Get Moving Mobilizing Patients After Joint Replacement Surgery

Get Moving! Mobilizing Patients After Joint Replacement Surgery Jaime Silangcruz DPT MS BME
Objectives 1) To learn how to safely mobilize total joint patients out of bed while adhering to their precautions 2) To learn how to properly adjust assistive devices for patient use 3) To learn complications that could be associated with total joint replacement and how to prevent them
Outline ● ● ● Introduction to joint replacement surgery Importance of early mobilization How to mobilize patient safely with proper body mechanics How to adjust assistive devices Possible complications Conclusion

https: //dribbble. com/shots/1617275 -Let-s-Partner-Up https: //www. outsourcing-pharma. com/Article/2015/04/22/Pfizer-reveals. PPD-as-third-strategic-CRO-partner#
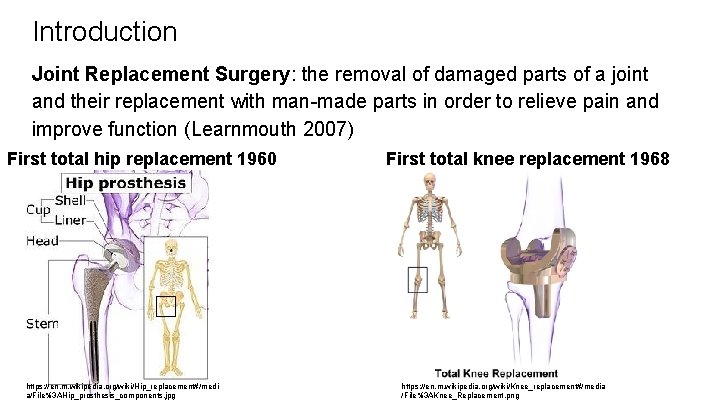
Introduction Joint Replacement Surgery: the removal of damaged parts of a joint and their replacement with man-made parts in order to relieve pain and improve function (Learnmouth 2007) First total hip replacement 1960 https: //en. m. wikipedia. org/wiki/Hip_replacement#/medi a/File%3 AHip_prosthesis_components. jpg First total knee replacement 1968 https: //en. m. wikipedia. org/wiki/Knee_replacement#/media /File%3 AKnee_Replacement. png
Candidates for Joint Replacement Surgery Patients who have hip or knee pain and have tried conservative treatment methods with no success (Affatato 2014) Factors that cause pain and necessitate joint replacement (Affatato 2014) ● Osteoarthritis (>90% of primary hip/knee replacements) (Etkin 2017) ● Post-traumatic arthritis ● Rheumatoid arthritis ● Avascular necrosis ● Hardware failure after ORIF ● Congenital hip dislocation/dysplasia Risk factors for OA (Blagojevic 2010) https: //www. shutterstock. com/searc h/%22 retirement+rheumatism%22 ● Overweight ● Repetitive stress on joint ● Previous knee injuries ● Age ● Fractures ● Genetics ● Bone deformities ● Metabolic diseases
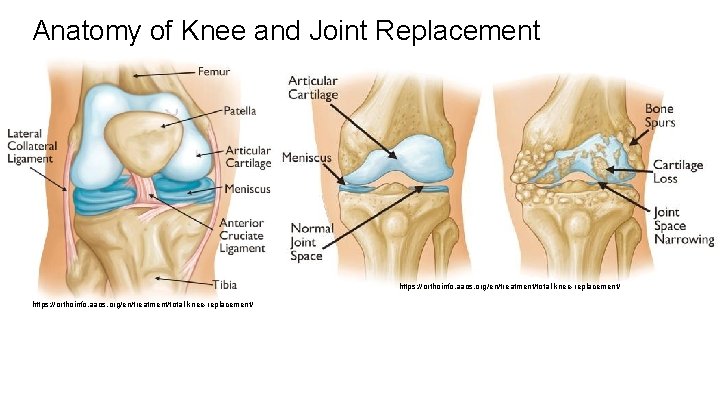
Anatomy of Knee and Joint Replacement https: //orthoinfo. aaos. org/en/treatment/total-knee-replacement/
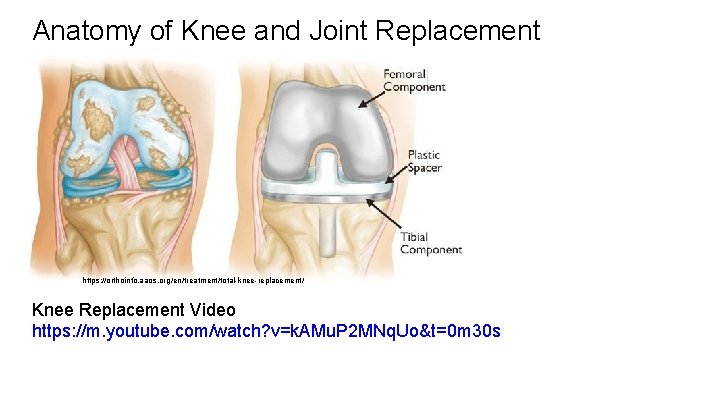
Anatomy of Knee and Joint Replacement https: //orthoinfo. aaos. org/en/treatment/total-knee-replacement/ Knee Replacement Video https: //m. youtube. com/watch? v=k. AMu. P 2 MNq. Uo&t=0 m 30 s
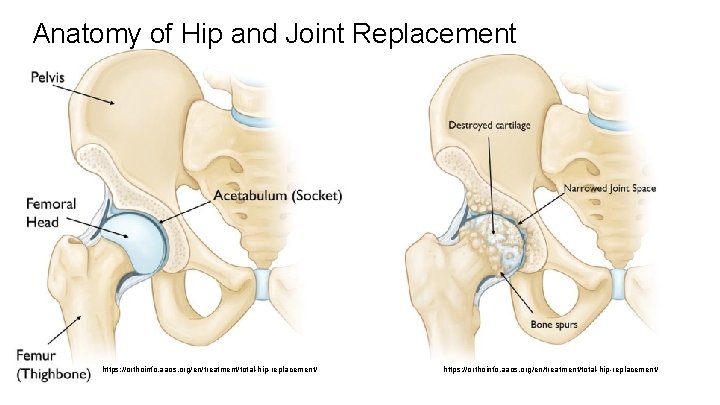
Anatomy of Hip and Joint Replacement https: //orthoinfo. aaos. org/en/treatment/total-hip-replacement/
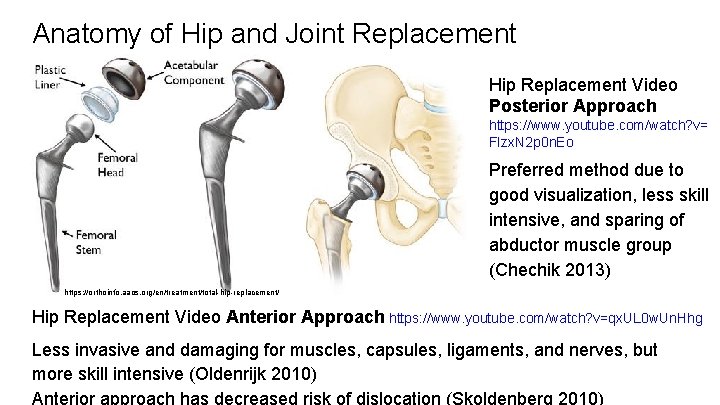
Anatomy of Hip and Joint Replacement Hip Replacement Video Posterior Approach https: //www. youtube. com/watch? v= FIzx. N 2 p 0 n. Eo Preferred method due to good visualization, less skill intensive, and sparing of abductor muscle group (Chechik 2013) https: //orthoinfo. aaos. org/en/treatment/total-hip-replacement/ Hip Replacement Video Anterior Approach https: //www. youtube. com/watch? v=qx. UL 0 w. Un. Hhg Less invasive and damaging for muscles, capsules, ligaments, and nerves, but more skill intensive (Oldenrijk 2010)
Joint Replacement Statistics Present Prevalence (Kremers 2015) ● Total hip replacement 2. 5 million ● Total knee replacement 4. 7 million ● Total hip+knee replacement 7 million Incidence (Sloan 2018) ● Total hip replacement 300 K/yr ● Total knee replacement 600 K/yr ● Total hip+knee replacement 900 K/yr Total knee replacement: 4. 6% all US OR procedures in 2011 (Pfutner 2013) ● Stroke 6. 8 million ● Myocardial infarction 7. 6 million ● Heart failure 5. 1 million https: //www. cherokeephoenix. org/Article/index/10131
Joint Replacement Statistics Expected Rise in Joint Replacements 2030 Estimate Prevalence (Kremers 2015) ● Increased life expectancy and ● Total hip+knee replacement 11 aging baby boomers million ● Increase in demand for improved Incidence (Sloan 2018) quality of life as average of ● Total hip replacement 635 K/yr joint replacement gets younger ● Total knee replacement 1. 28 M/yr (Ruiz 2013) ● Total hip+knee replacement 1. 9 M/yr Total hip+knee replacement: ~14. 5% all US OR procedures in 2030 http: //www. urbanhealth. com. my/health/international-day-of-persons-with-disabilities/
Importance of Early Mobilization https: //www. hopkinsmedicine. org/physical_medicine_rehabilitation/e ducation_training/amp/everybodymoves/index. html ● ● http: //www. apta. org/Blogs/PTTransforms/2 019/7/1/Every. BODYmoves/ Bedrest has detrimental effects on the cardiovascular, muscular, and skeletal systems including atelectasis, orthostatic hypotension, deep vein thrombosis, muscular atrophy, contractures, pressure sores, and osteoporosis (Stuempfle 2007) Benefits of early mobilization in the ICU results in decreased length of stay, delirium, readmission risk, death risk, infection risk (Hunter 2014) ● Early PT on day 0 vs day 1 post-op resulted in improved performance, reduced opioid use, shorter length of stay, and more patients discharged home (Sarpong 2019) ● Early weight bearing and physical activity improves the quality of bone tissue by improving fixation of prosthesis and decreasing incidence of early loosening (Mahendra 2009)
Quiz Time When was the first joint replacement done? Which joint replacement surgery is done the most? What is the most common reason why a joint replacement is needed? What are some of the benefits of early mobilization?
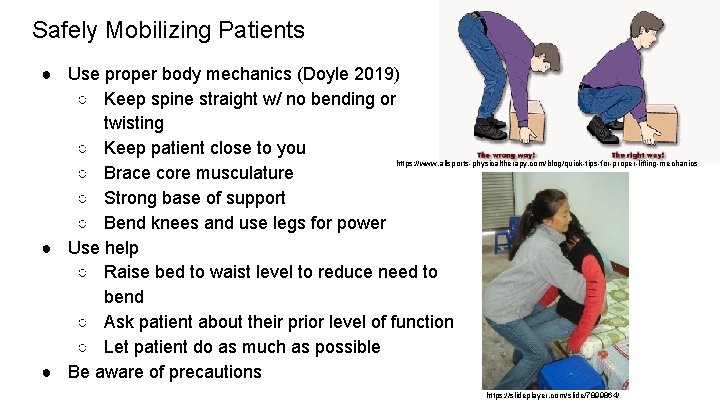
Safely Mobilizing Patients ● Use proper body mechanics (Doyle 2019) ○ Keep spine straight w/ no bending or twisting ○ Keep patient close to you https: //www. allsports-physicaltherapy. com/blog/quick-tips-for-proper-lifting-mechanics ○ Brace core musculature ○ Strong base of support ○ Bend knees and use legs for power ● Use help ○ Raise bed to waist level to reduce need to bend ○ Ask patient about their prior level of function ○ Let patient do as much as possible ● Be aware of precautions https: //slideplayer. com/slide/7899864/

Precautions Associated with Joint Replacement Surgery Knee replacement surgery ● Weight bearing as tolerated (WBAT) ● No pillow under knee (keep knee in extension, lock foot of bed) Hip replacement surgery posterior approach (to prevent dislocation) ● WBAT ● No hip flexion past 90 degrees (high chair, lock foot of bed) ● No adduction past midline (no crossing legs) ● No hip internal rotation past 0 degrees (no pigeon toes) https: //www. shirokoi. org/editv 2. php Hip replacement surgery anterior approach ● WBAT ● No forced extreme positions Special cases (antibiotic spacer) ● Partial weight bearing ● Toe-touch weight bearing ● Non-weight bearing ● No abduction
Bed Mobility: Getting Out of Bed General ● Make sure foot of bed is locked for knee replacement and posterior hip replacement ● Raise head of bed up ● Assist leg as needed Knee replacement and anterior hip replacement ● Get out on opposite side of surgical leg https: //www. meditek. ca/much-medsurg-hospital-bed -cost/ Posterior hip replacement ● Get out on same side of surgical leg to reduce risk of breaking precautions ● Make sure bed is adequate height to prevent hip bending past 90 degrees ● Roll onto side w/ abductor pillow between legs to prevent breaking of posterior hip precautions
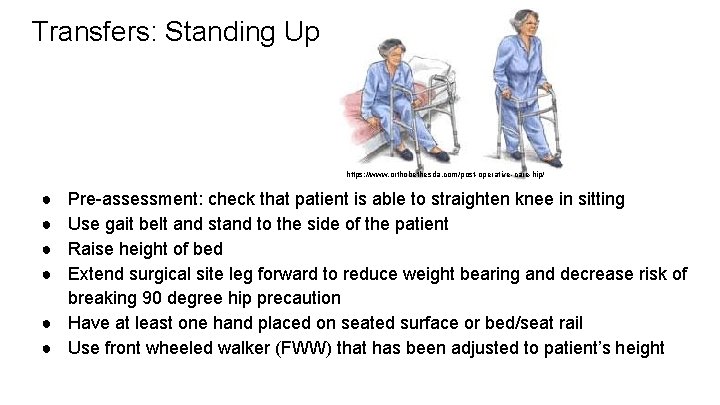
Transfers: Standing Up https: //www. orthobethesda. com/post-operative-care-hip/ ● ● Pre-assessment: check that patient is able to straighten knee in sitting Use gait belt and stand to the side of the patient Raise height of bed Extend surgical site leg forward to reduce weight bearing and decrease risk of breaking 90 degree hip precaution ● Have at least one hand placed on seated surface or bed/seat rail ● Use front wheeled walker (FWW) that has been adjusted to patient’s height
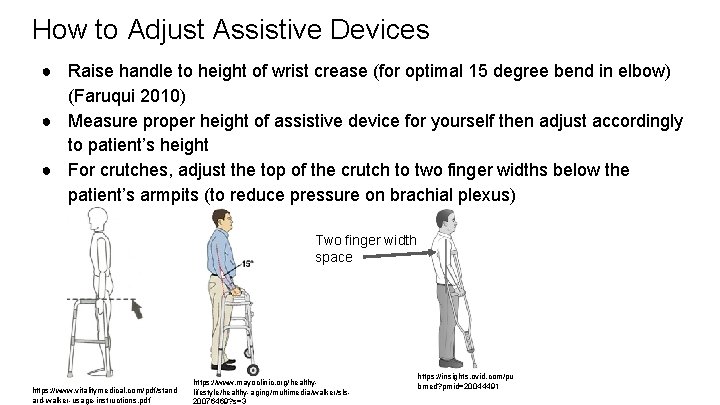
How to Adjust Assistive Devices ● Raise handle to height of wrist crease (for optimal 15 degree bend in elbow) (Faruqui 2010) ● Measure proper height of assistive device for yourself then adjust accordingly to patient’s height ● For crutches, adjust the top of the crutch to two finger widths below the patient’s armpits (to reduce pressure on brachial plexus) Two finger width space https: //www. vitalitymedical. com/pdf/stand ard-walker-usage-instructions. pdf https: //www. mayoclinic. org/healthylifestyle/healthy-aging/multimedia/walker/sls 20076469? s=3 https: //insights. ovid. com/pu bmed? pmid=20044491
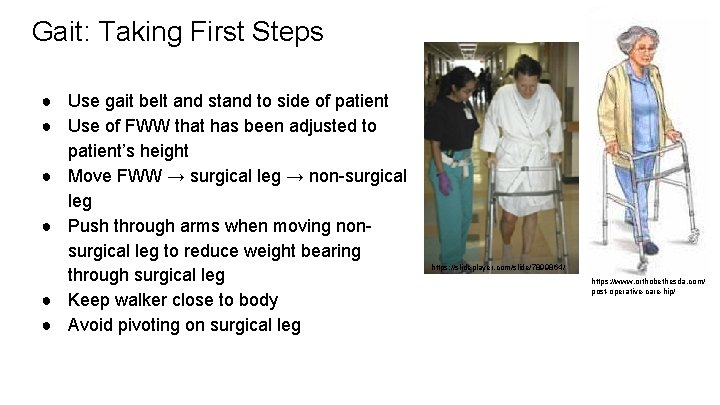
Gait: Taking First Steps ● Use gait belt and stand to side of patient ● Use of FWW that has been adjusted to patient’s height ● Move FWW → surgical leg → non-surgical leg ● Push through arms when moving nonsurgical leg to reduce weight bearing through surgical leg ● Keep walker close to body ● Avoid pivoting on surgical leg https: //slideplayer. com/slide/7899864/ https: //www. orthobethesda. com/ post-operative-care-hip/

Bed Mobility: Getting Back to Bed https: //m. youtube. com/watch? v=p. Csu. DA 5 W_9 g ● Have patient stand on opposite side of bed as surgical leg (ie if patient had a right hip replacement, stand on left side of bed) ● Have patient stand near the head of the bed ● Extend surgical site leg forward to reduce weight bearing and decrease risk of breaking 90 degree hip precaution ● Place at least one hand back on seated surface or bed/seat rail ● Assist leg as needed back into bed ● Place bed in trendelenburg position and ask patient to use arms and non-surgical leg to scoot up https: //fadavispt. mhmedical. com/con tent. aspx? bookid=1866§ionid=1 39617731
Quiz Time What are the precautions associated with a knee replacement? What are the precautions associated with a posterior hip replacement? What are the precautions associated with an antibiotic spacer? Which side of the bed do you get out of with a patient who has had an anterior hip replacement? When standing up after a knee replacement, which leg should be back? When walking after a hip replacement, which leg should move forward first? How high should you adjust a walker for a patient?
Practice Time 1) Practice helping a patient who just had a left knee replacement go to the bathroom 2) Practice helping a patient who just had a right posterior hip replacement revision (antibiotic spacer placement) with non-weightbearing precautions go to the bathroom using crutches.
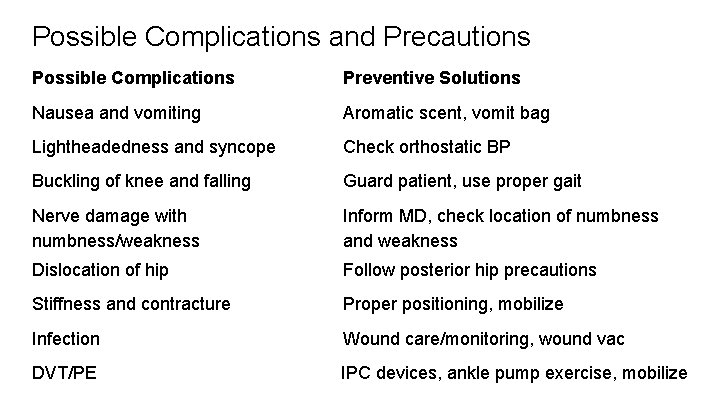
Possible Complications and Precautions Possible Complications Preventive Solutions Nausea and vomiting Aromatic scent, vomit bag Lightheadedness and syncope Check orthostatic BP Buckling of knee and falling Guard patient, use proper gait Nerve damage with numbness/weakness Inform MD, check location of numbness and weakness Dislocation of hip Follow posterior hip precautions Stiffness and contracture Proper positioning, mobilize Infection Wound care/monitoring, wound vac DVT/PE IPC devices, ankle pump exercise, mobilize
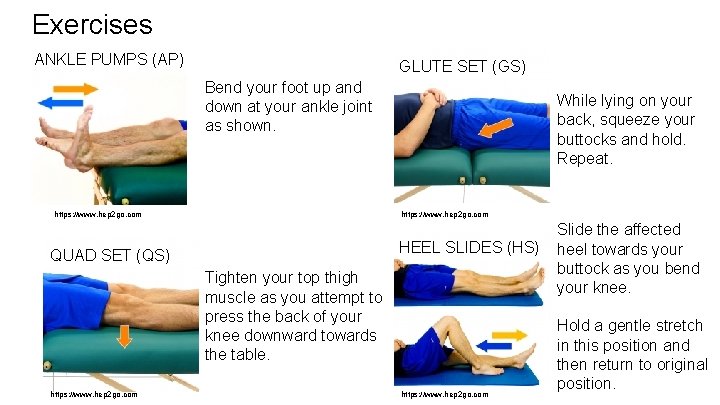
Exercises ANKLE PUMPS (AP) GLUTE SET (GS) Bend your foot up and down at your ankle joint as shown. While lying on your back, squeeze your buttocks and hold. Repeat. https: //www. hep 2 go. com HEEL SLIDES (HS) QUAD SET (QS) Tighten your top thigh muscle as you attempt to press the back of your knee downward towards the table. https: //www. hep 2 go. com Slide the affected heel towards your buttock as you bend your knee. Hold a gentle stretch in this position and then return to original position.
Quiz Time What do you do to prevent stiffness or contractures? What do you do to prevent DVT/PE?
Conclusion ● Hip and knee joint replacements are very common surgeries and are expected to increase in frequency in the future ● Early mobilization after joint replacement surgery is important to improve patient outcomes, reduce need for pain medication, reduce hospital length of stay, and improve patient’s ability to discharge home ● Safely mobilizing patients requires consideration of proper body mechanics, precautions, proper adjustment of assistive devices, and awareness of possible complications
References 1. Affatato S. “Perspectives in total hip arthroplasty: Advances in biomaterials and their tribological interactions. ” London: Woodhead Publishing, 2014. 2. Blagojevic M. , Jinks C. , Jeffery A. , Jordan K. P. "Risk factors for onset of osteoarthritis of the knee in older adults: a systematic review and meta-analysis. " Osteoarthritis and cartilage. 2010; 18. 1: 24 -33. 3. Chechik O, Khashan M, Lador R, Salai M, Amar E. “Surgical approach and prosthesis fixation in hip arthroplasty world wide. ” Arch Orthop Trauma Surg. 2013; 133(11): 1595 -600. 4. Coulter CL, Scarvell JM, Neeman TM, Smith PN. “Physiotherapist-directed rehabilitation exercises in the outpatient or home setting improve strength, gait speed and cadence after elective total hip replacement: a systematic review. ” Journal of physiotherapy. 2013; 59(4): 219 -26. 5. Etkin CD, Springer BD. “The American Joint Replacement Registry: The first 5 years. ” Arthroplast Today 2017; 3: 67 -69. 6. Evans JT, Walker RW, Evans JP, Blom AW, Sayers A, Whitehouse MR. “How long does a knee replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. ” Lancet. 2019; 393: 655– 663 7. Evans JT, Evans JP, Walker RW. “How long does a hip replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. ” Lancet 2019; 393: 647. 8. Faruqui SR, Jaeblon T. “Ambulatory assistive devices in orthopaedics: Uses and modifications. Journal of the American Academy of Orthopaedic Surgeons. ” J Am Acad Orthop Surg. 2010; 18: 41. 9. Hunter A, Johnson L, Willis W, Coustasse A. “Early Mobilization in ICU Patients. ” In proceedings of the Business and Health Administration Association Annual Conference 2014, Chicago, IL. 10. Iglesias SL, Gentile L, Mangupli MM, Pioli I, Nomides RE, Allende BL. “Femoral neck fractures in the elderly: from risk factors to pronostic features for survival. Journal of Trauma and Critical Care. ” 2017; 1(1).
References 11. Kremers HM, Larson DR, Berry DJ. “Prevalence of Total Hip and Knee Replacement in the United States. ” The Journal of Joint and Bone Surgery. 2015; 97: 1386 -1397. 12. Learnmouth ID, Young C, Rorabeck C. “The operation of the century: total hip replacement. ” Lancet. 2007; 370: 1508– 19. 13. Mahendra G, Pandit H, Kliskey K, Murray D, Gill HS, Athanasou N. “Necrotic and inflammatory changes in metal-on-metal resurfacing hip arthroplasties: relation to implant failure and pseudotumor formation. ” Acta orthopaedica 2009; 80(6): 653 -9. 14. Oldenrijk JV, Hoogland PV, Tuijthof GJ, Corveleijn R, Noordenbos TW, Schafroth MU. “Soft tissue damage after minimally invasive THA. ” Acta Orthopaedica. 2010; 81 (6): 696 -702 15. Pfuntner A, Wier LM, Stocks C. “Most Frequent Procedures Performed in U. S. Hospitals, 2011. HCUP Statistical Brief #165. ” October 2013. Agency for Healthcare Research and Quality, Rockville, MD. 16. Ruiz D, Koenig L, Dall ™, Gallo P, Ozikul AN, Parvizi J, Tongue J. “The Direct and Indirect Costs to Society of Treatment for End-Stage Knee Osteoarthritis. ” The Journal of Bone and Joint Surgery (American). 2013; 95 (16): 1473 17. Sarpong NO, Lakra A, Jennings E, Cooper HJ, Shah RP, Geller JA. “Same-Day Physical Therapy Following Total Knee Arthroplasty Leads to Improved Inpatient Physical Therapy Performance and Decreased Inpatient Opioid Consumption. ” J Arthroplasty. 2019. 18. Sköldenberg O, Ekman A, Salemyr M, Bodén H. “Reduced dislocation rate after hip arthroplasty for femoral neck fractures when changing from posterolateral to anterolateral approach: a prospective study of 372 hips. ” Acta orthopaedica. 2010; 81(5): 583 -7. 19. Sloan M. “Projected Volume of Primary and Revision Total Joint Arthroplasty in the United States, 2030 -2060. ” AAOS Annual Meeting. March 6, 2018. 20. Stuempfle K, Drury D. “The Physiological Consequences of Bed Rest. ” Journal of Exercise Physiology. 2007; 10(3): 32 -41
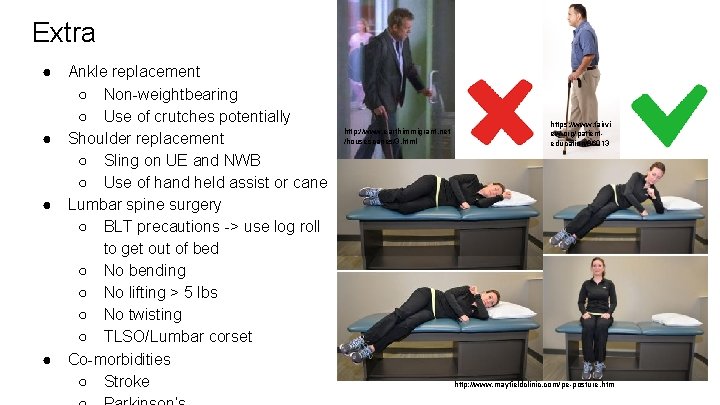
Extra ● ● Ankle replacement ○ Non-weightbearing ○ Use of crutches potentially Shoulder replacement ○ Sling on UE and NWB ○ Use of hand held assist or cane Lumbar spine surgery ○ BLT precautions -> use log roll to get out of bed ○ No bending ○ No lifting > 5 lbs ○ No twisting ○ TLSO/Lumbar corset Co-morbidities ○ Stroke http: //www. earthimmigrant. net /housescanes/3. html https: //www. fairvi ew. org/patienteducation/86013 http: //www. mayfieldclinic. com/pe-posture. htm
- Slides: 31