Nutrition Support therapy Enteral and Parenteral Nutrition Nutrition
- Slides: 12
Nutrition Support therapy Enteral and Parenteral Nutrition
Nutrition Support therapydefinition Nutrition Support Therapy is part of Nutrition Therapy which is the provision of enteral, and parenteral nutrition to maintain or restore optimal nutrition status and health.
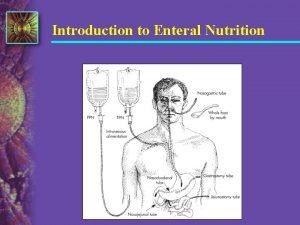
What is enteral nutrition? Enteral nutrition or Enteral Tube feeding is the provision of nutrients by a tube through the GI tract in patients who cannot attain sufficient oral intake from food and/or oral nutritional supplements for periods of more than five days (e. g. dysphagic patients). It aims to maintain a patient’s nutritional status and to improve their nutritional intake. ETF should be administered in patients when they are not safe for oral intake or when oral intake is not adequate to meet their nutritional requirements but has an accessible and functional GI tract
Indications for the provision of enteral feeding a stroke, which may impair ability to swallow cancer, which may cause fatigue, nausea, and vomiting that make it difficult to eat critical illness or injury, which reduces energy or ability to eat failure to thrive or inability to eat in young children or infants serious illness, which places the body in a state of stress, making it difficult to take in enough nutrients neurological or movement disorders that increase caloric requirements while making it more difficult to eat GI dysfunction or disease such as inflammatory bowel disease, although this may require intravenous (IV) nutrition instead (if bowel rest required)
Advantages of Enteral feedings have several advantages, including the following: It is more economical to feed enterally than intra- venously, considering equipment, time, and foods used. It is safer to feed enterally than intravenously. The risk of fluid and electrolyte imbalances and infection is less than for intravenous feedings.
Disadvantages Nutrition delivered by enteral tubes can cause the following complications: food entering the lungs, constipation, diarrhea, improper absorption of nutrients, nausea, vomiting, dehydration, electrolyte abnormalities, high blood sugar, vitamin and mineral deficiencies, and decreased liver proteins. Feeding tubes inserted through the nose, such as nasogastric or nasoenteric tubes, can cause irritation of the nose or throat, acute sinus infections, and ulceration of the larynx or esophagus Feeding tubes inserted through the skin of the abdominal wall, such as gastrostomy or jejunostomy tubes, can become clogged (occluded) or displaced, and wound infections can occur. Problems of preparation and safety. Bacterial contamination can be a factor if preparation is not carefully controlled. Home-prepared tube feedings are not recommended. Prepared formulas are preferred over the use of home-blenderized diets, which can clog tubes, are not sterile, and in which nutrient composition is not well defined. For further details, click https: //clinicalnutritionespen. com/article/S 1751 -4991(09)00033 -X/fulltext
Enteral formulas Enteral feedings depend on enteral formulas. Most enteral feeds are ready-to-use fluids, in microbialfree containers that provide macronutrients, micronutrients, fluids and, in some cases, soluble or insoluble fibre. They are usually nutritionally complete within a specific volume, providing the necessary nutrients to support the dietary needs of the patient. There are three categories of commercial enteral formulas: 1. Standard, intact, or routine enteral formulas= They are used for routine feedings for patients who need them as prescribed by physicians. Now, there are more than 35 products in the market. Each product is made of regular foods and individual nutrients. 2. Elemental or defined enteral formulas= Defined enteral formulas contain specific nutrients or modified nutrients, including simple and complex carbohydrates, amino acids, peptides, fatty acids, triglycerides, and so on. There about 15 or so in the market. 3. Disease-specific enteral formulas= Disease-specific enteral formulas are available for five or more clinical disorders such as those of the kidney, liver, pancreas (diabetes), lung, and the immune system.
What are the main characteristics of renal, pulmonary, hepatic and diabetic feeds? Renal feeds ² They usually contain limited amounts of sodium, potassium and phosphorus. ² Their protein content varies: there are low-protein feeds for the early stages of chronic kidney disease (CKD) and higher -protein feeds for end-stage CKD patients (i. e. patients undergoing hemodialysis or peritoneal dialysis). ² The feeds for end-stage CKD patients are usually energydense, facilitating the fluid restriction that is needed for them.
Pulmonary feeds ² They usually contain a higher percentage of their total energy in the form of fat to reduce the carbon dioxide that is produced by the feed metabolism. Hepatic feeds ² These are commonly low in aromatic amino acids (AAA) and methionine and high in branched-chain amino acids (BCAA). ² They usually have a high calorie/nitrogen ratio, are hypercaloric, low in sodium and contain dietary fibre to promote gut motility. ² They are usually low in copper, iron and manganese and are supplemented with fatsoluble vitamins, folic acid and B-complex vitamins. Diabetic feeds ² They usually have a lower carbohydrate content and a type of carbohydrate that is different from the standard formulas. ² They usually contain oligosaccharides, fructose and cornstarch, and in combination with their higher fibre content they aim at better glycaemic control as a result of delayed gastric emptying and a reduced intestinal transit.
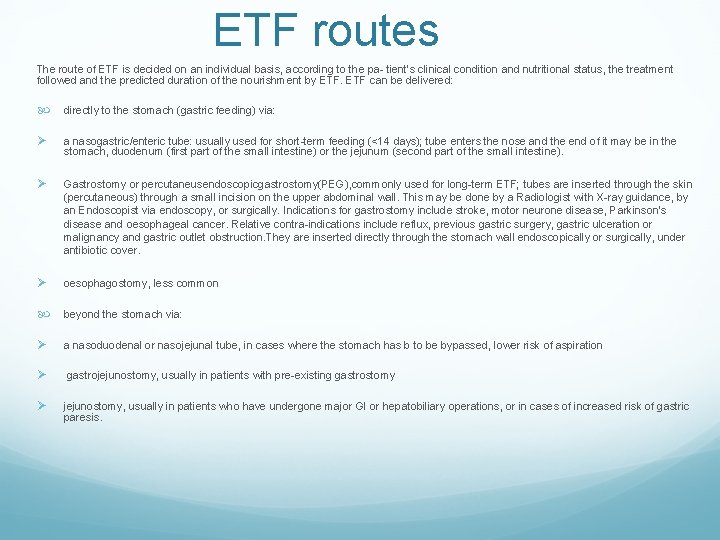
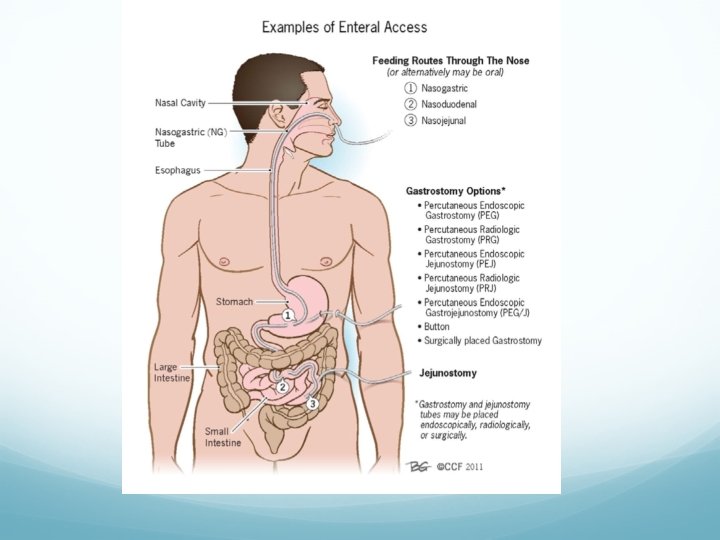
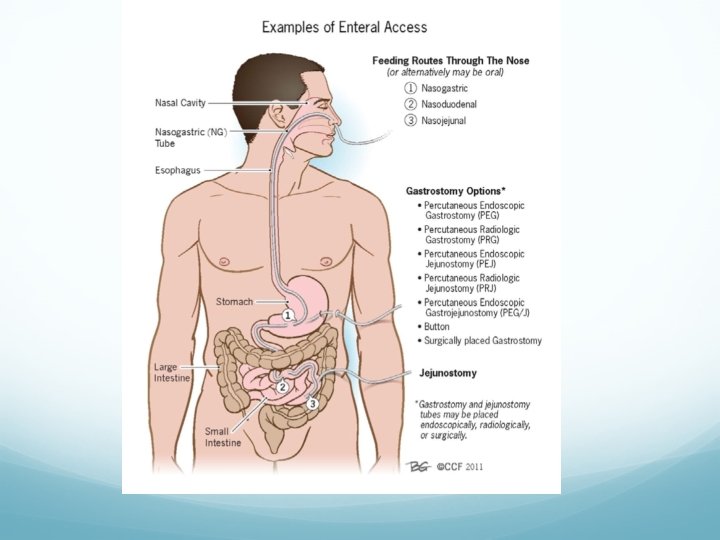
ETF routes The route of ETF is decided on an individual basis, according to the pa- tient’s clinical condition and nutritional status, the treatment followed and the predicted duration of the nourishment by ETF can be delivered: directly to the stomach (gastric feeding) via: Ø a nasogastric/enteric tube: usually used for short-term feeding (<14 days); tube enters the nose and the end of it may be in the stomach, duodenum (first part of the small intestine) or the jejunum (second part of the small intestine). Ø Gastrostomy or percutaneusendoscopicgastrostomy(PEG), commonly used for long-term ETF; tubes are inserted through the skin (percutaneous) through a small incision on the upper abdominal wall. This may be done by a Radiologist with X-ray guidance, by an Endoscopist via endoscopy, or surgically. Indications for gastrostomy include stroke, motor neurone disease, Parkinson's disease and oesophageal cancer. Relative contra-indications include reflux, previous gastric surgery, gastric ulceration or malignancy and gastric outlet obstruction. They are inserted directly through the stomach wall endoscopically or surgically, under antibiotic cover. Ø oesophagostomy, less common beyond the stomach via: Ø a nasoduodenal or nasojejunal tube, in cases where the stomach has b to be bypassed, lower risk of aspiration Ø gastrojejunostomy, usually in patients with pre-existing gastrostomy Ø jejunostomy, usually in patients who have undergone major GI or hepatobiliary operations, or in cases of increased risk of gastric paresis.
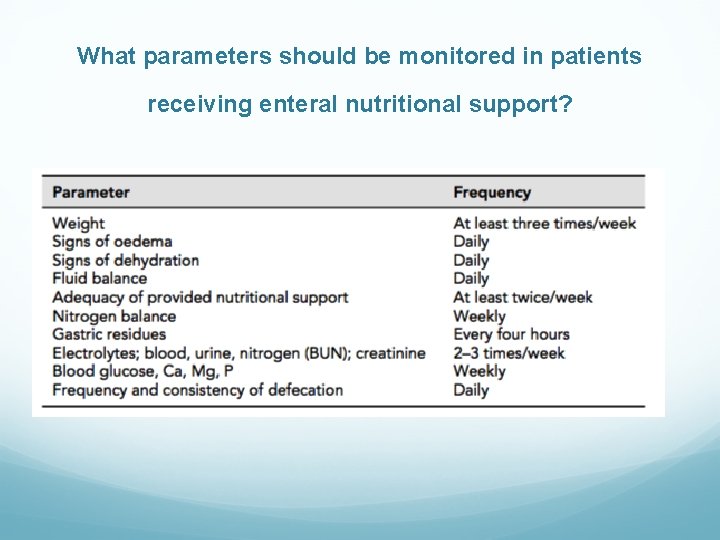
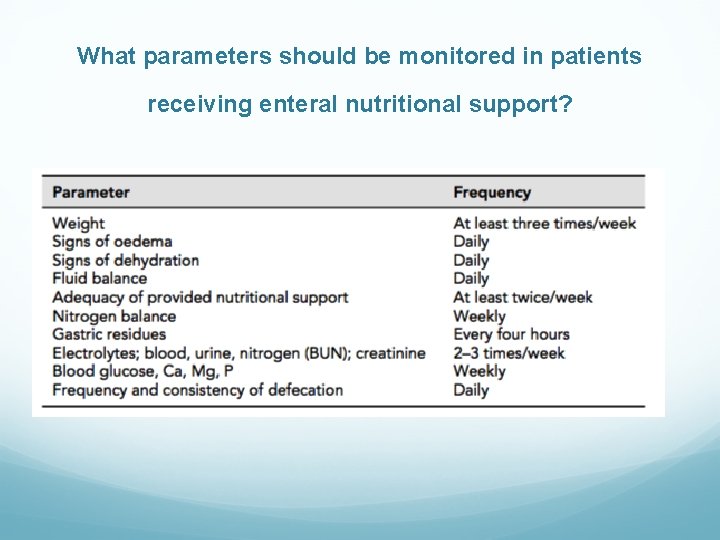
What parameters should be monitored in patients receiving enteral nutritional support?
 Sonda nasogastrica rx
Sonda nasogastrica rx Parenteral
Parenteral Formula enteral elemental
Formula enteral elemental Aralıklı infüzyon
Aralıklı infüzyon Enteral parenteral beslenme
Enteral parenteral beslenme Enteral parenteral beslenme
Enteral parenteral beslenme Nepro hcpcs code
Nepro hcpcs code Enteral nutrition
Enteral nutrition Outpatient parenteral antimicrobial therapy (opat)
Outpatient parenteral antimicrobial therapy (opat) Tpn calculations
Tpn calculations Continuous parenteral nutrition
Continuous parenteral nutrition Complication of parenteral nutrition
Complication of parenteral nutrition Ppn vs tpn
Ppn vs tpn