Current State of Surgical Training William Allum Chair






- Slides: 41

Current State of Surgical Training William Allum Chair, Joint Committee of Surgical Training
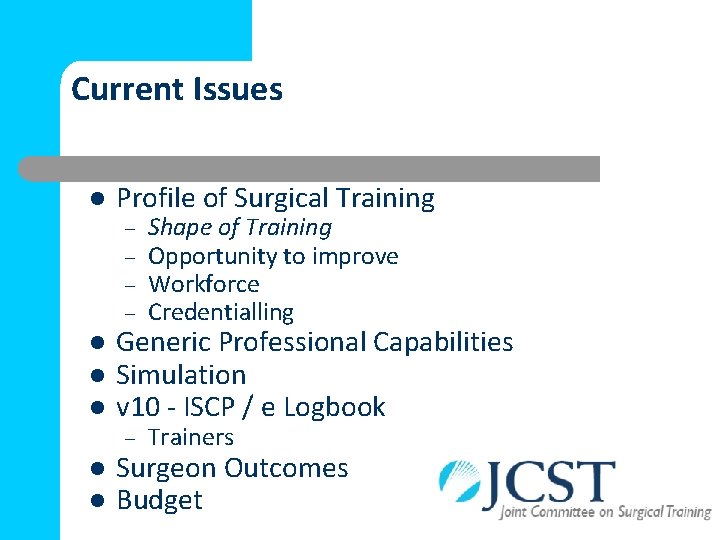
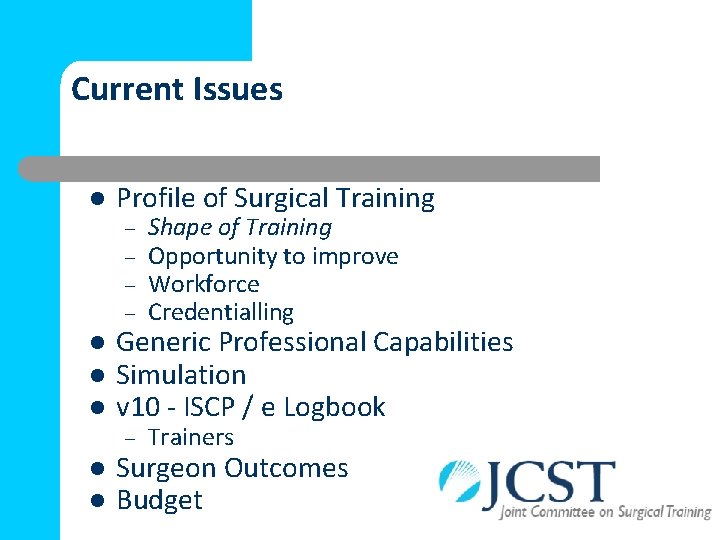
Current Issues l l l Profile of Surgical Training – – Shape of Training Opportunity to improve Workforce Credentialling – Trainers Generic Professional Capabilities Simulation v 10 - ISCP / e Logbook Surgeon Outcomes Budget
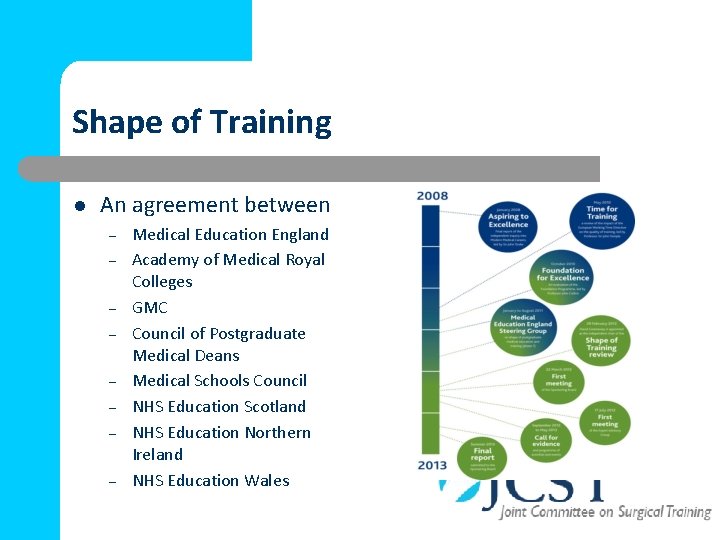
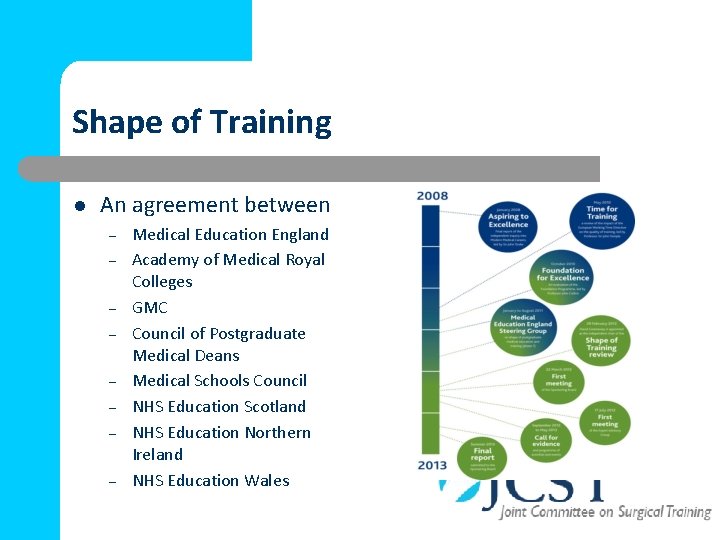
Shape of Training l An agreement between – – – – Medical Education England Academy of Medical Royal Colleges GMC Council of Postgraduate Medical Deans Medical Schools Council NHS Education Scotland NHS Education Northern Ireland NHS Education Wales
Key broad recommendations l l l Service requires Doctors with more general skills Requirement for Specialists remains Training – to CST within 6 years Credentialing for specific competencies Training must be more flexible and respond to patient/service needs Blurring the primary/ secondary care interface
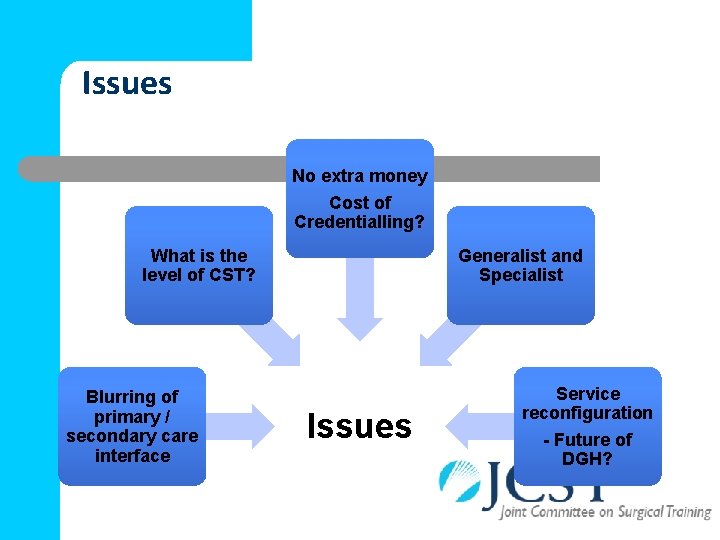
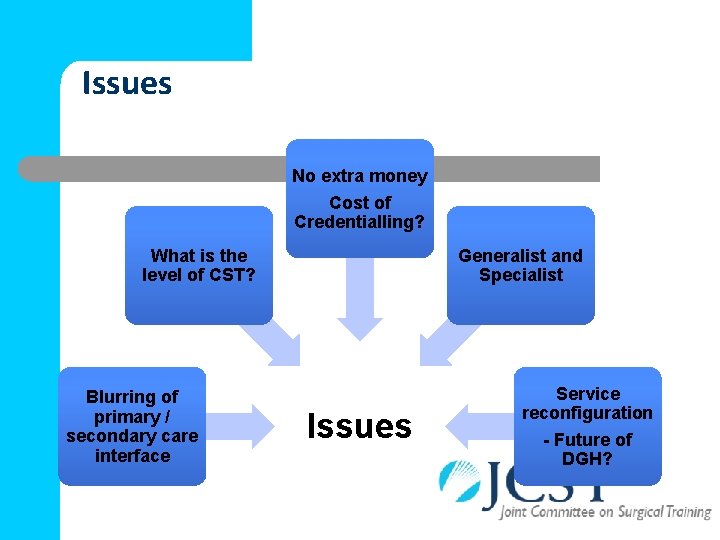
Issues No extra money Cost of Credentialling? What is the level of CST? Blurring of primary / secondary care interface Generalist and Specialist Issues Service reconfiguration - Future of DGH?
What has Happened? l UK-wide implementation group, chaired by Professor Ian Finlay (2014) l Division of the report into six workstreams (Autumn 2014) l Workstreams fed back to the implementation group l Report to 4 DH Ministers (Winter 2014/15) l 4 DH Ministers Statement (February 2015) l Implementation Group extended
Workshops l General themes and progression to CST l Primary – secondary care interface l Interaction with employers l Issues relating to SAS doctors l Academic pathway l Credentialing
What has Happened? l UK-wide implementation group, chaired by Professor Ian Finlay (2014) l Division of the report into six workstreams (Autumn 2014) l Workstreams fed back to the implementation group l Report to 4 DH Ministers (Winter 2014/15) l 4 DH Ministers Statement (February 2015) Implementation Group extended (Spring 2015) l
DH Statement 1. Implementation in an incremental fashion to minimize service disruption (short and medium term ) 2. Preserve current fit for purpose structures 3. Continue the UK Steering Group supported by 4 Nation Implementation Groups 4. Commission an impact assessment to report by summer 2015 5. Implement the recommendation that the careers of SAS doctors should be enhanced. 6. Pilot credentialing (eg cosmetic surgery) 7. Seek draft descriptions of training pathways to include CST within 6 years and credentialing for each theme
What might the implications be for craft specialties? l l l Relatively little Broad disciplines will remain Training will be general enough to permit most doctors to participate in and treat emergency patients Specialist interest will remain Some sub-specialist activities will be credentialed
What might the implications be for craft specialties? Training • Fewer trainers but better recognition • More use of simulation techniques • Immersion training • Competency based rather than time based • Training to enter team structures • ? Formal mentoring after CST
Strategy for Change in Surgical Training l Opportunity for Surgery l Improve quality of teaching and training – commitment from LEPs l Time for training and supervision l Rota review for emergency service provision l Role of Allied Healthcare Professional workforce
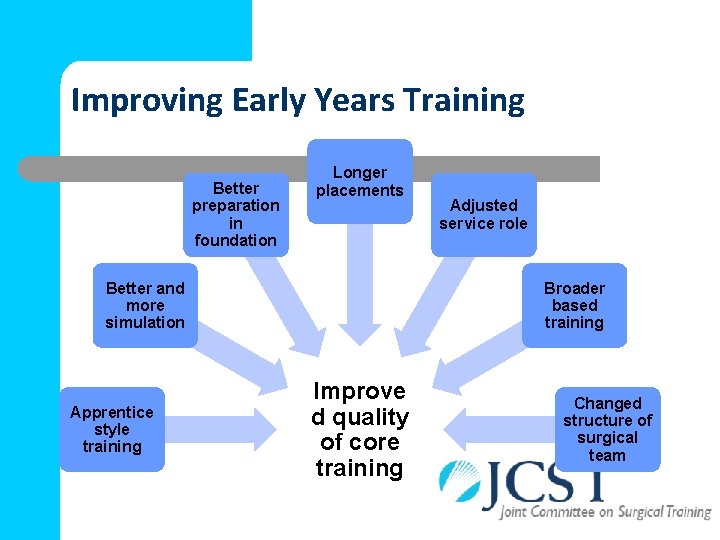
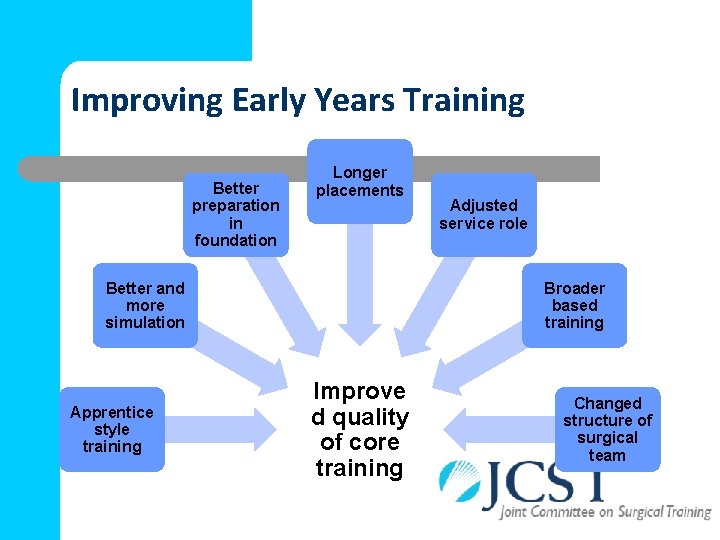
Improving Early Years Training Better preparation in foundation Longer placements Better and more simulation Apprentice style training Adjusted service role Broader based training Improve d quality of core training Changed structure of surgical team
Improving Surgical Training What are the Objectives l To improve quality of surgical care l To improve the quality of surgical training
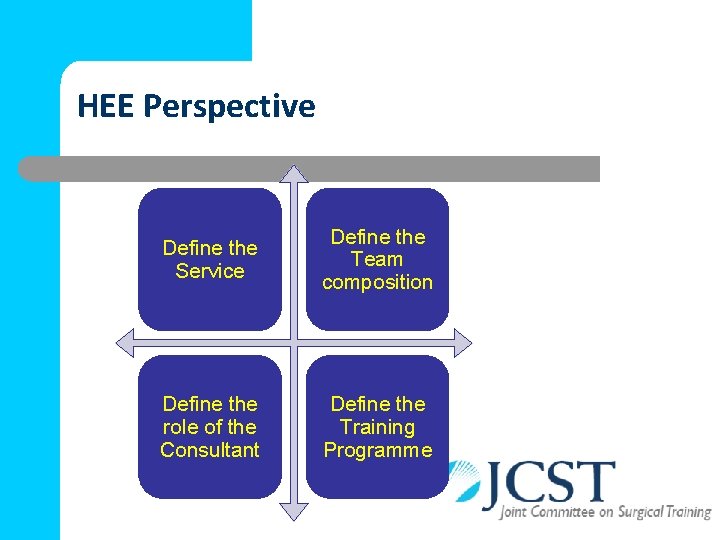
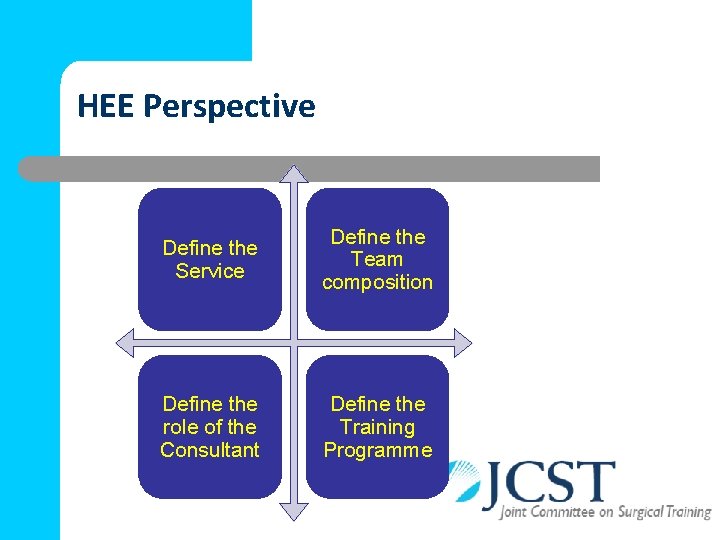
HEE Perspective Define the Service Define the Team composition Define the role of the Consultant Define the Training Programme
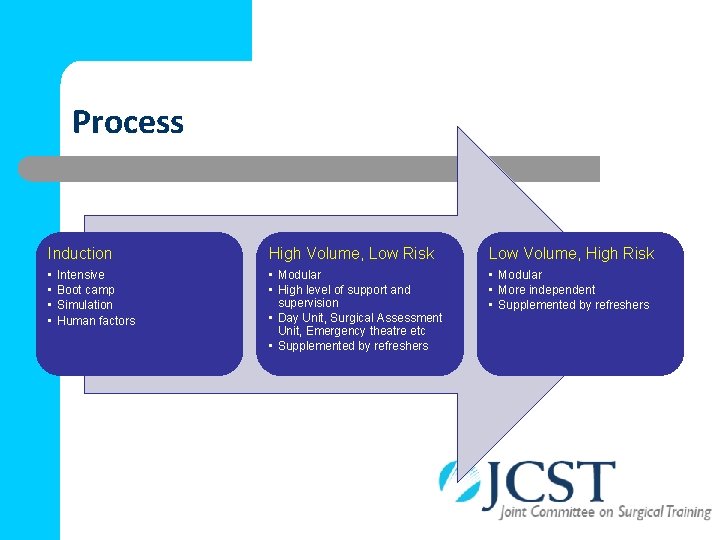
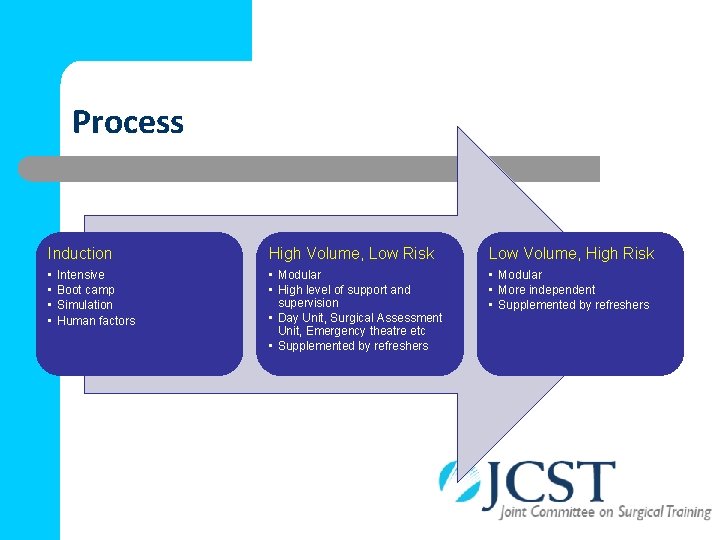
Process Induction High Volume, Low Risk Low Volume, High Risk • • • Modular • High level of support and supervision • Day Unit, Surgical Assessment Unit, Emergency theatre etc • Supplemented by refreshers • Modular • More independent • Supplemented by refreshers Intensive Boot camp Simulation Human factors
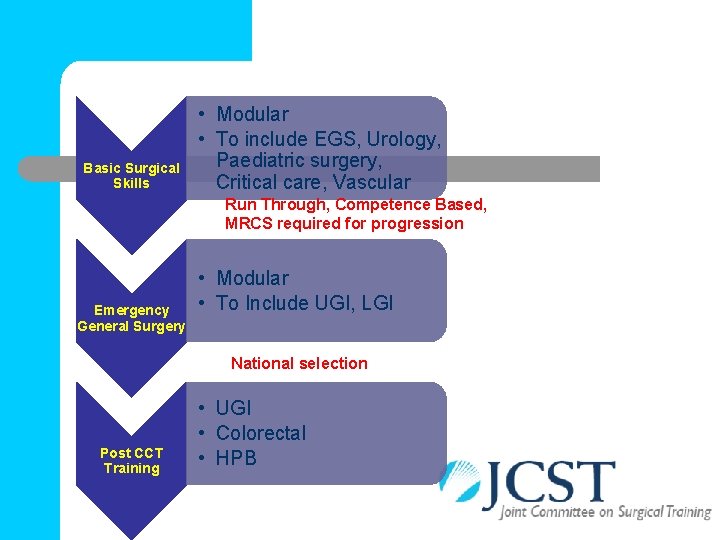
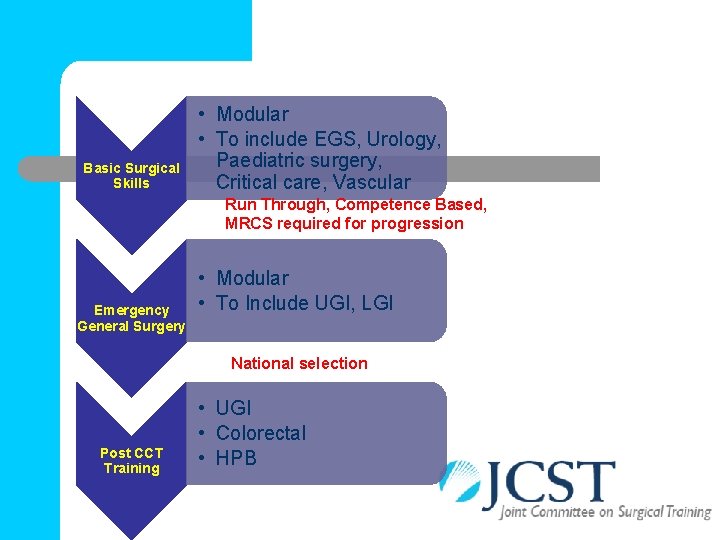
Basic Surgical Skills • Modular • To include EGS, Urology, Paediatric surgery, Critical care, Vascular Run Through, Competence Based, MRCS required for progression Emergency General Surgery • Modular • To Include UGI, LGI National selection Post CCT Training • UGI • Colorectal • HPB
Contemporary Challenges to Delivery of Surgical Simulation
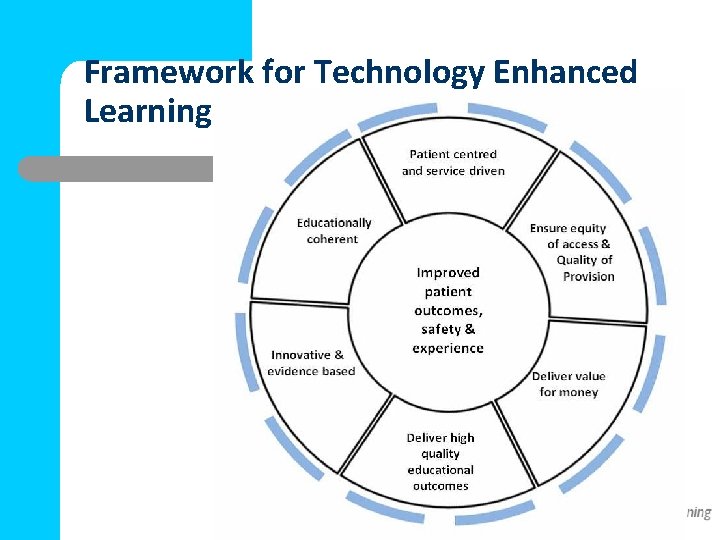
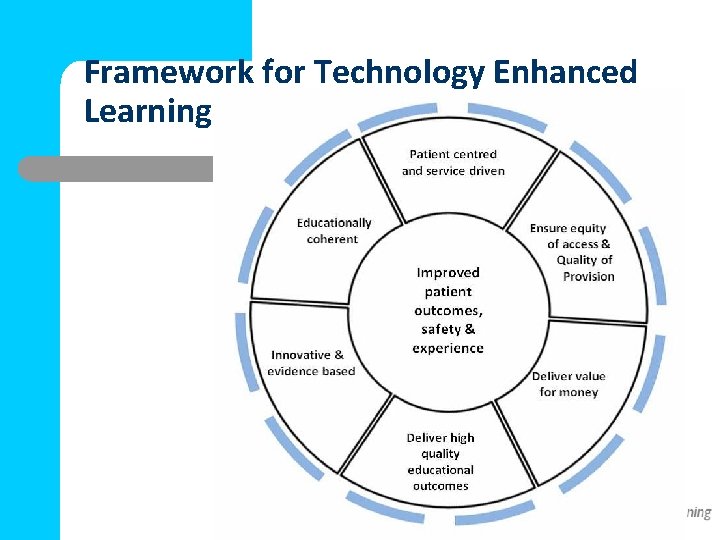
Framework for Technology Enhanced Learning

Simulation - Drivers l Clinical Experience l Change in working practices l EWTR l Technological and Scientific advances l Efficacy of Simulation

Challenges Human Resources l Trained Faculty – – – l Design curriculum Provide structured feedback Role model Time for Training – – Service vs Training Patient safety demands on trained surgeons
Challenges Educational Strategy l Structured curriculum – – – l Trainee clinic time vs simulation time – l Learning outcomes Assessment instruments Formative and summative feedback SDL Trainee Awareness
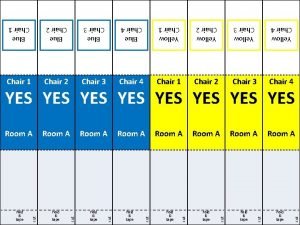
JCST Survey l In this post, did you receive simulation and clinical skills training?

Availability of Simulation by Deanery Yes No N/A East Midlands 42. 1% 36. 3% 21. 5% East of England 44. 4% 38. 5% 17. 1% KSS 65. 4% 27. 5% 7. 1% London 51. 1% 32. 6% 16. 3% North West Mersey 35. 9% 45. 9% 18. 2% North West 40. 3% 19. 4% Northern East 65. 4% 19. 8% 14. 8% N Ireland 27. 4% 48. 0% 24. 6% Scotland 41. 0% 39. 8% 19. 2% South West 32. 9% 47. 8% 19. 3% Thames Valley 48. 6% 37. 0% 14. 4% Wales 38. 9% 44. 3% 16. 8% Wessex 36. 0% 42. 5% 21. 5% West Midlands 39. 1% 38. 3% 22. 6% Yorkshire / Humber 58. 3% 29. 8% 11. 9% TOTAL 46. 0% 36. 5% 17. 5%
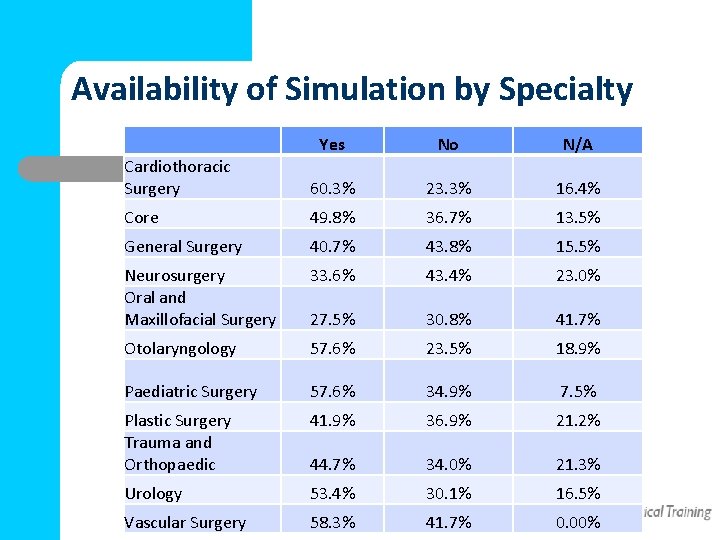
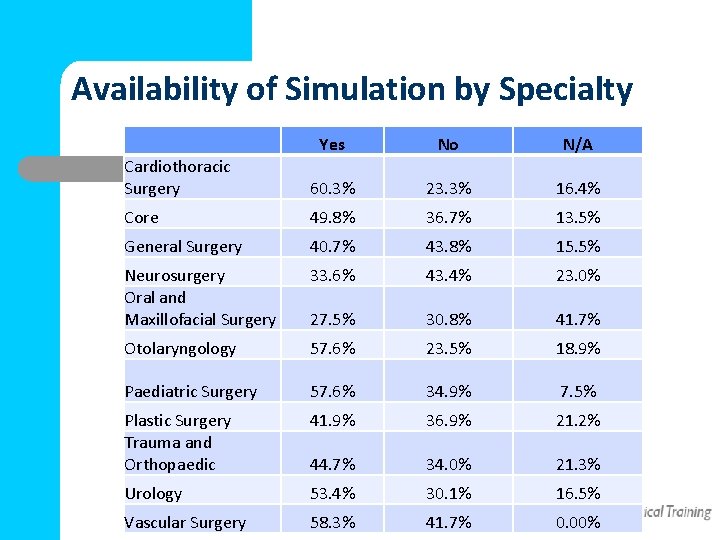
Availability of Simulation by Specialty Cardiothoracic Surgery Yes No N/A 60. 3% 23. 3% 16. 4% Core 49. 8% 36. 7% 13. 5% General Surgery 40. 7% 43. 8% 15. 5% Neurosurgery Oral and Maxillofacial Surgery 33. 6% 43. 4% 23. 0% 27. 5% 30. 8% 41. 7% Otolaryngology 57. 6% 23. 5% 18. 9% Paediatric Surgery 57. 6% 34. 9% 7. 5% Plastic Surgery Trauma and Orthopaedic 41. 9% 36. 9% 21. 2% 44. 7% 34. 0% 21. 3% Urology 53. 4% 30. 1% 16. 5% Vascular Surgery 58. 3% 41. 7% 0. 00%
Challenges Logistics l l l Task and Procedural Simulators Space for hardware Space for learners Funds to support and maintain Centralised resources Sharing resources
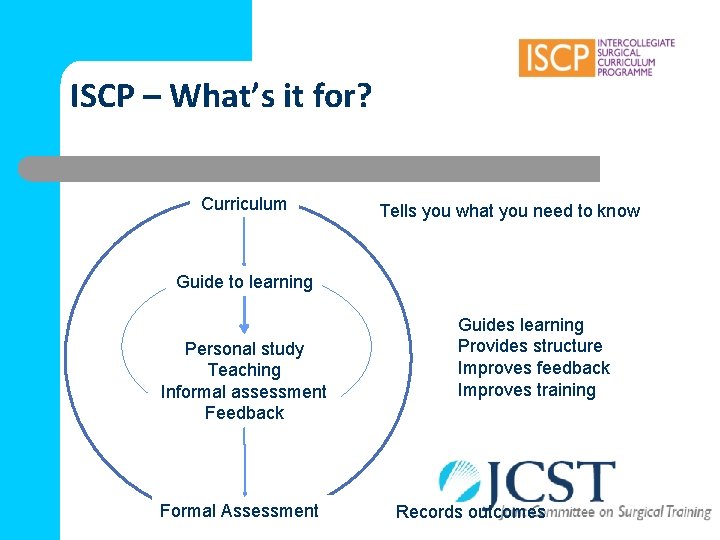
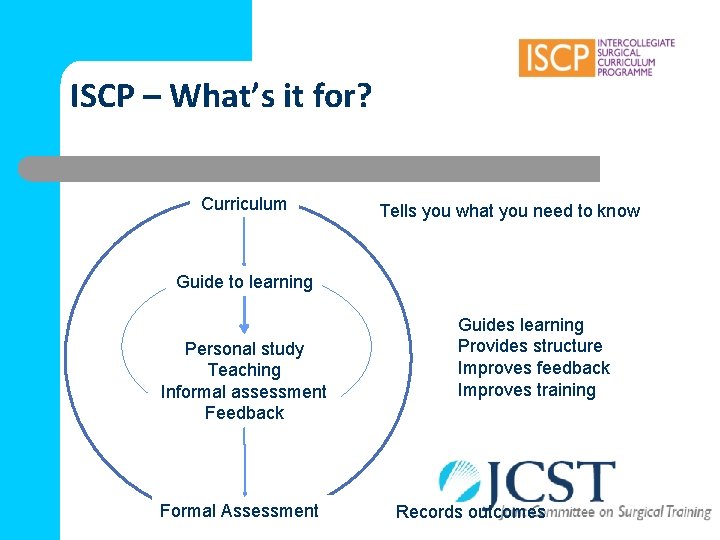
ISCP – What’s it for? Curriculum Tells you what you need to know Guide to learning Personal study Teaching Informal assessment Feedback Formal Assessment Guides learning Provides structure Improves feedback Improves training Records outcomes
ISCP v 10 l First ever complete re-write l Faster Better prepared for future developments l l l Planned for July / August release Beta version available now

ISCP v 10 l Web design Navigation Features l Content l l Easier to use More intuitive Simpler appearance Quicker Improve feedback Reduce tick box culture To improve training and learning To meet objectives of ISCP evaluation v 10 aims to keep ahead of the field l
http: //v 10 beta. iscp. ac. uk
Learning Agreement l l Central feature Planning of objectives Review of progress Simpler to complete – – – Logical No longer needs downloading of topics BUT Evidence will still be linked to topics
Improved WBAs l Emphasis on feedback l Structured free text at the top – Strengths – Weaknesses – Actions l Anonymous assessment of trainer quality l Reflective record
Supervisor Reports l Clinical supervisor l Educational supervisor l Structured feedback – 9 domains: knowledge, clinical skills. . . – Performance descriptors for each – Free text and performance grade for each domain
GMC Developments l Generic Professional Capabilities l Standards for Training l Equality and Diversity Guidance for Curricula and Assessment l Standards for Curricula and Assessment
Generic Professional Capabilities l Generic Professional Capabilities – – – Effective communication Leadership, team working, improving quality and patient safety Complex and vulnerable groups Education and training Research
Generic Professional Capabilities l Generic Professional Skills – – l Practical skills Clinical skills Generic Professional Knowledge – NHS structure

JCST Budget
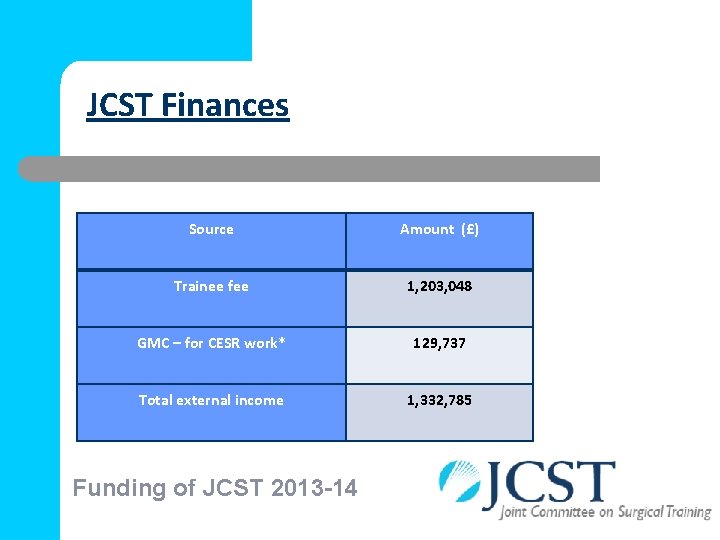
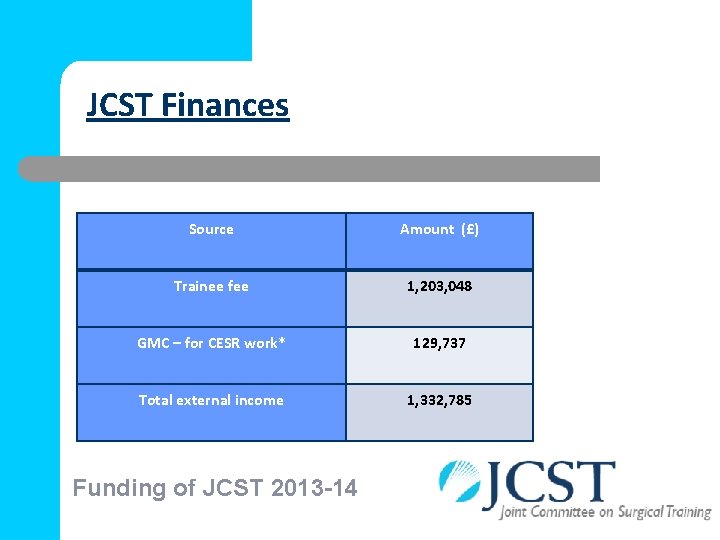
JCST Finances Source Amount (£) Trainee fee 1, 203, 048 GMC – for CESR work* 129, 737 Total external income 1, 332, 785 Funding of JCST 2013 -14
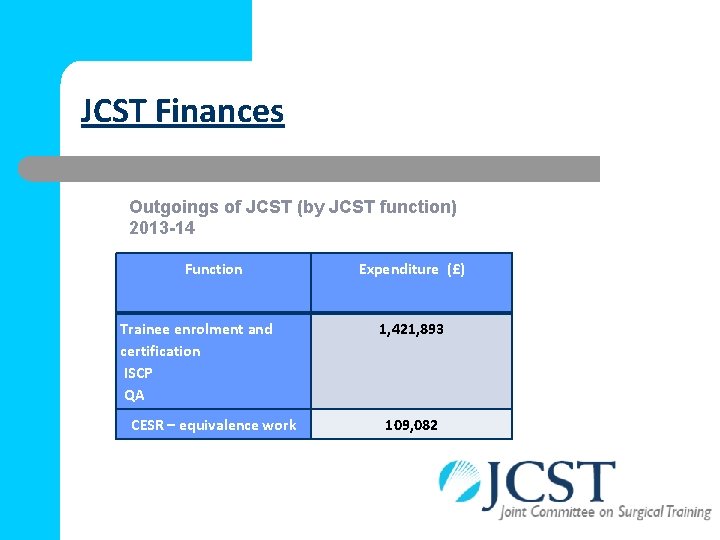
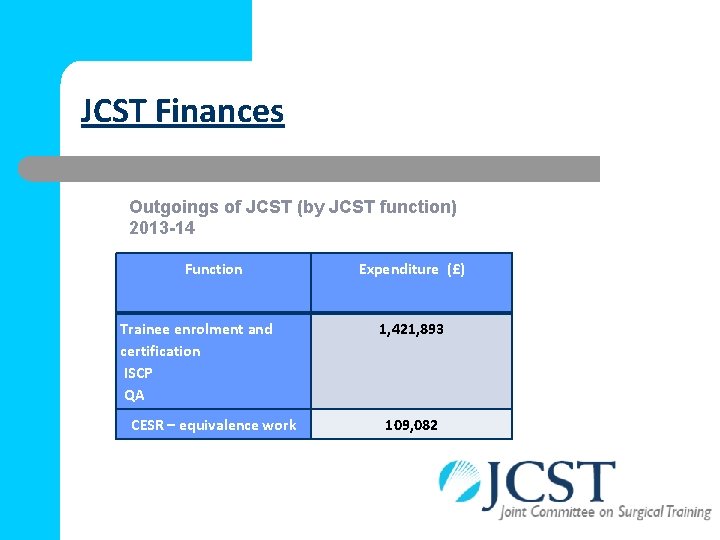
JCST Finances Outgoings of JCST (by JCST function) 2013 -14 Function Trainee enrolment and certification ISCP QA CESR – equivalence work Expenditure (£) 1, 421, 893 109, 082
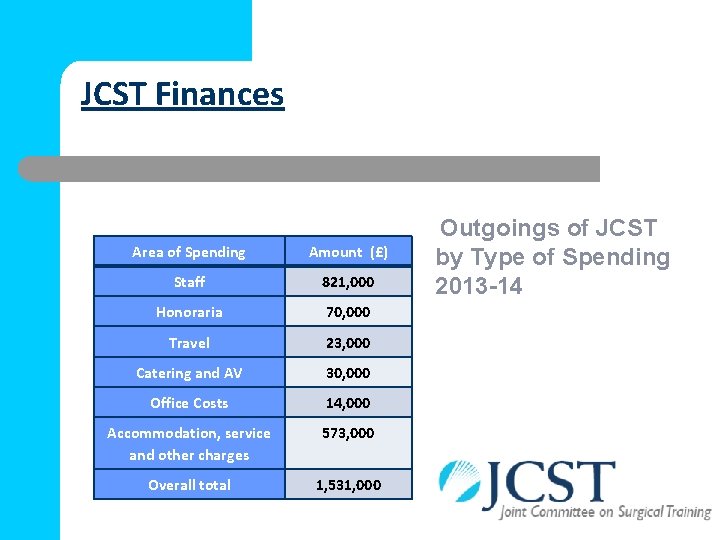
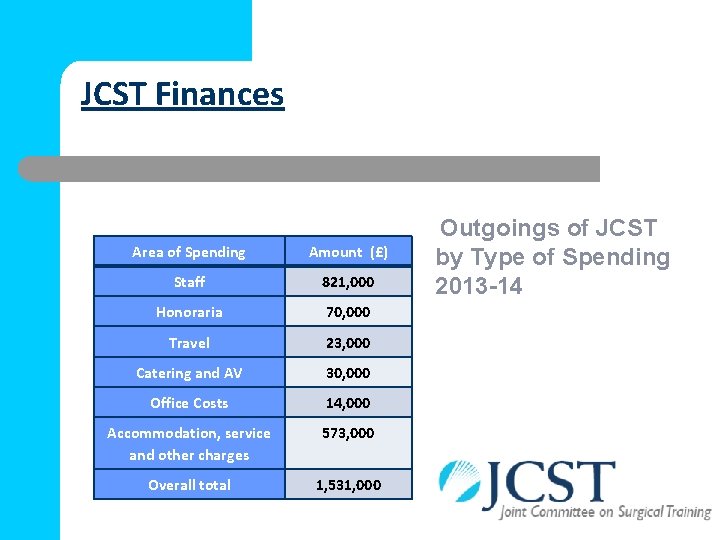
JCST Finances Area of Spending Amount (£) Staff 821, 000 Honoraria 70, 000 Travel 23, 000 Catering and AV 30, 000 Office Costs 14, 000 Accommodation, service and other charges 573, 000 Overall total 1, 531, 000 Outgoings of JCST by Type of Spending 2013 -14
 William allum surgeon
William allum surgeon Current state vs future state slide
Current state vs future state slide Diathermy machine diagram
Diathermy machine diagram Chair inspection checklist
Chair inspection checklist Line currents
Line currents Phase to phase voltage
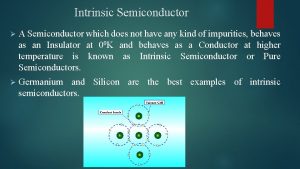
Phase to phase voltage Drift current and diffusion current in semiconductor
Drift current and diffusion current in semiconductor Line current and phase current
Line current and phase current Drift current density unit
Drift current density unit Ceramic composition resistors
Ceramic composition resistors The constant-current area of a fet lies between
The constant-current area of a fet lies between Balanced wye delta connection
Balanced wye delta connection Holding current and latching current
Holding current and latching current Diffusion current density
Diffusion current density Amperage can be described as
Amperage can be described as Hazard based safety engineering
Hazard based safety engineering Non planar circuit
Non planar circuit Current state example
Current state example Steady state current formula
Steady state current formula Value stream mapping esempi
Value stream mapping esempi Glossary icon
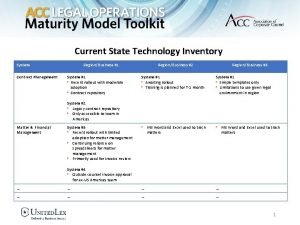
Glossary icon Overview of the current state of technology
Overview of the current state of technology Vsm 2013
Vsm 2013 Current trends in athletic training
Current trends in athletic training Aappm
Aappm Surgical toga gown
Surgical toga gown Vitamin c surgical sieve
Vitamin c surgical sieve Aorn prepping guidelines
Aorn prepping guidelines Inductive vs deductive learning
Inductive vs deductive learning Surgical audit cycle
Surgical audit cycle Dorsal recumbent position.
Dorsal recumbent position. Mnt critically ill
Mnt critically ill Surgical metabolism
Surgical metabolism Surgical planning laboratory
Surgical planning laboratory Surgical metabolism
Surgical metabolism Conclusion of medical surgical nursing
Conclusion of medical surgical nursing A nurse floats to a busy surgical unit
A nurse floats to a busy surgical unit Surgical conscience
Surgical conscience N
N Lyphadenitis
Lyphadenitis Care of the critically ill surgical patient
Care of the critically ill surgical patient Chloraprep contraindications
Chloraprep contraindications