CHAPTER 24 Drugs Used to Treat Respiratory Diseases













- Slides: 48

CHAPTER 24 Drugs Used to Treat Respiratory Diseases

�respiratory system is a series of airways that start with the nose and mouth and end at the alveoli in the lungs �respiratory system is divided into: ◦ upper respiratory tract: nose, sinuses, nasopharynx, tonsils, eustachian tubes and larynx(fig 24 -2 p. 301) ◦ lower respiratory tract: larynx, trachea, bronchioles, alveoli (fig 24 -3, p. 302)

Respiratory System: Structure and Function: (Box 24 -1 pg. 300 -301) � respiratory system brings oxygen (O 2) into lungs and removes carbon dioxide (CO 2) � air enters body through nose � nose and it’s structures serve 2 functions: ◦ olfactory (smell): upper part of each nostril, cells contain microscopic hairs that react to odors in the air. Hairs stimulate olfactory cells, send signal to brain where sense of smell is processed ◦ respiratory: the nose warms, humidifies, and filters inhaled air, both nasal passages have folds of skin called turbinates. These folds increase the amount of nasal tissue. Turbinate tissue contains many blood vessels, and are lined with membranes. Blood circulating through these membranes warms and humidifies the inhaled air

Respiratory System: Structure and Function cont… � particles in the inhaled air are filtered by large hairs at entrance � tubinates and narrow nasal passages cause turbulence of air flow with each inhalation � all nose surfaces are coated with a thin layer of mucous � because of turbulent air flow, particles are “thrown” against walls of nasal passages, they become trapped � cells lining back 2/3 of nasal passage contain cilia � cilia: small hair-like structures that project outward from the surfaces of some cells, they sweep particulate matter back toward naso-pharynx and pharynx � once in pharynx, particulate matter is swallowed or expectorated � warming, humidifying, filtering continues as air passes
Respiratory System: Structure and Function cont… � ANS (autonomic nervous system) controls the nasal structures, cholinergic stimulation causes vaso-dilation � blood vessels lining nasal mucous membranes dilate � when cholinergic fibers in secretory glands are stimulated, serous and mucous secretions are produced � sympathetic stimulation causes vaso-constriction
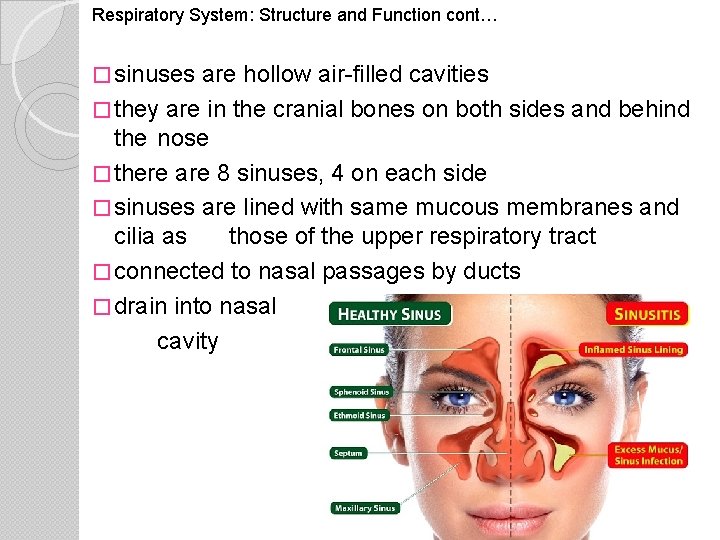
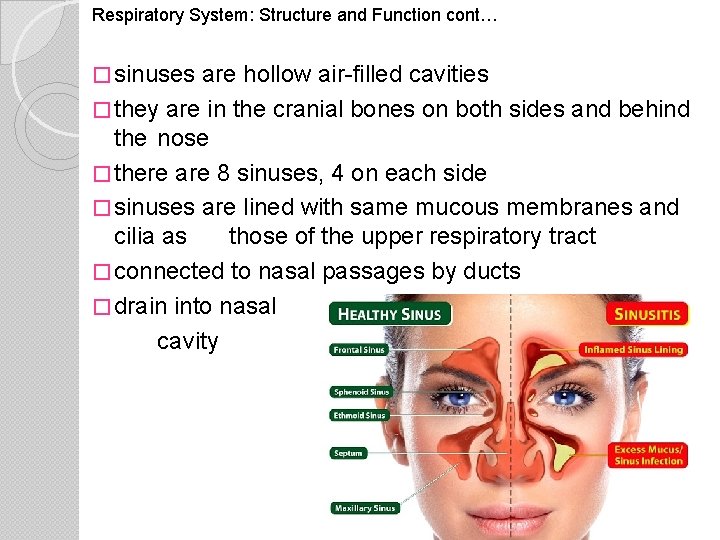
Respiratory System: Structure and Function cont… � sinuses are hollow air-filled cavities � they are in the cranial bones on both sides and behind the nose � there are 8 sinuses, 4 on each side � sinuses are lined with same mucous membranes and cilia as those of the upper respiratory tract � connected to nasal passages by ducts � drain into nasal cavity
Respiratory System: Structure and Function cont… � tonsils are on each side of pharynx, they are lymphatic tissues � located where mucus filled with particulate matter collects from ciliary action in the naso-pharynx � particulate matter includes virus particles and bacteria � lymph tissue is thought to play a role in immune defense mechanisms of upper airway � sneezing: reflex that clears the nasal passages of particulate matter, sneeze starts by irritation of nasal membranes caused by particulate matter � air then passes into pharynx (throat), then from pharynx to larynx (voice box) � piece of cartilage (epiglottis) acts as lid over pharynx, prevents food from entering airway during swallowing � during inhalation epiglottis lifts up to let air pass over
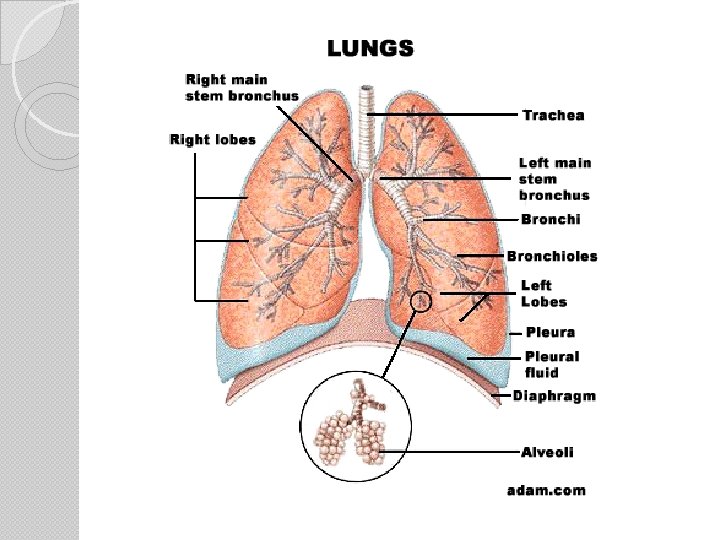
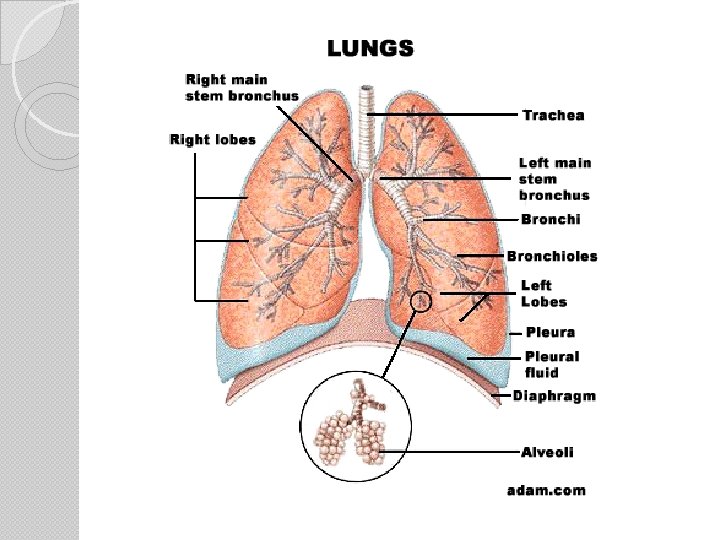
Respiratory System: Structure and Function cont… � trachea divides at lower end into right/left bronchus � each bronchus enters a lung � upon entering lung each bronchi divides many times into smaller branches called bronchioles � bronchioles eventually subdivide and end up in tiny onecelled air sacs called alveoli � alveoli look like small grape clusters, they are supplied by capillaries � O 2 and CO 2 are exchanged between the alveoli and capillaries � blood in capillaries picks up O 2 from alveoli, then blood is returned to the left side of heart and pumped to rest of body � alveoli pick up CO 2 from capillaries for exhalation


Respiratory System: Structure and Function cont… � lungs are spongy tissue � filled with alveoli, blood vessels and nerves � each lung is divided into lobes � right lung has 3 lobes � left lung has 2 lobes � lungs are separated from abdominal cavity by a muscle called the diaphragm � each lung is covered by a 2 -layered sac called the pleura � outer layer is attached to lung and other to the chest wall � pleura secretes a very thin fluid that fills the space between layers, fluid prevents the layers from rubbing together during inhaling/exhaling � ribs, sternum, vertebrae make up bony framework,
Respiratory System: Structure and Function cont… � respiratory tract, glands: tract fluids come from glands that line the mucous glands (goblet cells) and serous ◦ goblet cells: produce gel-like mucous that forms thin layer over inner surfaces of trachea, bronchioles. mucous secretion is caused by exposure to irritants (smoke, particles, bacteria) ◦ serous glands are controlled by cholinergic nervous system (ch. 14) when stimulated they secrete a watery fluid to the interior surface of the trachea, bronchi and bronchioles � secretions from both types of glands form respiratory tract fluid, this fluid forms a protective layer over trachea, bronchioles � foreign bodies are caught in fluid, swept upward by cilia
Respiratory System: Structure and Function cont… � the expectorated (coughed up) matter has pulmonary mucous secretions, foreign particles, and cells from the airway lining (coughed up matter called sputum, phlegm) � respiratory fluid can become thick and sticky and form mucous plugs (fig. 24 -3) � causes: ◦ cilia destroyed by chronic smoke inhalation ◦ dehydration dries the mucous ◦ anti-cholinergic agents inhibit water secretions from the serous glands (drying effect) � thick mucous plugs are hard to remove by coughing, microbes can grow in lower respiratory tract, this causes more secretions. Pneumonia can develop from trapped bacteria

Respiratory System: Structure and Function cont… � smooth muscles of trachea, bronchioles are controlled by ANS (parasympathetic and sympathetic systems) ◦ stimulation of cholinergic (parasympathetic) fibers causes bronchial constriction and increased mucous secretion ◦ stimulation of adrenergic (sympathetic) fibers causes dilation of the bronchi and bronchioles, mucus secretion decreases *see box 24 -2 pages 302 -303 for common respiratory disorders*
Delegation Guidelines Drugs Used to Treat Respiratory Diseases: Some drugs used to respiratory diseases are given parenterally- by subcutaneous, intramuscular or intravenous injection. Because you do NOT give parenteral dose forms, they are NOT included in this chapter. Should a nurse delegate the administration of such to you, you must: - remember that parenteral dosages are often very different from dosages other routes -Refuse the delegation. Make sure to explain why. Do NOT just ignore the request. Make sure the nurse knows that you cannot give
�Drug Therapy for Upper Respiratory Diseases: � antihistamines are drug of choice for allergic rhinitis: ◦ given orally and distributed through body ◦ reduce symptoms of nasal itching, sneezing, rhinorrhea, tearing and itchy eyes ◦ do NOT reduce nasal congestion � decongestants mucosa, cause vaso-constriction of nasal greatly reduces congestion � anti-inflammatory agents (p. 306) are given intranasally, used to treat nasal symptoms caused by mild-mod allergic rhinitis, not used to treat cold symptoms
Sympathomimetic Decongestants: stimulate the alpha adrenergic receptors of nasal mucous membranes � causes vaso-constriction, blood flow reduced to nasal area, sinus drainage is promoted � decongestants are drug of choice for relieving congestion from common cold and rhinitis � often given with antihistamines to: � ◦ reduce nasal congestion ◦ reduce sedation caused by antihistamines � oral and topical dose forms available (table 24 -1) � topical are nasal sprays/drops, no systemic effects, no NOT relieve other symptoms, can cause rhinitis medicamentosa � nasal decongestants provide temporary symptom relief, at first stuffiness is relieved and can ease breathing
Assisting With the Nursing Process Nasal Decongestants: ASSESSMENT: measure vital signs PLANNING: see table 24 -1 Pg. 305 for “Oral Dose Forms” IMPLEMENTATION: see table 24 -1 Pg. 305 for “Adult Dosage Range”, see ch. 12 for how to apply topical nose medications EVALUATION: report and record: - burning or stinging of nasal membranes: weaker solution may be needed - hypertension: may occur from excessive use, measure BP
Antihistamines: � compete with released histamine for receptor sites in arterioles, capillaries and glands in mucous membranes � do NOT prevent histamine release, they reduce symptoms of an allergic reaction if the amount of antihistamine is greater than the amount of histamine � antihistamines more effective if taken: ◦ before histamine is released ◦ when symptoms first appear � drugs of choice for treating allergic rhinitis and conjunctivitis � conjunctivitis is inflammation of eye tissues ◦ caused by bacterial or viral infections, allergies or environmental factors ◦ signs/symptoms: red eyelids, itching, thick discharge, sticky eyelids in morning
Antihistamines cont… � drugs reduce rhinorrhea, tearing, eye itching and sneezing � do NOT stop nasal congestion � best taken on a schedule for allergies � more effective if taken before exposure to allergen (4560 minutes before going outside during pollen season) � all anti-histamines have anti-cholinergic side effects: ◦ dilation of pupil, increased intraocular pressure in persons with glaucoma ◦ dry, thick secretions of mouth, nose, throat, bronchi ◦ decreased secretions and motility of GI tract ◦ increased heart rate ◦ decreased sweating � persons with asthma, prostate enlargement, glaucoma should only take antihistamines with medical supervision � goals of therapy: reduce sings/symptoms from allergic
Assisting With the Nursing Process Antihistamines: ASSESSMENT: observe for nasal congestion, measure intake/output PLANNING: see table 24 -2 Pg. 305 for “Oral Dose Forms” IMPLEMENTATION: see table 24 -2 Pg. 305 for “Adult Dosage Range” and “Maximum Daily Dose” EVALUATION: report and record: - sedation, cognitive impairment, memory problems, coordination problems: sedation most common side effect, tolerance may develop over time, provide for safety - drying effects: observe person’s cough and sputum production, because of drying effects anti-histamines may impair expectoration - blurred vision, constipation, urinary retention; mouth, throat, nose dryness: nurse may allow person to chew gum, suck on ice chips or hard candy. Provide safety
Respiratory Anti-Inflammatory Agents: �agents used to treat upper respiratory diseases: ◦ intra-nasal cortico-steroids ◦ cromolyn sodium (Nasalcrom) �intra-nasal cortico-steroids: �given to reduce inflammation �persons with allergic rhinitis who do not respond to other drugs may be given these �they help control nasal symptoms associated with mild-moderate allergic rhinitis �used for short courses of therapy for acute seasonal allergies �goals of therapy are to reduce: ◦ ◦ rhinorrhea rhinitis itching sneezing
Assisting With the Nursing Process intra-nasal cortico-steroids: ASSESSMENT: observe for nasal congestion PLANNING: see table 24 -3 Pg. 306 for “Oral Dose Forms” IMPLEMENTATION: see table 24 -3 Pg. 306 for “Adult Dosage Range” full therapeutic effect requires regular use, usually evident in a few days. Advise person to clear nasal passages before topical application. A decongestant may be ordered for use right before a topical corticosteroid, promotes adequate penetration EVALUATION: report and record: - nasal burning: usually mild and tends to resolve with continued therapy

cromolyn sodium (Nasalcrom): � anti-inflammatory agent � inhibits release of histamine and other substances of inflammation � to be effective, must be used before body receives a stimulus to release histamine � used with other drugs that prevent release of histamine � does NOT relieve nasal congestion � antihistamine or nasal decongestant may be needed when treatment is started � treatment is continued only if there is a decrease in symptoms � goals of therapy are to reduce: ◦ rhinorrhea ◦ itching ◦ sneezing
Assisting With the Nursing Process cromolyn sodium (Nasalcrom): ASSESSMENT: observe for nasal congestion PLANNING: dose forms: nasal spray: 40 mg/m. L in 13 m. L (gives 100 sprays), aerosol spray: 800 mcg from an 8. 1 g container (112 metered sprays), oral concentrate: 100 mg/5 m. L IMPLEMENTATION: adult dose: 1 spray in each nostril 34 x/day at regular intervals, maximum dose is 6 sprays in each nostril daily (2 -4 weeks for therapeutic effect to be evident), advise person to clear nasal passages of secretions before topical application EVALUATION: report and record: - nasal irritation- sneezing, itching, burning, stuffiness. Tolerance usually develops
Drug Therapy for Lower Respiratory Diseases: � expectorants: drugs that liquefy mucus to promote the ejection of mucus from lungs ◦ stimulate secretion of natural fluids from serous glands, flow of serous fluids helps liquefy thick mucous plugs ◦ ciliary action and coughing expel phlegm from respiratory system ◦ used to treat non-productive cough, bronchitis and pneumonia � antitussives (cough suppressants): drugs that suppress the cough center in brain ◦ used when person has a dry, hacking, non-productive cough ◦ cough is not stopped completely but should decrease frequency and suppress severe spasms that affect sleep
Drug Therapy for Lower Respiratory Diseases cont…. � brocho-dilators: trachea, drugs that relax smooth muscles of bronchi and bronchioles ◦ bronchiole and alveolar ducts open, which decreases resistance to airflow ◦ used to treat COPD ◦ anti-inflammatory agents- drugs that reduce inflammation, used for asthma. Cortico-steroids are most effective, commonly given by inhalation. � mucolytic agents: drugs that redcuce stickiness and thickness of pulmonary secretions ◦ act directly on mucous plugs to cause them to dissolve ◦ this eases the removal of secretions by cough, postural drainage, and suction ◦ agents used to treat acute/chronic respiratory disorders, before and after bronchoscopy, after chest surgery, and as part of tracheostomy care ◦ Muco-myst is often given by nebulizer (fig 24 -5, p. 308) Nebulizer is a device that produces a fine spray
Delegation Guidelines Drugs for Lower Respiratory Diseases: Many states and agencies do NOT let the MA-C’s give drugs by nebulizer. If allowed to do so, make sure you receive the necessary education and training. Also make sure that a nurse is available to supervise your work.
Drug Therapy for Lower Respiratory Diseases. . . Expectorants: � the following expectorants are used to treat lower respiratory diseases: ◦ guaifenesin (Robitussing) ◦ postassium iodide (SSKI) � guaifenesin (Robitussin) � enhances output of respiratory tract fluid � increased flow of secretions decreases mucous thickness and promotes ciliary action (ciliary action and coughing expel phlegm from respiratory tract) � used to relieve dry, non-productive cough and to remove mucous plugs � often used with broncho-dilators, decongestants, antihistamines or antitussive agents to make a nonproductive cough productive � goal of therapy is to reduce the frequency of nonproductive cough
Assisting With the Nursing Process guaifenesin (Robitussin): ASSESSMENT: note persons cough: productive or nonproductive; what is color, consistency, amount and appearance of sputum PLANNING: oral dose forms: 100, 200, 400, 600 mg tablets 200 mg capsules 100 and 200 mg/5 m. L liquid IMPLEMENTATION: adult dose: is 100 -400 mg every 4 -6 hours, dose should not exceed 2400 mg per day. Person should drink 8 -12 8 oz glasses of water daily EVALUATION: report and record: - GI upset, nausea, vomiting: side effects are rare

Drug Therapy for Lower Respiratory Diseases. . . potassium iodide (SSKI): � stimulates increased secretion from bronchial glands � this decreases thickness of mucous plugs � easier for person to cough up dry, hardened plugs blocking bronchial tubes � used in treatment of COPD when thick mucous is present, often used with other drugs to remove mucous � goals of therapy: ◦ reduce thickness of mucous ◦ allow a more productive cough to remove phlegm

Assisting With the Nursing Process potassium iodide(SSKI): ASSESSMENT: note persons cough: productive or nonproductive; what is color, consistency, amount and appearance of sputum PLANNING: oral dose forms: solution: 1 g/m. L I 30, 240 and 480 m. L containers syrup: 325 mg/5 m. L in 480 m. L containers IMPLEMENTATION: adult dosage: solution: 0. 3 m. L (300 mg) to 0. 6 m. L (600 mg) diluted in one glassful of water, juice or milk, 3 -4 x/day syrup: 5 -10 m. L 3 x/day, give with food/milk person should drink 8 -12 8 oz glasses of water/day EVALUATION: report and record: - nausea, vomiting, diarrhea: usually mild, give with food or milk to help gastric irritation
Antitussives: � cough suppressants, depress the cough center in brain � codeine is an effective cough suppressant � low-dose, short-term use for a cough should not produce addiction � goal of therapy: reduce frequency of a non-productive cough
Assisting With the Nursing Process antitussives: ASSESSMENT: note persons cough: productive or non-productive; what is color, consistency, amount and appearance of sputum PLANNING: see table 24 -4 (p. 309) for “oral dose forms: IMPLEMENTATION: see table 24 -4 (p. 309) for “Adult Oral Dosage Range” Benzonatate must be swallowed whole, drug numbs the tongue if chewed or crushed. Creates a choking hazard EVALUATION: report and record: - drowsiness, sedation: provide for safety - constipation: codeine is most constipating of antitussives, give stool softeners as ordered, follow care plan for fluid intake
Beta-Adrenergic Broncho-Dilating Agent: � relax smooth muscles of trachea, bronchioles � opens airways to greater amounts of air � drugs used to reverse airway constriction caused by acute and chronic asthma, bronchitis and emphysema � drugs have many side effects, because they stimulate receptors in heart, blood vessels, uterus, GI, urinary and central nervous systems � those given by inhalation usually have fewer side effects (lower doses are used, drug placed at site of action) � goals of therapy: ◦ ease breathing ◦ reduce wheezing
Assisting With the Nursing Process Beta-Adrenergic Broncho-Dilating Agent: ASSESSMENT: measure vitals, note pulse rate and rhythm, observe for confusion and orientation to person, time and place PLANNING: see table 24 -5 (p. 310) for “oral dose forms: IMPLEMENTATION: see table 24 -5 (p. 310) for “Adult Oral Dosage Range” person waits at least 10 minutes between inhalations, allows drug to dilate the bronchioles. The 2 nd dose can be inhaled more deeply into lungs, follow manufacturers instructions EVALUATION: report and record: - tachycardia, palpitations: dose related, measure heart rate and rhythm, report an increase of 20 beats or more per minute after a treatment. Report dysrhythmias and palpitations - tremors: dosage may need adjusted - nervousness, anxiety, restlessness, headache - nausea, vomiting: give drug with food and full glass of water - dizziness: provide for safety

Anti-Cholinergic Broncho-Dilating Agent: � 2 agents: ◦ ipratropium bromide (Atrovent, Atrovent HFA) ◦ tiotropium bromide (Spiriva) ipratropium bromide (Atrovent, Atrovent HFA): � act on bronchial smooth muscle � produce bronchodilation � used for long-term treatment of broncho-spasm associated with COPD � initial effect seen within first few minutes after inhaled � broncho-dilation lasts for 4 -6 hours � nasal spray used for rhinorrhea from rhinitis and common cold � does NOT relieve nasal congestion, sneezing or postnasal drip � goals of therapy: ◦ ease breathing (dose metered inhaler) ◦ reduce rhinorrhea (nasal spray)
Assisting With the Nursing Process ipratropium bromide (Atrovent, Atrovent HFA): ASSESSMENT: measure vitals PLANNING: aerosol canister: 18 mcg/metered dose inhaler (200 inhalations) nasal spray pumps: 0. 03% (21 mcg/spray) or 0. 06% (42 mcg/spray) IMPLEMENTATION: inhalation: usual dose is 2 inhalations 4 x/day, additional inhalations may be taken as required, should not exceed 12 inhalations in 24 hours. nasal spray: for rhinitis 2 sprays of a 0. 3% solution in each nostril 2 -3 x/day; for common cold 2 sprays of 0. 6% solution in each nostril 3 -4 x/day EVALUATION: report and record: - tachycardia, urinary retention, worsening of respiratory symptoms - mouth dryness, throat irritation: usually mild and tend to resolve with continued therapy. Provide oral hygiene, nurse may allow hard candy or ice chips

tiotropium bromide (Spiriva) • • • given by dry powder inhalation causes bronchial smooth muscles to relax, resulting in broncho-dilation drug used as a once-daily broncho-dilator to treat broncho- spasm associated with COPD. broncho-dilating effect does NOT happen at once, therefore the drug is used for maintenance treatment goal of therapy: easier breathing with less effort
Assisting With the Nursing Process tiotropium bromide (Spiriva): ASSESSMENT: measure vitals PLANNING: inhalation dose form is 18 mcg capsules for use in supplied Handi. Haler IMPLEMENTATION: usual dose is 1 capsule daily given through the Handi. Haler. EVALUATION: report and record: - tachycardia, urinary retention, worsening of respiratory symptoms - mouth dryness, throat irritation: usually mild and tend to resolve with continued therapy. Provide oral hygiene, nurse may allow hard candy or ice chips
Xanthine-Derivative Broncho-Dilating Agents: � act directly on the smooth muscle of the trachea, bronchi and bronchioles, to dilate the bronchi � increased the airflow in and out of alveoli � used with sympathomimetic broncho-dilators to reverse airway constriction caused by COPD � goal of therapy: breathing with less effort
Assisting With the Nursing Process Xanthine-Derivative Broncho-Dilating Agents: ASSESSMENT: measure vitals, note heart rate and rhythm, observe orientation to person, time and place. Observe for anxiety and nervousness. PLANNING: see table 24 -5 (pg. 310) for “Dose Forms” IMPLEMENTATION: see table 24 -5 (pg. 310) for “Adult Dosage Range” EVALUATION: report and record: - nausea, vomiting, epigastric pain, abdominal cramps. These occur from irritation caused by the stimulation of gastric acid secretion. Give drug with food/milk. - tachycardia, palpitations: usually dose related, measure heart rate and rhythm - tremors: a dosage adjustment may be needed - nervousness, anxiety, restlessness, headache: observe for changes in mental status
Respiratory Anti-inflammatory Agents: � cortico-steroids are given to reduce inflammation (ch. 28) � highly effective in treating COPD � they: ◦ relax smooth muscles ◦ enhance effects of beta-adrenergic broncho-dilators ◦ inhibit inflammatory responses that may cause bronchoconstriction � agents may be added to a dry therapy program if person does not respond to other broncho-dilators � goal of therapy: easier breathing with less effort
Assisting With the Nursing Process inhalant cortico-steroids: ASSESSMENT: observe mouth for signs/symptoms of infection PLANNING: see table 24 -6 (pg. 312) for “Inhalant Dose Forms” IMPLEMENTATION: see table 24 -6 (pg. 312) for “Adult Dosage Range”. Full therapeutic effect requires regular use, usually evident within a few days. Persons receiving broncho-dilators by inhalation should use them before the cortico-steroid inhalant. , this enhances inhalation. EVALUATION: report and record: - hoarseness, dry mouth: usually mild and tend to resolve with continued therapy - signs and symptoms of mouth infection: Provide oral hygiene. Follow care plan for using a mouthwash

Anti-Leukotriene Agents: � inflammatory cells are in the membrane lining the airway � a series of chemical reactions occur when the inflammatory cells are triggered by irritants � irritants include: smoke, allergens and viruses � one reaction is the release of leukotrienes � Leukotrienes are substances in the white blood cells. White blood cells are called leukocytes � leukotrienes produce allergic and inflammatory reactions similar to histamine � they produce many signs/symptoms of asthma (box 242) � these are anti-leukotriene agents: ◦ montelukast (Singulair) ◦ zafirlukast (Accolate)
montelukast (Singulair): � competes � it for receptor sites that trigger asthma symptoms reduces: ◦ broncho-constriction ◦ daytime asthma symptoms ◦ night-time awakening � goal of therapy: fewer episodes of acute asthma symptoms Assisting With the Nursing Process montelukast (Singulair): ASSESSMENT: measure vital signs PLANNING: oral dose forms: 5 and 10 mg tablets, 4 mg chewables, 4 mg granules IMPLEMENTATION: adult dose is 10 mg give once daily in the evening EVALUATION: report and record: - headache, nausea, indigestion: usually mild and resolve, give drug with food or milk
zafirlukast (Accolate): � competes for receptor sites that trigger symptoms of asthma � helps to reduce: ◦ broncho-constriction ◦ daytime asthma symptoms ◦ night-time awakening � goal of therapy: fewer episodes of acute asthma symptoms Assisting With the Nursing Process zafirlukast (Accolate): ASSESSMENT: measure vital signs PLANNING: oral dose forms 20 mg tablets IMPLEMENTATION: adult dose is 20 mg, 2 x/day EVALUATION: report and record: - headache, nausea: usually mild and resolve, give drug
 Boundaries meme
Boundaries meme Respiratory system
Respiratory system Global alliance against chronic respiratory diseases
Global alliance against chronic respiratory diseases What is the conducting zone of the respiratory system
What is the conducting zone of the respiratory system Pharmacology of drugs acting on respiratory system
Pharmacology of drugs acting on respiratory system Which seedless plants have been used to treat bee stings
Which seedless plants have been used to treat bee stings Is byetta used to treat pcos
Is byetta used to treat pcos Which seedless plants have been used to treat burns?
Which seedless plants have been used to treat burns? Chapter 24 lesson 1 sexually transmitted diseases
Chapter 24 lesson 1 sexually transmitted diseases Chapter 8 skin disorders and diseases review questions
Chapter 8 skin disorders and diseases review questions Chapter 6 musculoskeletal system diseases and disorders
Chapter 6 musculoskeletal system diseases and disorders Chapter 32 childhood communicable diseases bioterrorism
Chapter 32 childhood communicable diseases bioterrorism Chapter 24 sexually transmitted diseases and hiv/aids
Chapter 24 sexually transmitted diseases and hiv/aids Sarophytes
Sarophytes Chapter 22 genetics and genetically linked diseases
Chapter 22 genetics and genetically linked diseases Chapter 21 mental health diseases and disorders
Chapter 21 mental health diseases and disorders Chapter 17 reproductive system diseases and disorders
Chapter 17 reproductive system diseases and disorders Chapter 15 nervous system diseases and disorders
Chapter 15 nervous system diseases and disorders Chapter 8 skin disorders and diseases
Chapter 8 skin disorders and diseases 8 common nail disorders
8 common nail disorders Onychomycosis milady
Onychomycosis milady Cardiovascular system diseases and disorders chapter 8
Cardiovascular system diseases and disorders chapter 8 Milady chapter 8 skin disorders and diseases
Milady chapter 8 skin disorders and diseases Chapter 23 lesson 1 understanding communicable diseases
Chapter 23 lesson 1 understanding communicable diseases Chapter 10 lymphatic system diseases and disorders
Chapter 10 lymphatic system diseases and disorders Eva tray in labour room
Eva tray in labour room Drugs used in pregnancy
Drugs used in pregnancy What do the words that appeared on cyrus's tomb
What do the words that appeared on cyrus's tomb Equation for number needed to treat
Equation for number needed to treat Invitation to treat
Invitation to treat Romeo and juliet act 4 summary
Romeo and juliet act 4 summary Number needed to treat calculation
Number needed to treat calculation Offer
Offer How to treat laryngopharyngeal reflux
How to treat laryngopharyngeal reflux How to calculate number needed to treat
How to calculate number needed to treat Nnt calculation
Nnt calculation Relative risk reduction
Relative risk reduction Number needed to treat
Number needed to treat Guthing vs lynn case
Guthing vs lynn case Number needed to harm formula
Number needed to harm formula Powell v kempton park racecourse
Powell v kempton park racecourse Treat everyone with sincerity
Treat everyone with sincerity Summary of act 2 scene 4 of romeo and juliet
Summary of act 2 scene 4 of romeo and juliet Treat with sincerity
Treat with sincerity Social facilitation vs social loafing
Social facilitation vs social loafing Mole day treat ideas
Mole day treat ideas How to treat bursitis in the hip
How to treat bursitis in the hip Treat others the way you would like to be
Treat others the way you would like to be Treat with confidence
Treat with confidence