PAD DR SHWETA PHADKE Peripheral Arterial Disease and
- Slides: 29
PAD DR. SHWETA PHADKE.
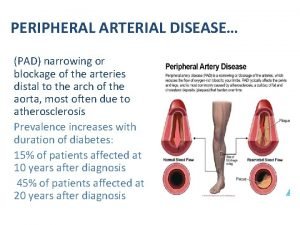
Peripheral Arterial Disease and Claudication • Peripheral Arterial Disease (PAD) A disorder caused by atherosclerosis that limits blood flow to the limbs • Claudication A symptom of PAD characterized by pain, aching, or fatigue in working skeletal muscles. Claudication arises when there is insufficient blood flow to meet the metabolic demands in leg muscles of ambulating patients
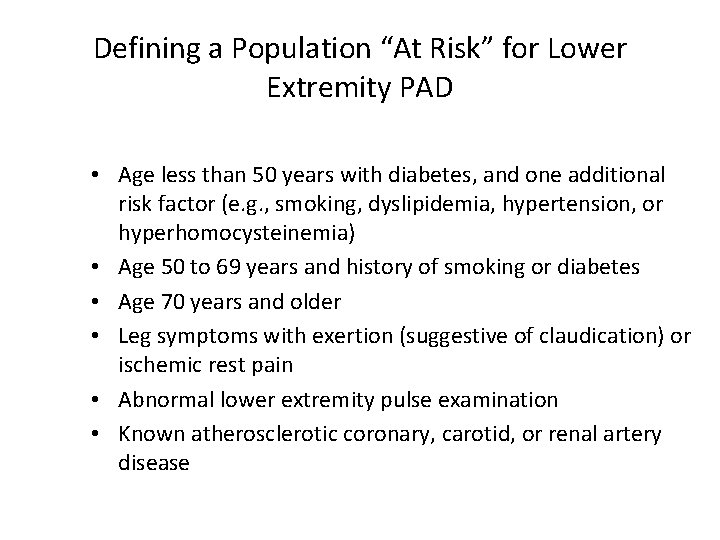
Defining a Population “At Risk” for Lower Extremity PAD • Age less than 50 years with diabetes, and one additional risk factor (e. g. , smoking, dyslipidemia, hypertension, or hyperhomocysteinemia) • Age 50 to 69 years and history of smoking or diabetes • Age 70 years and older • Leg symptoms with exertion (suggestive of claudication) or ischemic rest pain • Abnormal lower extremity pulse examination • Known atherosclerotic coronary, carotid, or renal artery disease
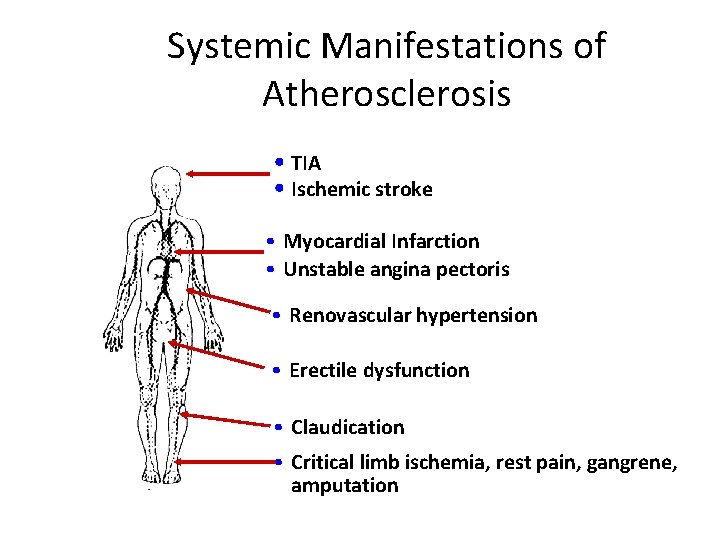
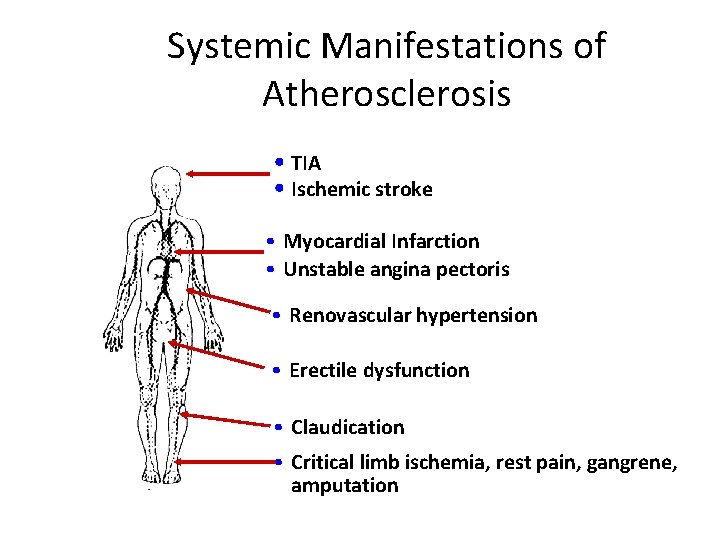
Systemic Manifestations of Atherosclerosis • TIA • Ischemic stroke • Myocardial Infarction • Unstable angina pectoris • Renovascular hypertension • Erectile dysfunction • Claudication • Critical limb ischemia, rest pain, gangrene, amputation
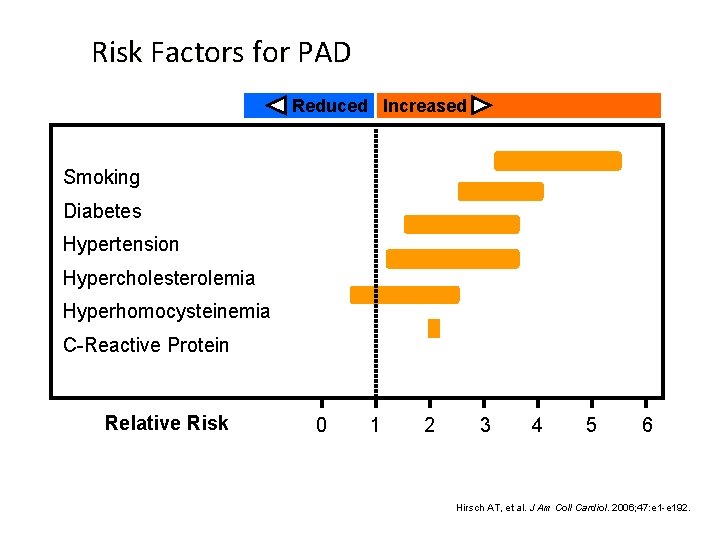
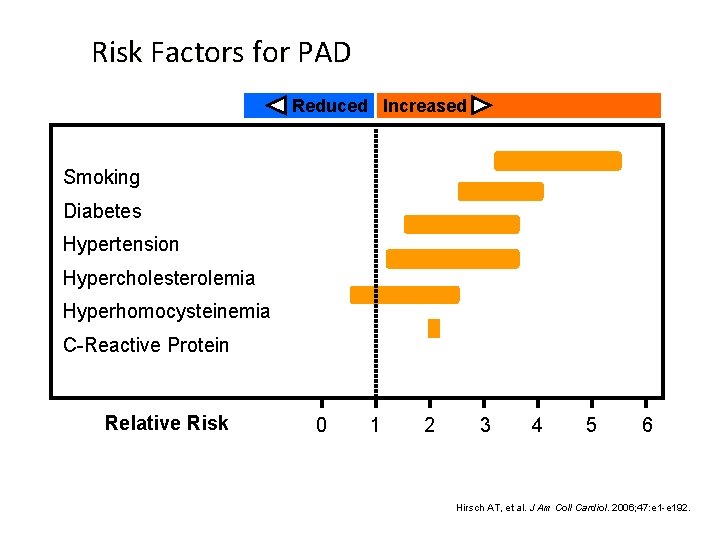
Risk Factors for PAD Reduced Increased Smoking Diabetes Hypertension Hypercholesterolemia Hyperhomocysteinemia C-Reactive Protein Relative Risk 0 1 2 3 4 5 6 Hirsch AT, et al. J Am Coll Cardiol. 2006; 47: e 1 -e 192.
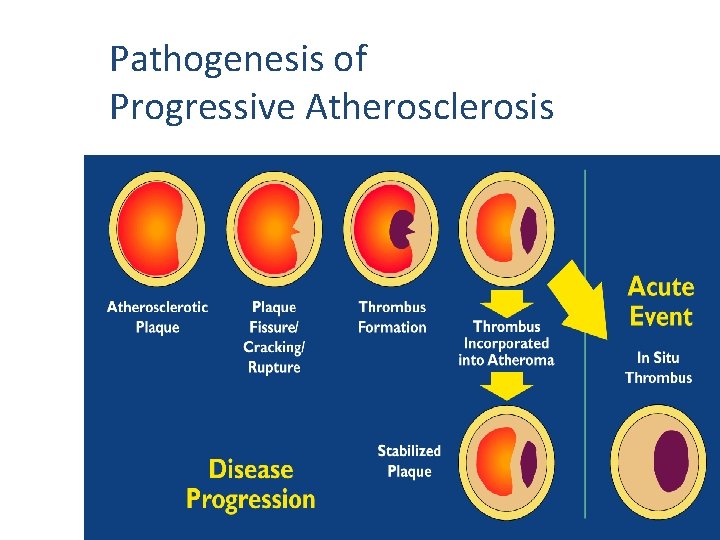
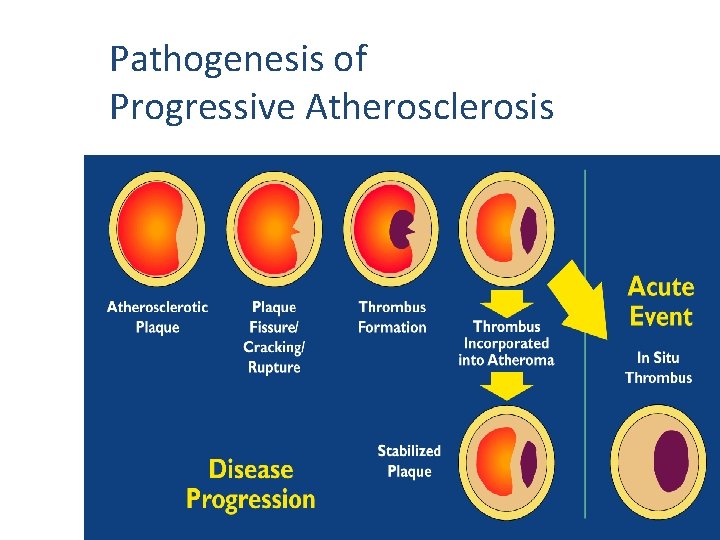
Pathogenesis of Progressive Atherosclerosis
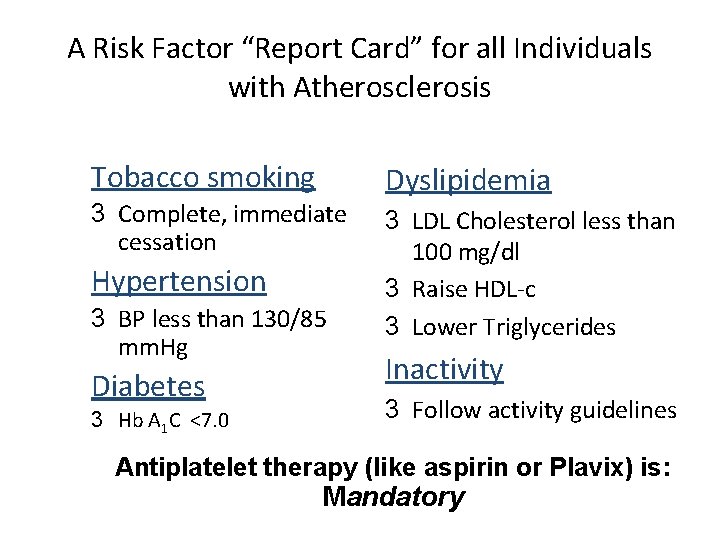
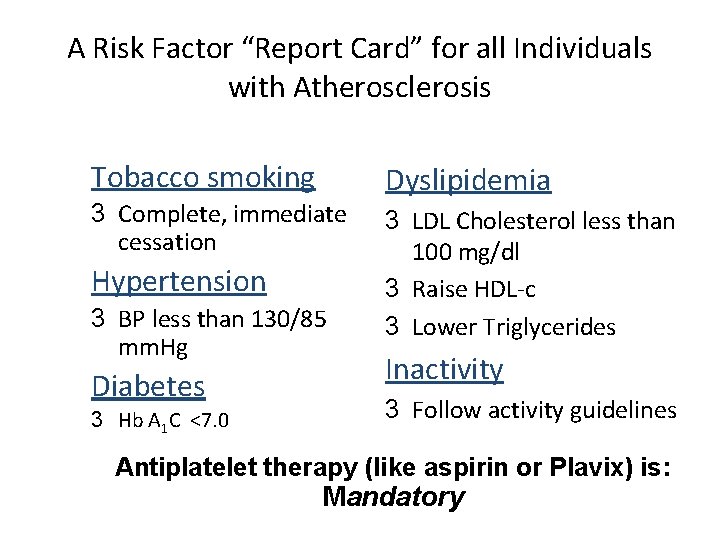
A Risk Factor “Report Card” for all Individuals with Atherosclerosis Tobacco smoking 3 Complete, immediate cessation Hypertension 3 BP less than 130/85 mm. Hg Diabetes 3 Hb A 1 C <7. 0 Dyslipidemia 3 LDL Cholesterol less than 100 mg/dl 3 Raise HDL-c 3 Lower Triglycerides Inactivity 3 Follow activity guidelines Antiplatelet therapy (like aspirin or Plavix) is: Mandatory
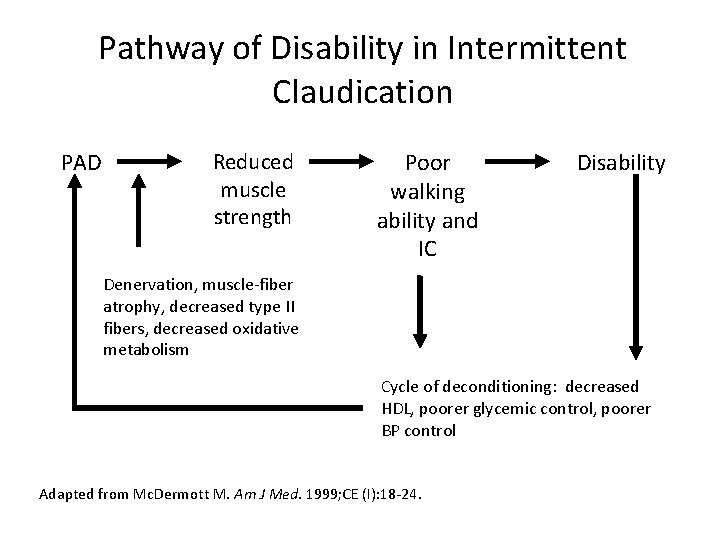
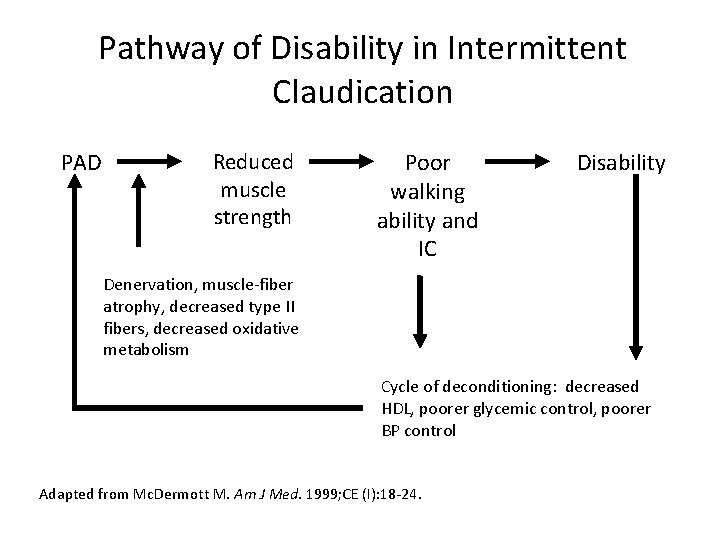
Pathway of Disability in Intermittent Claudication PAD Reduced muscle strength Poor walking ability and IC Disability Denervation, muscle-fiber atrophy, decreased type II fibers, decreased oxidative metabolism Cycle of deconditioning: decreased HDL, poorer glycemic control, poorer BP control Adapted from Mc. Dermott M. Am J Med. 1999; CE (I): 18 -24.
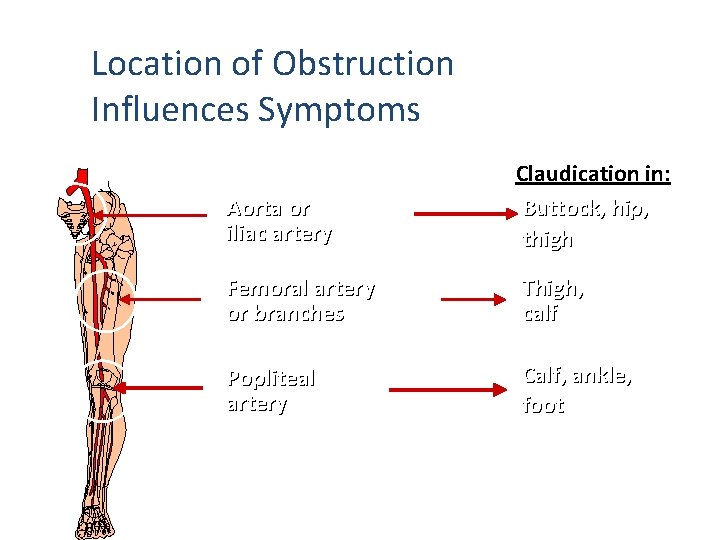
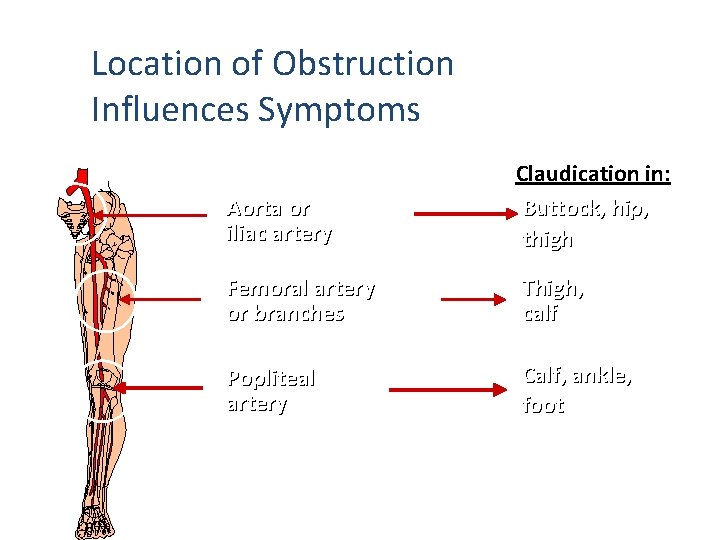
Location of Obstruction Influences Symptoms Obstruction in: Aorta or iliac artery Claudication in: Buttock, hip, thigh Femoral artery or branches Thigh, calf Popliteal artery Calf, ankle, foot
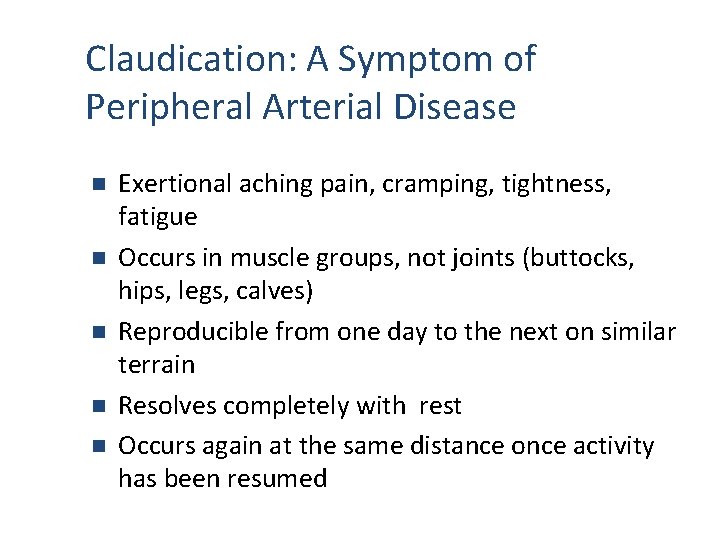
Claudication: A Symptom of Peripheral Arterial Disease n n n Exertional aching pain, cramping, tightness, fatigue Occurs in muscle groups, not joints (buttocks, hips, legs, calves) Reproducible from one day to the next on similar terrain Resolves completely with rest Occurs again at the same distance once activity has been resumed
Clinical Assessment of Peripheral Arterial Disease
Components of Clinical Assessment • Complete history – Risk factor assessment – Activity assessment • Review of medications • Physical examination – Inspection of lower extremities – Pulse exam
Questions for Patients • Do you develop discomfort in your legs when you walk? – Cramping, aching, fatigue • Do you get this pain when you are sitting standing, or lying? • Do symptoms only start when you walk? • Does the discomfort always occur at about the same distance? • Do symptoms resolve once you stop walking?
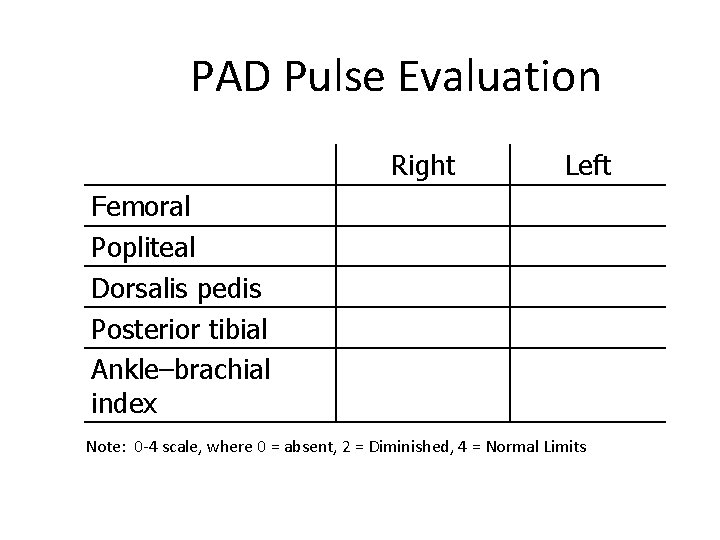
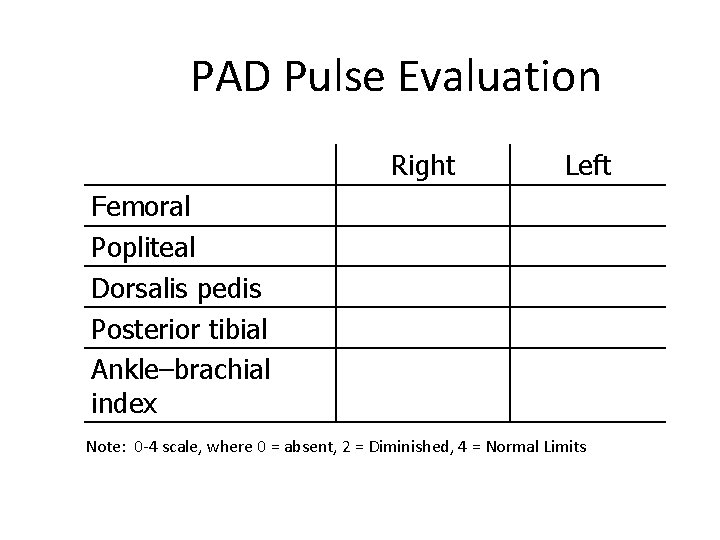
PAD Pulse Evaluation Right Left Femoral Popliteal Dorsalis pedis Posterior tibial Ankle–brachial index Note: 0 -4 scale, where 0 = absent, 2 = Diminished, 4 = Normal Limits
The Ankle-Brachial Index (ABI) • The first diagnostic assessment that should be done to evaluate a patient for PAD after a pulse exam in the presence of risk factors or if claudication is suspected. • Inexpensive, accurate and can be done in the primary care setting • The ABI is 95% sensitive and 99% specific for PAD • Predicts limb survival, potential for wound healing, and mortality
The Ankle-Brachial Index (ABI) • Indicated – In the absence of palpable pulses, or if pulses are diminished – In the presence or suspicion of claudication, foot pain at rest, or a nonhealing foot ulcer – Age greater than 70 years of age, >50 years with risk factors (diabetes, smoking)
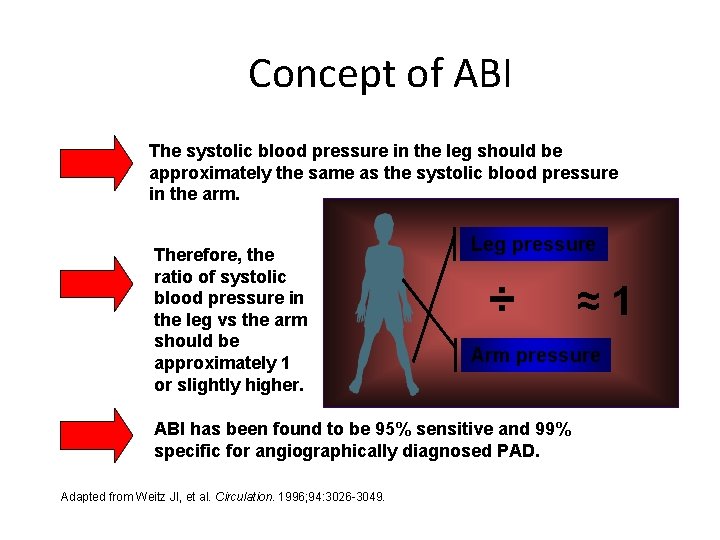
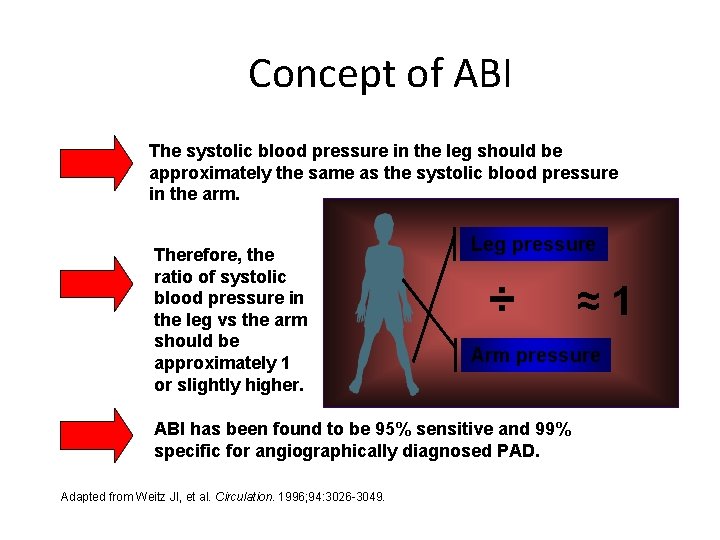
Concept of ABI The systolic blood pressure in the leg should be approximately the same as the systolic blood pressure in the arm. Therefore, the ratio of systolic blood pressure in the leg vs the arm should be approximately 1 or slightly higher. Leg pressure ÷ Arm pressure ABI has been found to be 95% sensitive and 99% specific for angiographically diagnosed PAD. Adapted from Weitz JI, et al. Circulation. 1996; 94: 3026 -3049. ≈1
Understanding the ABI • Performed with patient resting in supine position • All pressures are measured with a arterial Doppler and appropriately sized blood pressure cuff • Both brachial pressures are measured • Ankle pressures are measured using the posterior tibial and/or dorsalis pedis arteries
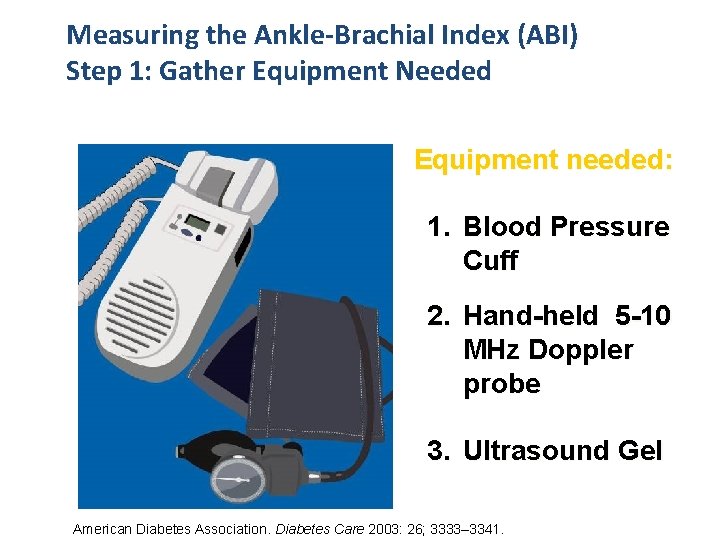
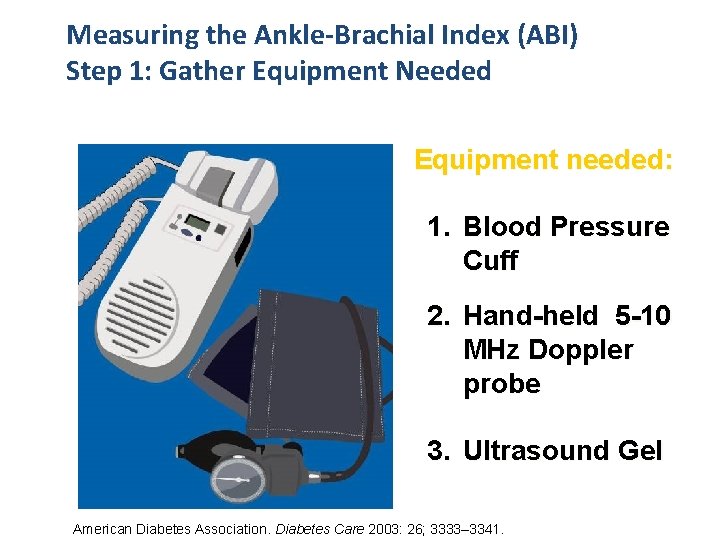
Measuring the Ankle-Brachial Index (ABI) Step 1: Gather Equipment Needed Equipment needed: 1. Blood Pressure Cuff 2. Hand-held 5 -10 MHz Doppler probe 3. Ultrasound Gel American Diabetes Association. Diabetes Care 2003: 26; 3333– 3341.
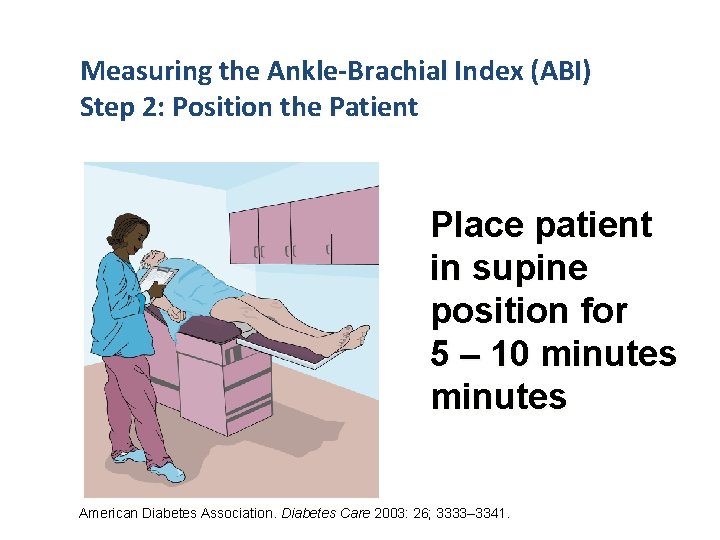
Measuring the Ankle-Brachial Index (ABI) Step 2: Position the Patient Place patient in supine position for 5 – 10 minutes American Diabetes Association. Diabetes Care 2003: 26; 3333– 3341.
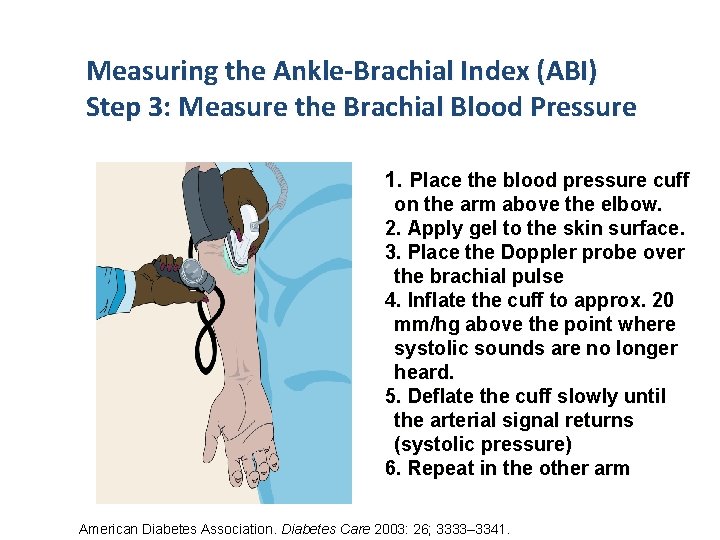
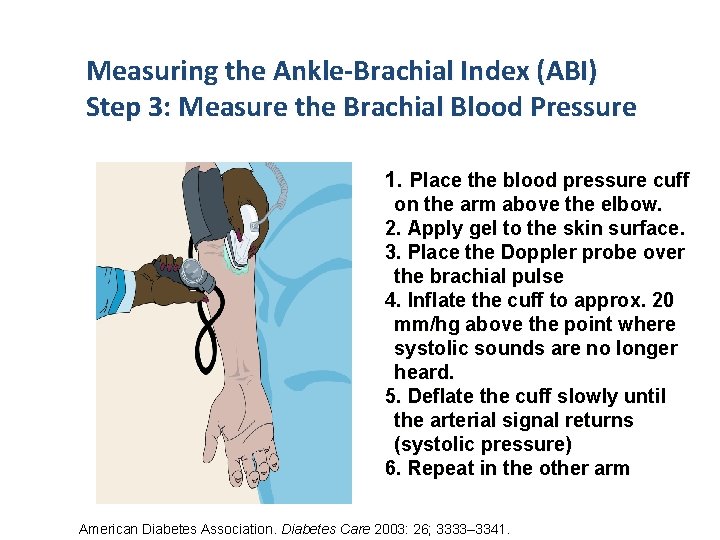
Measuring the Ankle-Brachial Index (ABI) Step 3: Measure the Brachial Blood Pressure 1. Place the blood pressure cuff on the arm above the elbow. 2. Apply gel to the skin surface. 3. Place the Doppler probe over the brachial pulse 4. Inflate the cuff to approx. 20 mm/hg above the point where systolic sounds are no longer heard. 5. Deflate the cuff slowly until the arterial signal returns (systolic pressure) 6. Repeat in the other arm American Diabetes Association. Diabetes Care 2003: 26; 3333– 3341.
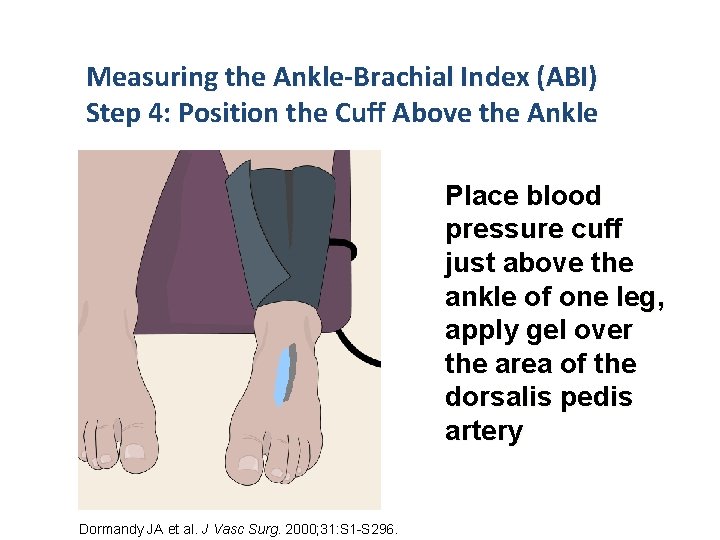
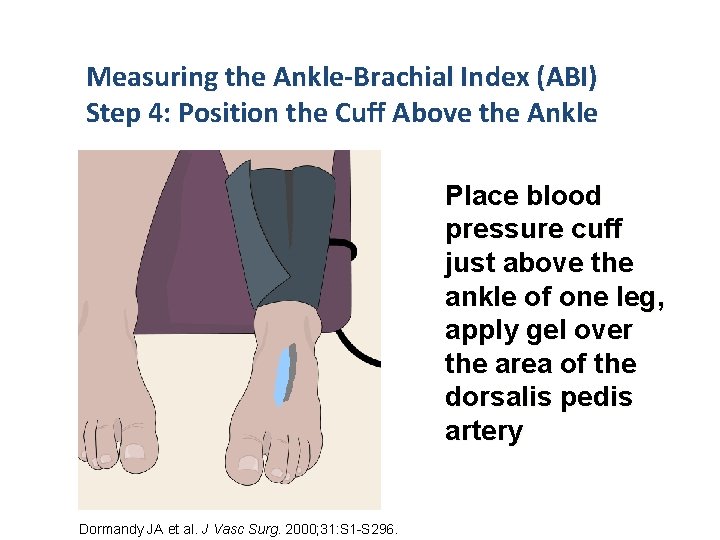
Measuring the Ankle-Brachial Index (ABI) Step 4: Position the Cuff Above the Ankle Place blood pressure cuff just above the ankle of one leg, apply gel over the area of the dorsalis pedis artery Dormandy JA et al. J Vasc Surg. 2000; 31: S 1 -S 296.
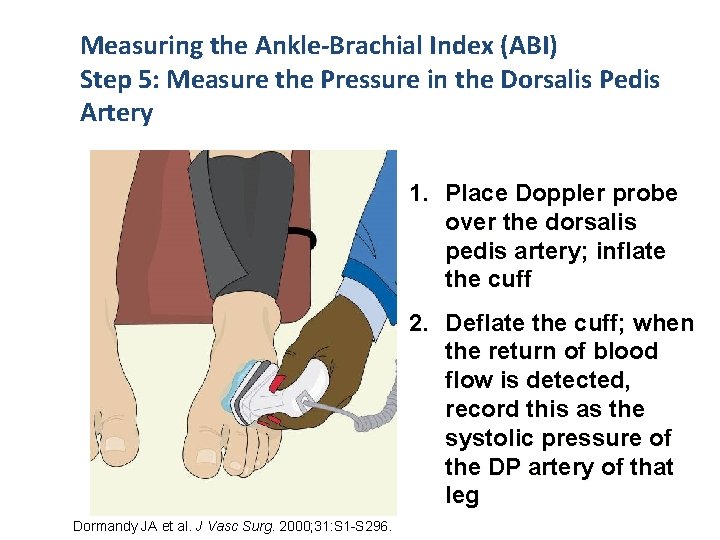
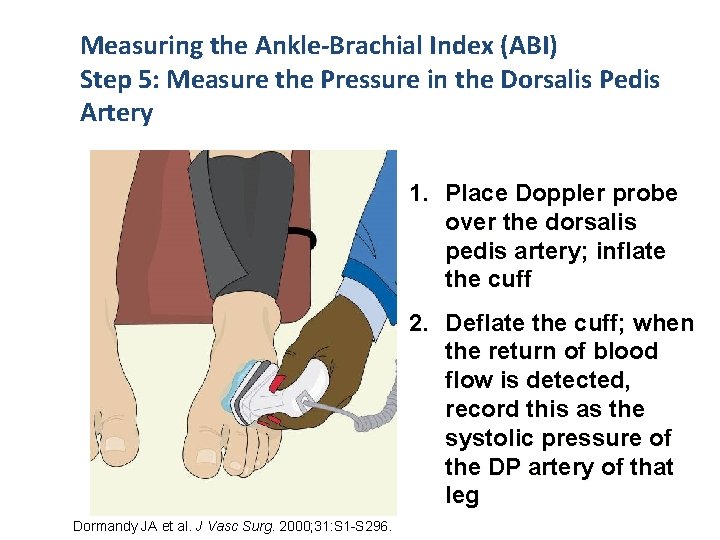
Measuring the Ankle-Brachial Index (ABI) Step 5: Measure the Pressure in the Dorsalis Pedis Artery 1. Place Doppler probe over the dorsalis pedis artery; inflate the cuff 2. Deflate the cuff; when the return of blood flow is detected, record this as the systolic pressure of the DP artery of that leg Dormandy JA et al. J Vasc Surg. 2000; 31: S 1 -S 296.
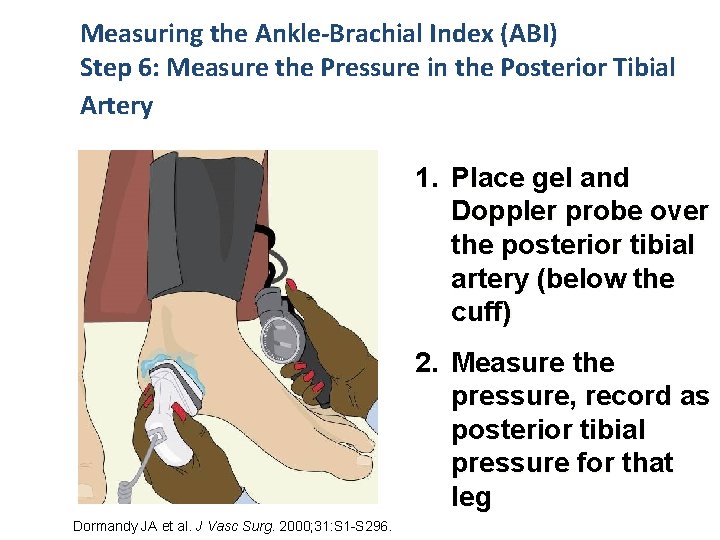
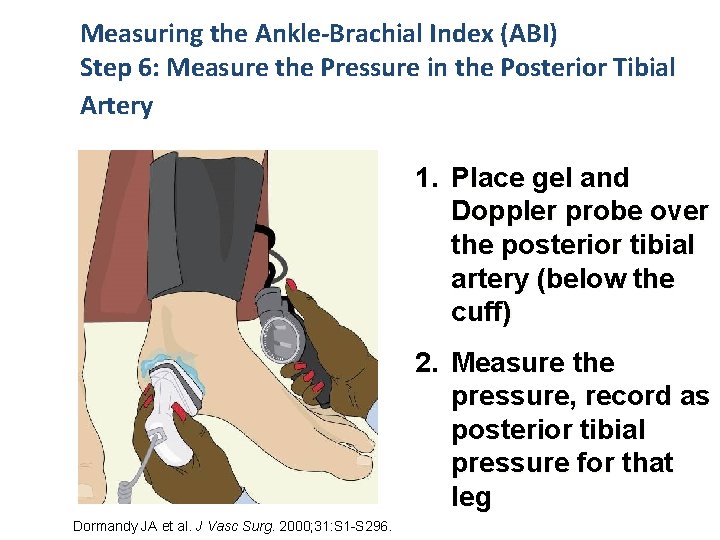
Measuring the Ankle-Brachial Index (ABI) Step 6: Measure the Pressure in the Posterior Tibial Artery 1. Place gel and Doppler probe over the posterior tibial artery (below the cuff) 2. Measure the pressure, record as posterior tibial pressure for that leg Dormandy JA et al. J Vasc Surg. 2000; 31: S 1 -S 296.
Measuring the Ankle-Brachial Index (ABI) Step 7: Repeat the Process in the Opposite Leg Repeat the same process in the other leg and record the pressures of the dorsalis pedis and posterior tibial arteries Dormandy JA et al. J Vasc Surg. 2000; 31: S 1 -S 296.
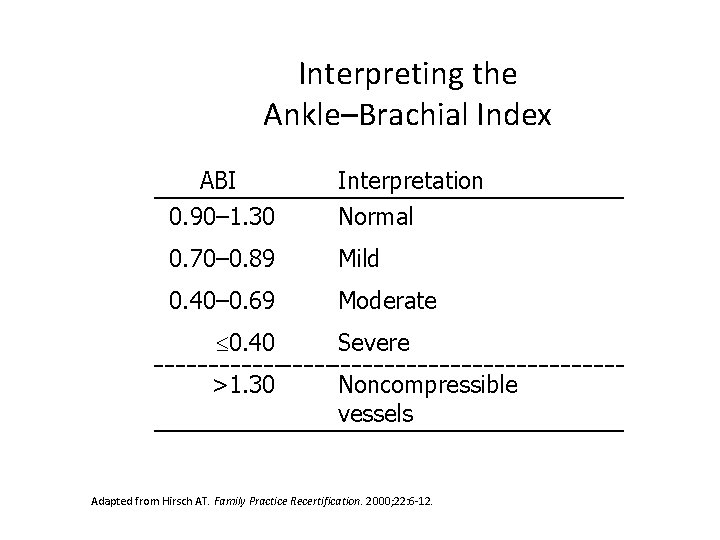
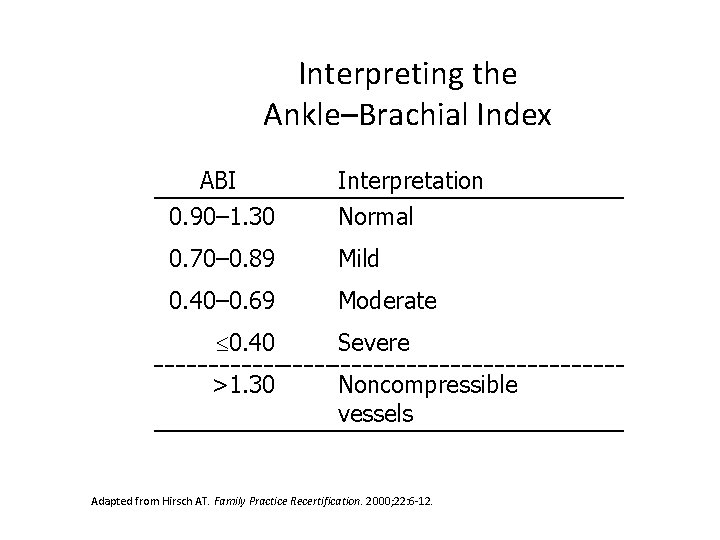
Interpreting the Ankle–Brachial Index ABI Interpretation 0. 90– 1. 30 Normal 0. 70– 0. 89 Mild 0. 40– 0. 69 Moderate 0. 40 Severe >1. 30 Noncompressible vessels Adapted from Hirsch AT. Family Practice Recertification. 2000; 22: 6 -12.
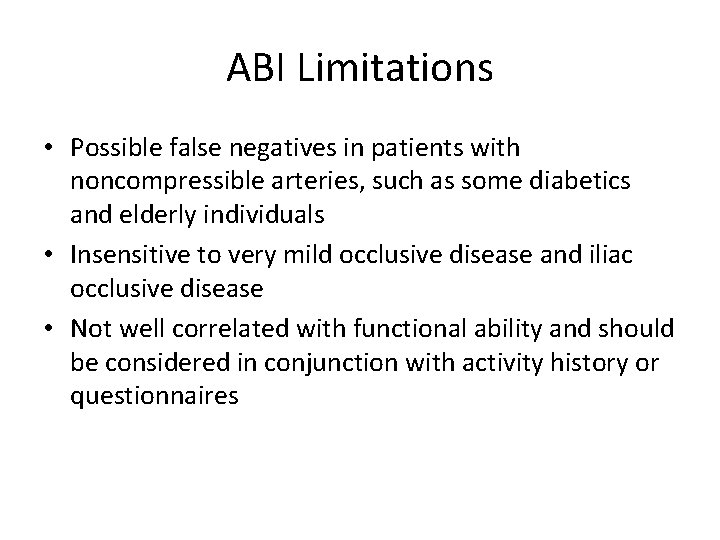
ABI Limitations • Possible false negatives in patients with noncompressible arteries, such as some diabetics and elderly individuals • Insensitive to very mild occlusive disease and iliac occlusive disease • Not well correlated with functional ability and should be considered in conjunction with activity history or questionnaires
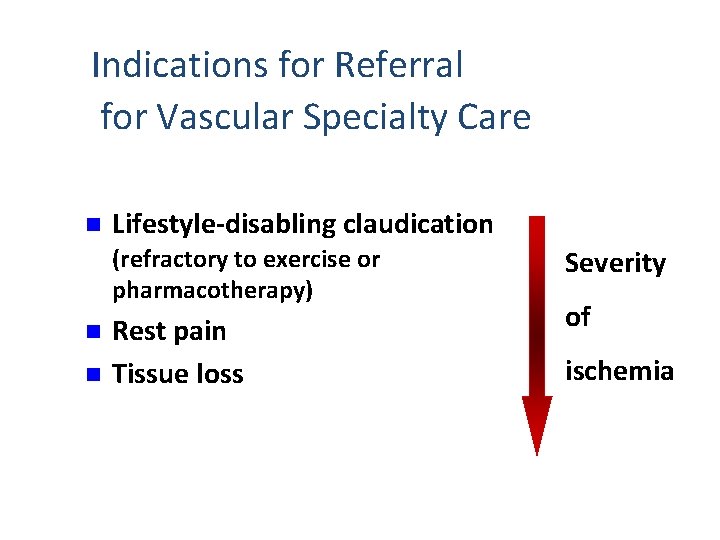
Indications for Referral for Vascular Specialty Care n Lifestyle-disabling claudication (refractory to exercise or pharmacotherapy) n n Rest pain Tissue loss Severity of ischemia
Summary • PAD is a common atherosclerotic disease associated with risk of cardiovascular ischemic events and significant functional disability • PAD can be effectively assessed in the primary care setting. • The ankle brachial index is an effective and efficient measurement tool for diagnosis of PAD • Early detection of PAD allows for appropriate disease management and decreased likelihood of ischemic events and disease progression
 Peripheral arterial disease
Peripheral arterial disease Shweta agrawal iit madras
Shweta agrawal iit madras Sujay phadke
Sujay phadke Synerzip
Synerzip Satish phadke speaker
Satish phadke speaker Pulses location
Pulses location Storied cambium
Storied cambium Communicable disease and non communicable disease
Communicable disease and non communicable disease Arterial arcades of jejunum and ileum
Arterial arcades of jejunum and ileum How to measure jvp clinically
How to measure jvp clinically Route of administration of drugs definition
Route of administration of drugs definition Blood supply to thoracic wall
Blood supply to thoracic wall Map formula bp
Map formula bp Arterial line placement
Arterial line placement Subdural hemorrhage
Subdural hemorrhage Frecuencia respiratoria en niños
Frecuencia respiratoria en niños Circulação
Circulação Valores da tensão arterial
Valores da tensão arterial Tensão arterial normal por idade
Tensão arterial normal por idade Tabela pressão arterial
Tabela pressão arterial Rias de hipertension arterial
Rias de hipertension arterial Qon ketishini vaqtincha to'xtatish usullari
Qon ketishini vaqtincha to'xtatish usullari Veia pulmonar sangue arterial
Veia pulmonar sangue arterial Arterial wave form
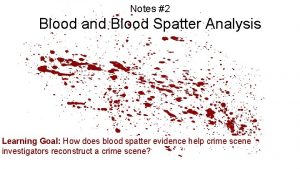
Arterial wave form 90 degree angle blood drop
90 degree angle blood drop Twin reversed arterial perfusion
Twin reversed arterial perfusion Aeromesenterie
Aeromesenterie Arterial blood vs venous blood
Arterial blood vs venous blood Cvp waveforms
Cvp waveforms R
R