Understanding alcoholic liver disease Dr Jack Leach Lead

- Slides: 20
Understanding alcoholic liver disease Dr Jack Leach Lead doctor, Smithfield services, Manchester, ARCH Initiatives, Merseyside General practitioner, St Helens and Bolton RCGP co-lead for alcohol training
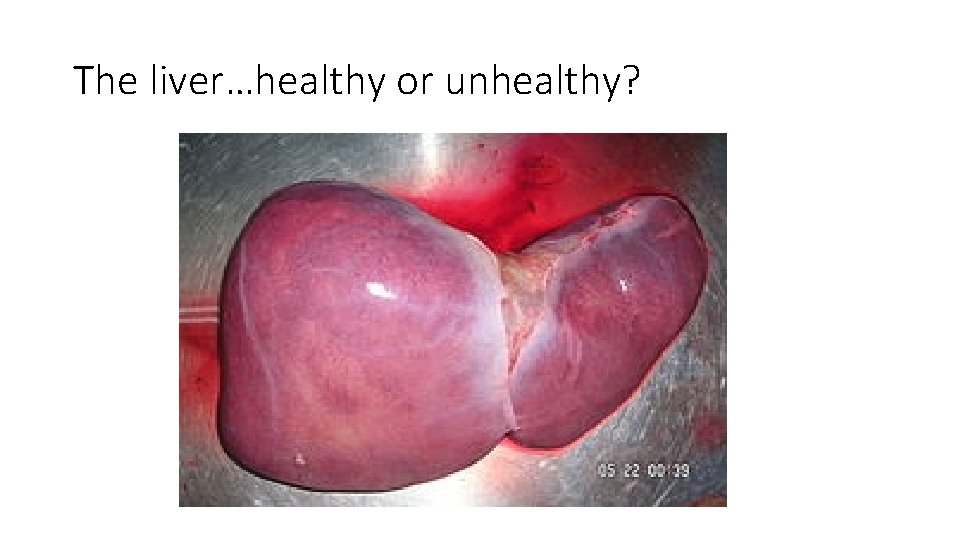
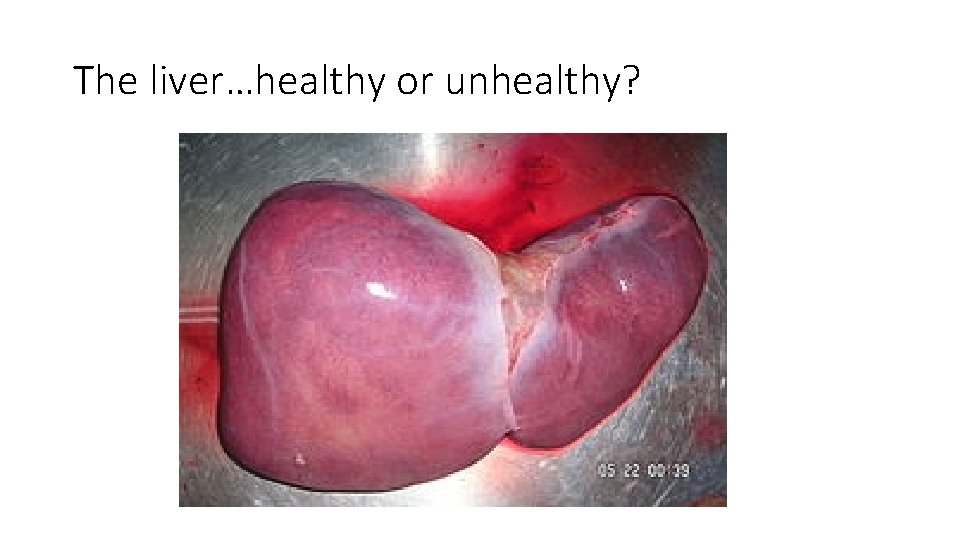
The liver…healthy or unhealthy?
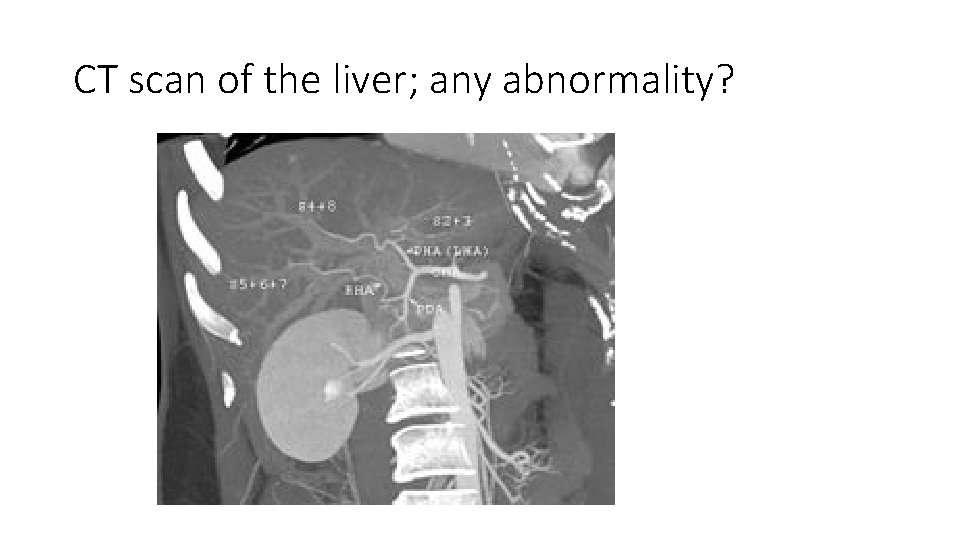
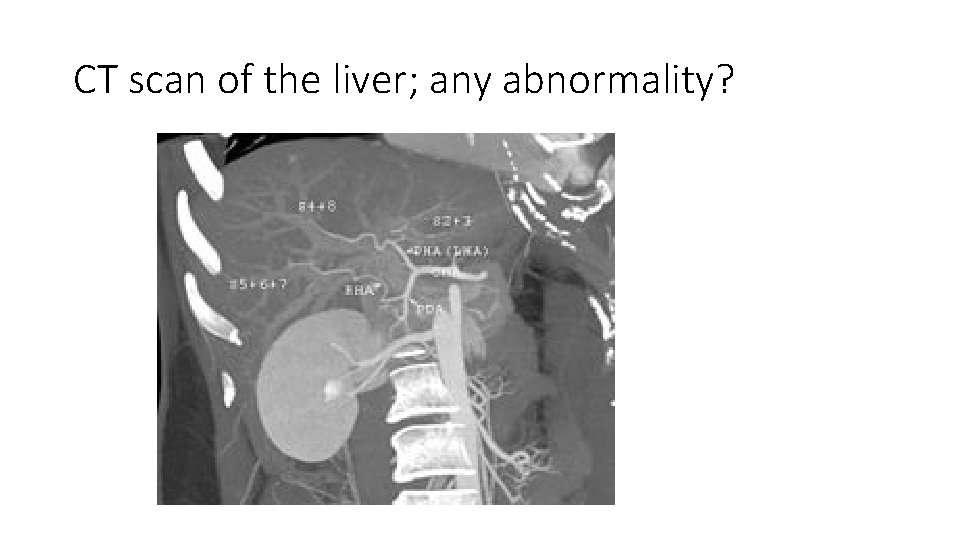
CT scan of the liver; any abnormality?
Alcoholic liver disease is a confusing area! I and I believe many health professionals in the alcohol field find alcoholic liver disease complicated and confusing. This presentation is an attempt to explain alcoholic liver disease in a simple and practically way. One reminder and six questions: Reminder; alcohol dependence is neither necessary nor sufficient for alcoholic liver disease. Dependent drinkers do not always have significant liver disease. Alcoholic liver disease may occur in non-dependent drinkers, though it is considerably commoner amongst them. Alcohol may cause acute and chronic toxic effects to the liver. The severity of chronic liver disease is related to the amount and duration of drinking, the patient’s vulnerability to liver damage and any associated liver disease.

SIX questions: 1. 2. 3. 4. 5. 6. Why is alcoholic liver disease important? How do you identify alcoholic liver disease? How do you assess the severity of liver disease How can liver disease be classified in a simple and practical way? Does stopping or reducing drinking improve chronic liver disease? What treatment is there for advanced liver disease?
1. Why is alcoholic liver disease important? • Problem drinking considerably increases risk of premature death (Valliant 1983) • Alcoholic liver disease is a major cause of illness and death worldwide. Disproportionately affecting deprived communities and the young (Babor 2003) • In England the commonest recorded cause of death from alcohol related disease is liver disease. Accounts for 2% of all cause deaths (12, 000). The death rate has been increasing. 70% of people dying from alcoholic liver disease do so in hospital (National end of life care network 2012, NHSIC 2012) • Alcohol is a major cause of physical, psychological and social illness, reducing quality of life and increasing health service use (Babor 2003, NHSIC 2012). In 2010 there were 43, 100 hospital admissions from alcoholic liver disease • Chronic alcoholic liver disease has a long and progressive course • Alcoholic liver disease is potentially preventable and treatable.
2. How do you identify liver disease? • Sub-clinical liver disease: Need a high degree of suspicion where there is prolonged and excessive drinking. Vaguely unwell with abnormal liver function tests. • Clinical liver disease: Unwell with signs of liver cell failure and portal hypertension. Consider other causes of liver disease and co-existing disease (NICE 2010). For example, viral and drug induced hepatitis, auto-immune hepatitis, liver and biliary tract cancer, biliary tract disease (e. g. gallstones) and metabolic diseases such as haemochromoatosis, Wilson’s disease and diabetes.
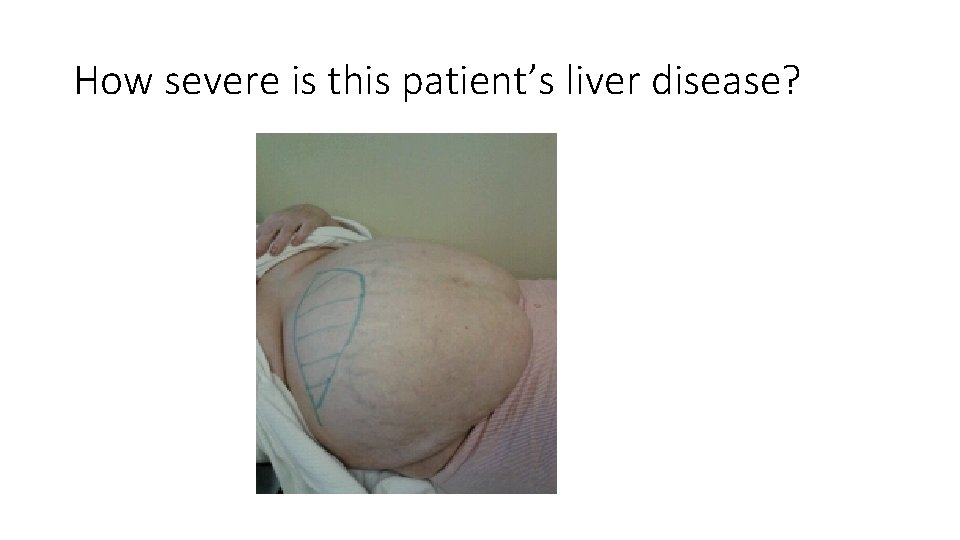
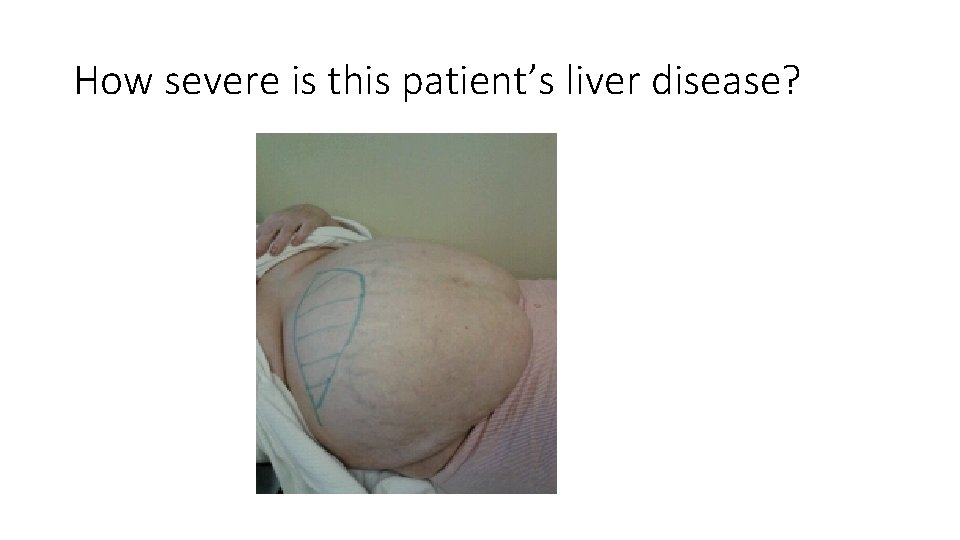
How severe is this patient’s liver disease?
3. How do you assess the severity of liver disease? Consider whether the patient has acute on chronic liver disease or chronic liver disease. Patients with acute liver cell failure are extremely unwell and need urgent hospital treatment. The severity of chronic alcoholic liver disease is assessed by: 1. Clinical assessment 2. Liver function tests 3. Special investigations e. g. ultrasound, fibroscan, MRI/CT and liver biopsy Validated scoring systems have been developed by liver transplant centres to measure the severity of liver disease and corresponding risk of death, such as the Child Pugh and model for end-stage liver disease (MELD) scales.
a. Clinical assessment • Signs of hepatitis (inflammation) Enlarged and tender liver • Signs of liver cell failure: • • • Features of excessive oestrogen e. g. spider naevi, gynaecremastia Failure to metabolise bilirubin; Jaundice Inadequate metabolism of fats, carbohydrates and protein; loss of weight, muscle wasting Hypoalbinaemia; with secondary congestive heart failure Failure to clear waste products; encephalopathy • Signs of portal hypertension: • • Ascites Oesophageal varices Enlarged spleen haemorroids
b. Liver function tests; how they confuse people! 1. Measures of inflammation: • Liver cell enzymes (GGT, ALT, CDT) 2. Measures of liver cell failure; production: • Low serum albumin • Prolonged prothrombin time (PT) 3. Measures of liver cell failure; clearance: • High total serum bilirubin 4. Measures of hepato-renal syndrome and electrolyte disturbance; • Serum electrolytes and creatinine
4. How can liver disease be classified in a simple and useful way? • Array of confusing terms. For example, fatty liver, alcoholic hepatitis, cirrhosis, compensated and decompensated liver disease. • From a practical purposes I believe useful to classify into three groups: 1. Acute liver failure • Features of liver cell failure, severe acute inflammation with disturbance of portal blood flow. • There is considerable risk of death • May be provoked by alcohol binge, detox, acute illness or severe infection • Unwell within short period (days) with symptoms such as vomiting, confusion, jaundice, abdominal pain and rapid increase in girth from ascites, electrolyte disturbance and risk of hepato-renal syndrome.
2, Mild chronic liver disease • Features of inflammation, liver function maintained • abnormal liver function tests; high liver enzymes (may be very high) but normal serum bilirubin, albumin and prothrombin time • Enlarged firm, non-tender liver. Not “ill” and no clinical features of liver disease 3. Severe chronic liver disease • Features of chronic liver cell failure and of disturbing liver architecture from fibrosis (cirrhosis) • Abnormal liver function tests; liver enzymes may be normal but high serum bilirubin, low serum albumin and prolonged prothrombin time • Clinical features of liver disease • Matter of urgency to reduce and ideally stop drinking. Advice of hepatologist.
5. What effect does stopping and reducing drinking have on severe liver disease? Stopping drinking can considerably and quickly improve liver function. This organ has remarkable regenerative ability. Even if a patient can not stop drinking but can reduce their consumption significantly, the decline in liver function may not only reduce but cease or even improve (dose related toxic effect of alcohol).
Is alcoholic cirrhosis irreversible? There is a widespread view that established cirrhosis is irreversible. BUT Alcoholic liver disease is a major reason for liver transplantation internationally (Abdul-Wahed 2010) Many transplant centres have a requirement of six months or more abstinence from drinking before they will carry out liver transplantation. For severe life threatening acute on chronic liver cell failure, some centres will waiver this condition. Anecdotal reports from transplant centres have found a significant proportion of patients with end stage liver disease who initially met the criteria for liver transplantation after 6 months of abstinence had significant improvement in liver function, no longer needing liver transplantation. This suggests that even established end-stage cirrhosis can improve with abstinence, implying that cirrhosis never becomes completely irreversible.
6. What treatment is there for advanced liver disease? What can effectively be done to reduce the risk of illness and death from liver disease in addition to reducing and stopping drinking? • Bleeding from oesophageal varices; early identification by endoscopy can reduce risk by medical (B blockers) and surgical treatment (banding) • Acute liver failure; general medical support, steroids and emergency liver transplantation can reduce mortality • Acute infections, such as those related to GIT pathogens; treatment of infection and medical support can help • Acute renal, metabolic and electrolyte disturbance such as with hepato-renal syndrome; general medical support can help • Chronic liver failure; nutrition support with low protein intake, treatment of ascites (medically with spironolactone, surgical drainage) may help • Acute and chronic liver failure; liver transplantation.
Survival rates from liver transplantation A number of case series have been published: • They find end-stage alcoholic liver disease accounts for over 30% of liver transplantations • The five year survival rate after liver transplantation is around 70% • The estimated five year survival rate for those with a comparable stage of liver disease NOT receiving liver transplantation is around 23%. Abdul Wahed 2010
Conclusions • Liver disease is complex and not well understood by many substance misuse professionals • Yet liver disease is a common and important cause of illness and death among problem drinkers. • Liver disease in problem drinkers may be aggravated by or caused by other diseases of the liver apart from alcohol • Primary care and substance misuse professionals should have sufficient knowledge and skills to identify and assess alcoholic liver disease • Stopping or reducing drinking improves outcome from alcoholic liver disease, even in advanced/end-stage liver disease • There is effective treatment for advanced alcoholic liver disease and its complications, in addition to stopping/reducing drinking. The two should be tackled together.
References • Abdul-Wahed M (2010). Liver transplantation for alcoholic liver disease. World Journal of Gastroenterology; 16(35): 4377 -4393. • Babor T et al (2003). Alcohol; no ordinary commodity. Oxford: Oxford Medical Publications. • Morgan M, Ritson B (2010). Alcohol and health. Fifth edition. Medical Council on Alcohol. • National end of life care network 2012. Deaths from liver disease; implication for end of life care in England. www. endoflifecare-intelligence. org. uk. endoflifecareintelligence. org. • NICE (2010) CG 100. Alcohol use disorders diagnosis and clinical management of alcohol related physical complications. • Vaillant G (1983). The natural history of alcoholism; causes, patterns and paths to recovery. • Wiesner et al (2003). . Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology; vol. 124 (1): 91 -106.
Copy of slides: jack. leach@nhs. net
 Cirrhosis
Cirrhosis Non-alcoholic fatty liver disease (nafld)
Non-alcoholic fatty liver disease (nafld) Darren leach
Darren leach Kimberly leach cuerpo
Kimberly leach cuerpo Community leach pit
Community leach pit Isabella leach
Isabella leach Leach gatti
Leach gatti Professor graham leach
Professor graham leach Richard leach maddox
Richard leach maddox Chronic liver stigmata
Chronic liver stigmata Gennifer shafer liver disease
Gennifer shafer liver disease Gastroenterology board review
Gastroenterology board review Peripheral stigmata of cld
Peripheral stigmata of cld Infiltrative liver disease
Infiltrative liver disease Stigmata of chronic liver disease
Stigmata of chronic liver disease Coma sign
Coma sign Nonalcoholic fatty liver disease
Nonalcoholic fatty liver disease Complication of liver cirrhosis
Complication of liver cirrhosis Stages of cirrhosis
Stages of cirrhosis Main characters of jack and the beanstalk
Main characters of jack and the beanstalk Dr jack lambert lyme disease
Dr jack lambert lyme disease