Drugs used to treat hypertension prof Jn Moji

- Slides: 69
Drugs used to treat hypertension prof. Ján Mojžiš Department of Pharmacology, Medical Faculty, P. J. Šafarik University Košice 1
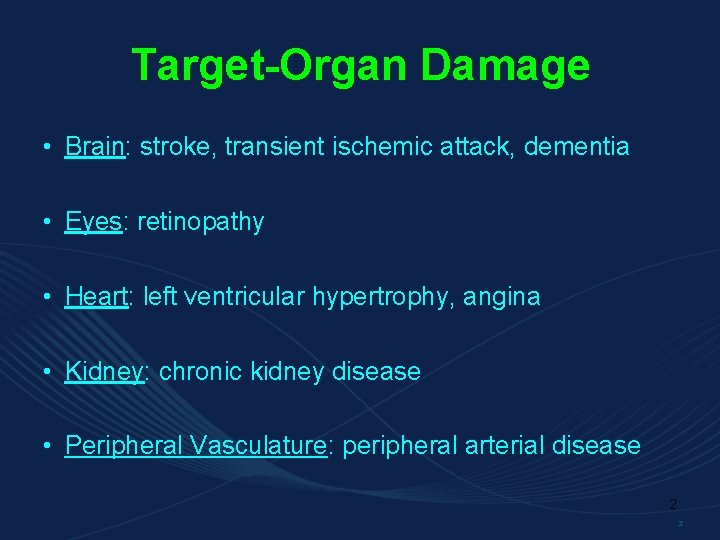
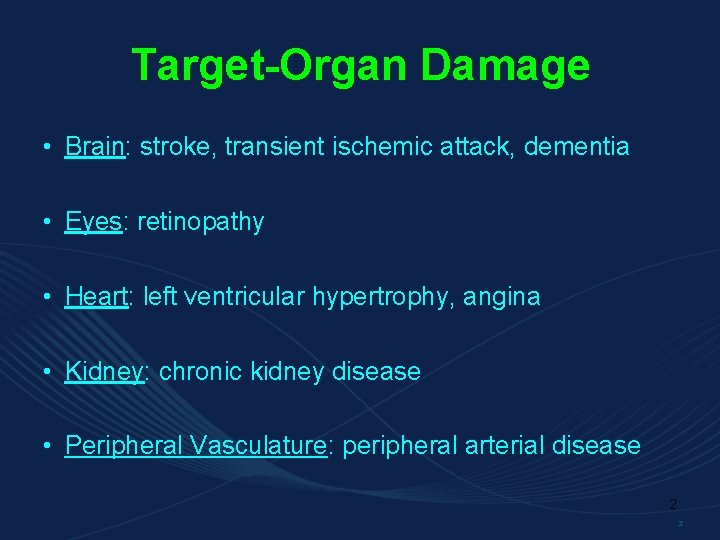
Target-Organ Damage • Brain: stroke, transient ischemic attack, dementia • Eyes: retinopathy • Heart: left ventricular hypertrophy, angina • Kidney: chronic kidney disease • Peripheral Vasculature: peripheral arterial disease 2 2
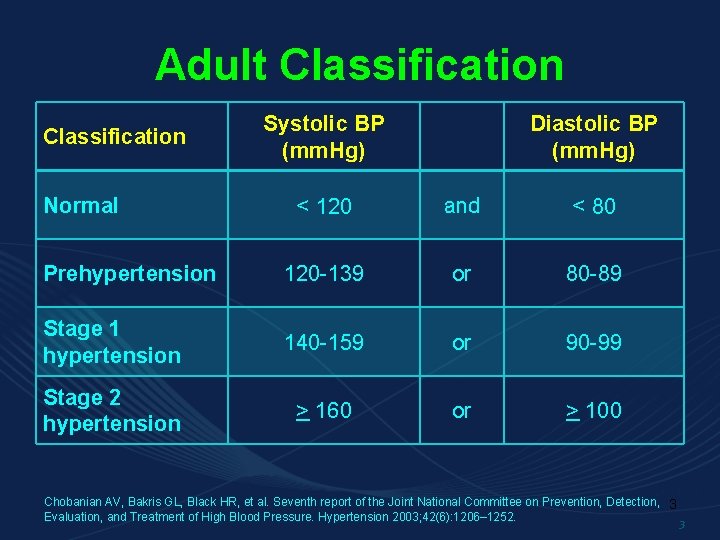
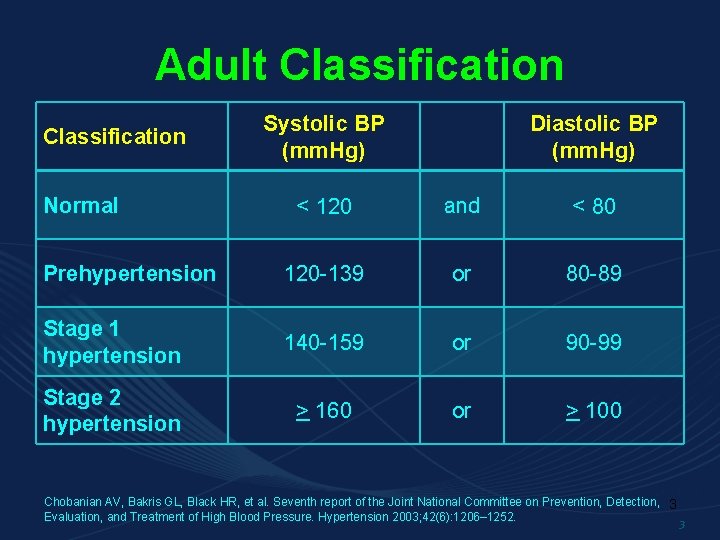
Adult Classification Systolic BP (mm. Hg) Diastolic BP (mm. Hg) < 120 and < 80 Prehypertension 120 -139 or 80 -89 Stage 1 hypertension 140 -159 or 90 -99 Stage 2 hypertension > 160 or > 100 Normal Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, 3 Evaluation, and Treatment of High Blood Pressure. Hypertension 2003; 42(6): 1206– 1252. 3
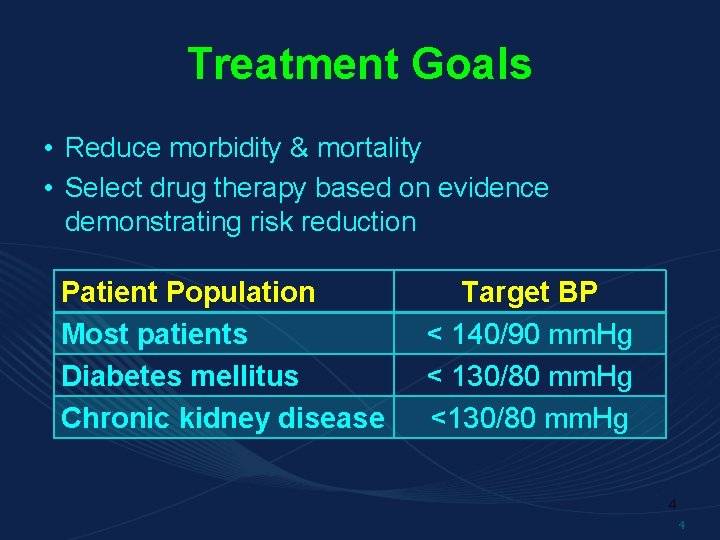
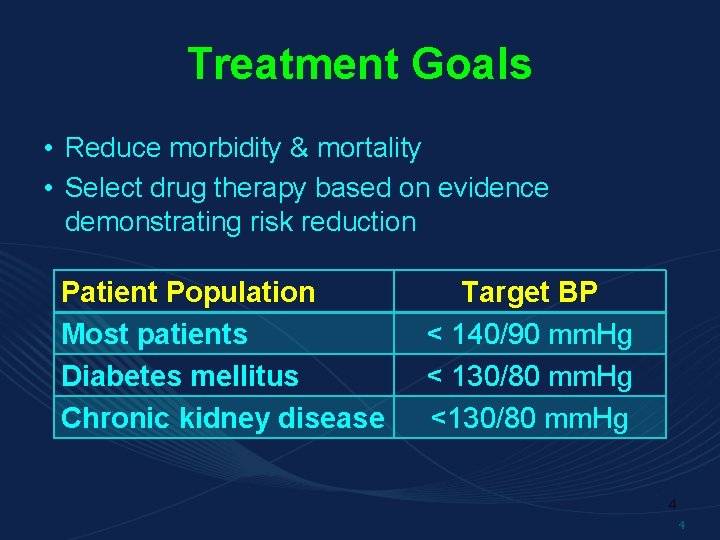
Treatment Goals • Reduce morbidity & mortality • Select drug therapy based on evidence demonstrating risk reduction Patient Population Most patients Diabetes mellitus Chronic kidney disease Target BP < 140/90 mm. Hg < 130/80 mm. Hg <130/80 mm. Hg 4 4
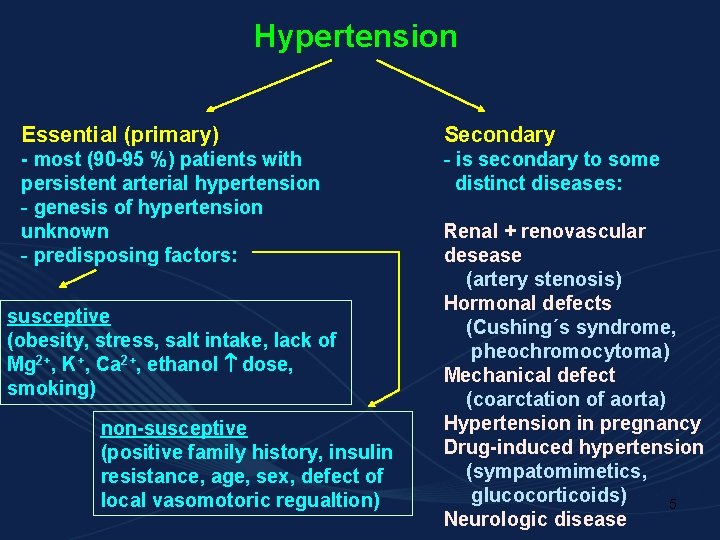
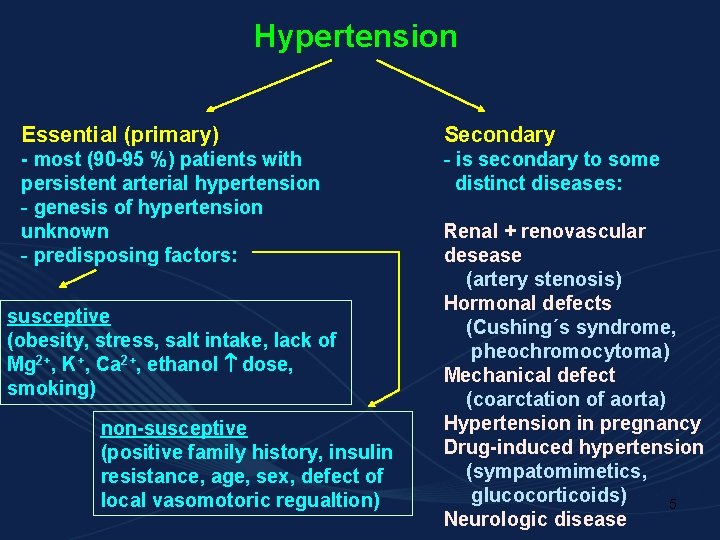
Hypertension Essential (primary) Secondary - most (90 -95 %) patients with persistent arterial hypertension - genesis of hypertension unknown - predisposing factors: - is secondary to some distinct diseases: susceptive (obesity, stress, salt intake, lack of Mg 2+, K+, Ca 2+, ethanol dose, smoking) non-susceptive (positive family history, insulin resistance, age, sex, defect of local vasomotoric regualtion) Renal + renovascular desease (artery stenosis) Hormonal defects (Cushing´s syndrome, pheochromocytoma) Mechanical defect (coarctation of aorta) Hypertension in pregnancy Drug-induced hypertension (sympatomimetics, glucocorticoids) 5 Neurologic disease
Treatment of hyperternsion A: Non-pharmacological Changes of lifestyl 6
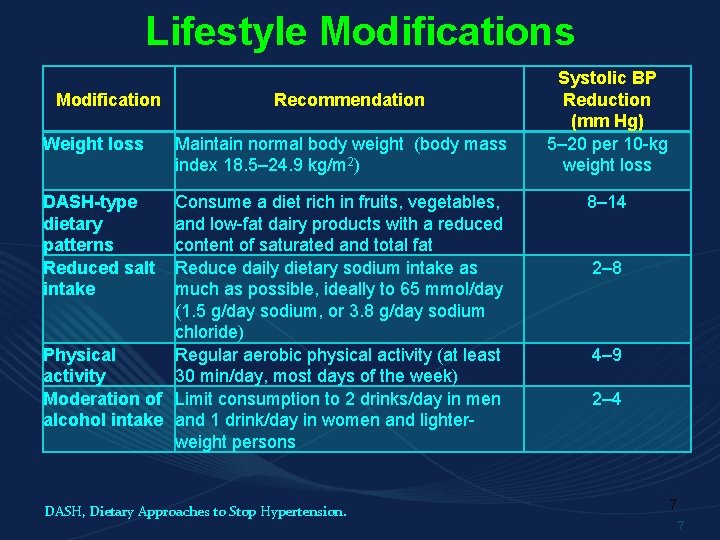
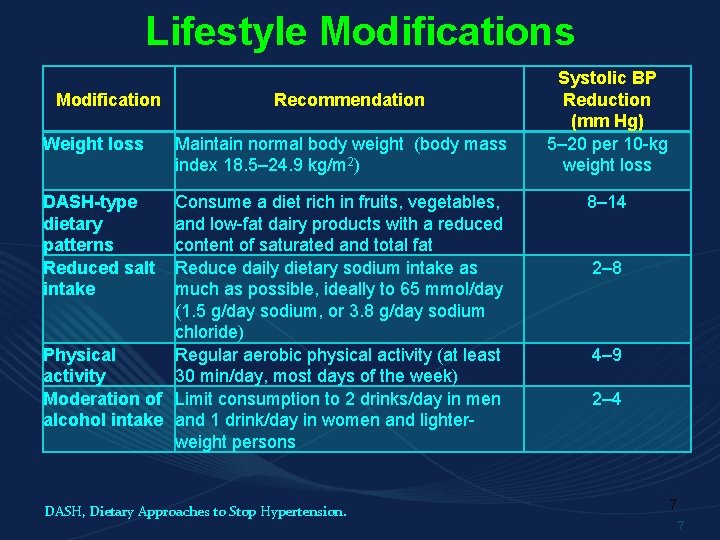
Lifestyle Modifications Modification Weight loss Recommendation Maintain normal body weight (body mass index 18. 5– 24. 9 kg/m 2) DASH-type dietary patterns Reduced salt intake Consume a diet rich in fruits, vegetables, and low-fat dairy products with a reduced content of saturated and total fat Reduce daily dietary sodium intake as much as possible, ideally to 65 mmol/day (1. 5 g/day sodium, or 3. 8 g/day sodium chloride) Physical Regular aerobic physical activity (at least activity 30 min/day, most days of the week) Moderation of Limit consumption to 2 drinks/day in men alcohol intake and 1 drink/day in women and lighterweight persons DASH, Dietary Approaches to Stop Hypertension. Systolic BP Reduction (mm Hg) 5– 20 per 10 -kg weight loss 8– 14 2– 8 4– 9 2– 4 7 7
Standard drink A standard drink is about 142 ml or 5 oz of wine (12% alcohol). 341 m. L or 12 oz of beer (5% alcohol) 43 m. L or 1. 5 oz of spirits (40% alcohol). 8
9
B. Pharmacological 1. Diuretics 2. -blockers 3. ACE-I, blockers of AT 1 receptor 4. Calcium channel blockers 5. Other 10
Diuretics • Thiazide – chlorthalidone, hydrochlorothiazide (HCTZ), indapamide, metipamid, clopamid • Loop – bumetanide, furosemide, torsemide • Potassium-sparing – spironolactone, amiloride 11 11
DIURETICS – cont. - drugs of first choice for treating patients with mild hypertension often combined with another drug in treatment of more severe hypertension THIAZIDES - preferable (to loop diuretics) for the treatment of uncomplicated hypertension - given by mouth as a single morning dose (to avoid nocturnal diuresis) - begin to act within 1 -2 hours and work for 12 -24 hours - treatment should be started using a low dose 12
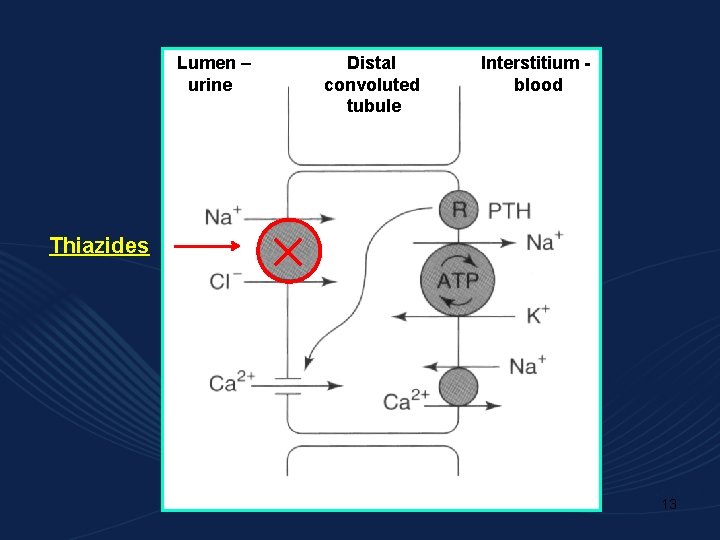
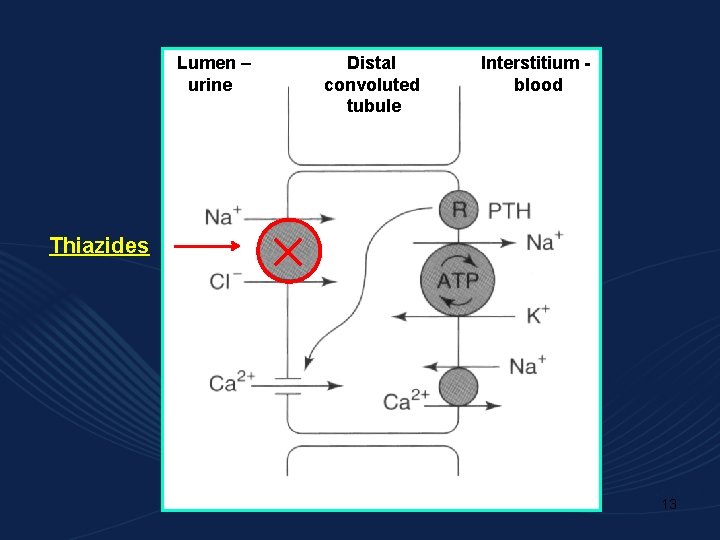
Lumen – urine Distal convoluted tubule Interstitium blood Thiazides 13
Mechanism of action: lower blood pressure by reduction of blood volume and by direct vascular effect - inhibition of sodium chloride transport in the early segment of the distal convoluted tubule natriuresis, decrease in preload and cardiac output - renal effect - slow decrease of total peripheral resistance (raised initially) during chronic treatment, suggesting an action on resistance vessels - extrarenal effects 14
Adverse effects - metabolic and electrolyte changes hyponatremia hypokalemia (combine with potassium-sparing diuretics) hypomagnesemia hyperuricemia (most diuretics reduce urate clearance) hyperglycemia hypercalcemia (thiazides reduce urinary calcium ion clearance) - idiosyncratic reactions (rashes - may be photosensitiv, purpura) - lithium toxicity with concurrent administration 15
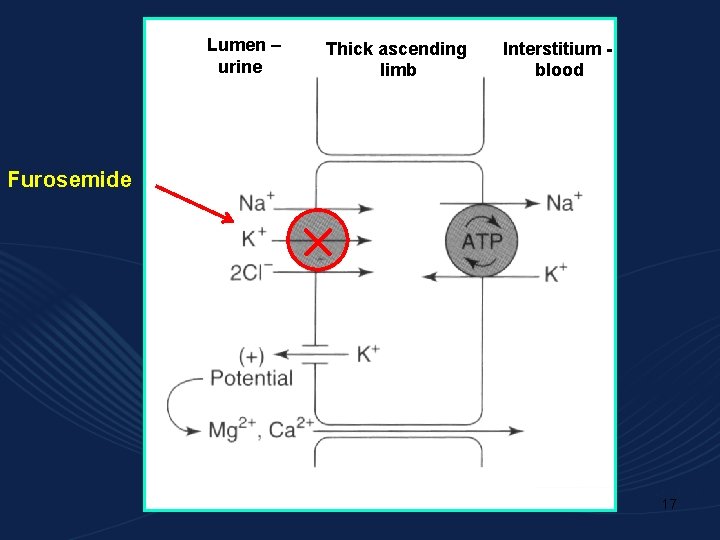
LOOP DIURETICS - useful in hypertensive patients with moderate or severe renal impairment, or in patients with hypertensive heart failure - relatively short-acting (diuresis occurs over the 4 hours following a dose) used in hypertension if response to thiazides is inadequate Mechanism of action: - they inhibit the co-transport of Na+, K+ and 2 Cl- of Ca 2+ and Mg 2+ excretion - they have useful pulmonary vasodilating effects (unknown mechanism) 16
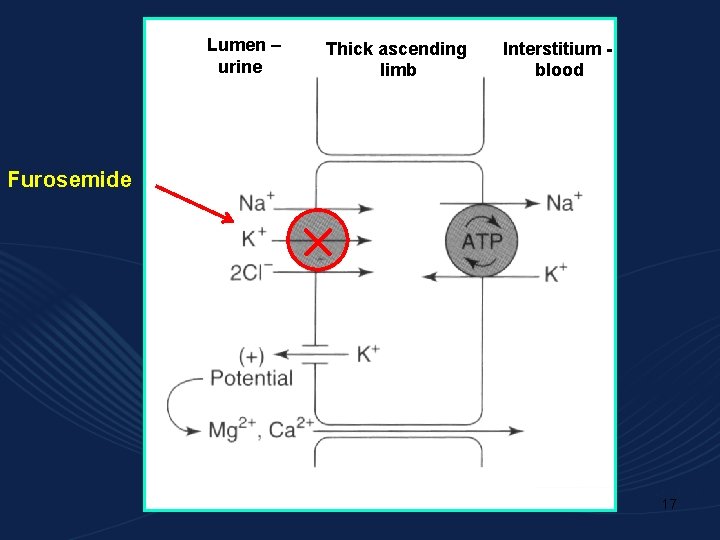
Lumen – urine Thick ascending limb Interstitium blood Furosemide 17
Adverse effects - hypokalemic metabolic alkalosis ( excretion of K+) - ototoxicity (dose dependent, reversible) - hypomagnesemia - hyperuricemia (block of uric acid tubular secretion) - sulfonamide allergy - risk of dehydration (> 4 L urine/ 24 h) Important drug interaction may occurs if loop diuretic is given with Li+ (antimanic drug). Decrease of Na+ reabsorption can lead to increase of Li+ reabsorption toxicity. 18
Potassium-sparing diuretics act in the distal tubule and the collecting tubule to inhibit Na+ reabsorption, K+ secretion, H+ secretion they are often used with a thiazide diuretic to spare potassium Spironolactone - it is an aldosterone antagonist - is useful in patients with high level of aldosterone - it has low diuretic efficacy its advantage is sparing of potassium - it is often used with loop or thiazide diuretics 19
Potassium-sparing diuretics – cont. Amiloride - it has similar potassium-spring action to that of spironolactone - its efect is independent on aldosterone concentration - it si also frequently used with other diuretics Adverse effects: may cause hyperkalemia especially in combination with ACE inhibitor, angiotensinreceptor blocker or potassium supplements 20
-adrenoreceptor antagonists 21
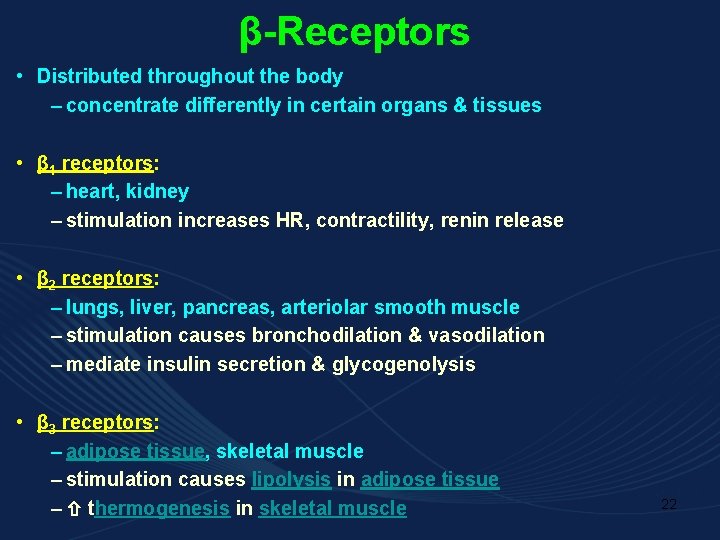
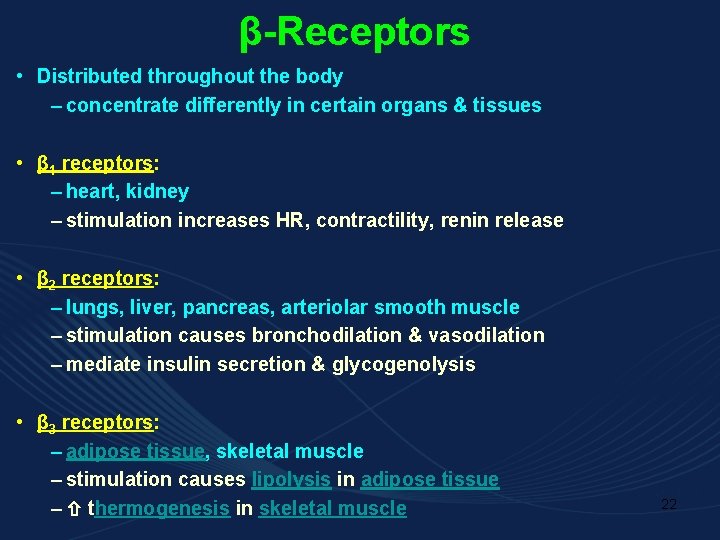
β-Receptors • Distributed throughout the body – concentrate differently in certain organs & tissues • β 1 receptors: – heart, kidney – stimulation increases HR, contractility, renin release • β 2 receptors: – lungs, liver, pancreas, arteriolar smooth muscle – stimulation causes bronchodilation & vasodilation – mediate insulin secretion & glycogenolysis • β 3 receptors: – adipose tissue, skeletal muscle – stimulation causes lipolysis in adipose tissue – thermogenesis in skeletal muscle 22
Mechanism of action - Negative chronotropic & inotropic cardiac effects - Inhibit renin release (weak association with antihypertensive effect) - Membrane-stabilizing action on cardiac cells at high enough doses (? ) Possible mechanisms include: -adrenoceptors located on sympathetic nerve terminals can promote noradrenaline release, and this is prevented by receptor antagonists 23
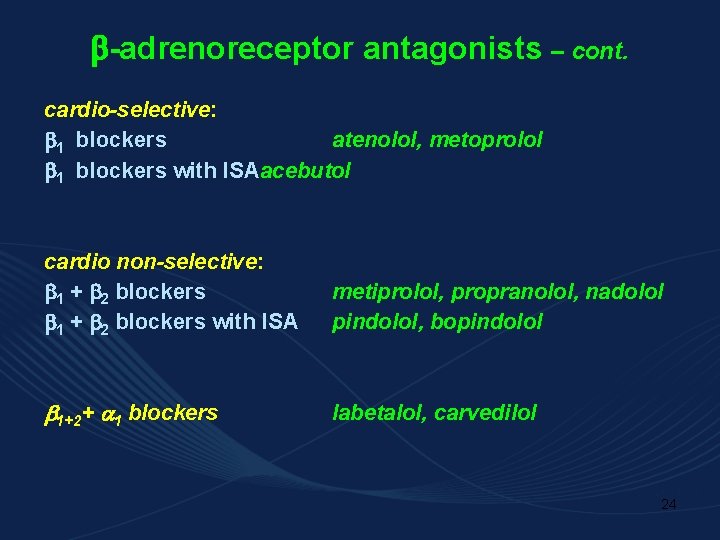
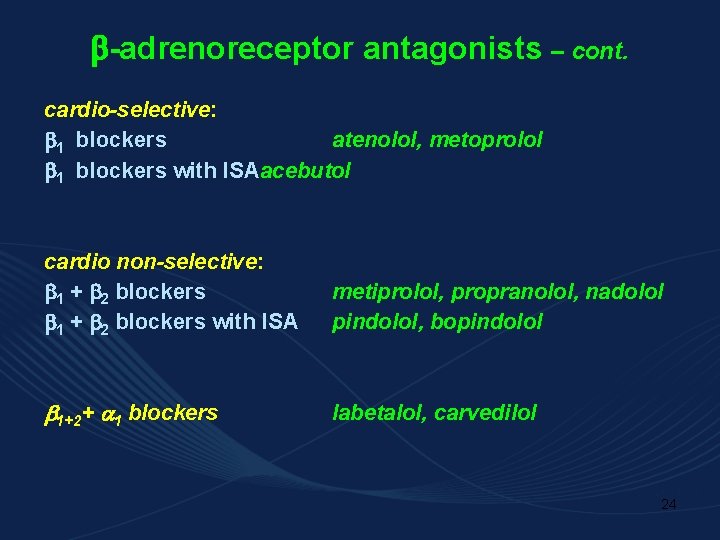
-adrenoreceptor antagonists – cont. cardio-selective: 1 blockers atenolol, metoprolol 1 blockers with ISAacebutol cardio non-selective: 1 + 2 blockers with ISA metiprolol, propranolol, nadolol pindolol, bopindolol 1+2+ 1 blockers labetalol, carvedilol 24
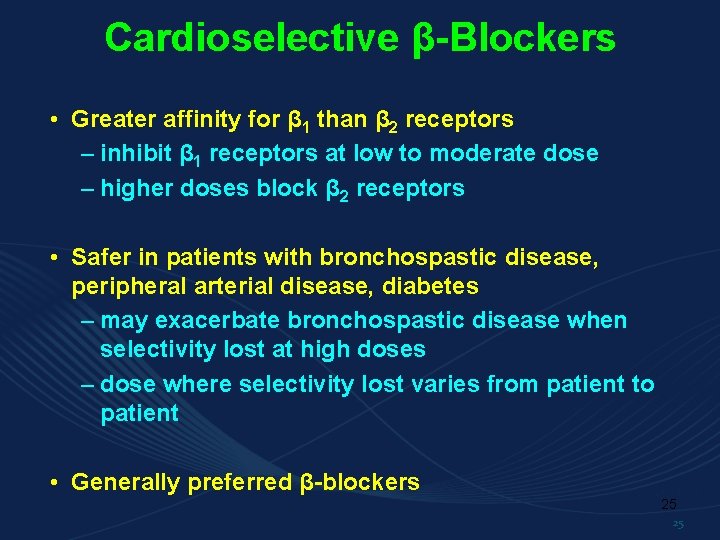
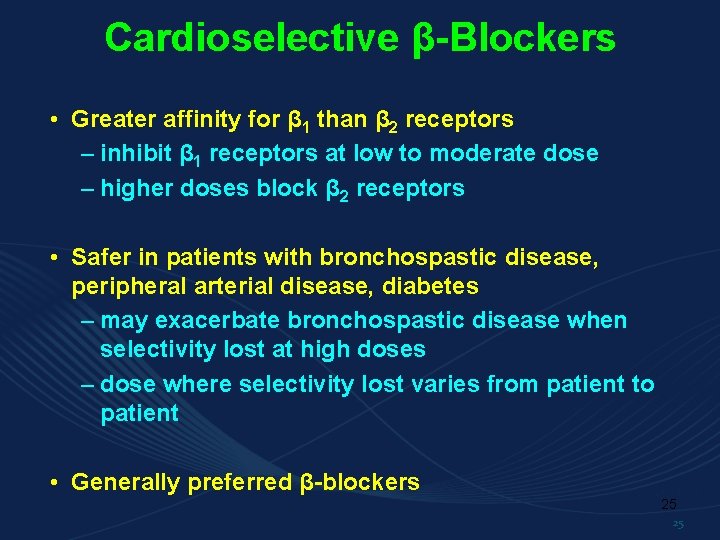
Cardioselective β-Blockers • Greater affinity for β 1 than β 2 receptors – inhibit β 1 receptors at low to moderate dose – higher doses block β 2 receptors • Safer in patients with bronchospastic disease, peripheral arterial disease, diabetes – may exacerbate bronchospastic disease when selectivity lost at high doses – dose where selectivity lost varies from patient to patient • Generally preferred β-blockers 25 25
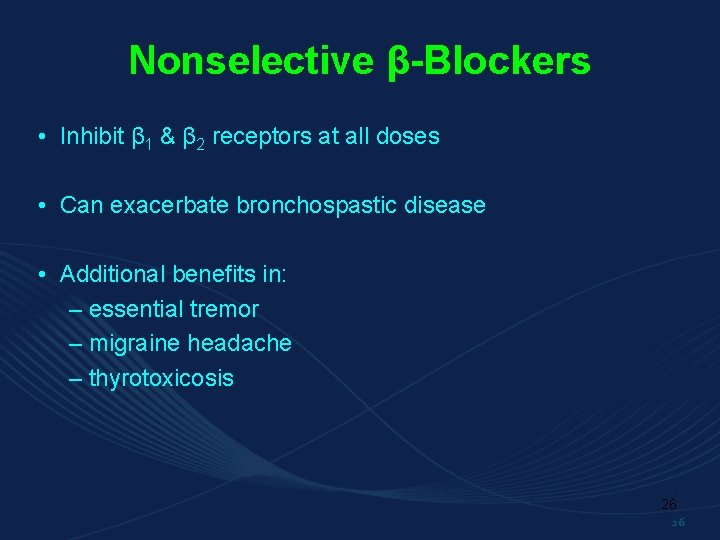
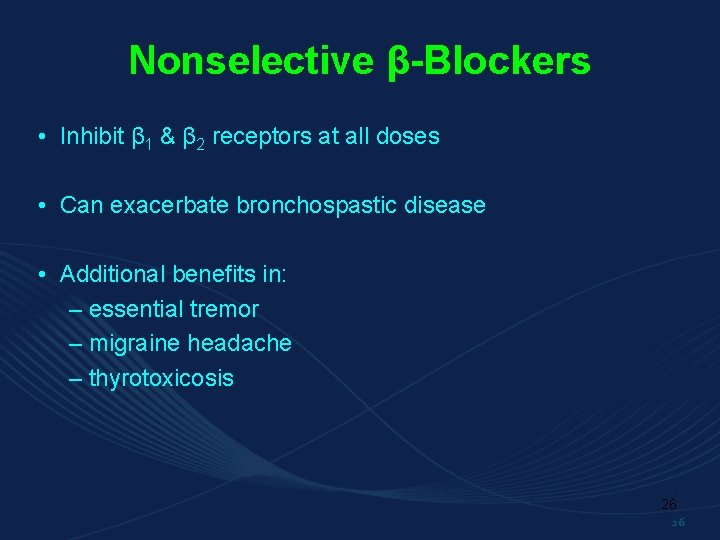
Nonselective β-Blockers • Inhibit β 1 & β 2 receptors at all doses • Can exacerbate bronchospastic disease • Additional benefits in: – essential tremor – migraine headache – thyrotoxicosis 26 26
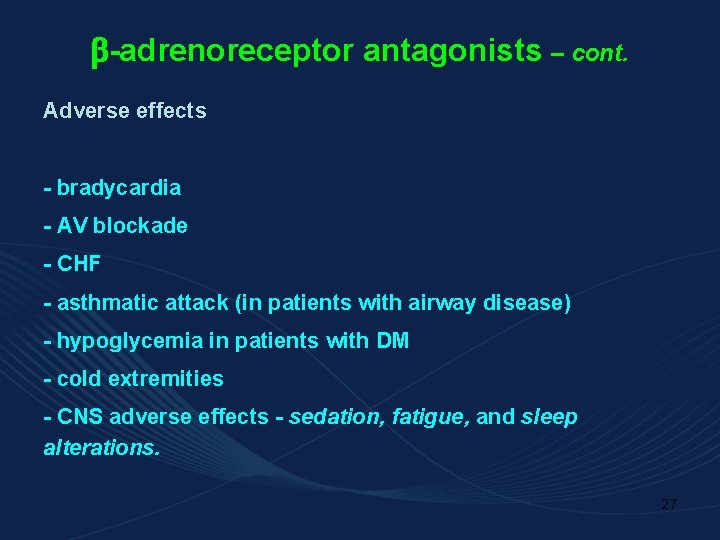
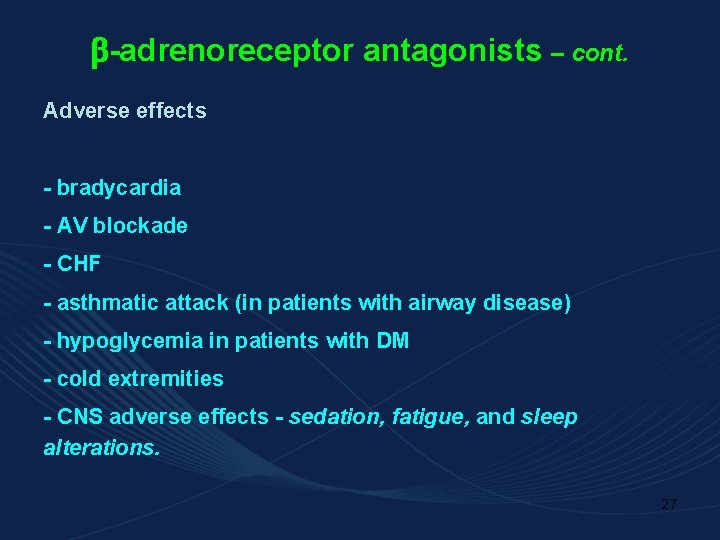
-adrenoreceptor antagonists – cont. Adverse effects - bradycardia - AV blockade - CHF - asthmatic attack (in patients with airway disease) - hypoglycemia in patients with DM - cold extremities - CNS adverse effects - sedation, fatigue, and sleep alterations. 27
Angiotensin-converting enzyme inhibitors (ACE-I) 28
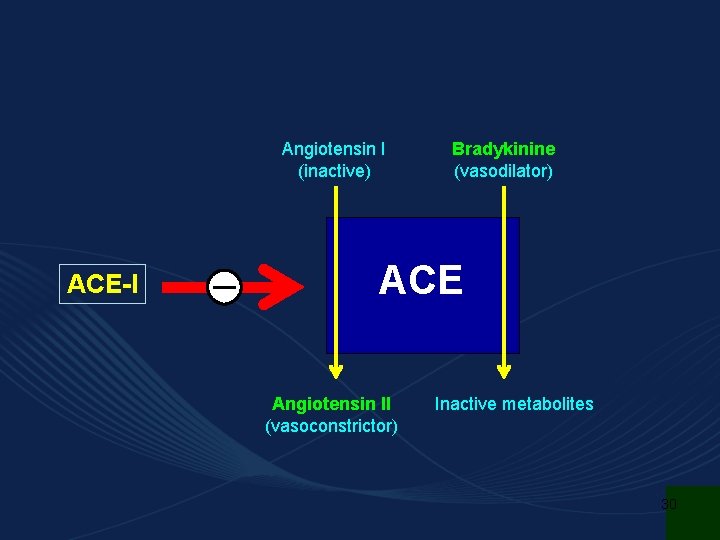
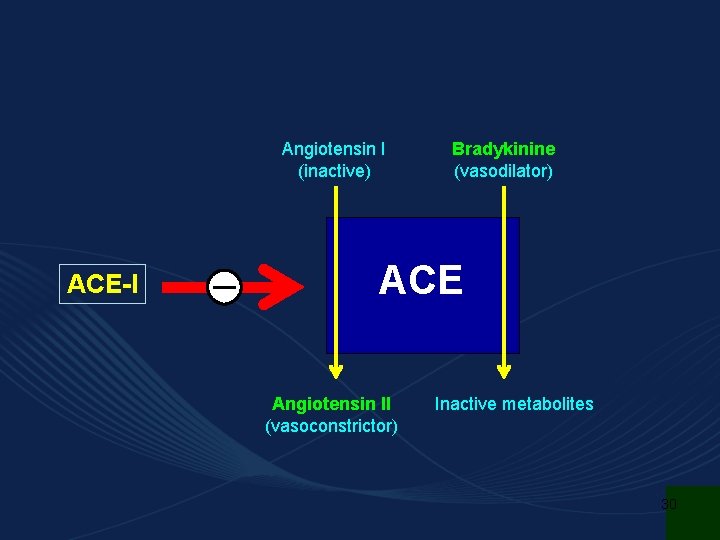
Captopril, enalapril, quinapril, lisinopril, perindopril, ramipril Indications - hypertension where thiazide diuretics and -blockers are contraindicated - useful in hypertensive patients with heart failure (beneficial effect) - diabetic nephropathy 29
Angiotensin I (inactive) ACE-I Bradykinine (vasodilator) ACE Angiotensin II (vasoconstrictor) Inactive metabolites 30
Effect of ACE-I RENIN Angiotensinogen ACE Inhibitors ANGIOTENSIN II Angiotensin I AT 1 Vasoconstriction RECEPTORS Proliferative Action AT 2 Vasodilatation Antiproliferative Action 31
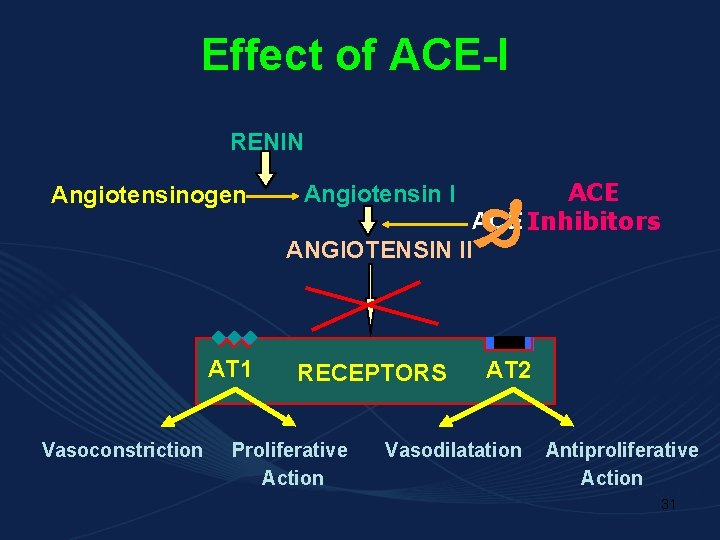
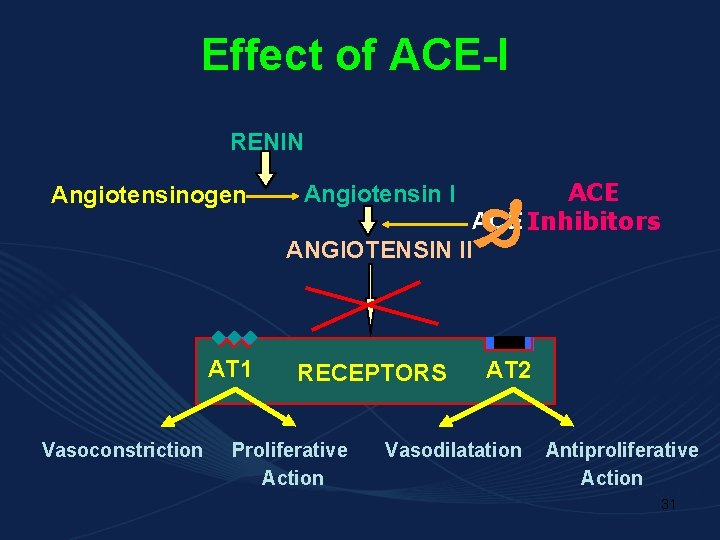
ACE-I – cont. Dilatation of arteriol reduction of peripheral vascular resistance, blood pressure and afterload Increase of Na+ and decrease of K+ excretion in kidney Decrease noradrenaline release reduction of sympathetic activity (use is not associated with reflex tachycardia) Inhibition of aldosterone secretion contributes to the antihypertensive effects of ACE-I Influence on the arteriolar and left ventricular remodelling that are believed to be important in the pathogenesis of human essential hypertension and post-infarction state 32
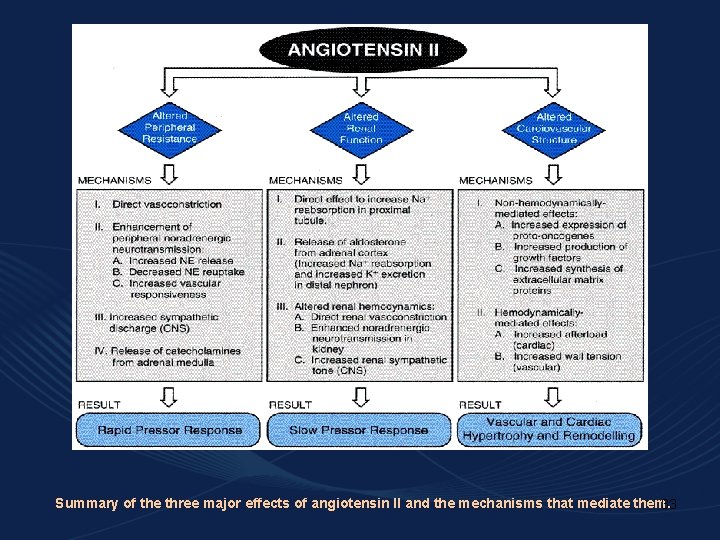
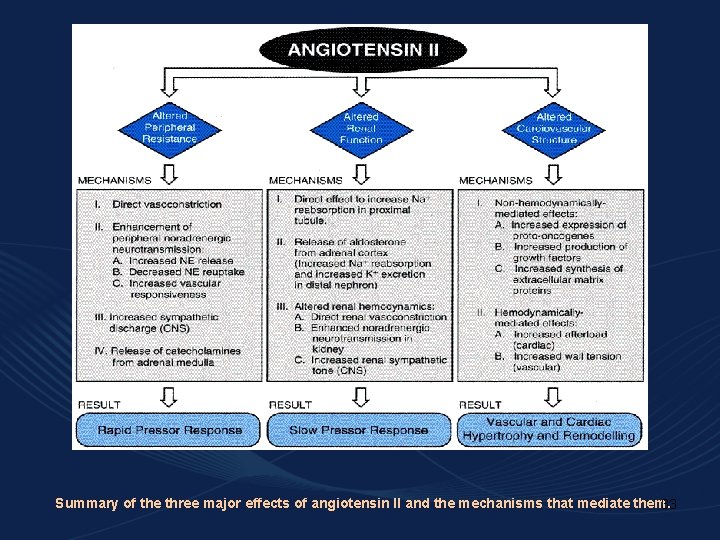
Summary of the three major effects of angiotensin II and the mechanisms that mediate them. 33
ACE-I – cont. Pharmacokinetics - active when administered orally - most of ACE-Is are highly polar, eliminated in the urine, without CNS penetration captopril, lisinopril - active per se enalapril, quinapril - prodrugs require metabolic activation enalapril, quinapril and lisinopril - given once daily captopril - administered twice daily 34
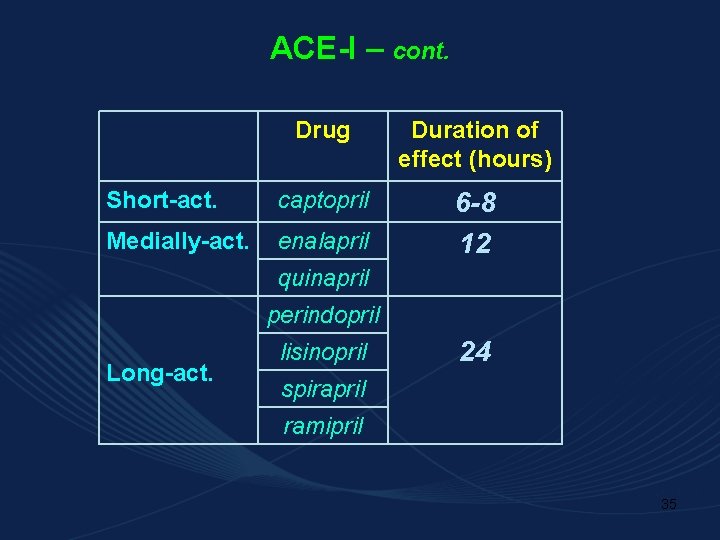
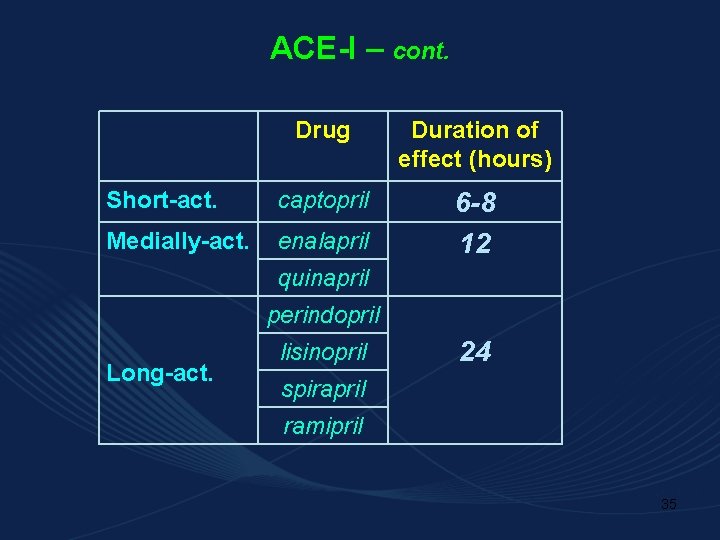
ACE-I – cont. Drug Duration of effect (hours) Short-act. captopril Medially-act. enalapril 6 -8 12 quinapril perindopril Long-act. lisinopril 24 spirapril ramipril 35
ACE-I – cont. Adverse effects -well tolerated First dose hypotension - particularly in those receiving diuretic therapy; the first dose should preferably be given at bedtime. Dry cough - the most frequent (5 -30%) symptom; Urticaria and angioneurotic edema - kinin concentrations urticarial reactions and angioneurotic edema Functional renal failure - mainly in patients with bilateral renal artery stenosis Fetal injury - results in oligohydramnios, craniofacial malformations 36
ACE-I – cont. Hyperkalemia – monitor !! - ACE-Is cause a modest increase in plasma potassium as a result of reduced aldosterone secretion. - potassium accumulation may be marked, especially if the patient is consuming high-potassium diet and/or potasssium- sparing diuretics. 37

BLOCKERS OF AT 1 RECEPTOR 38
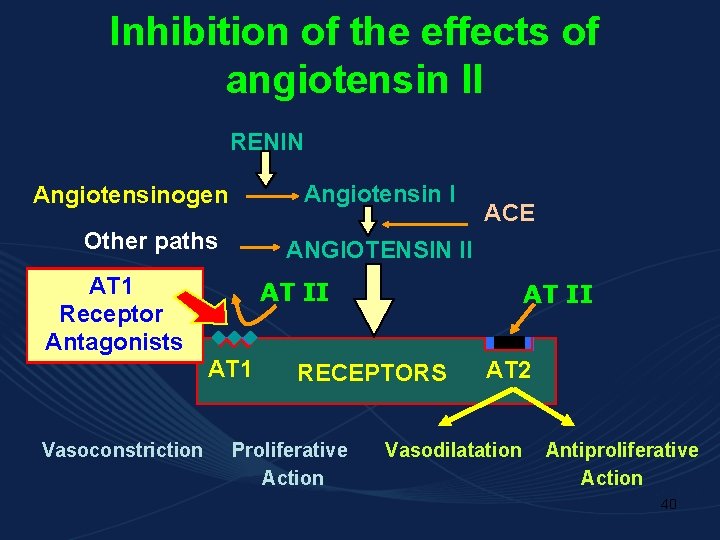
losartan, valosartan, irbesartan -it competitively inhibit angiotensin II at its AT 1 receptor site Mechanisms responsible for antihypertensive effect: inhibition of direct vasoconstrictive effect of A-II decrease of sympathetic nerve activity decrease of A-II-mediated aldosterone release decrease of RAS activity in CNS decrease of smooth muscle and cardiac hypertrophy and hyperplasia 39
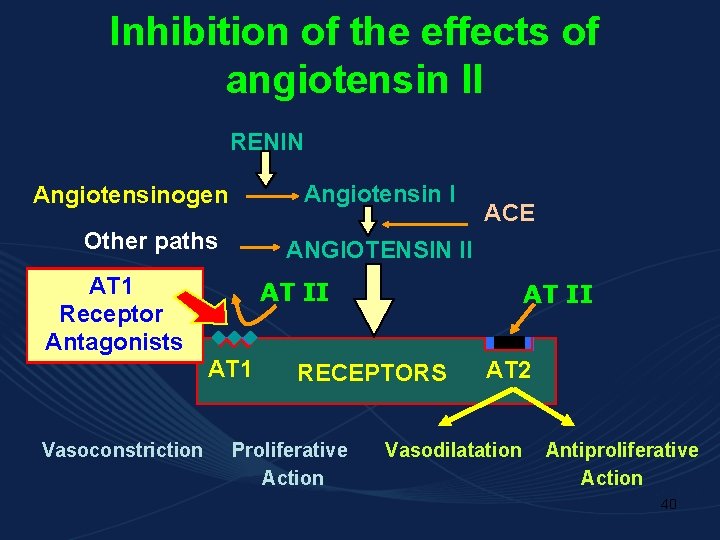
Inhibition of the effects of angiotensin II RENIN Angiotensin I Angiotensinogen Other paths AT 1 Receptor Antagonists ANGIOTENSIN II AT II AT 1 Vasoconstriction ACE RECEPTORS Proliferative Action AT 2 Vasodilatation Antiproliferative Action 40
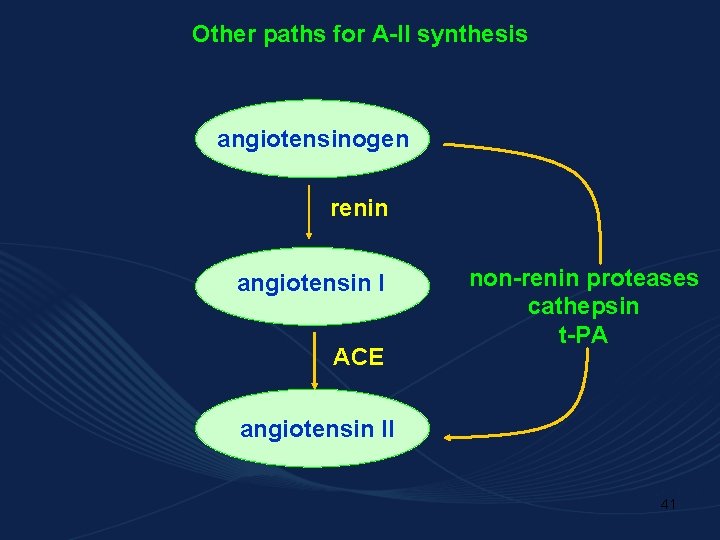
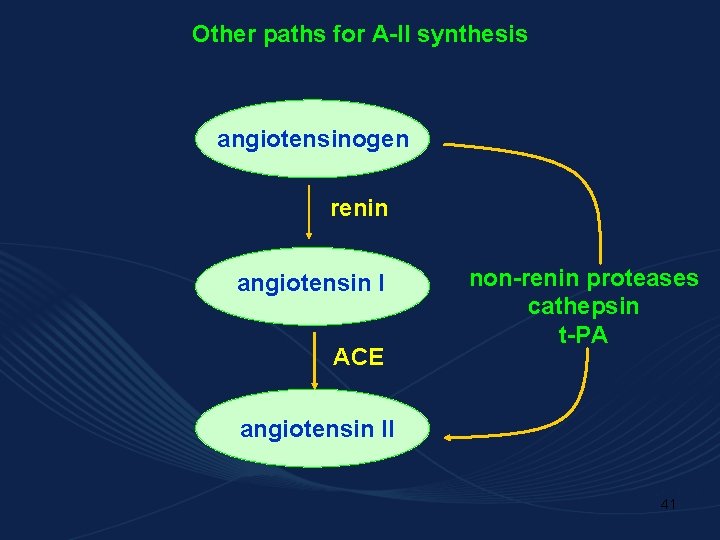
Other paths for A-II synthesis angiotensinogen renin angiotensin I ACE non-renin proteases cathepsin t-PA angiotensin II 41
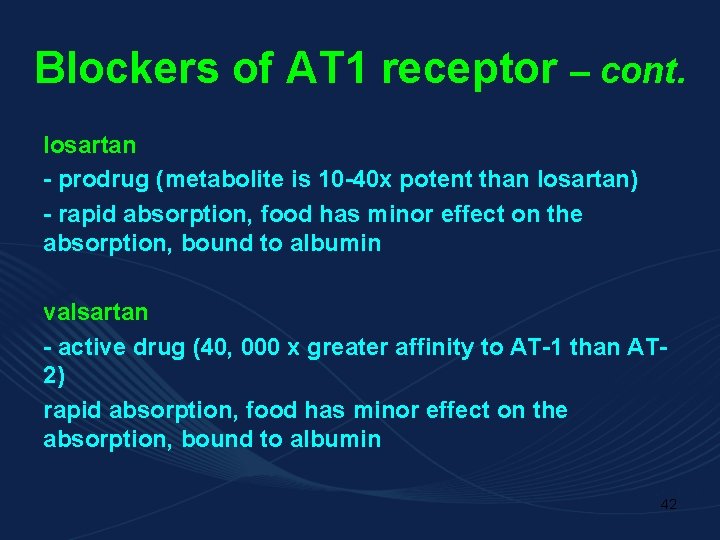
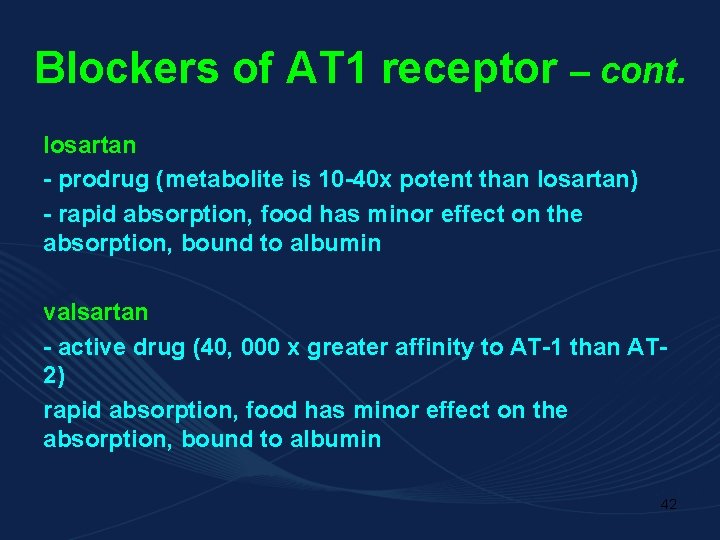
Blockers of AT 1 receptor – cont. losartan - prodrug (metabolite is 10 -40 x potent than losartan) - rapid absorption, food has minor effect on the absorption, bound to albumin valsartan - active drug (40, 000 x greater affinity to AT-1 than AT 2) rapid absorption, food has minor effect on the absorption, bound to albumin 42
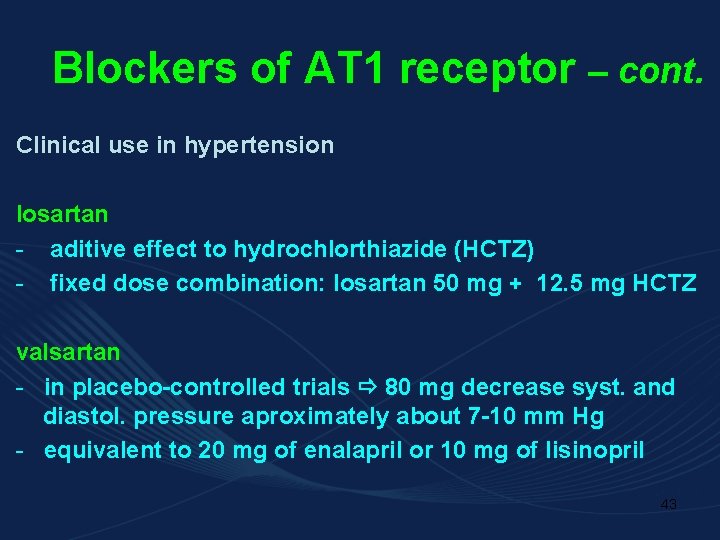
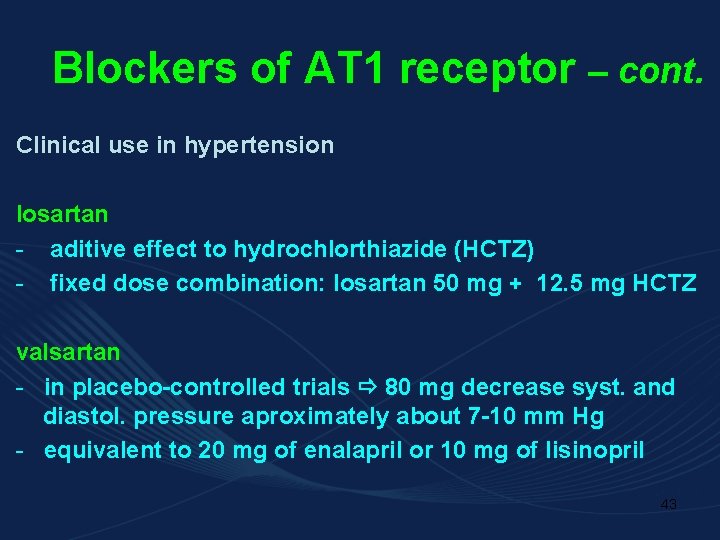
Blockers of AT 1 receptor – cont. Clinical use in hypertension losartan - aditive effect to hydrochlorthiazide (HCTZ) - fixed dose combination: losartan 50 mg + 12. 5 mg HCTZ valsartan - in placebo-controlled trials 80 mg decrease syst. and diastol. pressure aproximately about 7 -10 mm Hg - equivalent to 20 mg of enalapril or 10 mg of lisinopril 43
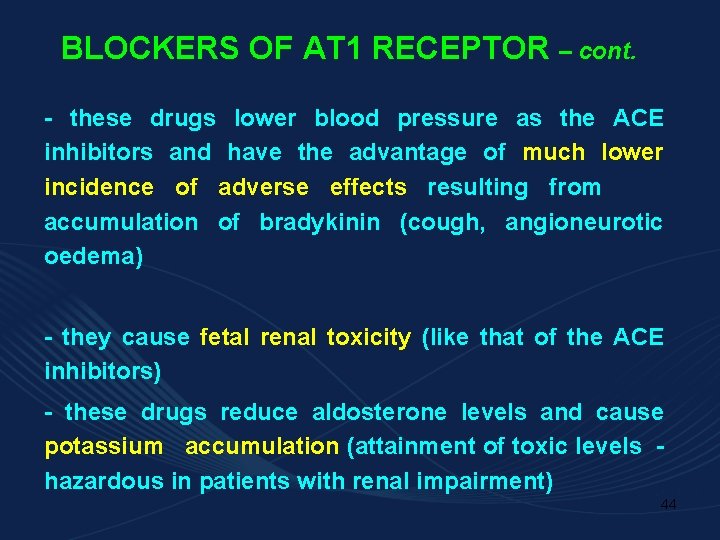
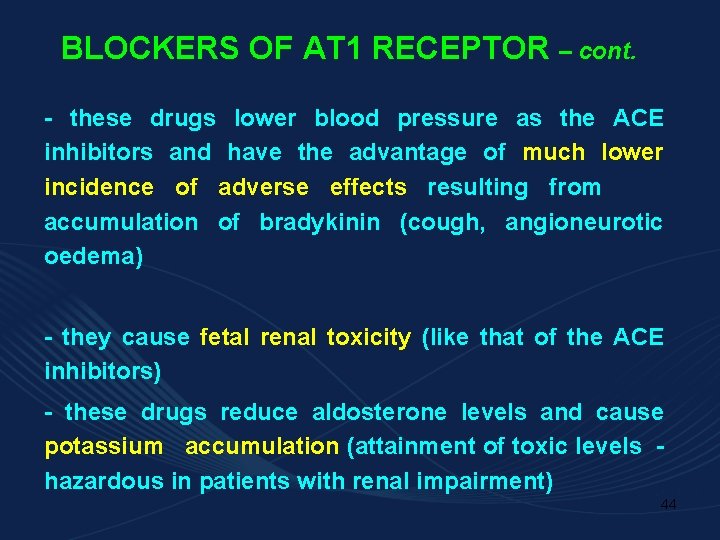
BLOCKERS OF AT 1 RECEPTOR – cont. - these drugs lower blood pressure as the ACE inhibitors and have the advantage of much lower incidence of adverse effects resulting from accumulation of bradykinin (cough, angioneurotic oedema) - they cause fetal renal toxicity (like that of the ACE inhibitors) - these drugs reduce aldosterone levels and cause potassium accumulation (attainment of toxic levels hazardous in patients with renal impairment) 44
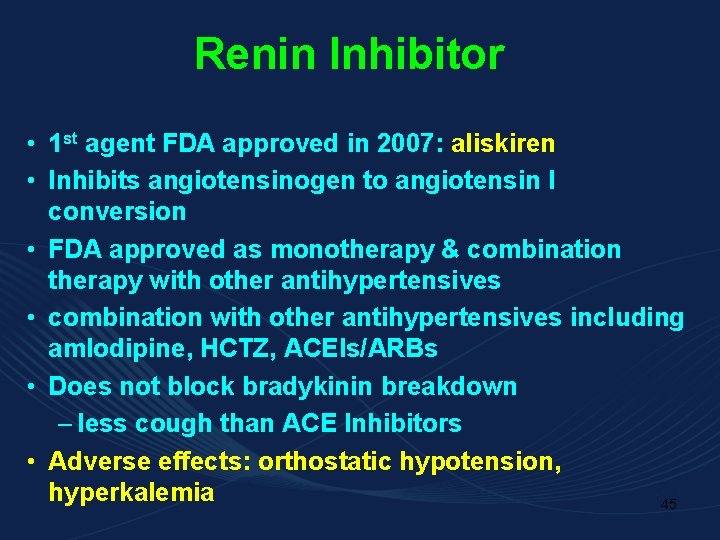
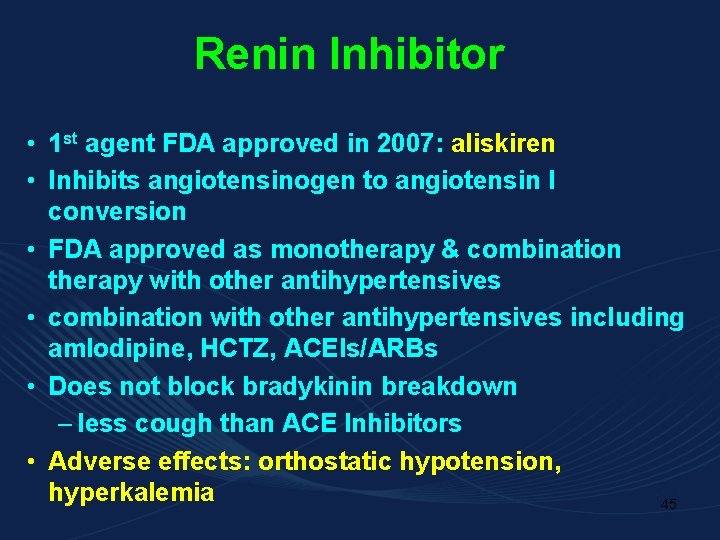
Renin Inhibitor • 1 st agent FDA approved in 2007: aliskiren • Inhibits angiotensinogen to angiotensin I conversion • FDA approved as monotherapy & combination therapy with other antihypertensives • combination with other antihypertensives including amlodipine, HCTZ, ACEIs/ARBs • Does not block bradykinin breakdown – less cough than ACE Inhibitors • Adverse effects: orthostatic hypotension, hyperkalemia 45
Calcium channel blockers (CCBs) 46
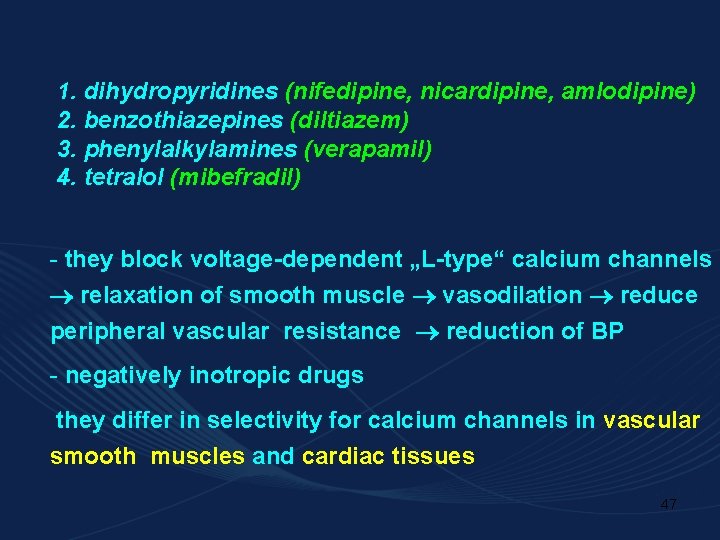
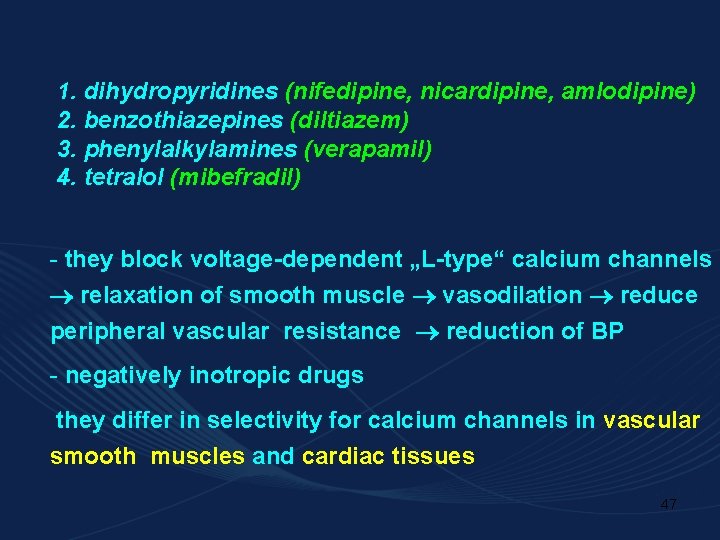
1. dihydropyridines (nifedipine, nicardipine, amlodipine) 2. benzothiazepines (diltiazem) 3. phenylalkylamines (verapamil) 4. tetralol (mibefradil) - they block voltage-dependent „L-type“ calcium channels relaxation of smooth muscle vasodilation reduce peripheral vascular resistance reduction of BP - negatively inotropic drugs they differ in selectivity for calcium channels in vascular smooth muscles and cardiac tissues 47
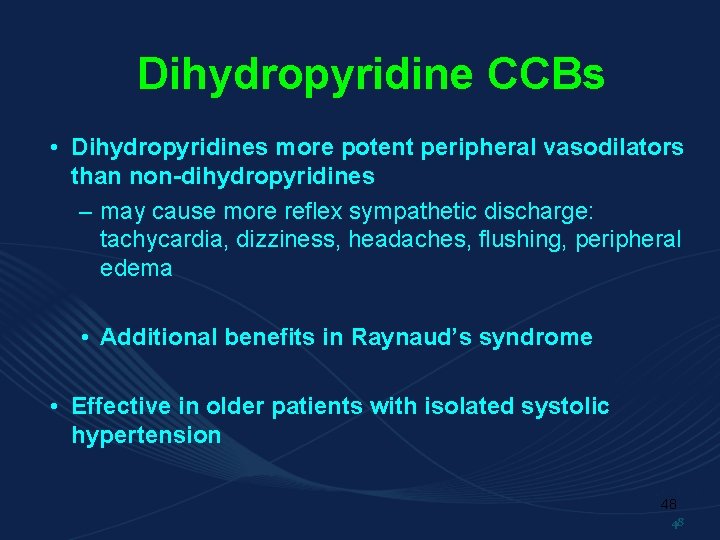
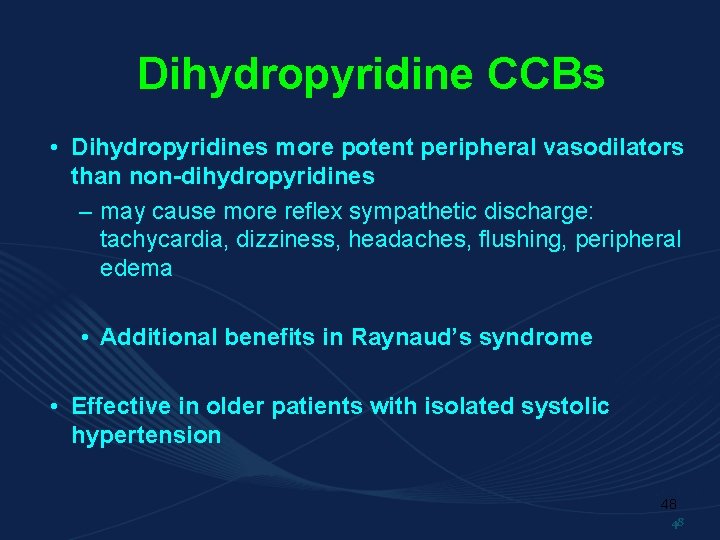
Dihydropyridine CCBs • Dihydropyridines more potent peripheral vasodilators than non-dihydropyridines – may cause more reflex sympathetic discharge: tachycardia, dizziness, headaches, flushing, peripheral edema • Additional benefits in Raynaud’s syndrome • Effective in older patients with isolated systolic hypertension 48 48
• Indication: all grades of essential hypertension • alone (nifedipine, amlodipine) in patients with mild hypertension for patients in whom thiazide diuretics and b-blockers are contraindicated • combinations • angina (with -blockers) 49
Non-dihydropyridine CCBs • extended release products preferred for hypertension • Block cardiac SA (diltiazem) or AV (verapamil) nodes: reduce HR • May produce heart block • Additional benefits in patients with atrial tachyarrhythmia 50 50
Unwanted effects - reflex tachycardia if nifedipine-like drugs are used - constipation - dizziness - headache, flushing, ankle swelling - fatigue - AV block 51
Mibefradil - newest calcium blocker - blockade of L and T channels - do not possess the negative inotropic effect of verapamil and diltiazem - it can depres cardiac conductance - it is not associated vith peripheral edema and reflex tachycardia of the dihydropyridines - antihypertensive effect is evident within the first week of therapy - efficacy may be diminished in dietary sodium restriction and diuretic co-therapy (both stimulate renin activity) 52
Other a) -adrenoreceptor antagonists b) centrally acting symatomimetics c) direct vasodilators 53
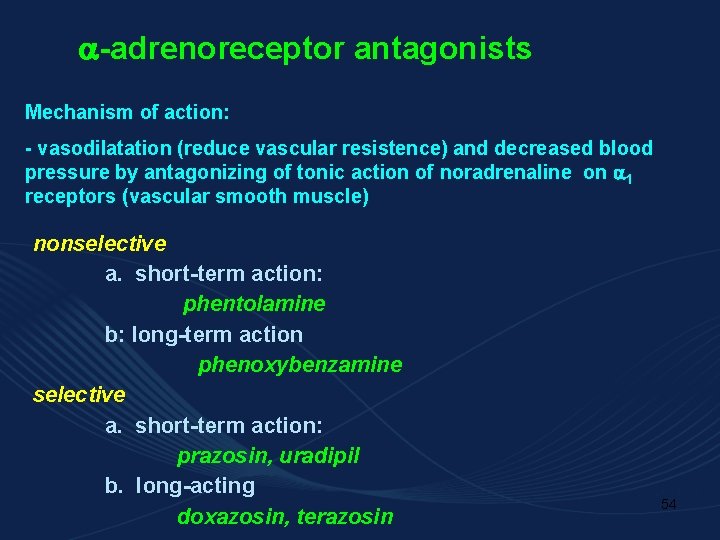
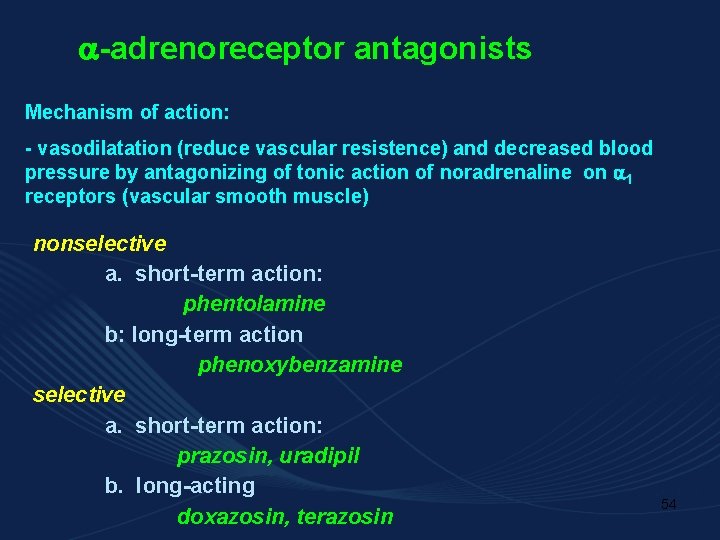
-adrenoreceptor antagonists Mechanism of action: - vasodilatation (reduce vascular resistence) and decreased blood pressure by antagonizing of tonic action of noradrenaline on 1 receptors (vascular smooth muscle) nonselective a. short-term action: phentolamine b: long-term action phenoxybenzamine selective a. short-term action: prazosin, uradipil b. long-acting doxazosin, terazosin 54
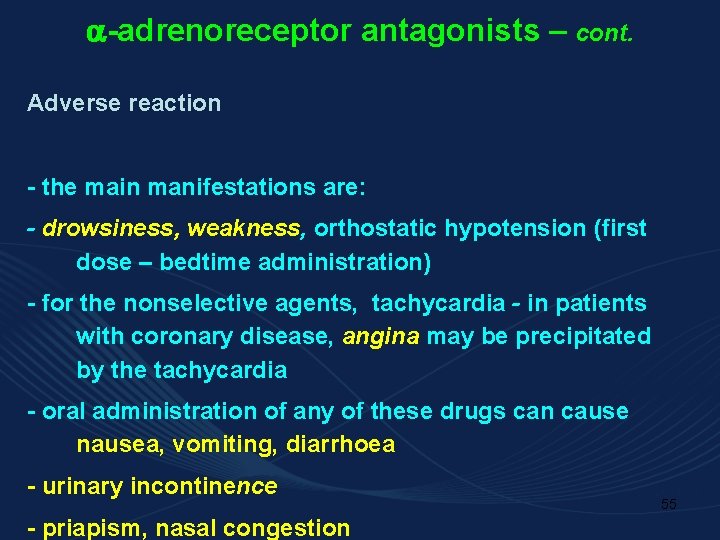
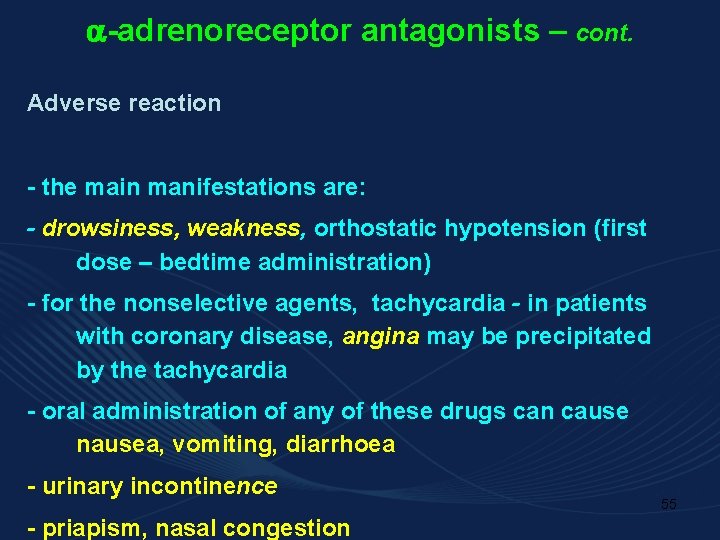
-adrenoreceptor antagonists – cont. Adverse reaction - the main manifestations are: - drowsiness, weakness, orthostatic hypotension (first dose – bedtime administration) - for the nonselective agents, tachycardia - in patients with coronary disease, angina may be precipitated by the tachycardia - oral administration of any of these drugs can cause nausea, vomiting, diarrhoea - urinary incontinence - priapism, nasal congestion 55
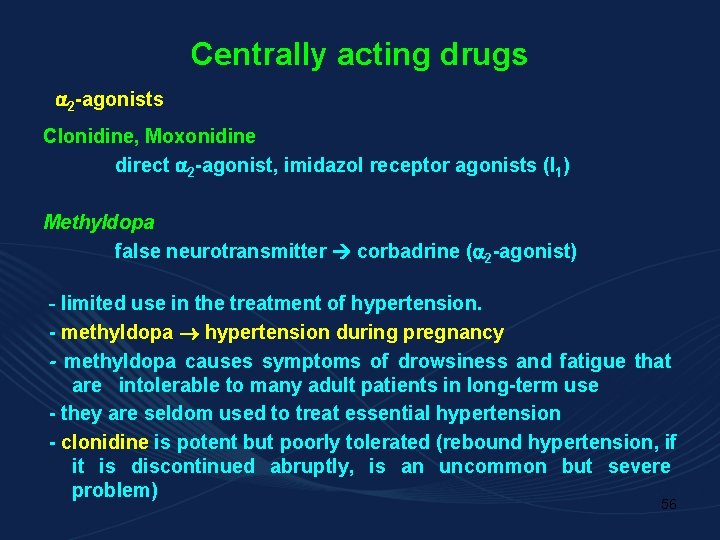
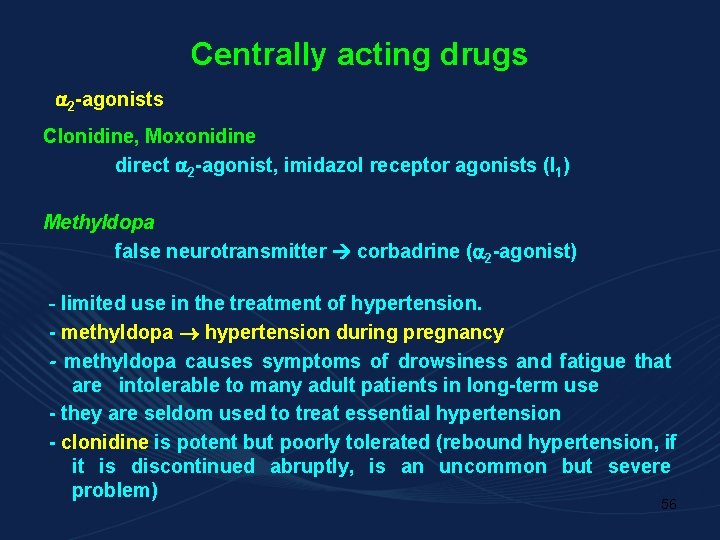
Centrally acting drugs 2 -agonists Clonidine, Moxonidine direct 2 -agonist, imidazol receptor agonists (I 1) Methyldopa false neurotransmitter corbadrine ( 2 -agonist) - limited use in the treatment of hypertension. - methyldopa hypertension during pregnancy - methyldopa causes symptoms of drowsiness and fatigue that are intolerable to many adult patients in long-term use - they are seldom used to treat essential hypertension - clonidine is potent but poorly tolerated (rebound hypertension, if it is discontinued abruptly, is an uncommon but severe problem) 56
Centrally acting drugs – cont. Adverse effects - drowsiness, fatigue (esp. methyldopa), depression, nightmares - nasal congestion, anticholinergic symptoms (constipation, bradycardia) – clonidine - dry mouth - hepatitis, drug fever (methyldopa) - sexual dysfunction, salt and water retention - hypertensive rebound associated with anxiety, sweating, tachycardia and extrasystoles (rarely hypertensive crisis) 57
Direct Arterial Vasodilators • Direct arterial smooth muscle relaxation causes antihypertensive effect (little or no venous vasodilation) – reduce impedence to myocardial contractility – potent reductions in perfusion pressure activate baroreceptor reflexes – baroreceptor activation: compensatory increase in sympathetic outflow; tachyphylaxis can cause loss of antihypertensive effect • counteract with concurrent β-blocker • clonidine if β-blocker contraindicated 58 58
Vasodilators – cont. - drugs which dilate blood vessels (and decrease peripheral vascular resistance) by acting on smooth muscle cells through non-autonomic mechanisms: * release of nitric oxide * opening of potassium channels 59
Drugs acting via NO release Sodium nitroprusside - short-acting agent (few minutes) administrated by infusion in hypertensive emergencies (hypertensive encephalopathy, shock, cardiac dysfunction) for max 24 hours (risk of cyanide cummulation toxicity) - photodeactivation - - adverse effects: too rapid reduction of BP, nausea, 60 palpitation, dizziness
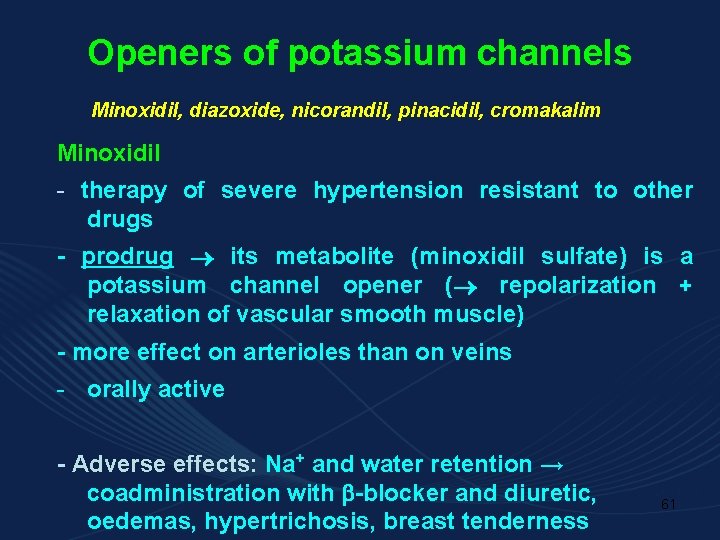
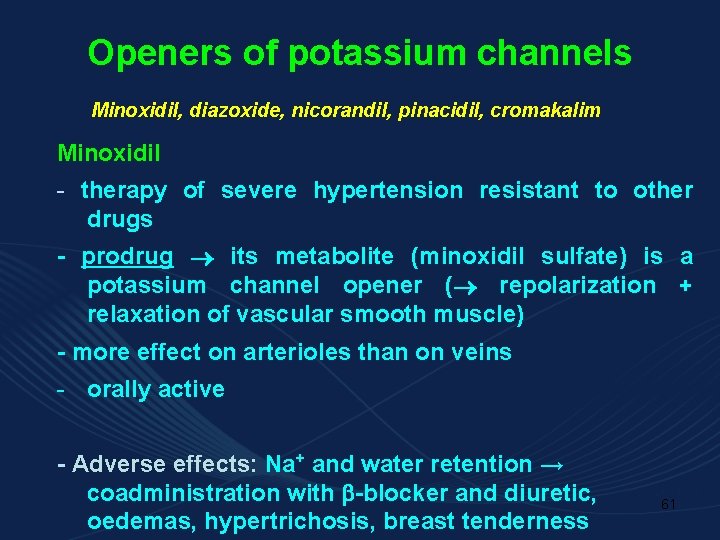
Openers of potassium channels Minoxidil, diazoxide, nicorandil, pinacidil, cromakalim Minoxidil - therapy of severe hypertension resistant to other drugs - prodrug its metabolite (minoxidil sulfate) is a potassium channel opener ( repolarization + relaxation of vascular smooth muscle) - more effect on arterioles than on veins - orally active - Adverse effects: Na+ and water retention → coadministration with -blocker and diuretic, oedemas, hypertrichosis, breast tenderness 61
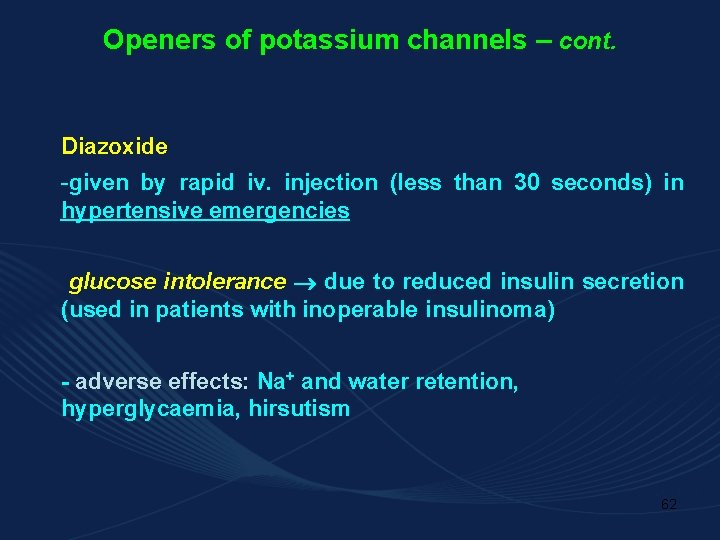
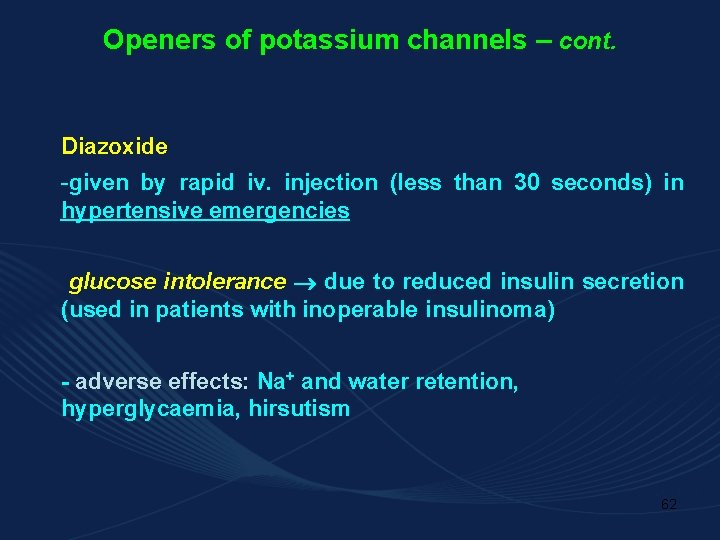
Openers of potassium channels – cont. Diazoxide -given by rapid iv. injection (less than 30 seconds) in hypertensive emergencies glucose intolerance due to reduced insulin secretion (used in patients with inoperable insulinoma) - adverse effects: Na+ and water retention, hyperglycaemia, hirsutism 62
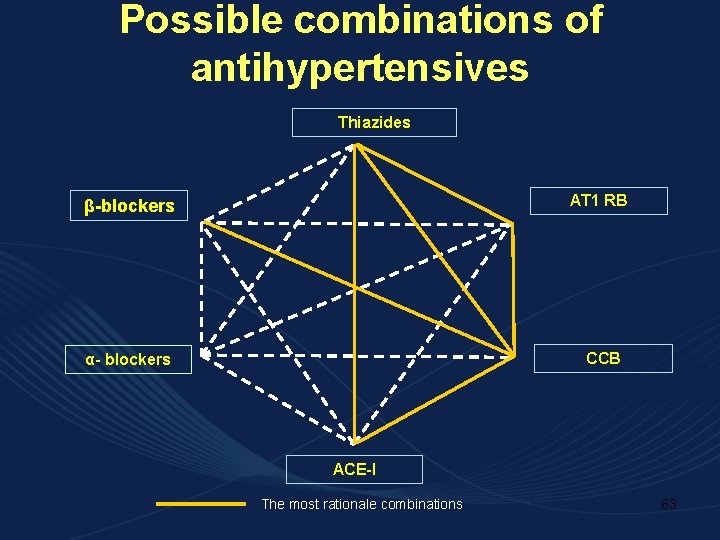
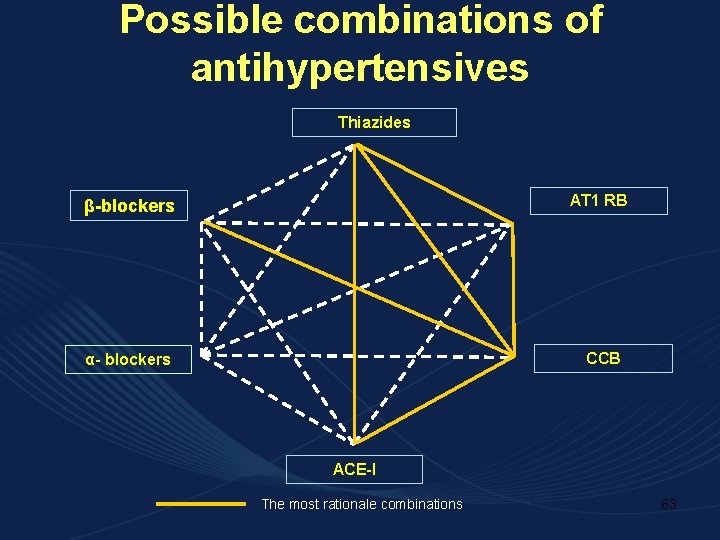
Possible combinations of antihypertensives Thiazides β-blockers AT 1 RB α- blockers CCB ACE-I The most rationale combinations 63
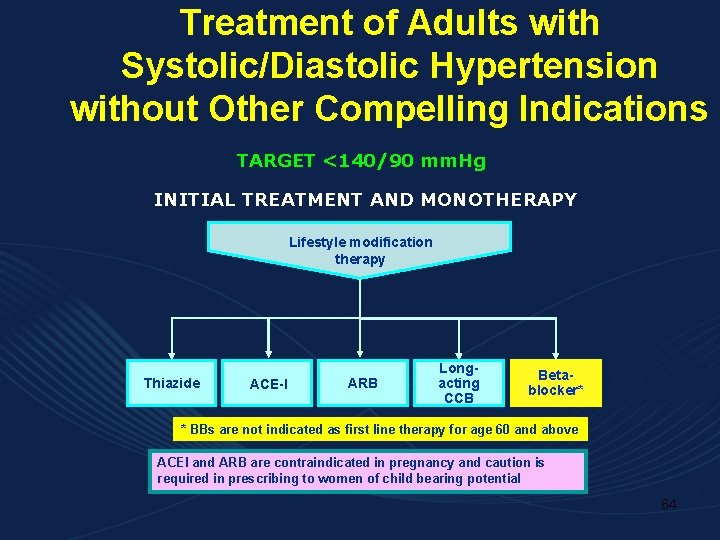
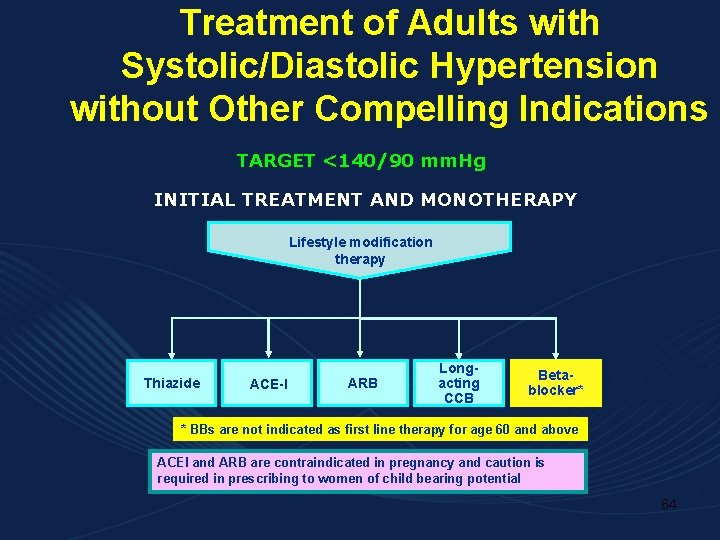
Treatment of Adults with Systolic/Diastolic Hypertension without Other Compelling Indications TARGET <140/90 mm. Hg INITIAL TREATMENT AND MONOTHERAPY Lifestyle modification therapy Thiazide ACE-I ARB Longacting CCB Betablocker* * BBs are not indicated as first line therapy for age 60 and above ACEI and ARB are contraindicated in pregnancy and caution is required in prescribing to women of child bearing potential 64
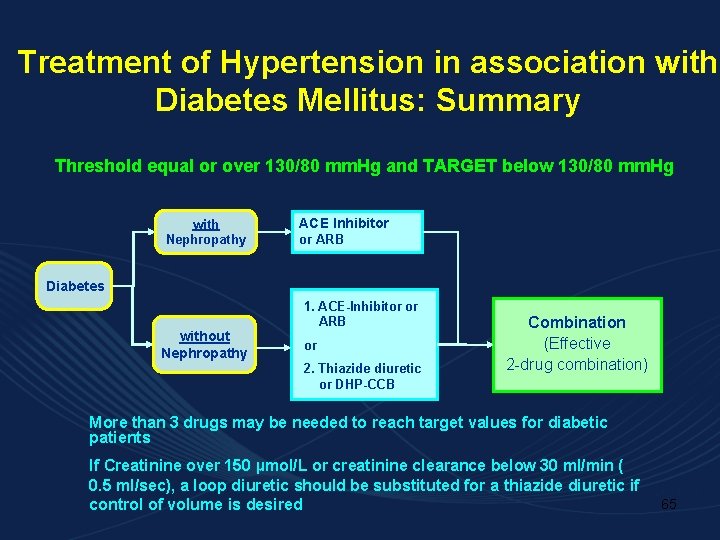
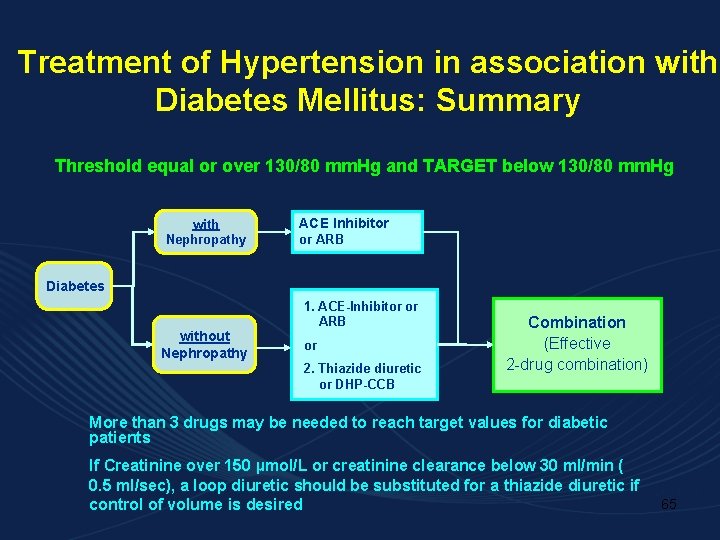
Treatment of Hypertension in association with Diabetes Mellitus: Summary Threshold equal or over 130/80 mm. Hg and TARGET below 130/80 mm. Hg with Nephropathy ACE Inhibitor or ARB Diabetes without Nephropathy 1. ACE-Inhibitor or ARB or 2. Thiazide diuretic or DHP-CCB Combination (Effective 2 -drug combination) More than 3 drugs may be needed to reach target values for diabetic patients If Creatinine over 150 µmol/L or creatinine clearance below 30 ml/min ( 0. 5 ml/sec), a loop diuretic should be substituted for a thiazide diuretic if control of volume is desired 65
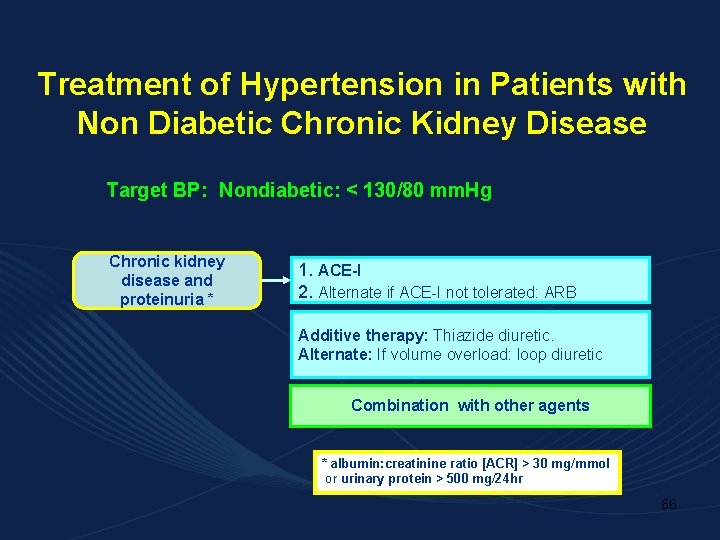
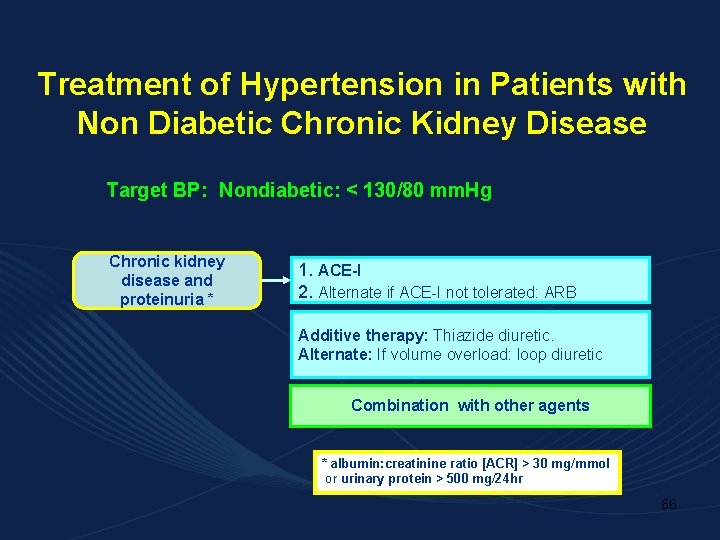
Treatment of Hypertension in Patients with Non Diabetic Chronic Kidney Disease Target BP: Nondiabetic: < 130/80 mm. Hg Chronic kidney disease and proteinuria * 1. ACE-I 2. Alternate if ACE-I not tolerated: ARB Additive therapy: Thiazide diuretic. Alternate: If volume overload: loop diuretic Combination with other agents * albumin: creatinine ratio [ACR] > 30 mg/mmol or urinary protein > 500 mg/24 hr 66
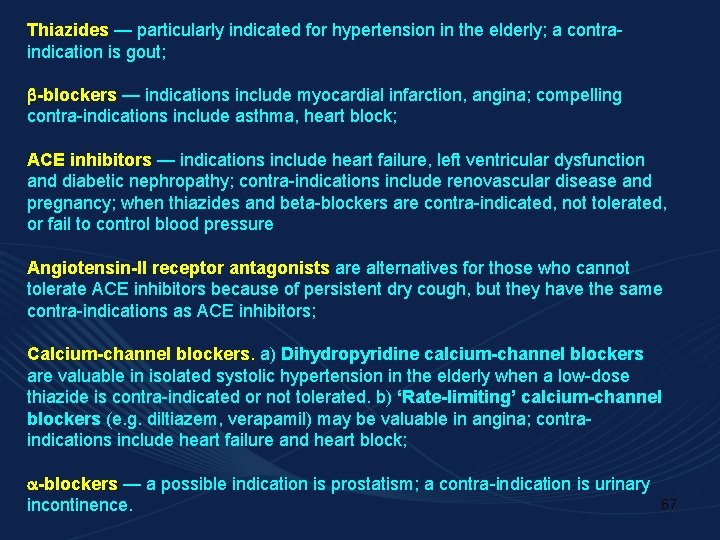
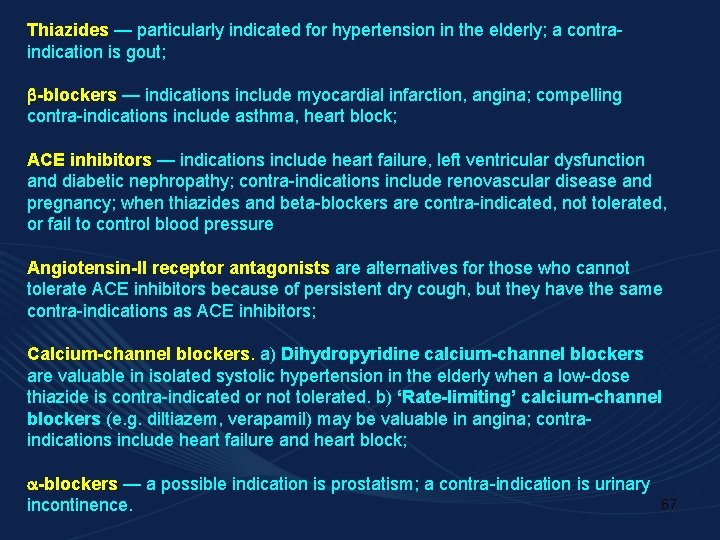
Thiazides — particularly indicated for hypertension in the elderly; a contraindication is gout; -blockers — indications include myocardial infarction, angina; compelling contra-indications include asthma, heart block; ACE inhibitors — indications include heart failure, left ventricular dysfunction and diabetic nephropathy; contra-indications include renovascular disease and pregnancy; when thiazides and beta-blockers are contra-indicated, not tolerated, or fail to control blood pressure Angiotensin-II receptor antagonists are alternatives for those who cannot tolerate ACE inhibitors because of persistent dry cough, but they have the same contra-indications as ACE inhibitors; Calcium-channel blockers. a) Dihydropyridine calcium-channel blockers are valuable in isolated systolic hypertension in the elderly when a low-dose thiazide is contra-indicated or not tolerated. b) ‘Rate-limiting’ calcium-channel blockers (e. g. diltiazem, verapamil) may be valuable in angina; contraindications include heart failure and heart block; -blockers — a possible indication is prostatism; a contra-indication is urinary incontinence. 67
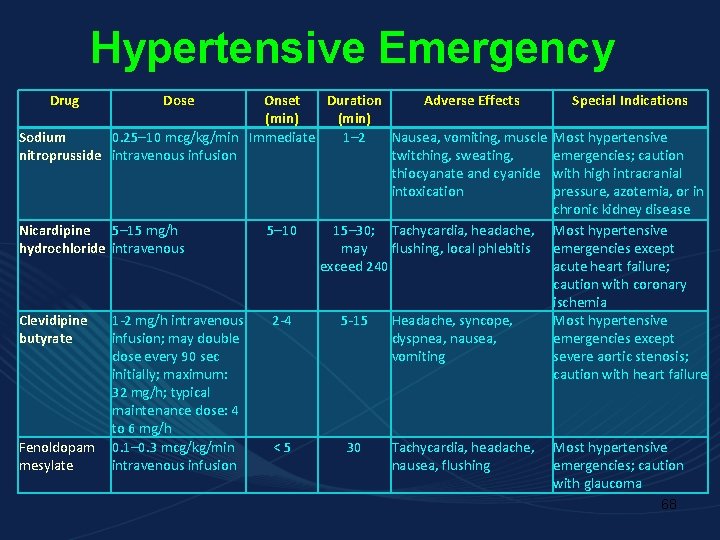
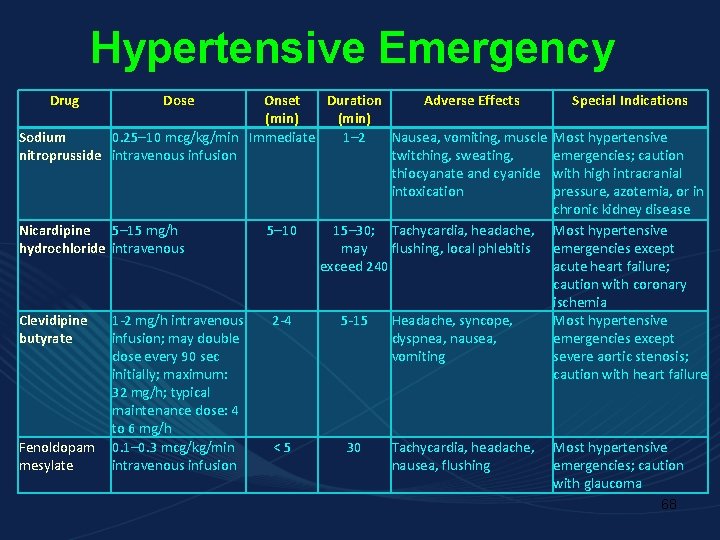
Hypertensive Emergency Drug Dose Onset Duration Adverse Effects (min) Sodium 0. 25– 10 mcg/kg/min Immediate 1– 2 Nausea, vomiting, muscle nitroprusside intravenous infusion twitching, sweating, thiocyanate and cyanide intoxication Nicardipine 5– 15 mg/h hydrochloride intravenous Clevidipine butyrate Fenoldopam mesylate 1 -2 mg/h intravenous infusion; may double dose every 90 sec initially; maximum: 32 mg/h; typical maintenance dose: 4 to 6 mg/h 0. 1– 0. 3 mcg/kg/min intravenous infusion 5– 10 15– 30; Tachycardia, headache, may flushing, local phlebitis exceed 240 2 -4 5 -15 <5 30 Headache, syncope, dyspnea, nausea, vomiting Tachycardia, headache, nausea, flushing Special Indications Most hypertensive emergencies; caution with high intracranial pressure, azotemia, or in chronic kidney disease Most hypertensive emergencies except acute heart failure; caution with coronary ischemia Most hypertensive emergencies except severe aortic stenosis; caution with heart failure Most hypertensive emergencies; caution with glaucoma 68
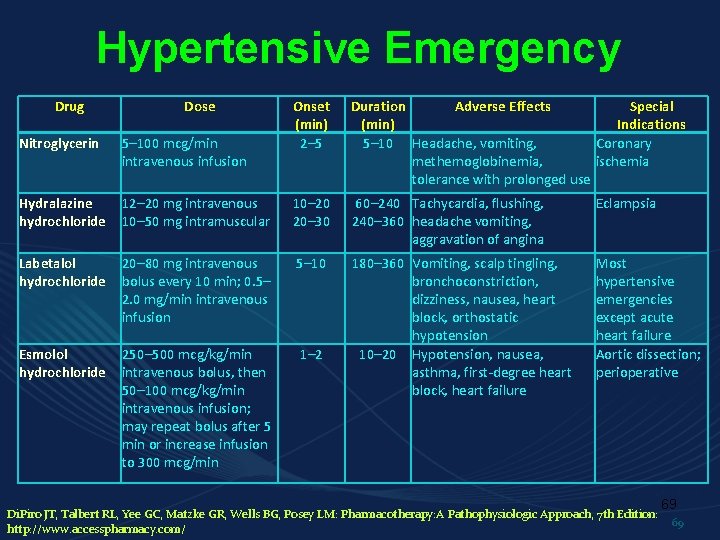
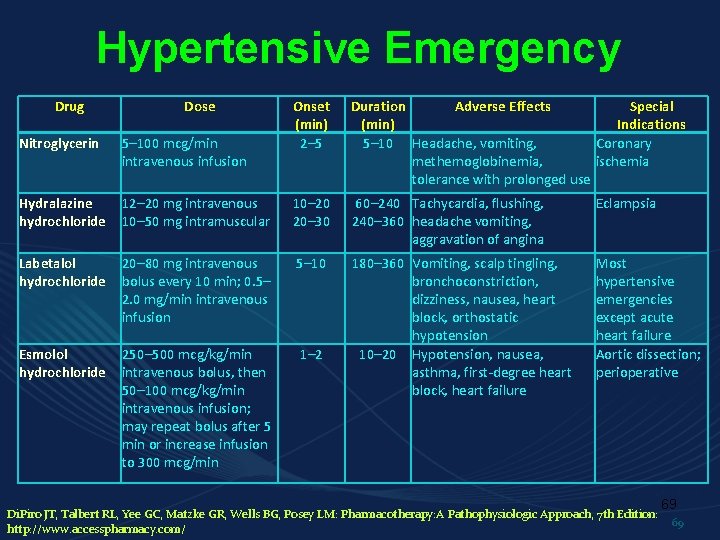
Hypertensive Emergency Drug Dose Onset (min) 2– 5 Duration Adverse Effects Special (min) Indications 5– 10 Headache, vomiting, Coronary methemoglobinemia, ischemia tolerance with prolonged use Nitroglycerin 5– 100 mcg/min intravenous infusion Hydralazine hydrochloride 12– 20 mg intravenous 10– 50 mg intramuscular 10– 20 20– 30 60– 240 Tachycardia, flushing, 240– 360 headache vomiting, aggravation of angina Eclampsia Labetalol hydrochloride 20– 80 mg intravenous bolus every 10 min; 0. 5– 2. 0 mg/min intravenous infusion 5– 10 Esmolol hydrochloride 250– 500 mcg/kg/min intravenous bolus, then 50– 100 mcg/kg/min intravenous infusion; may repeat bolus after 5 min or increase infusion to 300 mcg/min 1– 2 180– 360 Vomiting, scalp tingling, bronchoconstriction, dizziness, nausea, heart block, orthostatic hypotension 10– 20 Hypotension, nausea, asthma, first-degree heart block, heart failure Most hypertensive emergencies except acute heart failure Aortic dissection; perioperative Di. Piro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey LM: Pharmacotherapy: A Pathophysiologic Approach, 7 th Edition: http: //www. accesspharmacy. com/ 69 69
 How do we treat the life the life how we treat
How do we treat the life the life how we treat Antihypertensive drugs classification
Antihypertensive drugs classification Preci i potomci
Preci i potomci Lauren kocher
Lauren kocher Pozitivni digitalni tragovi
Pozitivni digitalni tragovi Katarina zeljic
Katarina zeljic Lirika epika dramatika
Lirika epika dramatika Sretni brojevi
Sretni brojevi Predci i potomci
Predci i potomci Which seedless plants have been used to treat bee stings?
Which seedless plants have been used to treat bee stings? Is byetta used to treat pcos
Is byetta used to treat pcos Why are seedless plants important
Why are seedless plants important 7 trays in labour room
7 trays in labour room Teratogens images
Teratogens images Diueritique
Diueritique Hypertension vs hypotension
Hypertension vs hypotension Hypertension
Hypertension Disease state awareness
Disease state awareness Syndrome méningé
Syndrome méningé Pah vs pulmonary hypertension
Pah vs pulmonary hypertension Hypertension
Hypertension Diagnosis hypertension
Diagnosis hypertension Hypertension
Hypertension Hypertensive emergency vs urgency
Hypertensive emergency vs urgency Demadex
Demadex Varices cardio tubérositaires
Varices cardio tubérositaires Stage 1 hypertension
Stage 1 hypertension Rules of halves in hypertension
Rules of halves in hypertension Systemic vascular resistance
Systemic vascular resistance Definition of hypertension
Definition of hypertension Masked hypertension
Masked hypertension Paedp echo
Paedp echo Causes of secondary hypertension
Causes of secondary hypertension Features of cld
Features of cld Hypertension vs hypotension
Hypertension vs hypotension Nt pro brain natriuretic peptide
Nt pro brain natriuretic peptide Signs of portal hypertension
Signs of portal hypertension Missed some points on the visual field test for dvla'
Missed some points on the visual field test for dvla' Hypertensive urgency
Hypertensive urgency Malignant hypertension management
Malignant hypertension management Definition of hypertension
Definition of hypertension Dash diet
Dash diet Aobp vs obpm
Aobp vs obpm Conclusion of hypertension
Conclusion of hypertension Pulmonary hypertension definition
Pulmonary hypertension definition Pulmonary hypertension causes
Pulmonary hypertension causes Mitral stenosis pulmonary hypertension
Mitral stenosis pulmonary hypertension Hypertensive encephalopathy
Hypertensive encephalopathy Pico question examples hypertension
Pico question examples hypertension Conclusion of hypertension
Conclusion of hypertension Hypertensive emergency
Hypertensive emergency Background
Background Presenting complaints of hypertension
Presenting complaints of hypertension Conclusion of hypertension
Conclusion of hypertension Medical nutrition therapy for hypertension
Medical nutrition therapy for hypertension Case scenario for hypertension
Case scenario for hypertension Cruveilhier sign varicose veins
Cruveilhier sign varicose veins Intracranial hypertension
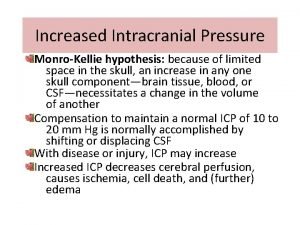
Intracranial hypertension Nursing management of portal hypertension
Nursing management of portal hypertension Intracranial hypertension
Intracranial hypertension Complication of liver cirrhosis
Complication of liver cirrhosis Health coaches for hypertension control
Health coaches for hypertension control Rules of halves in hypertension
Rules of halves in hypertension Hypertensive urgency vs emergency
Hypertensive urgency vs emergency Intimal hyperplasia
Intimal hyperplasia Sachin gupta md
Sachin gupta md Hypertension
Hypertension Pulmonary hypertension
Pulmonary hypertension Isolated systolic hypertension
Isolated systolic hypertension Hyperkaliémie cause
Hyperkaliémie cause