischemia Clinical Picture Management
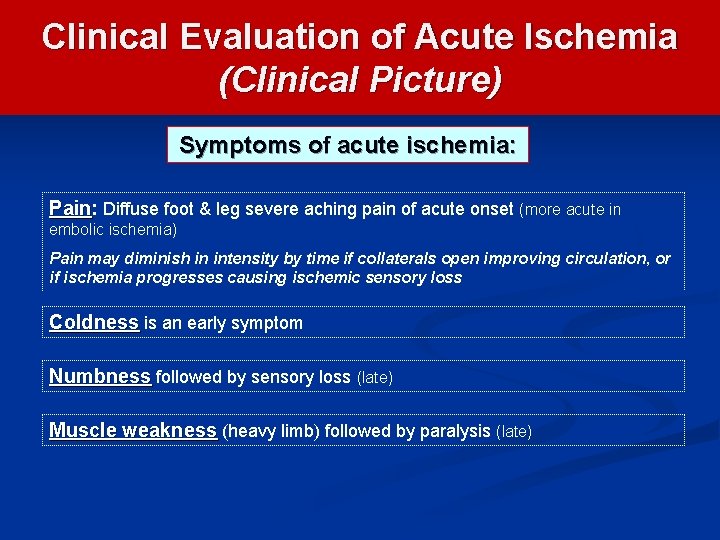
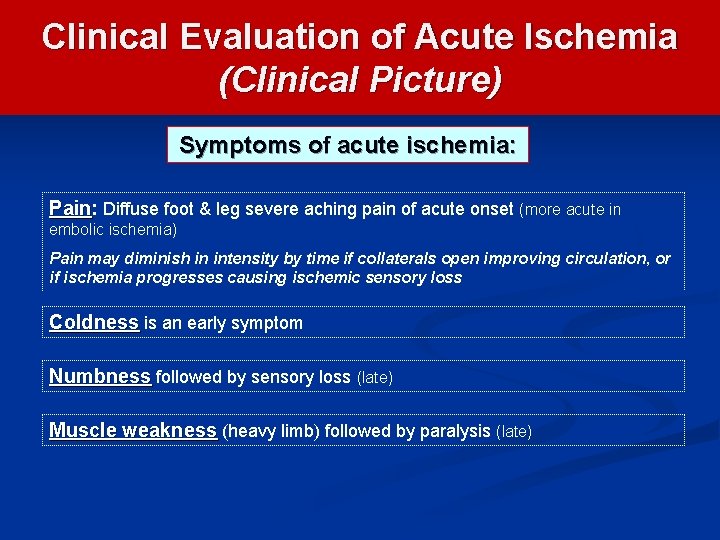
Clinical Evaluation of Acute Ischemia (Clinical Picture) Symptoms of acute ischemia: Pain Diffuse foot & leg severe aching pain of acute onset (more acute in embolic ischemia) Pain may diminish in intensity by time if collaterals open improving circulation, or if ischemia progresses causing ischemic sensory loss Coldness is an early symptom Numbness followed by sensory loss (late) Muscle weakness (heavy limb) followed by paralysis (late)
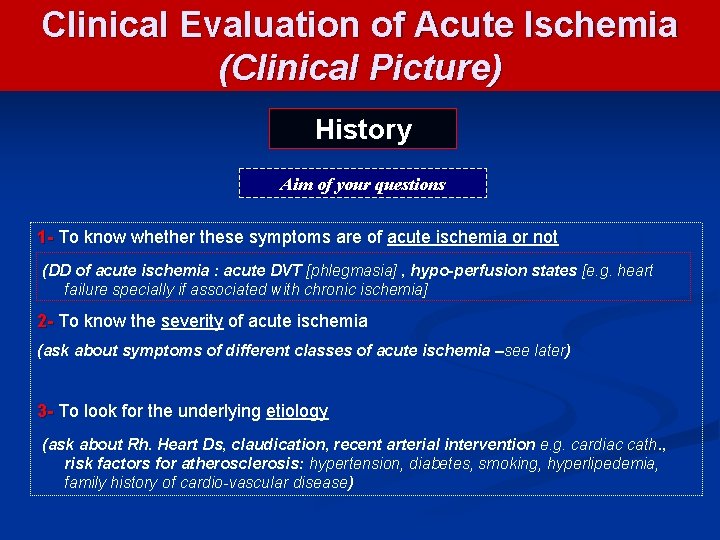
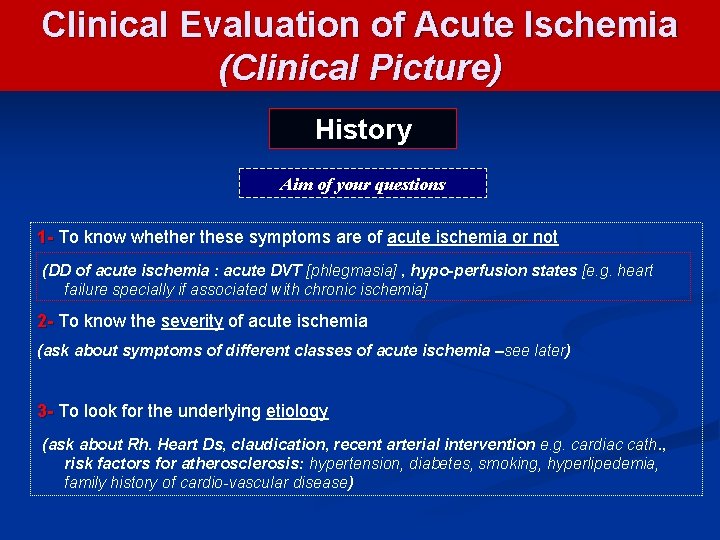
Clinical Evaluation of Acute Ischemia (Clinical Picture) History Aim of your questions 1 - To know whether these symptoms are of acute ischemia or not (DD of acute ischemia : acute DVT [phlegmasia] , hypo-perfusion states [e. g. heart failure specially if associated with chronic ischemia] 2 - To know the severity of acute ischemia (ask about symptoms of different classes of acute ischemia –see later) 3 - To look for the underlying etiology (ask about Rh. Heart Ds, claudication, recent arterial intervention e. g. cardiac cath. , risk factors for atherosclerosis: hypertension, diabetes, smoking, hyperlipedemia, family history of cardio-vascular disease)
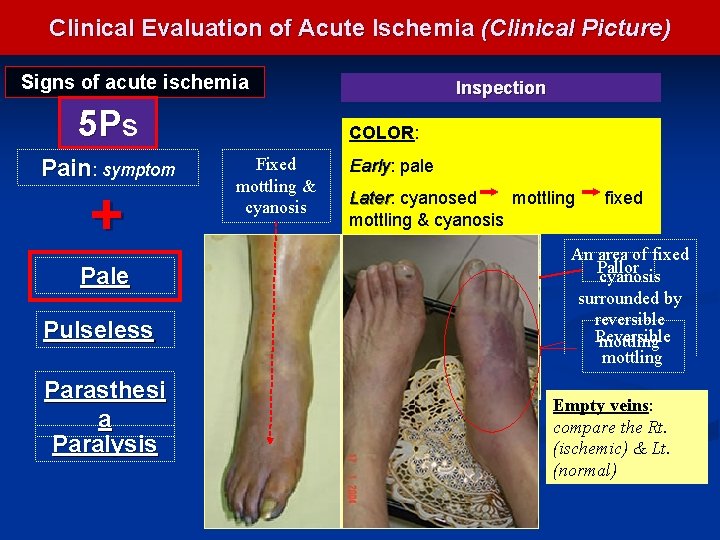
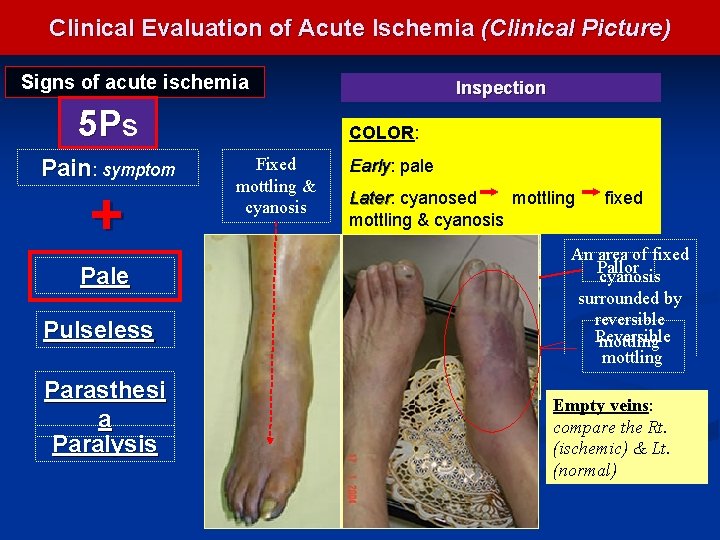
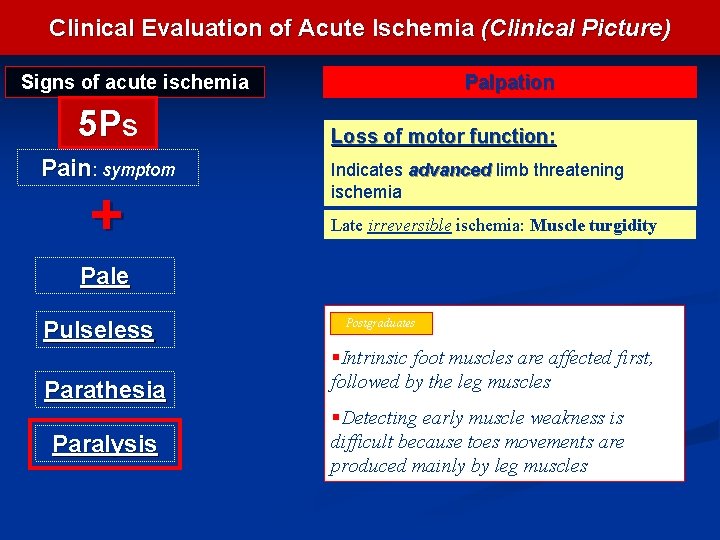
Clinical Evaluation of Acute Ischemia (Clinical Picture) Signs of acute ischemia 5 Ps Pain: symptom + Pale Pulseless Parasthesi a Paralysis Inspection COLOR: Fixed mottling & cyanosis Early: Early pale Later: mottling Later cyanosed mottling & cyanosis fixed An area of fixed Pallor cyanosis surrounded by reversible Reversible mottling Empty veins: compare the Rt. (ischemic) & Lt. (normal)
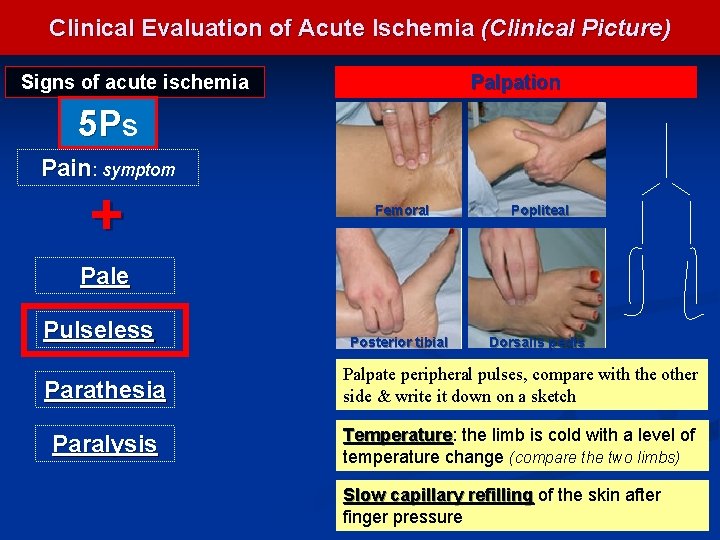
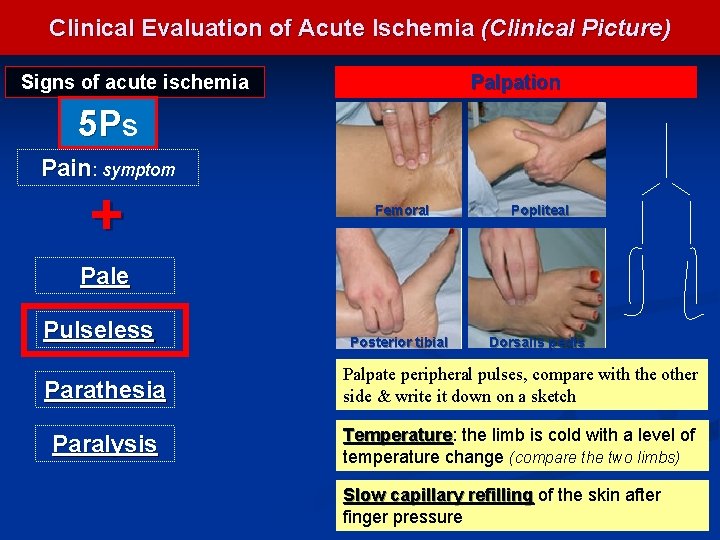
Clinical Evaluation of Acute Ischemia (Clinical Picture) Signs of acute ischemia Palpation 5 Ps Pain: symptom + Femoral Popliteal Posterior tibial Dorsalis pedis Pale Pulseless Parathesia Palpate peripheral pulses, compare with the other side & write it down on a sketch Paralysis Temperature: Temperature the limb is cold with a level of temperature change (compare the two limbs) Slow capillary refilling of the skin after finger pressure
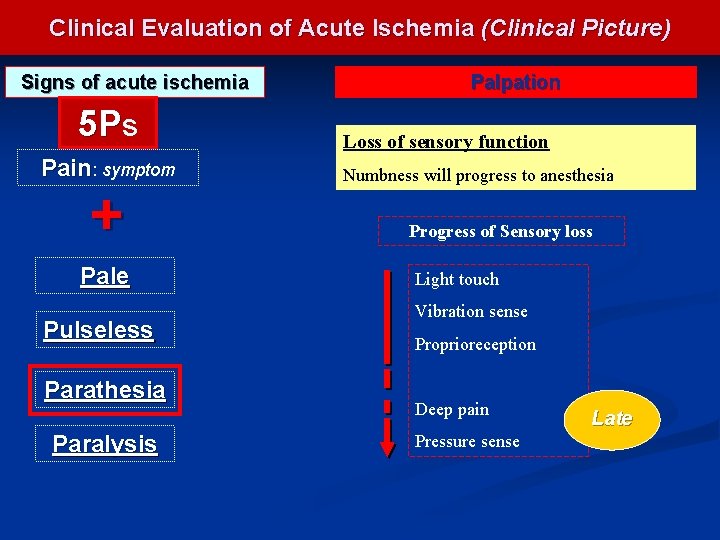
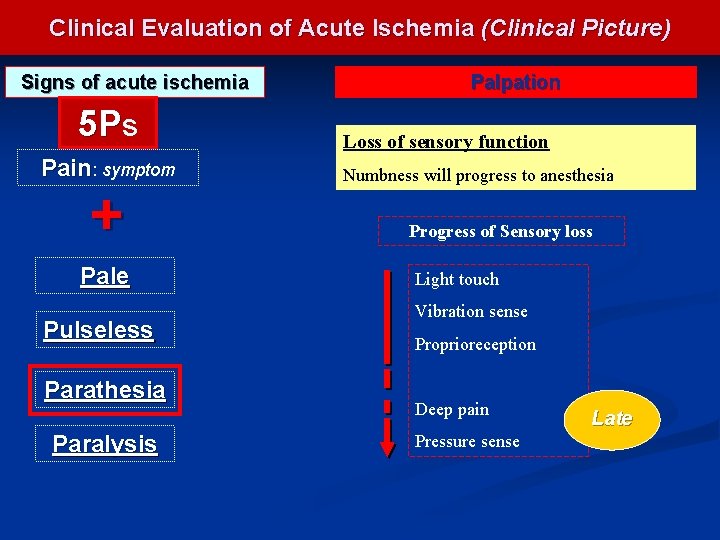
Clinical Evaluation of Acute Ischemia (Clinical Picture) Signs of acute ischemia 5 Ps Pain: symptom + Pale Pulseless Parathesia Paralysis Palpation Loss of sensory function Numbness will progress to anesthesia Progress of Sensory loss Light touch Vibration sense Proprioreception Deep pain Pressure sense Late
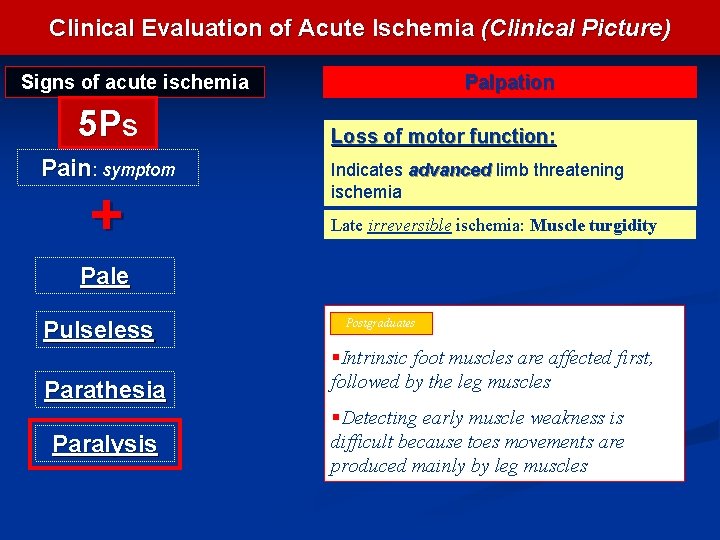
Clinical Evaluation of Acute Ischemia (Clinical Picture) Signs of acute ischemia 5 Ps Pain: symptom + Palpation Loss of motor function: Indicates advanced limb threatening ischemia Late irreversible ischemia: Muscle turgidity Pale Pulseless Parathesia Paralysis Postgraduates §Intrinsic foot muscles are affected first, followed by the leg muscles §Detecting early muscle weakness is difficult because toes movements are produced mainly by leg muscles
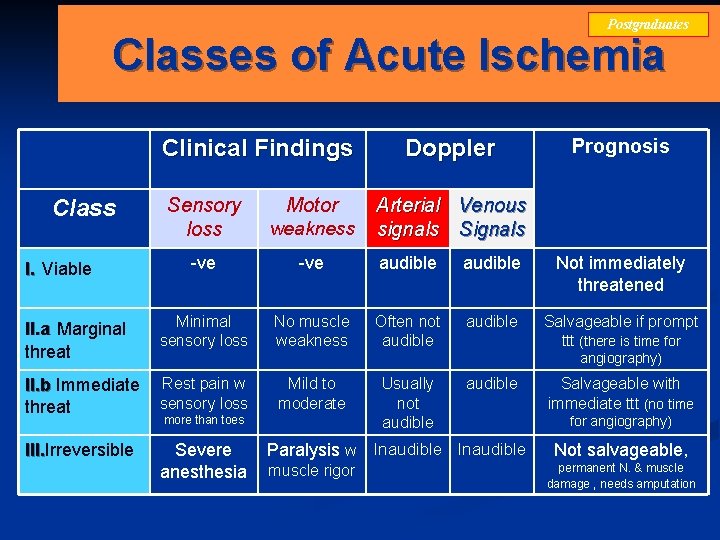
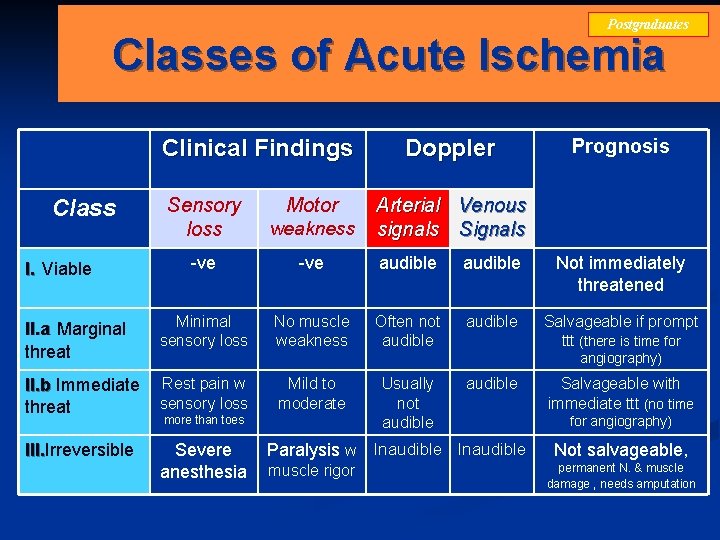
Postgraduates Classes of Acute Ischemia Clinical Findings Prognosis Sensory loss weakness -ve audible Not immediately threatened II. a Marginal threat Minimal sensory loss No muscle weakness Often not audible Salvageable if prompt ttt (there is time for II. b Immediate threat Rest pain w sensory loss III. Irreversible III. Severe anesthesia Class I. Viable Motor Doppler Arterial Venous signals Signals angiography) Mild to moderate more than toes Usually not audible Paralysis w Inaudible muscle rigor Salvageable with immediate ttt (no time for angiography) Not salvageable, permanent N. & muscle damage , needs amputation
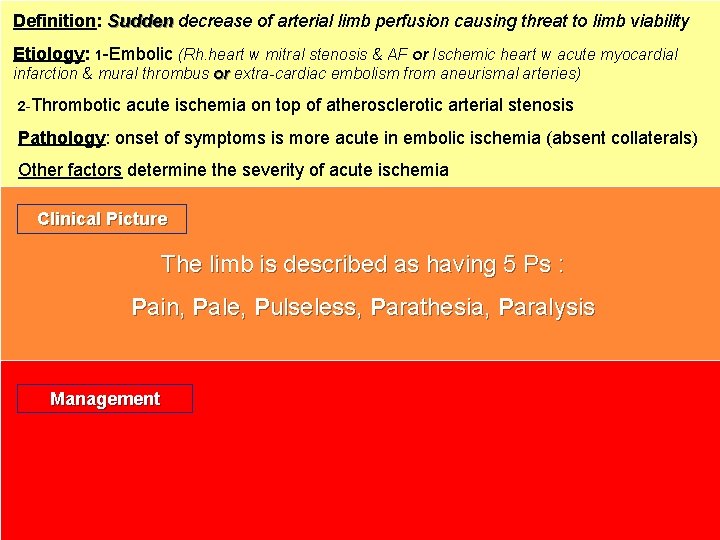
Definition: Sudden decrease of arterial limb perfusion causing threat to limb viability Etiology: 1 -Embolic (Rh. heart w mitral stenosis & AF or Ischemic heart w acute myocardial infarction & mural thrombus or extra-cardiac embolism from aneurismal arteries) 2 -Thrombotic acute ischemia on top of atherosclerotic arterial stenosis Pathology: onset of symptoms is more acute in embolic ischemia (absent collaterals) Other factors determine the severity of acute ischemia Clinical Picture The limb is described as having 5 Ps : Pain, Pale, Pulseless, Parathesia, Paralysis Management
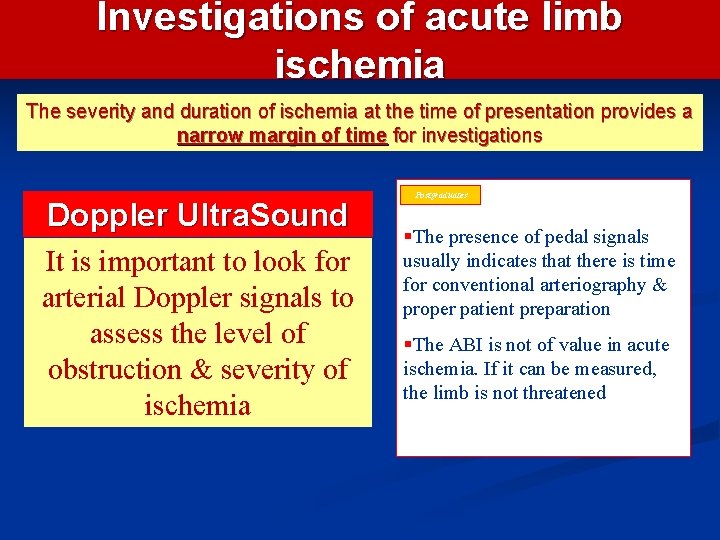
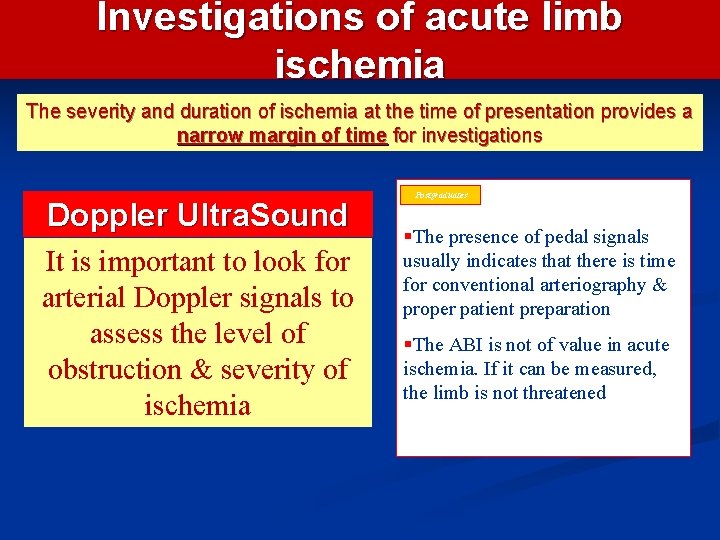
Investigations of acute limb ischemia The severity and duration of ischemia at the time of presentation provides a narrow margin of time for investigations Doppler Ultra. Sound It is important to look for arterial Doppler signals to assess the level of obstruction & severity of ischemia Postgraduates §The presence of pedal signals usually indicates that there is time for conventional arteriography & proper patient preparation §The ABI is not of value in acute ischemia. If it can be measured, the limb is not threatened
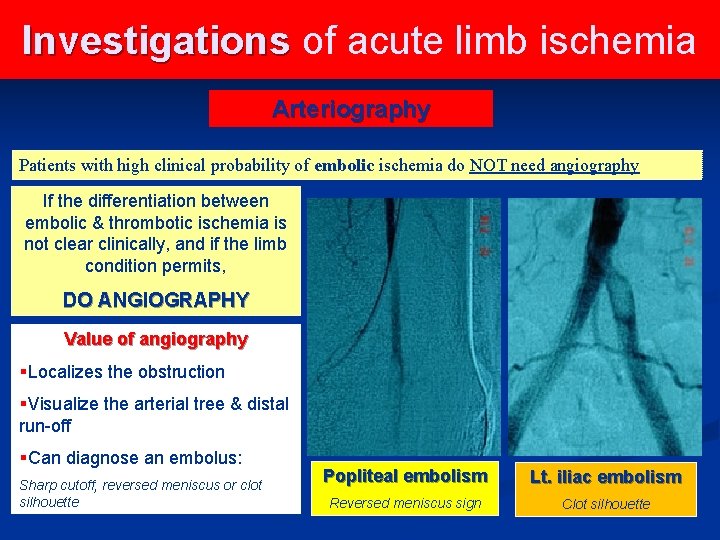
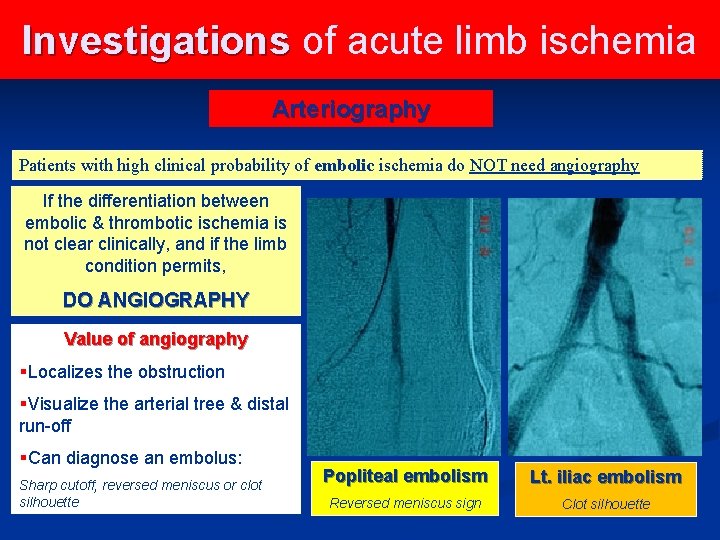
Investigations of acute limb ischemia Arteriography Patients with high clinical probability of embolic ischemia do NOT need angiography If the differentiation between embolic & thrombotic ischemia is not clear clinically, and if the limb condition permits, DO ANGIOGRAPHY Value of angiography §Localizes the obstruction §Visualize the arterial tree & distal run-off §Can diagnose an embolus: Sharp cutoff, reversed meniscus or clot silhouette Popliteal embolism Lt. iliac embolism Reversed meniscus sign Clot silhouette
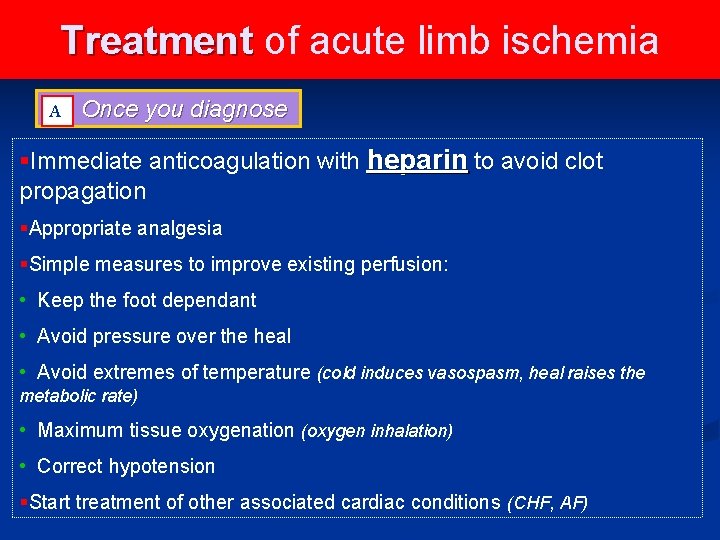
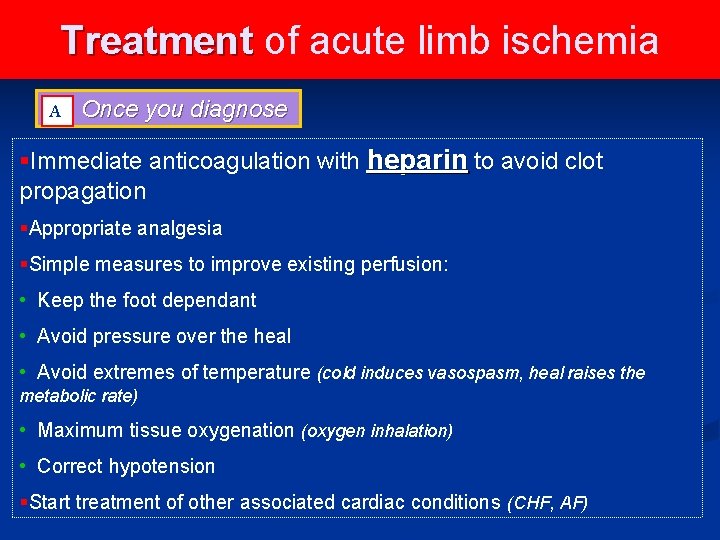
Treatment of acute limb ischemia A A Once you diagnose §Immediate anticoagulation with heparin to avoid clot propagation §Appropriate analgesia §Simple measures to improve existing perfusion: • Keep the foot dependant • Avoid pressure over the heal • Avoid extremes of temperature (cold induces vasospasm, heal raises the metabolic rate) • Maximum tissue oxygenation (oxygen inhalation) • Correct hypotension §Start treatment of other associated cardiac conditions (CHF, AF)
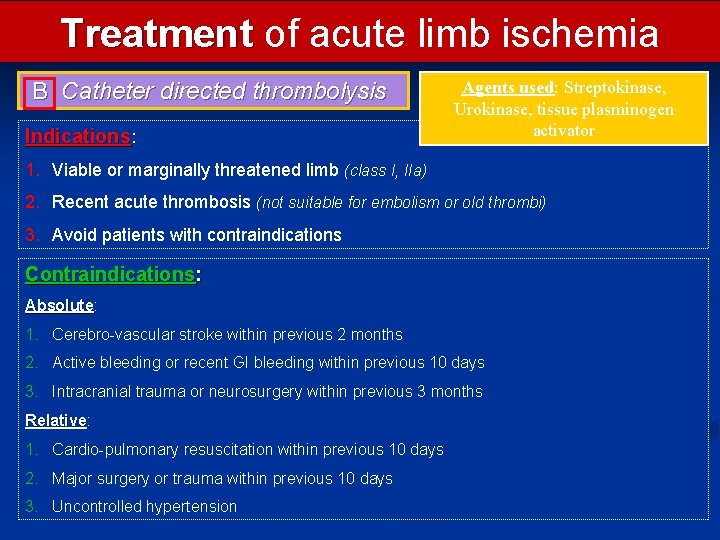
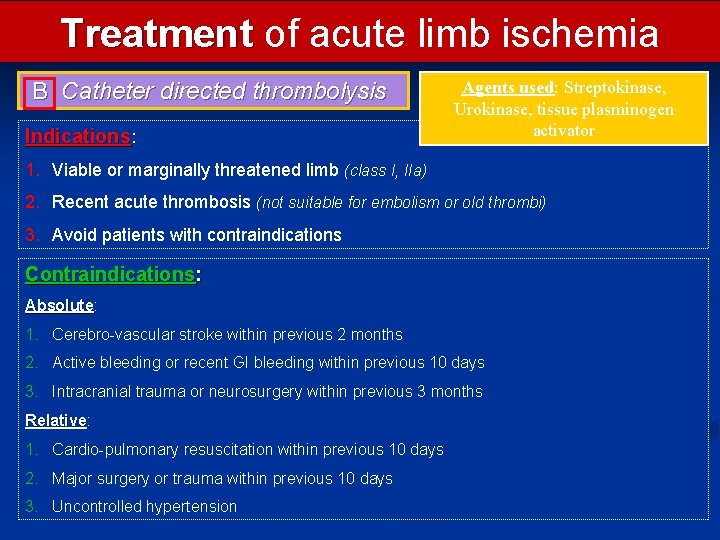
Treatment of acute limb ischemia B Catheter directed thrombolysis Indications: Agents used: Streptokinase, Urokinase, tissue plasminogen activator 1. Viable or marginally threatened limb (class I, IIa) 2. Recent acute thrombosis (not suitable for embolism or old thrombi) 3. Avoid patients with contraindications Contraindications: Absolute 1. Cerebro-vascular stroke within previous 2 months 2. Active bleeding or recent GI bleeding within previous 10 days 3. Intracranial trauma or neurosurgery within previous 3 months Relative: Relative 1. Cardio-pulmonary resuscitation within previous 10 days 2. Major surgery or trauma within previous 10 days 3. Uncontrolled hypertension
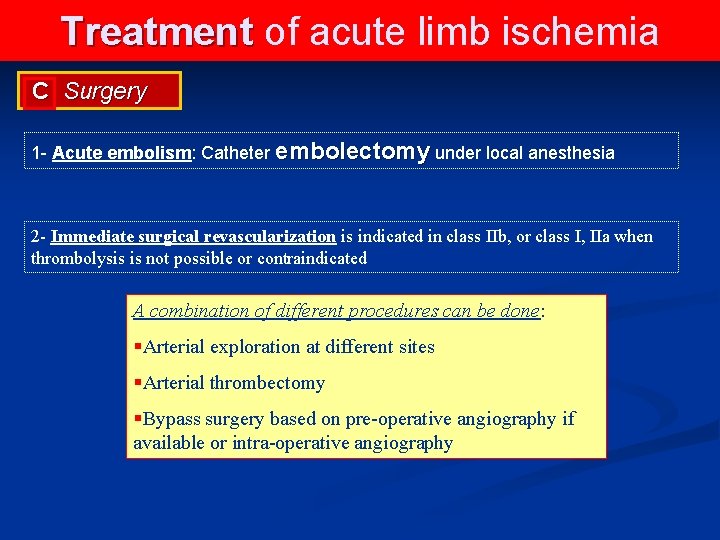
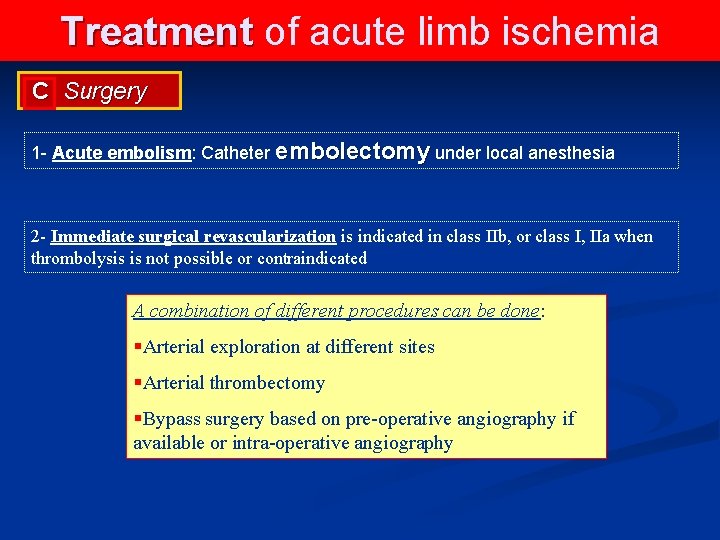
Treatment of acute limb ischemia C Surgery 1 - Acute embolism: Catheter embolectomy under local anesthesia 2 - Immediate surgical revascularization is indicated in class IIb, or class I, IIa when thrombolysis is not possible or contraindicated A combination of different procedures can be done: §Arterial exploration at different sites §Arterial thrombectomy §Bypass surgery based on pre-operative angiography if available or intra-operative angiography
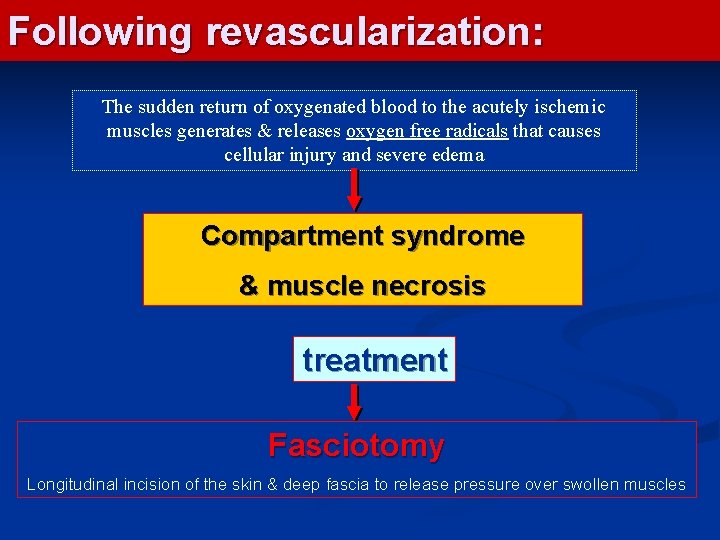
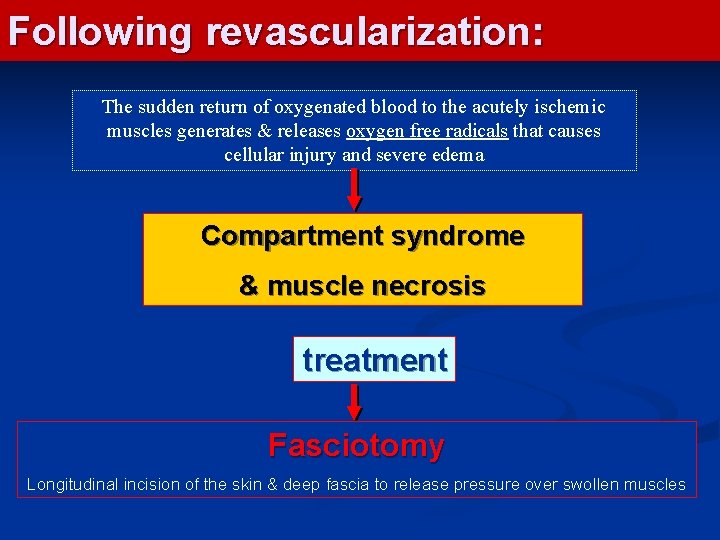
Following revascularization: The sudden return of oxygenated blood to the acutely ischemic muscles generates & releases oxygen free radicals that causes cellular injury and severe edema Compartment syndrome & muscle necrosis treatment Fasciotomy Longitudinal incision of the skin & deep fascia to release pressure over swollen muscles
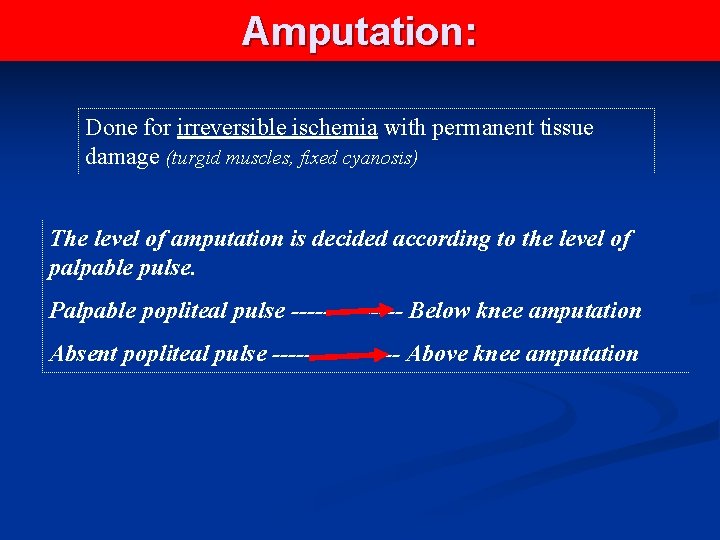
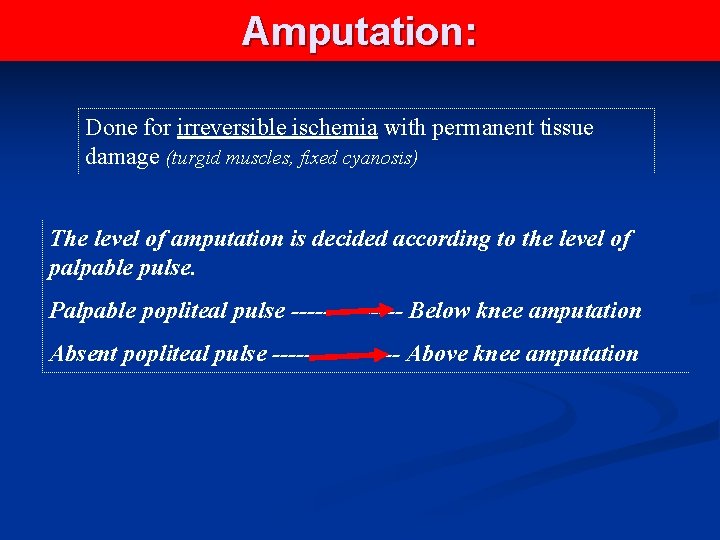
Amputation: Done for irreversible ischemia with permanent tissue damage (turgid muscles, fixed cyanosis) The level of amputation is decided according to the level of palpable pulse. Palpable popliteal pulse ------- Below knee amputation Absent popliteal pulse -------- Above knee amputation
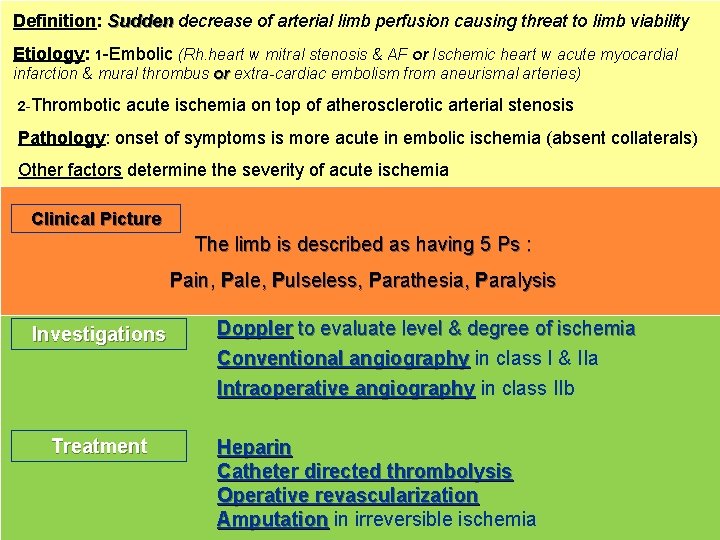
Definition: Sudden decrease of arterial limb perfusion causing threat to limb viability Etiology: 1 -Embolic (Rh. heart w mitral stenosis & AF or Ischemic heart w acute myocardial infarction & mural thrombus or extra-cardiac embolism from aneurismal arteries) 2 -Thrombotic acute ischemia on top of atherosclerotic arterial stenosis Pathology: onset of symptoms is more acute in embolic ischemia (absent collaterals) Other factors determine the severity of acute ischemia Clinical Picture The limb is described as having 5 Ps : Pain, Pale, Pulseless, Parathesia, Paralysis Investigations Treatment Doppler to evaluate level & degree of ischemia Conventional angiography in class I & IIa Intraoperative angiography in class IIb Heparin Catheter directed thrombolysis Operative revascularization Amputation in irreversible ischemia

Thank You
 Peripheral arterial disease
Peripheral arterial disease Hubert kairuki memorial university faculty of medicine
Hubert kairuki memorial university faculty of medicine Semmelweis university faculty of medicine
Semmelweis university faculty of medicine Applied medical sciences
Applied medical sciences Territorial matrix vs interterritorial matrix
Territorial matrix vs interterritorial matrix Faculty of veterinary medicine cairo university logo
Faculty of veterinary medicine cairo university logo Hacettepe university faculty of medicine
Hacettepe university faculty of medicine Conus arteriosus
Conus arteriosus Semmelweis university faculty of medicine
Semmelweis university faculty of medicine Faculty of veterinary medicine cairo university
Faculty of veterinary medicine cairo university Cairo university faculty of veterinary medicine
Cairo university faculty of veterinary medicine Peripheral arterial pulse sites
Peripheral arterial pulse sites Mrbs scholarship
Mrbs scholarship Department of medicine mcgill
Department of medicine mcgill Faculty of medicine dentistry and health sciences
Faculty of medicine dentistry and health sciences Emory anticoagulation clinic
Emory anticoagulation clinic Fascicular
Fascicular Communicable disease and non communicable disease
Communicable disease and non communicable disease University of split faculty of maritime studies
University of split faculty of maritime studies University of bridgeport computer science
University of bridgeport computer science University of bridgeport computer science faculty
University of bridgeport computer science faculty Mch fsu
Mch fsu Mendel university faculty of business and economics
Mendel university faculty of business and economics Singularity university faculty
Singularity university faculty Masaryk university medical faculty
Masaryk university medical faculty Feup university of porto
Feup university of porto Charles university faculty of humanities
Charles university faculty of humanities Faculty of law of the university of zagreb
Faculty of law of the university of zagreb University of montenegro faculty of law
University of montenegro faculty of law University of kragujevac faculty of technical sciences
University of kragujevac faculty of technical sciences University of cologne faculty of management
University of cologne faculty of management Leading university sylhet tuition fees
Leading university sylhet tuition fees Brown university computer science
Brown university computer science Lebanese university roumieh
Lebanese university roumieh Myfile yorku
Myfile yorku Elearningunideb
Elearningunideb Clemson electrical engineering
Clemson electrical engineering Faculty of mechanical engineering thammasat university
Faculty of mechanical engineering thammasat university Faculty of business and economics mendel university in brno
Faculty of business and economics mendel university in brno Masaryk university medical faculty
Masaryk university medical faculty Slidetodoc.com
Slidetodoc.com Thin and thick smear
Thin and thick smear Faculty of education khon kaen university
Faculty of education khon kaen university Communication arts chulalongkorn university
Communication arts chulalongkorn university Universitatea de medicina si farmacie victor babes
Universitatea de medicina si farmacie victor babes Lincoln memorial university college of veterinary medicine
Lincoln memorial university college of veterinary medicine King saud university college of medicine
King saud university college of medicine King saud university college of medicine
King saud university college of medicine Prodofol
Prodofol University of wisconsin integrative medicine anxiety
University of wisconsin integrative medicine anxiety Victor babeş university of medicine and pharmacy
Victor babeş university of medicine and pharmacy Victor babes university of medicine and pharmacy
Victor babes university of medicine and pharmacy King saud university college of medicine
King saud university college of medicine Veterinary medicine brno
Veterinary medicine brno Slu family medicine residency
Slu family medicine residency Al mustansiriya university college of medicine
Al mustansiriya university college of medicine Midwestern university college of dental medicine
Midwestern university college of dental medicine Seoul national university history
Seoul national university history University of kentucky college of medicine
University of kentucky college of medicine Unm internal medicine
Unm internal medicine Mercer medical library
Mercer medical library University of arizona emergency medicine
University of arizona emergency medicine Which of the following elevates the ribs?
Which of the following elevates the ribs? Aortic pressure curve
Aortic pressure curve Allen's test
Allen's test Tentorium cerebelli cranial nerve
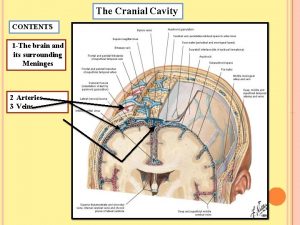
Tentorium cerebelli cranial nerve Puntos anatomicos para tomar la presion arterial
Puntos anatomicos para tomar la presion arterial Arterial arcades of jejunum and ileum
Arterial arcades of jejunum and ileum Circulação
Circulação Pulso pedioso
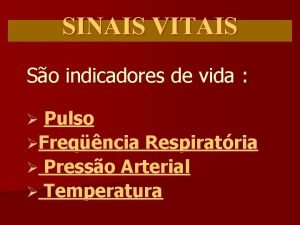
Pulso pedioso Sinais vitais
Sinais vitais