Management of Alcohol Use Disorders Educational Rounds for
- Slides: 68
Management of Alcohol Use Disorders Educational Rounds for Primary Care Physicians META: PHI 2015
About META: PHI Mentoring, Education, and Clinical Tools for Addiction: Primary Care–Hospital Integration • Goals: – Promote evidence-based addiction medicine treatment – Implement care pathways between the ED, hospital, WMS, primary care, and rapid access addiction medicine clinics • Seven sites in Ontario are currently involved, with plans to expand the spread of the project in the future • Funding and support provided by the Adopting Research to Improve Care (ARTIC) program (Council of Academic Hospitals of Ontario & Health Quality Ontario) https: //www. porticonetwork. ca/web/meta-phi META: PHI 2015
Sign-In Sheet • META: PHI mailing list: Forum for project team and other health care providers to discuss clinical cases, policies, and events related to addiction • All attendees invited to participate: Write name/e-mail address on sheet to be added META: PHI 2015
OVERVIEW META: PHI 2015
Managing Substance Use in Primary Care • Primary care ideal setting for treating substance use disorders – Other health concerns can also be addressed – Length of treatment more important than intensity of treatment – Patients prefer primary care setting META: PHI 2015
Current Practice in Primary Care • PCPs treat medical complications of addiction and provide referrals to psychosocial programs • PCPs generally do not provide anti-craving medications for alcohol or opioid dependence • PCPs tend to view substance misuse as a purely psychosocial or behavioural problem (i. e. not their problem to treat) • Addiction falls within the purview of PCPs – Like any other complex chronic illness, PCPs should treat underlying disorder as well as complications • Prescribe pharmacotherapy as appropriate • Refer to specialist if necessary • Provide long-term follow-up META: PHI 2015
Alcohol Use in Canada • Alcohol misuse a significant preventable cause of disease and death in Canada – Associated with liver disease, motor vehicle accidents, intimate partner violence, depression • Estimated direct health care cost of alcohol misuse in 2002 = $3. 3 billion (2) META: PHI 2015
PCP Goals for Managing Patients’ Alcohol Use 1. Screen all patients for problematic alcohol use at least once per year 2. Screen patients who present with medical or psychosocial problems that could be connected to problematic alcohol use 3. Diagnose patients with at-risk drinking or alcohol use disorder (AUD) 4. Offer patients with AUD appropriate counselling, pharmacotherapy, and referral META: PHI 2015
CANADIAN LOW-RISK DRINKING GUIDELINES META: PHI 2015
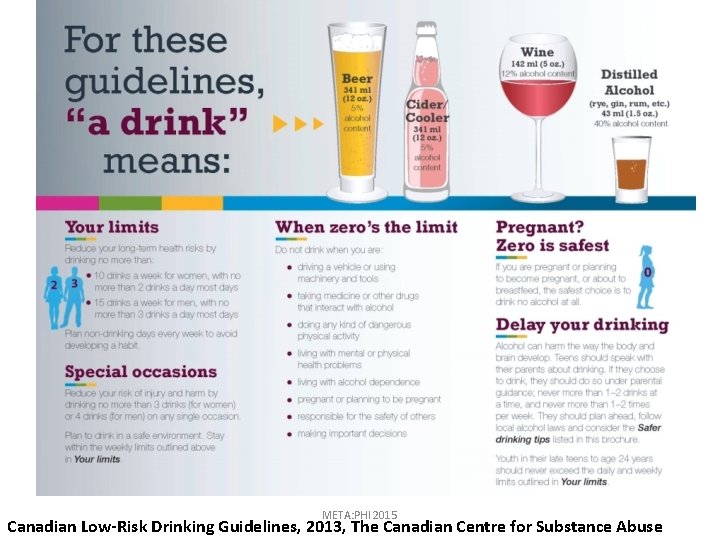
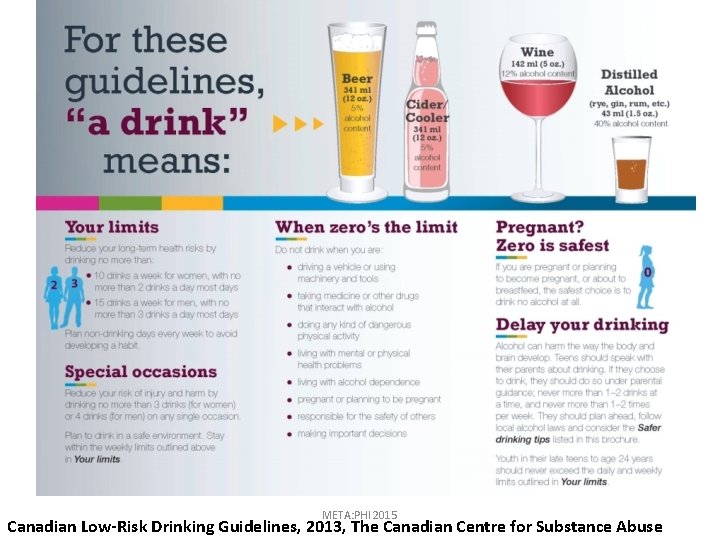
META: PHI 2015 Canadian Low-Risk Drinking Guidelines, 2013, The Canadian Centre for Substance Abuse
Summary • Men: No more than 3 drinks/day, no more than 15 drinks/week • Women: No more than 2 drinks/day, no more than 10 drinks/week • Exceeding these limits increases risk of alcohol -related harm – Approximately 14% of Canadians aged 15+ drink in excess of the low-risk guidelines (3) META: PHI 2015
DIAGNOSTIC SPECTRUM OF ALCOHOL USE META: PHI 2015
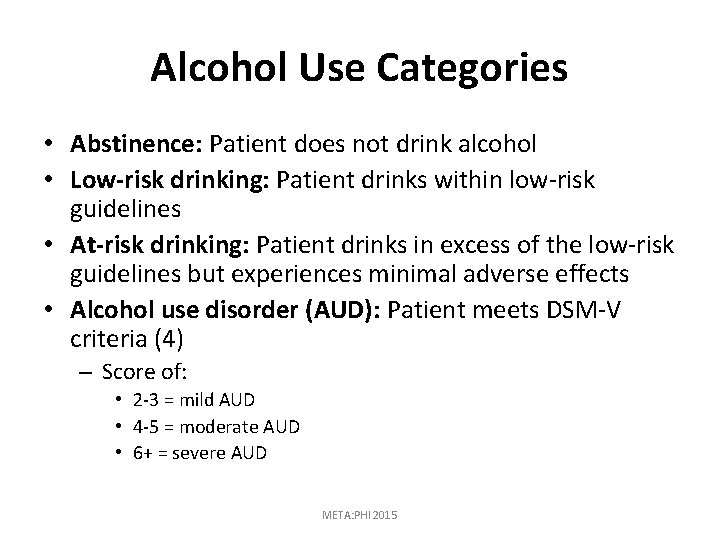
Alcohol Use Categories • Abstinence: Patient does not drink alcohol • Low-risk drinking: Patient drinks within low-risk guidelines • At-risk drinking: Patient drinks in excess of the low-risk guidelines but experiences minimal adverse effects • Alcohol use disorder (AUD): Patient meets DSM-V criteria (4) – Score of: • 2 -3 = mild AUD • 4 -5 = moderate AUD • 6+ = severe AUD META: PHI 2015
Alcohol Use Disorder DSM-V Criteria: Impaired Control • Alcohol is taken in larger amounts or for a longer period than intended • There is a persistent desire or unsuccessful efforts to cut down or control alcohol use • A great deal of time is spent in activities necessary to obtain alcohol, use alcohol, or control alcohol use • There are cravings or a strong desire to use alcohol META: PHI 2015
Alcohol Use Disorder DSM-V Criteria: Social Impairment • There is recurrent alcohol use resulting in a failure to fulfill important role obligations at work, school, or home • There is continued use despite persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of alcohol • Important social, occupational, or recreational activities are given up or reduced because of alcohol use META: PHI 2015
Alcohol Use Disorder DSM-V Criteria: Risky Use • There is recurrent alcohol use in situations where it is physically hazardous • Alcohol use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is caused or exacerbated by alcohol META: PHI 2015
Alcohol Use Disorder DSM-V Criteria: Physiological Dependence • Tolerance: There is either a need for markedly increased amounts of alcohol to achieve intoxication or desired effect or there is a markedly diminished effect with continued use of the same amount of alcohol • Withdrawal: There is either characteristic withdrawal syndrome for alcohol is taken to relieve or avoid withdrawal symptoms META: PHI 2015
SCREENING FOR PROBLEMATIC ALCOHOL USE META: PHI 2015
Single-item Screening Test • All patients should be screened at least yearly with a validated single-item screening test “How many times in past year have you had 5 (men)/4 (women) drinks in one day? ” (5) • Positive screen: once or more META: PHI 2015
Alcohol History • Combined screening and alcohol consumption history has higher detection rates than screening alone (6) • Can help determine between at-risk drinking and AUD • Consumption history helps to monitor changes in patients’ patterns META: PHI 2015
Taking an Alcohol History • Ask all patients (women and elderly most likely to be missed) • Ask daily or weekly amount – For vague responses, ask about previous week’s drinking, and/or present wide range of possible consumption (“Would you say your drinking is more on the order of 14 drinks or 30 drinks a week? ”) • Ask about maximum consumption on any day in past month – Patients often exclude sporadic heavy drinking days • Convert responses to standard drinks: 12 oz. beer bottle, 5 oz. glass of wine, 1½ oz. liquor. • Ask how many bottles they consume weekly, and the size of the bottle (spirits: 13 oz. or 26 oz. ; wine: 750 m. L or 1 L). META: PHI 2015
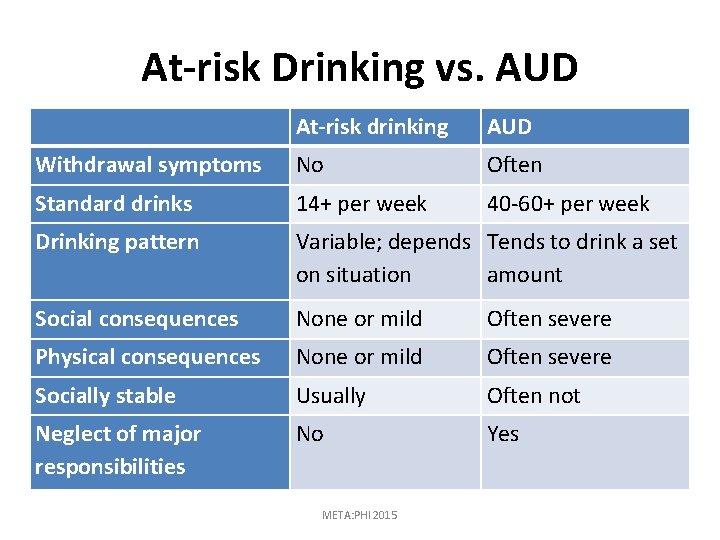
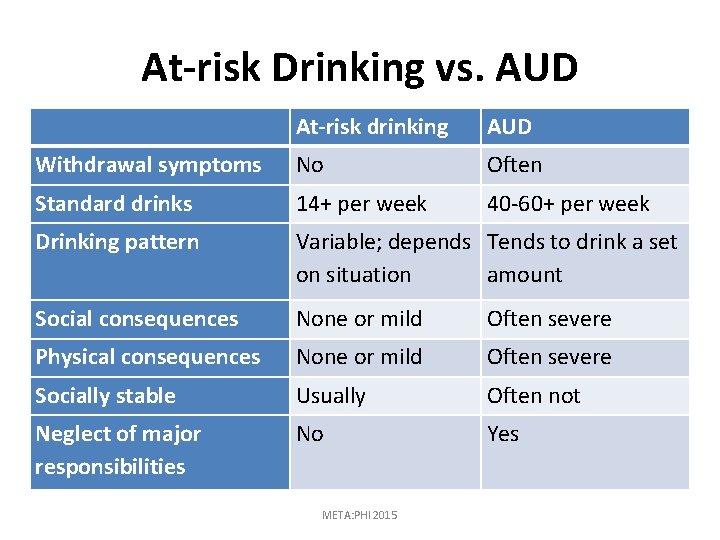
At-risk Drinking vs. AUD At-risk drinking AUD Withdrawal symptoms No Often Standard drinks 14+ per week 40 -60+ per week Drinking pattern Variable; depends Tends to drink a set on situation amount Social consequences None or mild Often severe Physical consequences None or mild Often severe Socially stable Usually Often not Neglect of major responsibilities No Yes META: PHI 2015
BRIEF ADVICE FOR AT-RISK DRINKERS AND PATIENTS WITH MILD AUDS META: PHI 2015
Protocol • Review low-risk drinking guidelines • Link drinking with health status, mood, sleep, and energy • Review precautions and contraindications to alcohol consumption – Pregnancy, active peptic ulcer disease or gastritis, cirrhosis of the liver, alcoholic or viral hepatitis, pancreatitis – Potential adverse effects of alcohol use if they have diabetes, bleeding disorders, or seizure disorders, or are taking medications (antidepressants, ASA, NSAIDs, opioids, sedatives) META: PHI 2015
Protocol (cont’d) • Assess patient’s stage of change – Not ready to change: Restate concern, encourage reflection, motivation, address barriers, reaffirm willingness to help – Ready to change: Help set goal, agree to plan, educational materials, community resources, medications, follow-up META: PHI 2015
Protocol (cont’d) • Have patient commit to a drinking goal: amount per occasion, frequency, and circumstances • Review strategies to reduce consumption: Drink no more than one standard drink per hour Start drinking later in the evening Sip drinks, don't gulp Avoid drinking on an empty stomach Dilute drinks with mixer Alternate alcoholic with non-alcoholic drinks 20 -minute pause between the decision to drink and drinking – Avoid your favourite drink – – – – META: PHI 2015
Protocol (cont’d) • Ask patient to keep a daily drinking diary • Order GGT and MCV – GGT and MCV are useful because elevated test result often motivates patient to change – Test results can be followed over time to monitor recovery and relapse • Have regular follow-up – Ask about alcohol consumption at each visit and note successes • Consider medication referral if problem persists META: PHI 2015
MANAGING PATIENTS WITH MODERATE OR SEVERE AUDS META: PHI 2015
Presenting a Diagnosis (1) • Be clear but sensitive: – “I’m concerned about your use of alcohol. It is above the levels recommended by the low-risk drinking guidelines and appears to be causing you harm. ” • Explain how the patient’s health condition is linked to alcohol use. – “Based on my assessment, you have an alcohol use disorder. ” – “Alcohol use disorders can be caused by many things, such as trauma (both in childhood and as an adult), genetics, mental health problems, and life stressors such as the end of a relationship or loss of a job. ” – “An alcohol use disorder is a chronic illness; it doesn’t mean that you’re weak, or that you’re not a good person. ” META: PHI 2015
Presenting a Diagnosis (cont’d) • Inform the patient that their prognosis is good with treatment: – “I know it can be very difficult to change your drinking patterns, but I can offer you some treatments that can help you (medications, counselling), and I can help connect you to treatment programs, counseling, or support groups. ” – “Within days or weeks of abstinence, most people have improved sleep, mood, and energy levels. ” – “This is a treatable condition. If you’re not ready to change right now, we can discuss it again at your next visit. ” META: PHI 2015
Protocol • Ask whether patient is willing to commit to a drinking goal (abstinence or reduced drinking). – If the patient is not ready to commit, ask about drinking and readiness to change at each visit. – If ready to commit, negotiate a written drinking goal: • Abstinence is more likely to be successful. • If reduced drinking goal is chosen, encourage a timelimited trial. META: PHI 2015
Protocol (cont’d) • Treat concurrent conditions (anxiety, depression, hypertension, liver disease) • Prescribe anti-craving medication • Encourage patient to make healthy lifestyle choices: – – – Stay away from people and places associated with drinking Spend time with supportive family and friends Take daily walks Maintain regular sleeping/waking schedule Plan regular activities outside the house as feasible • Review options formal treatment (residential, day, outpatient) • Recommend AA for group support, practical advice, and a way to overcome loneliness and boredom • Arrange follow-up; monitor drinking through self-report, GGT, MCV • Acknowledge successes, even if partial or temporary • If patient relapses, encourage contact and reconnection with treatment META: PHI 2015
MANAGING ALCOHOL WITHDRAWAL META: PHI 2015
Withdrawal Starts 6– 12 hours after last drink Peaks at 24– 72 hours Resolves in 3– 10 days (or longer) Tremor is most reliable feature (postural, intention, ataxic gait, not a resting tremor) • Other features: sweating, vomiting, anxiety, tachycardia, hypertension • • META: PHI 2015
Withdrawal (cont’d) • Consider office treatment of withdrawal for patients who: – Report frequent withdrawal symptoms – Are committed to abstinence, willing to start psychosocial addiction treatment and/or anti-alcohol medications – Have no history of seizures, DTs, or ED visits/hospitalizations due to withdrawal – Are not on high doses of opioids or sedating medications – Do not have cirrhosis with liver dysfunction – Have supports at home META: PHI 2015
Withdrawal Severity Scales • SHOT: Simple scale validated in the ED • CIWA-Ar: Standard monitoring scale, strong evidence of validity META: PHI 2015
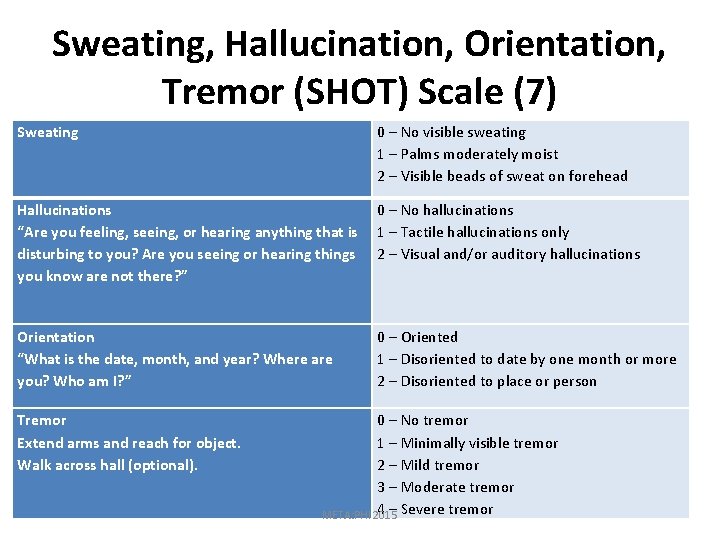
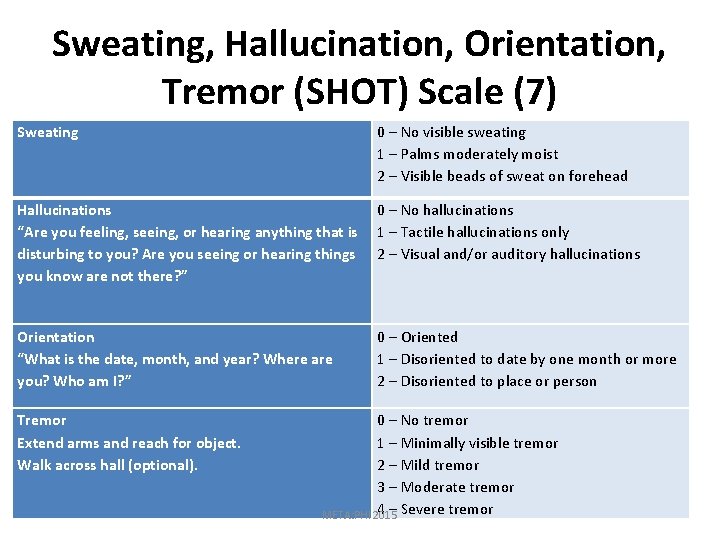
Sweating, Hallucination, Orientation, Tremor (SHOT) Scale (7) Sweating 0 – No visible sweating 1 – Palms moderately moist 2 – Visible beads of sweat on forehead Hallucinations 0 – No hallucinations “Are you feeling, seeing, or hearing anything that is 1 – Tactile hallucinations only disturbing to you? Are you seeing or hearing things 2 – Visual and/or auditory hallucinations you know are not there? ” Orientation “What is the date, month, and year? Where are you? Who am I? ” Tremor Extend arms and reach for object. Walk across hall (optional). 0 – Oriented 1 – Disoriented to date by one month or more 2 – Disoriented to place or person 0 – No tremor 1 – Minimally visible tremor 2 – Mild tremor 3 – Moderate tremor 4 – Severe tremor META: PHI 2015
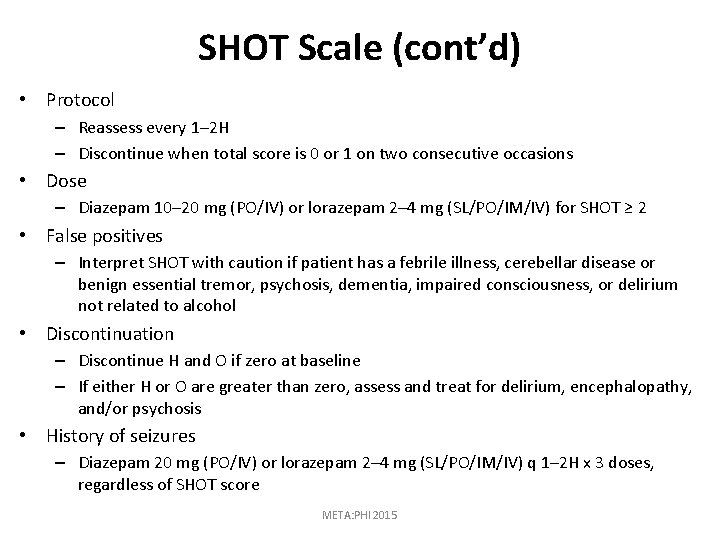
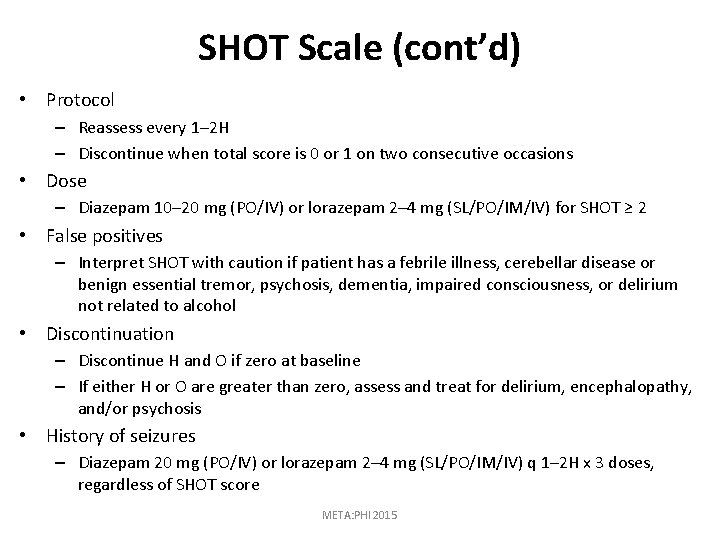
SHOT Scale (cont’d) • Protocol – Reassess every 1– 2 H – Discontinue when total score is 0 or 1 on two consecutive occasions • Dose – Diazepam 10– 20 mg (PO/IV) or lorazepam 2– 4 mg (SL/PO/IM/IV) for SHOT ≥ 2 • False positives – Interpret SHOT with caution if patient has a febrile illness, cerebellar disease or benign essential tremor, psychosis, dementia, impaired consciousness, or delirium not related to alcohol • Discontinuation – Discontinue H and O if zero at baseline – If either H or O are greater than zero, assess and treat for delirium, encephalopathy, and/or psychosis • History of seizures – Diazepam 20 mg (PO/IV) or lorazepam 2– 4 mg (SL/PO/IM/IV) q 1– 2 H x 3 doses, regardless of SHOT score META: PHI 2015
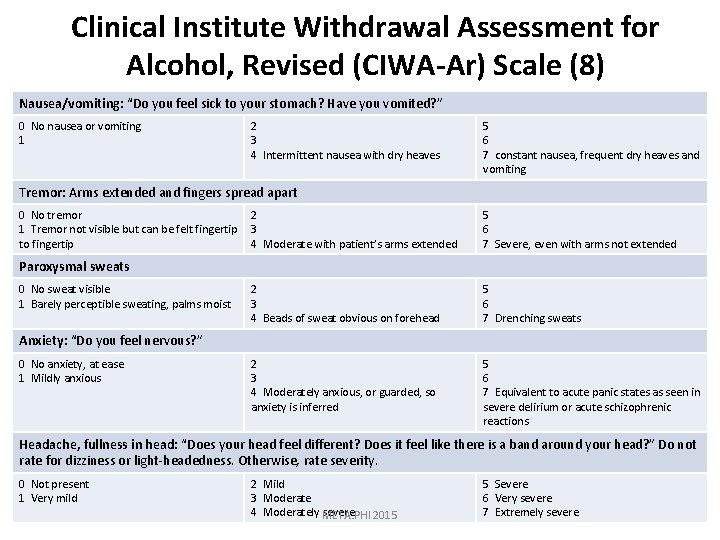
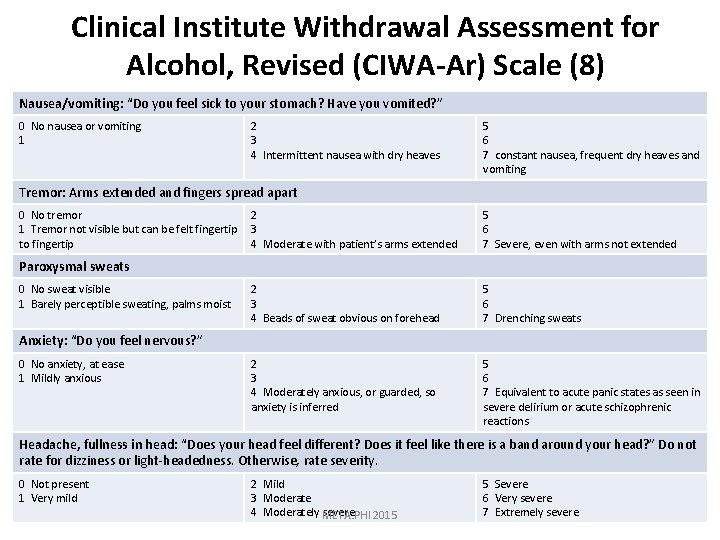
Clinical Institute Withdrawal Assessment for Alcohol, Revised (CIWA-Ar) Scale (8) Nausea/vomiting: “Do you feel sick to your stomach? Have you vomited? ” 0 No nausea or vomiting 1 2 3 4 Intermittent nausea with dry heaves 5 6 7 constant nausea, frequent dry heaves and vomiting Tremor: Arms extended and fingers spread apart 0 No tremor 1 Tremor not visible but can be felt fingertip to fingertip 2 3 4 Moderate with patient’s arms extended 5 6 7 Severe, even with arms not extended 2 3 4 Beads of sweat obvious on forehead 5 6 7 Drenching sweats 2 3 4 Moderately anxious, or guarded, so anxiety is inferred 5 6 7 Equivalent to acute panic states as seen in severe delirium or acute schizophrenic reactions Paroxysmal sweats 0 No sweat visible 1 Barely perceptible sweating, palms moist Anxiety: “Do you feel nervous? ” 0 No anxiety, at ease 1 Mildly anxious Headache, fullness in head: “Does your head feel different? Does it feel like there is a band around your head? ” Do not rate for dizziness or light-headedness. Otherwise, rate severity. 0 Not present 1 Very mild 2 Mild 3 Moderate 4 Moderately META: PHI severe 2015 5 Severe 6 Very severe 7 Extremely severe
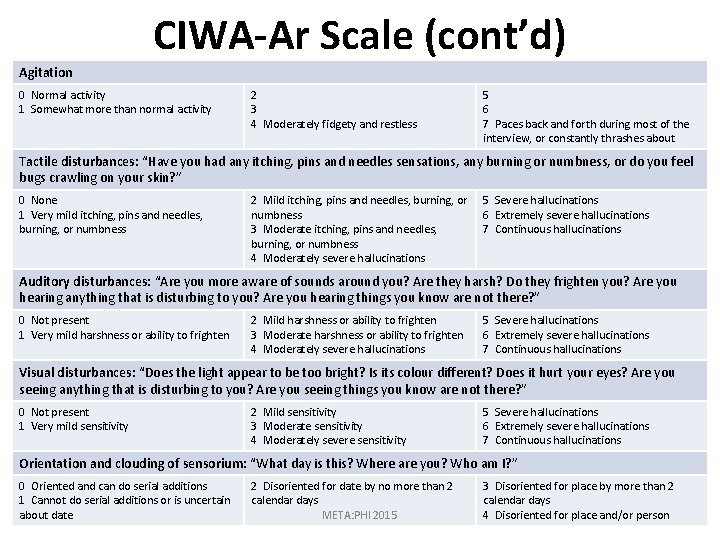
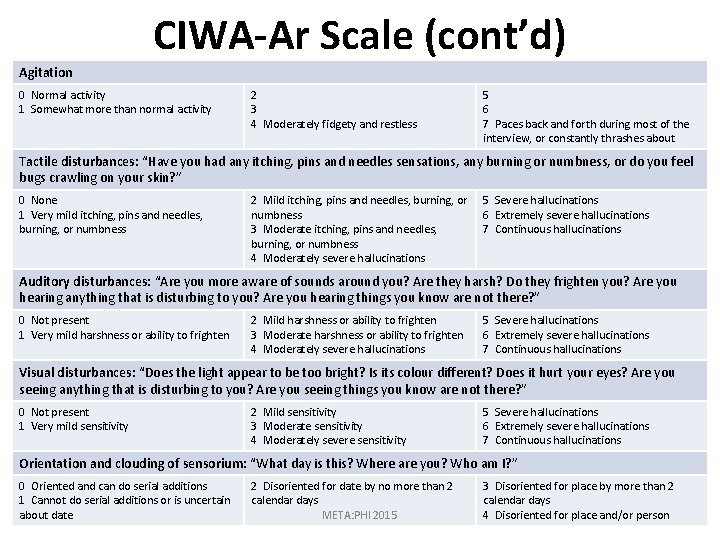
CIWA-Ar Scale (cont’d) Agitation 0 Normal activity 1 Somewhat more than normal activity 2 3 4 Moderately fidgety and restless 5 6 7 Paces back and forth during most of the interview, or constantly thrashes about Tactile disturbances: “Have you had any itching, pins and needles sensations, any burning or numbness, or do you feel bugs crawling on your skin? ” 0 None 1 Very mild itching, pins and needles, burning, or numbness 2 Mild itching, pins and needles, burning, or numbness 3 Moderate itching, pins and needles, burning, or numbness 4 Moderately severe hallucinations 5 Severe hallucinations 6 Extremely severe hallucinations 7 Continuous hallucinations Auditory disturbances: “Are you more aware of sounds around you? Are they harsh? Do they frighten you? Are you hearing anything that is disturbing to you? Are you hearing things you know are not there? ” 0 Not present 1 Very mild harshness or ability to frighten 2 Mild harshness or ability to frighten 3 Moderate harshness or ability to frighten 4 Moderately severe hallucinations 5 Severe hallucinations 6 Extremely severe hallucinations 7 Continuous hallucinations Visual disturbances: “Does the light appear to be too bright? Is its colour different? Does it hurt your eyes? Are you seeing anything that is disturbing to you? Are you seeing things you know are not there? ” 0 Not present 1 Very mild sensitivity 2 Mild sensitivity 3 Moderate sensitivity 4 Moderately severe sensitivity 5 Severe hallucinations 6 Extremely severe hallucinations 7 Continuous hallucinations Orientation and clouding of sensorium: “What day is this? Where are you? Who am I? ” 0 Oriented and can do serial additions 1 Cannot do serial additions or is uncertain about date 2 Disoriented for date by no more than 2 calendar days META: PHI 2015 3 Disoriented for place by more than 2 calendar days 4 Disoriented for place and/or person
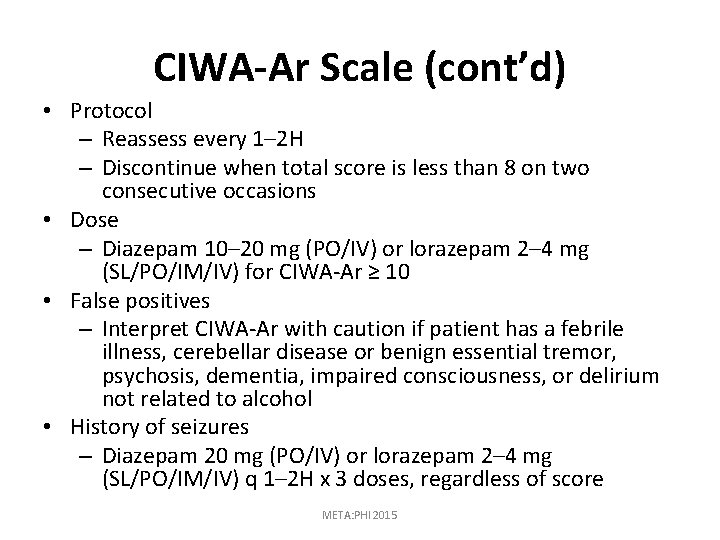
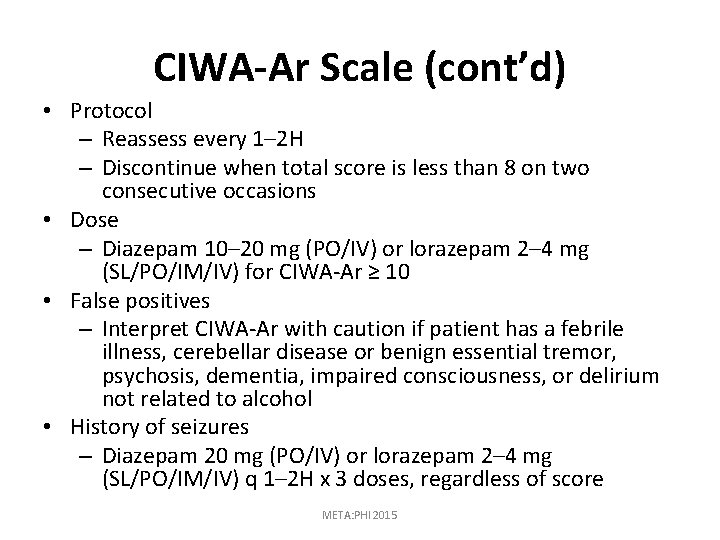
CIWA-Ar Scale (cont’d) • Protocol – Reassess every 1– 2 H – Discontinue when total score is less than 8 on two consecutive occasions • Dose – Diazepam 10– 20 mg (PO/IV) or lorazepam 2– 4 mg (SL/PO/IM/IV) for CIWA-Ar ≥ 10 • False positives – Interpret CIWA-Ar with caution if patient has a febrile illness, cerebellar disease or benign essential tremor, psychosis, dementia, impaired consciousness, or delirium not related to alcohol • History of seizures – Diazepam 20 mg (PO/IV) or lorazepam 2– 4 mg (SL/PO/IM/IV) q 1– 2 H x 3 doses, regardless of score META: PHI 2015
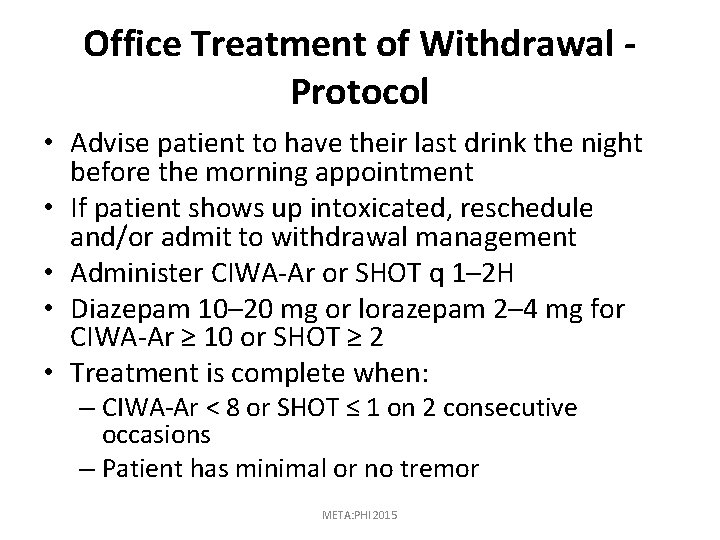
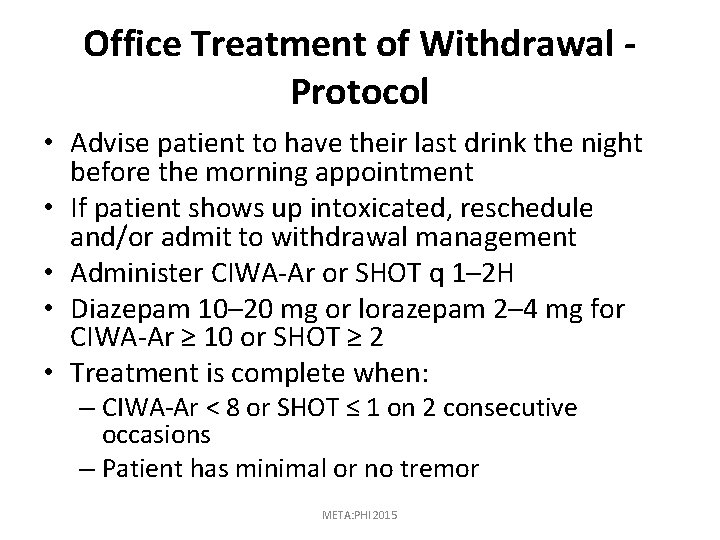
Office Treatment of Withdrawal - Protocol • Advise patient to have their last drink the night before the morning appointment • If patient shows up intoxicated, reschedule and/or admit to withdrawal management • Administer CIWA-Ar or SHOT q 1– 2 H • Diazepam 10– 20 mg or lorazepam 2– 4 mg for CIWA-Ar ≥ 10 or SHOT ≥ 2 • Treatment is complete when: – CIWA-Ar < 8 or SHOT ≤ 1 on 2 consecutive occasions – Patient has minimal or no tremor META: PHI 2015
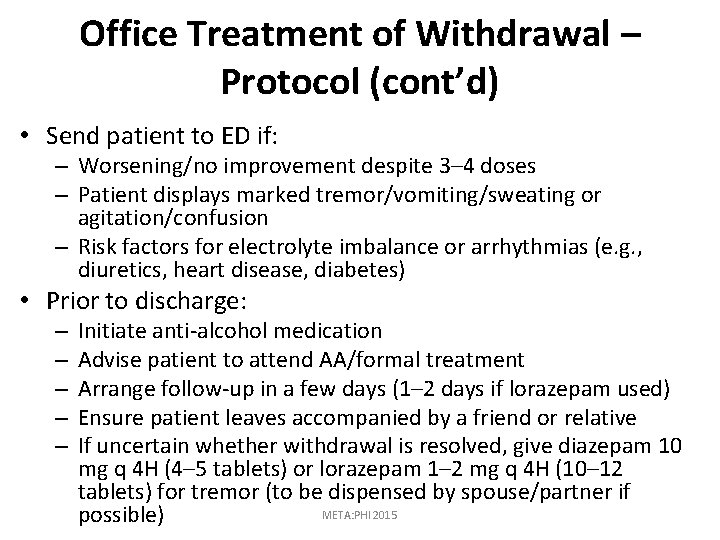
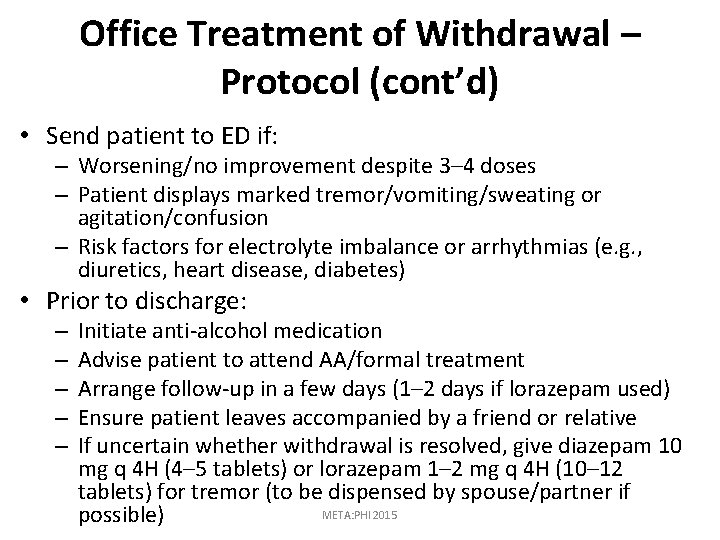
Office Treatment of Withdrawal – Protocol (cont’d) • Send patient to ED if: – Worsening/no improvement despite 3– 4 doses – Patient displays marked tremor/vomiting/sweating or agitation/confusion – Risk factors for electrolyte imbalance or arrhythmias (e. g. , diuretics, heart disease, diabetes) • Prior to discharge: – – – Initiate anti-alcohol medication Advise patient to attend AA/formal treatment Arrange follow-up in a few days (1– 2 days if lorazepam used) Ensure patient leaves accompanied by a friend or relative If uncertain whether withdrawal is resolved, give diazepam 10 mg q 4 H (4– 5 tablets) or lorazepam 1– 2 mg q 4 H (10– 12 tablets) for tremor (to be dispensed by spouse/partner if META: PHI 2015 possible)
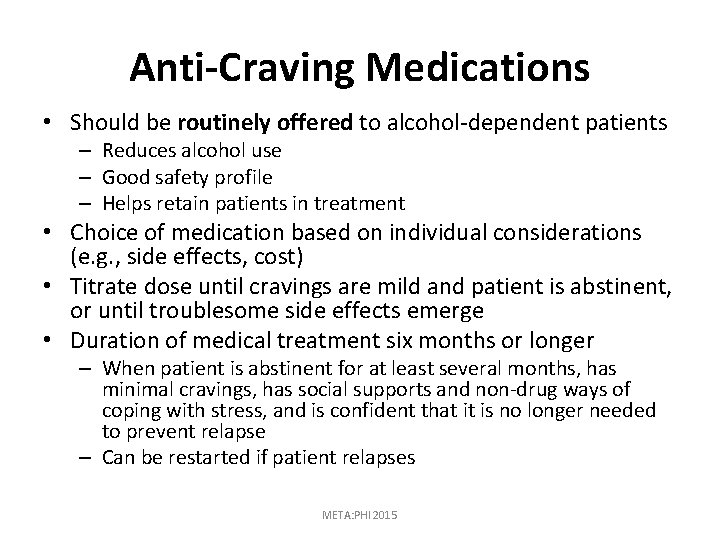
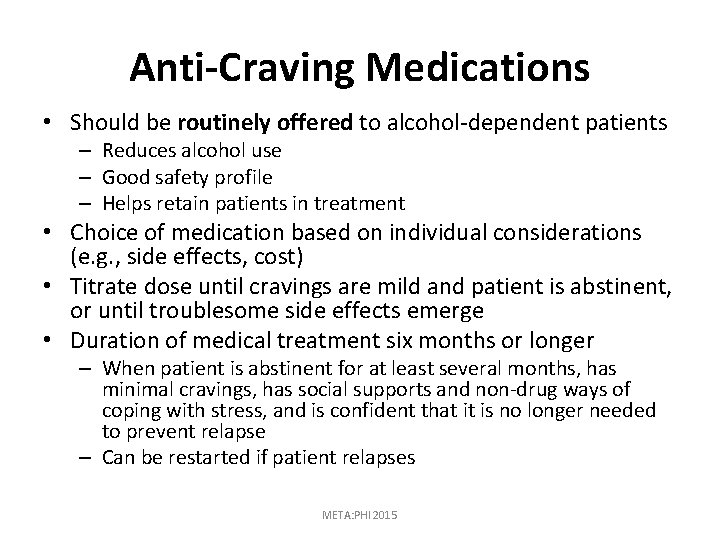
Anti-Craving Medications • Should be routinely offered to alcohol-dependent patients – Reduces alcohol use – Good safety profile – Helps retain patients in treatment • Choice of medication based on individual considerations (e. g. , side effects, cost) • Titrate dose until cravings are mild and patient is abstinent, or until troublesome side effects emerge • Duration of medical treatment six months or longer – When patient is abstinent for at least several months, has minimal cravings, has social supports and non-drug ways of coping with stress, and is confident that it is no longer needed to prevent relapse – Can be restarted if patient relapses META: PHI 2015
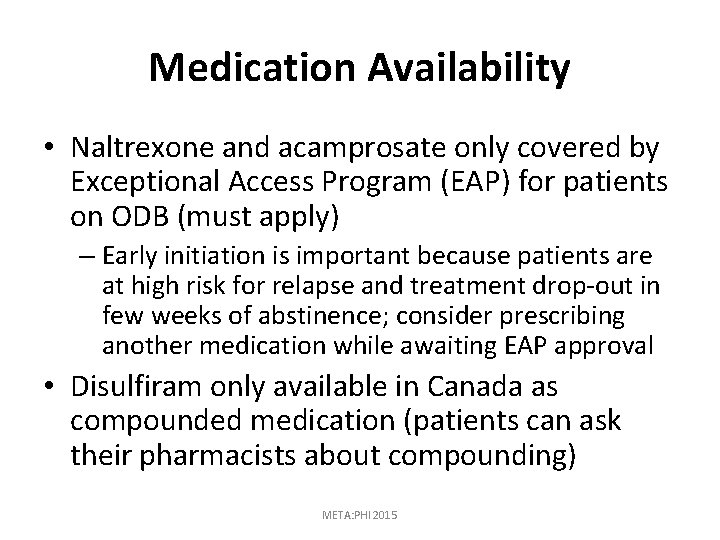
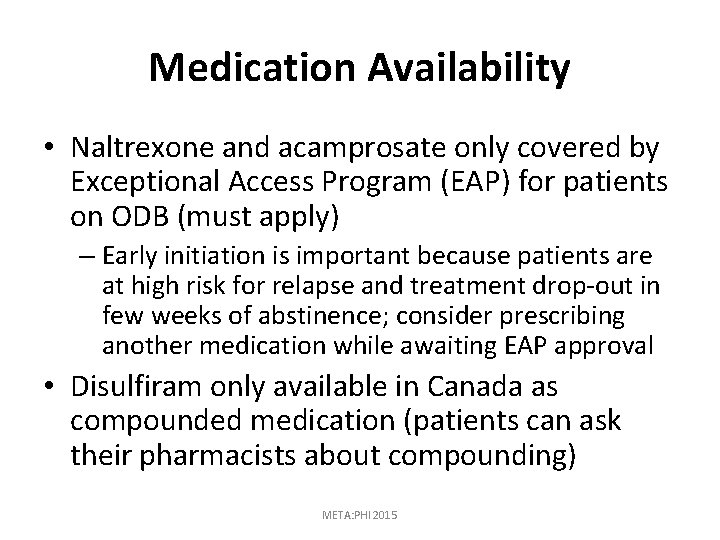
Medication Availability • Naltrexone and acamprosate only covered by Exceptional Access Program (EAP) for patients on ODB (must apply) – Early initiation is important because patients are at high risk for relapse and treatment drop-out in few weeks of abstinence; consider prescribing another medication while awaiting EAP approval • Disulfiram only available in Canada as compounded medication (patients can ask their pharmacists about compounding) META: PHI 2015
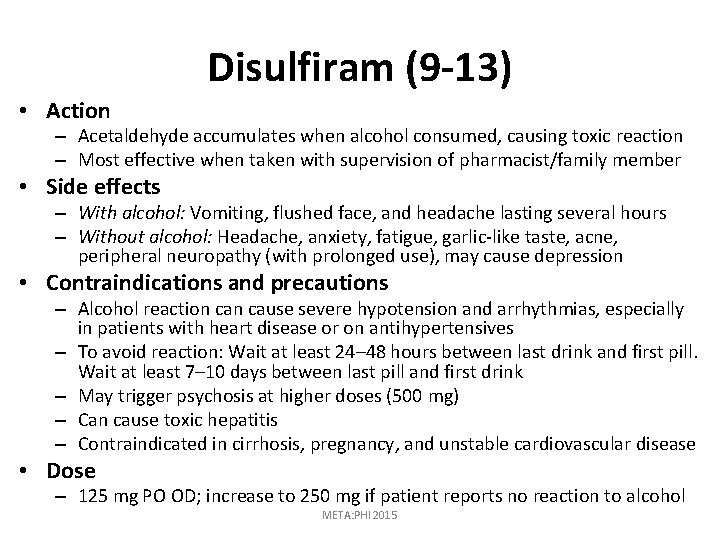
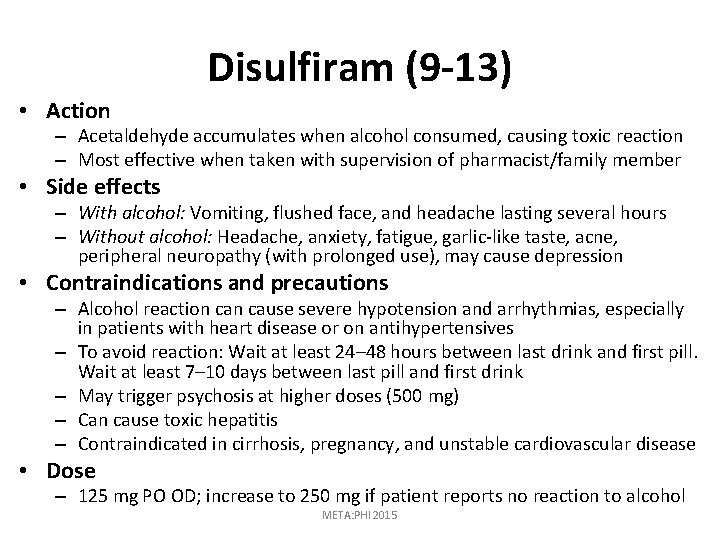
Disulfiram (9 -13) • Action – Acetaldehyde accumulates when alcohol consumed, causing toxic reaction – Most effective when taken with supervision of pharmacist/family member • Side effects – With alcohol: Vomiting, flushed face, and headache lasting several hours – Without alcohol: Headache, anxiety, fatigue, garlic-like taste, acne, peripheral neuropathy (with prolonged use), may cause depression • Contraindications and precautions – Alcohol reaction cause severe hypotension and arrhythmias, especially in patients with heart disease or on antihypertensives – To avoid reaction: Wait at least 24– 48 hours between last drink and first pill. Wait at least 7– 10 days between last pill and first drink – May trigger psychosis at higher doses (500 mg) – Can cause toxic hepatitis – Contraindicated in cirrhosis, pregnancy, and unstable cardiovascular disease • Dose – 125 mg PO OD; increase to 250 mg if patient reports no reaction to alcohol META: PHI 2015
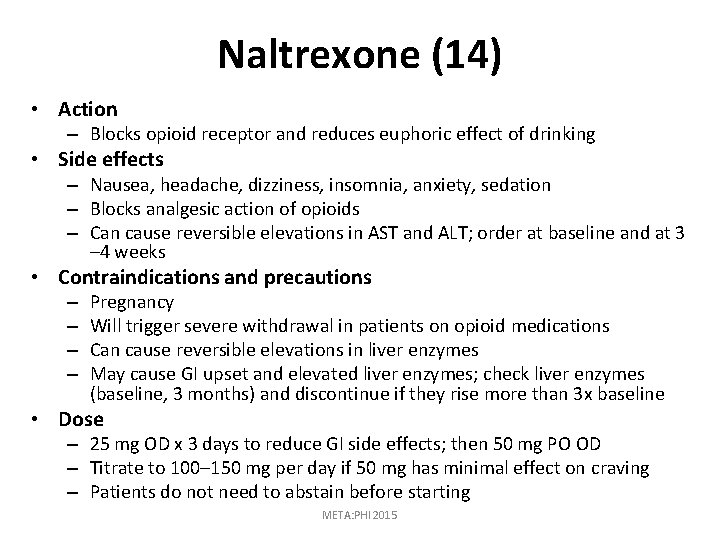
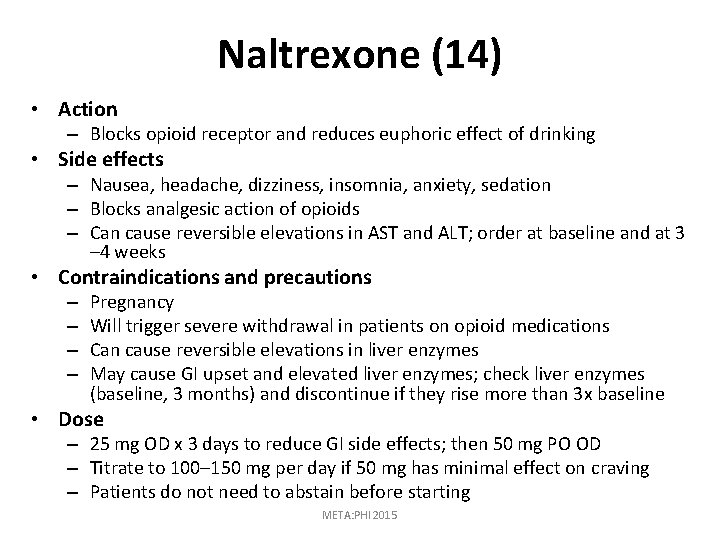
Naltrexone (14) • Action – Blocks opioid receptor and reduces euphoric effect of drinking • Side effects – Nausea, headache, dizziness, insomnia, anxiety, sedation – Blocks analgesic action of opioids – Can cause reversible elevations in AST and ALT; order at baseline and at 3 – 4 weeks • Contraindications and precautions – – Pregnancy Will trigger severe withdrawal in patients on opioid medications Can cause reversible elevations in liver enzymes May cause GI upset and elevated liver enzymes; check liver enzymes (baseline, 3 months) and discontinue if they rise more than 3 x baseline • Dose – 25 mg OD x 3 days to reduce GI side effects; then 50 mg PO OD – Titrate to 100– 150 mg per day if 50 mg has minimal effect on craving – Patients do not need to abstain before starting META: PHI 2015
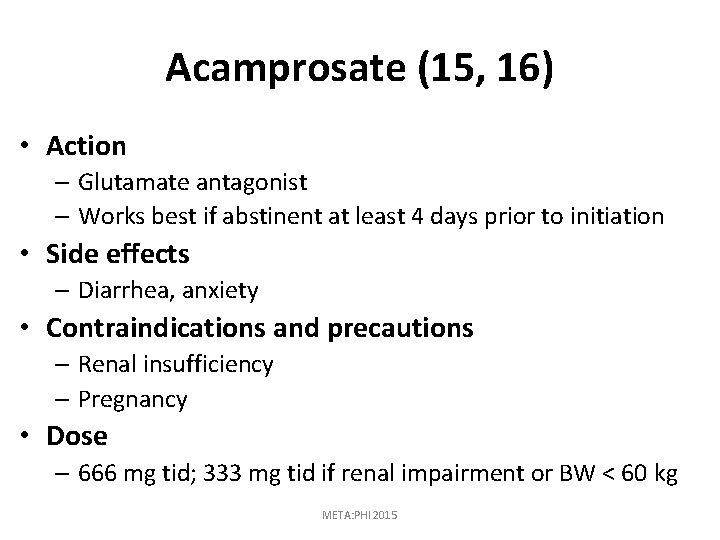
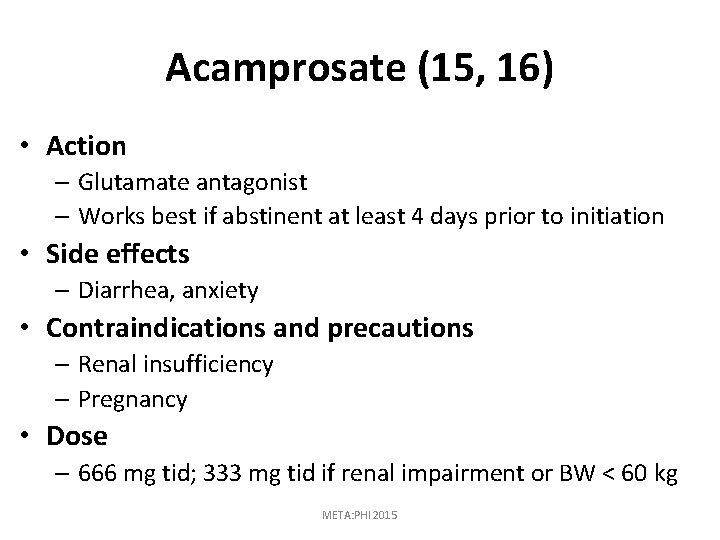
Acamprosate (15, 16) • Action – Glutamate antagonist – Works best if abstinent at least 4 days prior to initiation • Side effects – Diarrhea, anxiety • Contraindications and precautions – Renal insufficiency – Pregnancy • Dose – 666 mg tid; 333 mg tid if renal impairment or BW < 60 kg META: PHI 2015
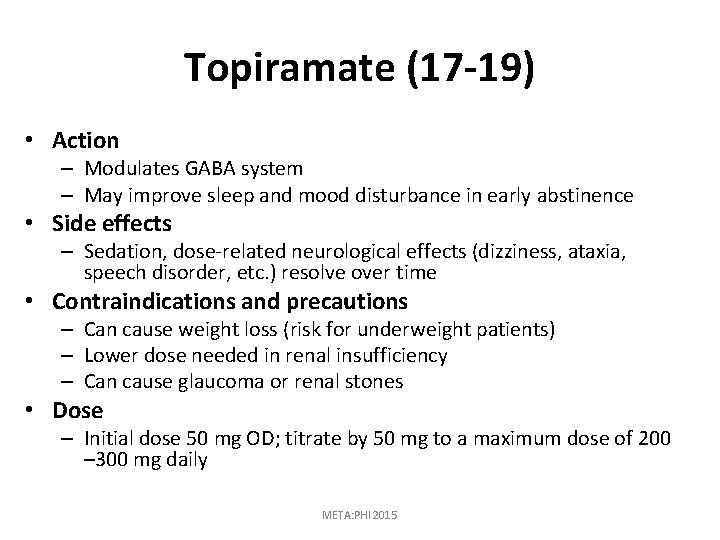
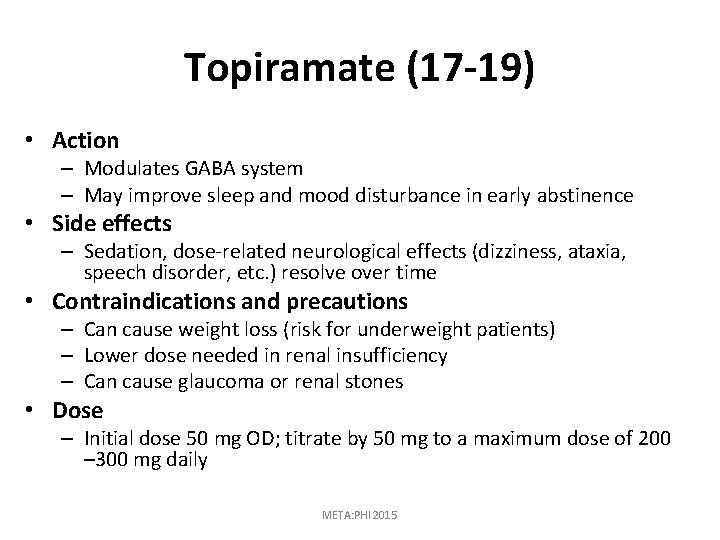
Topiramate (17 -19) • Action – Modulates GABA system – May improve sleep and mood disturbance in early abstinence • Side effects – Sedation, dose-related neurological effects (dizziness, ataxia, speech disorder, etc. ) resolve over time • Contraindications and precautions – Can cause weight loss (risk for underweight patients) – Lower dose needed in renal insufficiency – Can cause glaucoma or renal stones • Dose – Initial dose 50 mg OD; titrate by 50 mg to a maximum dose of 200 – 300 mg daily META: PHI 2015
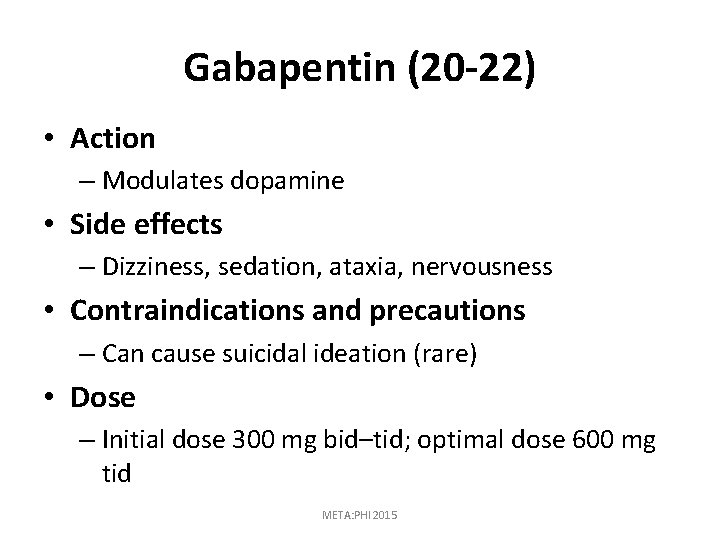
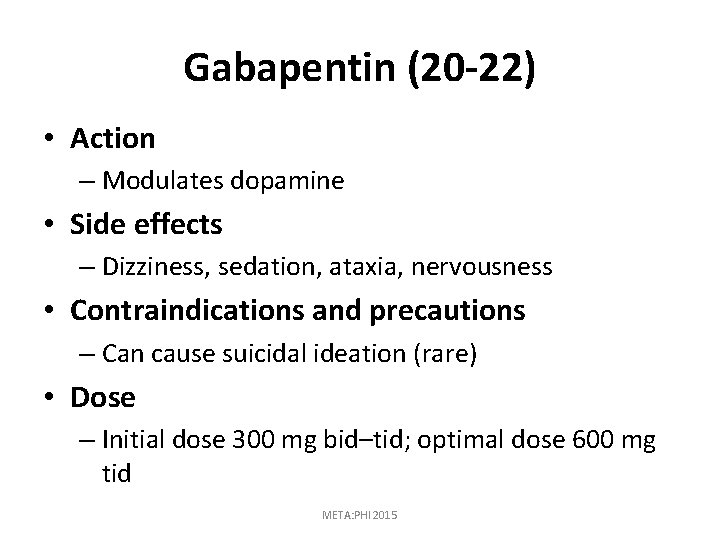
Gabapentin (20 -22) • Action – Modulates dopamine • Side effects – Dizziness, sedation, ataxia, nervousness • Contraindications and precautions – Can cause suicidal ideation (rare) • Dose – Initial dose 300 mg bid–tid; optimal dose 600 mg tid META: PHI 2015
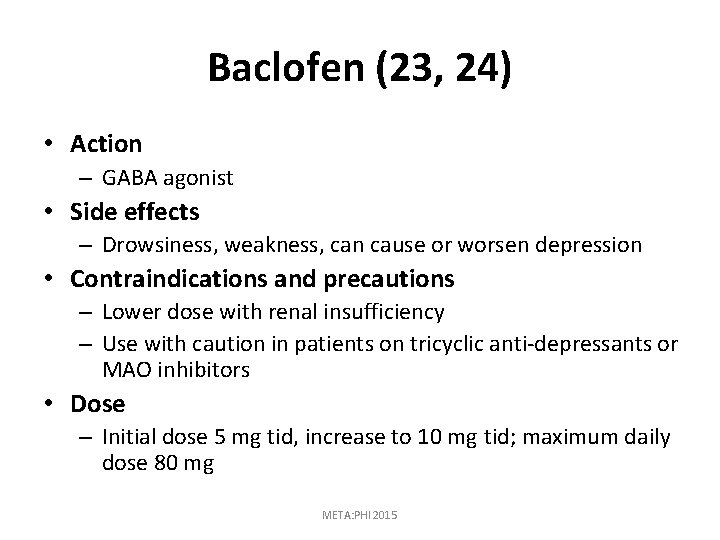
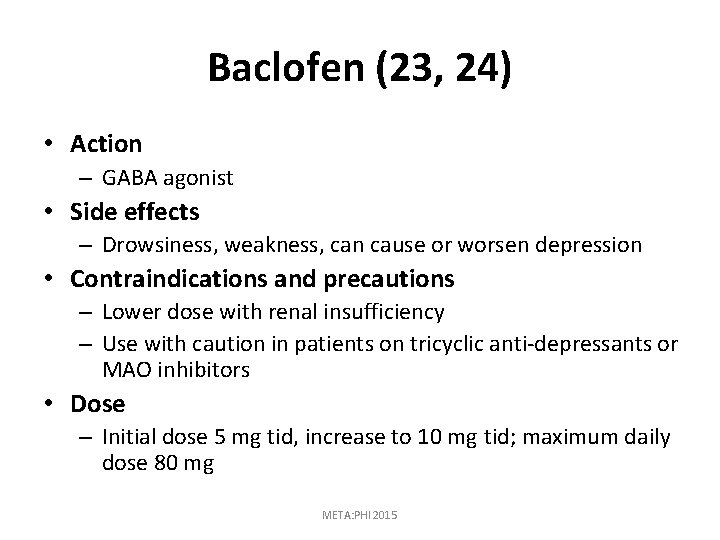
Baclofen (23, 24) • Action – GABA agonist • Side effects – Drowsiness, weakness, can cause or worsen depression • Contraindications and precautions – Lower dose with renal insufficiency – Use with caution in patients on tricyclic anti-depressants or MAO inhibitors • Dose – Initial dose 5 mg tid, increase to 10 mg tid; maximum daily dose 80 mg META: PHI 2015
MANAGEMENT OF COMMON OUTPATIENT ALCOHOL-RELATED PROBLEMS META: PHI 2015
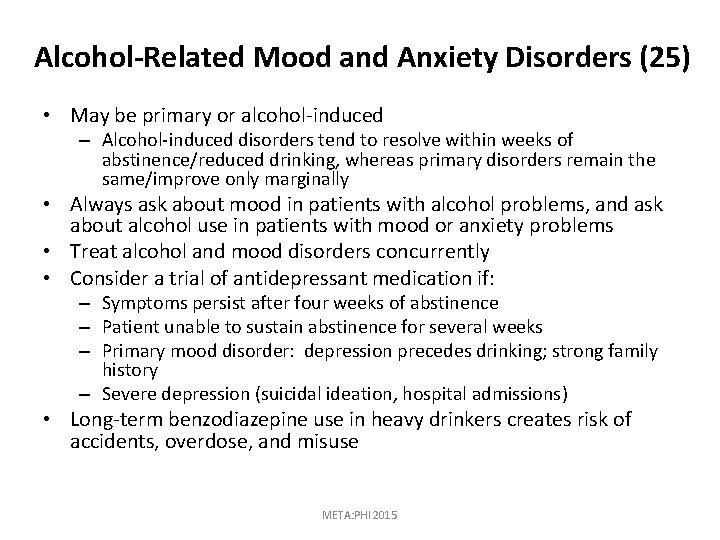
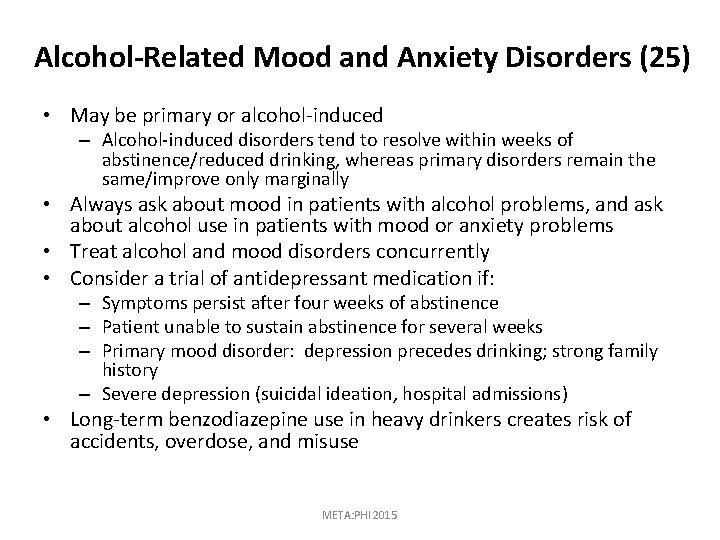
Alcohol-Related Mood and Anxiety Disorders (25) • May be primary or alcohol-induced – Alcohol-induced disorders tend to resolve within weeks of abstinence/reduced drinking, whereas primary disorders remain the same/improve only marginally • Always ask about mood in patients with alcohol problems, and ask about alcohol use in patients with mood or anxiety problems • Treat alcohol and mood disorders concurrently • Consider a trial of antidepressant medication if: – Symptoms persist after four weeks of abstinence – Patient unable to sustain abstinence for several weeks – Primary mood disorder: depression precedes drinking; strong family history – Severe depression (suicidal ideation, hospital admissions) • Long-term benzodiazepine use in heavy drinkers creates risk of accidents, overdose, and misuse META: PHI 2015
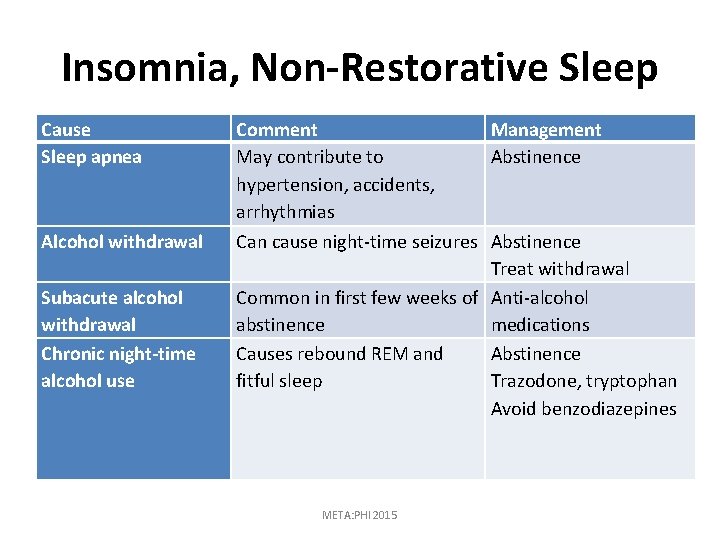
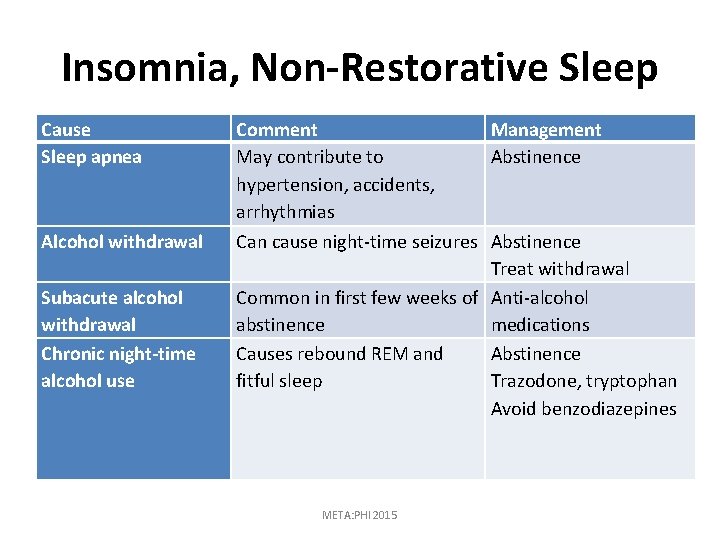
Insomnia, Non-Restorative Sleep Cause Sleep apnea Alcohol withdrawal Subacute alcohol withdrawal Chronic night-time alcohol use Comment Management May contribute to Abstinence hypertension, accidents, arrhythmias Can cause night-time seizures Abstinence Treat withdrawal Common in first few weeks of Anti-alcohol abstinence medications Causes rebound REM and Abstinence fitful sleep Trazodone, tryptophan Avoid benzodiazepines META: PHI 2015
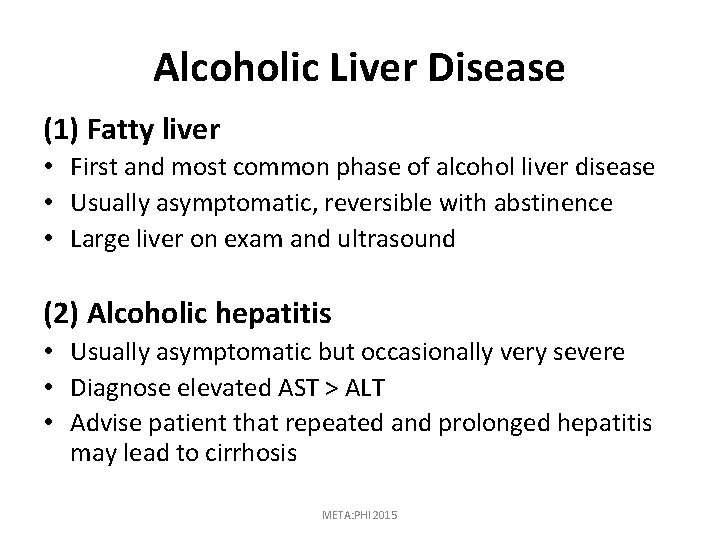
Alcoholic Liver Disease (1) Fatty liver • First and most common phase of alcohol liver disease • Usually asymptomatic, reversible with abstinence • Large liver on exam and ultrasound (2) Alcoholic hepatitis • Usually asymptomatic but occasionally very severe • Diagnose elevated AST > ALT • Advise patient that repeated and prolonged hepatitis may lead to cirrhosis META: PHI 2015
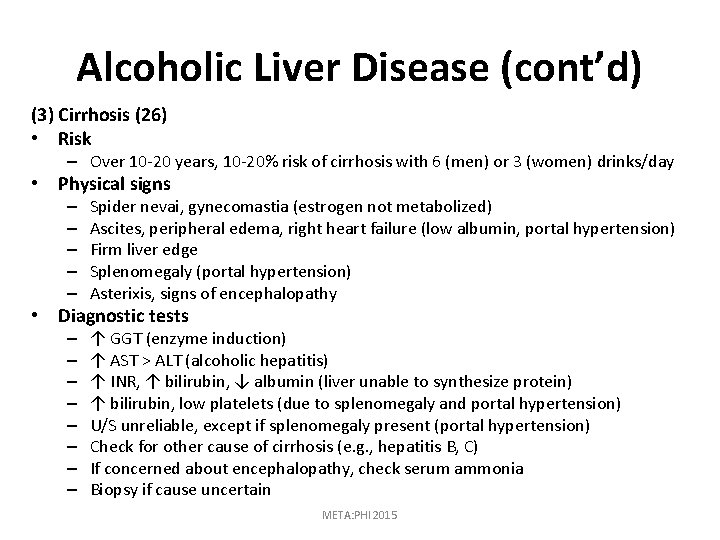
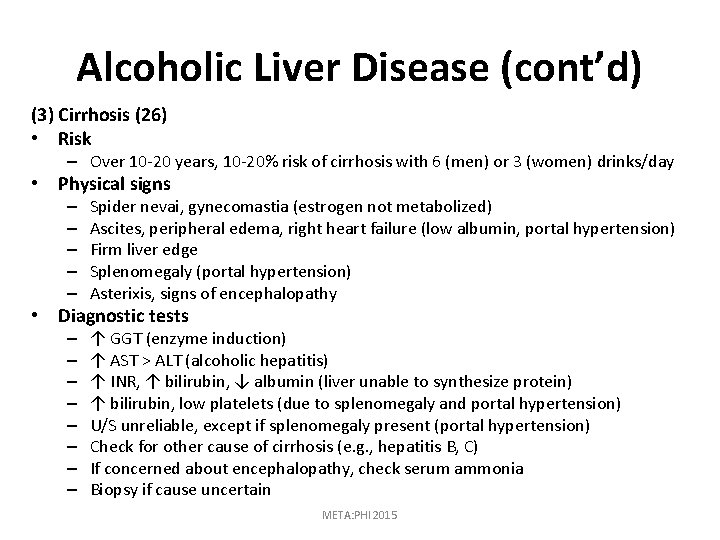
Alcoholic Liver Disease (cont’d) (3) Cirrhosis (26) • Risk – Over 10 -20 years, 10 -20% risk of cirrhosis with 6 (men) or 3 (women) drinks/day • Physical signs – – – Spider nevai, gynecomastia (estrogen not metabolized) Ascites, peripheral edema, right heart failure (low albumin, portal hypertension) Firm liver edge Splenomegaly (portal hypertension) Asterixis, signs of encephalopathy • Diagnostic tests – – – – ↑ GGT (enzyme induction) ↑ AST > ALT (alcoholic hepatitis) ↑ INR, ↑ bilirubin, ↓ albumin (liver unable to synthesize protein) ↑ bilirubin, low platelets (due to splenomegaly and portal hypertension) U/S unreliable, except if splenomegaly present (portal hypertension) Check for other cause of cirrhosis (e. g. , hepatitis B, C) If concerned about encephalopathy, check serum ammonia Biopsy if cause uncertain META: PHI 2015
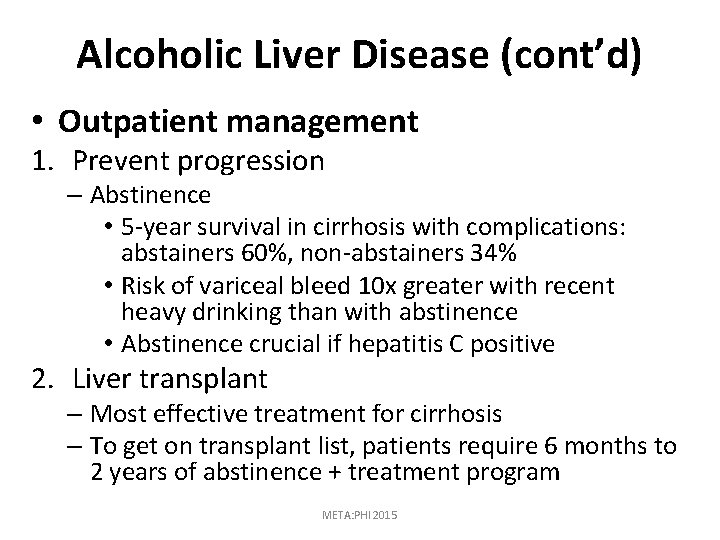
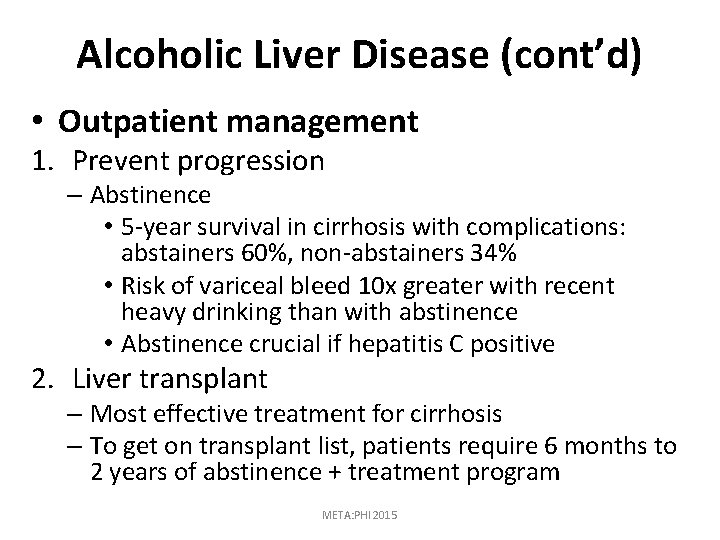
Alcoholic Liver Disease (cont’d) • Outpatient management 1. Prevent progression – Abstinence • 5 -year survival in cirrhosis with complications: abstainers 60%, non-abstainers 34% • Risk of variceal bleed 10 x greater with recent heavy drinking than with abstinence • Abstinence crucial if hepatitis C positive 2. Liver transplant – Most effective treatment for cirrhosis – To get on transplant list, patients require 6 months to 2 years of abstinence + treatment program META: PHI 2015
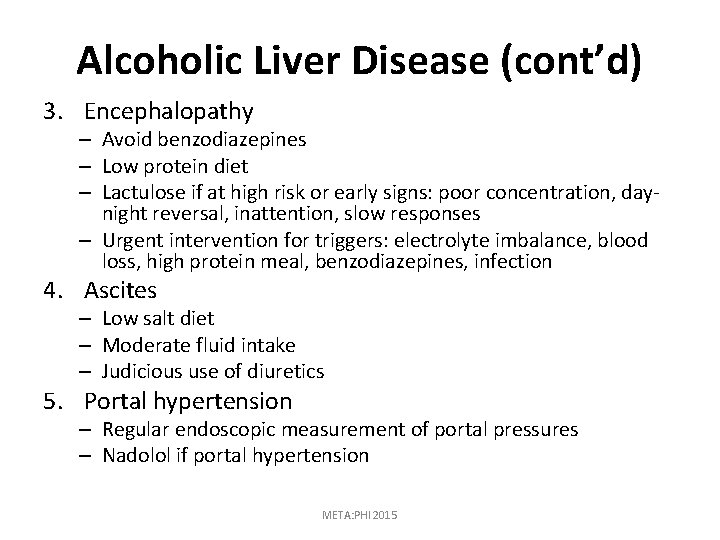
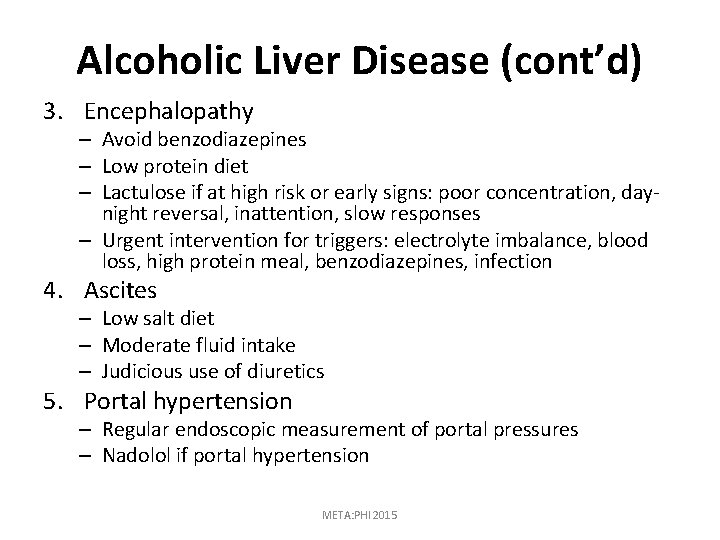
Alcoholic Liver Disease (cont’d) 3. Encephalopathy – Avoid benzodiazepines – Low protein diet – Lactulose if at high risk or early signs: poor concentration, daynight reversal, inattention, slow responses – Urgent intervention for triggers: electrolyte imbalance, blood loss, high protein meal, benzodiazepines, infection 4. Ascites – Low salt diet – Moderate fluid intake – Judicious use of diuretics 5. Portal hypertension – Regular endoscopic measurement of portal pressures – Nadolol if portal hypertension META: PHI 2015
Hypertension • Consumption of 3+ drinks/day can cause or exacerbate hypertension • Patients witch alcohol-induced hypertension tend to be refractory to antihypertensive medication • Hypertension resolves within weeks of abstinence or reduced drinking META: PHI 2015
Neurological Conditions • Alcohol-induced dementia, cerebellar, ataxia, peripheral neuropathy, parkinsonism • Conditions often improve with abstinence over weeks/months META: PHI 2015
Dilated Cardiomyopathy • Presents with heart failure and arrhythmias • Excellent prognosis; sometimes completely resolves within months of abstinence • GI bleed (gastritis, esophagitis, Mallory-Weiss tear, esophageal varices) META: PHI 2015
Prescribing Benzodiazepines and Opioids (27) • Risk of overdose and accidents greatly increased when combining benzodiazepines or opioids with alcohol • Both medications should be routinely tapered to the lowest effective dose in the elderly META: PHI 2015
Reporting to the Ministry of Transportation • Suggested criteria for reporting – Patient admits to drinking and driving – Family member informs physician that patient is drinking and driving – Patient drinks steadily throughout the day and regularly drives – Patient drove to your clinic while intoxicated – Patient regularly drives and has recently experienced a withdrawal seizure – Patient has other alcohol-related complications that impair driving ability (e. g. , cerebellar ataxia) – Patient has blackouts caused by alcohol consumption META: PHI 2015
Reporting to the Ministry of Transportation (cont’d) • Management of patients with suspended licenses – Explain to the patient that you have a legal obligation to report – Patients may ask you to give them a chance to abstain and attend treatment before deciding to report them; however, trusting the patient to comply with your instructions is not considered an adequate reason for failing to report – To lift suspension, patient must have attended treatment and maintained abstinence or low-risk drinking for specified number of months (usually one year) META: PHI 2015
Reporting to the Ministry of Transportation (cont’d) – Monthly appointments are recommended: • Ask about alcohol consumption and attendance at AA and treatment programs • Order GGT and MCV • With patient’s permission, ask spouse/partner or close family member to corroborate patient’s reported alcohol consumption META: PHI 2015
References 1. 2. 3. 4. 5. 6. 7. 8. 9. Spithoff S, Kahan M. Primary care management of alcohol use disorder and at-risk drinking Part 1: screening and assessment. Canadian family physician Medecin de famille canadien. 2015; 61: 509 -14. Rehm J, Gnam W, Popova S, Baliunas D, Brochu S, Fischer B, et al. The costs of alcohol, illegal drugs, and tobacco in Canada, 2002. Journal of studies on alcohol and drugs. 2007; 68(6): 886 -95. Drug and Alcohol Use Statistics [Internet]. Health Canada, Government of Canada. 2009. Available from: http: //www. hc-sc. gc. ca/hc-ps/drugs-drogues/stat/index-eng. php. American Psychiatric Association, Force DSMT. Diagnostic and statistical manual of mental disorders : DSM-5. 2013. Smith PC, Schmidt SM, Allensworth-Davies D, Saitz R. Primary care validation of a single-question alcohol screening test. Journal of general internal medicine. 2009; 24(7): 783 -8. Johnson JA, Lee A, Vinson D, Seale JP. Use of AUDIT-based measures to identify unhealthy alcohol use and alcohol dependence in primary care: a validation study. Alcoholism, clinical and experimental research. 2013; 37 Suppl 1: E 253 -9. Gray S, Borgundvaag B, Sirvastava A, Randall I, Kahan M. Feasibility and reliability of the SHOT: A short scale for measuring pretreatment severity of alcohol withdrawal in the emergency department. Acad Emerg Med. 2010; 17(10): 1048 -54. Sullivan JT, Sykora K, Schneiderman J, Naranjo CA, Sellers EM. Assessment of alcohol withdrawal: the revised clinical institute withdrawal assessment for alcohol scale (CIWA-Ar). British journal of addiction. 1989; 84(11): 1353 -7. De Sousa A. A one-year pragmatic trial of naltrexone vs disulfiram in the treatment of alcohol dependence. Alcohol and alcoholism (Oxford, Oxfordshire). 2004; 39(6): 528 -31. META: PHI 2015
References 10. 11. 12. 13. 14. 15. 16. 17. 18. de Sousa A, de Sousa A. An open randomized study comparing disulfiram and acamprosate in the treatment of alcohol dependence. Alcohol and alcoholism (Oxford, Oxfordshire). 2005; 40(6): 5458. Laaksonen E, Koski-Jannes A, Salaspuro M, Ahtinen H, Alho H. A randomized, multicentre, openlabel, comparative trial of disulfiram, naltrexone and acamprosate in the treatment of alcohol dependence. Alcohol and alcoholism (Oxford, Oxfordshire). 2008; 43(1): 53 -61. Mueser KT, Noordsy DL, Fox L, Wolfe R. Disulram treatment for alcoholism in severe mental illness. The American journal on addictions / American Academy of Psychiatrists in Alcoholism and Addictions. 2003; 12(3): 242 -52. Petrakis IL, Nich C, Ralevski E. Psychotic spectrum disorders and alcohol abuse: a review of pharmacotherapeutic strategies and a report on the effectiveness of naltrexone and disulfiram. Schizophrenia bulletin. 2006; 32(4): 644 -54. Anton RF, O'Malley SS, Ciraulo DA, Cisler RA, Couper D, Donovan DM, et al. Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. Jama. 2006; 295(17): 2003 -17. Snyder JL, Bowers T. The efficacy of acamprosate and naltrexone in the treatment of alcohol dependence: A relative benefits analysis of randomized controlled trials. The American journal of drug and alcohol abuse. 2008; 34(4): 449 -61. Rosner S, Leucht S, Lehert P, Soyka M. Acamprosate supports abstinence, naltrexone prevents excessive drinking: Evidence from a meta-analysis with unreported outcomes. Journal of psychopharmacology (Oxford, England). 2008; 22(1): 11 -23. Baltieri DA, Daro FR, Ribeiro PL, de Andrade AG. Comparing topiramate with naltrexone in the treatment of alcohol dependence. Addiction (Abingdon, England). 2008; 103(12): 2035 -44. Johnson B, Rosenthal N, Capece JA, Wiegand F, Mao L, Beyers K. Topiramate for treating alcohol dependence: A randomized controlled trial. Jama. 2007; 298(14): 1641 -51. META: PHI 2015
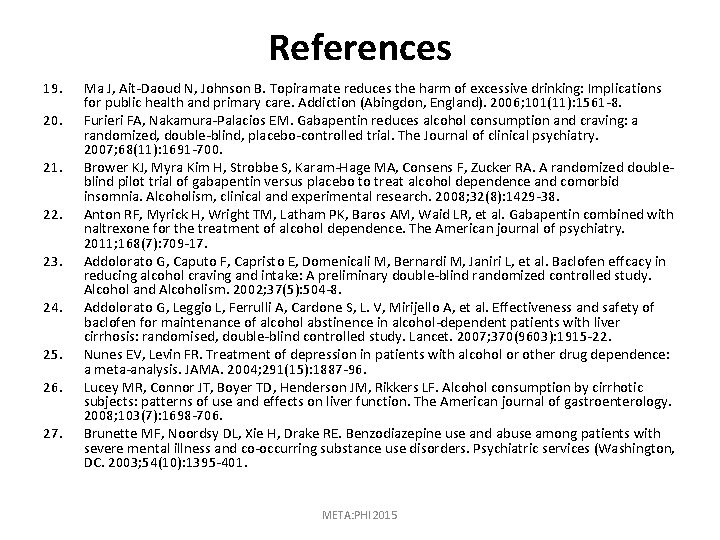
References 19. 20. 21. 22. 23. 24. 25. 26. 27. Ma J, Ait-Daoud N, Johnson B. Topiramate reduces the harm of excessive drinking: Implications for public health and primary care. Addiction (Abingdon, England). 2006; 101(11): 1561 -8. Furieri FA, Nakamura-Palacios EM. Gabapentin reduces alcohol consumption and craving: a randomized, double-blind, placebo-controlled trial. The Journal of clinical psychiatry. 2007; 68(11): 1691 -700. Brower KJ, Myra Kim H, Strobbe S, Karam-Hage MA, Consens F, Zucker RA. A randomized doubleblind pilot trial of gabapentin versus placebo to treat alcohol dependence and comorbid insomnia. Alcoholism, clinical and experimental research. 2008; 32(8): 1429 -38. Anton RF, Myrick H, Wright TM, Latham PK, Baros AM, Waid LR, et al. Gabapentin combined with naltrexone for the treatment of alcohol dependence. The American journal of psychiatry. 2011; 168(7): 709 -17. Addolorato G, Caputo F, Capristo E, Domenicali M, Bernardi M, Janiri L, et al. Baclofen effcacy in reducing alcohol craving and intake: A preliminary double-blind randomized controlled study. Alcohol and Alcoholism. 2002; 37(5): 504 -8. Addolorato G, Leggio L, Ferrulli A, Cardone S, L. V, Mirijello A, et al. Effectiveness and safety of baclofen for maintenance of alcohol abstinence in alcohol-dependent patients with liver cirrhosis: randomised, double-blind controlled study. Lancet. 2007; 370(9603): 1915 -22. Nunes EV, Levin FR. Treatment of depression in patients with alcohol or other drug dependence: a meta-analysis. JAMA. 2004; 291(15): 1887 -96. Lucey MR, Connor JT, Boyer TD, Henderson JM, Rikkers LF. Alcohol consumption by cirrhotic subjects: patterns of use and effects on liver function. The American journal of gastroenterology. 2008; 103(7): 1698 -706. Brunette MF, Noordsy DL, Xie H, Drake RE. Benzodiazepine use and abuse among patients with severe mental illness and co-occurring substance use disorders. Psychiatric services (Washington, DC. 2003; 54(10): 1395 -401. META: PHI 2015
 Formation of alcohols
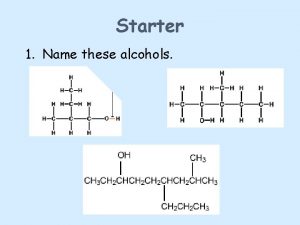
Formation of alcohols Secondary alcohol oxidation
Secondary alcohol oxidation Utmb grand rounds
Utmb grand rounds Round 75 to the nearest 10
Round 75 to the nearest 10 Maths quiz rounds names
Maths quiz rounds names Superfluous dimensions
Superfluous dimensions Layers of neurosis in gestalt therapy
Layers of neurosis in gestalt therapy A is an odd number which rounds to 100 000
A is an odd number which rounds to 100 000 Maintenance rounds
Maintenance rounds Schwartz rounds facilitator training
Schwartz rounds facilitator training Sam rounds
Sam rounds Quality teaching rounds coding sheet
Quality teaching rounds coding sheet Red white and blue tortilla chips
Red white and blue tortilla chips Readiness rounds
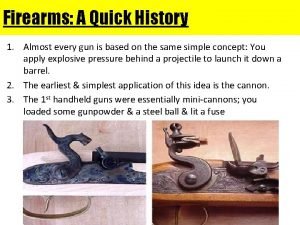
Readiness rounds Types of breech face marks
Types of breech face marks Richard elmore harvard
Richard elmore harvard Duke family medicine and community health
Duke family medicine and community health Nursing grand rounds presentation example
Nursing grand rounds presentation example Who analgesic ladder
Who analgesic ladder Borborygmi
Borborygmi Formuö
Formuö Novell typiska drag
Novell typiska drag Tack för att ni lyssnade bild
Tack för att ni lyssnade bild Ekologiskt fotavtryck
Ekologiskt fotavtryck Varför kallas perioden 1918-1939 för mellankrigstiden
Varför kallas perioden 1918-1939 för mellankrigstiden En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Adressändring ideell förening
Adressändring ideell förening Vilotidsbok
Vilotidsbok Sura för anatom
Sura för anatom Vad är densitet
Vad är densitet Datorkunskap för nybörjare
Datorkunskap för nybörjare Tack för att ni lyssnade bild
Tack för att ni lyssnade bild Mall för debattartikel
Mall för debattartikel För och nackdelar med firo
För och nackdelar med firo Nyckelkompetenser för livslångt lärande
Nyckelkompetenser för livslångt lärande Påbyggnader för flakfordon
Påbyggnader för flakfordon Tryck formel
Tryck formel Svenskt ramverk för digital samverkan
Svenskt ramverk för digital samverkan Bo bergman jag fryser om dina händer
Bo bergman jag fryser om dina händer Presentera för publik crossboss
Presentera för publik crossboss Teckenspråk minoritetsspråk argument
Teckenspråk minoritetsspråk argument Vem räknas som jude
Vem räknas som jude Treserva lathund
Treserva lathund Luftstrupen för medicinare
Luftstrupen för medicinare Bästa kameran för astrofoto
Bästa kameran för astrofoto Centrum för kunskap och säkerhet
Centrum för kunskap och säkerhet Lågenergihus nyproduktion
Lågenergihus nyproduktion Mat för unga idrottare
Mat för unga idrottare Verktyg för automatisering av utbetalningar
Verktyg för automatisering av utbetalningar Rutin för avvikelsehantering
Rutin för avvikelsehantering Smärtskolan kunskap för livet
Smärtskolan kunskap för livet Ministerstyre för och nackdelar
Ministerstyre för och nackdelar Tack för att ni har lyssnat
Tack för att ni har lyssnat Vad är referatmarkeringar
Vad är referatmarkeringar Redogör för vad psykologi är
Redogör för vad psykologi är Stål för stötfångarsystem
Stål för stötfångarsystem Atmosfr
Atmosfr Borra hål för knoppar
Borra hål för knoppar Orubbliga rättigheter
Orubbliga rättigheter Formel standardavvikelse
Formel standardavvikelse Tack för att ni har lyssnat
Tack för att ni har lyssnat Rita perspektiv
Rita perspektiv Informationskartläggning
Informationskartläggning Tobinskatten för och nackdelar
Tobinskatten för och nackdelar Blomman för dagen drog
Blomman för dagen drog Handledning reflektionsmodellen
Handledning reflektionsmodellen Egg för emanuel
Egg för emanuel Elektronik för barn
Elektronik för barn Antika plagg
Antika plagg