Lyme and Coinfections Why the controversy Dr Jack
![Lyme Disease Interpretations of the literature EM Rash Relatively low incidence 25% [1] to Lyme Disease Interpretations of the literature EM Rash Relatively low incidence 25% [1] to](https://slidetodoc.com/presentation_image_h/bdb3893922f21453ef39938607422bc3/image-10.jpg)
- Slides: 32
Lyme and Co-infections: Why the controversy? Dr Jack Lambert, Professor of Medicine and Infectious Diseases, Mater Hospital and UCD School of Medicine, Dublin 1 Pr
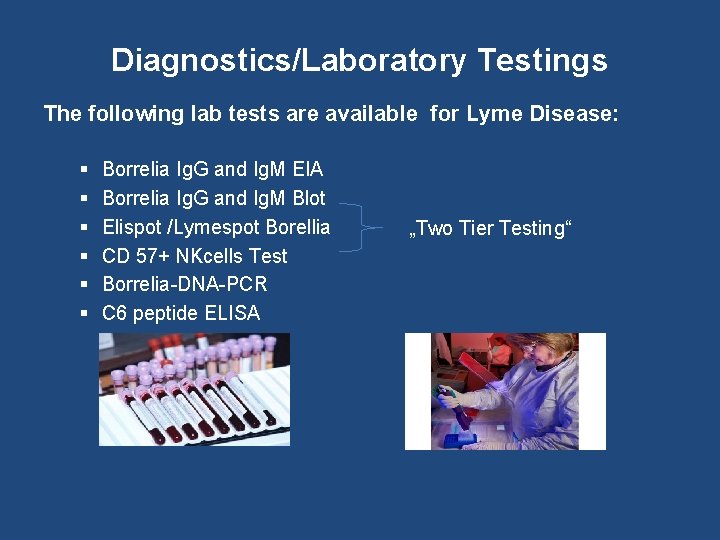
Diagnostics/Laboratory Testings The following lab tests are available for Lyme Disease: § § § Borrelia Ig. G and Ig. M EIA Borrelia Ig. G and Ig. M Blot Elispot /Lymespot Borellia CD 57+ NKcells Test Borrelia-DNA-PCR C 6 peptide ELISA „Two Tier Testing“
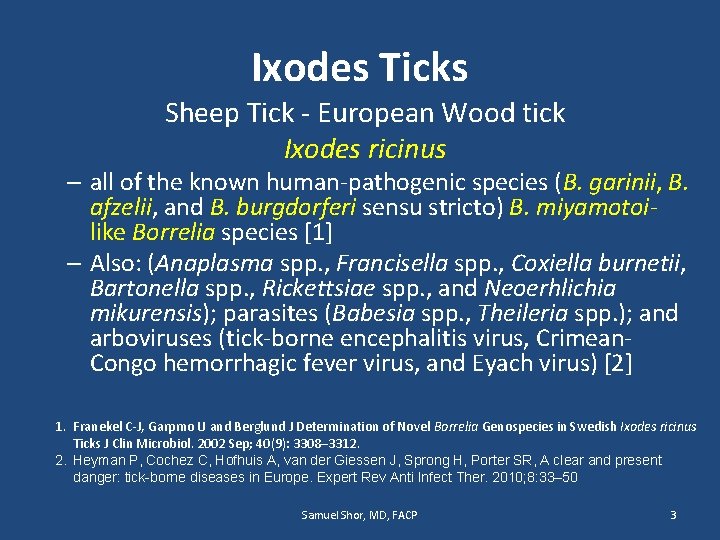
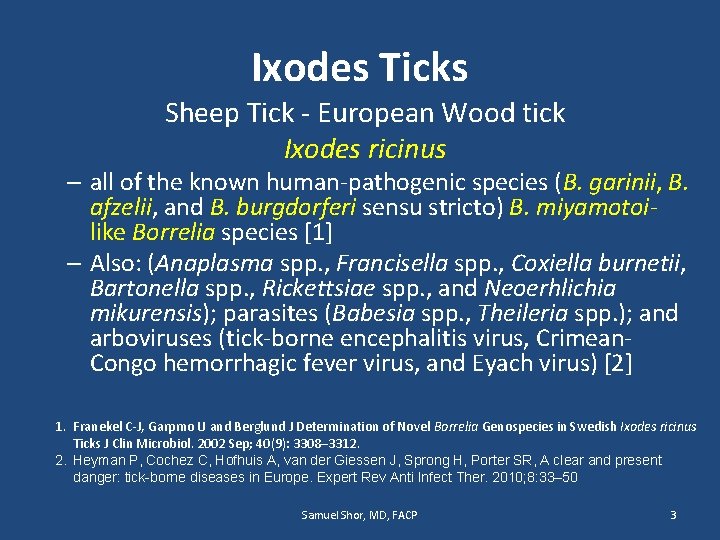
Ixodes Ticks Sheep Tick - European Wood tick Ixodes ricinus – all of the known human-pathogenic species (B. garinii, B. afzelii, and B. burgdorferi sensu stricto) B. miyamotoilike Borrelia species [1] – Also: (Anaplasma spp. , Francisella spp. , Coxiella burnetii, Bartonella spp. , Rickettsiae spp. , and Neoerhlichia mikurensis); parasites (Babesia spp. , Theileria spp. ); and arboviruses (tick-borne encephalitis virus, Crimean. Congo hemorrhagic fever virus, and Eyach virus) [2] 1. Franekel C-J, Garpmo U and Berglund J Determination of Novel Borrelia Genospecies in Swedish Ixodes ricinus Ticks J Clin Microbiol. 2002 Sep; 40(9): 3308– 3312. 2. Heyman P, Cochez C, Hofhuis A, van der Giessen J, Sprong H, Porter SR, A clear and present danger: tick-borne diseases in Europe. Expert Rev Anti Infect Ther. 2010; 8: 33– 50 Samuel Shor, MD, FACP 3
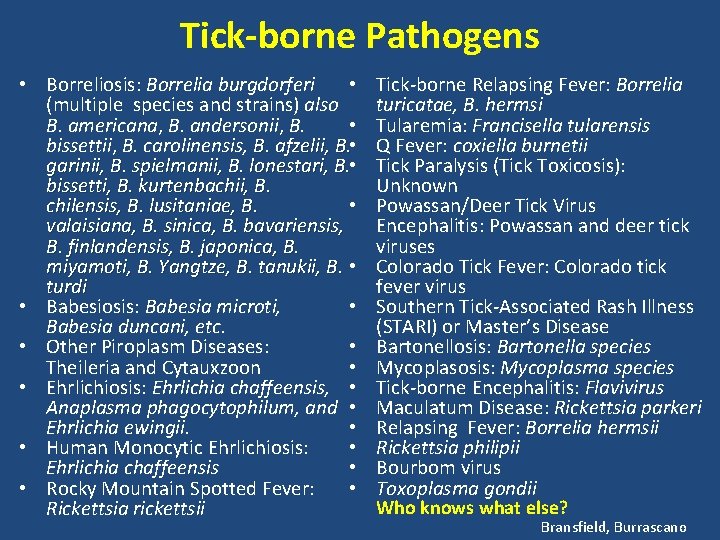
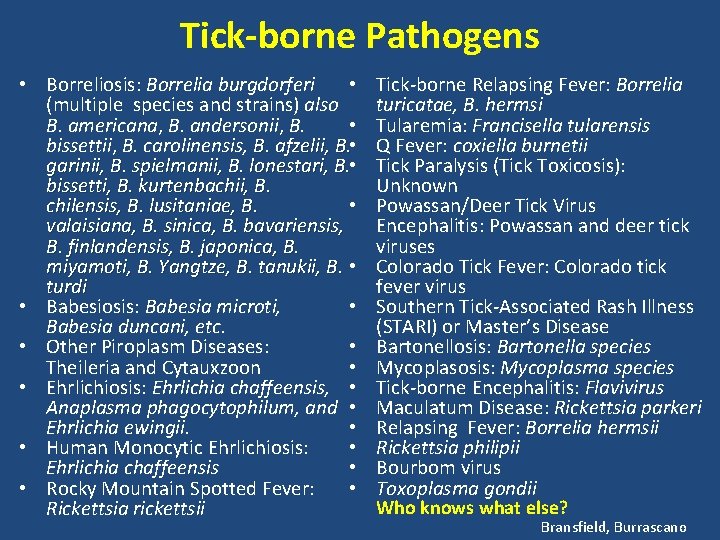
Tick-borne Pathogens • Borreliosis: Borrelia burgdorferi • (multiple species and strains) also B. americana, B. andersonii, B. • bissettii, B. carolinensis, B. afzelii, B. • garinii, B. spielmanii, B. lonestari, B. • bissetti, B. kurtenbachii, B. chilensis, B. lusitaniae, B. • valaisiana, B. sinica, B. bavariensis, B. finlandensis, B. japonica, B. miyamoti, B. Yangtze, B. tanukii, B. • turdi • Babesiosis: Babesia microti, • Babesia duncani, etc. • Other Piroplasm Diseases: • Theileria and Cytauxzoon • • Ehrlichiosis: Ehrlichia chaffeensis, • Anaplasma phagocytophilum, and • Ehrlichia ewingii. • • Human Monocytic Ehrlichiosis: • Ehrlichia chaffeensis • • Rocky Mountain Spotted Fever: • Rickettsia rickettsii Tick-borne Relapsing Fever: Borrelia turicatae, B. hermsi Tularemia: Francisella tularensis Q Fever: coxiella burnetii Tick Paralysis (Tick Toxicosis): Unknown Powassan/Deer Tick Virus Encephalitis: Powassan and deer tick viruses Colorado Tick Fever: Colorado tick fever virus Southern Tick-Associated Rash Illness (STARI) or Master’s Disease Bartonellosis: Bartonella species Mycoplasosis: Mycoplasma species Tick-borne Encephalitis: Flavivirus Maculatum Disease: Rickettsia parkeri Relapsing Fever: Borrelia hermsii Rickettsia philipii Bourbom virus Toxoplasma gondii Who knows what else? Bransfield, Burrascano
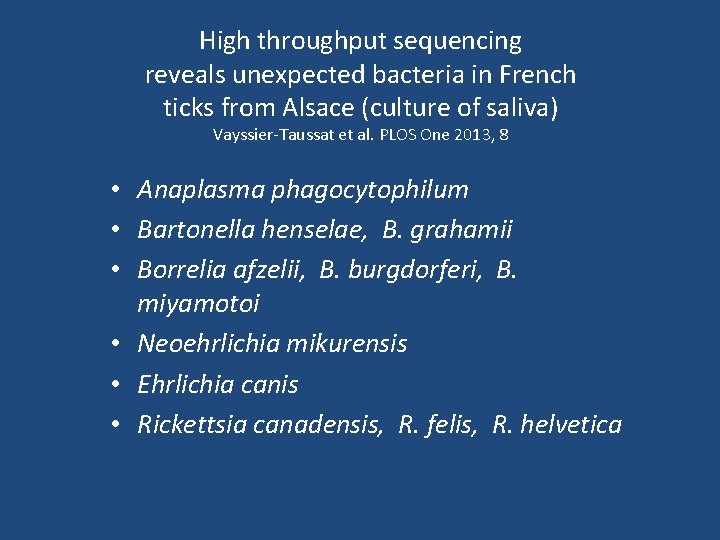
High throughput sequencing reveals unexpected bacteria in French ticks from Alsace (culture of saliva) Vayssier-Taussat et al. PLOS One 2013, 8 • Anaplasma phagocytophilum • Bartonella henselae, B. grahamii • Borrelia afzelii, B. burgdorferi, B. miyamotoi • Neoehrlichia mikurensis • Ehrlichia canis • Rickettsia canadensis, R. felis, R. helvetica
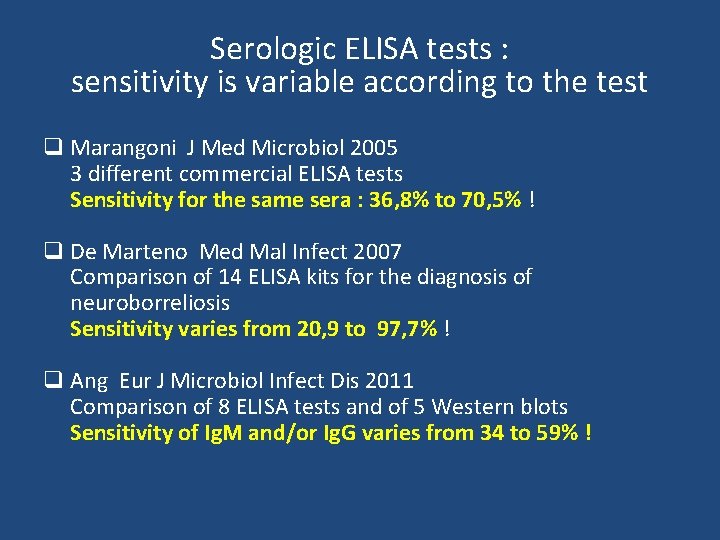
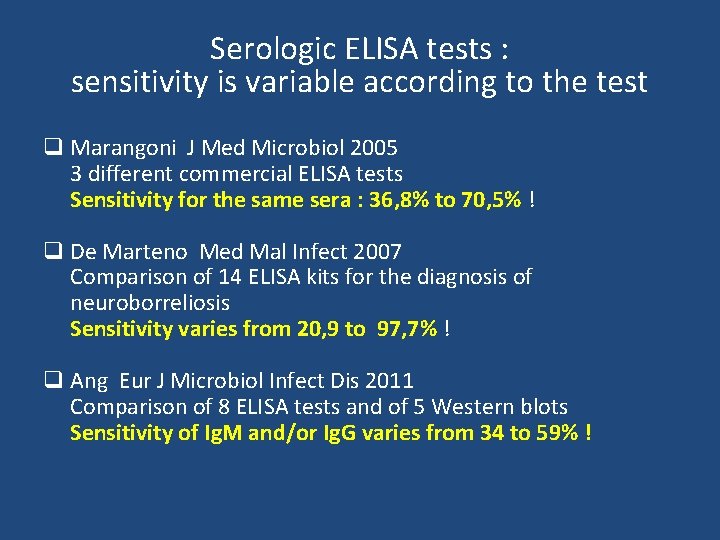
Serologic ELISA tests : sensitivity is variable according to the test q Marangoni J Med Microbiol 2005 3 different commercial ELISA tests Sensitivity for the same sera : 36, 8% to 70, 5% ! q De Marteno Med Mal Infect 2007 Comparison of 14 ELISA kits for the diagnosis of neuroborreliosis Sensitivity varies from 20, 9 to 97, 7% ! q Ang Eur J Microbiol Infect Dis 2011 Comparison of 8 ELISA tests and of 5 Western blots Sensitivity of Ig. M and/or Ig. G varies from 34 to 59% !
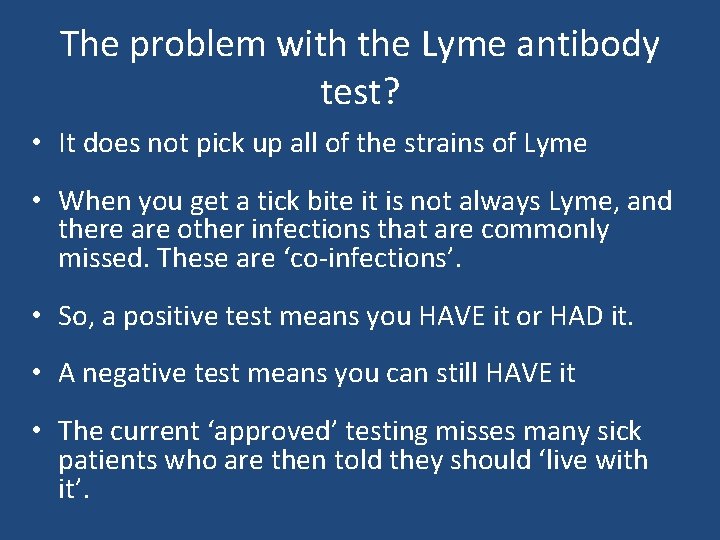
The problem with the Lyme antibody test? • It does not pick up all of the strains of Lyme • When you get a tick bite it is not always Lyme, and there are other infections that are commonly missed. These are ‘co-infections’. • So, a positive test means you HAVE it or HAD it. • A negative test means you can still HAVE it • The current ‘approved’ testing misses many sick patients who are then told they should ‘live with it’.
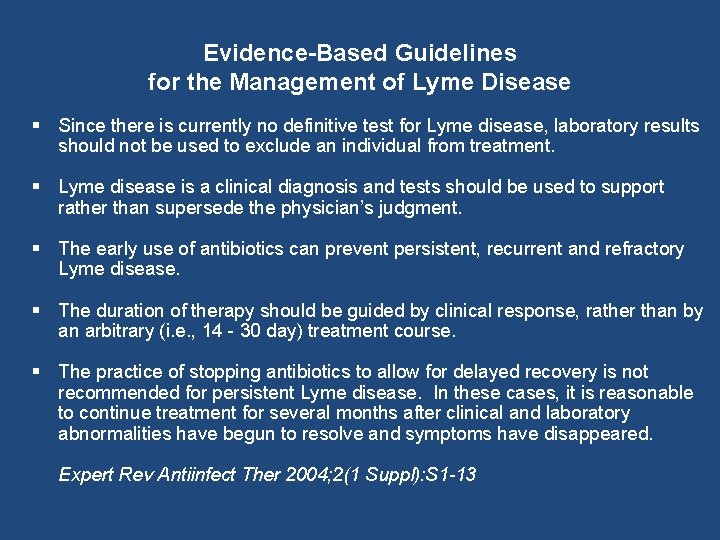
Evidence-Based Guidelines for the Management of Lyme Disease § Since there is currently no definitive test for Lyme disease, laboratory results should not be used to exclude an individual from treatment. § Lyme disease is a clinical diagnosis and tests should be used to support rather than supersede the physician’s judgment. § The early use of antibiotics can prevent persistent, recurrent and refractory Lyme disease. § The duration of therapy should be guided by clinical response, rather than by an arbitrary (i. e. , 14 - 30 day) treatment course. § The practice of stopping antibiotics to allow for delayed recovery is not recommended for persistent Lyme disease. In these cases, it is reasonable to continue treatment for several months after clinical and laboratory abnormalities have begun to resolve and symptoms have disappeared. Expert Rev Antiinfect Ther 2004; 2(1 Suppl): S 1 -13
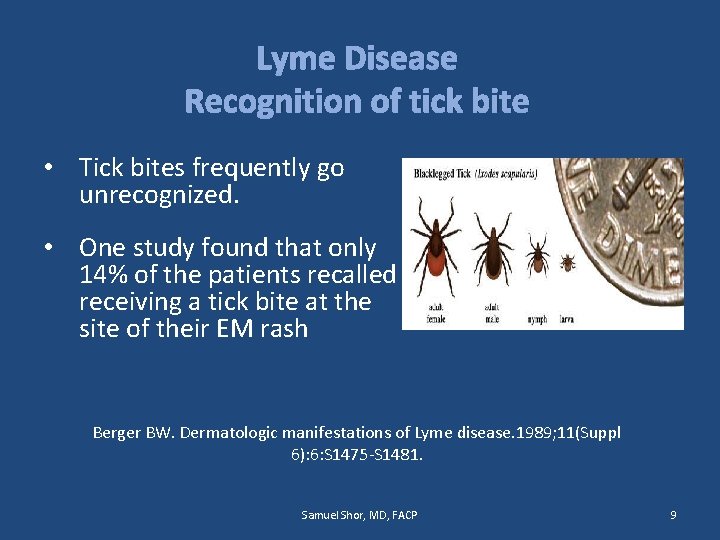
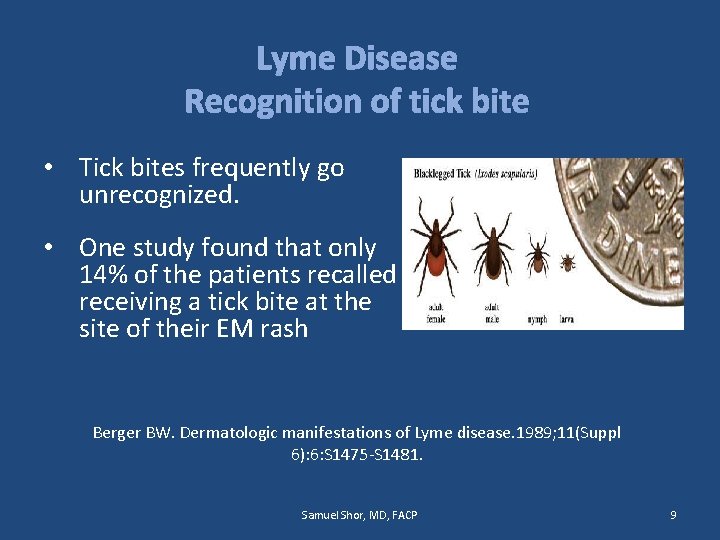
Lyme Disease Recognition of tick bite • Tick bites frequently go unrecognized. • One study found that only 14% of the patients recalled receiving a tick bite at the site of their EM rash Berger BW. Dermatologic manifestations of Lyme disease. 1989; 11(Suppl 6): 6: S 1475 -S 1481. Samuel Shor, MD, FACP 9
![Lyme Disease Interpretations of the literature EM Rash Relatively low incidence 25 1 to Lyme Disease Interpretations of the literature EM Rash Relatively low incidence 25% [1] to](https://slidetodoc.com/presentation_image_h/bdb3893922f21453ef39938607422bc3/image-10.jpg)
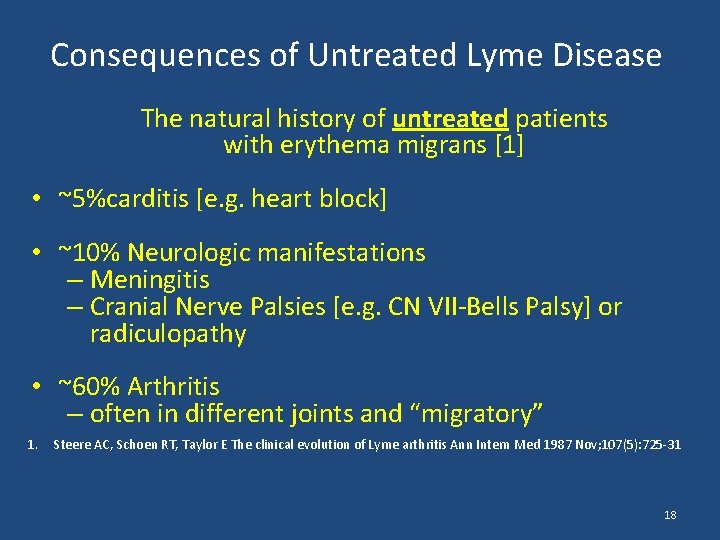
Lyme Disease Interpretations of the literature EM Rash Relatively low incidence 25% [1] to <50% [2, 3] and frequent atypical presentations [4] 1. Nadelman RB, Nowakowski J, Forseter G, et al. The clinical spectrum of early Lyme borreliosis in patients with culture-confirmed erythema migrans. Am J Med 1996; 100(5): 502– 8. 2. Boyer B, Goodfriend D, Sockwell D Risk and Protective Factor Survey of Lyme Disease Cases in Loudoun County, Virginia 2009 -2011 http: // 3. Reik L Jr, Burgdorfer W, Donaldson JO Neurologic abnormalities in Lyme disease without erythema chronicum migrans Am J Med 1986; 81: 73 -8 BJ 4. Hengge UR. Lyme Borreliosis. Lancet Infect Dis 2003; 3(8): 489 -500 Samuel Shor, MD, FACP 10
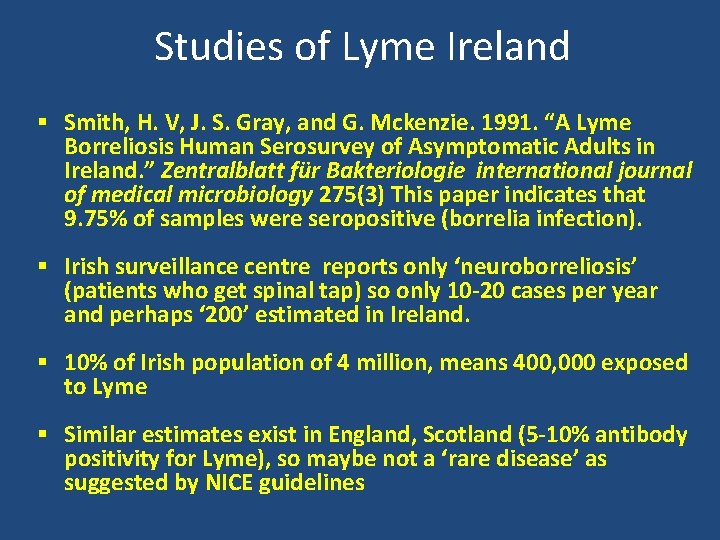
Studies of Lyme Ireland § Smith, H. V, J. S. Gray, and G. Mckenzie. 1991. “A Lyme Borreliosis Human Serosurvey of Asymptomatic Adults in Ireland. ” Zentralblatt für Bakteriologie international journal of medical microbiology 275(3) This paper indicates that 9. 75% of samples were seropositive (borrelia infection). § Irish surveillance centre reports only ‘neuroborreliosis’ (patients who get spinal tap) so only 10 -20 cases per year and perhaps ‘ 200’ estimated in Ireland. § 10% of Irish population of 4 million, means 400, 000 exposed to Lyme § Similar estimates exist in England, Scotland (5 -10% antibody positivity for Lyme), so maybe not a ‘rare disease’ as suggested by NICE guidelines
Lyme Disease Typical Acute Presentation ~3 days-3 weeks of exposure: Fever Headache Joint pain Fatigue Bacon RM Kugeler KJ, Mead PS. Centers for Disease Control and Prevention (CDC). Surveillance for Lyme disease – United States, 1992– 2006. MMWR. 2008; 57: SS 1 -10 Samuel Shor, MD, FACP 12
Symptoms in LD/Co-infections Every organ & organ system can be affected This is a list of some of the LD symptoms by body system and is not an exhaustive compilation of possible symptoms • Neuro: headaches, facial paralysis, seizures, meningitis, stiff neck, burning, tingling or prickly sensations (parathesia), loss of reflexes, or possible increased or normal reflexes with slow return, loss of coordination and equilibrium. • Neuropsych: mood swings, irritability, anxiety, rage ("Lyme Rage"), poor concentration, cognitive loss, memory loss, loss of appetite, mental deterioration, depression, disorientation, insomnia and numerous mood and psychiatric disorders that were not present prior to lyme disease or are extremely exacerbated by lyme disease. • Head: Headache, neck pain, facial pain and paralysis, difficulty chewing, pain in teeth, dry mouth, decreased sense of taste and smell, numb tongue/mouth, peculiar metallic, salty and other tastes in mouth are also common • Eyes: Pain due to inflammation (scleritis, uveitis, optic neuritis), dry eyes, sensitivity to light, ptosis of eyelids, conjunctivitis, blurry or double vision, floaters, difficulty with eye teaming and convergence, swelling around eyes/bags below eyes.
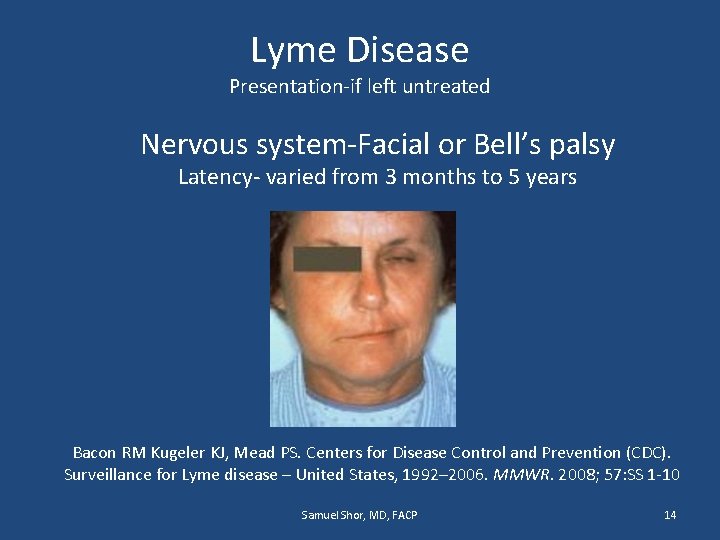
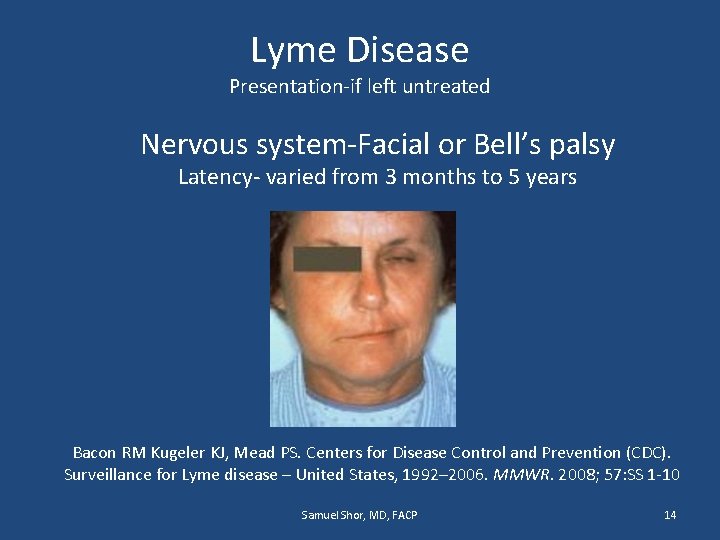
Lyme Disease Presentation-if left untreated Nervous system-Facial or Bell’s palsy Latency- varied from 3 months to 5 years Bacon RM Kugeler KJ, Mead PS. Centers for Disease Control and Prevention (CDC). Surveillance for Lyme disease – United States, 1992– 2006. MMWR. 2008; 57: SS 1 -10 Samuel Shor, MD, FACP 14
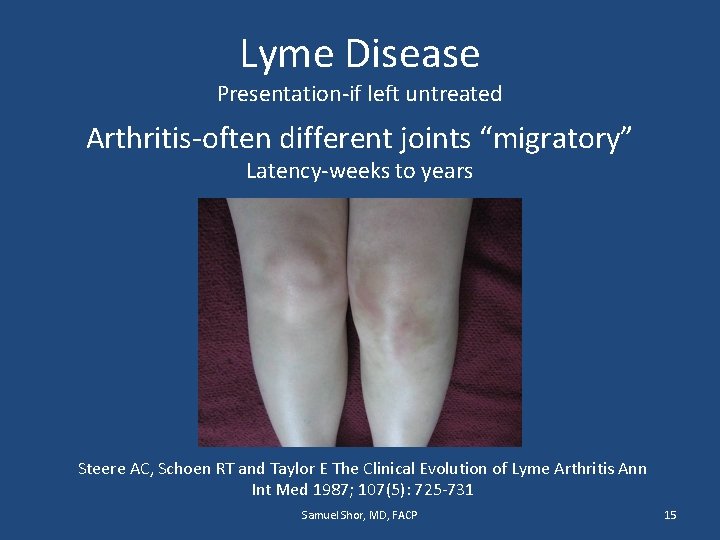
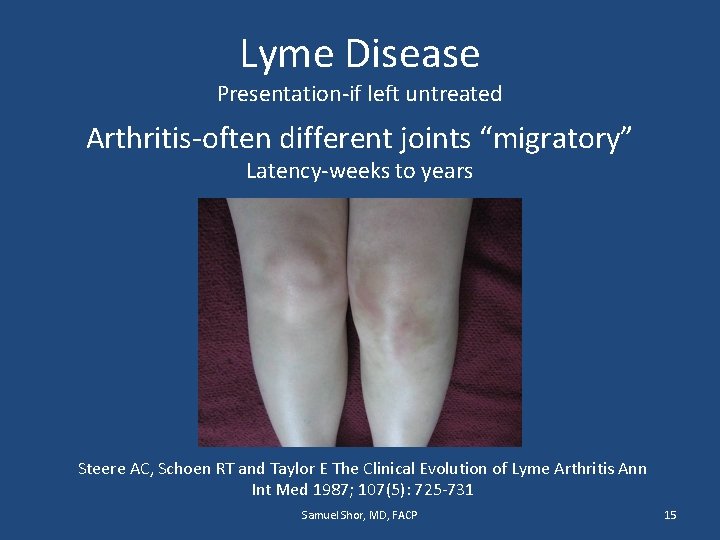
Lyme Disease Presentation-if left untreated Arthritis-often different joints “migratory” Latency-weeks to years Steere AC, Schoen RT and Taylor E The Clinical Evolution of Lyme Arthritis Ann Int Med 1987; 107(5): 725 -731 Samuel Shor, MD, FACP 15
How commonly is Lyme and Coinfections missed? • Only 10 -20 percent of patients identify or remember a tick bite • Only 50 percent or less who do identify a tick bite get the EM rash, and these rashes are often misdiagnosed by GPs (ie ringworm) • They are told they have ‘flu’. • When they show up later with lower white cells, caused by Lyme and co-infections, they are told they have ‘a virus’, ‘give it time and rest’.
How do you diagnose ‘Acute Lyme’ History history Multi-sytem involvement ECM rash may be missed (50%) Tick attached to skin may be identified in a minority of cases (15%) • It’s a clinical diagnosis. And early treatment will prevent later complications. And retreatment, longer course of treatment may be necessary, but guidelines say NO to this. • •
Consequences of Untreated Lyme Disease The natural history of untreated patients with erythema migrans [1] • ~5%carditis [e. g. heart block] • ~10% Neurologic manifestations – Meningitis – Cranial Nerve Palsies [e. g. CN VII-Bells Palsy] or radiculopathy • ~60% Arthritis – often in different joints and “migratory” 1. Steere AC, Schoen RT, Taylor E The clinical evolution of Lyme arthritis Ann Intern Med 1987 Nov; 107(5): 725 -31 18
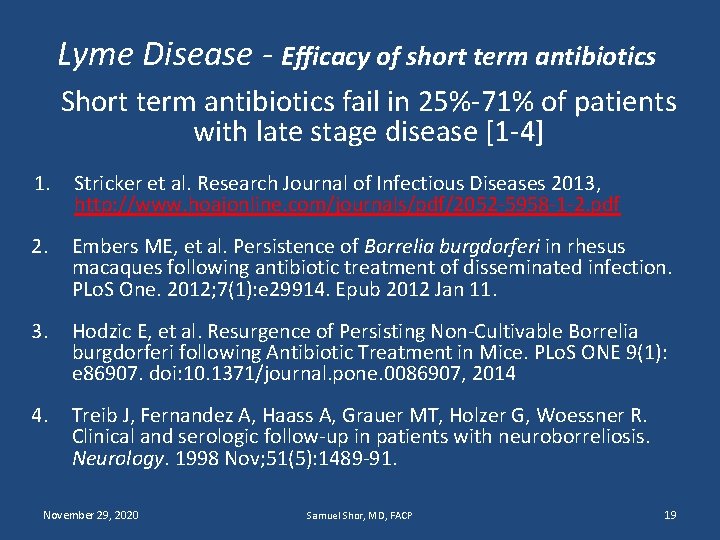
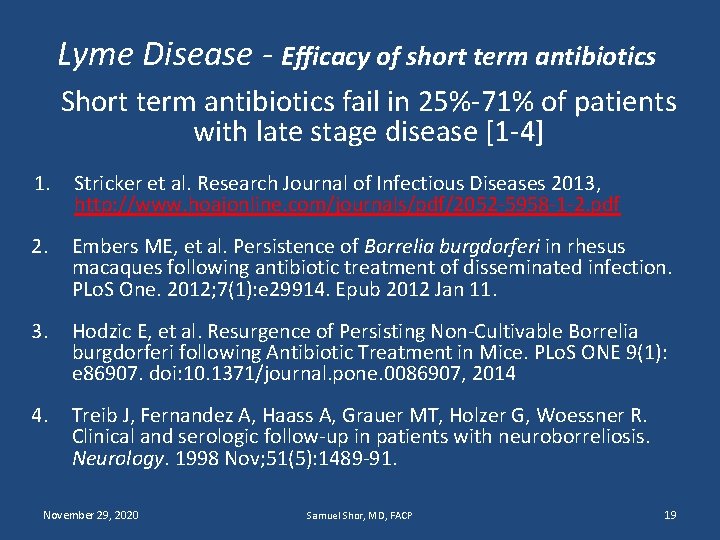
Lyme Disease - Efficacy of short term antibiotics Short term antibiotics fail in 25%-71% of patients with late stage disease [1 -4] 1. Stricker et al. Research Journal of Infectious Diseases 2013, http: //www. hoajonline. com/journals/pdf/2052 -5958 -1 -2. pdf 2. Embers ME, et al. Persistence of Borrelia burgdorferi in rhesus macaques following antibiotic treatment of disseminated infection. PLo. S One. 2012; 7(1): e 29914. Epub 2012 Jan 11. 3. Hodzic E, et al. Resurgence of Persisting Non-Cultivable Borrelia burgdorferi following Antibiotic Treatment in Mice. PLo. S ONE 9(1): e 86907. doi: 10. 1371/journal. pone. 0086907, 2014 4. Treib J, Fernandez A, Haass A, Grauer MT, Holzer G, Woessner R. Clinical and serologic follow-up in patients with neuroborreliosis. Neurology. 1998 Nov; 51(5): 1489 -91. November 29, 2020 Samuel Shor, MD, FACP 19
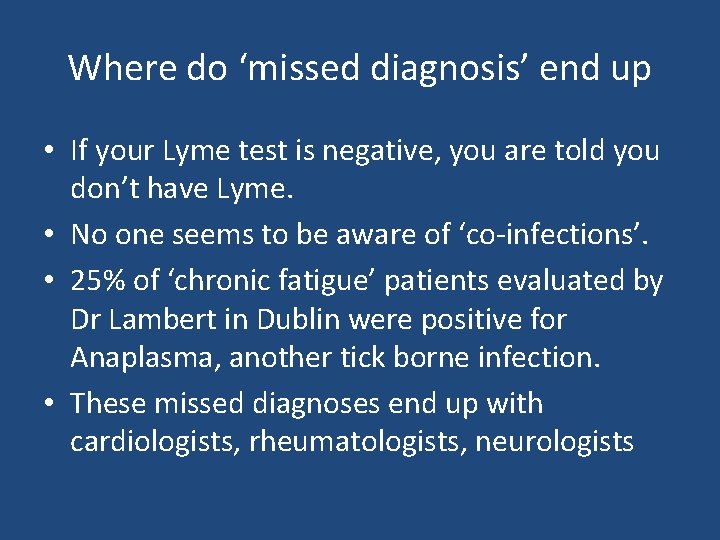
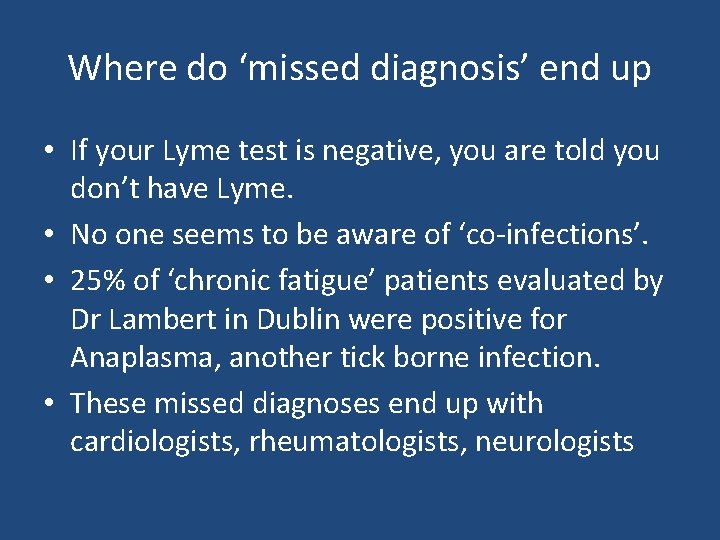
Where do ‘missed diagnosis’ end up • If your Lyme test is negative, you are told you don’t have Lyme. • No one seems to be aware of ‘co-infections’. • 25% of ‘chronic fatigue’ patients evaluated by Dr Lambert in Dublin were positive for Anaplasma, another tick borne infection. • These missed diagnoses end up with cardiologists, rheumatologists, neurologists
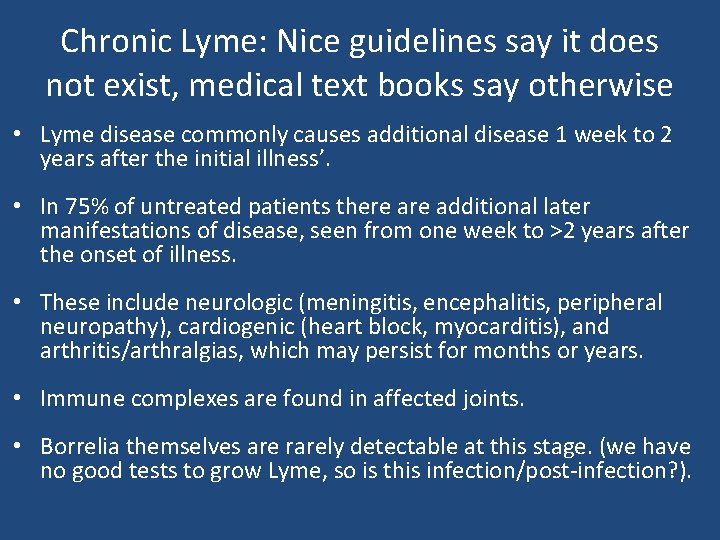
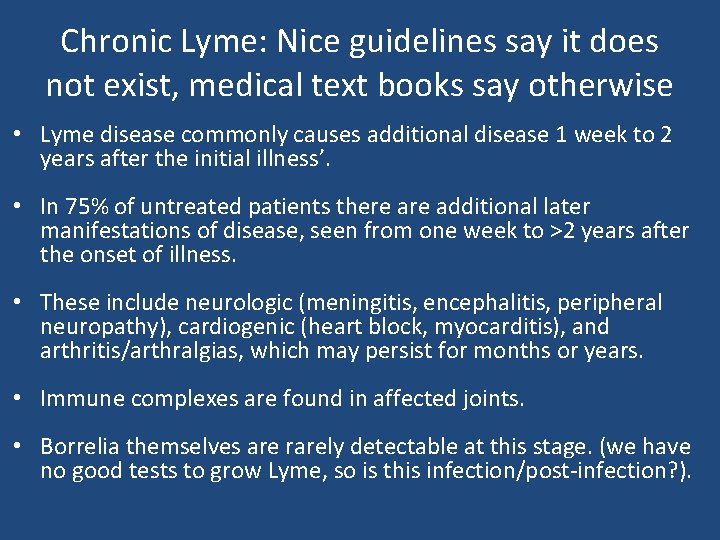
Chronic Lyme: Nice guidelines say it does not exist, medical text books say otherwise • Lyme disease commonly causes additional disease 1 week to 2 years after the initial illness’. • In 75% of untreated patients there additional later manifestations of disease, seen from one week to >2 years after the onset of illness. • These include neurologic (meningitis, encephalitis, peripheral neuropathy), cardiogenic (heart block, myocarditis), and arthritis/arthralgias, which may persist for months or years. • Immune complexes are found in affected joints. • Borrelia themselves are rarely detectable at this stage. (we have no good tests to grow Lyme, so is this infection/post-infection? ).
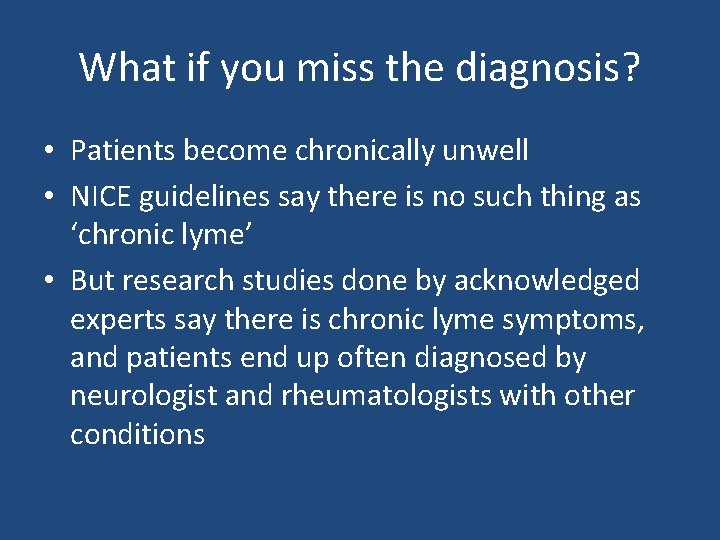
What if you miss the diagnosis? • Patients become chronically unwell • NICE guidelines say there is no such thing as ‘chronic lyme’ • But research studies done by acknowledged experts say there is chronic lyme symptoms, and patients end up often diagnosed by neurologist and rheumatologists with other conditions
Lyme Disease - Two Standards of Care Different interpretations of the literature Infectious Diseases Society of America International Lyme and Associated Diseases Society Samuel Shor, MD, FACP 23
IS there such a thing as chronic Lyme? • IDSA says the infection is gone after 2 -3 weeks of antibiotics and if patients are still sick it is ‘post-infectious’. • ILADS says you should treat the patients not the guidelines, and many patients get better with longer courses of antibiotic (s). • If you catch the bite before dissemination, its probably true that short course cures. • If you catch it late, it may be harder to treat • And even after treatment there may not be complete recovery with antibiotics alone.
Lyme Disease Post Treatment Lyme Disease Syndrome (PTLDS) “There is no convincing biologic evidence for the existence of symptomatic chronic B. burgdorferi infection among patients after receipt of recommended treatment regimens for Lyme disease. ” Wormser GP, et al The Clinical Assessment, Treatment, and Prevention of Lyme Disease, Human Granulocytic Anaplasmosis, and Babesiosis: Clinical Practice Guidelines by the Infectious Diseases Society of America Clinical Infectious Diseases 2006: 43 (1 November) ; 1089 -1134 Samuel Shor, MD, FACP 25
Lyme Disease Post Treatment Lyme Disease Syndrome (PTLDS) Evidence for persistence of B. burgdorferii in human models • Oksi J, Nikoskelainen J, Viljanen MK. Comparison of oral cefixime and intravenous ceftriaxone followed by oral amoxicillin in disseminated Lyme borreliosis. Eur J Clin Microbiol Infect Dis. 1998; 17(10): 715 -9. • Strle F, Preac-Mursic V, Cimperman J, Ruzic E, Maraspin V, Jereb M. Azithromycin versus doxycycline for treatment of erythema migrans: clinical and microbiological findings. Infection. 1993 Mar-Apr; 21(2): 83 -8. • Weber K, Wilske B, Preac-Mursic V, Thurmayer R. Azithromycin versus penicillin V for the treatment of early Lyme borreliosis. Infection 1993; 21(6): 367 -72 • Schmidli J, Hunziker T, Moesli P, Schaad UB. Cultivation of Borrelia burgdorferi from joint fluid three months after treatment of facial palsy due to Lyme borreliosis. J Infect Dis. Oct 1988; 158(4): 905 -906 • Preac-Mursic V, Pfister HW, Spiegel H, et al. First isolation of Borrelia burgdorferi from an iris biopsy. J Clin Neuroophthalmol. Sep 1993; 13(3): 155 -161; discussion 162. • Preac-Mursic V, Weber K, Pfister HW, et al. Survival of Borrelia burgdorferi in antibiotically treated patients with Lyme borreliosis. Infection. Nov-Dec 1989; 17(6): 355 -359. • Nocton JJ, Dressler F, Rutledge BJ, Rys PN, Persing DH, Steere AC. Detection of Borrelia burgdorferi DNA by polymerase chain reaction in synovial fluid from patients with Lyme arthritis. N Engl J Med. 1994 Jan 27; 330(4): 229 -34. • Oksi J, Marjamäki M, Nikoskelainen J, Viljanen MK. Borrelia burgdorferi detected by culture and PCR in clinical relapse of disseminated Lyme borreliosis. Ann Med. 1999 Jun; 31(3): 225 -32. • Feng J, et al Identification of novel activity against Borrelia burgdorferi persisters using an FDA approved drug library Emerging Microbes and Infections (2014)3, e 49; doi: 10. 1038/emi. 2014. 53 • Sharma, B. , Brown, A. , Matluck, N. , Hu, L. , Lewis, K. (2015) Borrelia burgdorferi, the causative agent of Lyme disease, forms drug-tolerant persister cells. Antimicrob Agents Chemother. 59: 4616 -24. Samuel Shor, MD, FACP 26
The debate between IDSA and ILADS • The IDSA view was the only one represented at the NICE review, and the only one that is included in most USA and EU guidelines • There was no representation by ILADS physicians on the NICE panel. And data provided on scientific journals describing chronic Lyme and describing the benefits of longer treatments were discounted Why?
CONCEPTS Chronic Lyme disease (CLD) Chronic Borreliosis Chronic Lyme disease (CLD) is a multi-systemic illness with diverse musculoskeletal, neuropsychiatric and/or cardiac clinical manifestations that result from an ongoing active infection with any of several pathogenic members of the Borrelia burgdorferi sensu lato (Bbsl) complex. Chronic Lyme disease: A Proposed Case Definition The ILADS Working group Samuel Shor, MD, FACP 28
The Challenge of Lyme • There are no good tests to diagnose, or to say if there is active infection. A ‘trial’ of antibiotics is often needed; we do this for many other diseases, but not Lyme • We need tests that actually measure the presence of the bacteria, not ‘indirect’ antibody and other immunological tests that doctors spend time in endless debates. • Until that time, we should treat patients, not guidelines.
The paradigm of altered immunity and chronic infection is not new • HIV: when patients with HIV get a low immune system they get reactivation of all sorts of bacterial and viral infections, and if you treat the HIV with medications, the immune system go back to normal • Transplant medicines: if you give too much immunosuppressing medicines to patients with organ transplants, infections flare up (shingles, herpes, Epstein Barr Virus, CMV) • Lyme and Co-infections are no different
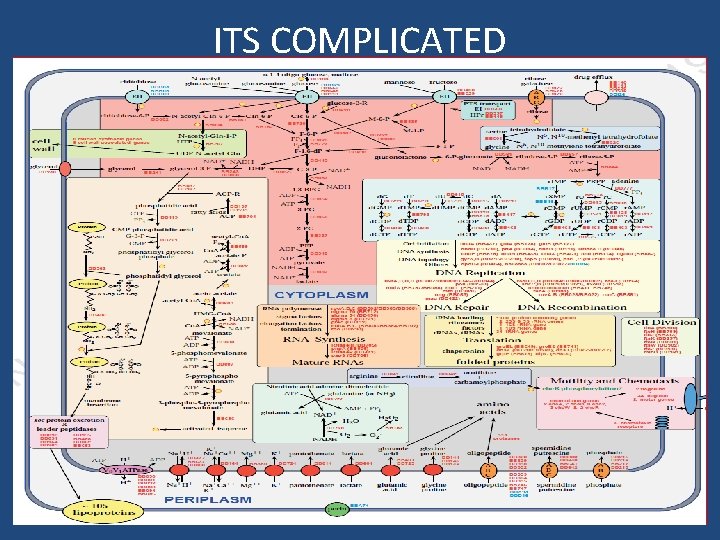
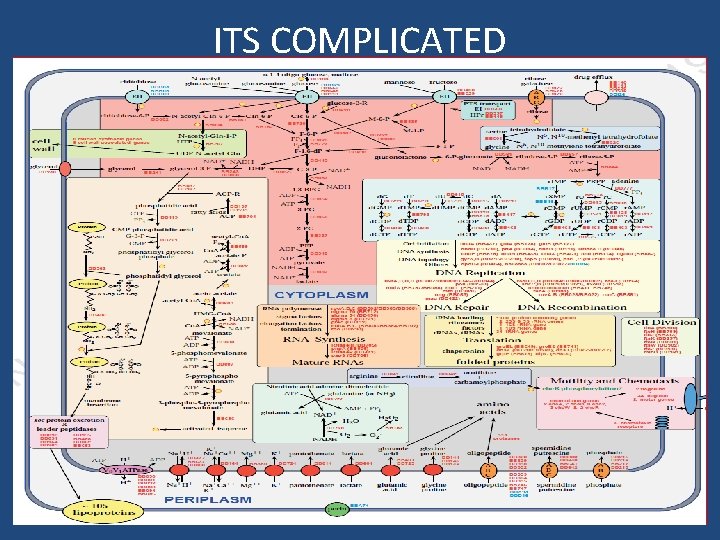
ITS COMPLICATED Different morphological forms of Borrelia burgdorferi Miklossy et al. (2008)
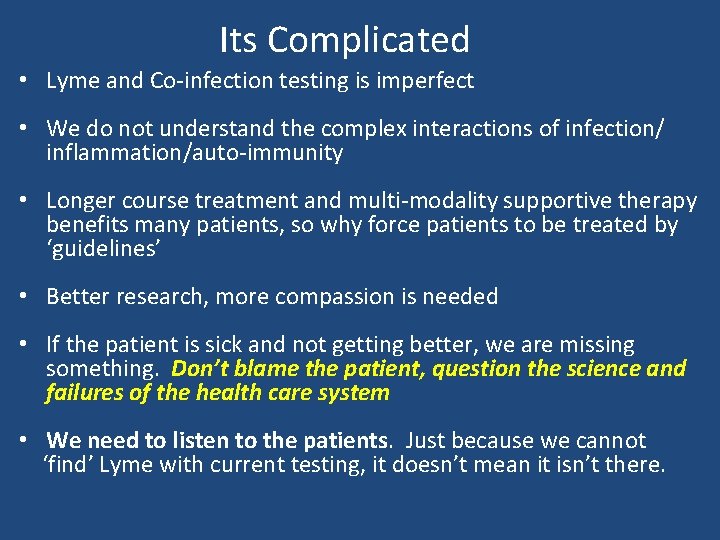
Its Complicated • Lyme and Co-infection testing is imperfect • We do not understand the complex interactions of infection/ inflammation/auto-immunity • Longer course treatment and multi-modality supportive therapy benefits many patients, so why force patients to be treated by ‘guidelines’ • Better research, more compassion is needed • If the patient is sick and not getting better, we are missing something. Don’t blame the patient, question the science and failures of the health care system • We need to listen to the patients. Just because we cannot ‘find’ Lyme with current testing, it doesn’t mean it isn’t there.
 Dr jack lambert lyme disease
Dr jack lambert lyme disease Hey bye bye
Hey bye bye Jack and the beanstalk character traits
Jack and the beanstalk character traits Met office inshore
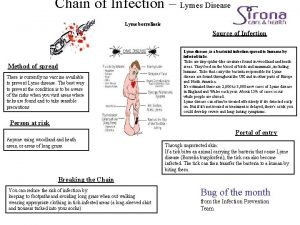
Met office inshore Chain of infection for lyme disease
Chain of infection for lyme disease Sarsaparilla lyme
Sarsaparilla lyme Lmaladie de lyme
Lmaladie de lyme Rizol gamma
Rizol gamma Point o woods old lyme
Point o woods old lyme Spirochetes shape
Spirochetes shape Azlocillin lyme disease
Azlocillin lyme disease Lyme
Lyme Dvm mph definition
Dvm mph definition Criterios de light exudado y trasudado
Criterios de light exudado y trasudado Dr steven harris lyme
Dr steven harris lyme Is it a real issue with genuine controversy and uncertainty
Is it a real issue with genuine controversy and uncertainty Without controversy great is the mystery of godliness
Without controversy great is the mystery of godliness Chapter 16 the south and the slavery controversy
Chapter 16 the south and the slavery controversy Chapter 16 the south and the slavery controversy
Chapter 16 the south and the slavery controversy Nature nurture verschil
Nature nurture verschil The south and the slavery controversy
The south and the slavery controversy Dont ask why why why
Dont ask why why why Why did jack want samneric to get him a coconut?
Why did jack want samneric to get him a coconut? What is urdu hindi controversy
What is urdu hindi controversy Why did azar kill the puppy
Why did azar kill the puppy The king james controversy
The king james controversy Inkhorn controversy
Inkhorn controversy Ford pinto controversy
Ford pinto controversy The adventures of huckleberry finn controversy
The adventures of huckleberry finn controversy Without controversy great is the mystery of godliness
Without controversy great is the mystery of godliness Conclusion of learning disability ppt
Conclusion of learning disability ppt Roll of thunder hear my cry timeline
Roll of thunder hear my cry timeline Structured academic controversy
Structured academic controversy