Parenteral Nutrition Chapter 14 General Comments on Parenteral




- Slides: 29
Parenteral Nutrition Chapter 14
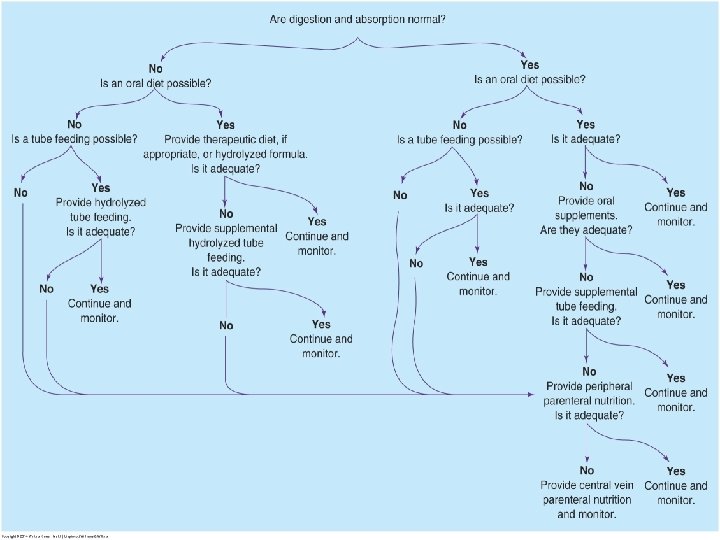
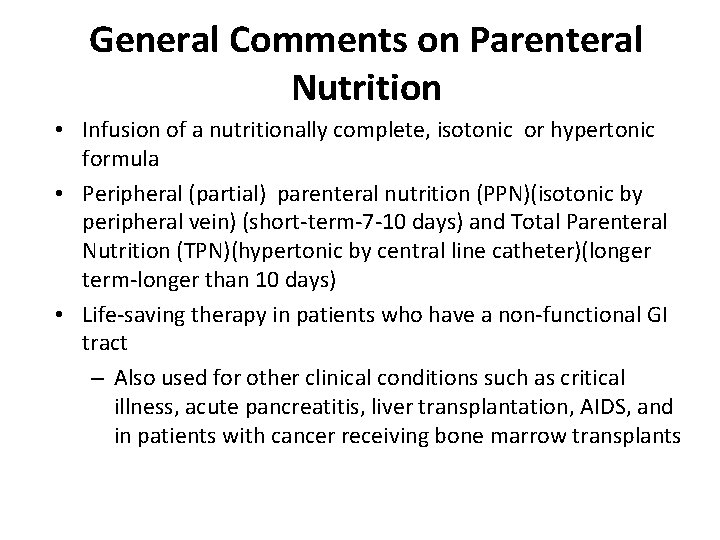
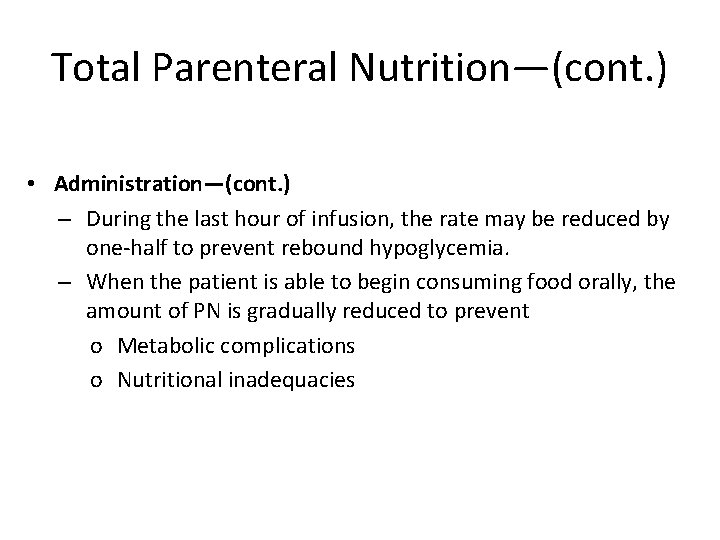
General Comments on Parenteral Nutrition • Infusion of a nutritionally complete, isotonic or hypertonic formula • Peripheral (partial) parenteral nutrition (PPN)(isotonic by peripheral vein) (short-term-7 -10 days) and Total Parenteral Nutrition (TPN)(hypertonic by central line catheter)(longer term-longer than 10 days) • Life-saving therapy in patients who have a non-functional GI tract – Also used for other clinical conditions such as critical illness, acute pancreatitis, liver transplantation, AIDS, and in patients with cancer receiving bone marrow transplants
General Comments on Parenteral Nutrition— (cont. ) Parenteral Feeding (going around i. e. circumventing the gastrointestinal tract) Nutrients go directly into blood stream bypassing gastrointestinal tractthis is done by intravenous needle to peripheral vein (PPN) or catheter to central vein (TPN) Used when a patient cannot, due to physical or psychological impairment, consume sufficient nutrients enterally Used when patients gi system will not adequately process food for body Actual infusion depends on site of infusion and patient’s fluid and nutrient requirements
General Comments on Parenteral Nutrition—(cont. ) • Overfeeding can cause a life-threatening complication known as the refeeding syndrome. • PN is expensive, requires constant monitoring, and has potential infectious, metabolic, and mechanical complications. • Used only when an enteral intake is inadequate or contraindicated and when prolonged nutritional support is needed • Should be initiated when oral intake has been or is expected to be inadequate over a 7 - to 14 -day period
General Comments on Parenteral Nutrition Usual fluid volume is 1. 5 -2. 5 L over a 24 hour period for most people
General Comments on Parenteral Nutrition— (cont. ) Composition of ingredients for intravenous delivery Dextrose Amino acids Lipid emulsion Sterile water Electrolytes Vitamins
General Comments on Parenteral Nutrition— (cont. ) Carbohydrate Dextrose Concentration is 10. 0 % (max for peripheral introduction) to 70 % (max for total parenteral nutrition) Restricted in ventilator patients because oxidation of glucose produces more carbon dioxide than does oxidation of fat
General Comments on Parenteral Nutrition— (cont. ) Protein Mixture of essential and non-essential amino acids Concentration 3. 5 -15 % Quantity of amino acids depends on patients estimated requirements and hepatic and renal function-why?
General Comments on Parenteral Nutrition— (cont. ) Lipid emulsions Safflower and soybean oil with egg lecithin used as an emulsifier (why the emulsifier and how does it work? ) Significant source of calories
General Comments on Parenteral Nutrition—(cont. ) Lipid emulsions Available in 10, 20, 30 % concentrations Usual dose is 0. 5 to 1 g/kg/day to supply 20 -30 % of total kcal requirement IV fat contradicted for severe hepatic pathology, hyperlipidemia or severe egg allergies Used cautiously with atherosclerosis, blood coagulation disorders
General Comments on Parenteral Nutrition— (cont. ) Electrolytes Dictated by patients blood chemistry values and physical assessment findings
General Comments on Parenteral Nutrition— (cont. ) Standard multivitamin and trace mineral preparations added to parenteral solutions to meet micronutrient needs
General Comments on Parenteral Nutrition—(cont. ) • Medications – Patients receiving PN may have insulin ordered if glucose levels are above 150 to 200 mg/d. L. – Heparin may be added to reduce fibrin buildup on the catheter tip. – Medications should not be added to PN solutions because of the potential incompatibilities of the medication and nutrients in the solution.
PPN -must be isotonic and therefore low in dextrose and amino acids to prevent phlebitis and increased risk of thrombus formation -need to maintain isotonic solutions of dextrose and amino acids while avoiding fluid overload limits the caloric and nutritional value of PPN
PPN delivers complete but limited nutrition the final concentration cannot exceed 10 % dextrose-also uses lower concentrations of amino acids vitamins and minerals are added lipid emulsion may be added to supplement calories depending on the patients tolerance
PPN -provides temporary nutritional support -short term- 7 -10 days and do not require more than 2000 to 2500 kcal per day
PPN -may be used for a post surgical ileus or anastomotic leak or for patients who require nutritional support but are unable to use TPN because of limited accessibility to a central vein -sometimes used to supplement an oral diet or tube feeding or transition from TPN to enteral intake
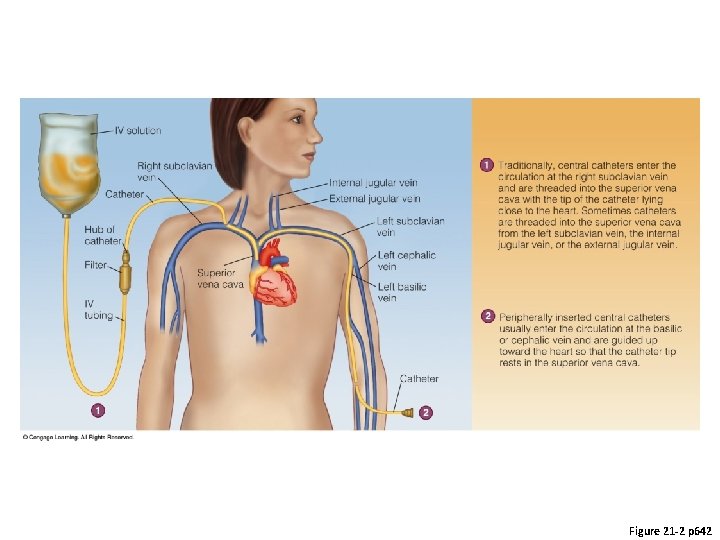
Total Parenteral Nutrition • Catheter placement – Patient’s anticipated length of need influences placement of the catheter. – For short-term central PN in the hospital, a temporary central venous catheter is placed percutaneously into the subclavian vein. – If PN is expected to be more than a few weeks, these are the catheters of choice: o A Hickman catheter or Port-a-Cath o Peripherally inserted central catheter (PICC)
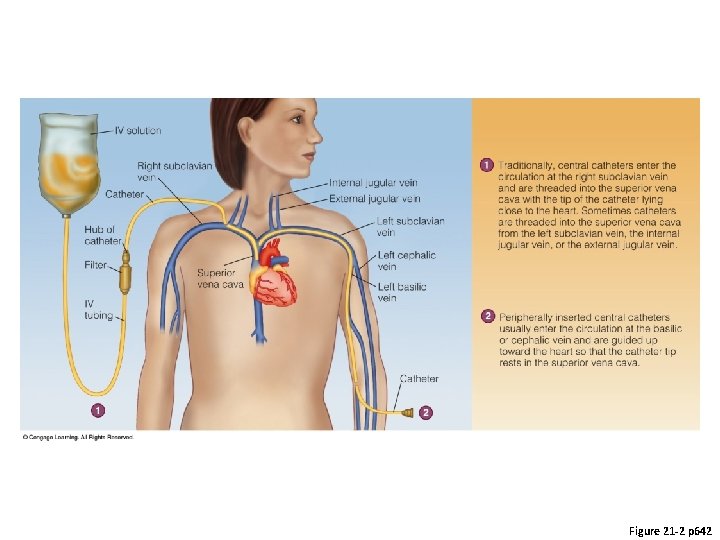
Figure 21 -2 p 642
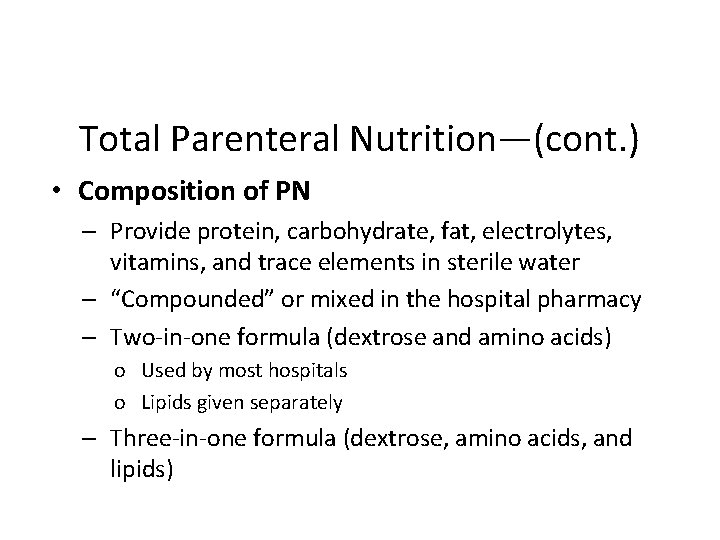
Total Parenteral Nutrition—(cont. ) • Composition of PN – Provide protein, carbohydrate, fat, electrolytes, vitamins, and trace elements in sterile water – “Compounded” or mixed in the hospital pharmacy – Two-in-one formula (dextrose and amino acids) o Used by most hospitals o Lipids given separately – Three-in-one formula (dextrose, amino acids, and lipids)

p 643
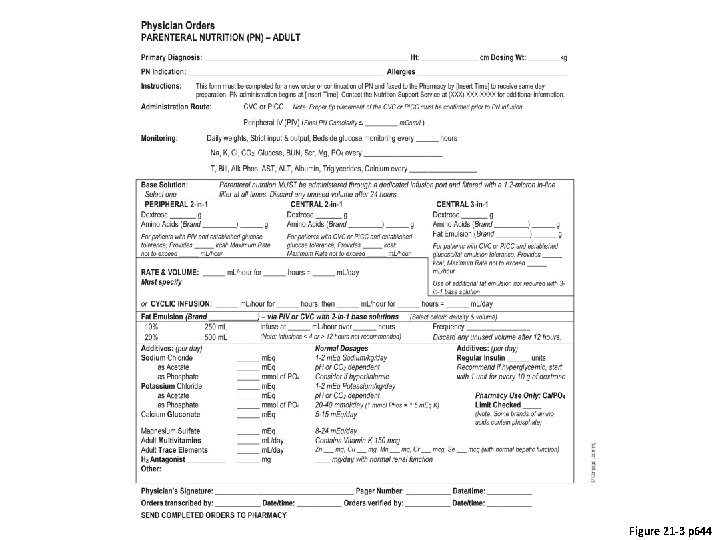
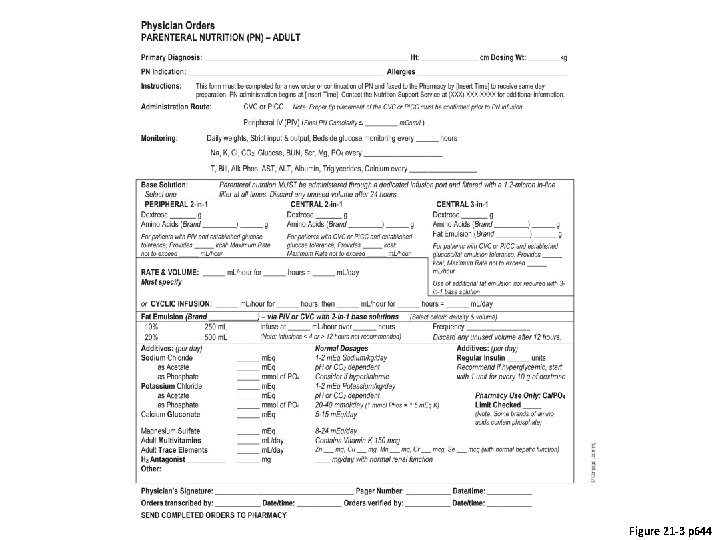
Figure 21 -3 p 644
Total Parenteral Nutrition—(cont. ) • Administration – Administered according to facility protocol – Generally initiated slowly (i. e. , 1 L in the first 24 hours) – Continuous drip by pump infusion is needed to maintain a slow, constant flow rate. – Rapid changes in the infusion rate can cause o Severe hyperglycemia or hypoglycemia o Potential for coma, convulsions, or death
Total Parenteral Nutrition—(cont. ) • Administration—(cont. ) – After the patient is stable, PN may be infused cyclically. – Cyclic PN allows serum glucose and insulin levels to drop during the periods when PN is not infused. – To give the pancreas time to adjust to the decreasing glucose load, the infusion rate is tapered near the end of each cycle.
Total Parenteral Nutrition—(cont. ) • Administration—(cont. ) – During the last hour of infusion, the rate may be reduced by one-half to prevent rebound hypoglycemia. – When the patient is able to begin consuming food orally, the amount of PN is gradually reduced to prevent o Metabolic complications o Nutritional inadequacies


p 653
