COMPLICATIONS OF CARDIOTHORACIC SURGERY Jacqueline PalmerPowell RN Nurse


- Slides: 81
COMPLICATIONS OF CARDIOTHORACIC SURGERY Jacqueline Palmer-Powell, RN Nurse Educator/CNS
n Complications Commonly Resulting From Cardio. Thoracic Surgery
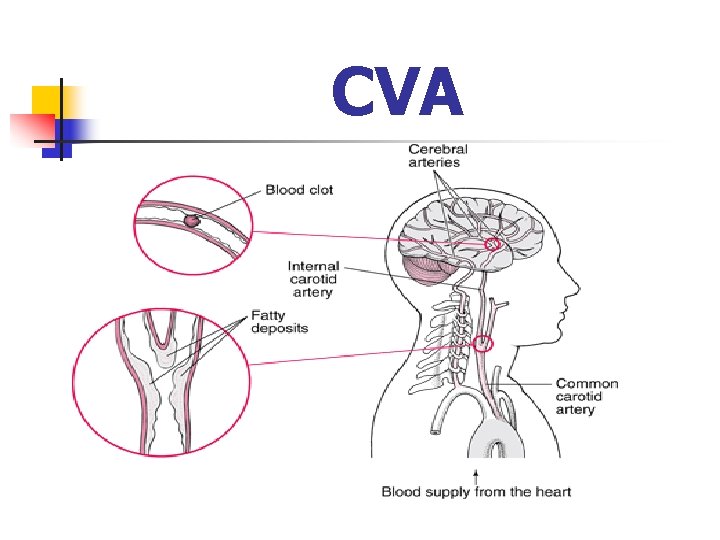
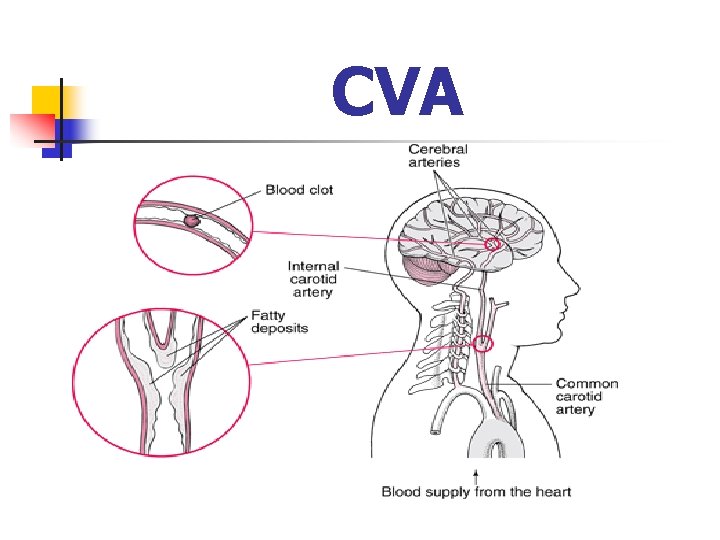
CVA
CVA n n n Devastating complication that results in lasting deficits of death. Other neurological complications which are more subtle occur with more frequency. Incidence -CABG with CPB: 2 -5% -Valve Surgery: 5 -10%
Risk Factors n n Prior history of stroke, HTN, DM Carotid disease, carotid bruit Advanced age Atrial Fib
Diagnosis & Treatment n n CT Scan demonstrates cerebral infarct within 1 -2 days No treatment exist other than palliative Early rehabilitation Family counseling
Hypotension n Definition: Systolic BP<100 Cause: hypovolemia, excessive vasodilation, sepsis, elevated or decreased HR Treatment: identify cause!, volume replacement, use of IV drips

Bleeding
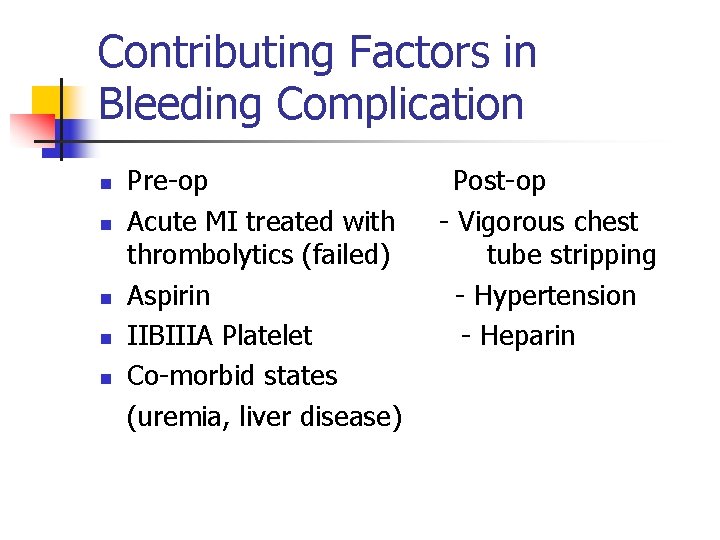
Contributing Factors in Bleeding Complication n n Pre-op Acute MI treated with thrombolytics (failed) Aspirin IIBIIIA Platelet Co-morbid states (uremia, liver disease) Post-op - Vigorous chest tube stripping - Hypertension - Heparin
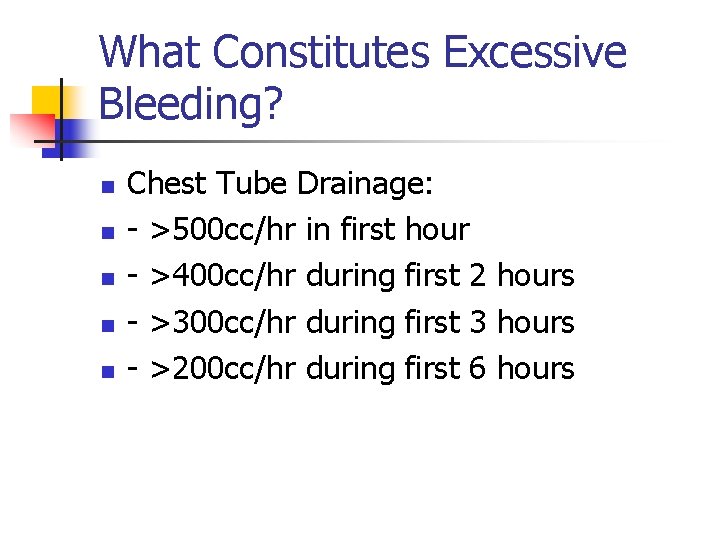
What Constitutes Excessive Bleeding? n n n Chest Tube Drainage: - >500 cc/hr in first hour - >400 cc/hr during first 2 hours - >300 cc/hr during first 3 hours - >200 cc/hr during first 6 hours
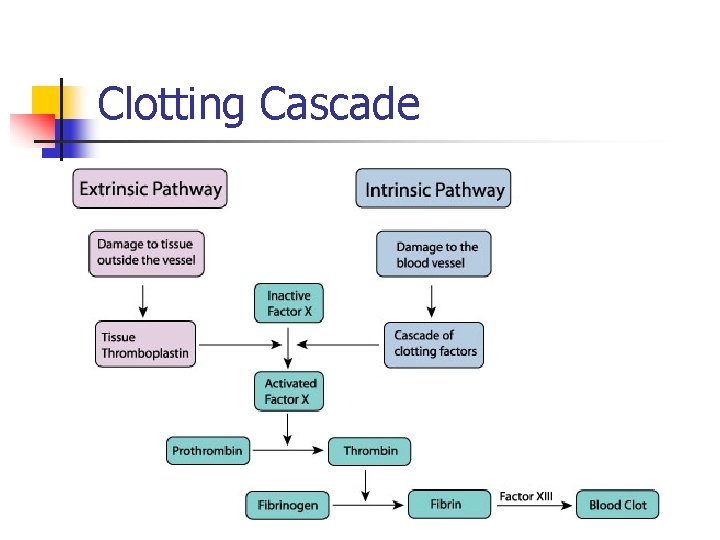
Basis of Coagulation n n Coagulation Cascade with the help of endothelium & platelets is the body’s defense to minimize blood loss. A vascular insults stimulates formation of platelet plug thru platelet activation, adhesion & aggregation. The plug is then stabilized thru clotting cascade to a fibrin clot
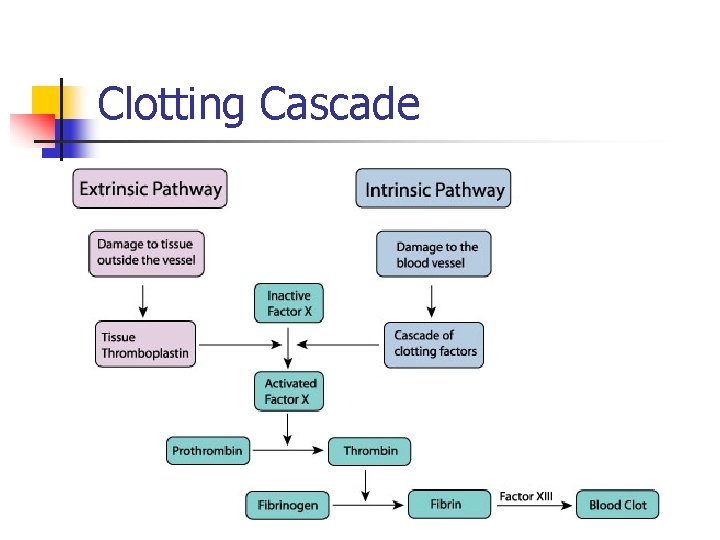
Clotting Cascade
Effect of CPB on Coagulation n n Major CPB induced coagulopathy results from platelet activation, dysfunction & destruction. Structural damage to platelets & RBC’s can occur thru shearing forces & turbulence in CPB pump, circuits & suction devices
Preventing Bleeding Before Surgery n n n Complete History - Questions about previous surgery, family history, bruising, heavy menses - medication history (Prescribed, OTC & herbal) Physical Exam Blood Work
Pre-op Bleeding Prevention n Identification of patient with co-morbid states that may contribute to bleeding: - Uremia: Causes platelet dysfunction thru impaired VWF interaction with platelets. - Acute liver dysfunction: may result in factor deficiency as a results of impaired factor production & may lead to DIC
Drugs Which Affect Bleeding n n n Aspirin NSAIDS IIBIIIA Platelet Inhibitors Coumadin Thrombolytics Heparin
Prevention & Treatment of Bleeding in OR n n n Thorough search for bleeding before chest closure including careful inspection of skin, sternum, suture sites Autotransfusion: pre-op blood donation (self-directed) with re-infusion after CPB Cell-saver-blood drained from chest tubes in OR collected thru special filters & reinfused after surgery
DIC n n Diagnosis: Increased products of fibrin degradation (d-dimer), thrombocytopenia & prolongation of both PT & PTT Treatment: Replacement with PRBC, FFP & platelets. If fibrinogen level low, replacement with cryoprecipitate is preferable. Drugs (Amikar, Aprotinin) may be useful in treating DIC. High mortality!
Drugs Used To Treat Bleeding n n n Protamine SO 4: Protein derived from salmon sperm. Used to neutralize effects of heparin DDAVP: Analog of vasopressin may be used when a patient continues to bleed despite normal coagulation profile & platelet counts Antifubrinolytics: Help to achieve homeostasis in patients with excessive fibrinolysis
Blood Products n Depending on patient presentation, history & lab results the bleeding may require infusion(s) of PRBC, platelets, FFP, &/or cryoprecipitate to control the bleeding & prevent hemodynamic instability
Re-Op for Bleeding Chest Exploration n <3% of patients require re-op to search for bleeding Bleeding causing tamponade or severe hypotension requires immediate re-op Coagulopathy must be distinguished from anatomic cause
Low Cardiac Output Syndrome
Signs & Symptoms of LCOS n n n Results directly from inadequate tissue perfusion & increased sympathetic activity. Cool, clammy skin with slow capillary refill Oliguria Mental status changes Metabolic acidosis Fall in SVO 2
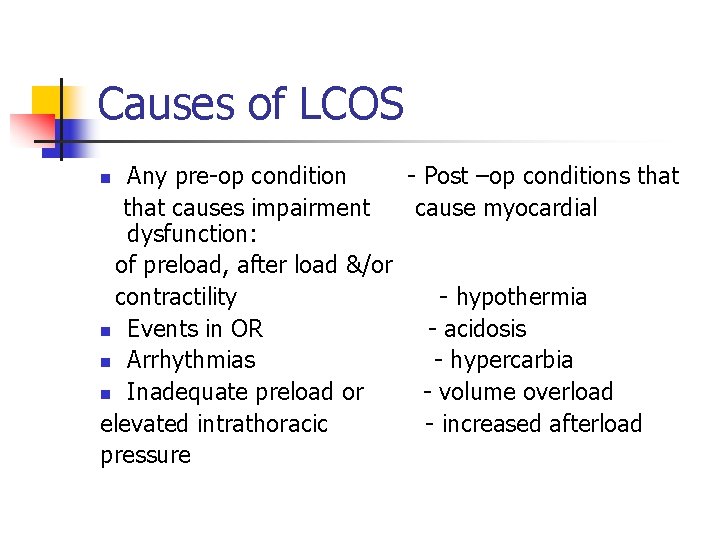
Causes of LCOS Any pre-op condition - Post –op conditions that causes impairment cause myocardial dysfunction: of preload, after load &/or contractility - hypothermia n Events in OR - acidosis n Arrhythmias - hypercarbia n Inadequate preload or - volume overload elevated intrathoracic - increased afterload pressure n
Treatment of LCOS n n Heart rate manipulation Preload Afterload Myocardial Contractility
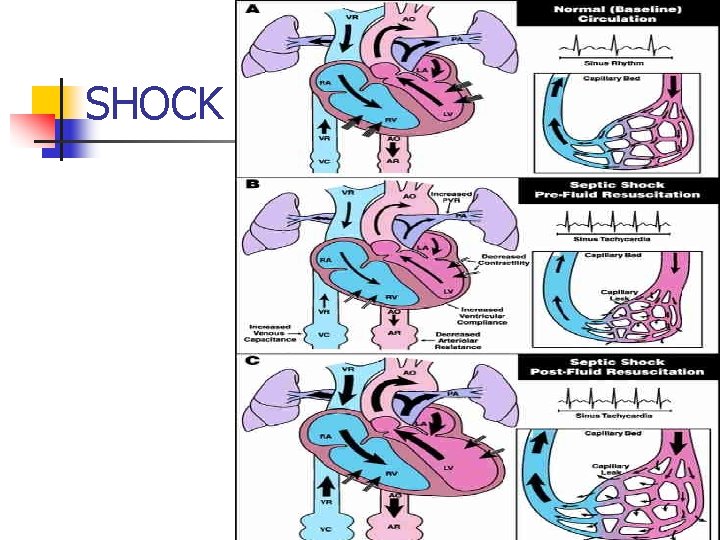
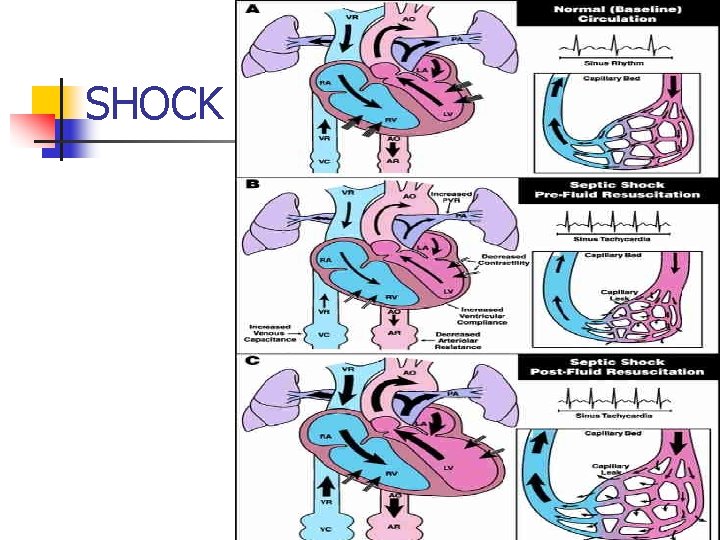
SHOCK
Shock n n n Clinical syndrome representing an extreme state of circulatory failure Impaired tissue perfusion leading to cellular dysfunction Complex group of signs & symptoms that can be caused by a variety of factors
Clinical Manifestations of Shock n n n Directly related to pathophysiologic mechnaisms are involved. Progression is variable & depends on: -Patient age & prior state of health Duration of shock state Response to treatment Correction of treatable cause
3 Stages of Shock n Early or compensatory n Intermediate or progressive n Late or irreversible
Classification n Vascular Tone (Distributive) n n Intravascular Volume n n Neurogenic Septic Anaphylactic Hypovolemic Ability of heart to act as pump n Cardiogenic
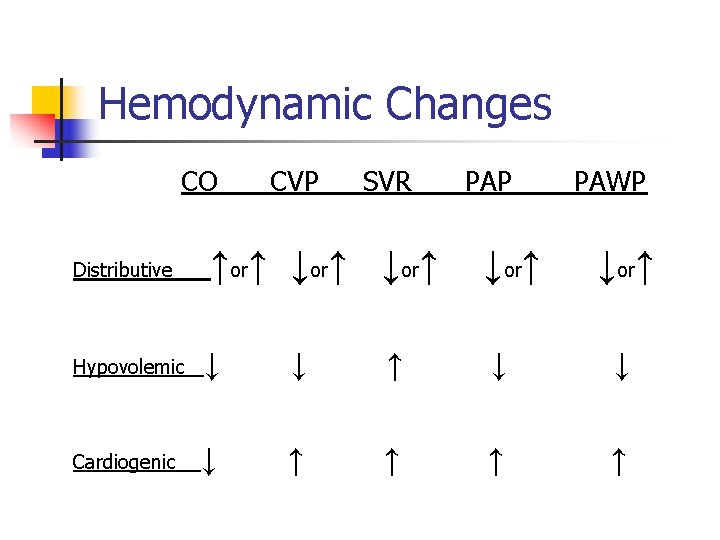
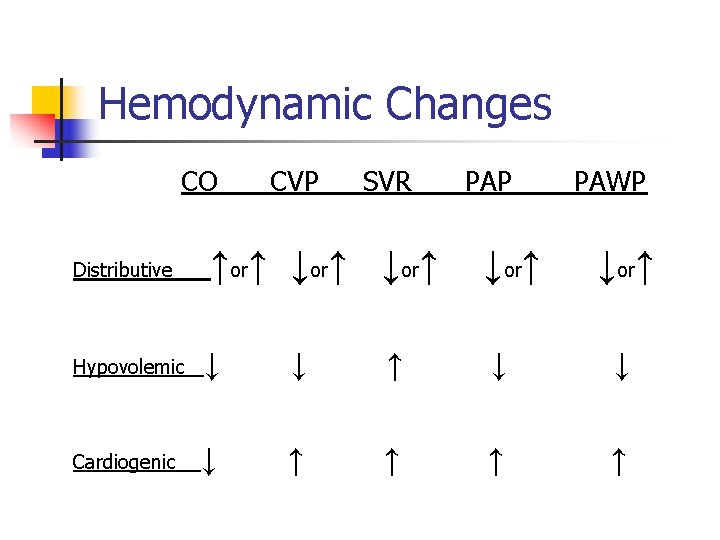
Hemodynamic Changes CO CVP SVR PAP PAWP ↑or↑ ↓or↑ Hypovolemic ↓ ↓ ↑ ↓ ↓ Cardiogenic ↓ ↑ ↑ Distributive ↓or↑
Treating Shock States n n Position: Supine/let elevation (if possible) Trendelenberg should be avoided: n n n Initiates aortic & carotid sinus reflex Impaired cerebral blood flow Decreased filling of coronary arteries
Fluids n n n Shock almost always involves a decrease in effective circulating volume Need for volume expansion Fluid challenge
Septic Shock n n n Occurs in patients as a result of overwhelming infection More common in infants, elderly & immuno-compromised Clinical presentation can be subtle in elderly, debilitated or malnourished patients
Warm Shock n Vasodilation → ↓ SVR ↑ or normal CO n BP ↓ but skin is pink, warm & dry n Urine output is adequate
Cold Shock n n n Vasoconstriction ↓ ↑ SVR ↓ CO ↓ BP ↓ Urine output Metabolic Acidosis
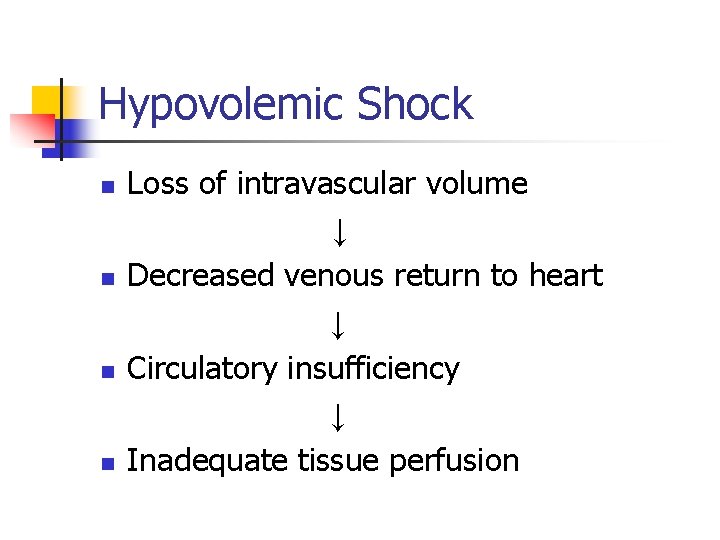
Hypovolemic Shock n n Loss of intravascular volume ↓ Decreased venous return to heart ↓ Circulatory insufficiency ↓ Inadequate tissue perfusion
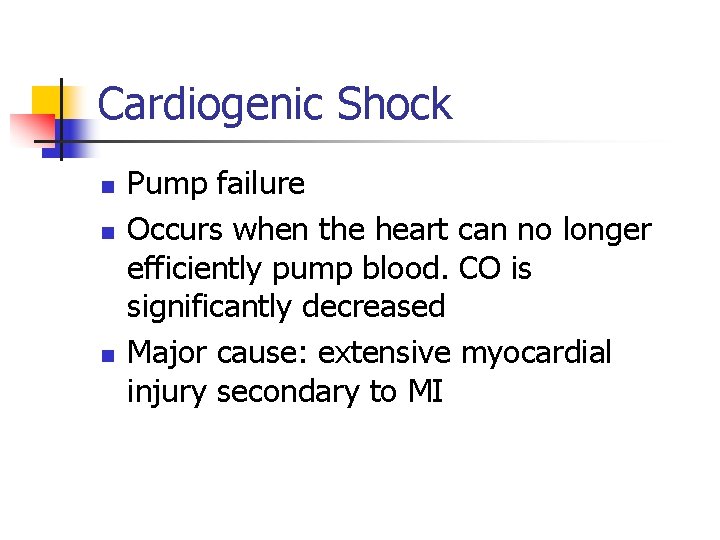
Cardiogenic Shock n n n Pump failure Occurs when the heart can no longer efficiently pump blood. CO is significantly decreased Major cause: extensive myocardial injury secondary to MI
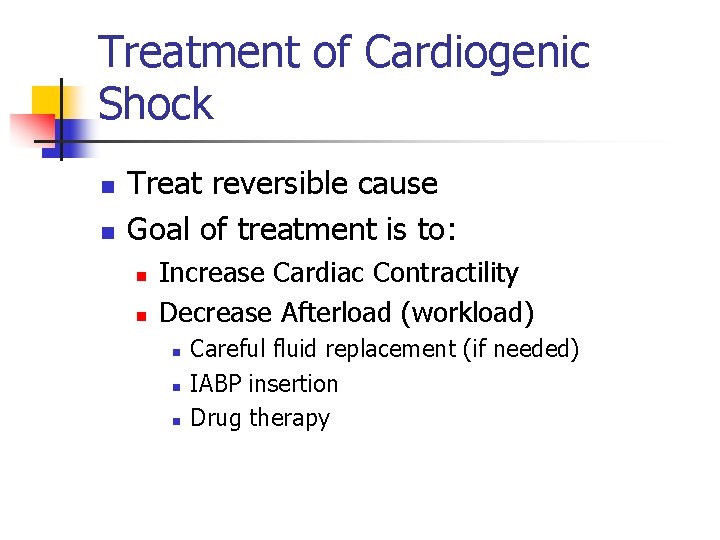
Treatment of Cardiogenic Shock n n Treat reversible cause Goal of treatment is to: n n Increase Cardiac Contractility Decrease Afterload (workload) n n n Careful fluid replacement (if needed) IABP insertion Drug therapy
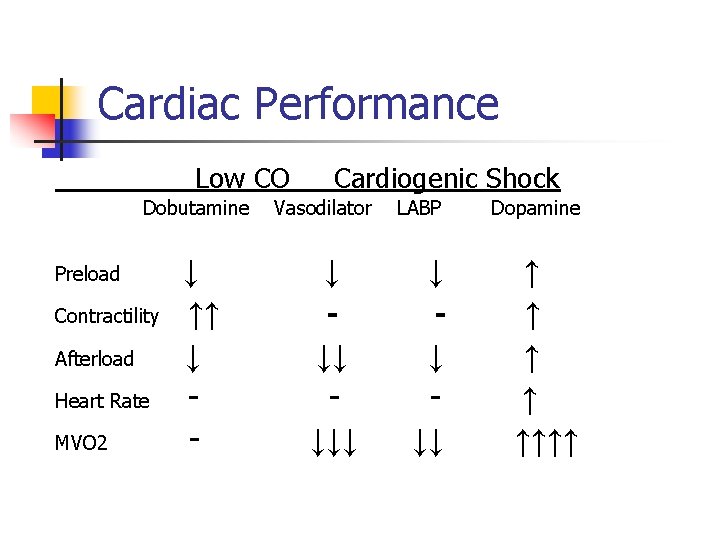
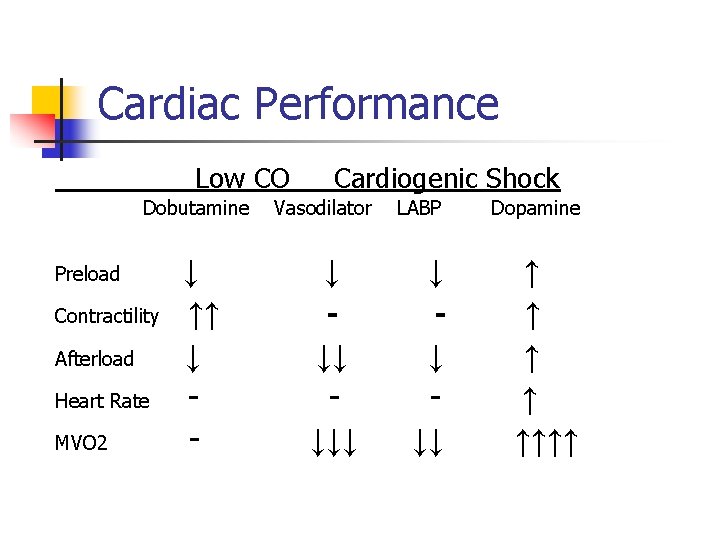
Cardiac Performance Low CO Dobutamine Preload Contractility Afterload Heart Rate MVO 2 ↓ ↑↑ ↓ - Cardiogenic Shock Vasodilator ↓ ↓↓ ↓↓↓ LABP Dopamine ↓ ↓ ↓↓ ↑ ↑ ↑↑↑↑
Treatment of Peri-Op/Post-Op Ischemia n n Evaluate/Investigation of cause Drugs: n n Belta Blockers Nitrates Vasopressors Calcium Blockers
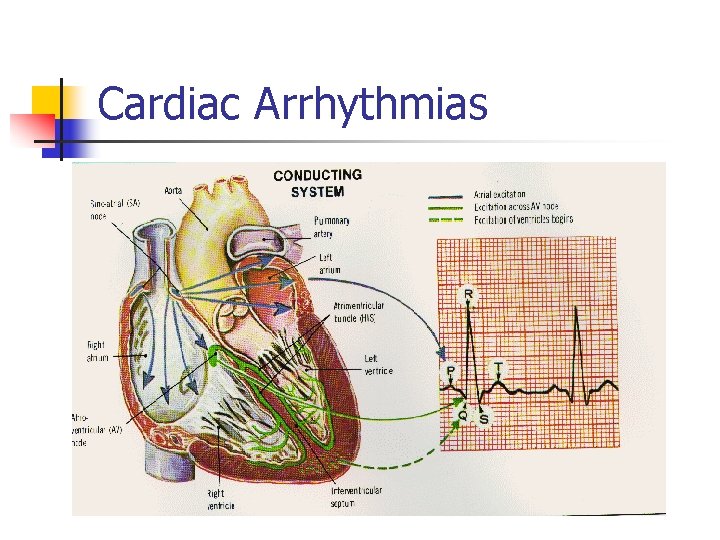
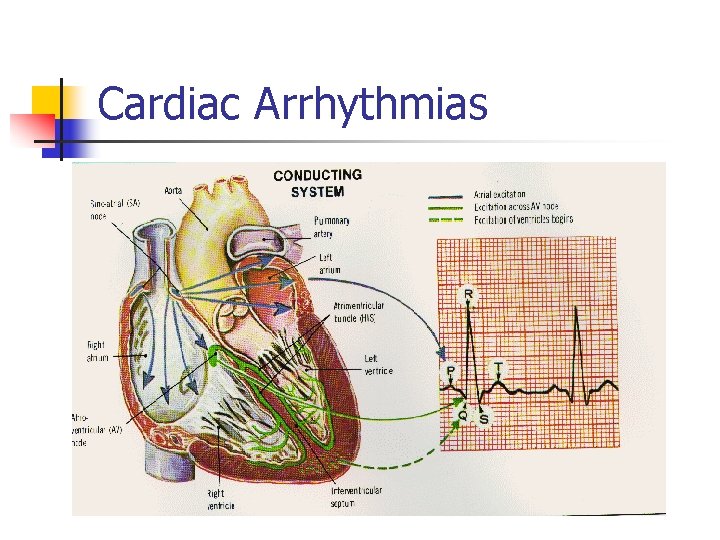
Cardiac Arrhythmias
Atrial Fibrillation n n Nearly 30% of patients undergoing coronary surgery & up to 50% of patients with valvular disease develop AF Occurs in up to 5% of patients afterr any major surgery
Myocardial Ischemia
Myocardial Ischemia n n Ischemia results from an imbalance between myocardial O 2 supply & demand. Can be due to: n n n ↑ Demand ↓ Supply Coronary Vasospasm
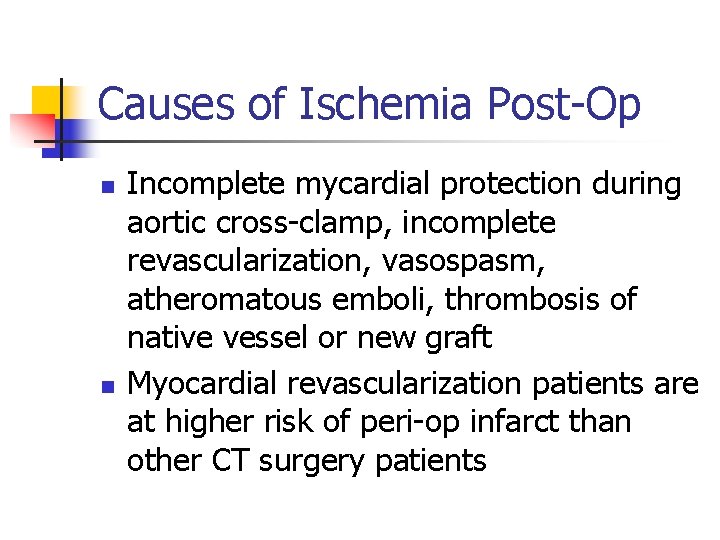
Causes of Ischemia Post-Op n n Incomplete mycardial protection during aortic cross-clamp, incomplete revascularization, vasospasm, atheromatous emboli, thrombosis of native vessel or new graft Myocardial revascularization patients are at higher risk of peri-op infarct than other CT surgery patients
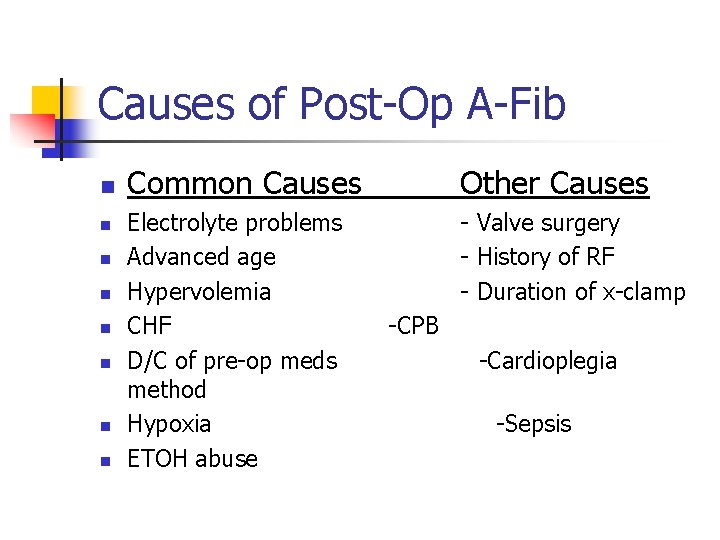
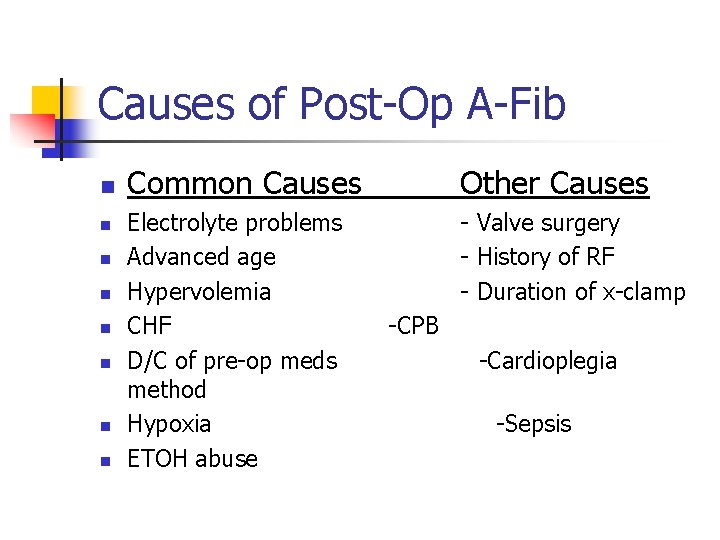
Causes of Post-Op A-Fib n n n n Common Causes Other Causes Electrolyte problems Advanced age Hypervolemia CHF D/C of pre-op meds method Hypoxia ETOH abuse - Valve surgery - History of RF - Duration of x-clamp -CPB -Cardioplegia -Sepsis
Treatment of AF n n Prompt identification & treatment of cause Chemical cardioversion n First give drugs to treat rate Then drugs to convert to SR Synchronized cardio version
Brady Arrhythmias n n n Sinus Bradycardia Heart Blocks Cause: n n Overuse of Beta blockers pre-op Manipulation or destruction of SA or AV nodes Hypoxia Vagal stimulation
Treatment n Treat Cause n Pacing n Drugs
Ventricular Arrhythmias n n n Range from occasional premature beats to bigeminy, trigeminy, non-sustained VT to sustained VT & VF Benign arrhythmias occur in 20 -60% of patients post-op. Infrequently produce symptoms or require treatment Incidence of sustained VT/VF after cardiac surgery = 0. 4 -1. 4%
Pre-disposing Factors in Development of VT n n n Myocardial ischemia Decreased CO Decreased EF (<40%) Metabolic derangements Drug interactions Hypoxemia
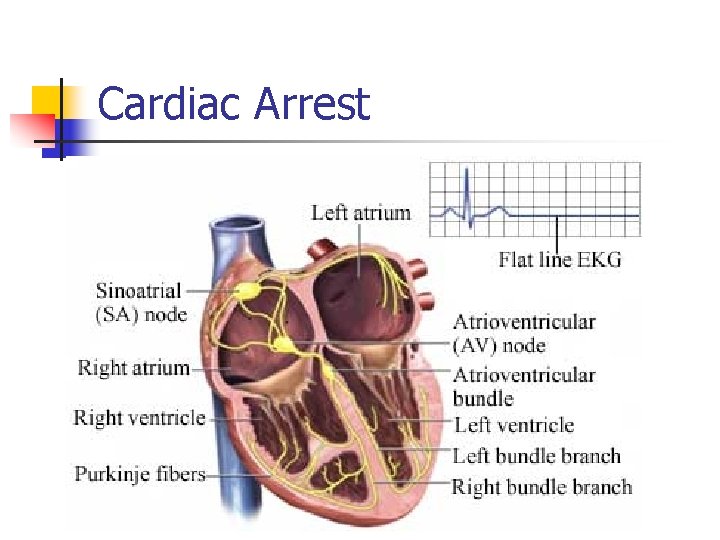
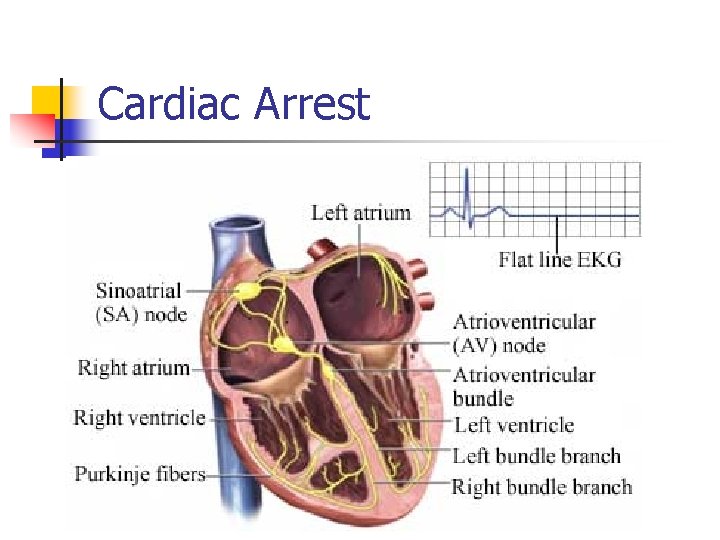
Cardiac Arrest
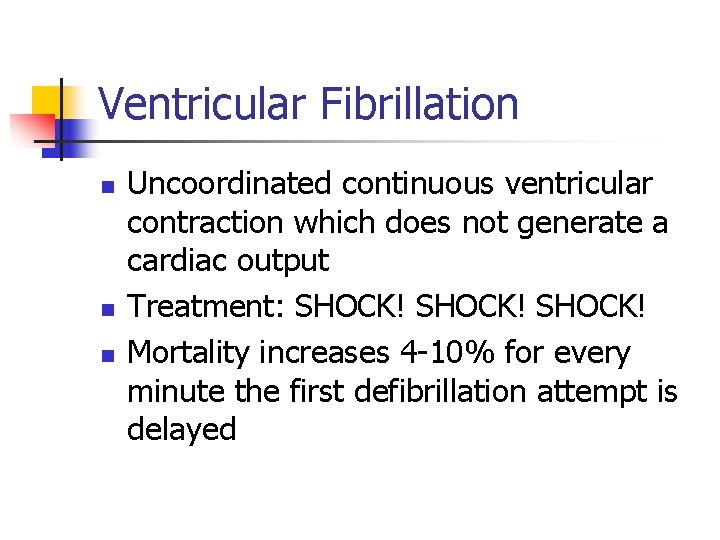
Ventricular Fibrillation n Uncoordinated continuous ventricular contraction which does not generate a cardiac output Treatment: SHOCK! Mortality increases 4 -10% for every minute the first defibrillation attempt is delayed
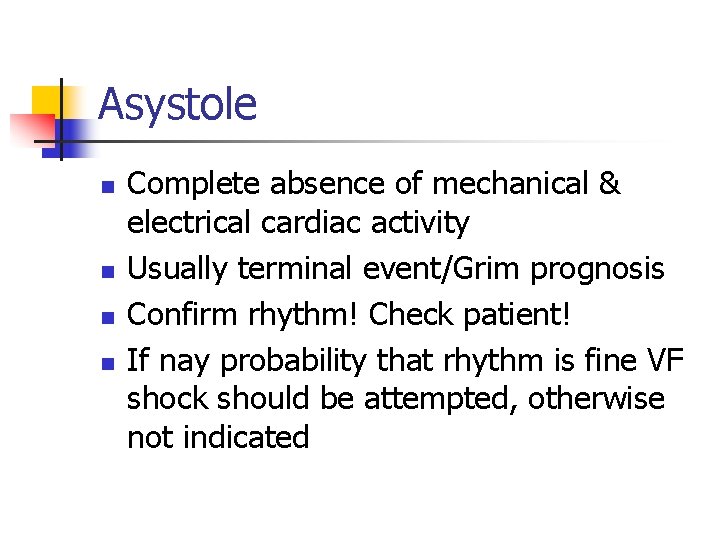
Asystole n n Complete absence of mechanical & electrical cardiac activity Usually terminal event/Grim prognosis Confirm rhythm! Check patient! If nay probability that rhythm is fine VF shock should be attempted, otherwise not indicated
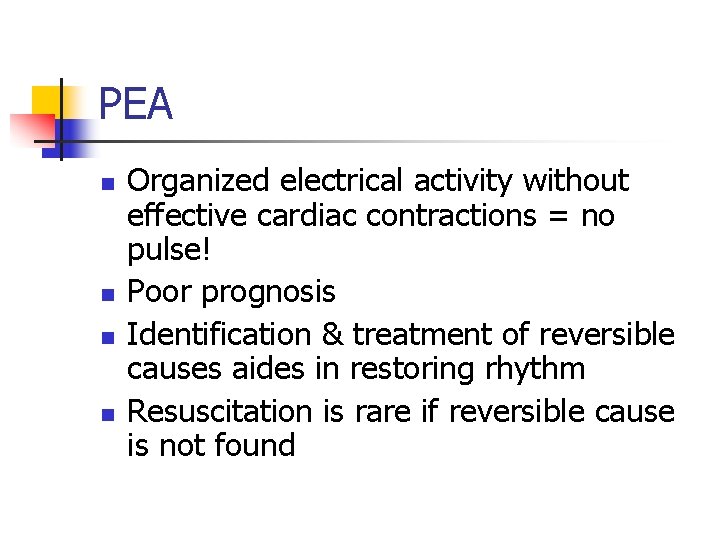
PEA n n Organized electrical activity without effective cardiac contractions = no pulse! Poor prognosis Identification & treatment of reversible causes aides in restoring rhythm Resuscitation is rare if reversible cause is not found
Open Cardiac Massage n Indications: Cardiac arrest associated with penetrating thoracic trauma, arrest during thoracic surgery or when chest wall deformity or recent sternotomy precludes effective closed massage
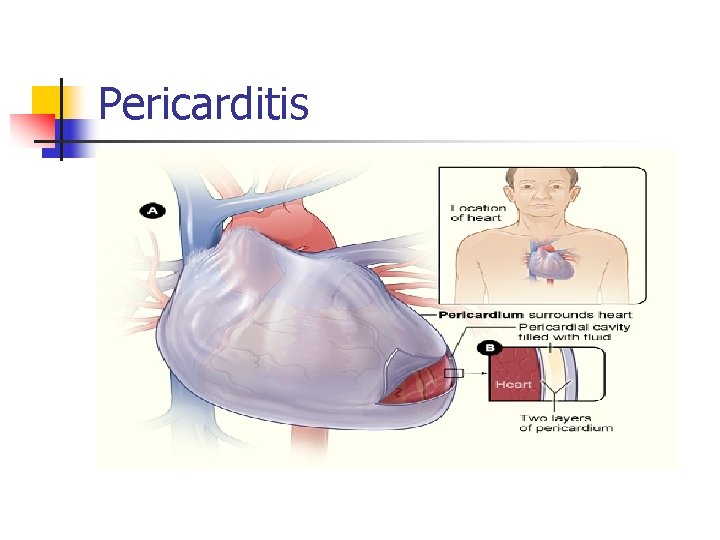
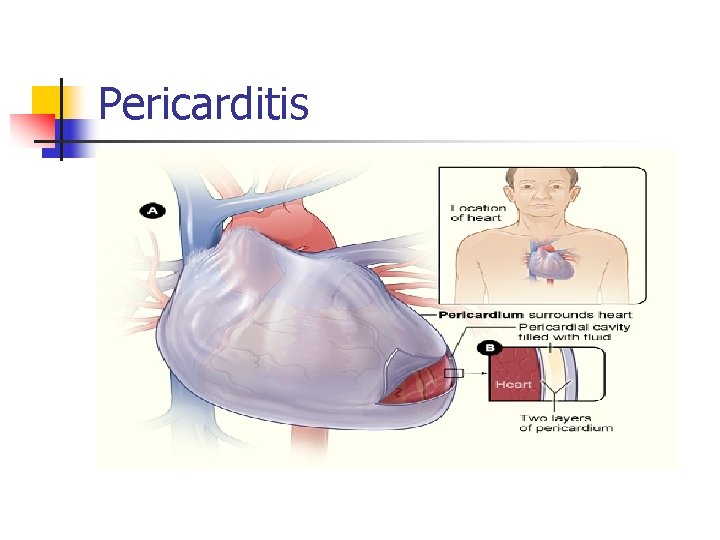
Pericarditis
Cause n n n n Infections Uremia Neoplasm Radiation Rheumatic Fever Post-MI Post-Pericardiotomy
Clinical Manifestations n n n n Occurs approximately 4 weeks post-op Pain Friction rub Dyspnea Fever EKG changes Leukocytosis
Pericardial Effusion n Generally rapid accumulation of excess fluid within the pericardial space May arise from acute pericarditis Large effusions may compress adjoining structures & cause tamponade if left untreated
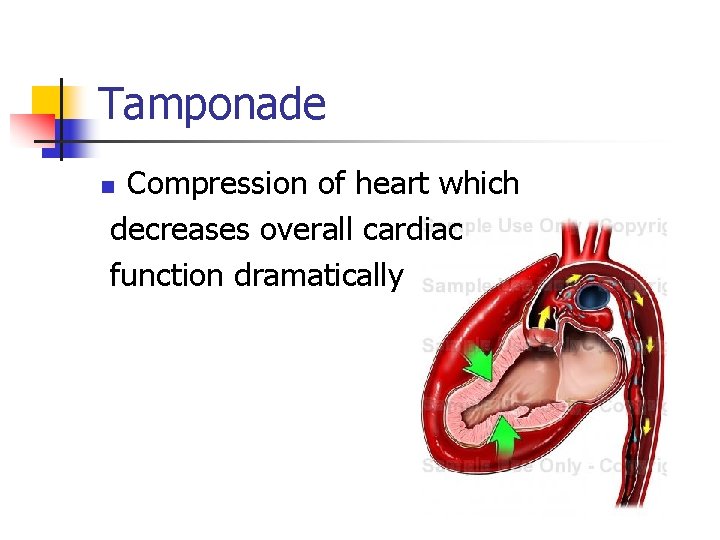
Tamponade Compression of heart which decreases overall cardiac function dramatically n
Clinical Signs n n n Decreased CO patients who initially had adequate ventricular performance Increased bleeding in early post-op period with sudden decrease in drainage & hemodynamic worsening May occur in patients with initial bleeding whose coagulation profile was corrected leading to formation of pericardial clot
Symptoms n n n n Rapid increase in R&L atrial pressure which tends to equalize Muffled heart sounds Increased jugular venous pressure (distended neck veins) Widening of mediastinum by CXR EKG changes Pulsus paradoxus (late effusion) Vague symptoms: LE edema, hepatomegaly, pleural effusion (late)
Treatment n n Surgery-re-exploration via median sternotomy Sub-xiphoid incision Small right anterior thoracic incision (late tamponade) Echocardiographic guided puncture
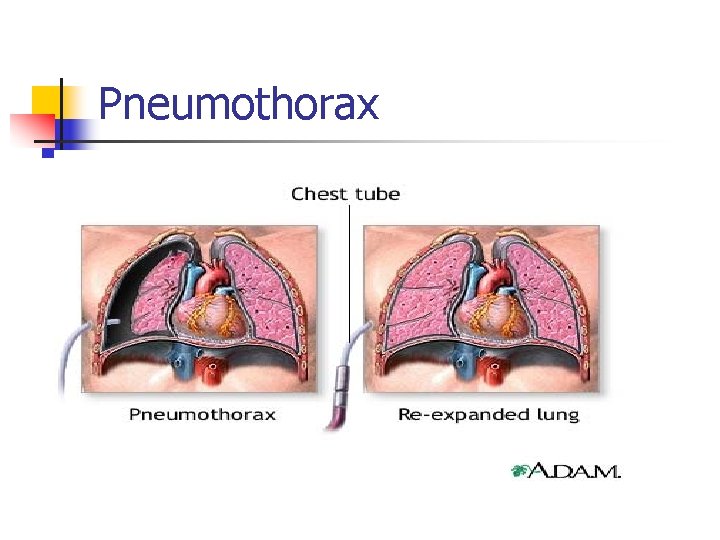
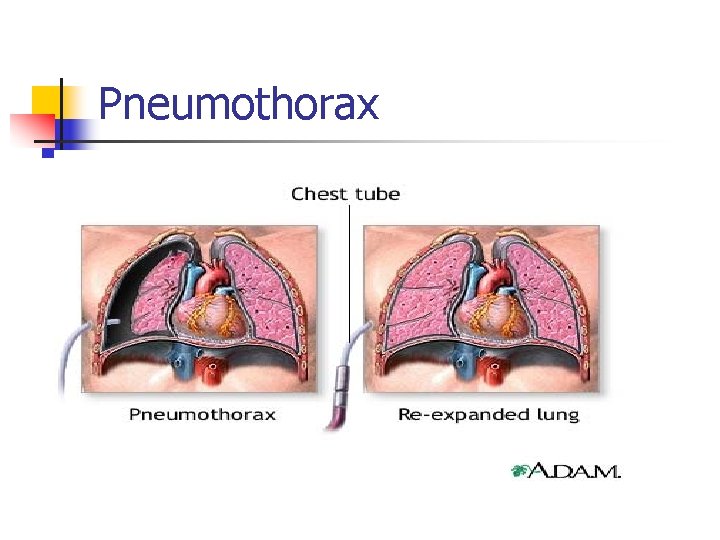
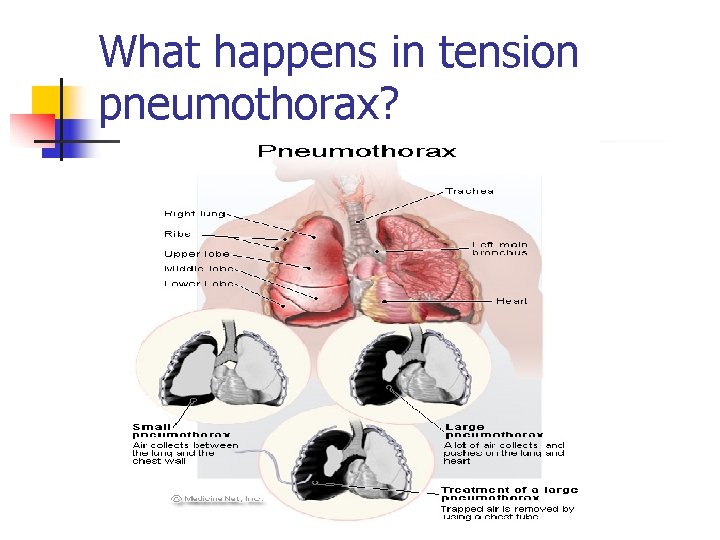
Pneumothorax
Pneumothorax n n Complete or partial collapse of a lung resulting from accumulation of air in the space between chest wall & lung (intrapleural space) May be classified as either “open” or “closed”
Diagnosis n Clinical Presentation -Diagnostics: Dyspenea -Clinical presentation & history n Pain -Chest x-ray n Decreased air movement on affected side (decreased breath sounds) n
Tension Pnuemothorax n Collection of air between chest wall & lung with no escape of air during expiration. This causes a rapid increase of air within pleural cavity, causing shifting of intrathoracic organs & increased intrathoracic pressure
Symptoms n n n Air hunger Violent agitation Cyanosis Tracheal deviation Subcutaneous emphysema
Treatment of Tension Pneumo n n Rapid Assessment! CT insertion Insertion of large-b ore needle to relieve intro-thoracic pressure Treatment of hypoxia
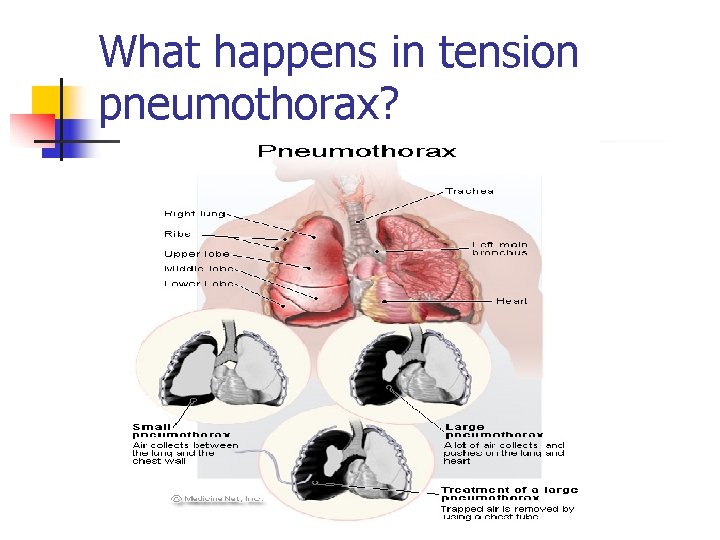
What happens in tension pneumothorax?

Infection
Mediastinitis n Infection of mediastinum resulting from inadequate healing after median sternotomy, potentially involving all structures of the mediastinum & chest wall
Treatment of Mediastinitis n n Appropriate antibiotic coverage Complete sternal resection Use of closed irrigation/drainage system Wound closure with muscle flap
Clinical Manifestations n n n Sternal dehiscene Purulent drainage Pain associated with chest motion Fever Leukocytosis + Wound cultures
Pathogenesis n All patients undergoing cardiac surgery especially when CPB is used are potential candidates for infection because of depressed inflammatory response & large exposure of blood elements to foreign materials which increases chances of contamination
Common Pathogens n n n Staph aureus Staph epidermis Gram negative bacteria Fungi Mixed flora
Risk Factors n n n Diabetes COPD Bilateral mammary Smoking Prolonged ventilation Obesity Age >70 Use of bone wax Chronic renal failure Long operative time Excessive use of cautery
Prevention n n n n Handwashing by staff Antiseptic pre-op soap showers by patient Careful trimming of skin hair just prior to surgery Aggressive treatment of elevated glucose in diabetic patients Maintenance of sterility during all invasive procedures Use of minimal amount of bone wax Judicious use of cautery Prophylactic antibiotics
Avoid n Bilateral IMA in patients with n n n n Diabetes COPD Immunosupperssion Morbid obesity Use of bone wax Indiscriminate use of cautery Cross contamination
 Cardiothoracic
Cardiothoracic Cardiothoracic surgeon salary
Cardiothoracic surgeon salary Role of scrub nurse
Role of scrub nurse Nurse logic ati
Nurse logic ati Emdr congres
Emdr congres Jacqueline deurloo
Jacqueline deurloo Was trinkt jacqueline
Was trinkt jacqueline Caso de jacqueline yañez
Caso de jacqueline yañez Jacqueline bijou
Jacqueline bijou Dr jacqueline chan
Dr jacqueline chan Detoxamin side effects
Detoxamin side effects Jacqueline greiner
Jacqueline greiner Jacqueline saburido
Jacqueline saburido Dr jacqueline wong
Dr jacqueline wong Jacqueline kerkhoffs
Jacqueline kerkhoffs Jacqueline pei
Jacqueline pei Dr jacqueline swanton
Dr jacqueline swanton Jacqueline conard
Jacqueline conard Dr jacqueline belter
Dr jacqueline belter Dr jacqueline watts
Dr jacqueline watts Glenville high school jacqueline bell
Glenville high school jacqueline bell Toula pronunciation
Toula pronunciation Jacqueline lagarde
Jacqueline lagarde Reggie stephey today
Reggie stephey today Andrea jacqueline serrano
Andrea jacqueline serrano Locomotion book summary
Locomotion book summary Jacqueline saburido
Jacqueline saburido Jacqueline riu blois
Jacqueline riu blois Reggie stephey
Reggie stephey Syllabus dienstverlening en producten
Syllabus dienstverlening en producten Peacock spider life cycle
Peacock spider life cycle Jacqueline conard
Jacqueline conard Jacqueline torgler
Jacqueline torgler Jacqueline besser
Jacqueline besser Jacqueline altieri
Jacqueline altieri Jacqueline emmons
Jacqueline emmons Dr jacqueline watson
Dr jacqueline watson Jacqueline westcott
Jacqueline westcott Jacqueline saburido 2018
Jacqueline saburido 2018 Jacqueline deurloo
Jacqueline deurloo Famille von paulus
Famille von paulus Programme tv ce soir toutes les chaines franaises
Programme tv ce soir toutes les chaines franaises Jacqueline keintzel
Jacqueline keintzel Jacqueline bichsel
Jacqueline bichsel Jacqueline saburido 2017
Jacqueline saburido 2017 Jacqueline nijenhuis
Jacqueline nijenhuis Jacqueline butcher
Jacqueline butcher Juyter lab
Juyter lab Teorema de chebyshev
Teorema de chebyshev Jacqueline westcott
Jacqueline westcott Dr. tachere
Dr. tachere Complications of myelofibrosis
Complications of myelofibrosis Post dated pregnancy complications
Post dated pregnancy complications Complications of bacterial meningitis
Complications of bacterial meningitis Light's criteria
Light's criteria Complications of asthma
Complications of asthma Septic arthritis complications
Septic arthritis complications Eswl complications
Eswl complications Complications after cesarean section
Complications after cesarean section Myoisitis
Myoisitis Heart failure complications
Heart failure complications Chess score syncope
Chess score syncope Complication of liver cirrhosis
Complication of liver cirrhosis Aspects of the setting
Aspects of the setting Colostomy nursing responsibilities
Colostomy nursing responsibilities Rapamune
Rapamune Complications of hydrocephalus
Complications of hydrocephalus Indications of tracheostomy
Indications of tracheostomy Ptmc complications
Ptmc complications Hyperlipidemia complications
Hyperlipidemia complications Arachnoiditis treatment
Arachnoiditis treatment Calcium infusion protocol
Calcium infusion protocol C section layers
C section layers Hypothyroidism complications
Hypothyroidism complications Kesselbachs plexus
Kesselbachs plexus Layer of episiotomy
Layer of episiotomy Septic arthritis complications
Septic arthritis complications Complications of eclampsia
Complications of eclampsia C section complications
C section complications Susibtable
Susibtable Iv site pain and swelling
Iv site pain and swelling Blood transfusion complications
Blood transfusion complications