Paediatrics for Finals A Whistle Stop Tour Monica





- Slides: 70
Paediatrics for Finals: A Whistle Stop Tour Monica Parker & Craig Anderson FY 1 Hepatobiliary and Pancreatic Surgery at Freeman Hospital FY 1 Intensive Care Medicine at Sunderland Royal Hospital
What we will cover… • Normal Development & Key Milestones • Developmental Delay • A little bit on very small babies • Paediatric Respiratory Medicine • Paediatric Musculoskeletal Conditions • Fluids in Paediatrics • Quiz
Child Development • The rapid acquisition of skills acquired by children between birth and 5 years
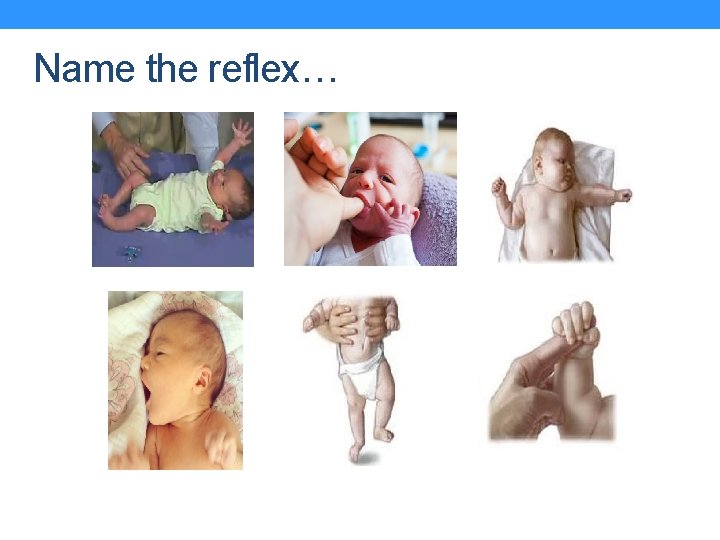
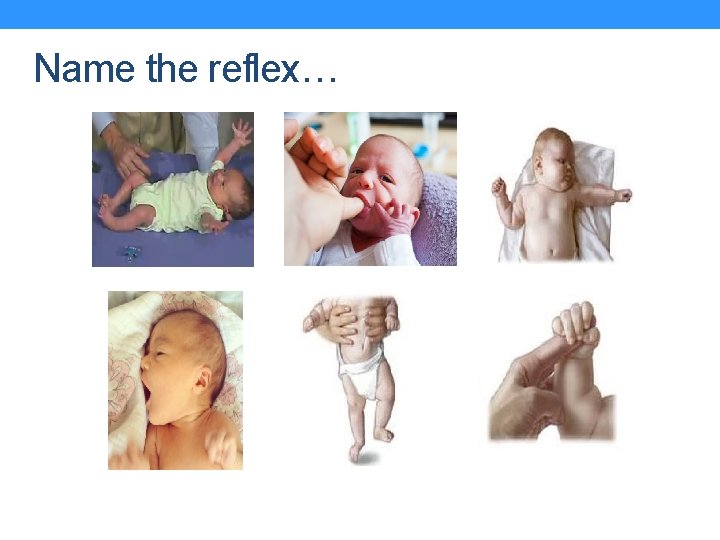
Name the reflex…
Primitive Reflexes Present at birth, should disappear by 4 -6 months 1. 2. 3. 4. 5. 6. Moro – sudden head extension elicits symmetrical extension then flexion of the limbs Sucking- object placed in mouth elicits sucking Atonic neck reflex – with the infant lying supine, turning the head to one side elicits the arm outstretching on the side to which the head is turned Rooting – a stimulus near the mouth elicits turning of the head towards the stimulus Stepping- when held and walked, the feet move in a stepping sequence Grasp – an object placed in the palm at the base of the fingers elicits flexion of the fingers of the hand
Why assess development? • Reassurance about normality • “Child health” monitoring • Recognition of abnormal patterns of development • Specific (e. g. motor) or global delay • Isolated or syndromic • Organic or Social • Regression
Developmental Milestones • Acquisition of a key skill • Median age – age at which half population acquire the skill • Limit age – age at which a skill should have been achieved (2 SD from the mean)
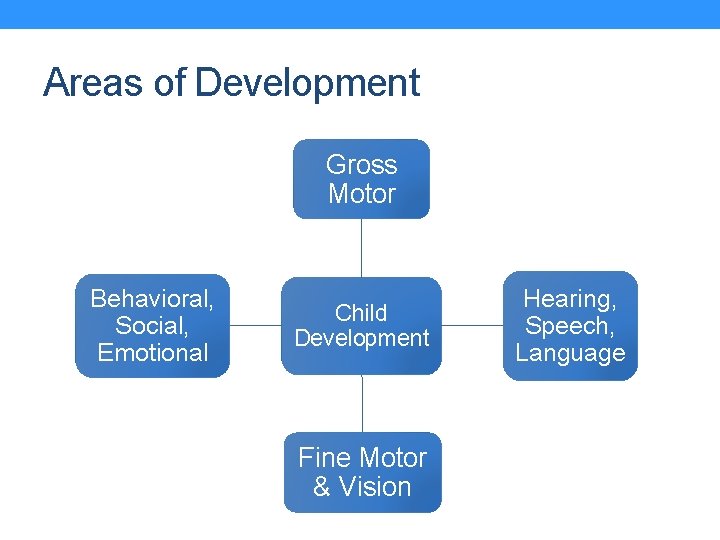
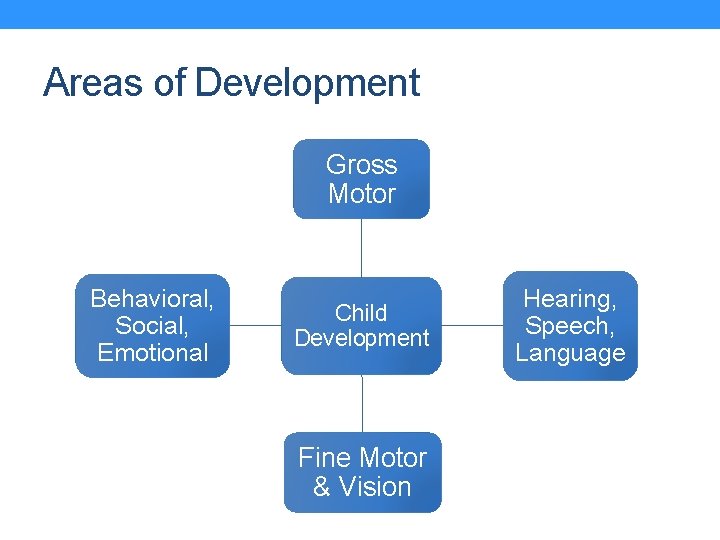
Areas of Development Gross Motor Behavioral, Social, Emotional Child Development Fine Motor & Vision Hearing, Speech, Language
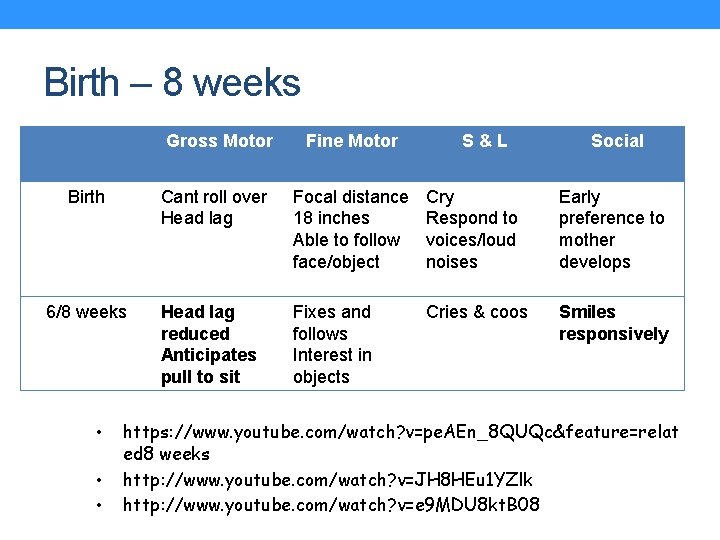
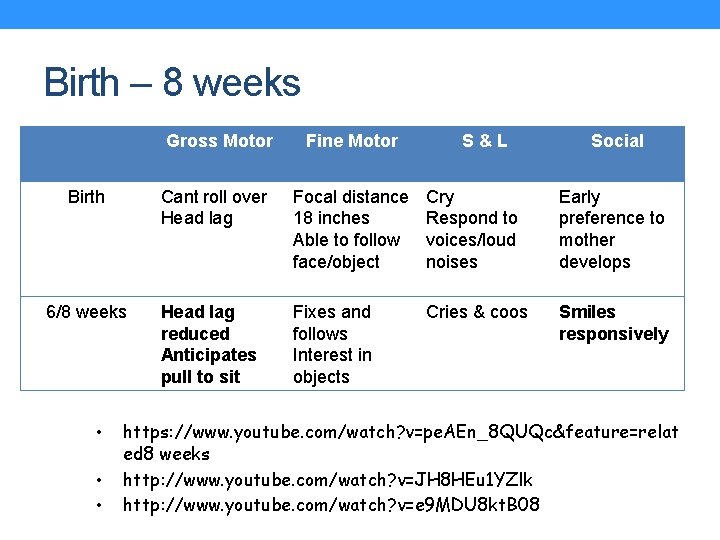
Birth – 8 weeks Gross Motor Fine Motor S&L Social Birth Cant roll over Head lag Focal distance 18 inches Able to follow face/object Cry Respond to voices/loud noises Early preference to mother develops 6/8 weeks Head lag reduced Anticipates pull to sit Fixes and follows Interest in objects Cries & coos Smiles responsively • • • https: //www. youtube. com/watch? v=pe. AEn_8 QUQc&feature=relat ed 8 weeks http: //www. youtube. com/watch? v=JH 8 HEu 1 YZlk http: //www. youtube. com/watch? v=e 9 MDU 8 kt. B 08

3 – 12 months Gross Motor Fine Motor S&L Social 3 months Lifts & turns head Grasps rattle Follows Cooing and Smiles moving object gurgling responsively Turns head to sounds Reacts to peek-abright colours boo 6 months No head lag Sits supported Rolls over Mouthing Reaches for objects babbles Plays with feet Holds bottle while feeding 9 months Sits independently 12 months Pulls to stand Crawling Slight walking Pincer grip Bangs blocks together 2 words Waves bye Claps hand Stranger anxiety
3 – 12 months 4 month old http: //www. youtube. com/watch? v=Tx 90 L 0 n. D 1 E 4 4 - 6 month https: //www. youtube. com/watch? v=Y 8 k. Abzx. KHL 0&feature=related 6 – 8 month http: //www. youtube. com/watch? v=u. Qmq. RIR 2 Yx. A 10 month http: //www. youtube. com/watch? v=d. AGQ 1 u. CJRKM
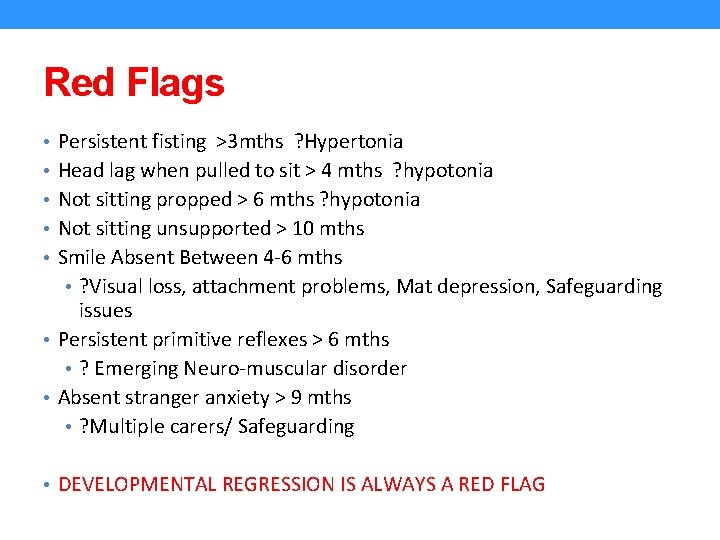
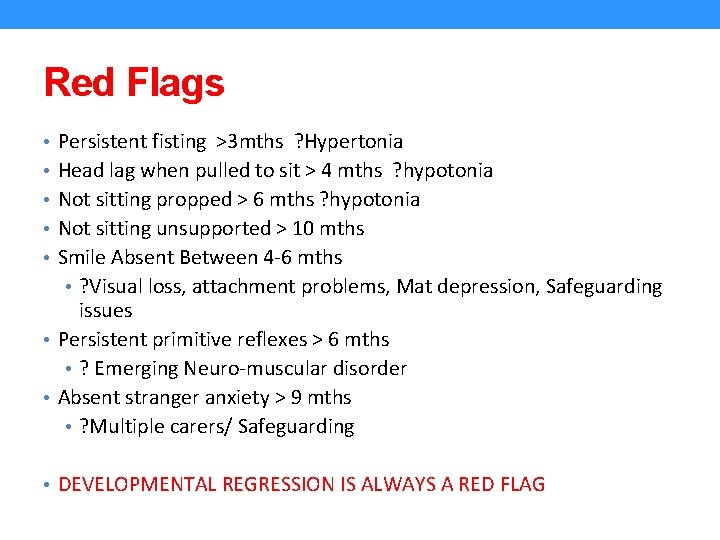
Red Flags • Persistent fisting >3 mths ? Hypertonia • Head lag when pulled to sit > 4 mths ? hypotonia • Not sitting propped > 6 mths ? hypotonia • Not sitting unsupported > 10 mths • Smile Absent Between 4 -6 mths • ? Visual loss, attachment problems, Mat depression, Safeguarding issues • Persistent primitive reflexes > 6 mths • ? Emerging Neuro-muscular disorder • Absent stranger anxiety > 9 mths • ? Multiple carers/ Safeguarding • DEVELOPMENTAL REGRESSION IS ALWAYS A RED FLAG
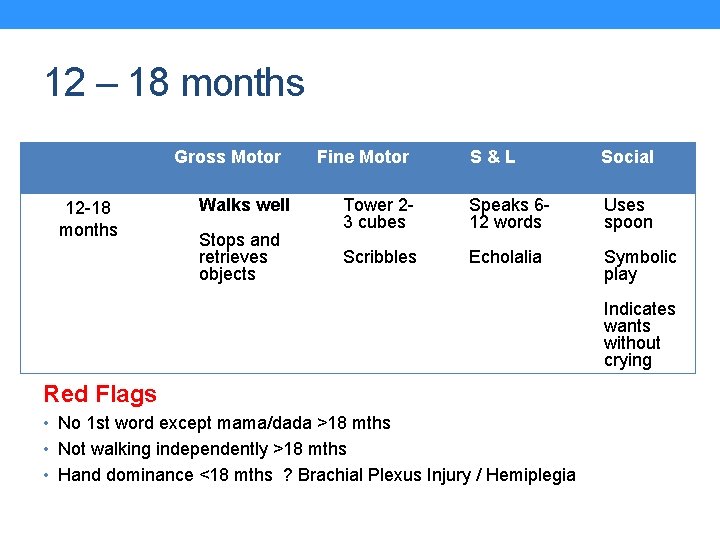
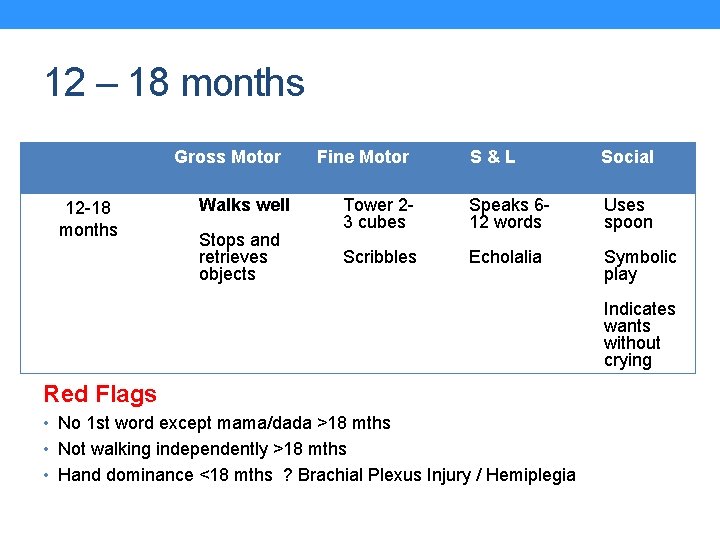
12 – 18 months Gross Motor 12 -18 months Walks well Stops and retrieves objects Fine Motor S&L Social Tower 23 cubes Speaks 612 words Uses spoon Scribbles Echolalia Symbolic play Indicates wants without crying Red Flags • No 1 st word except mama/dada >18 mths • Not walking independently >18 mths • Hand dominance <18 mths ? Brachial Plexus Injury / Hemiplegia
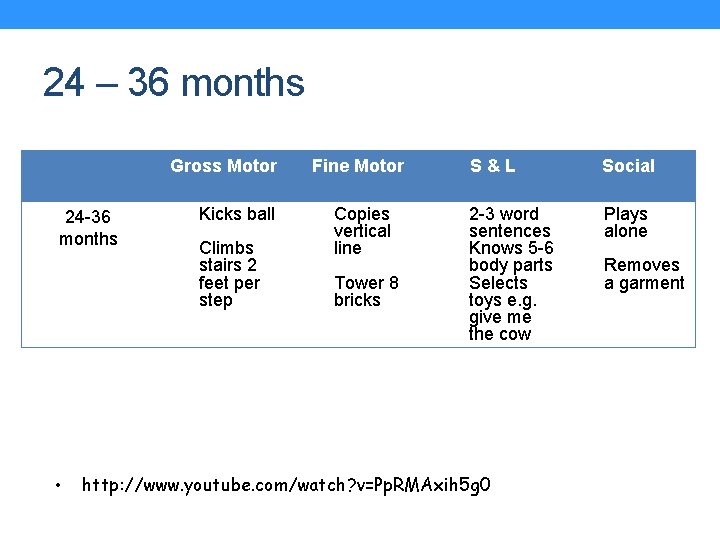
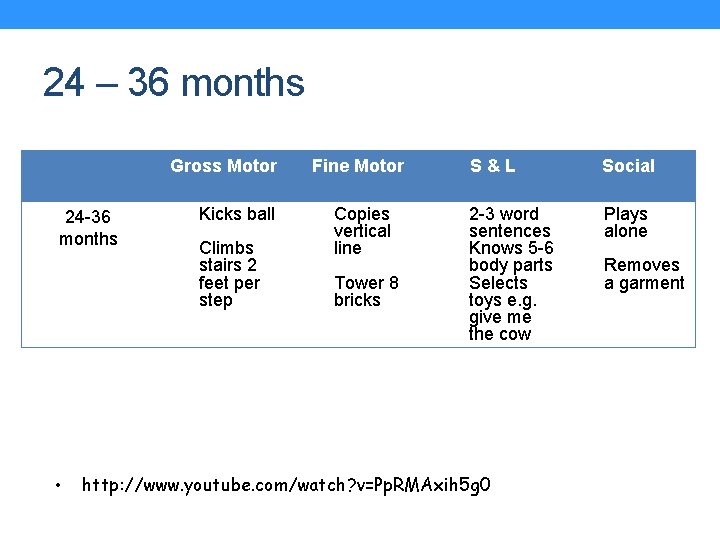
24 – 36 months Gross Motor 24 -36 months • Kicks ball Climbs stairs 2 feet per step Fine Motor Copies vertical line Tower 8 bricks S&L Social 2 -3 word sentences Knows 5 -6 body parts Selects toys e. g. give me the cow Plays alone http: //www. youtube. com/watch? v=Pp. RMAxih 5 g 0 Removes a garment
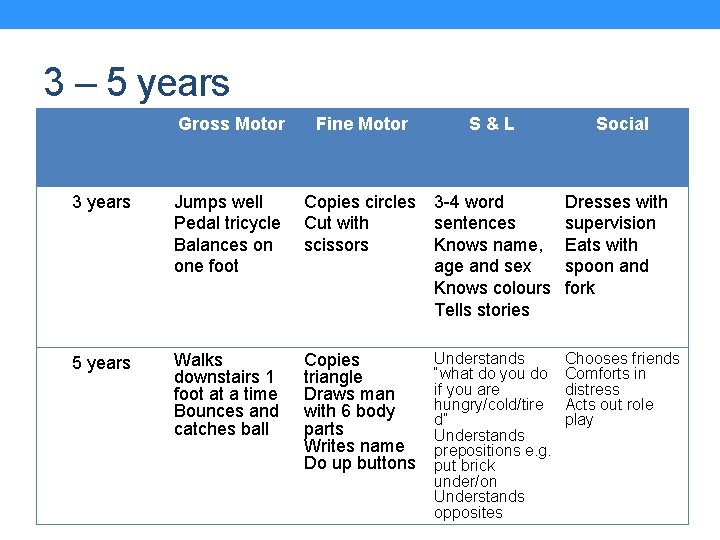
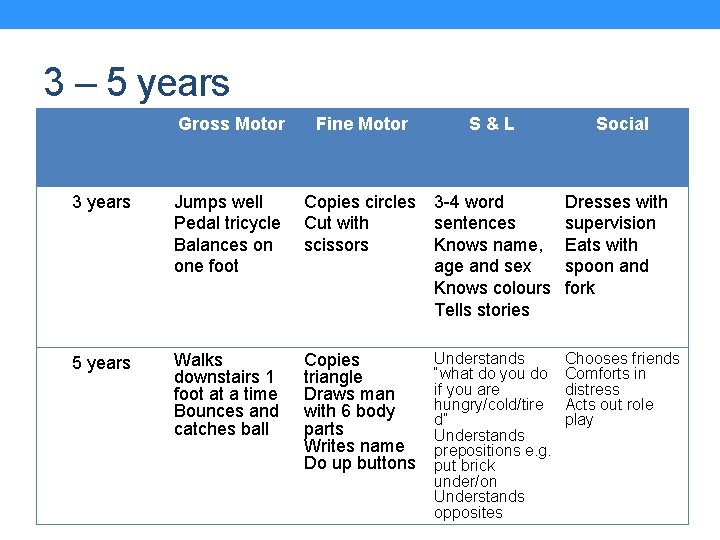
3 – 5 years Gross Motor Fine Motor S&L Social 3 years Jumps well Pedal tricycle Balances on one foot Copies circles Cut with scissors 3 -4 word sentences Knows name, age and sex Knows colours Tells stories Dresses with supervision Eats with spoon and fork 5 years Walks downstairs 1 foot at a time Bounces and catches ball Copies triangle Draws man with 6 body parts Writes name Do up buttons Understands “what do you do if you are hungry/cold/tire d” Understands prepositions e. g. put brick under/on Understands opposites Chooses friends Comforts in distress Acts out role play
Meet Rosie… • 2 years and 3 months old • GP has referred due to concerns that she is not walking yet • What else do you need to know?
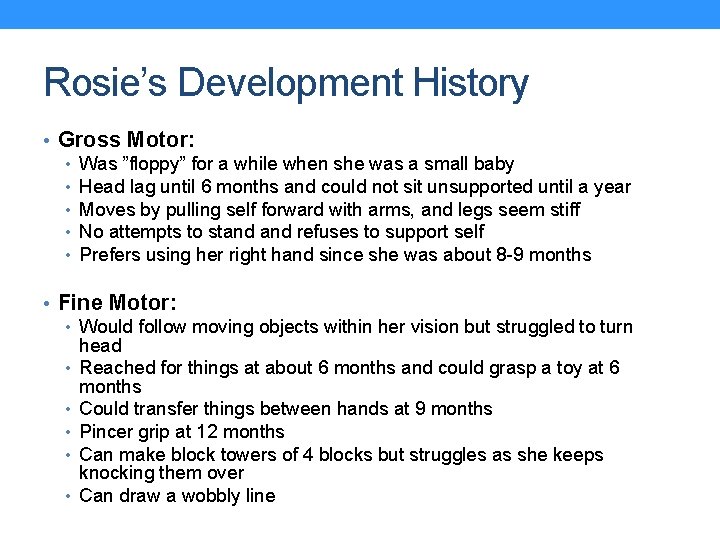
Rosie’s Development History • Gross Motor: • Was ”floppy” for a while when she was a small baby • Head lag until 6 months and could not sit unsupported until a year • Moves by pulling self forward with arms, and legs seem stiff • No attempts to stand refuses to support self • Prefers using her right hand since she was about 8 -9 months • Fine Motor: • Would follow moving objects within her vision but struggled to turn head • Reached for things at about 6 months and could grasp a toy at 6 months • Could transfer things between hands at 9 months • Pincer grip at 12 months • Can make block towers of 4 blocks but struggles as she keeps knocking them over • Can draw a wobbly line
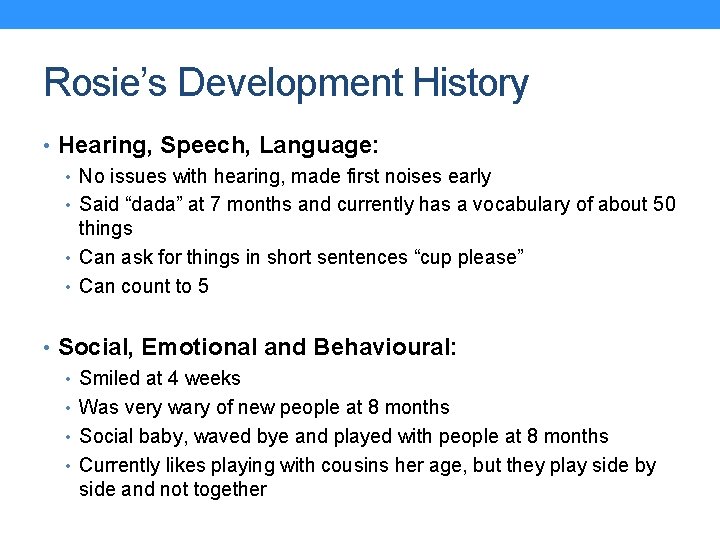
Rosie’s Development History • Hearing, Speech, Language: • No issues with hearing, made first noises early • Said “dada” at 7 months and currently has a vocabulary of about 50 things • Can ask for things in short sentences “cup please” • Can count to 5 • Social, Emotional and Behavioural: • Smiled at 4 weeks • Was very wary of new people at 8 months • Social baby, waved bye and played with people at 8 months • Currently likes playing with cousins her age, but they play side by side and not together
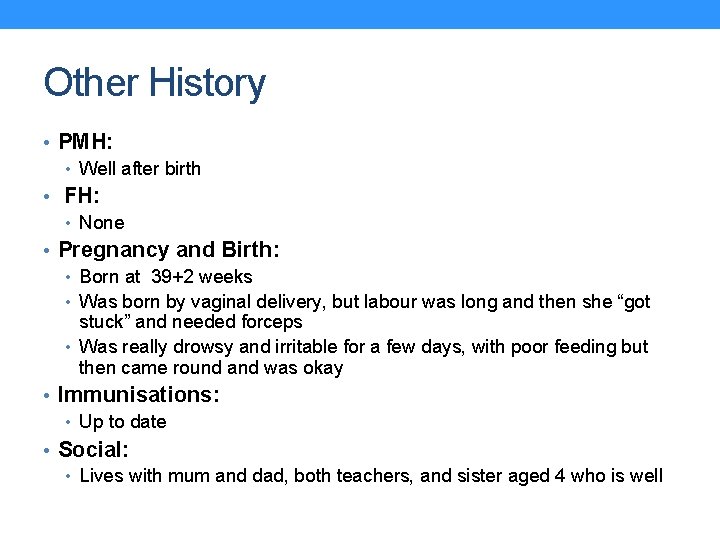
Other History • PMH: • Well after birth • FH: • None • Pregnancy and Birth: • Born at 39+2 weeks • Was born by vaginal delivery, but labour was long and then she “got stuck” and needed forceps • Was really drowsy and irritable for a few days, with poor feeding but then came round and was okay • Immunisations: • Up to date • Social: • Lives with mum and dad, both teachers, and sister aged 4 who is well
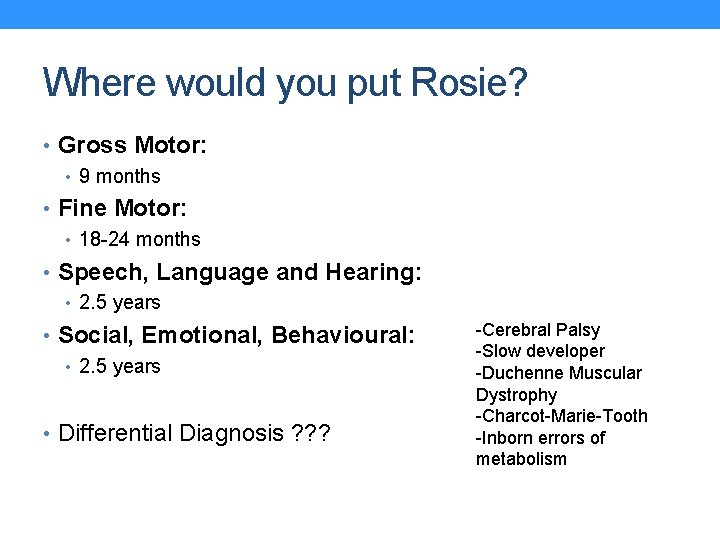
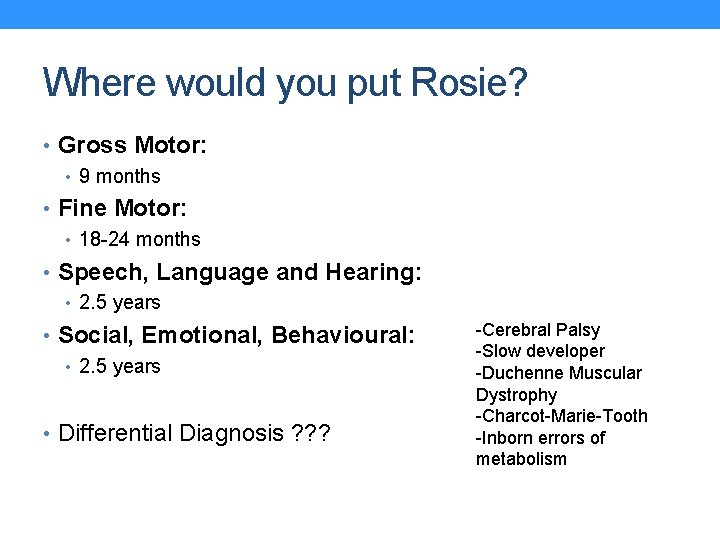
Where would you put Rosie? • Gross Motor: • 9 months • Fine Motor: • 18 -24 months • Speech, Language and Hearing: • 2. 5 years • Social, Emotional, Behavioural: • 2. 5 years • Differential Diagnosis ? ? ? -Cerebral Palsy -Slow developer -Duchenne Muscular Dystrophy -Charcot-Marie-Tooth -Inborn errors of metabolism
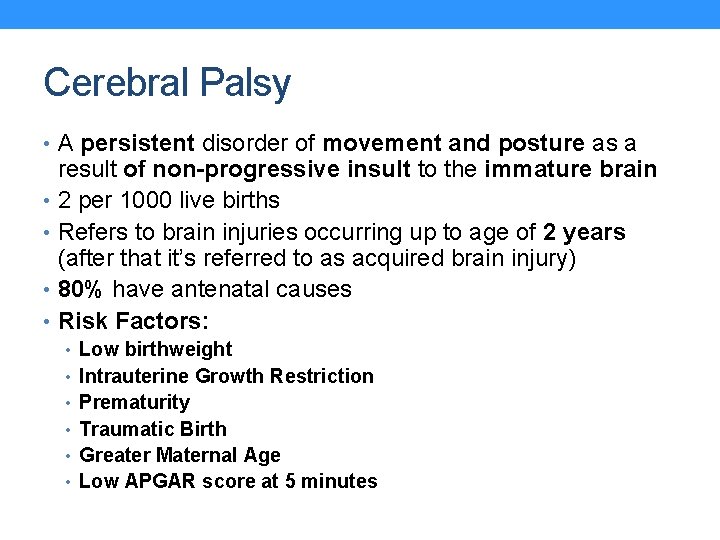
Cerebral Palsy • A persistent disorder of movement and posture as a result of non-progressive insult to the immature brain • 2 per 1000 live births • Refers to brain injuries occurring up to age of 2 years (after that it’s referred to as acquired brain injury) • 80% have antenatal causes • Risk Factors: • Low birthweight • Intrauterine Growth Restriction • Prematurity • Traumatic Birth • Greater Maternal Age • Low APGAR score at 5 minutes
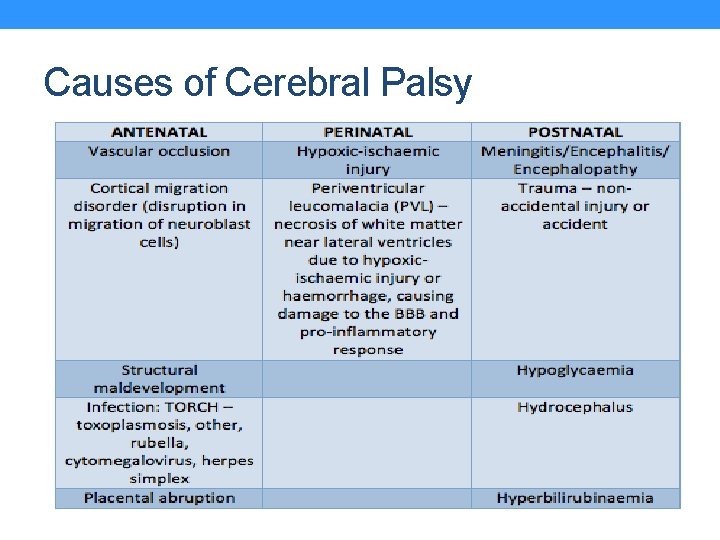
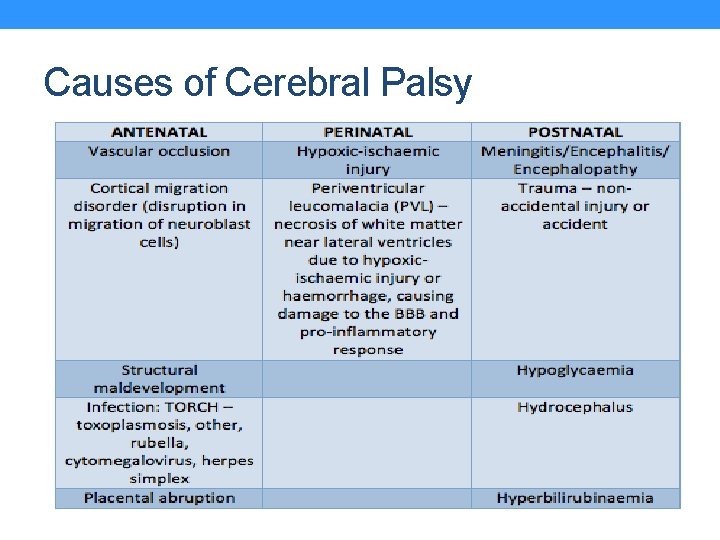
Causes of Cerebral Palsy
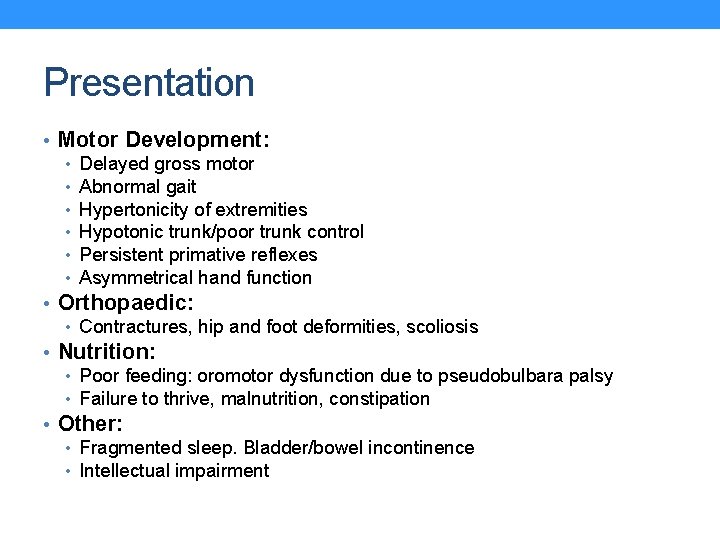
Presentation • Motor Development: • Delayed gross motor • Abnormal gait • Hypertonicity of extremities • Hypotonic trunk/poor trunk control • Persistent primative reflexes • Asymmetrical hand function • Orthopaedic: • Contractures, hip and foot deformities, scoliosis • Nutrition: • Poor feeding: oromotor dysfunction due to pseudobulbara palsy • Failure to thrive, malnutrition, constipation • Other: • Fragmented sleep. Bladder/bowel incontinence • Intellectual impairment
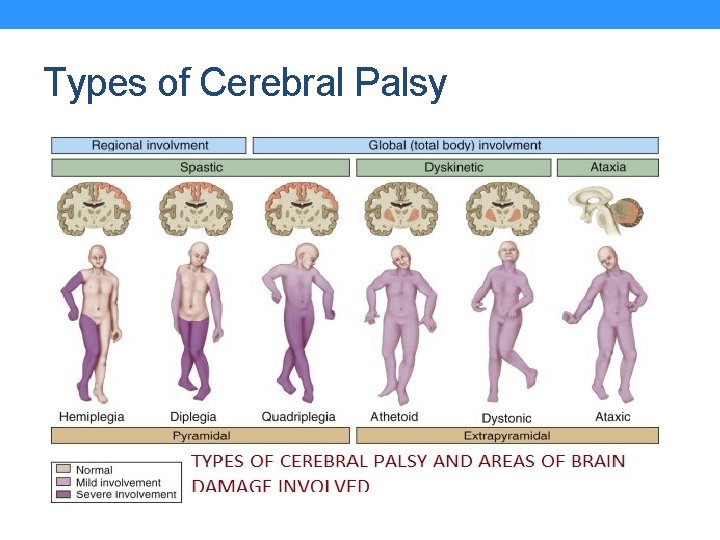
Types of Cerebral Palsy • Spastic: Upper motor neuron damage to corticospinal tracts • Limb hypertonia, brisk reflexes, upward plantars • Clasp knife spasticity • Initially floppy baby • Three subtypes: • Hemiplegic: Unilateral involvement of arm/leg. Neonatal stroke/HIE • Diplegic: Mainly legs involved. HIE or PVL related • Quadriplegic: All 4 limbs affected and trunk involved. Tends to be severe, associated seizures & intellectual impairment. Severe HIE.
Types of Cerebral Palsy • Dyskinetic: Extrapyramidial tracts – basal ganglia • Involuntary, uncontrolled movements • Muscle tone affected less • Chorea, athetoid or dystonic types • Related to hyperbilirubinaemia or HIE • Ataxic: Cerebellum • Related to genetics • Incoordinate movements, intention tremor and ataxic gait
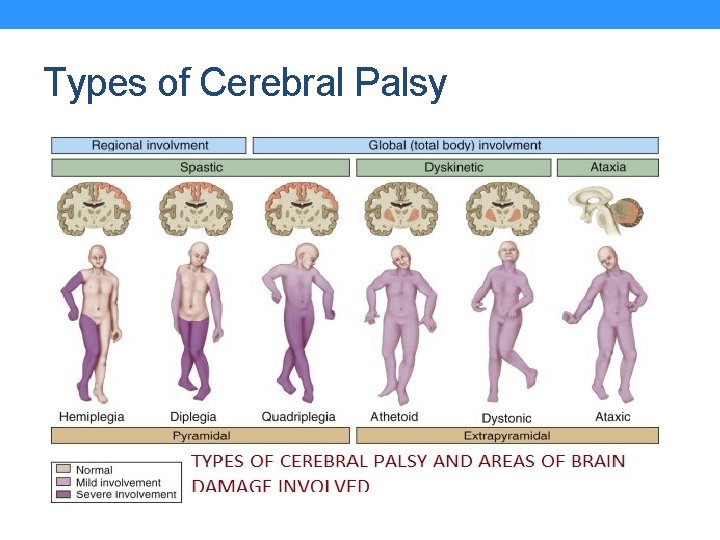
Types of Cerebral Palsy
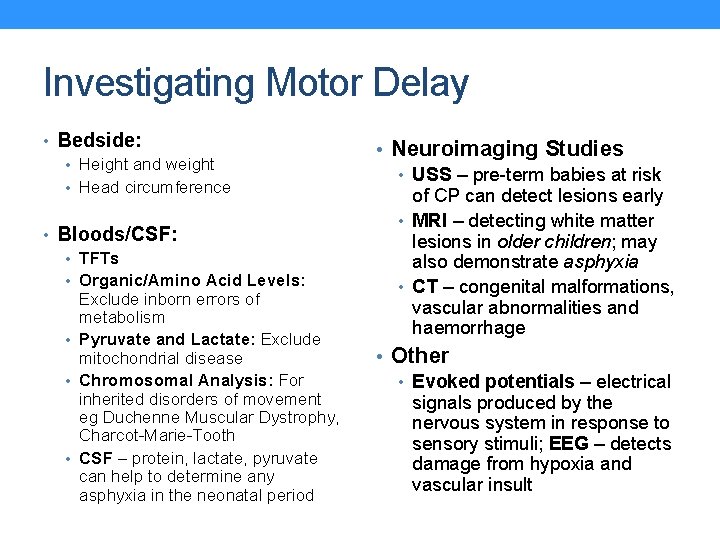
Investigating Motor Delay • Bedside: • Height and weight • Head circumference • Bloods/CSF: • TFTs • Organic/Amino Acid Levels: Exclude inborn errors of metabolism • Pyruvate and Lactate: Exclude mitochondrial disease • Chromosomal Analysis: For inherited disorders of movement eg Duchenne Muscular Dystrophy, Charcot-Marie-Tooth • CSF – protein, lactate, pyruvate can help to determine any asphyxia in the neonatal period • Neuroimaging Studies • USS – pre-term babies at risk of CP can detect lesions early • MRI – detecting white matter lesions in older children; may also demonstrate asphyxia • CT – congenital malformations, vascular abnormalities and haemorrhage • Other • Evoked potentials – electrical signals produced by the nervous system in response to sensory stimuli; EEG – detects damage from hypoxia and vascular insult
Management • MULTIDISCIPLINARY TEAM • Conservative • Mobility aids and splinting • Physical methods of pain • • relief: Heat, cold, vibration SALT: To aid with swallowing/speech Communication Devices Education: Many do not have intellectual impairment and can go to mainstream school; others may need additional educational support Support for family Medical Treatment • Baclofen: Relieving muscle spasm, • Botulism Toxin • Diazepam Surgical Treatment • Last resort for children with severe spasticity or fixed contractures • Repair of scoliosis/hip dislocation • Tendon lengthening • Osteotomy to realign a limb • Selective posterior rhizotomy: Motor nerve root surgery for severe spasticity
Meet Julian… • 8 years old • Has a genetic condition and has frequent follow up • Here today for his check up in general paeds clinic • What do you want to know? ?
Julian’s History • Parents knew that Julian would have his condition before he was born: high risk screening test, and then had amniocentesis • Difficulty feeding at first and had dysmorphic facial features • Was found to have a “hole in the heart” and had to have it repaired when he was 2 years old • Had clicky hips and had to have surgery on his right hip when he was 5 years old • Since his last surgery he has been well • Goes to a mainstream school but gets one to one help
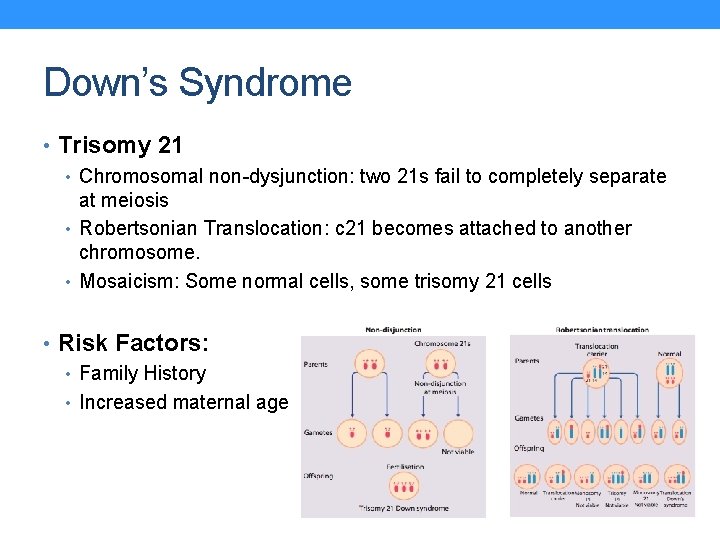
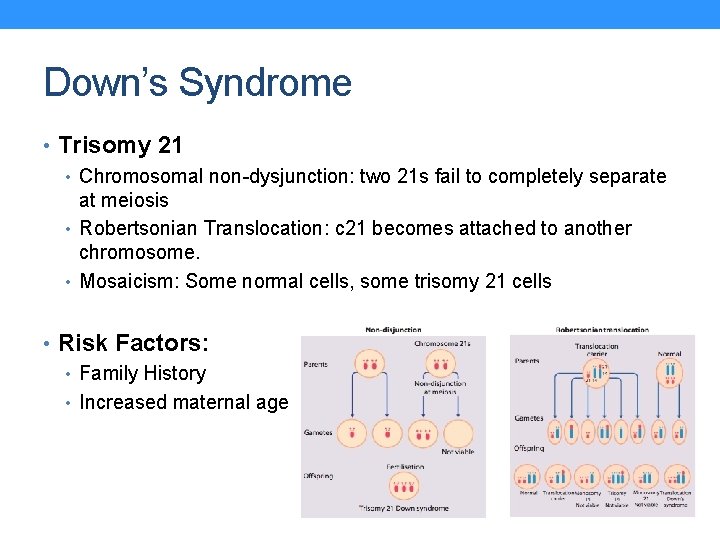
Down’s Syndrome • Trisomy 21 • Chromosomal non-dysjunction: two 21 s fail to completely separate at meiosis • Robertsonian Translocation: c 21 becomes attached to another chromosome. • Mosaicism: Some normal cells, some trisomy 21 cells • Risk Factors: • Family History • Increased maternal age
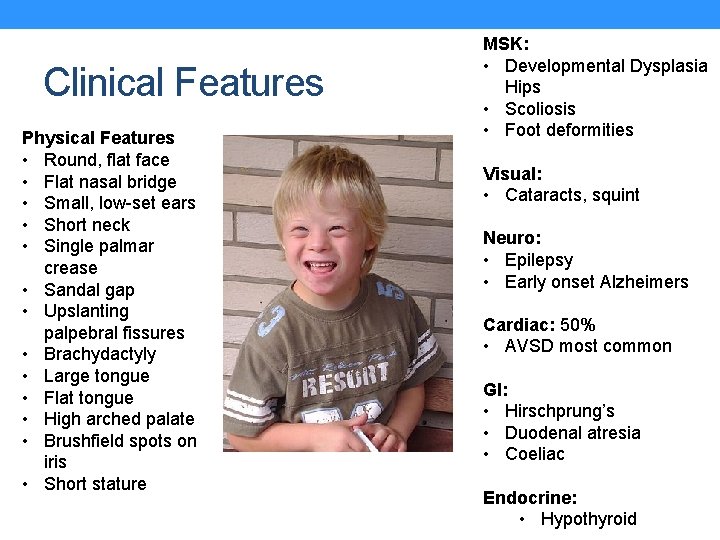
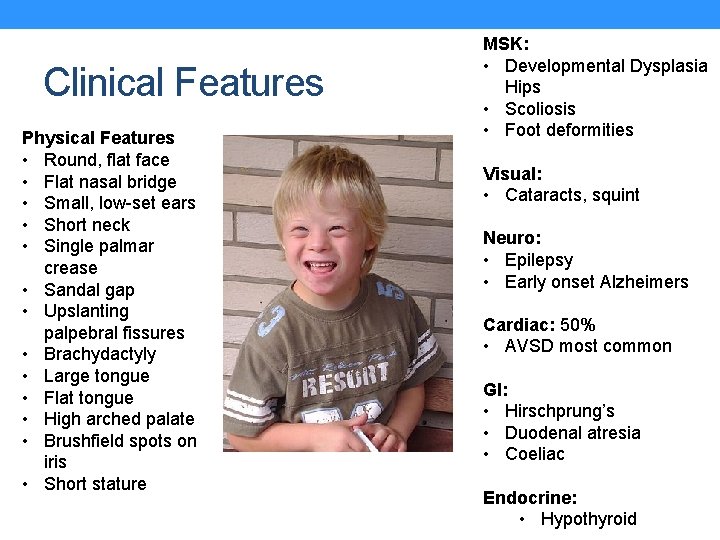
Clinical Features Physical Features • Round, flat face • Flat nasal bridge • Small, low-set ears • Short neck • Single palmar crease • Sandal gap • Upslanting palpebral fissures • Brachydactyly • Large tongue • Flat tongue • High arched palate • Brushfield spots on iris • Short stature MSK: • Developmental Dysplasia Hips • Scoliosis • Foot deformities Visual: • Cataracts, squint Neuro: • Epilepsy • Early onset Alzheimers Cardiac: 50% • AVSD most common GI: • Hirschprung’s • Duodenal atresia • Coeliac Endocrine: • Hypothyroid
Diagnosis Pregnancy Screening: • Combined Screening Test is recommended: • Bloods: Beta-HCG + PAPP-A (10 -14 weeks) • Ultrasound: Nuchal translucency – thickened nuchal fold increases the risk of fetus having Down Syndrome (11 weeks + 2 days – 14 weeks + 1 day) • If high risk CVS or amniocentesis After Birth: • Suspected diagnosis confirmed by a senior paediatrician • Karyotyping: Illustrates additional chromosome 21 • Fluorescent in situ hybridisation (FISH) test: blood test, takes 1 -2 days to return
Management • Education for the parents, • • referral to support services and organisations Schooling: Many able to go to mainstream school with appropriate educational support MDT Approach: Paediatricians, physios, SALT, OT Physiotherapy: Particularly where orthopaedic problems are pronounced Genetic Counselling: For parents, to look for Robertsonian Translocation • Screening for Complications • Cardiac assessment • Hip ultrasound • Audiology • TFTs tested annually • Coeliac Screening • Ophthalmic assessment earlier than normal
Prematurity and Medical Complications • Defined as birth before 37 weeks gestation • Higher risk of medical complications the earlier the baby is born
Respiratory Problems • Surfactant Deficiency: Infant Respiratory Distress Syndrome • Pneumothorax • Apnoea of Prematurity • Bronchopulmonary Dysplasia: “Chronic Lung Disease”; oxygen requirement at 36/40 corrected gestation
Neurological Problems: Pre-Term Brain Injuries • Intraventricular Haemorrhage: Occurs in low birth weight babies and babies <32 weeks. • Leads to hydrocephalus, drowsy, floppy unresponsive baby, seizures • Transfontanelle US in all babies <32 weeks • Treated with ventricular shunts (ventriculoperitoneal) • Hypoxic-Ischaemic Brain Injury: Caused by asphyxia, either pre-delivery, during delivery or post-delivery • Periventricular Leucomalacia: White matter injury caused by severe HIE. Causes spastic diplegic cerebral palsy.
Other complications to be aware of… • GI: • Necrotising Enterocolitis: Premature baby, fed cow’s milk. Immune reaction leading to severe intestinal ischaemia & invasion of bacteria. Vomiting, bloody stool and abdominal distension. TPN and IV Abx • Poor Feeding: Failure to Thrive • Cardiovascular: • Patent Ductus Arteriosus • Other: • Hypoglycaemia: Less glycogen stores • Osteopenia of Prematurity: Depleted calcium/phosphate • Retinopathy of Prematurity: Related to over-oxygenation • Hypothermia: Place in incubator
Asthma • Affects 15 -20% children • Difficult to diagnose in under 5’s (i) Transient Early Wheeze • Viral associated wheeze • Usually resolves by age 5 • RF: maternal smoking, prematurity • Features which increase likelihood of asthma • Diurnal variation • Triggers eg pets, cold, exercise • Atopy
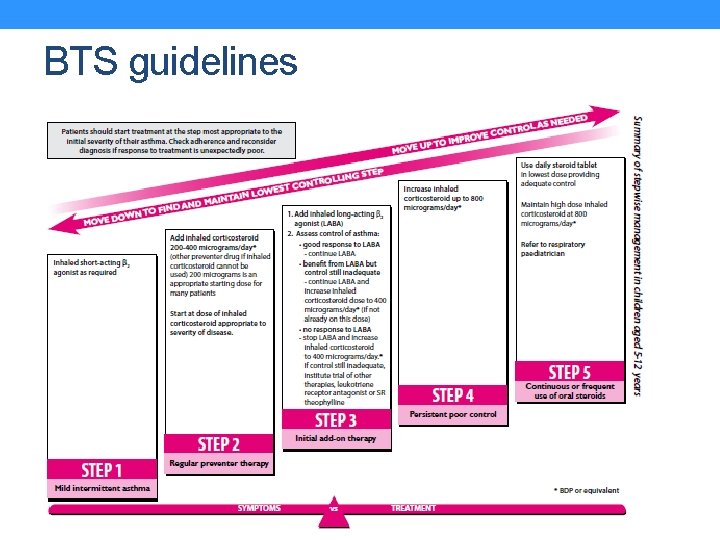
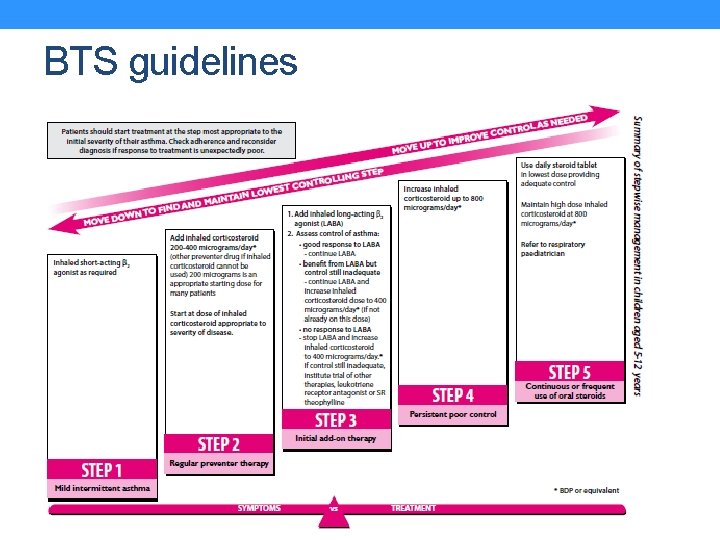
BTS guidelines
Inhaler technique • Wash hands/introduce self/check patient details • Check understand that inhaler contains medication to treat asthma and explain what would like to do • Explanation of technique: • • • Check expiration Shake Sit/stand upright Uncap Put near to mouth and breathe out fully Make seal of lips around inhaler Press canister and inhale deeply simultaneously Hold breath for 10 seconds/as long as can manage Breathe out slowly Repeat if needed. • Demonstration • Watch patient demonstrate technique and make any corrections. • Safety net eg seek emergency help if symptoms not improving with inhaler or requiring more frequently than every 4 hours.
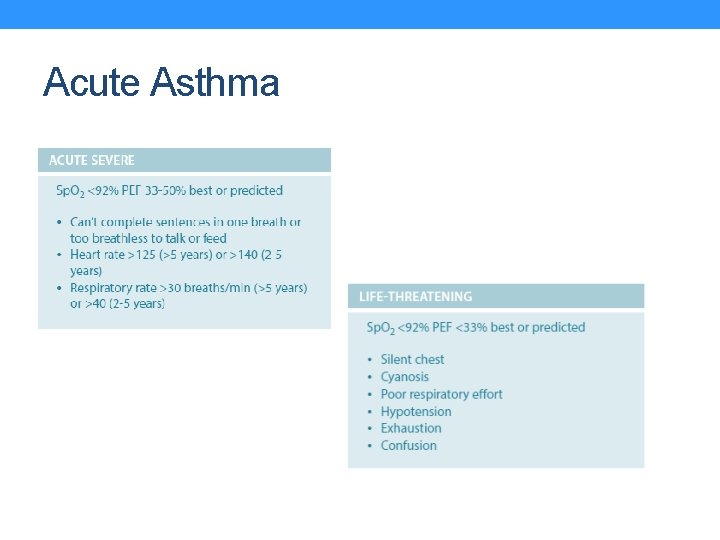
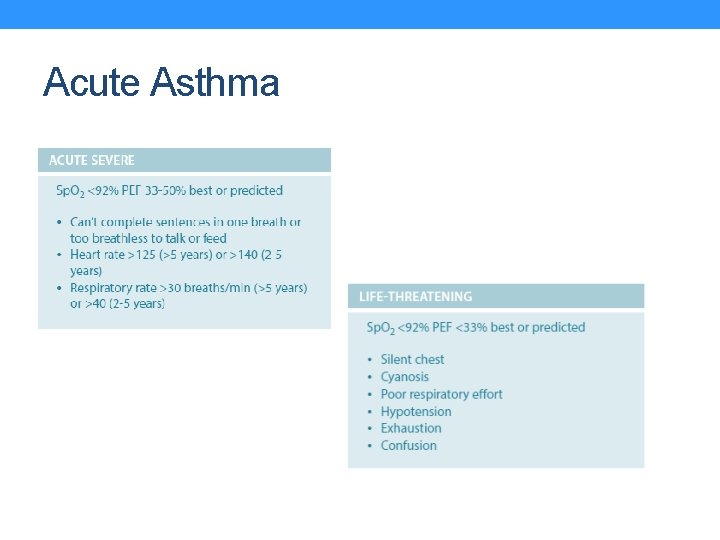
Acute Asthma
Cystic Fibrosis • • • 1 in 2500 births – most common Caucasian genetic disorder All newborn babes screened as part of Guthrie Test Autosomal recessive condition causing deficit in CFTR protein ΔF 508 most common mutation In the lungs, abnormal Na/Cl transport causes thickened mucus – inadequate clearance, prone to infection • 20% patients will present in neonatal period with meconium ileus • Most CF children presents as • Malabsorption • Faltering growth • Recurrent chest infections • Investigations • Sweat test: chloride > 60 mmol/L • Spirometry: obstructive pattern
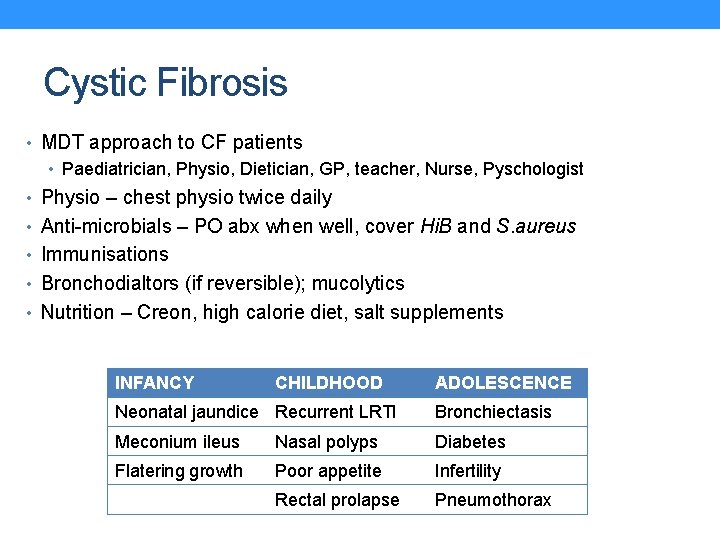
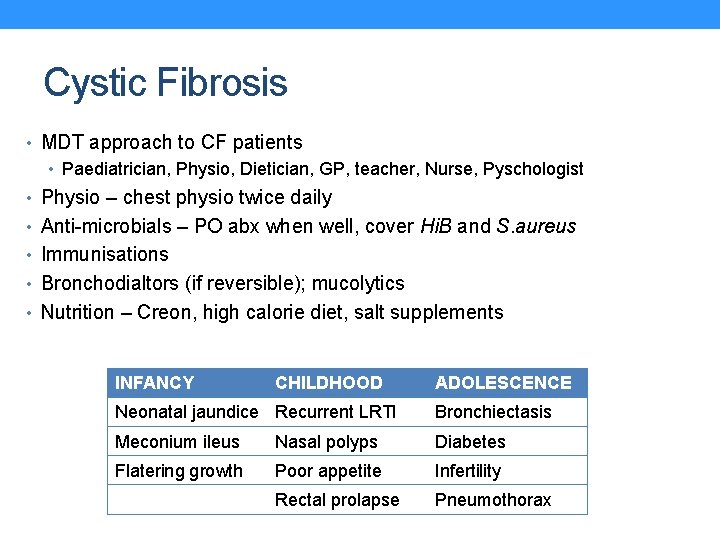
Cystic Fibrosis • MDT approach to CF patients • Paediatrician, Physio, Dietician, GP, teacher, Nurse, Pyschologist • Physio – chest physio twice daily • Anti-microbials – PO abx when well, cover Hi. B and S. aureus • Immunisations • Bronchodialtors (if reversible); mucolytics • Nutrition – Creon, high calorie diet, salt supplements INFANCY CHILDHOOD ADOLESCENCE Neonatal jaundice Recurrent LRTI Bronchiectasis Meconium ileus Nasal polyps Diabetes Flatering growth Poor appetite Infertility Rectal prolapse Pneumothorax

“The Limping Child”
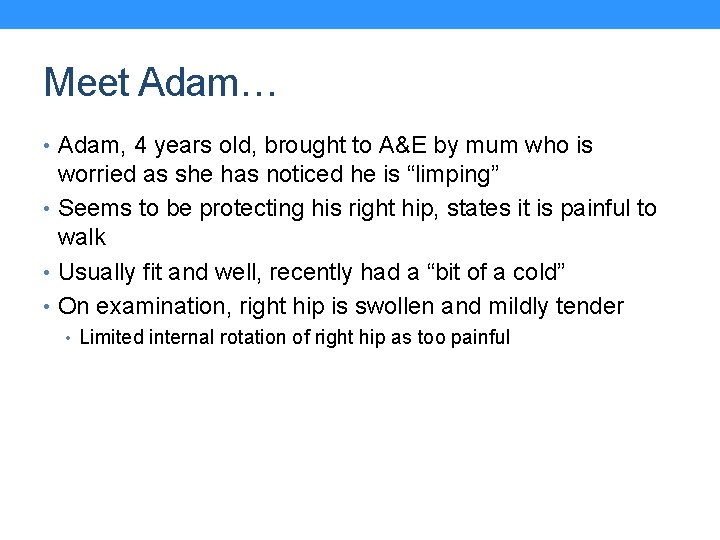
Meet Adam… • Adam, 4 years old, brought to A&E by mum who is worried as she has noticed he is “limping” • Seems to be protecting his right hip, states it is painful to walk • Usually fit and well, recently had a “bit of a cold” • On examination, right hip is swollen and mildly tender • Limited internal rotation of right hip as too painful
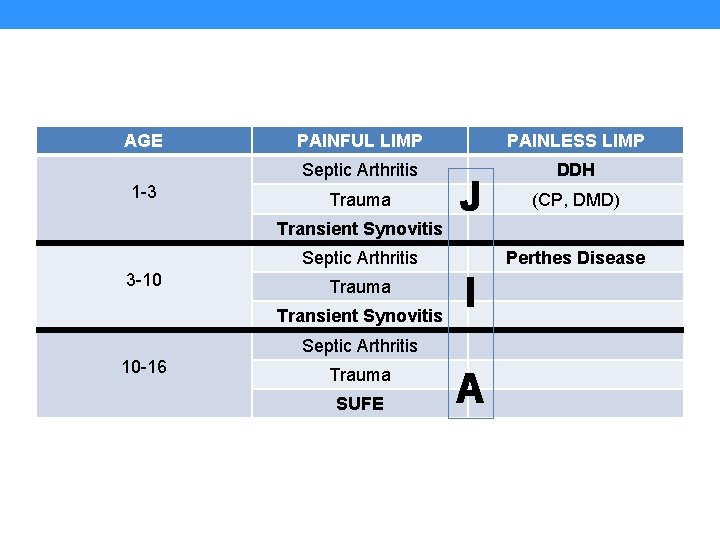
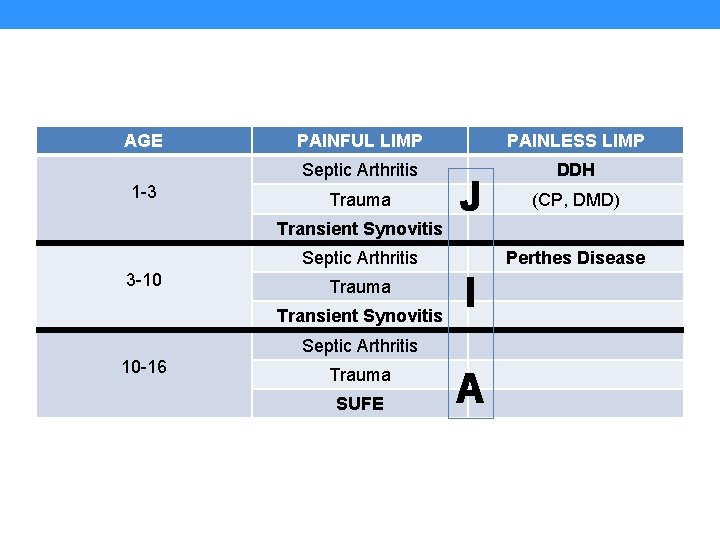
AGE 1 -3 PAINFUL LIMP PAINLESS LIMP Septic Arthritis DDH Trauma Transient Synovitis J Septic Arthritis 3 -10 Trauma Transient Synovitis Perthes Disease I Septic Arthritis 10 -16 Trauma SUFE (CP, DMD) A
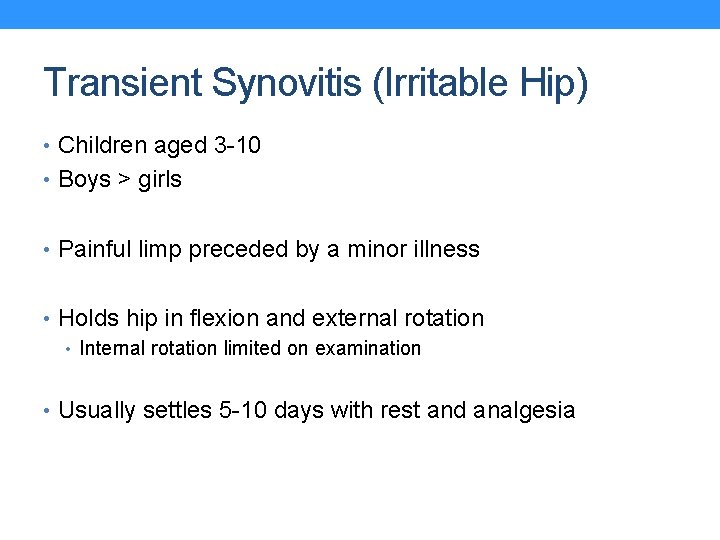
Transient Synovitis (Irritable Hip) • Children aged 3 -10 • Boys > girls • Painful limp preceded by a minor illness • Holds hip in flexion and external rotation • Internal rotation limited on examination • Usually settles 5 -10 days with rest and analgesia
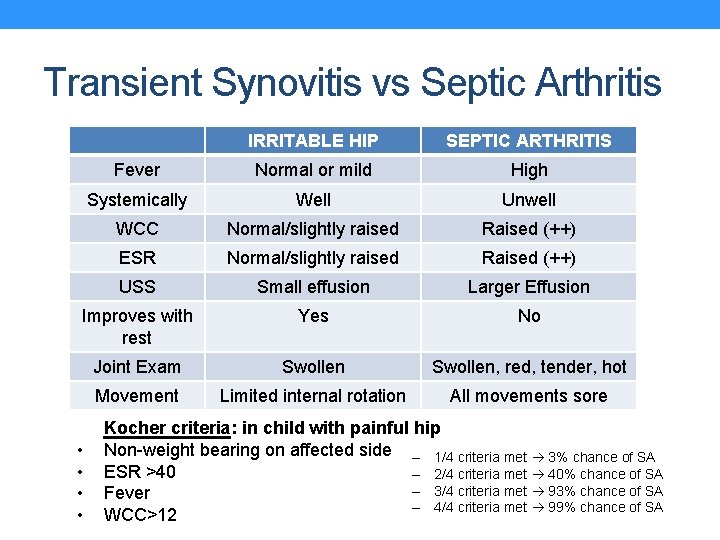
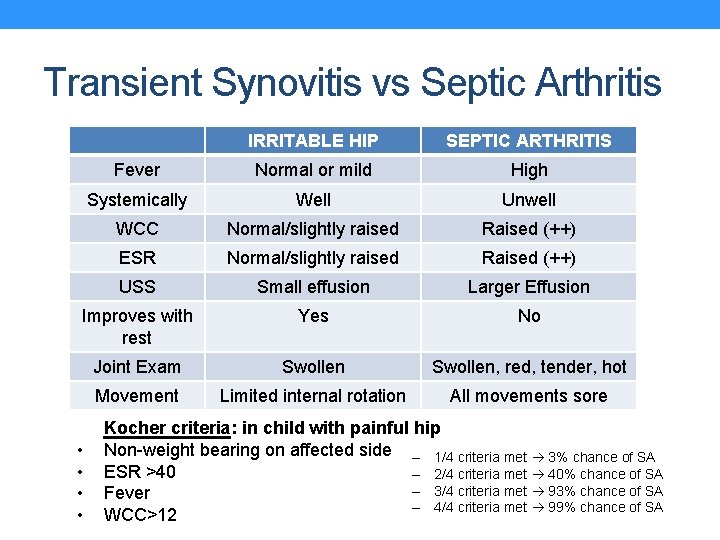
Transient Synovitis vs Septic Arthritis IRRITABLE HIP SEPTIC ARTHRITIS Fever Normal or mild High Systemically Well Unwell WCC Normal/slightly raised Raised (++) ESR Normal/slightly raised Raised (++) USS Small effusion Larger Effusion Improves with rest Yes No Joint Exam Swollen, red, tender, hot Movement Limited internal rotation All movements sore • • Kocher criteria: in child with painful hip Non-weight bearing on affected side – 1/4 criteria met 3% chance of SA ESR >40 – 2/4 criteria met 40% chance of SA – 3/4 criteria met 93% chance of SA Fever – 4/4 criteria met 99% chance of SA WCC>12
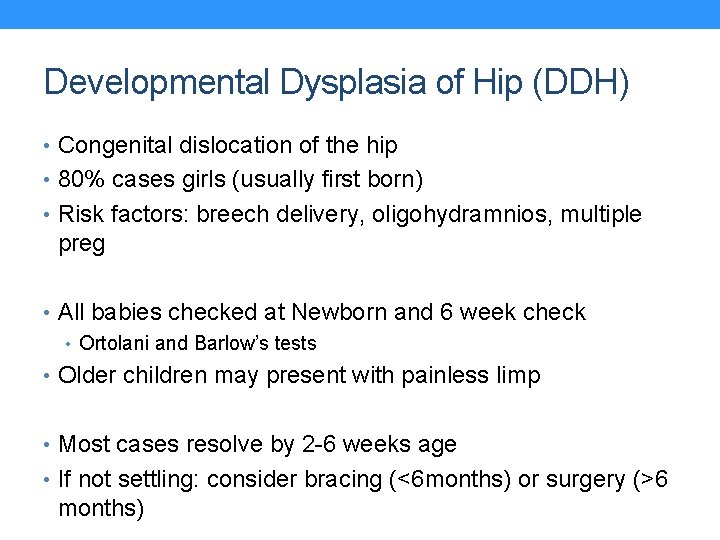
Developmental Dysplasia of Hip (DDH) • Congenital dislocation of the hip • 80% cases girls (usually first born) • Risk factors: breech delivery, oligohydramnios, multiple preg • All babies checked at Newborn and 6 week check • Ortolani and Barlow’s tests • Older children may present with painless limp • Most cases resolve by 2 -6 weeks age • If not settling: consider bracing (<6 months) or surgery (>6 months)
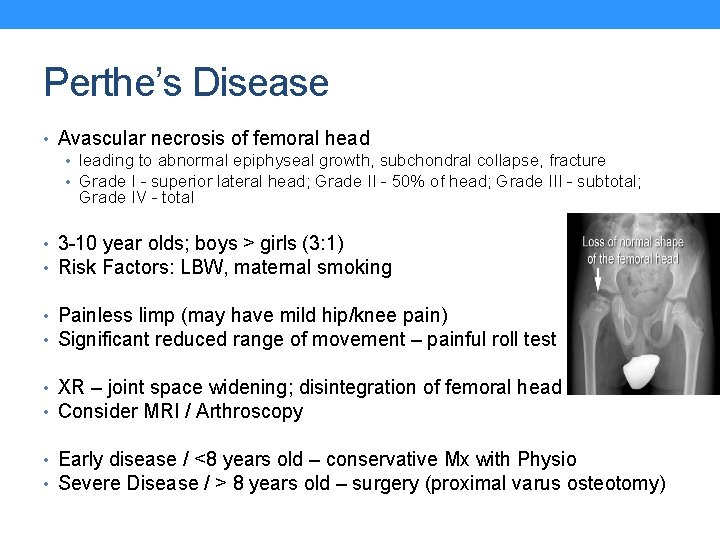
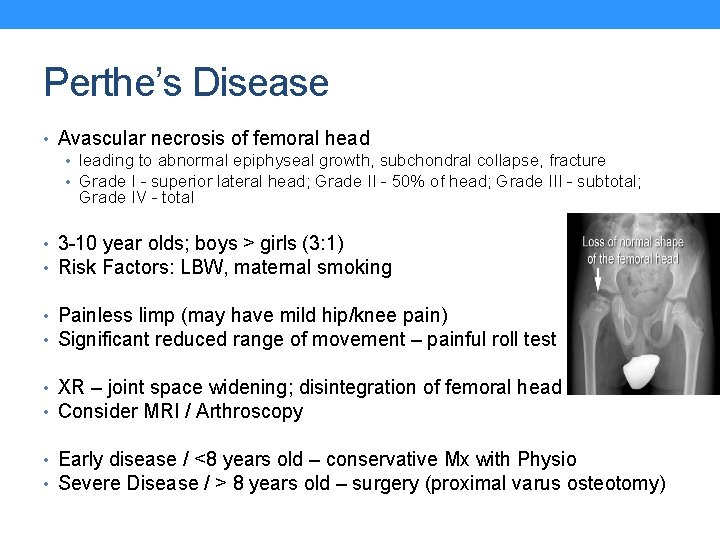
Perthe’s Disease • Avascular necrosis of femoral head • leading to abnormal epiphyseal growth, subchondral collapse, fracture • Grade I - superior lateral head; Grade II - 50% of head; Grade III - subtotal; Grade IV - total • 3 -10 year olds; boys > girls (3: 1) • Risk Factors: LBW, maternal smoking • Painless limp (may have mild hip/knee pain) • Significant reduced range of movement – painful roll test • XR – joint space widening; disintegration of femoral head • Consider MRI / Arthroscopy • Early disease / <8 years old – conservative Mx with Physio • Severe Disease / > 8 years old – surgery (proximal varus osteotomy)
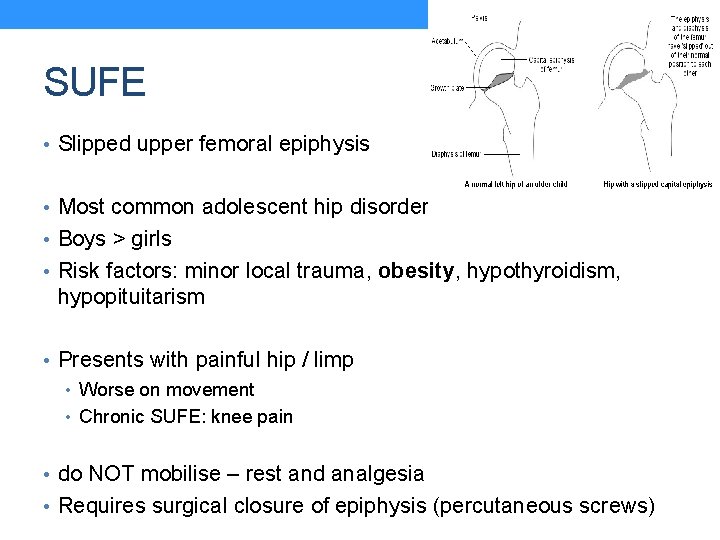
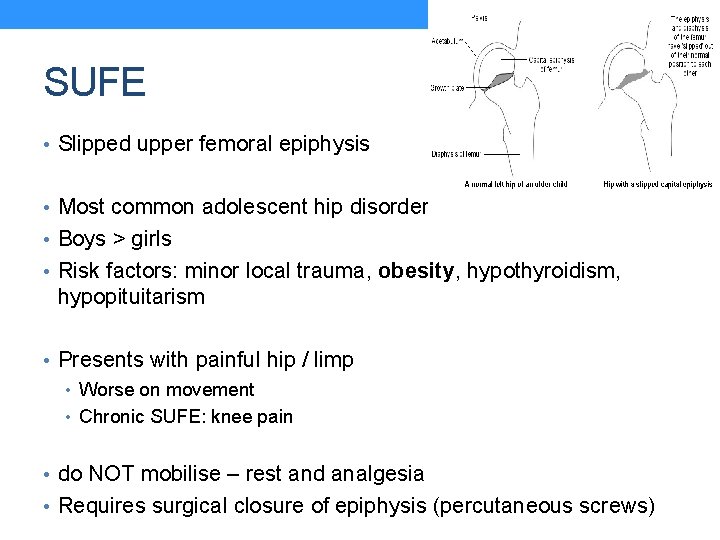
SUFE • Slipped upper femoral epiphysis • Most common adolescent hip disorder • Boys > girls • Risk factors: minor local trauma, obesity, hypothyroidism, hypopituitarism • Presents with painful hip / limp • Worse on movement • Chronic SUFE: knee pain • do NOT mobilise – rest and analgesia • Requires surgical closure of epiphysis (percutaneous screws)
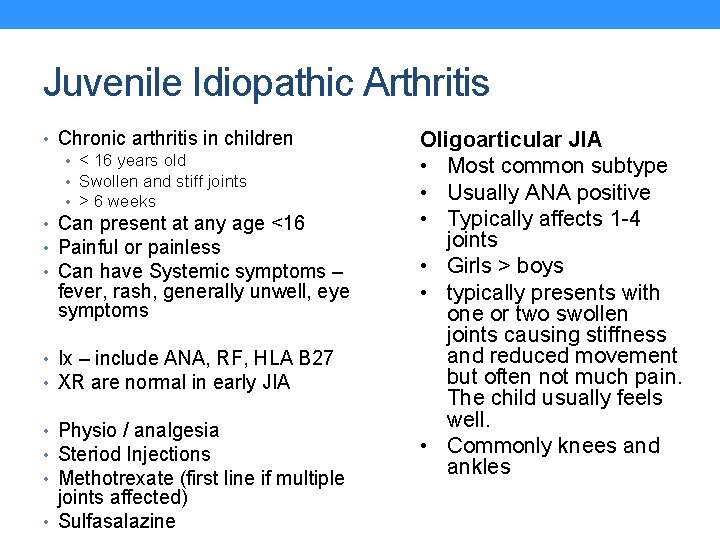
Juvenile Idiopathic Arthritis • Chronic arthritis in children • < 16 years old • Swollen and stiff joints • > 6 weeks • Can present at any age <16 • Painful or painless • Can have Systemic symptoms – fever, rash, generally unwell, eye symptoms • Ix – include ANA, RF, HLA B 27 • XR are normal in early JIA • Physio / analgesia • Steriod Injections • Methotrexate (first line if multiple joints affected) • Sulfasalazine Oligoarticular JIA • Most common subtype • Usually ANA positive • Typically affects 1 -4 joints • Girls > boys • typically presents with one or two swollen joints causing stiffness and reduced movement but often not much pain. The child usually feels well. • Commonly knees and ankles
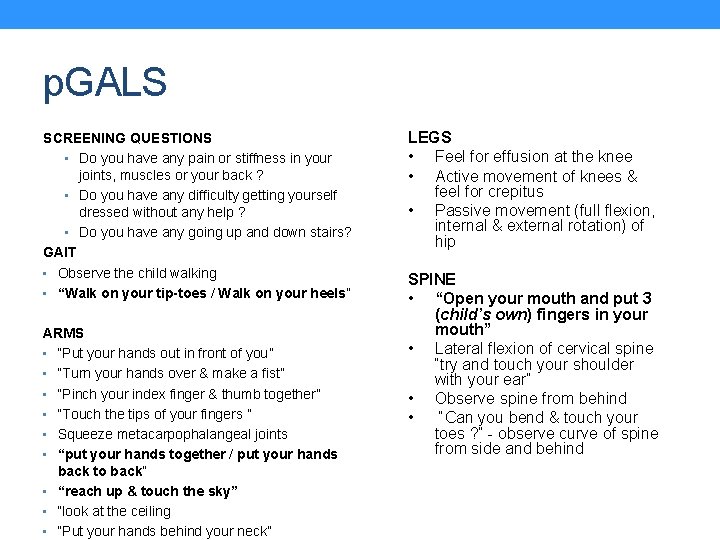
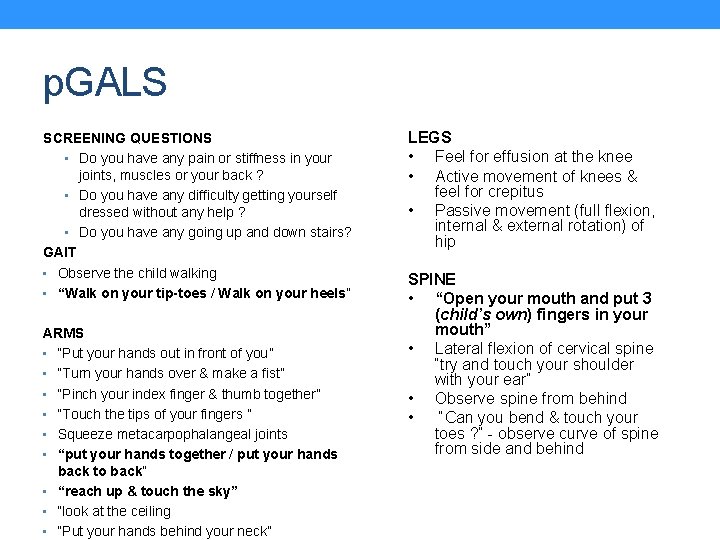
p. GALS SCREENING QUESTIONS • Do you have any pain or stiffness in your joints, muscles or your back ? • Do you have any difficulty getting yourself dressed without any help ? • Do you have any going up and down stairs? GAIT • Observe the child walking • “Walk on your tip-toes / Walk on your heels” ARMS • “Put your hands out in front of you” • “Turn your hands over & make a fist” • “Pinch your index finger & thumb together” • “Touch the tips of your fingers ” • Squeeze metacarpophalangeal joints • “put your hands together / put your hands back to back” • “reach up & touch the sky” • “look at the ceiling • “Put your hands behind your neck” LEGS • Feel for effusion at the knee • Active movement of knees & feel for crepitus • Passive movement (full flexion, internal & external rotation) of hip SPINE • “Open your mouth and put 3 (child’s own) fingers in your mouth” • Lateral flexion of cervical spine “try and touch your shoulder with your ear” • Observe spine from behind • “Can you bend & touch your toes ? ” - observe curve of spine from side and behind
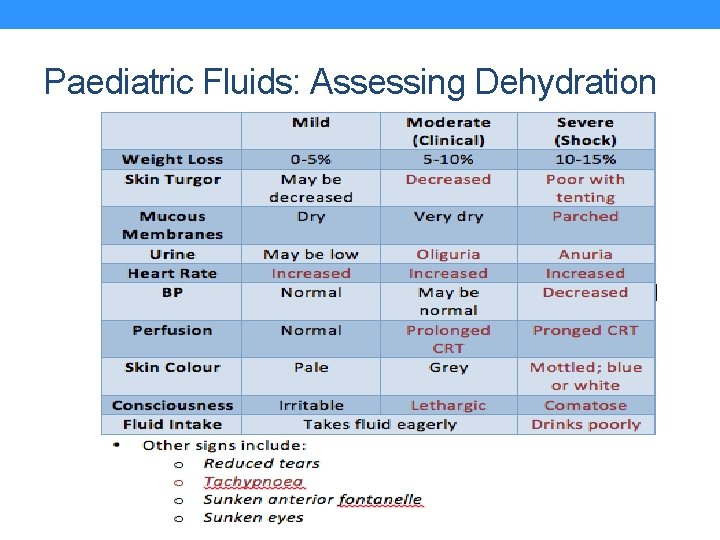
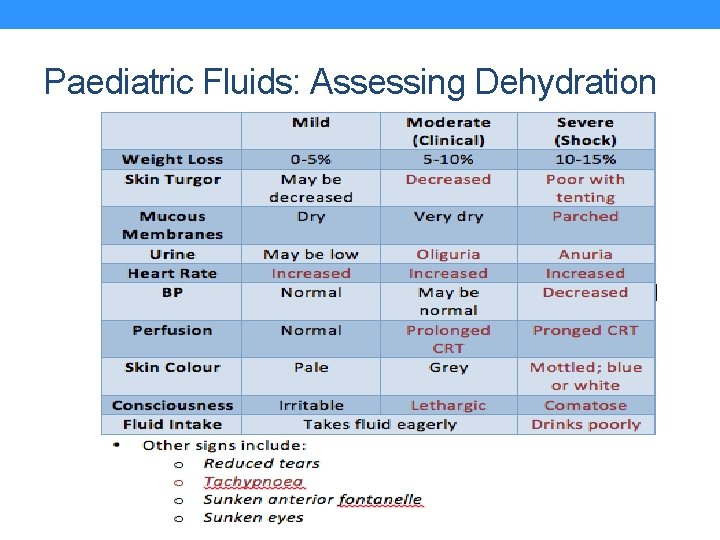
Paediatric Fluids: Assessing Dehydration
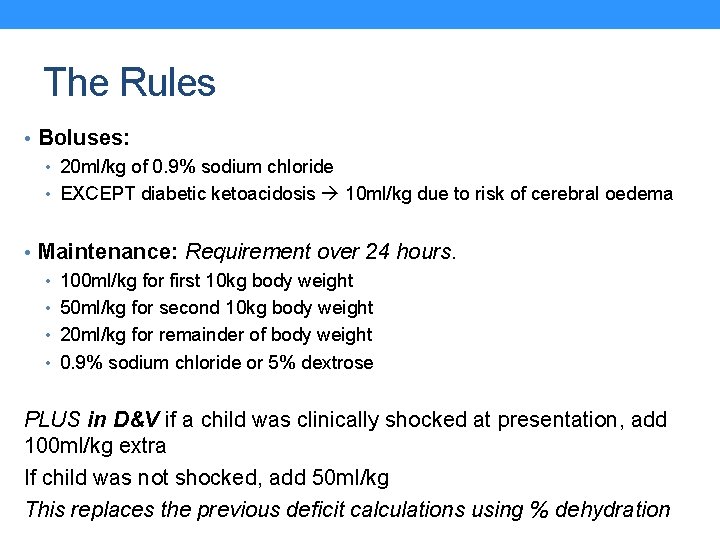
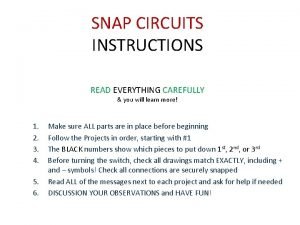
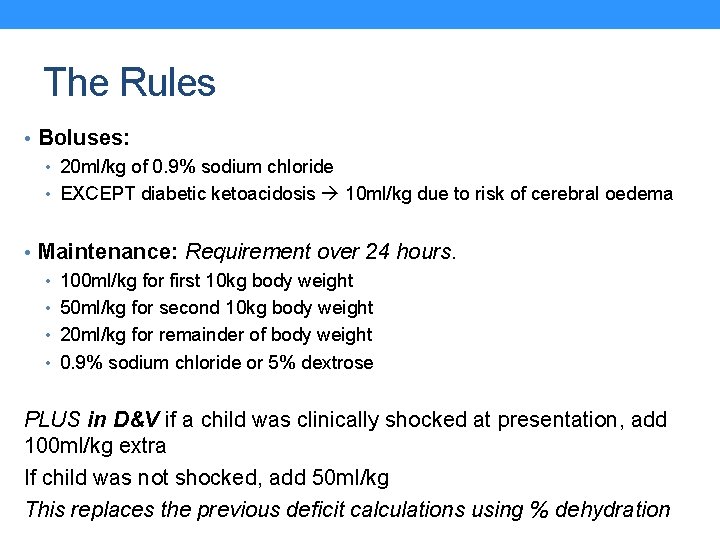
The Rules • Boluses: • 20 ml/kg of 0. 9% sodium chloride • EXCEPT diabetic ketoacidosis 10 ml/kg due to risk of cerebral oedema • Maintenance: Requirement over 24 hours. • 100 ml/kg for first 10 kg body weight • 50 ml/kg for second 10 kg body weight • 20 ml/kg for remainder of body weight • 0. 9% sodium chloride or 5% dextrose PLUS in D&V if a child was clinically shocked at presentation, add 100 ml/kg extra If child was not shocked, add 50 ml/kg This replaces the previous deficit calculations using % dehydration
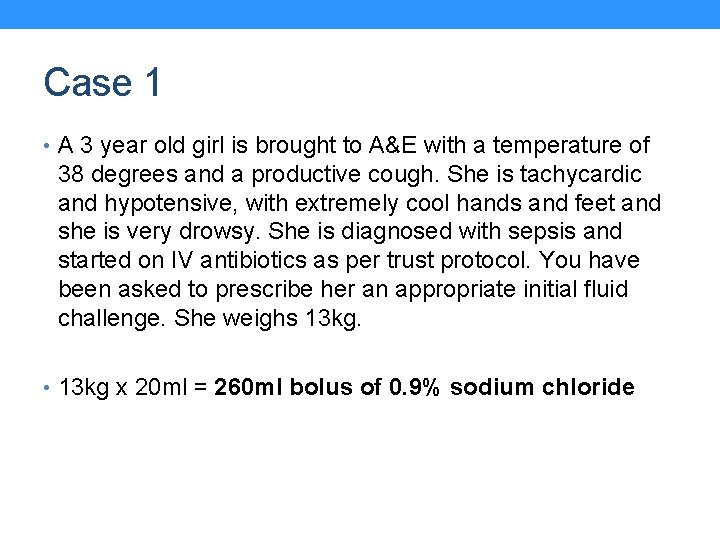
Case 1 • A 3 year old girl is brought to A&E with a temperature of 38 degrees and a productive cough. She is tachycardic and hypotensive, with extremely cool hands and feet and she is very drowsy. She is diagnosed with sepsis and started on IV antibiotics as per trust protocol. You have been asked to prescribe her an appropriate initial fluid challenge. She weighs 13 kg. • 13 kg x 20 ml = 260 ml bolus of 0. 9% sodium chloride
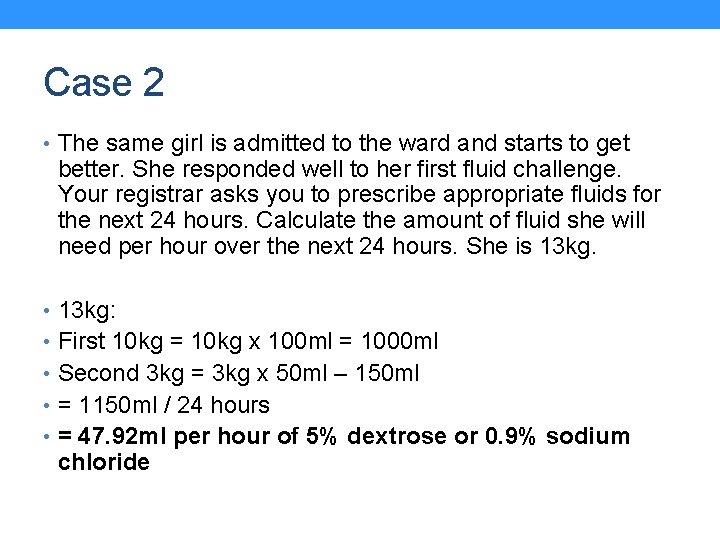
Case 2 • The same girl is admitted to the ward and starts to get better. She responded well to her first fluid challenge. Your registrar asks you to prescribe appropriate fluids for the next 24 hours. Calculate the amount of fluid she will need per hour over the next 24 hours. She is 13 kg. • 13 kg: • First 10 kg = 10 kg x 100 ml = 1000 ml • Second 3 kg = 3 kg x 50 ml – 150 ml • = 1150 ml / 24 hours • = 47. 92 ml per hour of 5% dextrose or 0. 9% sodium chloride
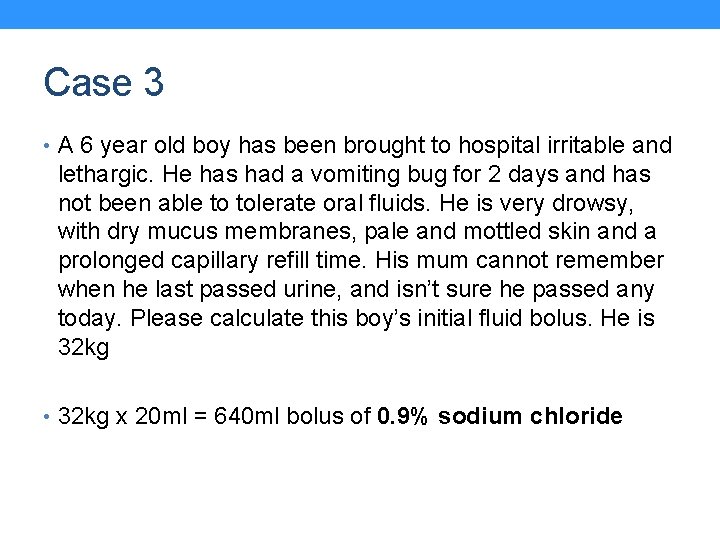
Case 3 • A 6 year old boy has been brought to hospital irritable and lethargic. He has had a vomiting bug for 2 days and has not been able to tolerate oral fluids. He is very drowsy, with dry mucus membranes, pale and mottled skin and a prolonged capillary refill time. His mum cannot remember when he last passed urine, and isn’t sure he passed any today. Please calculate this boy’s initial fluid bolus. He is 32 kg • 32 kg x 20 ml = 640 ml bolus of 0. 9% sodium chloride
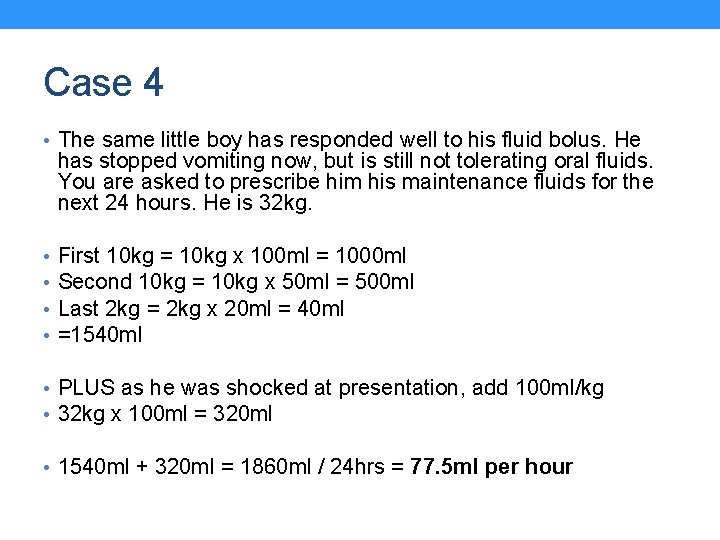
Case 4 • The same little boy has responded well to his fluid bolus. He has stopped vomiting now, but is still not tolerating oral fluids. You are asked to prescribe him his maintenance fluids for the next 24 hours. He is 32 kg. • • First 10 kg = 10 kg x 100 ml = 1000 ml Second 10 kg = 10 kg x 50 ml = 500 ml Last 2 kg = 2 kg x 20 ml = 40 ml =1540 ml • PLUS as he was shocked at presentation, add 100 ml/kg • 32 kg x 100 ml = 320 ml • 1540 ml + 320 ml = 1860 ml / 24 hrs = 77. 5 ml per hour
Quiz Time…. • We will cover: • Paediatric Dermatology • Vaccinations • Common Pathogens

Name the rash. . . Dermatitis Measles Varicella (chicken-pox) Rubella (German Measles) Psoriasis Erythema infectiosum/fifth disease

Name the rash. . . Varicella (chicken-pox) Rubella (German Measles) Measles Dermatitis Psoriasis Erythema infectiosum/fifth disease
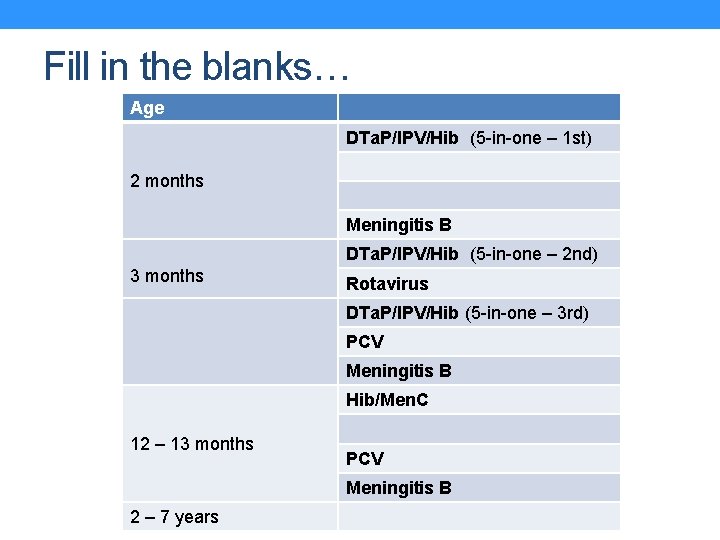
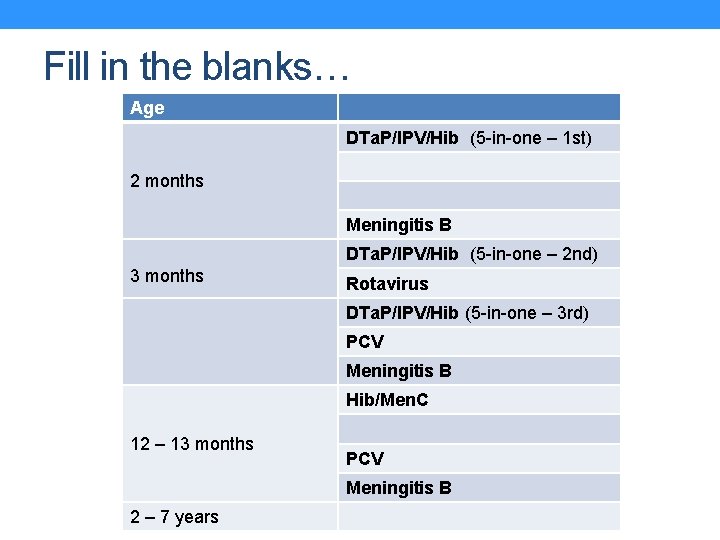
Fill in the blanks… Age DTa. P/IPV/Hib (5 -in-one – 1 st) 2 months Meningitis B DTa. P/IPV/Hib (5 -in-one – 2 nd) 3 months Rotavirus DTa. P/IPV/Hib (5 -in-one – 3 rd) PCV Meningitis B Hib/Men. C 12 – 13 months PCV Meningitis B 2 – 7 years
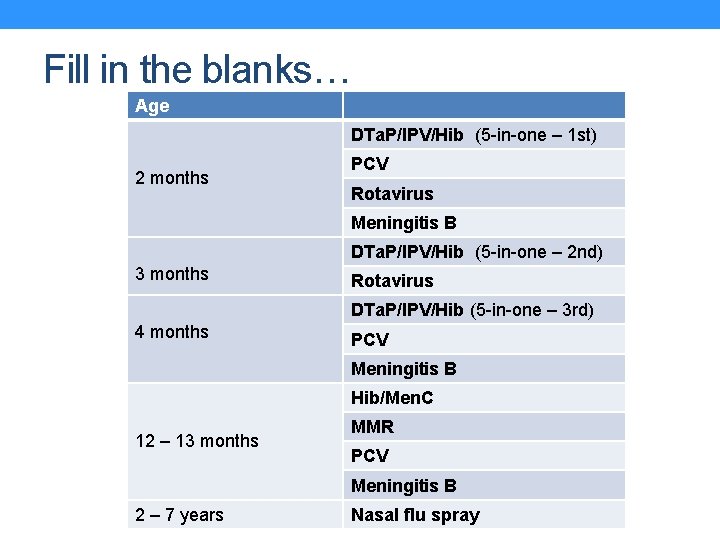
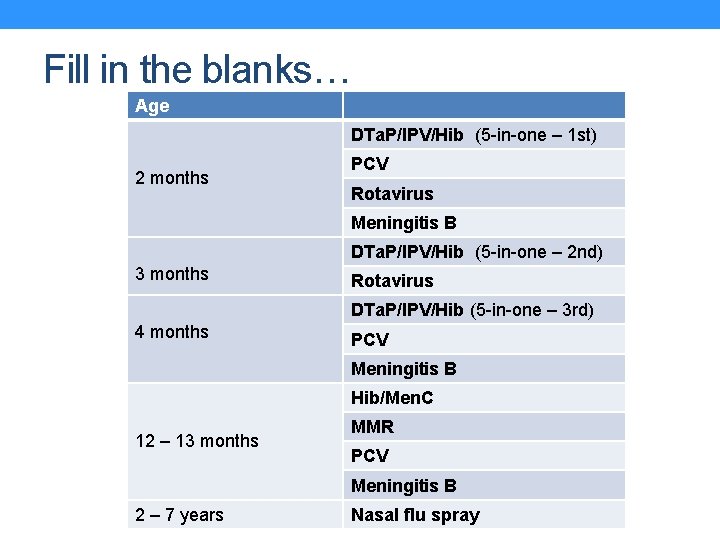
Fill in the blanks… Age DTa. P/IPV/Hib (5 -in-one – 1 st) 2 months PCV Rotavirus Meningitis B DTa. P/IPV/Hib (5 -in-one – 2 nd) 3 months Rotavirus DTa. P/IPV/Hib (5 -in-one – 3 rd) 4 months PCV Meningitis B Hib/Men. C 12 – 13 months MMR PCV Meningitis B 2 – 7 years Nasal flu spray
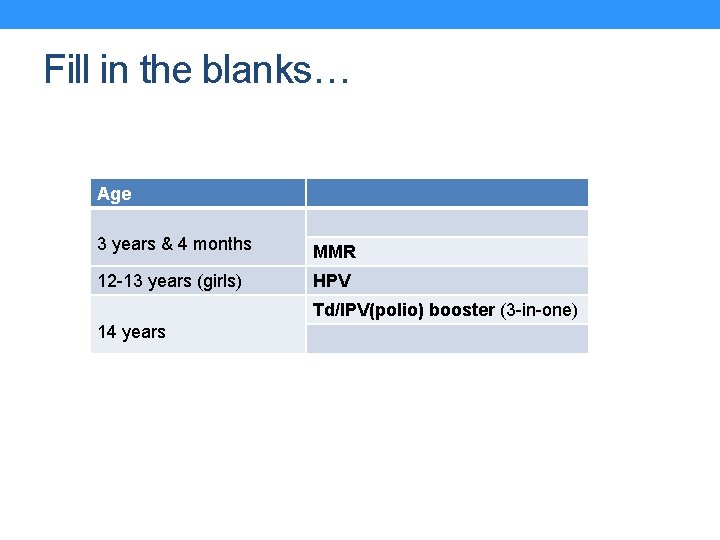
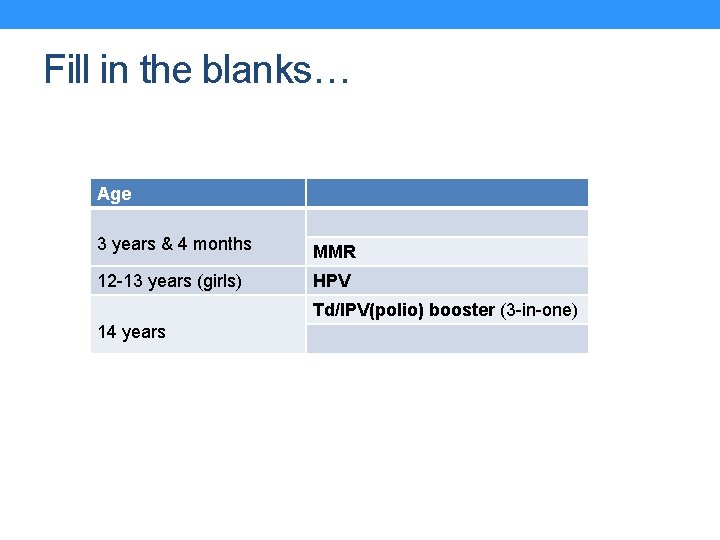
Fill in the blanks… Age 3 years & 4 months MMR 12 -13 years (girls) HPV Td/IPV(polio) booster (3 -in-one) 14 years
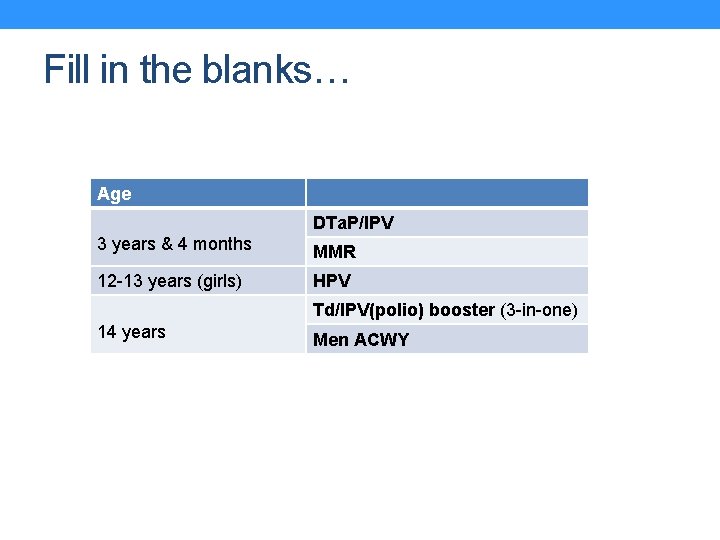
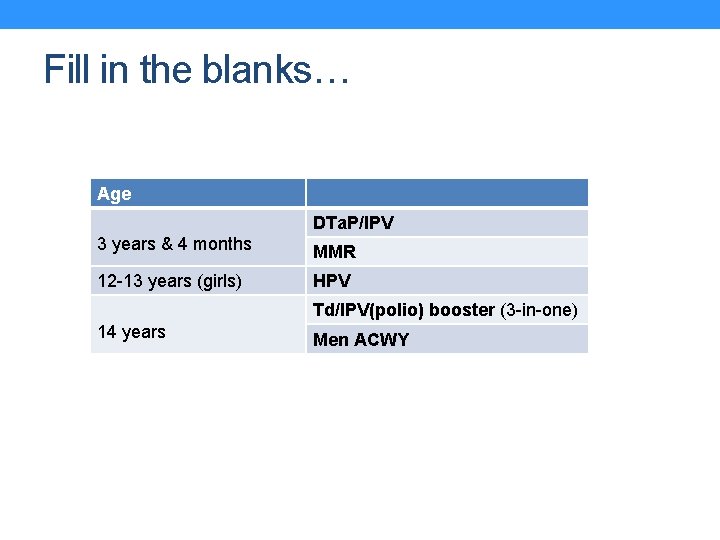
Fill in the blanks… Age DTa. P/IPV 3 years & 4 months MMR 12 -13 years (girls) HPV Td/IPV(polio) booster (3 -in-one) 14 years Men ACWY
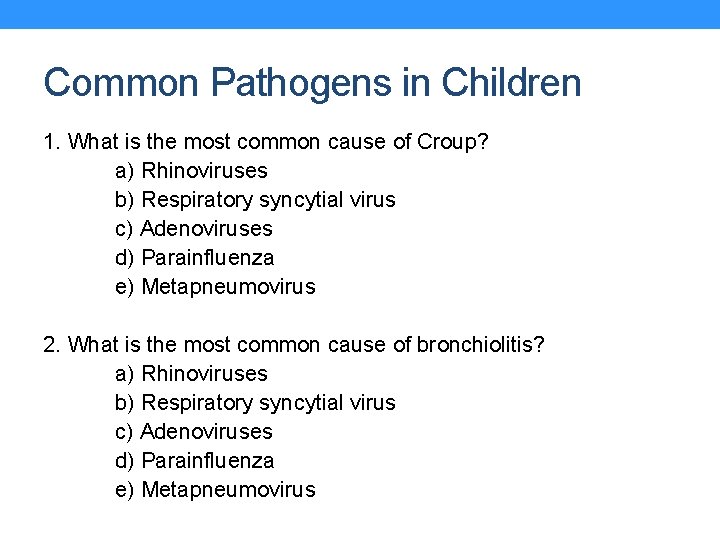
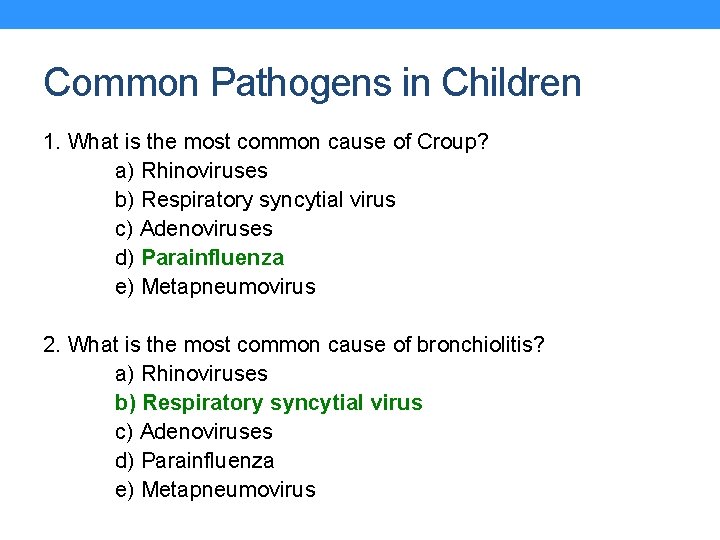
Common Pathogens in Children 1. What is the most common cause of Croup? a) Rhinoviruses b) Respiratory syncytial virus c) Adenoviruses d) Parainfluenza e) Metapneumovirus 2. What is the most common cause of bronchiolitis? a) Rhinoviruses b) Respiratory syncytial virus c) Adenoviruses d) Parainfluenza e) Metapneumovirus
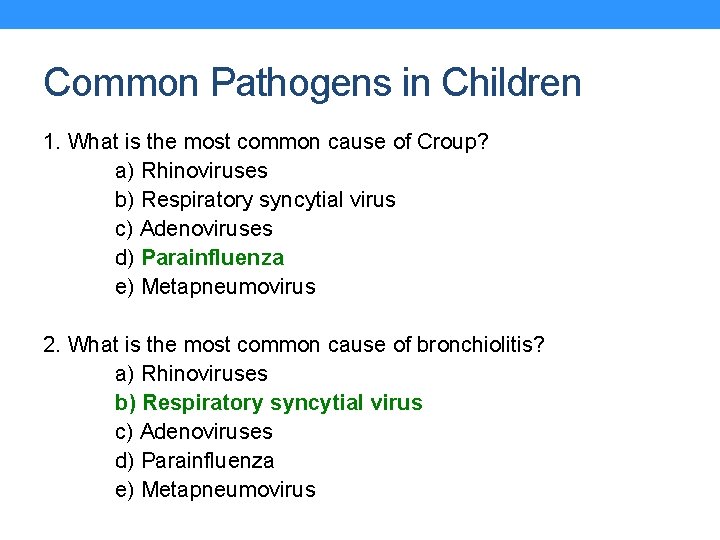
Common Pathogens in Children 1. What is the most common cause of Croup? a) Rhinoviruses b) Respiratory syncytial virus c) Adenoviruses d) Parainfluenza e) Metapneumovirus 2. What is the most common cause of bronchiolitis? a) Rhinoviruses b) Respiratory syncytial virus c) Adenoviruses d) Parainfluenza e) Metapneumovirus

THANK YOU ANY QUESTIONS? Craig. Anderson@chsft. nhs. uk Monica. Parker@nuth. nhs. uk
 Tour escort jobs
Tour escort jobs History world tour
History world tour Shanghai world financial tour eiffel tour petronas
Shanghai world financial tour eiffel tour petronas Paed
Paed Lectures paediatrics
Lectures paediatrics Polysyllabic babble
Polysyllabic babble London school of paediatrics
London school of paediatrics History taking paediatrics
History taking paediatrics Prelim, midterm finals grading system
Prelim, midterm finals grading system Rvba pennant finals
Rvba pennant finals Sbu finals schedule
Sbu finals schedule One stop teacher shop
One stop teacher shop Aperture stop
Aperture stop A tea kettle begins to whistle physical or chemical change
A tea kettle begins to whistle physical or chemical change Traffic whistle signals
Traffic whistle signals Faster than fairies
Faster than fairies A policeman's whistle has a _____.
A policeman's whistle has a _____. Paralell circuit
Paralell circuit F f# g g# a a#
F f# g g# a a# Inadvertant whistle
Inadvertant whistle Bean whistle
Bean whistle Cooker whistle counter app
Cooker whistle counter app Business ethics whistle blowing
Business ethics whistle blowing Nascent soap emulsion
Nascent soap emulsion Windy whistle
Windy whistle The referee blew his whistle
The referee blew his whistle Whistle
Whistle Kalimat berobjek adalah
Kalimat berobjek adalah Upward movement of the internal phase of emulsion
Upward movement of the internal phase of emulsion Trög för kemist
Trög för kemist Vad är ett minoritetsspråk
Vad är ett minoritetsspråk Ledarskapsteorier
Ledarskapsteorier Datorkunskap för nybörjare
Datorkunskap för nybörjare Indikation för kejsarsnitt på moderns önskan
Indikation för kejsarsnitt på moderns önskan Returpilarna
Returpilarna Steg för steg rita
Steg för steg rita Iso 22301 utbildning
Iso 22301 utbildning Redogör för vad psykologi är
Redogör för vad psykologi är Bästa kameran för astrofoto
Bästa kameran för astrofoto Lek med former i förskolan
Lek med former i förskolan Svenskt ramverk för digital samverkan
Svenskt ramverk för digital samverkan Klassen rim
Klassen rim Nyckelkompetenser för livslångt lärande
Nyckelkompetenser för livslångt lärande Mantel för kvinnor i antikens rom
Mantel för kvinnor i antikens rom Tidbok för yrkesförare
Tidbok för yrkesförare Modell för handledningsprocess
Modell för handledningsprocess Vilken grundregel finns det för tronföljden i sverige?
Vilken grundregel finns det för tronföljden i sverige? Ministerstyre för och nackdelar
Ministerstyre för och nackdelar Bamse för de yngsta
Bamse för de yngsta Verktyg för automatisering av utbetalningar
Verktyg för automatisering av utbetalningar Tillitsbaserad ledning
Tillitsbaserad ledning Kanaans land
Kanaans land Cellorov
Cellorov Stig kerman
Stig kerman Sju för caesar
Sju för caesar Varför kallas perioden 1918-1939 för mellankrigstiden?
Varför kallas perioden 1918-1939 för mellankrigstiden? Verksamhetsanalys exempel
Verksamhetsanalys exempel Matematisk modellering eksempel
Matematisk modellering eksempel Cks
Cks Shaktismen
Shaktismen Jag har nigit för nymånens skära text
Jag har nigit för nymånens skära text Inköpsprocessen steg för steg
Inköpsprocessen steg för steg Påbyggnader för flakfordon
Påbyggnader för flakfordon Strategi för svensk viltförvaltning
Strategi för svensk viltförvaltning A gastrica
A gastrica Relativ standardavvikelse formel
Relativ standardavvikelse formel Typiska novell drag
Typiska novell drag Tack för att ni har lyssnat
Tack för att ni har lyssnat Rutin för avvikelsehantering
Rutin för avvikelsehantering Myndigheten för delaktighet
Myndigheten för delaktighet Läkarutlåtande för livränta
Läkarutlåtande för livränta