ENTERAL NUTRITION MEETING NUTRIENT NEEDS Selection of Feeding



- Slides: 42

ENTERAL NUTRITION MEETING NUTRIENT NEEDS
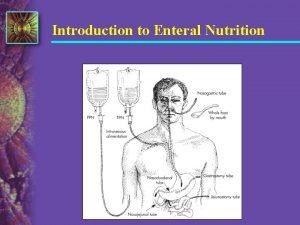
Selection of Feeding Route ¨ Page 536, Krause – Figure 23 -1 ¨ Algorithm or Decision Tree – Adequate oral intake – Oral intake + supplements – Enteral nutrition support • • Patient’s medical status Anticipated duration of tube feeding Risk for aspiration Advantages and disadvantages of access route
Enteral Formula Selection ¨ Selection Algorithm: Page 538, Krause – Figure 23 -3 ¨ Feed as close to the farm as possible: e. g. the most intact formula the patient will tolerate ¨ Intact nutrient, general purpose formulas are the least expensive and may be more physiological
Enteral Formulary – What products are available? – More cost effective to have formulary – Include multiple products, one main brand of each category

Where can you get information about enteral products? ¨ Nutrition Care Manual formulary page ¨ http: //nutritioncaremanual. org/universi 13 ¨ Novartis Nutrition USA http: //www. novartisnutrition. com/us/home ¨ Abbot Nutrition Product Handbook http: //abbottnutrition. com/product. Handbook/ default. asp Nestle Nutrition http: //www. nestleclinicalnutrition. com/
Nutrition Care Manual Formulary You can ¨ View compositional information about adult and pediatric formulas ¨ Calculate nutrient delivery based on volume ¨ Compare two formulas in the same category ¨ BUT: be aware that the most reliable and up to date source of information about a formula is from the mfr.

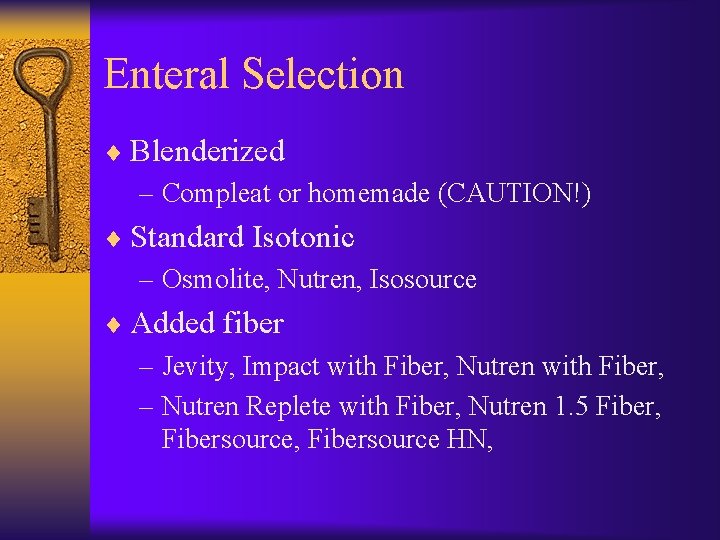
Enteral Selection ¨ Blenderized – Compleat or homemade (CAUTION!) ¨ Standard Isotonic – Osmolite, Nutren, Isosource ¨ Added fiber – Jevity, Impact with Fiber, Nutren with Fiber, – Nutren Replete with Fiber, Nutren 1. 5 Fiber, Fibersource HN,
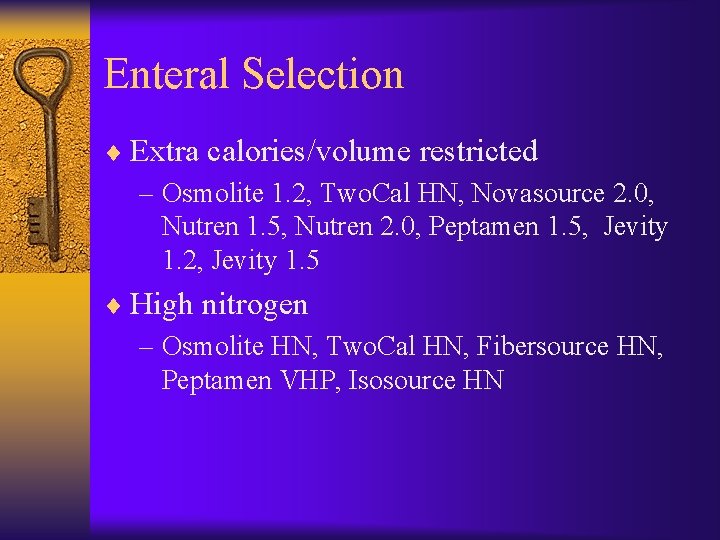
Enteral Selection ¨ Extra calories/volume restricted – Osmolite 1. 2, Two. Cal HN, Novasource 2. 0, Nutren 1. 5, Nutren 2. 0, Peptamen 1. 5, Jevity 1. 2, Jevity 1. 5 ¨ High nitrogen – Osmolite HN, Two. Cal HN, Fibersource HN, Peptamen VHP, Isosource HN
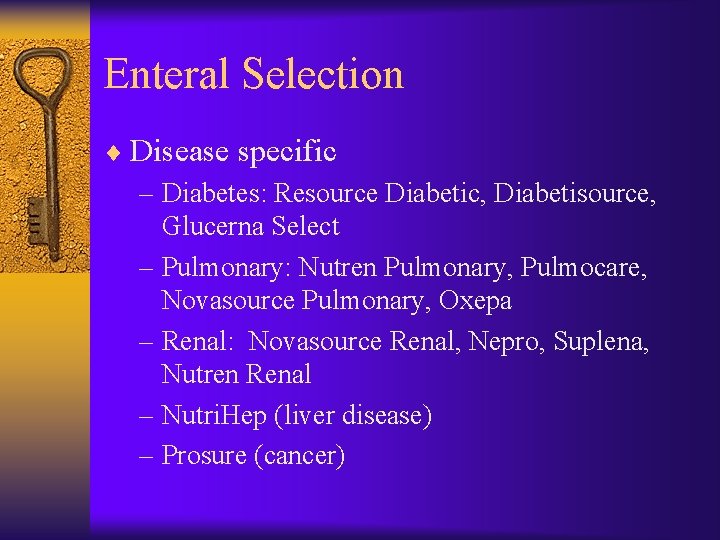
Enteral Selection ¨ Disease specific – Diabetes: Resource Diabetic, Diabetisource, Glucerna Select – Pulmonary: Nutren Pulmonary, Pulmocare, Novasource Pulmonary, Oxepa – Renal: Novasource Renal, Nepro, Suplena, Nutren Renal – Nutri. Hep (liver disease) – Prosure (cancer)
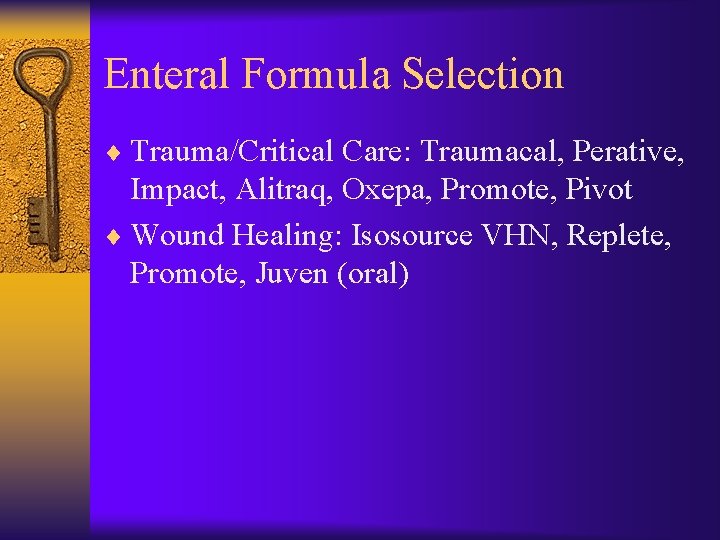
Enteral Formula Selection ¨ Trauma/Critical Care: Traumacal, Perative, Impact, Alitraq, Oxepa, Promote, Pivot ¨ Wound Healing: Isosource VHN, Replete, Promote, Juven (oral)
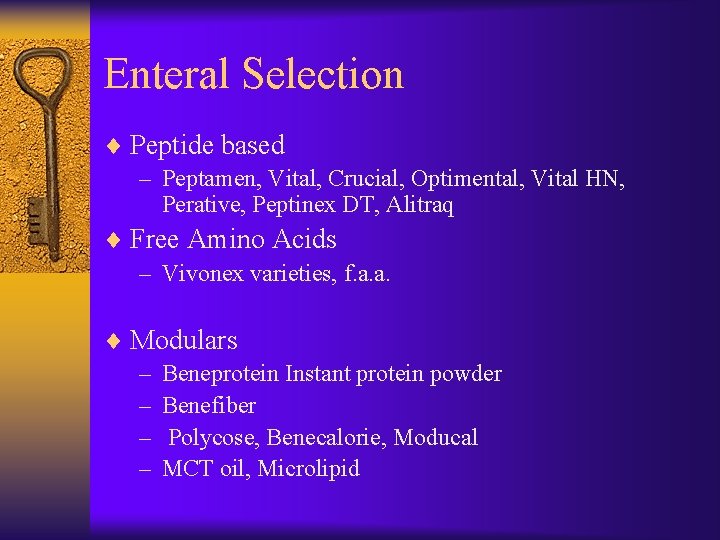
Enteral Selection ¨ Peptide based – Peptamen, Vital, Crucial, Optimental, Vital HN, Perative, Peptinex DT, Alitraq ¨ Free Amino Acids – Vivonex varieties, f. a. a. ¨ Modulars – Beneprotein Instant protein powder – Benefiber – Polycose, Benecalorie, Moducal – MCT oil, Microlipid
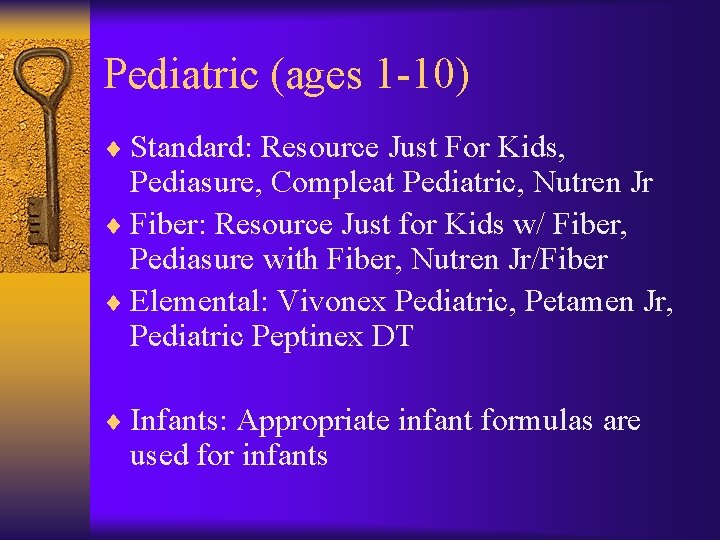
Pediatric (ages 1 -10) ¨ Standard: Resource Just For Kids, Pediasure, Compleat Pediatric, Nutren Jr ¨ Fiber: Resource Just for Kids w/ Fiber, Pediasure with Fiber, Nutren Jr/Fiber ¨ Elemental: Vivonex Pediatric, Petamen Jr, Pediatric Peptinex DT ¨ Infants: Appropriate infant formulas are used for infants
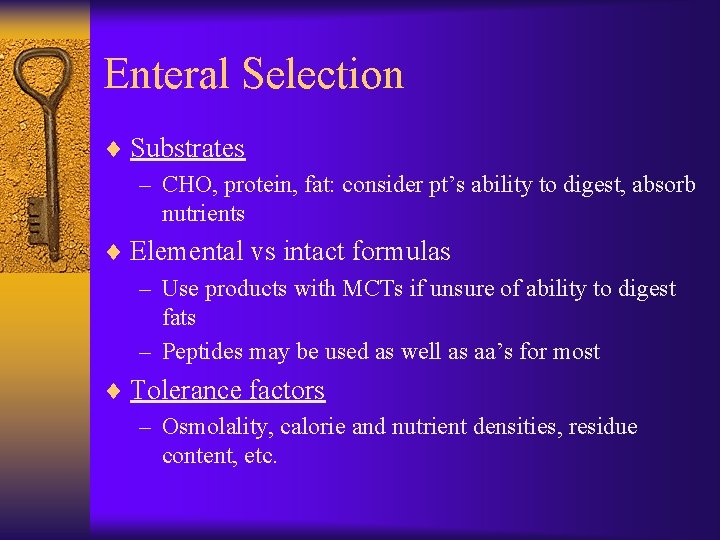
Enteral Selection ¨ Substrates – CHO, protein, fat: consider pt’s ability to digest, absorb nutrients ¨ Elemental vs intact formulas – Use products with MCTs if unsure of ability to digest fats – Peptides may be used as well as aa’s for most ¨ Tolerance factors – Osmolality, calorie and nutrient densities, residue content, etc.
Physical Properties of Enteral Formulas ¨ Osmolality – Vomiting – GI emptying – Diarrhea – Retention – Nausea – Dehydration ¨ Residue ¨ Viscosity – Size of tube is important
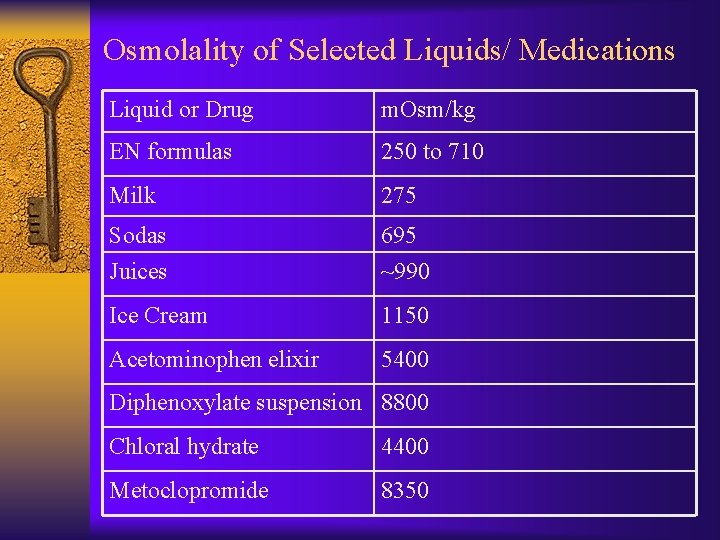
Osmolarity vs Osmolality ¨ Osmolarity – Measure of osmotically active particles per liter of solution ¨ Osmolality * – Measure of osmotically active particles per kg of solvent in which particles are dispersed – milliosmoles of solute per kg of solvent (m. Osm/kg)
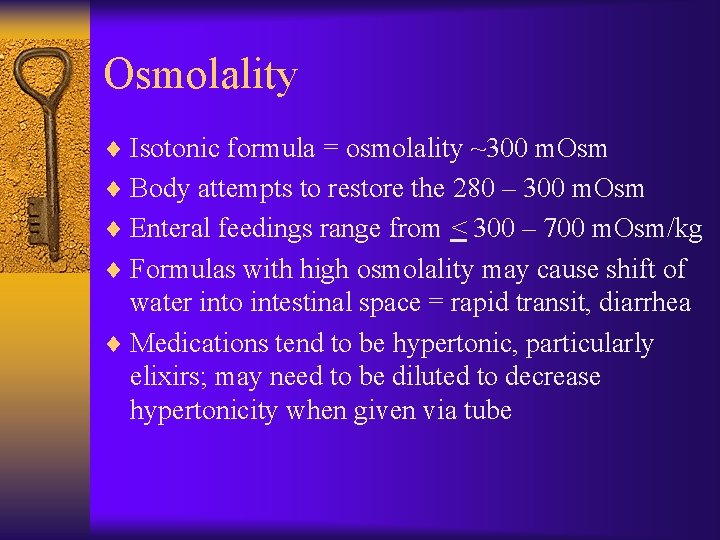
Osmolality ¨ Isotonic formula = osmolality ~300 m. Osm ¨ Body attempts to restore the 280 – 300 m. Osm ¨ Enteral feedings range from < 300 – 700 m. Osm/kg ¨ Formulas with high osmolality may cause shift of water into intestinal space = rapid transit, diarrhea ¨ Medications tend to be hypertonic, particularly elixirs; may need to be diluted to decrease hypertonicity when given via tube
Lower Osmolality ¨ Large (intact) proteins ¨ Large starch molecules
Higher Osmolality ¨ Hydrolyzed protein or amino acids ¨ Disaccharides ¨ Smaller particles
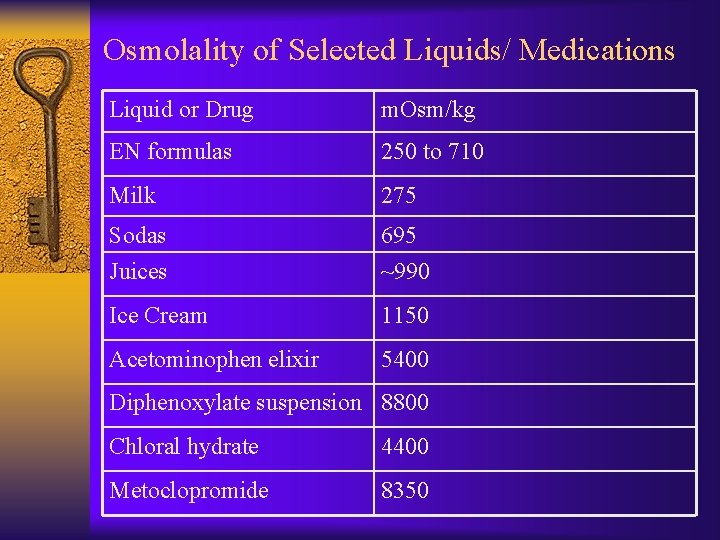
Osmolality of Selected Liquids/ Medications Liquid or Drug m. Osm/kg EN formulas 250 to 710 Milk 275 Sodas Juices 695 ~990 Ice Cream 1150 Acetominophen elixir 5400 Diphenoxylate suspension 8800 Chloral hydrate 4400 Metoclopromide 8350
Meeting Nutrient Needs ¨ Calculate kcal, protein, fluid, and nutrient needs according to age, sex, medical status ¨ Select appropriate formula based on nutritional needs, feeding route, and GI function
Estimation of Energy Needs • Indirect calorimetry: the gold standard, particularly with critically ill, obese, pts who do not respond well to treatment • Most clinicians use standard energy estimation equations to estimate calorie needs
In-Class Use of Predictive Equations for EEE and REE ¨ Use actual body weight in calculations in class ¨ Use Mifflin-St. Jeor plus activity factors, if applicable, in ambulatory patients ¨ Use Harris-Benedict x injury factor with actual weight in hospitalized, stressed patients. Do not use activity factor unless patients are in rehab or unusually active. ¨ ADA Nutrition Care Manual, www. nutritioncaremanual. org, accessed 1 -06
In-Class Use of Predictive Equations for EEE and REE ¨ Use 1992 Ireton-Jones in patients with burns and trauma where Penn State data not available ¨ Use Penn State equation in the ICU where minute ventilation and temperature available
In-Class Use of Predictive Equations for EEE/REE ¨ In calculating protein needs, use actual weight, but use the lower end of ranges for persons with Class I obesity or above. ¨ It’s always best to estimate a range of needs, which reflects the imprecision of the tools available for our use.
Quick Method ¨ Use 25 -35 kcal/kg in hospitalized non-obese patients ¨ FAO-WHO. Energy and protein requirements. Geneva: WHO, 1985. Technical report series 724. ¨ Use 20 -21 kcal/kg actual body weight in obese patients (BMI>30) ¨ Amato P, Keating KP, Querica RA, et al. Formulaic methods of estimating caloric requirements in mechanically ventilated obese patients: a reappraisal. Nutr Clin Pract 1995; 10: 229 -230.
Meeting Nutrient Needs ¨ Enteral Formulas – caloric density: – 1. 0 -1. 2 kcal/ml – 1. 5 kcal/ml – 2. 0 kcal/ml – Energy and nutrient concentration affect volume needed • 1 kcal/m. L = standard formula • 1. 5 -2 kcal/m. L = volume limitations
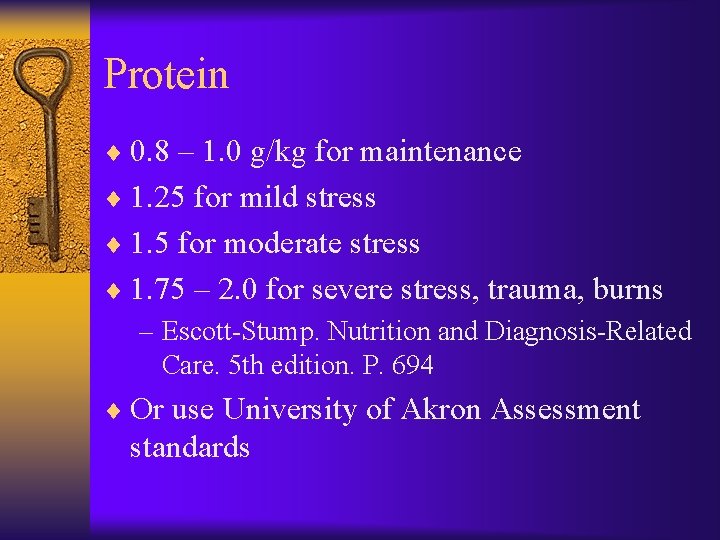
Protein ¨ 0. 8 – 1. 0 g/kg for maintenance ¨ 1. 25 for mild stress ¨ 1. 5 for moderate stress ¨ 1. 75 – 2. 0 for severe stress, trauma, burns – Escott-Stump. Nutrition and Diagnosis-Related Care. 5 th edition. P. 694 ¨ Or use University of Akron Assessment standards
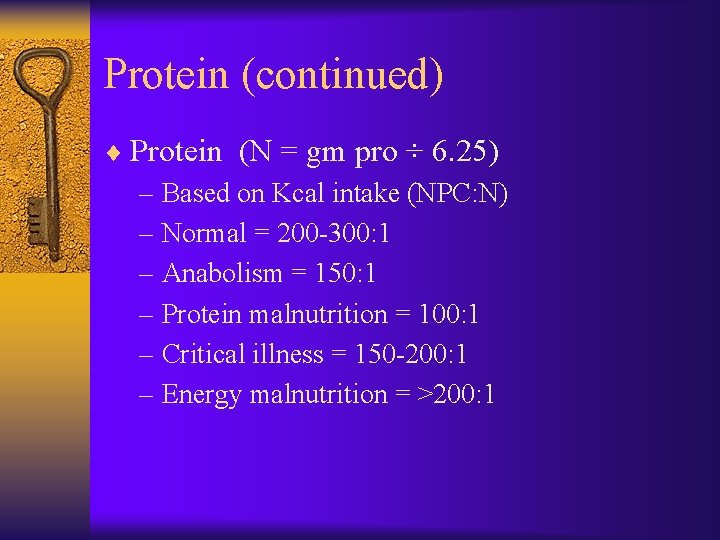
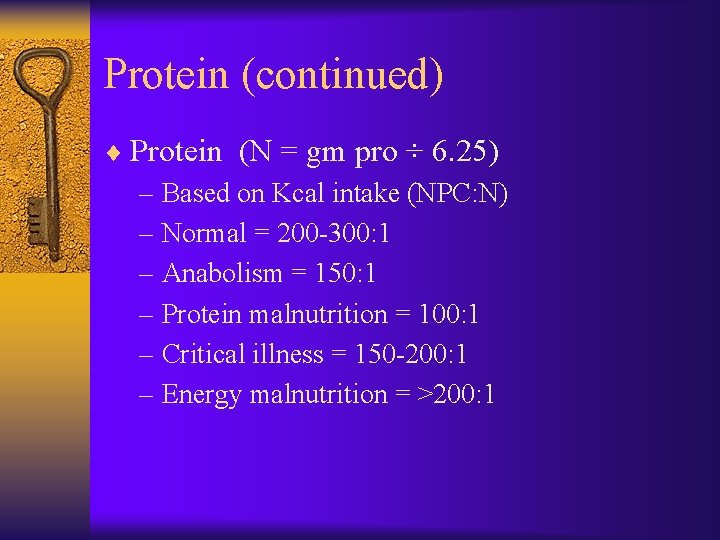
Protein (continued) ¨ Protein (N = gm pro ÷ 6. 25) – Based on Kcal intake (NPC: N) – Normal = 200 -300: 1 – Anabolism = 150: 1 – Protein malnutrition = 100: 1 – Critical illness = 150 -200: 1 – Energy malnutrition = >200: 1
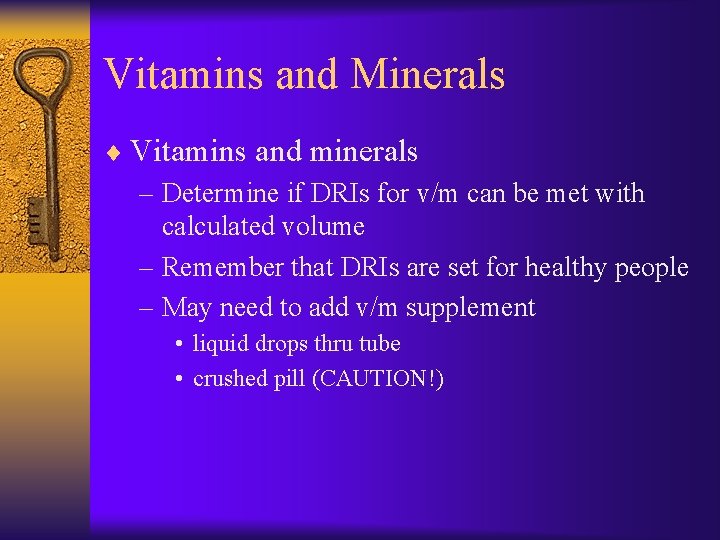
Vitamins and Minerals ¨ Vitamins and minerals – Determine if DRIs for v/m can be met with calculated volume – Remember that DRIs are set for healthy people – May need to add v/m supplement • liquid drops thru tube • crushed pill (CAUTION!)
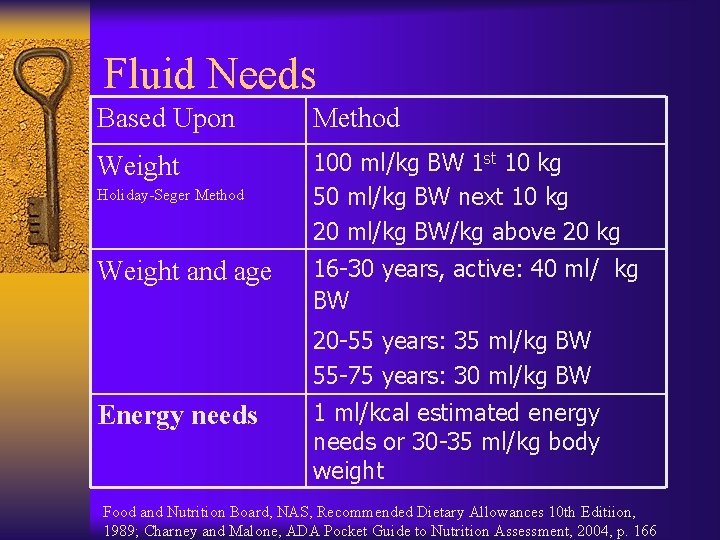
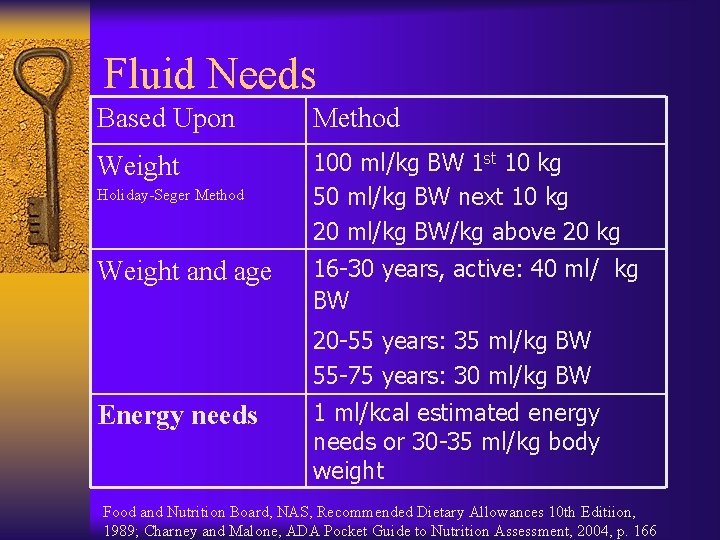
Fluid Needs Based Upon Method Weight 100 ml/kg BW 1 st 10 kg 50 ml/kg BW next 10 kg 20 ml/kg BW/kg above 20 kg Holiday-Seger Method Weight and age 16 -30 years, active: 40 ml/ kg BW 20 -55 years: 35 ml/kg BW 55 -75 years: 30 ml/kg BW Energy needs 1 ml/kcal estimated energy needs or 30 -35 ml/kg body weight Food and Nutrition Board, NAS, Recommended Dietary Allowances 10 th Editiion, 1989; Charney and Malone, ADA Pocket Guide to Nutrition Assessment, 2004, p. 166
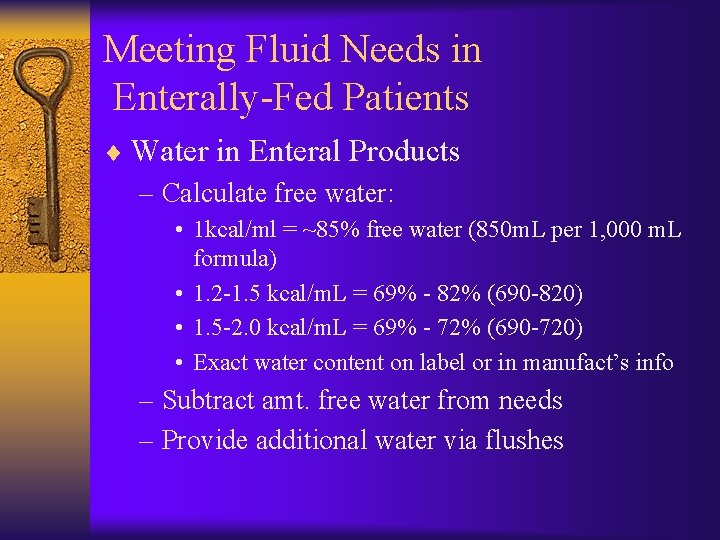
Meeting Fluid Needs in Enterally-Fed Patients ¨ Water in Enteral Products – Calculate free water: • 1 kcal/ml = ~85% free water (850 m. L per 1, 000 m. L formula) • 1. 2 -1. 5 kcal/m. L = 69% - 82% (690 -820) • 1. 5 -2. 0 kcal/m. L = 69% - 72% (690 -720) • Exact water content on label or in manufact’s info – Subtract amt. free water from needs – Provide additional water via flushes
Meeting Fluid Needs in Enterally Fed Patients ¨ Water Flushes – Irrigate tube q 4 hrs with 20 -60 m. L water with continuous feeds – Irrigate tubes before and after each intermittent or bolus feed with 20 -60 m. L water – In case of clogging, tube should be flushed using 60 m. L syringe with 30 -60 m. L warm water – Use smaller vol for fluid-restricted pts
Meeting Fluid Needs in Enterally -Fed Patients ¨ Water – Increase fluids as tolerated to compensate for losses: • • • fever or environmental temp increased urine output diarrhea/vomiting draining wounds ostomy output, fistulas increased fiber intake, concentrated or highprotein formulas
Enteral Nutrition Monitoring ¨ Wt (at least 3 times/week) ¨ Signs/symptoms of edema (daily) ¨ Signs/symptoms of dehydration (daily) ¨ Fluid I/O (daily) ¨ Adequacy of intake (at least 2 x weekly) ¨ Nitrogen balance: becoming less common (weekly, if appropriate)
Enteral Nutrition Monitoring ¨ Serum electrolytes, BUN, creatinine (2 – 3 x weekly) ¨ Serum glucose, calcium, magnesium, phosphorus (weekly or as ordered) ¨ Stool output and consistency (daily)
Enteral Feeding Tolerance ¨ Signs and symptoms: —Consciousness —Respiratory distress —Nausea, vomiting, diarrhea —Constipation, cramps —Aspiration —Abdominal distention
Monitoring Gastric Residuals ¨ Performed by inserting a syringe into the feeding tube and withdrawing gastric contents and measuring volume ¨ Often a part of nursing protocols/physician orders for tubefed patients
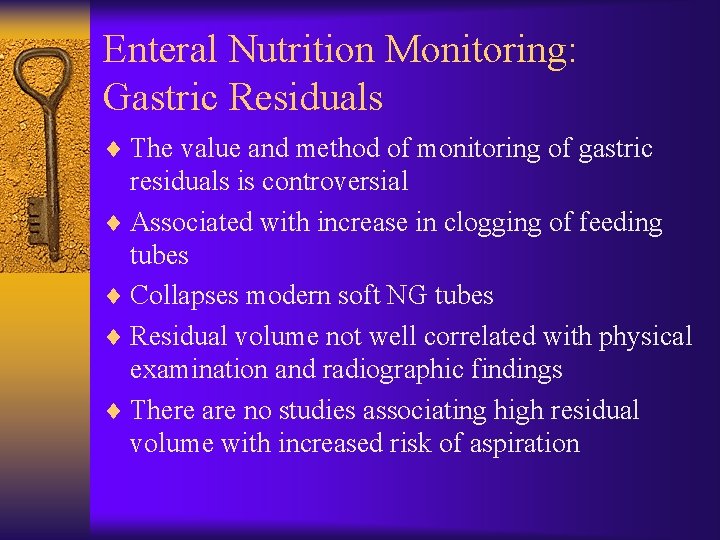
Enteral Nutrition Monitoring: Gastric Residuals ¨ The value and method of monitoring of gastric residuals is controversial ¨ Associated with increase in clogging of feeding tubes ¨ Collapses modern soft NG tubes ¨ Residual volume not well correlated with physical examination and radiographic findings ¨ There are no studies associating high residual volume with increased risk of aspiration
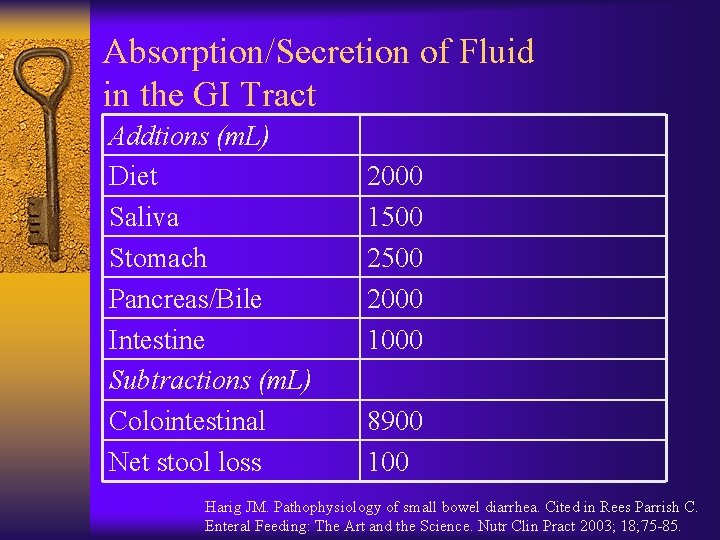
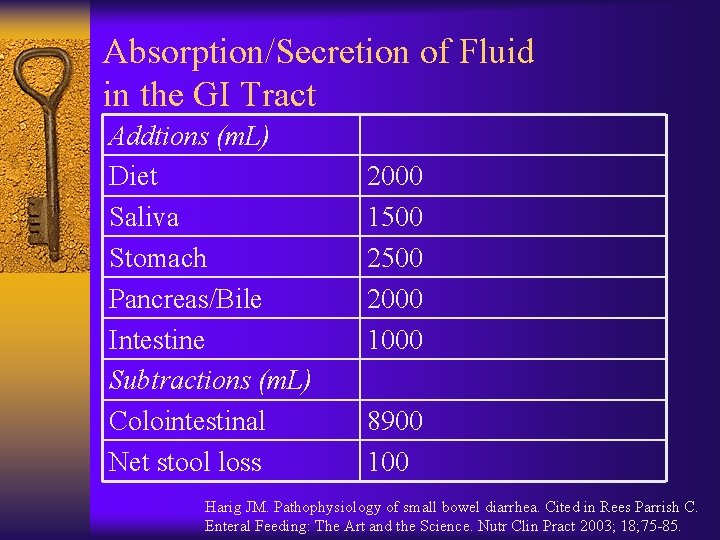
Absorption/Secretion of Fluid in the GI Tract Addtions (m. L) Diet Saliva Stomach Pancreas/Bile Intestine Subtractions (m. L) Colointestinal Net stool loss 2000 1500 2000 1000 8900 100 Harig JM. Pathophysiology of small bowel diarrhea. Cited in Rees Parrish C. Enteral Feeding: The Art and the Science. Nutr Clin Pract 2003; 18; 75 -85.
Enteral Nutrition Monitoring: Gastric Residuals ¨ Monitoring of gastric residuals in tubefed pts assumes that high residuals occur only in tubefed pts ¨ In one study, 40% of normal volunteers had RVs that would be considered significant based on current standards ¨ For consistency, all hospitalized pts, with or without EN should have their RVs routinely assessed to evaluate GI function Rees Parrish C. Enteral Feeding: The Art and the Science. Nutr Clin Pract 2003; 18; 75 -85.
Enteral Nutrition Monitoring: Gastric Residuals ¨ Clinically assess the patient for abdominal distension, fullness, bloating, discomfort ¨ Place the pt on his/her right side for 15 -20 minutes before checking a RV to avoid cascade effect ¨ Try a prokinetic agent or antiemetic ¨ Seek transpyloric access of feeding tube ¨ Raise threshold for RV to 200 -300 m. L ¨ Consider stopping RV checks in stable pts Rees Parrish C. Enteral Feeding: The Art and the Science. Nutr Clin Pract 2003; 18; 75 -85.
 Nutrient broth vs nutrient agar
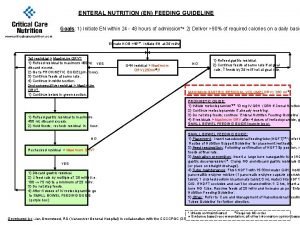
Nutrient broth vs nutrient agar Enteral feeding guideline
Enteral feeding guideline Ati nasogastric tube
Ati nasogastric tube Continuous feeding vs bolus feeding
Continuous feeding vs bolus feeding Foods used in nutrition activities should be nutrient-dense
Foods used in nutrition activities should be nutrient-dense Glucerna cpt code
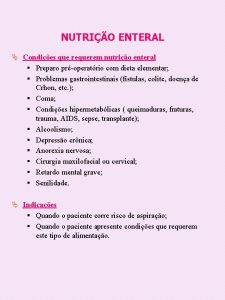
Glucerna cpt code Enteral nutrition
Enteral nutrition Formula semi elemental
Formula semi elemental Nutrition for individual needs
Nutrition for individual needs Target needs and learning needs
Target needs and learning needs Satisfaction
Satisfaction Henry murray theory
Henry murray theory Strategic gender needs and practical gender needs
Strategic gender needs and practical gender needs Primary needs and secondary needs
Primary needs and secondary needs Meeting the needs of guests with kindness and goodwill.
Meeting the needs of guests with kindness and goodwill. Individual needs examples
Individual needs examples Unit 5: meeting individual care and support needs
Unit 5: meeting individual care and support needs Health and social care unit 5 coursework example p3
Health and social care unit 5 coursework example p3 Methods of meeting customer needs
Methods of meeting customer needs Developmental needs meeting strategy
Developmental needs meeting strategy Chapter 10:3 psychosocial changes of aging
Chapter 10:3 psychosocial changes of aging Unit 5 meeting individual care and support needs
Unit 5 meeting individual care and support needs What is meeting and types of meeting
What is meeting and types of meeting Today meeting or today's meeting
Today meeting or today's meeting Meeting objective
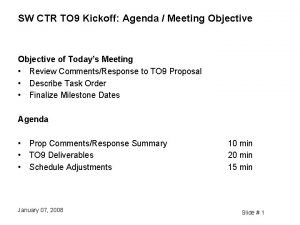
Meeting objective What is meeting and types of meeting
What is meeting and types of meeting Multiway selection in c
Multiway selection in c Natural selection vs artificial selection
Natural selection vs artificial selection K selection r selection
K selection r selection Procedure of pure line selection
Procedure of pure line selection Balancing selection vs stabilizing selection
Balancing selection vs stabilizing selection Natural selection vs artificial selection
Natural selection vs artificial selection Difference between continuous and discontinuous variation
Difference between continuous and discontinuous variation Similarities
Similarities Two way selection and multiway selection
Two way selection and multiway selection K selection r selection
K selection r selection Disruptive selevtion
Disruptive selevtion Nutrient cycle in the serengeti
Nutrient cycle in the serengeti Energy in trophic levels
Energy in trophic levels Nutrient cycles in marine ecosystems
Nutrient cycles in marine ecosystems Tamoxifen nutrient depletion
Tamoxifen nutrient depletion Functions of nutrients
Functions of nutrients Six nutrient groups
Six nutrient groups