Vigneshwar Kasirajan M D Division of Cardiothoracic Surgery




- Slides: 37
Vigneshwar Kasirajan, M. D. Division of Cardiothoracic Surgery
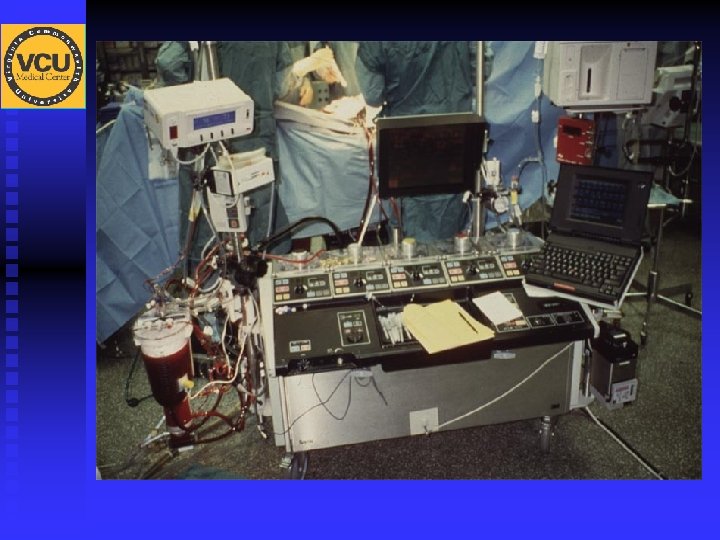
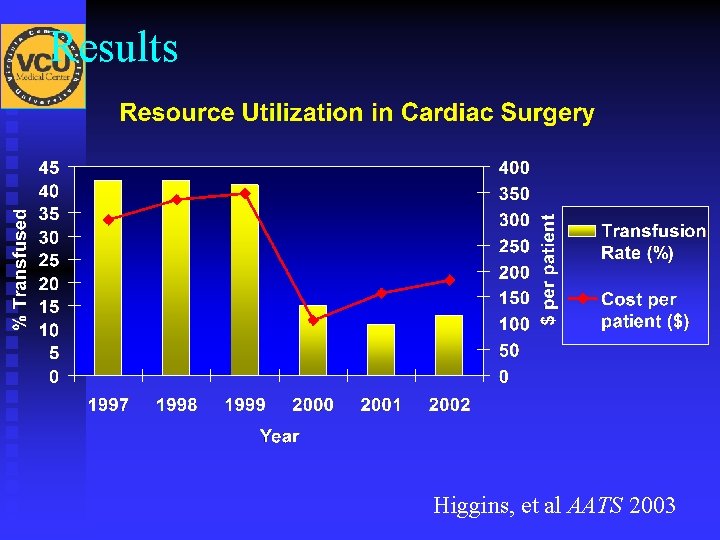
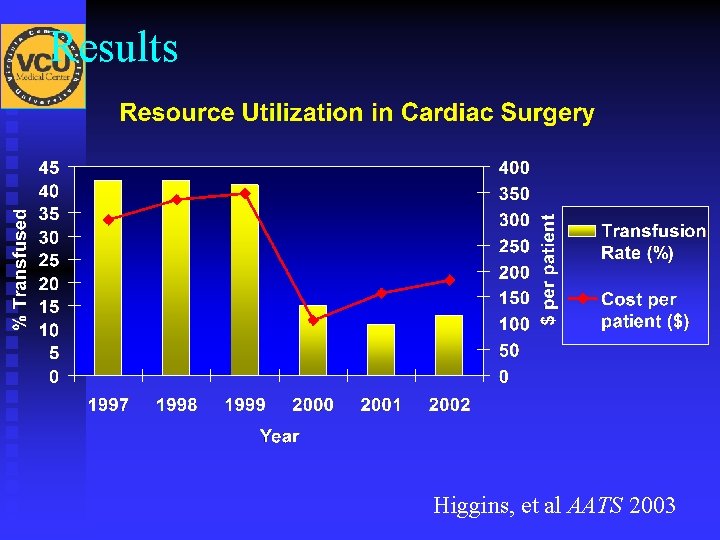
Results Higgins, et al AATS 2003
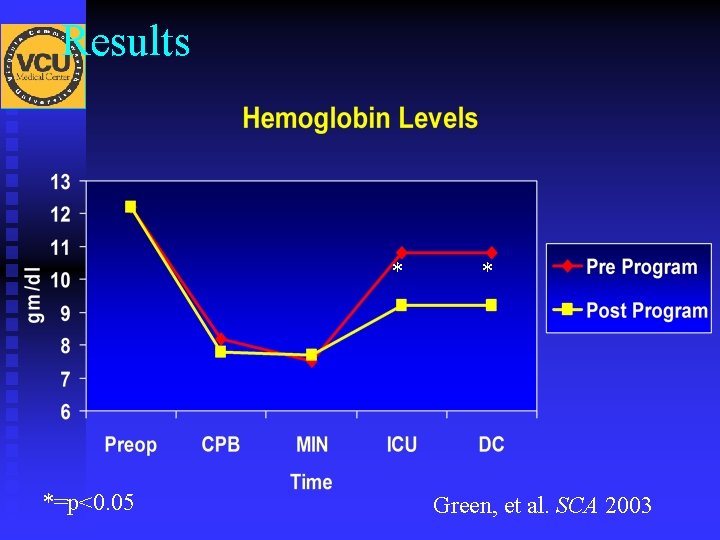
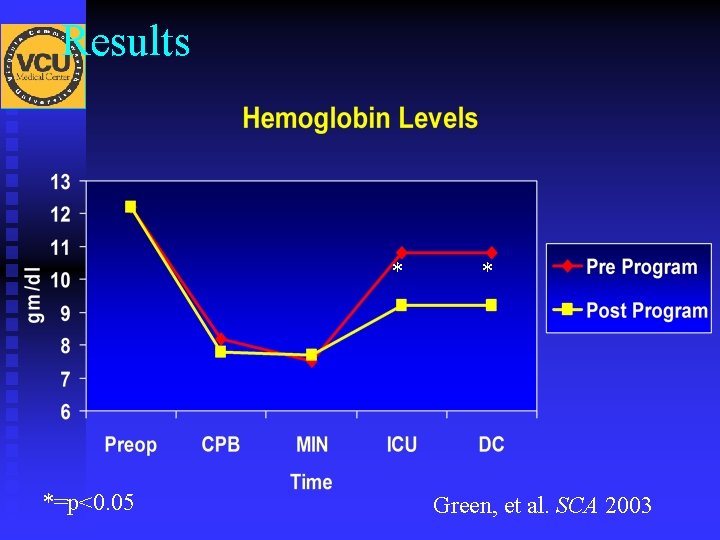
Results * *=p<0. 05 * Green, et al. SCA 2003
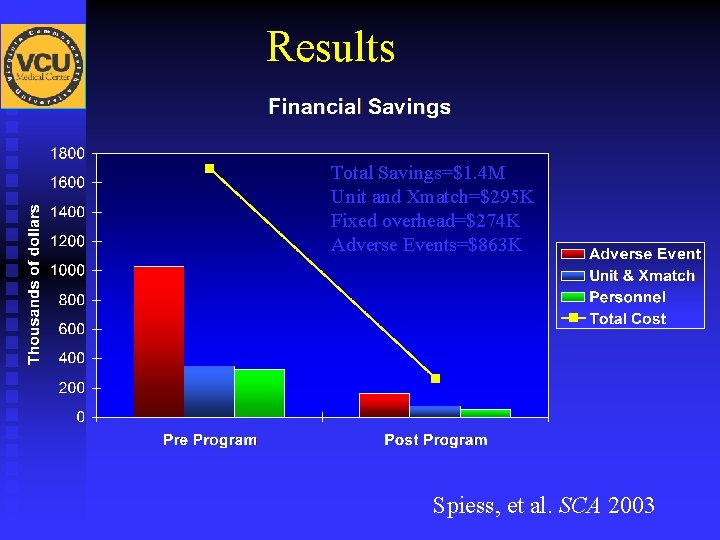
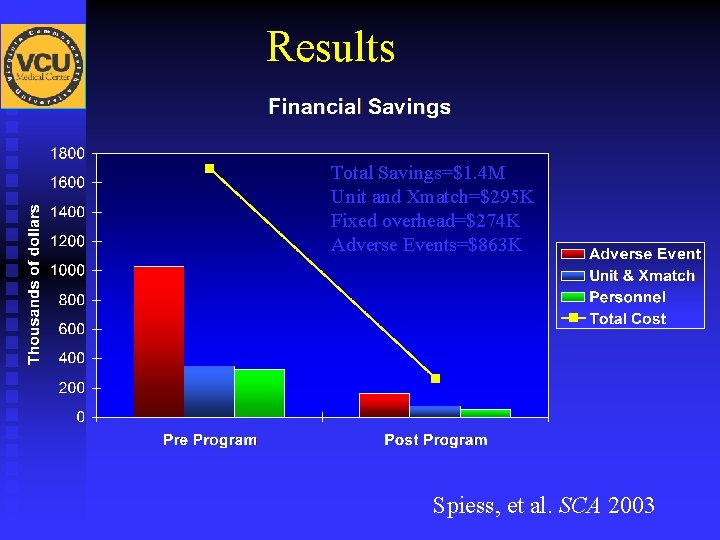
Results Total Savings=$1. 4 M Unit and Xmatch=$295 K Fixed overhead=$274 K Adverse Events=$863 K Spiess, et al. SCA 2003
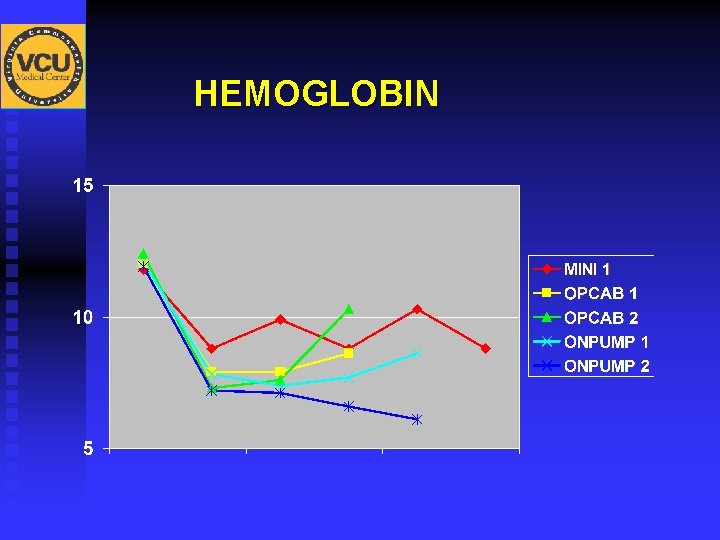
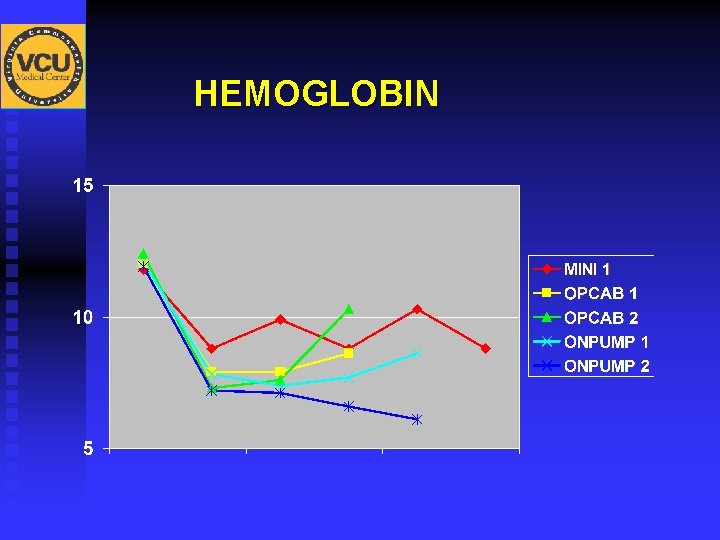
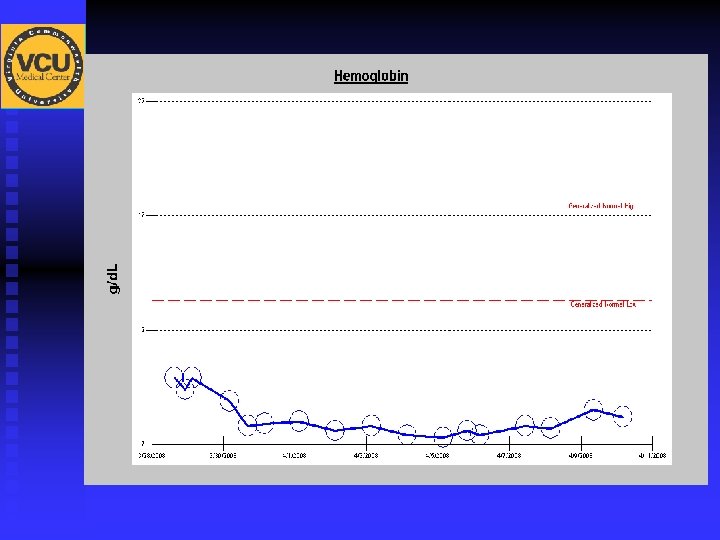
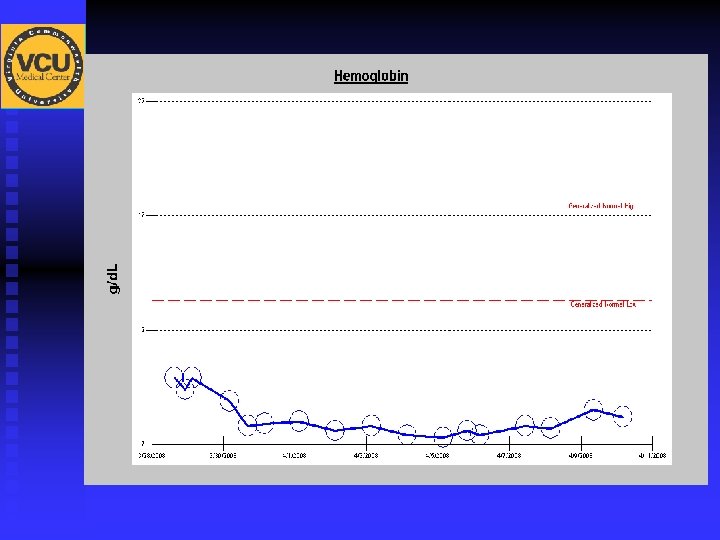
HEMOGLOBIN
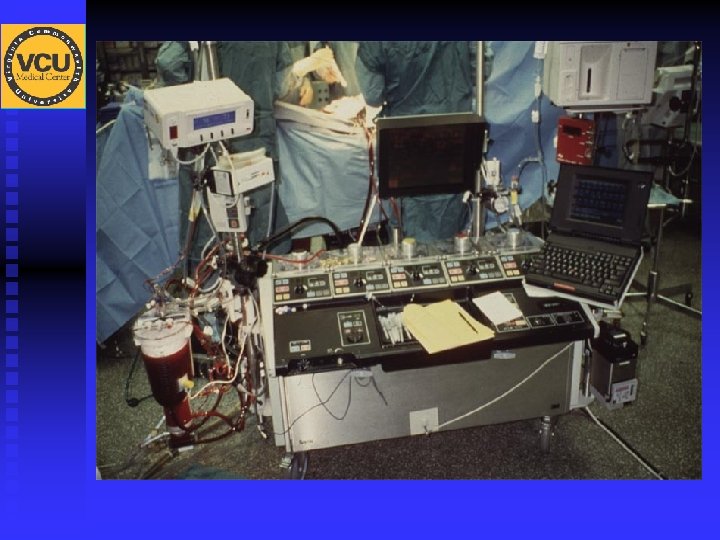
Retrograde Autologous Priming (RAP) Eight month data review at VCU MEDICAL CENTER November ’ 04 -June ‘ 05
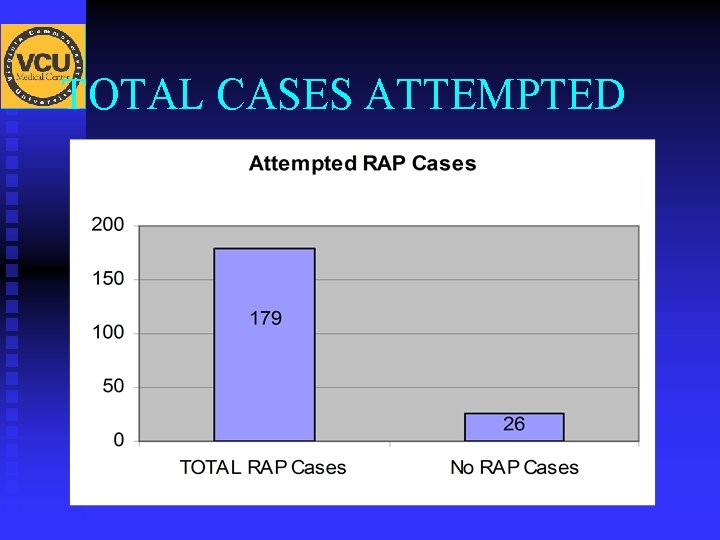
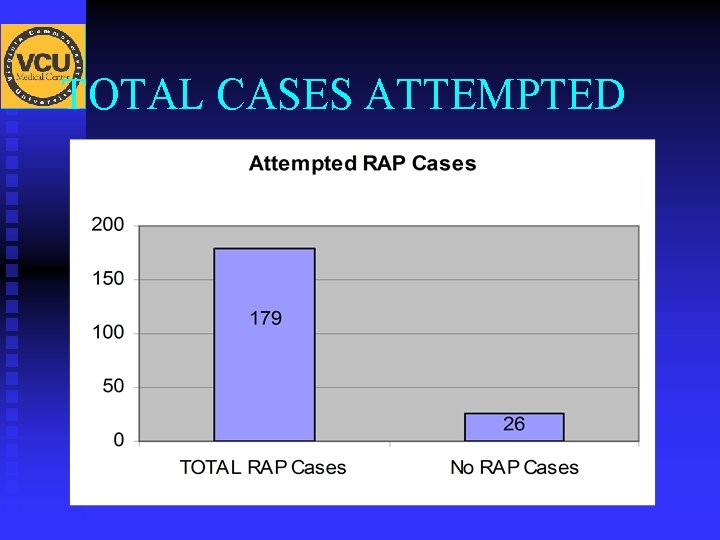
TOTAL CASES ATTEMPTED
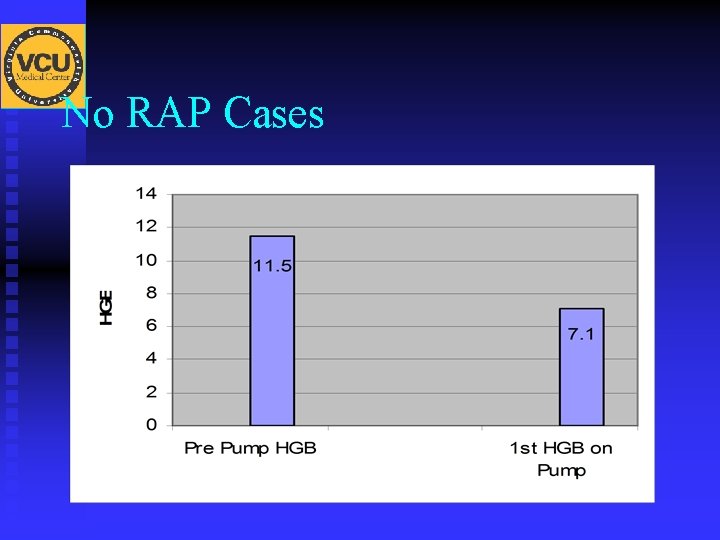
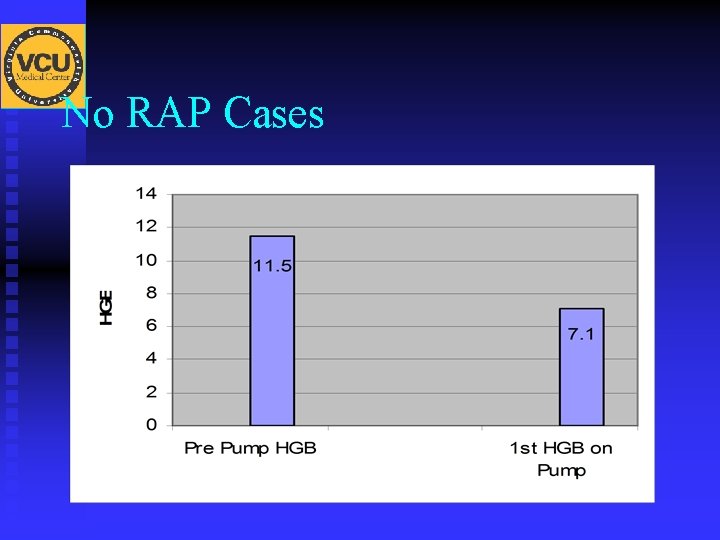
No RAP Cases
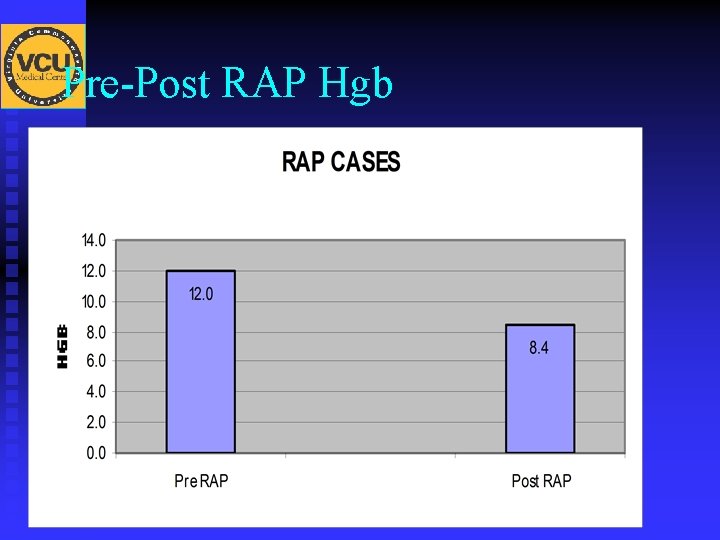
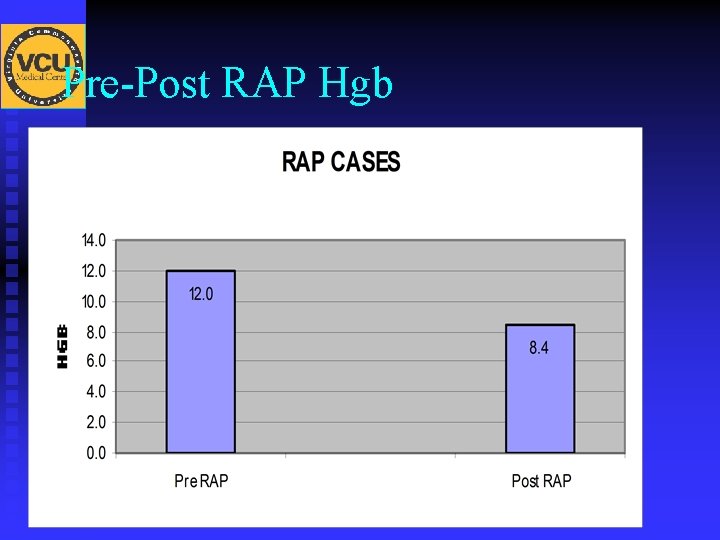
Pre-Post RAP Hgb
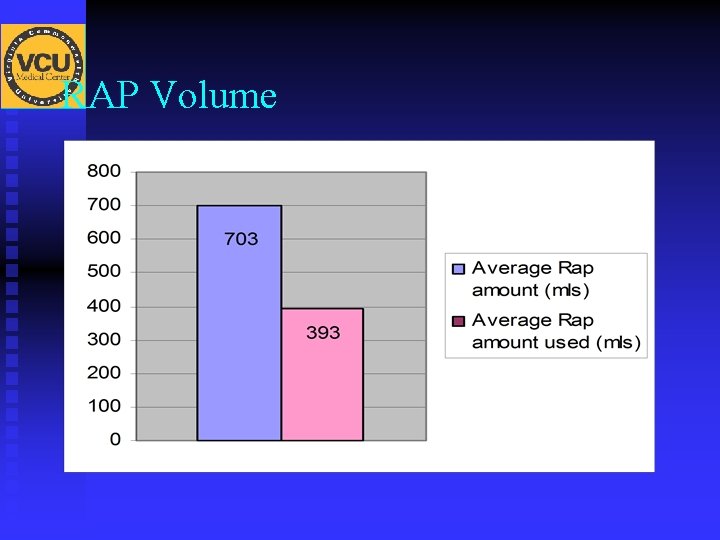
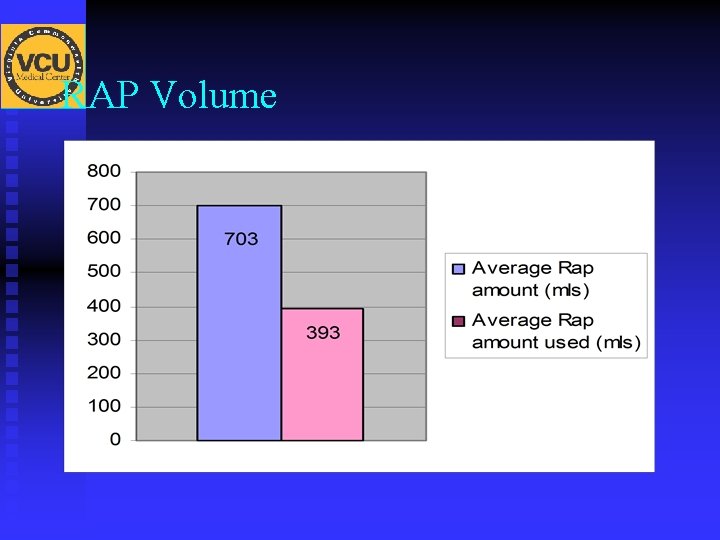
RAP Volume
AUTOLOGOUS BLOOD OFF BY ANESTHESIA AFTER INDUCTION AVERAGED 516 mls.
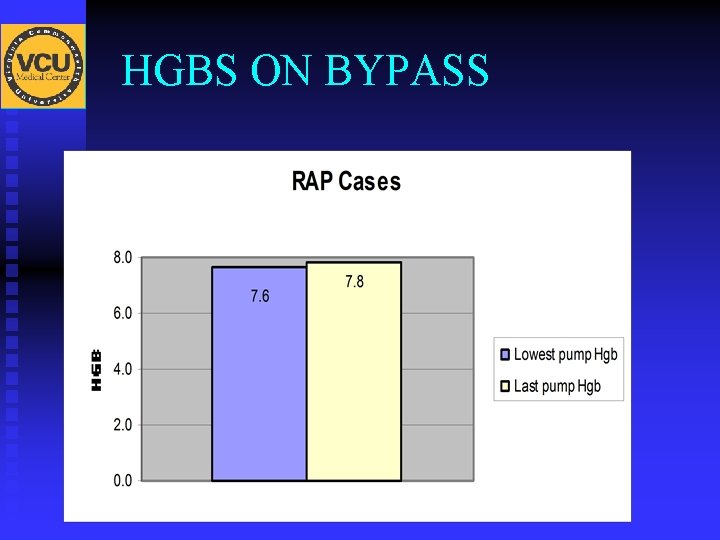
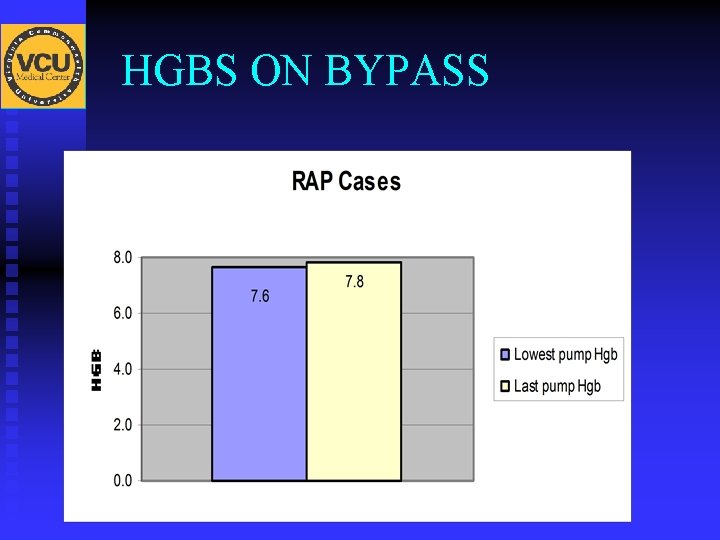
HGBS ON BYPASS

PATIENT’S HGB AFTER ARRIVING TO ICU AVERAGED 10. 2 g/dl
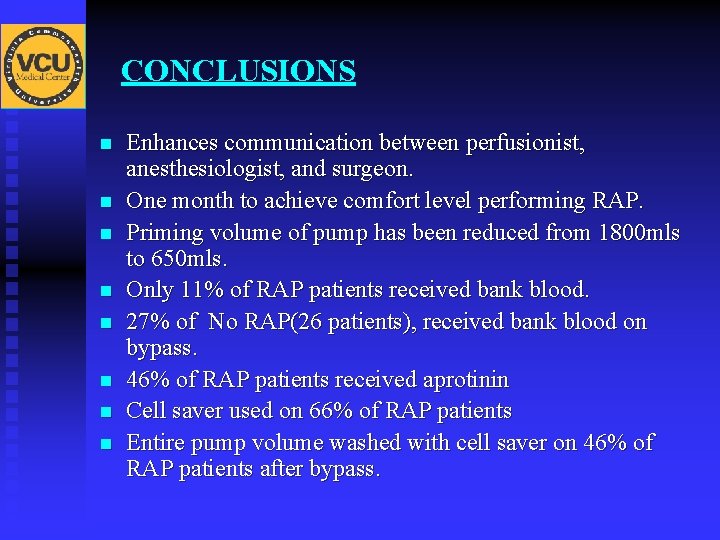
CONCLUSIONS n n n n Enhances communication between perfusionist, anesthesiologist, and surgeon. One month to achieve comfort level performing RAP. Priming volume of pump has been reduced from 1800 mls to 650 mls. Only 11% of RAP patients received bank blood. 27% of No RAP(26 patients), received bank blood on bypass. 46% of RAP patients received aprotinin Cell saver used on 66% of RAP patients Entire pump volume washed with cell saver on 46% of RAP patients after bypass.
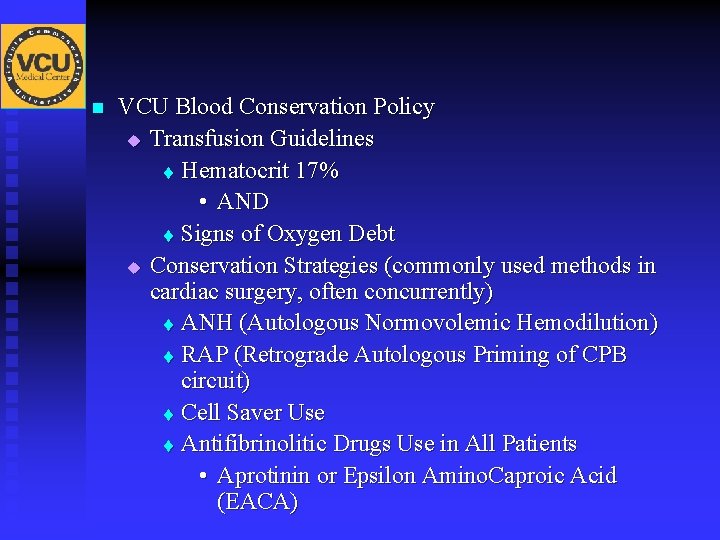
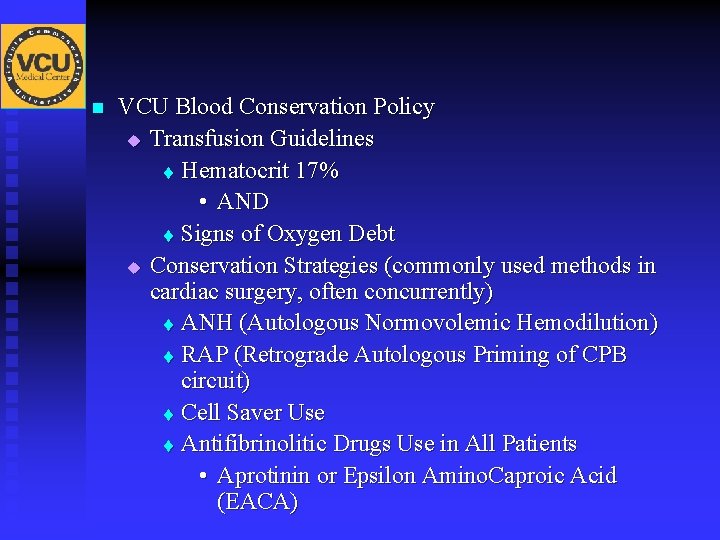
n VCU Blood Conservation Policy u Transfusion Guidelines t Hematocrit 17% • AND t Signs of Oxygen Debt u Conservation Strategies (commonly used methods in cardiac surgery, often concurrently) t ANH (Autologous Normovolemic Hemodilution) t RAP (Retrograde Autologous Priming of CPB circuit) t Cell Saver Use t Antifibrinolitic Drugs Use in All Patients • Aprotinin or Epsilon Amino. Caproic Acid (EACA)
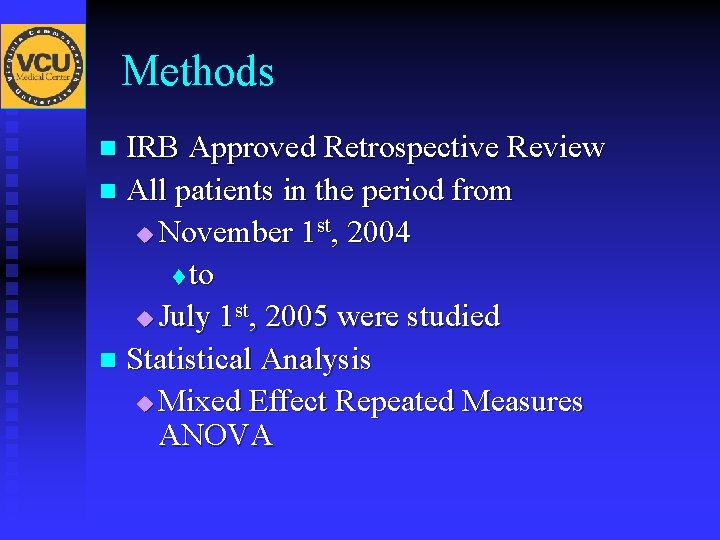
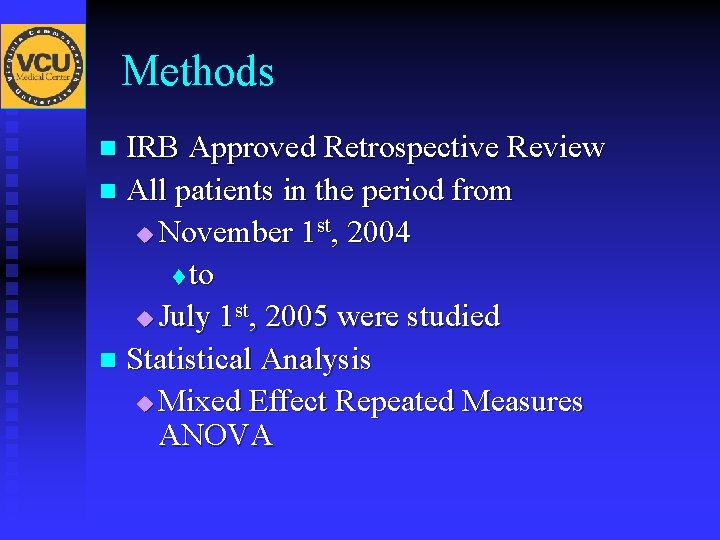
Methods IRB Approved Retrospective Review n All patients in the period from u November 1 st, 2004 t to u July 1 st, 2005 were studied n Statistical Analysis u Mixed Effect Repeated Measures ANOVA n
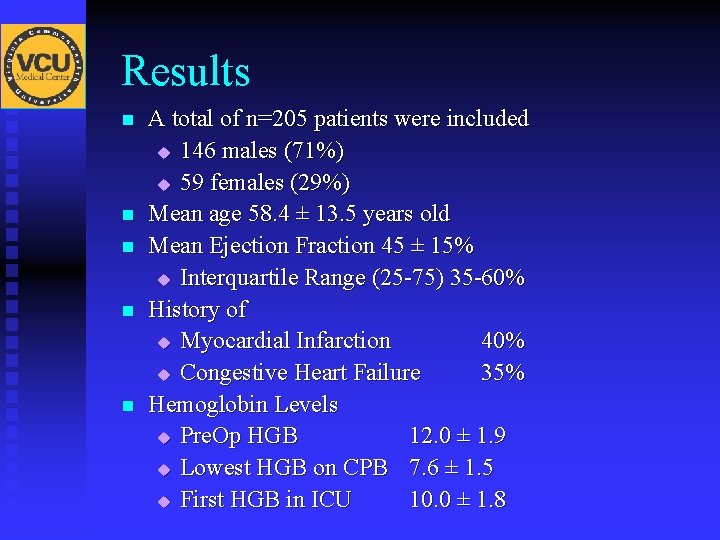
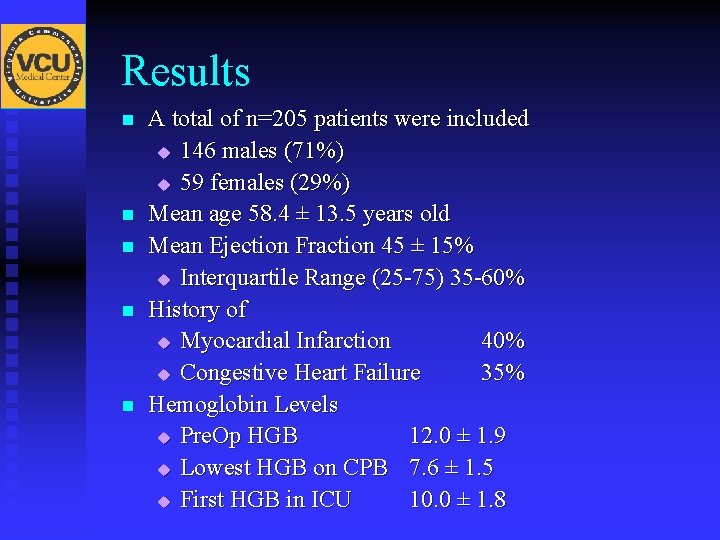
Results n n n A total of n=205 patients were included u 146 males (71%) u 59 females (29%) Mean age 58. 4 ± 13. 5 years old Mean Ejection Fraction 45 ± 15% u Interquartile Range (25 -75) 35 -60% History of u Myocardial Infarction 40% u Congestive Heart Failure 35% Hemoglobin Levels u Pre. Op HGB 12. 0 ± 1. 9 u Lowest HGB on CPB 7. 6 ± 1. 5 u First HGB in ICU 10. 0 ± 1. 8
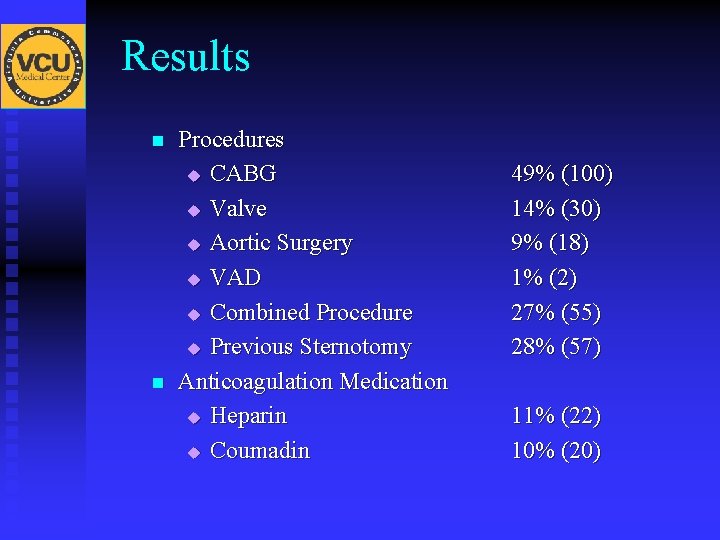
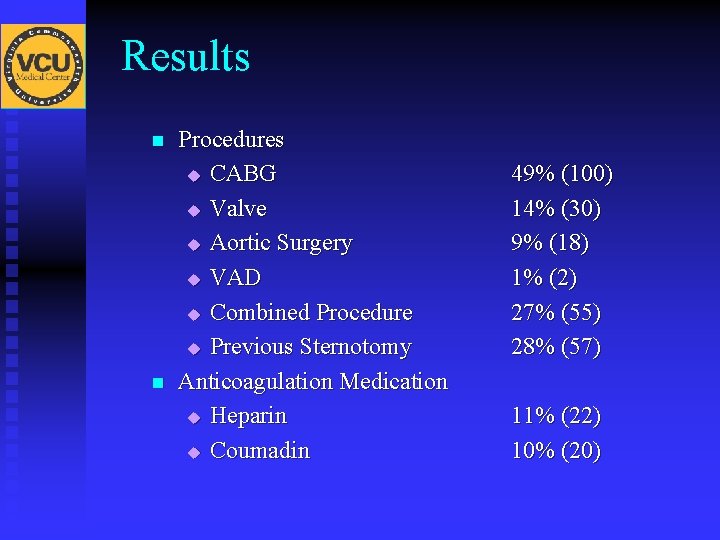
Results n n Procedures u CABG u Valve u Aortic Surgery u VAD u Combined Procedure u Previous Sternotomy Anticoagulation Medication u Heparin u Coumadin 49% (100) 14% (30) 9% (18) 1% (2) 27% (55) 28% (57) 11% (22) 10% (20)
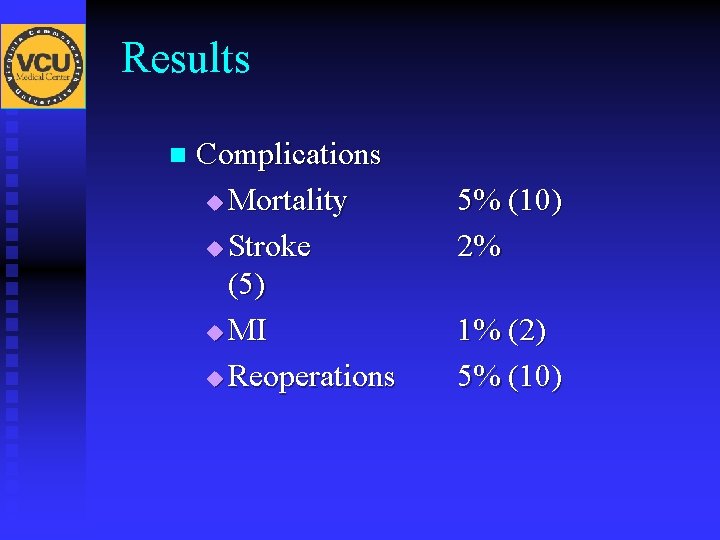
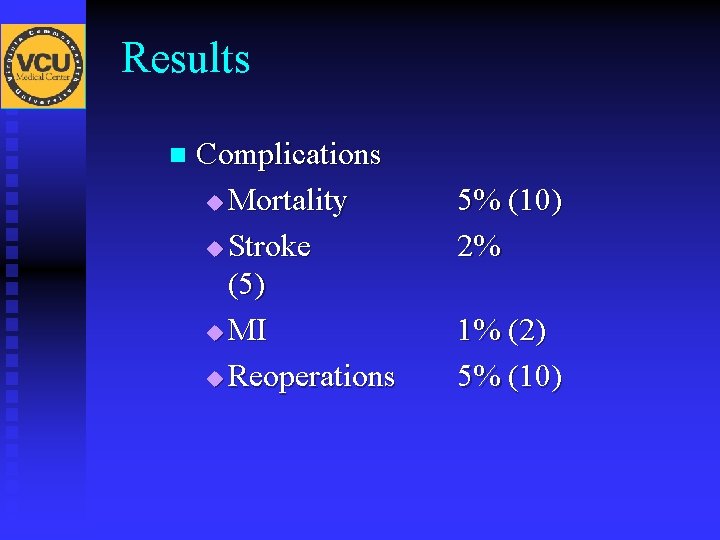
Results n Complications u Mortality u Stroke (5) u MI u Reoperations 5% (10) 2% 1% (2) 5% (10)
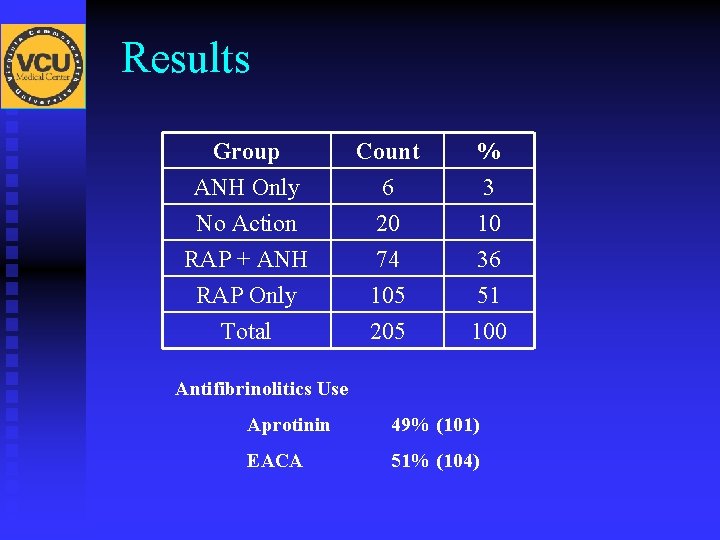
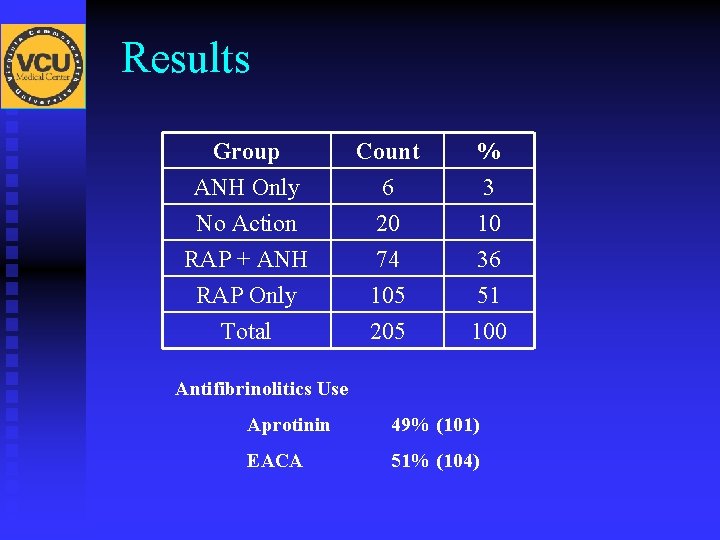
Results Group ANH Only No Action RAP + ANH Count 6 20 74 % 3 10 36 RAP Only Total 105 205 51 100 Antifibrinolitics Use Aprotinin 49% (101) EACA 51% (104)
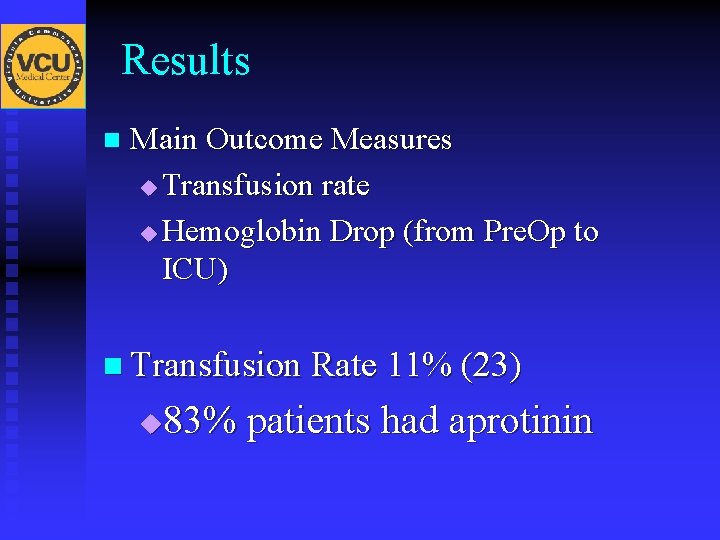
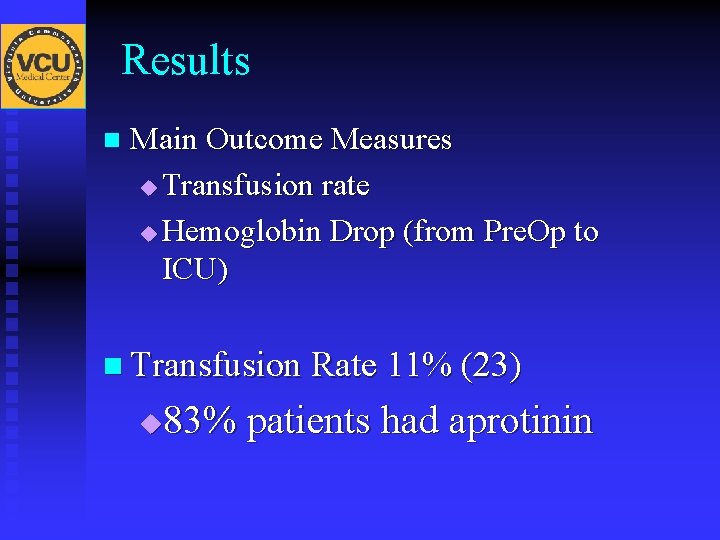
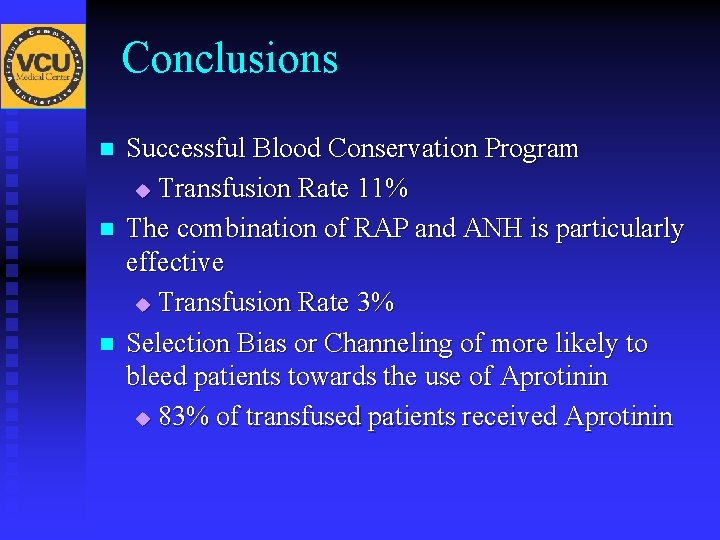
Results n Main Outcome Measures u Transfusion rate u Hemoglobin Drop (from Pre. Op to ICU) n Transfusion Rate 11% (23) 83% patients had aprotinin u
Results n Blood Conservation Maneuver Groups
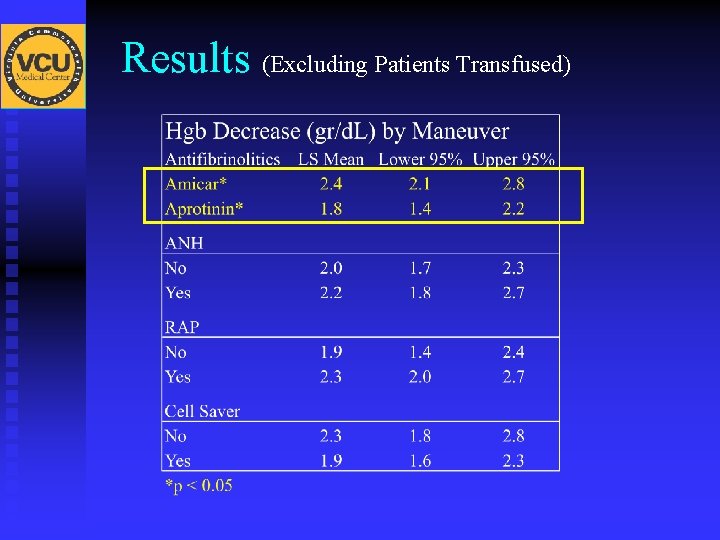
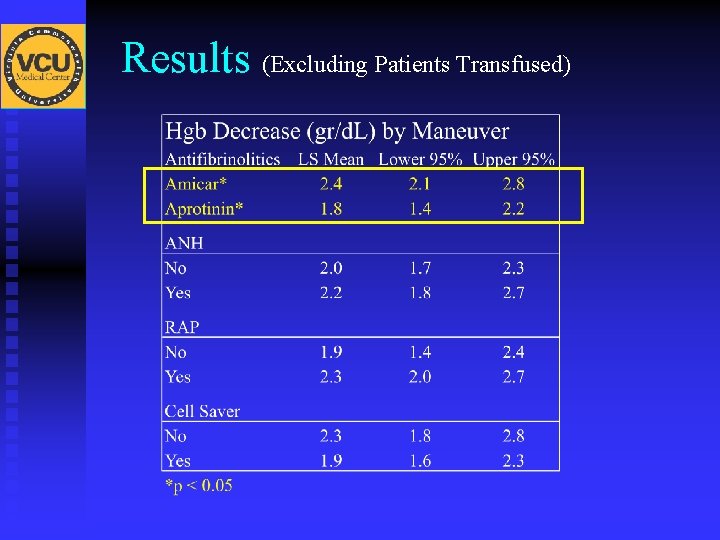
Results (Excluding Patients Transfused)
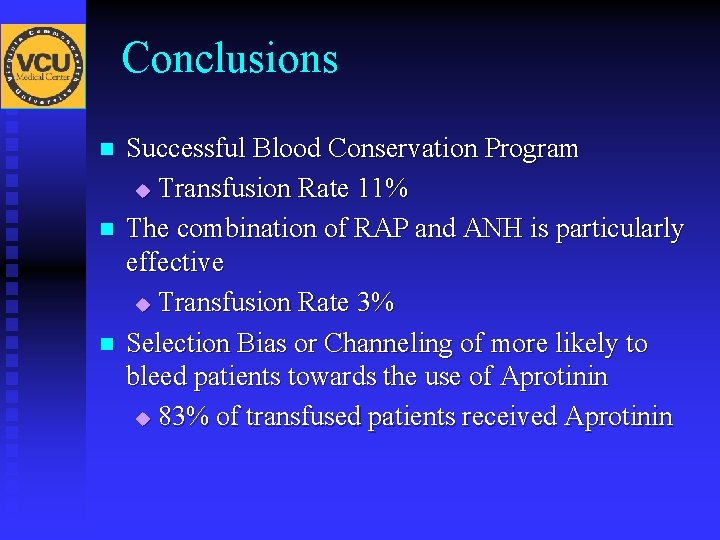
Conclusions n n n Successful Blood Conservation Program u Transfusion Rate 11% The combination of RAP and ANH is particularly effective u Transfusion Rate 3% Selection Bias or Channeling of more likely to bleed patients towards the use of Aprotinin u 83% of transfused patients received Aprotinin
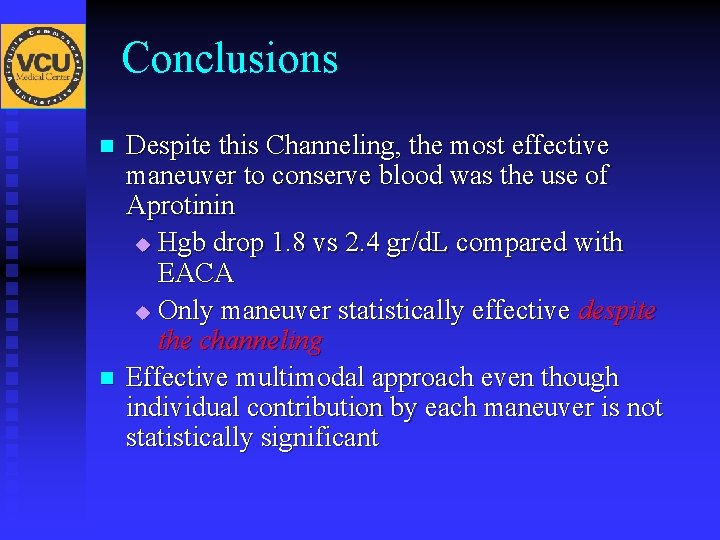
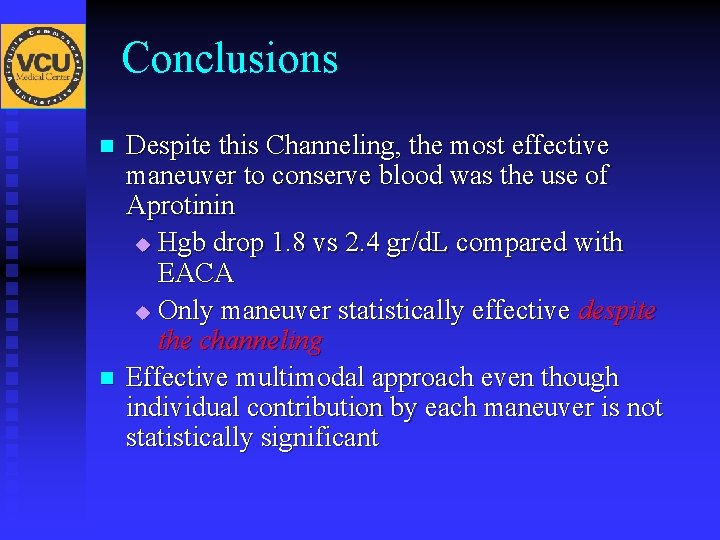
Conclusions n n Despite this Channeling, the most effective maneuver to conserve blood was the use of Aprotinin u Hgb drop 1. 8 vs 2. 4 gr/d. L compared with EACA u Only maneuver statistically effective despite the channeling Effective multimodal approach even though individual contribution by each maneuver is not statistically significant
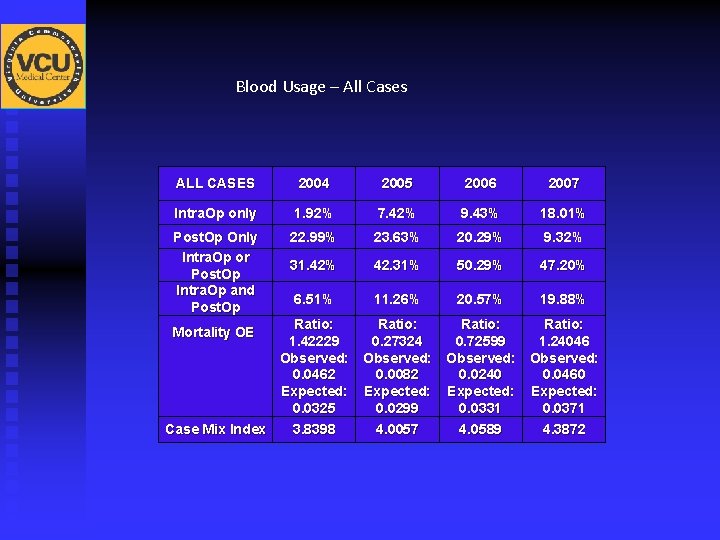
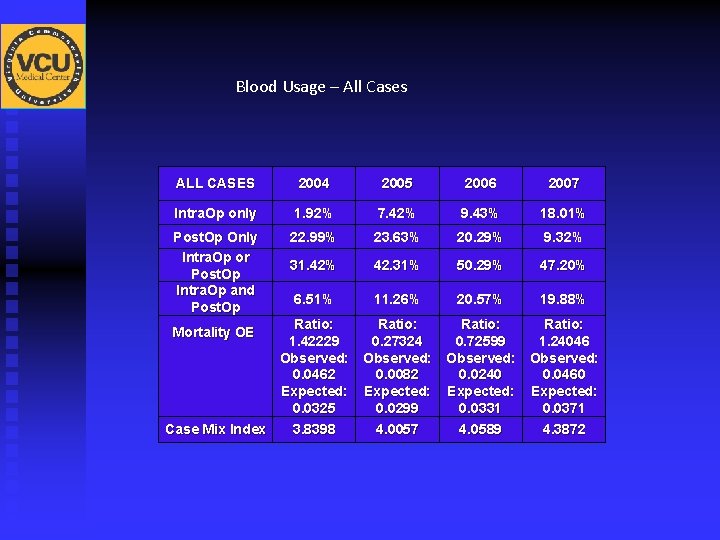
Blood Usage – All Cases ALL CASES 2004 2005 2006 2007 Intra. Op only 1. 92% 7. 42% 9. 43% 18. 01% Post. Op Only Intra. Op or Post. Op Intra. Op and Post. Op 22. 99% 23. 63% 20. 29% 9. 32% 31. 42% 42. 31% 50. 29% 47. 20% 6. 51% 11. 26% 20. 57% 19. 88% Ratio: 1. 42229 0. 27324 0. 72599 1. 24046 Observed: 0. 0462 0. 0082 0. 0240 0. 0460 Expected: 0. 0325 0. 0299 0. 0331 0. 0371 Case Mix Index 3. 8398 4. 0057 4. 0589 4. 3872 Mortality OE
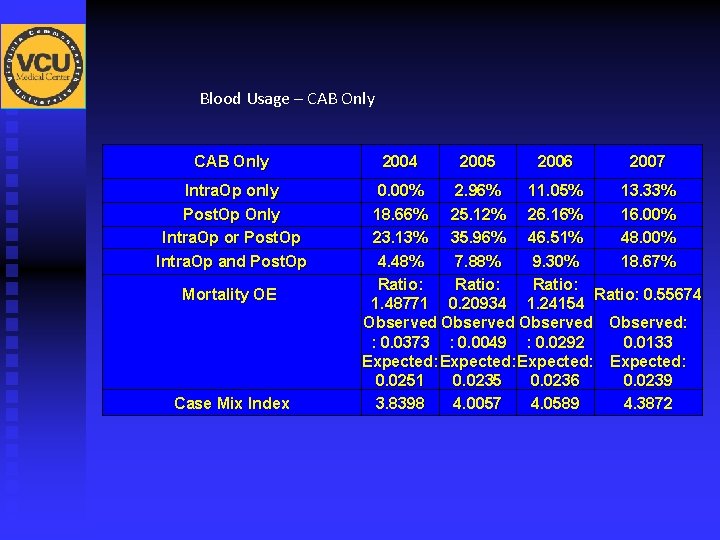
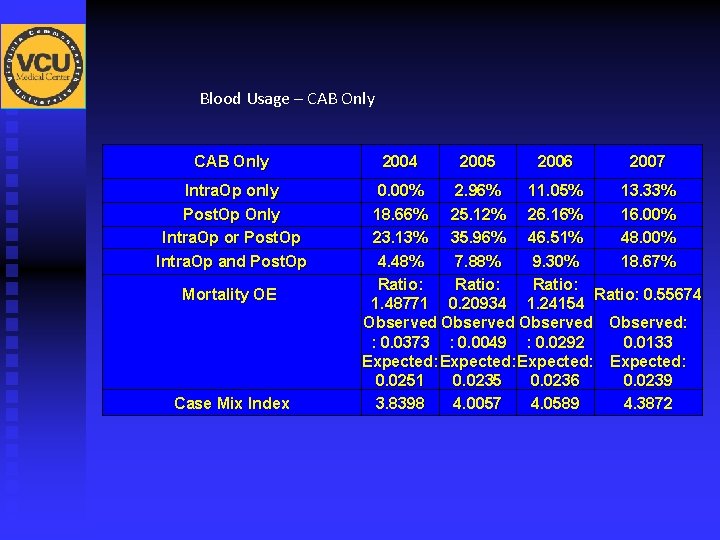
Blood Usage – CAB Only Intra. Op only Post. Op Only Intra. Op or Post. Op Intra. Op and Post. Op Mortality OE Case Mix Index 2004 2005 2006 2007 0. 00% 2. 96% 11. 05% 13. 33% 18. 66% 25. 12% 26. 16% 16. 00% 23. 13% 35. 96% 46. 51% 48. 00% 4. 48% 7. 88% 9. 30% 18. 67% Ratio: 0. 55674 1. 48771 0. 20934 1. 24154 Observed: : 0. 0373 : 0. 0049 : 0. 0292 0. 0133 Expected: 0. 0251 0. 0235 0. 0236 0. 0239 3. 8398 4. 0057 4. 0589 4. 3872
POST CABG COMPLICATIONS
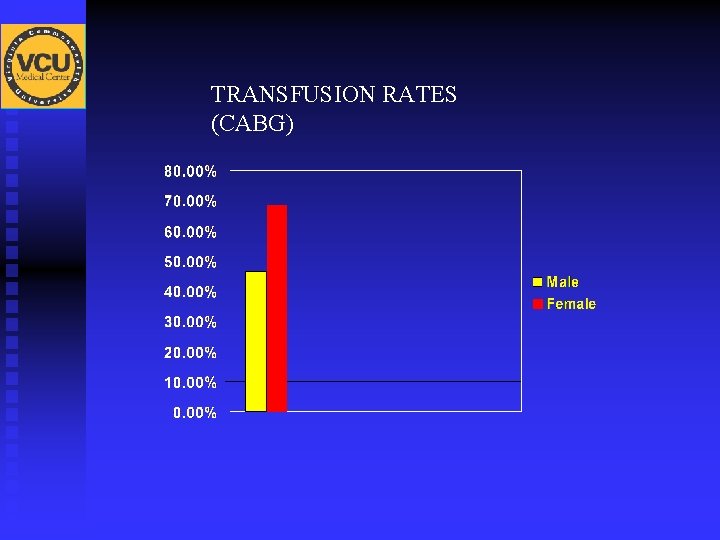
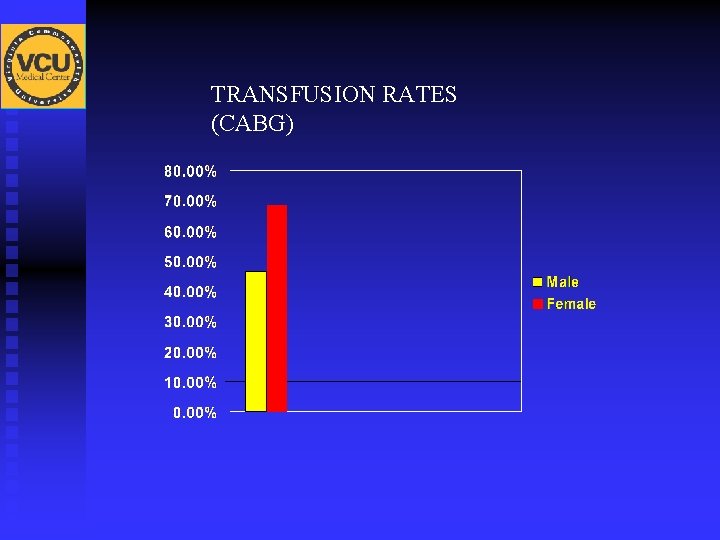
TRANSFUSION RATES (CABG)

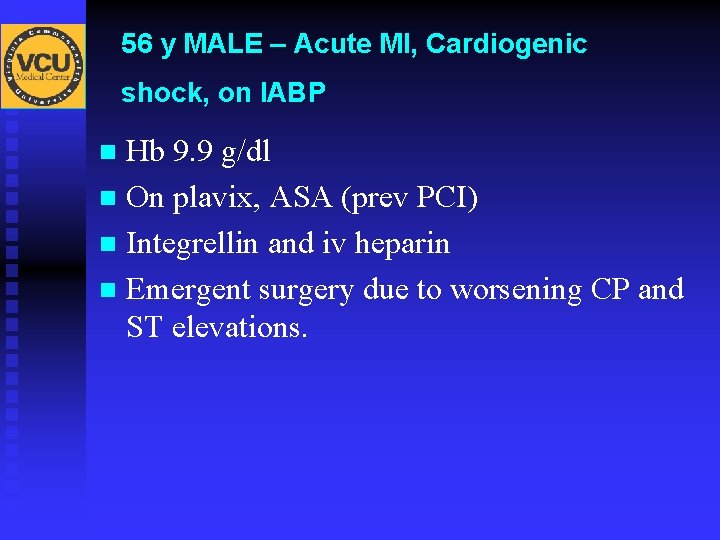
56 y MALE – Acute MI, Cardiogenic shock, on IABP Hb 9. 9 g/dl n On plavix, ASA (prev PCI) n Integrellin and iv heparin n Emergent surgery due to worsening CP and ST elevations. n

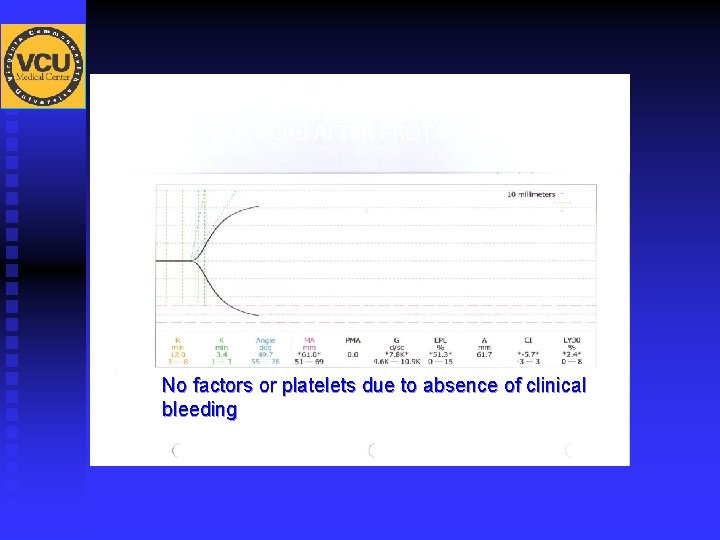
TEG PRE CPB

Hb 6. 0 – 1 prbc Hb < 5 – 2 prbcs
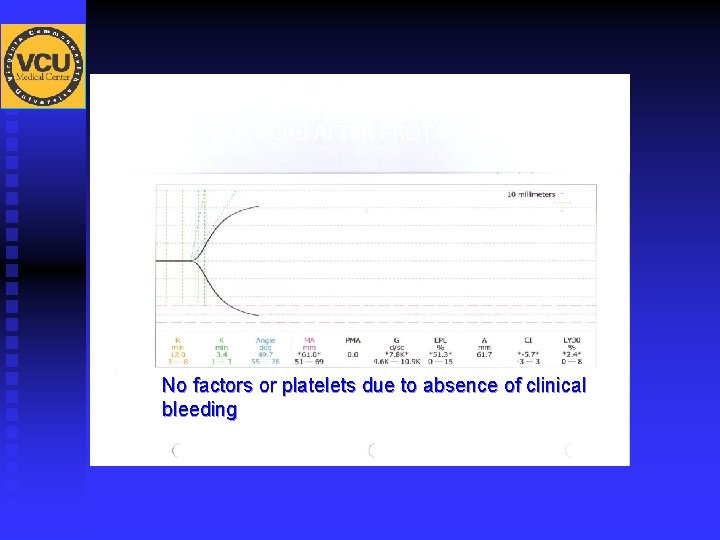
TEG POST CPB AFTER PROTAMINE No factors or platelets due to absence of clinical bleeding
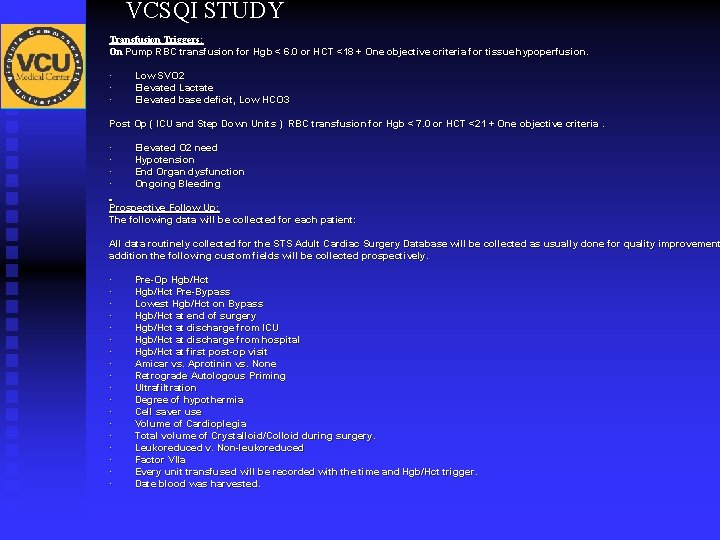
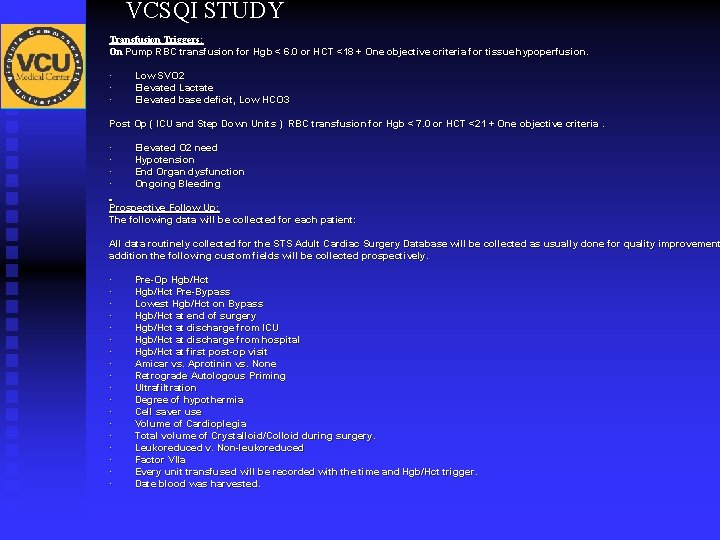
VCSQI STUDY Transfusion Triggers: On Pump RBC transfusion for Hgb < 6. 0 or HCT <18 + One objective criteria for tissue hypoperfusion. · · · Low SVO 2 Elevated Lactate Elevated base deficit, Low HCO 3 Post Op ( ICU and Step Down Units ) RBC transfusion for Hgb < 7. 0 or HCT <21 + One objective criteria. · · Elevated O 2 need Hypotension End Organ dysfunction Ongoing Bleeding Prospective Follow Up: The following data will be collected for each patient: All data routinely collected for the STS Adult Cardiac Surgery Database will be collected as usually done for quality improvement addition the following custom fields will be collected prospectively. · · · · · Pre-Op Hgb/Hct Pre-Bypass Lowest Hgb/Hct on Bypass Hgb/Hct at end of surgery Hgb/Hct at discharge from ICU Hgb/Hct at discharge from hospital Hgb/Hct at first post-op visit Amicar vs. Aprotinin vs. None Retrograde Autologous Priming Ultrafiltration Degree of hypothermia Cell saver use Volume of Cardioplegia Total volume of Crystalloid/Colloid during surgery. Leukoreduced v. Non-leukoreduced Factor VIIa Every unit transfused will be recorded with the time and Hgb/Hct trigger. Date blood was harvested.
 Cardiothoracic surgeon salary
Cardiothoracic surgeon salary Cardiothoracic
Cardiothoracic Short division vs long division
Short division vs long division Synthetic division examples
Synthetic division examples Division key vocabulary
Division key vocabulary Synthetic dividion
Synthetic dividion Shuochao yao
Shuochao yao Chafford hundred medical centre online login
Chafford hundred medical centre online login Moat shared ownership
Moat shared ownership Surgery etymology
Surgery etymology Wrong site surgery prevention
Wrong site surgery prevention Time out steps
Time out steps Nagpal surgery
Nagpal surgery Post lasik iol power calculation ppt
Post lasik iol power calculation ppt Lateral position
Lateral position Strabismus perth
Strabismus perth Milada cosmetic surgery hospital
Milada cosmetic surgery hospital Sbk surgery
Sbk surgery Anesthesia for bariatric surgery
Anesthesia for bariatric surgery Wound classification surgery
Wound classification surgery Bariatrc surgery
Bariatrc surgery Early recovery after surgery
Early recovery after surgery Umass memorial pharmacy residency
Umass memorial pharmacy residency Dunchurch surgery
Dunchurch surgery Who discovered plastic surgery
Who discovered plastic surgery Guided surgery flap
Guided surgery flap Carla bruni surgery
Carla bruni surgery Intermediate-risk surgery list
Intermediate-risk surgery list Robot assisted surgery
Robot assisted surgery Rectory meadow surgery
Rectory meadow surgery Bypass graft surgery
Bypass graft surgery Gabriel sharma
Gabriel sharma Chapter 56 oral and maxillofacial surgery
Chapter 56 oral and maxillofacial surgery Ecbd surgery
Ecbd surgery Stages of damage control surgery
Stages of damage control surgery Cyle williams
Cyle williams Dr tracy robinson
Dr tracy robinson Woolbridge surgery
Woolbridge surgery