ALCOHOLIC LIVER DISEASE Sadie T Velsquez M D




- Slides: 37
ALCOHOLIC LIVER DISEASE Sadie T. Velásquez, M. D.
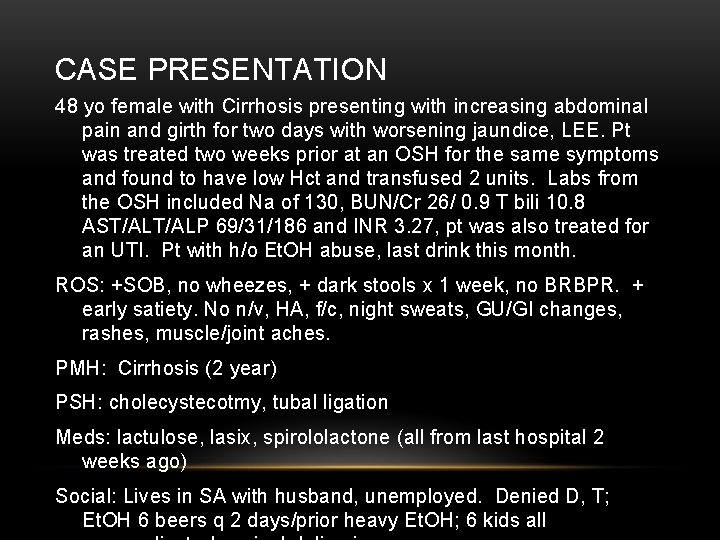
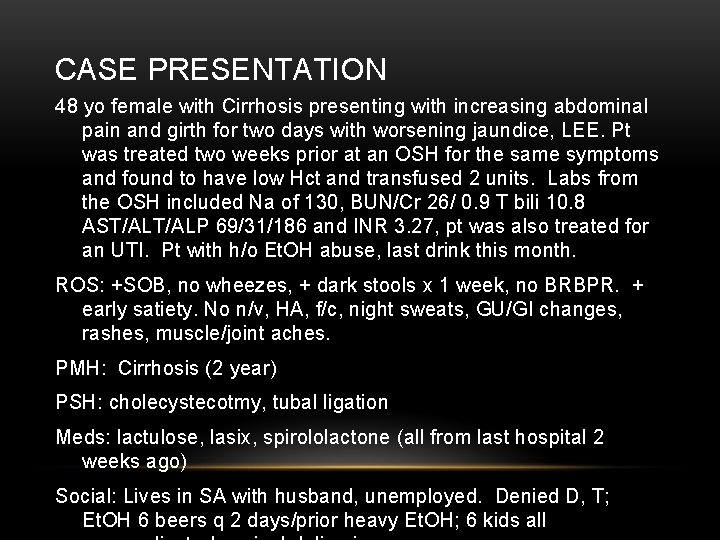
CASE PRESENTATION 48 yo female with Cirrhosis presenting with increasing abdominal pain and girth for two days with worsening jaundice, LEE. Pt was treated two weeks prior at an OSH for the same symptoms and found to have low Hct and transfused 2 units. Labs from the OSH included Na of 130, BUN/Cr 26/ 0. 9 T bili 10. 8 AST/ALP 69/31/186 and INR 3. 27, pt was also treated for an UTI. Pt with h/o Et. OH abuse, last drink this month. ROS: +SOB, no wheezes, + dark stools x 1 week, no BRBPR. + early satiety. No n/v, HA, f/c, night sweats, GU/GI changes, rashes, muscle/joint aches. PMH: Cirrhosis (2 year) PSH: cholecystecotmy, tubal ligation Meds: lactulose, lasix, spirololactone (all from last hospital 2 weeks ago) Social: Lives in SA with husband, unemployed. Denied D, T; Et. OH 6 beers q 2 days/prior heavy Et. OH; 6 kids all
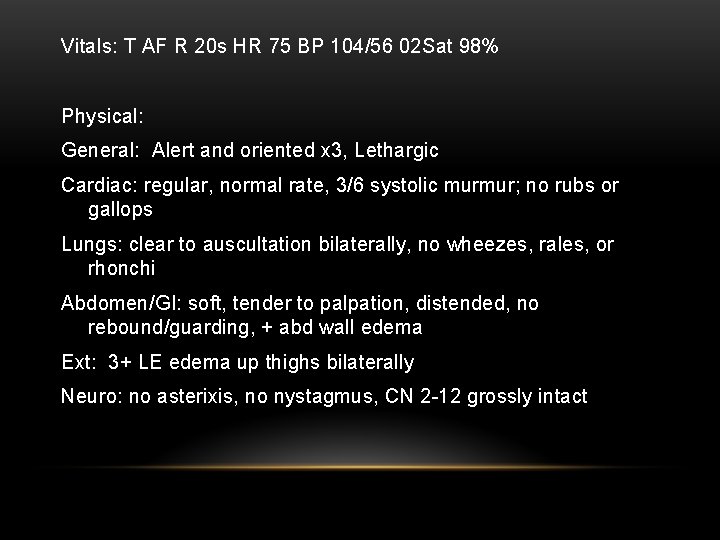
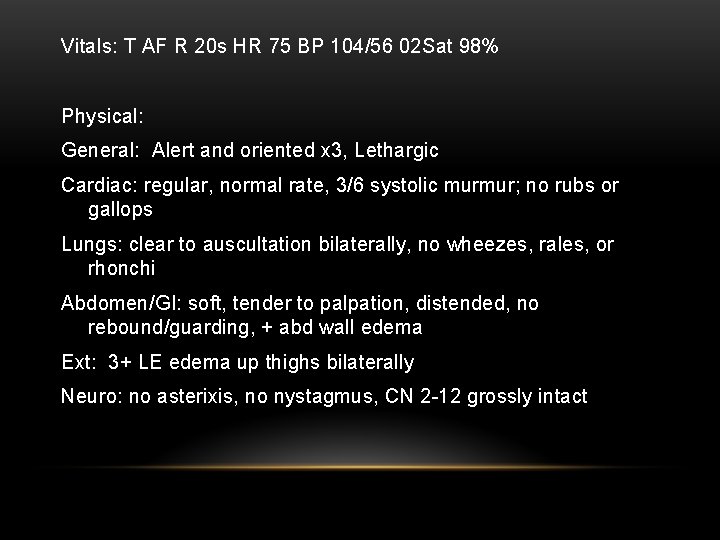
Vitals: T AF R 20 s HR 75 BP 104/56 02 Sat 98% Physical: General: Alert and oriented x 3, Lethargic Cardiac: regular, normal rate, 3/6 systolic murmur; no rubs or gallops Lungs: clear to auscultation bilaterally, no wheezes, rales, or rhonchi Abdomen/GI: soft, tender to palpation, distended, no rebound/guarding, + abd wall edema Ext: 3+ LE edema up thighs bilaterally Neuro: no asterixis, no nystagmus, CN 2 -12 grossly intact
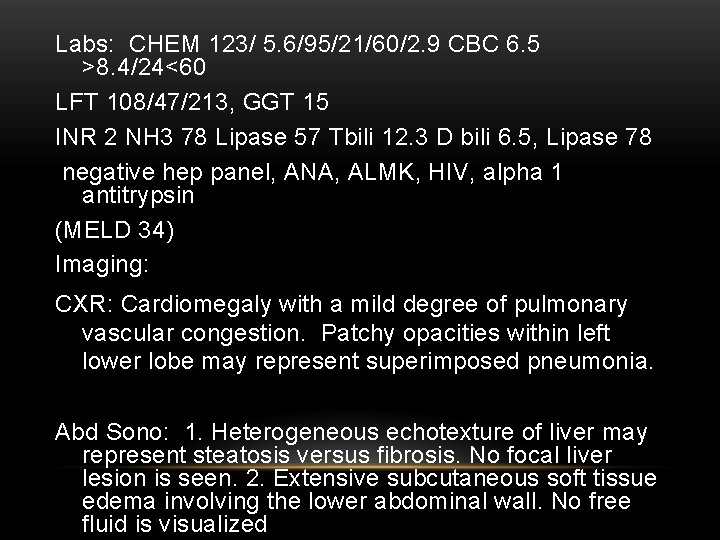
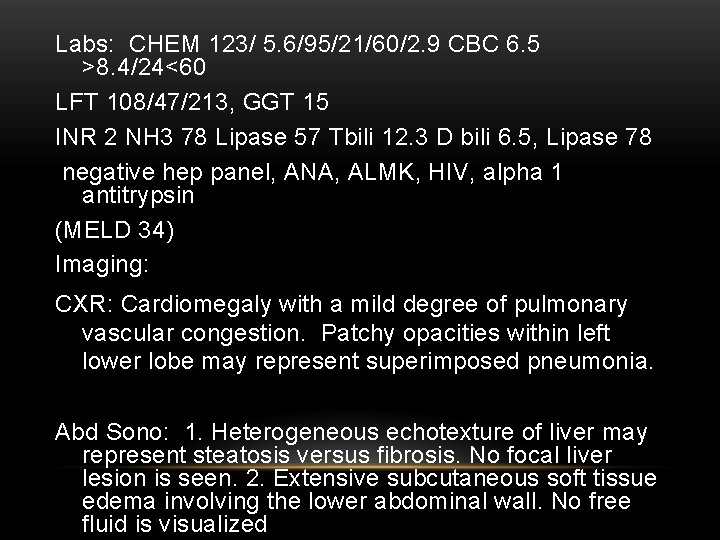
Labs: CHEM 123/ 5. 6/95/21/60/2. 9 CBC 6. 5 >8. 4/24<60 LFT 108/47/213, GGT 15 INR 2 NH 3 78 Lipase 57 Tbili 12. 3 D bili 6. 5, Lipase 78 negative hep panel, ANA, ALMK, HIV, alpha 1 antitrypsin (MELD 34) Imaging: CXR: Cardiomegaly with a mild degree of pulmonary vascular congestion. Patchy opacities within left lower lobe may represent superimposed pneumonia. Abd Sono: 1. Heterogeneous echotexture of liver may represent steatosis versus fibrosis. No focal liver lesion is seen. 2. Extensive subcutaneous soft tissue edema involving the lower abdominal wall. No free fluid is visualized
ALCOHOLIC LIVER DISEASE AASLD Practice Guidelines
OBJECTIVES • Metabolism of Alcohol • Genetics of Alcohol abuse • Risk factors for Alcoholic Liver Disease • Screening • Diagnosis • Prognosis • Treatment
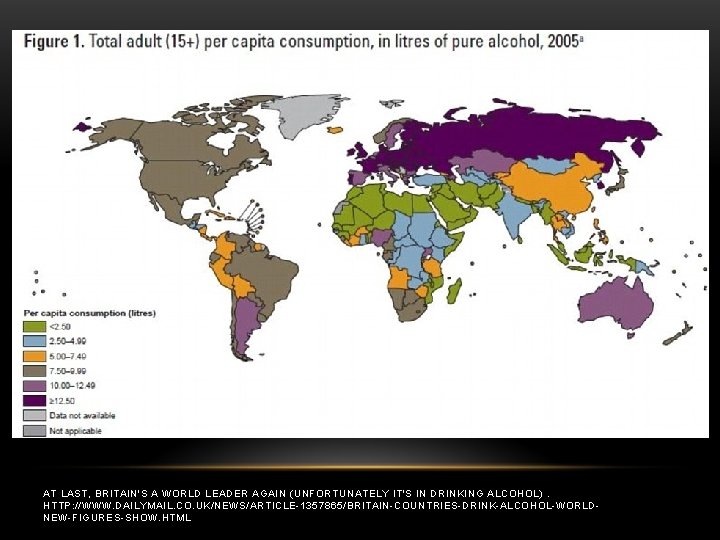
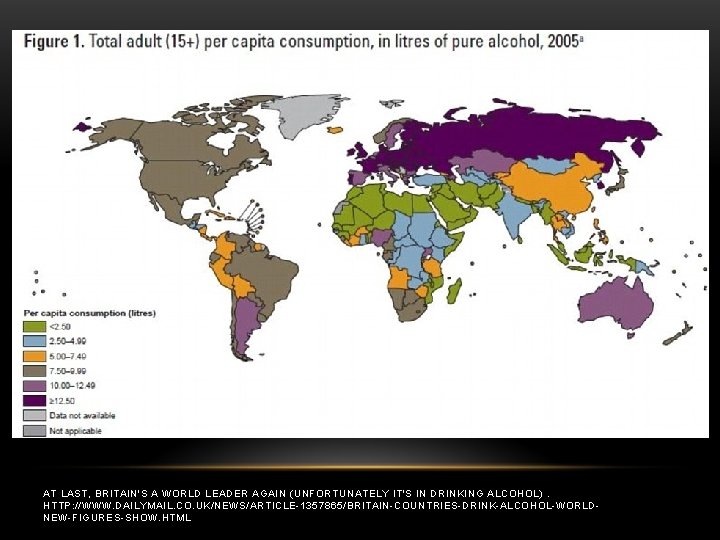
AT LAST, BRITAIN'S A WORLD LEADER AGAIN (UNFORTUNATELY IT'S IN DRINKING ALCOHOL). HTTP: //WWW. DAILYMAIL. CO. UK/NEWS/ARTICLE-1357865/BRITAIN-COUNTRIES-DRINK-ALCOHOL-WORLDNEW-FIGURES-SHOW. HTML
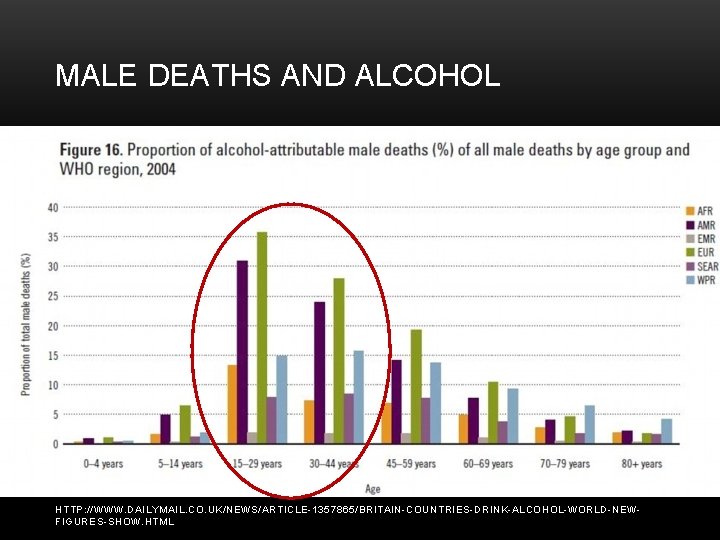
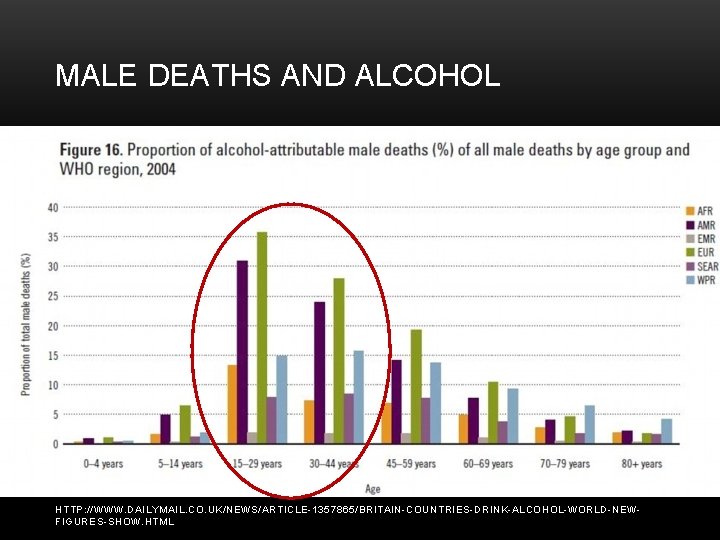
MALE DEATHS AND ALCOHOL HTTP: //WWW. DAILYMAIL. CO. UK/NEWS/ARTICLE-1357865/BRITAIN-COUNTRIES-DRINK-ALCOHOL-WORLD-NEWFIGURES-SHOW. HTML
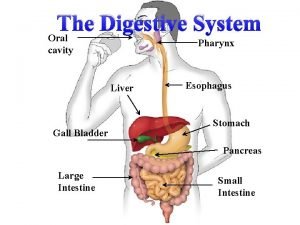
HOW DOES ALCOHOL DAMAGE THE LIVER?
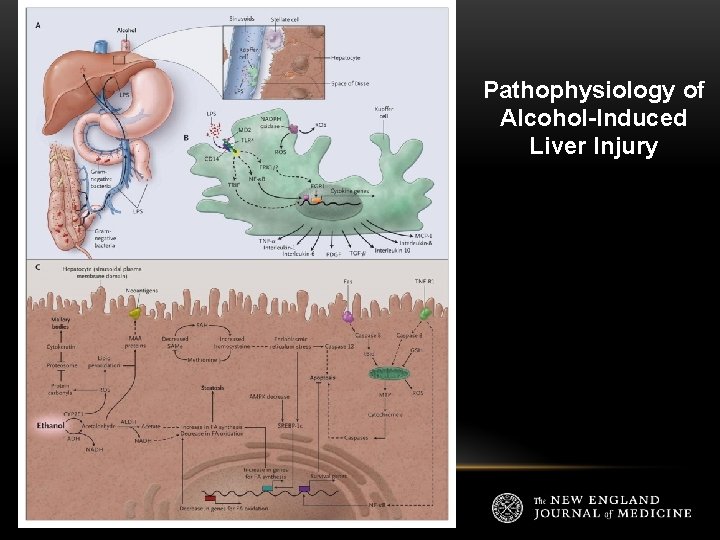
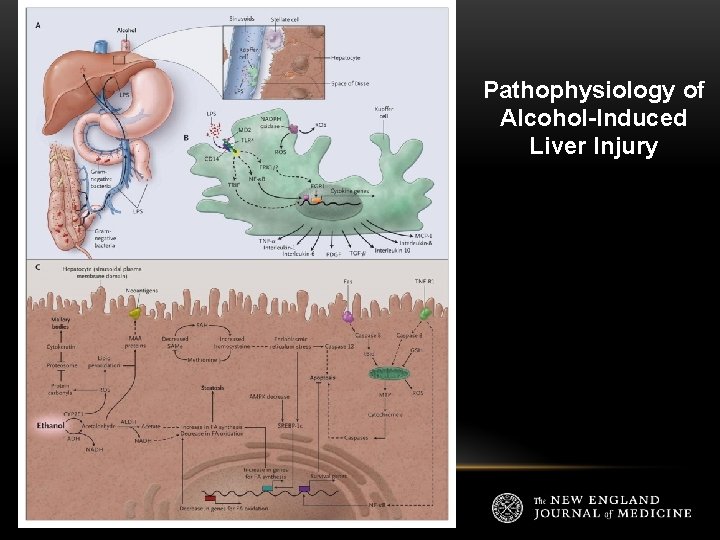
Pathophysiology of Alcohol-Induced Liver Injury
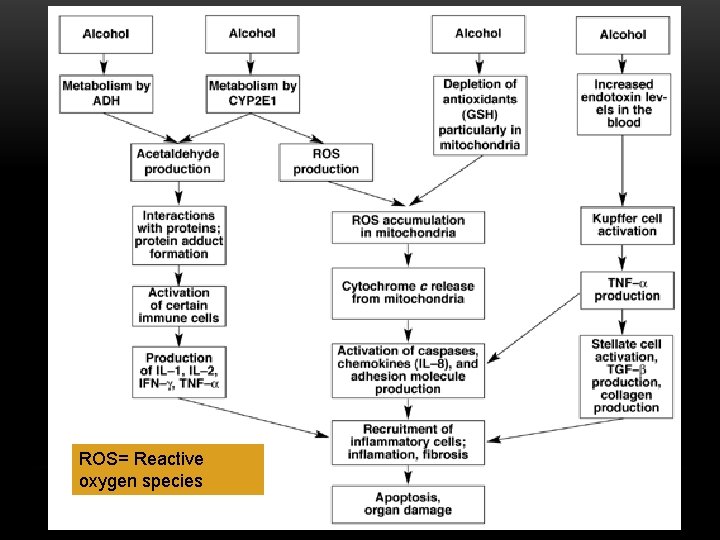
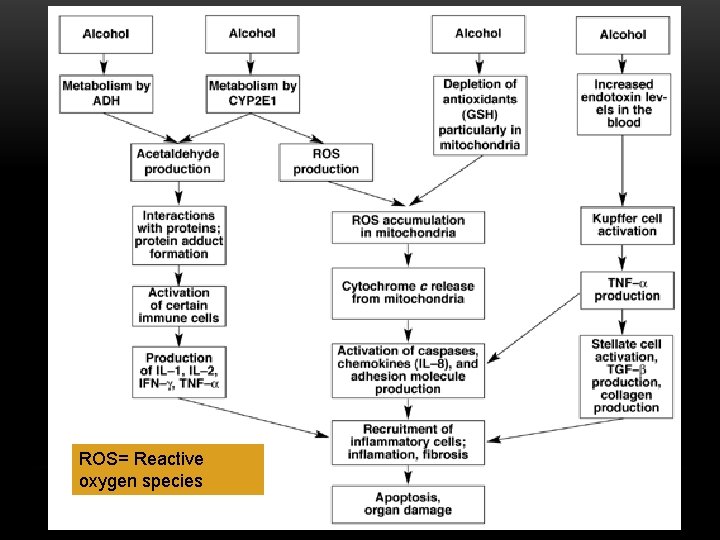
ROS= Reactive oxygen species
WHY DO SOME GET ALD AND OTHERS DON’T?
GENETICS OF ALCOHOL ABUSE/ALD • In the 70 s, they found that up to a third of confirmed alcoholics have completely normal liver histology. • In the 1980 s, Hrubec and Omenn found evidence supporting a genetic component to predisposition from a large study of 15924 male twin pairs. The concordance rate for alcoholic cirrhosis was 14. 6% in monozygotic twins and 5. 4% in dizygotic twins. • In 1992, Day noted that ‘why only a few alcoholics develop significant liver disease remains largely a mystery’ and also discusses the idea of a ‘polygenic’ disorder and the using a molecular genetic approach to identify those at ‘high risk’ for ALD. • Uhl maps out genes in 2001 in drug abusers supporting polygenic contributions of common allelic variants to polysubstance abuse vulnerability.
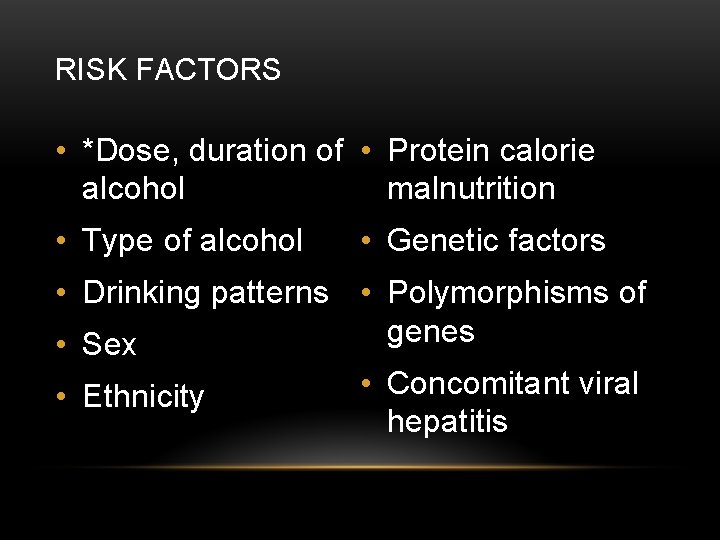
RISK FACTORS • *Dose, duration of • Protein calorie alcohol malnutrition • Type of alcohol • Genetic factors • Drinking patterns • Polymorphisms of genes • Sex • Ethnicity • Concomitant viral hepatitis
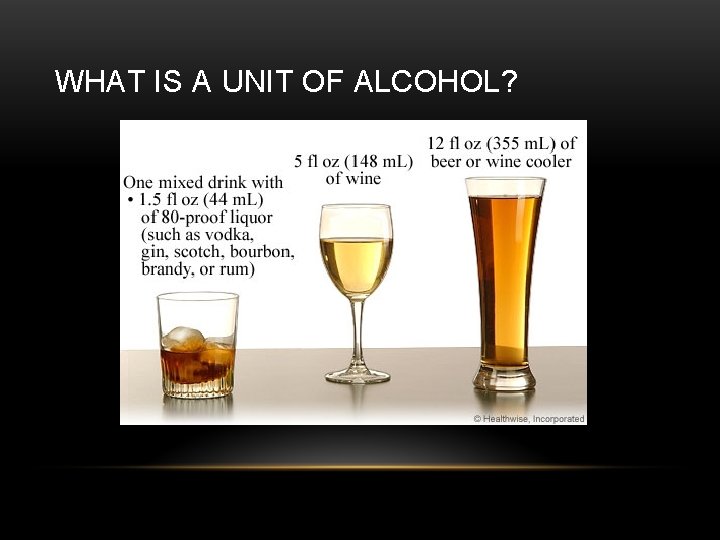
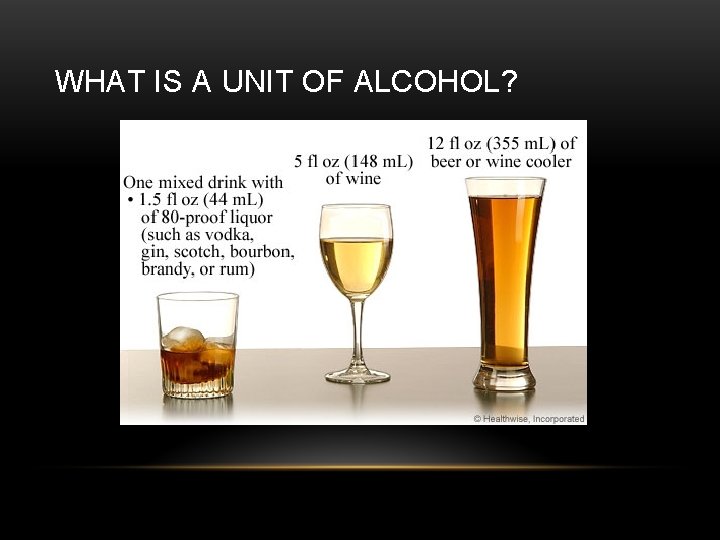
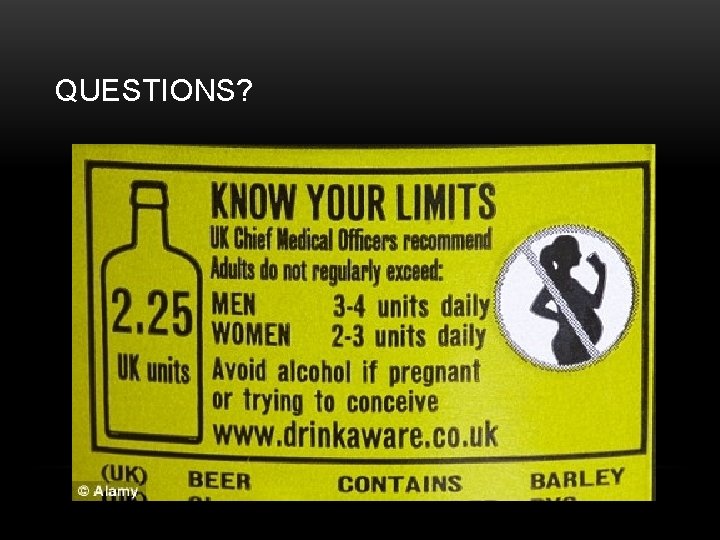
WHAT IS A UNIT OF ALCOHOL?

SCREENING FOR ALCOHOL ABUSE • CAGE Questionnaire 1. Have you ever felt you should CUT down on your drinking? 2. Have people ANNOYED you by criticizing your drinking? 3. Have you ever felt GUILTY about your drinking? 4. Have you ever had a drink first thing in the morning to steady your nerves or to get rid of a hangover (EYE-OPENER)? • (EACH REPSONSE 0 OR 1 → ≥ 2 IS SIGNIFICANT) • Sensitivity of 71% and specificity of 90%
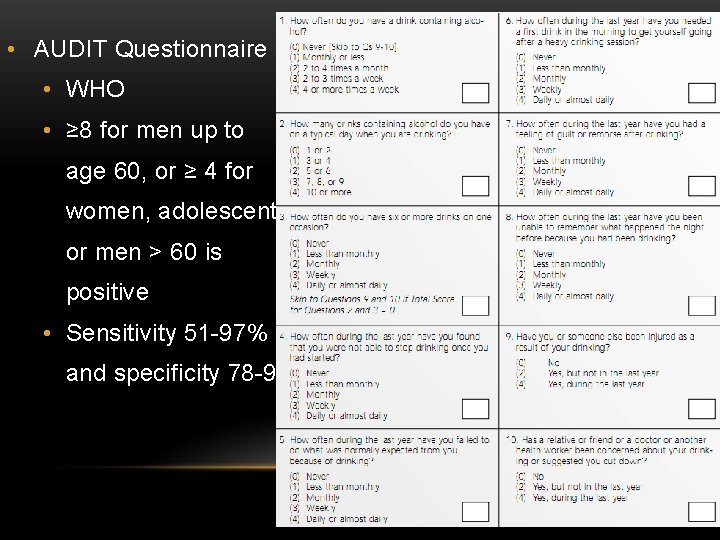
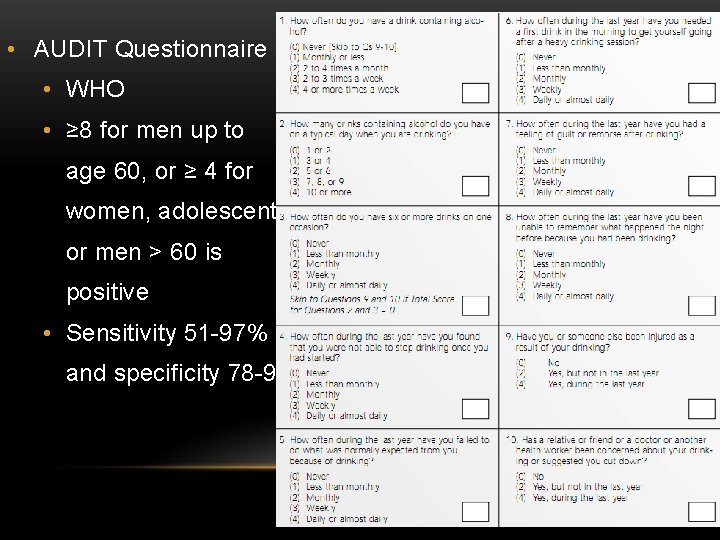
• AUDIT Questionnaire • WHO • ≥ 8 for men up to age 60, or ≥ 4 for women, adolescents or men > 60 is positive • Sensitivity 51 -97% and specificity 78 -96%
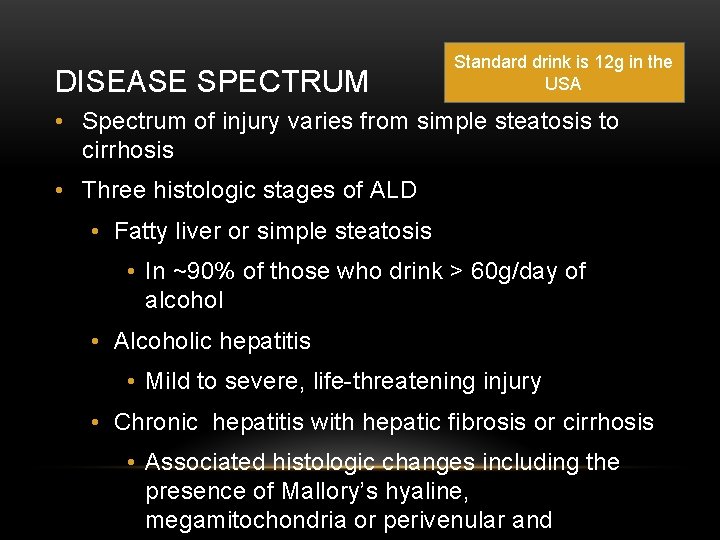
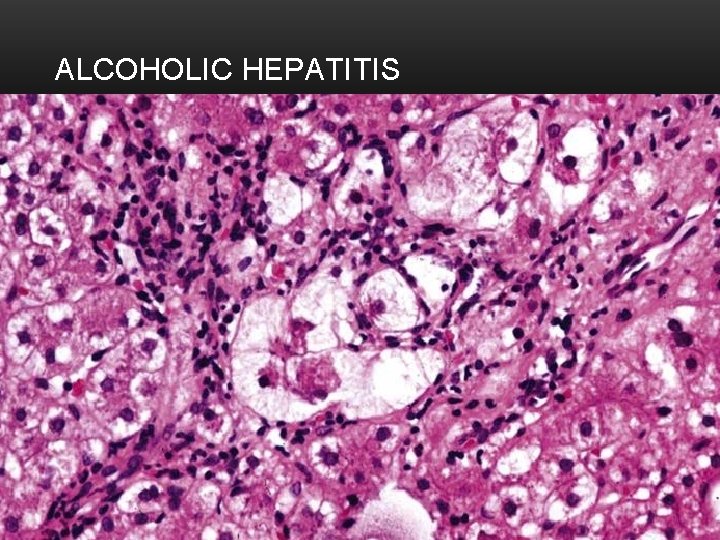
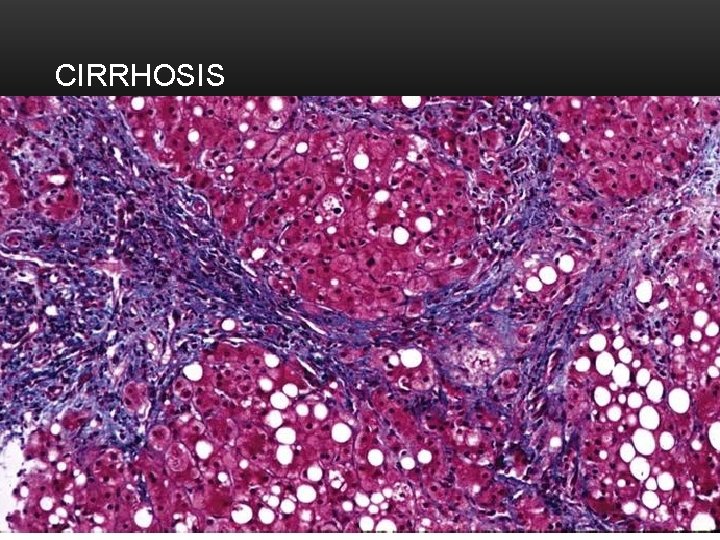
DISEASE SPECTRUM Standard drink is 12 g in the USA • Spectrum of injury varies from simple steatosis to cirrhosis • Three histologic stages of ALD • Fatty liver or simple steatosis • In ~90% of those who drink > 60 g/day of alcohol • Alcoholic hepatitis • Mild to severe, life-threatening injury • Chronic hepatitis with hepatic fibrosis or cirrhosis • Associated histologic changes including the presence of Mallory’s hyaline, megamitochondria or perivenular and
DIAGNOSIS • History of significant alcohol intake • Clinical evidence of liver disease • Supporting laboratory abnormalities • May have elevated GGT, macrocytosis • AST typically 2 -6 x normal • AST/L ratio >2 in 70%, but greater value in patients without cirrhosis • Need to rule-out other etiologies of liver disease
DIAGNOSIS • Physical exam may be normal or suggest advanced cirrhosis • Exam findings most common with ALD: • Parotid enlargement • Dupuytren’s contracture • Feminization • HE • Ascites • Spider nevi • Weakness • Edema

DIAGNOSIS • Hepatic imaging: Ultrasound, CT or MRI • Value is to exclude other causes of abnormal liver tests • Higher volume index of the caudate lobe, more frequent visualization of the R posterior hepatic notch and smaller size of regenerative nodules of the liver are suggestive findings • Liver biopsy • Confirm the diagnosis • Convey prognostic importance • If no treatment for ALD or AH is contemplated, it usually is not necessary to make a histologic diagnosis
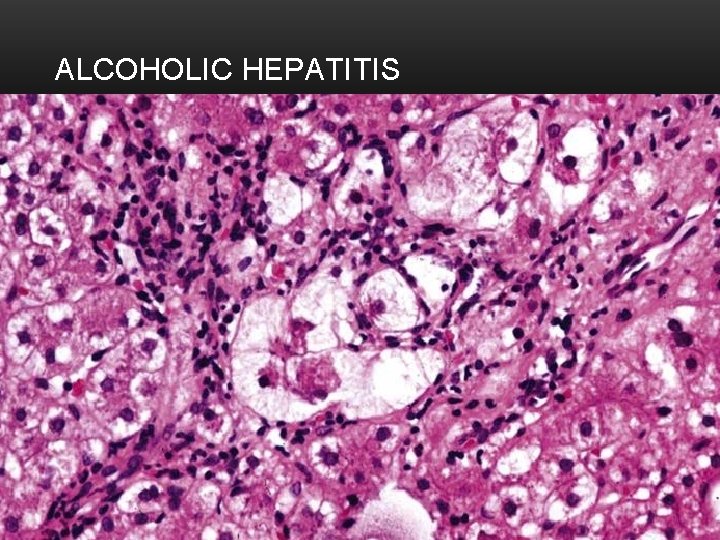
ALCOHOLIC HEPATITIS
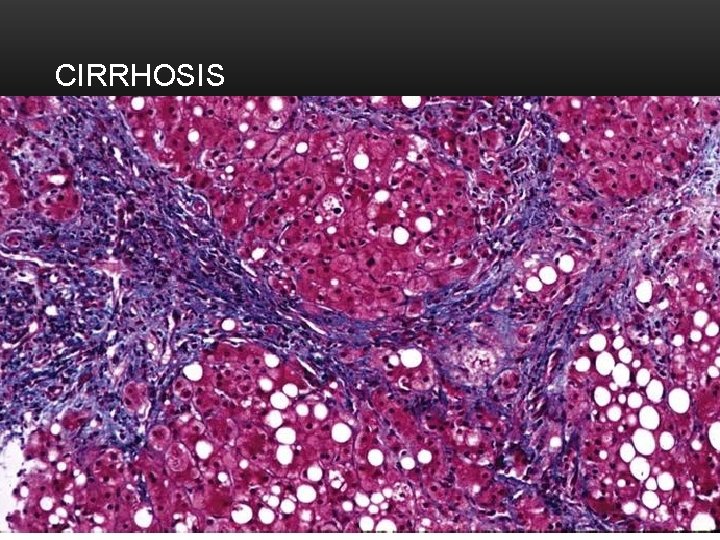
CIRRHOSIS
PROGNOSIS • Maddrey’s discriminant function (MDF) • MELD score • Glasgow Alcoholic Hepatitis score
PROGNOSIS • Maddrey’s discriminant function (MDF) • 4. 6 (Patient’s prothrombin time – control prothrombin time) + total bilirubin • ≥ 32 have the highest risk of dying with 30 day mortality of 30 -50% • HE and elevated MDF were at the highest risk • Sensitivity ~ 83 -86%, specificity 48 -60%
PROGNOSIS • MELD score • 3. 8 x log(bilirubin in mg/d. L) + 11. 2 x log(INR) + 9. 6 x log(creatinine) + 6. 4 • Poor prognosis if >18 • Change of ≥ 2 in the first week independently predicts in-hospital mortality • Sensitivity ~85%, specificity ~ 84%
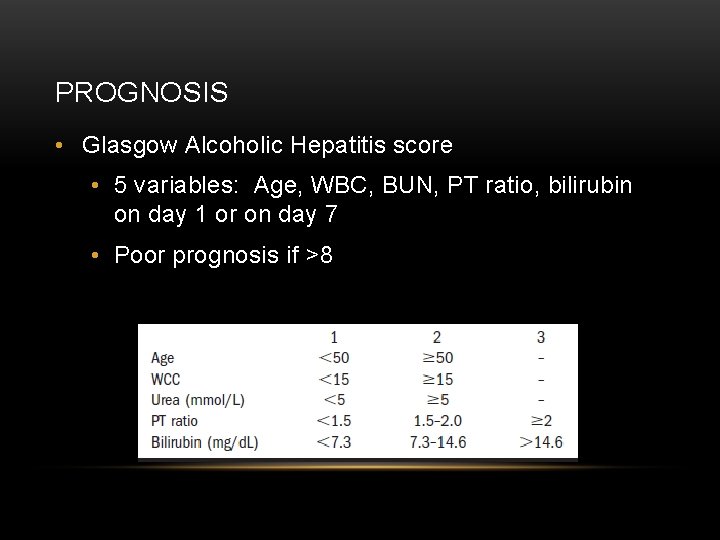
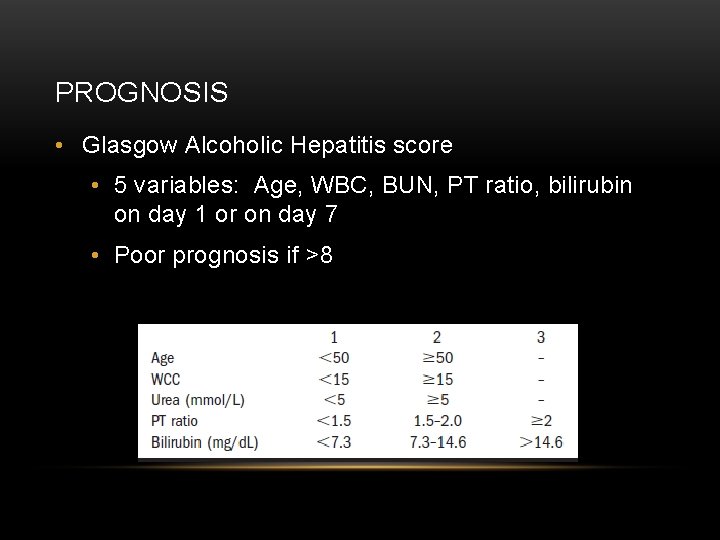
PROGNOSIS • Glasgow Alcoholic Hepatitis score • 5 variables: Age, WBC, BUN, PT ratio, bilirubin on day 1 or on day 7 • Poor prognosis if >8
TREATMENT • Abstinence • Naltrexone or acamprosate may be considered in combination with counseling • Nutritional therapy • Steroids • Anticytokine Therapy • Combination therapy • Liver transplantation
TREATMENT- STEROIDS • MDF ≥ 32 +/- HE without contraindications • Prednisolone 40 mg/day for 4 weeks then tapered over 2 -4 weeks • Recent study in NEJM on NAC + prednisolone • If steroids contraindicated, consider pentoxifylline therapy


Establish disease severity Low Risk: MDF <32 and 1 st week decrease in bilirubin, or MELD <18 and 1 st week decrease on MELD by 2 points High Risk: MDF≥ 32, presence of HE or MELD ≥ 18 Nutritional Assessment/Intervent ion Supportive Care and Close Follow-up Consider Liver Biopsy if Diagnosis is uncertain Prenisolone If steroids contraindicated or early renal failure: Pentoxifyline
LIVER TRANSPLANTATION • ALD is the second most common indication for liver transplantation in the Western world • 95% of those with ESLD related to alcohol are never formally evaluated for LT • 6 -month period of abstinence is recommended for listing • Overall survival rates similar between alcohol-related and other LT recipients • Transplant recipients for alcoholic liver disease are highly likely to drink after transplantation (11 -49%), but only a small fraction revert to heavy use or abuse
SUMMARY • Screen for alcohol use and evaluate those with evidence of liver disease • Rule-out other etiologies of liver disease • Consider liver biopsy if contemplating tx or uncertainty of the dx • Risk stratify using MDF and MELD • Encourage abstinence +/- medical therapy • Assess for nutritional, vitamin, mineral deficiencies in AH or advanced ALD and treat aggressively • Steroids for severe disease, MDF ≥ 32, or pentoxifylline • Frequent interval feedings to improve nitrogen balance in patients with alcoholic cirrhosis • Consider appropriate patients for LT
REFERENCES • O'Shea RS, Dasarathy S, Mc. Cullough AJ; Practice Guideline Committee of the American Association for the Study of Liver Diseases; Practice Parameters Committee of the American College of Gastroenterology. Alcoholic liver disease. Hepatology. 2010 Jan; 51(1): 307 -28. • Uhl GR, Liu QR, Walther D, Hess J, Naiman D. Polysubstance abusevulnerability genes: genome scans for association, using 1, 004 subjects and 1, 494 single-nucleotide polymorphisms. Am J Hum Genet 2001; 69: 1290 -1300. • Brown K. Alcohol hepatotoxicity: a genotypic predisposition? Am J Gastroenterol 1992; 87: 677 -678. • Day CP, Bassendine MF. Genetic predisposition to alcoholic liver disease. Gut 1992; 33: 1444 -1447. • Goodwin DW, Schulsinger F, Hermansen L, Guze SB, Winokur G. Alcohol problems in adoptees raised apart from alcoholic biological parents. Arch Gen Psychiatry 1973; 28: 238 -243. • Glucocorticoids plus N-acetylcysteine in Severe Alcoholic Hepatitis. NEJM 2011 Nov 10; 365; 19: 1781 -1789. • Reed T, Page WF, Viken RJ, Christian JC. Genetic predisposition to organ-specific endpoints of alcoholism. Alcohol Clin Exp Res 1996; 20: 1528 -1533. • Mathurin P, Abdelnour M, Ramond MJ, Carbonell N, Fartoux L, Serfaty L, et al. Early change in bilirubin levels is an important prognostic factor in severe alcoholic hepatitis treated with prednisolone. HEPATOLOGY 2003; 38: 1363 -1369. • Schuckit. New Findings in the Genetics of Alcoholism. JAMA 1999; 281: 1875 -1876.
QUESTIONS?
 Non-alcoholic fatty liver disease (nafld)
Non-alcoholic fatty liver disease (nafld) Cirrhosis
Cirrhosis Sadie is so fearful of being overwhelmed
Sadie is so fearful of being overwhelmed Sadie kopelman
Sadie kopelman Jason is so preoccupied with staying clean
Jason is so preoccupied with staying clean Inokuchi shunt
Inokuchi shunt Features of cld
Features of cld Defination of liver
Defination of liver Gastroenterology board review
Gastroenterology board review Peripheral stigmata of cld
Peripheral stigmata of cld Gennifer shafer liver disease
Gennifer shafer liver disease Stigmata of chronic liver disease
Stigmata of chronic liver disease Nonalcoholic fatty liver disease
Nonalcoholic fatty liver disease Infiltrative liver disease
Infiltrative liver disease Why does liver disease cause splenomegaly
Why does liver disease cause splenomegaly Communicable disease and non communicable disease
Communicable disease and non communicable disease Alcoholic hepatitis
Alcoholic hepatitis Alcoholic ketoacidosis
Alcoholic ketoacidosis Hydroalcoholic solution are
Hydroalcoholic solution are Anne dymek
Anne dymek Alcoholic fermentation steps
Alcoholic fermentation steps What is alcoholic fermentation
What is alcoholic fermentation Genogram symbols
Genogram symbols Turkish drinks non alcoholic
Turkish drinks non alcoholic Division of alcoholic beverages and tobacco
Division of alcoholic beverages and tobacco Alcoholic brain vs normal brain
Alcoholic brain vs normal brain White liniment turpentine oil
White liniment turpentine oil Carcinoid tumor metastatic liver prognosis
Carcinoid tumor metastatic liver prognosis Larynx function in digestive system
Larynx function in digestive system Porta hepatis
Porta hepatis Chapter 58 care of patients with liver problems
Chapter 58 care of patients with liver problems Liver lobules
Liver lobules Esophagogastric junction
Esophagogastric junction Coarse echotexture
Coarse echotexture Normal range alkaline phosphatase in child
Normal range alkaline phosphatase in child Liver cancer symptons
Liver cancer symptons Glisson üçgeni
Glisson üçgeni Acute liver failure criteria
Acute liver failure criteria