Chapter 31 and Chapter 32 Enteral and Parenteral

- Slides: 56
Chapter 31 and Chapter 32 Enteral and Parenteral Nutrition
Enteral Nutrition delivered via tube in gastrointestinal (GI) tract Placed in stomach or small intestine Type of tube and placement method vary per patient condition Short term versus long term • Pulmonary aspiration risk • Nurse responsibilities include placing and caring for the tube, administering nutrient formula, and preventing complications Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 2
Tube Feeding Indications Ø Anorexia Ø Orofacial Ø Neurologic conditions Ø Psychiatric conditions Ø Chemotherapy Ø Radiation therapy fractures Ø Head/neck cancer Ø Burns Ø Nutritional deficiencies 3
Patient-Centered Care Many social, religious, and cultural events involve food; patients requiring long-term tube feeding may feel a sense of loss regarding their ability to participate in life activities A multidisciplinary team can help patients and family caregivers use strategies to preserve or enhance quality of life Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 4
Tube Feeding Delivery options include Ø Continuous pump Ø Gravity Ø Bolus by syringe Ø Cyclic feedings 5
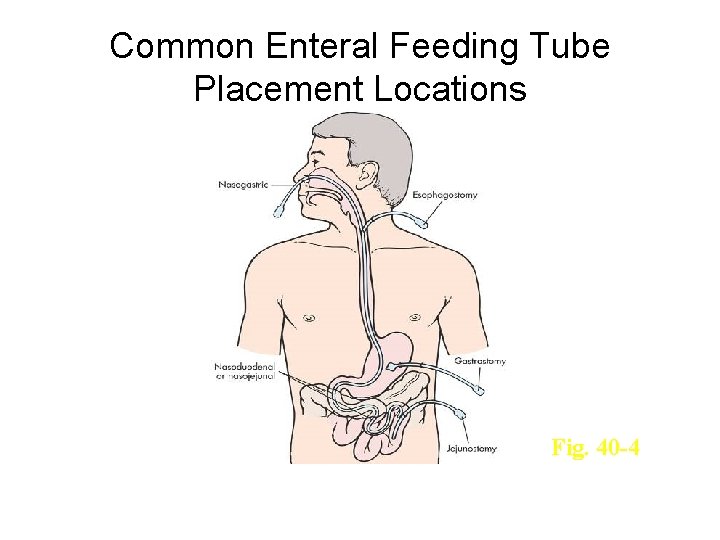
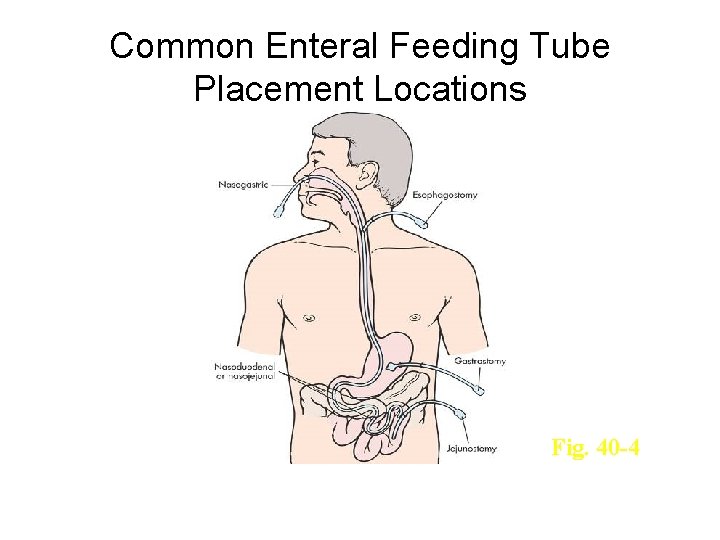
Common Enteral Feeding Tube Placement Locations Fig. 40 -4 6
Evidence-Based Practice • Blind placement • Inadvertent pulmonary intubation • Aspiration • Verification of correct tube placement • Regurgitation Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 7
Tube Feeding Nasogastric and nasointestinal tubes Ø Inserted through the nasal cavity Ø Radiopaque: Allowing visualization ray Ø Advantages Ø Disadvantages 8 from X-
Tube Feeding: NG Ø General nursing considerations • Daily weights • Assess for bowel sounds before feedings • Accurate I&O • Initial glucose checks • Label with date and time started • Feedings infusing >8 hours discarded • Pump tubing changed q 24 h • Complications 9
Safety Guidelines 1. Be aware of factors that increase risk for complications related to feeding tube insertion. 2. Know the purpose of the feeding and the intended location of the tip of the feeding tube. 3. Take precautions to prevent microbial contamination of enteral formulas Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 10
Safety Guidelines, cont. 4. Be aware of safety measures to prevent pulmonary aspiration and accidental tube displacement. 5. Consult with a pharmacist regarding medications and their route of delivery. 6. Be vigilant when manipulating components of enteral feeding systems for procedures. Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 11
Inserting and Removing a Small-Bore Nasogastric or Nasoenteric Feeding Tube Skill 31 -1 Placement of a feeding tube requires a health care provider’s order All candidates require an assessment of their coagulation status Removable guidewires or stylets may be used to aid tube placement; use caution because these add to risk of injury Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 12
Delegation and Collaboration The task of feeding tube insertion cannot be delegated to nursing assistive personnel (NAP) However, NAP may help with patient positioning and comfort measures during tube insertion Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 13
Recording and Reporting • Record and report type and size of tube placed, location of distal tip of tube, patient’s tolerance of procedure, and confirmation of tube position by x-ray film examination • Record removal of tube and patient’s tolerance • Report any type of unexpected outcome and the interventions performed • Tube removal: record level of comfort Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 14
Special Considerations Teaching Offer oral hygiene frequently • Report any problems with the tube • Pediatric Sizing gastric tube • X-ray confirmation not usually performed • Routine tube flushing not recommended • Observe for vagal stimulation in infants • Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 15
Special Considerations, cont. Gerontologic • Ensure adequate lubrication Home care Assess patient’s/caregiver’s ability • Assess environment for safety and sanitation • Teach assessment of tube placement • Teach how to secure feeding tube • Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 16
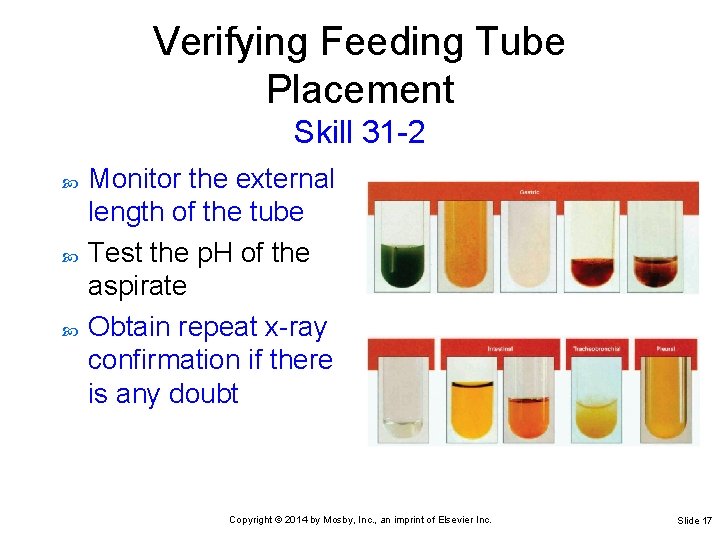
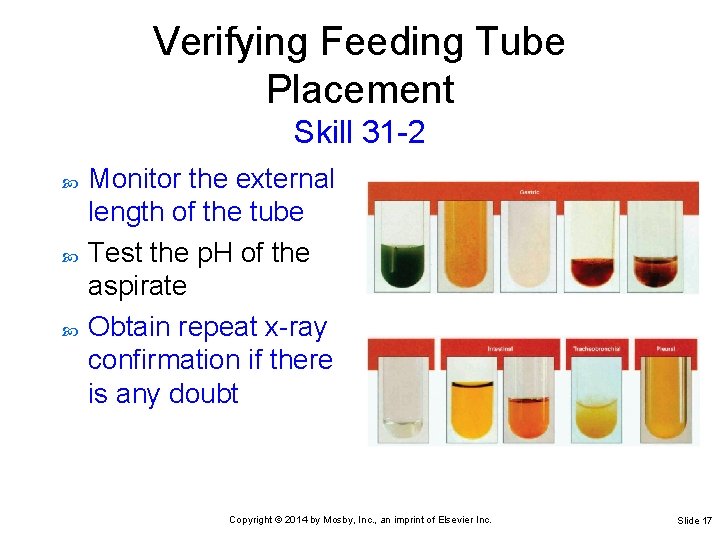
Verifying Feeding Tube Placement Skill 31 -2 Monitor the external length of the tube Test the p. H of the aspirate Obtain repeat x-ray confirmation if there is any doubt Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 17
Delegation and Collaboration Verification of tube placement cannot be delegated to NAP With regard to tube placement, what observations does the nurse direct NAP to report? Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 18
Recording and Reporting • Record and report p. H and appearance of aspirate Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 19
Special Considerations Teaching • Pediatric • Do not pull or alter position of tube Decrease amount of air insufflated according to size of the patient before withdrawal of gastric secretions Home care • Do not use tube if placement is in doubt Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 20
Irrigating a Feeding Tube Skill 31 -3 All types of feeding tubes require routine irrigation to keep a tube patent Inability to instill air or fluid suggests that a tube is occluded Curdled enteral formula and improperly crushed medications are the most common causes of feeding tube occlusion Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 21
Special Considerations Pediatric • Irrigation of tube requires a smaller volume of solution in children: 1 to 3 m. L for neonates and 3 to 5 m. L for pediatric patients Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 22
Administering Enteral Nutrition: Nasoenteric, Gastrostomy, or Jejunostomy Tube Skill 31 -4 What is the most common type of enteral nutrition? Small bowel feeding may reduce risk of aspiration An enteral pump is used to control the administration rate of small bowel and many continuous gastric feedings Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 23
Delegation and Collaboration The task of administration of nasoenteric tube feeding can be delegated to NAP The nurse directs NAP to: Elevate the patient’s head and not adjust feeding rate • Report any difficulty infusing the feeding or any discomfort voiced by the patient, including any gagging, paroxysms of coughing, or choking • Provide frequent oral hygiene • Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 24
Recording and Reporting • Record and report amount and type of feeding, method of infusion, patient’s response to tube feeding (e. g. , gastric residual volume [GRV], cramping), patency of tube, condition of skin at tube site • Record on intake and output form volume of formula and any additional water • Report type of feeding, status of feeding tube, patient’s tolerance, and adverse outcomes Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 25
Special Considerations Teaching Patient should remain upright for 1 hour after feedings, if tolerated • Troubleshoot tube and patient signs and symptoms • Pediatric • Procedures for infants and patients at risk for necrotizing enterocolitis; GRV Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 26
Special Considerations, cont. Gerontologic • Some older adults have decreased gastric emptying; GRV checks are needed Home care Report symptoms of discomfort during enteral feedings • Perform skin care around the tube • Recognize signs and symptoms of infection at insertion site • Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 27
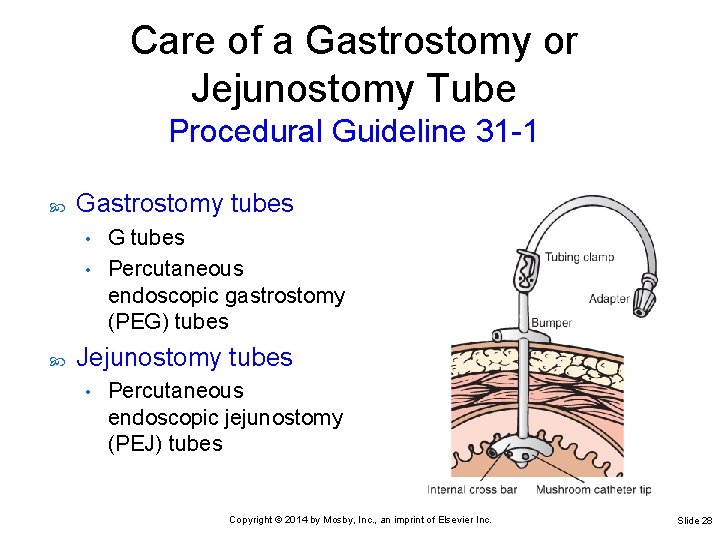
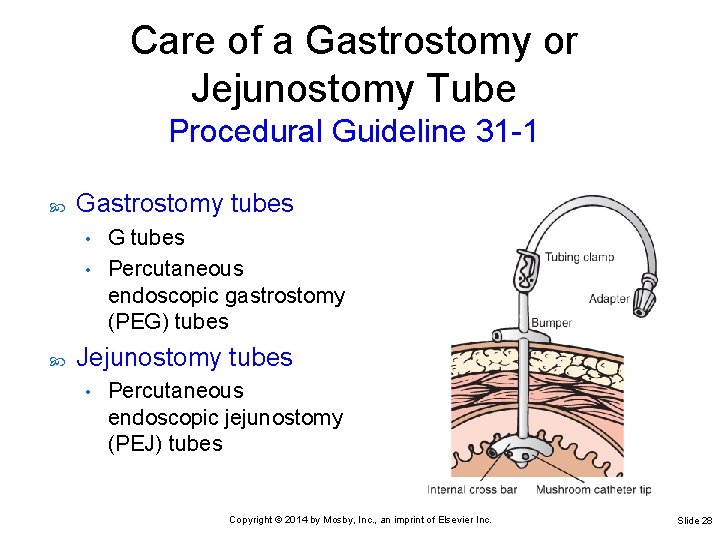
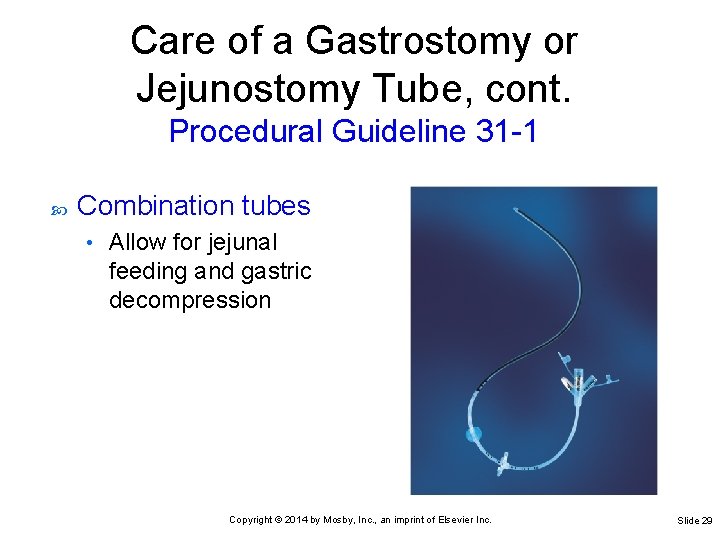
Care of a Gastrostomy or Jejunostomy Tube Procedural Guideline 31 -1 Gastrostomy tubes G tubes • Percutaneous endoscopic gastrostomy (PEG) tubes • Jejunostomy tubes • Percutaneous endoscopic jejunostomy (PEJ) tubes Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 28
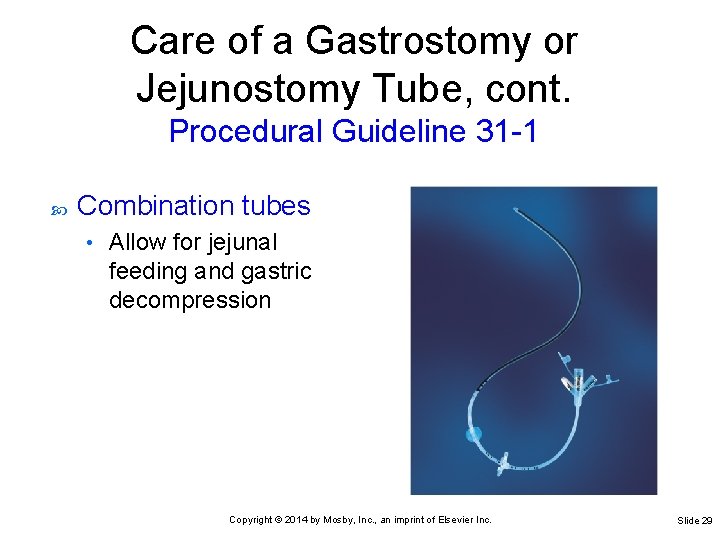
Care of a Gastrostomy or Jejunostomy Tube, cont. Procedural Guideline 31 -1 Combination tubes • Allow for jejunal feeding and gastric decompression Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 29
Delegation and Collaboration Care of a PEG or PEJ tube cannot be delegated to NAP The nurse directs NAP to: Inform the nurse of any patient complaints of discomfort at insertion site • Inform the nurse of any drainage on insertion site dressing • Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 30
Medication Administration Preferably medications should be in liquid form. May crush certain medications Tubing must be flushed before and after the medication Keep head of bed 30 degrees or higher Monitor for aspiration If continuous infusion, stop feeding Always check for residual Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 31
Parenteral Nutrition (PN) • Specialized form of nutritional support • Given intravenously by an infusion pump • For patients with significant gastrointestinal (GI) dysfunction • An adjunctive therapy to enteral tube feeding in critically ill patients • May be used short term or long term Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 32
Common Indications for PN Chronic diarrhea and vomiting Complicated surgery or trauma Gastrointestinal obstruction Gastrointestinal tract anomalies and fistulae Intractable diarrhea Burns Malnutrition 33
Risks Associated With Parenteral Nutrition • Catheter-related bloodstream infection (CRBSI) • Sludge accumulating in gallbladder • Acute cholecystitis • Liver disease • Very severe GI disease • Long-term PN metabolic bone disease • Allergic reaction Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 34
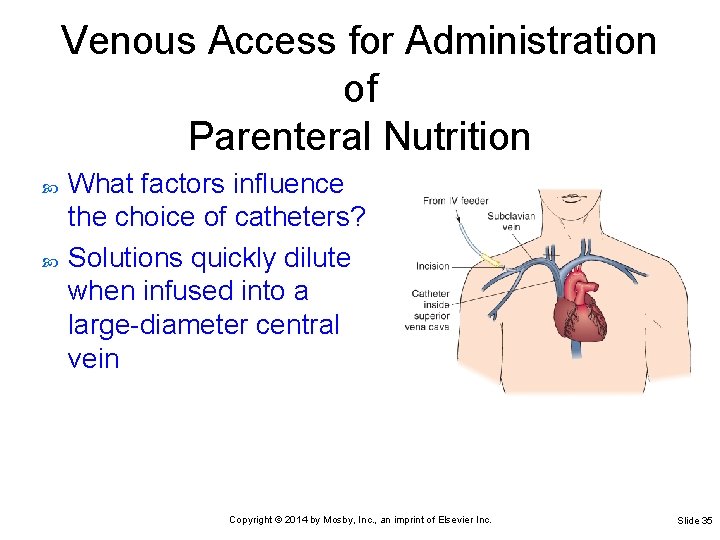
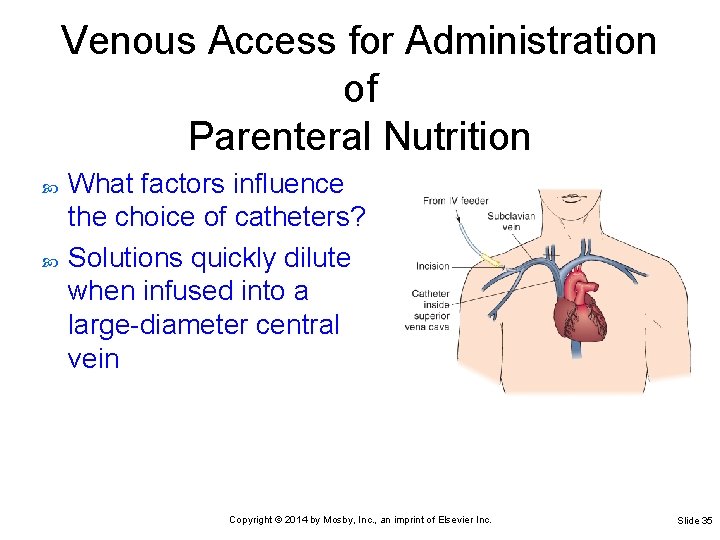
Venous Access for Administration of Parenteral Nutrition What factors influence the choice of catheters? Solutions quickly dilute when infused into a large-diameter central vein Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 35
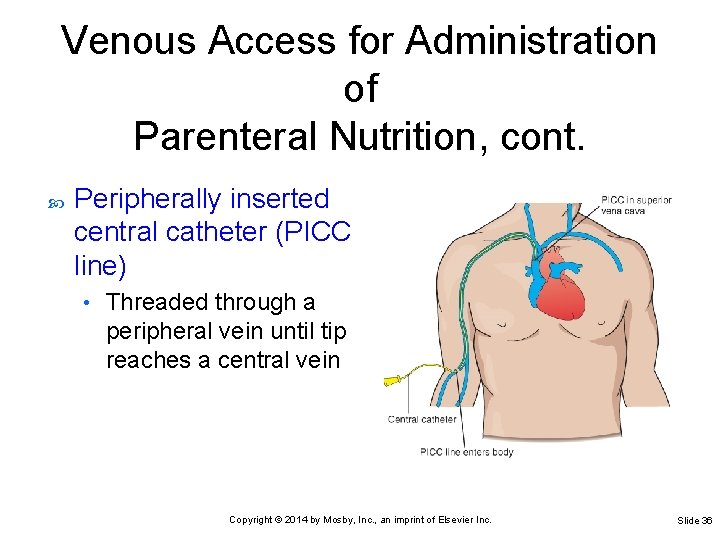
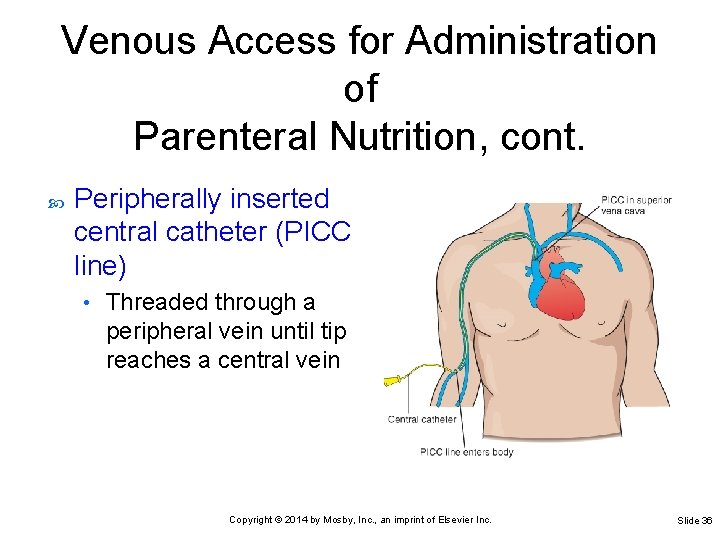
Venous Access for Administration of Parenteral Nutrition, cont. Peripherally inserted central catheter (PICC line) • Threaded through a peripheral vein until tip reaches a central vein Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 36
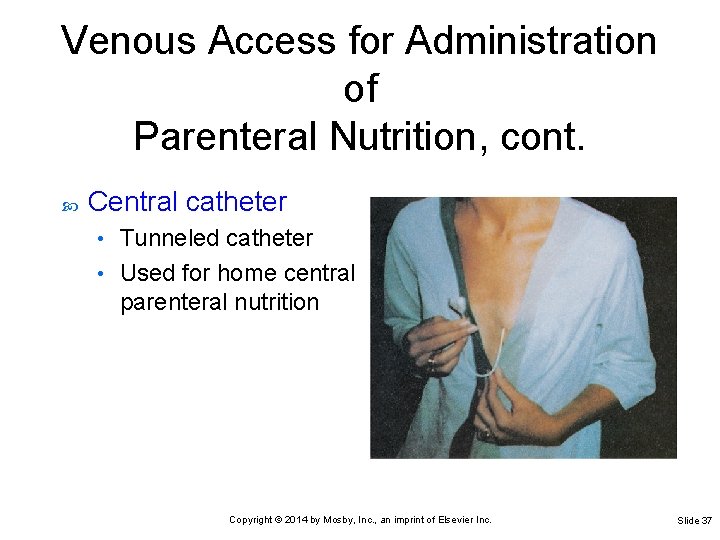
Venous Access for Administration of Parenteral Nutrition, cont. Central catheter Tunneled catheter • Used for home central parenteral nutrition • Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 37
Components of a Parenteral Nutrition Solution Energy sources are amino acids, glucose, and lipids Also included are electrolytes, minerals, trace elements, vitamins, and water If lipid emulsion is added, the PN solution is called a 3: 1, 3 -in-1, or total nutrition admixture (TNA) Patients who receive glucose/amino acids but no lipids are at risk for essential fatty acid deficiency (EFAD) Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 38
Medications • Regular insulin • Medications that reduce gastric acidity • Routine addition of any medications is discouraged when the compatibility and the stability of the components are not known • Bedside addition of any medication is prohibited by most hospital policies Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 39
Administration of Parenteral Nutrition Dietitians or pharmacists typically provide advice on nutrition support goals and/or write PN orders PN solutions prepared by pharmacist or trained technician under strict aseptic techniques • Must be refrigerated until 30 minutes before use • Must be labeled with nutrient content, all additives, time mixed, date and time of expiration Nurses administer ordered PN at the bedside Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 40
Laboratory Monitoring • Blood glucose levels • Electrolytes • Serum proteins • Complete blood count Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 41
Monitoring Patient Status and Outcomes Intake and output • Patient’s body weight • Measured every 8 hours Measured at least three times weekly Patient’s temperature • Measured every 4 hours, with vital signs Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 42
Evidence-Based Practice PN recommendations include: Early nutritional assessment is crucial to determine a patient’s need for PN as a single or adjunct therapy • Blood glucose should be maintained in a range of 70 to 180 mg/d. L • The ideal method for delivering PN is through a central venous catheter • Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 43
Patient-Centered Care Accommodate religious and cultural beliefs Avoidance of animal products • Daytime fasting during Ramadan • Use of mechanical devices on the Sabbath • Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 44
Safety Guidelines 1. Know the complications associated with PN. 2. Monitor a patient’s vital signs, electrolyte levels, glucose levels, triglyceride levels, weight, and fluid intake and output, and compare baseline with treatment values. 3. Know the patient’s recent temperature range. Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 45
Safety Guidelines, cont. 4. Routinely assess the site of a central venous access device for signs of infection. 5. Use strict aseptic technique in the care and maintenance of central venous catheters and PICC lines. Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 46
Administering Parenteral Nutrition Through a Central Line Skill 32 -1 Use strict aseptic technique Apply critical thinking Anticipate changes in a patient’s condition that signal developing complications • Use good judgment to maintain the IV system and ensure that it is functioning properly • Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 47
Delegation and Collaboration The task of administering central peripheral nutrition (CPN) cannot be delegated to nursing assistive personnel (NAP) The nurse directs NAP to: Report pump alarms, wet catheter dressings, elevated temperatures, and patient complaints • Perform fingerstick blood glucose monitoring and report any abnormal results • Report vital signs that are out of range • Weigh patient as directed • Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 48
Recording and Reporting • Record condition of central venous access device, rate and type of infusion, catheter lumen used for infusion, intake and output (I&O) every 8 hours, blood glucose levels, vital signs, and weight • If signs of infection, occlusion, fluid retention, or infiltration occur, notify the health care provider Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 49
Special Considerations Teaching Explain purpose and goal of CPN • Inform about daily care of central line • Pediatric • Consider developmental needs of children on long -term CPN; perform regular assessment of development and encourage expected milestones Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 50
Special Considerations, cont. Gerontologic • Impaired ability to tolerate higher fluid volumes due to cardiac or renal impairment Home care • Teaching for home CPN administration will be given after discharge or may be initiated in hospital and continued at home Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 51
Administering Parenteral Nutrition Through a Peripheral Line Skill 32 -2 Indications for peripheral parenteral nutrition (PPN): Adequate peripheral access • Ability to tolerate larger volumes of fluid • Ability to tolerate lipid emulsions • This therapy is for short-term use, usually 2 weeks or less Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 52
Delegation and Collaboration The task of administering PPN through a peripheral intravenous (IV) line cannot be delegated to NAP The nurse directs NAP to: Report patient complaint of burning, pain, or redness at IV site, shortness of breath, and vital sign changes • Report infusion pump alarms or moist IV site dressing • Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 53
Recording and Reporting • Record in nurses’ notes or on appropriate flow sheets condition of IV site, types of solutions, rate and status of infusion, catheter lumen used for infusion, I&O every 8 hours, blood glucose levels, vital signs, weight, and other assessment findings Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 54
Recording and Reporting, cont. • Record in nurses’ notes any adverse reactions • If signs of fat intolerance, infection, occlusion, fluid retention, or infiltration occur, notify the health care provider Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 55

Special Considerations Teaching • PPN administration does not occur in the home Gerontologic • Some older adults may have fragile peripheral veins or poor fluid tolerance, making PPN undesirable Copyright © 2014 by Mosby, Inc. , an imprint of Elsevier Inc. Slide 56