Communication and Optimal Resolution CANDOR Grand Rounds Presentation
![Involving Patients in Post-Event Learning • “[Patients] know our systems probably better than we Involving Patients in Post-Event Learning • “[Patients] know our systems probably better than we](https://slidetodoc.com/presentation_image_h/aa167f7456507663763042300a8855c9/image-26.jpg)





- Slides: 45
Communication and Optimal Resolution (CANDOR): Grand Rounds Presentation Presenter: Timothy B. Mc. Donald, MD, JD
Do Less Harm Video Module 1 2
Presentation Goals • Highlight the gap between optimal response to medical injury and current practices, and identify the reasons for this gap. • Describe the CANDOR (Communication and Optimal Resolution) process and how this toolkit will help organizations improve their response to medical injury. • Discuss next steps in the CANDOR implementation process. Module 1 3
The Problem • Despite major initiatives, patient harm from medical care occurs too often. • Limited progress in improving quality and patient safety is due to our inability to learn from care breakdowns. • Our response to injured patients rarely addresses their needs. Module 1 4
Patient Safety Background • 2010 data from Medicare: • 13. 5% of hospitalized beneficiaries experienced an adverse event. • 1. 5% experienced harm that contributed to death. • 44% of adverse events were preventable. Levinson D, et al. OIG Report, Nov 2010 Module 1 5
Following Harm: Not Always Transparent, Not Always Learning Health Affairs (2012) “Survey Shows That At Least Some Physicians Are Not Always Open or Honest With Patients” Lisa I. Iezzoni, Sowmya R. Rao, Catherine M. Des. Roches, Christine Vogeli, and Eric G. Campbell Module 1 6
Consequences of Failed Response to Medical Injury • • • Compounds suffering of patients and family Heightens distress of clinicians Increases likelihood of litigation Is a lost opportunity for improving quality Degrades institutional culture/climate Reduces public trust in health care Module 1 7
What Do Patients Want? • The truth – What is it? • The facts – What are they? • Emotional first aid – Empathy and compassion – Recognition and validation of emotions – Nonabandonment • Accountability, including apology • Future prevention Module 1 8
Why It is Not Happening: Barriers Perceived and Real • Barriers – Fears • • • Litigation Data Bank Shame, blame Reputation Lack of skills – Lack of process • Benefits – – – – Learning Improving Less litigation Lower costs Integrity Morale Healing Module 1 9
Michelle Malizzo-Ballog Module 1 10
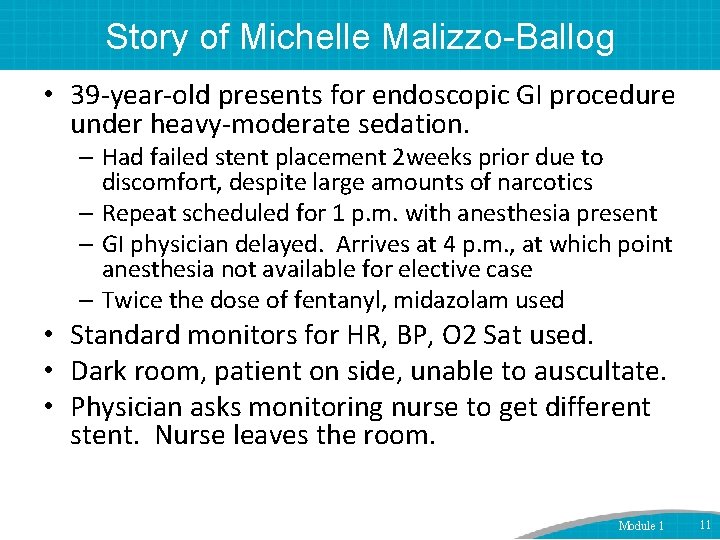
Story of Michelle Malizzo-Ballog • 39 -year-old presents for endoscopic GI procedure under heavy-moderate sedation. – Had failed stent placement 2 weeks prior due to discomfort, despite large amounts of narcotics – Repeat scheduled for 1 p. m. with anesthesia present – GI physician delayed. Arrives at 4 p. m. , at which point anesthesia not available for elective case – Twice the dose of fentanyl, midazolam used • Standard monitors for HR, BP, O 2 Sat used. • Dark room, patient on side, unable to auscultate. • Physician asks monitoring nurse to get different stent. Nurse leaves the room. Module 1 11
…Case Continued • Upon return, patient found to be in respiratory distress. • Code called. • No response to reversal agents. • Team assumes allergic reaction to medication as etiology of arrest. • Michelle resuscitated but brain dead. Module 1 12
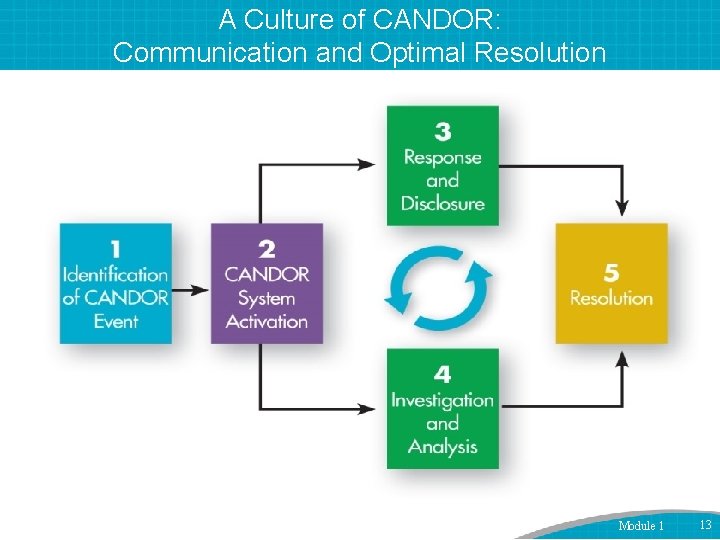
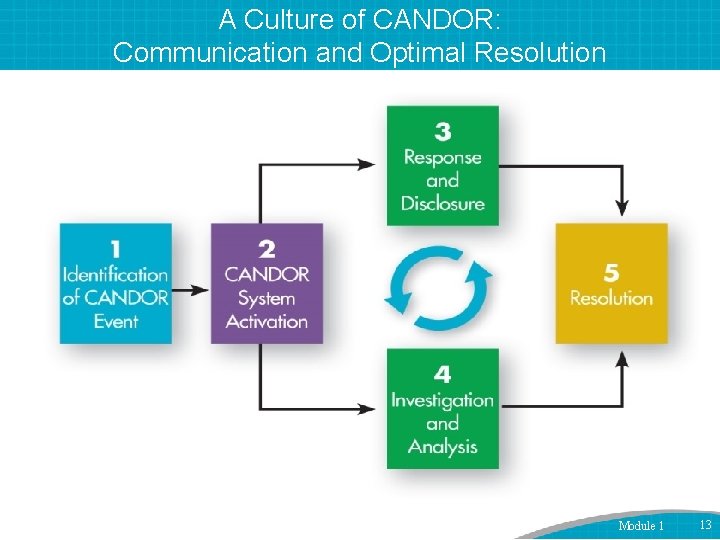
A Culture of CANDOR: Communication and Optimal Resolution Module 1 13
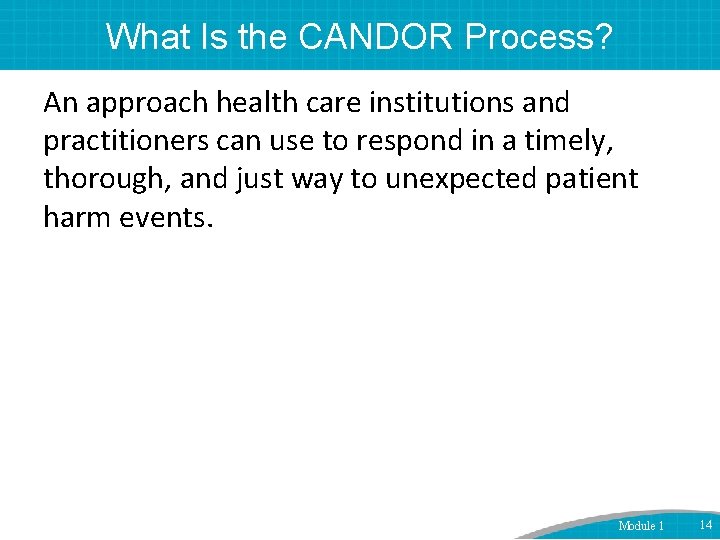
What Is the CANDOR Process? An approach health care institutions and practitioners can use to respond in a timely, thorough, and just way to unexpected patient harm events. Module 1 14
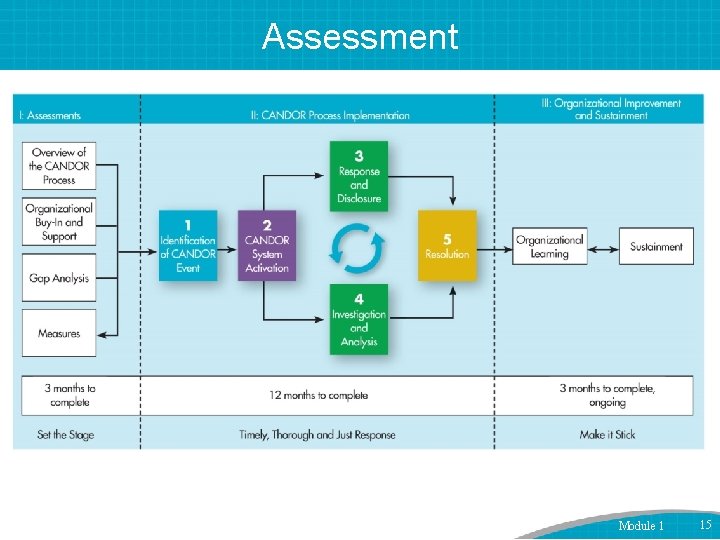
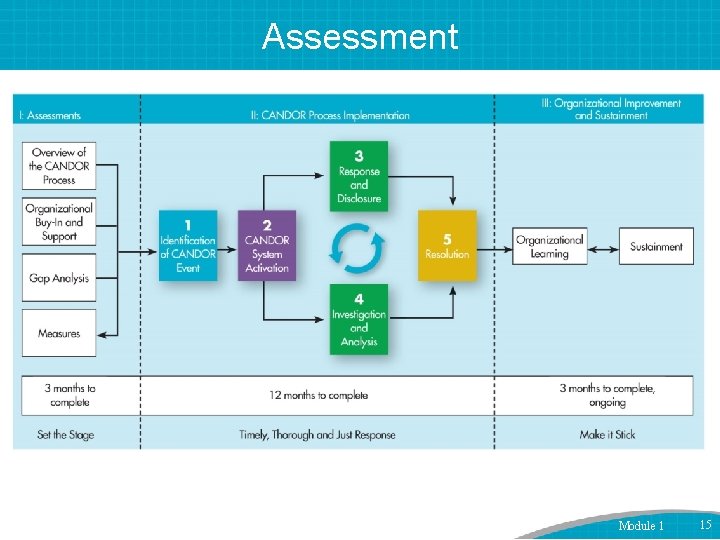
Assessment Module 1 15
Current State Analysis CANDOR represents major culture change for almost all organizations. “We already do this” is often said but rarely accurate. • Gap Analysis: Key informant interviews with various leaders, frontline staff Module 1 16
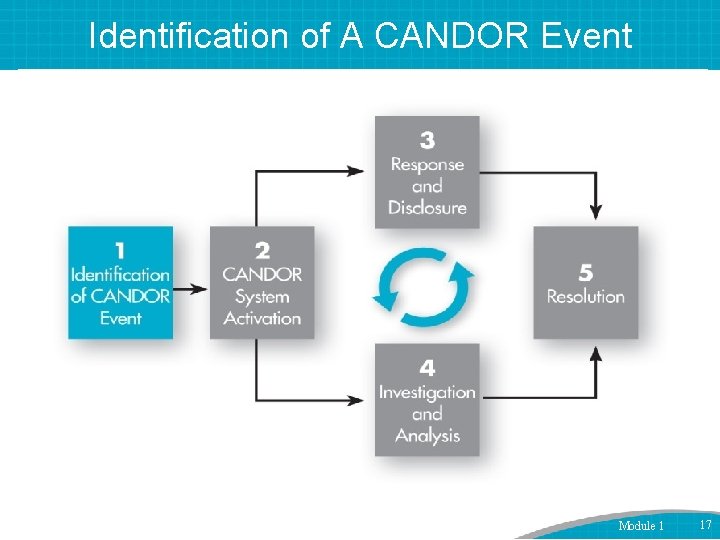
Identification of A CANDOR Event Module 1 17
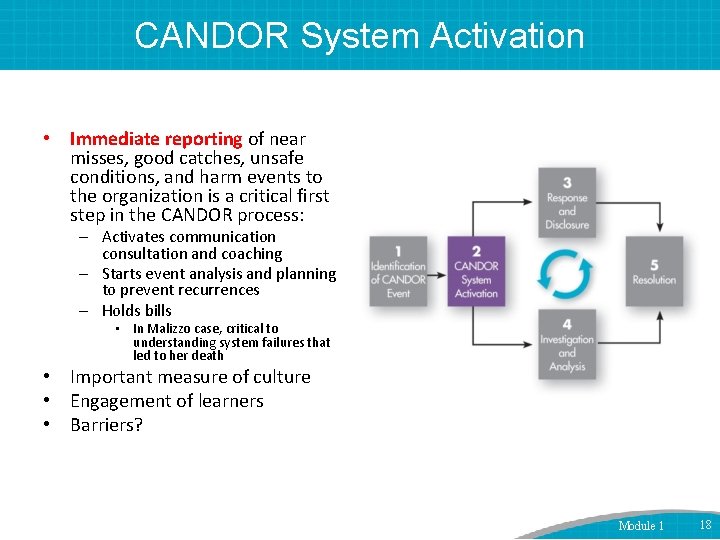
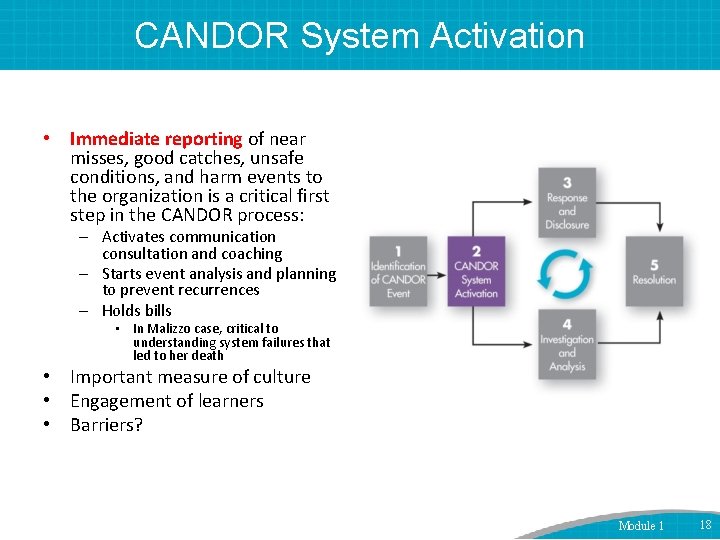
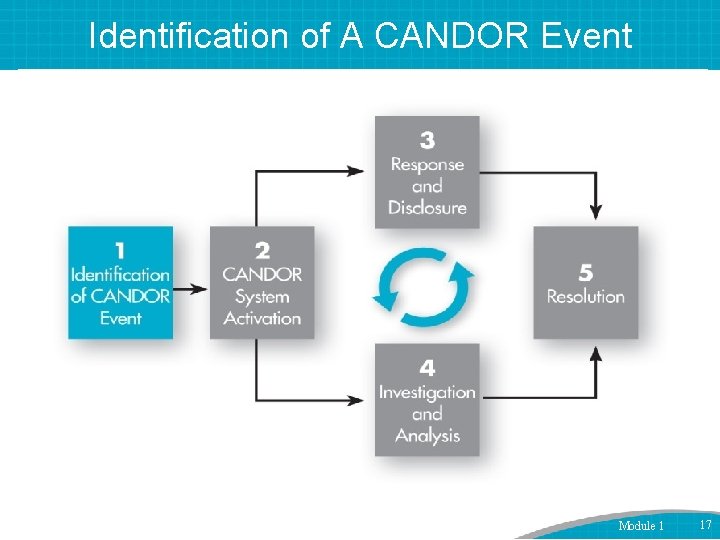
CANDOR System Activation • Immediate reporting of near misses, good catches, unsafe conditions, and harm events to the organization is a critical first step in the CANDOR process: – Activates communication consultation and coaching – Starts event analysis and planning to prevent recurrences – Holds bills • In Malizzo case, critical to understanding system failures that led to her death • Important measure of culture • Engagement of learners • Barriers? Module 1 18
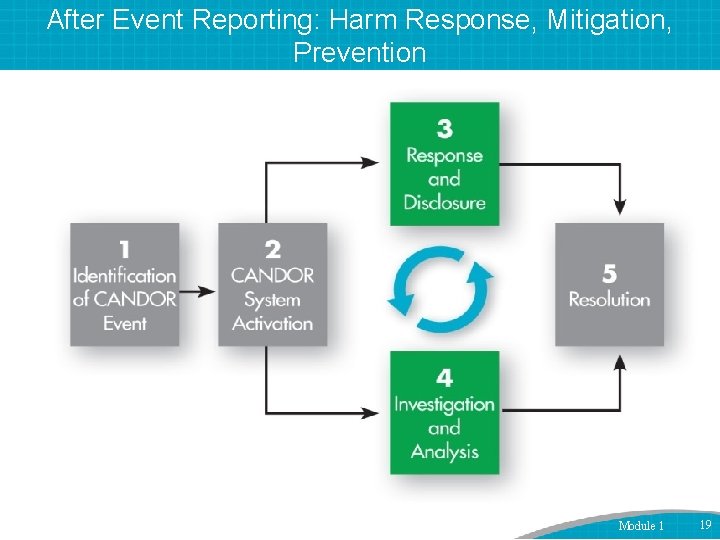
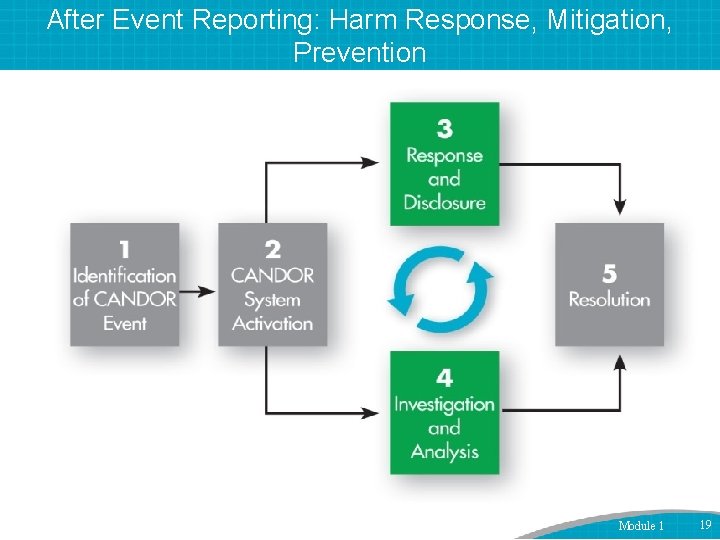
After Event Reporting: Harm Response, Mitigation, Prevention Module 1 19
Investigation: Best Practices Protected Interdisciplinary, human factors expertise Timely Just Comprehensive Leads to broad performance, process improvements • Involves rapid feedback and dissemination • • • Module 1 20
Who Is to Blame in Malizzo Case? • Traditional approach – Nurse who left patient unmonitored – Physician who ordered too much fentanyl, midazolam – GI attending who decided to proceed with case despite lack of anesthesia coverage – Others? Module 1 21
Just Culture • Seeks middle ground between historical “shame/blame-bad apple” approach and “blame-free” model after medical injury. • Distinguishes between human error (console), at-risk behavior (coach), reckless behavior (punish). • Why do we still focus on blame? Module 1 22
Safety Attitudes “The single greatest impediment to error prevention in the medical industry is that we punish people for making mistakes. ” -- Lucian Leape, MD, Professor, Harvard School of Public Health Testimony to Congress “Fallibility is part of the human condition. We cannot change the human condition. But we can change the conditions under which people work. ” --James Reason, Ph. D, Professor, The University of Manchester Module 1 23
What Is a Systems Approach? Human error cannot be eliminated. – Futile goal. – Misdirects resources/focus. – Causes culture of blame and secrecy. • “Name, blame, shame, and train” mentality. • Promotes secrecy, collusion, repression. It is about reducing HARM. Ask what is responsible…not who is responsible. – Then, focus on solutions. Module 1 24
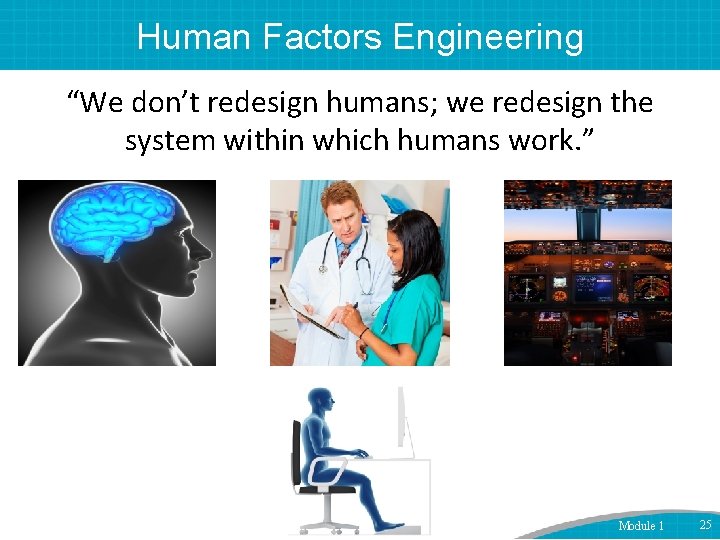
Human Factors Engineering “We don’t redesign humans; we redesign the system within which humans work. ” Module 1 25
![Involving Patients in PostEvent Learning Patients know our systems probably better than we Involving Patients in Post-Event Learning • “[Patients] know our systems probably better than we](https://slidetodoc.com/presentation_image_h/aa167f7456507663763042300a8855c9/image-26.jpg)
Involving Patients in Post-Event Learning • “[Patients] know our systems probably better than we know our systems because they have been through them so much. ” • “…The whole investigation process is incomplete when you don’t involve [patients]. ” • “Patients and families could offer a unique perspective on norms and quality of care that would otherwise be lost. ” Etchegaray et al Health Aff 2014 Module 1 26
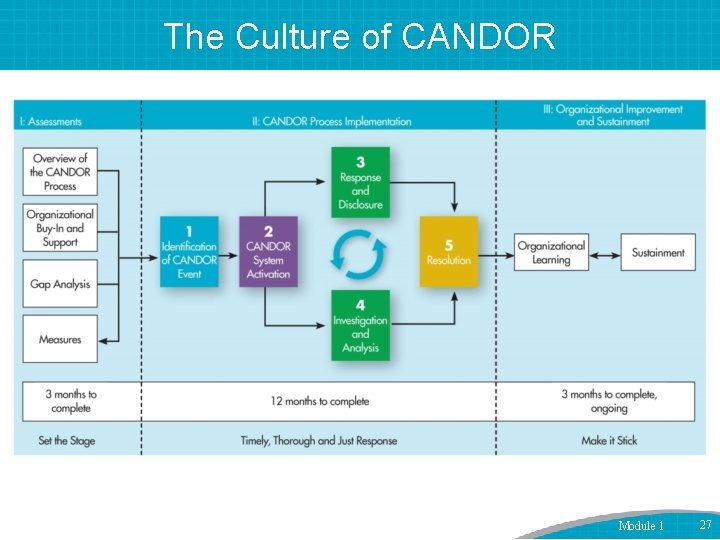
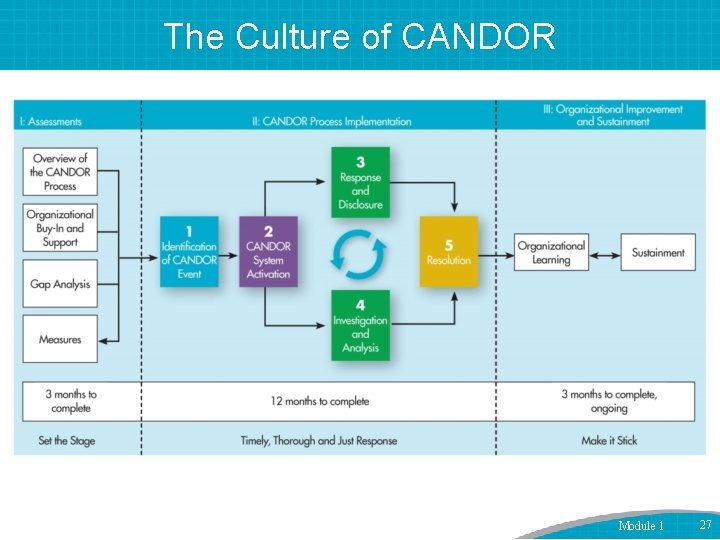
The Culture of CANDOR Module 1 27
Post-Event Reporting: Communication • Patient • Family • Caregivers Module 1 28
Communication After a Harm Event • Not everyone is a good communicator. • Identify good communicators. • Understand conversations can be emotionally difficult. • Have backup resources. • Use just-in-time training and “coaching. ” Module 1 29

Inappropriate Disclosure to A Patient Module 1 30

Strategies for Disclosure: Guidelines and Framework Step 1: Get help – Remember disclosure is a process not an event. – Explain what happened (facts as known). – Describe implications for patient, treatment plan. – Offer genuine expression of regret/apology. – Plan for investigation/analysis. – Discuss how recurrences will be prevented. – Establish contact, supports, followup. – Organizational leadership is key. Module 1 31
Additional Tips • Be yourself—authenticity matters. • Anticipate potential reactions and questions. • Avoid blame. – “The lab always does this. ” – “If only radiology had called me…” – Blaming other providers, “system. ” • Weigh pros and cons of who goes in the room. • Take advantage of coaching and consultation. • Involve trainees, team members when appropriate. • Follow organizational processes. Module 1 32

How Are We Doing? • One-third to two-thirds of errors are not disclosed. – Blendon et al. , NEJM 2002; Gallagher, JAMA 2009 • Even when disclosure happens, it often does not meet patient expectations. – Gallagher et al. , JAMA 2003; Kaldijian et al. , JGIM 2007; Gallagher, JAMA 2009 • Clinicians often lack adequate disclosure training. – Wu et al. , JAMA 1991; White et al. , Acad Med 2008; Bell et al. , Acad Med 2010; Liao et al. , Acad Med 2014 Module 1 33
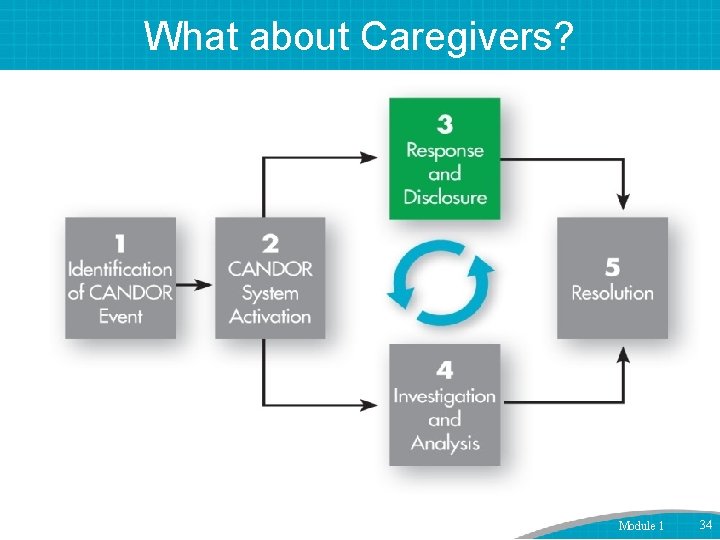
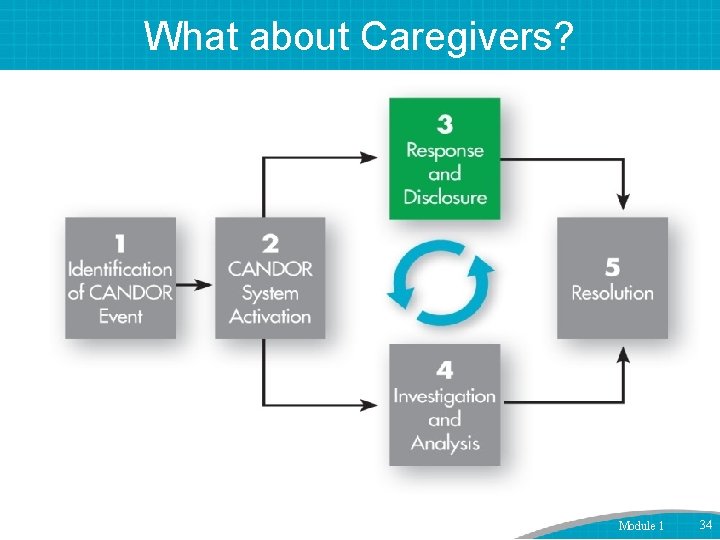
What about Caregivers? Module 1 34
Care for the Caregiver • Involvement in a medical error increases: – Burnout. – Likelihood of involvement in future errors. – Risk of depression. – Risk of suicide. – Leaving the practice of medicine. Module 1 35
National Quality Forum Safe Practice #8 • Care for the Caregiver: – – – – Available to all employees involved. Timely and systematic. Just treatment. Respectful. Compassionate. Supportive medical care. Participation in event investigation, risk identification, and mitigation activities to prevent future events. • Supporting providers helps them care for their patients. Module 1 36
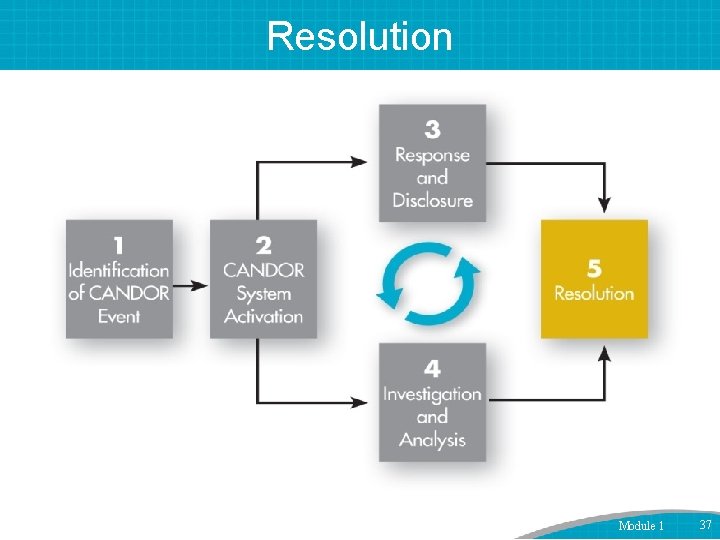
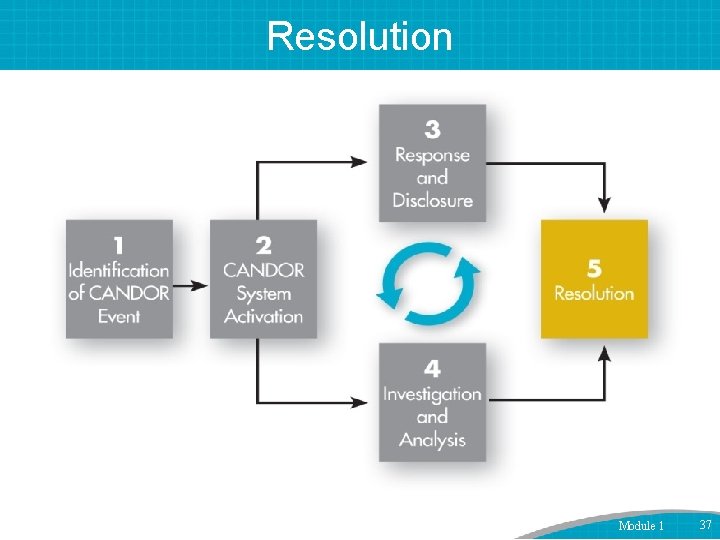
Resolution Module 1 37
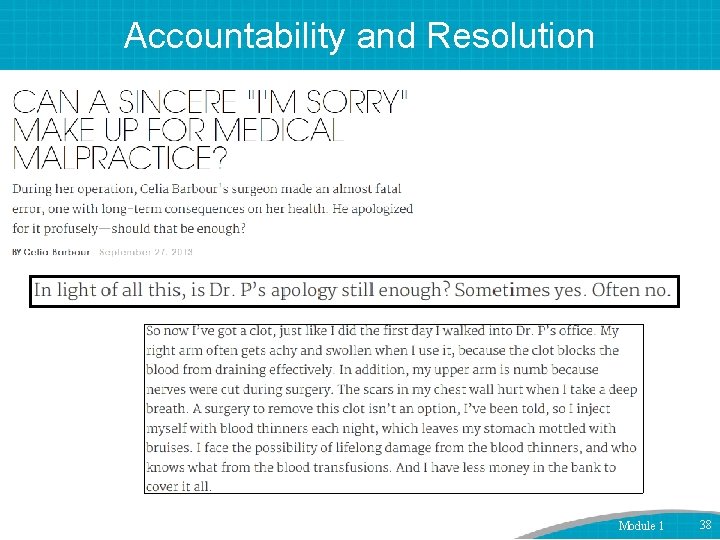
Accountability and Resolution Module 1 38
Accountability: More Than Words • Interview study with cancer patients who thought something serious and harmful went wrong in their care. • Patients seek action following the disclosure that are congruent with the words. – “If you’re just going to apologize and you’re not going to fix anything, that’s insulting to my intelligence. ” – “There’s got to be accountability. I don’t want to hear ‘I’m sorry. ’ ‘I’m sorry’ is nothing. I want to hear what steps have been taken to correct the problem. ” – “Don’t tell me you were sorry that the problem occurred. That just puts a band aid on something…. I want to see results. ” Module 1 39
What Are Resolution Conversations? • Discussions with patients/family after the initial communications about the adverse event – Often take place after event analysis is completed. – Many different forms, by different people, occur over time: • • Explanation of event’s cause and prevention. Responsibility/blame. Nonfinancial, financial resolution. Other followup. • Emotional tone differs from initial disclosure. • CANDOR will train risk managers, organization leaders in approaching these difficult discussions. Module 1 40
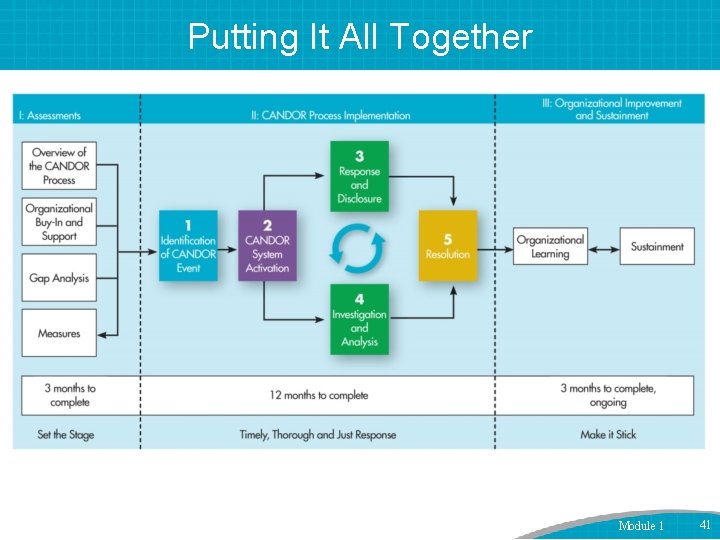
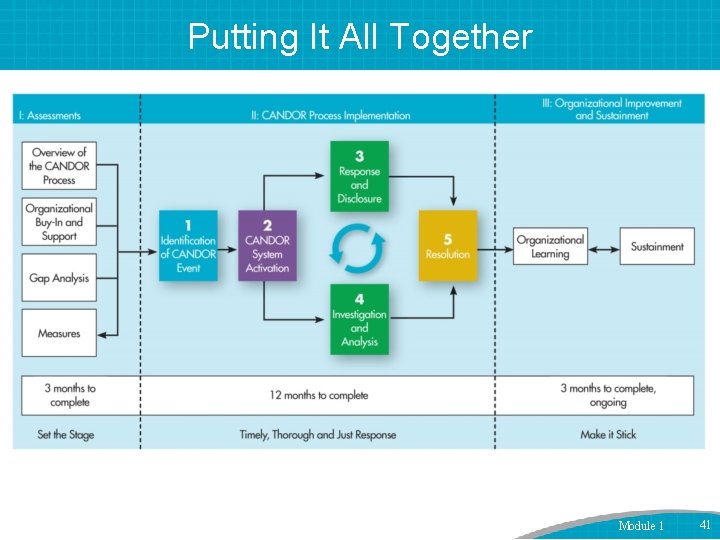
Putting It All Together Module 1 41

Example Case Module 1 42
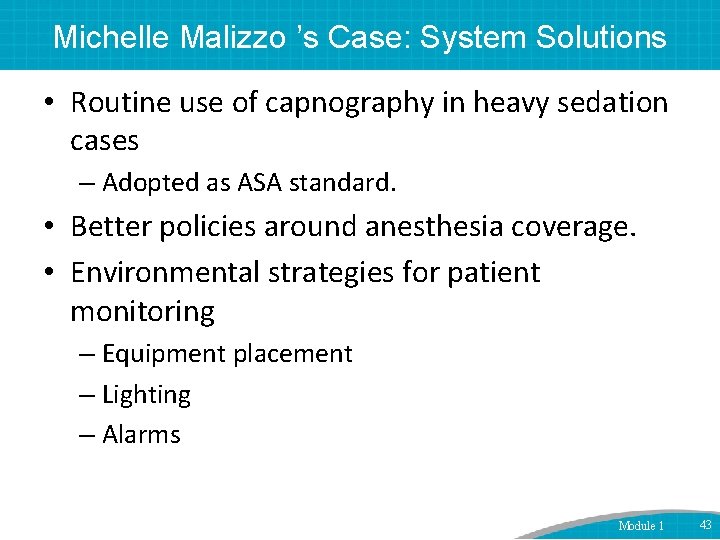
Michelle Malizzo ’s Case: System Solutions • Routine use of capnography in heavy sedation cases – Adopted as ASA standard. • Better policies around anesthesia coverage. • Environmental strategies for patient monitoring – Equipment placement – Lighting – Alarms Module 1 43
Next Steps • • • Organizational assessment Communication training Event analysis tools and training Data capture, analysis, feedback Ongoing support Module 1 44

Questions? Module 1 45