Nonaccidental injury and the Orthopaedic Surgeon Peter Worlock



- Slides: 30
Non-accidental injury and the Orthopaedic Surgeon. Peter Worlock Newcastle General Hospital
Role of doctors: • Be aware of problem. • Recognise unusual injury patterns. • Initiate investigation.
Soft tissue injuries: • Bites. • Burns. • Bruising.

Bites:
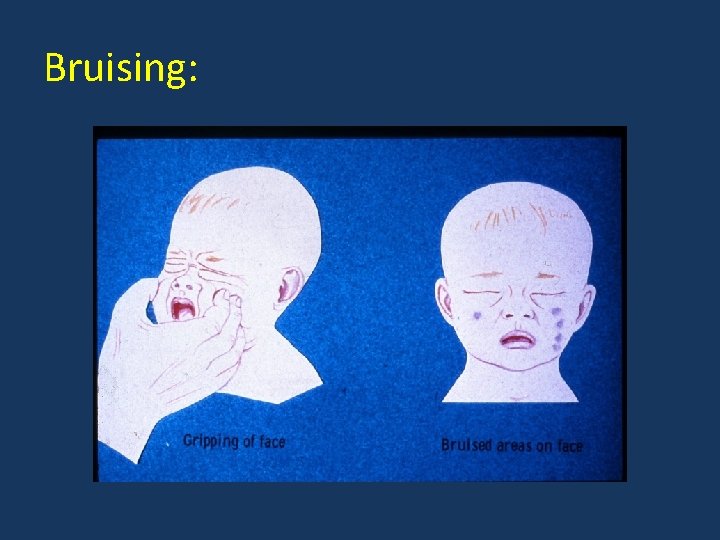
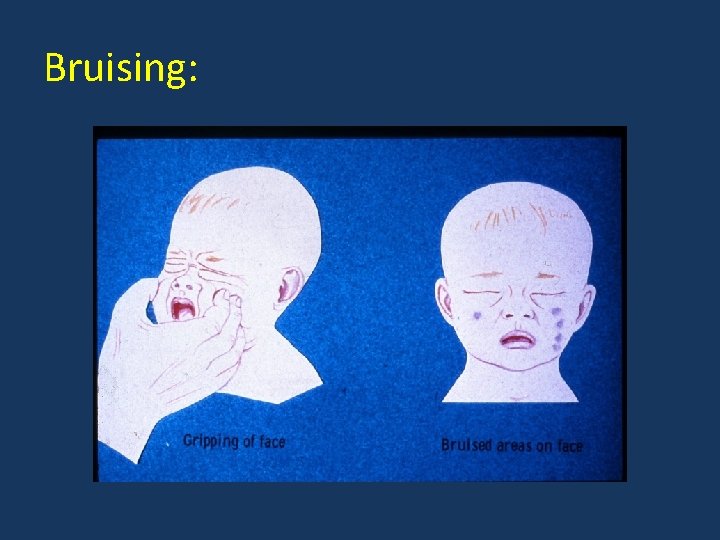
Bruising:
Soft tissue injuries – normal children: • Head/face injuries rare <18 months. • Lumbar injuries unusual before age of 5 years. • Bruising of hands/feet and lower legs is most common injury. Roberton et al, 1982
Soft tissue injuries – NAI: • Head/face injuries present in 60%. • Lumbar injuries common under age of 5 years. Roberton et al, 1982
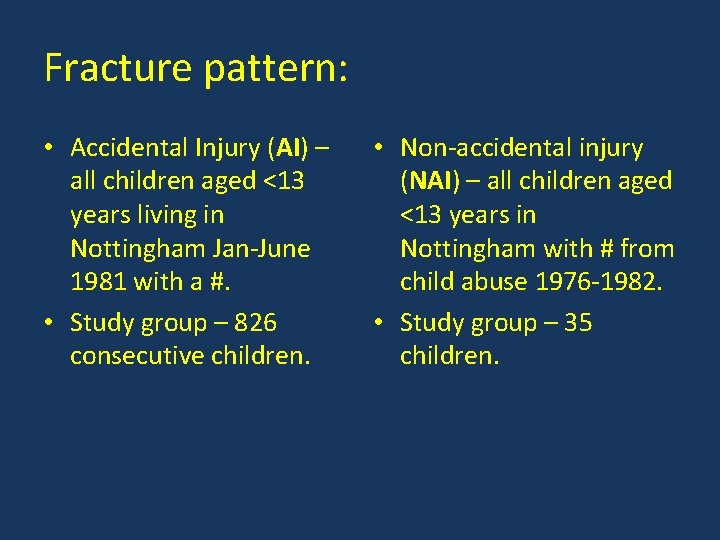
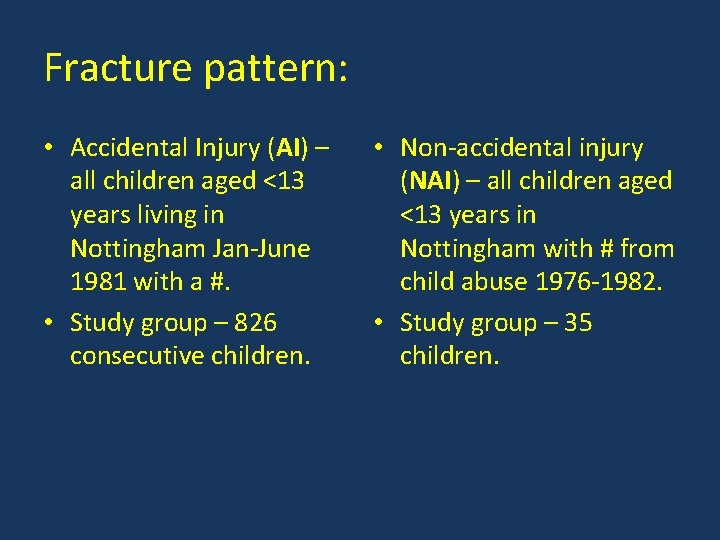
Fracture pattern: • Accidental Injury (AI) – all children aged <13 years living in Nottingham Jan-June 1981 with a #. • Study group – 826 consecutive children. • Non-accidental injury (NAI) – all children aged <13 years in Nottingham with # from child abuse 1976 -1982. • Study group – 35 children.
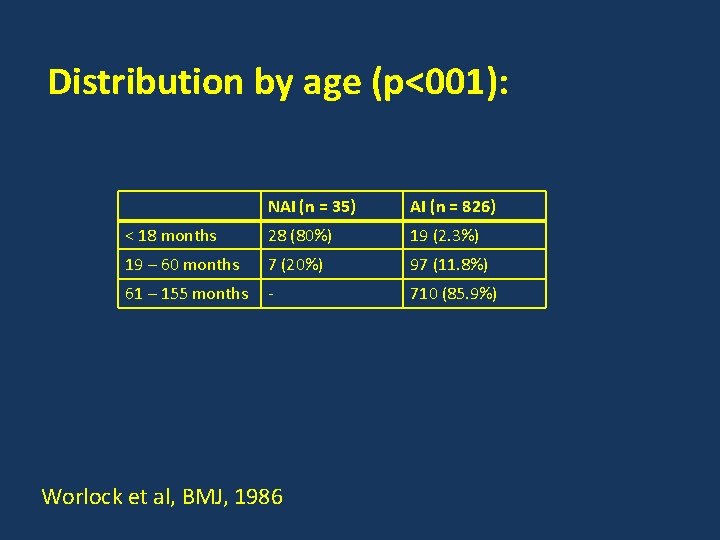
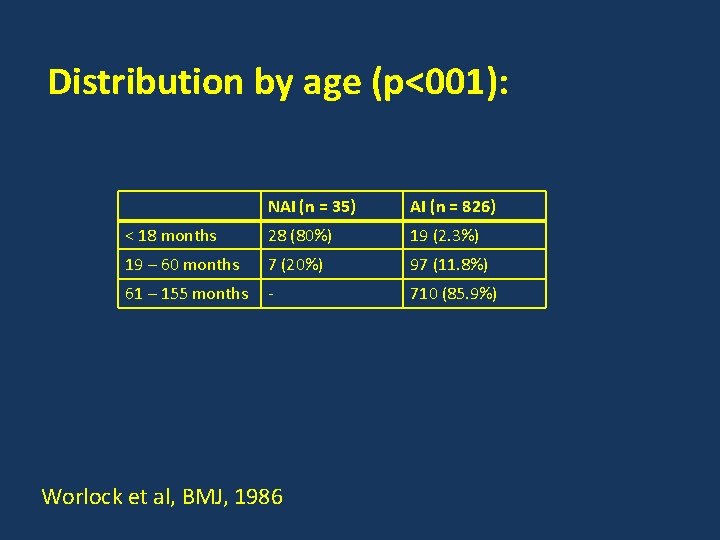
Distribution by age (p<001): NAI (n = 35) AI (n = 826) < 18 months 28 (80%) 19 (2. 3%) 19 – 60 months 7 (20%) 97 (11. 8%) 61 – 155 months - 710 (85. 9%) Worlock et al, BMJ, 1986
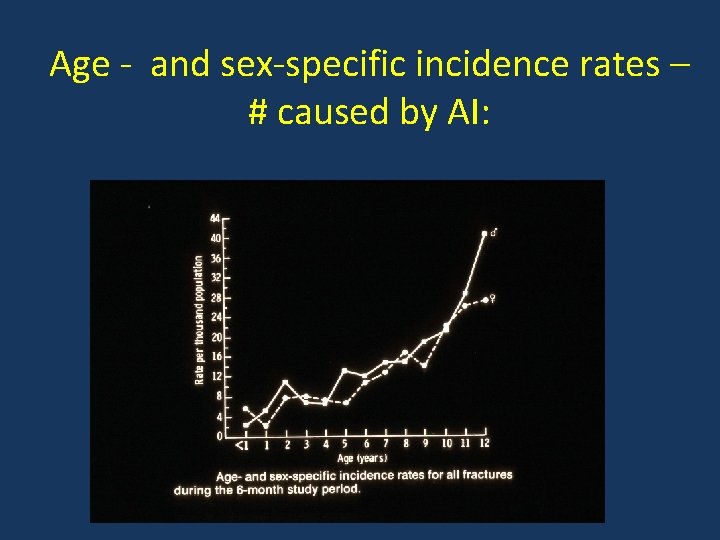
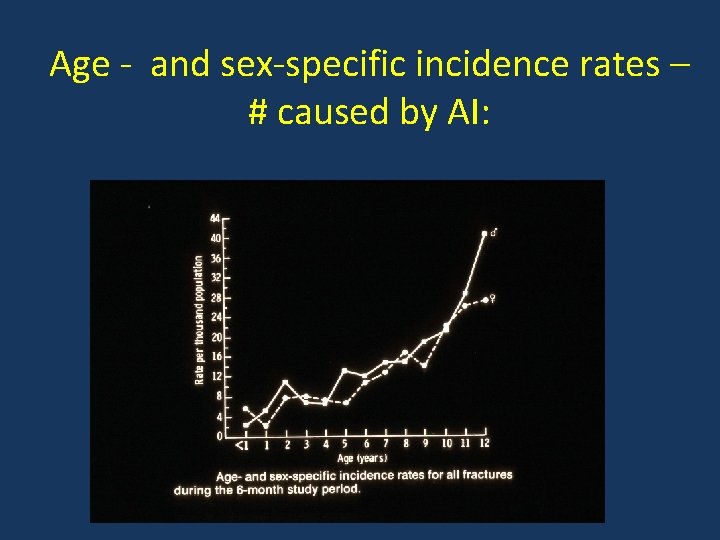
Age - and sex-specific incidence rates – # caused by AI:

AI group # incidence during six month study period (p<0. 001): Pop. at risk Incidence < 18 months 10, 989 1. 7/1000 19 – 60 months 23, 564 4. 8/1000 61 -155 months 68, 288 10. 4/1000 Worlock et al, BMJ, 1986
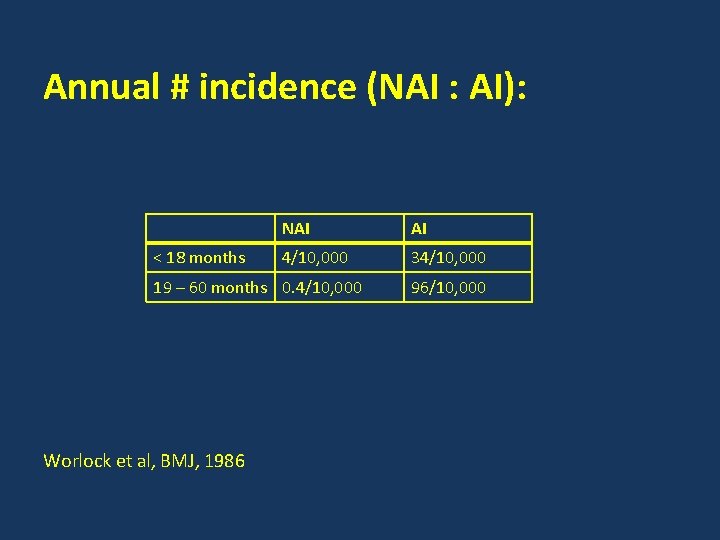
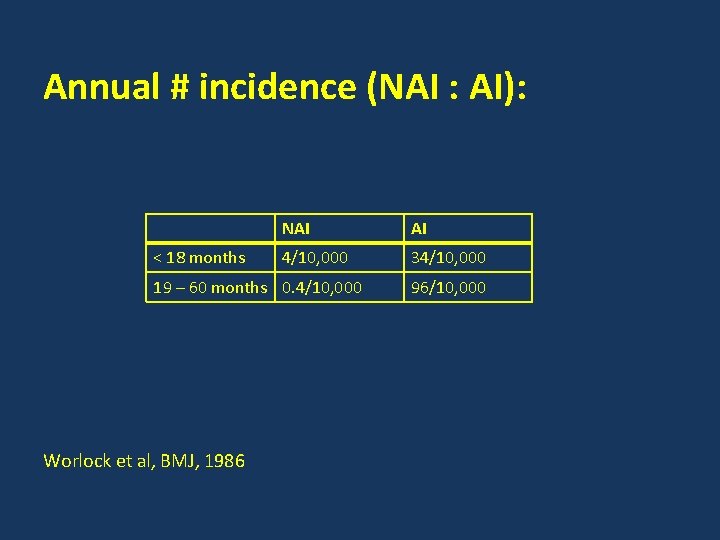
Annual # incidence (NAI : AI): < 18 months NAI AI 4/10, 000 34/10, 000 19 – 60 months 0. 4/10, 000 Worlock et al, BMJ, 1986 96/10, 000
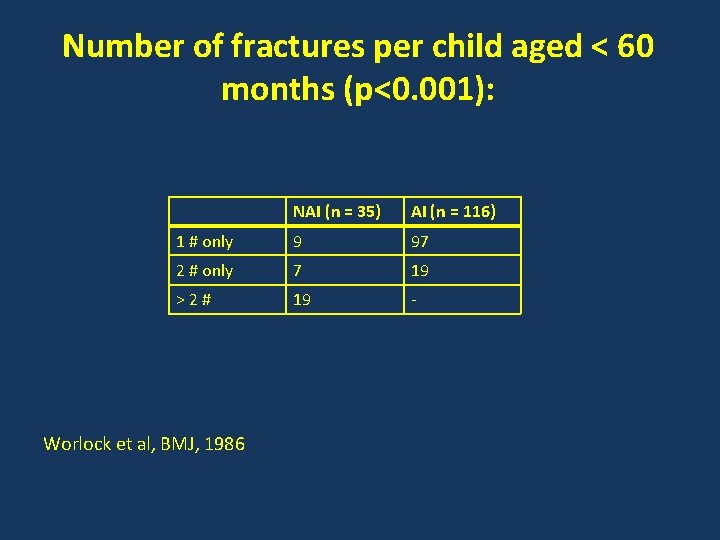
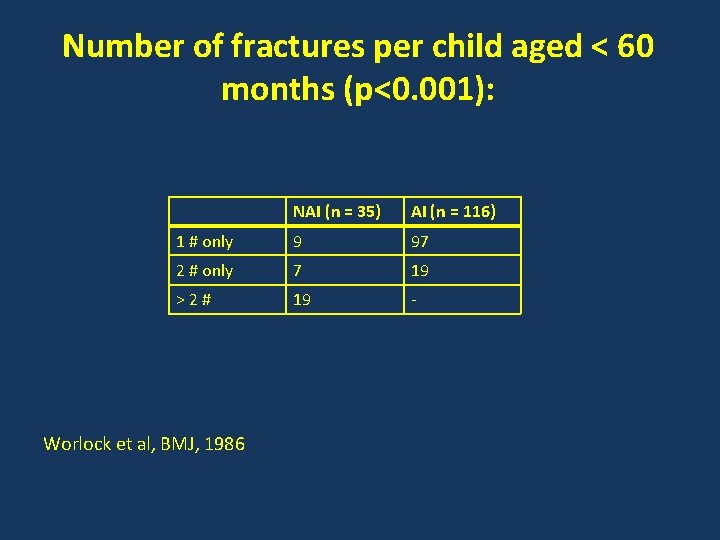
Number of fractures per child aged < 60 months (p<0. 001): NAI (n = 35) AI (n = 116) 1 # only 9 97 2 # only 7 19 >2# 19 - Worlock et al, BMJ, 1986
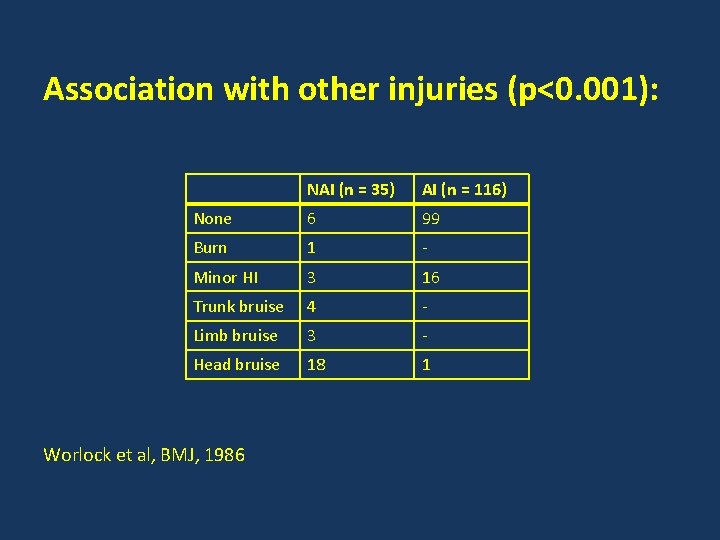
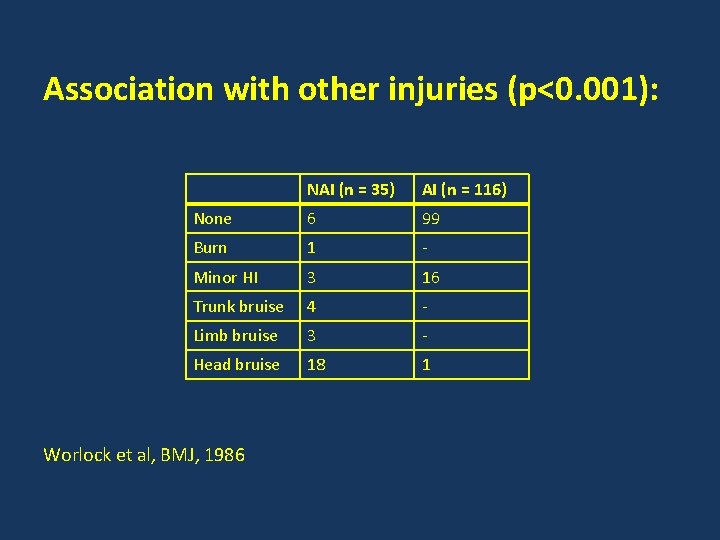
Association with other injuries (p<0. 001): NAI (n = 35) AI (n = 116) None 6 99 Burn 1 - Minor HI 3 16 Trunk bruise 4 - Limb bruise 3 - Head bruise 18 1 Worlock et al, BMJ, 1986
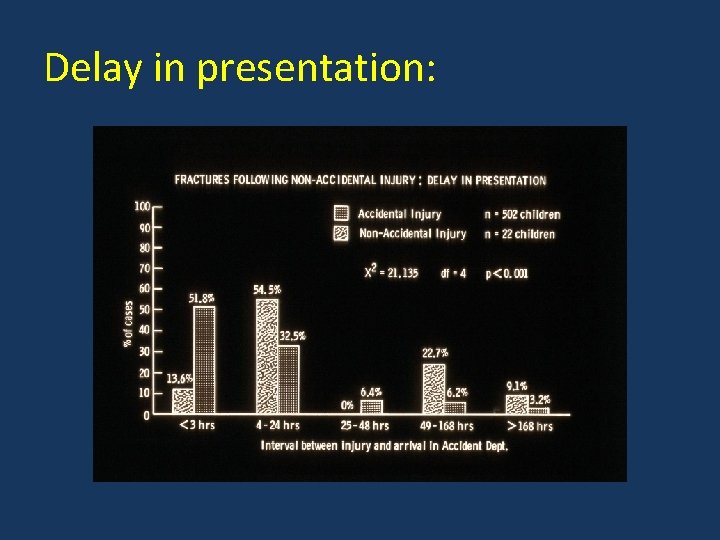
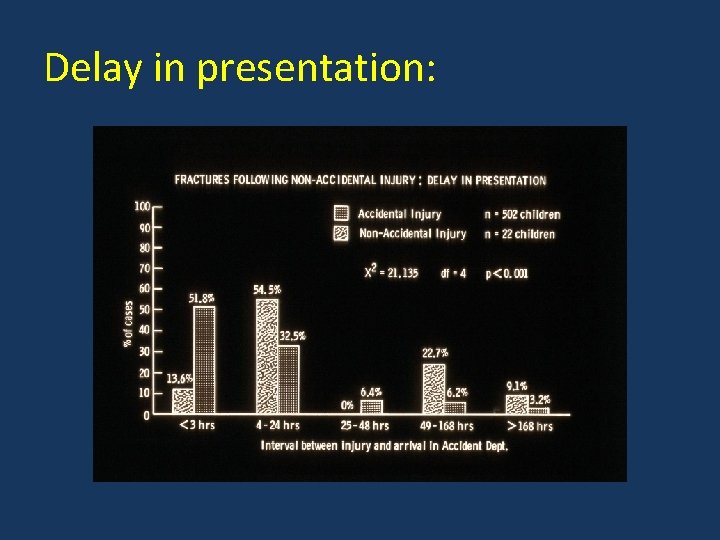
Delay in presentation:
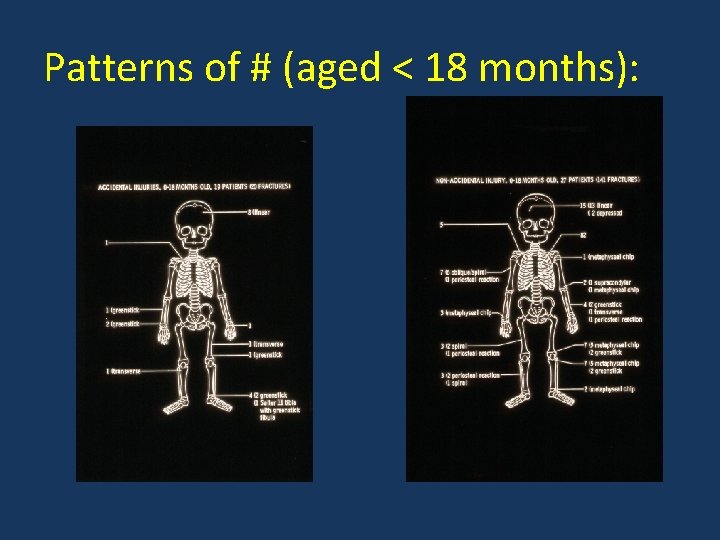
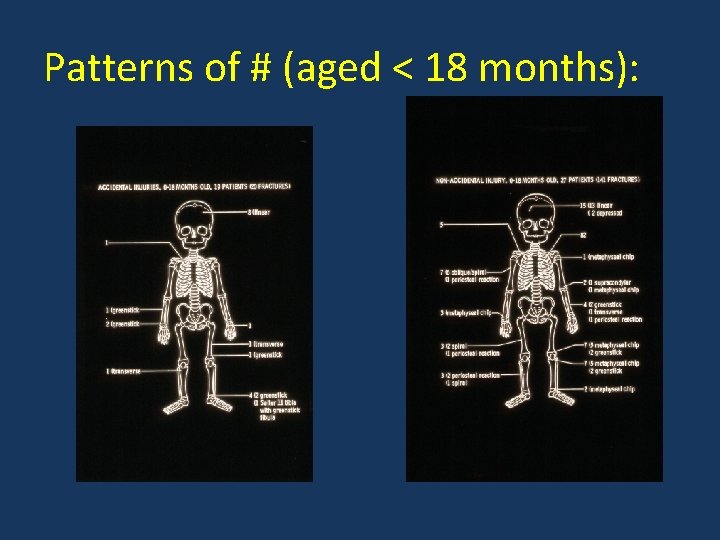
Patterns of # (aged < 18 months):
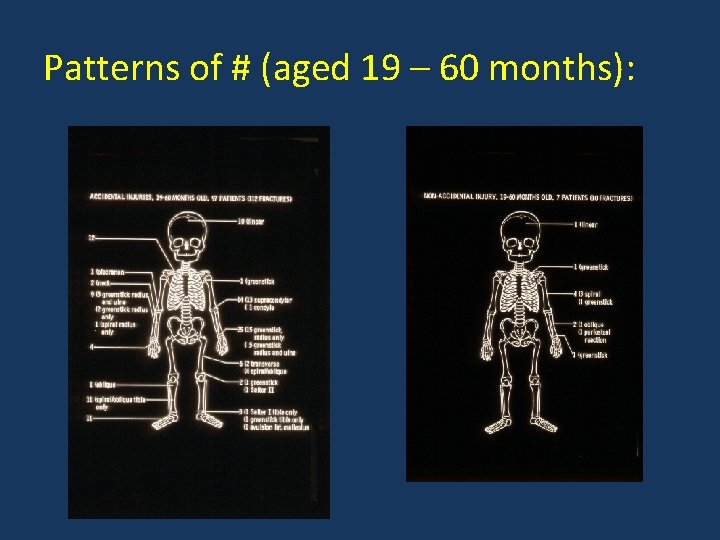
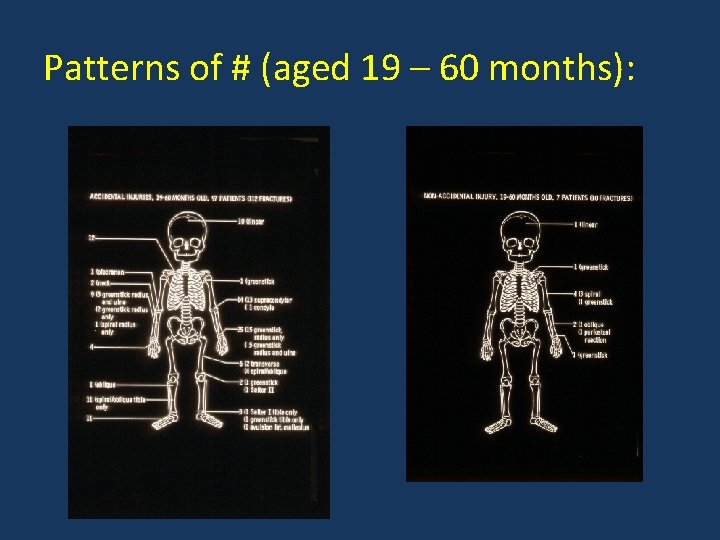
Patterns of # (aged 19 – 60 months):
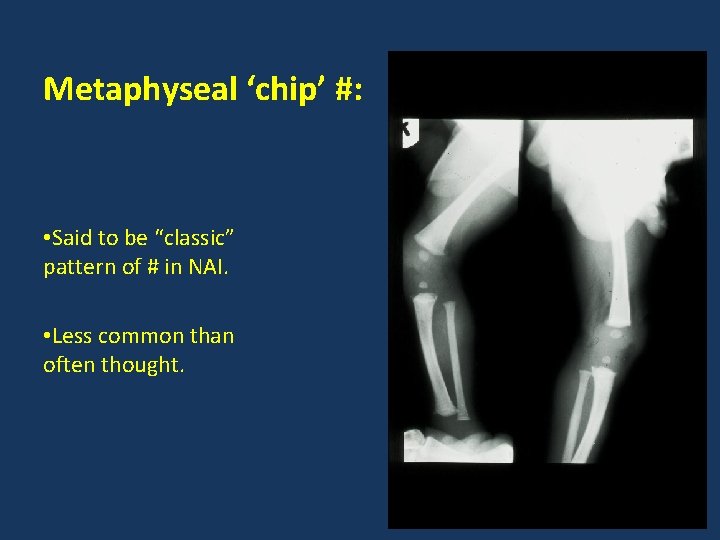
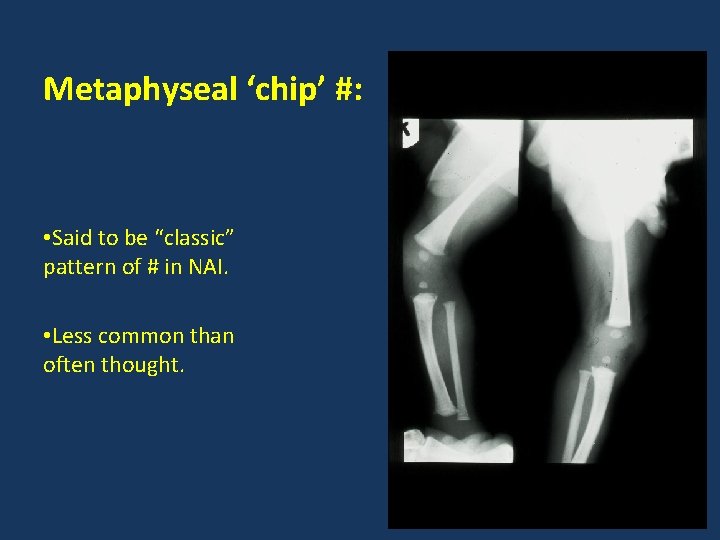
Metaphyseal ‘chip’ #: • Said to be “classic” pattern of # in NAI. • Less common than often thought.
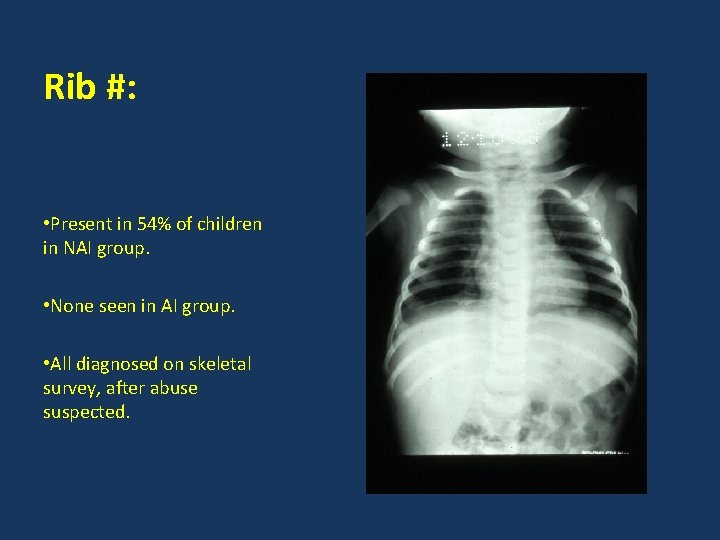
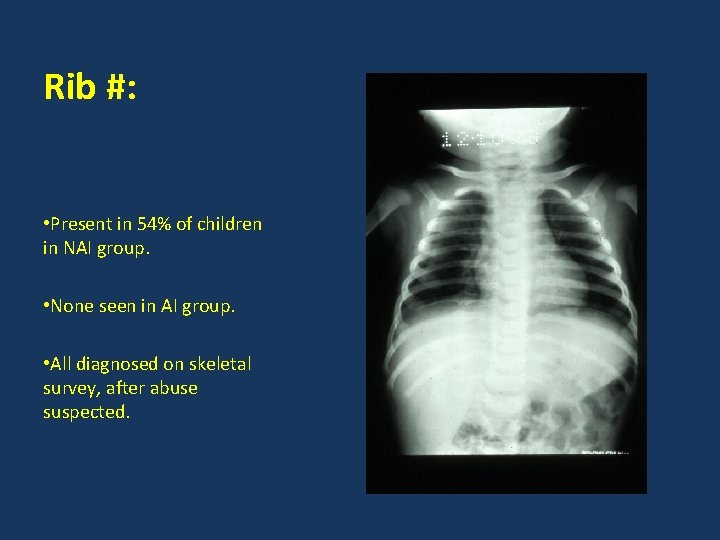
Rib #: • Present in 54% of children in NAI group. • None seen in AI group. • All diagnosed on skeletal survey, after abuse suspected.

Spiral # of humeral shaft: • Seen in 9 out of 35 children in NAI group. • None seen in AI group (p<0. 001)
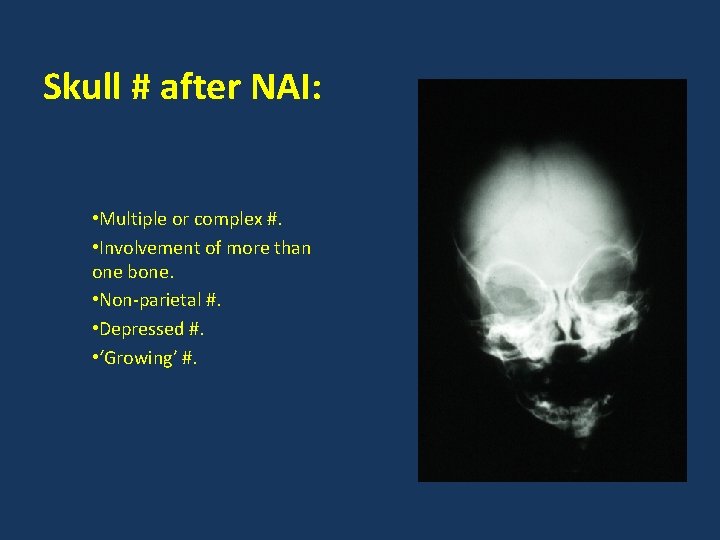
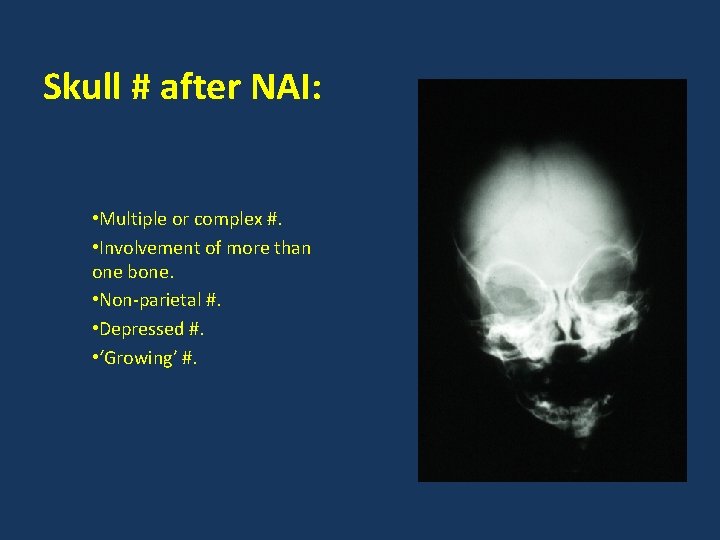
Skull # after NAI: • Multiple or complex #. • Involvement of more than one bone. • Non-parietal #. • Depressed #. • ‘Growing’ #.
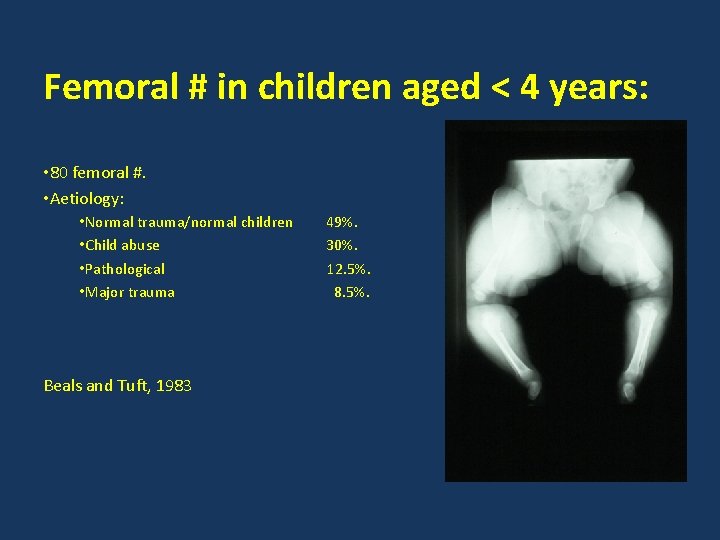
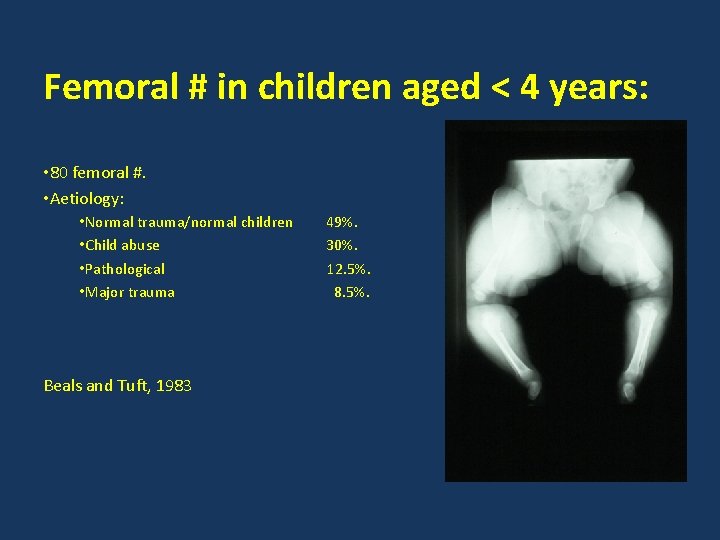
Femoral # in children aged < 4 years: • 80 femoral #. • Aetiology: • Normal trauma/normal children • Child abuse • Pathological • Major trauma Beals and Tuft, 1983 49%. 30%. 12. 5%. 8. 5%.
Risk of injury on falling out of bed: • 76 children fallen from bed, cot or chair. • Height of falls from 1 – 3 ft. • Injuries: – Minor bruise/no injury – Head/face bruise or laceration – Linear skull # – Limb # (in pt with OI) Nimityongskul & Anderson, 1987 63. 5%. 30. 0%. 1. 3%.
NAI and osteogenesis imperfecta: • Type I: autosomal dominant with blue sclera. Most common type. • Type II: autosomal recessive with blue sclera. Lethal in foetal or perinatal period. • Type III: autosomal recessive with normal sclera. Moderate/severe bone fragility with rapidly progressive deformity.
NAI and osteogenesis imperfecta: • Type IV: autosomal dominant, but occasional spontaneous mutation. Normal sclera. Mild/moderate bone fragility with variable deformity. • Rare! Incidence: 1 in 120, 000 live births.
NAI and osteogenesis imperfecta: • Occurrence in absence of blue sclera, no family history and lack of progressive deformity is about 1 in 3, 000 live births. • A city of 500, 000 people with 6000 live births per year would produce one case of Type IV OI by spontaneous mutation every 100 – 300 years. Taitz, BMJ, 1987
Other conditions causing spontaneous # in infancy : • Prematurity. Usually <1500 g at birth, with evidence of rickets and/or osteoporosis on XR. Raised Alk. Phosphatase. • Copper deficiency. Can occur in pre-term babies given Cu-deficient feed, after TPN lacking Cu or in severe malabsorption with Cu-deficient diet. Children with # all have severe haematological abnormalities and osteoporosis on XR.
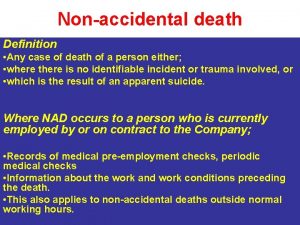
NAI and the Orthopaedic Surgeon: • # uncommon in normal children < 18 months, but # due to NAI most common in this age group. • 1 child in 8 aged < 18 months with a # may be victim of abuse. • Rib # on skeletal survey, in absence of major chest trauma, is virtually diagnostic of NAI.
NAI and the Orthopaedic Surgeon: • Metaphyseal ‘chip’ # relatively uncommon. • Diaphyseal injuries in NAI are due to gripping/twisting – spiral # or periosteal new bone formation. • You need to be able to recognise unusual injury patterns.
NAI and the Orthopaedic Surgeon: • Be prepared to initiate investigation. • Know your own hospital’s procedure for investigating suspected NAI. • Do not accuse parents – leave interviewing family to the experts. • Children’s Act 1992 – safety and well-being of the child is paramount.
 Peter worlock orthopaedic surgeon
Peter worlock orthopaedic surgeon Stephen brennan bon secours
Stephen brennan bon secours Phong tran orthopaedic surgeon
Phong tran orthopaedic surgeon Battering intentional or unintentional
Battering intentional or unintentional David worlock
David worlock Orthopaedic surgery south east london
Orthopaedic surgery south east london Sally tennant orthopaedic
Sally tennant orthopaedic Rch fracture guidelines
Rch fracture guidelines Cappagh hospital pre assessment
Cappagh hospital pre assessment Oncology gpo landscape
Oncology gpo landscape Charcot joint
Charcot joint Professor abudu royal orthopaedic hospital
Professor abudu royal orthopaedic hospital Dr. hamilton naki
Dr. hamilton naki Dip mukherjee surgeon
Dip mukherjee surgeon Oral surgeon hamlin
Oral surgeon hamlin Uscis civil surgeon locator
Uscis civil surgeon locator I693 reminder letter
I693 reminder letter Thorasic surgeon
Thorasic surgeon Asherman chest seal
Asherman chest seal Cardiothoracic surgeon salary
Cardiothoracic surgeon salary Oliver hautmann
Oliver hautmann Cluster surgeon
Cluster surgeon Omar mansour rate my professor
Omar mansour rate my professor I693 form
I693 form Dr vijayant gupta
Dr vijayant gupta Ann lyons colorectal surgeon
Ann lyons colorectal surgeon Ssmdt
Ssmdt Neil moat cardiac surgeon
Neil moat cardiac surgeon Rajesh shah thoracic surgeon
Rajesh shah thoracic surgeon William allum surgeon
William allum surgeon Thoracic surgeon
Thoracic surgeon