General Thoracic Surgery CardioThoracic Department Papworth Hospital University








- Slides: 71
General Thoracic Surgery Cardio-Thoracic Department Papworth Hospital University of Cambridge Hospital Trust Cambridge, UK Phase III Lecture Programme Oncology lung cancer Marcello Migliore
History In 1910 Alton Oschner, esteemed surgeon, recalled that as a student at Washington University he was asked to witness an autopsy of a patient with lung cancer, having been told lung cancer was so rare that he may never see another case. He saw the next case 17 years later. Within the next 6 months 8 more cases were seen at that hospital and this began what he called an epidemic.

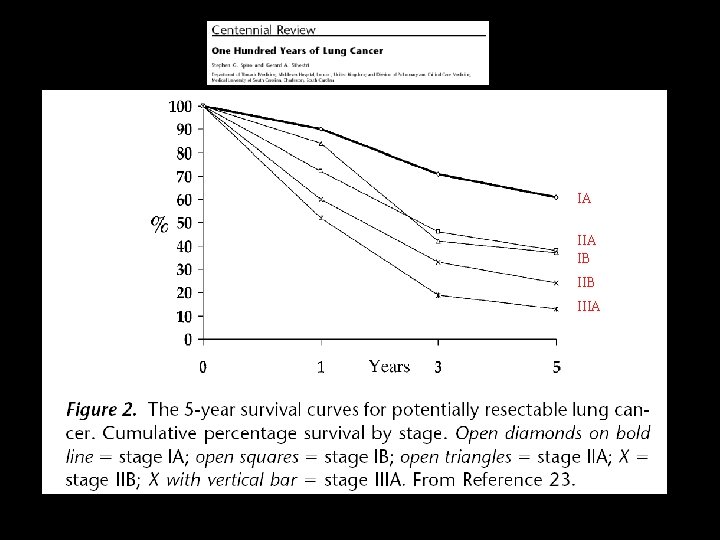
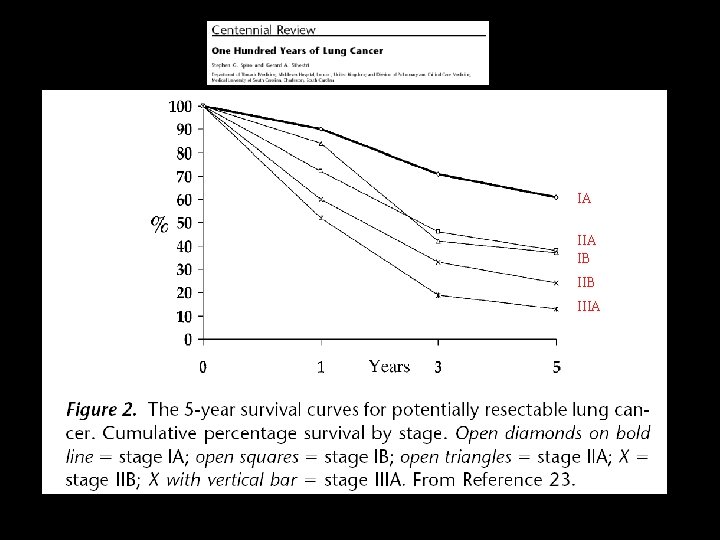
IA IB IIIA
Epidemiology • 1950 Doll and Hill in the British Medical Journal confirmed suspicions that lung cancer was associated with cigarette smoking
Epidemiology • In 1930 in the USA, lung cancer rates were less than 5 per 100, 000 • In 1998 the death rate per 100, 000 population for men reached 77. 2 in Belgium and 75. 5 in Scotland.
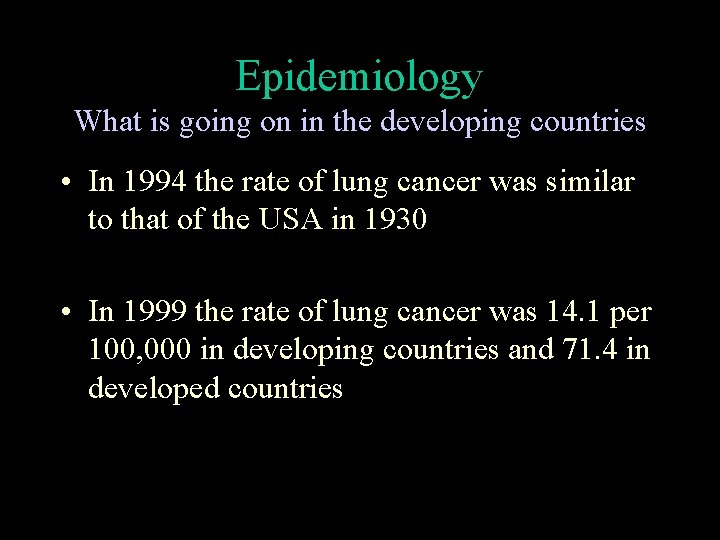
Epidemiology What is going on in the developing countries • In 1994 the rate of lung cancer was similar to that of the USA in 1930 • In 1999 the rate of lung cancer was 14. 1 per 100, 000 in developing countries and 71. 4 in developed countries


Lung cancer Only 25% of patients will undergo surgery with the hope of curing the disease Most 75% will not have surgery
Lung cancer c p TNM

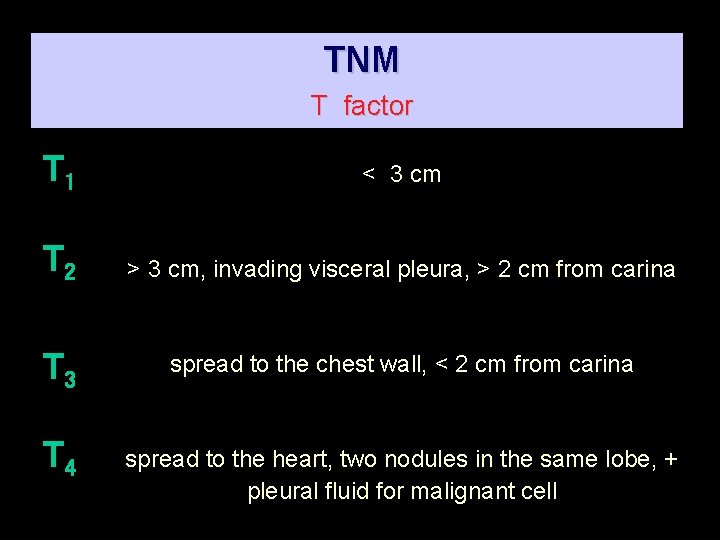
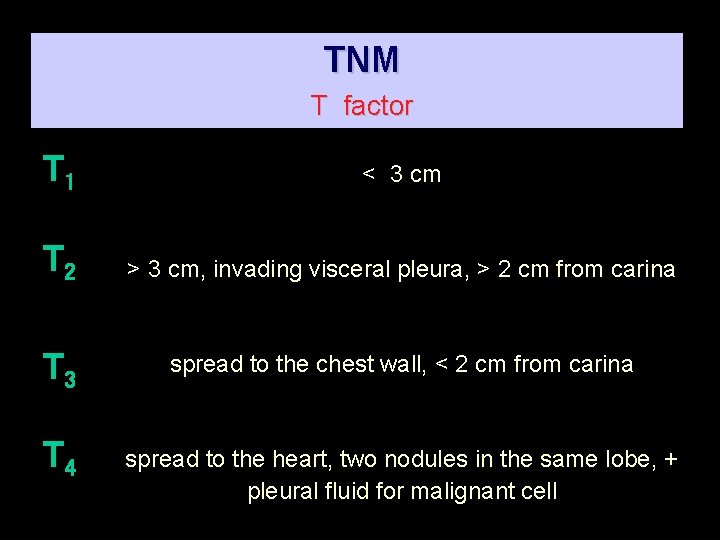
TNM T factor T 1 < 3 cm T 2 > 3 cm, invading visceral pleura, > 2 cm from carina T 3 spread to the chest wall, < 2 cm from carina T 4 spread to the heart, two nodules in the same lobe, + pleural fluid for malignant cell
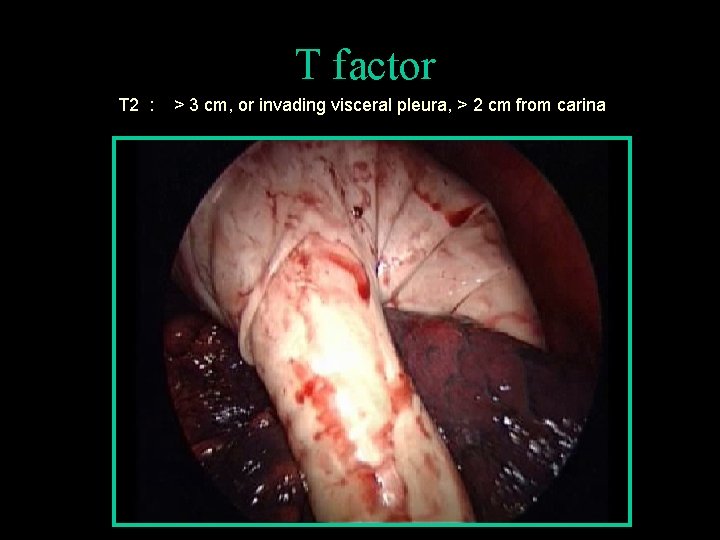
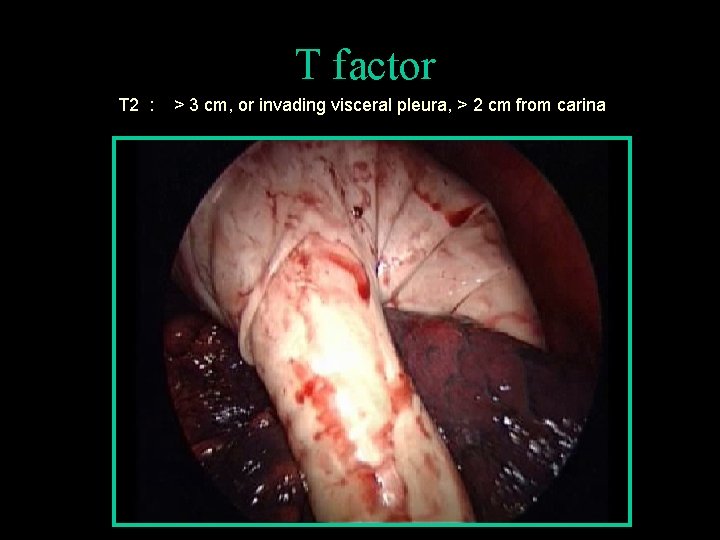
T factor T 2 : > 3 cm, or invading visceral pleura, > 2 cm from carina
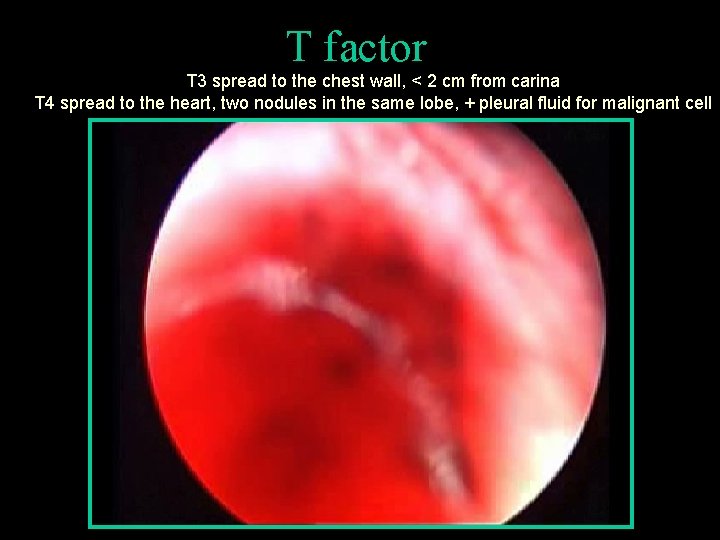
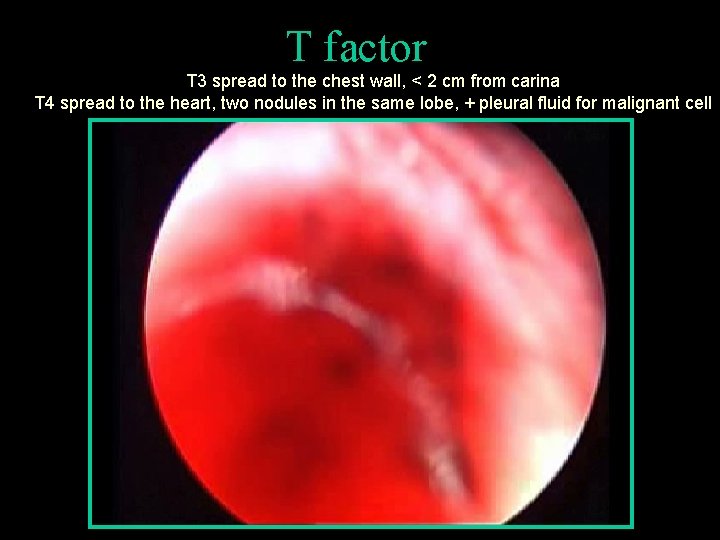
T factor T 3 spread to the chest wall, < 2 cm from carina T 4 spread to the heart, two nodules in the same lobe, + pleural fluid for malignant cell
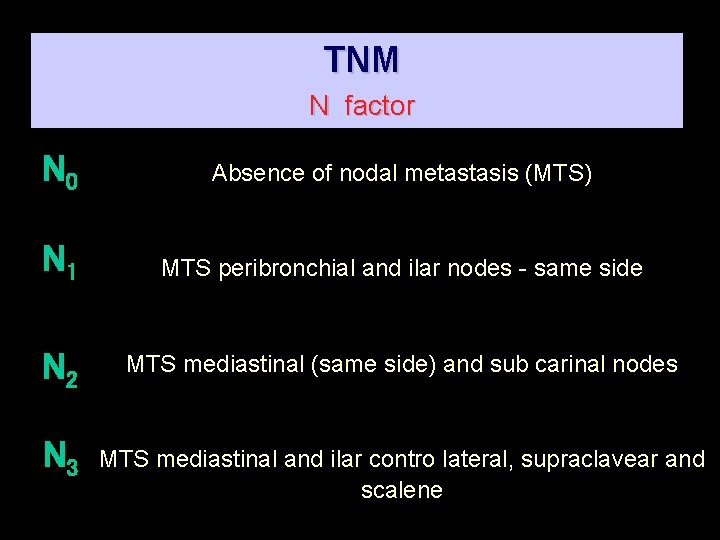
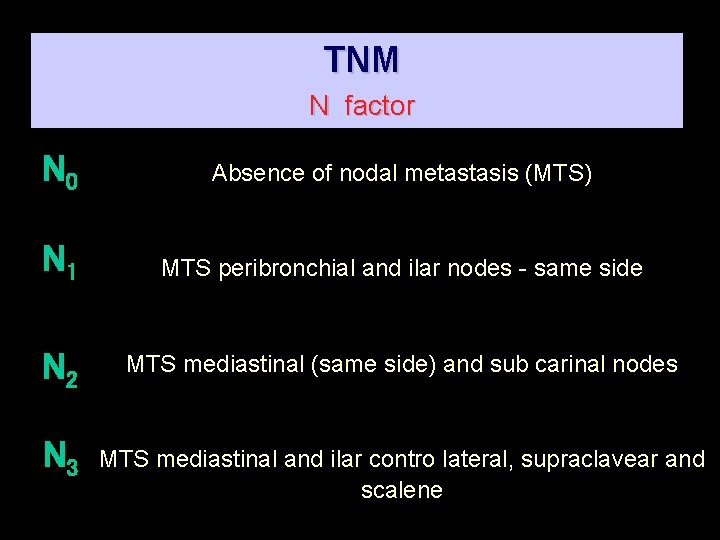
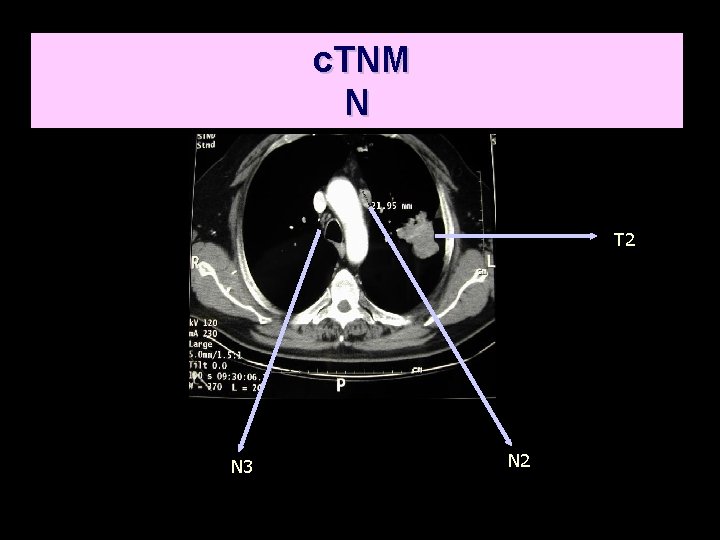
TNM N factor N 0 Absence of nodal metastasis (MTS) N 1 MTS peribronchial and ilar nodes - same side N 2 MTS mediastinal (same side) and sub carinal nodes N 3 MTS mediastinal and ilar contro lateral, supraclavear and scalene
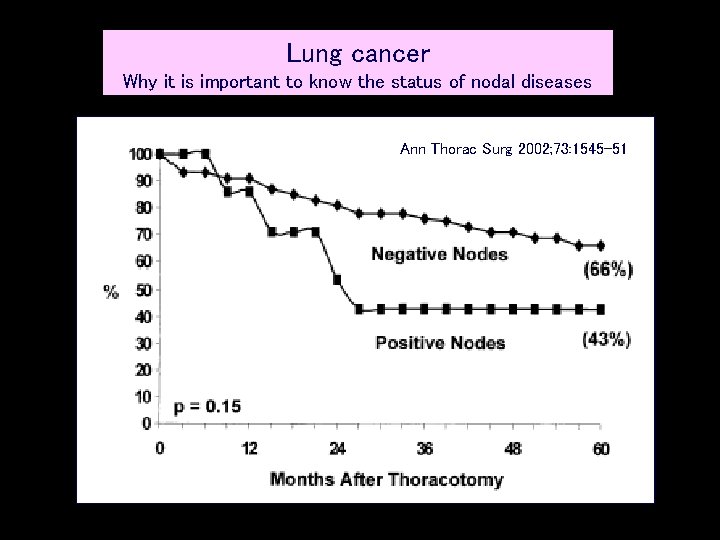
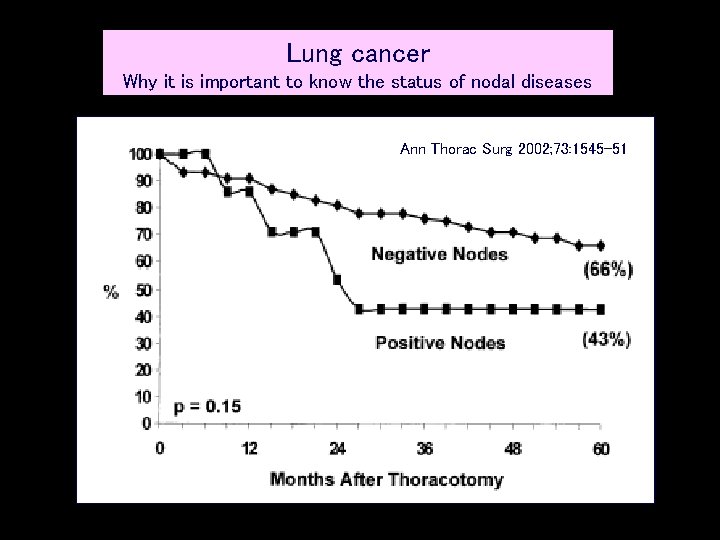
Lung cancer Why it is important to know the status of nodal diseases Ann Thorac Surg 2002; 73: 1545 -51
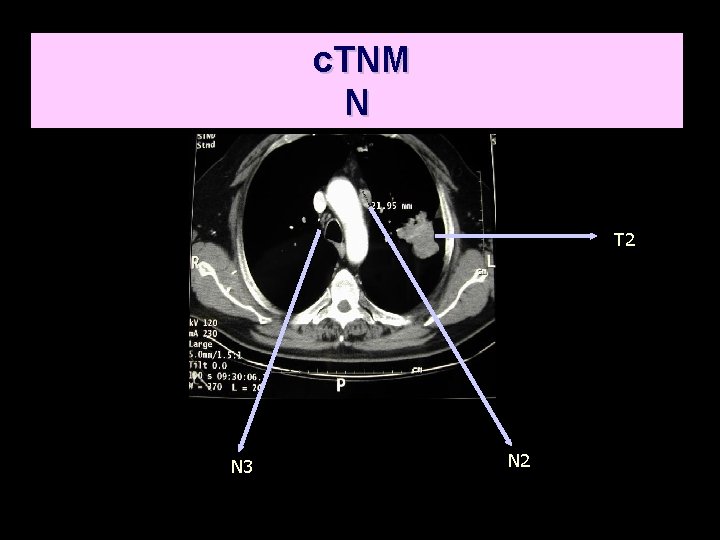
c. TNM N T 2 N 3 N 2
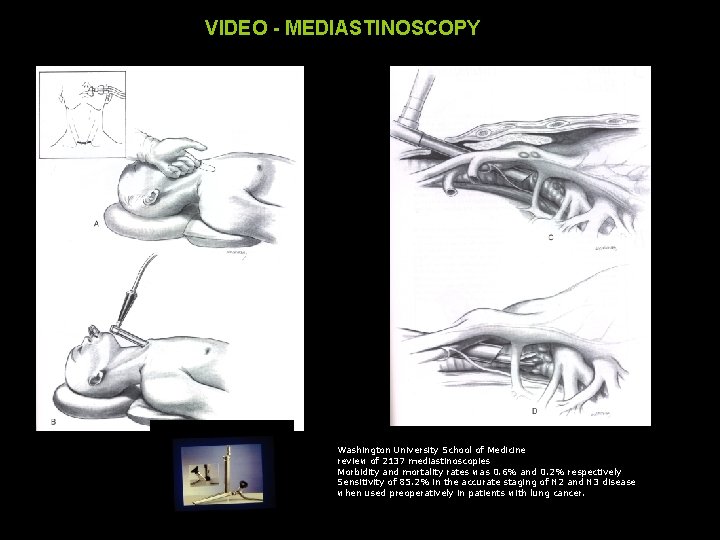
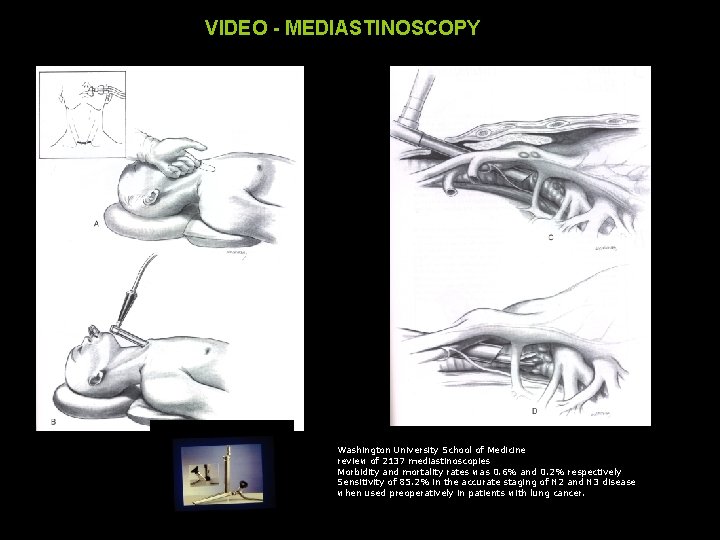
VIDEO - MEDIASTINOSCOPY Washington University School of Medicine review of 2137 mediastinoscopies Morbidity and mortality rates was 0. 6% and 0. 2% respectively Sensitivity of 85. 2% in the accurate staging of N 2 and N 3 disease when used preoperatively in patients with lung cancer.

TNM M factor Distant MTS Or two nodules in different lobes
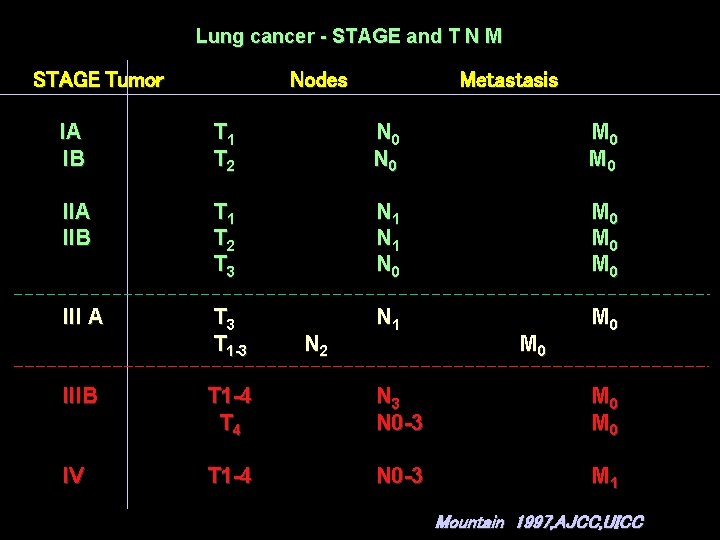
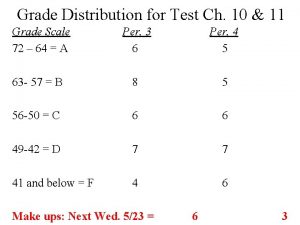
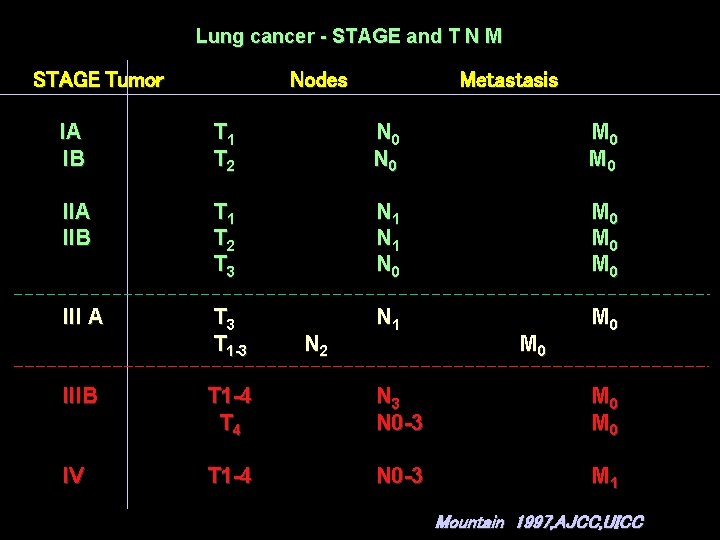
Lung cancer - STAGE and T N M STAGE Tumor Nodes Metastasis IA IB T 1 T 2 N 0 M 0 IIA IIB T 1 T 2 T 3 N 1 N 0 M 0 M 0 III A T 3 T 1 -3 N 1 M 0 N 2 M 0 IIIB T 1 -4 T 4 N 3 N 0 -3 M 0 IV T 1 -4 N 0 -3 M 1 Mountain 1997, AJCC, UICC
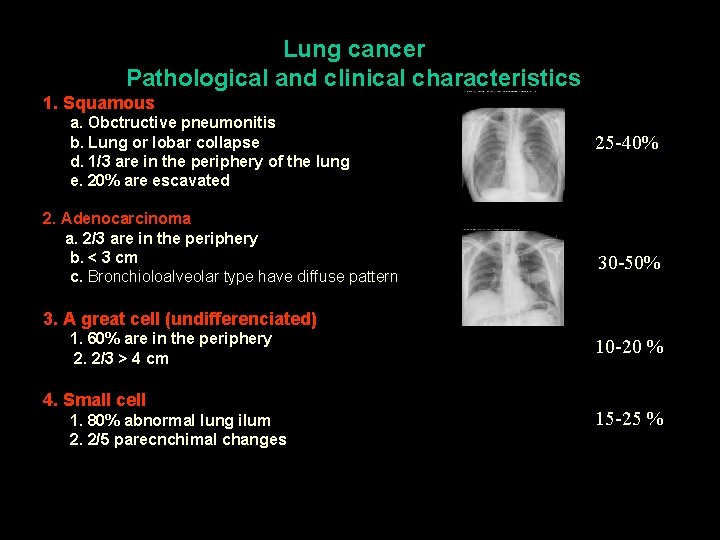
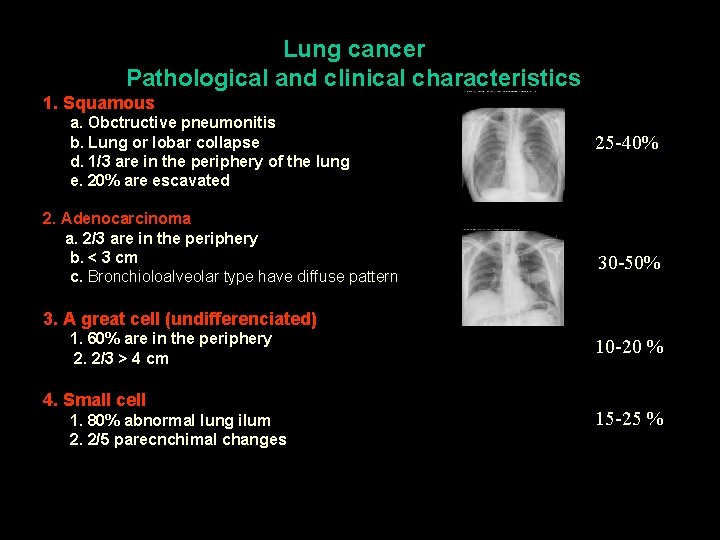
Lung cancer Pathological and clinical characteristics 1. Squamous a. Obctructive pneumonitis b. Lung or lobar collapse d. 1/3 are in the periphery of the lung e. 20% are escavated 2. Adenocarcinoma a. 2/3 are in the periphery b. < 3 cm c. Bronchioloalveolar type have diffuse pattern 25 -40% 30 -50% 3. A great cell (undifferenciated) 1. 60% are in the periphery 2. 2/3 > 4 cm 4. Small cell 1. 80% abnormal lung ilum 2. 2/5 parecnchimal changes 10 -20 % 15 -25 %
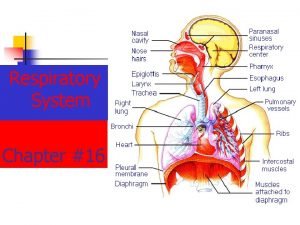
Lung cancer Clinical presentation 1. Broncho-pulmonary 2. Extrapulmonary but intrathoracic 3. Extrapulmonary metastatic 4. Extra pulmonary non metastatic ( i. e. paraneoplastic)
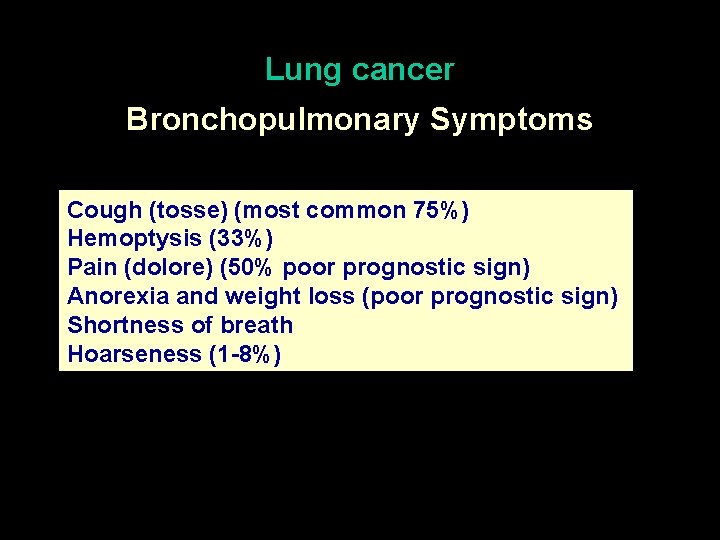
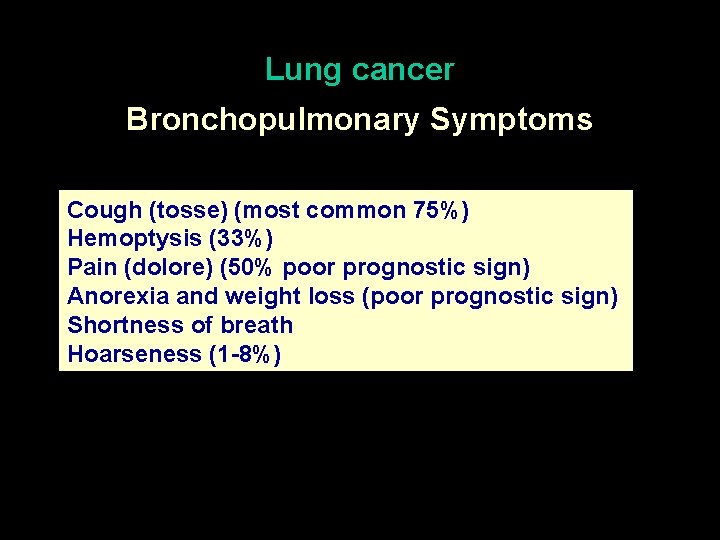
Lung cancer Bronchopulmonary Symptoms Cough (tosse) (most common 75%) Hemoptysis (33%) Pain (dolore) (50% poor prognostic sign) Anorexia and weight loss (poor prognostic sign) Shortness of breath Hoarseness (1 -8%)
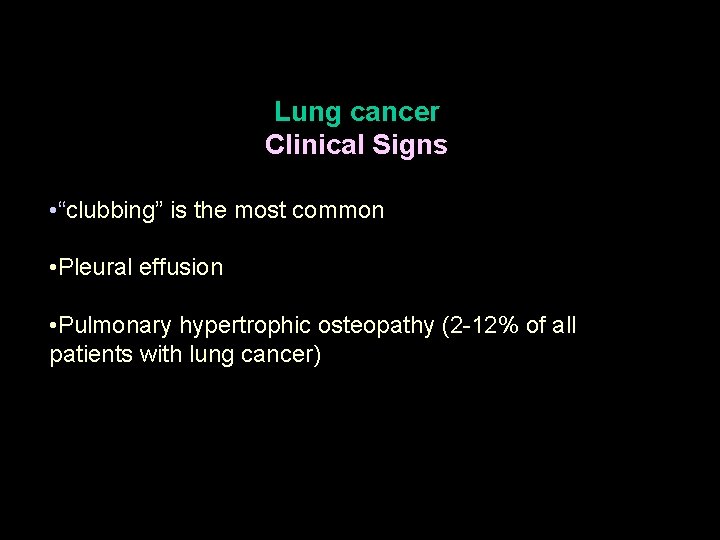
Lung cancer Clinical Signs • “clubbing” is the most common • Pleural effusion • Pulmonary hypertrophic osteopathy (2 -12% of all patients with lung cancer)
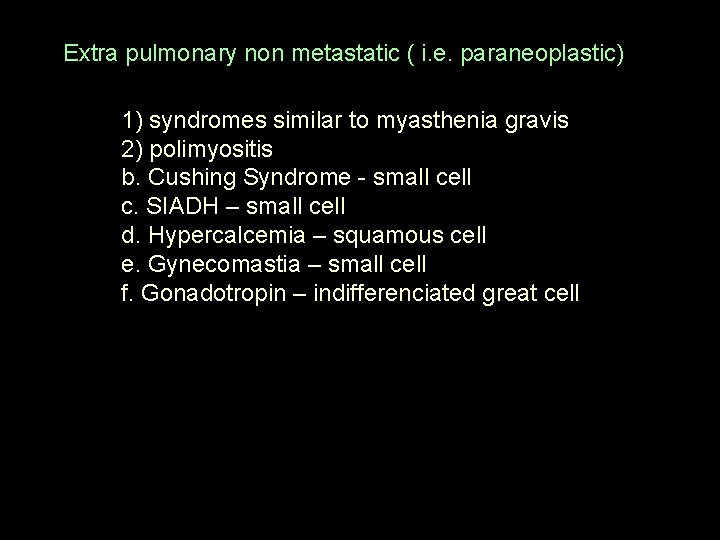
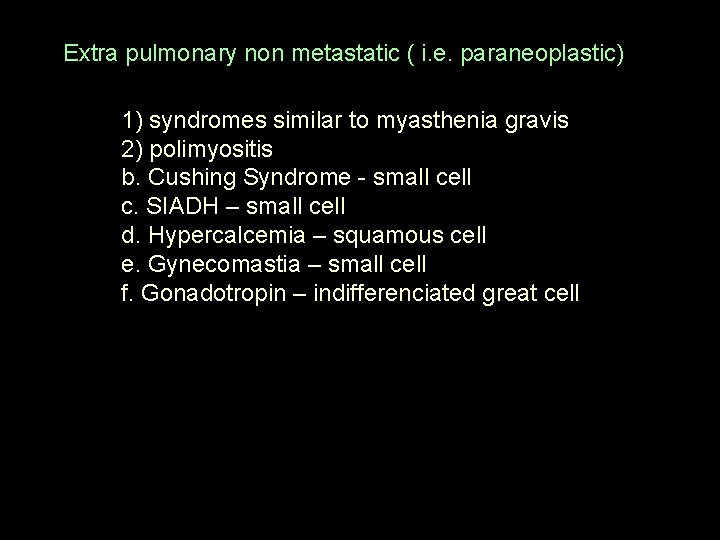
Extra pulmonary non metastatic ( i. e. paraneoplastic) 1) syndromes similar to myasthenia gravis 2) polimyositis b. Cushing Syndrome - small cell c. SIADH – small cell d. Hypercalcemia – squamous cell e. Gynecomastia – small cell f. Gonadotropin – indifferenciated great cell
Lung cancer Diagnosis Invasive Not invasive
. . . In every new lung nodule it is necessary to achieve a final pathologic diagnosis to exclude the presence of cancer EVIDENCE BASED MEDICINE
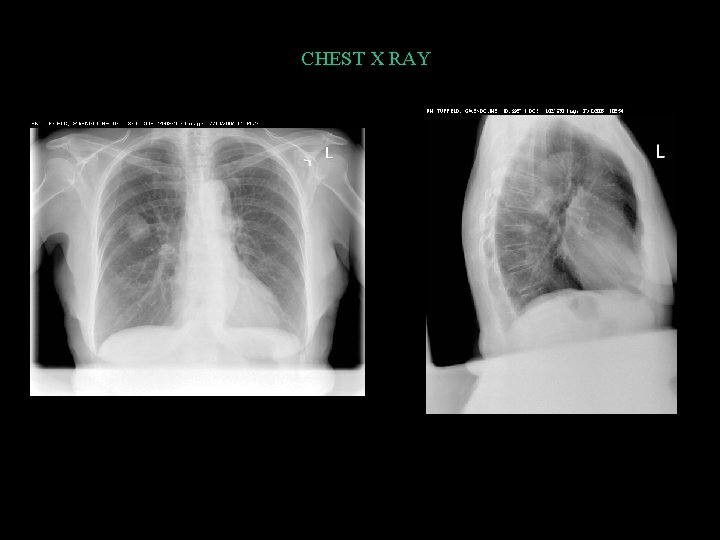
Lung cancer – diagnosis Chest x ray Generally radiographic alterations are present 7 months before symptoms reveal the tumor It shows nodules > 1 cm The most common finding is the coin lesion It failed to demonstrate a reducing in lung cancer mortality
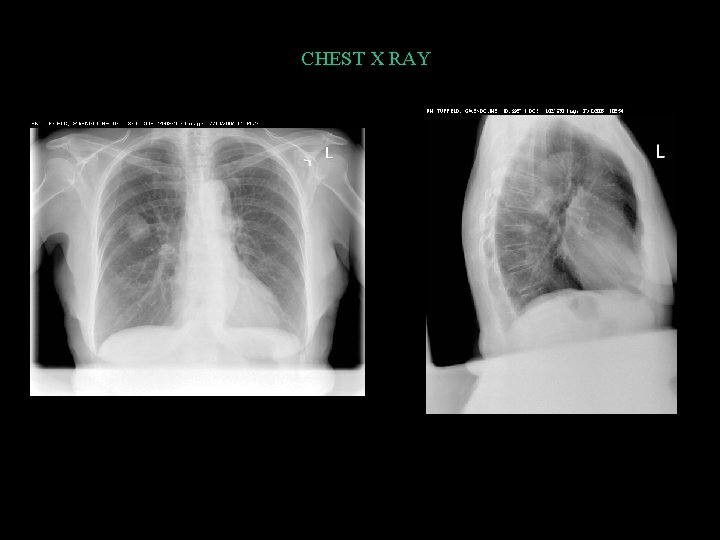
CHEST X RAY
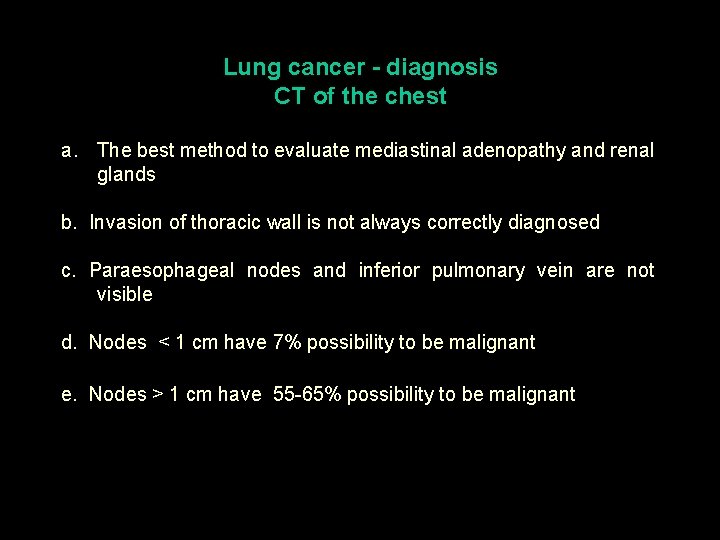
Lung cancer - diagnosis CT of the chest a. The best method to evaluate mediastinal adenopathy and renal glands b. Invasion of thoracic wall is not always correctly diagnosed c. Paraesophageal nodes and inferior pulmonary vein are not visible d. Nodes < 1 cm have 7% possibility to be malignant e. Nodes > 1 cm have 55 -65% possibility to be malignant
Lung cancer Diagnosis CT of the chest Three studies revealed that using Spiral CT as a screening method it was possible to discover 84 -93 % of lung cancer in the initial stage (IA) with a low percentage of false positive (20%).

Lung cancer Diagnosis Magnetic Resonance (MR) It is better to evaluate the vascular invasion
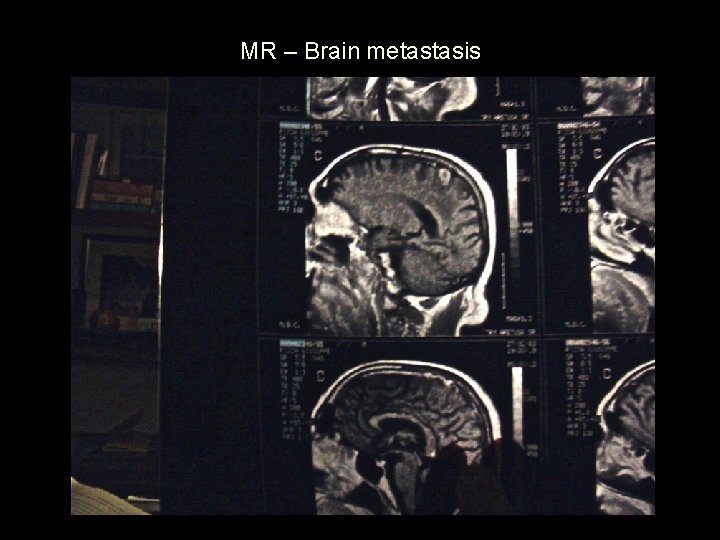
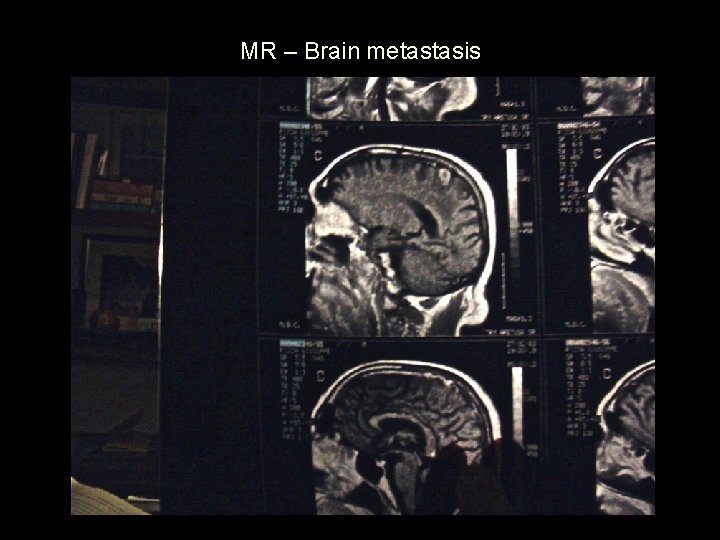
MR – Brain metastasis
PET (Positron Emission Tomography) Higher specificity has the PET con FDG (F 18 fluoro deossiglucosio) (sensibility 95% - specificity 85%) but it is useful in nodules greater than 6 mm. It reduces the need to send the patient for an invasive method such as mediastinoscopy.
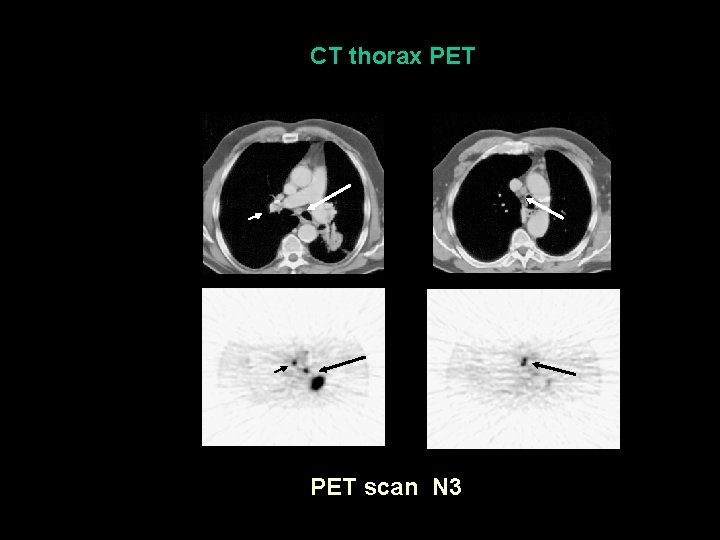
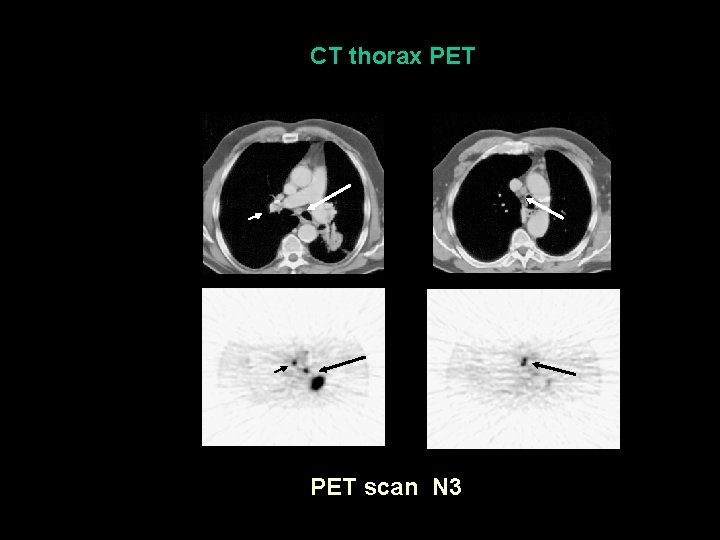
CT thorax PET scan N 3
Lung cancer Diagnosis Sputum cytology Sensitive in 20 - 70%, but it is correlated with the position of the tumour Squamous carcinoma is more common to be positive than small cell or adenocarcinoma. When cytology is positive a final diagnosis in 85% is possible
Lung cancer Diagnosis Invasive diagnosis
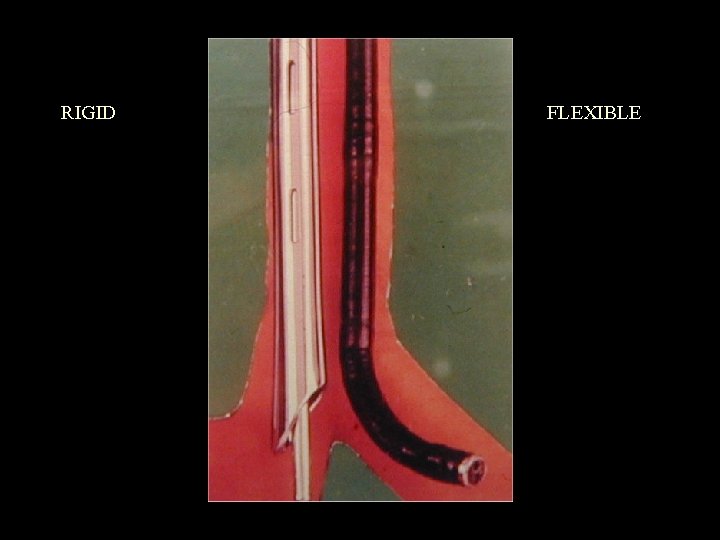
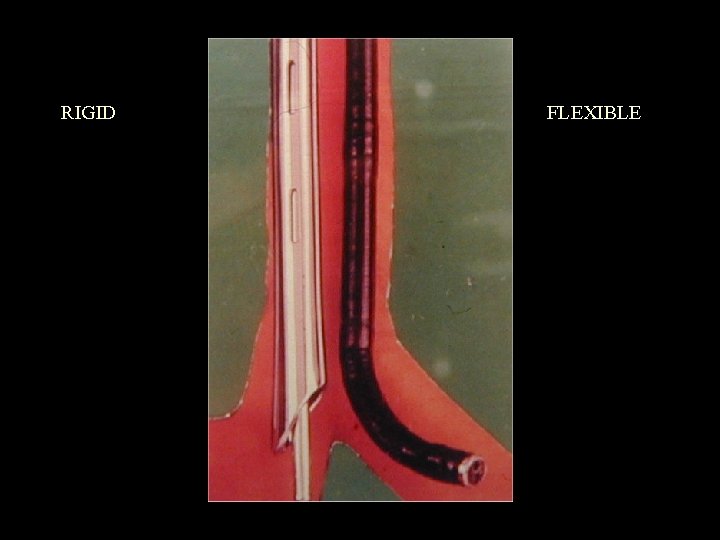
RIGID FLEXIBLE
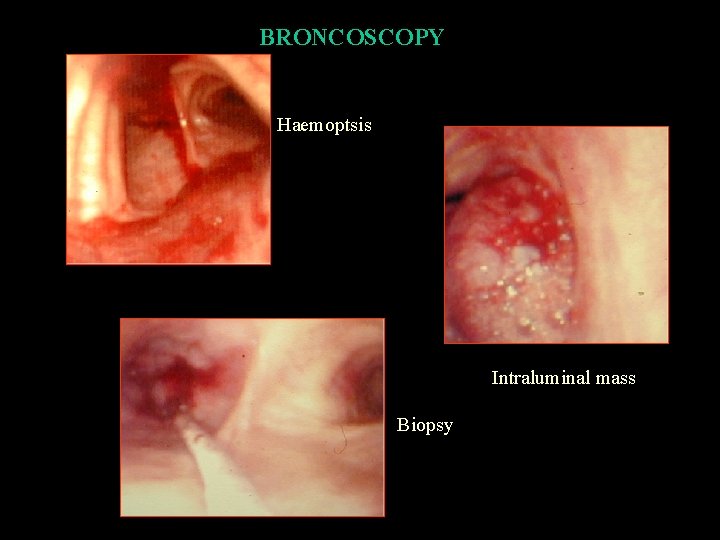
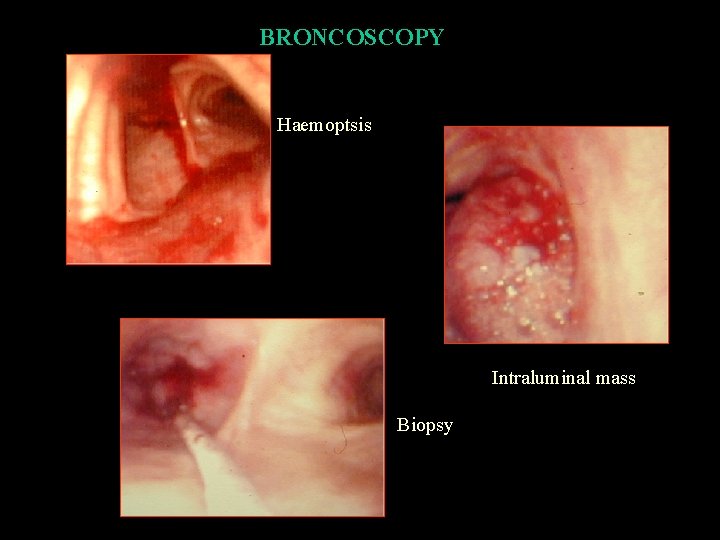
BRONCOSCOPY Haemoptsis Intraluminal mass Biopsy
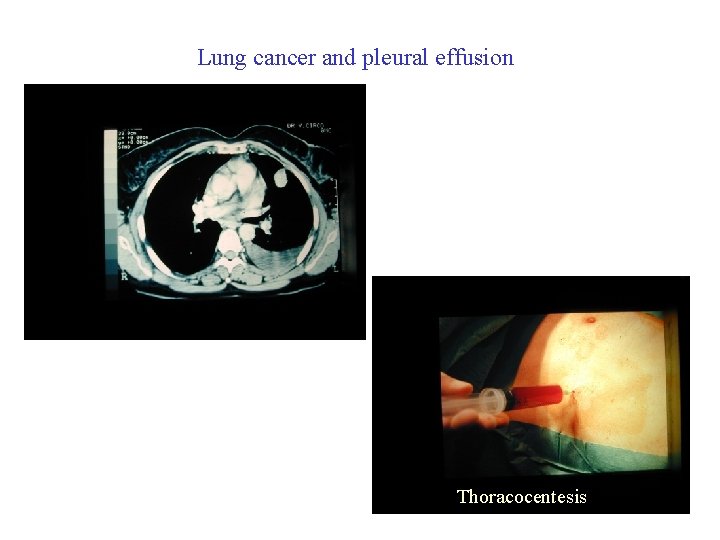
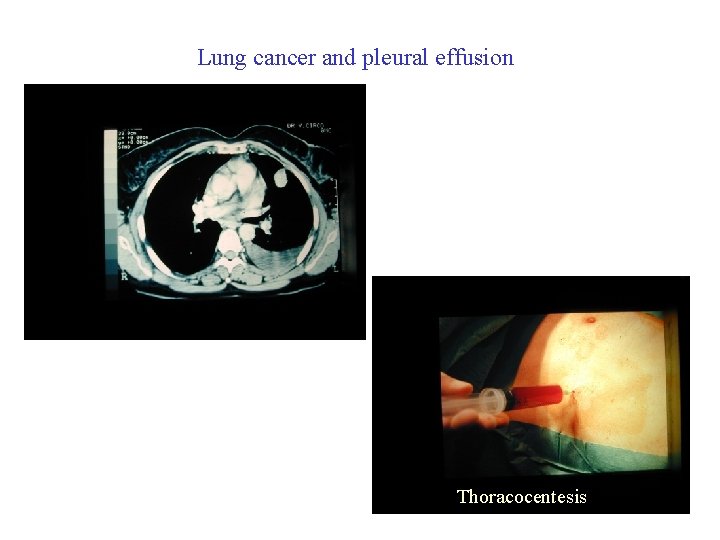
Lung cancer and pleural effusion Thoracocentesis

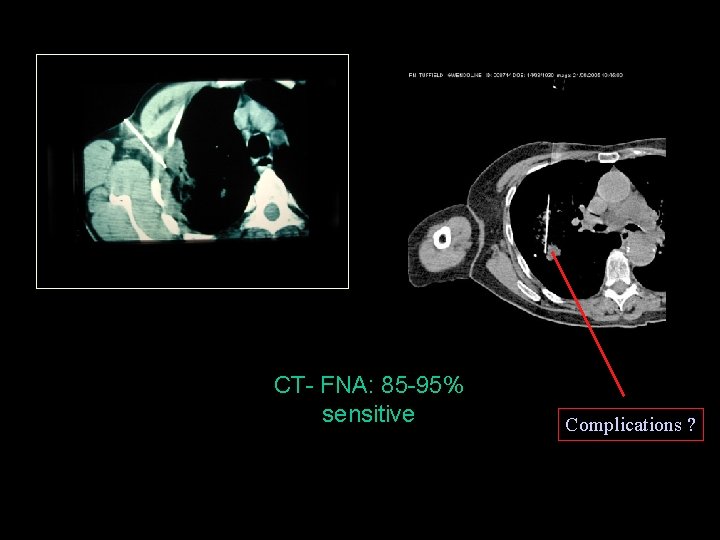
Lung cancer - diagnosis CT GUIDED BIOPSY Percutaneous o transbronchial In peripheric lesion is accurate in 85 -95%
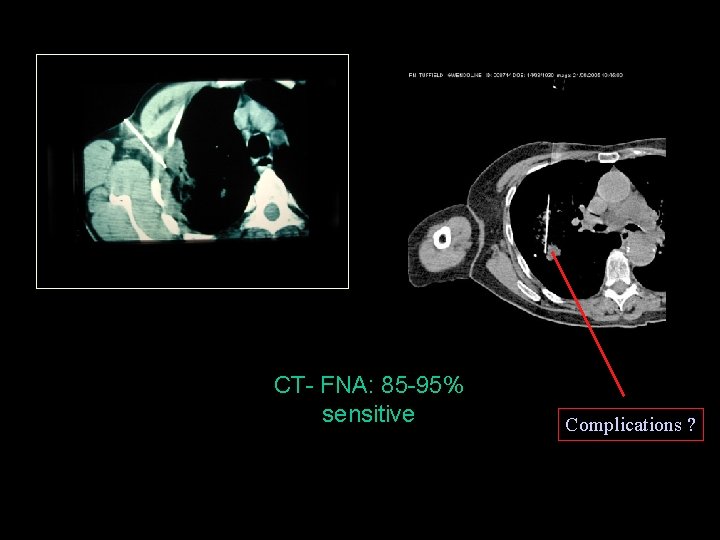
CT- FNA: 85 -95% sensitive Complications ?
Lung cancer – invasive diagnosis VATS Thoracotomy
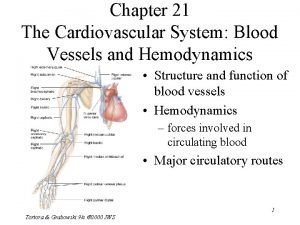
Lung cancer TREATMENT SURGERY
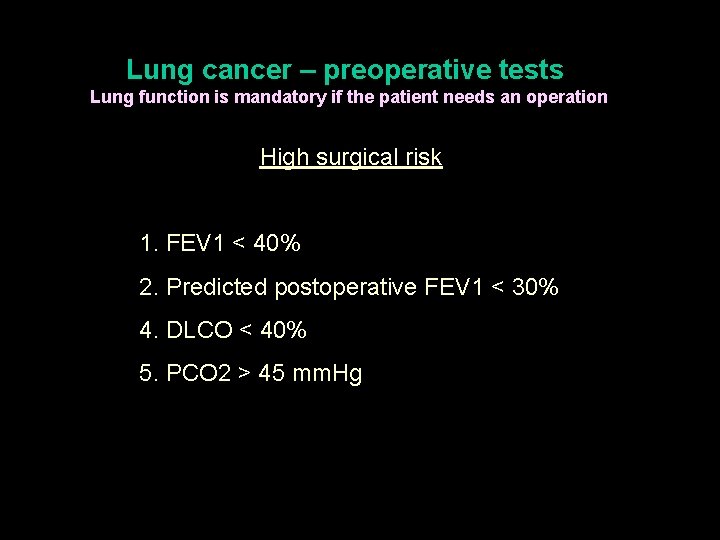
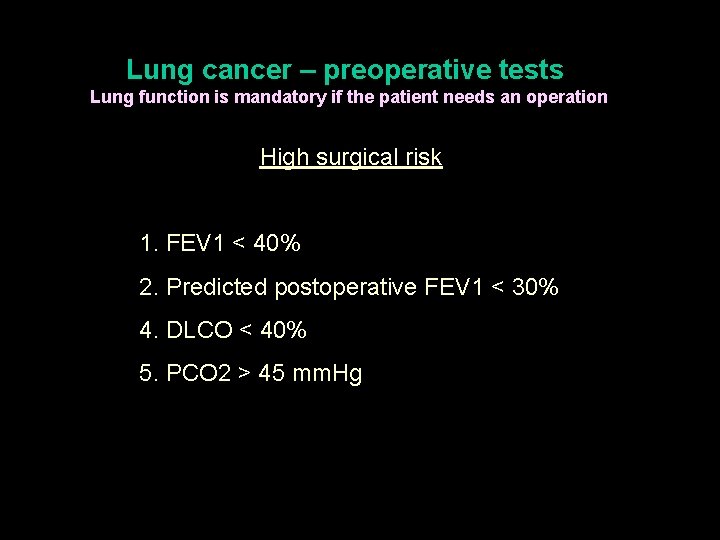
Lung cancer – preoperative tests Lung function is mandatory if the patient needs an operation High surgical risk 1. FEV 1 < 40% 2. Predicted postoperative FEV 1 < 30% 4. DLCO < 40% 5. PCO 2 > 45 mm. Hg
The goal of surgical treatment in oncology is twofold • to achieve long term survival with a good quality of life • to avoid recurrence
Surgical treatment of lung cancer Indications • c. TNM • Lung Function Tests • Intra-operative
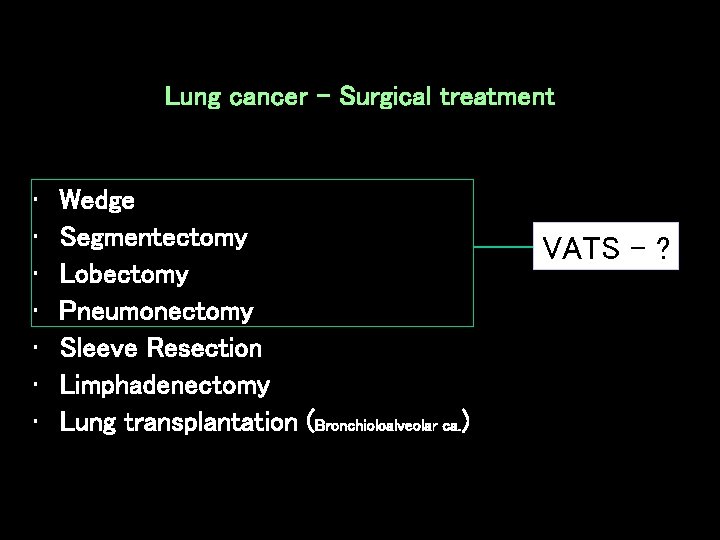
Lung cancer - Surgical treatment • • Wedge Segmentectomy Lobectomy Pneumonectomy Sleeve Resection Limphadenectomy Lung transplantation (Bronchioloalveolar ca. ) VATS - ?
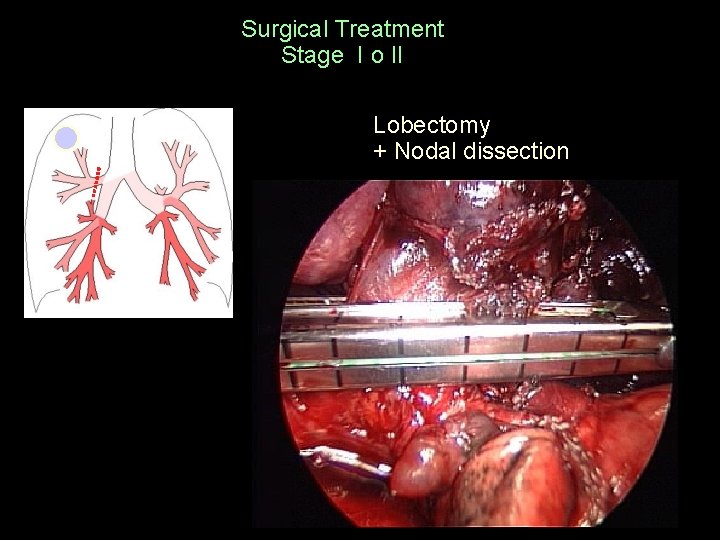
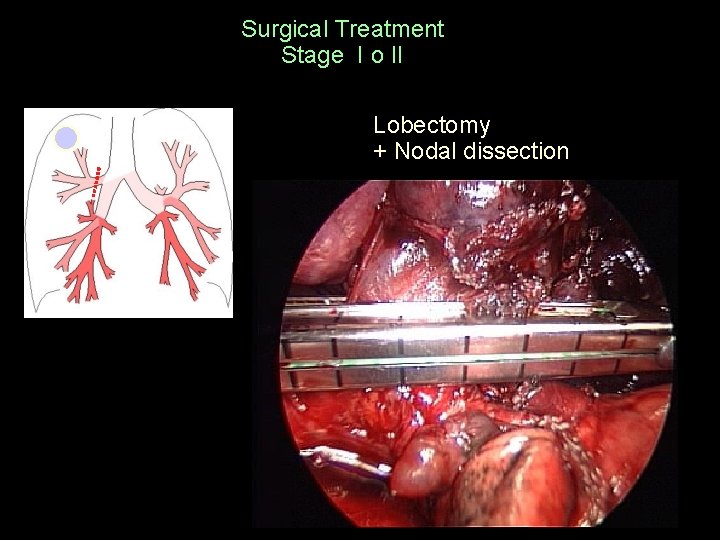
Surgical Treatment Stage I o II Lobectomy + Nodal dissection
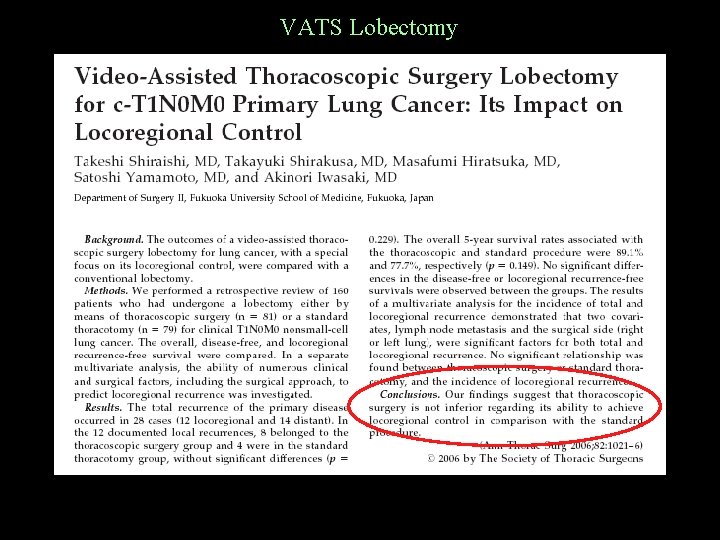
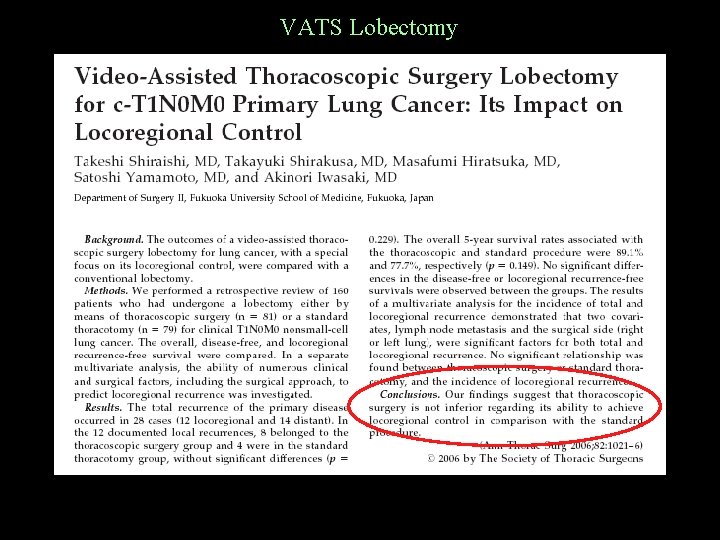
VATS Lobectomy
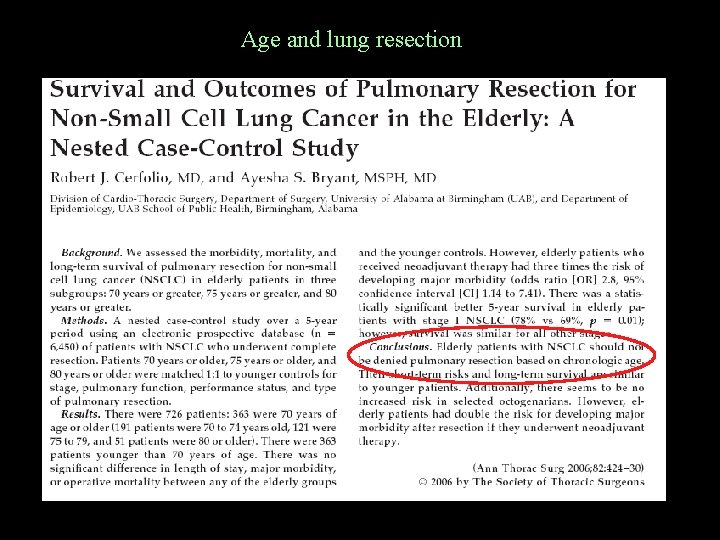
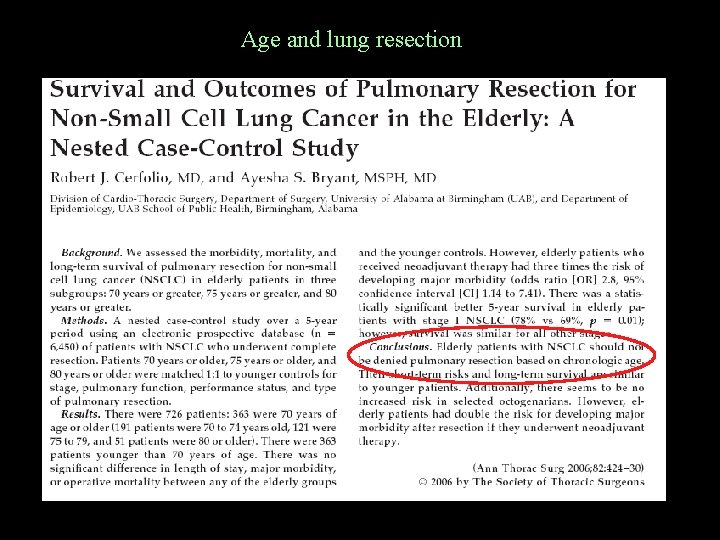
Age and lung resection
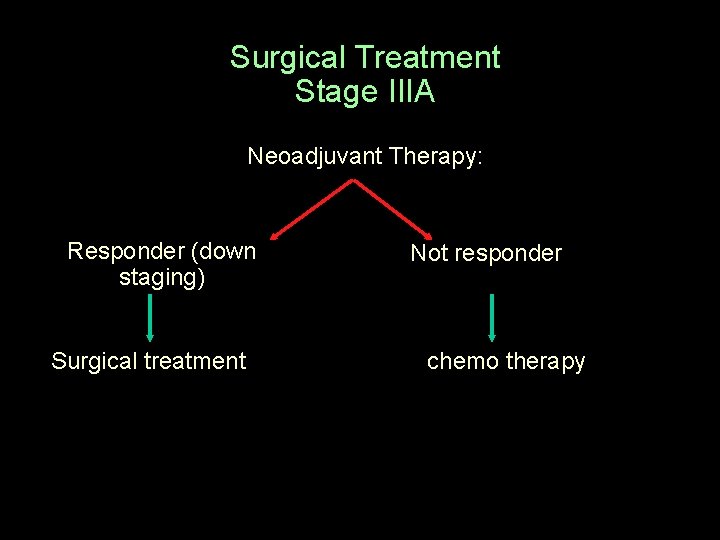
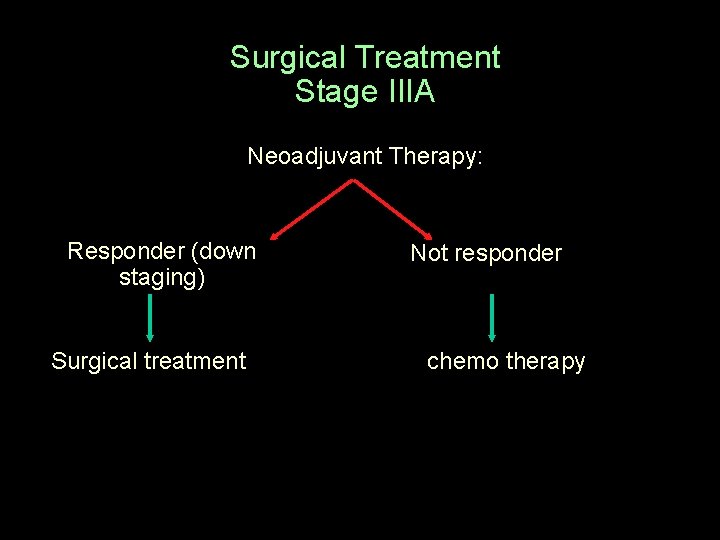
Surgical Treatment Stage IIIA Neoadjuvant Therapy: Responder (down staging) Surgical treatment Not responder chemo therapy
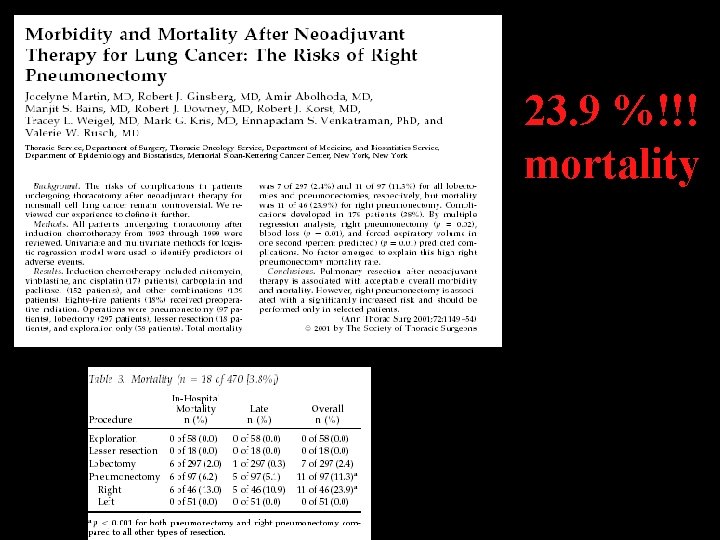
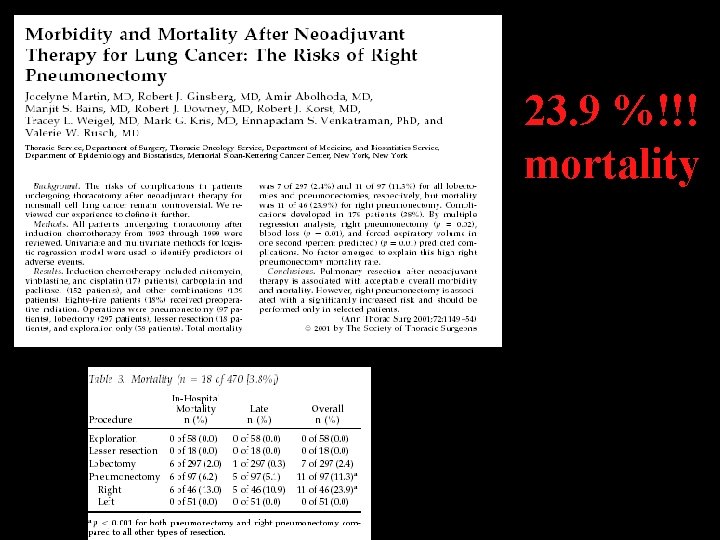
23. 9 %!!! mortality
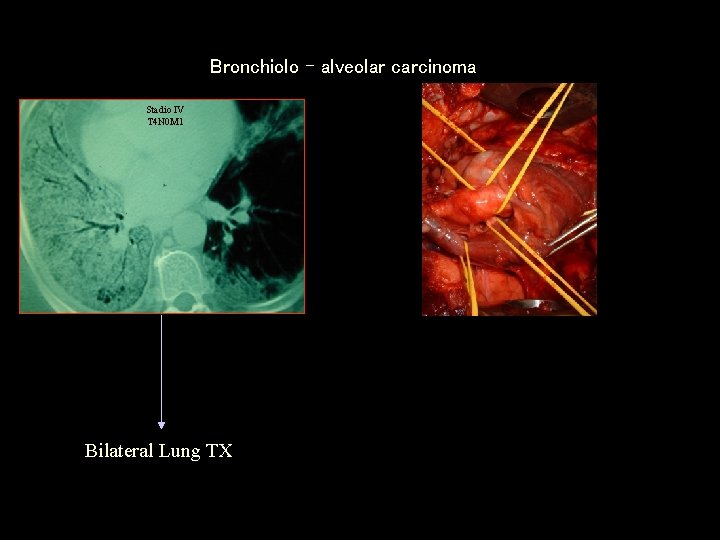
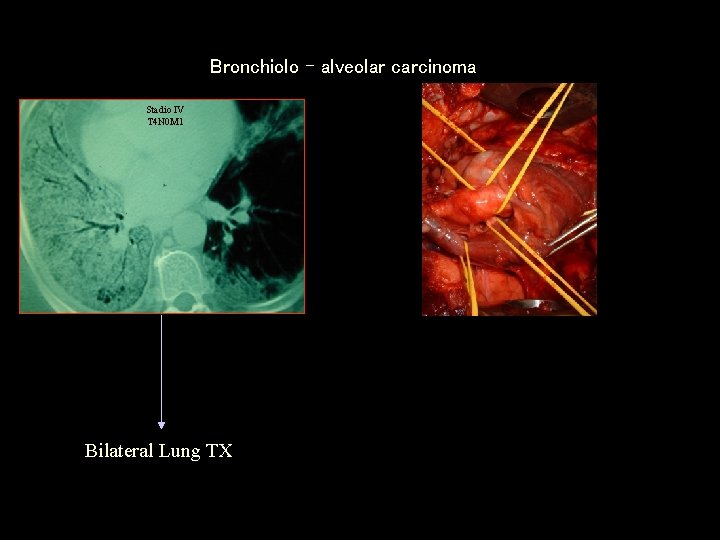
Bronchiolo – alveolar carcinoma Stadio IV T 4 N 0 M 1 Bilateral Lung TX
Lung cancer TREATMENT CHEMO RADIO OTHER (stent, laser, photodynamic therapy)
Chemotherapy Advanced NSCLC • Over the last 10 years new agents have provided a better median survival of 7 -10 months with 35 -40% alive at 1 year.
Chemotherapy Small Cell Lung Cancer • • The most frustrating cancer to treat 1970 mean survival was 5 months Nowadays 18 -20 months (limited disease) Nowdays 6 -9 months (extensive disease)
Radiotherapy • As a curative modality, radiotherapy has been disappointing. • The combination of chemo and radiotherapy has provided better median and long term survival than radiotherapy alone • Radiotherapy has proven most successful in palliating lung cancer symptoms in up to 80% of instances.
Other (stent, laser, photodymanic therapy, cryosurgey) • The main indication is in patients with the occlusion of the main bronchus or lobar bronchi • Also indicated in patients in early-stage disease who are not candidates for surgical procedures. It may also be used to reduce symptoms in late-stage disease.
NEW APPROACHES • Mutation in Epidermal Growth Factor Receptor (EGFR). Aberrant signalling from the EGFR is known in lung cancer. • Two oral inhibitors of EGF, geftinib and erlotinib, inhibit the EGFR and both have demonstrated antitumor activity. • Responses to these agent are few. Mainly nonsmokers, women, BAC.
NEW APPROACHES Immunotherapy uses drugs that boost the patient's immune system to fight cancer. Gene Therapy. Research is underway to determine if methods can be developed to attack genetic mutations that are causing cancer. Angiogenesis Inhibitors. Under investigation are agents that inhibit the formation of new blood vessels (called angiogenesis). The spread of new blood vessels is controlled by compounds called growth factors, such as vascular endothelial cell growth factor (VEGF). Angiogenesis inhibitors are agents that literally turn off the growth factors themselves or their receptors.
SUMMARY – in general • One hundred year ago lung cancer was rare • Only 25 % of patients with lung cancer will have the chance to have the cancer removed, and therefore the hope of a cure. The majority will undergo oncologic treatment. • Chest x ray modification is present 7 months before the first symptoms. Chest x ray reveals only nodules > 1 cm. • Modern diagnostic tools are “latecomers” and their main role is to evaluate the possibility of surgical treatment. • All the non invasive diagnostic tests do not determine the histology. (evidence based medicine).
SUMMARY – surgical treatment • Patients in stage I and II can undergo surgery after the evaluation of the respiratory condition • Patients in stage IIIA are potentially resectable, but they first need neoadjuvant therapy
SUMMARY – surgical treatment • VATS is probably the best treatment for patients in stage I • To avoid or discuss in detail with the patient if R pneumonectomy is indicated following neoadjuvant treatment for the high mortality risks • In case of advanced BAC Lung Transplantation is an option.
SUMMARY – non surgical treatment • Chemotherapy is the only option for SCLC • Radiotherapy is successful in palliating lung cancer symptoms • The combination of chemo and radiotherapy has provided better median and long term survival.
To achieve the best long term survival it is necessary to reduce the time interval between The first clinical symptoms and the final diagnosis and treatment
2008 Anatomical lung resection is the most appropriate treatment to achieve better long term survival adding the hope of curing the cancer in patients at the initial stage with good lung function
The future

The future in the treatment of lung cancer • early diagnosis • Surgery associated with otherapies
 Cardiothoracic surgeon salary
Cardiothoracic surgeon salary Chest physiotherapy for nurses ppt
Chest physiotherapy for nurses ppt Thoracic surgery
Thoracic surgery Milada cosmetic surgery hospital
Milada cosmetic surgery hospital Ospital ng maynila surgery department
Ospital ng maynila surgery department Wvu department of surgery
Wvu department of surgery General surgery selection criteria
General surgery selection criteria Principles of periodontal surgery
Principles of periodontal surgery Frcs exam questions
Frcs exam questions Organization structure of hospital pharmacy
Organization structure of hospital pharmacy Hesf1
Hesf1 Hospital organizational structure
Hospital organizational structure Flagler hospital billing department
Flagler hospital billing department Erpno
Erpno Janet tetrault general hospital
Janet tetrault general hospital Cheltenham general hospital
Cheltenham general hospital Jewish general hospital archives
Jewish general hospital archives Saiful anwar general hospital
Saiful anwar general hospital Deirdre staunton sligo general hospital
Deirdre staunton sligo general hospital Hospital fernando quiroz issste
Hospital fernando quiroz issste Heart and general hospital
Heart and general hospital St joseph's general hospital comox
St joseph's general hospital comox Posturing medical
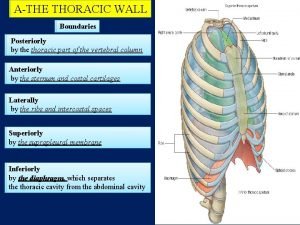
Posturing medical Arterial supply of thorax
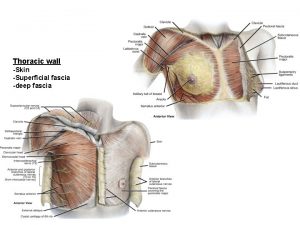
Arterial supply of thorax Fascia superficialis thorax
Fascia superficialis thorax Umbliculus
Umbliculus Sibson's fascia
Sibson's fascia Deep popliteal lymph nodes
Deep popliteal lymph nodes Dressed to the
Dressed to the High ilium flare out
High ilium flare out Azgos vein
Azgos vein Jugular notc
Jugular notc Chronic pain management irwin
Chronic pain management irwin Pig thoracic cavity diagram
Pig thoracic cavity diagram Collateral branch of intercostal nerve
Collateral branch of intercostal nerve Thoracic inlet x ray
Thoracic inlet x ray Diaphragm thoracic level
Diaphragm thoracic level Thoracic kyphosis
Thoracic kyphosis Aortic knob
Aortic knob Thoracic aorta supplies blood to
Thoracic aorta supplies blood to Thoracic membranes
Thoracic membranes Venturi mask uses
Venturi mask uses Body cavity
Body cavity Basic anatomy terminology
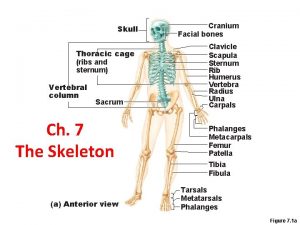
Basic anatomy terminology Intercostal muscles
Intercostal muscles Thoracic configuration
Thoracic configuration Pouchlike structure at the start of the thoracic duct
Pouchlike structure at the start of the thoracic duct Thoracic vertebrae not labeled
Thoracic vertebrae not labeled Thoracic aortic aneurysm
Thoracic aortic aneurysm Thoracic wall boundaries
Thoracic wall boundaries Regio thorax
Regio thorax Thoracic outlet wedge pillow
Thoracic outlet wedge pillow Neurogeen thoracic outlet syndroom
Neurogeen thoracic outlet syndroom Rajesh shah thoracic surgeon
Rajesh shah thoracic surgeon Tympanic part of temporal bone
Tympanic part of temporal bone Inferior articular process
Inferior articular process Muscles of thoracic spine
Muscles of thoracic spine Muscles of thoracic spine
Muscles of thoracic spine Thoracic cavity labeled
Thoracic cavity labeled Thoracic duct
Thoracic duct Thoracic cage anterior view
Thoracic cage anterior view Goblet cells of respiratory epithelium
Goblet cells of respiratory epithelium Sacrum of ox
Sacrum of ox Thoracic duct
Thoracic duct Thoracic cavity
Thoracic cavity Thoracic lumbar fascia
Thoracic lumbar fascia Thoracic wall
Thoracic wall Cervical lateral flexion
Cervical lateral flexion Posterior axillary
Posterior axillary Jugular notch
Jugular notch Thoracic surgeon
Thoracic surgeon Soft, spongy, cone-shaped organs in the thoracic cavity.
Soft, spongy, cone-shaped organs in the thoracic cavity.