Pediatric Hip Dr Fadel Naim Orthopedic Surgeon IUG











- Slides: 110
Pediatric Hip Dr. Fadel Naim Orthopedic Surgeon IUG
Developmental Dysplasia of the Hip ( DDH )
The main aim of this presentation is to: – emphasize the importance of the early identification of DDH – The earlier an abnormality of the infant hip is detected, the simpler and more effective the treatment will be
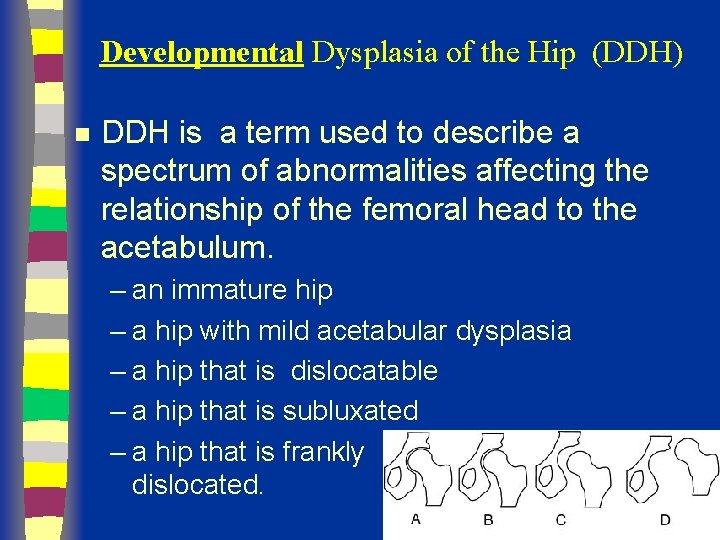
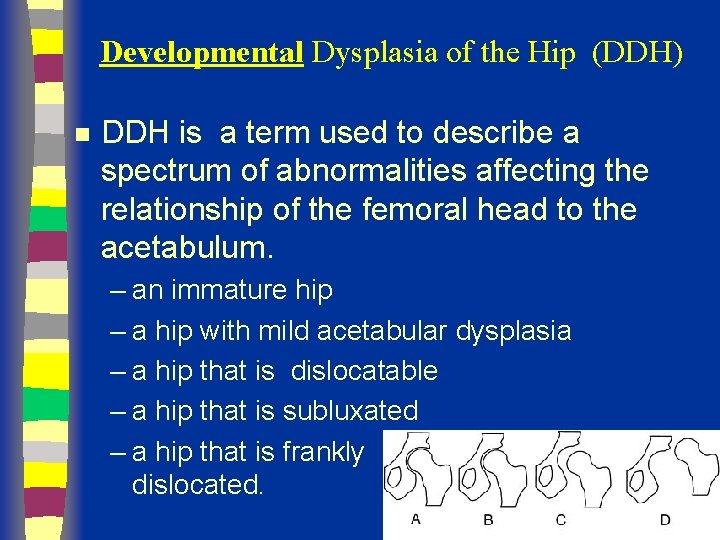
Developmental Dysplasia of the Hip (DDH) n DDH is a term used to describe a spectrum of abnormalities affecting the relationship of the femoral head to the acetabulum. – an immature hip – a hip with mild acetabular dysplasia – a hip that is dislocatable – a hip that is subluxated – a hip that is frankly dislocated.
n Teratologic Hip : Fixed dislocation Occurrs prenatally Often with other anomalies n Dislocated Hip : Completely out May or may not be reducible n Subluxated Hip : Only partially in n Unstable Hip n Acetabular Dysplasia : Shallow Acetabulu : Femoral head can be dislocated Head Subluxated or in place
Epidemiology n 1 in 100 newborns examined have evidence of instability ( positive Barlow or Ortolani) n 1 in 1000 live births true dislocation n most detectable at birth in nursery n 60% stabilize in 1 st week and 88% stabilize in first 2 months without treatment remaining 12% true dislocations and persist without treatment
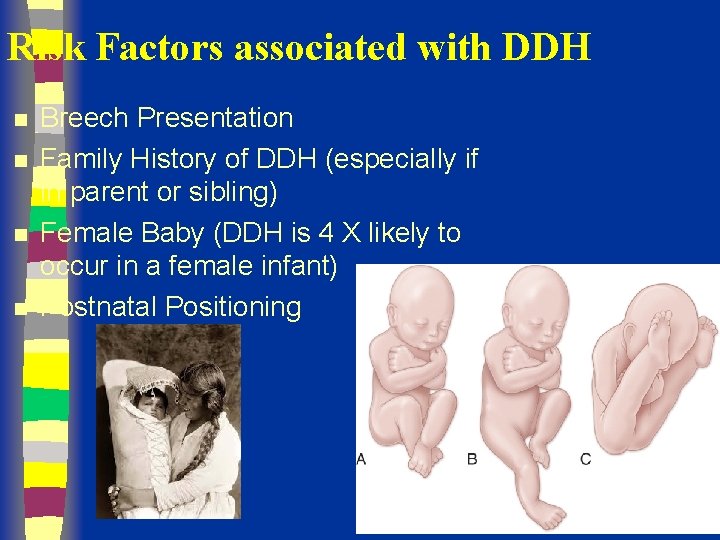
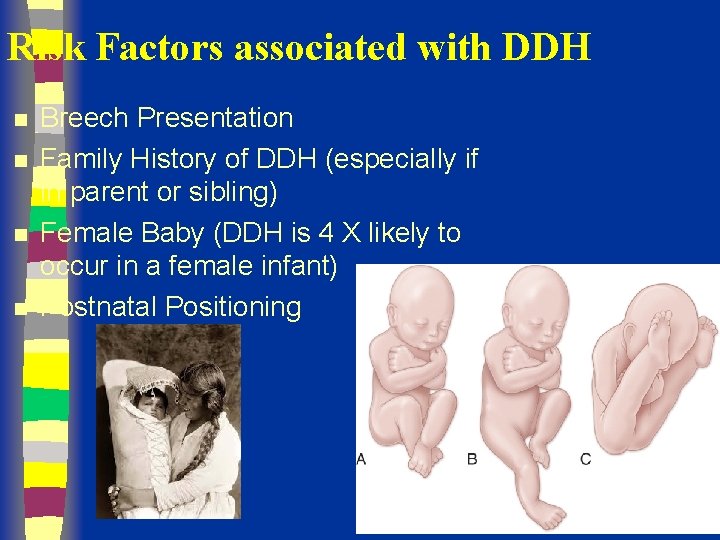
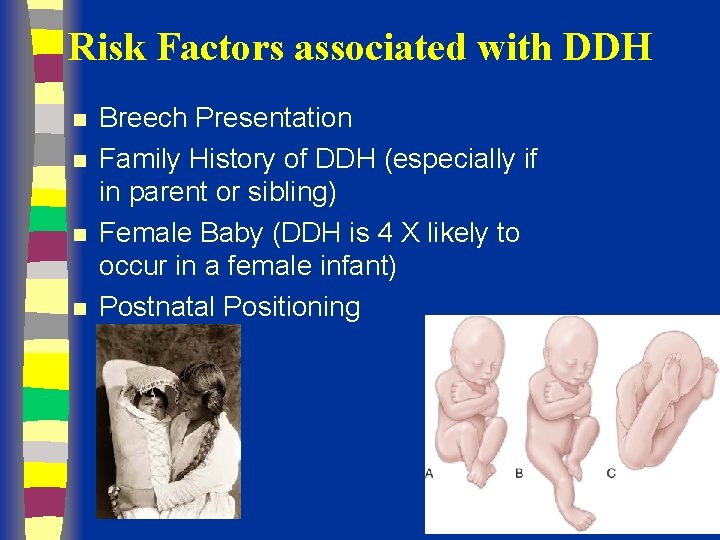
Risk Factors associated with DDH n n Breech Presentation Family History of DDH (especially if in parent or sibling) Female Baby (DDH is 4 X likely to occur in a female infant) Postnatal Positioning
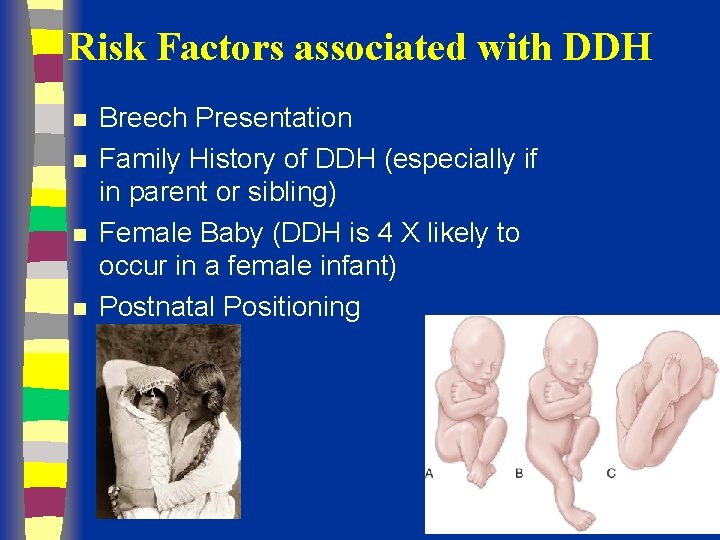
Risk Factors associated with DDH n n Breech Presentation Family History of DDH (especially if in parent or sibling) Female Baby (DDH is 4 X likely to occur in a female infant) Postnatal Positioning
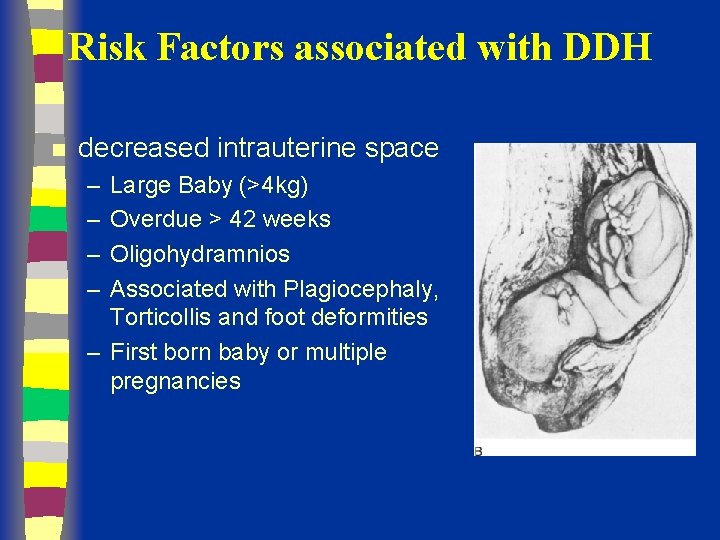
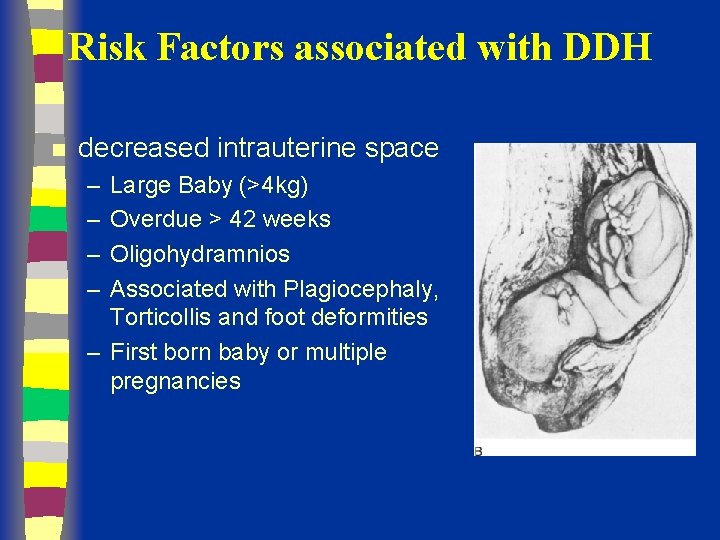
Risk Factors associated with DDH n decreased intrauterine space – – Large Baby (>4 kg) Overdue > 42 weeks Oligohydramnios Associated with Plagiocephaly, Torticollis and foot deformities – First born baby or multiple pregnancies
PHYSICAL EXAMINATION n The reliability of physical examination changes as the child grows, therefore examination techniques vary depending on the age of the child.
Diagnosis n n Clinical risk factors Physical exam – Ortolani Test – Barlow Test
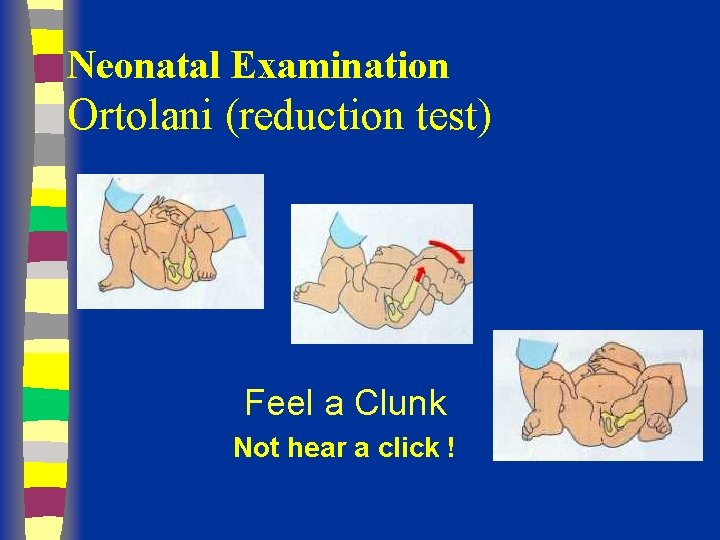
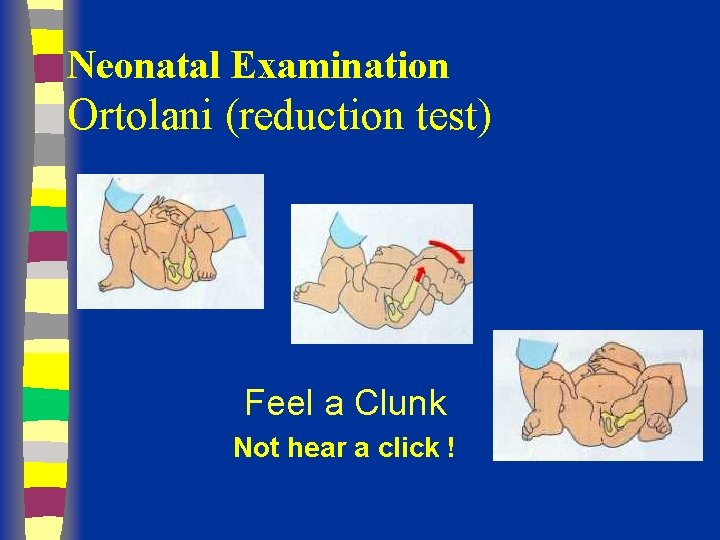
Neonatal Examination Ortolani (reduction test) Feel a Clunk Not hear a click !
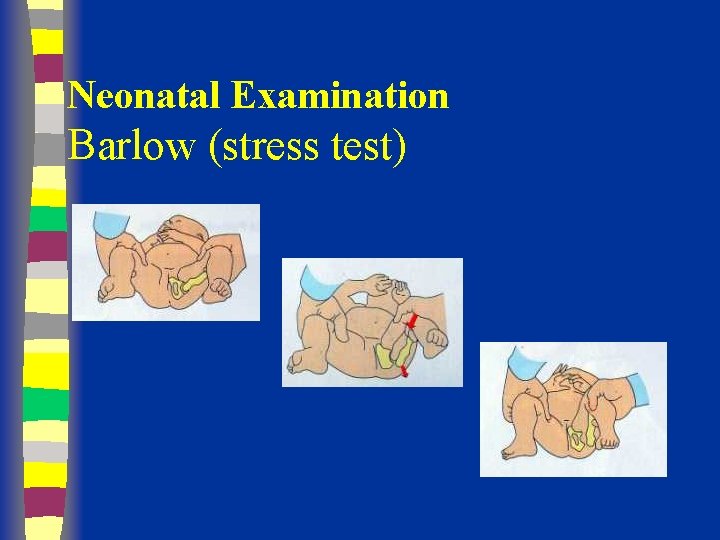
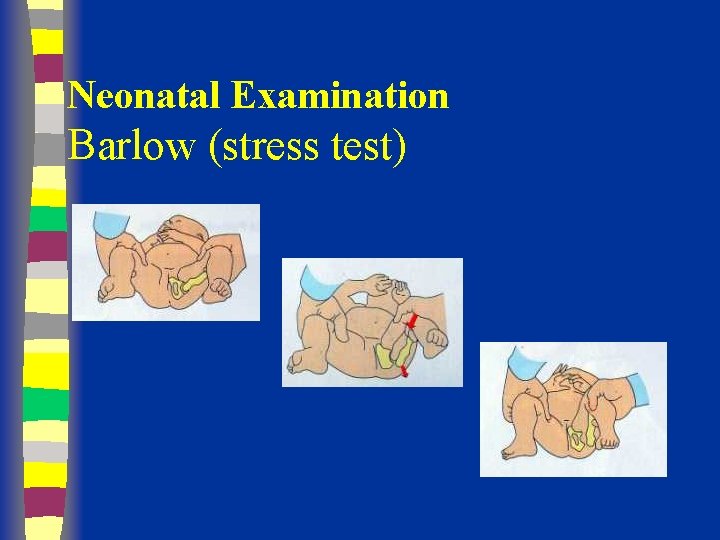
Neonatal Examination Barlow (stress test)
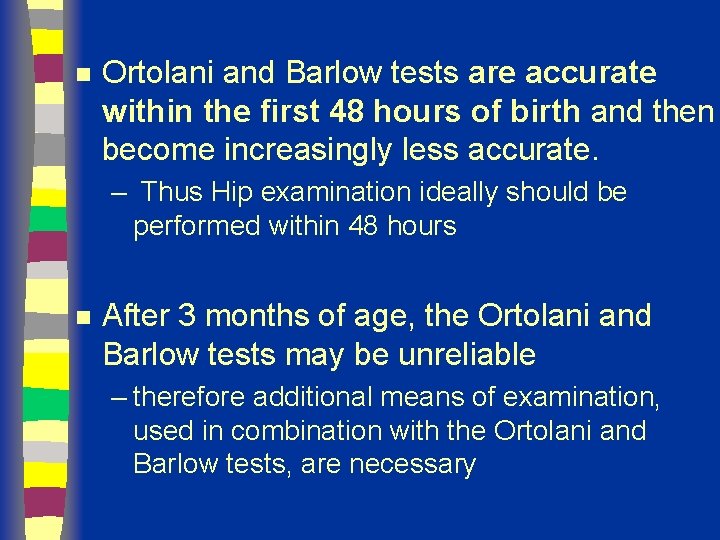
n Ortolani and Barlow tests are accurate within the first 48 hours of birth and then become increasingly less accurate. – Thus Hip examination ideally should be performed within 48 hours n After 3 months of age, the Ortolani and Barlow tests may be unreliable – therefore additional means of examination, used in combination with the Ortolani and Barlow tests, are necessary
Older Infants (> 3 months of age) n n n restricted abduction at the hips leg length discrepancy asymmetrical thigh and gluteal skin folds
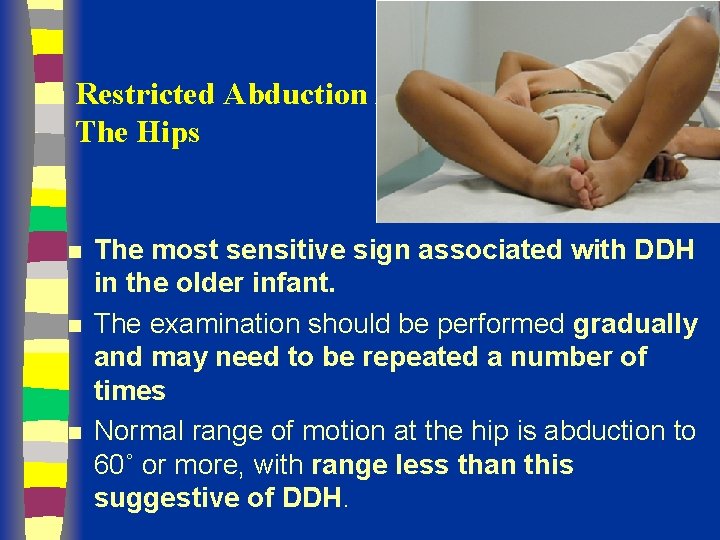
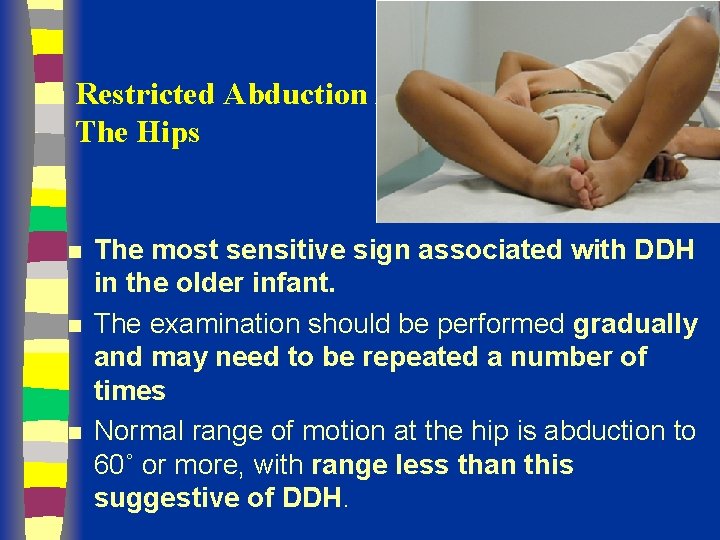
Restricted Abduction At The Hips n n n The most sensitive sign associated with DDH in the older infant. The examination should be performed gradually and may need to be repeated a number of times Normal range of motion at the hip is abduction to 60˚ or more, with range less than this suggestive of DDH.
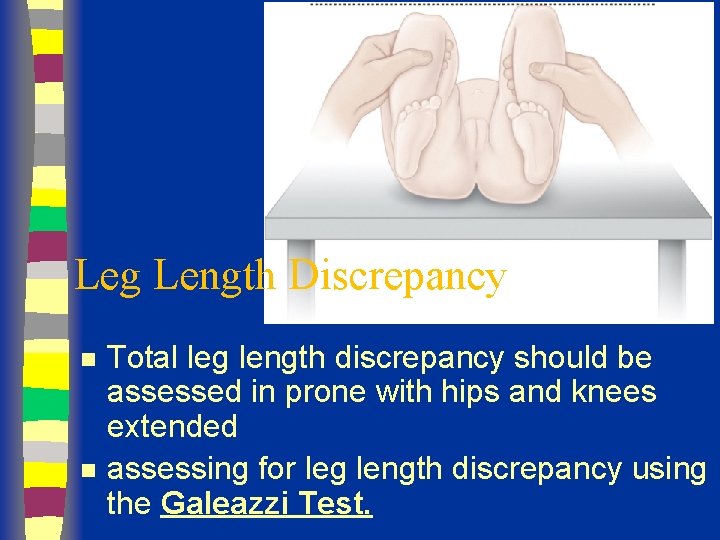
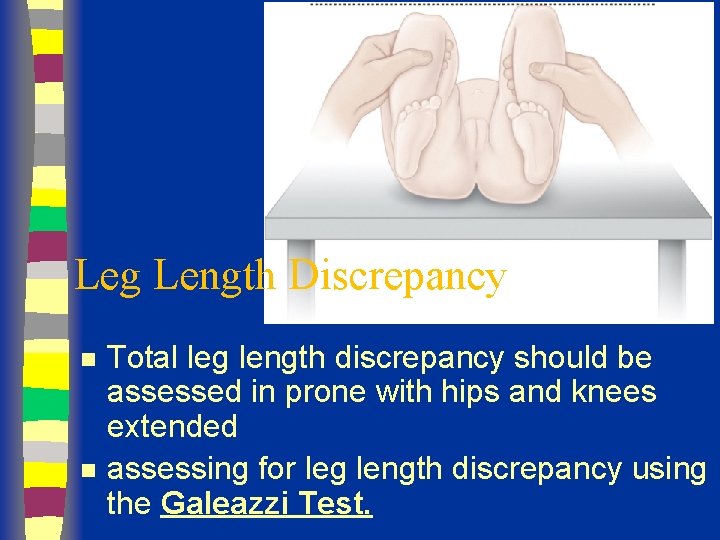
Leg Length Discrepancy n n Total leg length discrepancy should be assessed in prone with hips and knees extended assessing for leg length discrepancy using the Galeazzi Test.
Asymmetrical Skin Folds n n Asymmetrical skin folds alone do not constitute a diagnosis of DDH However this information can be used in combination with other physical signs during assessment.
Bilateral Dislocation n Diagnosis more diffecult – Abduction may be decreased symmetrically with bilateral dislocations. – Galeazzi Test may be negative in bilateral dislocations – There may be no asymmetrical skin folds
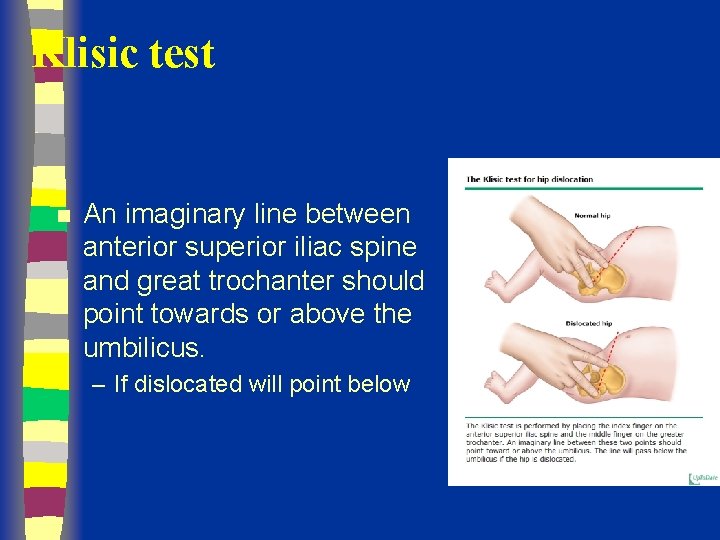
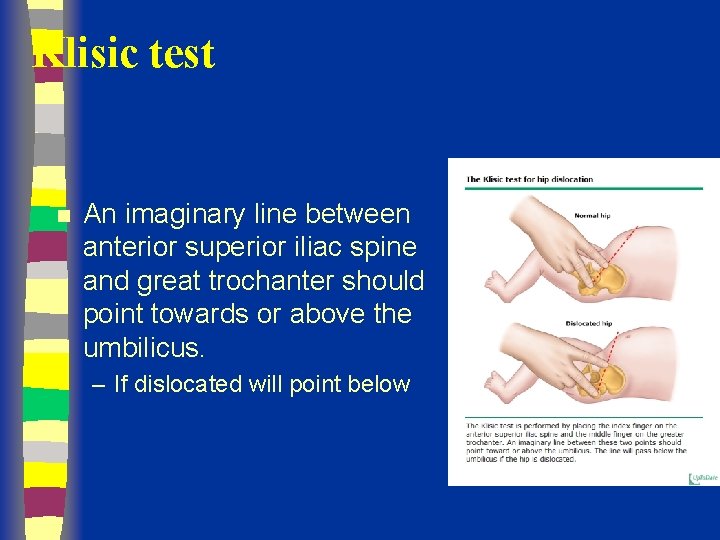
Klisic test n An imaginary line between anterior superior iliac spine and great trochanter should point towards or above the umbilicus. – If dislocated will point below
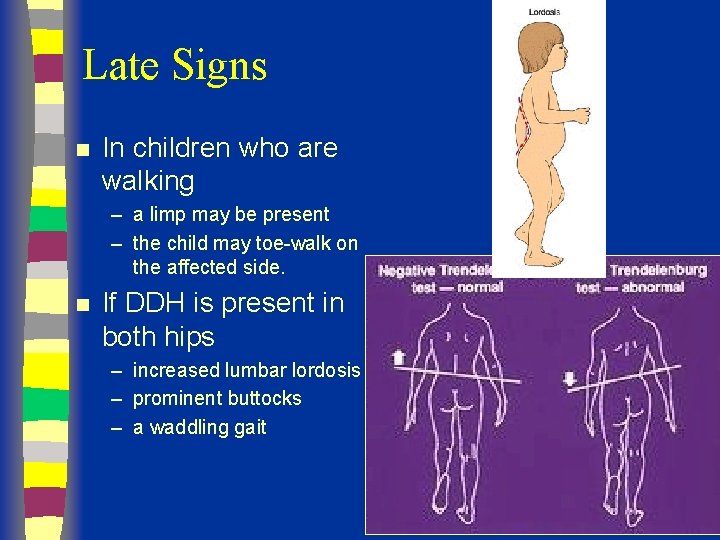
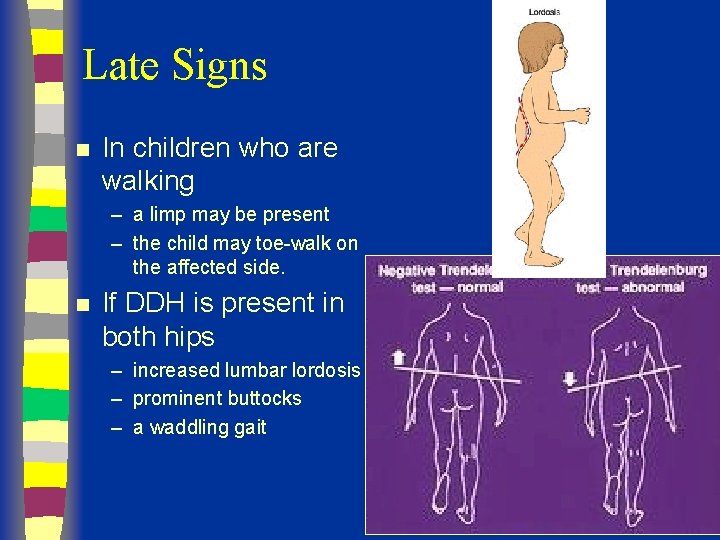
Late Signs n In children who are walking – a limp may be present – the child may toe-walk on the affected side. n If DDH is present in both hips – increased lumbar lordosis – prominent buttocks – a waddling gait
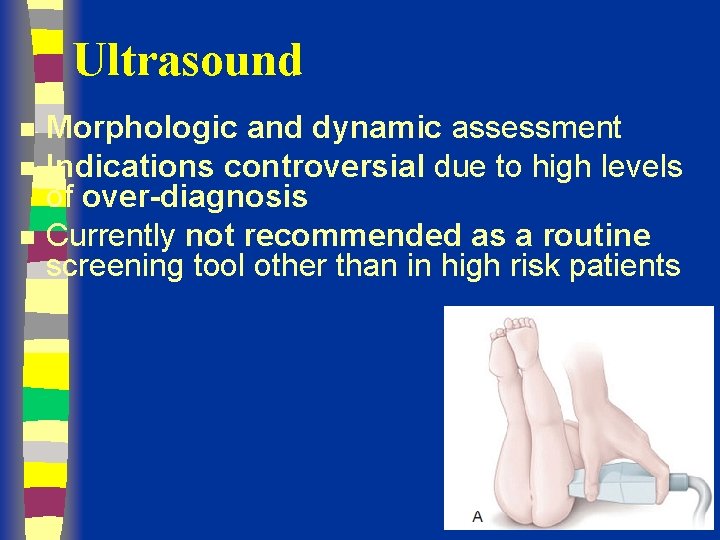
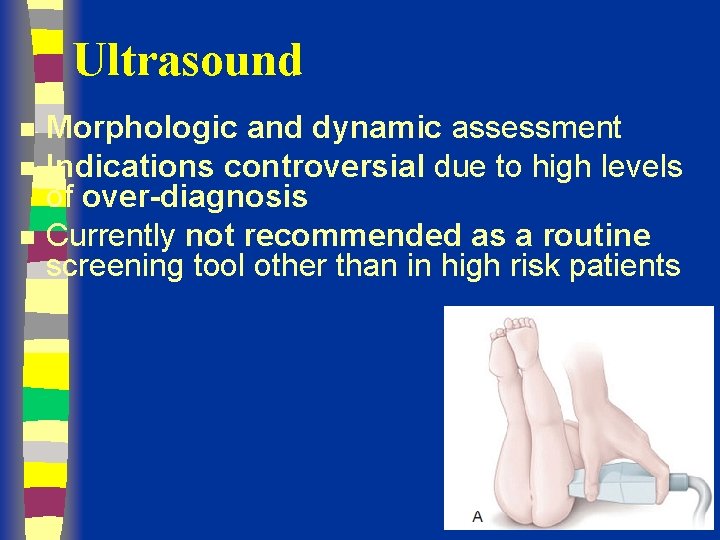
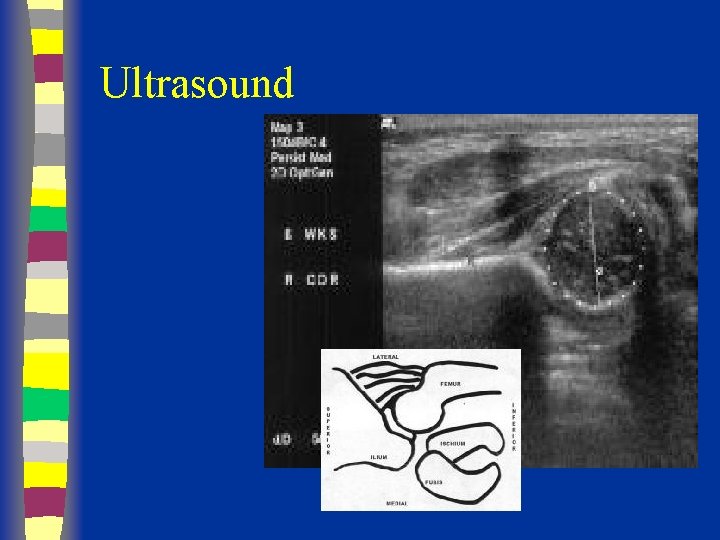
Ultrasound n n n Morphologic and dynamic assessment Indications controversial due to high levels of over-diagnosis Currently not recommended as a routine screening tool other than in high risk patients
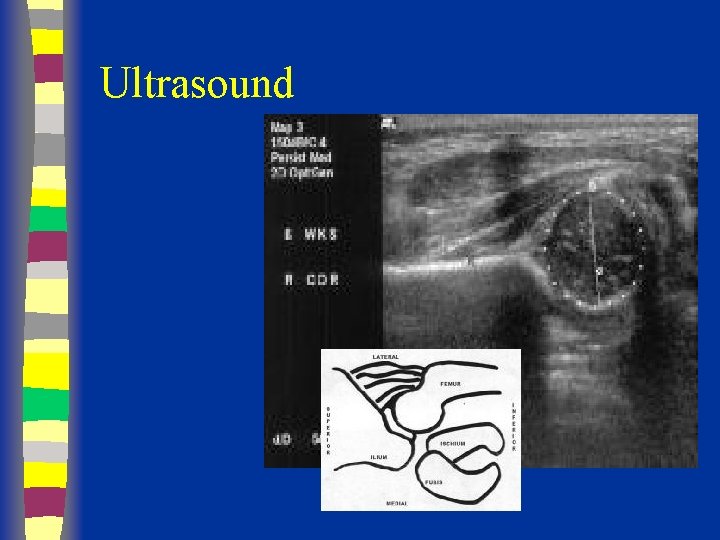
Ultrasound
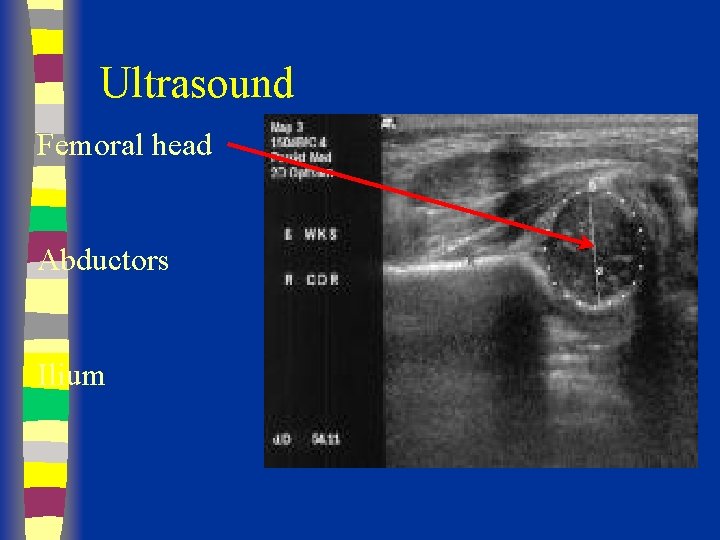
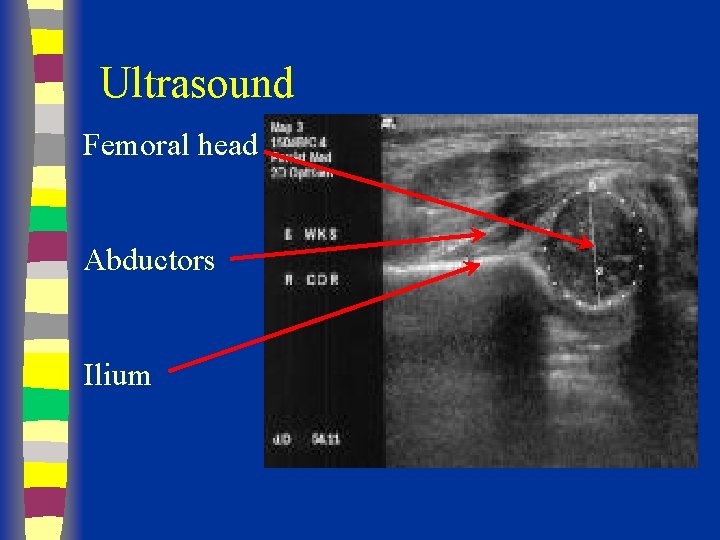
Ultrasound Femoral head Abductors Ilium
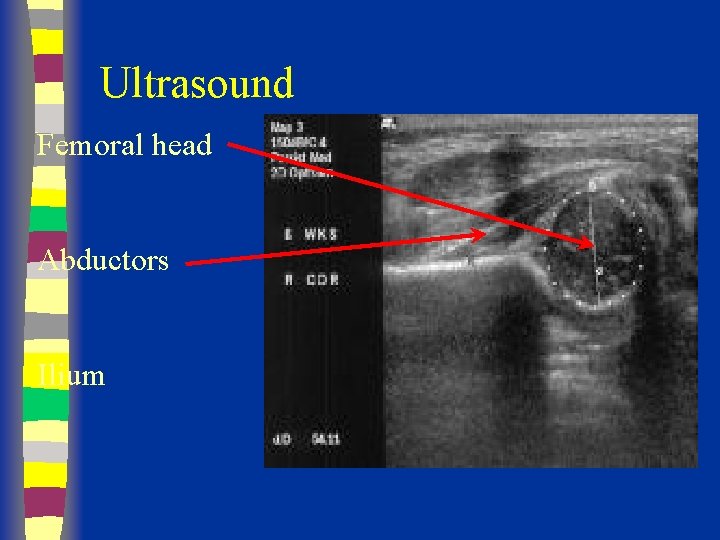
Ultrasound Femoral head Abductors Ilium
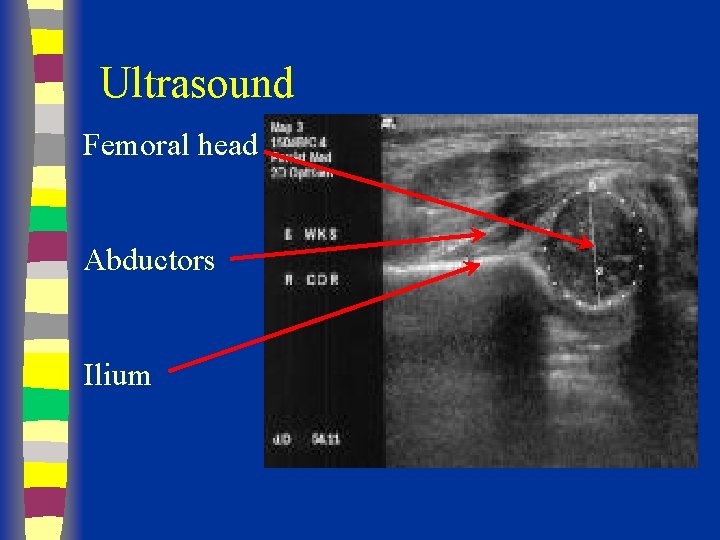
Ultrasound Femoral head Abductors Ilium
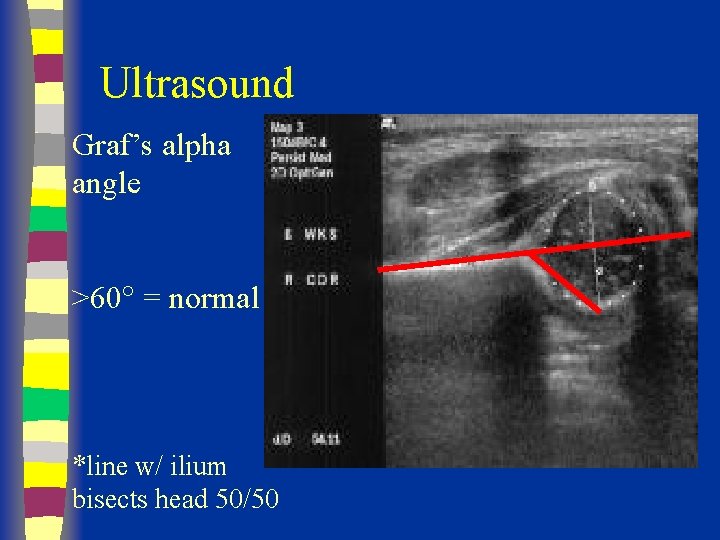
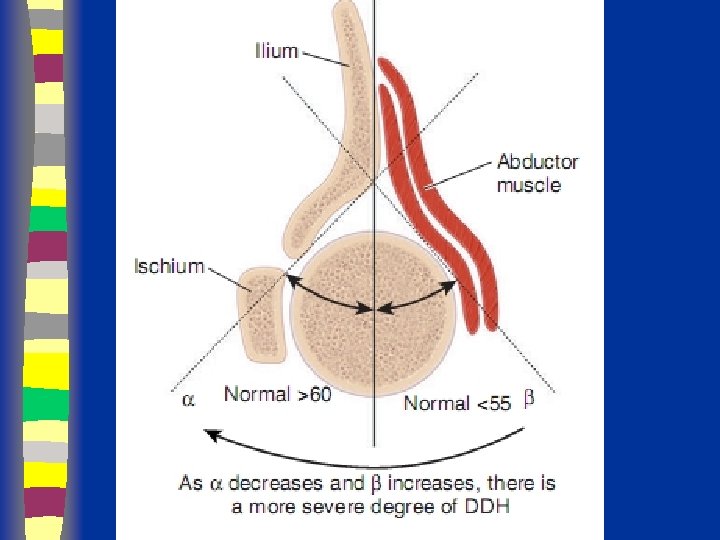
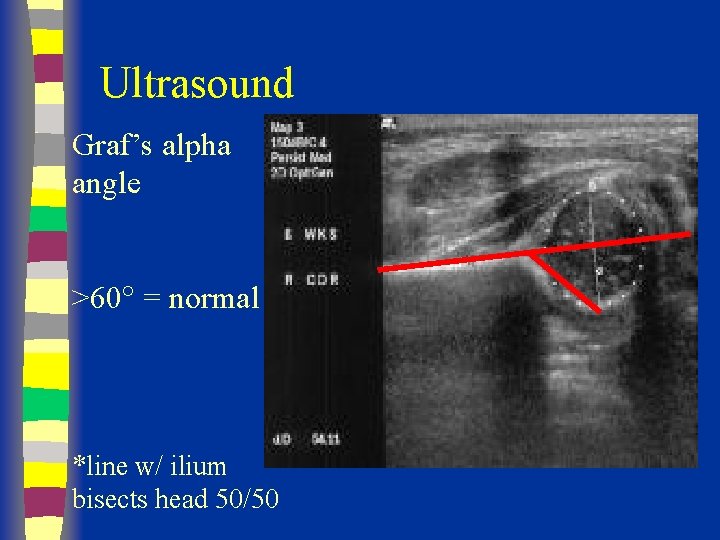
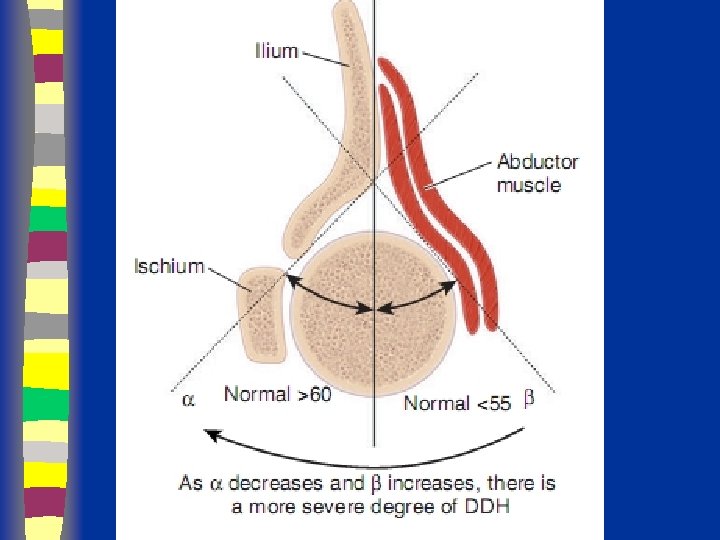
Ultrasound Graf’s alpha angle >60 = normal *line w/ ilium bisects head 50/50
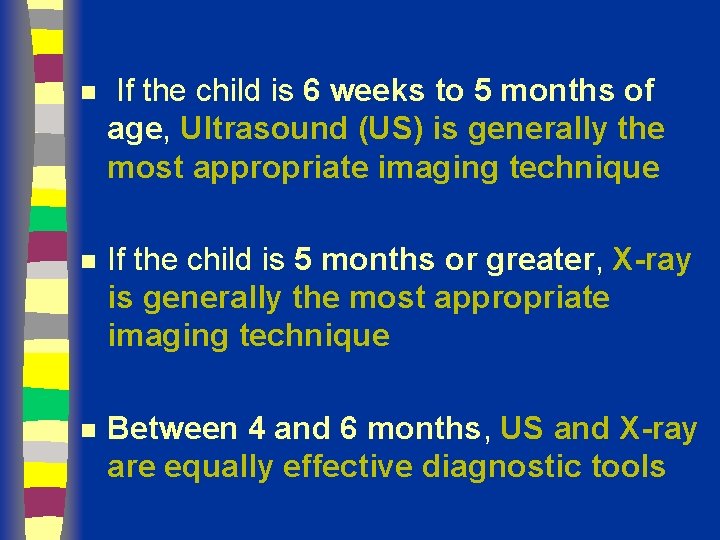
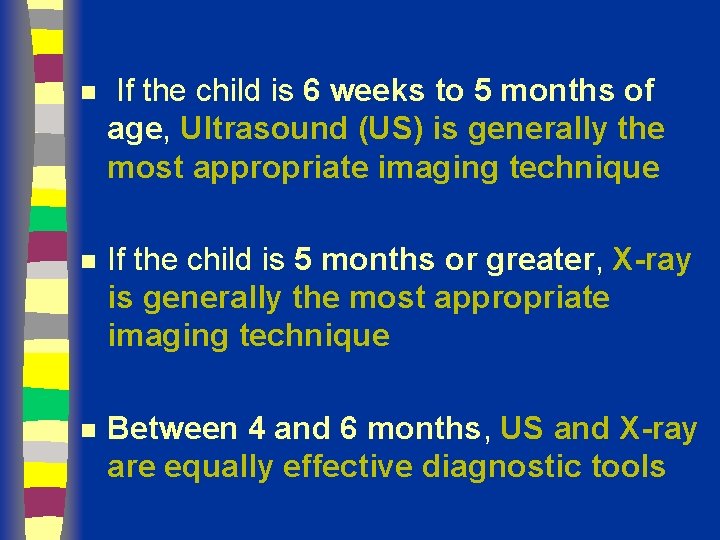
n If the child is 6 weeks to 5 months of age, Ultrasound (US) is generally the most appropriate imaging technique n If the child is 5 months or greater, X-ray is generally the most appropriate imaging technique n Between 4 and 6 months, US and X-ray are equally effective diagnostic tools
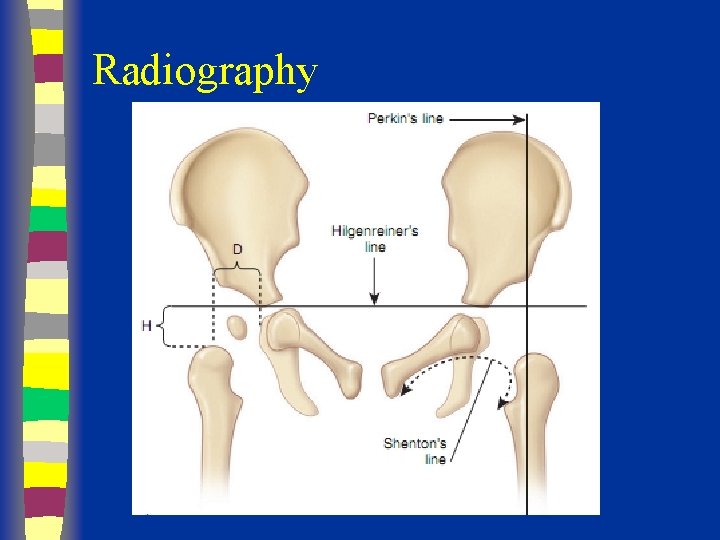
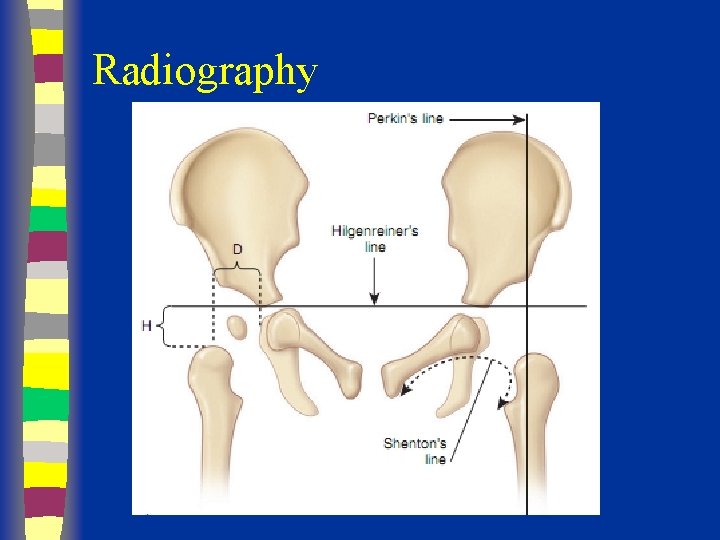
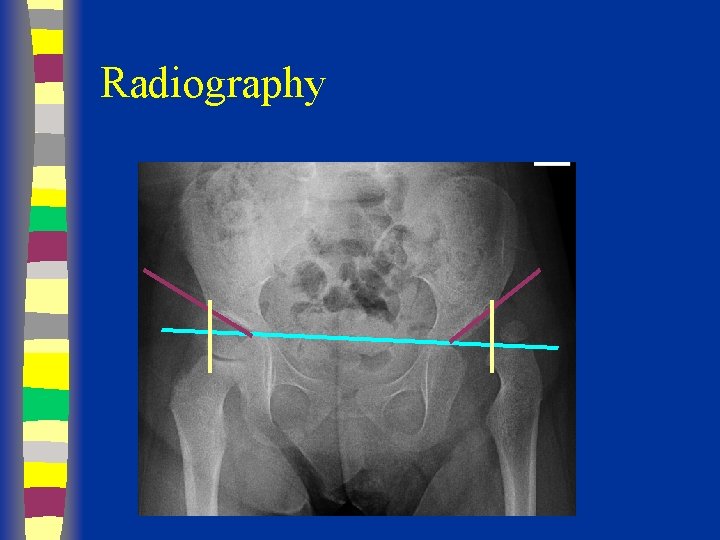
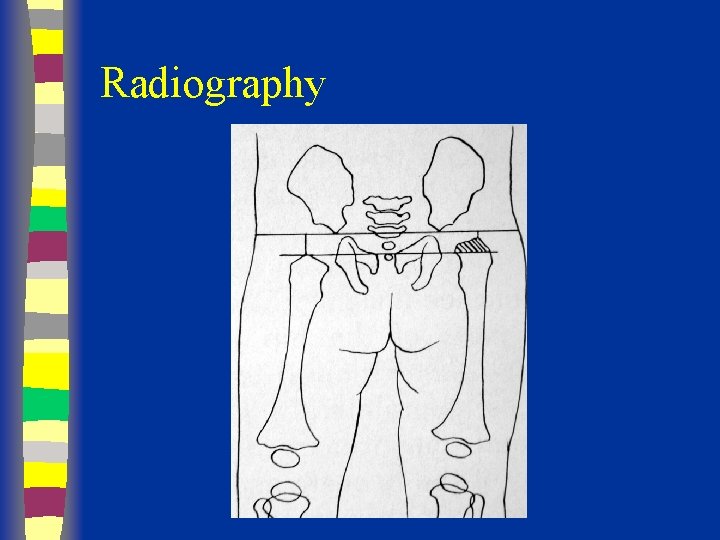
Radiography
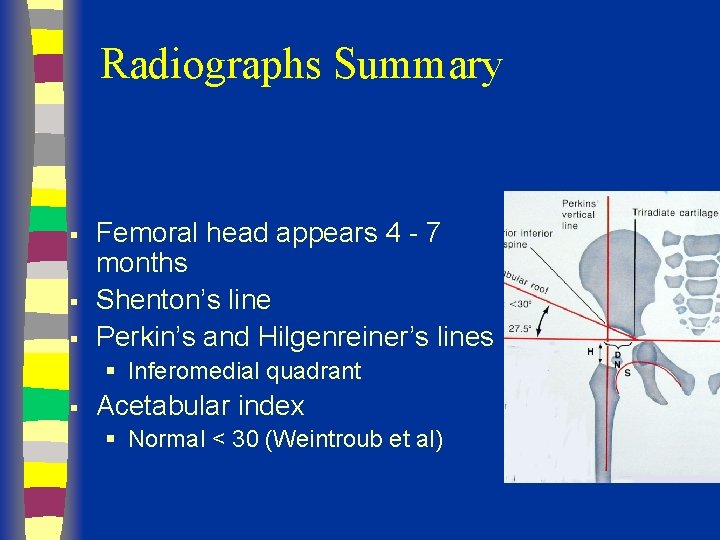
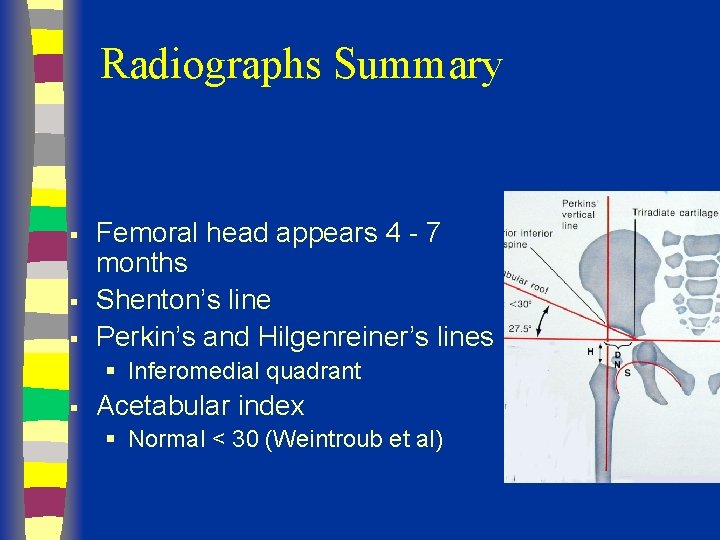
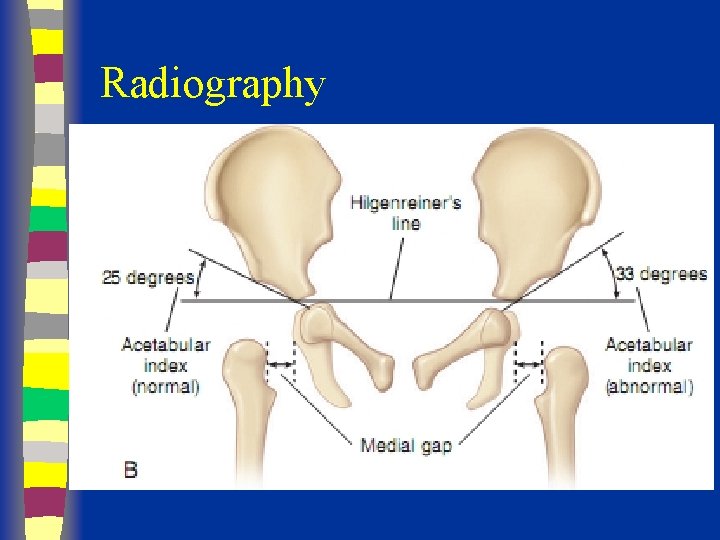
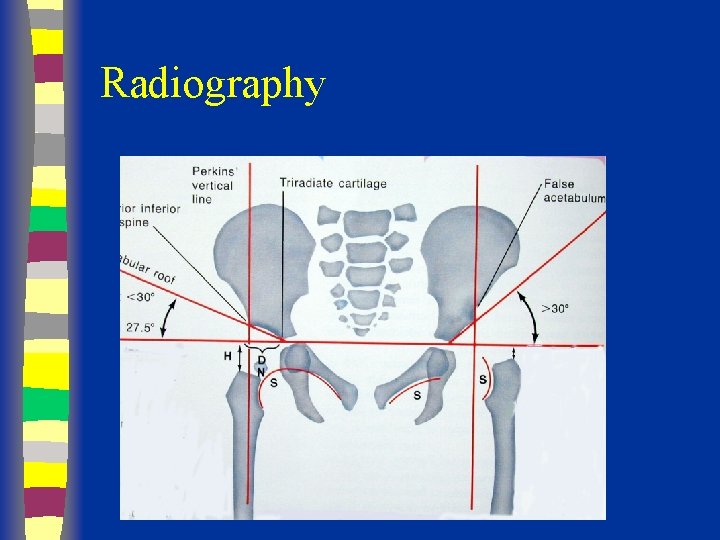
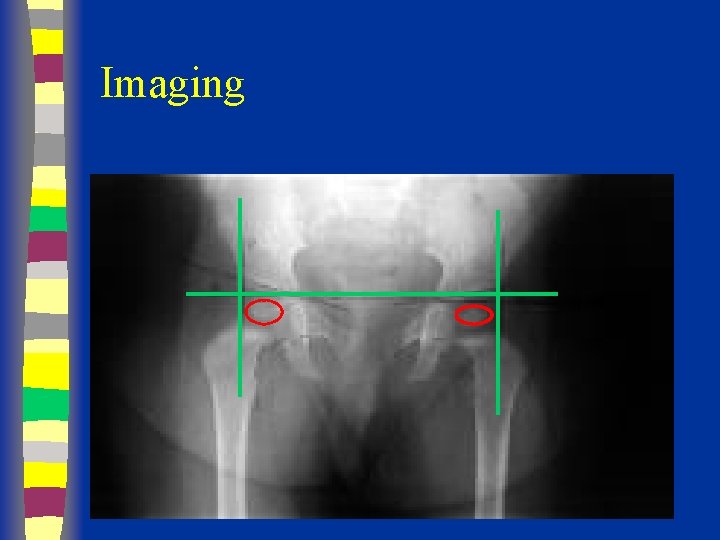
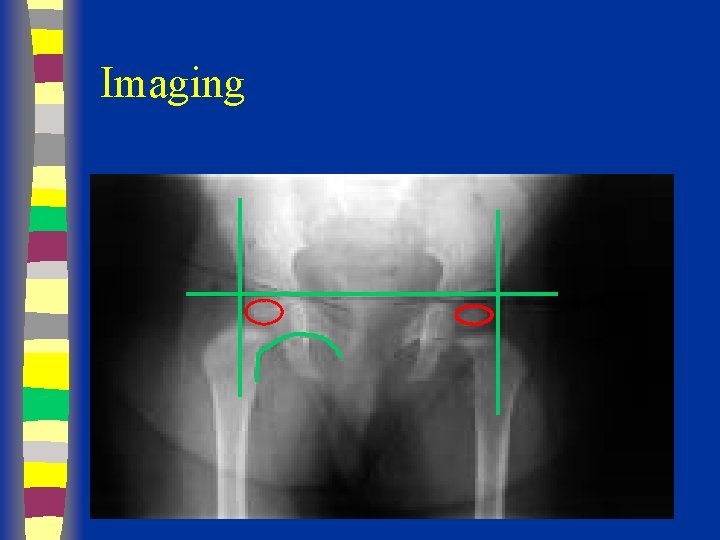
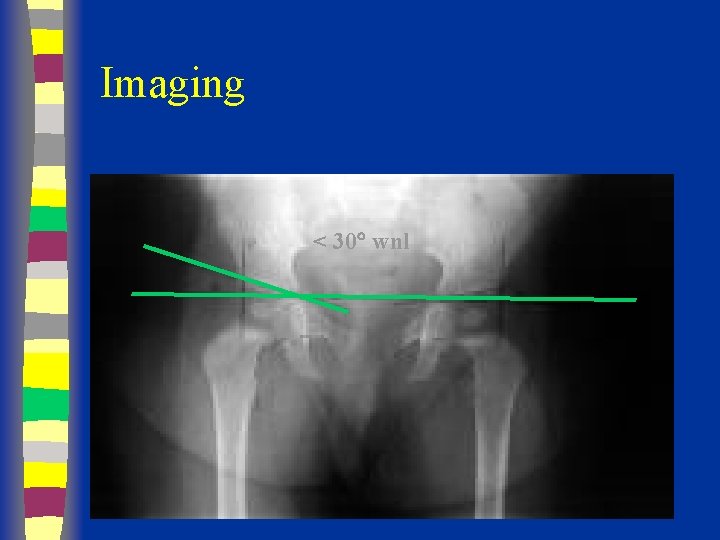
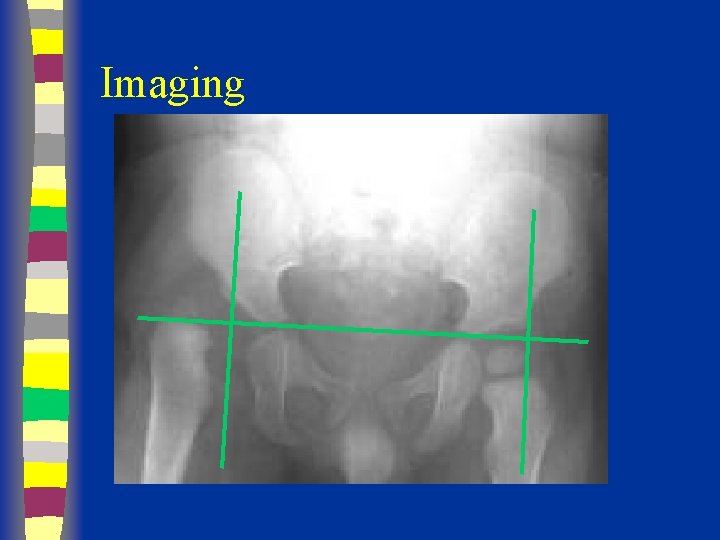
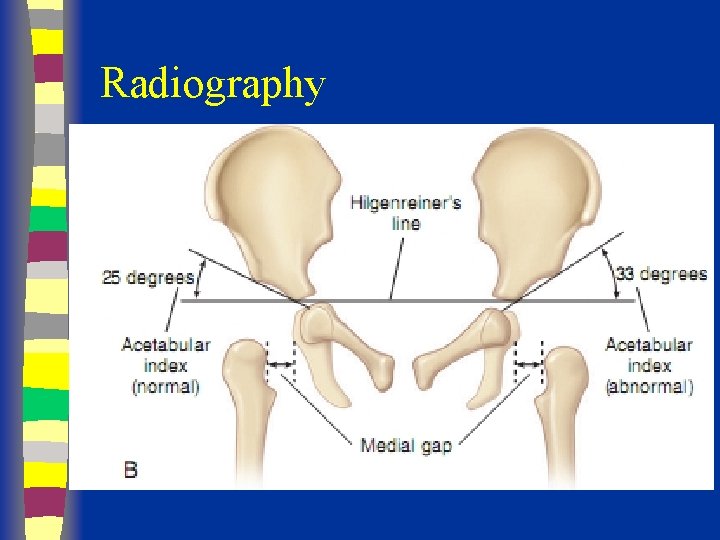
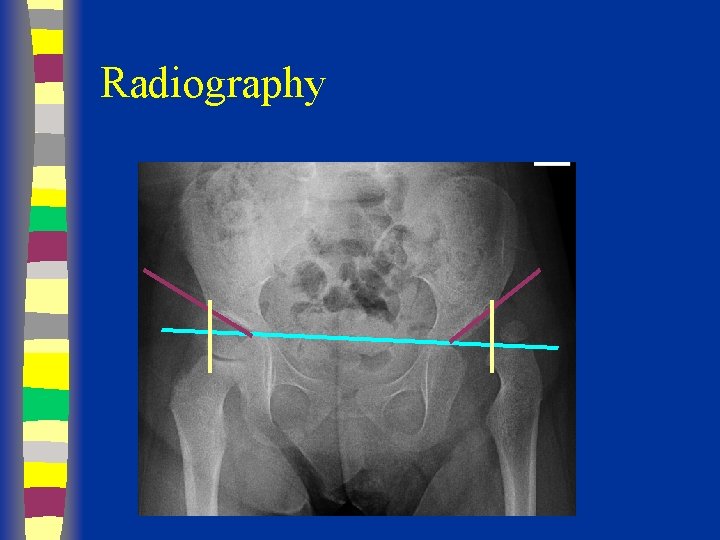
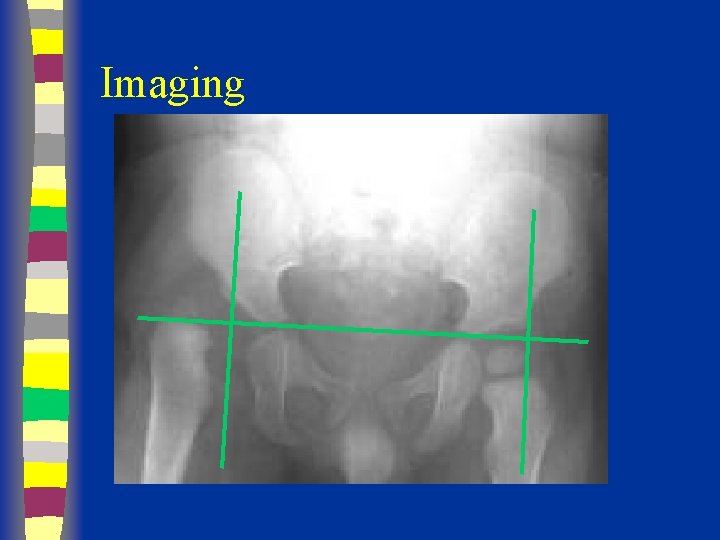
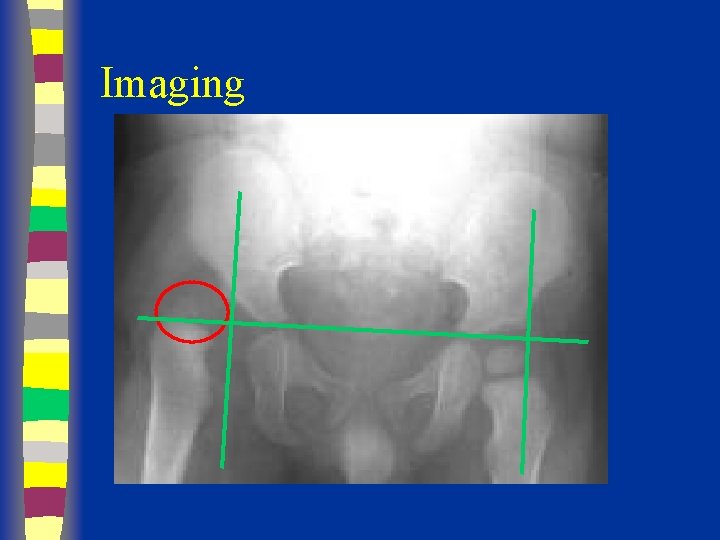
Radiographs Summary § § § Femoral head appears 4 - 7 months Shenton’s line Perkin’s and Hilgenreiner’s lines § Inferomedial quadrant § Acetabular index § Normal < 30 (Weintroub et al)
Radiography
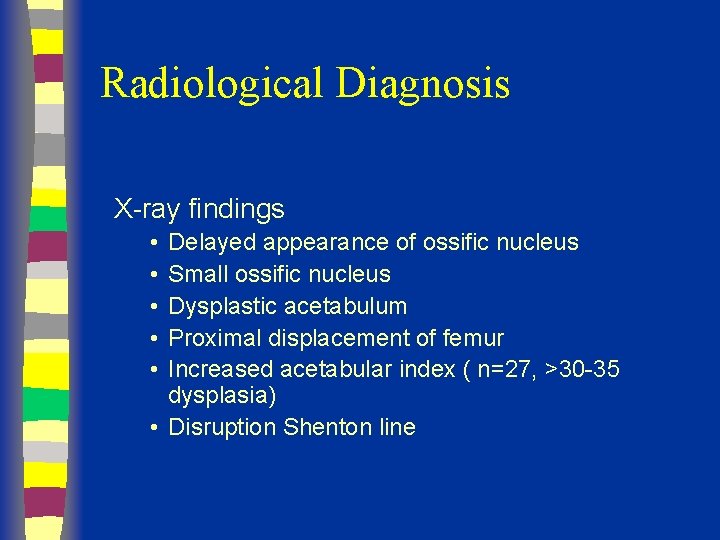
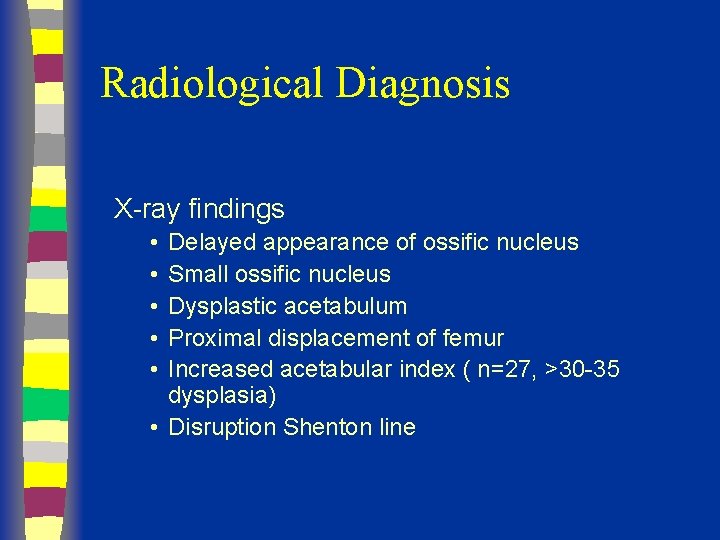
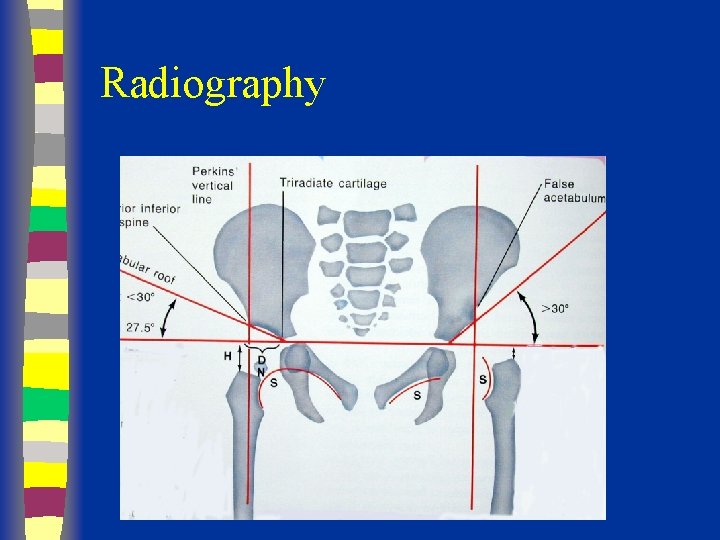
Radiological Diagnosis X-ray findings • • • Delayed appearance of ossific nucleus Small ossific nucleus Dysplastic acetabulum Proximal displacement of femur Increased acetabular index ( n=27, >30 -35 dysplasia) • Disruption Shenton line
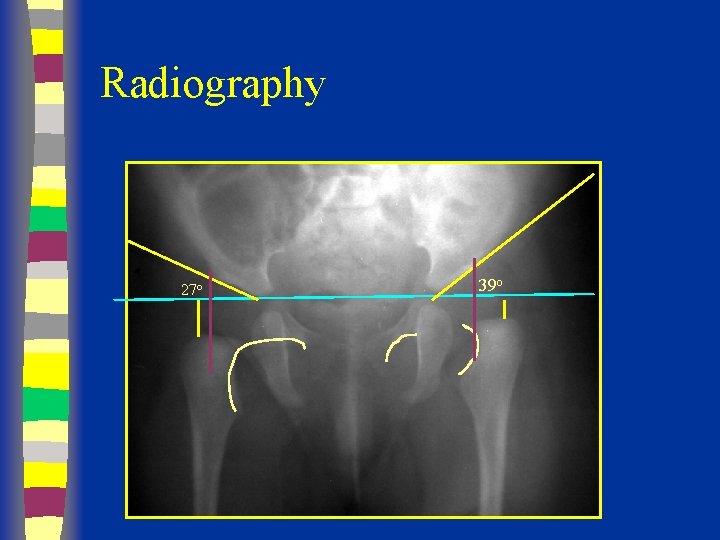
Radiography
Radiography
Radiography in out
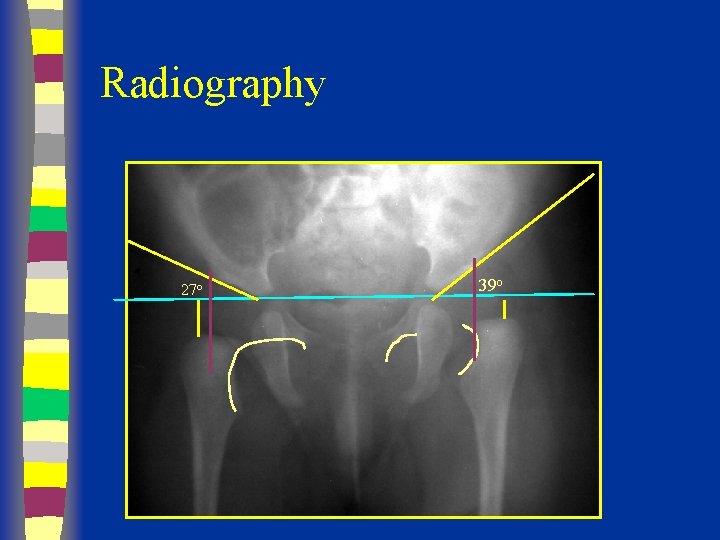
Radiography 27 o 39 o
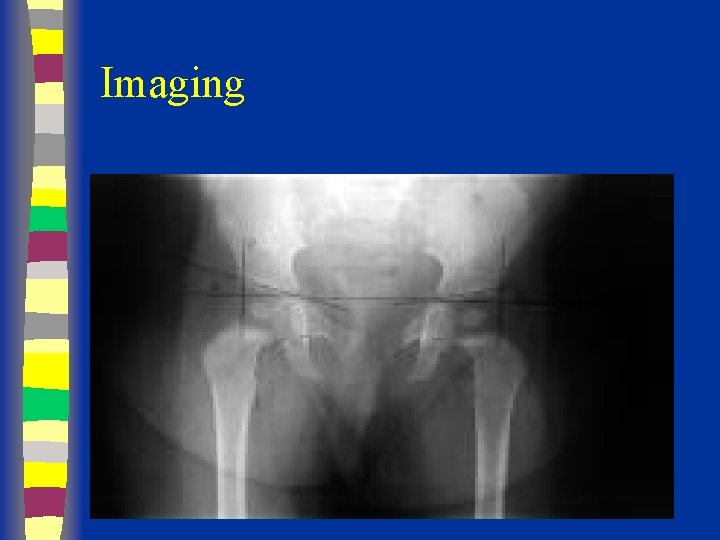
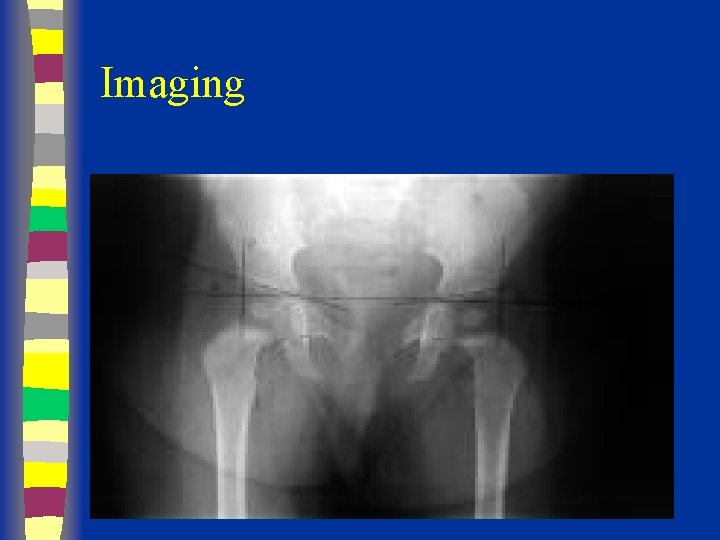
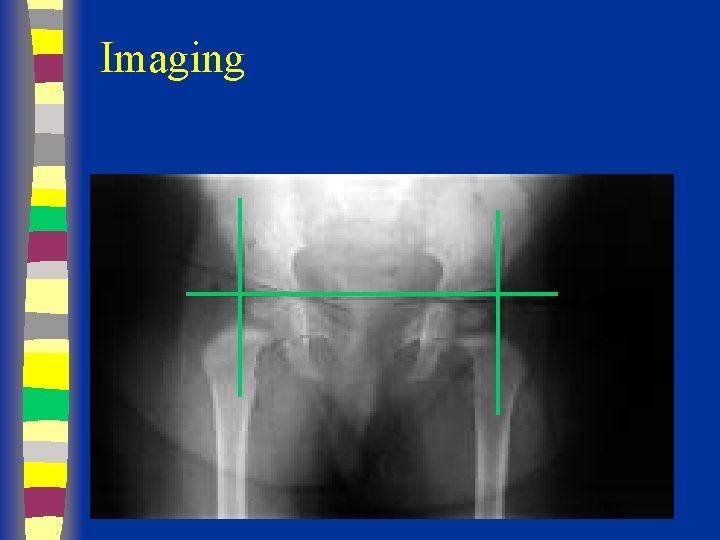
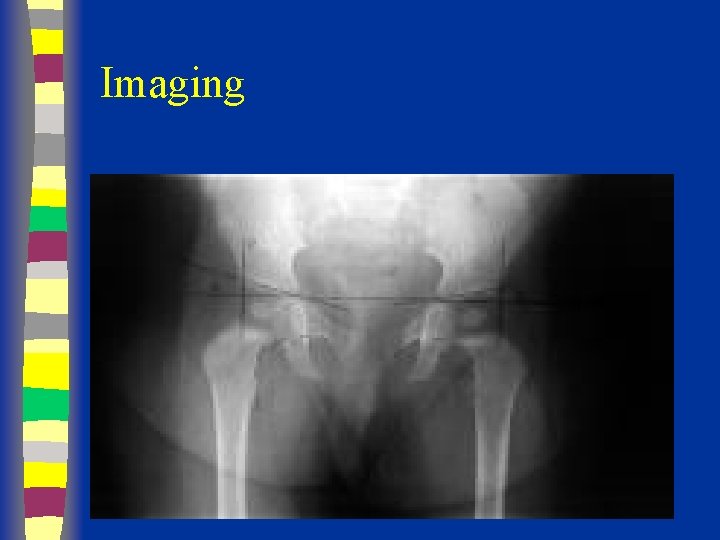
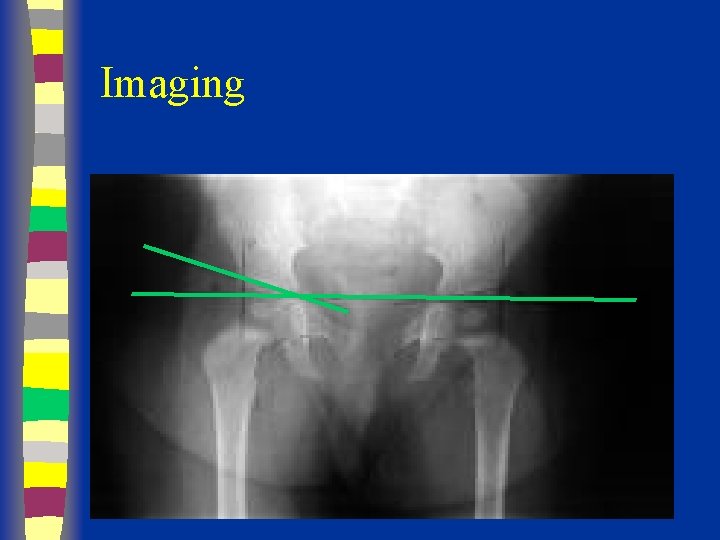
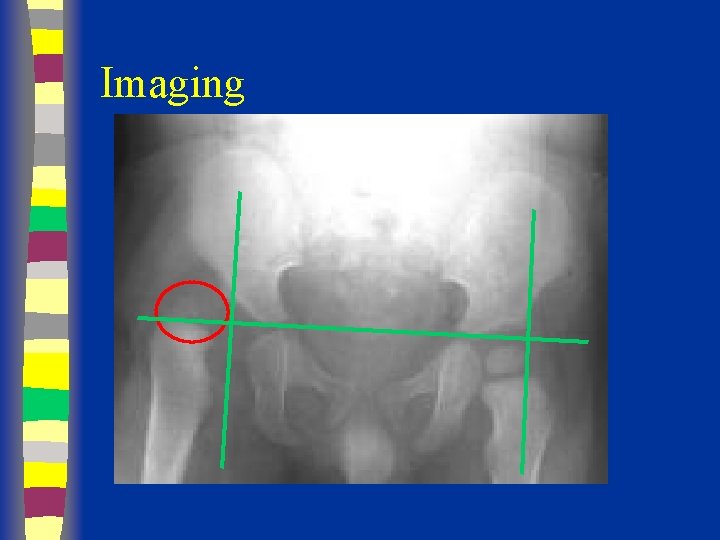
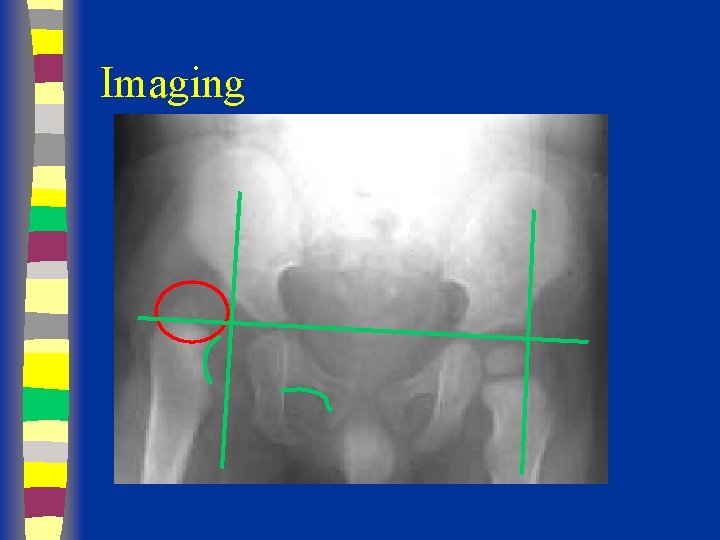
Imaging
Imaging
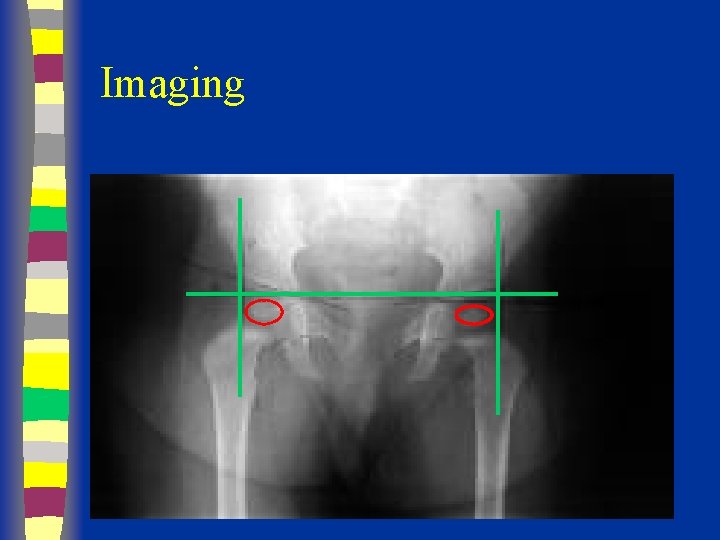
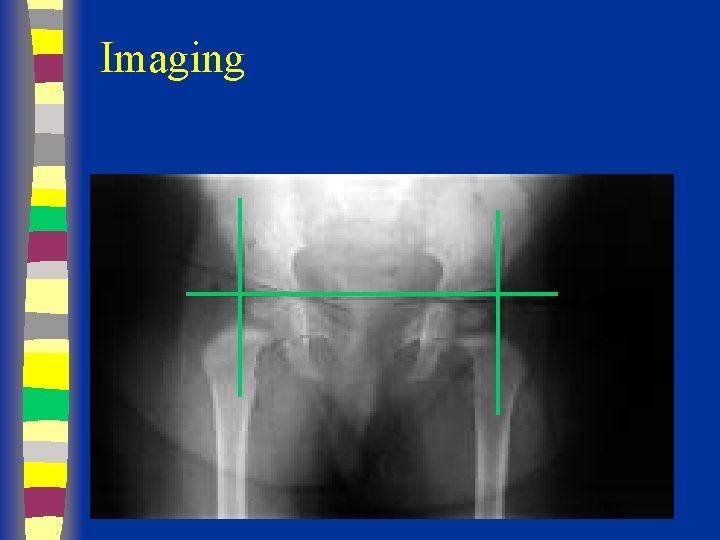
Imaging
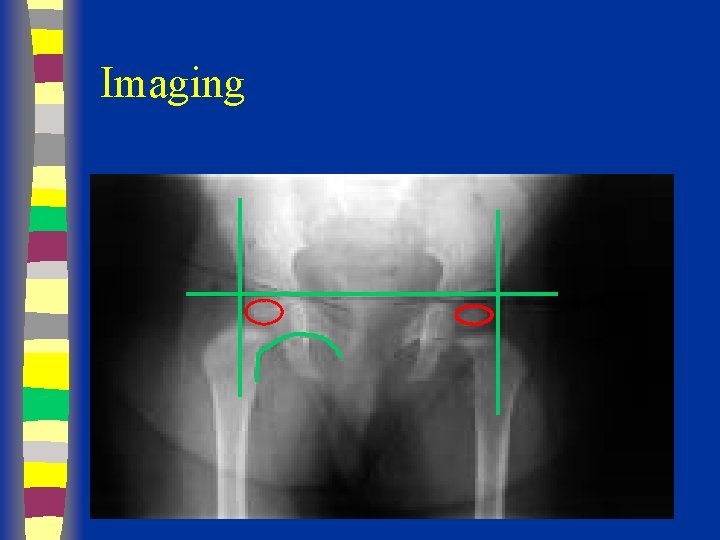
Imaging
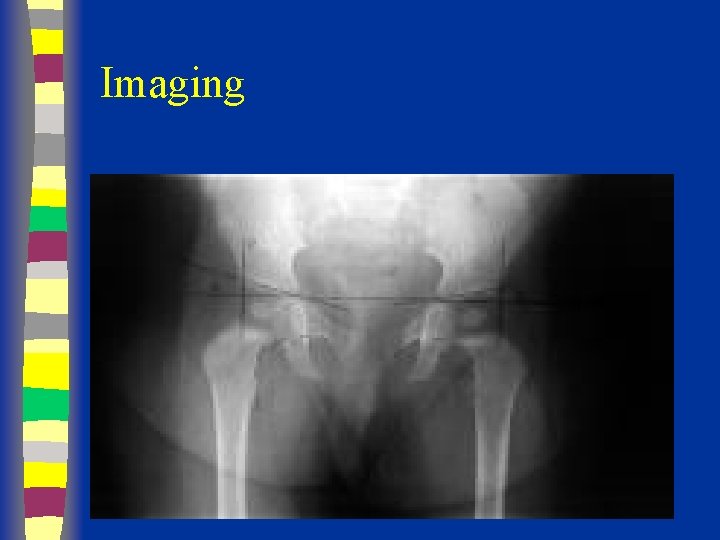
Imaging
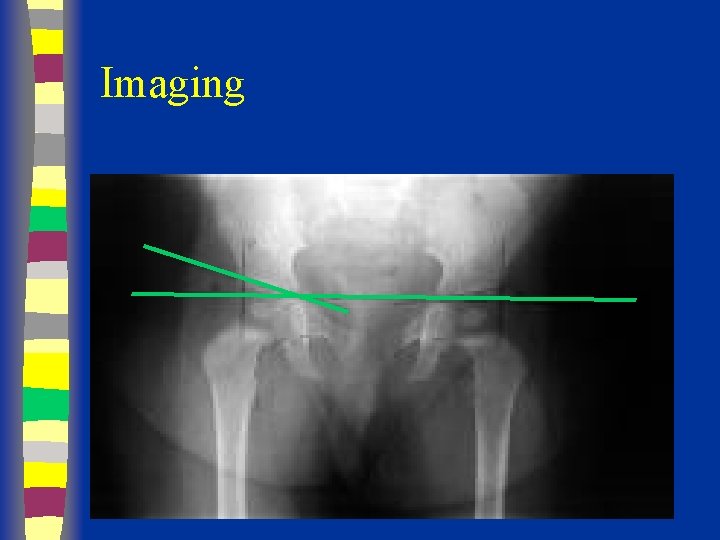
Imaging
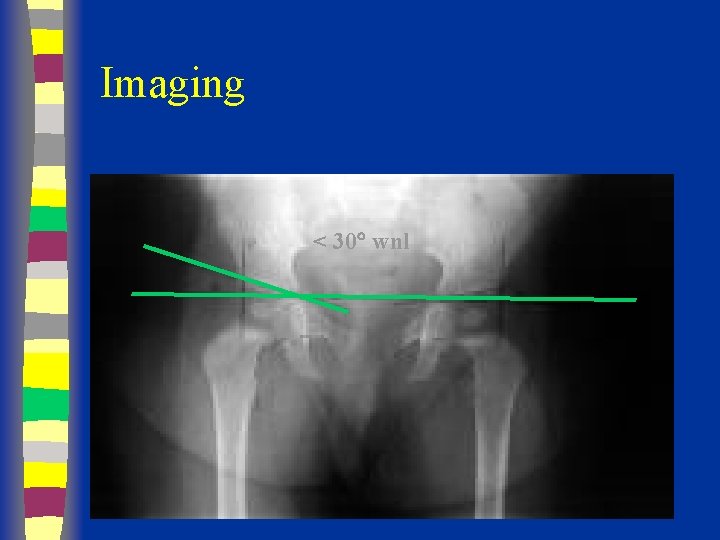
Imaging < 30 wnl
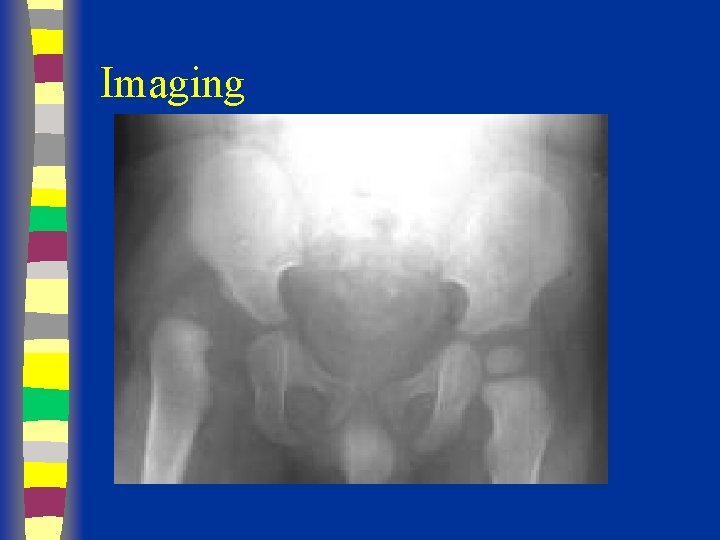
Imaging
Imaging
Imaging
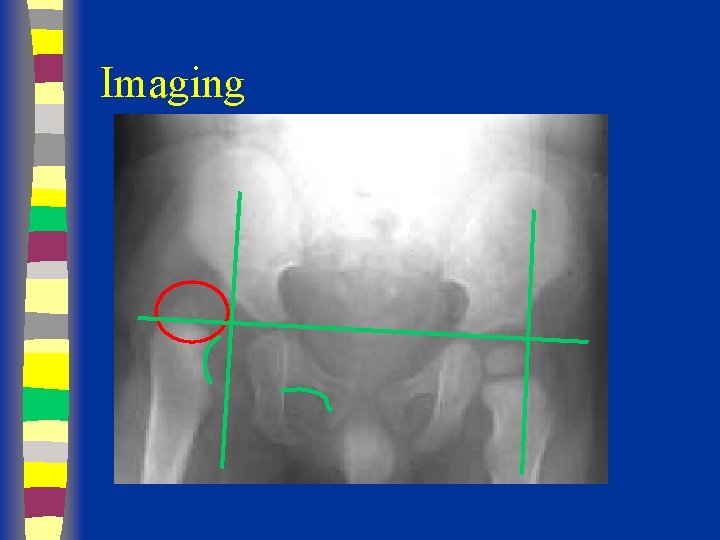
Imaging
Treatment Options § § § Age of patient at presentation Family factors Reducibility of hip Stability after reduction Amount of acetabular dysplasia
Treatment n The presence of the spherical femoral head within the acetabulum is critical for stimulating normal development of the acetabulum n Aims – Obtain and Maintain concentric reduction – In an Atruamatic fashion – Without disrupting the blood supply
Treatment n Method depends on Age n The earlier started, the easier the treatment n The earlier started, the better the results n Should be detected EARLY
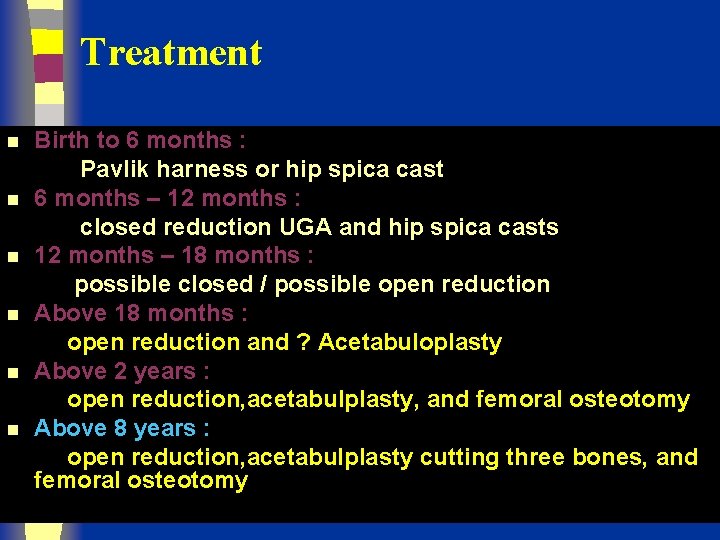
Treatment n n n Birth to 6 months : Pavlik harness or hip spica cast 6 months – 12 months : closed reduction UGA and hip spica casts 12 months – 18 months : possible closed / possible open reduction Above 18 months : open reduction and ? Acetabuloplasty Above 2 years : open reduction, acetabulplasty, and femoral osteotomy Above 8 years : open reduction, acetabulplasty cutting three bones, and femoral osteotomy
Treatment Hip instability in the neonatal period Most resolve spontaneously n n n Observation Pavlik harness Double /triple diapers ? ?
Treatment Hip instability in the neonatal period Double / Triple Diapers n n n Often inadequate : therefore inappropriate Gives illusion patient is in “treatment” while wasting valuable time Most hip instability improves spontaneously in early infancy , giving this ineffective management credit

Treatment Birth – 6 months Hip instability (dislocatable) Established dislocation (reducible) n n n Should be actively treated until hip is normal clinically and radiographically Pavlik harness Hip Spica Cast
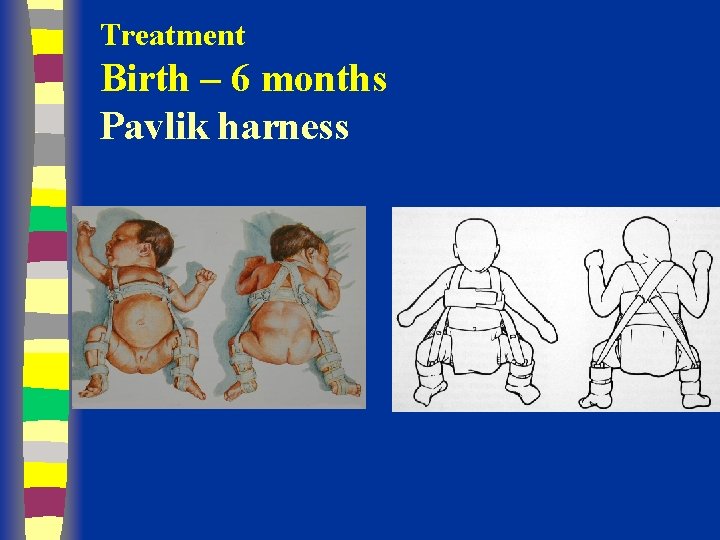
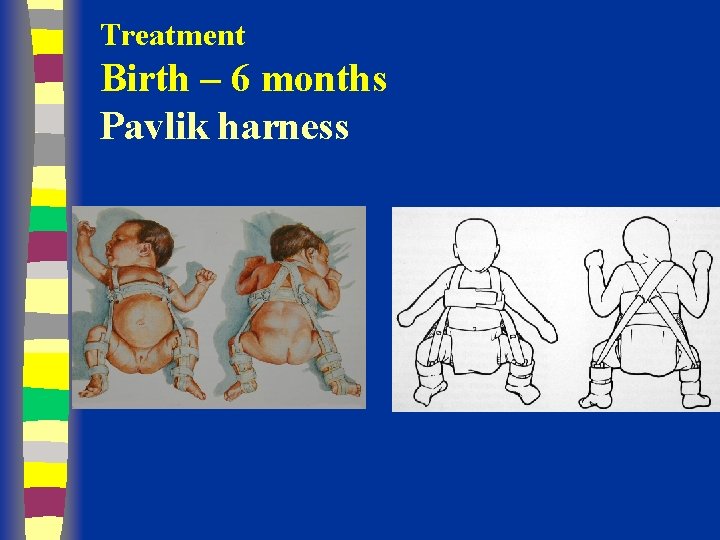
Treatment Birth – 6 months Pavlik harness
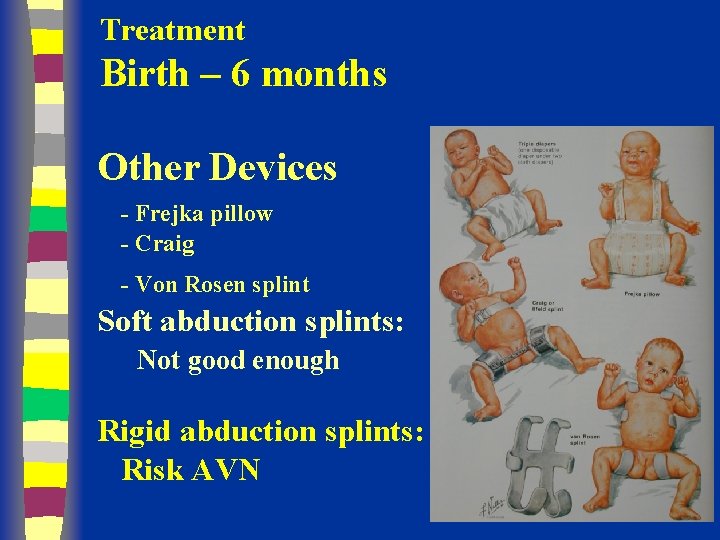
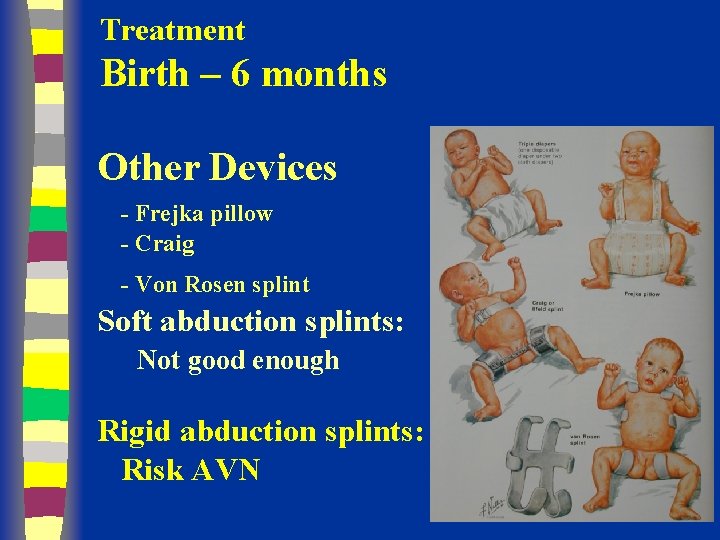
Treatment Birth – 6 months Other Devices - Frejka pillow - Craig - Von Rosen splint Soft abduction splints: Not good enough Rigid abduction splints: Risk AVN
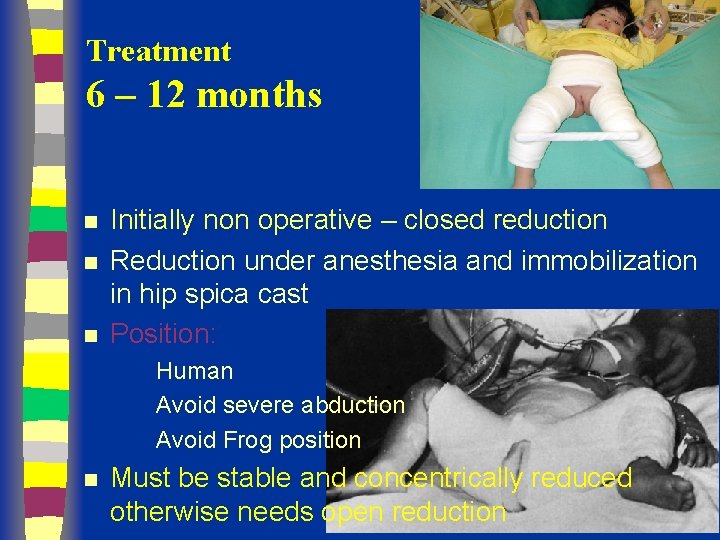
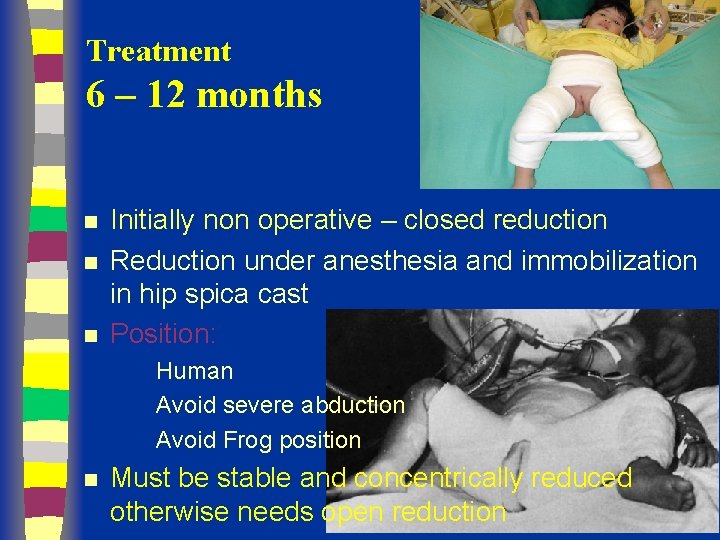
Treatment 6 – 12 months n n n Initially non operative – closed reduction Reduction under anesthesia and immobilization in hip spica cast Position: Human Avoid severe abduction Avoid Frog position n Must be stable and concentrically reduced otherwise needs open reduction
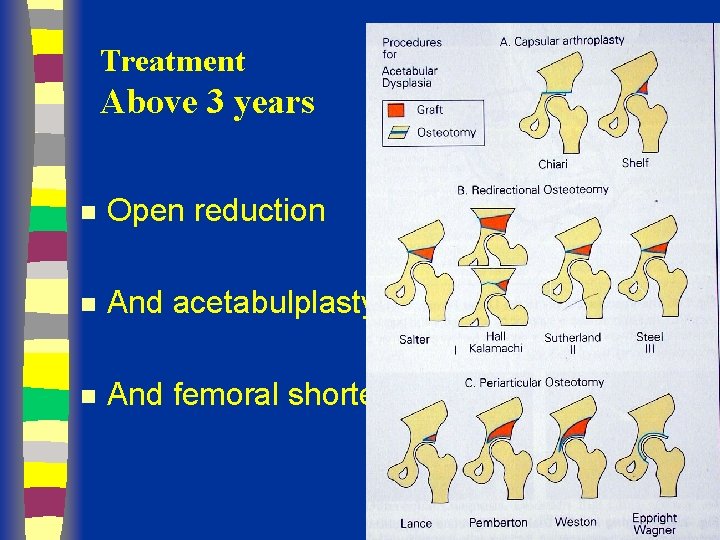
Treatment Above 18 months n Open reduction ? and acetabulplasty ? And femoral shortening – if high
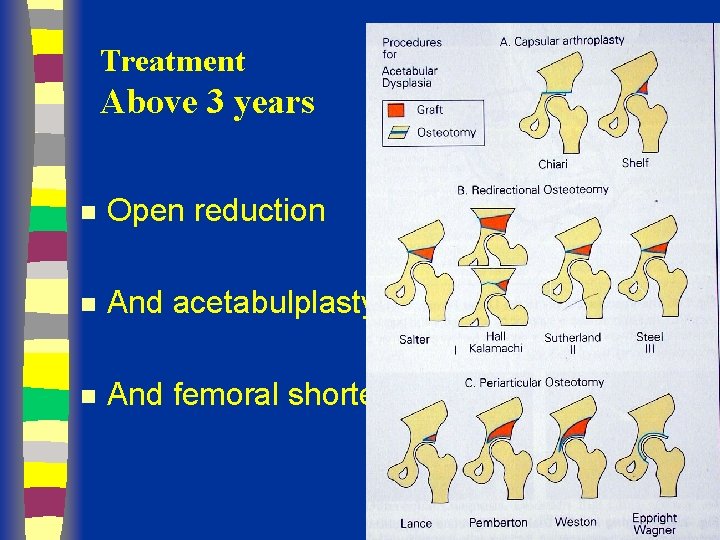
Treatment Above 3 years n Open reduction n And acetabulplasty n And femoral shortening
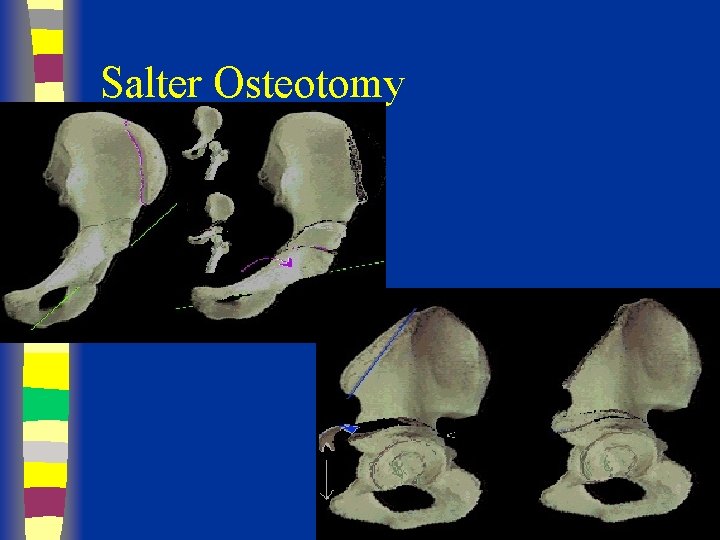
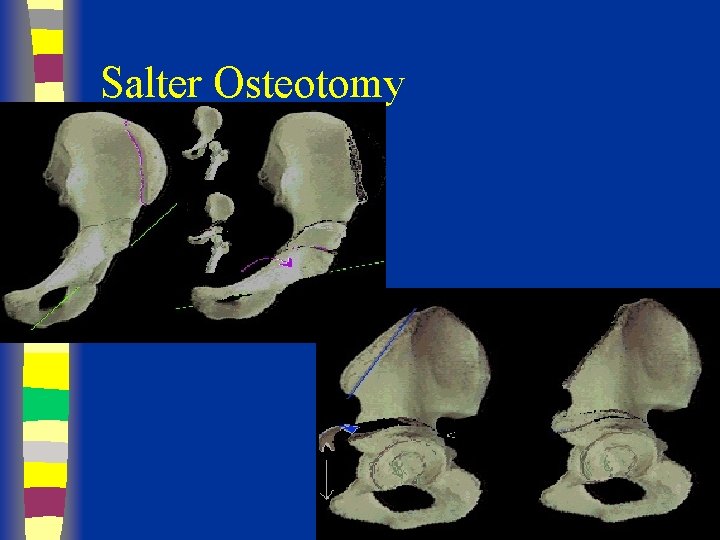
Salter Osteotomy
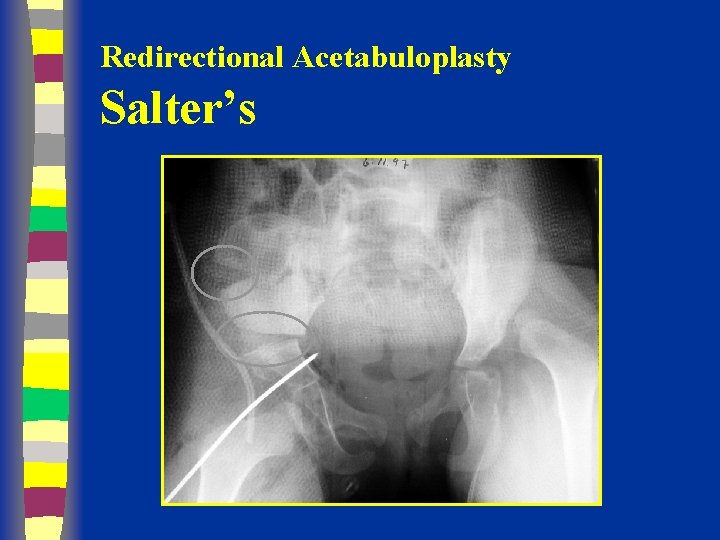
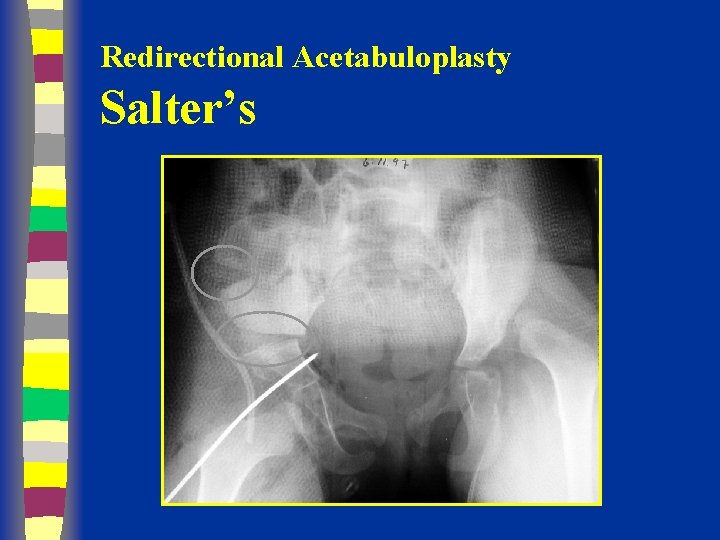
Redirectional Acetabuloplasty Salter’s
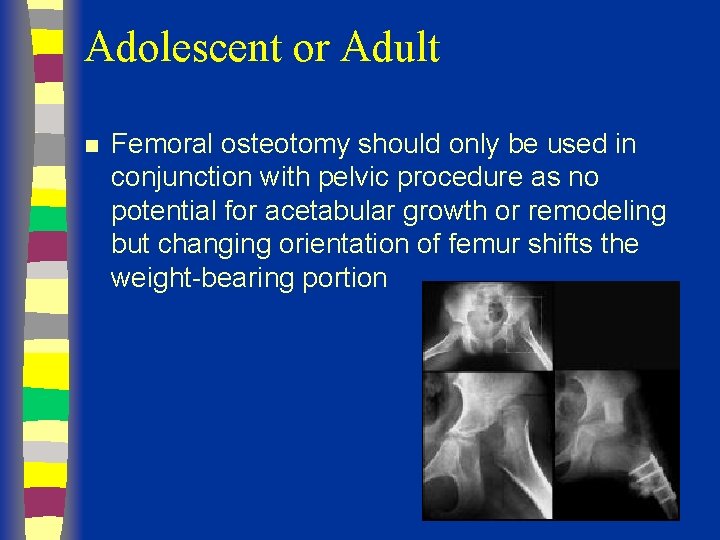
Adolescent or Adult n Femoral osteotomy should only be used in conjunction with pelvic procedure as no potential for acetabular growth or remodeling but changing orientation of femur shifts the weight-bearing portion
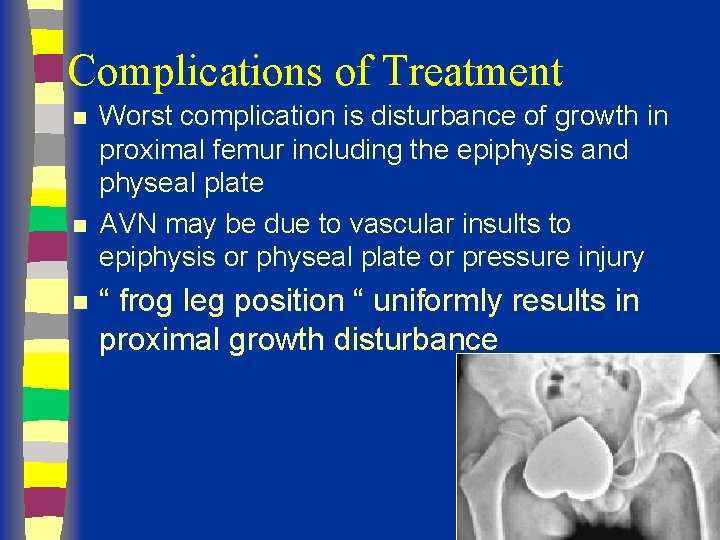
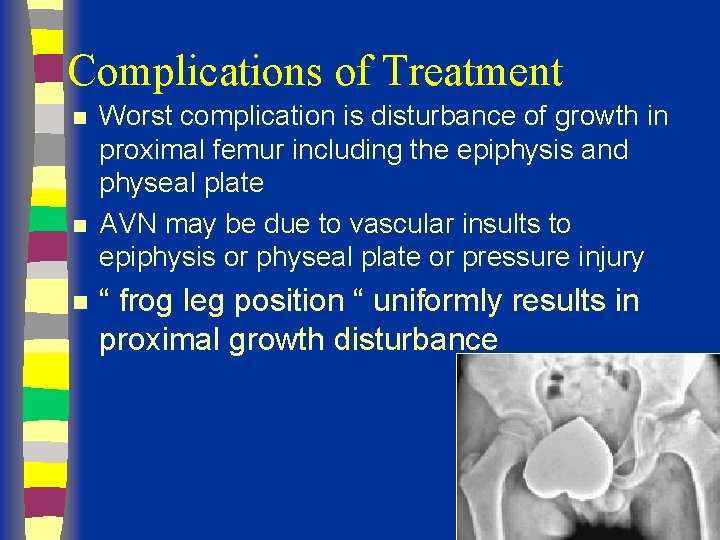
Complications of Treatment n n n Worst complication is disturbance of growth in proximal femur including the epiphysis and physeal plate AVN may be due to vascular insults to epiphysis or physeal plate or pressure injury “ frog leg position “ uniformly results in proximal growth disturbance
Legg Calve Perthes Disease Prepared by Dr fadel Naim MD Orthopedic surgeon 66
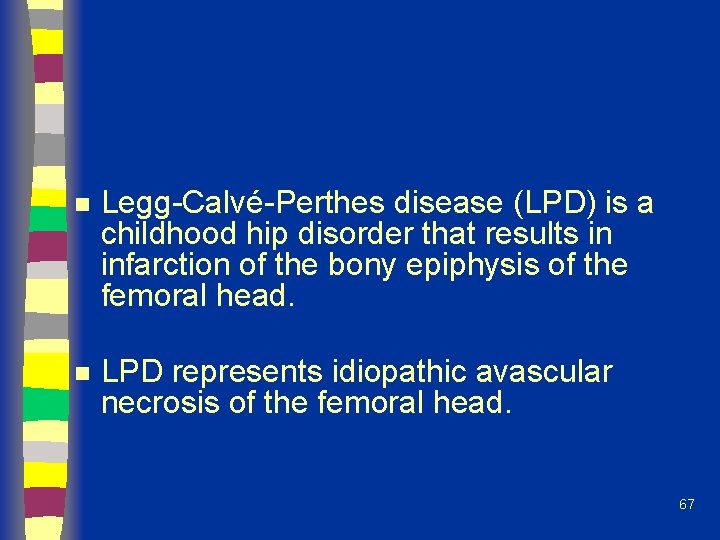
n Legg-Calvé-Perthes disease (LPD) is a childhood hip disorder that results in infarction of the bony epiphysis of the femoral head. n LPD represents idiopathic avascular necrosis of the femoral head. 67
Epidemiology n Disorder of the hip in young children n Usually ages 4 -8 yo As early as 2 yo, as late as teens Boys: Girls= 4 -5: 1 Bilateral 10 -12% No evidence of inheritance incidence of positive family hx ranges from 1. 6% to 20% n n n 68
Etiology n n n Unknown Past theories: infection, inflammation, trauma, congenital Most current theories involve vascular compromise 69
Pathophysiology n The primary pathologic abnormality is osteonecrosis resulting in flattening and collapse of the femoral head. n The basic underlying cause of LPD is insufficient blood supply to the femoral head. n Healing occurs by revascularization of the necrotic femoral head. 70
Radiographic Stages n Four Waldenstrom stages: – 1) Initial stage – 2) Fragmentation stage – 3) Reossification stage – 4) Healed stage 71
Initial Stage n Early radiographic signs: – Widening of medial joint space – “Crescent sign” – Irregular physeal plate – Blurry/ radiolucent metaphysis 72

73
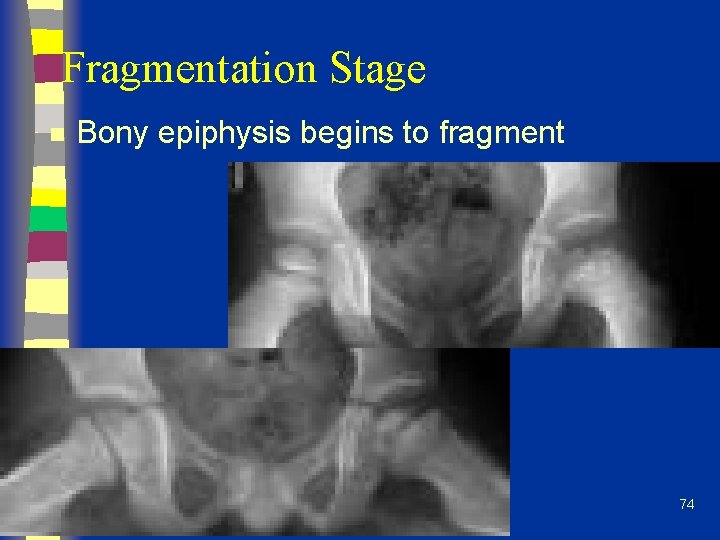
Fragmentation Stage n Bony epiphysis begins to fragment 74

Reossification Stage 75
Presentation n n Often insidious onset of a limp C/O pain in groin, thigh, knee 17% relate trauma hx Can have an acute onset 76
Legg-Calve-Perthes Disease n n n n CLINICAL FINDINGS Prolonged limp Waddling gait Pain in groin or thigh Limited painful motion Tenderness to palpation over hip Gluteal Atrophy Trendelenberg sign Positive Leg Length Discrepancy
Physical Exam Decreased ROM, especially abduction and internal rotation n Adductor contracture n Trendelenburg test often positive n Muscular atrophy of thigh/buttock/calf n Limb length discrepency n 78
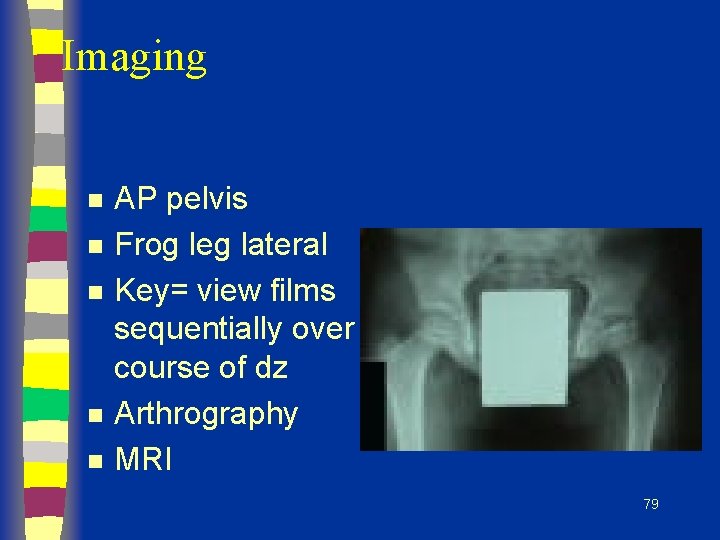
Imaging n n n AP pelvis Frog leg lateral Key= view films sequentially over course of dz Arthrography MRI 79
Differential Diagnosis n n Important to rule out infectious etiology (septic arthritis, toxic synovitis) Others: – Chondrolysis – JRA – Osteomyelitis – Lymphoma -Neoplasm -Sickle Cell -Traumatic AVN -Medication 80
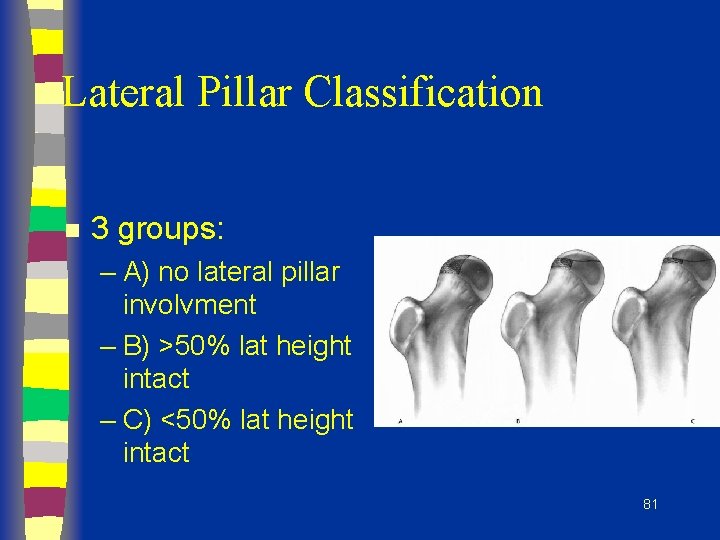
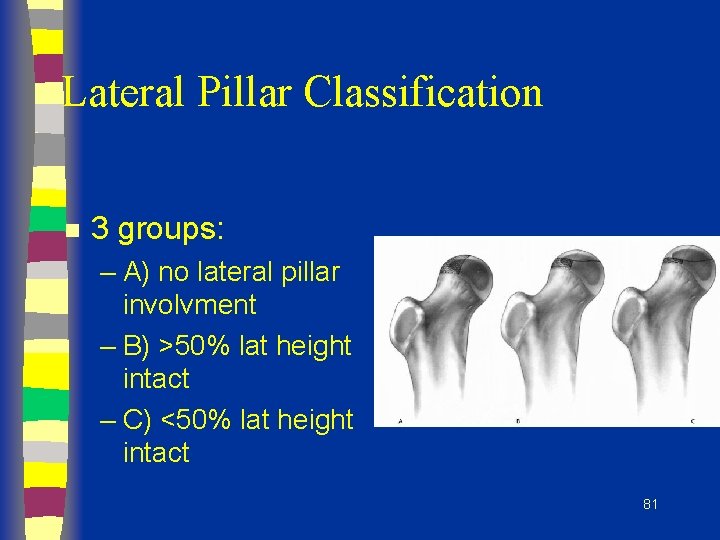
Lateral Pillar Classification n 3 groups: – A) no lateral pillar involvment – B) >50% lat height intact – C) <50% lat height intact 81
Prognosis n n 60% of kids do well without tx AGE is key prognostic factor: – <6 yo= good outcome regardless of tx – 6 -8 yo= not always good results with just containment – >9 yo= containment option is questionable, poorer prognosis, significant residual defect n Flat femoral head incongruent with acetabulum= worst prognosis 82
The Goal of Treatment n The goal of treatment is four-fold: I) to reduce hip irritability 2) restore and maintain hip mobility 3) to prevent the ball from extruding or collapsing 4) to regain a spherical femoral head 83
Non-operative Tx n Improve ROM 1 st –-abduction usually affected most of ROM – -use PT to regain abduction (overcome spasm) and internal rotation – -may require several weeks of abduction traction 84
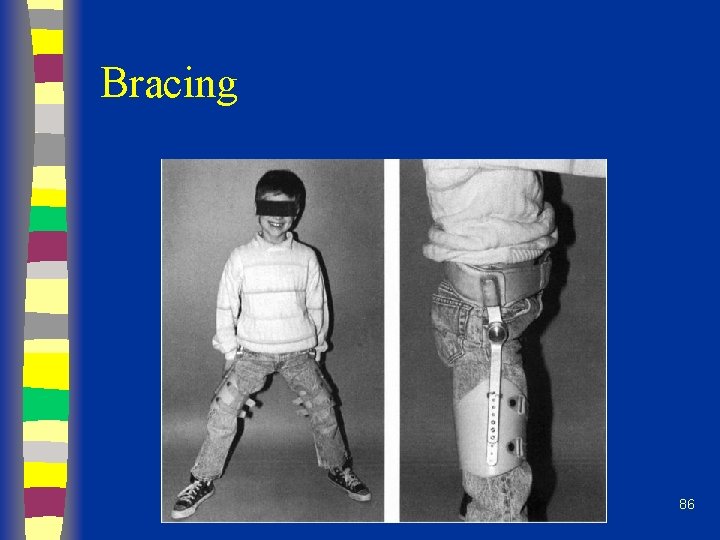
Non-operative Tx n Bracing: – Removable abduction orthosis – Pietrie casts – Hips abducted and internally rotated n n n Not necessarily NWB Hips braced in abd/ int rotation to transmit weight over wide area of acetabulum, prevents head collapse Wean from brace when improved x-ray healing signs 85
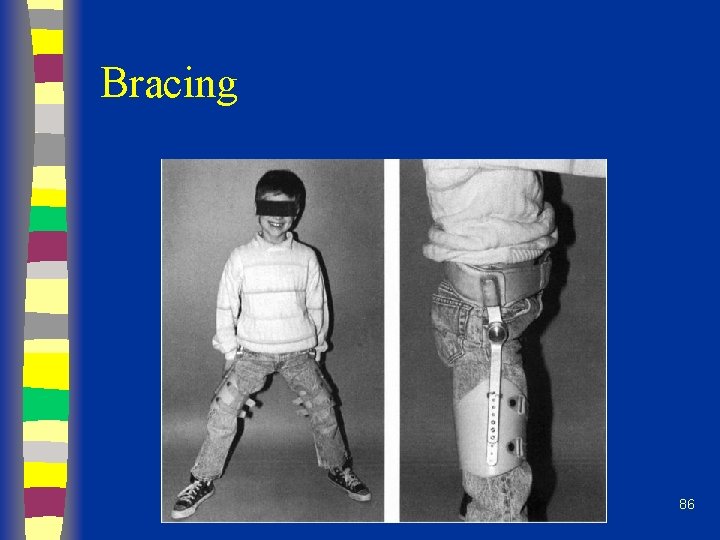
Bracing 86
Non-operative Tx n Check serial radiographs – Q 3 -4 mos with ROM testing n Continue bracing until: – Lateral column ossifies – Sclerotic areas in epiphysis gone n Cast/brace uninvolved side 87
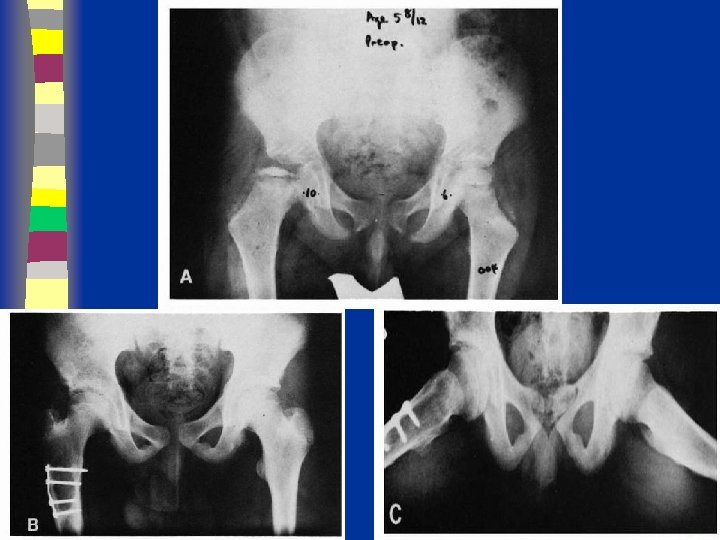
Operative Tx n n If non-op tx cannot maintain containment Surgically ideal pt: – 6 -9 yo – Catterral II-III – Good ROM – In collapsing phase 88
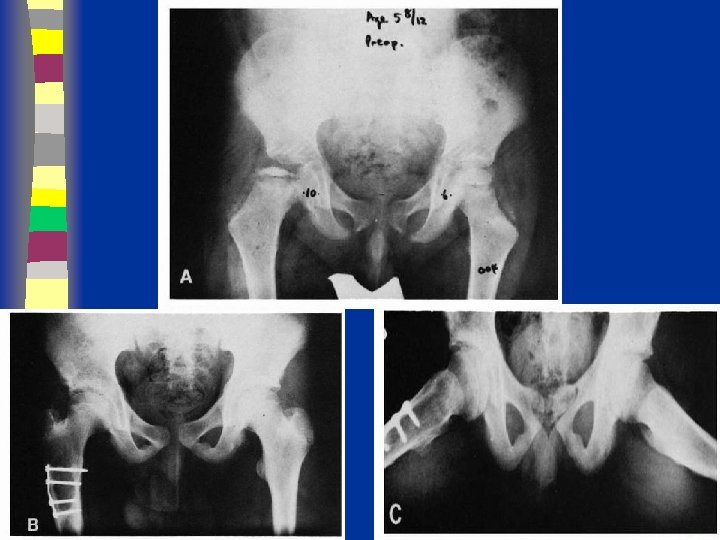
Surgical Tx n Surgical options: – Excise lat extruding head portion to stop hinging abduction – Acetabular (innominate) osteotomy to cover head – Varus femoral osteotomy – Arthrodesis 89
Late Effects of LCP n n Coxa magna Physeal arrest patterns Irregular head formation Osteochondritis dessicans 91

SCFE
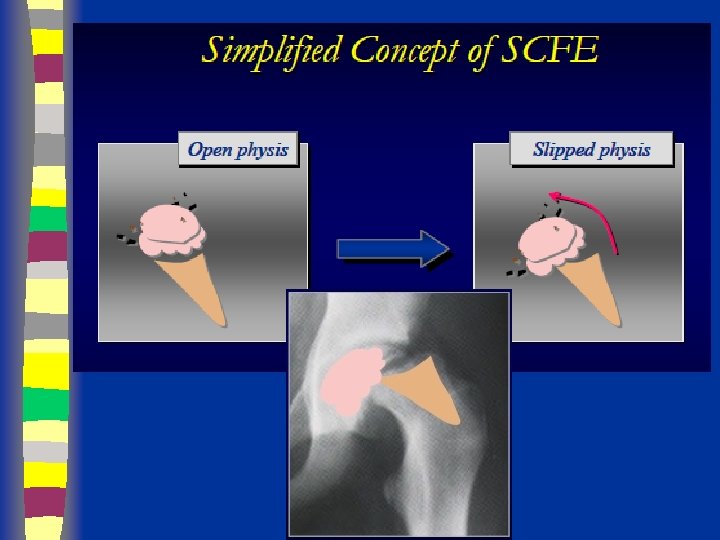
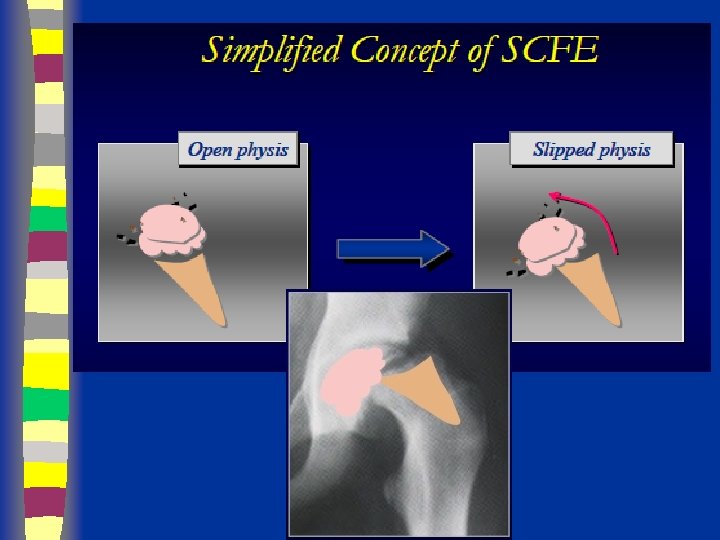
Definition n The femoral neck and shaft displace upward anteriorly on the capital epiphysis, which displaces primarily posteriorly relative to the femoral neck

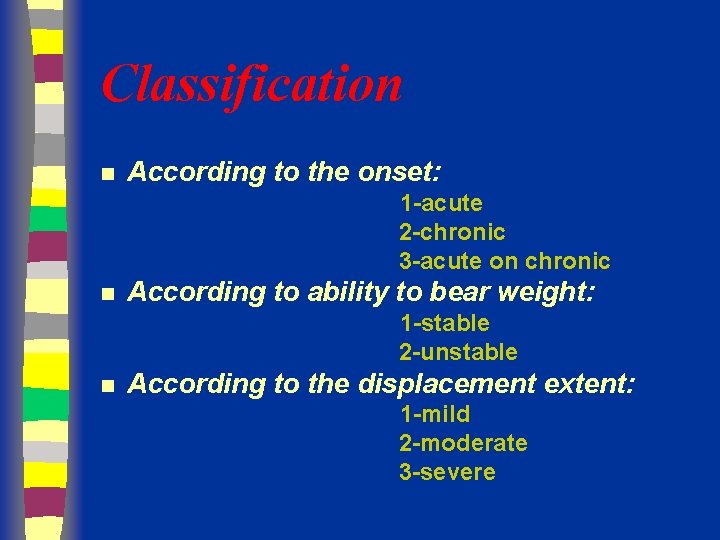
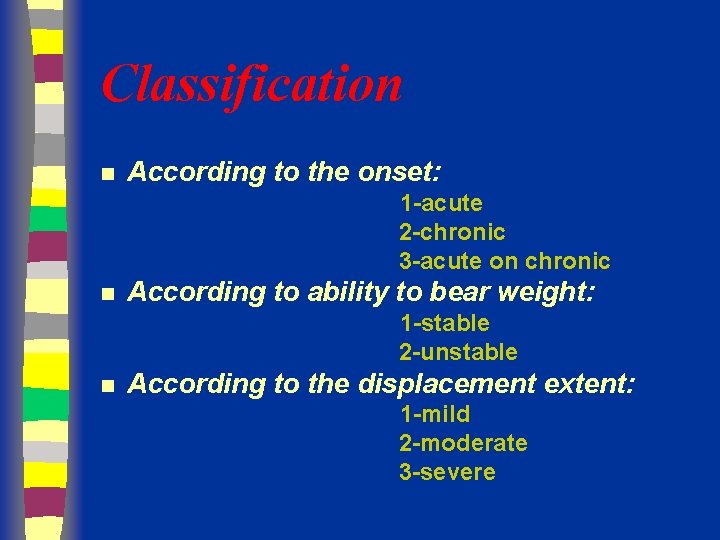
Classification n According to the onset: 1 -acute 2 -chronic 3 -acute on chronic n According to ability to bear weight: 1 -stable 2 -unstable n According to the displacement extent: 1 -mild 2 -moderate 3 -severe
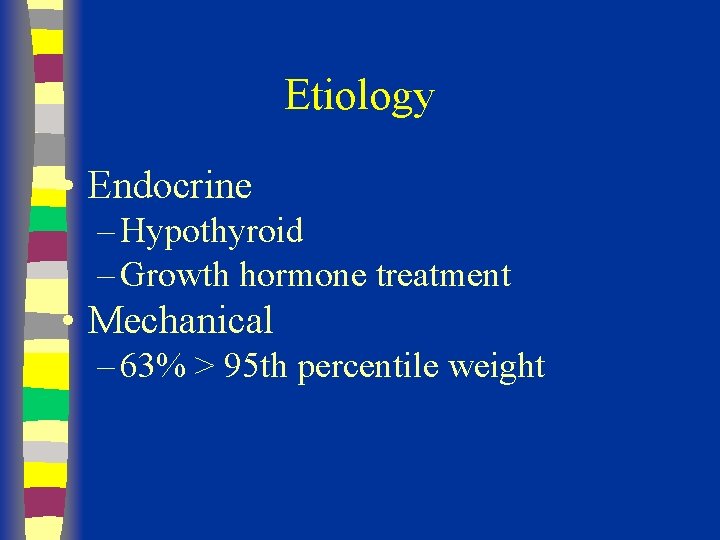
Etiology • Endocrine – Hypothyroid – Growth hormone treatment • Mechanical – 63% > 95 th percentile weight
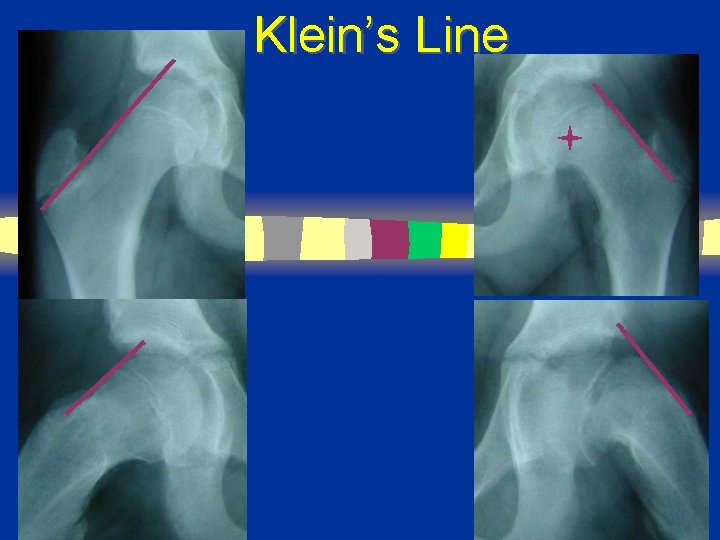
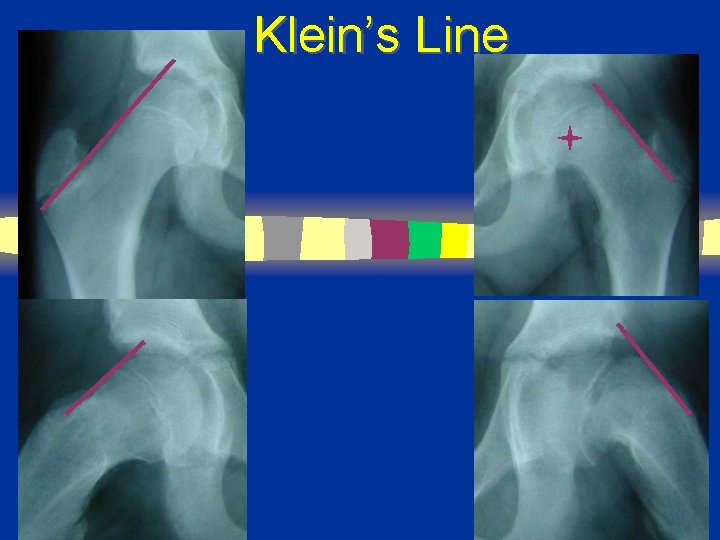
Klein’s Line


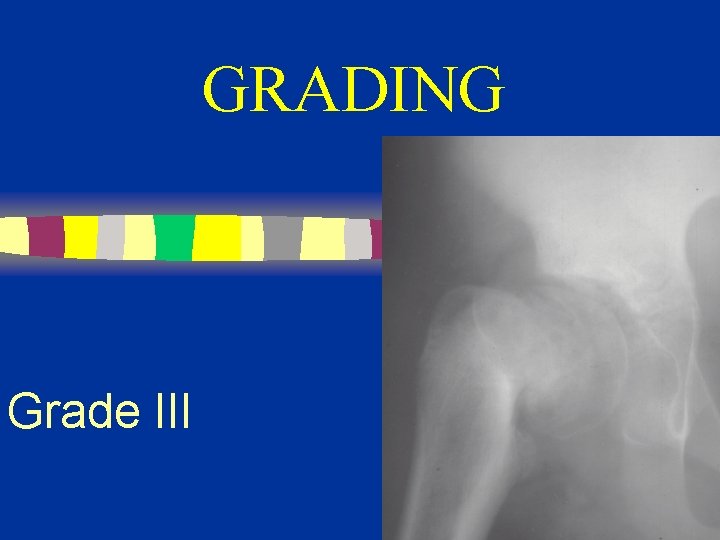
GRADING n. Grade III

GRADE I < 1/3 Slip
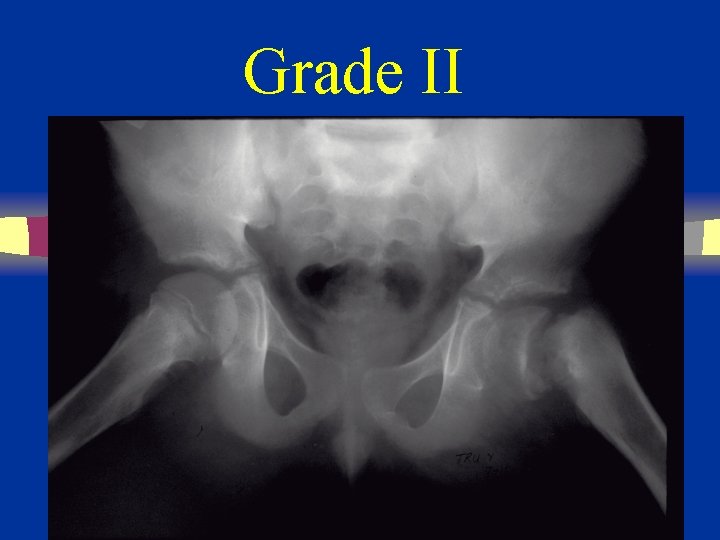
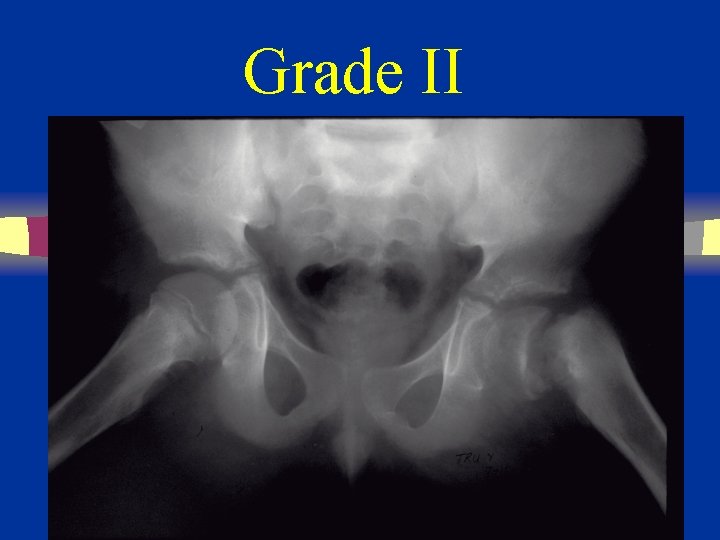
Grade II
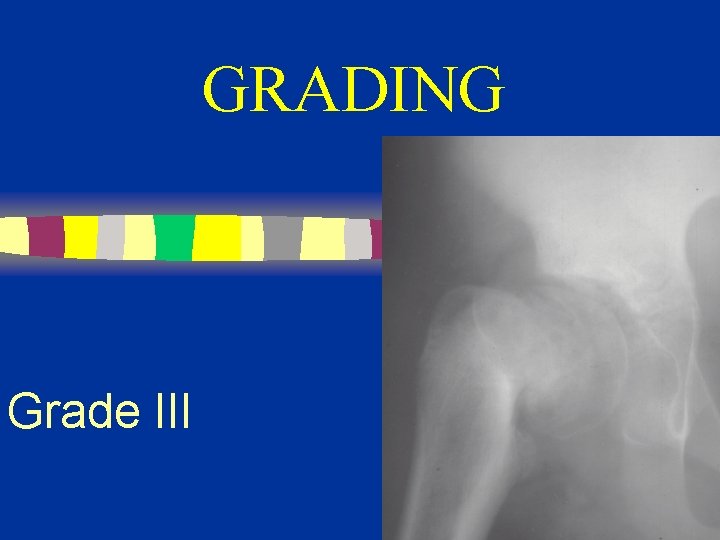
GRADING Grade III
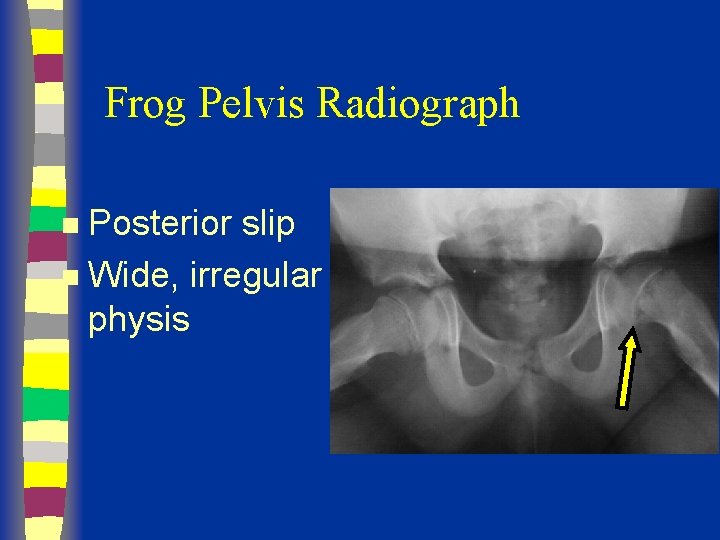
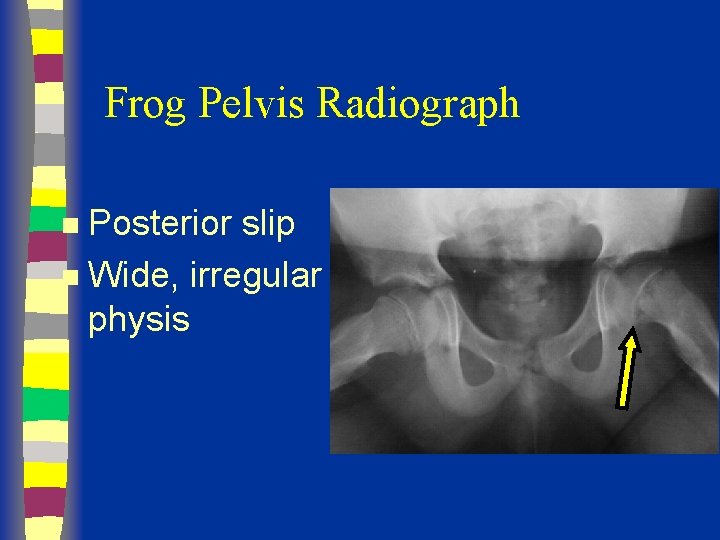
Frog Pelvis Radiograph Posterior slip n Wide, irregular physis n

Pre-Op

Early Post-Op
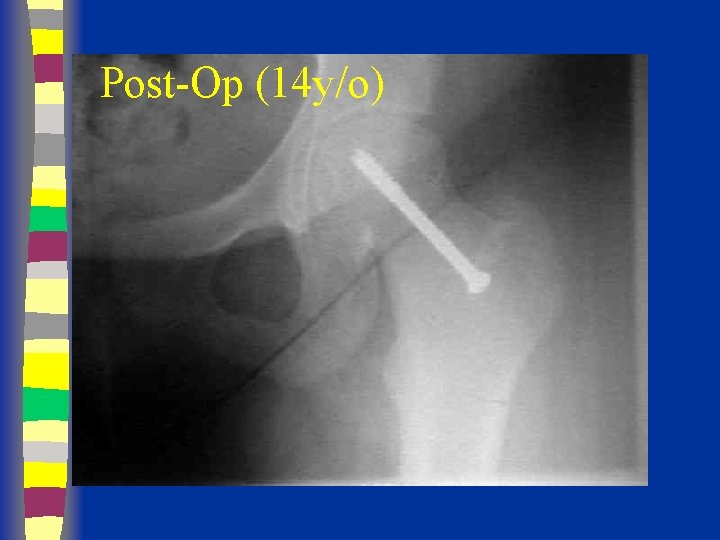
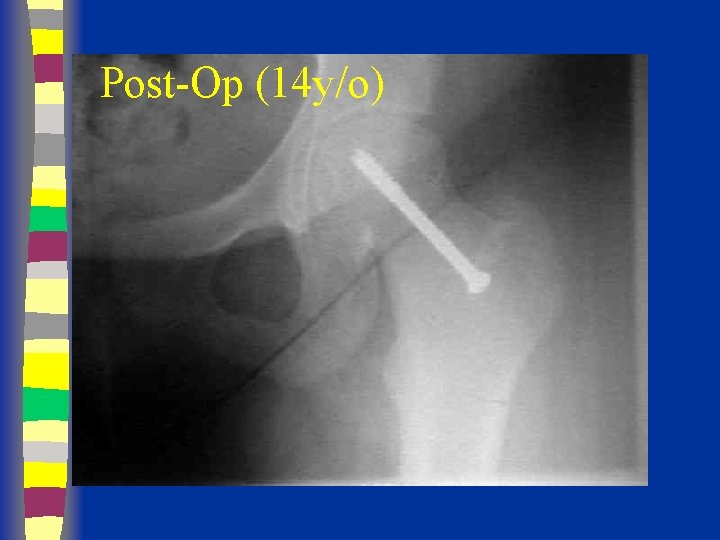
Post-Op (14 y/o)
COMPLICATIONS n n AVN Chondrolysis Hardware Penetration Long-term results are dependent upon avoiding these complications

Thank you for attention
 Emory pediatric orthopedics
Emory pediatric orthopedics Shyamnath gollakota
Shyamnath gollakota Iug anticodon
Iug anticodon Moodle iug
Moodle iug Poem about hip hop
Poem about hip hop Hip hop hip the hippity
Hip hop hip the hippity Biografia e naim frasherit
Biografia e naim frasherit Ahmet naim oktay
Ahmet naim oktay Kiralik konak olay örgüsü
Kiralik konak olay örgüsü Orthopedic history
Orthopedic history Lokmanya tilak hospital chinchwad
Lokmanya tilak hospital chinchwad Bakody test
Bakody test Uva powerpoint
Uva powerpoint Orthopedic case presentation
Orthopedic case presentation Dr wilcox orthopedic
Dr wilcox orthopedic Dr. craig shank orthopedic surgery
Dr. craig shank orthopedic surgery Concussion
Concussion Orthopedic case presentation
Orthopedic case presentation Abbott saunders test
Abbott saunders test Icats nhs
Icats nhs Search engine optimization for orthopedic practices
Search engine optimization for orthopedic practices Idea orthopedic impairment
Idea orthopedic impairment Nachlas test
Nachlas test Causes of orthopedic impairment
Causes of orthopedic impairment Banobagi doctors
Banobagi doctors Antonio orlando
Antonio orlando I693 reminder letter
I693 reminder letter Cardiothoracic surgeon salary
Cardiothoracic surgeon salary Phong tran orthopaedic surgeon
Phong tran orthopaedic surgeon Kieran barry orthopaedic surgeon cork
Kieran barry orthopaedic surgeon cork Civil surgeon near me
Civil surgeon near me Oral surgeon hamlin
Oral surgeon hamlin Moat house surgery
Moat house surgery Oliver hautmann
Oliver hautmann Thoracic surgeon
Thoracic surgeon Macra plastic surgeon
Macra plastic surgeon Dr vijayant gupta
Dr vijayant gupta Peter worlock
Peter worlock Thorasic surgeon
Thorasic surgeon Rajesh shah thoracic surgeon
Rajesh shah thoracic surgeon Cluster surgeon
Cluster surgeon Hamilton the surgeon
Hamilton the surgeon Kristin brodie
Kristin brodie Ann lyons colorectal surgeon
Ann lyons colorectal surgeon Uscis civil surgeon locator
Uscis civil surgeon locator Thorasic surgeon
Thorasic surgeon William allum surgeon
William allum surgeon Surgery root word
Surgery root word Omar mansour surgeon
Omar mansour surgeon Dip mukherjee surgeon
Dip mukherjee surgeon Hip hop questions to ask
Hip hop questions to ask Vznik hip hopu
Vznik hip hopu Hip international limited
Hip international limited Posterior hip precautions
Posterior hip precautions Transtibial gait deviations
Transtibial gait deviations Hip and leg muscles
Hip and leg muscles Hip hop presentation
Hip hop presentation Hip bone
Hip bone Ischiofemoral ligament
Ischiofemoral ligament Chapter 17 the thigh hip groin and pelvis
Chapter 17 the thigh hip groin and pelvis Hip dysplasia ppt
Hip dysplasia ppt Muscles that cross hip and knee
Muscles that cross hip and knee Sloping flat roof truss details
Sloping flat roof truss details Army hip pocket scholarship
Army hip pocket scholarship Hip and shoulder support water rescue
Hip and shoulder support water rescue Hip internal rotation
Hip internal rotation Flexor strain elbow
Flexor strain elbow Cappagh hospital day ward
Cappagh hospital day ward Hip hop php
Hip hop php Protocolo sctp
Protocolo sctp Hip hop turkeys
Hip hop turkeys Inferior gluteal artery
Inferior gluteal artery Gummy bear regional and directional terms review
Gummy bear regional and directional terms review Hip pointer injury pictures
Hip pointer injury pictures Pelvic internal rotation
Pelvic internal rotation Right hip bone
Right hip bone History of hip hop timeline
History of hip hop timeline Babcock triangle acetabulum
Babcock triangle acetabulum Parts of a pants
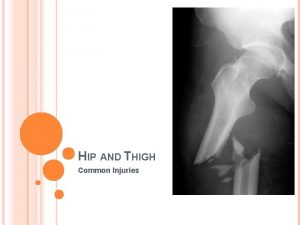
Parts of a pants Hip fracture x rays
Hip fracture x rays Bilateral hip disarticulation
Bilateral hip disarticulation Hip hughes buddhism
Hip hughes buddhism Quais são os elementos construtivos da dança
Quais são os elementos construtivos da dança Hip hi
Hip hi Hip-ennial
Hip-ennial Hip club
Hip club Anatomy of shoulder joint ppt
Anatomy of shoulder joint ppt Hip internal rotation goniometry
Hip internal rotation goniometry Acsm body fat chart
Acsm body fat chart Waist and hip
Waist and hip Gable roof plan
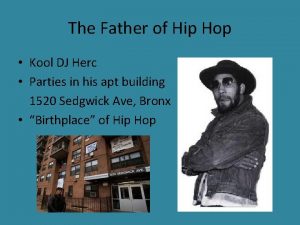
Gable roof plan Father of hip hop
Father of hip hop Hip osteokinematics
Hip osteokinematics Shakespeare is hip-hop flocabulary answer key
Shakespeare is hip-hop flocabulary answer key Hip retroversion vs anteversion
Hip retroversion vs anteversion Indications of suspension therapy
Indications of suspension therapy Hands up on your hips
Hands up on your hips Closed packed position of hip
Closed packed position of hip Hip hop merkmale
Hip hop merkmale Medical term for standing
Medical term for standing Thigh contusion
Thigh contusion Distinguished toastmaster
Distinguished toastmaster Spreschen
Spreschen Acetabulum hip
Acetabulum hip Diarrhea reflexology
Diarrhea reflexology Ishial bursitis
Ishial bursitis Hip hop music magazines
Hip hop music magazines Hip hop prezentace
Hip hop prezentace Von rosen splint
Von rosen splint Hip spica cast
Hip spica cast Hip bath benefits
Hip bath benefits