Anesthesia for Thoracic Surgery Thoracotomy minimal invasive surgery



- Slides: 49
Anesthesia for Thoracic Surgery 高雄麻醉科系 黃佳絨
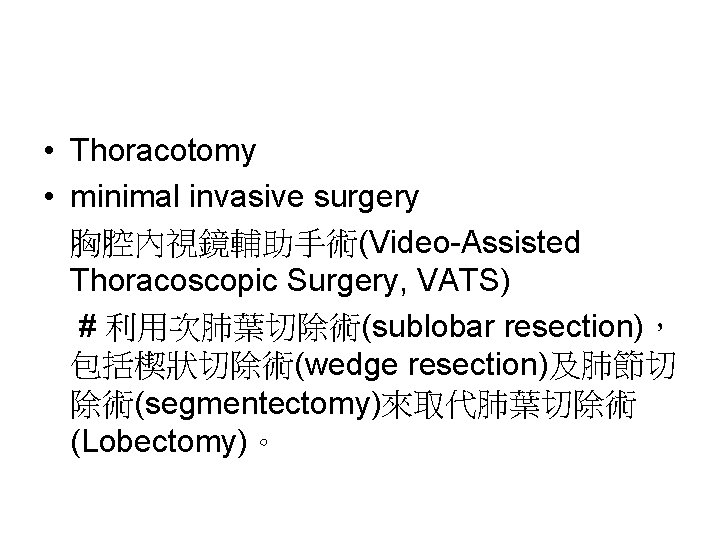
• Thoracotomy • minimal invasive surgery 胸腔內視鏡輔助手術(Video-Assisted Thoracoscopic Surgery, VATS) # 利用次肺葉切除術(sublobar resection), 包括楔狀切除術(wedge resection)及肺節切 除術(segmentectomy)來取代肺葉切除術 (Lobectomy)。
• 更好視野 OLV • 更快恢復 early extubation
OLV
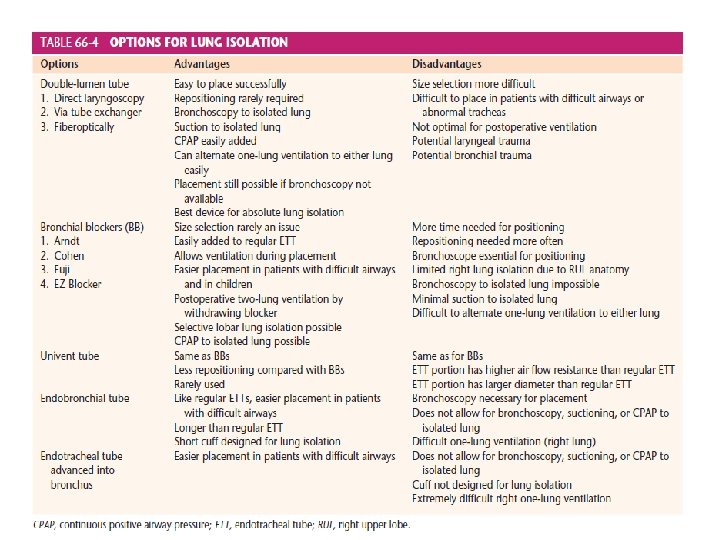
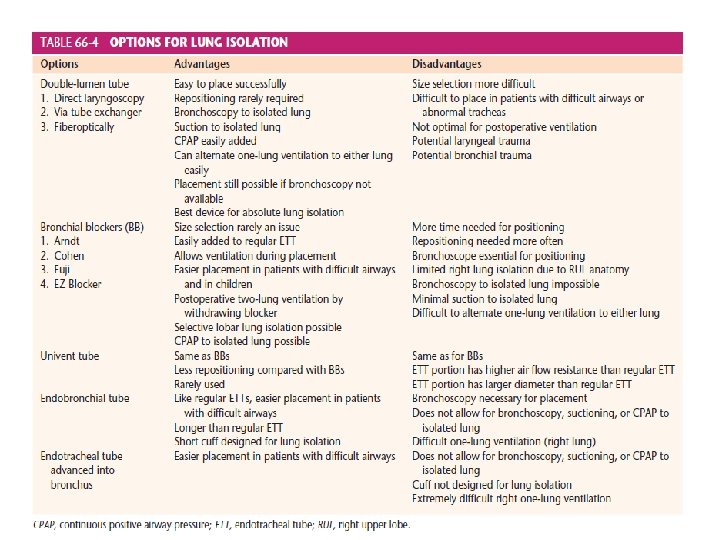
LUNG ISOLATION
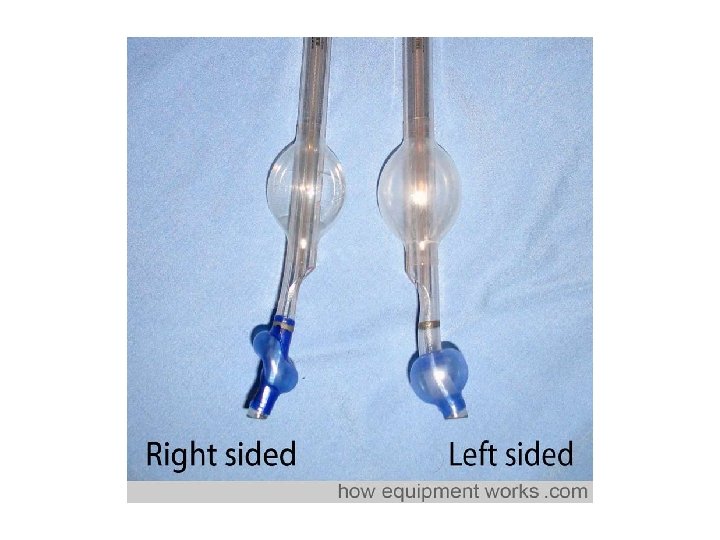
• Double Lumen Endotracheal Tube
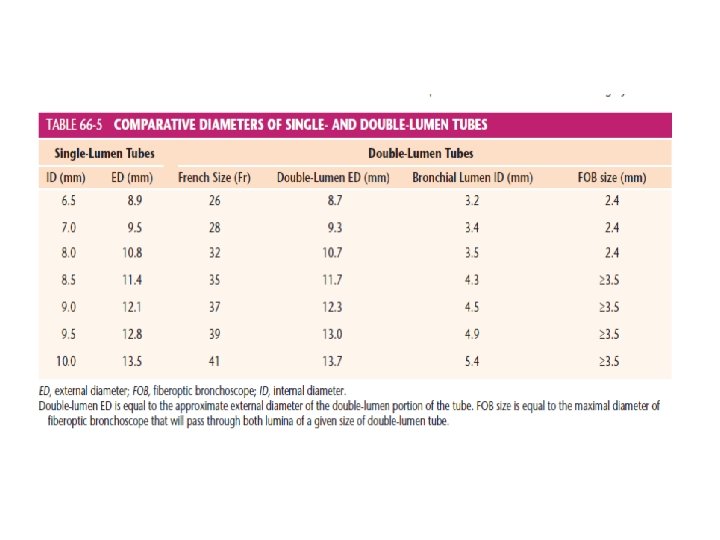
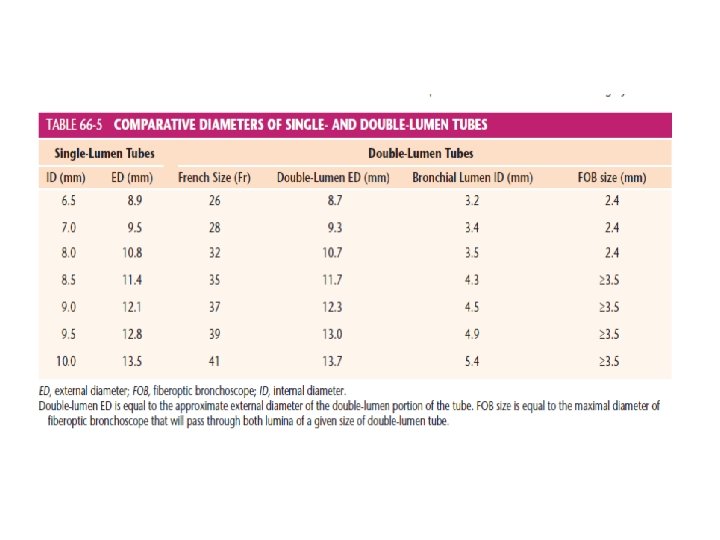
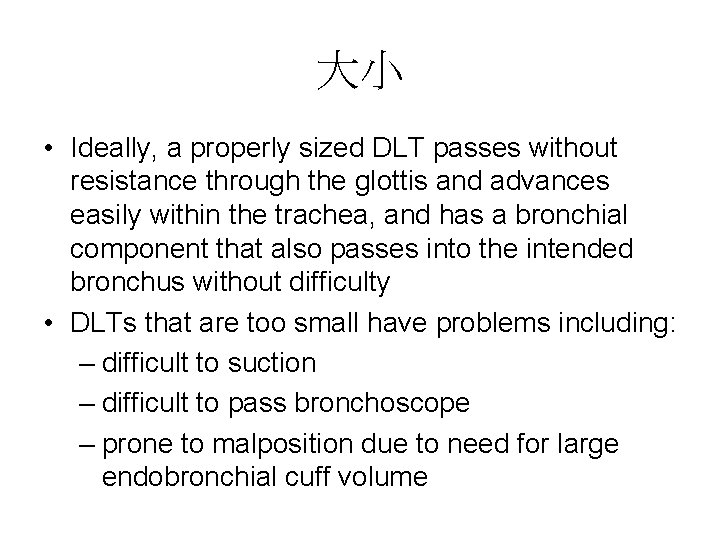
大小 • Ideally, a properly sized DLT passes without resistance through the glottis and advances easily within the trachea, and has a bronchial component that also passes into the intended bronchus without difficulty • DLTs that are too small have problems including: – difficult to suction – difficult to pass bronchoscope – prone to malposition due to need for large endobronchial cuff volume
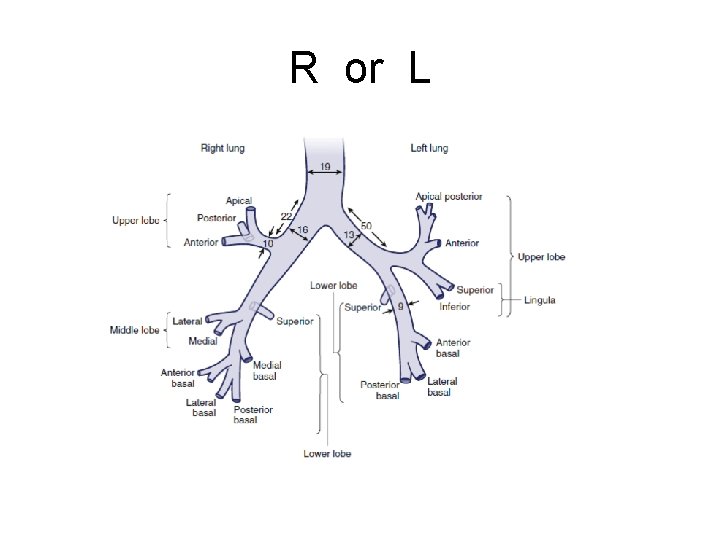
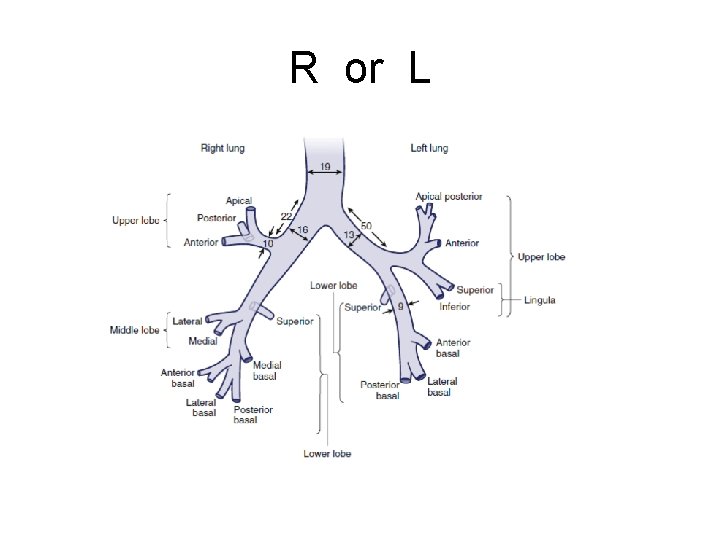
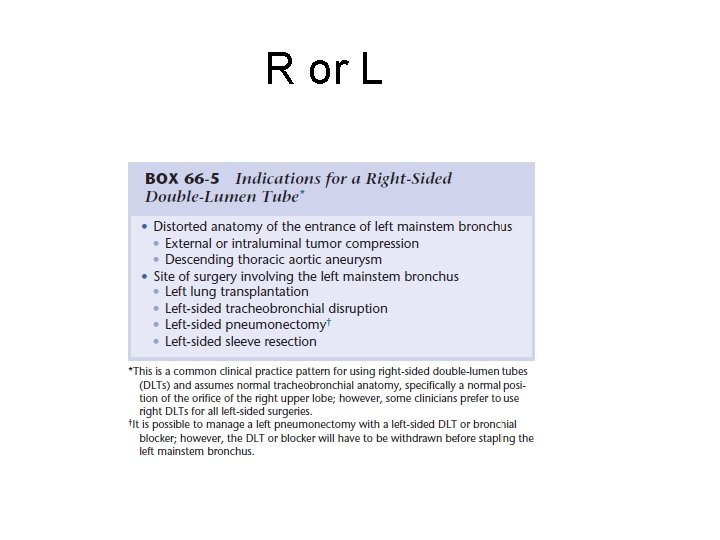
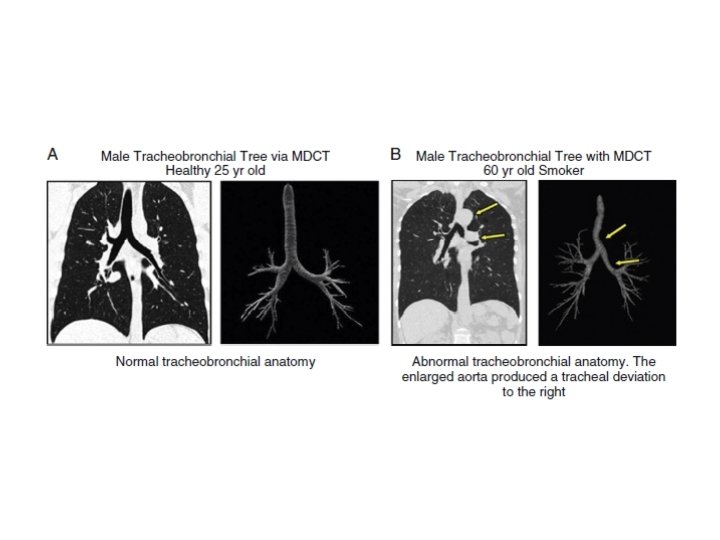
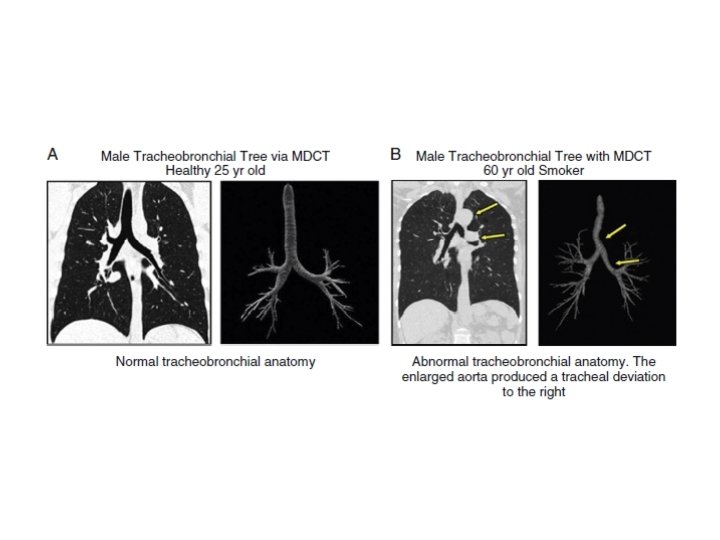
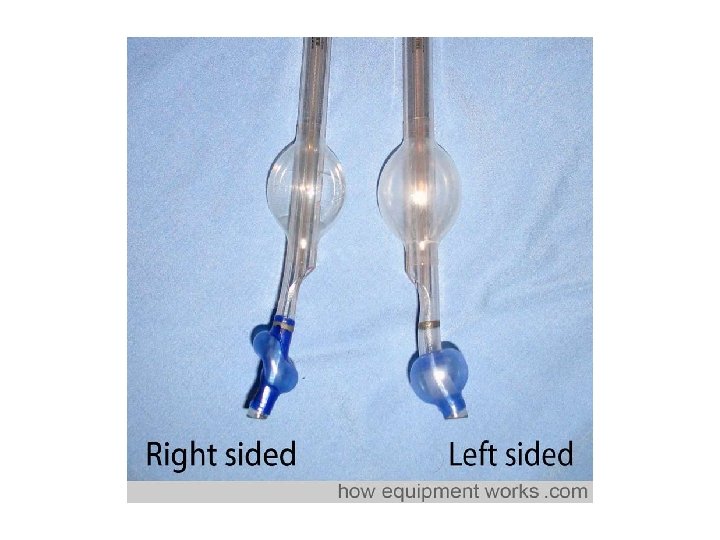
R or L
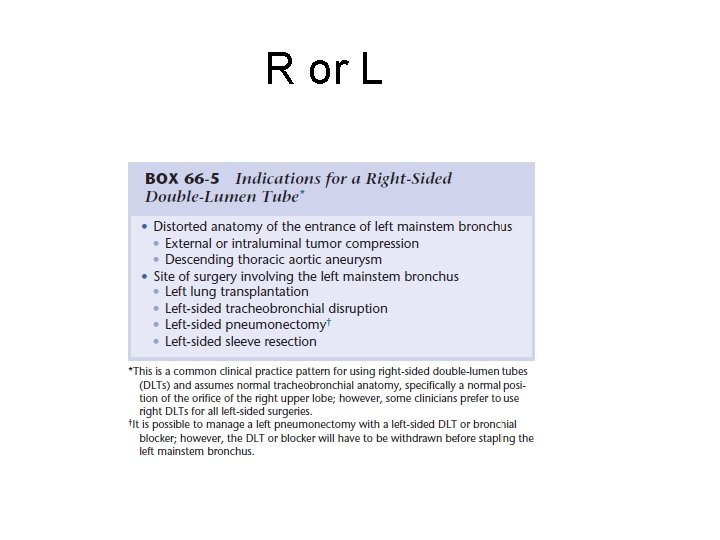
R or L
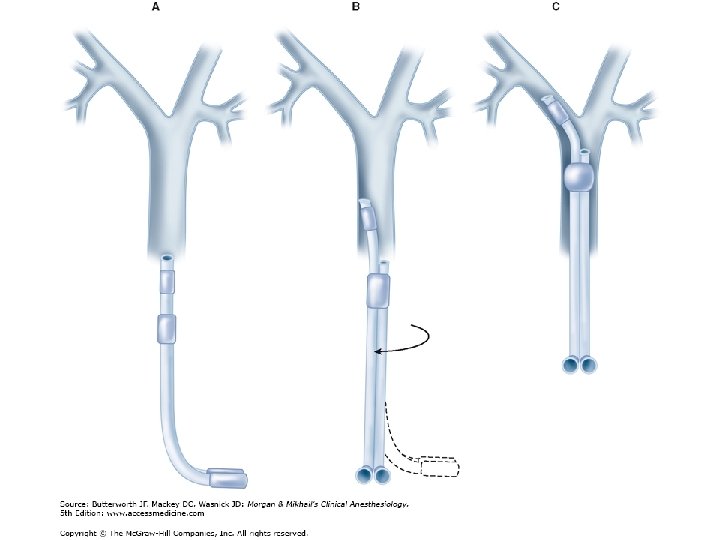
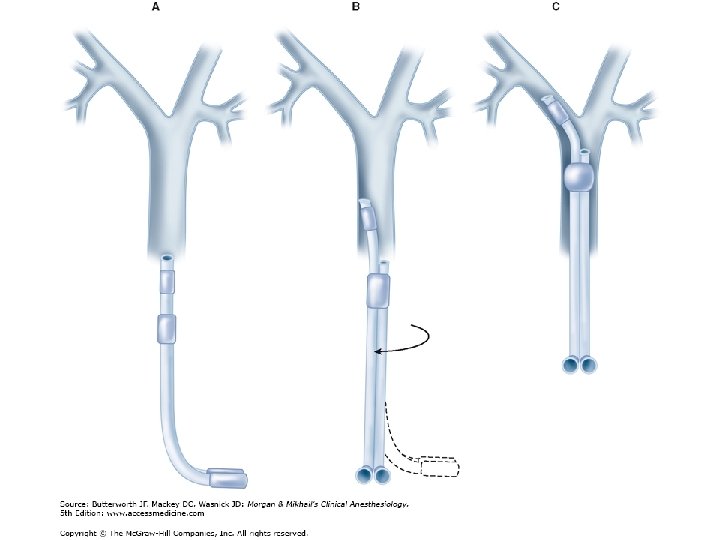
Placement of double-lumen tube
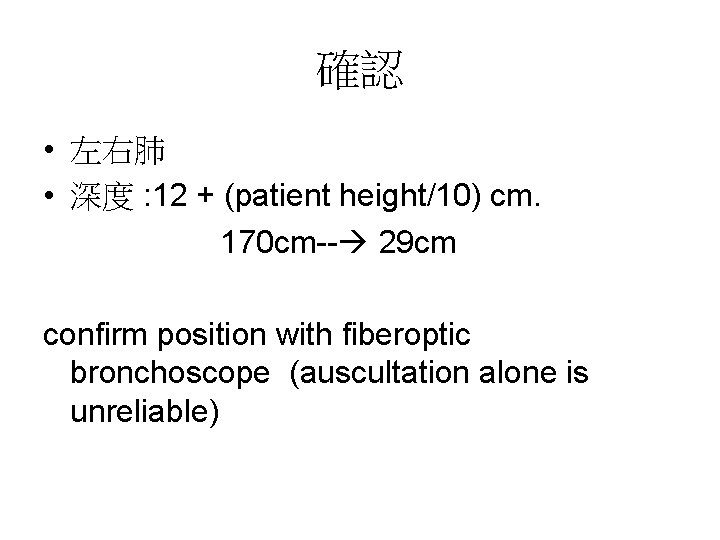
確認 • 左右肺 • 深度 : 12 + (patient height/10) cm. 170 cm-- 29 cm confirm position with fiberoptic bronchoscope (auscultation alone is unreliable)
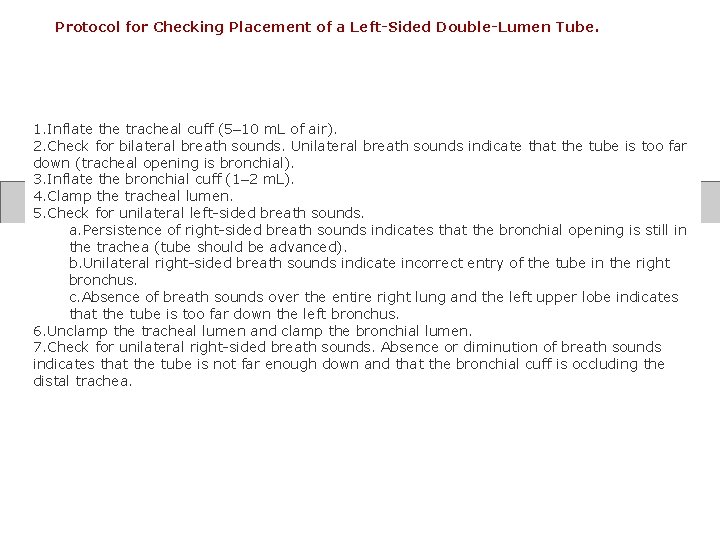
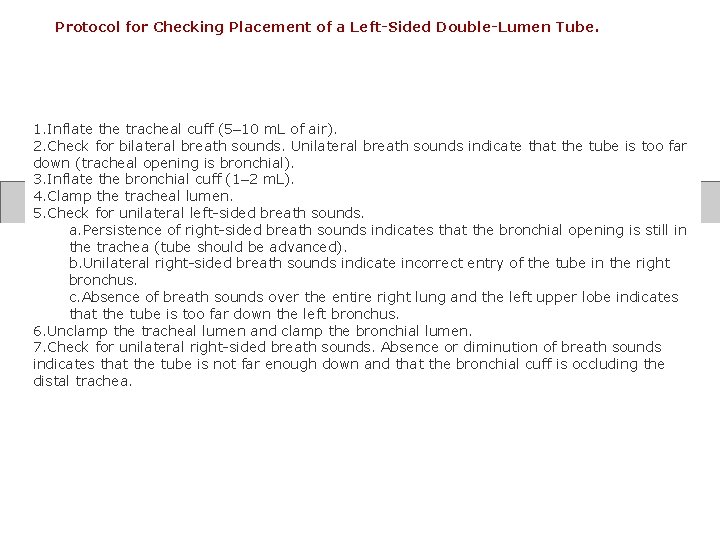
Protocol for Checking Placement of a Left-Sided Double-Lumen Tube. 1. Inflate the tracheal cuff (5– 10 m. L of air). 2. Check for bilateral breath sounds. Unilateral breath sounds indicate that the tube is too far down (tracheal opening is bronchial). 3. Inflate the bronchial cuff (1– 2 m. L). 4. Clamp the tracheal lumen. 5. Check for unilateral left-sided breath sounds. a. Persistence of right-sided breath sounds indicates that the bronchial opening is still in the trachea (tube should be advanced). b. Unilateral right-sided breath sounds indicate incorrect entry of the tube in the right bronchus. c. Absence of breath sounds over the entire right lung and the left upper lobe indicates that the tube is too far down the left bronchus. 6. Unclamp the tracheal lumen and clamp the bronchial lumen. 7. Check for unilateral right-sided breath sounds. Absence or diminution of breath sounds indicates that the tube is not far enough down and that the bronchial cuff is occluding the distal trachea.
Problems with double-lumen tubes • (1) the tube tip is too distal: • (2) the tube tip is too proximal: • (3) the tube is in (the wrong side).
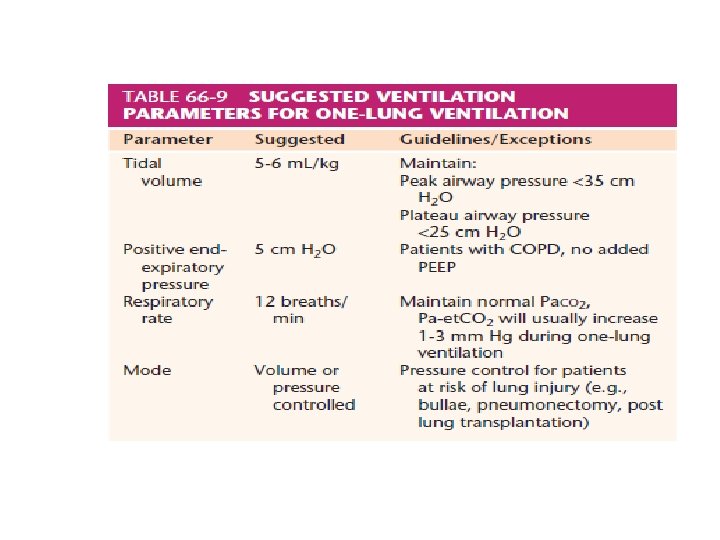
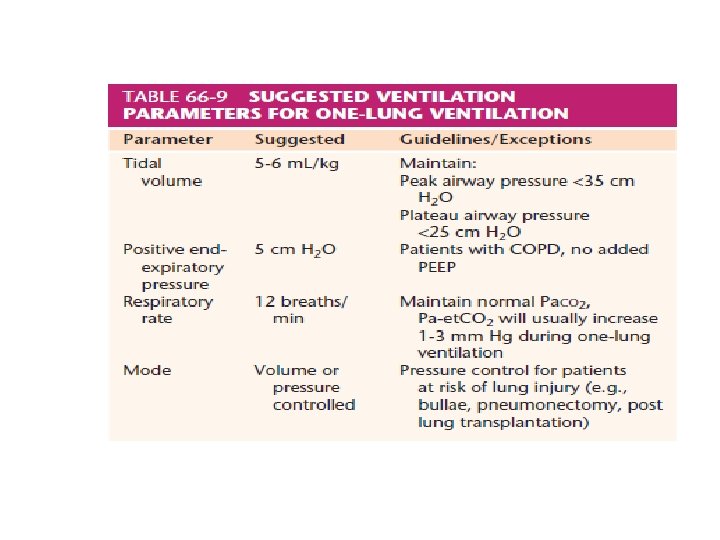
OLV • Clamp tube • Ventilator 設定 • O 2 (100% ? )
塌陷問題 • 有ventilation • 沒有 ventilation • OLV 前 使用? % O 2 (on the speed of collapse of the nonventilated lung during OLV. )
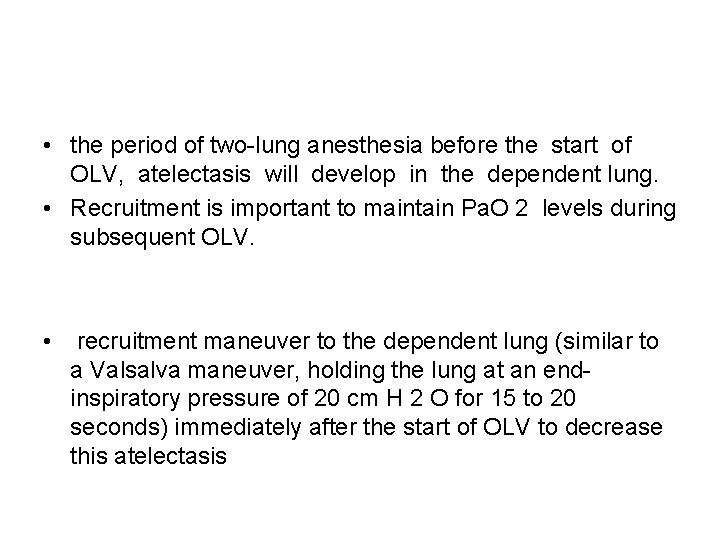
• the period of two-lung anesthesia before the start of OLV, atelectasis will develop in the dependent lung. • Recruitment is important to maintain Pa. O 2 levels during subsequent OLV. • recruitment maneuver to the dependent lung (similar to a Valsalva maneuver, holding the lung at an endinspiratory pressure of 20 cm H 2 O for 15 to 20 seconds) immediately after the start of OLV to decrease this atelectasis
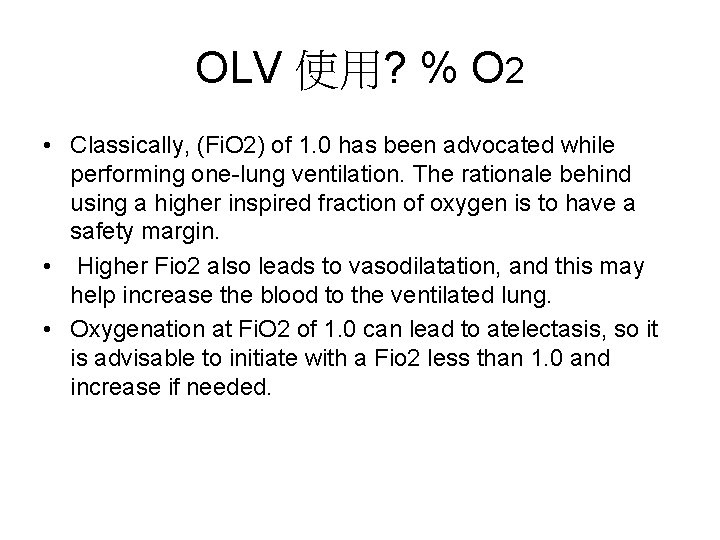
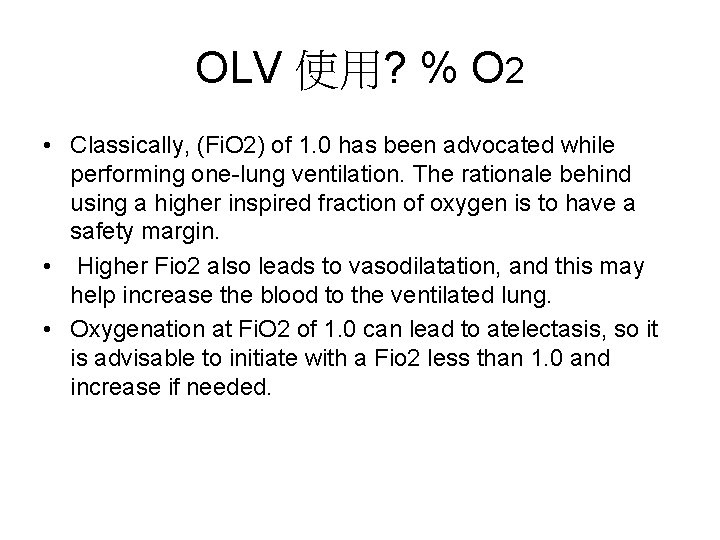
OLV 使用? % O 2 • Classically, (Fi. O 2) of 1. 0 has been advocated while performing one-lung ventilation. The rationale behind using a higher inspired fraction of oxygen is to have a safety margin. • Higher Fio 2 also leads to vasodilatation, and this may help increase the blood to the ventilated lung. • Oxygenation at Fi. O 2 of 1. 0 can lead to atelectasis, so it is advisable to initiate with a Fio 2 less than 1. 0 and increase if needed.
• A highly reactive form of the oxygen molecule, called the oxygen free radical, which destroys proteins and membranes in the epithelial cells, probably causes this damage.

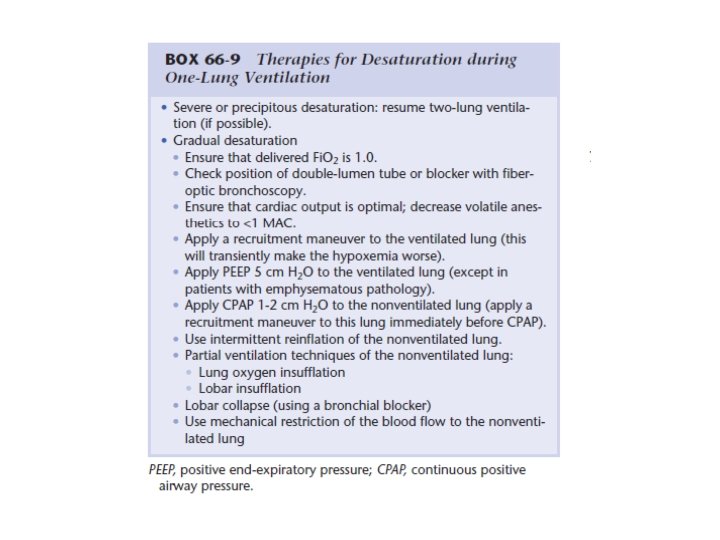
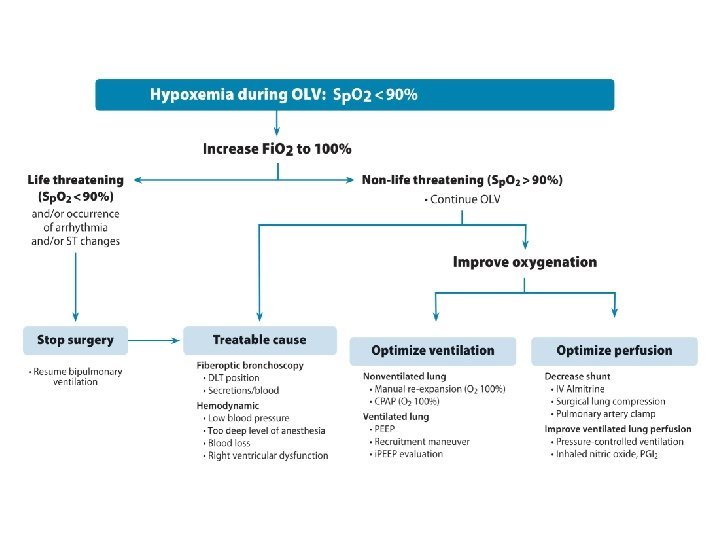
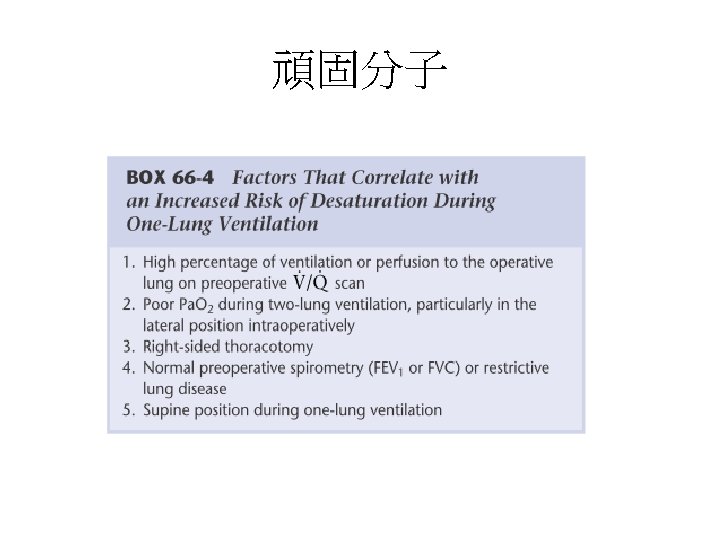
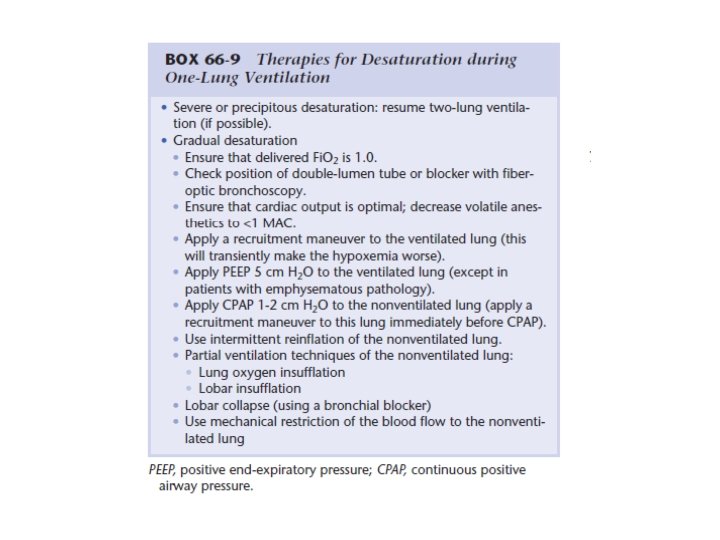
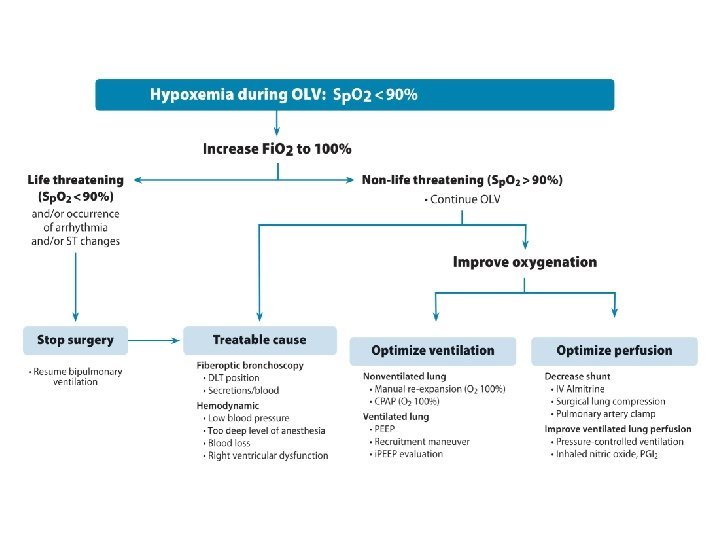
• hypoxia develops during the performance of one lung ventilation
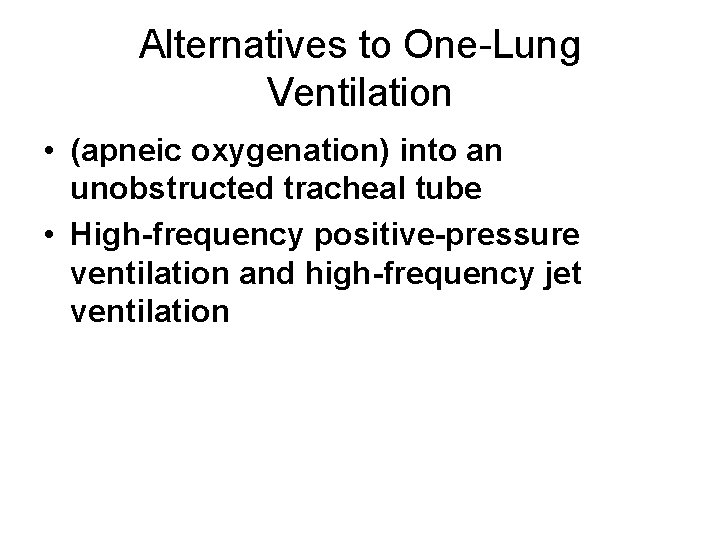
Alternatives to One-Lung Ventilation • (apneic oxygenation) into an unobstructed tracheal tube • High-frequency positive-pressure ventilation and high-frequency jet ventilation
不盡人意 • two lung ventilation.
手術結束重返two lung ventilation • Re- expansion • Air leak • lung protection. The ventilated dependent lung is prone to ventilator-induced lung injury due to higher tidal volumes used. The non-dependent non ventilated lung is prone to injury by surgical trauma and ischemia-reperfusion injuries.
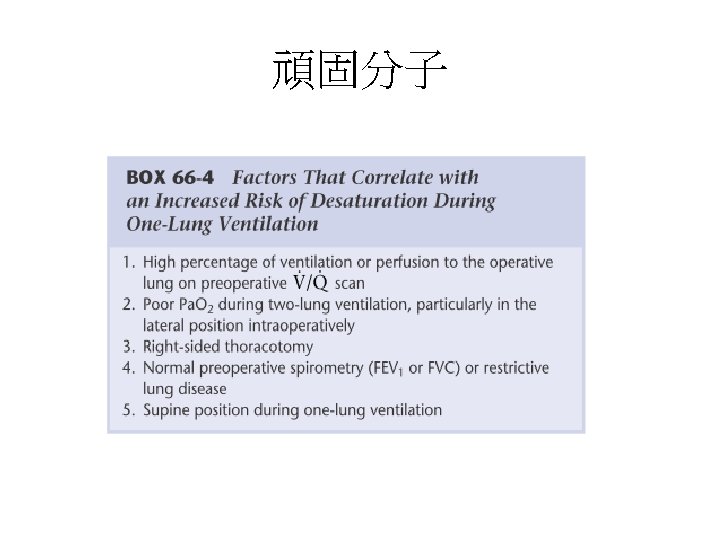
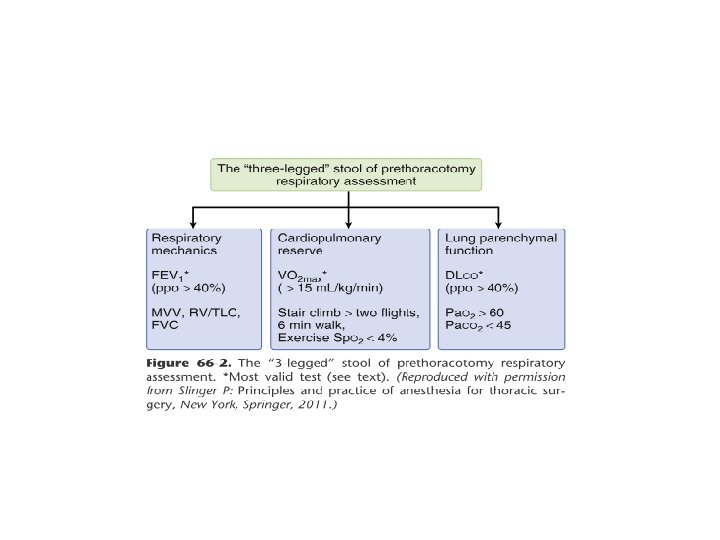
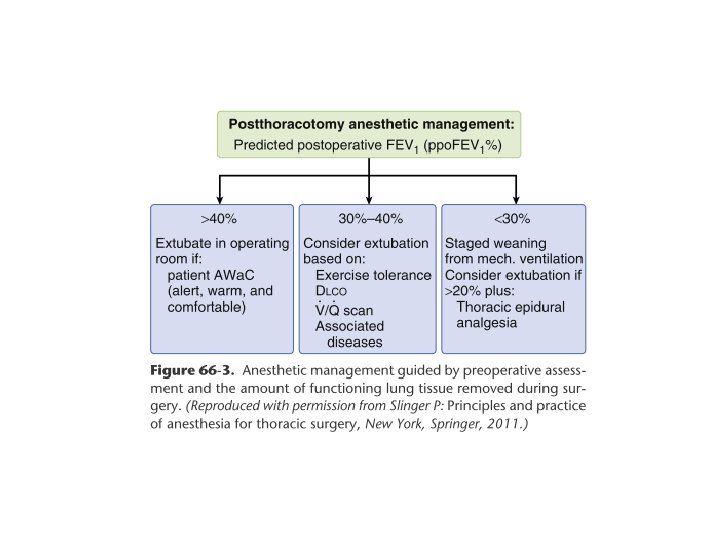
Preoperative Considerations • Difficult intubation • Prediction of desaturation during OLV • Postthoracotomy anesthetic management ---- extubation
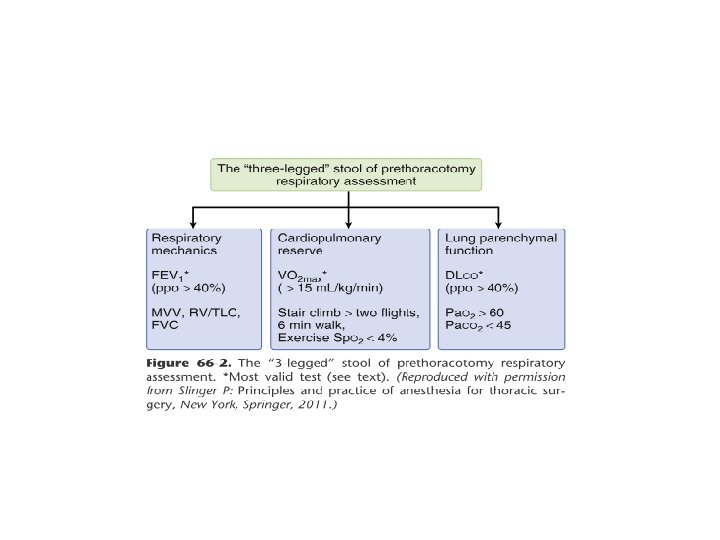
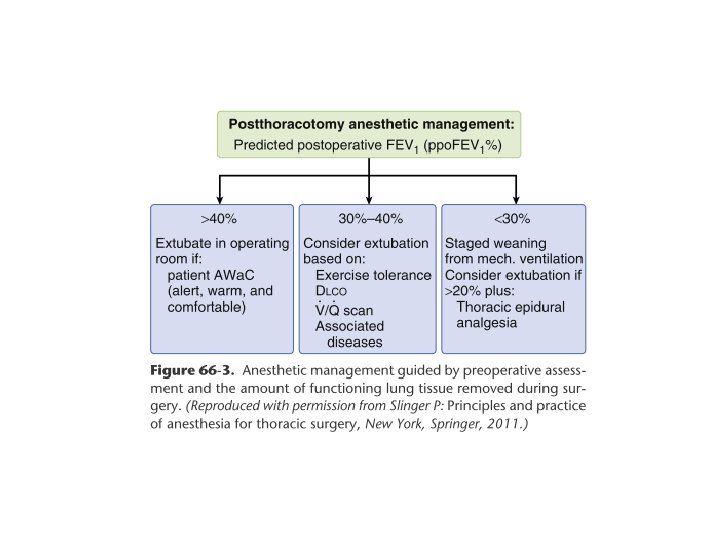
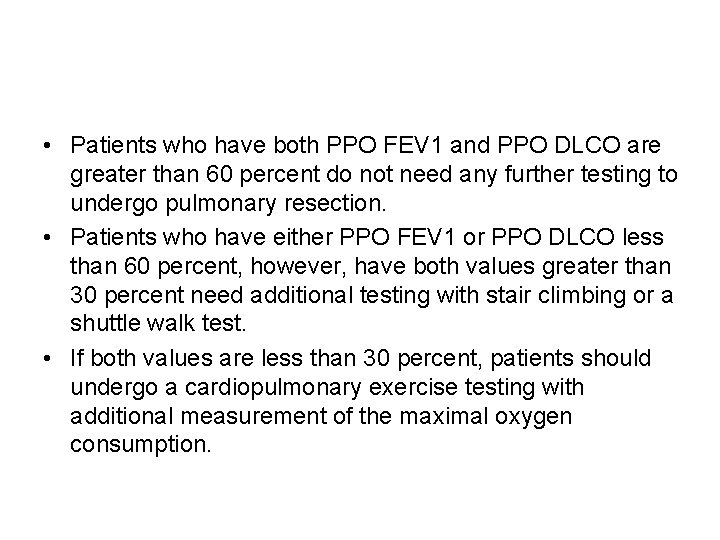
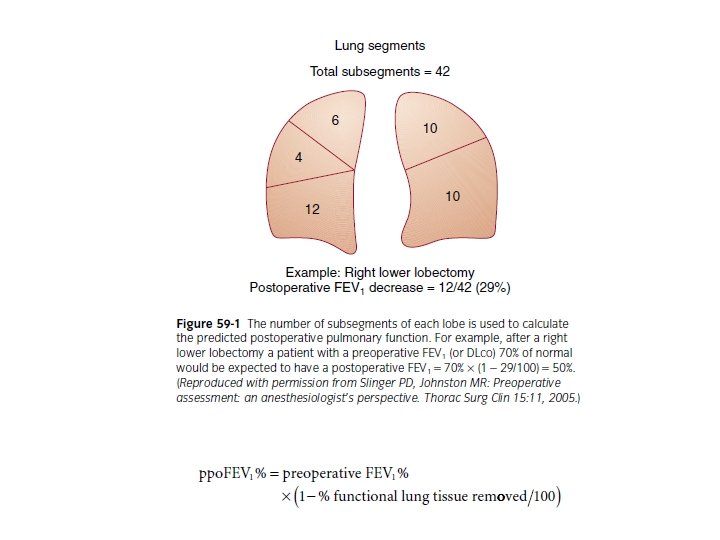
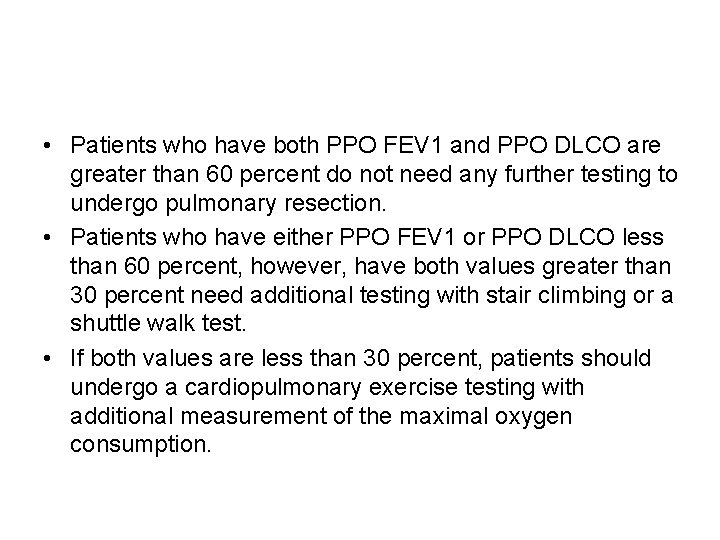
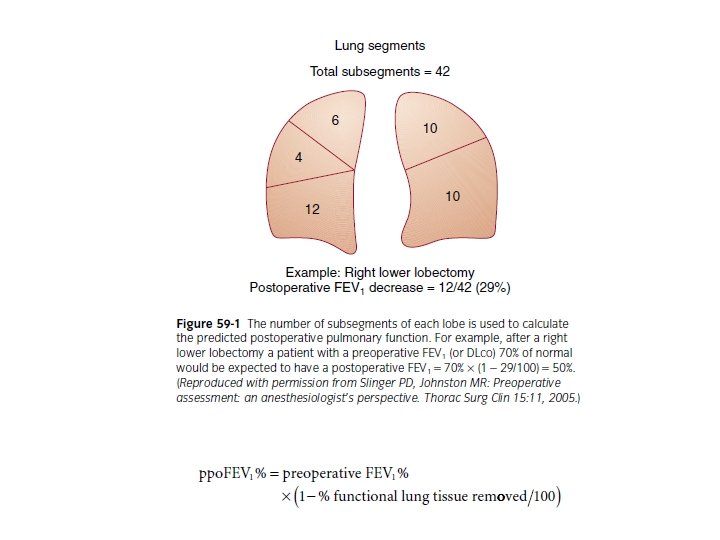
• Patients who have both PPO FEV 1 and PPO DLCO are greater than 60 percent do not need any further testing to undergo pulmonary resection. • Patients who have either PPO FEV 1 or PPO DLCO less than 60 percent, however, have both values greater than 30 percent need additional testing with stair climbing or a shuttle walk test. • If both values are less than 30 percent, patients should undergo a cardiopulmonary exercise testing with additional measurement of the maximal oxygen consumption.
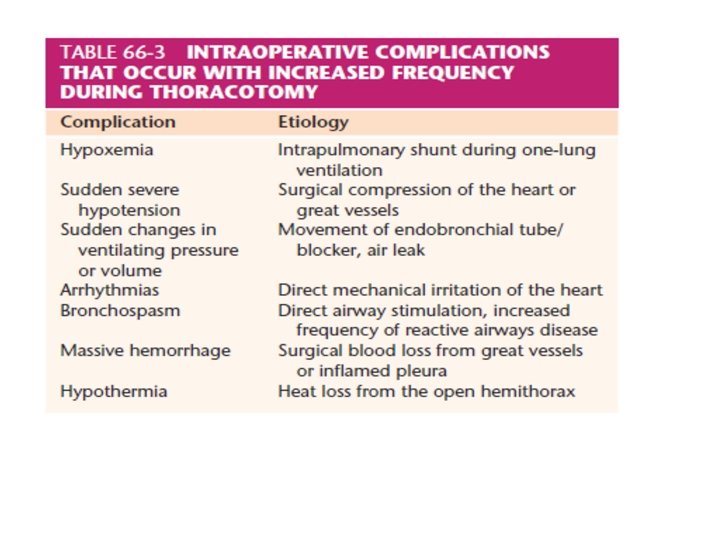
• Fluid management: • Temperature • Prevent bronchospasm
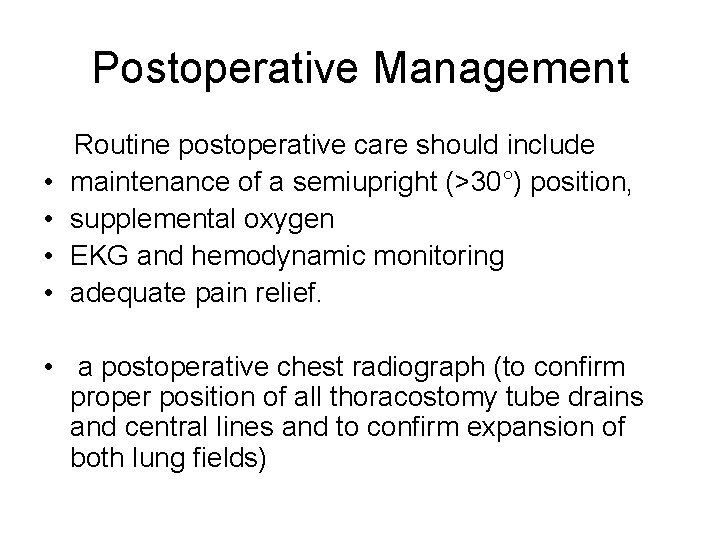
Postoperative Management • • Routine postoperative care should include maintenance of a semiupright (>30°) position, supplemental oxygen EKG and hemodynamic monitoring adequate pain relief. • a postoperative chest radiograph (to confirm proper position of all thoracostomy tube drains and central lines and to confirm expansion of both lung fields)