MODULE I Comfort Sleep and Rest Management 1













- Slides: 75
MODULE I Comfort, Sleep and Rest Management 1
Chapter 42 Sleep
Physiology of Sleep � Circadian rhythms ◦ Affected by light, temperature, social activities, and work routines. � The biological rhythm of sleep frequently becomes synchronized with other body functions.
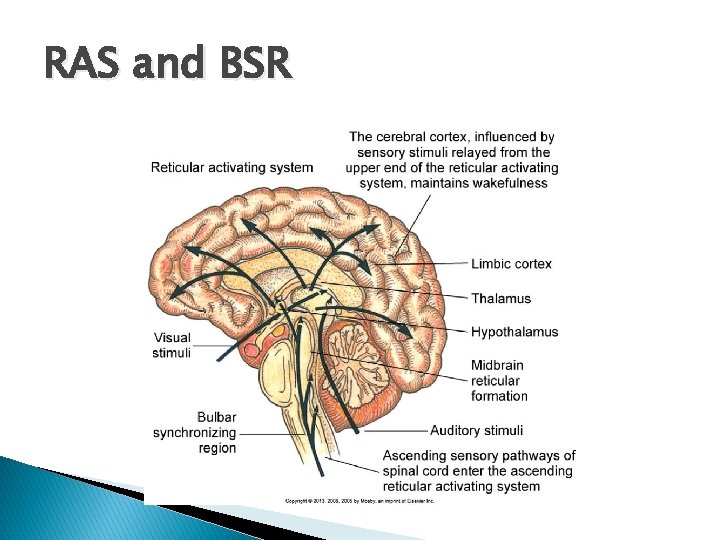
Physiology of Sleep: Sleep Regulation � Regulated by a sequence of physiological states integrated by central nervous system (CNS) activity � Hypothalamus � Reticular activating system (RAS) � Bulbar synchronizing region (BSR)
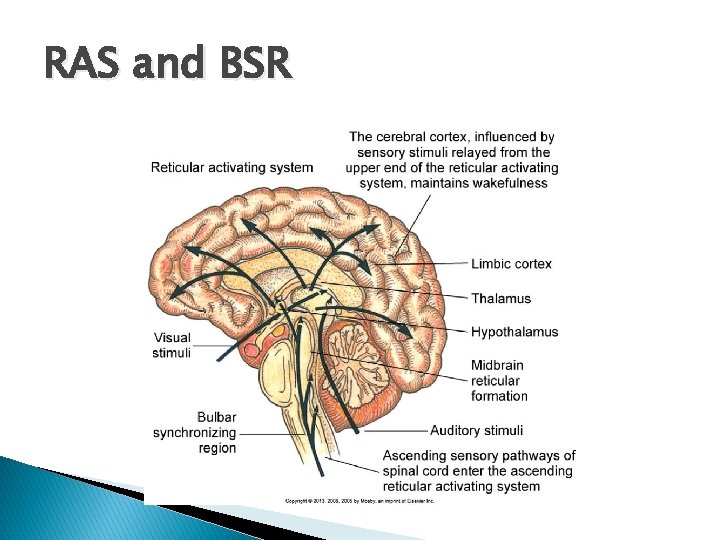
RAS and BSR
Case Study Walter Murphy is 82 years old and has resided in the local nursing home for the past 3 months. His wife, Mary, still lives at home but visits Walter on a daily basis. Walter is confined to a wheelchair as a result of osteoarthritis and a mild stroke he experienced 1 year ago. Even though he has physical limitations, he is alert and oriented. � Over the past several weeks, Mary found her husband to be very sleepy when visiting him just before lunchtime. Walter tells Mary that he has trouble falling asleep at night, and once he does fall asleep, he reawakens frequently during the night. �
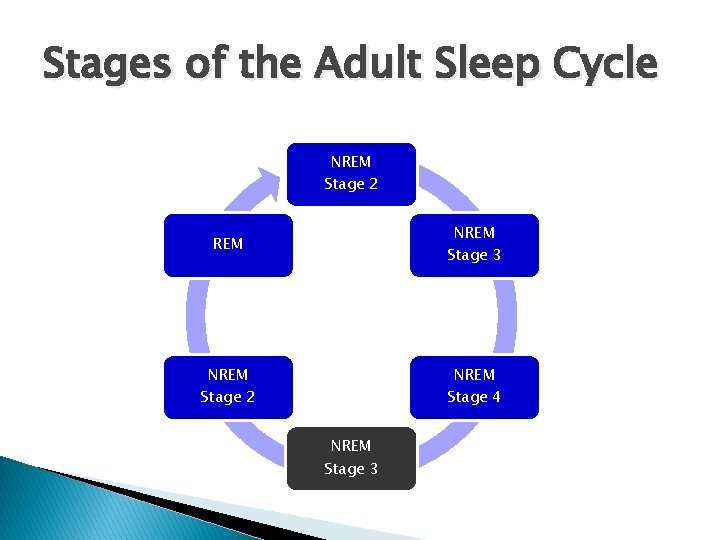
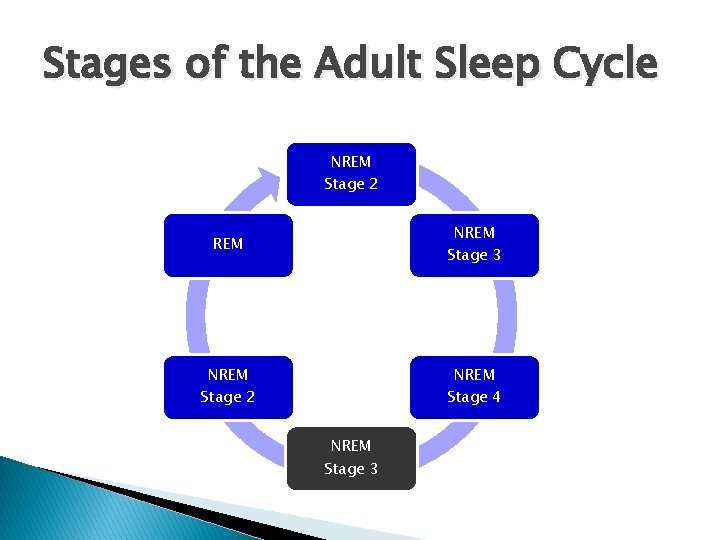
Stages of the Adult Sleep Cycle NREM Stage 2 REM NREM Stage 3 NREM Stage 2 NREM Stage 4 NREM Stage 3
Functions of Sleep � Purpose of sleep ◦ Remains unclear ◦ Physiological and psychological restoration ◦ Maintenance of biological functions � Dreams ◦ Occur in nonrapid eye movement (NREM) and rapid eye movement (REM) sleep ◦ Important for learning, memory, and adaptation to stress
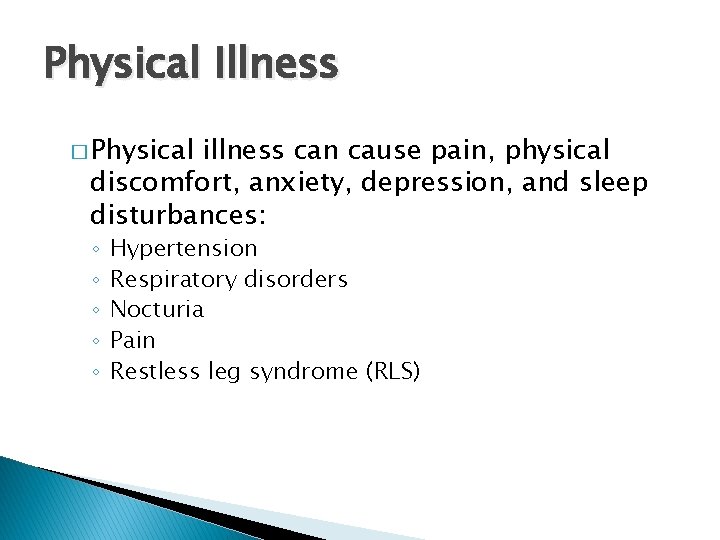
Physical Illness � Physical illness can cause pain, physical discomfort, anxiety, depression, and sleep disturbances: ◦ ◦ ◦ Hypertension Respiratory disorders Nocturia Pain Restless leg syndrome (RLS)

Terminology � � � Hypersomnolence = Excessive sleepiness. A polysomnogram involves the use of electroencephalography (EEG), electromyography (EMG), and electro-oculography (EOG) to monitor stages of sleep and wakefulness during nighttime sleep. Sleep hygiene = Practices that a patient associates with sleep. Cataplexy is sudden muscle weakness during intense emotions such as anger, sadness, or laughter; it can occur at any time during the day. Sleep paralysis is the feeling of being unable to move or talk just before waking or falling asleep.
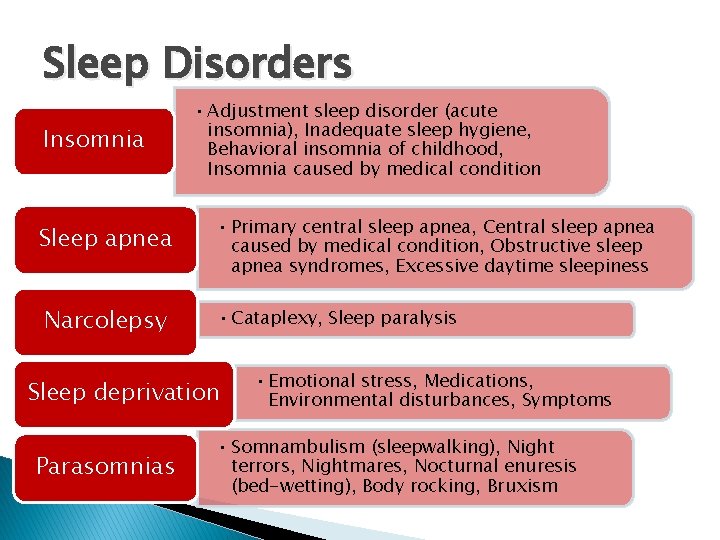
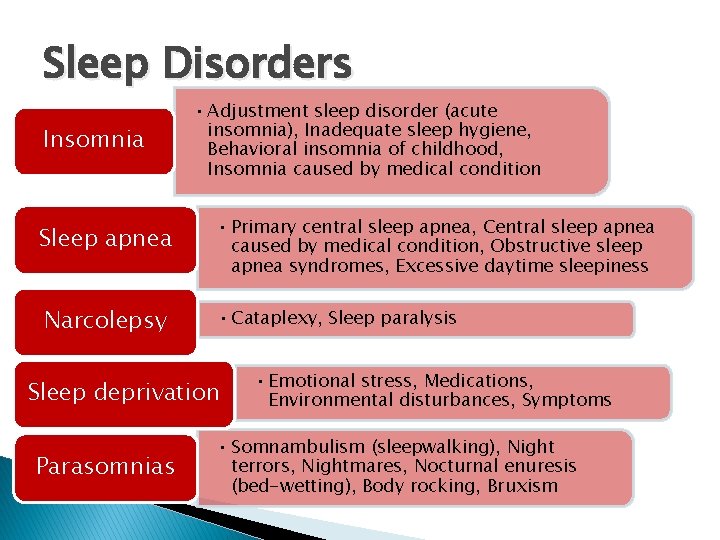
Sleep Disorders Insomnia • Adjustment sleep disorder (acute insomnia), Inadequate sleep hygiene, Behavioral insomnia of childhood, Insomnia caused by medical condition Sleep apnea • Primary central sleep apnea, Central sleep apnea caused by medical condition, Obstructive sleep apnea syndromes, Excessive daytime sleepiness Narcolepsy • Cataplexy, Sleep paralysis Sleep deprivation Parasomnias • Emotional stress, Medications, Environmental disturbances, Symptoms • Somnambulism (sleepwalking), Night terrors, Nightmares, Nocturnal enuresis (bed-wetting), Body rocking, Bruxism
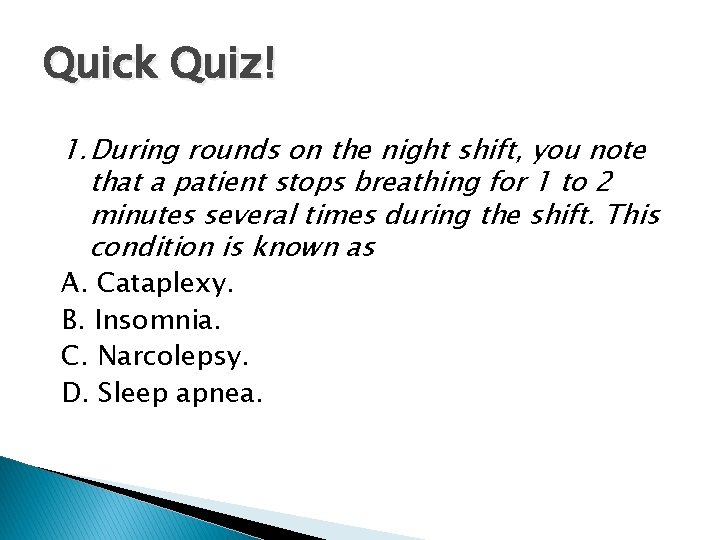
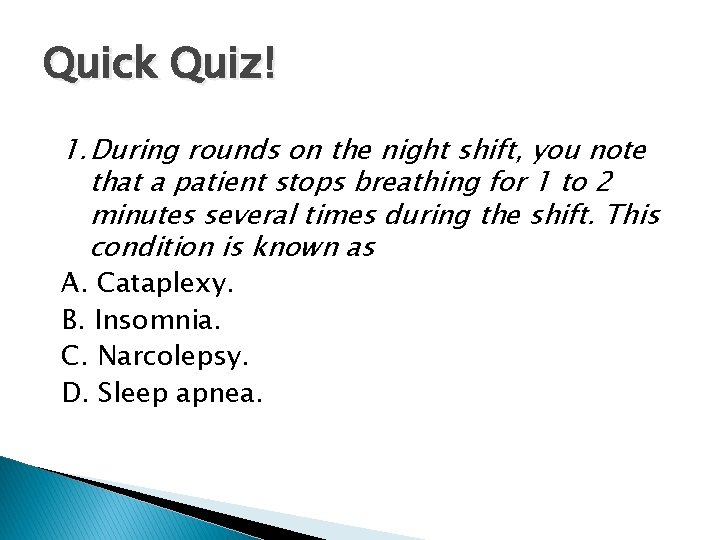
Quick Quiz! 1. During rounds on the night shift, you note that a patient stops breathing for 1 to 2 minutes several times during the shift. This condition is known as A. Cataplexy. B. Insomnia. C. Narcolepsy. D. Sleep apnea.

Sleep and Rest � Rest contributes to: ◦ Mental relaxation ◦ Freedom from anxiety ◦ State of mental, physical, and spiritual activity � Bed rest does not guarantee that a patient will feel rested.
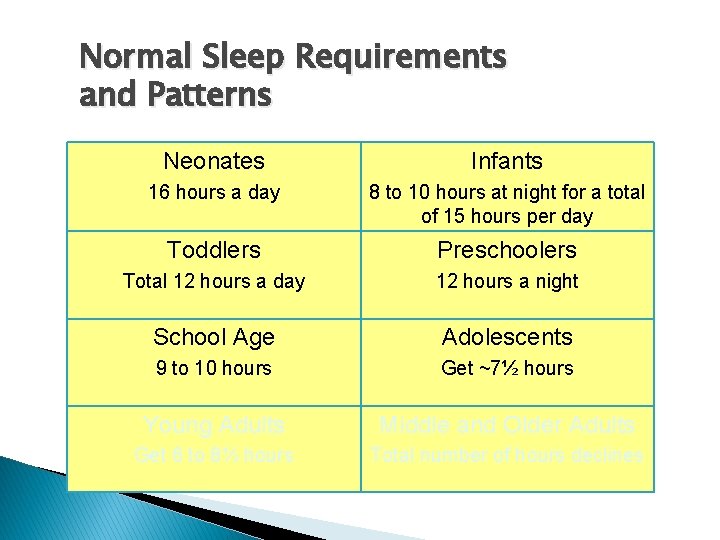
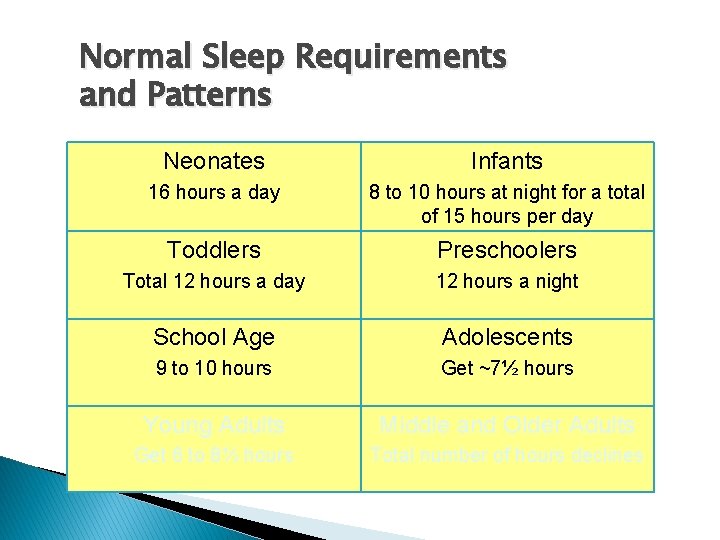
Normal Sleep Requirements and Patterns Neonates Infants 16 hours a day 8 to 10 hours at night for a total of 15 hours per day Toddlers Preschoolers Total 12 hours a day 12 hours a night School Age Adolescents 9 to 10 hours Get ~7½ hours Young Adults Middle and Older Adults Get 6 to 8½ hours Total number of hours declines
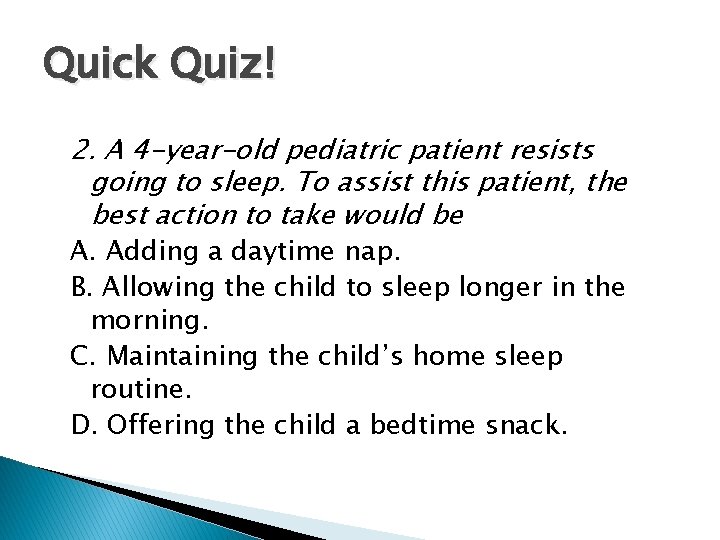
Quick Quiz! 2. A 4 -year-old pediatric patient resists going to sleep. To assist this patient, the best action to take would be A. Adding a daytime nap. B. Allowing the child to sleep longer in the morning. C. Maintaining the child’s home sleep routine. D. Offering the child a bedtime snack.

Factors Affecting Sleep Physical illness Drugs and substances Lifestyle Usual sleep patterns Emotional stress Environment Hypertension, respiratory, musculoskeletal, chronic illness, GI, nausea Work schedule, social activities, routines Worries, physical health, death, losses Hypnotics, diuretics, narcotics, antidepressants, alcohol, caffeine, betablockers, anticonvulsants May be disrupted by social activity or work schedule Noise, routines

Quick Quiz! 3. A patient suffers from sleep pattern disturbance. To promote adequate sleep, the most important nursing intervention is A. Administering a sleep aid. B. Synchronizing the medication, treatment, and vital signs schedule. C. Encouraging the patient to exercise immediately before sleep. D. Discussing with the patient the benefits of beginning a long-term night-time medication regimen. iok

Case Study (cont’d) � Anna is a 23 -year-old nursing student assigned to the nursing home for her second semester in nursing school. She has had experience in nursing homes, having worked in one center as a nurse assistant during the last two summers. Anna’s assignment is to care for Mr. Murphy over the next 4 weeks. � What factors could Anna consider when preparing to care for Mr. Murphy?
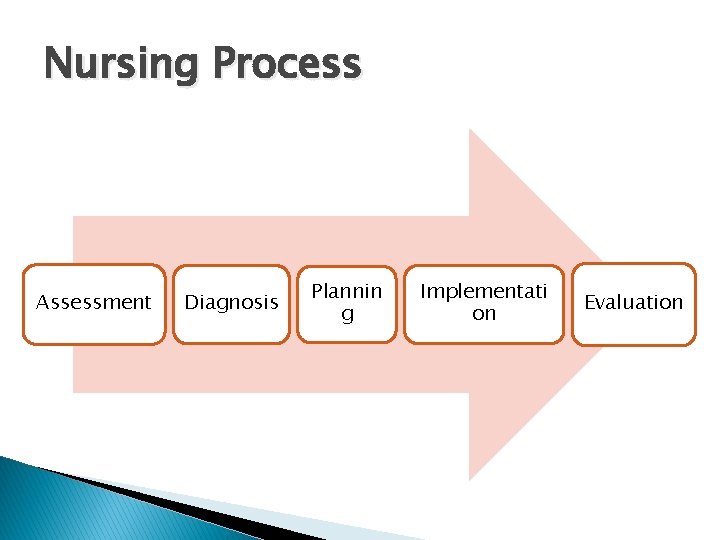
Nursing Process Assessment Diagnosis Plannin g Implementati on Evaluation
Case Study (cont’d) � As Anna prepares to conduct an assessment of Mr. Murphy, she knows it is important to consider how sleep is altered in older adults. Because they typically have less deep sleep and more awakenings, it will be important to consider what factors in the nursing home disrupt sleep. � She has learned that his osteoarthritis pain is a contributing factor to the sleep disturbances. His immobility from the stroke adds discomfort. � Anna also plans to assess Mr. Murphy’s medications carefully to determine whether any drugs are adding to a sleep alteration.
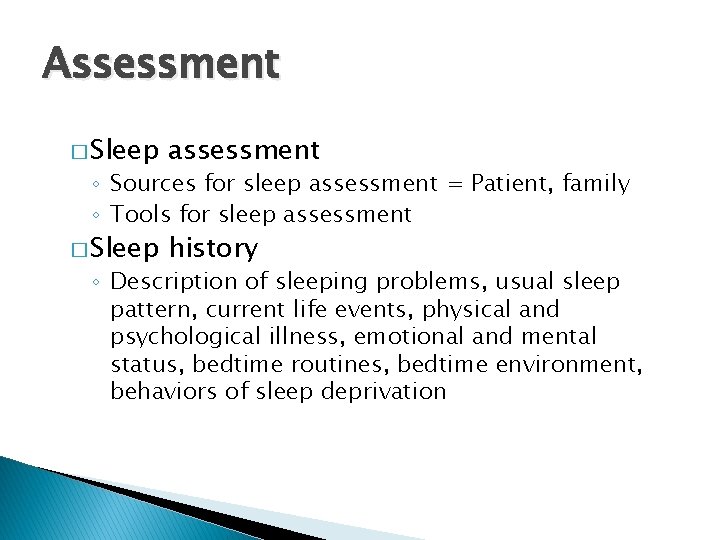
Assessment � Sleep assessment � Sleep history ◦ Sources for sleep assessment = Patient, family ◦ Tools for sleep assessment ◦ Description of sleeping problems, usual sleep pattern, current life events, physical and psychological illness, emotional and mental status, bedtime routines, bedtime environment, behaviors of sleep deprivation
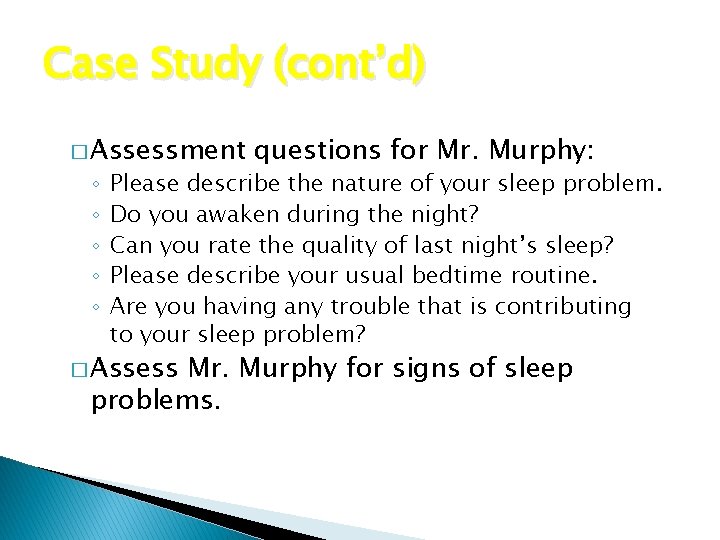
Case Study (cont’d) � Assessment ◦ ◦ ◦ questions for Mr. Murphy: Please describe the nature of your sleep problem. Do you awaken during the night? Can you rate the quality of last night’s sleep? Please describe your usual bedtime routine. Are you having any trouble that is contributing to your sleep problem? � Assess Mr. Murphy for signs of sleep problems.
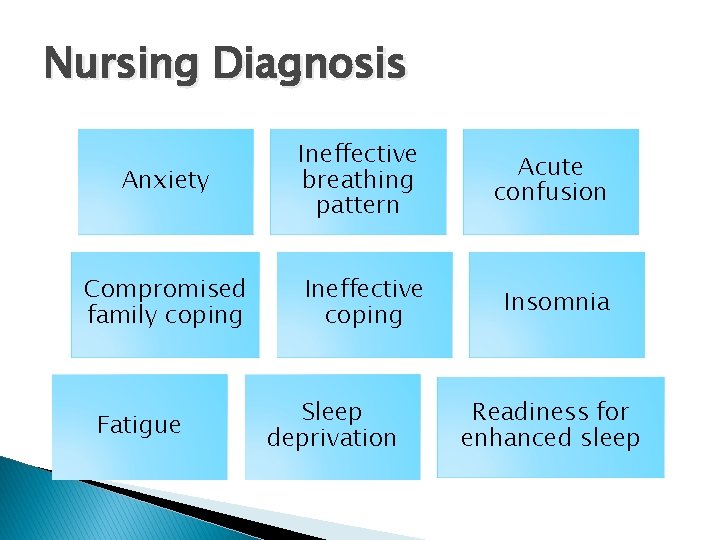
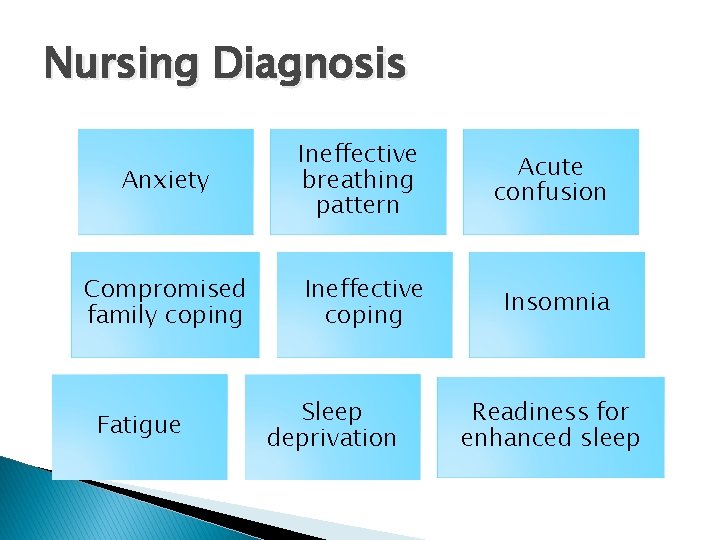
Nursing Diagnosis Anxiety Ineffective breathing pattern Acute confusion Compromised family coping Ineffective coping Insomnia Fatigue Sleep deprivation Readiness for enhanced sleep
Case Study (cont’d) � Nursing diagnosis: insomnia ◦ Related to excessive environmental stimuli � Goal ◦ Mr. Murphy will attain a sense of restfulness after sleep in 1 month.
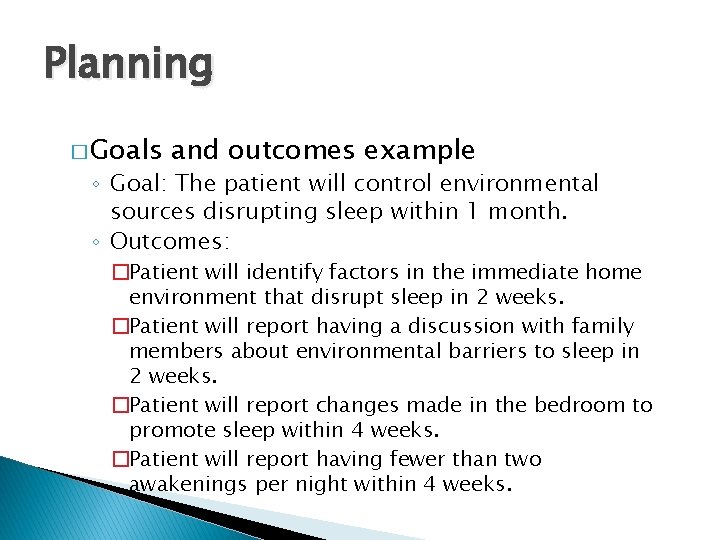
Planning � Goals and outcomes example ◦ Goal: The patient will control environmental sources disrupting sleep within 1 month. ◦ Outcomes: �Patient will identify factors in the immediate home environment that disrupt sleep in 2 weeks. �Patient will report having a discussion with family members about environmental barriers to sleep in 2 weeks. �Patient will report changes made in the bedroom to promote sleep within 4 weeks. �Patient will report having fewer than two awakenings per night within 4 weeks.

Implementation � Health ◦ ◦ ◦ ◦ promotion Environmental controls Promoting bedtime routines Promoting safety Promoting comfort Establishing periods of rest and sleep Stress reduction Bedtime snacks Pharmacological approaches
Implementation (cont’d)
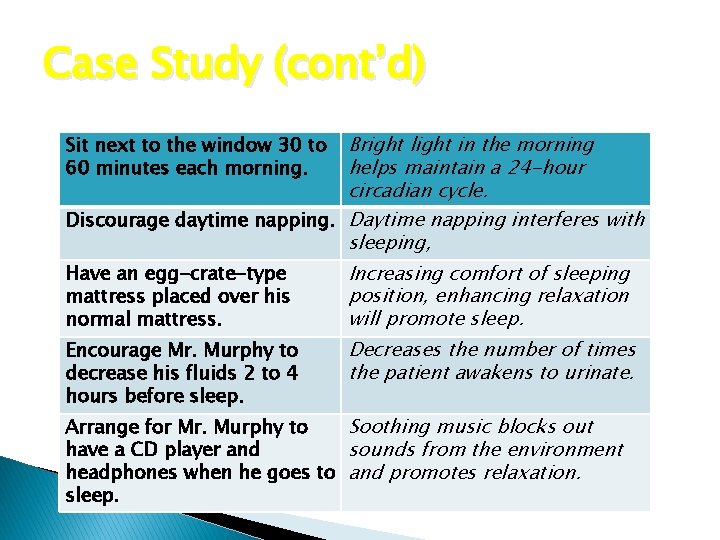
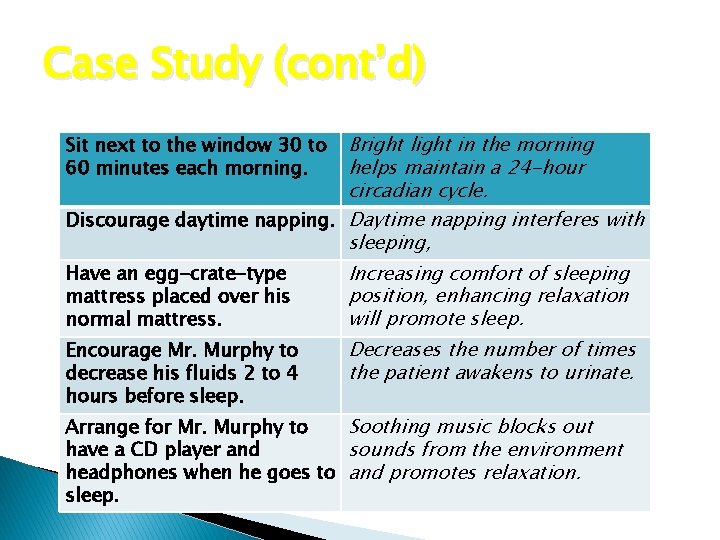
Case Study (cont’d) Bright light in the morning helps maintain a 24 -hour circadian cycle. Discourage daytime napping. Daytime napping interferes with sleeping, Sit next to the window 30 to 60 minutes each morning. Have an egg-crate-type mattress placed over his normal mattress. Increasing comfort of sleeping position, enhancing relaxation will promote sleep. Encourage Mr. Murphy to decrease his fluids 2 to 4 hours before sleep. Decreases the number of times the patient awakens to urinate. Arrange for Mr. Murphy to Soothing music blocks out have a CD player and sounds from the environment headphones when he goes to and promotes relaxation. sleep.
Implementation (cont’d) � Acute ◦ ◦ ◦ care Environmental controls Promoting comfort Establishing periods of rest and sleep Promoting safety Stress reduction � Restorative or continuing care ◦ Promoting comfort ◦ Controlling physiological disturbances ◦ Pharmacological approaches
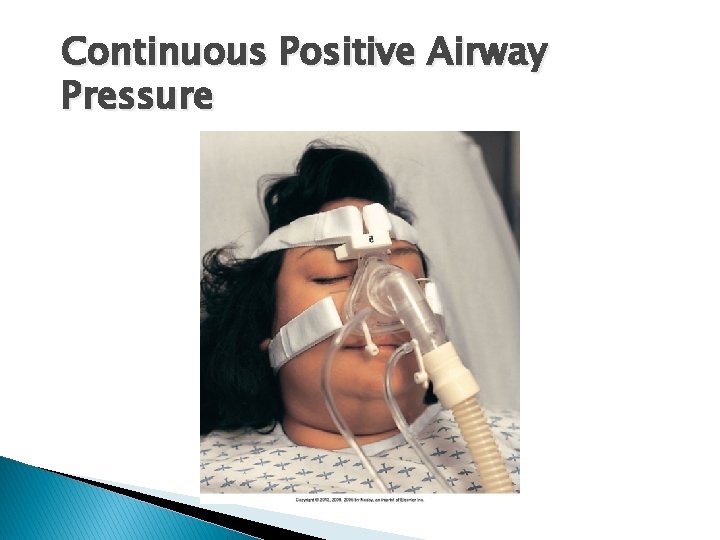
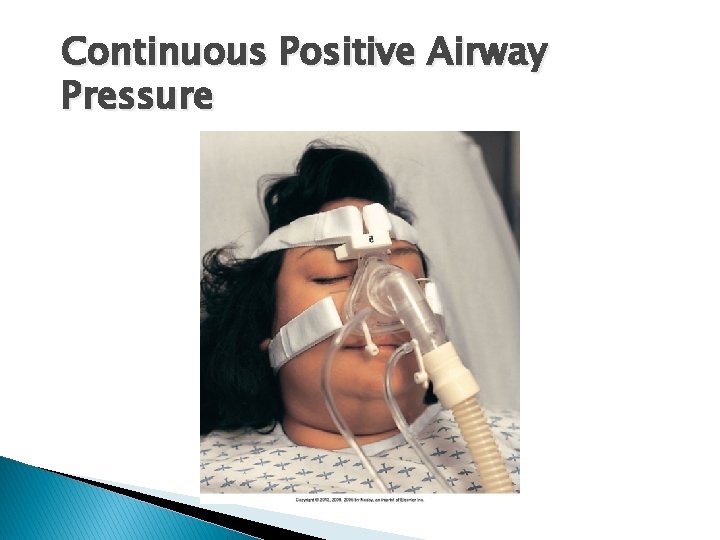
Continuous Positive Airway Pressure
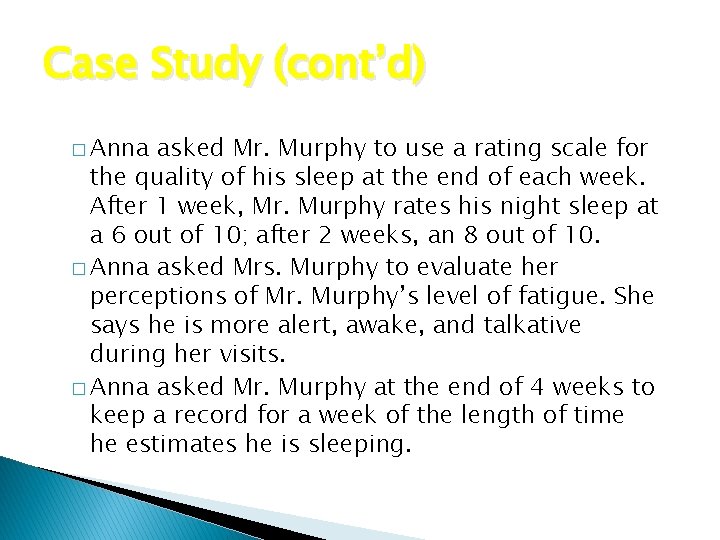
Case Study (cont’d) � Anna asked Mr. Murphy to use a rating scale for the quality of his sleep at the end of each week. After 1 week, Mr. Murphy rates his night sleep at a 6 out of 10; after 2 weeks, an 8 out of 10. � Anna asked Mrs. Murphy to evaluate her perceptions of Mr. Murphy’s level of fatigue. She says he is more alert, awake, and talkative during her visits. � Anna asked Mr. Murphy at the end of 4 weeks to keep a record for a week of the length of time he estimates he is sleeping.
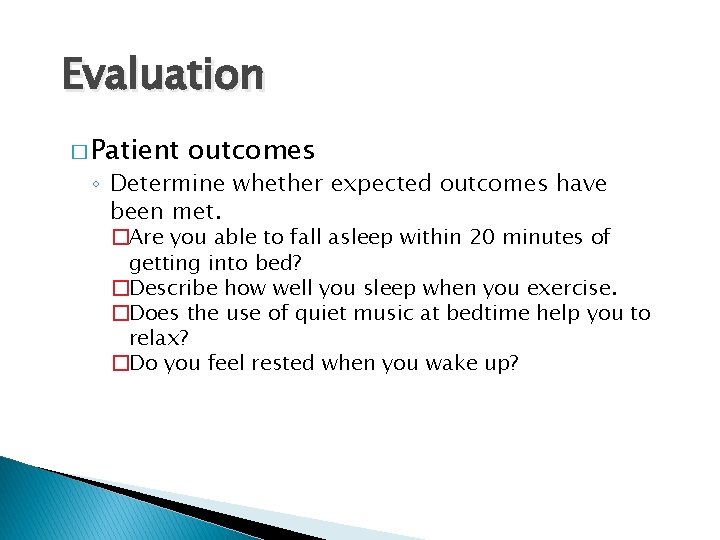
Evaluation � Patient outcomes ◦ Determine whether expected outcomes have been met. �Are you able to fall asleep within 20 minutes of getting into bed? �Describe how well you sleep when you exercise. �Does the use of quiet music at bedtime help you to relax? �Do you feel rested when you wake up?
Chapter 43 Pain Management
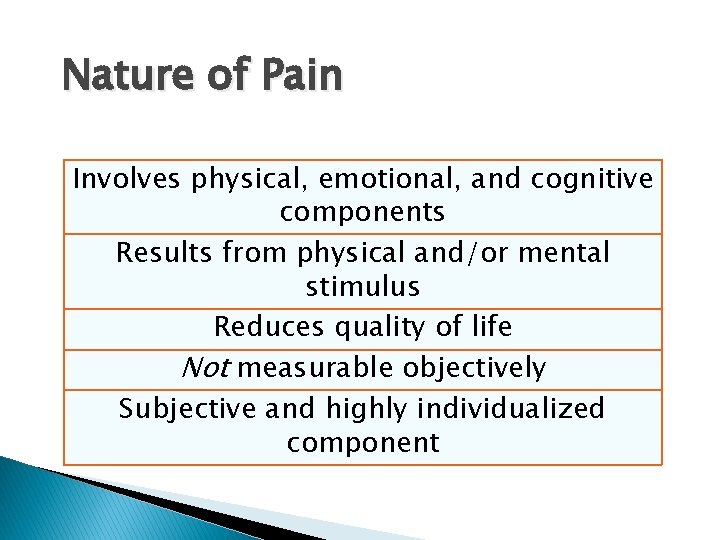
Nature of Pain Involves physical, emotional, and cognitive components Results from physical and/or mental stimulus Reduces quality of life Not measurable objectively Subjective and highly individualized component

Transmission of Pain Impulse
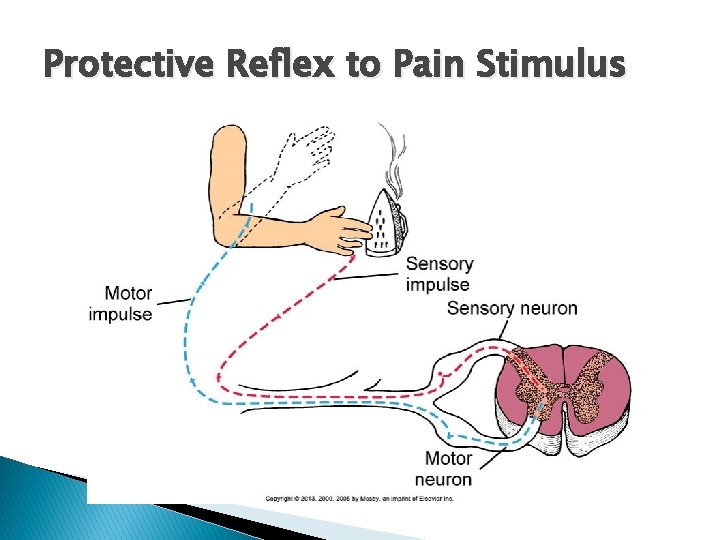
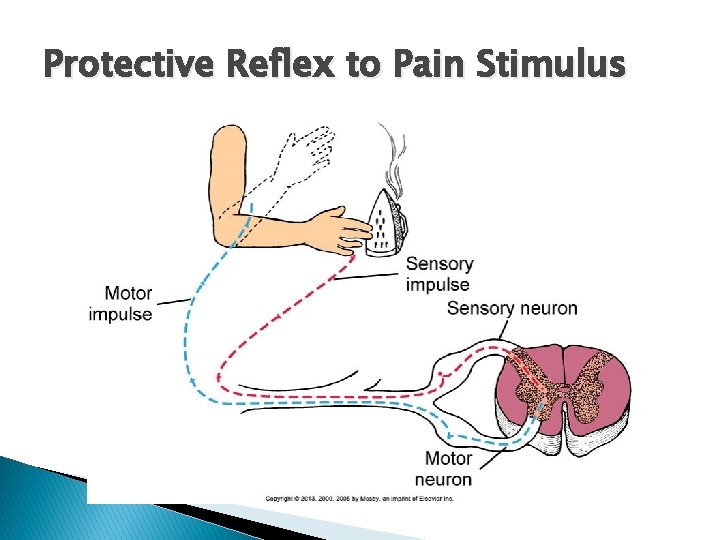
Physiology of Pain � Cellular damage by thermal, mechanical, or chemical stimuli causes release of neurotransmitters. ◦ Prostaglandins, bradykinin, potassium, histamine, substance P � Neurotransmitters surround the pain fibers, spreading the pain message and causing an inflammatory response. � Nerve impulse travel along afferent (sensory) nerve fibers to the spinal cord.
Physiology of Pain (cont’d) � Pain impulses ascend the spinal cord to the thalamus, which transmits information to higher brain centers that perceive pain. � Two types of sensory nerve fibers: ◦ Fast myelinated A-delta fibers: send sharp, localized, distinct sensations ◦ Slow, small, unmyelinated C fibers: send poorly localized, burning, persistent pain

Physiology of Pain (cont’d) Transduction Conversion of stimulus into electrical energy Transmission Sending of impulse across a sensory pain nerve fiber (nociceptor) Perception Modulation The patient’s Inhibition of pain/ experience of pain release of inhibitory neurotransmitters
Physiology of Pain (cont’d) � Gate-control Wall) theory of pain (Melzack and ◦ Pain has emotional and cognitive components, in addition to a physical sensation. ◦ Gating mechanisms in the central nervous system (CNS) regulate or block pain impulses. ◦ Pain impulses pass through when a gate is open and are blocked when a gate is closed. ◦ Closing the gate is the basis for nonpharmacological pain relief interventions.
Case Study � Mrs. Ellis is a 70 -year-old African American woman with hypertension, diabetes, and rheumatoid arthritis. Her current health priority is the discomfort and disability associated with her rheumatoid arthritis. � Arthritis has severely deformed her hands and feet. The pain in her feet is so severe that she often walks only short distances. The pain interferes with sleep and reduces her energy both physically and emotionally. As a result, she does not leave home often.
Protective Reflex to Pain Stimulus
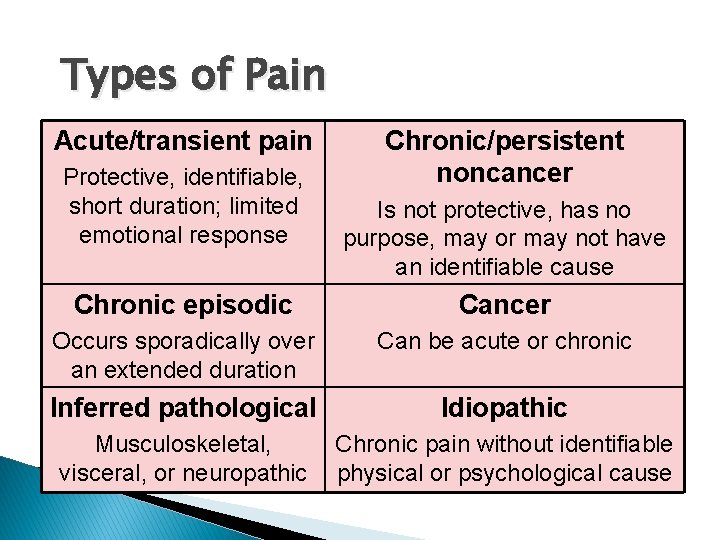
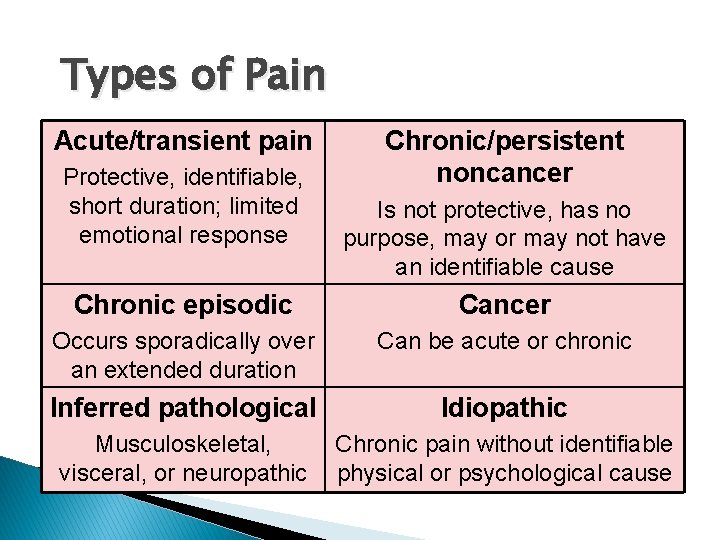
Types of Pain Acute/transient pain Protective, identifiable, short duration; limited emotional response Chronic/persistent noncancer Is not protective, has no purpose, may or may not have an identifiable cause Chronic episodic Cancer Occurs sporadically over an extended duration Can be acute or chronic Inferred pathological Idiopathic Musculoskeletal, visceral, or neuropathic Chronic pain without identifiable physical or psychological cause
Nursing Knowledge Base � Attitude of health care providers ◦ Malingerer or complainer � Assumptions about patients in pain ◦ Biases based on culture, education, experiences ◦ Acknowledge pain through patient’s experiences ◦ Limit your ability to help the patient
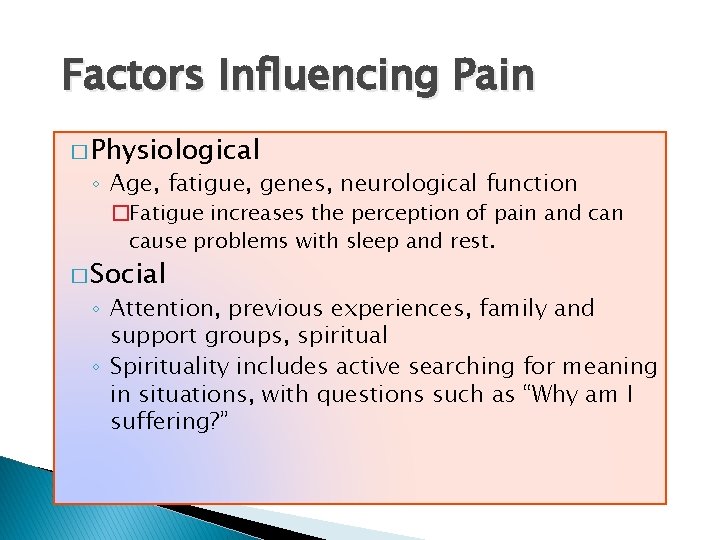
Factors Influencing Pain � Physiological ◦ Age, fatigue, genes, neurological function �Fatigue increases the perception of pain and can cause problems with sleep and rest. � Social ◦ Attention, previous experiences, family and support groups, spiritual ◦ Spirituality includes active searching for meaning in situations, with questions such as “Why am I suffering? ”
Factors Influencing Pain (cont’d) � Psychological ◦ Anxiety ◦ Coping style � Pain tolerance ◦ The level of pain a person is willing to accept � Cultural ◦ Meaning of pain ◦ Ethnicity
Nursing Process and Pain � Pain management needs to be systematic. � Pain management needs to consider the patient’s quality of life. � Clinical guidelines are available to manage pain: ◦ American Pain Society ◦ National Guideline Clearing House (www. guideline. gov) ◦ Agency for Healthcare Research and Quality (AHRQ)
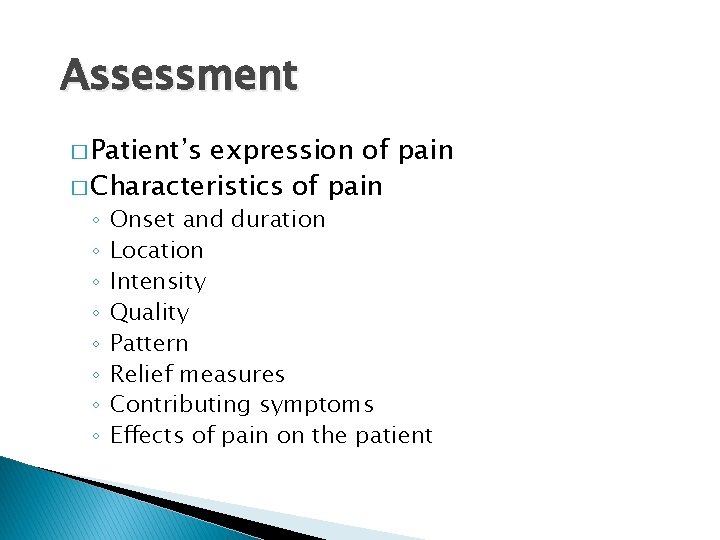
Assessment � Patient’s expression of pain � Characteristics of pain ◦ ◦ ◦ ◦ Onset and duration Location Intensity Quality Pattern Relief measures Contributing symptoms Effects of pain on the patient

Sample Pain Scales
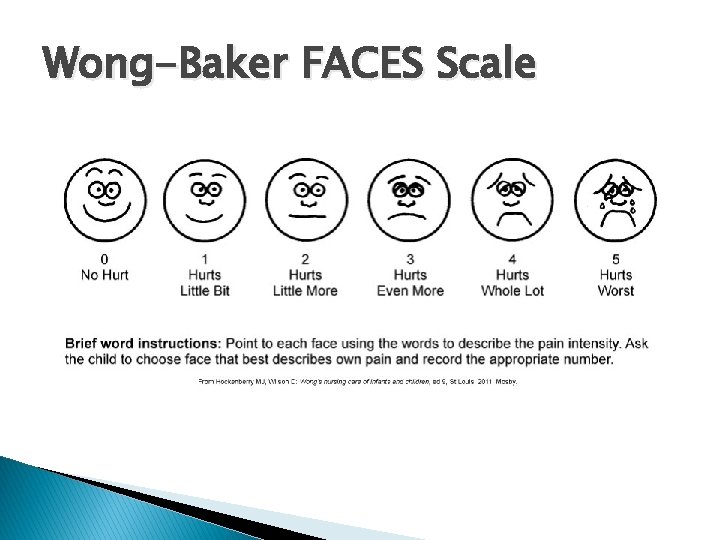
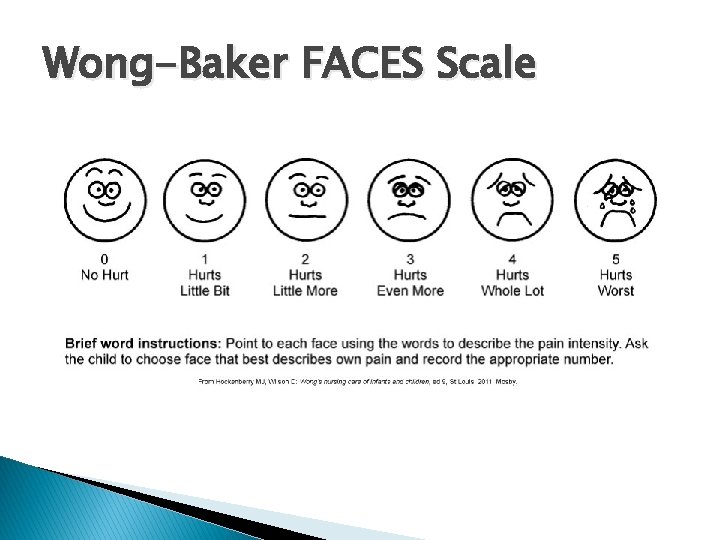
Wong-Baker FACES Scale
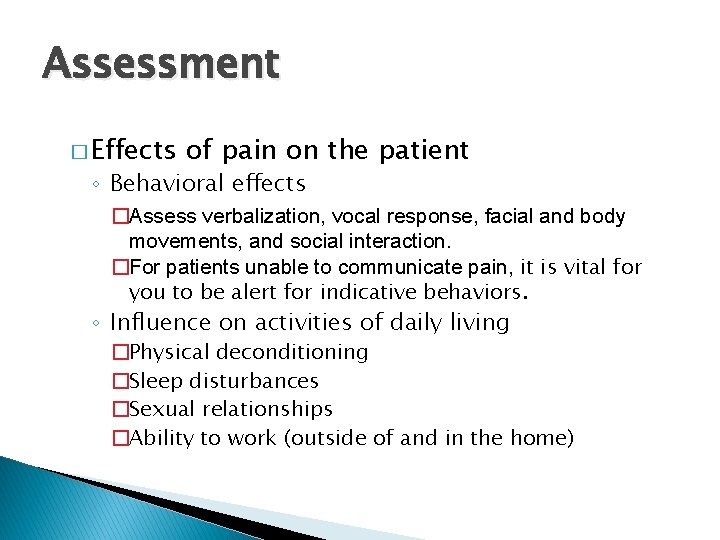
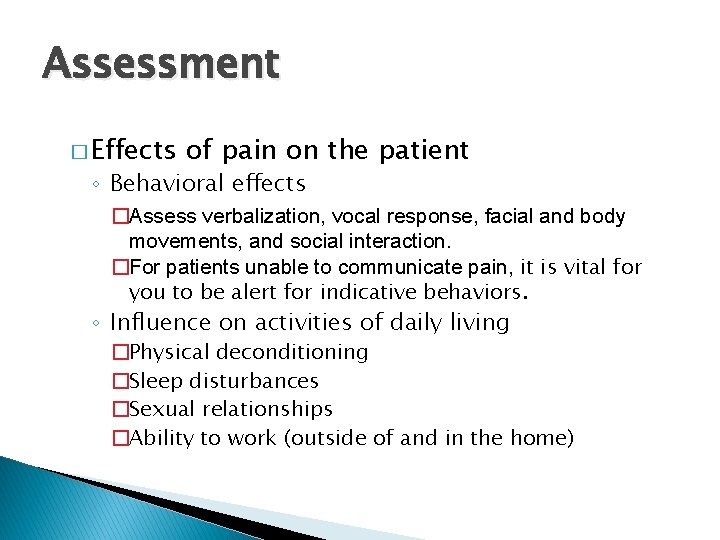
Assessment � Effects of pain on the patient ◦ Behavioral effects �Assess verbalization, vocal response, facial and body movements, and social interaction. �For patients unable to communicate pain, it is vital for you to be alert for indicative behaviors. ◦ Influence on activities of daily living �Physical deconditioning �Sleep disturbances �Sexual relationships �Ability to work (outside of and in the home)
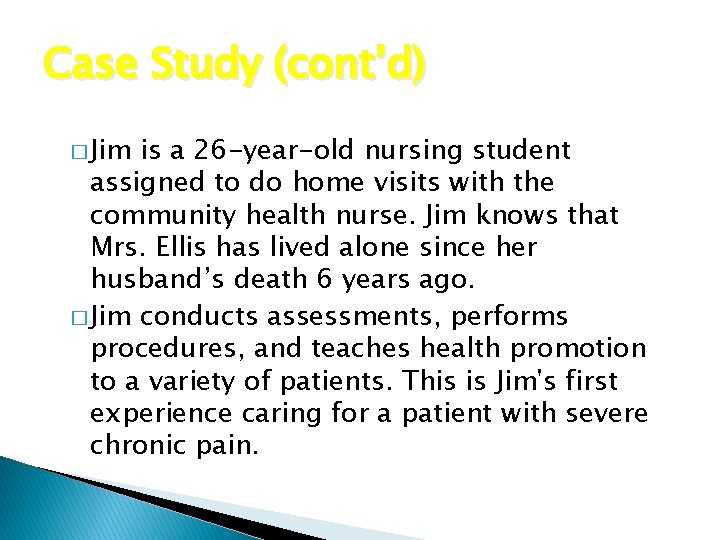
Case Study (cont’d) � Jim is a 26 -year-old nursing student assigned to do home visits with the community health nurse. Jim knows that Mrs. Ellis has lived alone since her husband’s death 6 years ago. � Jim conducts assessments, performs procedures, and teaches health promotion to a variety of patients. This is Jim's first experience caring for a patient with severe chronic pain.
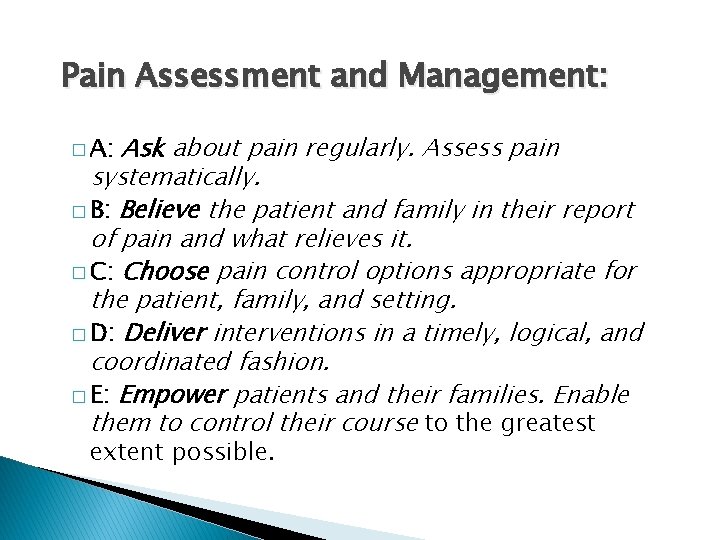
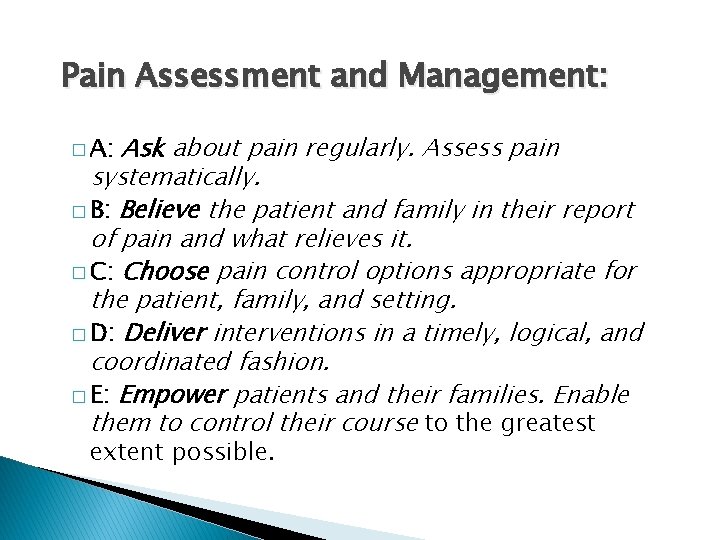
Pain Assessment and Management: Ask about pain regularly. Assess pain systematically. � B: Believe the patient and family in their report of pain and what relieves it. � C: Choose pain control options appropriate for the patient, family, and setting. � D: Deliver interventions in a timely, logical, and coordinated fashion. � E: Empower patients and their families. Enable them to control their course to the greatest � A: extent possible.
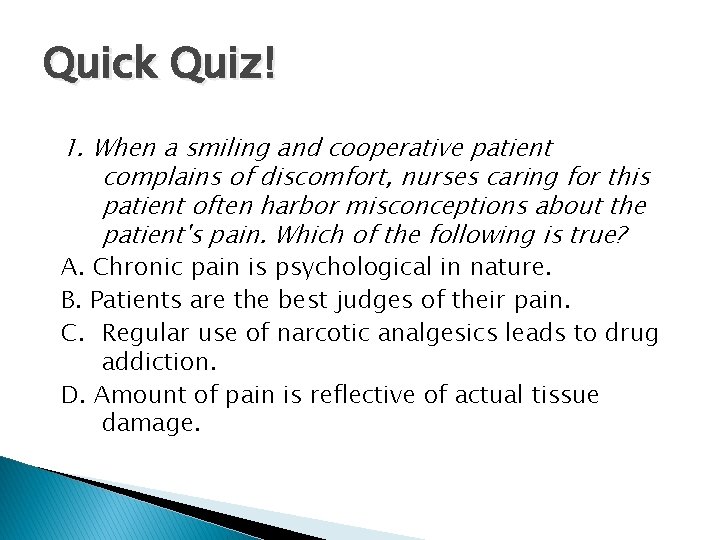
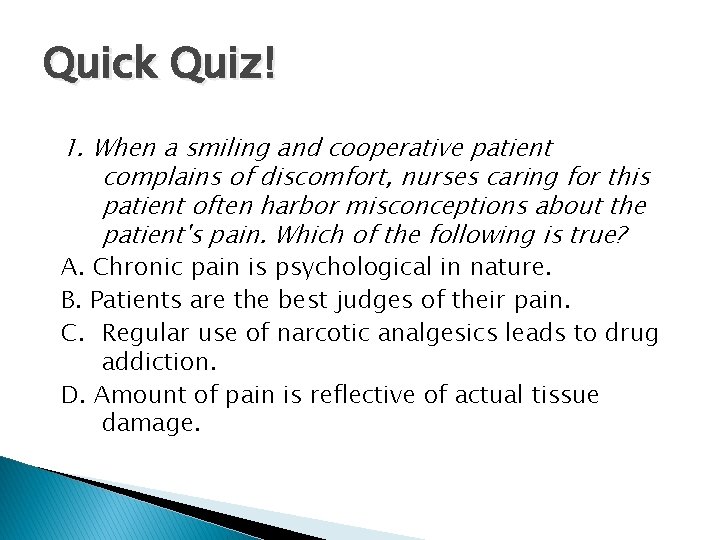
Quick Quiz! 1. When a smiling and cooperative patient complains of discomfort, nurses caring for this patient often harbor misconceptions about the patient's pain. Which of the following is true? A. Chronic pain is psychological in nature. B. Patients are the best judges of their pain. C. Regular use of narcotic analgesics leads to drug addiction. D. Amount of pain is reflective of actual tissue damage.
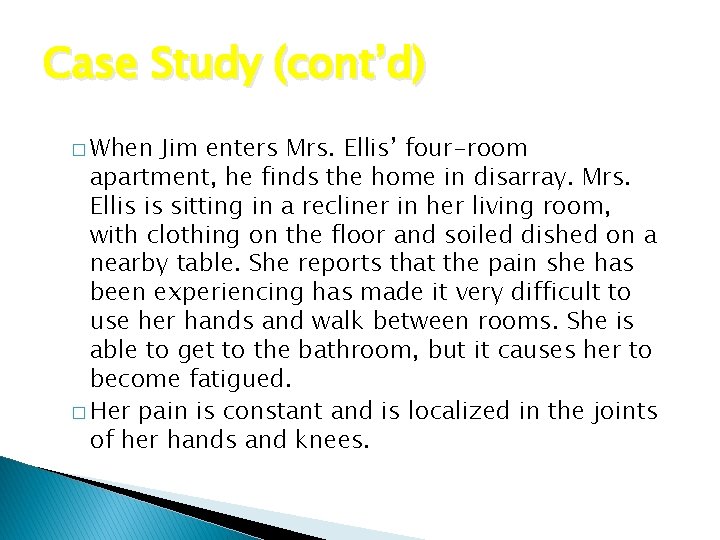
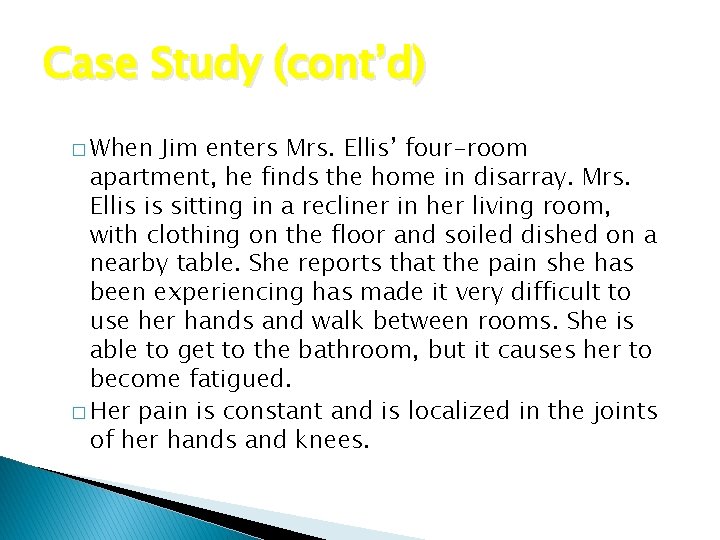
Case Study (cont’d) � When Jim enters Mrs. Ellis’ four-room apartment, he finds the home in disarray. Mrs. Ellis is sitting in a recliner in her living room, with clothing on the floor and soiled dished on a nearby table. She reports that the pain she has been experiencing has made it very difficult to use her hands and walk between rooms. She is able to get to the bathroom, but it causes her to become fatigued. � Her pain is constant and is localized in the joints of her hands and knees.
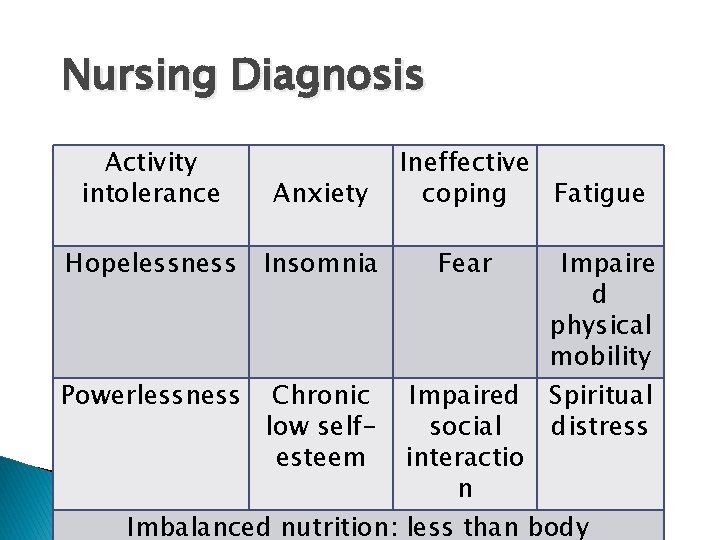
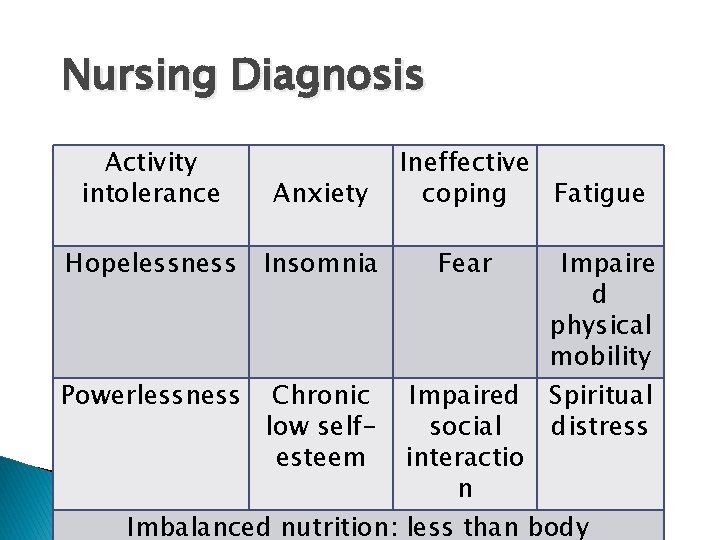
Nursing Diagnosis Activity intolerance Anxiety Hopelessness Insomnia Powerlessness Chronic low selfesteem Ineffective coping Fatigue Fear Impaire d physical mobility Spiritual distress Impaired social interactio n Imbalanced nutrition: less than body
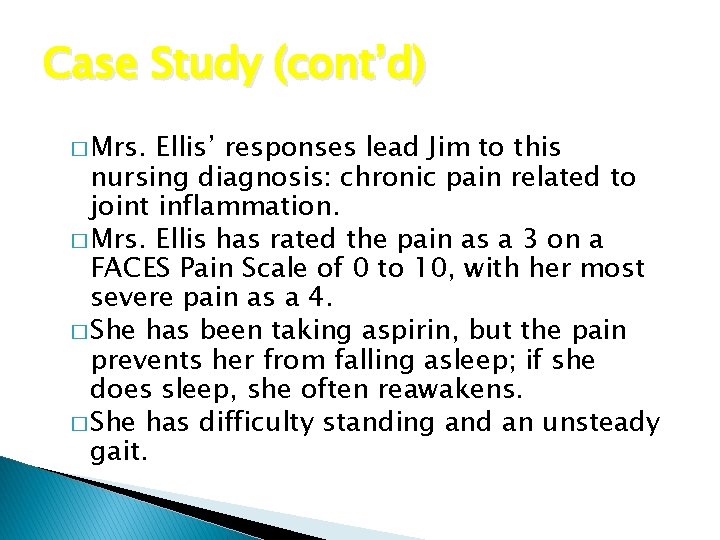
Case Study (cont’d) � Mrs. Ellis’ responses lead Jim to this nursing diagnosis: chronic pain related to joint inflammation. � Mrs. Ellis has rated the pain as a 3 on a FACES Pain Scale of 0 to 10, with her most severe pain as a 4. � She has been taking aspirin, but the pain prevents her from falling asleep; if she does sleep, she often reawakens. � She has difficulty standing and an unsteady gait.
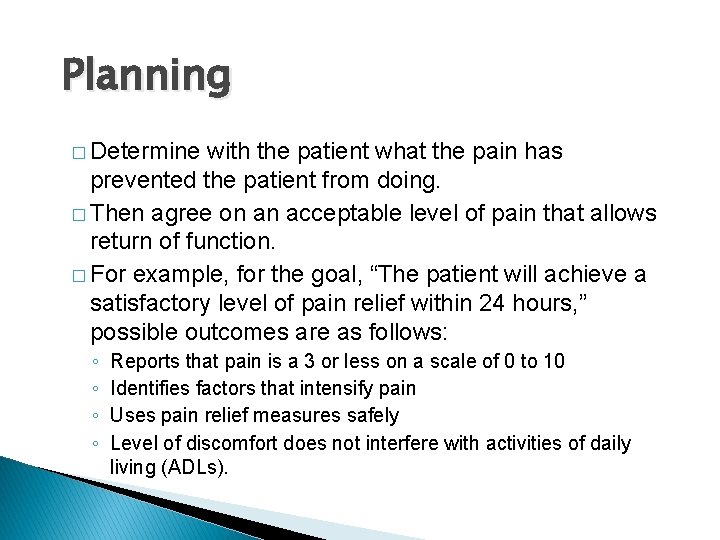
Planning � Determine with the patient what the pain has prevented the patient from doing. � Then agree on an acceptable level of pain that allows return of function. � For example, for the goal, “The patient will achieve a satisfactory level of pain relief within 24 hours, ” possible outcomes are as follows: ◦ ◦ Reports that pain is a 3 or less on a scale of 0 to 10 Identifies factors that intensify pain Uses pain relief measures safely Level of discomfort does not interfere with activities of daily living (ADLs).
Implementation: Health Promotion � Nonpharmacological interventions ◦ ◦ pain relief Relaxation, guided imagery Biofeedback Distraction, music Cutaneous stimulation �Massage, transcutaneous electrical nerve stimulation (TENS), heat, cold, acupressure ◦ Herbals ◦ Reducing pain perception

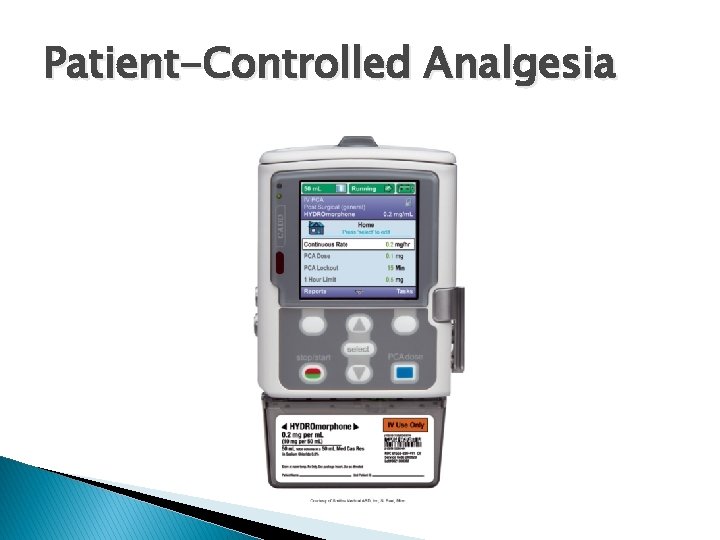
Implementation: Health Promotion (cont’d) � Pharmacological pain relief ◦ Acute pain management ◦ Analgesics �Nonopioids �Opioids �Adjuvants/co-analgesics ◦ Delivery systems �Patient-controlled analgesia (PCA) �Local/regional anesthesia �Topical agents
Case Study (cont’d) � Jim discussed with Mrs. Ellis’ primary health care provider the possibility of starting a diseasemodifying antirheumatic drug (DMARD), a biological response modifier, a nonsteroidal anti -inflammatory drug (NSAID), or an analgesic. � Jim had Mrs. Ellis take analgesics approximately 30 minutes before ambulating, performing selfcare activities, or going to sleep. He instructed her to take medication with a light snack or meal and a full glass of water. During instruction, he explained that the drug will relieve the pain.
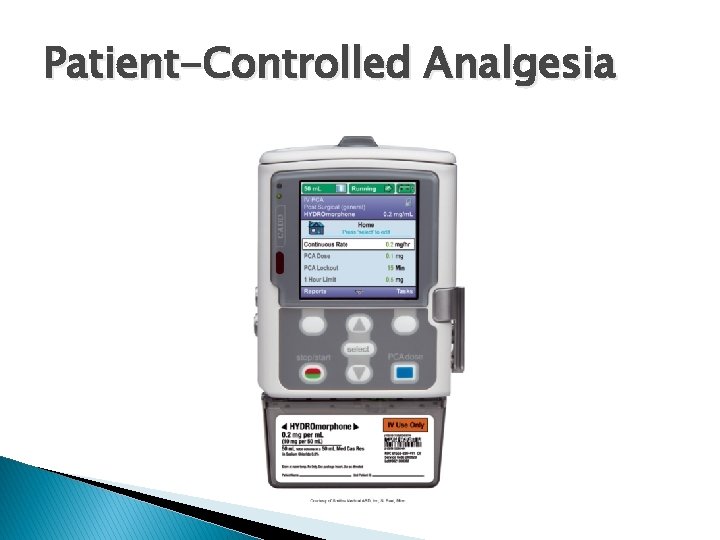
Patient-Controlled Analgesia
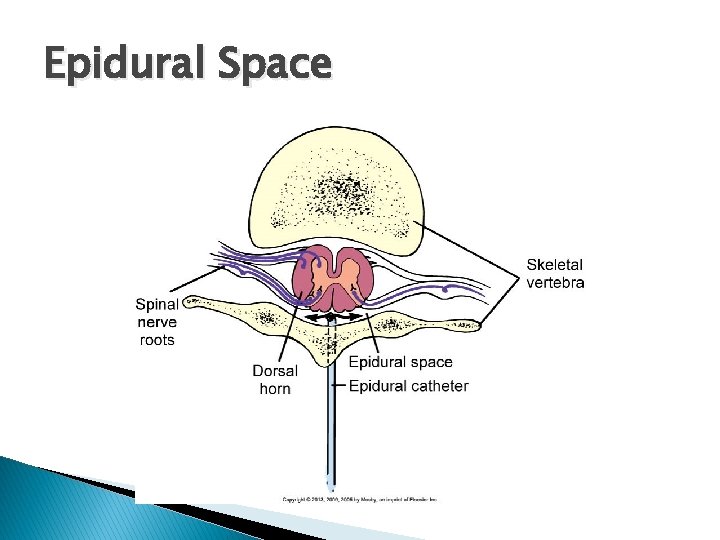
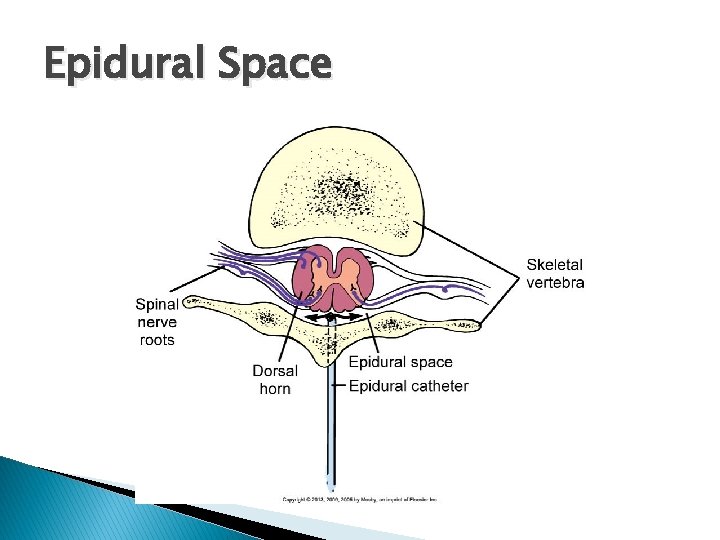
Epidural Space
Case Study (cont’d) � Jim also suggested the following to Mrs. Ellis: ◦ Place a sturdy stool in the shower stall and run warm water continuously over joints of the hands and feet. ◦ Apply moist, warm compresses to the joints of the hands 3 times a day. ◦ Referral to a physical therapist to determine possible use of a walker or other assistive device � What are the rationales for these additional measures?
Implementation � Nursing implications ◦ You maintain responsibility for providing emotional support to patients receiving local or regional anesthesia. ◦ After administration of a local anesthetic, protect the patient from injury until full sensory and motor function return. ◦ Nursing implications for managing epidural analgesia are numerous. ◦ Nurses monitor IV sites, lines, and controllers.
Quick Quiz! 2. A patient has just undergone an appendectomy. When discussing with the patient several pain relief interventions, the most appropriate recommendation would be A. Adjunctive therapy. B. Nonopioids. C. NSAIDs. D. PCA pain management.
Chronic Noncancer and Cancer Pain Management � Cancer pain may be chronic or acute. � Breakthrough pain = A transient flare of moderate to severe pain superimposed on continuous or persistent pain. � Transdermal pain patches may be used.
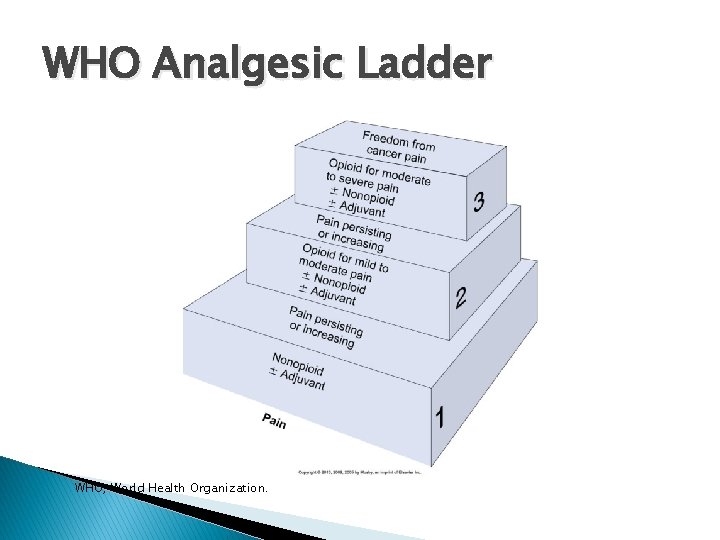
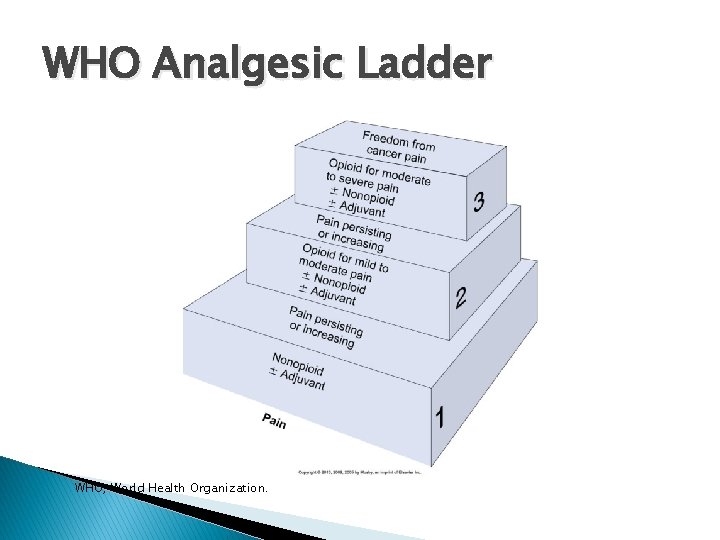
WHO Analgesic Ladder WHO, World Health Organization.
Barriers to Effective Pain Management � � Physical dependence: A state of adaptation that is manifested by a drug class–specific withdrawal syndrome produced by abrupt cessation, rapid dose reduction, decreasing blood level of the drug, and/or administration of an antagonist Addiction: A primary, chronic, neurobiological disease with genetic, psychosocial, and environmental factors influencing its development and manifestations Drug tolerance: A state of adaptation in which exposure to a drug induces changes that result in a diminution of one or more effects of the drug over time Placebos

Restorative and Continuing Care � Pain centers, palliative care, and hospices ◦ Pain centers treat patients on an inpatient or outpatient basis. ◦ The goal of palliative care is to learn how to live life fully with an incurable condition. ◦ Hospices are programs for end-of-life care. ◦ The American Nurses Association (ANA) supports aggressive treatment of pain and suffering even if it hastens a patient’s death.
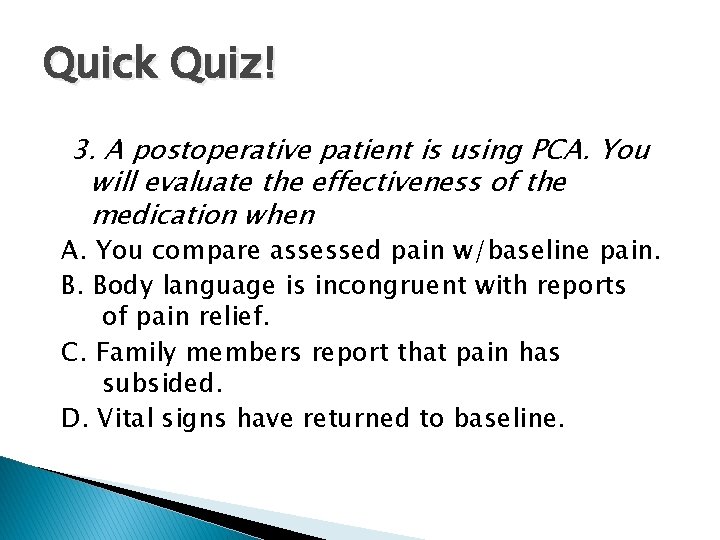
Quick Quiz! 3. A postoperative patient is using PCA. You will evaluate the effectiveness of the medication when A. You compare assessed pain w/baseline pain. B. Body language is incongruent with reports of pain relief. C. Family members report that pain has subsided. D. Vital signs have returned to baseline.
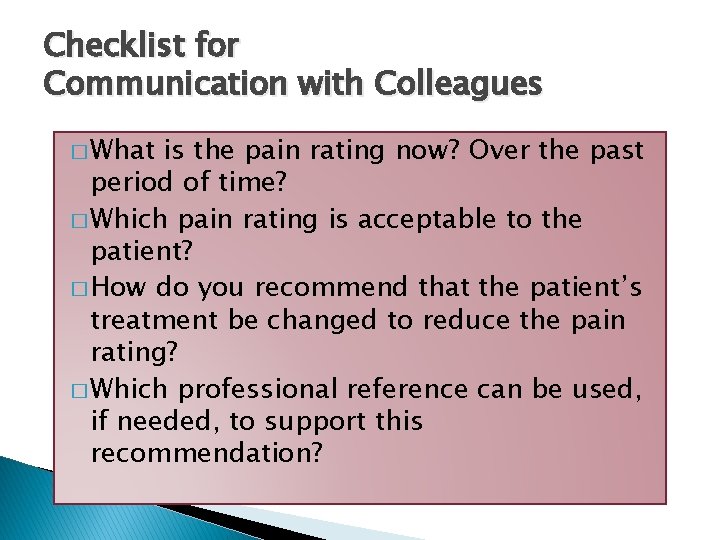
Checklist for Communication with Colleagues � What is the pain rating now? Over the past period of time? � Which pain rating is acceptable to the patient? � How do you recommend that the patient’s treatment be changed to reduce the pain rating? � Which professional reference can be used, if needed, to support this recommendation?

Case Study (cont’d) � When Jim observed Mrs. Ellis’ ability to stand walk from the living room to the kitchen, she was able to ambulate with the walker; her gait was slow but steady. � Mrs. Ellis reports that she has less discomfort from bathing after using warm water over her joints, although dressing is still causing some discomfort when manipulating buttons. � Mrs. Ellis rates her pain at a 2 after taking the analgesic.
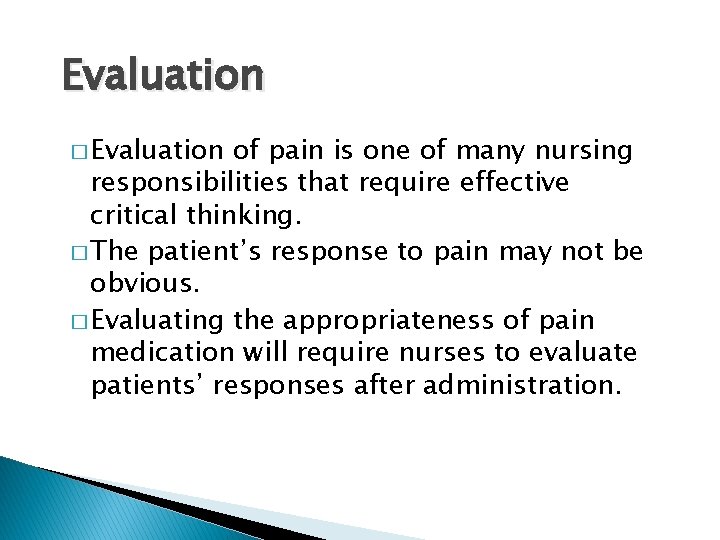
Evaluation � Evaluation of pain is one of many nursing responsibilities that require effective critical thinking. � The patient’s response to pain may not be obvious. � Evaluating the appropriateness of pain medication will require nurses to evaluate patients’ responses after administration.

Safety Guidelines � The patient is the only person who should press the button to administer the pain medication when PCA is used. � Monitor the patient for signs and symptoms of oversedation and respiratory depression.
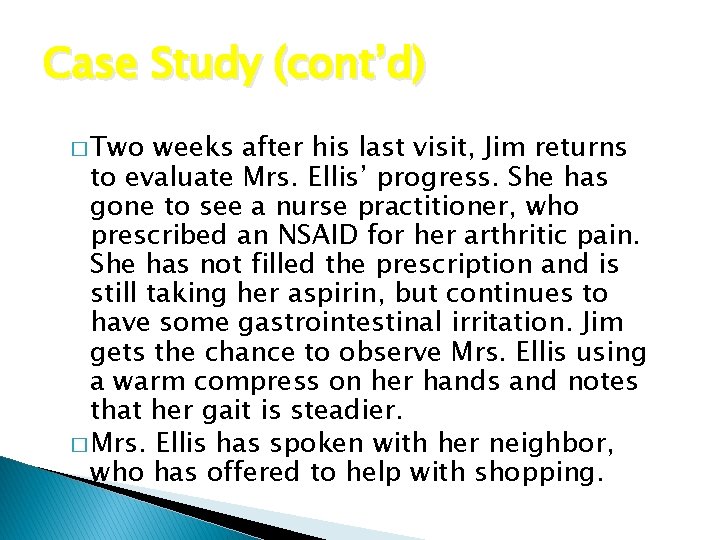
Case Study (cont’d) � Two weeks after his last visit, Jim returns to evaluate Mrs. Ellis’ progress. She has gone to see a nurse practitioner, who prescribed an NSAID for her arthritic pain. She has not filled the prescription and is still taking her aspirin, but continues to have some gastrointestinal irritation. Jim gets the chance to observe Mrs. Ellis using a warm compress on her hands and notes that her gait is steadier. � Mrs. Ellis has spoken with her neighbor, who has offered to help with shopping.