Evolution of the Oncology Landscape An Overview of























- Slides: 89

Evolution of the Oncology Landscape: An Overview of Value, Quality, and Quality Measurements PP-ON-US-1174 10/2016 © Lilly USA, LLC 2016. ALL RIGHTS RESERVED. 1
Disclaimer This program is sponsored by, and the speaker is presenting on behalf of, Lilly USA, LLC. The presentation is consistent with FDA guidelines and is not approved for continuing education credit. This presentation is based on existing, publicly available information but may not represent the current activities of any specific provider or healthcare organization. This presentation was created using multiple sources and does not necessarily represent the opinions and/or viewpoints of Eli Lilly and Company or any other party. All product names, logos, brands, and other trademarks are the property of their respective trademark owners. Those trademark owners are not affiliated with Lilly and they do not sponsor or endorse this material. 2
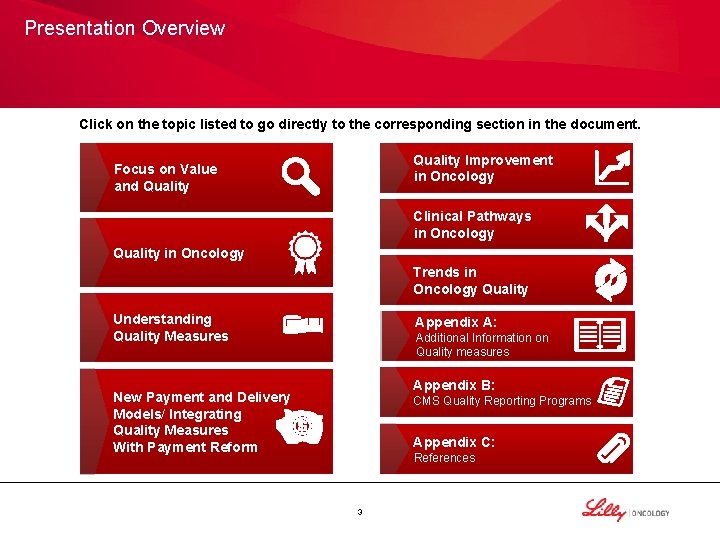
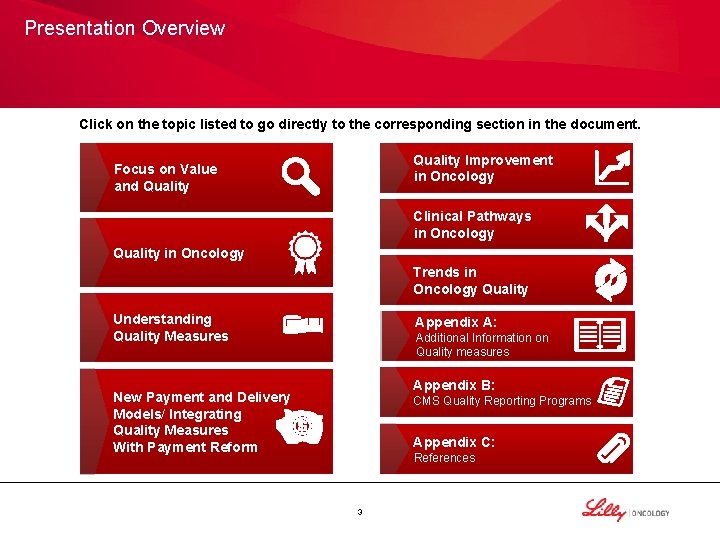
Presentation Overview Click on the topic listed to go directly to the corresponding section in the document. Quality Improvement in Oncology Focus on Value and Quality Clinical Pathways in Oncology Quality in Oncology Trends in Oncology Quality Understanding Quality Measures Appendix A: Additional Information on Quality measures Appendix B: New Payment and Delivery Models/ Integrating Quality Measures With Payment Reform CMS Quality Reporting Programs Appendix C: References 3
Presentation Objectives • Gain an understanding of quality measurement and reporting • Attain greater knowledge of quality in current and innovative payment delivery systems • Distinguish the influence of quality measures as they are integrated into cancer care • Understand the various stakeholders in the oncology landscape and their roles in defining value 4
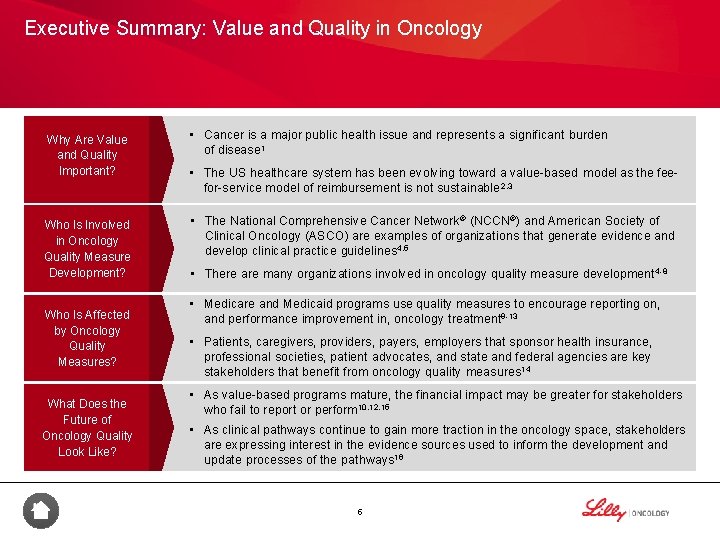
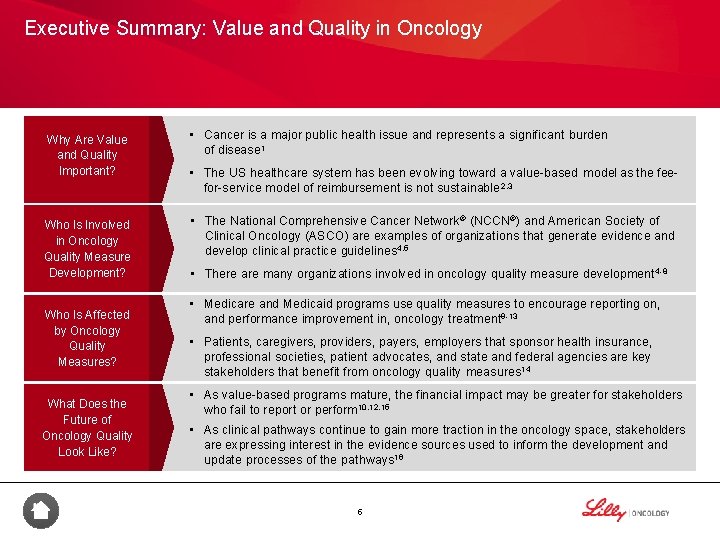
Executive Summary: Value and Quality in Oncology Why Are Value and Quality Important? Who Is Involved in Oncology Quality Measure Development? Who Is Affected by Oncology Quality Measures? What Does the Future of Oncology Quality Look Like? • Cancer is a major public health issue and represents a significant burden of disease 1 • The US healthcare system has been evolving toward a value-based model as the feefor-service model of reimbursement is not sustainable 2, 3 • The National Comprehensive Cancer Network ® (NCCN®) and American Society of Clinical Oncology (ASCO) are examples of organizations that generate evidence and develop clinical practice guidelines 4, 5 • There are many organizations involved in oncology quality measure development 4 -8 • Medicare and Medicaid programs use quality measures to encourage reporting on, and performance improvement in, oncology treatment 9 -13 • Patients, caregivers, providers, payers, employers that sponsor health insurance, professional societies, patient advocates, and state and federal agencies are key stakeholders that benefit from oncology quality measures 14 • As value-based programs mature, the financial impact may be greater for stakeholders who fail to report or perform 10, 12, 15 • As clinical pathways continue to gain more traction in the oncology space, stakeholders are expressing interest in the evidence sources used to inform the development and update processes of the pathways 16 5
Focus on Value and Quality in Oncology 6
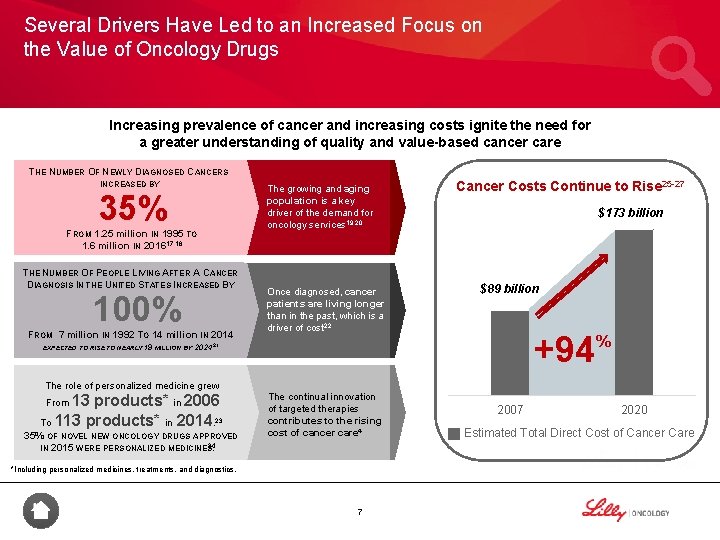
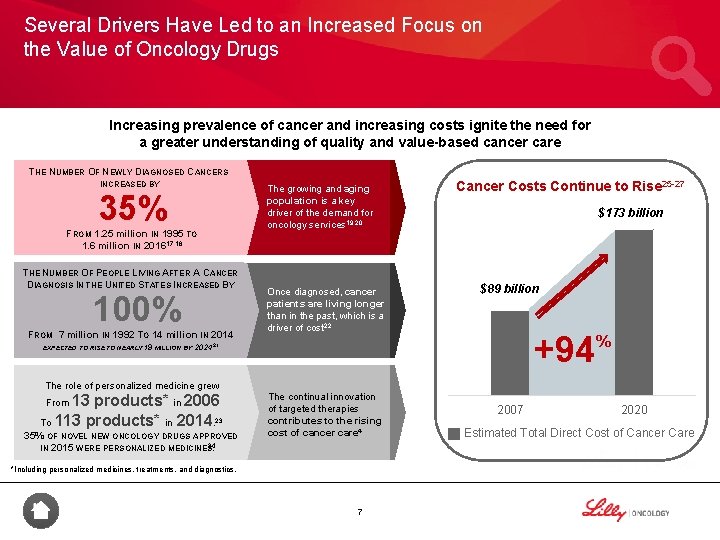
Several Drivers Have Led to an Increased Focus on the Value of Oncology Drugs Increasing prevalence of cancer and increasing costs ignite the need for a greater understanding of quality and value-based cancer care THE NUMBER OF NEWLY DIAGNOSED CANCERS INCREASED BY 35% FROM 1. 25 million IN 1995 TO 1. 6 million IN 201617, 18 THE NUMBER OF PEOPLE LIVING AFTER A CANCER DIAGNOSIS IN THE UNITED STATES INCREASED BY 100% FROM 7 million IN 1992 TO 14 million IN 2014 EXPECTED TO RISE TO NEARLY 19 MILLION BY The growing and aging population is a key driver of the demand for oncology services 19, 20 Once diagnosed, cancer patients are living longer than in the past, which is a driver of cost 22 Cancer Costs Continue to Rise 25 -27 $173 billion $89 billion +94 202421 The role of personalized medicine grew 13 products* in 2006 To 113 products* in 2014. 23 From 35% OF NOVEL NEW ONCOLOGY DRUGS APPROVED IN 2015 WERE PERSONALIZED MEDICINES 24. The continual innovation of targeted therapies contributes to the rising cost of cancer care 4 *Including personalized medicines, treatments, and diagnostics. 7 2007 % 2020 Estimated Total Direct Cost of Cancer Care
Summary • The healthcare system is changing from a volume-based to a value-based paradigm 2 • An aging and growing population and increasing numbers of cancer survivors have led to an increased focus on the value of oncology drugs 19, 20, 22 8

Quality in Oncology 9

System Inefficiencies Are Driving the Demand to Deliver Quality Care 14 Unsustainable Payment Option Fee-for-service system is volume-driven, which creates inflation pressure 3, 28, 29 Misaligned Treatment Care often is not patient-centered; in addition, not following established guidelines or pathways may be costly and not best practice 29, 30 Lack of Information Decisions about care often not based on the latest scientific evidence 29 Rising Costs Increased burden on all stakeholders including payers, providers, patients, employers, and taxpayers 3 Pace of Innovation Clinicians struggle to remain current with the volume of innovation 4 10

Healthcare “Quality” Has Many Dimensions As a leader in patient care, the Institute of Medicine (IOM) has identified 6 aims of high-quality care that have been widely adopted by other organizations active in improving the quality of healthcare. 31 Effective Equitable Efficient QUALITY Patient. Centered Safe Timely 11
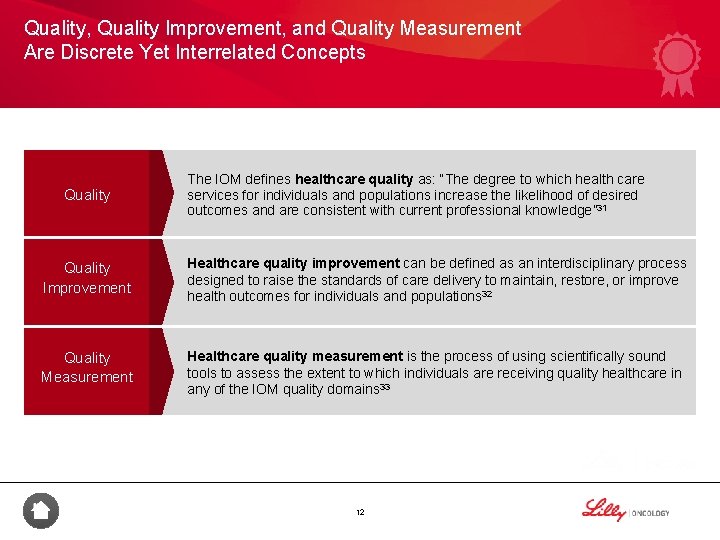
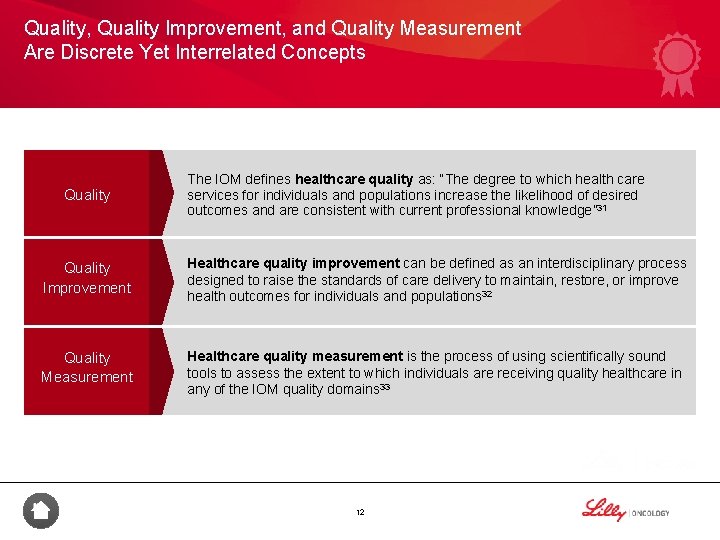
Quality, Quality Improvement, and Quality Measurement Are Discrete Yet Interrelated Concepts Quality The IOM defines healthcare quality as: “The degree to which health care services for individuals and populations increase the likelihood of desired outcomes and are consistent with current professional knowledge” 31 Quality Improvement Healthcare quality improvement can be defined as an interdisciplinary process designed to raise the standards of care delivery to maintain, restore, or improve health outcomes for individuals and populations 32 Quality Measurement Healthcare quality measurement is the process of using scientifically sound tools to assess the extent to which individuals are receiving quality healthcare in any of the IOM quality domains 33 12
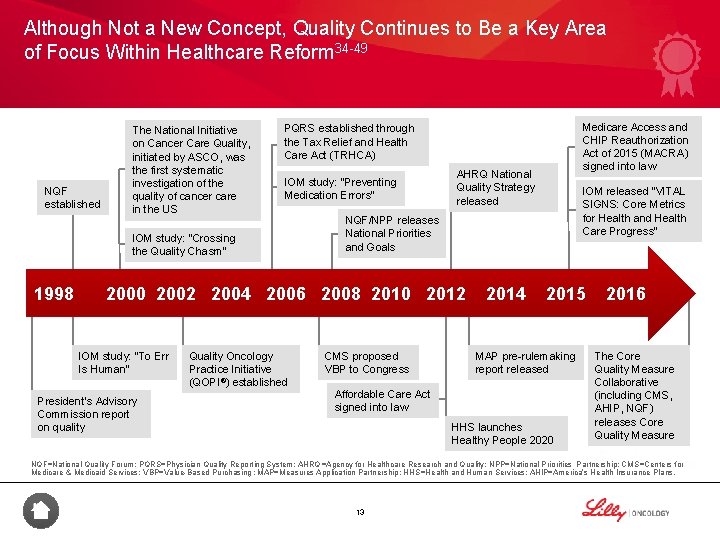
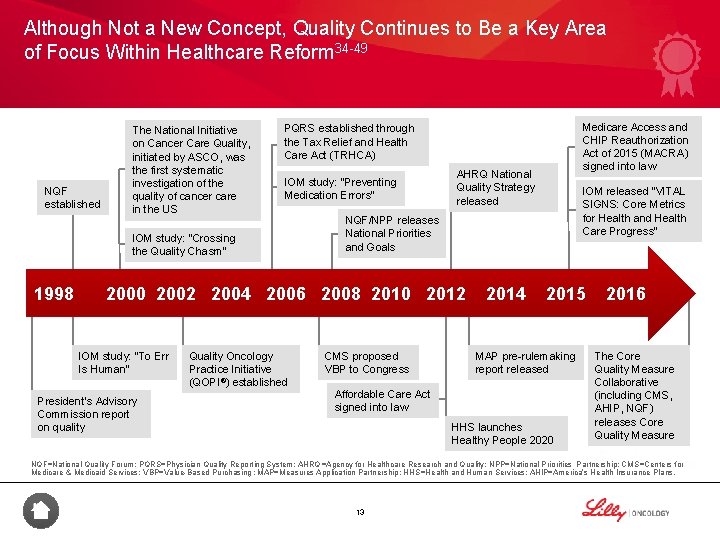
Although Not a New Concept, Quality Continues to Be a Key Area of Focus Within Healthcare Reform 34 -49 NQF established The National Initiative on Cancer Care Quality, initiated by ASCO, was the first systematic investigation of the quality of cancer care in the US IOM study: “Preventing Medication Errors” IOM study: “Crossing the Quality Chasm” 1998 AHRQ National Quality Strategy released President’s Advisory Commission report on quality Quality Oncology Practice Initiative (QOPI®) established IOM released "VITAL SIGNS: Core Metrics for Health and Health Care Progress” NQF/NPP releases National Priorities and Goals 2000 2002 2004 2006 2008 2010 2012 IOM study: “To Err Is Human” Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) signed into law PQRS established through the Tax Relief and Health Care Act (TRHCA) CMS proposed VBP to Congress 2014 2015 MAP pre-rulemaking report released Affordable Care Act signed into law HHS launches Healthy People 2020 2016 The Core Quality Measure Collaborative (including CMS, AHIP, NQF) releases Core Quality Measure NQF=National Quality Forum; PQRS=Physician Quality Reporting System; AHRQ =Agency for Healthcare Research and Quality; NPP=National Priorities Partnership; CMS=Centers for Medicare & Medicaid Services; VBP=Value-Based Purchasing; MAP=Measures Application Partnership; HHS=Health and Human Services; AHIP=America’s Health Insurance Plans. 13
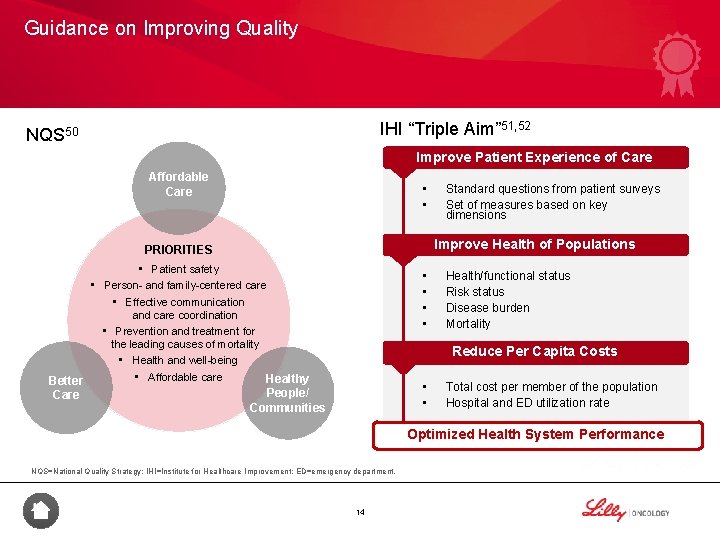
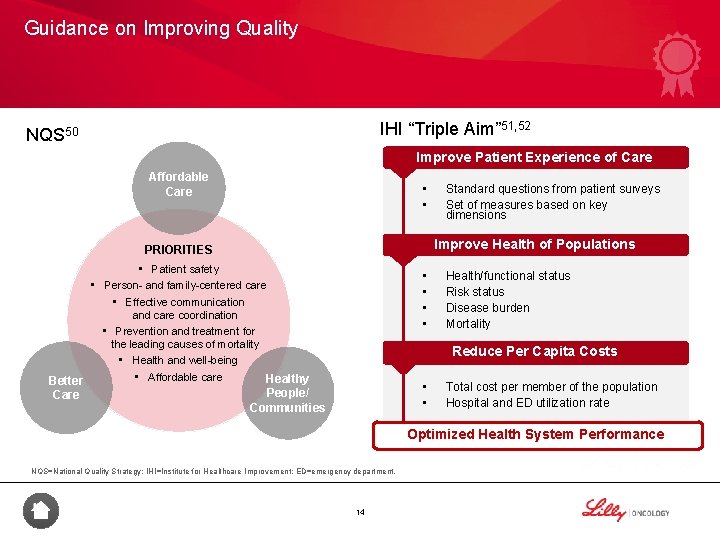
Guidance on Improving Quality IHI “Triple Aim” 51, 52 NQS 50 Improve Patient Experience of Care Affordable Care • • Standard questions from patient surveys Set of measures based on key dimensions Improve Health of Populations PRIORITIES • Patient safety • Person- and family-centered care • Effective communication and care coordination • Prevention and treatment for the leading causes of mortality • Health and well-being • Affordable care Healthy Better People/ Care Communities • • Health/functional status Risk status Disease burden Mortality Reduce Per Capita Costs • • Total cost per member of the population Hospital and ED utilization rate Optimized Health System Performance NQS=National Quality Strategy; IHI=Institute for Healthcare Improvement; ED=emergency department. 14
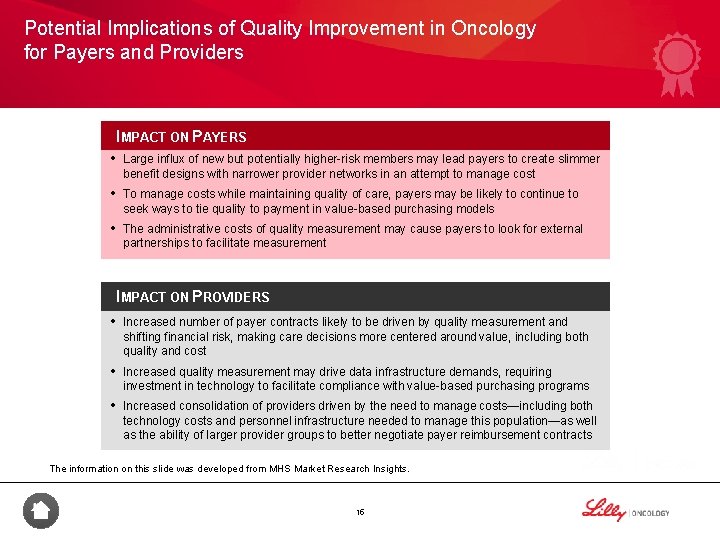
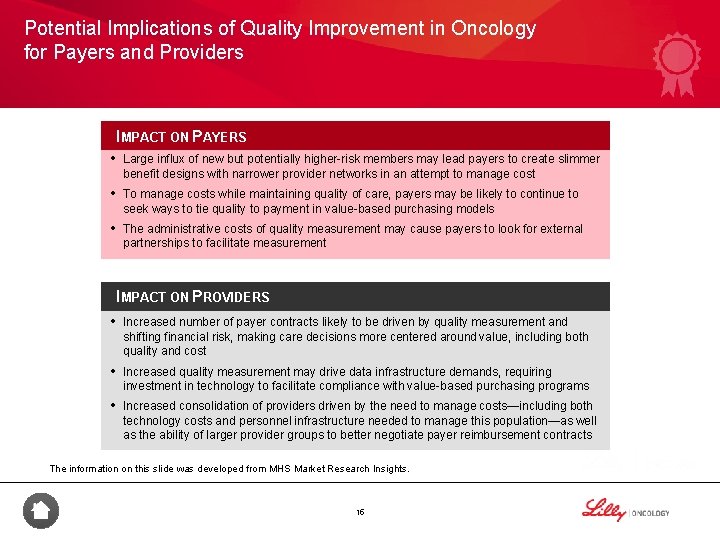
Potential Implications of Quality Improvement in Oncology for Payers and Providers IMPACT ON PAYERS • Large influx of new but potentially higher-risk members may lead payers to create slimmer benefit designs with narrower provider networks in an attempt to manage cost • To manage costs while maintaining quality of care, payers may be likely to continue to seek ways to tie quality to payment in value-based purchasing models • The administrative costs of quality measurement may cause payers to look for external partnerships to facilitate measurement IMPACT ON PROVIDERS • Increased number of payer contracts likely to be driven by quality measurement and shifting financial risk, making care decisions more centered around value, including both quality and cost • Increased quality measurement may drive data infrastructure demands, requiring investment in technology to facilitate compliance with value-based purchasing programs • Increased consolidation of providers driven by the need to manage costs—including both technology costs and personnel infrastructure needed to manage this population—as well as the ability of larger provider groups to better negotiate payer reimbursement contracts The information on this slide was developed from MHS Market Research Insights. 15
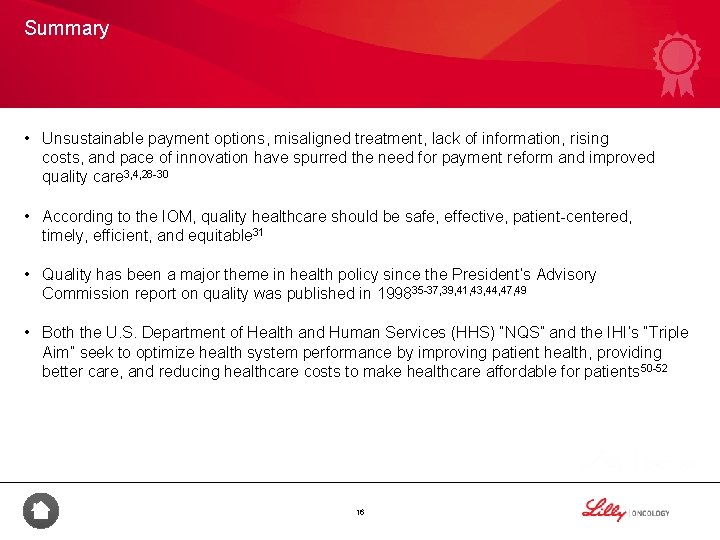
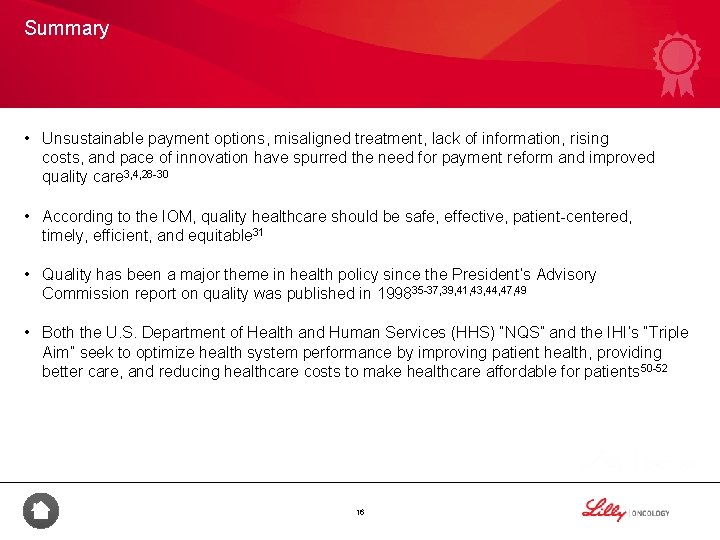
Summary • Unsustainable payment options, misaligned treatment, lack of information, rising costs, and pace of innovation have spurred the need for payment reform and improved quality care 3, 4, 28 -30 • According to the IOM, quality healthcare should be safe, effective, patient-centered, timely, efficient, and equitable 31 • Quality has been a major theme in health policy since the President’s Advisory Commission report on quality was published in 199835 -37, 39, 41, 43, 44, 47, 49 • Both the U. S. Department of Health and Human Services (HHS) “NQS” and the IHI’s “Triple Aim” seek to optimize health system performance by improving patient health, providing better care, and reducing healthcare costs to make healthcare affordable for patients 50 -52 16

Understanding Quality Measures 17
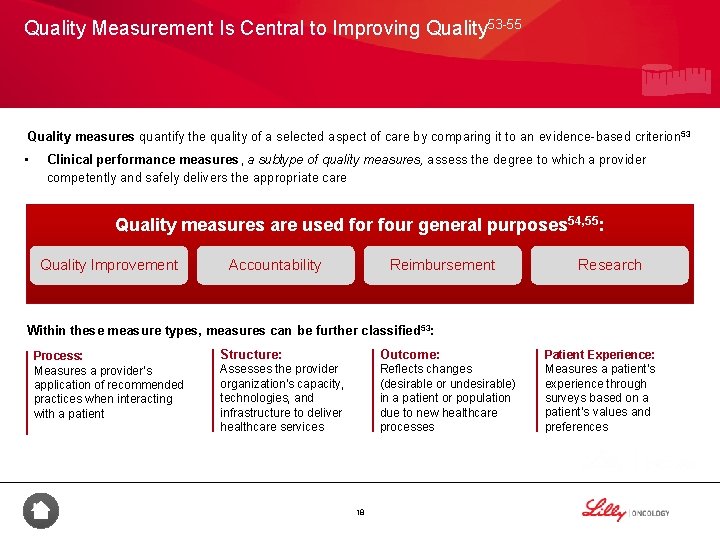
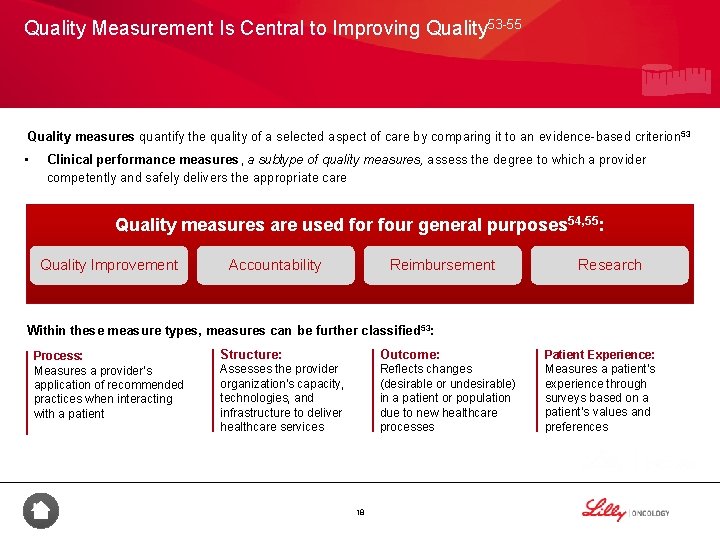
Quality Measurement Is Central to Improving Quality 53 -55 Quality measures quantify the quality of a selected aspect of care by comparing it to an evidence-based criterion 53 • Clinical performance measures, a subtype of quality measures, assess the degree to which a provider competently and safely delivers the appropriate care Quality measures are used for four general purposes 54, 55: Quality Improvement Accountability Reimbursement Research Within these measure types, measures can be further classified 53: Process: Measures a provider’s application of recommended practices when interacting with a patient Structure: Outcome: Assesses the provider organization’s capacity, technologies, and infrastructure to deliver healthcare services Reflects changes (desirable or undesirable) in a patient or population due to new healthcare processes 18 Patient Experience: Measures a patient’s experience through surveys based on a patient’s values and preferences
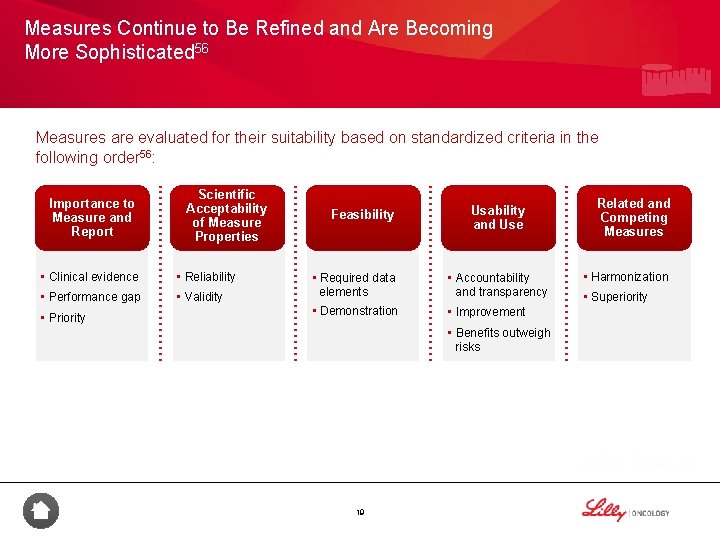
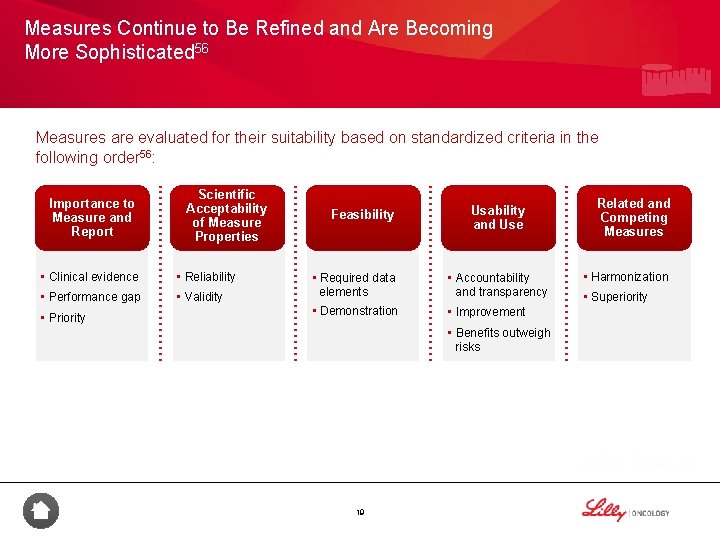
Measures Continue to Be Refined and Are Becoming More Sophisticated 56 Measures are evaluated for their suitability based on standardized criteria in the following order 56: Importance to Measure and Report Scientific Acceptability of Measure Properties • Clinical evidence • Reliability • Performance gap • Validity • Priority Feasibility Usability and Use • Required data elements • Accountability and transparency • Demonstration • Improvement • Benefits outweigh risks 19 Related and Competing Measures • Harmonization • Superiority
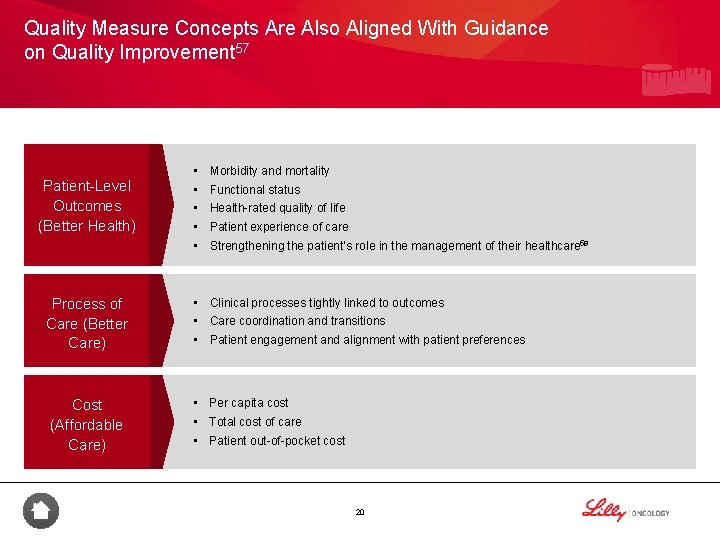
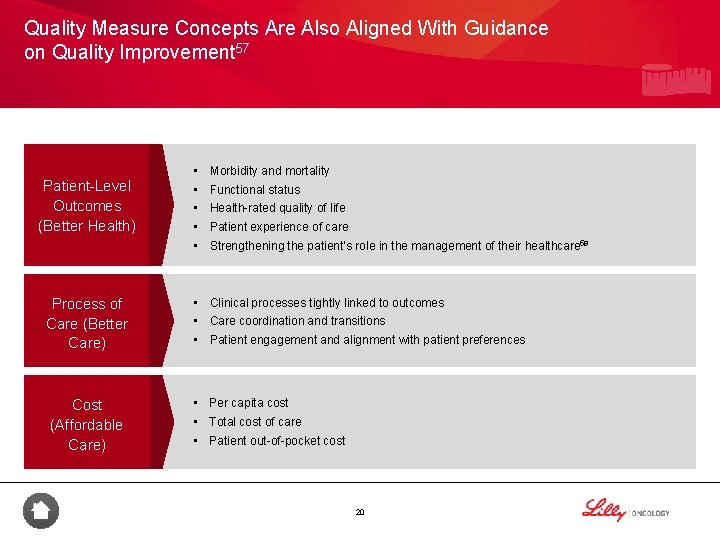
Quality Measure Concepts Are Also Aligned With Guidance on Quality Improvement 57 Patient-Level Outcomes (Better Health) Process of Care (Better Care) Cost (Affordable Care) • • • Morbidity and mortality Functional status Health-rated quality of life Patient experience of care Strengthening the patient’s role in the management of their healthcare 58 • Clinical processes tightly linked to outcomes • Care coordination and transitions • Patient engagement and alignment with patient preferences • Per capita cost • Total cost of care • Patient out-of-pocket cost 20

Summary • Quality measures can be classified as process, structure, outcome, or patient experience, depending on what is being measured 54 • Measures are evaluated for their suitability based on the following standardized criteria in the following order 56: – – – Importance to measure and report Scientific acceptability of measure properties Feasibility Usability and use Related and competing measures • Measures in the public domain are aligned with the 3 aims of the NQS: better health, better care, and affordable care 57 21

New Payment and Delivery Models 22
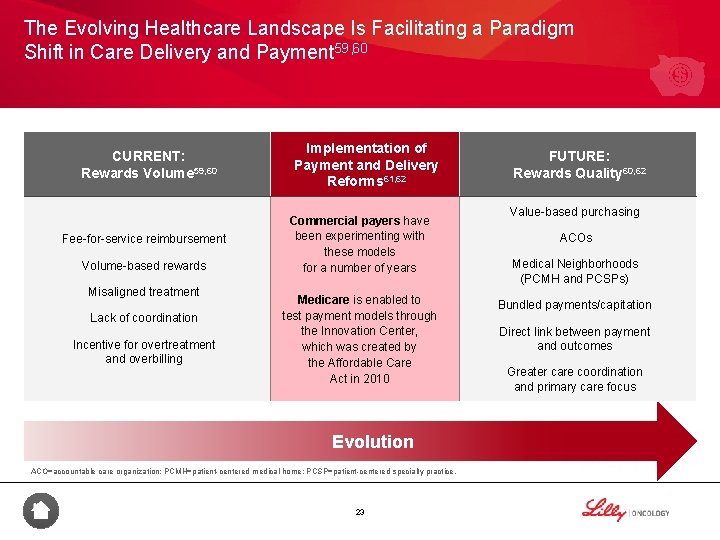
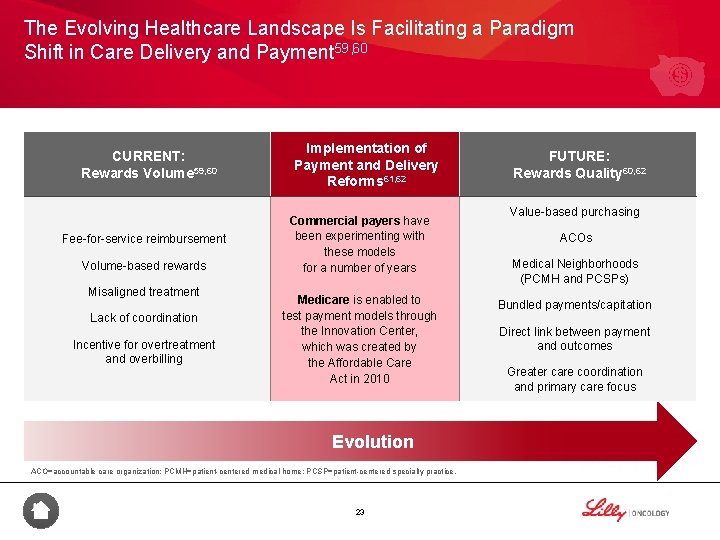
The Evolving Healthcare Landscape Is Facilitating a Paradigm Shift in Care Delivery and Payment 59, 60 CURRENT: Rewards Volume 59, 60 Fee-for-service reimbursement Volume-based rewards Misaligned treatment Lack of coordination Incentive for overtreatment and overbilling Implementation of Payment and Delivery Reforms 61, 62 Commercial payers have been experimenting with these models for a number of years Medicare is enabled to test payment models through the Innovation Center, which was created by the Affordable Care Act in 2010 Evolution ACO=accountable care organization; PCMH=patient-centered medical home; PCSP=patient-centered specialty practice. 23 FUTURE: Rewards Quality 60, 62 Value-based purchasing ACOs Medical Neighborhoods (PCMH and PCSPs) Bundled payments/capitation Direct link between payment and outcomes Greater care coordination and primary care focus
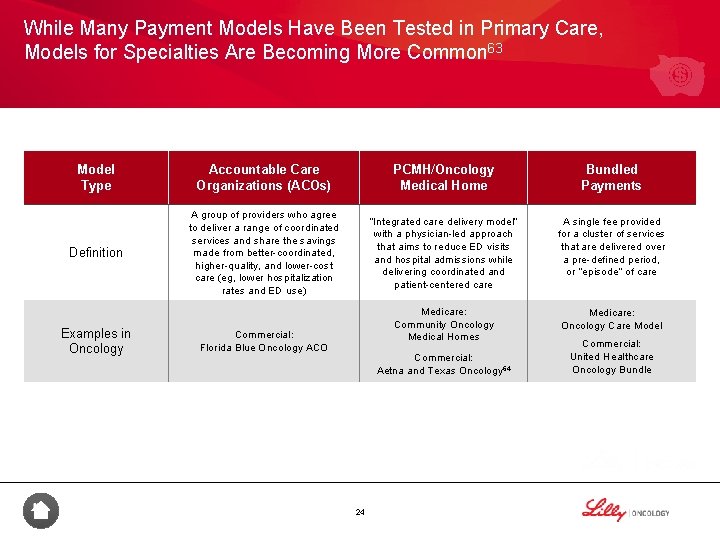
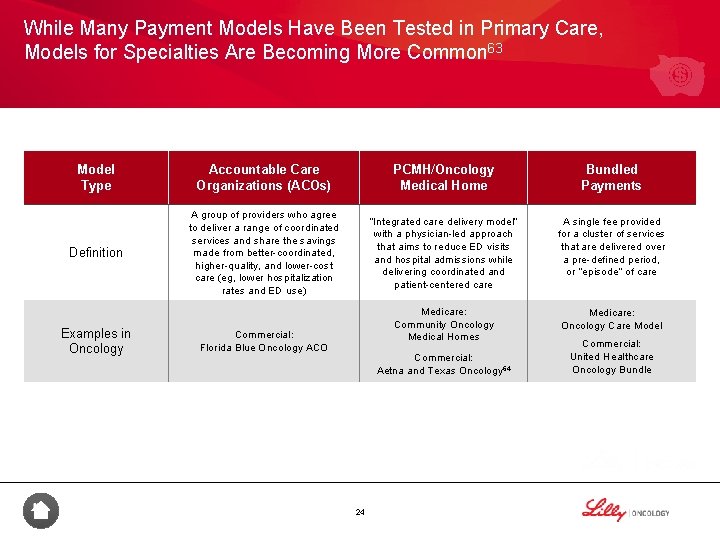
While Many Payment Models Have Been Tested in Primary Care, Models for Specialties Are Becoming More Common 63 Model Type Accountable Care Organizations (ACOs) PCMH/Oncology Medical Home Bundled Payments Definition A group of providers who agree to deliver a range of coordinated services and share the savings made from better-coordinated, higher-quality, and lower-cost care (eg, lower hospitalization rates and ED use) “Integrated care delivery model” with a physician-led approach that aims to reduce ED visits and hospital admissions while delivering coordinated and patient-centered care A single fee provided for a cluster of services that are delivered over a pre-defined period, or “episode” of care Medicare: Community Oncology Medical Homes Medicare: Oncology Care Model Examples in Oncology Commercial: Florida Blue Oncology ACO Commercial: Aetna and Texas Oncology 64 24 Commercial: United Healthcare Oncology Bundle
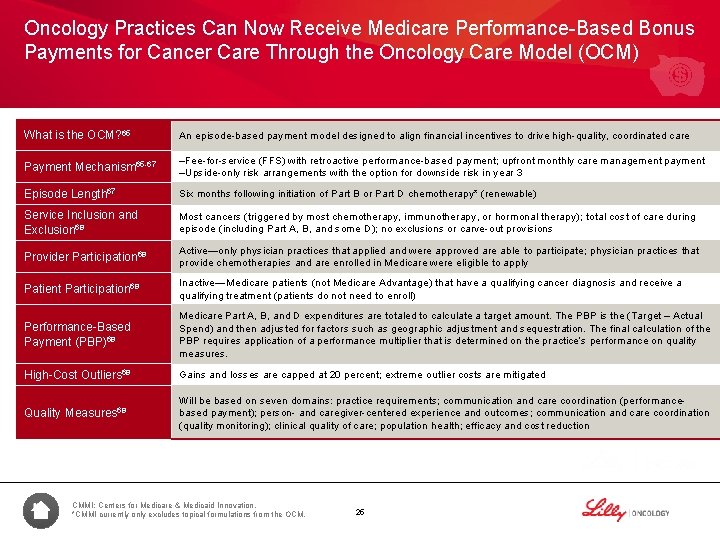
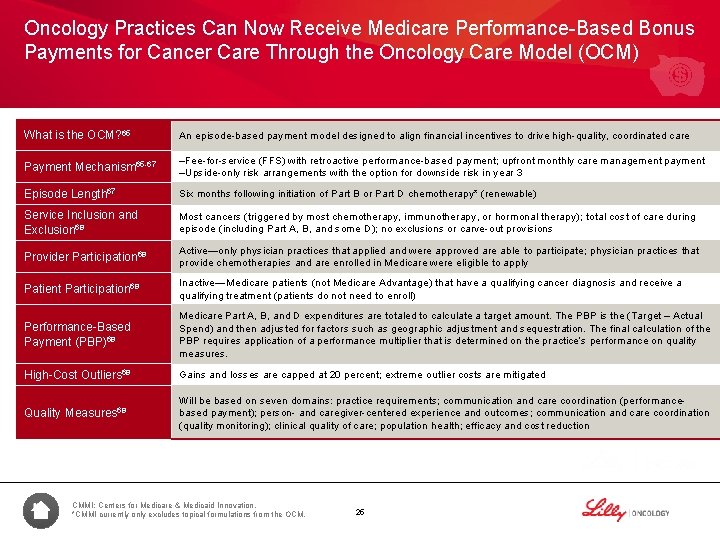
Oncology Practices Can Now Receive Medicare Performance-Based Bonus Payments for Cancer Care Through the Oncology Care Model (OCM) What is the OCM? 65 An episode-based payment model designed to align financial incentives to drive high-quality, coordinated care Payment Mechanism 65 -67 –Fee-for-service (FFS) with retroactive performance-based payment; upfront monthly care management payment –Upside-only risk arrangements with the option for downside risk in year 3 Episode Length 67 Six months following initiation of Part B or Part D chemotherapy* (renewable) Service Inclusion and Exclusion 68 Most cancers (triggered by most chemotherapy, immunotherapy, or hormonal therapy); total cost of care during episode (including Part A, B, and some D); no exclusions or carve-out provisions Provider Participation 68 Active—only physician practices that applied and were approved are able to participate; physician practices that provide chemotherapies and are enrolled in Medicare were eligible to apply Patient Participation 68 Inactive—Medicare patients (not Medicare Advantage) that have a qualifying cancer diagnosis and receive a qualifying treatment (patients do not need to enroll) Performance-Based Payment (PBP)68 Medicare Part A, B, and D expenditures are totaled to calculate a target amount. The PBP is the (Target – Actual Spend) and then adjusted for factors such as geographic adjustment and sequestration. The final calculation of the PBP requires application of a performance multiplier that is determined on the practice’s performance on quality measures. High-Cost Outliers 68 Gains and losses are capped at 20 percent; extreme outlier costs are mitigated Quality Measures 68 Will be based on seven domains: practice requirements; communication and care coordination (performancebased payment); person- and caregiver-centered experience and outcomes; communication and care coordination (quality monitoring); clinical quality of care; population health; efficacy and cost reduction CMMI: Centers for Medicare & Medicaid Innovation. *CMMI currently only excludes topical formulations from the OCM. 25

Although the OCM Is a Step Towards Value-Based Payments in Oncology, Participants Will Still Be Paid Based on FFS payments continue as usual to the participating practice Monthly Enhanced Oncology Services (MEOS) payment of $160 Per-Beneficiary Per Month (PBPM)66 • Enhanced services include 24/7 clinician access, patient navigation, care planning, and use of clinical guidelines 69 • OCM practices can bill for MEOS each of the 6 months of the episode 69 • OCM practices can bill for MEOS for nearly all cancer types and focuses on chemotherapy treatment (topical chemotherapy is excluded)68, 69 • MEOS is subject to recoupment at reconciliation 69 OCM practitioners cannot bill for 69: • • • Chronic Care Management (CCM) Transitional Care Management (TCM) Home Health Care Supervision Hospice Care Supervision End Stage Renal Disease (ESRD) Semi-annual potential for performance-based payment for savings on total cost of care compared with a risk-adjusted target amount (one-sided and two-sided risk arrangements available)70 26
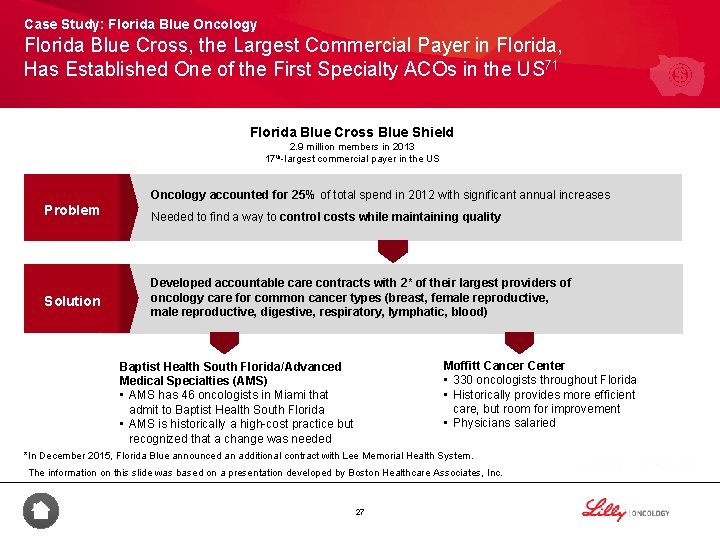
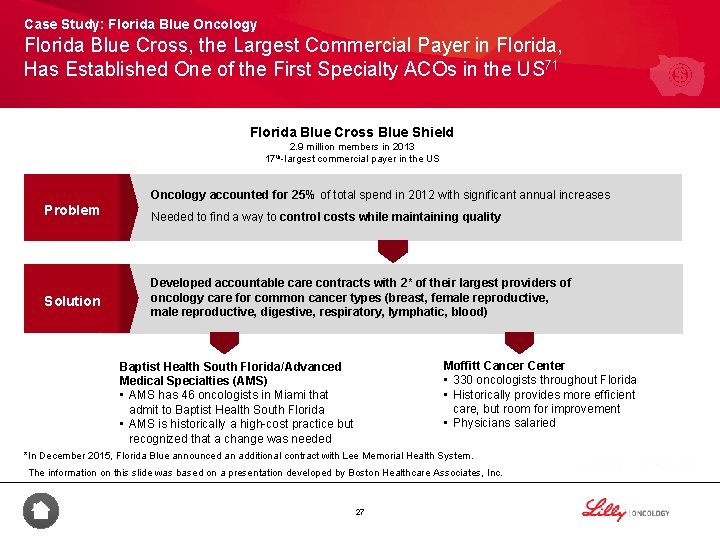
Case Study: Florida Blue Oncology Florida Blue Cross, the Largest Commercial Payer in Florida, Has Established One of the First Specialty ACOs in the US 71 Florida Blue Cross Blue Shield 2. 9 million members in 2013 17 th-largest commercial payer in the US Oncology accounted for 25% of total spend in 2012 with significant annual increases Problem Solution Needed to find a way to control costs while maintaining quality Developed accountable care contracts with 2* of their largest providers of oncology care for common cancer types (breast, female reproductive, digestive, respiratory, lymphatic, blood) Baptist Health South Florida/Advanced Medical Specialties (AMS) • AMS has 46 oncologists in Miami that admit to Baptist Health South Florida • AMS is historically a high-cost practice but recognized that a change was needed Moffitt Cancer Center • 330 oncologists throughout Florida • Historically provides more efficient care, but room for improvement • Physicians salaried *In December 2015, Florida Blue announced an additional contract with Lee Memorial Health System. The information on this slide was based on a presentation developed by Boston Healthcare Associates, Inc. 27
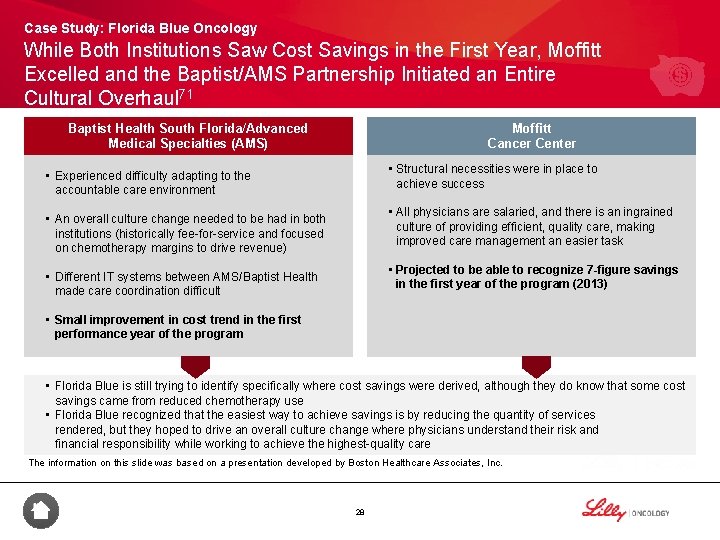
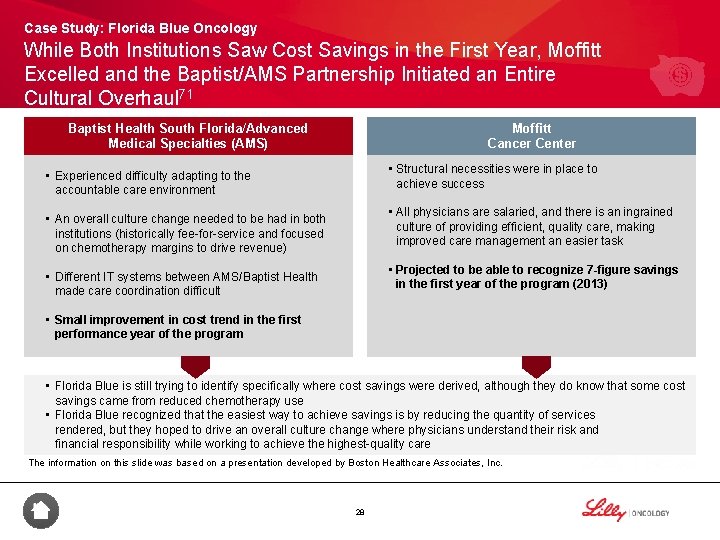
Case Study: Florida Blue Oncology While Both Institutions Saw Cost Savings in the First Year, Moffitt Excelled and the Baptist/AMS Partnership Initiated an Entire Cultural Overhaul 71 Baptist Health South Florida/Advanced Medical Specialties (AMS) Moffitt Cancer Center • Structural necessities were in place to achieve success • Experienced difficulty adapting to the accountable care environment • All physicians are salaried, and there is an ingrained culture of providing efficient, quality care, making improved care management an easier task • An overall culture change needed to be had in both institutions (historically fee-for-service and focused on chemotherapy margins to drive revenue) • Projected to be able to recognize 7 -figure savings in the first year of the program (2013) • Different IT systems between AMS/Baptist Health made care coordination difficult • Small improvement in cost trend in the first performance year of the program • Florida Blue is still trying to identify specifically where cost savings were derived, although they do know that some cost savings came from reduced chemotherapy use • Florida Blue recognized that the easiest way to achieve savings is by reducing the quantity of services rendered, but they hoped to drive an overall culture change where physicians understand their risk and financial responsibility while working to achieve the highest-quality care The information on this slide was based on a presentation developed by Boston Healthcare Associates, Inc. 28
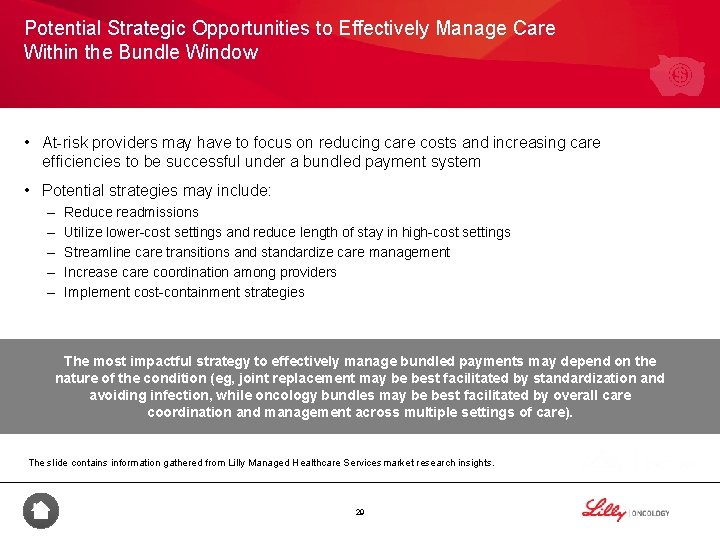
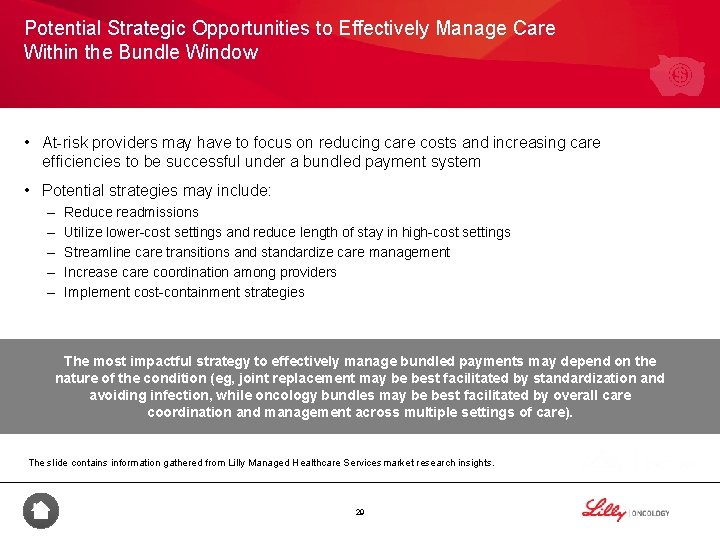
Potential Strategic Opportunities to Effectively Manage Care Within the Bundle Window • At-risk providers may have to focus on reducing care costs and increasing care efficiencies to be successful under a bundled payment system • Potential strategies may include: – – – Reduce readmissions Utilize lower-cost settings and reduce length of stay in high-cost settings Streamline care transitions and standardize care management Increase care coordination among providers Implement cost-containment strategies The most impactful strategy to effectively manage bundled payments may depend on the nature of the condition (eg, joint replacement may be best facilitated by standardization and avoiding infection, while oncology bundles may be best facilitated by overall care coordination and management across multiple settings of care). The slide contains information gathered from Lilly Managed Healthcare Services market research insights. 29
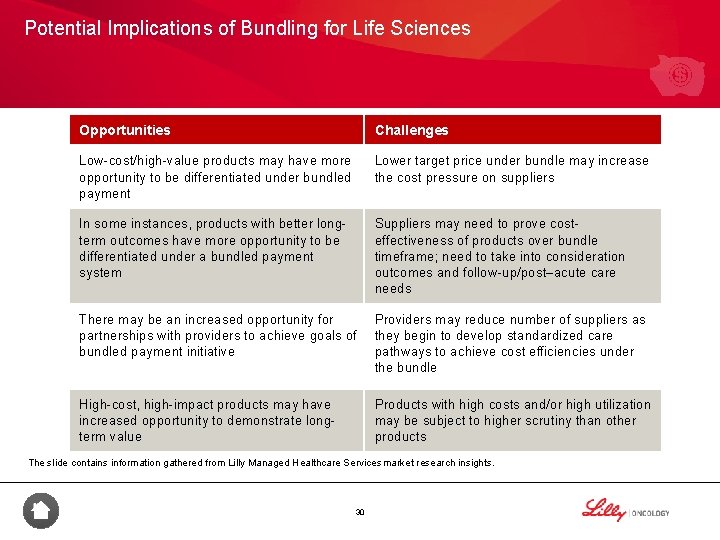
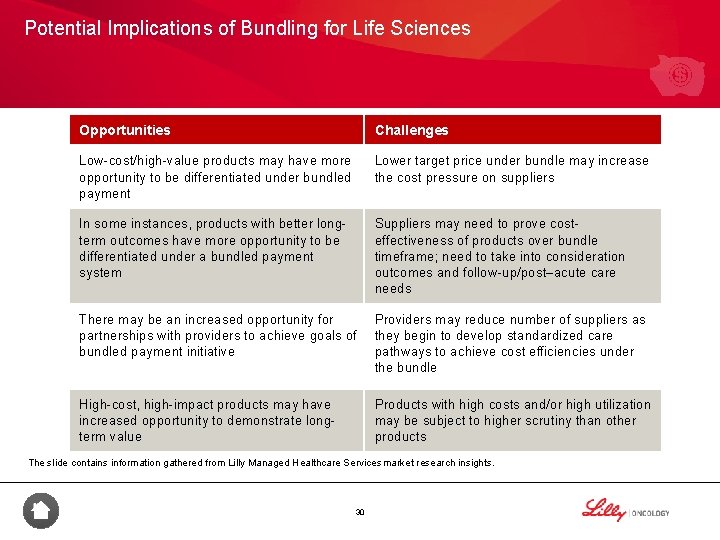
Potential Implications of Bundling for Life Sciences Opportunities Challenges Low-cost/high-value products may have more opportunity to be differentiated under bundled payment Lower target price under bundle may increase the cost pressure on suppliers In some instances, products with better longterm outcomes have more opportunity to be differentiated under a bundled payment system Suppliers may need to prove costeffectiveness of products over bundle timeframe; need to take into consideration outcomes and follow-up/post–acute care needs There may be an increased opportunity for partnerships with providers to achieve goals of bundled payment initiative Providers may reduce number of suppliers as they begin to develop standardized care pathways to achieve cost efficiencies under the bundle High-cost, high-impact products may have increased opportunity to demonstrate longterm value Products with high costs and/or high utilization may be subject to higher scrutiny than other products The slide contains information gathered from Lilly Managed Healthcare Services market research insights. 30
Summary • Payment reform is shifting risk to providers and moving towards bundled payments and capitation-style patients, placing greater importance on measuring quality to ensure patients are receiving evidence-based care in a cost-conscious environment 59 -60 • Commercial payers have tested multiple model types in payment reform in oncology, while Medicare has only recently launched an Oncology ACO model (the Oncology Care Model)60 -63 31

Integrating Quality Measures With Payment Reform 32
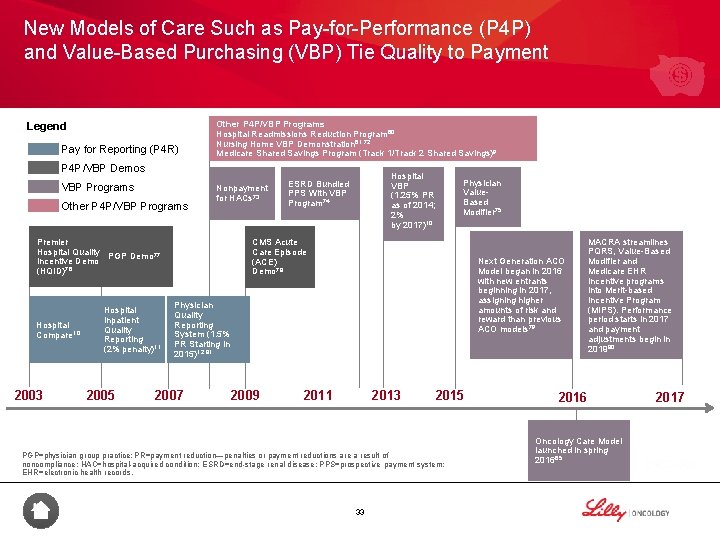
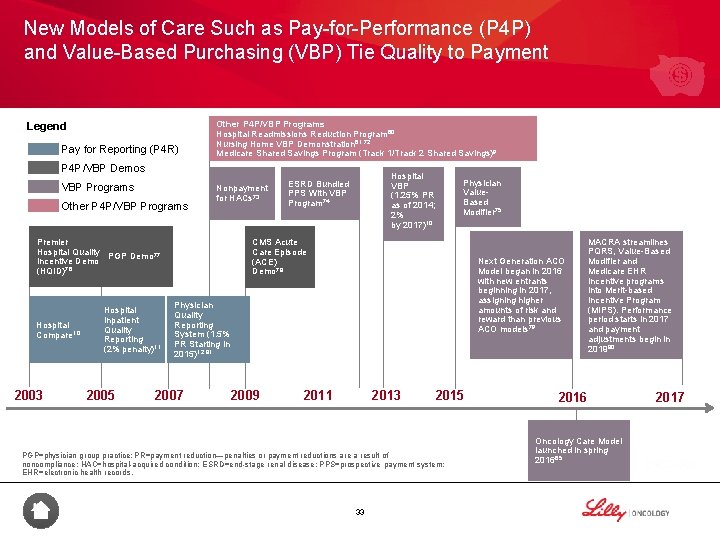
New Models of Care Such as Pay-for-Performance (P 4 P) and Value-Based Purchasing (VBP) Tie Quality to Payment Legend Pay for Reporting (P 4 R) Other P 4 P/VBP Programs Hospital Readmissions Reduction Program 60 Nursing Home VBP Demonstration 61, 72 Medicare Shared Savings Program (Track 1/Track 2 Shared Savings)9 P 4 P/VBP Demos VBP Programs Other P 4 P/VBP Programs Nonpayment for HACs 73 Premier Hospital Quality PGP Demo 77 Incentive Demo 76 (HQID) Hospital Compare 10 2003 Hospital Inpatient Quality Reporting (2% penalty)11 2005 Hospital VBP (1. 25% PR as of 2014; 2% by 2017)10 ESRD Bundled PPS With VBP Program 74 Physician Value. Based Modifier 75 CMS Acute Care Episode (ACE) Demo 78 Next Generation ACO Model began in 2016 with new entrants beginning in 2017, assigning higher amounts of risk and reward than previous ACO models 79 Physician Quality Reporting System (1. 5% PR Starting in 2015)12, 81 2007 2009 2011 2013 2015 PGP=physician group practice; PR=payment reduction—penalties or payment reductions are a result of noncompliance; HAC=hospital-acquired condition; ESRD=end-stage renal disease; PPS=prospective payment system; EHR=electronic health records. 33 MACRA streamlines PQRS, Value-Based Modifier and Medicare EHR Incentive programs into Merit-based Incentive Program (MIPS). Performance period starts in 2017 and payment adjustments begin in 201980 2016 Oncology Care Model launched in spring 201665 2017
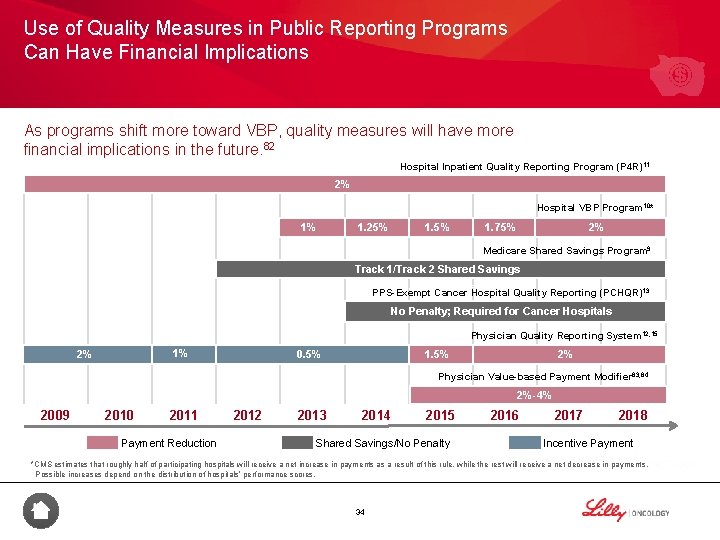
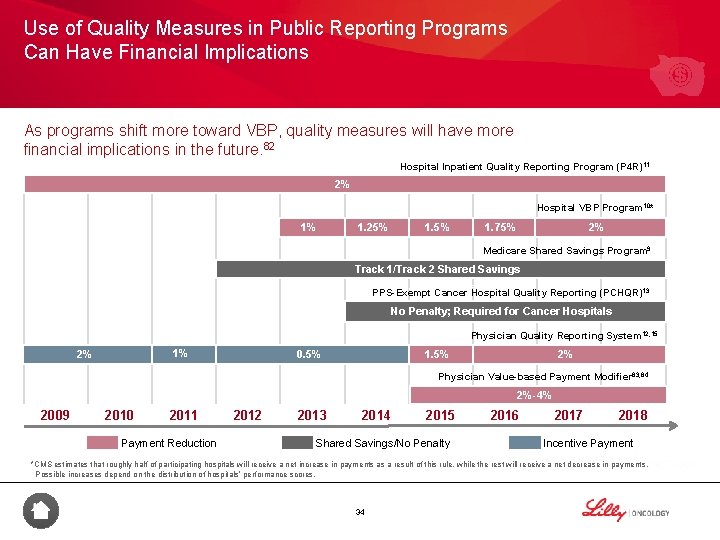
Use of Quality Measures in Public Reporting Programs Can Have Financial Implications As programs shift more toward VBP, quality measures will have more financial implications in the future. 82 Hospital Inpatient Quality Reporting Program (P 4 R)11 2% Hospital VBP Program 10* 1% 1. 25% 1. 5% 2% 1. 75% Medicare Shared Savings Program 9 Track 1/Track 2 Shared Savings Upside/Downside Risk PPS-Exempt Cancer Hospital Quality Reporting (PCHQR)13 No Penalty; Required for Cancer Hospitals Physician Quality Reporting System 12, 15 1% 2% 0. 5% 1. 5% 2% Physician Value-based Payment Modifier 83, 84 2%-4% 2009 2010 2011 Payment Reduction 2012 2013 2014 2015 Shared Savings/No Penalty 2016 2017 2018 Incentive Payment *CMS estimates that roughly half of participating hospitals will receive a net increase in payments as a result of this rule, while the rest will receive a net decrease in payments. Possible increases depend on the distribution of hospitals’ performance scores. 34
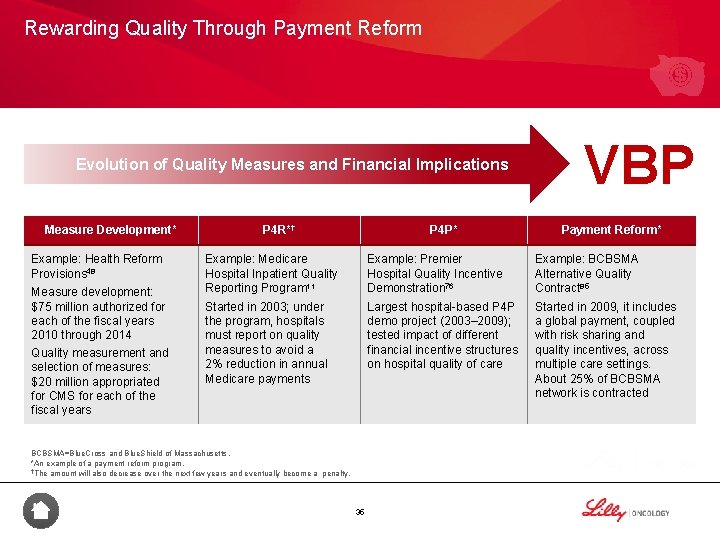
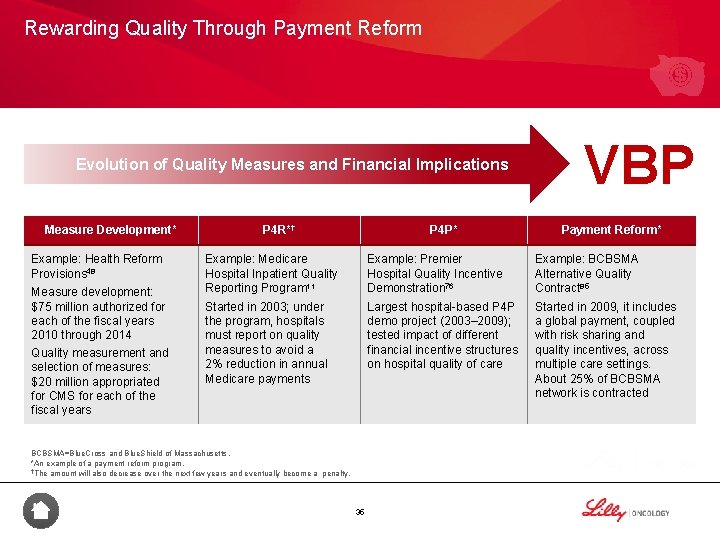
Rewarding Quality Through Payment Reform Evolution of Quality Measures and Financial Implications Measure Development* Example: Health Reform Provisions 48 Measure development: $75 million authorized for each of the fiscal years 2010 through 2014 Quality measurement and selection of measures: $20 million appropriated for CMS for each of the fiscal years P 4 R*† P 4 P* VBP Payment Reform* Example: Medicare Hospital Inpatient Quality Reporting Program 11 Example: Premier Hospital Quality Incentive Demonstration 76 Example: BCBSMA Alternative Quality Contract 85 Started in 2003; under the program, hospitals must report on quality measures to avoid a 2% reduction in annual Medicare payments Largest hospital-based P 4 P demo project (2003– 2009); tested impact of different financial incentive structures on hospital quality of care Started in 2009, it includes a global payment, coupled with risk sharing and quality incentives, across multiple care settings. About 25% of BCBSMA network is contracted BCBSMA=Blue. Cross and Blue. Shield of Massachusetts. *An example of a payment reform program. †The amount will also decrease over the next few years and eventually become a penalty. 35
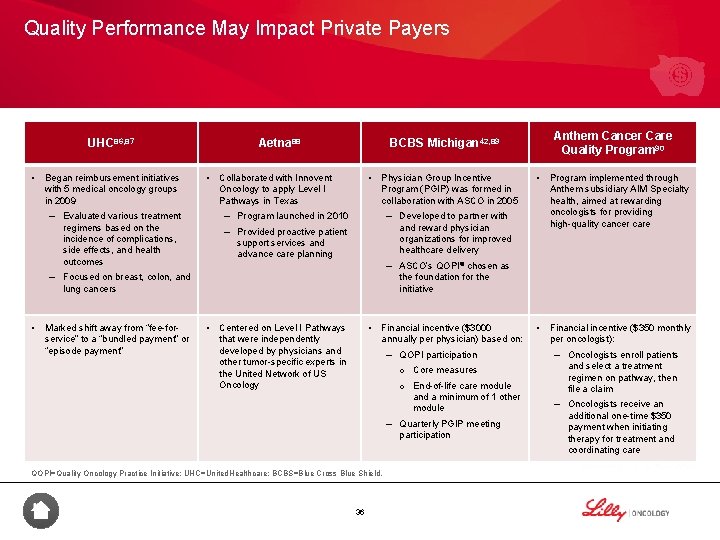
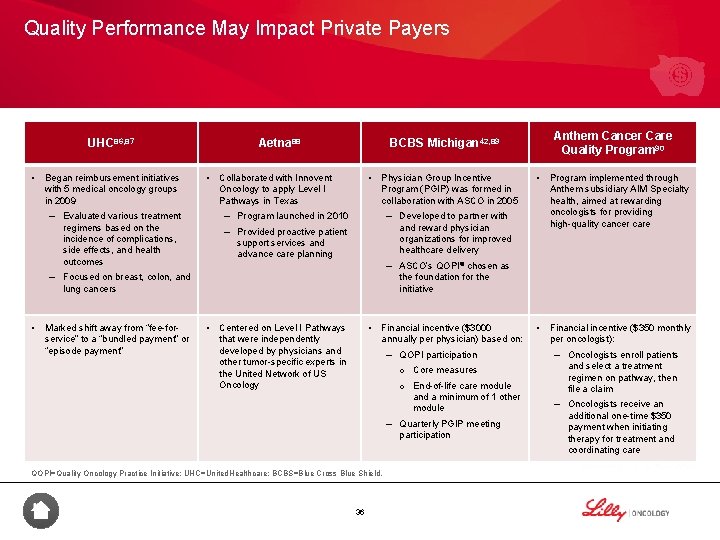
Quality Performance May Impact Private Payers UHC 86, 87 • Began reimbursement initiatives with 5 medical oncology groups in 2009 Aetna 88 • – Evaluated various treatment • Collaborated with Innovent Oncology to apply Level I Pathways in Texas Physician Group Incentive Program (PGIP) was formed in collaboration with ASCO in 2005 – Program launched in 2010 regimens based on the incidence of complications, side effects, and health outcomes Program implemented through Anthem subsidiary AIM Specialty health, aimed at rewarding oncologists for providing high-quality cancer care • Financial incentive ($350 monthly per oncologist): and reward physician organizations for improved healthcare delivery – Provided proactive patient support services and advance care planning – ASCO’s QOPI® chosen as the foundation for the initiative lung cancers Marked shift away from “fee-forservice” to a “bundled payment” or “episode payment” • – Developed to partner with – Focused on breast, colon, and • Anthem Cancer Care Quality Program 90 BCBS Michigan 42, 89 • • Centered on Level I Pathways that were independently developed by physicians and other tumor-specific experts in the United Network of US Oncology Financial incentive ($3000 annually per physician) based on: – QOPI participation – Oncologists enroll patients o Core measures and select a treatment regimen on pathway, then file a claim o End-of-life care module and a minimum of 1 other module – Quarterly PGIP meeting participation QOPI=Quality Oncology Practice Initiative; UHC=United. Healthcare; BCBS=Blue Cross Blue Shield. 36 – Oncologists receive an additional one-time $350 payment when initiating therapy for treatment and coordinating care
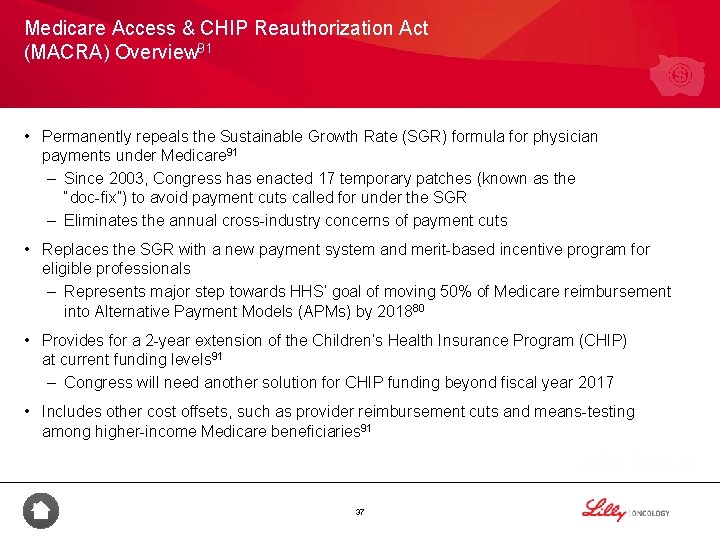
Medicare Access & CHIP Reauthorization Act (MACRA) Overview 91 • Permanently repeals the Sustainable Growth Rate (SGR) formula for physician payments under Medicare 91 – Since 2003, Congress has enacted 17 temporary patches (known as the “doc-fix”) to avoid payment cuts called for under the SGR – Eliminates the annual cross-industry concerns of payment cuts • Replaces the SGR with a new payment system and merit-based incentive program for eligible professionals – Represents major step towards HHS’ goal of moving 50% of Medicare reimbursement into Alternative Payment Models (APMs) by 201880 • Provides for a 2 -year extension of the Children’s Health Insurance Program (CHIP) at current funding levels 91 – Congress will need another solution for CHIP funding beyond fiscal year 2017 • Includes other cost offsets, such as provider reimbursement cuts and means-testing among higher-income Medicare beneficiaries 91 37
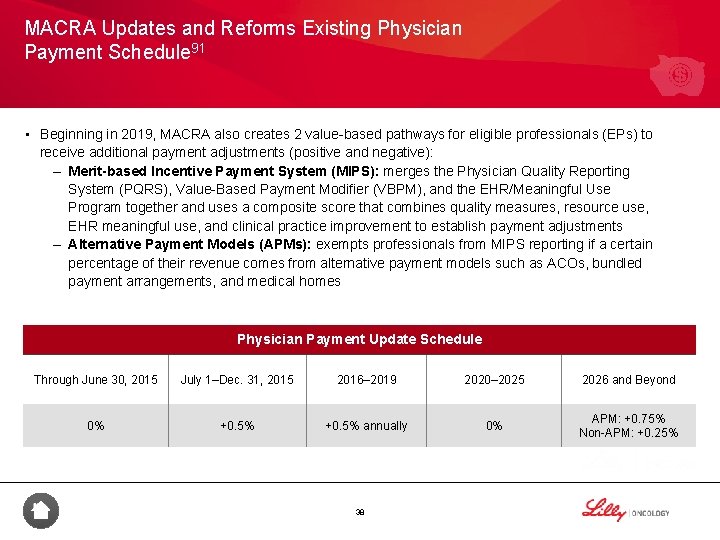
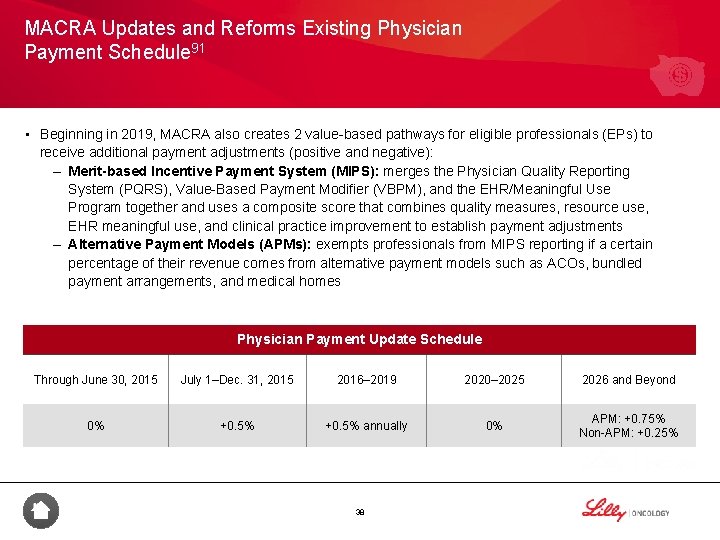
MACRA Updates and Reforms Existing Physician Payment Schedule 91 • Beginning in 2019, MACRA also creates 2 value-based pathways for eligible professionals (EPs) to receive additional payment adjustments (positive and negative): – Merit-based Incentive Payment System (MIPS): merges the Physician Quality Reporting System (PQRS), Value-Based Payment Modifier (VBPM), and the EHR/Meaningful Use Program together and uses a composite score that combines quality measures, resource use, EHR meaningful use, and clinical practice improvement to establish payment adjustments – Alternative Payment Models (APMs): exempts professionals from MIPS reporting if a certain percentage of their revenue comes from alternative payment models such as ACOs, bundled payment arrangements, and medical homes Physician Payment Update Schedule Through June 30, 2015 July 1–Dec. 31, 2015 2016– 2019 2020– 2025 2026 and Beyond 0% +0. 5% annually 0% APM: +0. 75% Non-APM: +0. 25% 38
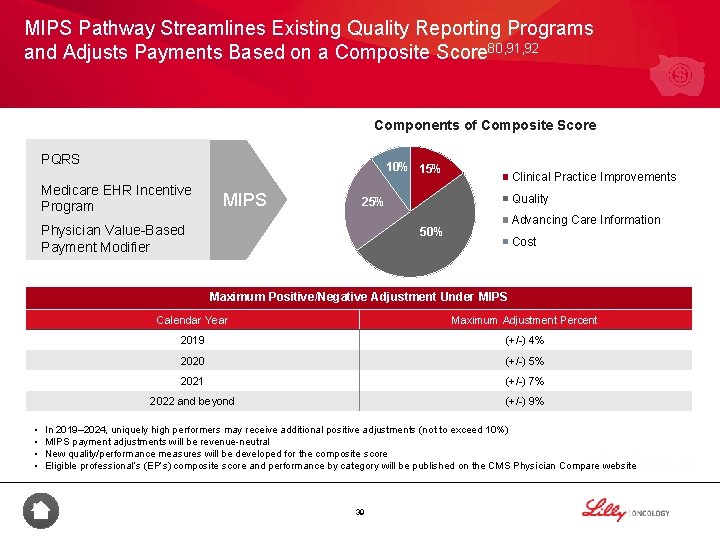
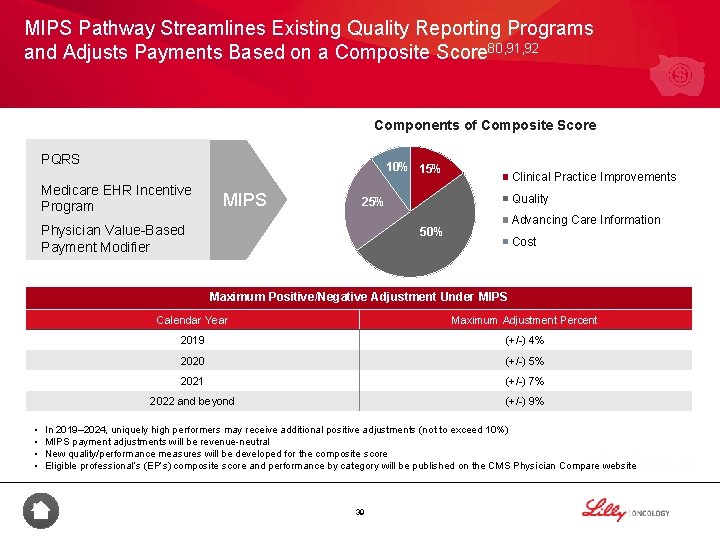
MIPS Pathway Streamlines Existing Quality Reporting Programs and Adjusts Payments Based on a Composite Score 80, 91, 92 Components of Composite Score PQRS 10% 15% Medicare EHR Incentive Program MIPS Clinical Practice Improvements Quality 25% Physician Value-Based Payment Modifier Advancing Care Information 50% Cost Maximum Positive/Negative Adjustment Under MIPS • • Calendar Year Maximum Adjustment Percent 2019 (+/-) 4% 2020 (+/-) 5% 2021 (+/-) 7% 2022 and beyond (+/-) 9% In 2019– 2024, uniquely high performers may receive additional positive adjustments (not to exceed 10%) MIPS payment adjustments will be revenue-neutral New quality/performance measures will be developed for the composite score Eligible professional’s (EP’s) composite score and performance by category will be published on the CMS Physician Compare website 39
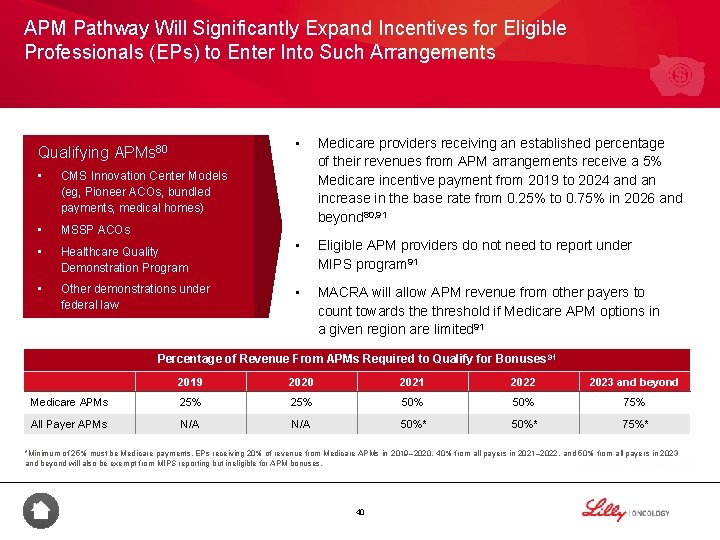
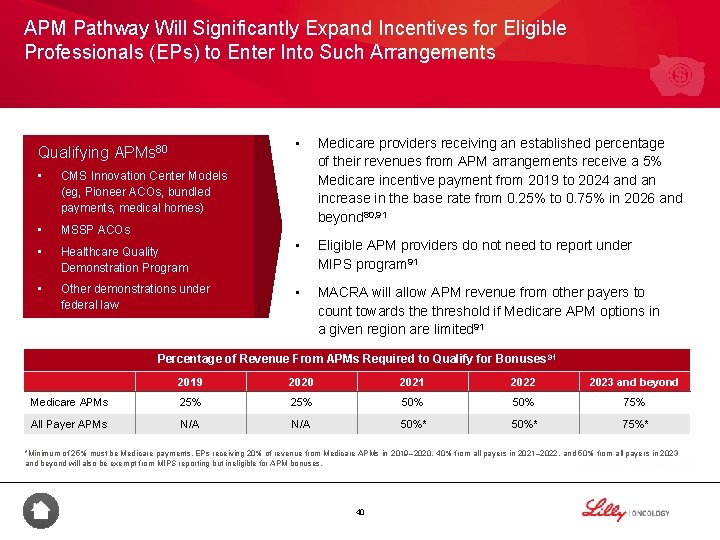
APM Pathway Will Significantly Expand Incentives for Eligible Professionals (EPs) to Enter Into Such Arrangements Qualifying APMs 80 • CMS Innovation Center Models (eg, Pioneer ACOs, bundled payments, medical homes) • MSSP ACOs • Healthcare Quality Demonstration Program • Other demonstrations under federal law • Medicare providers receiving an established percentage of their revenues from APM arrangements receive a 5% Medicare incentive payment from 2019 to 2024 and an increase in the base rate from 0. 25% to 0. 75% in 2026 and beyond 80, 91 • Eligible APM providers do not need to report under MIPS program 91 • MACRA will allow APM revenue from other payers to count towards the threshold if Medicare APM options in a given region are limited 91 Percentage of Revenue From APMs Required to Qualify for Bonuses 91 2019 2020 2021 2022 2023 and beyond Medicare APMs 25% 50% 75% All Payer APMs N/A 50%* 75%* *Minimum of 25% must be Medicare payments. EPs receiving 20% of revenue from Medicare APMs in 2019– 2020, 40% from all payers in 2021– 2022, and 50% from all payers in 2023 and beyond will also be exempt from MIPS reporting but ineligible for APM bonuses. 40
Summary • Moving forward, pay-for-reporting initiatives will soon be replaced with more sophisticated value-based purchasing programs 9, 12, 60, 61, 65, 72 -82 • Many activities now reflect the healthcare environment’s shift from rewarding volume to rewarding value, including measure development, pay for reporting, pay for performance, and payment reform 9 -13, 15, 48, 76, 82, 85 • Payers have noticed the importance of quality performance and have taken steps to include it in their systems by implementing reimbursement initiatives and quality measures with medical groups and hospitals and reporting on physician and practice performance 42, 86 -90 41

Quality Improvement in Oncology 42
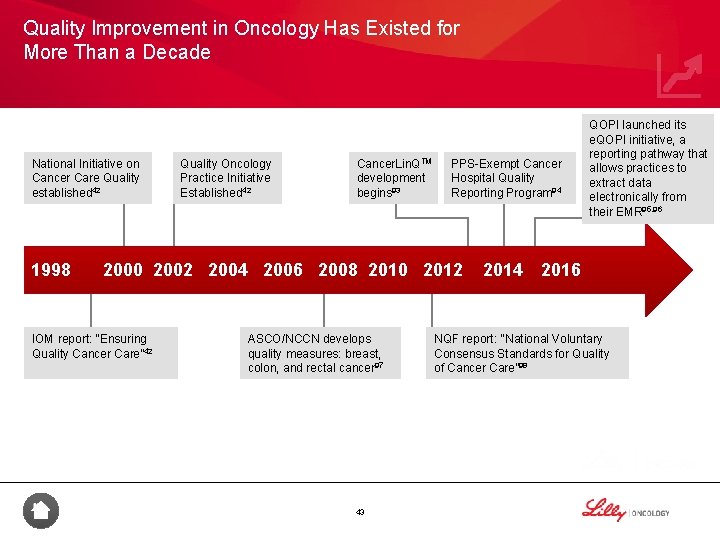
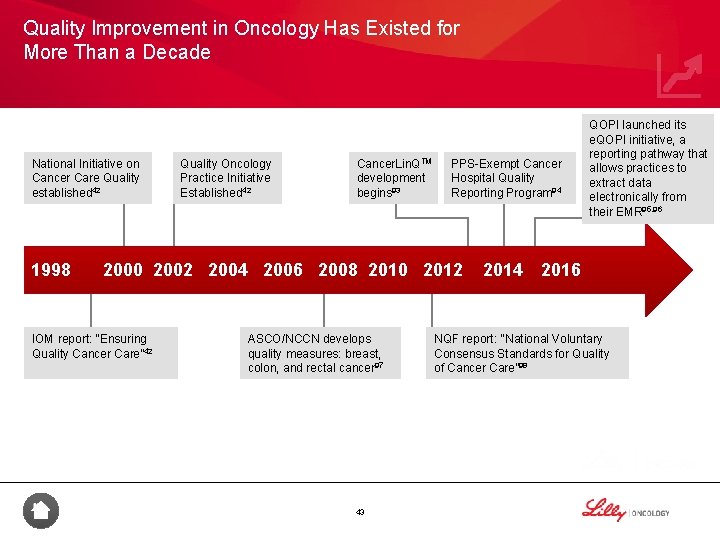
Quality Improvement in Oncology Has Existed for More Than a Decade National Initiative on Cancer Care Quality established 42 1998 Quality Oncology Practice Initiative Established 42 Cancer. Lin. QTM development begins 93 PPS-Exempt Cancer Hospital Quality Reporting Program 94 2000 2002 2004 2006 2008 2010 2012 IOM report: “Ensuring Quality Cancer Care” 42 ASCO/NCCN develops quality measures: breast, colon, and rectal cancer 97 43 QOPI launched its e. QOPI initiative, a reporting pathway that allows practices to extract data electronically from their EMR 95, 96 2014 2016 NQF report: "National Voluntary Consensus Standards for Quality of Cancer Care” 98

Several Organizations Are Involved in Oncology Quality Improvement Organizations That Develop Clinical Guidelines for Oncology 4, 5* Oncology Quality Measures in Public Reporting Programs 4, 99, 100* • CMS Public reporting programs (eg, PQRS, OQR, PCHQR) Use of Oncology Quality Measures to Help Improve Outcomes 77, 87* • United. Healthcare oncology bundle • VBP demonstrations (eg, PGP demo) • ASCO • NCCN Evidence-Based Quality Measures Key Quality Measure Developers in the Oncology Space 4, 6, 7* • • NQF Endorsement Is the Gold Standard for Healthcare Quality 8 ASCO QOPI COA Co. C NCQA STS QIP COA=Community Oncology Alliance; Co. C=Commission on Cancer; NCQA=National Committee for Quality Assurance; STS=Society of Thoracic Surgeons; QIP=Quality Insights of Pennsylvania; PQRS=Physician Quality Reporting System; OQR=Outpatient Quality Reporting Program. *Examples of oncology quality improvement programs/organizations. 44
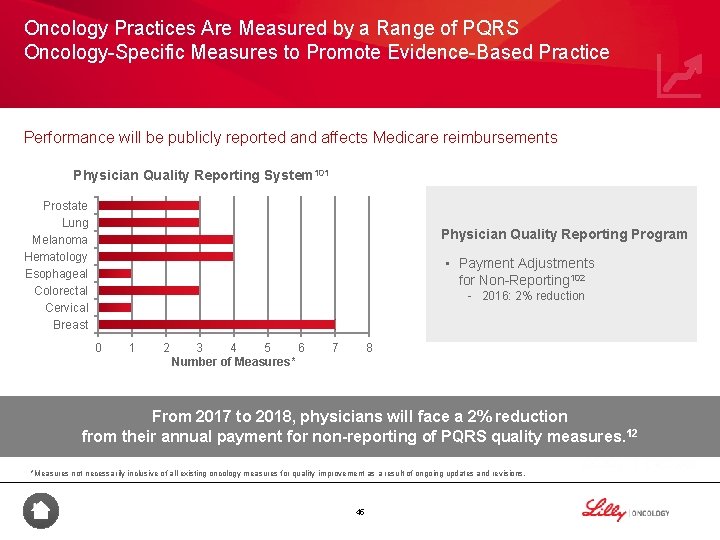
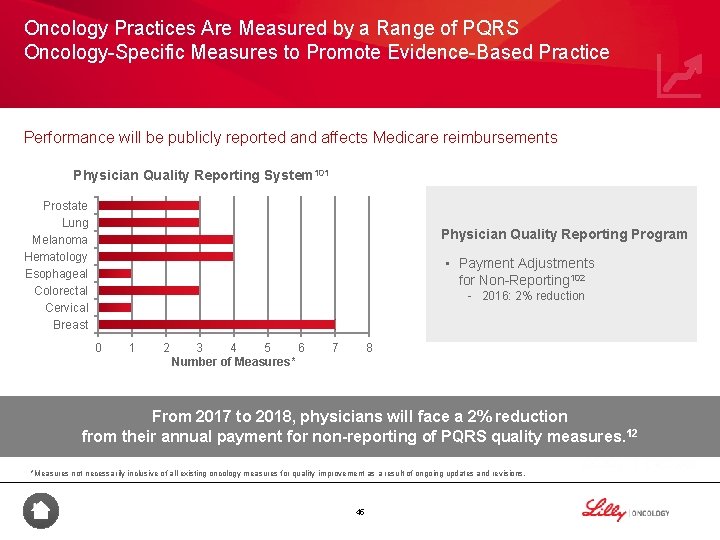
Oncology Practices Are Measured by a Range of PQRS Oncology-Specific Measures to Promote Evidence-Based Practice Performance will be publicly reported and affects Medicare reimbursements Physician Quality Reporting System 101 Prostate Lung Melanoma Hematology Esophageal Colorectal Cervical Breast Physician Quality Reporting Program • Payment Adjustments for Non-Reporting 102 - 2016: 2% reduction 0 1 2 3 4 5 6 Number of Measures* 7 8 From 2017 to 2018, physicians will face a 2% reduction from their annual payment for non-reporting of PQRS quality measures. 12 *Measures not necessarily inclusive of all existing oncology measures for quality improvement as a result of ongoing updates and revisions. 45
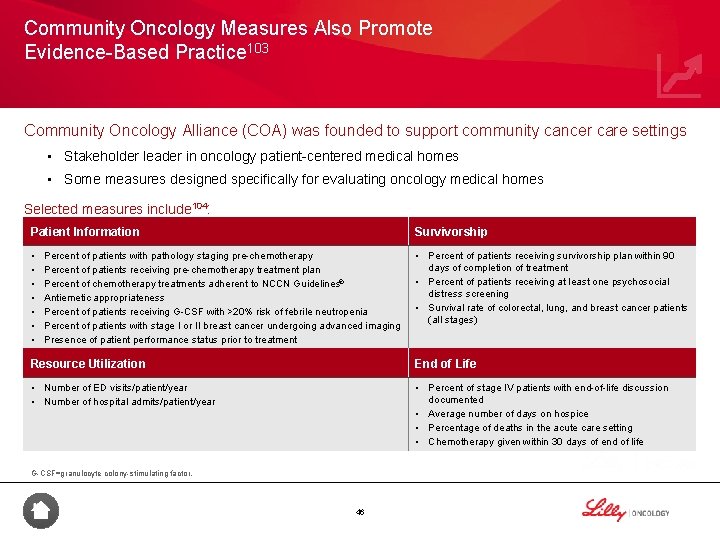
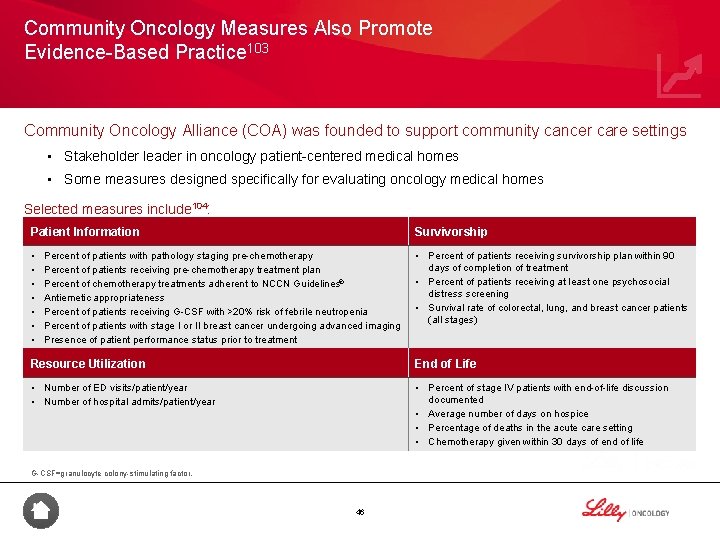
Community Oncology Measures Also Promote Evidence-Based Practice 103 Community Oncology Alliance (COA) was founded to support community cancer care settings • Stakeholder leader in oncology patient-centered medical homes • Some measures designed specifically for evaluating oncology medical homes Selected measures include 104: Patient Information Survivorship • • Percent of patients receiving survivorship plan within 90 days of completion of treatment • Percent of patients receiving at least one psychosocial distress screening • Survival rate of colorectal, lung, and breast cancer patients (all stages) Percent of patients with pathology staging pre-chemotherapy Percent of patients receiving pre-chemotherapy treatment plan Percent of chemotherapy treatments adherent to NCCN Guidelines® Antiemetic appropriateness Percent of patients receiving G-CSF with >20% risk of febrile neutropenia Percent of patients with stage I or II breast cancer undergoing advanced imaging Presence of patient performance status prior to treatment Resource Utilization End of Life • Number of ED visits/patient/year • Number of hospital admits/patient/year • Percent of stage IV patients with end-of-life discussion documented • Average number of days on hospice • Percentage of deaths in the acute care setting • Chemotherapy given within 30 days of end of life G-CSF=granulocyte colony-stimulating factor. 46
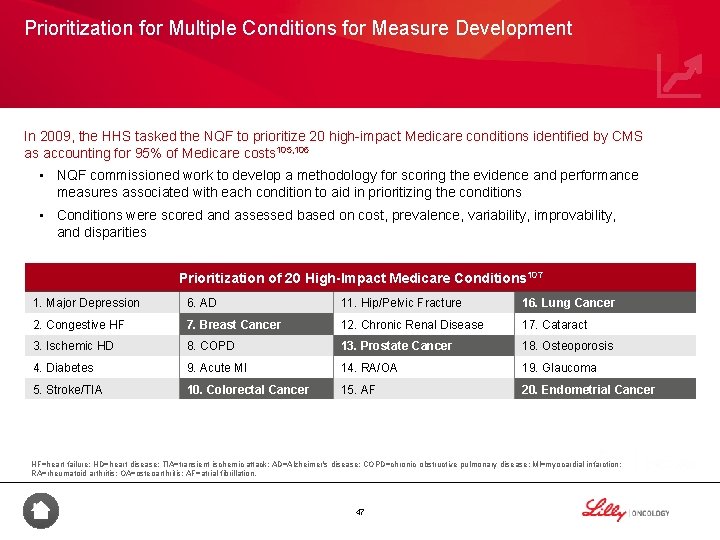
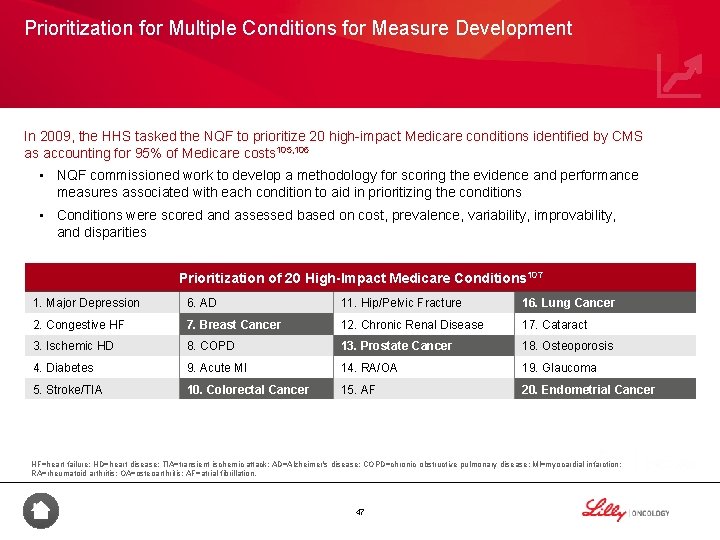
Prioritization for Multiple Conditions for Measure Development In 2009, the HHS tasked the NQF to prioritize 20 high-impact Medicare conditions identified by CMS as accounting for 95% of Medicare costs 105, 106 • NQF commissioned work to develop a methodology for scoring the evidence and performance measures associated with each condition to aid in prioritizing the conditions • Conditions were scored and assessed based on cost, prevalence, variability, improvability, and disparities Prioritization of 20 High-Impact Medicare Conditions 107 1. Major Depression 6. AD 11. Hip/Pelvic Fracture 16. Lung Cancer 2. Congestive HF 7. Breast Cancer 12. Chronic Renal Disease 17. Cataract 3. Ischemic HD 8. COPD 13. Prostate Cancer 18. Osteoporosis 4. Diabetes 9. Acute MI 14. RA/OA 19. Glaucoma 5. Stroke/TIA 10. Colorectal Cancer 15. AF 20. Endometrial Cancer HF=heart failure; HD=heart disease; TIA=transient ischemic attack; AD=Alzheimer's disease; COPD=chronic obstructive pulmonary disease; MI=myocardial infarction; RA=rheumatoid arthritis; OA=osteoarthritis; AF=atrial fibrillation. 47

Case Study: Use of Quality Measures in NSCLC 108 Program Overview Snapshot • Sponsors: The National Cancer Database (NCDB)* (a joint collaboration between the American College of Surgeons and the American Cancer Society) • Sector: Private • Size: Analysis of 8000 eligible NSCLC patients • Timing: 2006– 2011 • Presented at American Association for Thoracic Surgery 96 th Annual Meeting in May 2016 Design Results Conclusion • Four specific quality measures were investigated for eligible patients with Stage IIIA NSCLC who underwent surgery† • Overall median survival for those who did not receive any of the measures, to those who received all 4 measures: • 0 measures: 12. 7 months • 1 measure: 25. 0 months • 2 measures: 31. 4 months • 3 measures: 36. 6 months • 4 measures: 43. 5 months • Despite the benefits of receiving all 4 quality measures as part of patient care, the investigators found that only 12. 8% of individuals with clinical stage IIIA NSCLC received all four interventions • While this study demonstrated that achieving these selected quality measures, both individually and collectively, was associated with improved overall survival, patient, institutional, and tumor factors independently influenced whether patients received these key quality measures *Contains patient, tumor, and treatment data for approximately 70% of cancer patients receiving care at Commission on Cancer–accredited centers. †The four quality measures investigated were neoadjuvant multiagent chemotherapy, lobar (or greater) resection, sampling of at least 10 lymph nodes, and R 0 resection, which means that the tumor has been removed to the extent that the margins are free of cancerous cells. 48

Summary • Since quality became a major theme in health policy, organizations have been shaping how it relates to oncology 42, 93 -98 • Programs and organizations such as the PQRS and the NQF are dedicated to improving quality in the oncology space 12, 101 -103, 105 -107 49
Clinical Pathways in Oncology 50
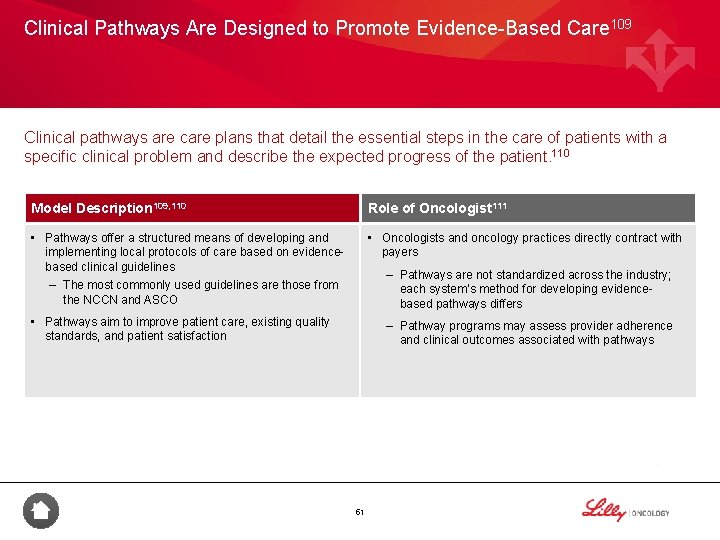
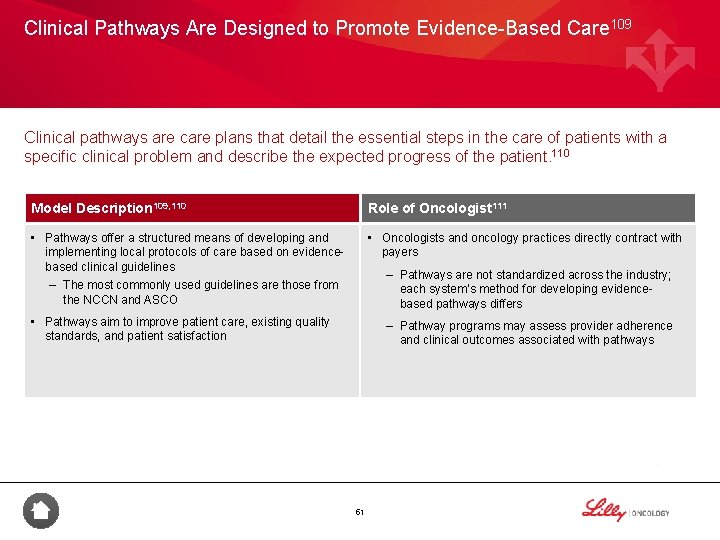
Clinical Pathways Are Designed to Promote Evidence-Based Care 109 Clinical pathways are care plans that detail the essential steps in the care of patients with a specific clinical problem and describe the expected progress of the patient. 110 Model Description 109, 110 Role of Oncologist 111 • Pathways offer a structured means of developing and implementing local protocols of care based on evidencebased clinical guidelines – The most commonly used guidelines are those from the NCCN and ASCO • Oncologists and oncology practices directly contract with payers – Pathways are not standardized across the industry; each system’s method for developing evidencebased pathways differs • Pathways aim to improve patient care, existing quality standards, and patient satisfaction – Pathway programs may assess provider adherence and clinical outcomes associated with pathways 51
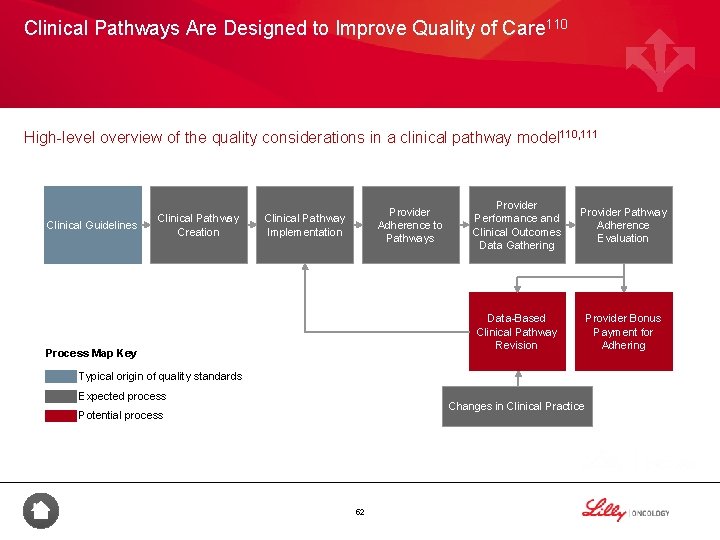
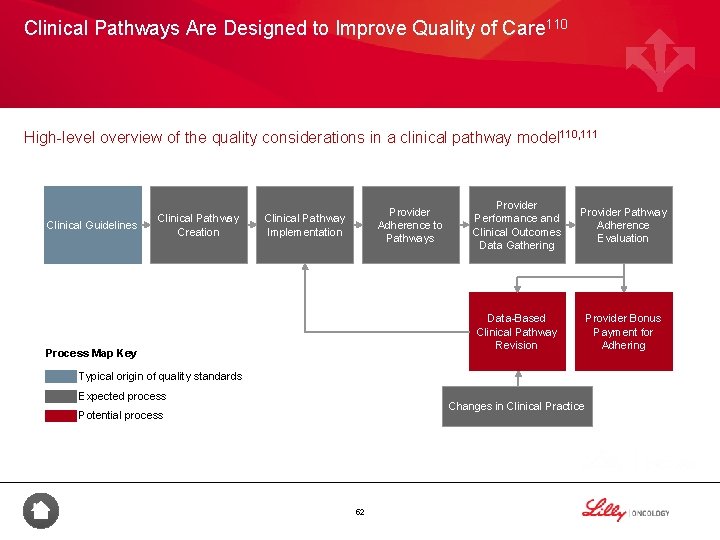
Clinical Pathways Are Designed to Improve Quality of Care 110 High-level overview of the quality considerations in a clinical pathway model 110, 111 Clinical Guidelines Clinical Pathway Creation Provider Adherence to Pathways Clinical Pathway Implementation Process Map Key Provider Performance and Clinical Outcomes Data Gathering Provider Pathway Adherence Evaluation Data-Based Clinical Pathway Revision Provider Bonus Payment for Adhering Typical origin of quality standards Expected process Changes in Clinical Practice Potential process 52

Evolution in the Clinical Pathway Space Legend Partnership/strategy Implementation Endorsement Impact Innovent Oncology (US Oncology/Aetna publish cost savings with equivalent clinical outcomes in NSCLC 112 Acquisition UPMC implements pathways 114 P 4 and Innovent Oncology founded 118, 119 Cancer Care Northwest/Premera Blue Cross report savings due to clinical pathways 121 2005 2006 NSCLC=non-small cell lung cancer. NCCN, US Oncology, and Mc. Kesson announce value pathways collaboration 116 P 4 acquired by Cardinal 115 UPMC founds Via Oncology spinoff 114 2007 Care. First BCBS/P 4 collaboration begins multistate pathways program 122 2008 2009 Care. First BCBS/P 4 report at ASCO cost savings in breast, lung, and colon cancer 113 US Oncology (including Innovent) acquired by Mc. Kesson 119 ITA Partners, an independent decisionsupport provider, changes name to eviti 120 Michigan Oncology Clinical Pathways program launches 123 Indiana Oncology Society endorses Via Oncology 124 2010 Association of Northern California Oncologists endorses pathways and recommends front-end compliance models such as Innovent Oncology and Via Oncology 125, 126 2011 2012 2013 Innovent Oncology/Aetna publish cost savings with equivalent clinical outcomes in colon cancer 127 53 Anthem Blue. Cross Blue. Shield launches its Cancer Care Quality Program 117 Humana partners with New Century Health and Oncology Analytics to administer their Oncology Quality Management Program 117 2014 2015
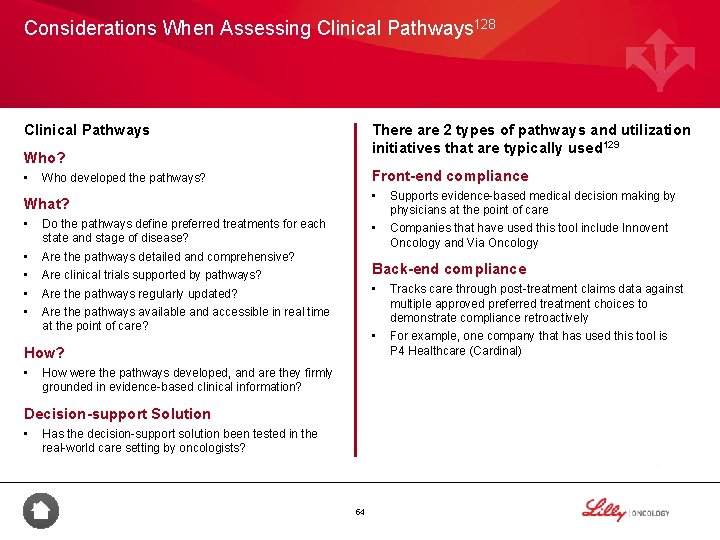
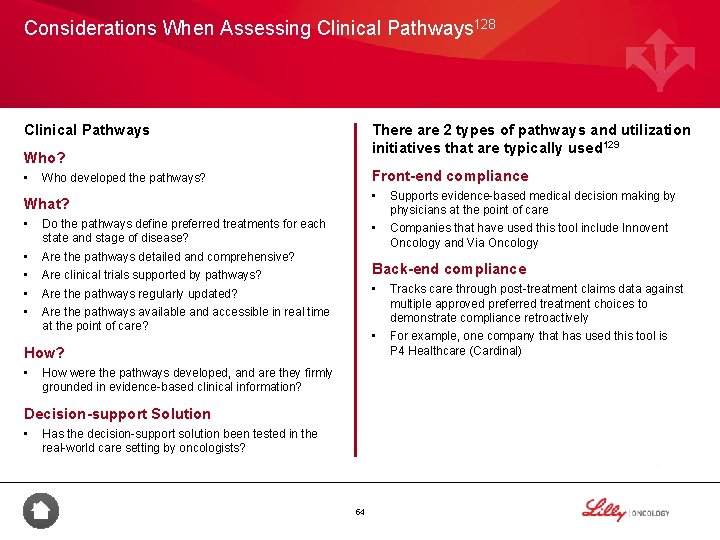
Considerations When Assessing Clinical Pathways 128 Clinical Pathways There are 2 types of pathways and utilization initiatives that are typically used 129 Who? • Front-end compliance Who developed the pathways? What? • Do the pathways define preferred treatments for each state and stage of disease? • • Are the pathways detailed and comprehensive? • Companies that have used this tool include Innovent Oncology and Via Oncology Back-end compliance Are the pathways regularly updated? • Tracks care through post-treatment claims data against multiple approved preferred treatment choices to demonstrate compliance retroactively • For example, one company that has used this tool is P 4 Healthcare (Cardinal) Are the pathways available and accessible in real time at the point of care? How were the pathways developed, and are they firmly grounded in evidence-based clinical information? Decision-support Solution • Supports evidence-based medical decision making by physicians at the point of care Are clinical trials supported by pathways? How? • • Has the decision-support solution been tested in the real-world care setting by oncologists? 54
Summary • Clinical pathways are designed to offer a structured means of developing and implementing local protocols of care, while aiming to improve patient care, existing quality standards, and patient satisfaction 109 -111 – Clinical pathways are often driven by evidence-based guidelines 109 -111 55

Trends in Oncology Quality 56
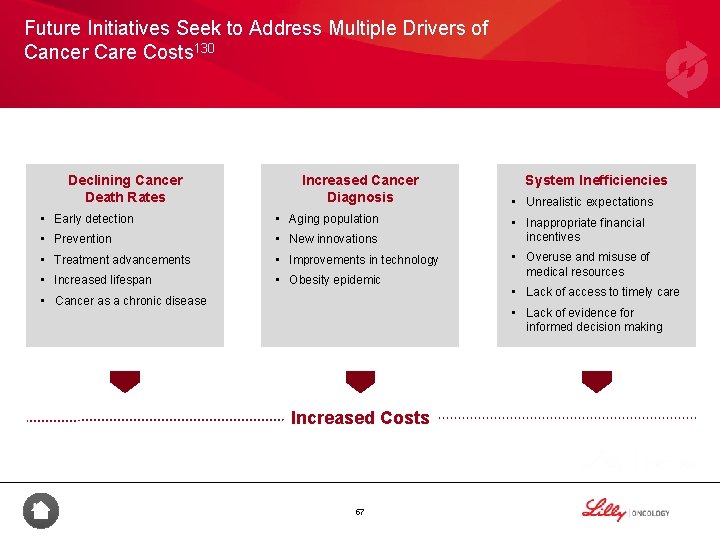
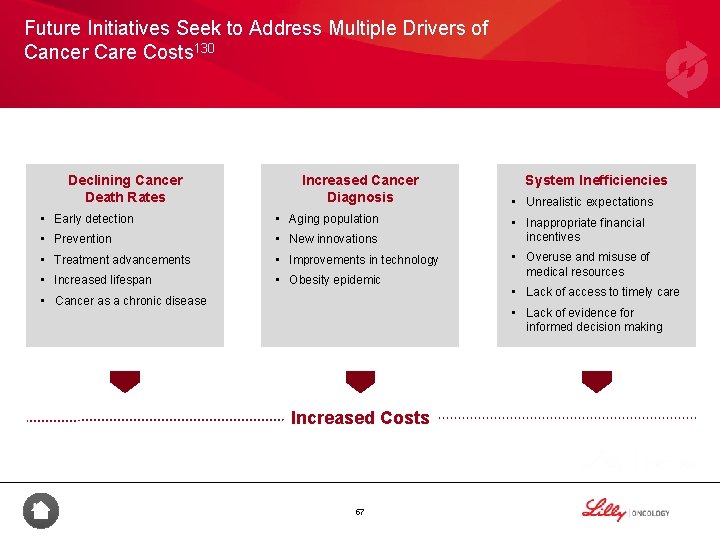
Future Initiatives Seek to Address Multiple Drivers of Cancer Care Costs 130 Declining Cancer Death Rates Increased Cancer Diagnosis • Early detection • Aging population • Prevention • New innovations • Treatment advancements • Improvements in technology • Increased lifespan • Obesity epidemic • Cancer as a chronic disease System Inefficiencies • Unrealistic expectations • Inappropriate financial incentives • Overuse and misuse of medical resources • Lack of access to timely care • Lack of evidence for informed decision making Increased Costs 57

Quality Measurement Programs Will Launch New Measures Designed to Address Gaps 131 Quality measures can be harmonized to streamline reporting efforts and address gaps in cancer care New Measures to Address Gaps • Disease-specific • Appropriateness of care Harmonization of Measures Streamlined Reporting Efforts • Patient outcomes • Next-generation • Quality of care • Unique patient population • Assessment of value in cancer care delivery Harmonization of cancer measures may help reduce reporting burden on providers and address measurement gaps. 58
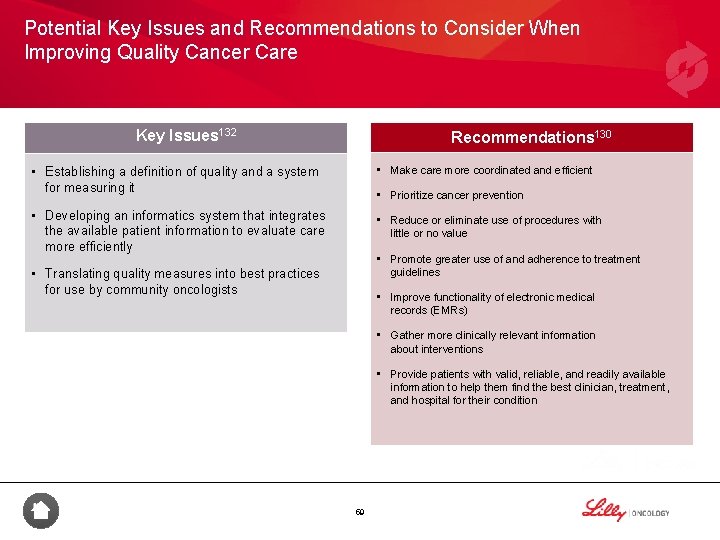
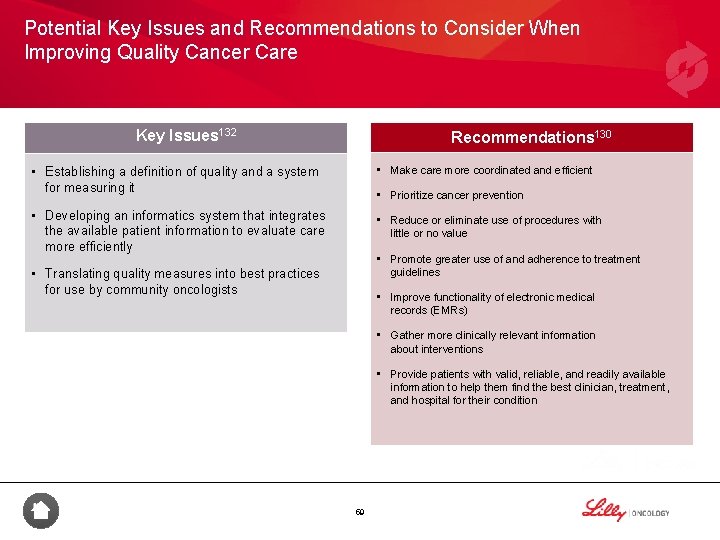
Potential Key Issues and Recommendations to Consider When Improving Quality Cancer Care Key Issues 132 Recommendations 130 • Make care more coordinated and efficient • Establishing a definition of quality and a system for measuring it • Prioritize cancer prevention • Developing an informatics system that integrates the available patient information to evaluate care more efficiently • Reduce or eliminate use of procedures with little or no value • Promote greater use of and adherence to treatment guidelines • Translating quality measures into best practices for use by community oncologists • Improve functionality of electronic medical records (EMRs) • Gather more clinically relevant information about interventions • Provide patients with valid, reliable, and readily available information to help them find the best clinician, treatment, and hospital for their condition 59
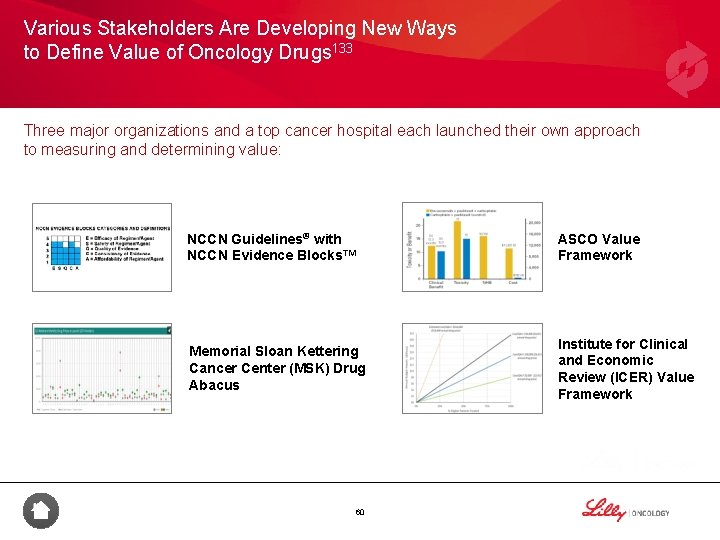
Various Stakeholders Are Developing New Ways to Define Value of Oncology Drugs 133 Three major organizations and a top cancer hospital each launched their own approach to measuring and determining value: NCCN Guidelines® with NCCN Evidence Blocks™ ASCO Value Framework Memorial Sloan Kettering Cancer Center (MSK) Drug Abacus Institute for Clinical and Economic Review (ICER) Value Framework 60

While Their Aim Is to Define Value, the Frameworks Have Disparate Approaches to Design and Intended Use 133 The key parameters used by all organizations to define value are: • Clinical performance • Cost Drug Abacus and ICER include other metrics such as: • Disease burden • Other economic evaluations 4 ASCO NCCN MSK ICER Framework Evidence Blocks Drug Abacus Value Framework Developed as tools to assist the physician and patient in shared decision making Efficacy Evidence Strength Developed as methods to determine a value-based price for drugs Side Effects/Toxicity Treatment Cost to Patient Other Benefits Disease Rarity/ Severity Population Health Burden (QALY) Treatment Duration Economic Evaluations 61
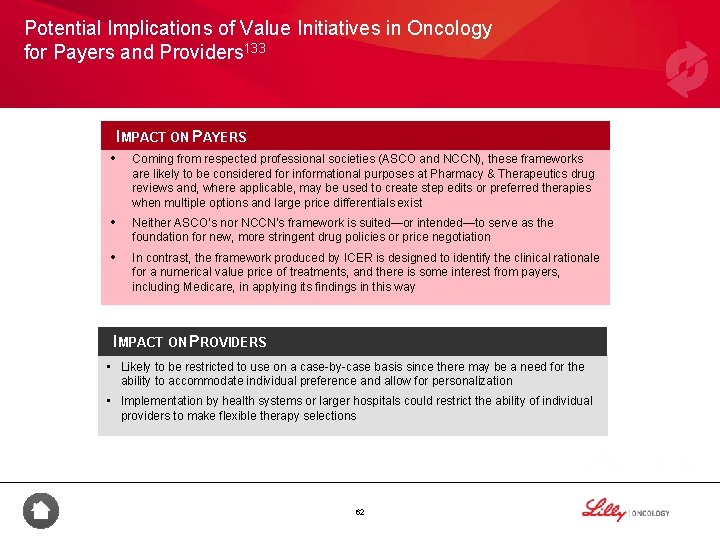
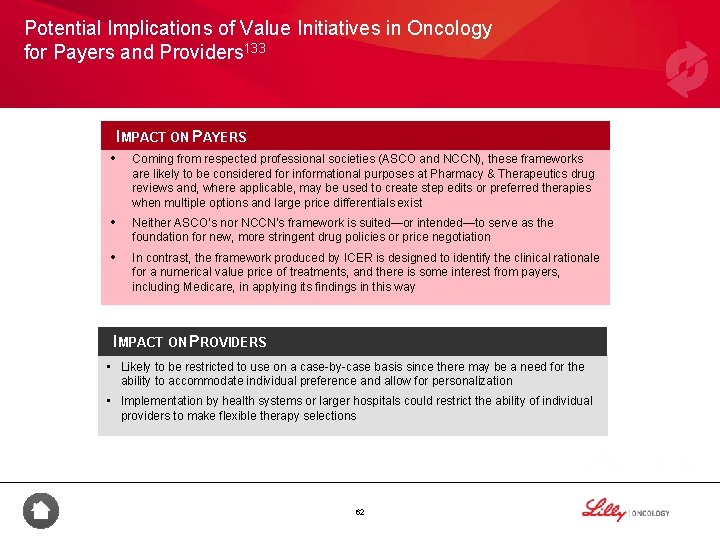
Potential Implications of Value Initiatives in Oncology for Payers and Providers 133 IMPACT ON PAYERS • Coming from respected professional societies (ASCO and NCCN), these frameworks are likely to be considered for informational purposes at Pharmacy & Therapeutics drug reviews and, where applicable, may be used to create step edits or preferred therapies when multiple options and large price differentials exist • Neither ASCO’s nor NCCN’s framework is suited—or intended—to serve as the foundation for new, more stringent drug policies or price negotiation • In contrast, the framework produced by ICER is designed to identify the clinical rationale for a numerical value price of treatments, and there is some interest from payers, including Medicare, in applying its findings in this way IMPACT ON PROVIDERS • Likely to be restricted to use on a case-by-case basis since there may be a need for the ability to accommodate individual preference and allow for personalization • Implementation by health systems or larger hospitals could restrict the ability of individual providers to make flexible therapy selections 62

Summary • Declining cancer death rates, increased cancer diagnoses, and system inefficiencies are driving increased costs in cancer care 130 • Various entities have developed conceptual frameworks for assessing the value of oncology drugs based on varying inputs and metrics 133 • No single tool is likely to emerge as the determiner of value, as stakeholders need multiple characteristics in a value tool, including flexibility in accommodating any mitigating factors that influence value, evidence support for population health decisions, and ability to personalize based on individual preferences 133 • Harmonization of cancer measures may help reduce reporting burden on providers and address measurement gaps 131 • Promoting adherence to treatment guidelines and helping patients to become more engaged in their care some recommended ways to improve the quality of cancer care 130 63
Appendix A: Additional Information on Quality Measures 64
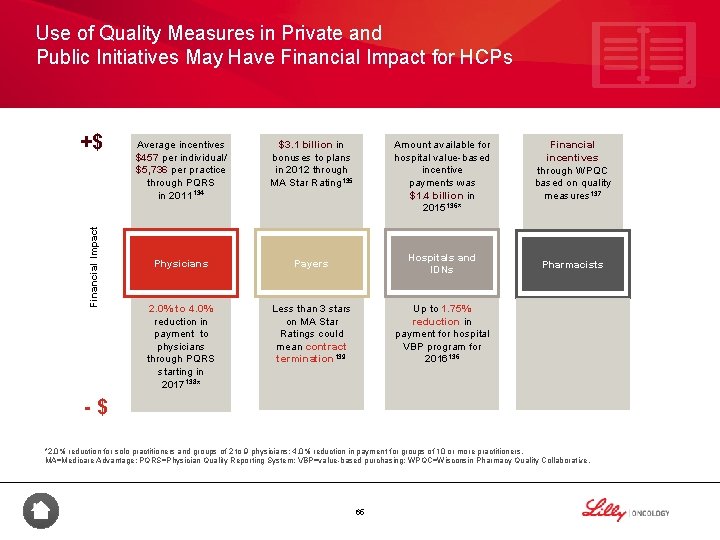
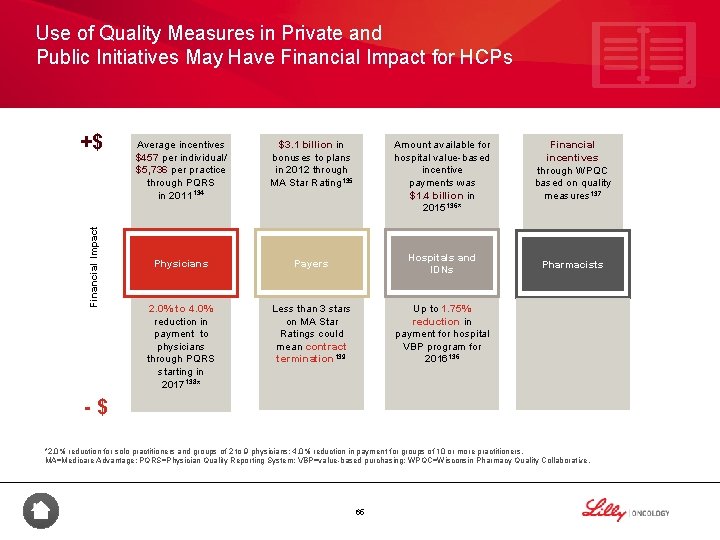
Use of Quality Measures in Private and Public Initiatives May Have Financial Impact for HCPs Financial Impact +$ Average incentives $457 per individual/ $5, 736 per practice through PQRS in 2011134 $3. 1 billion in bonuses to plans in 2012 through MA Star Rating 135 Physicians Payers Hospitals and IDNs 2. 0% to 4. 0% reduction in payment to physicians through PQRS starting in 2017138* Less than 3 stars on MA Star Ratings could mean contract termination 139 Up to 1. 75% reduction in payment for hospital VBP program for 2016136 Amount available for hospital value-based incentive payments was $1. 4 billion in 2015136* Financial incentives through WPQC based on quality measures 137 Pharmacists -$ *2. 0% reduction for solo practitioners and groups of 2 to 9 physicians; 4. 0% reduction in payment for groups of 10 or more practitioners. MA=Medicare Advantage; PQRS=Physician Quality Reporting System; VBP=value-based purchasing; WPQC=Wisconsin Pharmacy Quality Collaborative. 65

HHS Has Stated a Commitment to Increase Payment Linked to Quality to 90% by 2018 HHS Recently Announced Goals to Increase the Percentage of FFS Payments That Are Linked to Quality or Alternative Payment Models Over the Coming Years 140, 141 Goals Historical Performance 2016 2011 2014 2018 0% 22% 30% 50% 68% 85% 90% Alternative payment models FFS linked to quality All Medicare FFS=fee-for-service; HHS=US Department of Health and Human Services. 66
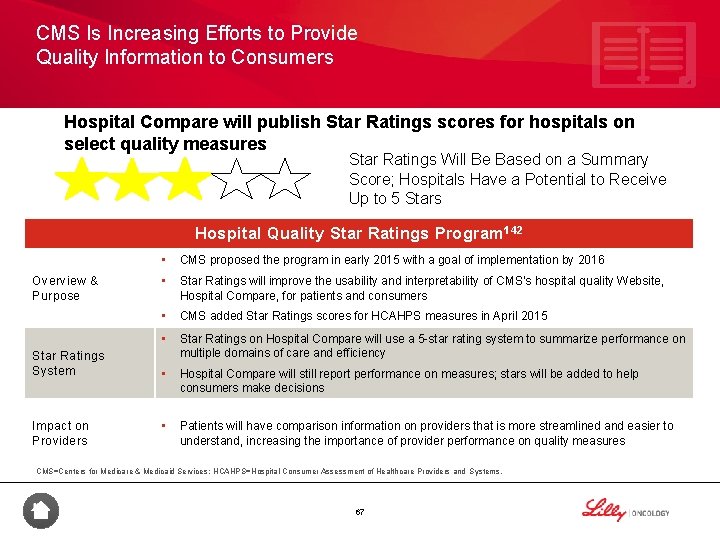
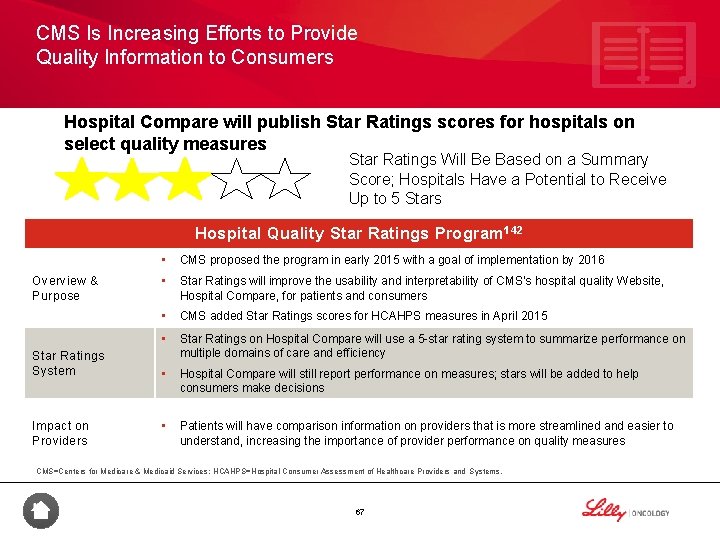
CMS Is Increasing Efforts to Provide Quality Information to Consumers Hospital Compare will publish Star Ratings scores for hospitals on select quality measures Star Ratings Will Be Based on a Summary Score; Hospitals Have a Potential to Receive Up to 5 Stars Hospital Quality Star Ratings Program 142 Overview & Purpose Star Ratings System Impact on Providers • CMS proposed the program in early 2015 with a goal of implementation by 2016 • Star Ratings will improve the usability and interpretability of CMS’s hospital quality Website, Hospital Compare, for patients and consumers • CMS added Star Ratings scores for HCAHPS measures in April 2015 • Star Ratings on Hospital Compare will use a 5 -star rating system to summarize performance on multiple domains of care and efficiency • Hospital Compare will still report performance on measures; stars will be added to help consumers make decisions • Patients will have comparison information on providers that is more streamlined and easier to understand, increasing the importance of provider performance on quality measures CMS=Centers for Medicare & Medicaid Services; HCAHPS=Hospital Consumer Assessment of Healthcare Providers and Systems. 67
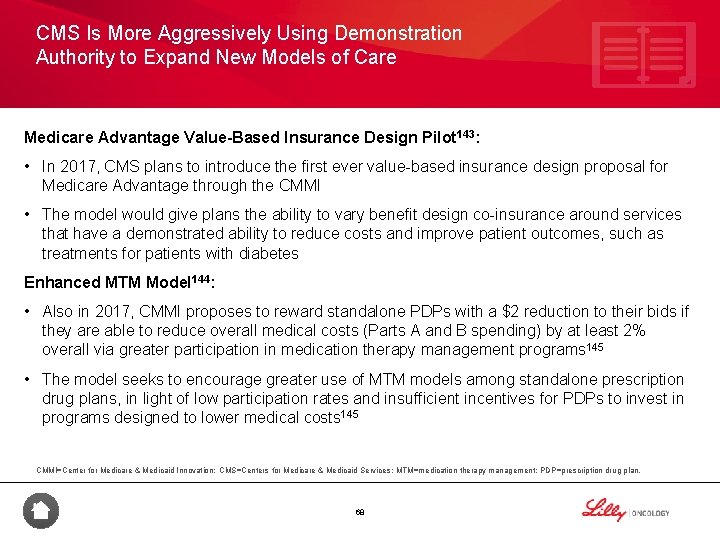
CMS Is More Aggressively Using Demonstration Authority to Expand New Models of Care Medicare Advantage Value-Based Insurance Design Pilot 143: • In 2017, CMS plans to introduce the first ever value-based insurance design proposal for Medicare Advantage through the CMMI • The model would give plans the ability to vary benefit design co-insurance around services that have a demonstrated ability to reduce costs and improve patient outcomes, such as treatments for patients with diabetes Enhanced MTM Model 144: • Also in 2017, CMMI proposes to reward standalone PDPs with a $2 reduction to their bids if they are able to reduce overall medical costs (Parts A and B spending) by at least 2% overall via greater participation in medication therapy management programs 145 • The model seeks to encourage greater use of MTM models among standalone prescription drug plans, in light of low participation rates and insufficient incentives for PDPs to invest in programs designed to lower medical costs 145 CMMI=Center for Medicare & Medicaid Innovation; CMS=Centers for Medicare & Medicaid Services; MTM=medication therapy management; PDP=prescription drug plan. 68
Appendix B: CMS Quality Reporting Programs 69
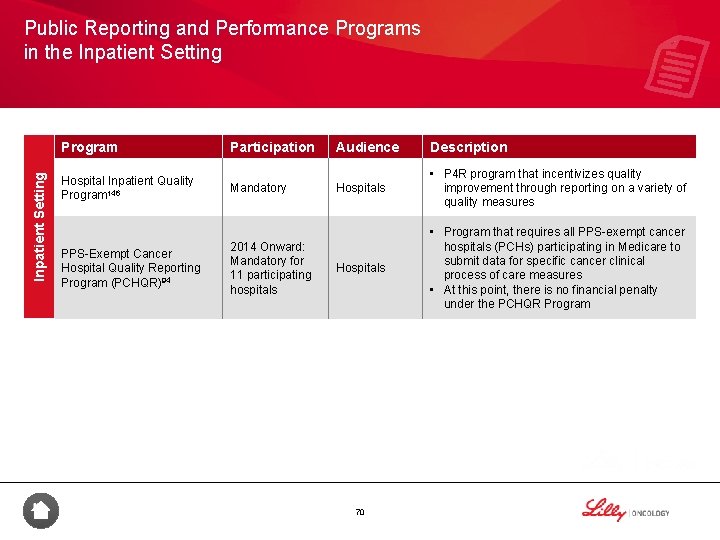
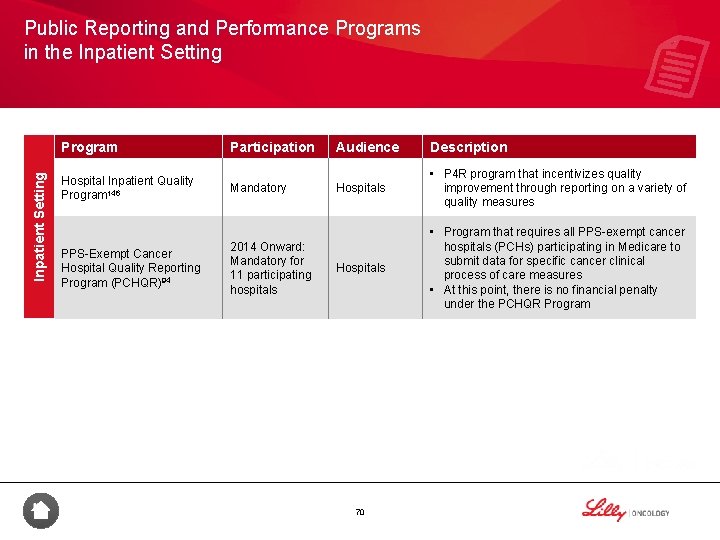
Public Reporting and Performance Programs in the Inpatient Setting Program Participation Hospital Inpatient Quality Program 146 Mandatory PPS-Exempt Cancer Hospital Quality Reporting Program (PCHQR)94 2014 Onward: Mandatory for 11 participating hospitals Audience Description Hospitals • P 4 R program that incentivizes quality improvement through reporting on a variety of quality measures Hospitals • Program that requires all PPS-exempt cancer hospitals (PCHs) participating in Medicare to submit data for specific cancer clinical process of care measures • At this point, there is no financial penalty under the PCHQR Program 70
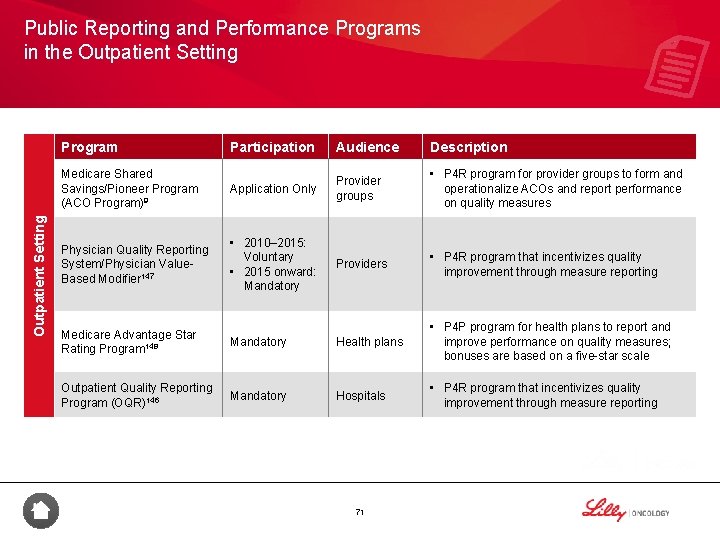
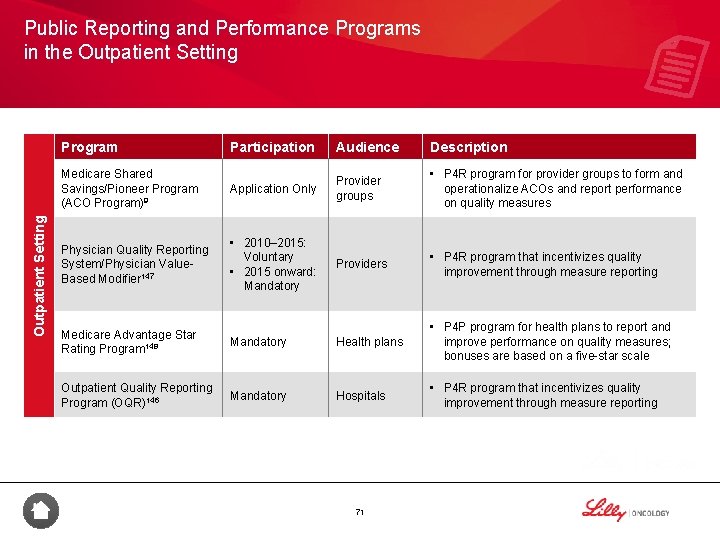
Public Reporting and Performance Programs in the Outpatient Setting Program Participation Audience Description Medicare Shared Savings/Pioneer Program (ACO Program)9 Application Only Provider groups • P 4 R program for provider groups to form and operationalize ACOs and report performance on quality measures Physician Quality Reporting System/Physician Value. Based Modifier 147 • 2010– 2015: Voluntary • 2015 onward: Mandatory Providers • P 4 R program that incentivizes quality improvement through measure reporting Medicare Advantage Star Rating Program 148 Mandatory Health plans • P 4 P program for health plans to report and improve performance on quality measures; bonuses are based on a five-star scale Outpatient Quality Reporting Program (OQR)146 Mandatory Hospitals • P 4 R program that incentivizes quality improvement through measure reporting 71

Public Reporting and Performance Programs in the Outpatient Setting Program Medicaid Adult Core Set 149 Participation Voluntary Audience Description • As of January 2014, state data on the adult quality measures became part of the Secretary’s annual report on the quality of State Medicaid care for adults enrolled in Medicaid program • In December 2015, updated 2016 Adult Core Set was released Ambulatory Surgical Center Quality Reporting Program (ASCQR)150 Mandatory Ambulatory surgical centers 72 • P 4 R program that incentivizes quality improvement through measure reporting

Appendix C: References 73

References 1. Brown ML, Lipscomb J, Snyder C. The burden of illness of cancer: economic cost and quality of life. Annu Rev Public Health. 2001; 22: 91113. 2. Mc. Kesson. Value-based reimbursement vs. volume-based care. http: //www. mckesson. com/population-health-management/populationhealth/know-the-challenges/. Accessed July 5, 2016. 3. American Society of Clinical Oncology. ASCO in Action. http: //www. asco. org/advocacy-policy/asco-in-action/oncology-practice-front-andcenter-national-payment-reform-debate. Published January 27, 2013. Accessed July 18, 2016. 4. American Society of Clinical Oncology. The state of cancer care in America: 2016: a report by the American Society of Clinical Oncology. http: //jop. ascopubs. org/content/12/4/339. full. pdf+html. Accessed June 24, 2016. 5. National Comprehensive Cancer Network. NCCN ® categories of evidence and consensus. http: //www. nccn. org/professionals/physician_gls/categories_of_consensus. asp. Accessed June 24, 2016. 6. The Society of Thoracic Surgeons. Quality performance measures. http: //www. sts. org/quality-research-patient-safety/qualityperformance-measures. Accessed June 24, 2016. 7. Quality Insights of Pennsylvania. About us. http: //www. qipa. org/About-Us. aspx. Accessed June 24, 2016. 8. National Quality Forum. Measuring performance. http: //www. qualityforum. org/Measuring_Performance. aspx. Accessed September 8, 2016. 9. Centers for Medicare & Medicaid Services. Shared Savings Program. https: //www. cms. gov/Medicare-Fee-for-Service. Payment/sharedsavingsprogram/. Accessed June 24, 2016. 10. Centers for Medicare & Medicaid Services. Hospital value-based purchasing. https: //www. cms. gov/Medicare/Quality-initiatives-patientassessment-instruments/hospital-value-based-purchasing/index. html. Last updated October 30, 2015. Accessed June 24, 2016. 74
References 11. Centers for Medicare & Medicaid Services. Hospital Inpatient Quality Reporting program. https: //www. cms. gov/Medicare/Quality-Initiatives. Patient-Assessment-Instruments/Hospital. Quality. Inits/Hospital. RHQDAPU. html. Last updated September 13, 2013. Accessed June 24, 2016. 12. Centers for Medicare & Medicaid Services. Payment adjustment information. https: //www. cms. gov/Medicare/Quality-Initiatives-Patient. Assessment-Instruments/PQRS/Payment-Adjustment-Information. html. Accessed July 18, 2016. 13. National Quality Forum. Performance measurement coordination strategy for PPS-exempt cancer hospitals. http: //www. qualityforum. org/Publications/2012/06/MAP_Cancer_Hospitals_Final_Report. aspx. Published June 2012. Accessed July 18, 2016. 14. Spinks T, Ganz PA, Sledge GW Jr, et al. Delivering high-quality cancer care: the critical role of quality measurement. Health (Amst). 2014; 2(1): 53 -62. 15. Centers for Medicare & Medicaid Services. Analysis and payment. http: //www. cms. gov/Medicare/Quality-Initiatives-Patient-Assessment. Instruments/PQRS/Analysis. And. Payment. html. Accessed June 24, 2016. Avalere Health, LLC. Clinical Pathways: Overview of Current Practices and Potential Implications for Patients, Payers, and Providers. http: //avalere-health-production. s 3. amazonaws. com/uploads/pdfs/1438002728_AH_Pathways_final. pdf. Published July 2015. Accessed September 22, 2016. 17. Wingo PA, Tong T, Bolden S. Cancer statistics, 1995. CA Cancer J Clin. 1995; 45(1): 8 -30. 18. American Cancer Society. Cancer facts & figures 2016. http: //www. cancer. org/acs/groups/content/@research/documents/document/acspc 047079. pdf. Accessed September 8, 2016. 19. Erikson C, Salsberg E, Forte G, et al. Future supply and demand for oncologists: challenges to assuring access to oncology services. J Oncol Pract. 2007; 3(2): 79 -86. http: //www. ncbi. nlm. nih. gov/pmc/articles/PMC 2793740/pdf/jop 79. pdf. Accessed September 8, 2016. 20. American Society of Clinical Oncology. Workforce initiatives. http: //www. asco. org/practice-guidelines/cancer-care-initiatives/workforceinitiatives. Accessed July 18, 2016. 75
References 21. National Cancer Institute. Progress & trends: decreased mortality, increased survival rates. http: //www. cancer. gov/aboutnci/budget/plan/progress. Accessed August 11, 2016. 22. De Moor JS, Mariotto AB, Parry C, et al. Cancer survivors in the United States: prevalence across the survivorship trajectory and implications for care. Cancer Epidemiol Biomarkers Prev. 2013; 22(4): 561 -570. 23. Personalized Medicine Coalition. Personalized medicine by the numbers. http: //www. personalizedmedicinecoalition. org/Userfiles/PMCCorporate/file/pmc_personalized_medicine_by_the_numbers. pdf. Accessed September 9, 2016. 24. Personalized Medicine Coalition. 2015 Progress Report. Personalized Medicine at FDA. http: //www. personalizedmedicinecoalition. org/Userfiles/PMC-Corporate/file/2015_Progress_Report_PM_at_FDA. pdf. Accessed August 26, 2016. 25. American Cancer Society. Cancer treatment & survivorship facts & figures. 2016 -2017. http: //www. cancer. org/acs/groups/content/@research/documents/document/acspc-048074. pdf. Accessed July 18, 2016. 26. Mariotto AB, Yabroff KR, Shao Y, et al. Projections of the cost of cancer care in the united states: 2010 -2020. J Natl Cancer Inst. 2011; 103(2): 117 -128. 27. American Cancer Society. Cancer facts & figures 2008. http: //www. cancer. org/acs/groups/content/@nho/documents/document/2008 cafffinalsecuredpdf. Accessed September 8, 2016. 28. Miller HD. From volume to value: better ways to pay for health care. Health Affairs. 2009: 28(5): 1418 -1428. 29. Institute of Medicine. Delivering high-quality cancer care. https: //www. nationalacademies. org/hmd/~/media/Files/Report%20 Files/2013/Quality-Cancer-Care/qualitycancercare_rb. pdf. Published September 2013. Accessed July 18, 2016. 30. AHC Media. They’re Back! Once Out of Favor, Clinical Pathways Are Surging. http: //www. ahcmedia. com/articles/134515 -theyre-backclinical-pathways-are-in-favor-again. Published February 14, 2015. Accessed August 15, 2016. 76
References 31. Institute of Medicine. Crossing the quality chasm: a new health system for the 21 st century. http: //www. nap. edu/catalog/10027. html. Washington, DC: National Academy Press; 2001. 32. American College of Medical Quality. Definition of clinical quality improvement. http: //www. acmq. org/policies 1 and 2. pdf. Accessed July 18, 2016. 33. Agency for Healthcare Research and Quality. Understanding quality measurement. http: //www. ahrq. gov/professionals/quality-patientsafety/quality-resources/tools/chtoolbx/understand/index. html. Accessed September 8, 2016. 34. Anumula N, Sanelli PC. Physician quality reporting system. AJNR Am J Neuroradiol. 2011; 32(11): 2000 -2001. 35. National Quality Forum. NQF’s history. https: //www. qualityforum. org/about_nqf/history/. Accessed July 18, 2016. 36. Institute of Medicine. Preventing medication errors. http: //www. nationalacademies. org/hmd/~/media/Files/Report%20 Files/2006/Preventing. Medication-Errors-Quality-Chasm-Series/medicationerrorsnew. ashx. Published July 2006. Accessed July 18, 2016. 37. Agency for Healthcare Research and Quality. The national quality strategy (NQS). http: //www. ahrq. gov/workingforquality/. Accessed July 18, 2016. 38. Congress. gov. Medicare access and CHIP reauthorization act of 2015. https: //www. congress. gov/bill/114 th-congress/house-bill/2/text/pl. Accessed June 24, 2016. 39. National Priorities Partnership. National priorities and goals: aligning our efforts to transform America’s healthcare. Washington, DC: National Quality Forum; 2008. http: //www. qualityforum. org/Work. Area/linkit. aspx? Link. Identifier=id&Item. ID=70345. Accessed September 8, 2016. 40. National Academies. Vital signs: core metrics for health and health care progress. www. nationalacademies. org/hmd/Reports/2015/Vital-Signs. Core-Metrics. aspx. Published April 28, 2015. Accessed July 18, 2016. 41. Institute of Medicine. To err is human: building a safer health system. http: //www. nationalacademies. org/hmd/~/media/Files/Report % 20 Files/1999/To-Err-is-Human/To%20 Err%20 is%20 Human%201999%20%20 report%20 brief. pdf. Published November 1999. Accessed August 19, 2016. 77
References 42. Blayney DW, Stella PJ, Ruane T, et al. Partnering with payers for success: quality oncology practice initiative, Blue Cross Blue Shield of Michigan, and the Michigan Oncology Quality Consortium. J Oncol Pract. 2009; 5(6): 281 -284. 43. Centers for Medicare & Medicaid Services. Report to Congress: plan to implement a Medicare hospital value-based purchasing program. http: //www. cms. gov/Medicare-Fee-for-Service. Payment/Acute. Inpatient. PPS/downloads/Hospital. VBPPlan. RTCFINALSUBMITTED 2007. pdf. Published November 21, 2007. Accessed July 18, 2016. 44. National Quality Forum. MAP pre-rulemaking report: 2013 recommendations under consideration by HHS. http: //www. qualityforum. org/Work. Area/linkit. aspx? Link. Identifier=id&Item. ID=72738. Published February 2013. Accessed July 18, 2016. 45. Centers for Medicare & Medicaid Services. CMS and major commercial health plans, in concert with physician groups and other stakeholders, announce alignment and simplification of quality measures. https: //www. cms. gov/Newsroom/Media. Release. Database/Pressreleases/2016 -Press-releases-items/2016 -02 -16. html. Published February 16, 2016. Accessed June 24, 2016. 46. Centers for Medicare & Medicaid Services. Core Measures. https: //www. cms. gov/Medicare/Quality-Initiatives-Patient-Assessment. Instruments/Quality. Measures/Core-Measures. html. Updated February 16, 2016. Accessed June 24, 2016. 47. Agency for Healthcare Research and Quality. President’s advisory commission on consumer protection and quality in the health care industry. http: //archive. ahrq. gov/hcqual/. Accessed July 18, 2016. 48. The Patient Protection and Affordable Care Act. Public Law 111 -148, 124 Stat 119 (2010). http: //www. gpo. gov/fdsys/pkg/BILLS 111 hr 3590 enr/pdf/BILLS-111 hr 3590 enr. pdf. Accessed July 18, 2016. 49. US Department of Health and Human Services. About healthy people. http: //www. healthypeople. gov/2020/about/default. aspx. Accessed July 18, 2016. 50. Agency for Healthcare Research and Quality. 2011 Report to Congress: National strategy for quality improvement in health care. http: //www. ahrq. gov/workingforquality/nqs 2011 annlrpt. htm. Accessed July 18, 2016. 78
References 51. Institute for Healthcare Improvement. The IHI triple aim. http: //www. ihi. org/Engage/Initiatives/Triple. Aim/Pages/default. aspx. Accessed July 18, 2016. 52. Institute for Healthcare Improvement. Triple aim—concept design. http: //www. ihi. org/Engage/Initiatives/Triple. Aim/Documents/Concept. Design. pdf. Accessed July 18, 2016. 53. Agency for Healthcare Research and Quality. Varieties of measures in NQMC. https: //www. qualitymeasures. ahrq. gov/help-andabout/summaries/varieties-of-measures-in-nqmc. Accessed July 18, 2016. 54. Medicare. gov. Linking quality to payment. https: //www. medicare. gov/hospitalcompare/linking-quality-to-payment. html. Accessed August 15, 2016. 55. Agency for Healthcare Research and Quality. Uses of quality measures. https: //www. qualitymeasures. ahrq. gov/help-and-about/qualitymeasure-tutorials/uses-of-quality-measures. Accessed July 18, 2016. 56. National Quality Forum. Measure evaluation criteria. http: //www. qualityforum. org/docs/measure_evaluation_criterias. aspx. Accessed September 8, 2016. 57. National Quality Forum. Building high value health systems: the role of performance measurement & HIT. http: //www. amrpa. org/uploads/docuploads/Building%20 High%20 Value%20%20 Health%20 Systems%20 Janet%20 Corrigan. pdf. Accessed July 18, 2016. 58. Centers for Medicare & Medicaid Services. CMS Quality Strategy 2016. https: //www. cms. gov/medicare/quality-initiatives-patient-assessment -instruments/qualityinitiativesgeninfo/downloads/cms-quality-strategy. pdf. Accessed August 15, 2016. 59. Center for American Progress. Alternatives to fee-for-service payments in health care. http: //cdn. americanprogress. org/wpcontent/uploads/2012/09/Feefor. Service-1. pdf. Accessed July 18, 2016. 60. American Public Health Association. Major Affordable Care Act delivery and payment reforms. https: //www. apha. org/~/media/files/pdf/topics/aca/delivery_reforms_table_apha_oct 2013. ashx. Published October 2013. Accessed July 18, 2016. 79
References 61. Centers for Medicare & Medicaid Services. Innovation Models. https: //innovation. cms. gov/initiatives/#views=models. Accessed August 15, 2016. 62. Valence Health. Models of Value-Based Reimbursement. http: //valencehealth. com/uploads/default/Valence_Health_Models_of_Value. Based_Reimbursement_White_Paper. pdf. Published 2013. Accessed August 15, 2016. 63. Journal of Oncology Practice. A JOP webinar: alternative payment models in oncology. http: //jop. ascopubs. org/site/misc/docs/JOP_payment_reform_webinar_slides. pdf. December 9, 2015. Accessed June 24, 2016. 64. Cancer Center Business Development. Barkley R. Oncology Payment Reform: What’s In and What’s Out? https: //www. accccancer. org/ossn_network/TX/presentations/Tx. SCO-Fall 2015 -Barkley. pdf. Published September 12, 2015. Accessed September 22, 2016. 65. Centers for Medicare & Medicaid Services. Oncology care model overview and application process. https: //innovation. cms. gov/Files/slides/OCMintro. pdf. Published February 19, 2015. Accessed June 24, 2016. 66. Centers for Medicare & Medicaid Services. Oncology care model. https: //innovation. cms. gov/initiatives/Oncology-Care/. Updated July 13, 2016. Accessed June 24, 2016. 67. Centers for Medicare & Medicaid Services. Oncology care model. https: //www. cms. gov/Newsroom/Media. Release. Database/Factsheets/2015 -Fact-sheets-items/2015 -02 -12. html. Accessed July 18, 2016. 68. Centers for Medicare & Medicaid Services. Oncology care model (OCM) request for applications (RFA). https: //innovation. cms. gov/Files/x/ocmrfa. pdf. Updated June 3, 2015. Accessed August 15, 2016. 69. Centers for Medicare & Medicaid Services. CMS Manual System. https: //www. cms. gov/Regulations-and. Guidance/Transmittals/Downloads/R 139 DEMO. pdf. Published February 11, 2016. Accessed August 15, 2016. 70. Centers for Medicare & Medicaid Services. OCM Performance-based Payment Methodology. https: //innovation. cms. gov/Files/x/ocmmethodology. pdf. Published June 27, 2016. Accessed August 16, 2016. 80
References 71. Boston Healthcare Associates. Florida Blue Cross. http: //bostonhealthcare. com/wp-content/uploads/2014/03/Florida-Blue-Oncology. ACO. pptx. Accessed September 22, 2016. 72. Centers for Medicare & Medicaid Services. Nursing home value-based purchasing demonstration. https: //www. cms. gov/Medicare/Demonstration-Projects/Demo. Projects. Eval. Rpts/downloads/nhp 4 p_opendoor. pdf. Accessed July 19, 2016. 73. National Business Coalition on Health Care Purchaser Toolkit: Hospital-acquired condition payment policy. http: //www. nbch. org/nbch/files/cc. Library. Files/Filename/00001630/HAC%20 Payment%20 Policy%20 Toolkit%20%28 final%20 version%2 9%20081109. pdf. Published Aug. 2009. Accessed July 19, 2016. 74. Centers for Medicare & Medicaid Services. CMS implements value-based purchasing for dialysis facilities. http: //www. cms. gov/Newsroom/Media. Release. Database/Press-Releases/2010 -Press-Releases-Items/2010 -12 -29. html. Published December 29, 2010. Accessed July 19, 2016. 75. Centers for Medicare & Medicaid Services. Value-based payment modifier. http: //www. cms. gov/Medicare-Fee-for-Service. Payment/Physician. Feedback. Program/Value. Based. Payment. Modifier. html. Accessed July 19, 2016. 76. Centers for Medicare & Medicaid Services. Premier hospital quality incentive demonstration: rewarding superior quality care. http: //www. cms. gov/Medicare/Quality-Initiatives-Patient-Assessment. Instruments/Hospital. Quality. Inits/Downloads/Hospital. Premier. Press. Release-Fact. Sheet. pdf. Published December 2011. Accessed July 19, 2016. 77. Centers for Medicare & Medicaid Services. Medicare physician group practice demonstration. https: //www. cms. gov/Medicare/Demonstration -Projects/Demo. Projects. Eval. Rpts/downloads/PGP_Fact_Sheet. pdf. July 2011. Accessed July 19, 2016. 78. Centers for Medicare & Medicaid Services. CMS announces sites for a demonstration to encourage greater collaboration and improve quality using bundled hospital payments [press release]. http: //www. cms. gov/Medicare/Demonstration. Projects/Demo. Projects. Eval. Rpts/downloads/ACEPress. Release. pdf. Published Jan. 6, 2009. Accessed July 20, 2016. 79. Centers for Medicare & Medicaid Services. Next generation accountable care organization model (NGACO Model). https: //www. cms. gov/Newsroom/Media. Release. Database/Fact-sheets/2016 -Fact-sheets-items/2016 -01 -11. html. January 11, 2016. Accessed August 11, 2016. 81
References 80. American College of Physicians. MACRA, MIPS, and APMs – What to except from all these acronyms. https: //www. acponline. org/meetingscourses/courses-recordings/leadership-academy/macra-mips-apms. Updated March 2, 2016. Accessed June 24, 2016. 81. American Academy of Orthopaedic Surgeons. Physician quality reporting system (PQRS). http: //www. aaos. org/Quality/Performance_Measures/Physician_Quality_Reporting_System_(PQRS)/? ssopc=1. Accessed July 20, 2016. 82. Healthcare Financial Management Association. Value in health care: current state and future directions. http: //www. hfma. org/Work. Area/linkit. aspx? Link. Identifier=id&Item. ID=5220. Accessed August 19, 2016. 83. Centers for Medicare & Medicaid Services. Summary of 2015 Physician Value-based Payment Modifier Policies. https: //www. cms. gov/Medicare-Fee-for-Service. Payment/Physician. Feedback. Program/Downloads/CY 2015 Value. Modifier. Policies. pdf. Accessed August 29, 2016. 84. Saignite. 10 FAQs about VBM and the impacts of PQRS reporting. http: //www. saignite. com/resources/10 -faqs-about-pqrs-and-the-valuebased-payment-modifier. Accessed August 29, 2016. 85. Blue Cross Blue Shield of Massachusetts. The alternative QUALITY contract. http: //www. bluecrossma. com/visitor/pdf/alternative-qualitycontract. pdf. Published May 2010. Accessed July 20, 2016. 86. Goozner M. United Healthcare, five oncology practices try bundled payments. JNCI. 2011; 103(1): 8 -10. 87. United. Healthcare. Cancer care payment program pilot key facts. http: //graphics 8. nytimes. com/ref/business/UHCCancer. Care. Program. pdf. Accessed July 25, 2016. 88. Health. ACE. Aetna: And US Oncology Introduce Innovent Oncology Program to Promote Evidence-Based Guidelines, Specialized Patient Care and Efficiency in Cancer Treatment. http: //oncology. healthace. com/052010/Oncology_Report_052010_S 8. pdf. Accessed September 8, 2016. 89. American Society of Clinical Oncology. Blue Cross Blue Shield of Michigan first health plan to provide reimbursement for participation in QOPI [editorial]. J Oncol Pract. 2008; 4(6): 287 -288. http: //www. ncbi. nlm. nih. gov/pmc/articles/PMC 2793918/pdf/jop 287. pdf. Accessed September 8, 2016. 82
References 90. AIS. Anthem cancer pathways program rewards network docs for high-quality cancer care. http: //www. aimspecialtyhealth. com/Resources/documents/inthenews/Cancer. Pathways. Program. Rewards. Docs-AISReport. May 2015. pdf. Published May 2015. Accessed July 5, 2016. 91. Avalere Policy 360. Focus Report: H. R. 2 – Medicare Access and CHIP Reauthorization Act of 2015. http: //policy 360. avalere. com/wpcontent/uploads/2015/04/20150421 -Policy-360 -Focus-Report-SGR-Repeal-Bill_Revised. pdf. Published March 27, 2015. Accessed July 25, 2016. 92. Centers for Medicare & Medicaid Services. Quality Payment Program. https: //www. cms. gov/Medicare/Quality-Initiatives-Patient-Assessment -Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/NPRM-QPP-Fact-Sheet. pdf. Accessed September 22, 2016. 93. American Society of Clinical Oncology. ASCO launches formal development of Cancer. Lin. Q™, a learning health system to transform cancer care and improve outcomes for patents [press release]. http: //www. asco. org/about-asco/press-center/news-releases/asco-launches-formaldevelopment-cancerlinq%E 2%84%A 2 -learning-health. Published November 12, 2013. Accessed July 25, 2016. 94. Quality. Net. PPS-exempt Cancer Hospital Quality Reporting (PCHQR) program overview. https: //qualitynet. org/dcs/Content. Server? cid= 1228772356060&pagename=Qnet. Public%2 FPage%2 FQnet. Tier 2&c=Page. Accessed September 8, 2016. 95. ASCO Institute for Quality. e. QOPI Measures. http: //www. instituteforquality. org/qopi/eqopi-measures. Accessed August 16, 2016. 96. American Society of Clinical Oncology. RE: CMS-3310 -FC & CMS-3311 -FC. Medicare and Medicaid Programs; Electronic Health Record Incentive Program – Stage 3 and Modifications to Meaningful Use in 2015 through 2017. http: //www. asco. org/sites/newwww. asco. org/files/content-files/blog-release/documents/2015 -meaningful-use-3 -comments. pdf. Published December 15, 2015. Accessed August 16, 2016. 97. Desch CE, Mc. Niff KK, Schneider EC, et al. American Society of Clinical Oncology/National Comprehensive Cancer Network quality measures. J Clin Oncol. 2008; 26(21): 3631 -3637. 98. National Quality Forum. National voluntary consensus standards for quality of cancer care [abstract]. http: //www. qualityforum. org/Work. Area/linkit. aspx? Link. Identifier=id&Item. ID=22020. Published May 2009. Accessed July 25, 2016. 83
References 99. Quality. Net. Hospital Outpatient Quality Reporting (OQR) program overview. https: //www. qualitynet. org/dcs/Content. Server? c=Page&pagename=Qnet. Public%2 FPage%2 FQnet. Tier 2&cid=1191255879384. Accessed July 25, 2016. 100. Quality Reporting Center. PPS-Exempt Cancer Hospital Quality Reporting (PCHQR) Program. http: //www. qualityreportingcenter. com/inpatient/pch/. Accessed September 8, 2016. 101. Centers for Medicare & Medicaid Services. 2014 Physician Quality Reporting System (PQRS) measures list. https: //www. acponline. org/system/files/documents/running_practice/payment_coding/pqrs/2014_pqrs_measure_list. pdf. Published December 13, 2013. Accessed September 8, 2016. 102. Centers for Medicare & Medicaid Services. 2013 Physician Quality Reporting System (PQRS): 2015 PQRS payment adjustment. http: //www. cms. gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/PQRS/Downloads/2013_PQRS 2015_Payment. Adjustment. Tip. Sheet 060313. pdf. Published June 2013. Accessed July 25, 2016. 103. Community Oncology Alliance. Oncology Medical Home Initiative. http: //www. medicalhomeoncology. org/User. Files/COA_Oncology_Medical_Home_Initiative_9 -21 -12. pdf. Updated September 21, 2012. Accessed September 22, 2016. 104. Oncology Medical Home. http: //www. medicalhomeoncology. org/User. Files/OMHMeasures 111015 v 2. pdf. Updated November 10, 2015. Accessed June 24, 2016. 105. National Quality Forum. Consensus-based entities regarding healthcare performance measurement. https: //www. qualityforum. org/About_NQF/HHS_Performance_Measurement. aspx. Accessed July 25, 2016. 106. National Quality Forum. Measure Prioritization Advisory Committee report: prioritization of high-impact Medicare conditions and measure gaps. http: //www. qualityforum. org/Work. Area/linkit. aspx? Link. Identifier=id&Item. ID=71009. Published May 2010. Accessed July 25, 2016. 107. National Archives and Records Administration. Department of Health and Human Services: secretarial review and publication of the annual report to Congress submitted by the contracted consensus-based entity regarding performance measurement. Federal Register. 2013; 78(148): 46696 -46731. https: //www. gpo. gov/fdsys/pkg/FR-2013 -08 -01/pdf/FR-2013 -08 -01. pdf. Accessed September 8, 2016. 84
References 108. Science. Daily. Stage IIIA non-small cell lung cancer survival rates improved when care includes four specific quality measures. https: //www. sciencedaily. com/releases/2016/05/160516103323. htm. Accessed August 18, 2016. 109. Forringer J. Approaching the clinical pathways movement with an objective eye and the potential for improvement in end-of-life care. Managed Care Oncol. 2010; 4(4): 15 -19. http: //www. niahealthcare. com/media/257881/finalmco-improving%20 value_q 410. pdf. Accessed September 8, 2016. 110. Campbell H, Hotchkiss R, Bradshaw N, Porteous M. Integrated care pathways. BMJ. 1998; 316(7125): 133 -137. 111. Gesme DH, Wiseman M. Strategic use of clinical pathways. J Oncol Pract. 2011; 7(1): 54 -56. 112. Neubauer MA, Hoverman R, Kolodziej M, et al. Cost effectiveness of evidence-based treatment guidelines for the treatment of non-smallcell lung cancer in the community setting. J Oncol Pract. 2010; 6(1): 12 -18. 113. Koeller JM, Kreys E. Second-year results of the first large-scale, multistate BCBS clinical oncology pathway program. J Clin Oncol. 2012; (suppl; abstract e 16552). 114. Brufsky A, Lokay K, Mc. Donald M. Driving evidence-based standardization of care within a framework of personalized medicine. Am Soc Clin Oncol Educ Book. 2012: e 62 -e 65. 115. Pittsburgh Business Times. Highmark chooses P 4 Healthcare to develop cancer treatment protocols. http: //www. bizjournals. com/pittsburgh/print-edition/2010/11/19/highmark-p 4 -healthcare-cancer-treatment. html. Published November 19, 2010. Accessed July 25, 2016. 116. Mc. Kesson. The NCCN, The US Oncology Network and Mc. Kesson Specialty Health Collaborate to Offer New Value Pathways for Cancer Care. http: //www. mckesson. com/about-mckesson/newsroom/press-releases/2012/the-nccn--the-us-oncology-network-and-mckessonspecialty-health-collaborate-to-offer-new-value-pathways-for-cancer-care/. Published November 29, 2012. Accessed July 25, 2016. 117. Wong W. The evolution of clinical pathways for oncology. Journal of Clinical Pathways. 2015; 1(1): 37 -42. http: //www. journalofclinicalpathways. com/evolution-clinical-pathways-oncology. Accessed September 8, 2016. 85

References 118. Cardinal. Health. Highmark selects P 4 healthcare to help physicians improve quality, outcomes, cost-effectiveness of oncology care. http: //s 1. q 4 cdn. com/238390398/files/doc_news/2010/CAH_News_2010_11_11_General_Releases. pdf. Published November 11, 2010. Accessed July 25, 2016. 119. Mc. Kesson completes acquisition of US Oncology. http: //www. mckesson. com/about-mckesson/newsroom/pressreleases/2010/mckesson-completes-acquisition-of-us-oncology/. Published December 30, 2010. Accessed July 25, 2016. 120. Eviti. ITA Partners Becomes eviti, Inc. http: //www. eviti. com/cancer_care/news-releases/ita-partners-eviti-inc-aligning-company-marketleading-oncology-decision-support-platform/. Published January 17, 2012. Accessed July 25, 2016. 121. Puget Sound Business Journal. Neurath P. Clinic reports big savings from standardized care. http: //www. bizjournals. com/seattle/stories/2006/09/25/story 10. html. Published September 24, 2006. Accessed July 25, 2016. 122. Carlson B. Controlling the cost of care through clinical pathways. Biotechnol Healthc. 2009; 6(1): 23 -26. 123. Michigan Oncology Clinical Treatment Pathways Program. Pathways. http: //mioncologypathways. com/pathways/. Accessed July 25, 2016. 124. Via Oncology. Indiana University Health aims to transform cancer care with Via Oncology Pathways [press release]. http: //www. viaoncology. com/admin/uploads/iuh_via_pathways. pdf. Published August 1, 2012. Accessed July 25, 2016. 125. Association of Northern California Oncologists. ANCO’s Payer Provider Partnership Strategy. http: //www. anco-online. org/P 3. html. Accessed July 25, 2016. 126. Butcher L. State oncology groups advance clinical pathways. Oncology Times. 2011; 33(16): 14 -16. 127. Hoverman JR, Cartwright TH, Patt DA, et al. Pathways, outcomes, and costs in colon cancer: retrospective evaluations in two distinct databases. J Oncol Pract. 2011; 7(3 suppl): 52 s-59 s. 128. Ellis PG. All pathways are not created equal. Onc Times. 2010; 32(10). 86
References 129. Holcombe D. Oncology management programs for payers and physicians: evaluating current models and diagnosing successful strategies for payers and physicians. J Oncol Pract. 2011; 7(3 Suppl): e 46 s-e 49 s. 130. Balogh E, Patlak M, Nass SL; Institute of Medicine of the National Academies. Delivering affordable cancer care in the 21 st century: workshop summary. Washington, DC: National Academies Press; 2013. 131. National Quality Forum. Endorsement summary: cancer measures. http: //www. qualityforum. org/Work. Area/linkit. aspx? Link. Identifier=id&Item. ID=72130. Published October 2012. Accessed July 25, 2016. 132. American Society of Clinical Oncology. Organizations collaborate to improve the quality of cancer care. J Oncol Pract. 2006; 2(3): 116 -119. http: //www. ncbi. nlm. nih. gov/pmc/articles/PMC 2794585/pdf/jop 116. pdf. Accessed September 8, 2016. 133. Green M, Dipaula K. Kantar Health. The path toward drug value definition: implications of value initiatives in oncology. http: //www. kantarhealth. com/docs/white-papers/the-path-toward-drug-value-definition-implications-of-value-initiatives-in- oncology. pdf. Published March 2016. Accessed August 30, 2016. 134. Centers for Medicare & Medicaid Services. 2012 Reporting Experience. http: //www. cms. gov/Medicare/Quality-Initiatives-Patient. Assessment-Instruments/PQRS/Downloads/2012 -PQRS-and-e. Rx-Experience-Report. zip. Accessed April 14, 2016. 135. Kaiser Family Foundation. Medicare Advantage Plan Star Ratings and Bonus Payments in 2012. http: //www. kff. org/medicare/upload/8257. pdf. Accessed April 14, 2016. 136. Centers for Medicaid & Medicare Services. FY 2015 Inpatient Prospective Payment System Final Rule. Federal Register. Volume 79. No. 163. August 2014. Accessed April 14, 2016. 137. Business Wire. Mc. Kesson to launch Medication Therapy Management Pilo Program. http: //www. businesswire. com/news/home/20070709005505/en/Mc. Kesson-Launch-Medication-Therapy-Management-Pilot-Program. Accessed April 21, 2016. 138. Centers for Medicaid & Medicare Services. Changes for the Physician Value-based Payment Modifier in the CY 2015. https: //www. cms. gov/Newsroom/Media. Release. Database/Fact-sheets/2014 -Fact-sheets-items/2014 -10 -31 -5. html? Accessed August 29, 2016. 87
References 139. Centers for Medicaid & Medicare Services. Announcement of calendar year (CY) 2016 Medicare Advantage capitation rates and Medicare Advantage and Part D payment policies and final call letter. Published April 6, 2015. https: //www. cms. gov/medicare/healthplans/medicareadvtgspecratestats/downloads/announcement 2016. pdf. Accessed April 13, 2016. 140. Adapted from slide presented at Healthcare Information and Management Systems Society Annual Conference & Exhibition by Kate Goodrich, MD, MHS, Centers for Medicare & Medicaid Services. https: //www. cms. gov/Regulations-and. Guidance/Legislation/EHRIncentive. Programs/Downloads/HIMSS 16_101 MIPSListening. Session. pdf. Accessed April 21, 2016. 141. US Department of Health and Human Services. Better, smarter, healthier: In historic announcement, HHS sets clear goals and timeline for shifting Medicare reimbursements from volume to value. Published January 26, 2015. http: //www. hhs. gov/news/press/2015 pres/01/20150126 a. html. Accessed April 14, 2016. 142. Centers for Medicaid & Medicare Services. Hospital Compare Star Ratings Fact Sheet. Published April 16, 2015. www. cms. gov/Newsroom/Media. Release. Database/Fact-sheets/2015 -Fact-sheets-items/2015 -04 -16. html. Accessed April 14, 2016. 143. Centers for Medicaid & Medicare Services. Medicare Advantage Value-Based Insurance Design Model. https: //www. cms. gov/Newsroom/Media. Release. Database/Fact-sheets/2015 -Fact-sheets-items/2015 -09 -01. html. Accessed April 14, 2016. 144. Centers for Medicaid & Medicare Services. Medicare Announces Part D Enhanced Medication Therapy Management Model. https: //www. cms. gov/Newsroom/Media. Release. Database/Press-releases/2015 -Press-releases-items/2015 -09 -28. html. Accessed April 14, 2016. 145. Centers for Medicaid & Medicare Services. Part D Enhanced Medication Therapy Management (MTM) Model Test. https: //innovation. cms. gov/Files/slides/enhancedmtm-introslides. pdf. Accessed April 30, 2016. 146. Centers for Medicare & Medicaid Services. CMS Hospital Outpatient Quality Reporting program. https: //www. cms. gov/Medicare/Quality. Initiatives-Patient-Assessment-Instruments/Hospital. Quality. Inits/Hospital. Outpatient. Quality. Reporting. Program. html. Accessed July 25, 2016. 147. Centers for Medicare & Medicaid Services. Physician Quality Reporting System (PQRS) overview. http: //www. cms. gov/Medicare/Quality. Initiatives-Patient-Assessment-Instruments/PQRS/Downloads/PQRS_Overview. Fact. Sheet_2013_08_06. pdf. Accessed July 25, 2016. 88
References 148. Kaiser Family Foundation. Medicare Advantage plan star ratings and bonus payments in 2012. http: //kaiserfamilyfoundation. files. wordpress. com/2013/01/8257. pdf. Published November 2011. Accessed July 25, 2016. 149. Centers for Medicare & Medicaid Services. Core set of health care quality measures for Medicaid (adult core set). http: //www. medicaid. gov/Medicaid-CHIP-Program-Information/By-Topics/Quality-of-Care/Downloads/Medicaid-Adult-Core-Set. Manual. pdf. Published June 2016. Accessed July 25, 2016. 150. Centers for Medicare & Medicaid Services. ASC quality reporting. http: //cms. hhs. gov/Medicare/Quality-Initiatives-Patient-Assessment. Instruments/ASC-Quality-Reporting/index. html. Accessed July 25, 2016. 89
 Vbpm orthopaedic
Vbpm orthopaedic Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập điện thế nghỉ
điện thế nghỉ 101012 bằng
101012 bằng Dot
Dot Thế nào là sự mỏi cơ
Thế nào là sự mỏi cơ Chúa yêu trần thế
Chúa yêu trần thế Phản ứng thế ankan
Phản ứng thế ankan Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan Tia chieu sa te
Tia chieu sa te Công thức tính độ biến thiên đông lượng
Công thức tính độ biến thiên đông lượng Một số thể thơ truyền thống
Một số thể thơ truyền thống Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Sơ đồ cơ thể người
Sơ đồ cơ thể người Thế nào là số nguyên tố
Thế nào là số nguyên tố đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Môn thể thao bắt đầu bằng từ đua
Môn thể thao bắt đầu bằng từ đua Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể ưu thế lai là gì
ưu thế lai là gì Thẻ vin
Thẻ vin Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Tư thế ngồi viết
Tư thế ngồi viết Cái miệng nó xinh thế
Cái miệng nó xinh thế Chó sói
Chó sói Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Tư thế ngồi viết
Tư thế ngồi viết Thế nào là giọng cùng tên? *
Thế nào là giọng cùng tên? * Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Ng-html
Ng-html Sự nuôi và dạy con của hươu
Sự nuôi và dạy con của hươu đại từ thay thế
đại từ thay thế Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Diễn thế sinh thái là
Diễn thế sinh thái là Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Tư thế worm breton
Tư thế worm breton Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Lời thề hippocrates
Lời thề hippocrates Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Bổ thể
Bổ thể Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Pediatric oncology branch
Pediatric oncology branch Vall d'hebron institute of oncology
Vall d'hebron institute of oncology George kannourakis oncology
George kannourakis oncology Oncology nurse burnout
Oncology nurse burnout Clinicaloptions com oncology
Clinicaloptions com oncology Funds flow model
Funds flow model Nrg oncology meeting
Nrg oncology meeting Medicare oncology care model
Medicare oncology care model Smith integrative oncology
Smith integrative oncology Dr raymond wynn radiation oncology
Dr raymond wynn radiation oncology Oncology
Oncology Unc pediatric hematology oncology fellowship
Unc pediatric hematology oncology fellowship Pediatric board review course
Pediatric board review course Southmead oncology
Southmead oncology Pico question
Pico question Denali oncology group alaska
Denali oncology group alaska Sdtm oncology domains
Sdtm oncology domains Macmillan acute oncology
Macmillan acute oncology Feasible interesting novel ethical relevant
Feasible interesting novel ethical relevant Oncology haematology helpline triage tool
Oncology haematology helpline triage tool Oncology triage tool
Oncology triage tool Umkc hematology oncology fellowship
Umkc hematology oncology fellowship Ucla radiation oncology westwood
Ucla radiation oncology westwood Rad onc job market
Rad onc job market Ukons
Ukons Premier oncology hematology management society
Premier oncology hematology management society Pumberton sign
Pumberton sign Sachs immuno oncology bd&l and investment forum
Sachs immuno oncology bd&l and investment forum Oncology triage tool
Oncology triage tool Lurbinectedin posologie
Lurbinectedin posologie Ohc oncology
Ohc oncology Hematology wikipedia
Hematology wikipedia Oncology nursing management in cancer care
Oncology nursing management in cancer care Wisconsin oncology network
Wisconsin oncology network Tu domain sdtm
Tu domain sdtm 20092006 color
20092006 color Minimal common oncology data elements
Minimal common oncology data elements Reflexology for cancer
Reflexology for cancer Odac oncology
Odac oncology Dr saleh oncology
Dr saleh oncology Bogardus radiation oncology billing
Bogardus radiation oncology billing Unit 3 abbreviations medical terminology
Unit 3 abbreviations medical terminology Toby talbot oncology
Toby talbot oncology Putting evidence into practice
Putting evidence into practice Bmc oncology department
Bmc oncology department Via oncology epic
Via oncology epic Connective tissue oncology society
Connective tissue oncology society