Nutrition in the Neonate Importance of Nutrition in
- Slides: 26
Nutrition in the Neonate
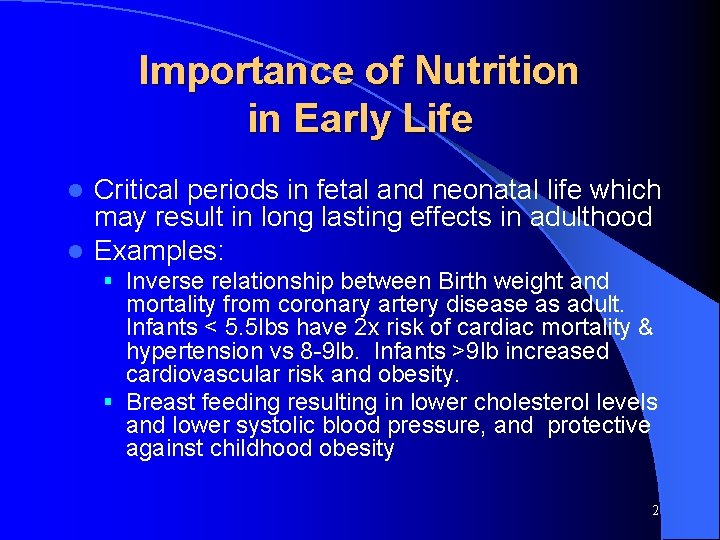
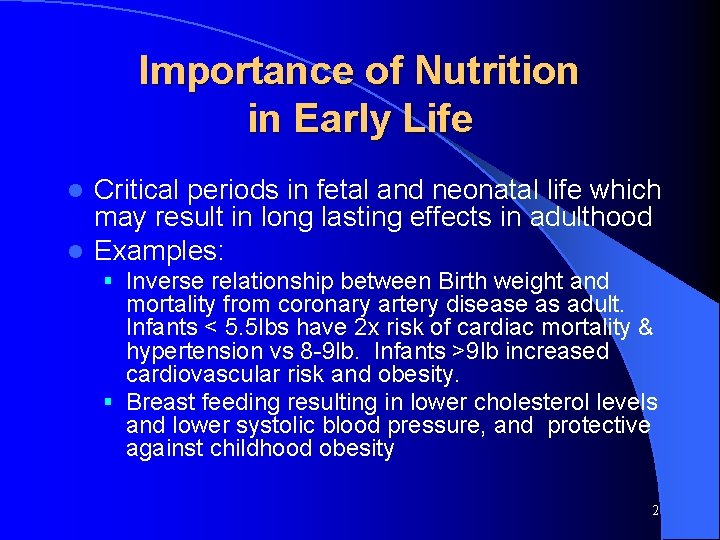
Importance of Nutrition in Early Life Critical periods in fetal and neonatal life which may result in long lasting effects in adulthood l Examples: l § Inverse relationship between Birth weight and mortality from coronary artery disease as adult. Infants < 5. 5 lbs have 2 x risk of cardiac mortality & hypertension vs 8 -9 lb. Infants >9 lb increased cardiovascular risk and obesity. § Breast feeding resulting in lower cholesterol levels and lower systolic blood pressure, and protective against childhood obesity 2
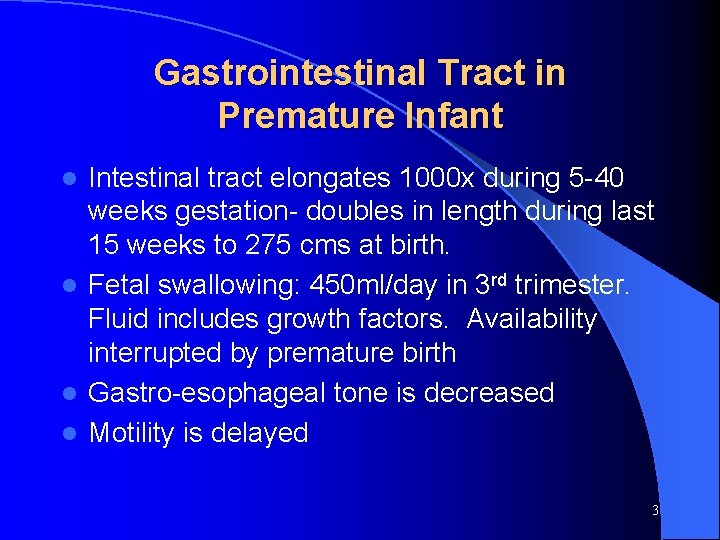
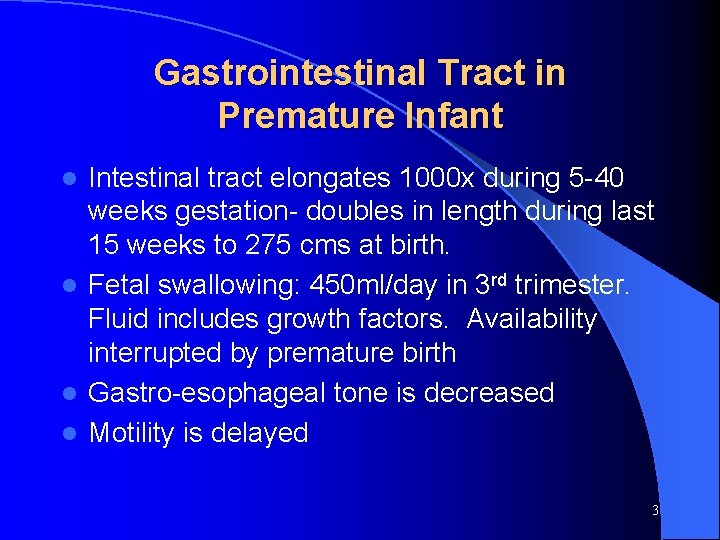
Gastrointestinal Tract in Premature Infant Intestinal tract elongates 1000 x during 5 -40 weeks gestation- doubles in length during last 15 weeks to 275 cms at birth. l Fetal swallowing: 450 ml/day in 3 rd trimester. Fluid includes growth factors. Availability interrupted by premature birth l Gastro-esophageal tone is decreased l Motility is delayed l 3
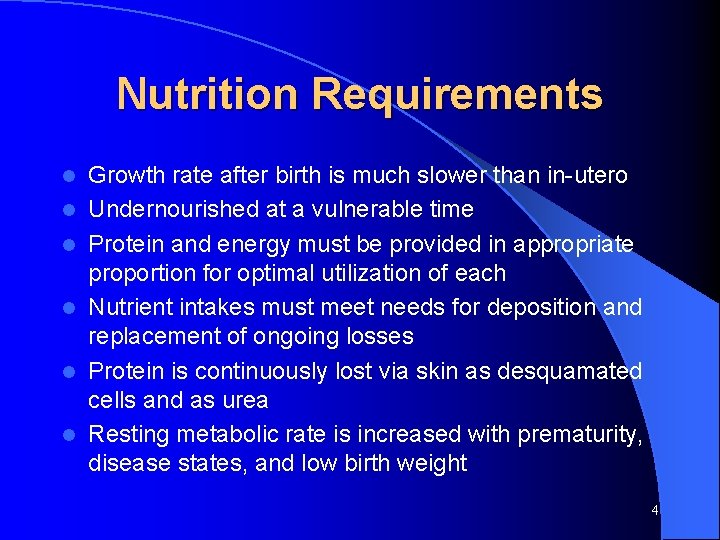
Nutrition Requirements l l l Growth rate after birth is much slower than in-utero Undernourished at a vulnerable time Protein and energy must be provided in appropriate proportion for optimal utilization of each Nutrient intakes must meet needs for deposition and replacement of ongoing losses Protein is continuously lost via skin as desquamated cells and as urea Resting metabolic rate is increased with prematurity, disease states, and low birth weight 4
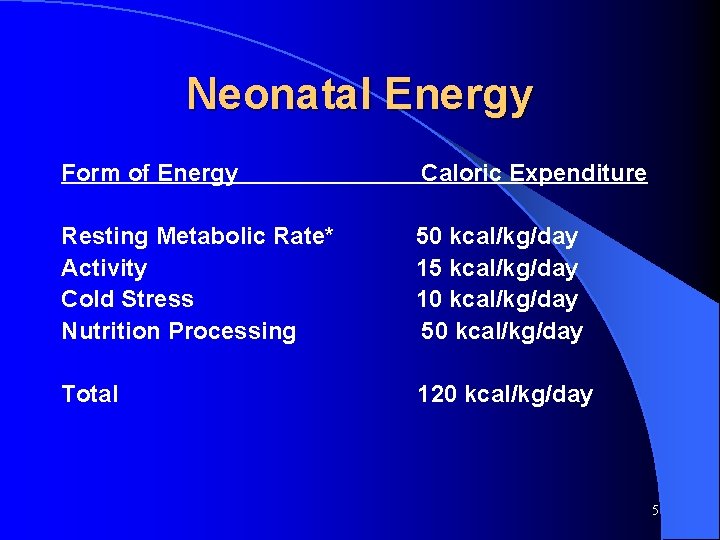
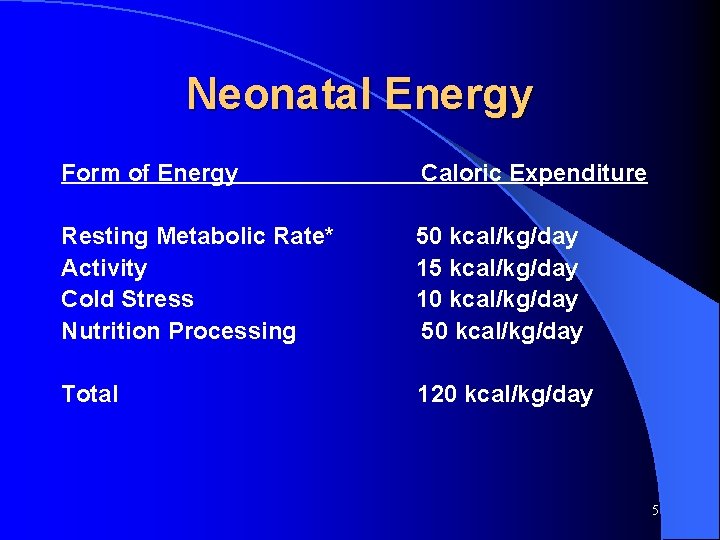
Neonatal Energy Form of Energy Caloric Expenditure Resting Metabolic Rate* Activity Cold Stress Nutrition Processing 50 kcal/kg/day 15 kcal/kg/day 10 kcal/kg/day 50 kcal/kg/day Total 120 kcal/kg/day 5
Nutrition Requirements. Carbohydrates l l l Primary energy substrate for brain metabolism Hepatic glycogen content is limited Gluconeogenesis (production of glucose from amino acids and lipid oxidation) is large contributor to glucose production Glucose regulatory hormones and enzymes are not fully developed Increased risk for hypoglycemia Hyperglycemia: exceeding normal glucose turnover rates; stress; relative insulin deficiency; hepatic peripheral insulin resistance 6
Nutrition Requirements- Lipids l l l Source of essential Fatty Acids and LCPUFA Linoleic and linolenic acid comprise cell membranes LC-PUFA (AA & DHA) important for brain and retinal development Energy substrate readily utilized by VLBW Decreases amino acid oxidation and protein breakdown when lipid provides 50% of non-protein calories Provides greater energy and is isotonic compared to high concentration dextrose 7
Benefits of Early Parenteral Nutriton Provides nutritional support and supplements enteral feedings as the gut is adapts and matures l Greater weight, length, and head circumference percentiles at discharge l Improved long term neurodevelopmental outcome l 8
Indications for TPN l l l l Prematurity < 1500 grams GI anomalies or surgery Feeding intolerance / ileus Necrotizing enterocolitis Cardiac disease Chronic diarrhea Pulmonary disease Severe asphyxia 9
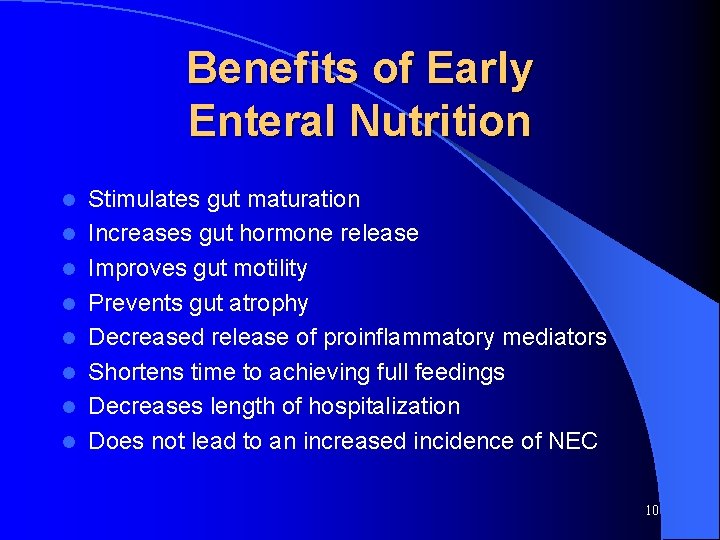
Benefits of Early Enteral Nutrition l l l l Stimulates gut maturation Increases gut hormone release Improves gut motility Prevents gut atrophy Decreased release of proinflammatory mediators Shortens time to achieving full feedings Decreases length of hospitalization Does not lead to an increased incidence of NEC 10
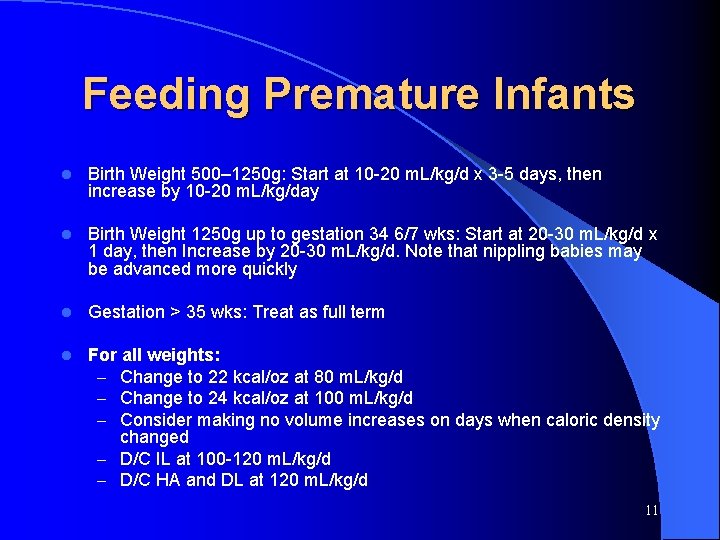
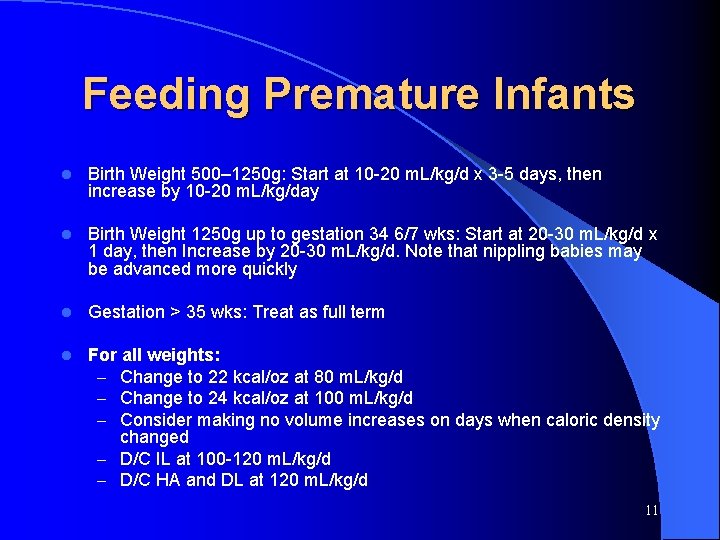
Feeding Premature Infants l Birth Weight 500– 1250 g: Start at 10 -20 m. L/kg/d x 3 -5 days, then increase by 10 -20 m. L/kg/day l Birth Weight 1250 g up to gestation 34 6/7 wks: Start at 20 -30 m. L/kg/d x 1 day, then Increase by 20 -30 m. L/kg/d. Note that nippling babies may be advanced more quickly l Gestation > 35 wks: Treat as full term l For all weights: – Change to 22 kcal/oz at 80 m. L/kg/d – Change to 24 kcal/oz at 100 m. L/kg/d – Consider making no volume increases on days when caloric density changed – D/C IL at 100 -120 m. L/kg/d – D/C HA and DL at 120 m. L/kg/d 11
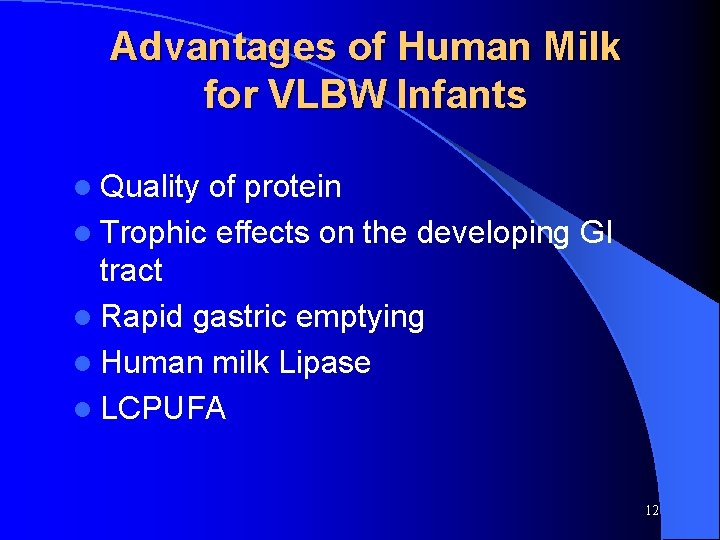
Advantages of Human Milk for VLBW Infants l Quality of protein l Trophic effects on the developing GI tract l Rapid gastric emptying l Human milk Lipase l LCPUFA 12
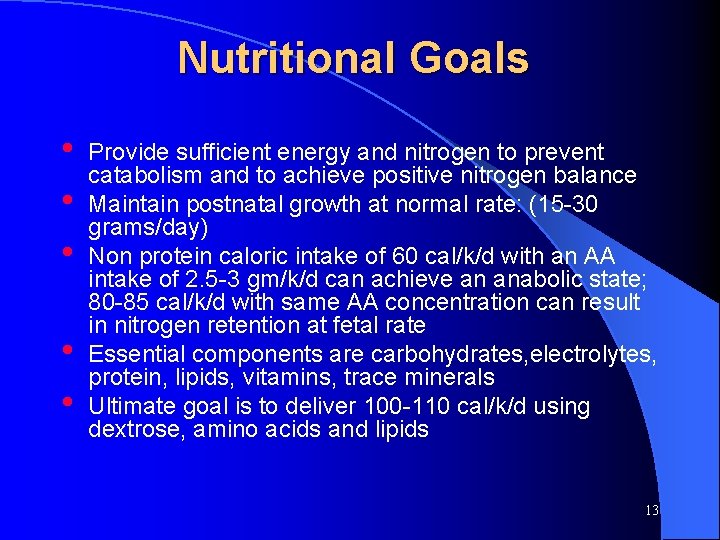
Nutritional Goals • • • Provide sufficient energy and nitrogen to prevent catabolism and to achieve positive nitrogen balance Maintain postnatal growth at normal rate: (15 -30 grams/day) Non protein caloric intake of 60 cal/k/d with an AA intake of 2. 5 -3 gm/k/d can achieve an anabolic state; 80 -85 cal/k/d with same AA concentration can result in nitrogen retention at fetal rate Essential components are carbohydrates, electrolytes, protein, lipids, vitamins, trace minerals Ultimate goal is to deliver 100 -110 cal/k/d using dextrose, amino acids and lipids 13
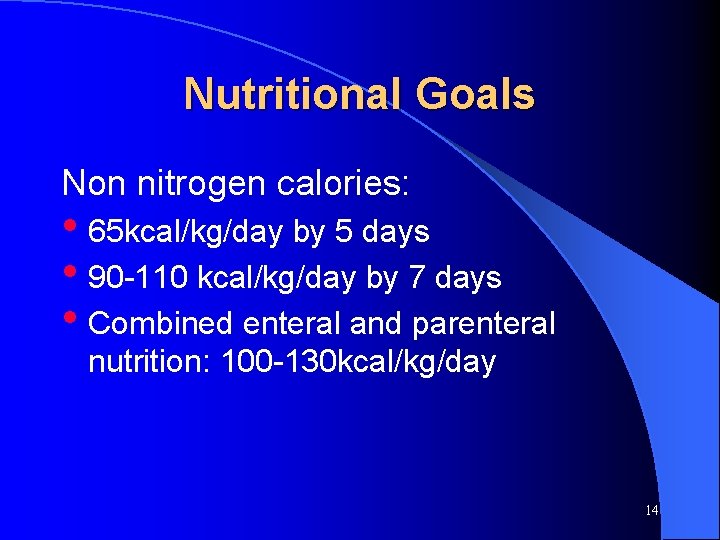
Nutritional Goals Non nitrogen calories: • 65 kcal/kg/day by 5 days • 90 -110 kcal/kg/day by 7 days • Combined enteral and parenteral nutrition: 100 -130 kcal/kg/day 14
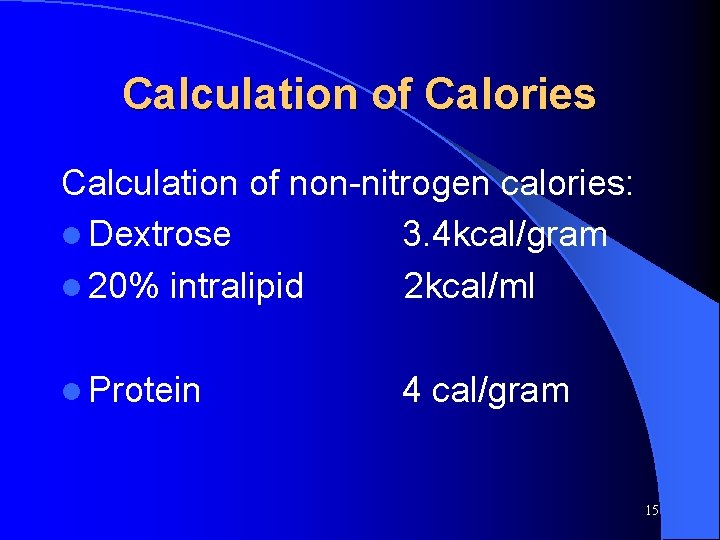
Calculation of Calories Calculation of non-nitrogen calories: l Dextrose 3. 4 kcal/gram l 20% intralipid 2 kcal/ml l Protein 4 cal/gram 15
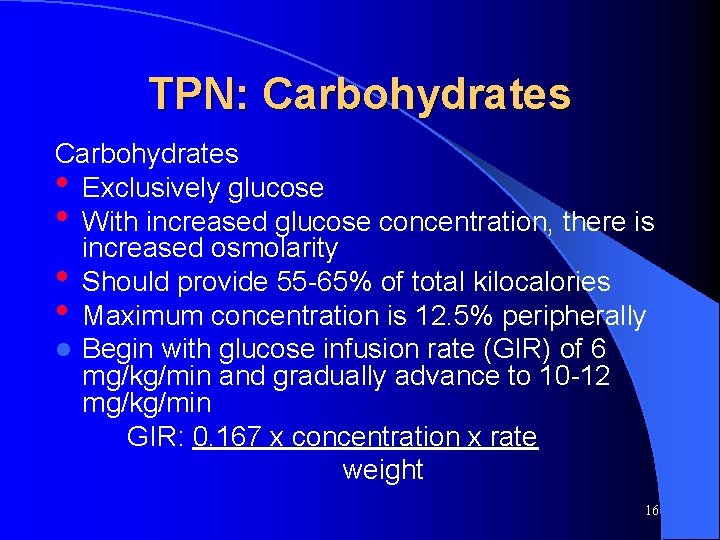
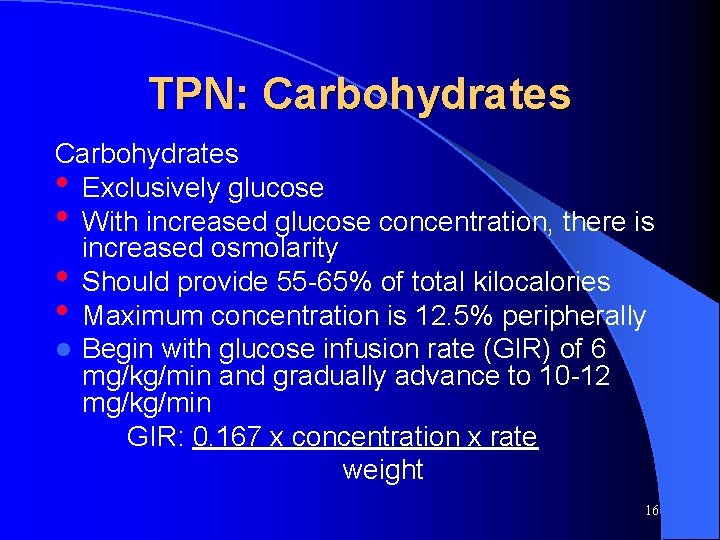
TPN: Carbohydrates • Exclusively glucose • With increased glucose concentration, there is increased osmolarity • Should provide 55 -65% of total kilocalories • Maximum concentration is 12. 5% peripherally l Begin with glucose infusion rate (GIR) of 6 mg/kg/min and gradually advance to 10 -12 mg/kg/min GIR: 0. 167 x concentration x rate weight 16
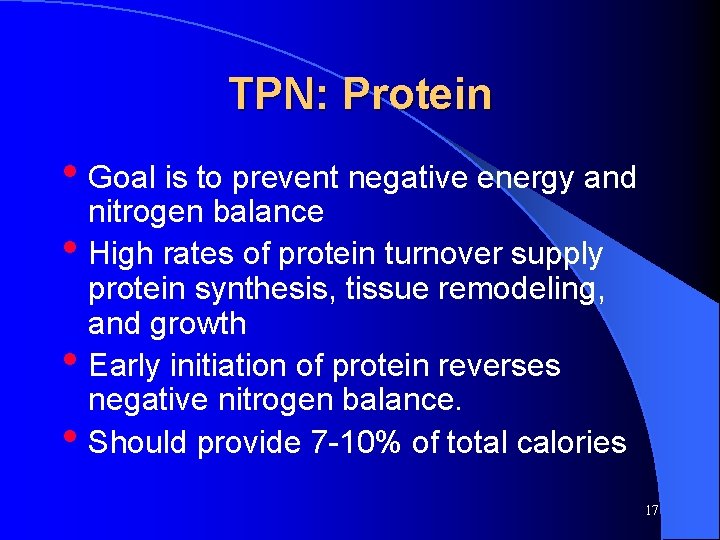
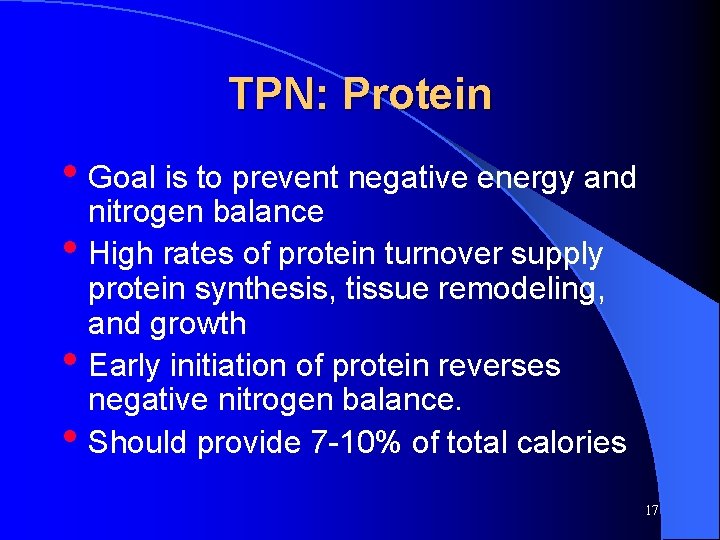
TPN: Protein • Goal is to prevent negative energy and • • • nitrogen balance High rates of protein turnover supply protein synthesis, tissue remodeling, and growth Early initiation of protein reverses negative nitrogen balance. Should provide 7 -10% of total calories 17
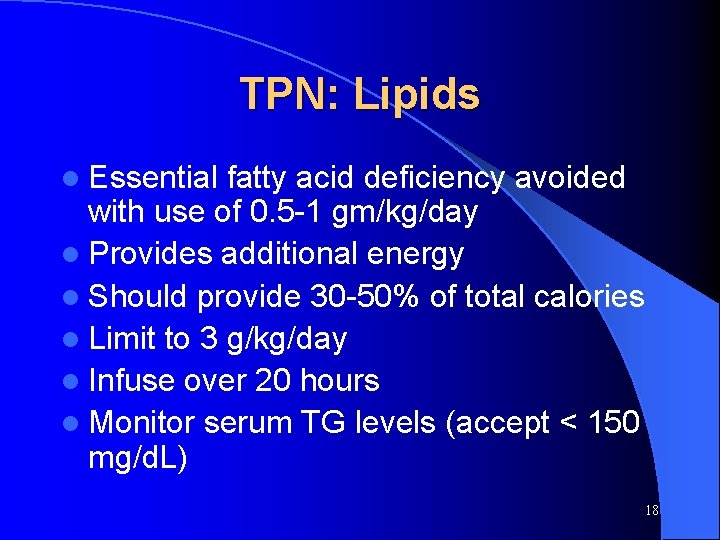
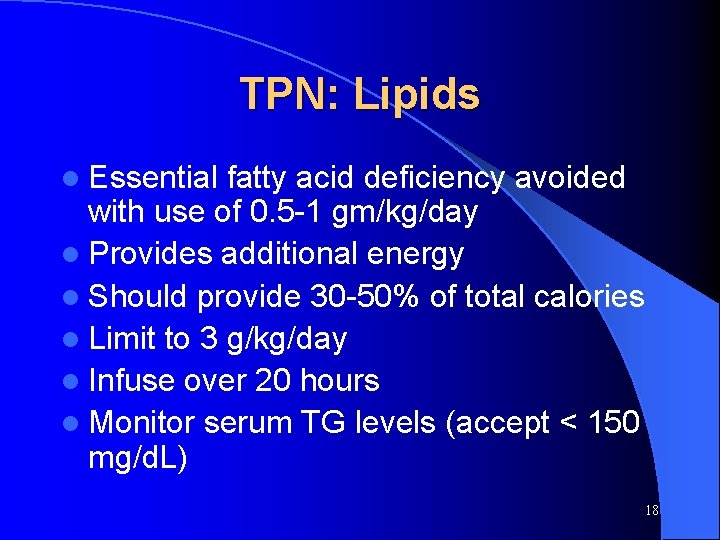
TPN: Lipids l Essential fatty acid deficiency avoided with use of 0. 5 -1 gm/kg/day l Provides additional energy l Should provide 30 -50% of total calories l Limit to 3 g/kg/day l Infuse over 20 hours l Monitor serum TG levels (accept < 150 mg/d. L) 18
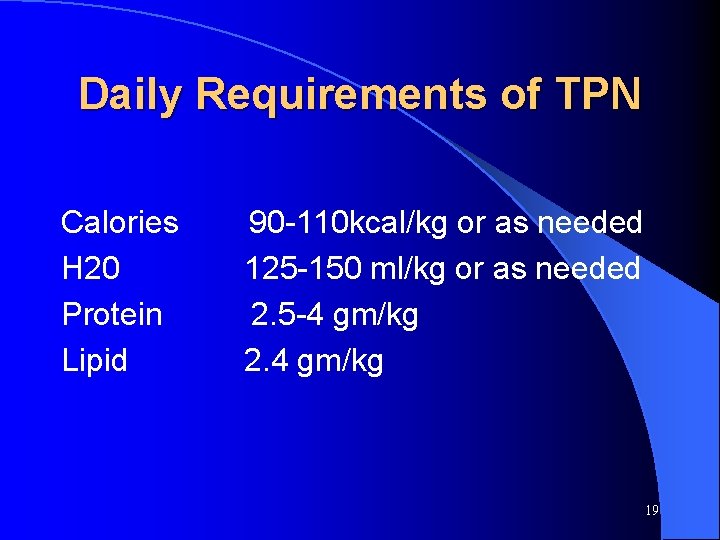
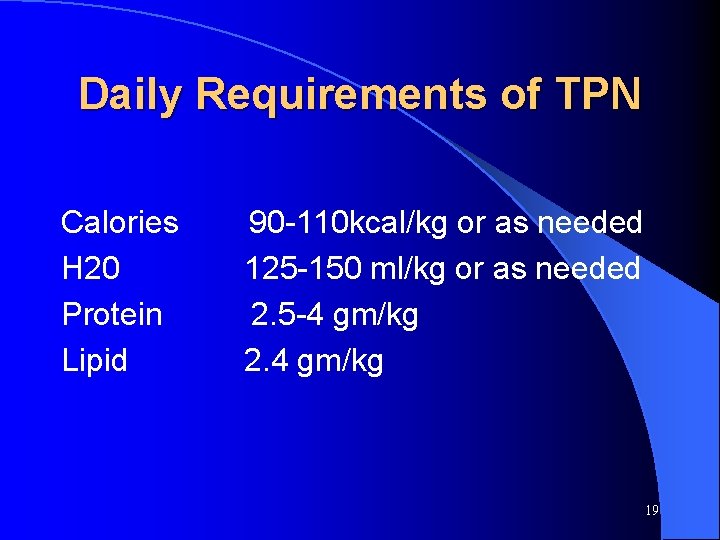
Daily Requirements of TPN Calories H 20 Protein Lipid 90 -110 kcal/kg or as needed 125 -150 ml/kg or as needed 2. 5 -4 gm/kg 2. 4 gm/kg 19
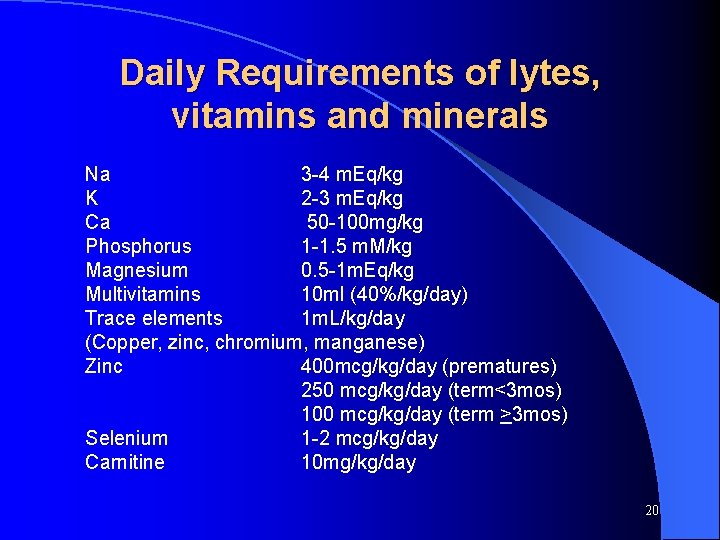
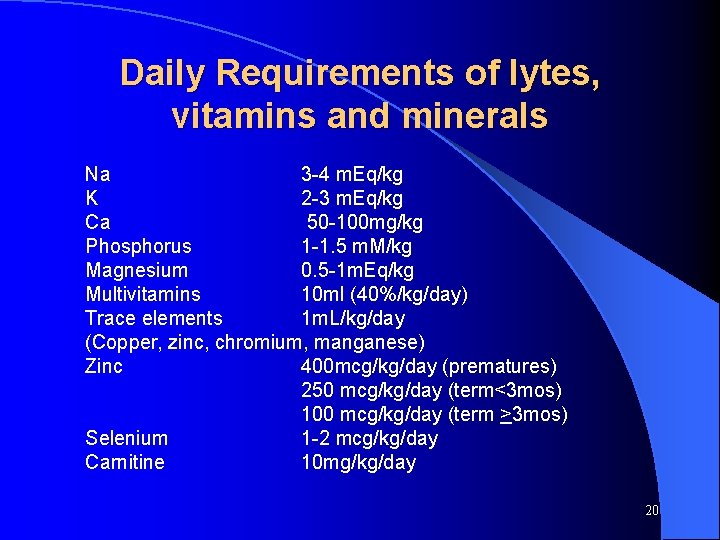
Daily Requirements of lytes, vitamins and minerals Na 3 -4 m. Eq/kg K 2 -3 m. Eq/kg Ca 50 -100 mg/kg Phosphorus 1 -1. 5 m. M/kg Magnesium 0. 5 -1 m. Eq/kg Multivitamins 10 ml (40%/kg/day) Trace elements 1 m. L/kg/day (Copper, zinc, chromium, manganese) Zinc 400 mcg/kg/day (prematures) 250 mcg/kg/day (term<3 mos) 100 mcg/kg/day (term >3 mos) Selenium 1 -2 mcg/kg/day Carnitine 10 mg/kg/day 20
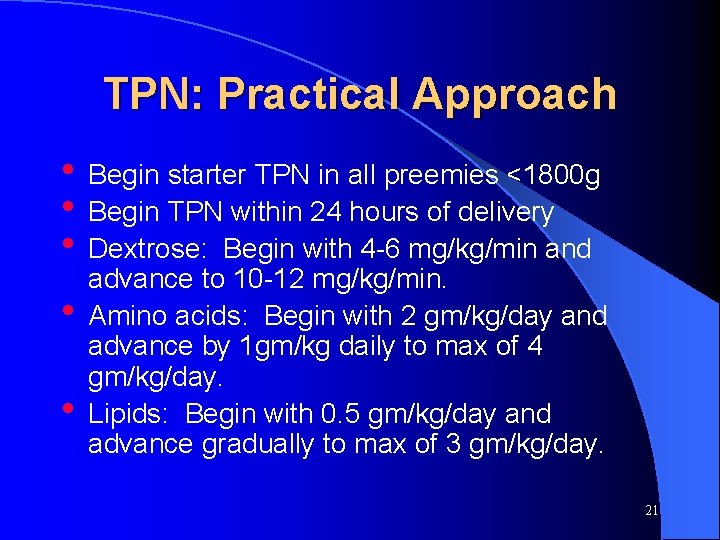
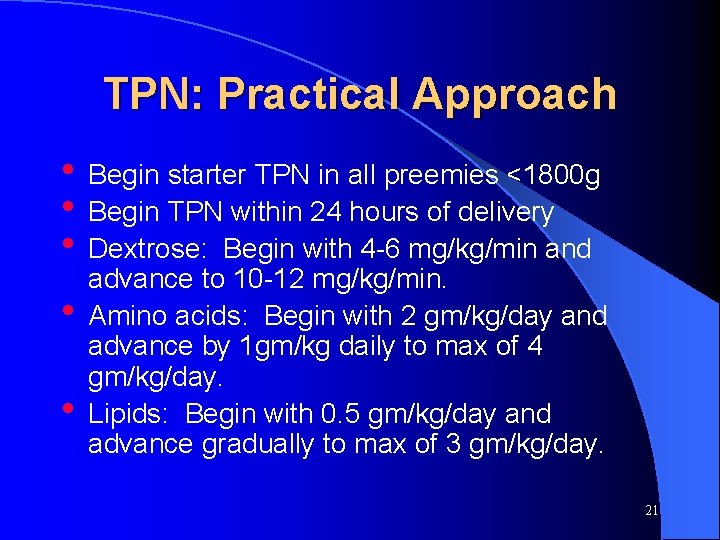
TPN: Practical Approach • Begin starter TPN in all preemies <1800 g • Begin TPN within 24 hours of delivery • Dextrose: Begin with 4 -6 mg/kg/min and • • advance to 10 -12 mg/kg/min. Amino acids: Begin with 2 gm/kg/day and advance by 1 gm/kg daily to max of 4 gm/kg/day. Lipids: Begin with 0. 5 gm/kg/day and advance gradually to max of 3 gm/kg/day. 21
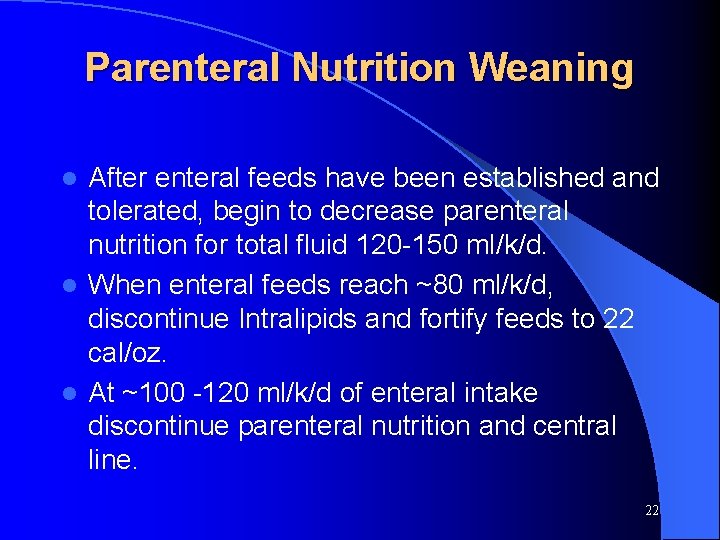
Parenteral Nutrition Weaning After enteral feeds have been established and tolerated, begin to decrease parenteral nutrition for total fluid 120 -150 ml/k/d. l When enteral feeds reach ~80 ml/k/d, discontinue Intralipids and fortify feeds to 22 cal/oz. l At ~100 -120 ml/k/d of enteral intake discontinue parenteral nutrition and central line. l 22
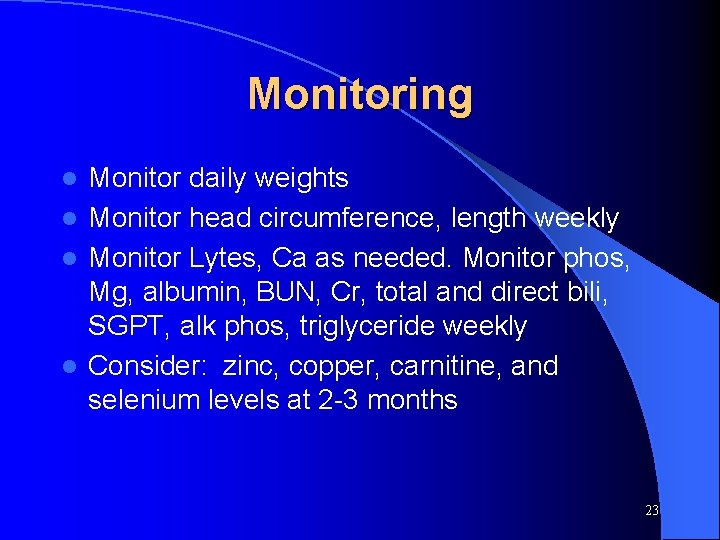
Monitoring Monitor daily weights l Monitor head circumference, length weekly l Monitor Lytes, Ca as needed. Monitor phos, Mg, albumin, BUN, Cr, total and direct bili, SGPT, alk phos, triglyceride weekly l Consider: zinc, copper, carnitine, and selenium levels at 2 -3 months l 23
Complications of TPN Catheter related: l l l Thrombus (SVC syndrome, chylothorax) Infection Extravasation (pleural and pericardial effusions) Air or fat embolus Infiltration with tissue injury 24
Complications of TPN Metabolic: • Electrolyte imbalance • Hypo-hyperglycemia • Hyperlipidemia • Trace mineral and Vit deficiency • Cholestasis • Osteopenia 25
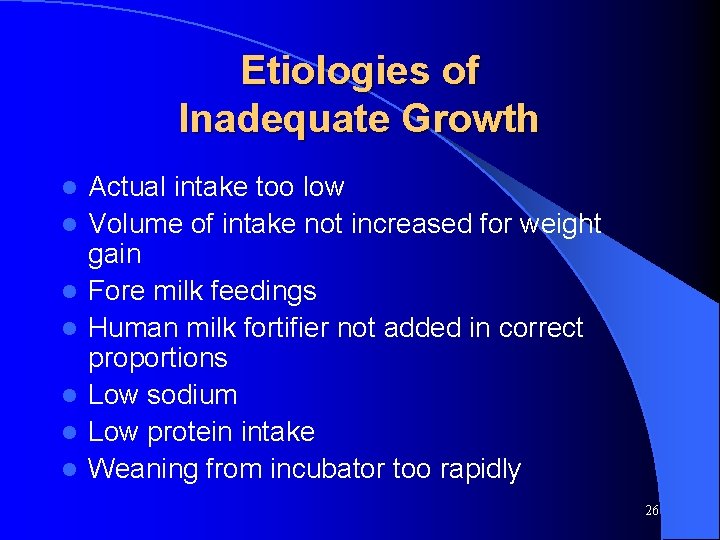
Etiologies of Inadequate Growth l l l l Actual intake too low Volume of intake not increased for weight gain Fore milk feedings Human milk fortifier not added in correct proportions Low sodium Low protein intake Weaning from incubator too rapidly 26
 Neonatal bradycardia algorithm
Neonatal bradycardia algorithm Definition of high risk neonate
Definition of high risk neonate Petechiae neonate
Petechiae neonate Priformus
Priformus Lesson 1 the importance of nutrition
Lesson 1 the importance of nutrition Nutrition survey definition
Nutrition survey definition 101012 bằng
101012 bằng Lời thề hippocrates
Lời thề hippocrates Thang điểm glasgow
Thang điểm glasgow đại từ thay thế
đại từ thay thế Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Công thức tính độ biến thiên đông lượng
Công thức tính độ biến thiên đông lượng Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Sự nuôi và dạy con của hổ
Sự nuôi và dạy con của hổ Dạng đột biến một nhiễm là
Dạng đột biến một nhiễm là Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Nguyên nhân của sự mỏi cơ sinh 8
Nguyên nhân của sự mỏi cơ sinh 8 Bổ thể
Bổ thể Phản ứng thế ankan
Phản ứng thế ankan Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan Hát lên người ơi
Hát lên người ơi điện thế nghỉ
điện thế nghỉ Một số thể thơ truyền thống
Một số thể thơ truyền thống Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Các số nguyên tố là gì
Các số nguyên tố là gì Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Phối cảnh
Phối cảnh