Death pronouncement and certification The final medical act

![Special issues Avoided diagnoses • • Suicide [automatic ME case] AIDS Tuberculosis Drug/alcohol abuse Special issues Avoided diagnoses • • Suicide [automatic ME case] AIDS Tuberculosis Drug/alcohol abuse](https://slidetodoc.com/presentation_image_h2/57b12ed3b0c19edafaedcc749dc77ec0/image-20.jpg)

- Slides: 55
Death pronouncement and certification The final medical act May 6, 2009 Lee Buenconsejo-Lum, MD Residency Program Director Department of Family Medicine and Community Health John A. Burns School of Medicine University of Hawaii
Overview l l l Pronouncing death Purpose and usage of mortality data Common errors Implications for inaccurate death certificate Case examples
What to do when you’re the on-call resident PRONOUNCING DEATH
Pronouncing death l Pronouncement of death is defined as the opinion or determination that, based on a physical assessment, life has ceased. l Pronouncing a death is a series of events that include examining patients to determine death, notifying families and in recording proper documentation of a death.
Prior to pronouncing death l l l Interview the nurse/nursing staff to get details about the patient, family dynamics and the circumstances of the death. Review the chart and any prior family meetings / discussions Determine if there any special problems or concerns.
Prior to pronouncing death l Assess the immediate situation l Was the death expected or unexpected? l Was the family present? If not have they been notified?
Prior to pronouncing death l Find out about autopsy and organ donation l Has family requested an autopsy? Is there an indication for an autopsy? l Unexplained death l Death within 24 hours of admission (Medical Examiner) l Death within 24 hours of surgery or invasive procedure l Suicide / homicide (Medical Examiner) l What is the cost of autopsy? l Is the patient an organ donor? If not, has family considered organ donation?
Medical Examiner (ME) cases l l l Suicide / homicide Certain injuries and accidents Death within 24 hours of admission to hospital Do not remove any lines, ETT, foley You still should speak with the family and let them know that the final determination will be done by the Medical Examiner Give family time to bereave with the body before transport to morgue
Prior to pronouncing death l Determine the patient and/or family's faith or spiritual tradition l Has the family's faith-base support person been notified? l Are there any special faith or cultural procedures (autopsy, embalming, and preparation of the body), rituals or traditions that the family would like to observe with the patient?
Pronouncing death l If family is present, introduce yourself, express sympathy, see if they have any questions l l Hopefully the primary resident or attending physician has explained and communicated well and checked for understanding May have new family members present who have not heard the prior explanations
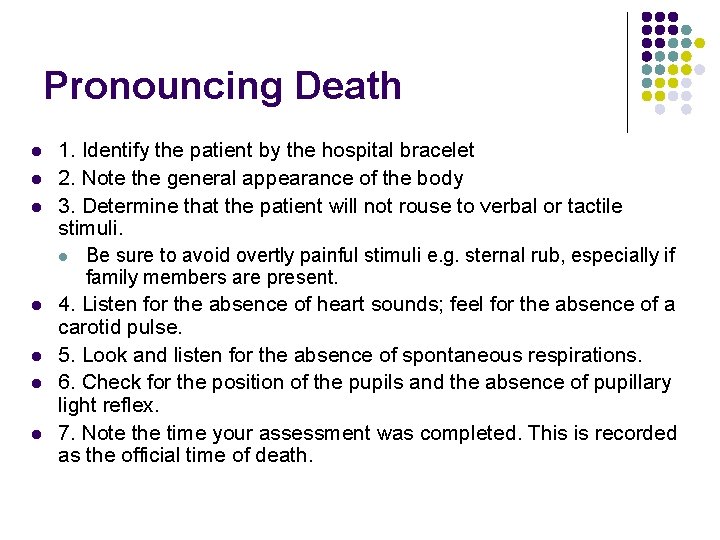
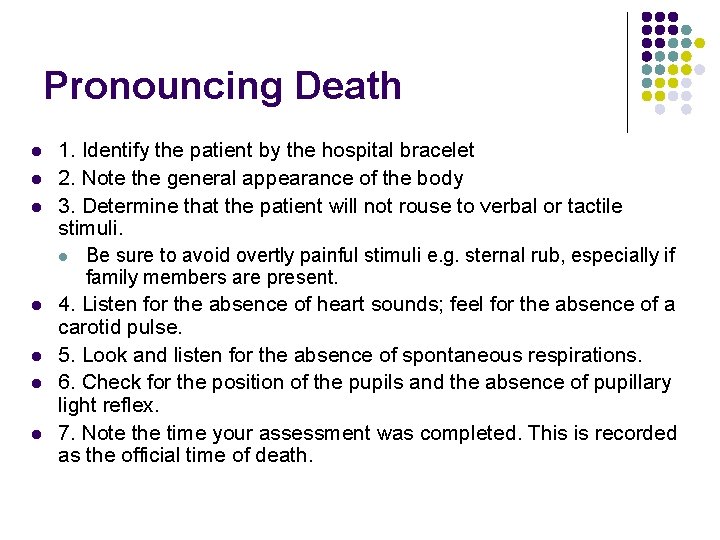
Pronouncing Death l l l l 1. Identify the patient by the hospital bracelet 2. Note the general appearance of the body 3. Determine that the patient will not rouse to verbal or tactile stimuli. l Be sure to avoid overtly painful stimuli e. g. sternal rub, especially if family members are present. 4. Listen for the absence of heart sounds; feel for the absence of a carotid pulse. 5. Look and listen for the absence of spontaneous respirations. 6. Check for the position of the pupils and the absence of pupillary light reflex. 7. Note the time your assessment was completed. This is recorded as the official time of death.
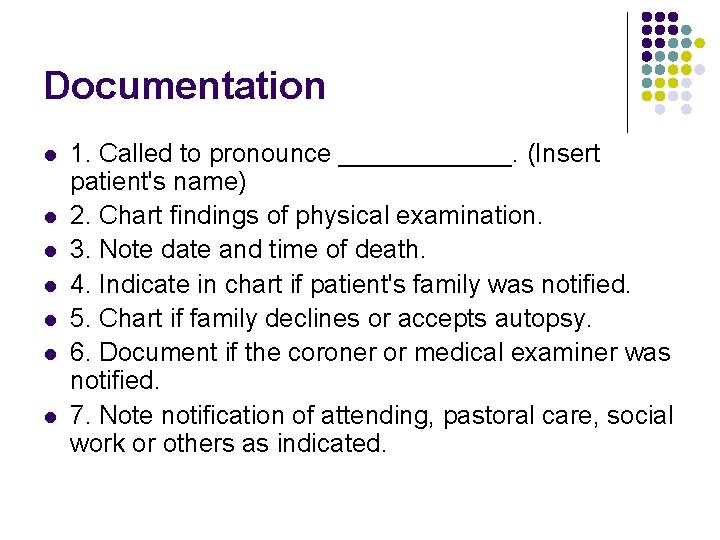
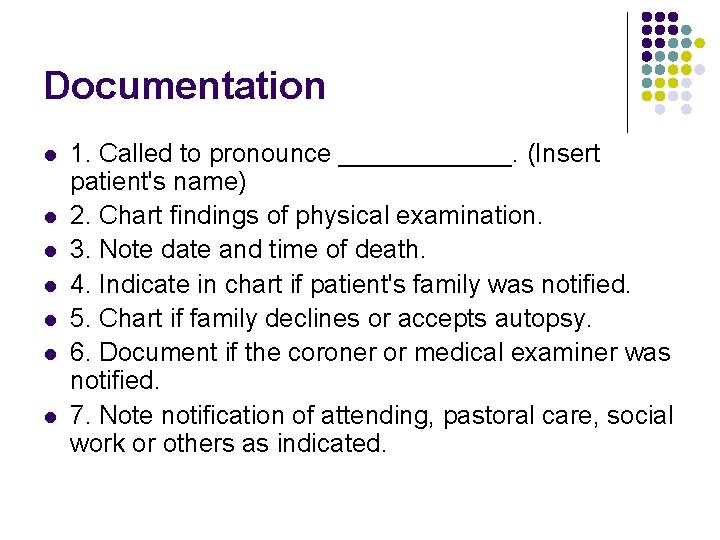
Documentation l l l l 1. Called to pronounce ______. (Insert patient's name) 2. Chart findings of physical examination. 3. Note date and time of death. 4. Indicate in chart if patient's family was notified. 5. Chart if family declines or accepts autopsy. 6. Document if the coroner or medical examiner was notified. 7. Note notification of attending, pastoral care, social work or others as indicated.
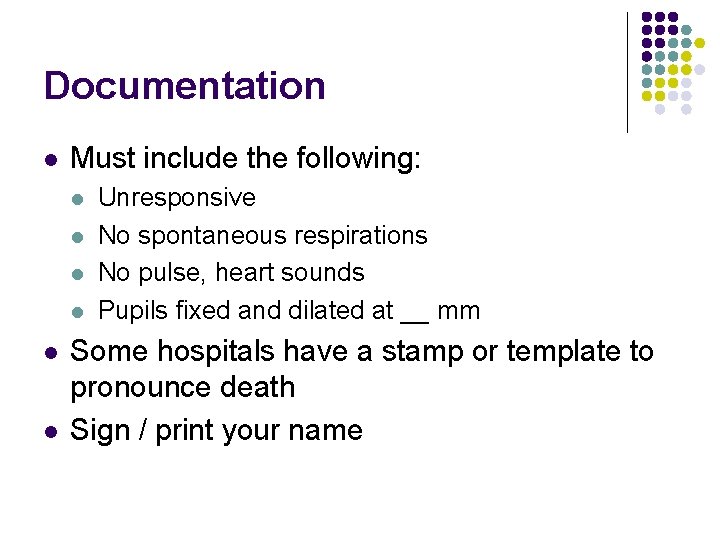
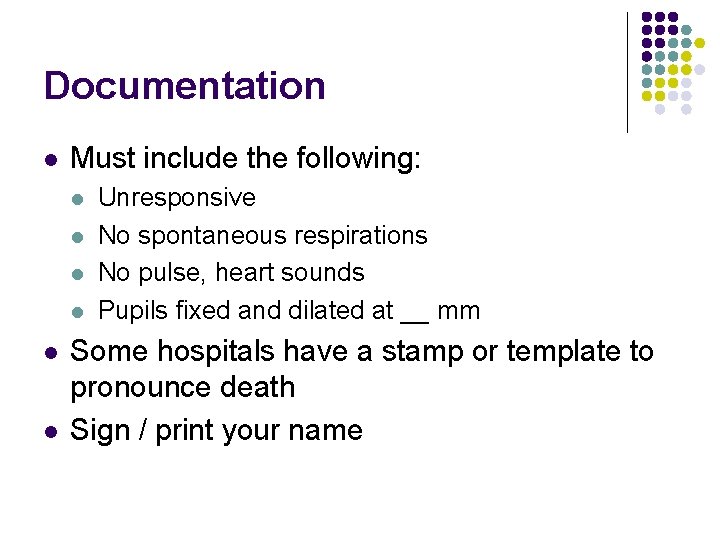
Documentation l Must include the following: l l l Unresponsive No spontaneous respirations No pulse, heart sounds Pupils fixed and dilated at __ mm Some hospitals have a stamp or template to pronounce death Sign / print your name
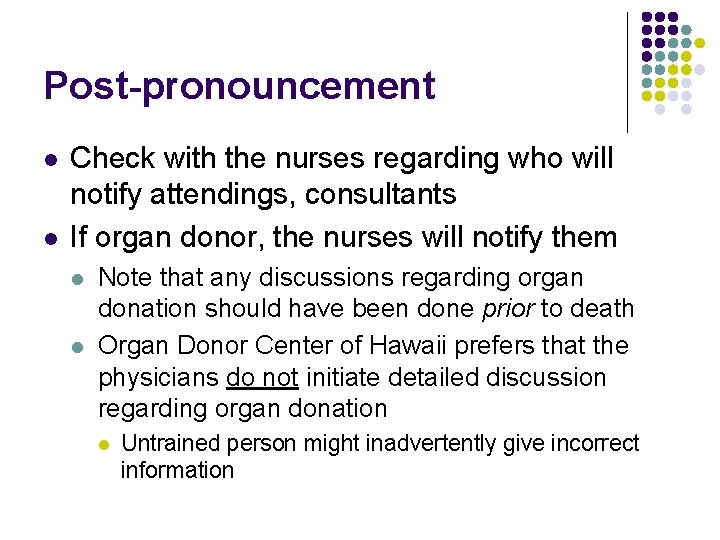
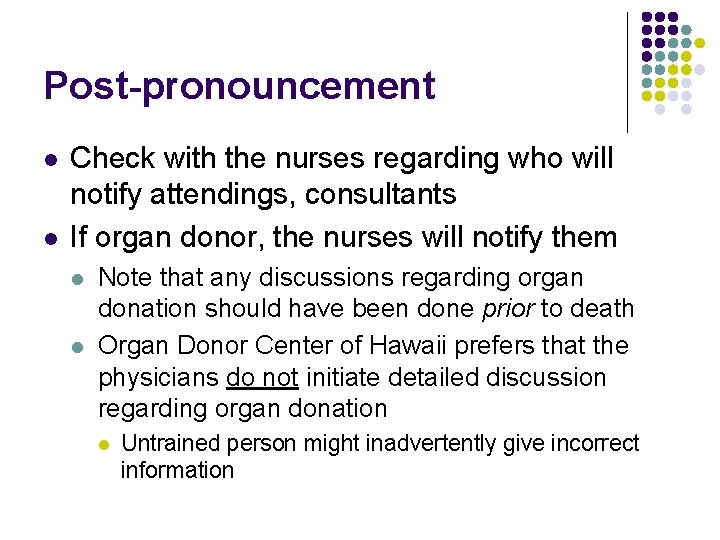
Post-pronouncement l l Check with the nurses regarding who will notify attendings, consultants If organ donor, the nurses will notify them l l Note that any discussions regarding organ donation should have been done prior to death Organ Donor Center of Hawaii prefers that the physicians do not initiate detailed discussion regarding organ donation l Untrained person might inadvertently give incorrect information
Post-pronouncement l l Update your sign-out sheet If you’re the primary resident and have time, dictate the death (discharge) summary l l l Final diagnosis Additional diagnosis Reason for admission Hospital course by problem Pronouncement note and time of death

Why is this important DEATH CERTIFICATION
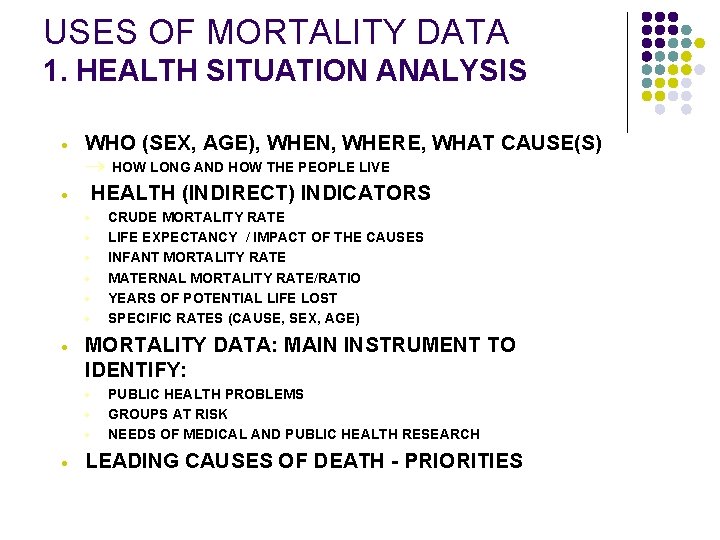
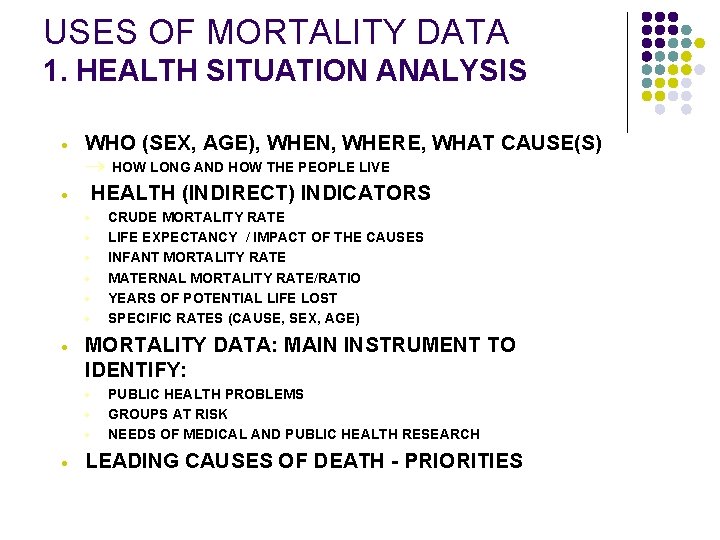
USES OF MORTALITY DATA 1. HEALTH SITUATION ANALYSIS · · WHO (SEX, AGE), WHEN, WHERE, WHAT CAUSE(S) ® HOW LONG AND HOW THE PEOPLE LIVE HEALTH (INDIRECT) INDICATORS · · · · MORTALITY DATA: MAIN INSTRUMENT TO IDENTIFY: · · CRUDE MORTALITY RATE LIFE EXPECTANCY / IMPACT OF THE CAUSES INFANT MORTALITY RATE MATERNAL MORTALITY RATE/RATIO YEARS OF POTENTIAL LIFE LOST SPECIFIC RATES (CAUSE, SEX, AGE) PUBLIC HEALTH PROBLEMS GROUPS AT RISK NEEDS OF MEDICAL AND PUBLIC HEALTH RESEARCH LEADING CAUSES OF DEATH - PRIORITIES
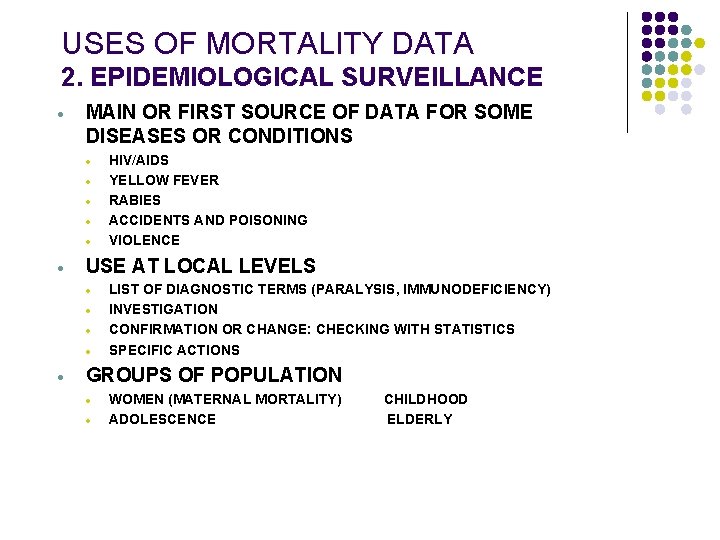
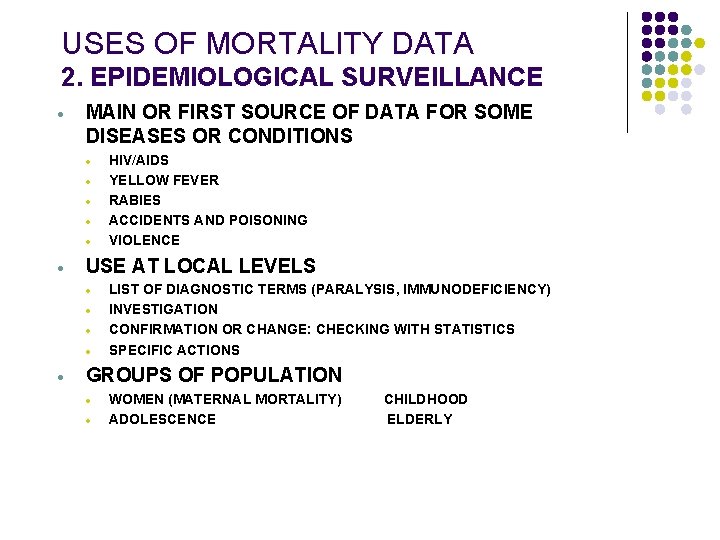
USES OF MORTALITY DATA 2. EPIDEMIOLOGICAL SURVEILLANCE · MAIN OR FIRST SOURCE OF DATA FOR SOME DISEASES OR CONDITIONS · · · USE AT LOCAL LEVELS · · · HIV/AIDS YELLOW FEVER RABIES ACCIDENTS AND POISONING VIOLENCE LIST OF DIAGNOSTIC TERMS (PARALYSIS, IMMUNODEFICIENCY) INVESTIGATION CONFIRMATION OR CHANGE: CHECKING WITH STATISTICS SPECIFIC ACTIONS GROUPS OF POPULATION · · WOMEN (MATERNAL MORTALITY) ADOLESCENCE CHILDHOOD ELDERLY
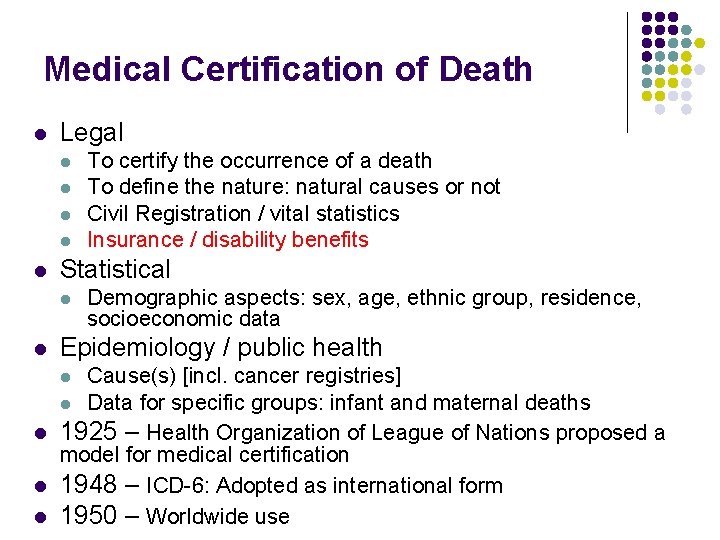
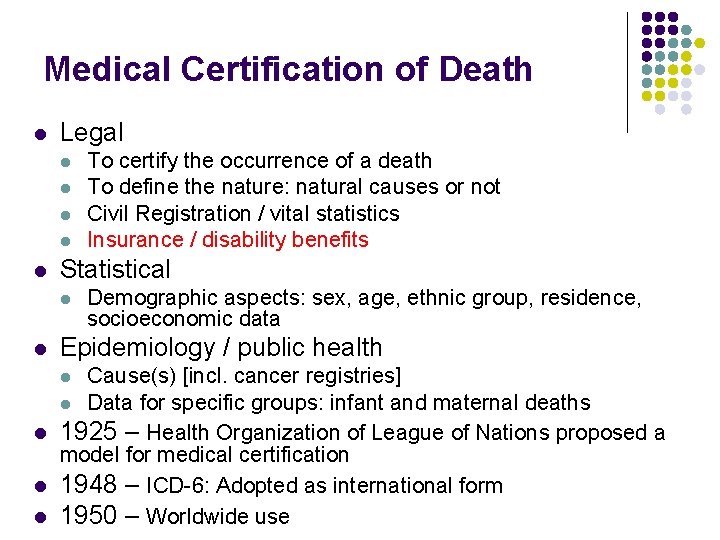
Medical Certification of Death l Legal l l Statistical l l To certify the occurrence of a death To define the nature: natural causes or not Civil Registration / vital statistics Insurance / disability benefits Demographic aspects: sex, age, ethnic group, residence, socioeconomic data Epidemiology / public health Cause(s) [incl. cancer registries] l Data for specific groups: infant and maternal deaths l 1925 – Health Organization of League of Nations proposed a model for medical certification l 1948 – ICD-6: Adopted as international form l 1950 – Worldwide use l
![Special issues Avoided diagnoses Suicide automatic ME case AIDS Tuberculosis Drugalcohol abuse Special issues Avoided diagnoses • • Suicide [automatic ME case] AIDS Tuberculosis Drug/alcohol abuse](https://slidetodoc.com/presentation_image_h2/57b12ed3b0c19edafaedcc749dc77ec0/image-20.jpg)
Special issues Avoided diagnoses • • Suicide [automatic ME case] AIDS Tuberculosis Drug/alcohol abuse Manipulation of information (e. g. homicides, dengue) Injuries and poisoning [automatic ME case] Cardiac arrest infarction ? Incomplete and imprecise information • • • Information on pregnancy Pneumonia (etiology / terminal) Infarction (acute or old / of the myocardium) Endocarditis (acute or chronic / valve / rheumatic ? ) Senility / signs & symptoms ARI
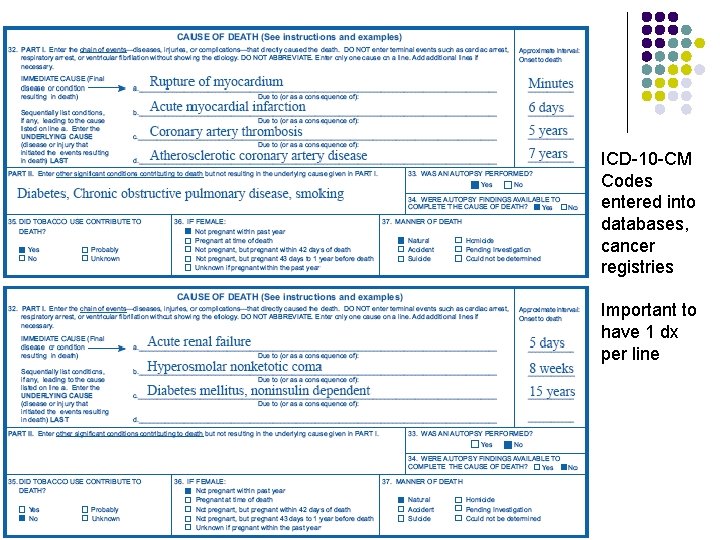
Medical certification Full information required, not only causes of death Sequence • • • “a” due to “b” due to “c” due to “d” Part I / Part II ONE Diagnosis per line Use of Abbreviations (no!) • ARI, MI, etc. Handwriting !
Death certificates – avoiding common errors l Do not delay completion l l l l Make a copy / notation of cause of death from the inpatient chart (at the time of death) Give to the attending The final death certificate comes days later to the office Do not use abbreviations Spell out the month, do not use numbers Do not alter the document, erase, white out Print clearly or type, using black ink
Causality of death l l Sequential chain of events that led to death Time interval between onset of a condition and death l l Ok to state approximately, “minutes”, “hours”, “days” Part II. Significant conditions that contributed to death but that did not result in the underlying cause of death l Avoid laundry lists
Causality l l l DO NOT WRITE THE MECHANISM OF DEATH (see handouts) Mechanism is not helpful for public health purposes Medical judgment is required when picking the best alternative for writing the cause-ofdeath statement. Truthfulness, completeness, and reasonable accuracy should be the goal
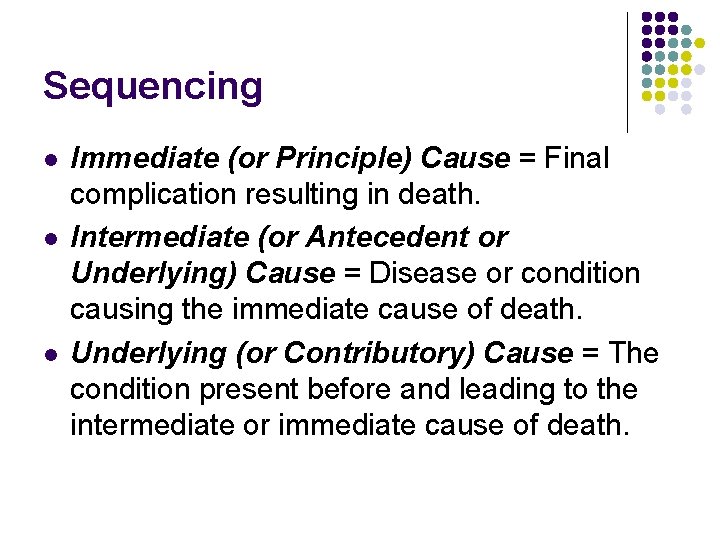
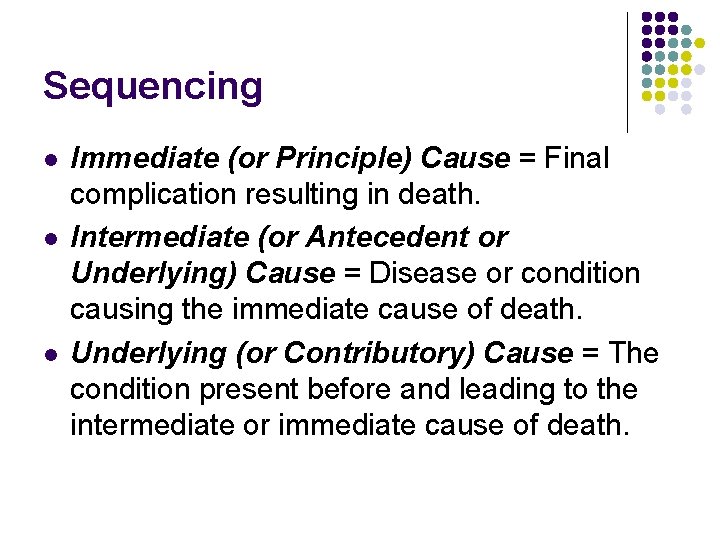
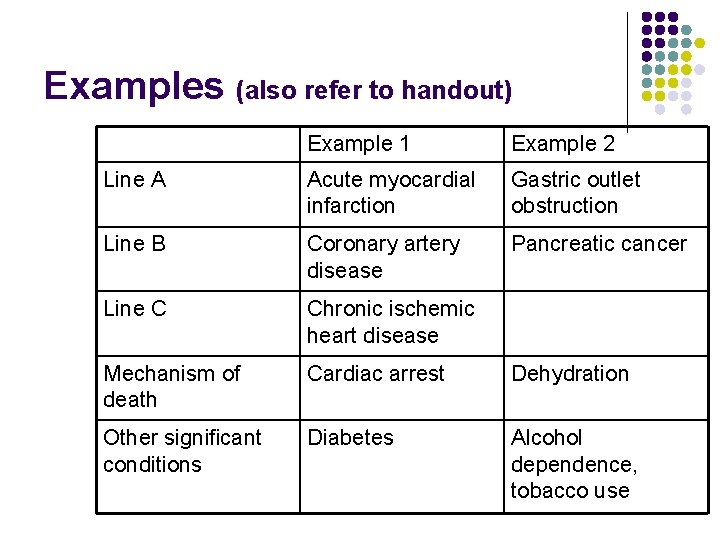
Sequencing l l l Immediate (or Principle) Cause = Final complication resulting in death. Intermediate (or Antecedent or Underlying) Cause = Disease or condition causing the immediate cause of death. Underlying (or Contributory) Cause = The condition present before and leading to the intermediate or immediate cause of death.
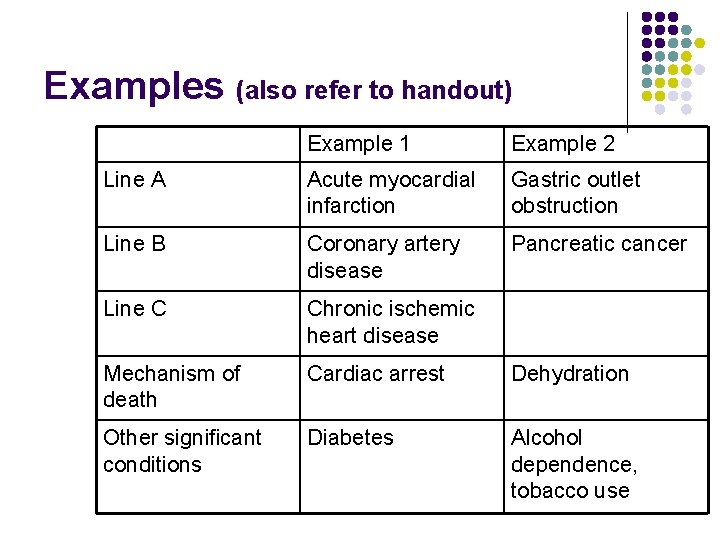
Examples (also refer to handout) Example 1 Example 2 Line A Acute myocardial infarction Gastric outlet obstruction Line B Coronary artery disease Pancreatic cancer Line C Chronic ischemic heart disease Mechanism of death Cardiac arrest Dehydration Other significant conditions Diabetes Alcohol dependence, tobacco use
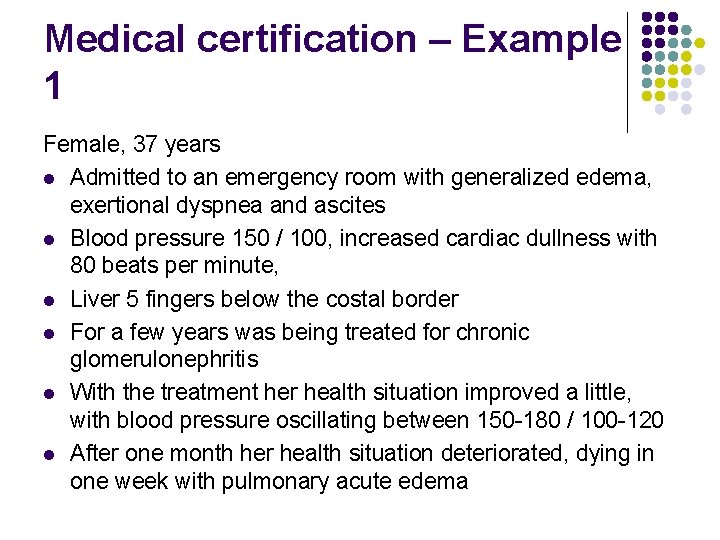
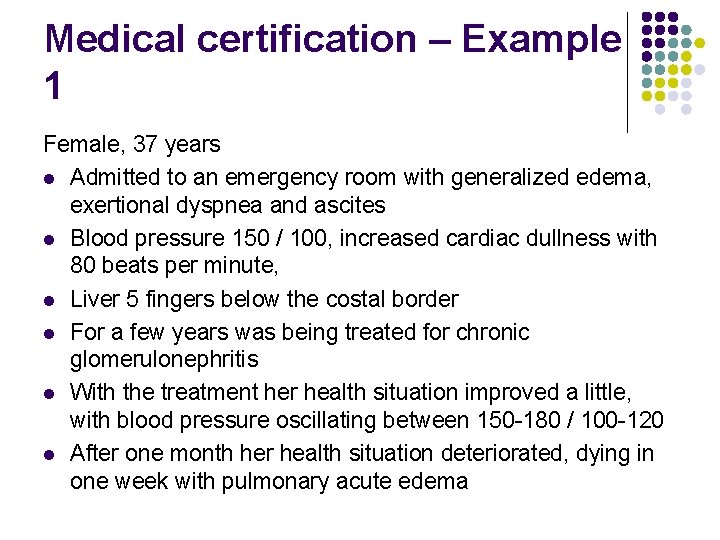
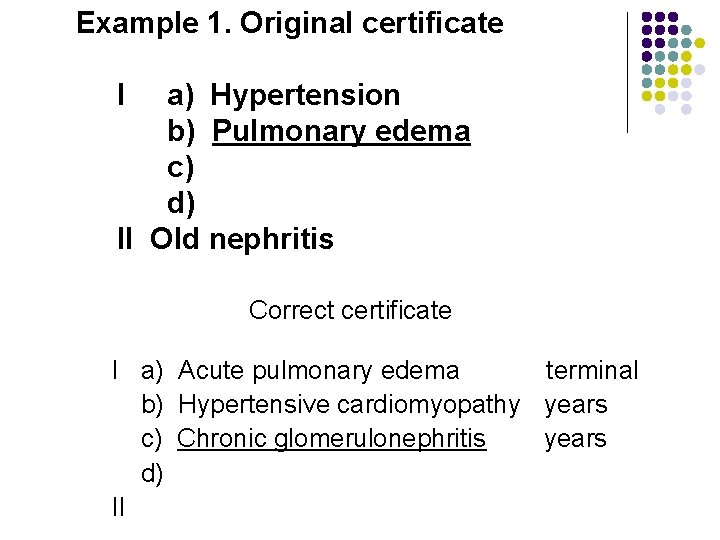
Medical certification – Example 1 Female, 37 years l Admitted to an emergency room with generalized edema, exertional dyspnea and ascites l Blood pressure 150 / 100, increased cardiac dullness with 80 beats per minute, l Liver 5 fingers below the costal border l For a few years was being treated for chronic glomerulonephritis l With the treatment her health situation improved a little, with blood pressure oscillating between 150 -180 / 100 -120 l After one month her health situation deteriorated, dying in one week with pulmonary acute edema
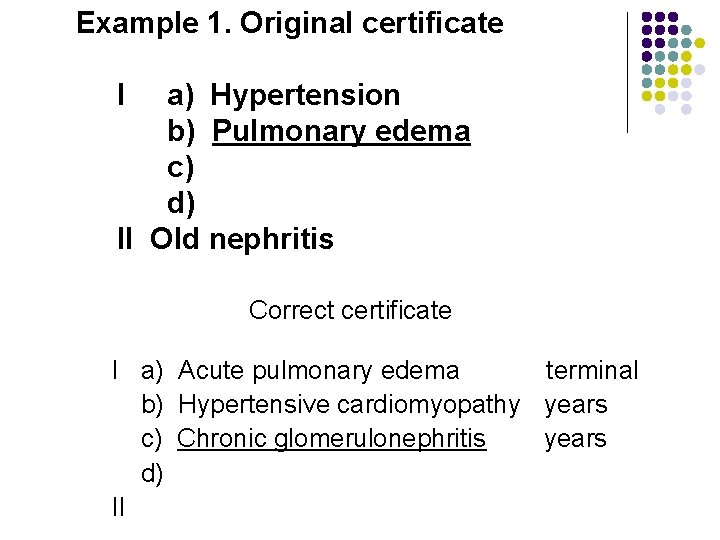
Example 1. Original certificate I a) Hypertension b) Pulmonary edema c) d) II Old nephritis Correct certificate I a) Acute pulmonary edema terminal b) Hypertensive cardiomyopathy years c) Chronic glomerulonephritis years d) II
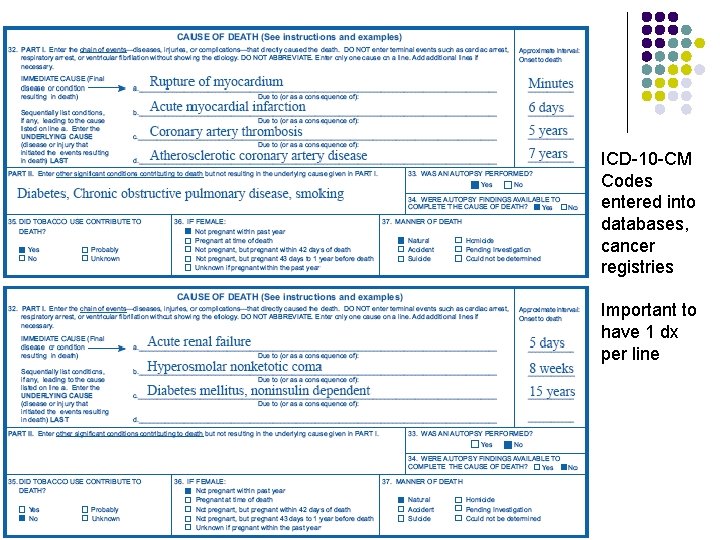
ICD-10 -CM Codes entered into databases, cancer registries Important to have 1 dx per line
Final thoughts (before the cases) l The cause of death statement is l l Your best opinion Is not set in stone Can be changed Poses little legal risk

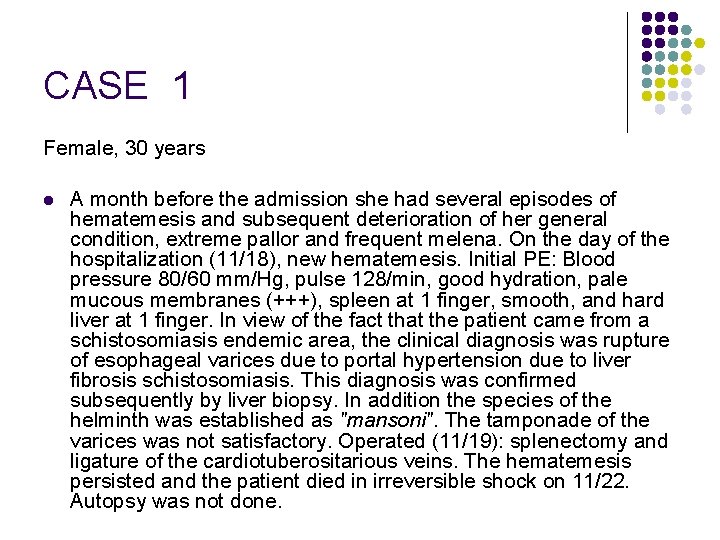
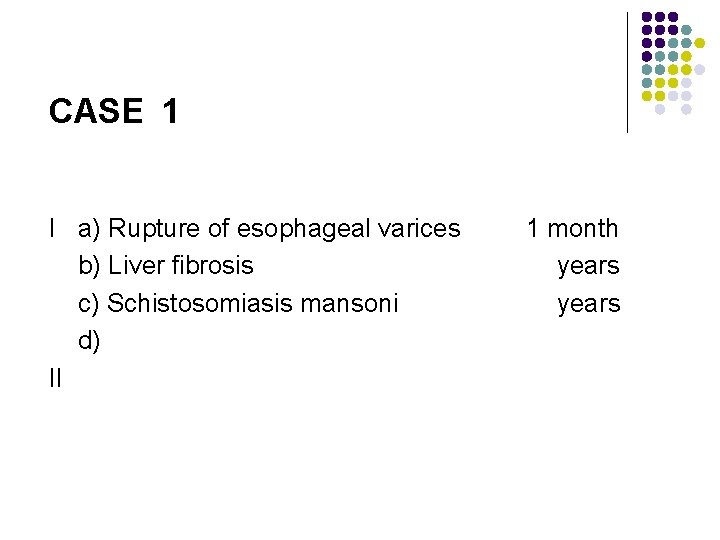
CASE 1 Female, 30 years l A month before the admission she had several episodes of hematemesis and subsequent deterioration of her general condition, extreme pallor and frequent melena. On the day of the hospitalization (11/18), new hematemesis. Initial PE: Blood pressure 80/60 mm/Hg, pulse 128/min, good hydration, pale mucous membranes (+++), spleen at 1 finger, smooth, and hard liver at 1 finger. In view of the fact that the patient came from a schistosomiasis endemic area, the clinical diagnosis was rupture of esophageal varices due to portal hypertension due to liver fibrosis schistosomiasis. This diagnosis was confirmed subsequently by liver biopsy. In addition the species of the helminth was established as "mansoni". The tamponade of the varices was not satisfactory. Operated (11/19): splenectomy and ligature of the cardiotuberositarious veins. The hematemesis persisted and the patient died in irreversible shock on 11/22. Autopsy was not done.
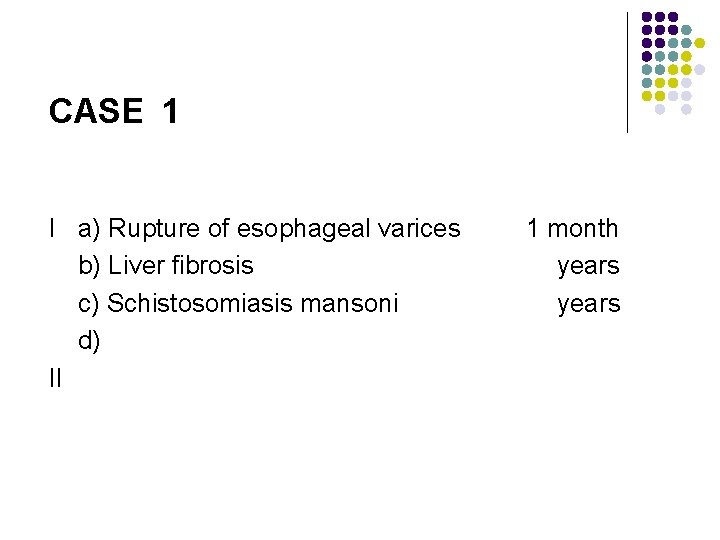
CASE 1 I a) Rupture of esophageal varices b) Liver fibrosis c) Schistosomiasis mansoni d) II 1 month years
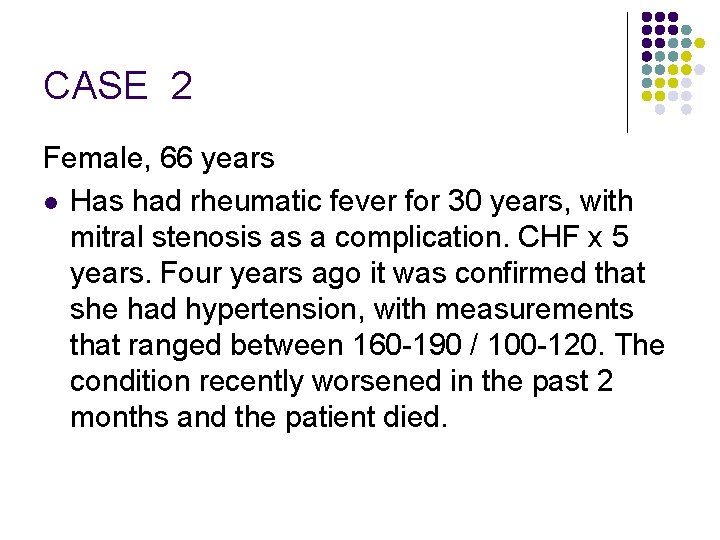
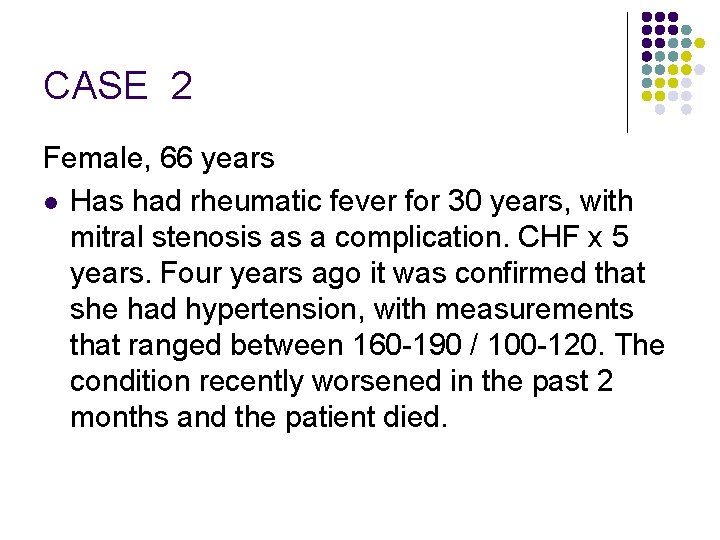
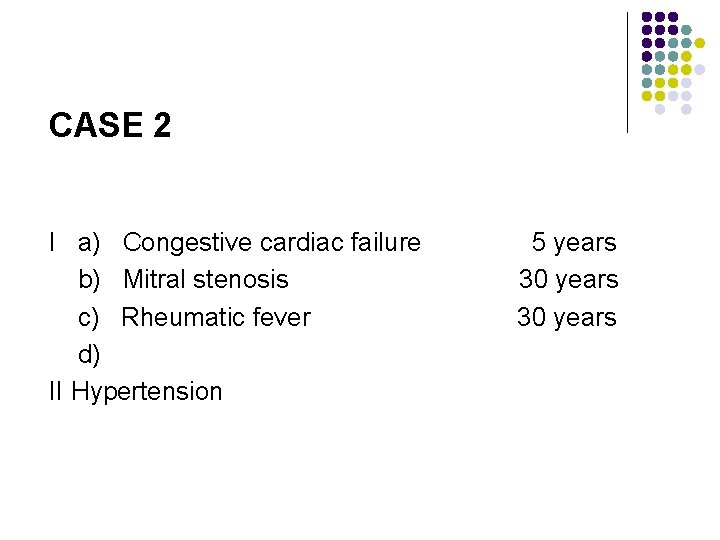
CASE 2 Female, 66 years l Has had rheumatic fever for 30 years, with mitral stenosis as a complication. CHF x 5 years. Four years ago it was confirmed that she had hypertension, with measurements that ranged between 160 -190 / 100 -120. The condition recently worsened in the past 2 months and the patient died.
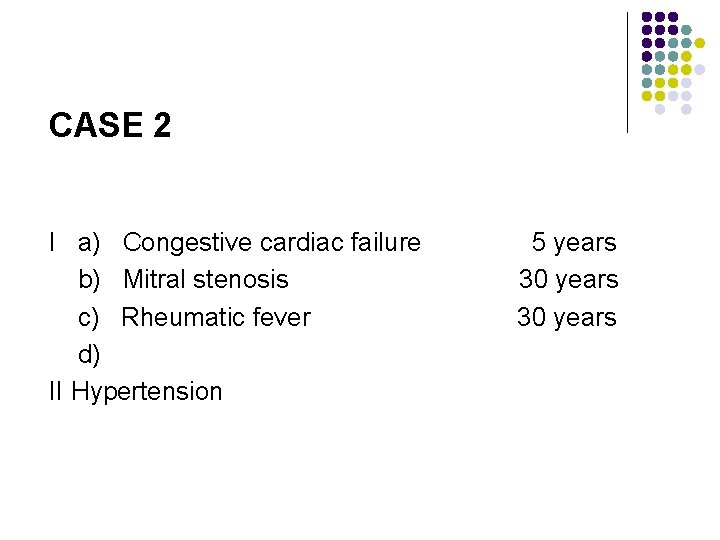
CASE 2 I a) Congestive cardiac failure b) Mitral stenosis c) Rheumatic fever d) II Hypertension 5 years 30 years
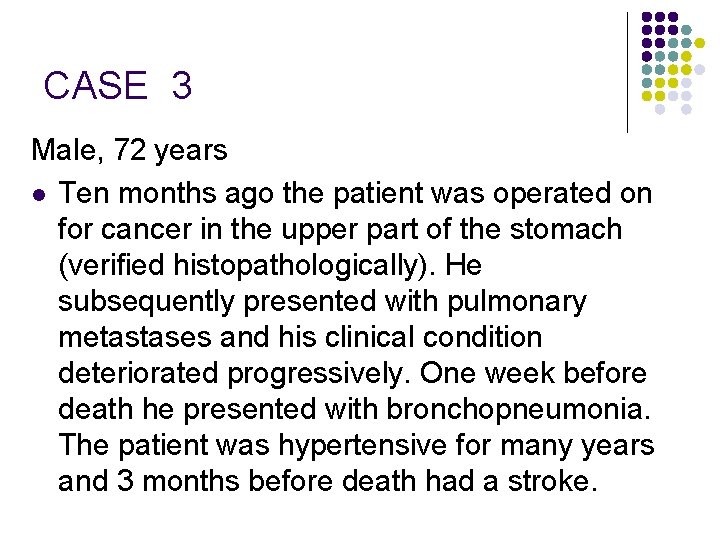
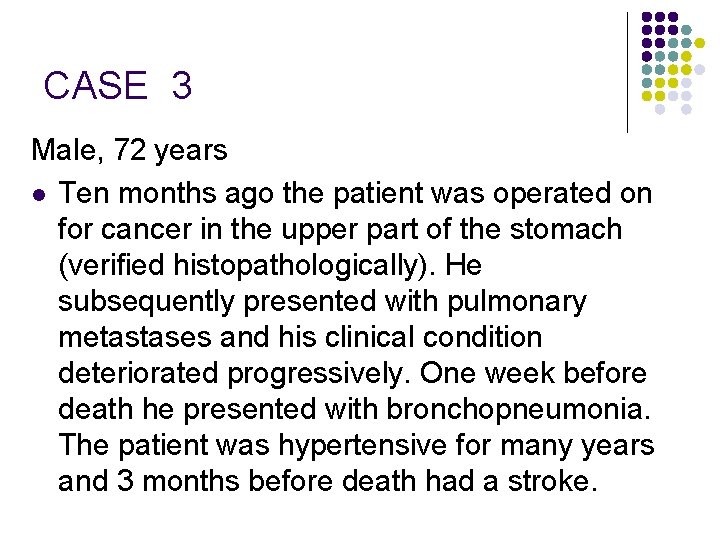
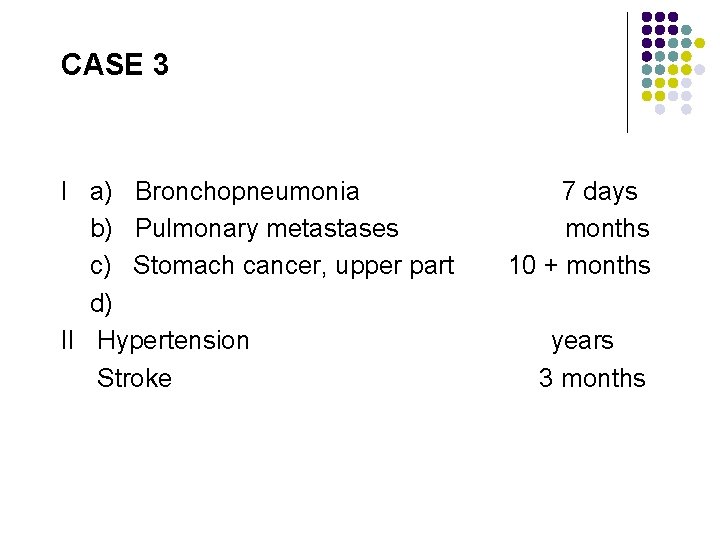
CASE 3 Male, 72 years l Ten months ago the patient was operated on for cancer in the upper part of the stomach (verified histopathologically). He subsequently presented with pulmonary metastases and his clinical condition deteriorated progressively. One week before death he presented with bronchopneumonia. The patient was hypertensive for many years and 3 months before death had a stroke.
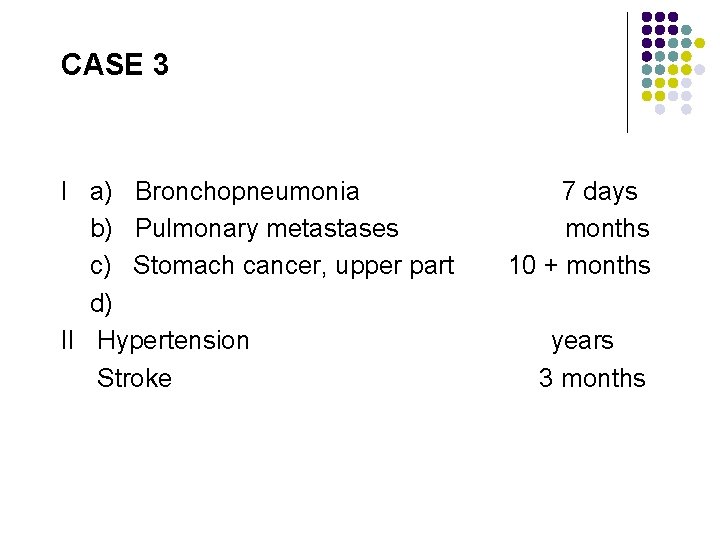
CASE 3 I a) Bronchopneumonia b) Pulmonary metastases c) Stomach cancer, upper part d) II Hypertension Stroke 7 days months 10 + months years 3 months
CASE 4 Female, 3 years l Girl with Tetralogy of Fallot, doing relatively well, in preparation to being submitted to surgery. One morning she was found dead by her mother.
CASE 4 I a) Tetralogy of Fallot b) c) d) II 3 years
CASE 5 Male, 42 years l The mason was working on a scaffolding on the twelfth floor when he accidentally fell to the ground and died instantly. The Coroner reported multiple injuries (skull, hip and limbs).
CASE 5 (ME case) I a) Multiple injury of head, hip, and limbs b) Accidental fall from scaffolding while working c) d) II
CASE 6 Female, 50 years l Two years ago the patient found nodes in the left breast. PE revealed breast mass, retracted nipple, and palpable axillary nodes. She was taken to surgery in the month of April with diagnosis of malignant neoplasm of the breast with nodal metastases. She stayed well for four months, when her general health condition began to deteriorate, presenting with a nodular liver, jaundice and ascites. Two days before dying she entered in hepatic coma. The patient died in December of the same year and an autopsy was not performed.
CASE 6 I a) Hepatic coma 2 days b) Liver metastases months c) Malignant neoplasm of central part of the breast 2 yrs d) II
CASE 7 Male, 3 hours l Child born via NSVD (Apgar score of 2). The pregnancy was normal up to the eighth month, when the mother started to present with hemorrhage and did not seek assistance during the first 24 hours. She was then taken to the hospital where was she admitted with pre-shock. A diagnosis of hemorrhagic abruptio placentae was made. The baby was born cyanotic with signs of anoxia and died in three hours.
CASE 7 I a) Anoxia 3 hours b) Hemorrhagic abruptio placentae 2 days c) d) II
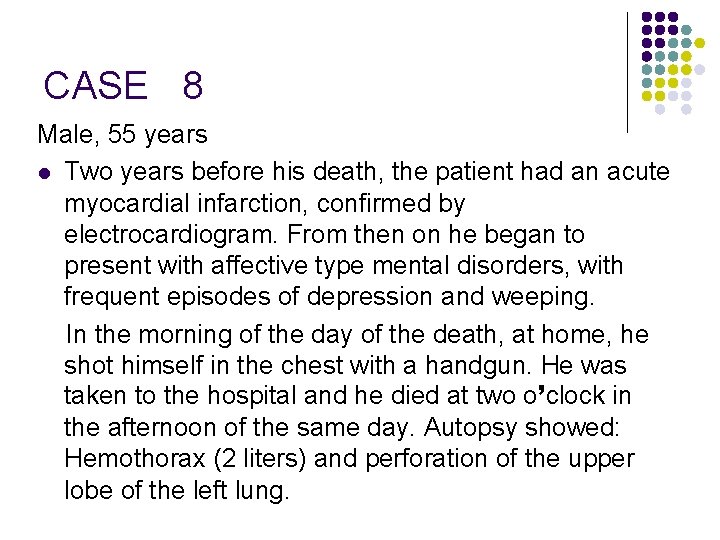
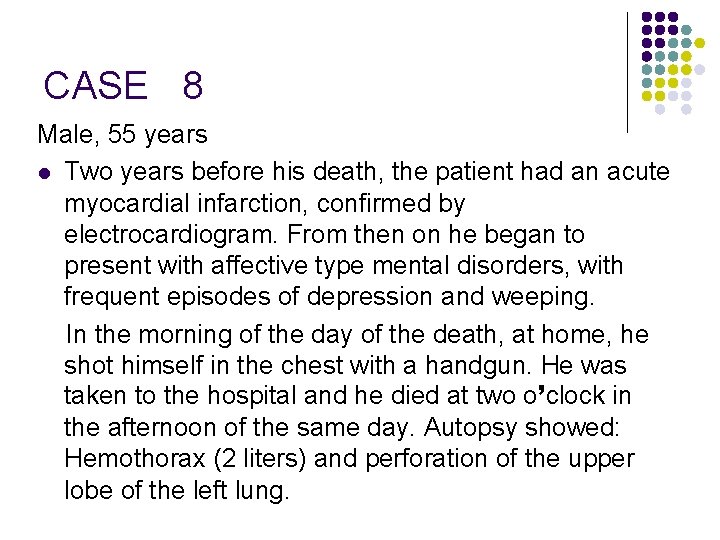
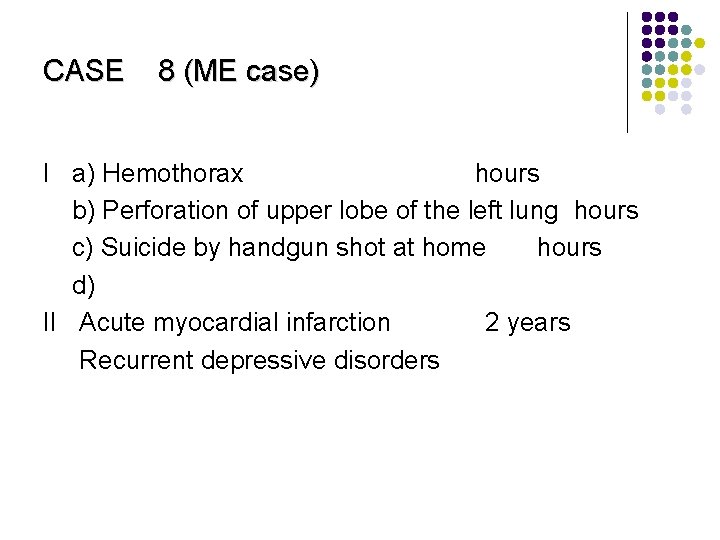
CASE 8 Male, 55 years l Two years before his death, the patient had an acute myocardial infarction, confirmed by electrocardiogram. From then on he began to present with affective type mental disorders, with frequent episodes of depression and weeping. In the morning of the day of the death, at home, he shot himself in the chest with a handgun. He was taken to the hospital and he died at two o’clock in the afternoon of the same day. Autopsy showed: Hemothorax (2 liters) and perforation of the upper lobe of the left lung.
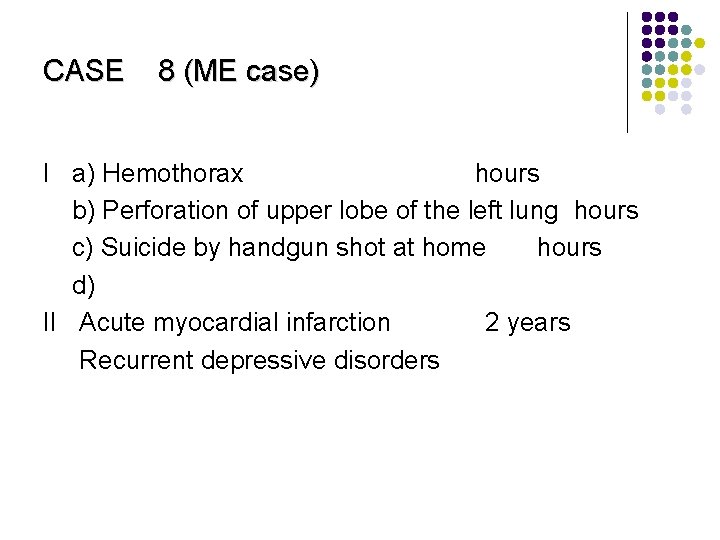
CASE 8 (ME case) I a) Hemothorax hours b) Perforation of upper lobe of the left lung hours c) Suicide by handgun shot at home hours d) II Acute myocardial infarction 2 years Recurrent depressive disorders
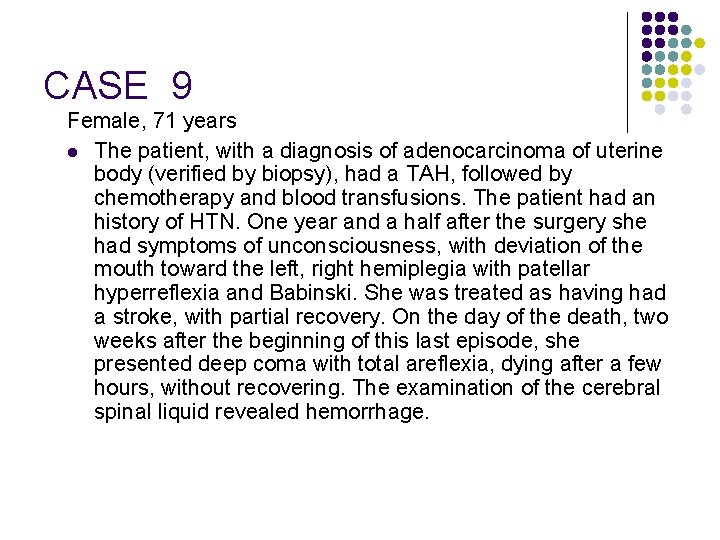
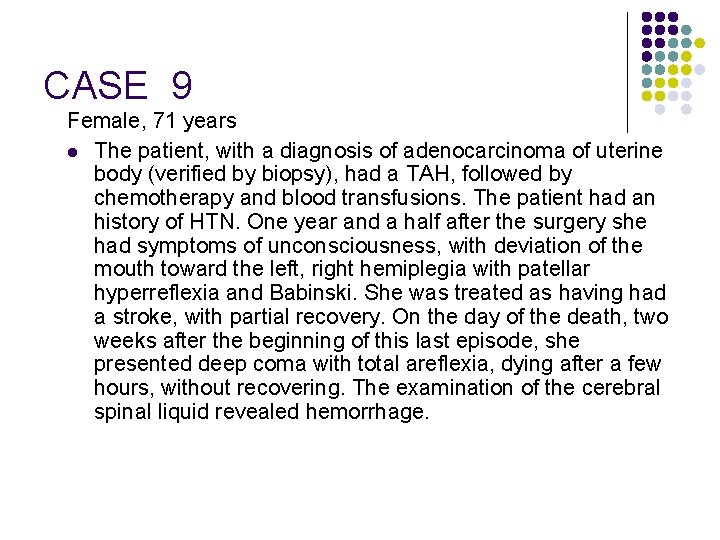
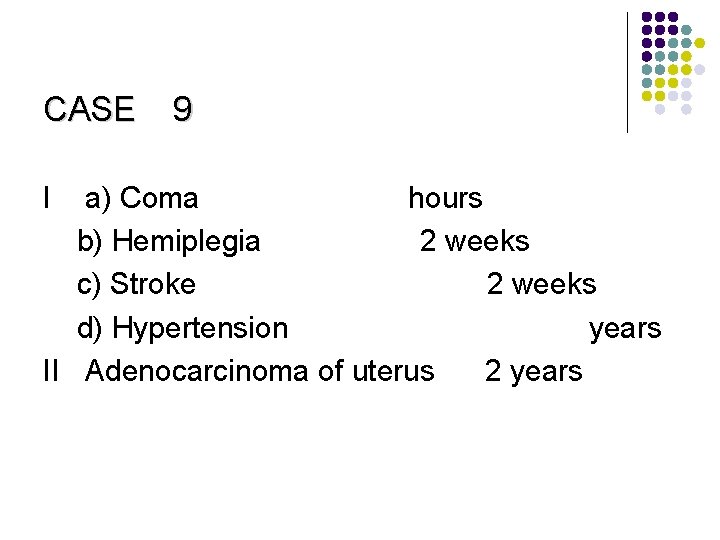
CASE 9 Female, 71 years l The patient, with a diagnosis of adenocarcinoma of uterine body (verified by biopsy), had a TAH, followed by chemotherapy and blood transfusions. The patient had an history of HTN. One year and a half after the surgery she had symptoms of unconsciousness, with deviation of the mouth toward the left, right hemiplegia with patellar hyperreflexia and Babinski. She was treated as having had a stroke, with partial recovery. On the day of the death, two weeks after the beginning of this last episode, she presented deep coma with total areflexia, dying after a few hours, without recovering. The examination of the cerebral spinal liquid revealed hemorrhage.
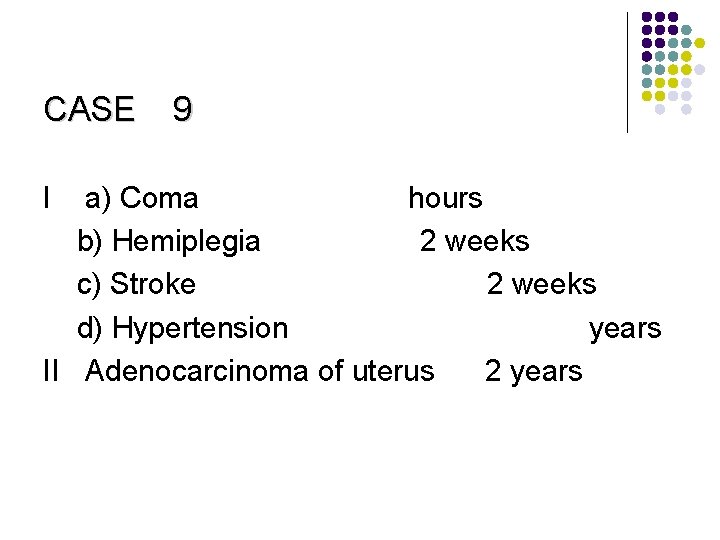
CASE I 9 a) Coma hours b) Hemiplegia 2 weeks c) Stroke 2 weeks d) Hypertension years II Adenocarcinoma of uterus 2 years
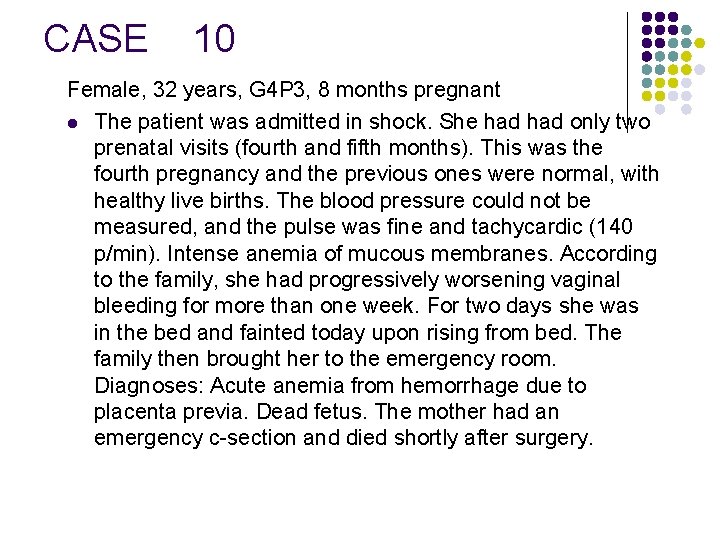
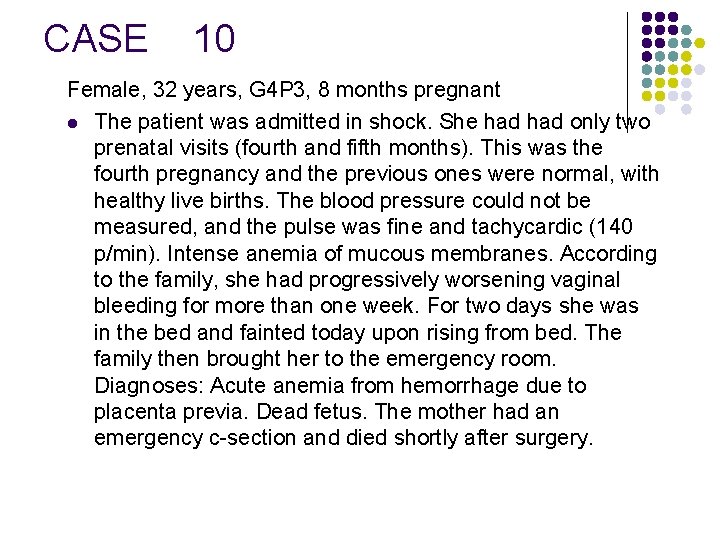
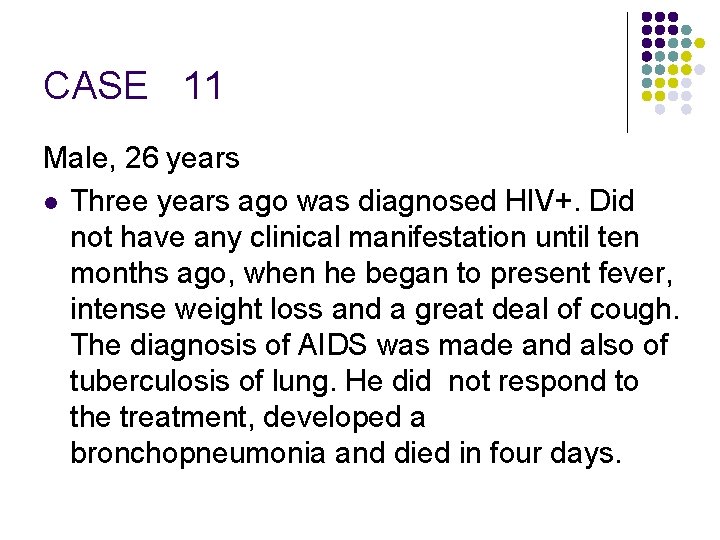
CASE 10 Female, 32 years, G 4 P 3, 8 months pregnant l The patient was admitted in shock. She had only two prenatal visits (fourth and fifth months). This was the fourth pregnancy and the previous ones were normal, with healthy live births. The blood pressure could not be measured, and the pulse was fine and tachycardic (140 p/min). Intense anemia of mucous membranes. According to the family, she had progressively worsening vaginal bleeding for more than one week. For two days she was in the bed and fainted today upon rising from bed. The family then brought her to the emergency room. Diagnoses: Acute anemia from hemorrhage due to placenta previa. Dead fetus. The mother had an emergency c-section and died shortly after surgery.
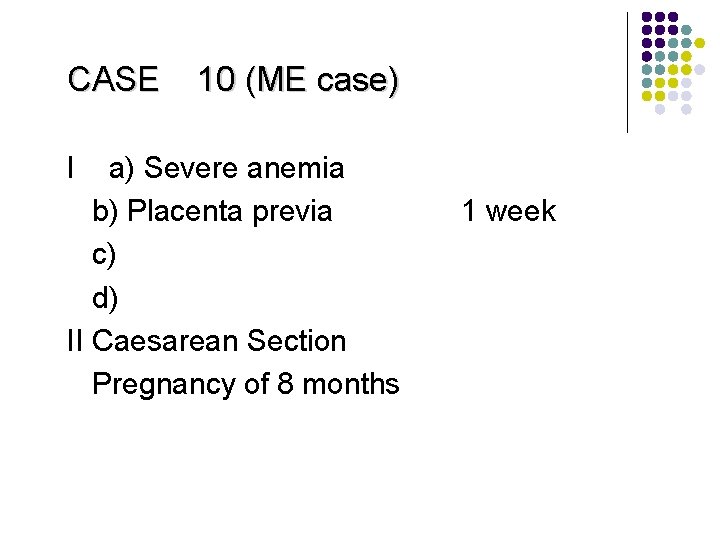
CASE 10 (ME case) I a) Severe anemia b) Placenta previa c) d) II Caesarean Section Pregnancy of 8 months 1 week
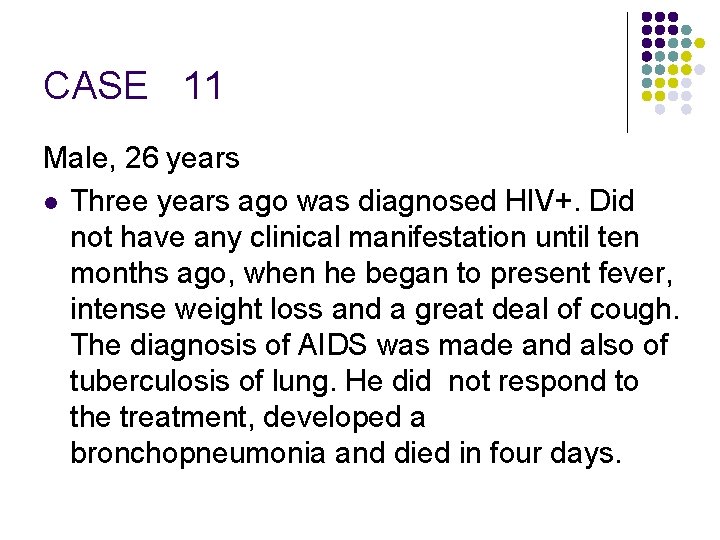
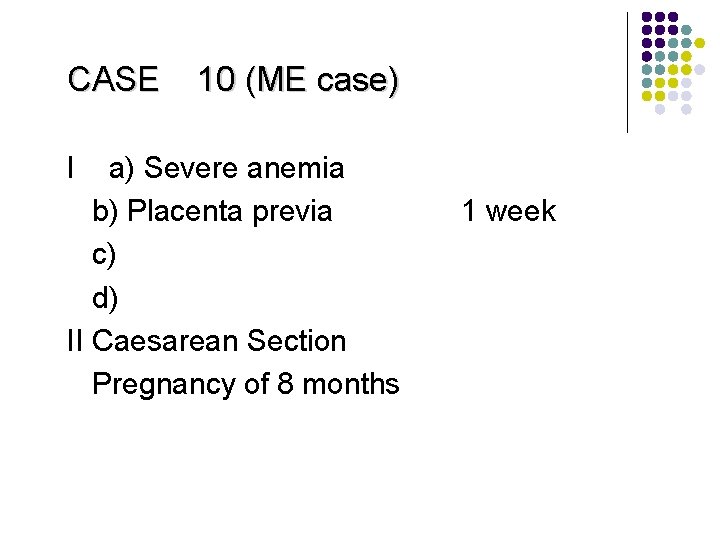
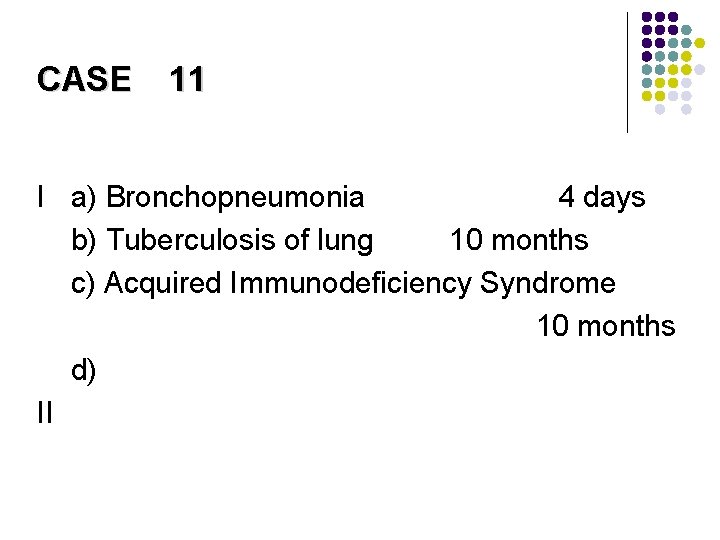
CASE 11 Male, 26 years l Three years ago was diagnosed HIV+. Did not have any clinical manifestation until ten months ago, when he began to present fever, intense weight loss and a great deal of cough. The diagnosis of AIDS was made and also of tuberculosis of lung. He did not respond to the treatment, developed a bronchopneumonia and died in four days.
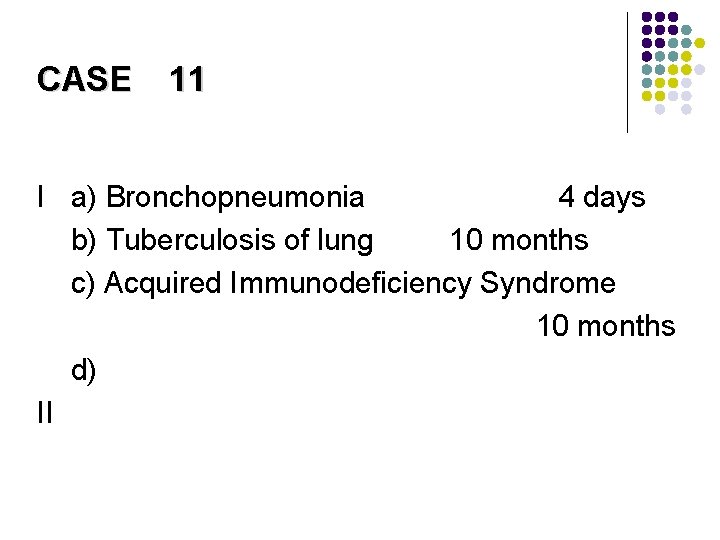
CASE 11 I a) Bronchopneumonia 4 days b) Tuberculosis of lung 10 months c) Acquired Immunodeficiency Syndrome 10 months d) II
CASE 12 Female, 64 years l The lady was exiting a bus, at a bus stop, and was hit by a motorcycle, which ran over her abdomen. She presented alive, in presumed hemorrhagic shock to the ED, with signs of splenic rupture. A splenectomy was done. The patient lost 1. 9 liters of blood and died before the end of the surgery.
CASE 12 (ME case) I a) Rupture of the spleen b) Hit by a motorcycle while exiting a minibus c) d) II Splenectomy
 Death pronouncement note example
Death pronouncement note example Bold pronouncement hook
Bold pronouncement hook What is bold statement
What is bold statement Somatic death vs molecular death
Somatic death vs molecular death Verifying death geeky medics
Verifying death geeky medics Macbeth summary
Macbeth summary National board of certified medical interpreters
National board of certified medical interpreters Death of a salesman act 1 questions
Death of a salesman act 1 questions Hepburn osteometric board
Hepburn osteometric board Act 120 training
Act 120 training Act 120 training
Act 120 training Death of a salesman act 2 summary
Death of a salesman act 2 summary Uniform determination of death act 1981
Uniform determination of death act 1981 Death of a salesman summary act 2
Death of a salesman summary act 2 Death of a salesman audiobook act 1
Death of a salesman audiobook act 1 Summary death of a salesman act 1
Summary death of a salesman act 1 Death of a salesman act 1 summary
Death of a salesman act 1 summary Iba things fall apart
Iba things fall apart Death of a salesman act 3
Death of a salesman act 3 Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Frameset trong html5
Frameset trong html5 Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Tư thế worm breton
Tư thế worm breton Hát lên người ơi
Hát lên người ơi Các môn thể thao bắt đầu bằng từ đua
Các môn thể thao bắt đầu bằng từ đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Cong thức tính động năng
Cong thức tính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 Phản ứng thế ankan
Phản ứng thế ankan Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Bàn tay mà dây bẩn
Bàn tay mà dây bẩn Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thế nào là sự mỏi cơ
Thế nào là sự mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Ví dụ về giọng cùng tên
Ví dụ về giọng cùng tên Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Dạng đột biến một nhiễm là
Dạng đột biến một nhiễm là Bảng số nguyên tố lớn hơn 1000
Bảng số nguyên tố lớn hơn 1000 Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì