Patient Assessment Allison Hamlin RN MCHS Learning Targets











- Slides: 53
Patient Assessment Allison Hamlin, RN MCHS
Learning Targets – I can Identify normal and abnormal V/S measurements. – I can measure and record vital signs according to industry standards. – I can explain terms related to patient assessment (Hypothermia, hyperthermia, tachycardia, bradycardia, dyspnea, Cheyne stokes, Apnea, rales, hypertension, hypotension, biopsy, culture and sensitivity, void, emesis, feces, stool, sputum) – I can measure and record height and weight according to industry standards. – I can explain why urine, stool, and sputum specimens are collected. – I can determine the difference in subjective vs objective
Vital Signs • • Are important indicators of health Detect changes in normal body function May signal life-threatening conditions Provide information about responses to treatment

Vital Signs • • Temperature Pulse Respirations Blood Pressure
Vital Signs Are Measured: – Upon admission – As often as required by the person’s condition – Before & after surgery and other procedures – After a fall or accident – When prescribed drugs that affect the respiratory or circulatory system – When there are complaints of pain, dizziness, shortness of breath, chest pain – As stated on the care plan
When Measuring Vital Signs • Usually taken with the person sitting or lying • The person is at rest • Always report: – A change from a previous measurement – Vital signs above or below the normal range – If you are unable to measure the vital signs
Temperature • Measurement of balance between heat lost and produced by the body. – Heat is produced by: • Metabolism of food • Muscle and gland activity – Heat may be lost through: • Perspiration, Respiration, Excretion • Measured with the Fahrenheit (F) or Celsius or Centigrade (C) scales
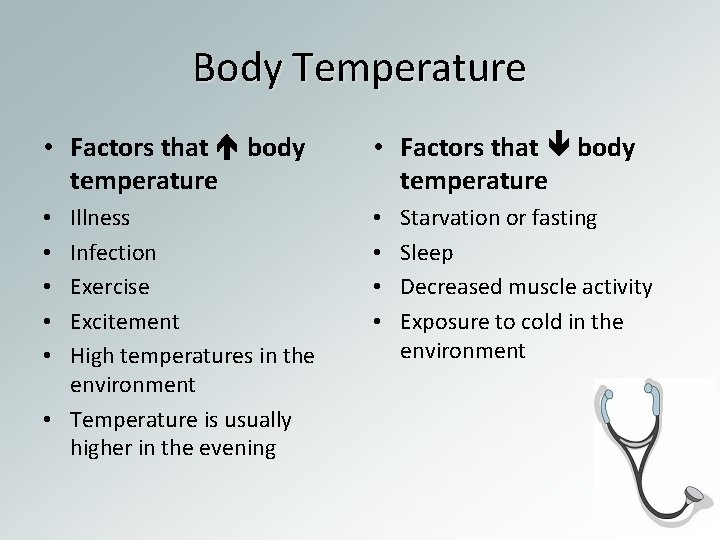
Body Temperature • Factors that body temperature Illness Infection Exercise Excitement High temperatures in the environment • Temperature is usually higher in the evening • • • Starvation or fasting Sleep Decreased muscle activity Exposure to cold in the environment
Temperature Sites • Oral - by mouth – most common method – May be affected by hot or cold food, smoking, oxygen, chewing gum – Wait 15 minutes or use alternate site • Rectal - in the rectum -most accurate site – Do not use if patient has rectal surgery or bleeding • Axillary - under arm – less reliable site – Used when other sites are inaccessible – Do not use immediately after bathing
Temperature Sites • Tympanic or aural - in the ear – Measures in 1 to 3 seconds • Temporal Artery – temporal artery on the forehead • Record route temperature was taken • • O - Oral R- Rectal T – Tympanic A – Axillary

Normal Body Temperature Oral 98. 6 ( 97. 6 - 99. 6) Rectal 99. 6 (98. 6 - 100. 6) Axillary 97. 6 (96. 6 - 98. 6) Typmanic 98. 6 (98. 6 - 100. 6) Temporal 99. 6 (98. 6 - 100. 6) Glass Thermometer shake down to 94** Hypothermia – temperature below normal Hyperthermia – temperature above normal
Types of Thermometers • Clinical (glass) thermometer no longer contain mercury. – Come in oral and rectal. – Disposable covers are usually used. • Electronic can be used for oral, rectal, or axillary and use disposable probe covers. • Tympanic placed in auditory canal and uses disposable cover. • Strips that contain special chemicals or dots that change colors can also be used.
Pulse • The pressure of blood pushing against the wall of an artery as the heart beats and rests. • Measured for one minute while noting: – rate - beats per minute – rhythm - regular or irregular – volume - strength or intensity - described as strong, weak, thready, bounding
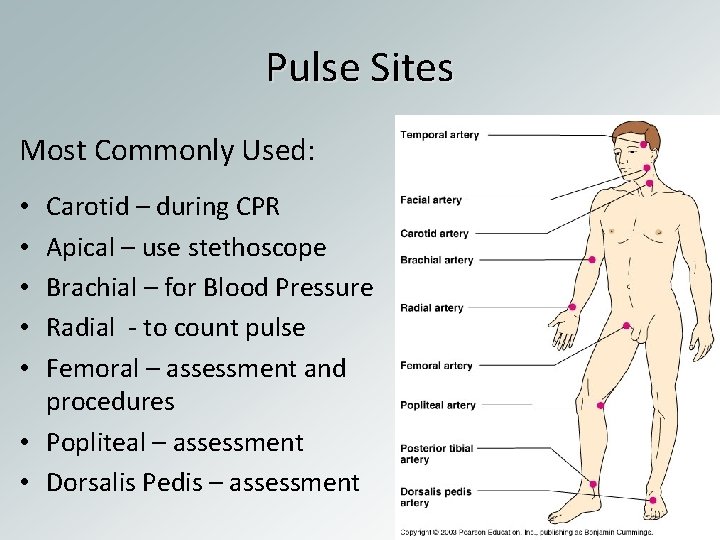
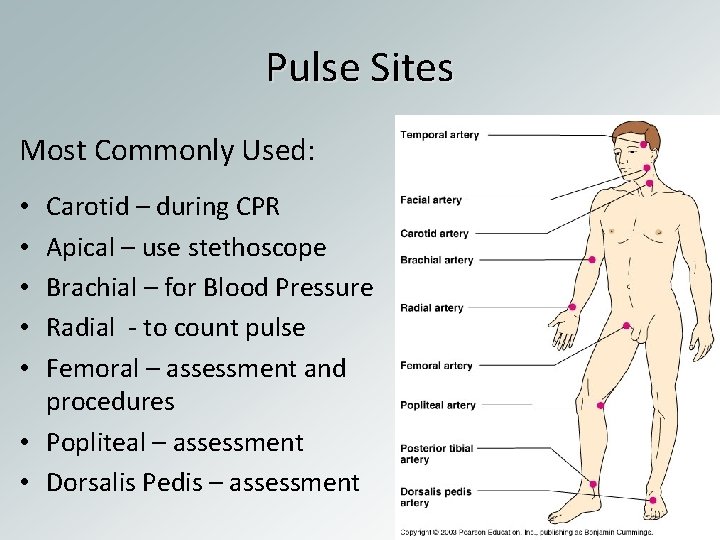
Pulse Sites Most Commonly Used: Carotid – during CPR Apical – use stethoscope Brachial – for Blood Pressure Radial - to count pulse Femoral – assessment and procedures • Popliteal – assessment • Dorsalis Pedis – assessment • • •
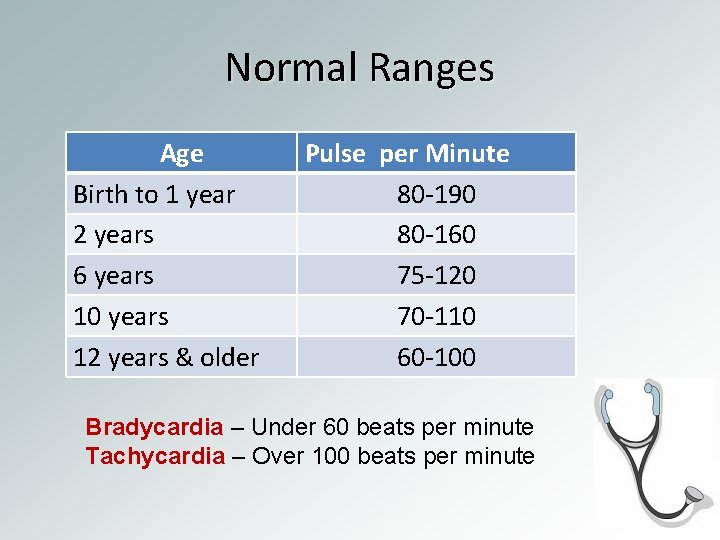
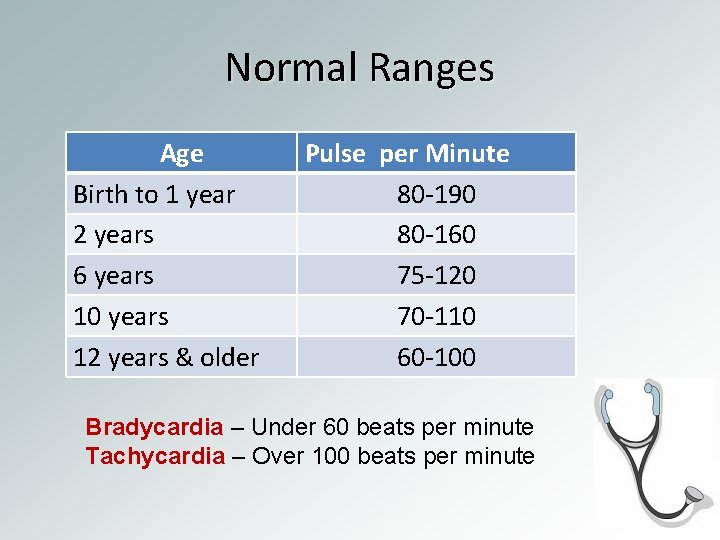
Normal Ranges Age Birth to 1 year 2 years 6 years 10 years 12 years & older Pulse per Minute 80 -190 80 -160 75 -120 70 -110 60 -100 Bradycardia – Under 60 beats per minute Tachycardia – Over 100 beats per minute

Factors that Affect Pulse • Factors that pulse • • • Exercise Stimulant drugs Excitement Fever Shock Nervous tension • Factors that pulse • • Sleep Depressant drugs Heart disease Coma
Respirations • Process of breathing air into (inhalation) and out of (exhalation) the lungs. • Oxygen enters the lungs during inhalation. • Carbon dioxide leaves the lungs during exhalation. • The chest rises during inhalation and falls during exhalation. • Normal rate 12 -20 breaths per minute
Assessing Respiration • Respirations is measured when the person is at rest. • Rate may change is patient is aware that it is being counted. • To prevent this, count respirations right after taking a pulse. • Keep your fingers or stethoscope over the pulse site. • To count respirations, watch the chest rise and fall.
Assessing Respiration • Character and quality of respirations is also assessed: – – – Deep Shallow Labored or difficult Noises – wheezing, stertorous (a heavy, snoring type of sound) Moist or rattling sounds • Dyspnea – difficult or labored breathing • Apnea – absence of respirations • Cheyne-Stokes – periods of dyspnea followed by periods of apnea; often noted in the dying patient • Rales – bubbling or noisy sounds caused by fluids or mucus in the air passages
Blood Pressure • Measure of the pressure blood exerts on the walls of arteries • Blood pressure is controlled by: – The force of heart contractions • weakened heart drop in BP – The amount of blood pumped with each heartbeat • loss of blood drop in BP – How easily the blood flows through the blood vessels • Narrowing of vessels increase in BP • Dilatation of vessels decrease in BP
Factors that Affect Blood Pressure Factors that blood pressure • Excitement, anxiety, nervous tension • Stimulant drugs • Exercise and eating Factors that blood pressure • Rest or sleep • Depressant drugs • Shock • Excessive loss of blood

Measuring BP • A sphygmomanometer is used to measure BP – Aneroid – has a round dial and needle – Mercury – has a column of mercury – Electronic – automated device • BP is measured in millimeters (mm) of mercury (Hg). • The systolic pressure is recorded over the diastolic pressure.
Normal Range of Blood Pressure • Systolic: Pressure on the walls of arteries when the heart is contracting. Normal range – less than 120 mm Hg • Diastolic: Constant pressure when heart is at rest Normal range – less than 80 mm Hg • Hypertension—BP that remains above a systolic of 140 mm Hg or a diastolic of 90 mm Hg • Hypotension—Systolic below 90 mm Hg and/or a diastolic below 60 mm Hg

Measuring Height and Weight • Used to determine if patient is underweight or overweight • Height and weight charts are used as averages • Weight greater or less than 20% considered normal • BMI or Body Mass Index a statistical measure of body weight based on a person's weight and height. • BMI from 18. 5 to 24. 9 is considered normal
Measuring Height and Weight General Guidelines: • • Use the same scale every day Make sure the scale is balanced before use Weigh the patient at the same time each day Remove jacket, robe, and shoes before weighing OBSERVE SAFETY PRECAUTIONS! Prevent injury from falls and the protruding height lever. Some people are weight conscious. Make only positive comments when weighing patients
Types of Scales • Clinical scales contain a balance beam and measuring rod • Bed scales or Chair scales are used for patients unable to stand • Infant scales come in balanced, aneroid, or digital – When weighing an infant…keep one hand slightly over but not touching the infant – A tape measure is used to measure infant height.

Common Types of Specimens • Random urine specimen – Collected for a routine urinalysis. – No special measures are needed. • Midstream specimen (clean-voided or clean-catch) – The perineal area is cleaned before collecting the specimen. – Sterile gloves and container are needed. • Double voided – Patient voids and the specimen is discarded – After 30 minutes, patient voids again and specimen is collected for testing

Urine Specimens • Can provide valuable information about the patients state of health • Urine is commonly tested for: – Bacteria, pus, or blood as found in bladder and kidney infection – Sugar and acetone as found in diabetes – Hormones as found in pregnancy – Drugs
Testing Urine • Using reagent strips – Universal Precautions must be used at all times – Dip the strip into urine. – Compare the strip with the color chart on the bottle at the required time interval. – Record and report results
Stool Specimen • Stool, or feces, may be tested for: – Blood – Fat – Microbes – Worms – Other abnormal contents • The stool specimen must not be contaminated with urine.

Sputum Specimen • Sputum specimens may be tested for blood, microbes, and abnormal cells. • The person coughs up sputum from the bronchi and trachea. – It is easier to collect a specimen in the morning.
Other Types of Specimens • Specimens may be obtained from other body tissue and fluid. • A biopsy is done by removing a small piece of tissue for further examination. • A culture and sensitivity is done by swabbing a body surface and testing for the presence of microbes

Seven Warning Signs of Cancer
Warning Sign What to Look For • Blood in urine or stool Unusual bleeding • Discharge from any parts or discharge of your body, for example nipples, penis, etc
Warning Sign A sore that does not heal What to Look For • Sores that: • don't seem to be getting better over time • are getting bigger • getting more painful • are starting to bleed
Warning Sign What to Look For • Changes in the color, consistency, size, or Change in bowel shape of stools. or bladder (diarrhea, constipated) habits • Blood present in urine or stool
Warning Sign What to Look For • Any lump found in the Lump in breast or breast when doing a self other part of examination. the body • Any lump in the scrotum when doing a self exam. • Other lumps found on the body.
Warning Sign What to Look For Nagging cough • Change in voice/hoarseness • Cough that does not go away • Sputum with blood
Warning Sign What to Look For • Use the ABCD RULE • Obvious change in moles Asymmetry: Does the mole look the same in all parts or are there differences? • Border: Are the borders sharp or ragged? • Color: What are the colors seen in the mole? • Diameter: Is the mole bigger than a pencil eraser (6 mm)?
Warning Sign What to Look For Difficulty in swallowing • Feeling of pressure in throat or chest which makes swallowing uncomfortable • Feeling full without food or with a small amount of food
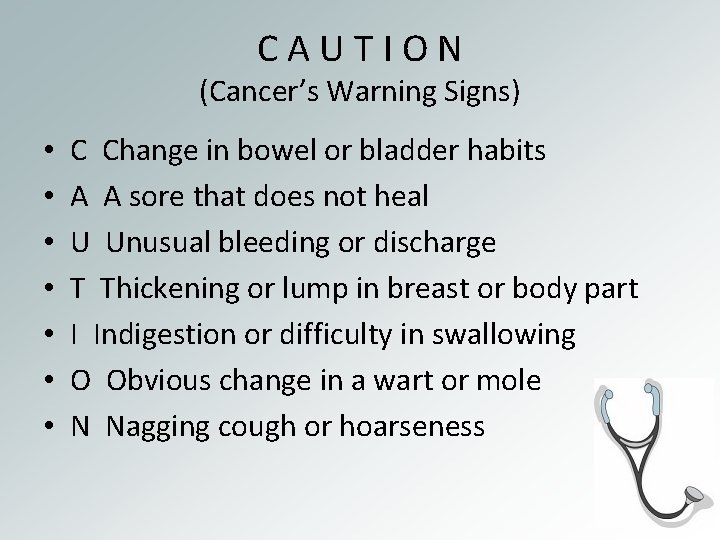
C A U T I O N (Cancer’s Warning Signs) • • C Change in bowel or bladder habits A A sore that does not heal U Unusual bleeding or discharge T Thickening or lump in breast or body part I Indigestion or difficulty in swallowing O Obvious change in a wart or mole N Nagging cough or hoarseness
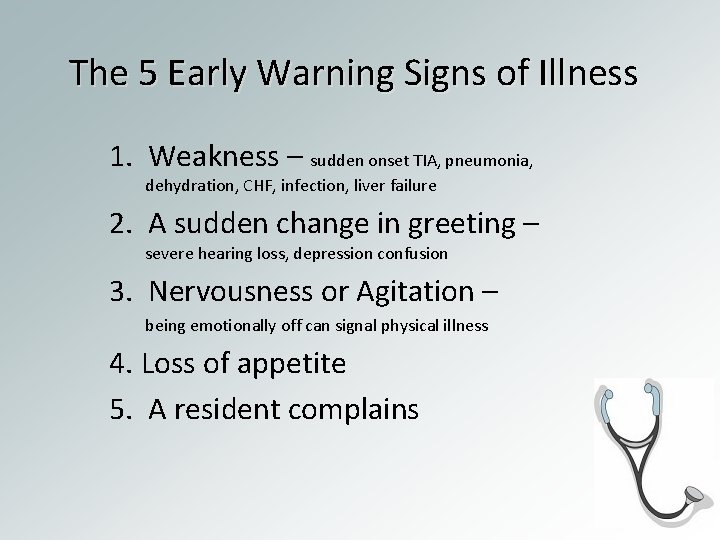
The 5 Early Warning Signs of Illness 1. Weakness – sudden onset TIA, pneumonia, dehydration, CHF, infection, liver failure 2. A sudden change in greeting – severe hearing loss, depression confusion 3. Nervousness or Agitation – being emotionally off can signal physical illness 4. Loss of appetite 5. A resident complains
ABC’s of Observation • Appearance • Behavior – actions, conduct, pain • Communication
Signs and Symptoms • Signs -- Objective data are seen, heard, felt, smelled. You can see urine, hear a cough, feel a pulse and smell a foul odor. • Symptoms -- Subjective data are thing a person tells you about that you cannot observe through your senses. Examples include nausea, pain and dizziness.
Observations by Body Systems Using sight, touch, hearing, and smell

Integumentary System • Color – flushed, pale, ashen, icteric, cyanotic, (don’t forget nails) • Temperature – warm, hot cool • Moisture – dry, moist, perspiring • Abnormalities – rashes, bruises, wounds
Musculoskeletal System • Posture – stooped, fetal position, straight • Mobility – in bed, balance, ambulation • Range of Motion – performance of ADL’s

Circulatory System • • Pulse – strength, regularity, rate Blood Pressure Skin color Extremities – edema
Respiratory System • Respirations – rate, regularity, depth, dyspnea, SOB (exertion, at rest), stertorous • Cough – frequency, dry, productive • Sputum – color, consistency
Nervous System • Mental state – orientation • Ability to communicate • Senses – Eyes – pupils equal, reddened, drainage – Ears – drainage, hearing – Nose – drainage, bleeding
Urinary System • Frequency, amount, color, dysuria • Clarity, blood or sediment, incontinent • Pain or burning upon urination
Digestive System • Appetite – amount of solids/liquids consumed, belching, burping, intolerance to foods • Eating – difficulty chewing or swallowing • Nausea/Vomiting • Bowel elimination – frequency, amount, consistency, color, diarrhea, constipation, flatus