The Impact of Enteral Feeding Protocols on Enteral

- Slides: 21
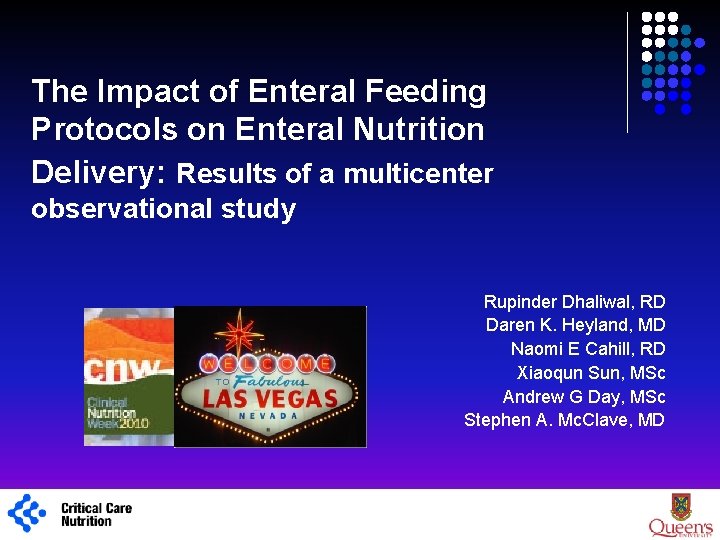
The Impact of Enteral Feeding Protocols on Enteral Nutrition Delivery: Results of a multicenter observational study Rupinder Dhaliwal, RD Daren K. Heyland, MD Naomi E Cahill, RD Xiaoqun Sun, MSc Andrew G Day, MSc Stephen A. Mc. Clave, MD 1
Background l Feeding protocols are considered to be an effective strategy to maximize the benefits and minimize the risks of enteral nutrition in critically ill patients. l Components of feeding protocols may include orders for l l l The benefits of such protocols would be: l l 1 Early initiation of enteral nutrition Use of motility agents Gastric residual volumes Head of the bed elevation Use of small bowel feeding tubes to standardize the delivery of EN to automate the provision of EN
What do Guidelines say? “Use of a feeding protocol that incorporates prokinetics at initiation, higher GRVs (250 mls) and use of post pyloric feeding tubes should be considered” “Use of enteral feeding protocols increases the overall percentage of goal calories provided and should be implemented. ” Avoid holding EN for GRVs < 500 mls. Grade: C, B 1 “Evaluating gastric residual volume (GRV) in critically ill patients is an optional part of a monitoring plan to assess tolerance of EN. “ Avoid holding EN when GRV < 250 mls. Consensus, imperative
RCT Level of Evidence § RCTs of aggressive feeding protocols § Results in better protein-energy intake § Associated with reduced complications and improved survival Taylor et al Crit Care Med 1999; Martin CMAJ 2004; Doig GS JAMA 2008 However, the estimates of their effectiveness are limited due to: § the nature of small single-center studies § the bundling with many other interventions in cluster randomized controlled trials. 1
Purpose To evaluate the effect of an ICU site-based feeding protocol on nutrition practices and outcomes in the context of an international multicenter, observational study. Objective To compare the following performance criteria between sites that did or did not use a feeding protocol: § Use of EN § Time to start EN § Adequacy of enteral nutrition § Adequacy of overall nutrition § Clinical outcomes 1

Primary Outcomes Overall nutritional adequacy Enteral nutrition adequacy Overall nutritional adequacy = as the total amount of calories or protein received (from EN + appropriate PN + propofol) /prescribed x 100% Overall EN adequacy = as the total amount of calories or protein received (from EN) /prescribed x 100% 1
Methods Data from two international, prospectively, observational cohort studies conducted in 2007 and 2008 were combined. Patients: § Consecutively enrolled mechanically ventilated adults § In ICU > 3 days Data was collected from ICU admission to a maximum of 12 days: § sites recorded the presence or absence of a feeding protocol § timing, type and amount of nutrition received § strategies utilized to improve nutrition delivery (m. agents, small bowel feeds, HOB) § 60 day mortality, hospital and ICU length of stay and duration of mechanical ventilation § Each participating ICU aimed to recruit 20 patients. Nutrition practices and clinical outcomes were compared between ICUs that used a feeding protocol and those who did not. 1
Data Management Data entered on to our secure online edcs, built-in range checks and data query process. 1 www. criticalcarenutrition. com
Data Analysis Data from 2007 and 2008 combined, 334 total sites, 65 sites participated both years, 269 unique ICUs Hospital and ICU characteristics compared at the site level All other variables were compared at the patient level Clustered 2 stage sample design: patient and site, so potential for heterogeneity between ICUs. Advanced statistical methods were done to account for heterogeneity (adjusted chi square tests, multilevel modelling). 1
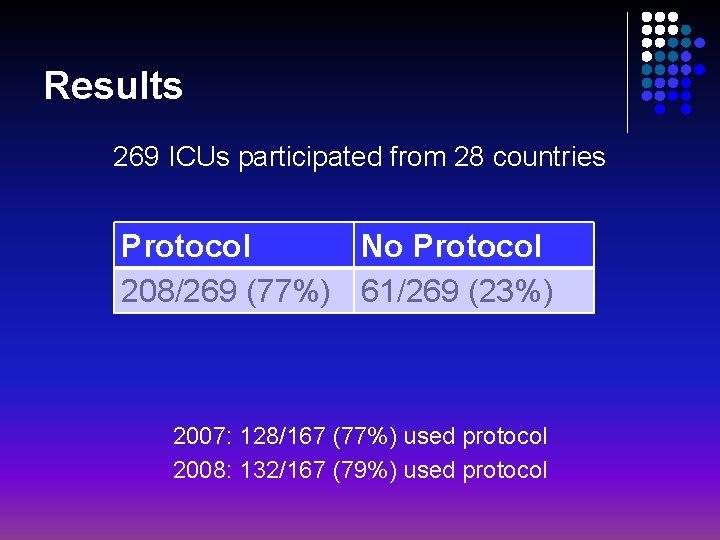
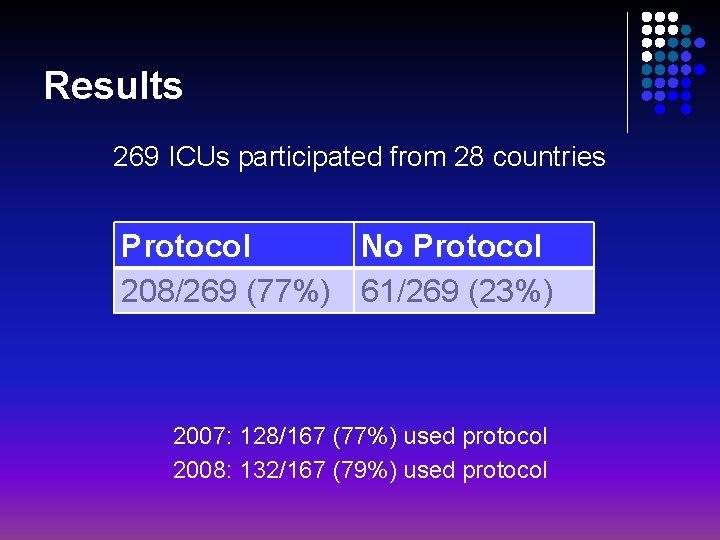
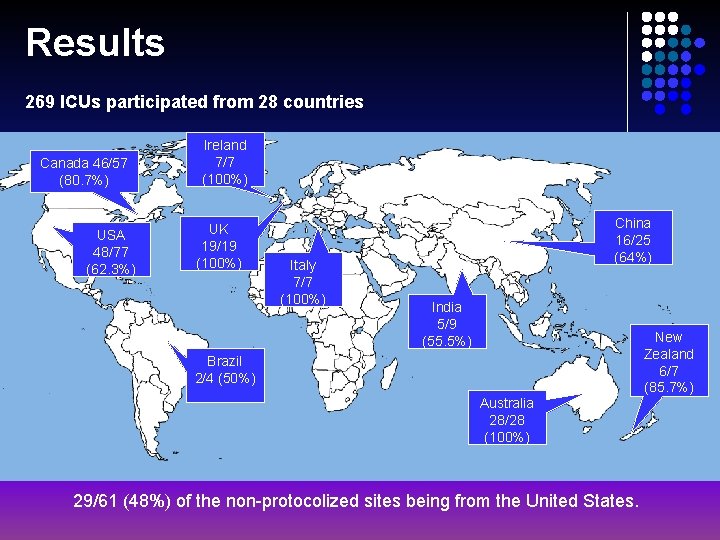
Results 269 ICUs participated from 28 countries Protocol No Protocol 208/269 (77%) 61/269 (23%) 2007: 128/167 (77%) used protocol 2008: 132/167 (79%) used protocol
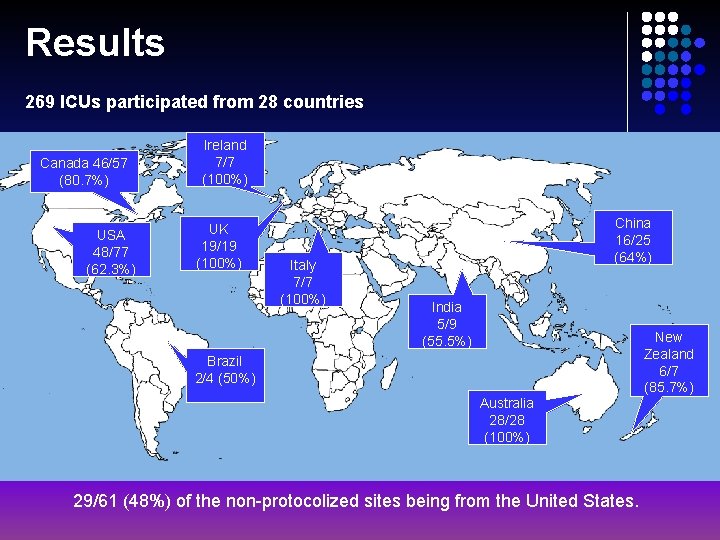
Results 269 ICUs participated from 28 countries Canada 46/57 (80. 7%) USA 48/77 (62. 3%) Ireland 7/7 (100%) UK 19/19 (100%) Italy 7/7 (100%) China 16/25 (64%) India 5/9 (55. 5%) Brazil 2/4 (50%) Australia 28/28 (100%) 29/61 (48%) of the non-protocolized sites being from the United States. New Zealand 6/7 (85. 7%)
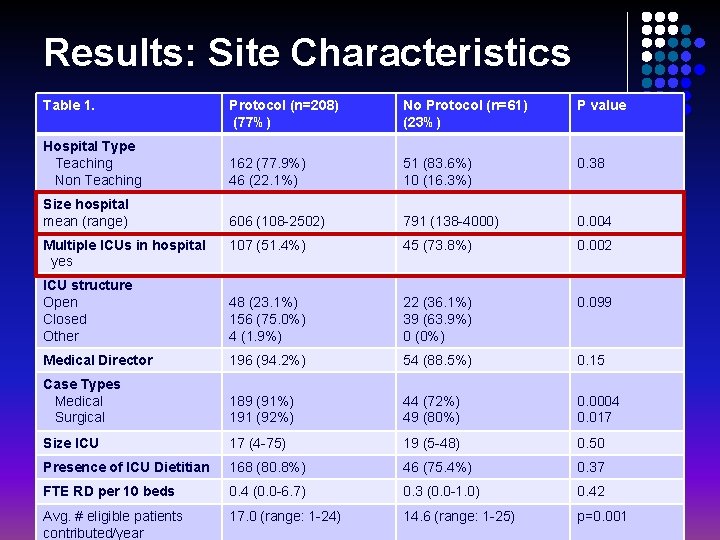
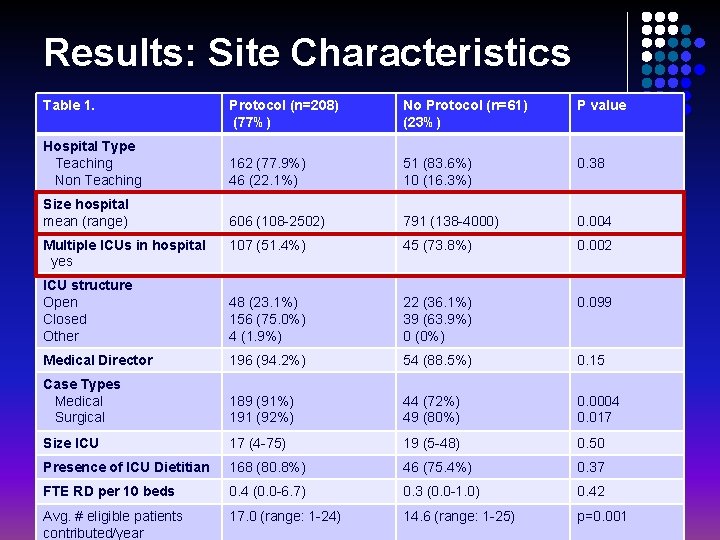
Results: Site Characteristics Table 1. Protocol (n=208) (77%) No Protocol (n=61) (23%) P value Hospital Type Teaching Non Teaching 162 (77. 9%) 46 (22. 1%) 51 (83. 6%) 10 (16. 3%) 0. 38 Size hospital mean (range) 606 (108 -2502) 791 (138 -4000) 0. 004 107 (51. 4%) 45 (73. 8%) 0. 002 ICU structure Open Closed Other 48 (23. 1%) 156 (75. 0%) 4 (1. 9%) 22 (36. 1%) 39 (63. 9%) 0 (0%) 0. 099 Medical Director 196 (94. 2%) 54 (88. 5%) 0. 15 Case Types Medical Surgical 189 (91%) 191 (92%) 44 (72%) 49 (80%) 0. 0004 0. 017 Size ICU 17 (4 -75) 19 (5 -48) 0. 50 Presence of ICU Dietitian 168 (80. 8%) 46 (75. 4%) 0. 37 FTE RD per 10 beds 0. 4 (0. 0 -6. 7) 0. 3 (0. 0 -1. 0) 0. 42 Avg. # eligible patients contributed/year 17. 0 (range: 1 -24) 14. 6 (range: 1 -25) p=0. 001 Multiple ICUs in hospital yes
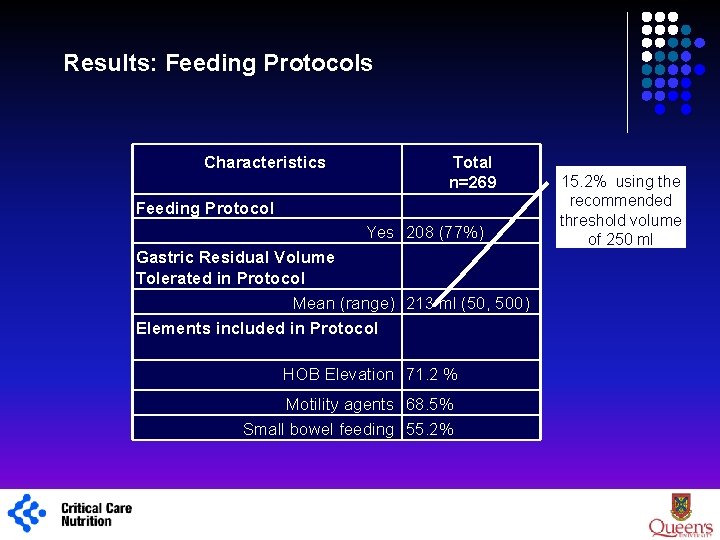
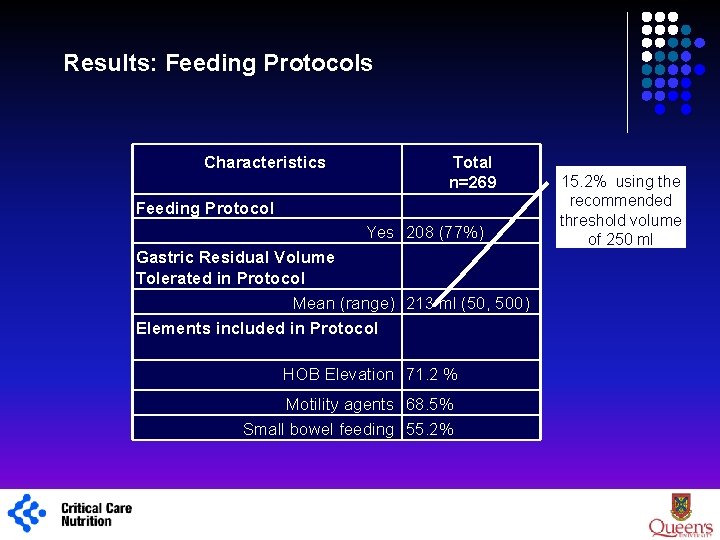
Results: Feeding Protocols Characteristics Total n=269 Feeding Protocol Yes 208 (77%) Gastric Residual Volume Tolerated in Protocol Mean (range) 213 ml (50, 500) Elements included in Protocol HOB Elevation 71. 2 % Motility agents 68. 5% Small bowel feeding 55. 2% 1 15. 2% using the recommended threshold volume of 250 ml
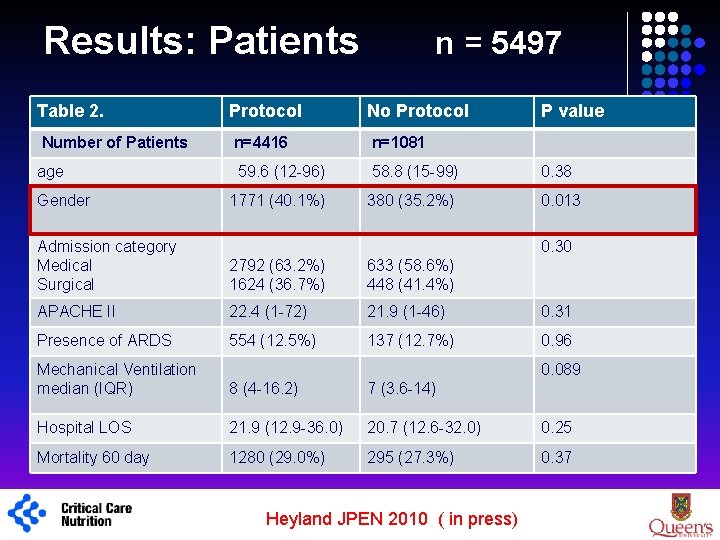
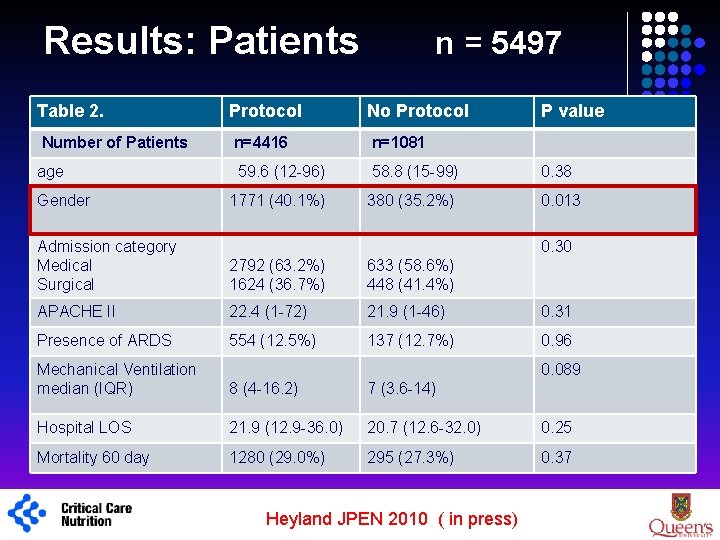
Results: Patients Table 2. Protocol No Protocol Number of Patients n=4416 n=1081 age 59. 6 (12 -96) 58. 8 (15 -99) 0. 38 1771 (40. 1%) 380 (35. 2%) 0. 013 Gender 1 n = 5497 P value Admission category Medical Surgical 0. 30 2792 (63. 2%) 1624 (36. 7%) 633 (58. 6%) 448 (41. 4%) APACHE II 22. 4 (1 -72) 21. 9 (1 -46) 0. 31 Presence of ARDS 554 (12. 5%) 137 (12. 7%) 0. 96 Mechanical Ventilation median (IQR) 0. 089 8 (4 -16. 2) 7 (3. 6 -14) Hospital LOS 21. 9 (12. 9 -36. 0) 20. 7 (12. 6 -32. 0) 0. 25 Mortality 60 day 1280 (29. 0%) 295 (27. 3%) 0. 37 Heyland JPEN 2010 ( in press)
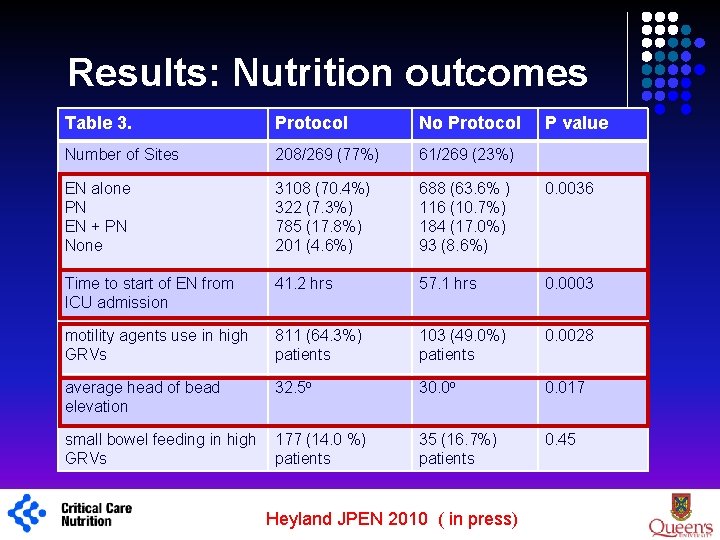
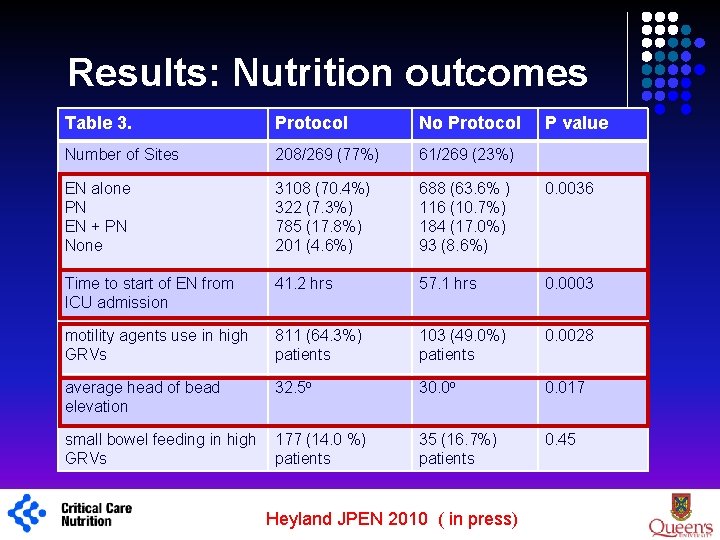
Results: Nutrition outcomes 1 Table 3. Protocol No Protocol Number of Sites 208/269 (77%) 61/269 (23%) EN alone PN EN + PN None 3108 (70. 4%) 322 (7. 3%) 785 (17. 8%) 201 (4. 6%) 688 (63. 6% ) 116 (10. 7%) 184 (17. 0%) 93 (8. 6%) 0. 0036 Time to start of EN from ICU admission 41. 2 hrs 57. 1 hrs 0. 0003 motility agents use in high GRVs 811 (64. 3%) patients 103 (49. 0%) patients 0. 0028 average head of bead elevation 32. 5 o 30. 0 o 0. 017 small bowel feeding in high GRVs 177 (14. 0 %) patients 35 (16. 7%) patients 0. 45 Heyland JPEN 2010 ( in press) P value
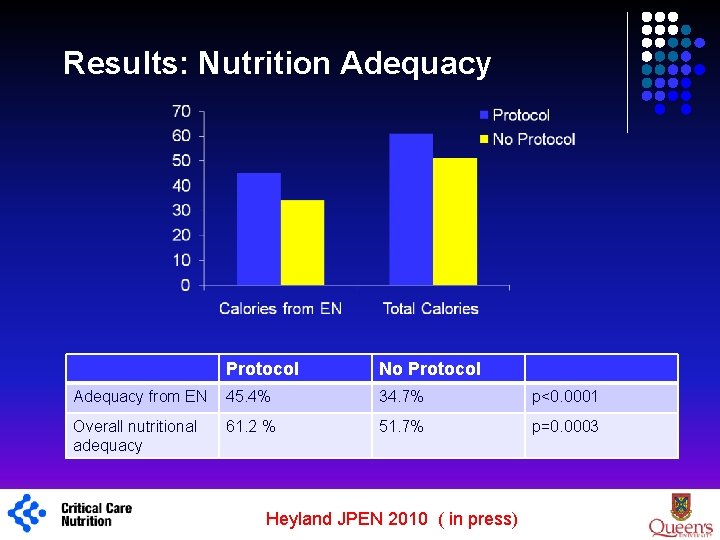
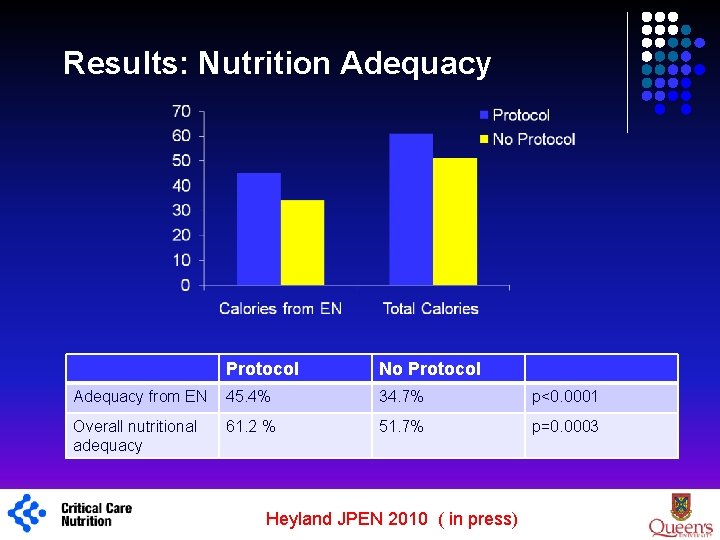
Results: Nutrition Adequacy 1 Protocol No Protocol Adequacy from EN 45. 4% 34. 7% p<0. 0001 Overall nutritional adequacy 61. 2 % 51. 7% p=0. 0003 Heyland JPEN 2010 ( in press)
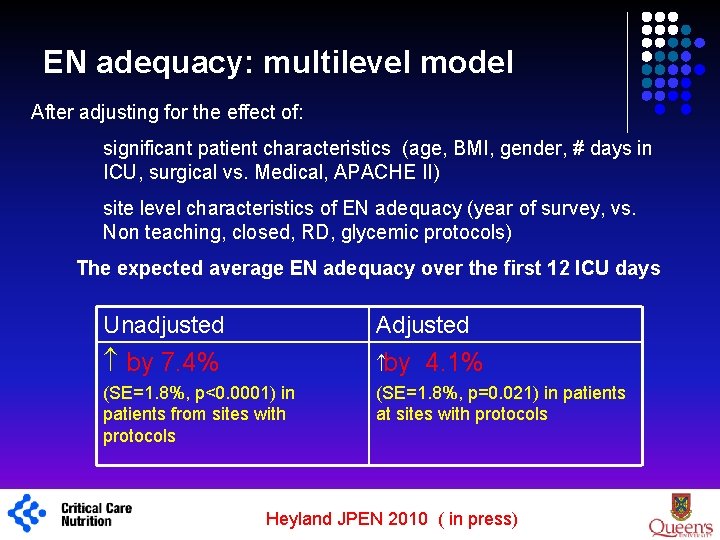
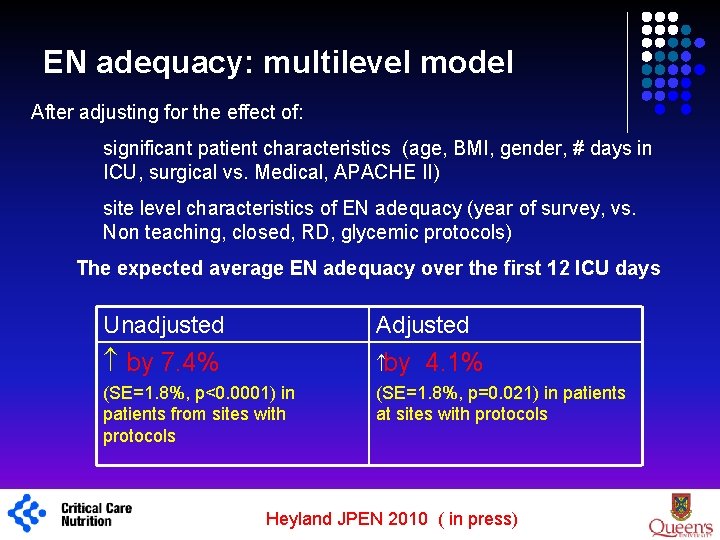
EN adequacy: multilevel model After adjusting for the effect of: significant patient characteristics (age, BMI, gender, # days in ICU, surgical vs. Medical, APACHE II) site level characteristics of EN adequacy (year of survey, vs. Non teaching, closed, RD, glycemic protocols) The expected average EN adequacy over the first 12 ICU days Unadjusted Adjusted by 7. 4% by 4. 1% (SE=1. 8%, p=0. 021) in patients at sites with protocols (SE=1. 8%, p<0. 0001) in patients from sites with protocols 1 Heyland JPEN 2010 ( in press)
Conclusions 1 l There is great variation in the use of feeding protocols in ICUs across the World. l The presence of an enteral feeding protocol is associated with significant improvements in the use of EN, timing of initiation of EN, the use of motility agents and nutrition adequacy delivered. l We suggest that the use of feeding protocols become standard of care in ICUs. l Despite the use of protocols, overall nutrition adequacy is still below target, further refinement and optimization of the characteristics of feeding protocols is warranted. l The positive effect of feeding protocols on clinical outcomes is yet to be established. Heyland JPEN 2010 ( in press)
Strengths and Weaknesses l observational nature of the study design l did not standardize the specific nutrition interventions included in the feeding protocols l did not optimize the utilization of protocols at each site. We are unable to comment on the quality of these existing protocols or the level of compliance at the bed-side. Strengths l large number of participating sites from around the world l Use of a structured, validated data capture system, which enhances the generalizability and validity of the observations. 1 Heyland JPEN 2010 ( in press)
Efficacy of Enhanced Protein-Energy Provision via the Enteral Route in Critically Ill Patients: The PEP u. P Protocol A Single center feasibility trial Daren K. Heyland Professor of Medicine Queen’s University, Kingston General Hospital Kingston, ON Canada
Acknowledgements 1 l The authors are grateful to the critical care practitioners from all participating ICU sites for their dedication and commitment to collecting data for this study. l Colleagues at the Clinical Evaluation Research Unit l Naomi Cahill currently holds a Canadian Institutes for Health Research (CIHR) Fellowship in Knowledge Translation. l All authors declare no conflicts of interest relevant to the subject of this manuscript.
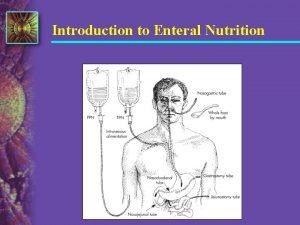
 Specialized nutrition support
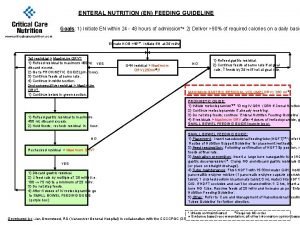
Specialized nutrition support Enteral feeding guideline
Enteral feeding guideline Levin ng tube
Levin ng tube đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Tư thế worm breton
Tư thế worm breton ưu thế lai là gì
ưu thế lai là gì Thẻ vin
Thẻ vin Tư thế ngồi viết
Tư thế ngồi viết Cái miệng nó xinh thế chỉ nói điều hay thôi
Cái miệng nó xinh thế chỉ nói điều hay thôi Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Bổ thể
Bổ thể Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Tư thế ngồi viết
Tư thế ngồi viết Thế nào là giọng cùng tên
Thế nào là giọng cùng tên Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Hát lên người ơi alleluia
Hát lên người ơi alleluia Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập Diễn thế sinh thái là
Diễn thế sinh thái là Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Công thức tính thế năng
Công thức tính thế năng