Assessment and management of patients with Hepatic and

















- Slides: 85
Assessment and management of patients with Hepatic and Biliary Disorders Chapter 39 -40 (11 th ed. ) 49 -50 (13 th ed. ) Mr. Mahmoud Nasrallah First Semester 2015 -2016
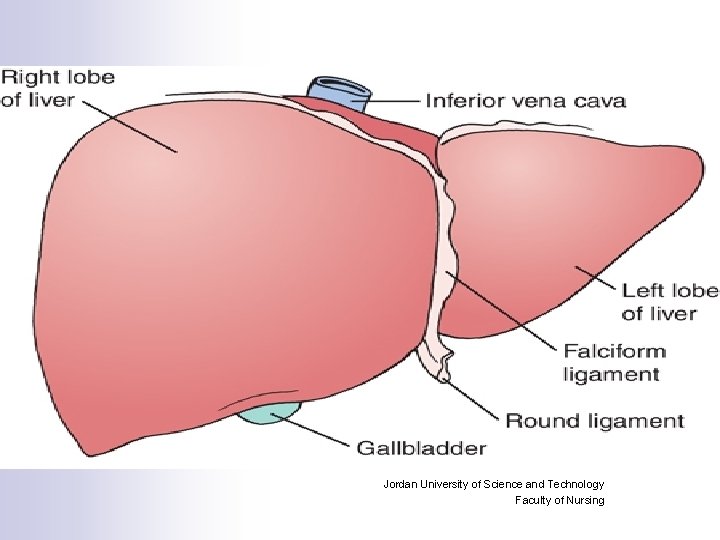
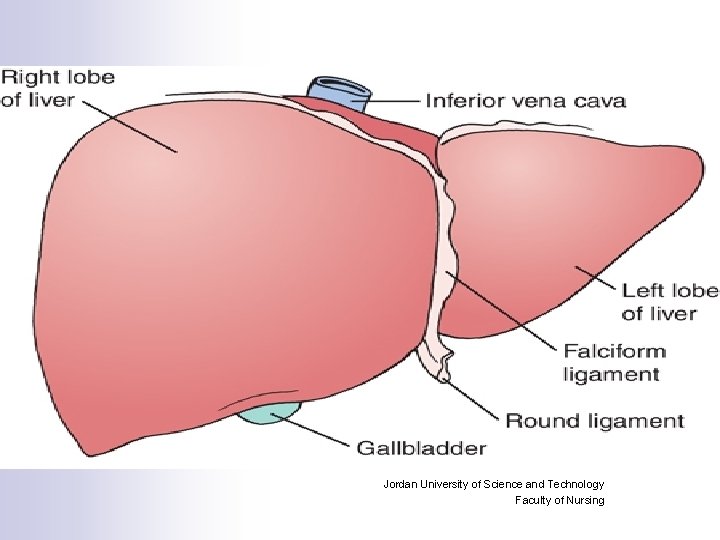
Jordan University of Science and Technology Faculty of Nursing

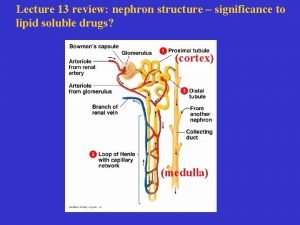
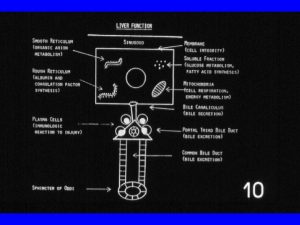
Functions of the Liver: n n n n n Glucose Metabolism and regulation of blood glucose concentration. Ammonia conversion to urea that can be excreted in the urea. Protein Metabolism: Synthesis almost all plasma proteins. Fat Metabolism: Breakdown of fatty acids for the production of energy and Ketone bodies Vitamin and Iron Storage: A, B 12 and D And several of the BComplex. Drug Metabolism Bile formation: Composed mainly from water and electrolytes and contain some fatty acids, chol. , bilirubin and bile salts. Bilirubin Excretion Activation of Vit. D in cooperation of the Kidneys
Assessment: n Health history n Ø Physical Exam Skin Abdomen • Diagnostic Evaluation Ø
Health History: n n n n Present or previous exposure or ingestion of hepatotoxic agents, drugs Family history or history of cirrhosis, hepatitis, cancer History of blood transfusions, injection, dental treatment, hemodialysis Hepatic vein thrombosis Dietary intake Duration and onset of present symptoms Life-Style Past health history

Physical Examination n Ø Skin Inspection Pallor, Jaundice: Skin, Mucosa, and Sclera Ø Muscle atrophy, Edema, Skin excoriation from scratching (pruritis) Petechia, Echomosis, Spider angiomas, and palmar erythema. • Abdominal Assessment: Ø Dilated abdominal wall veins, Ascites, Abdominal dullness. Palpation for liver tenderness, Size (Firm, sharp ridge with a smooth surface). Cirrhosis of the liver: smooth, hard, shrunken, fibrotic Acute Hepatitis: Soft edges and easily moves Percussion of upper and lower borders. Ø Ø Ø
Diagnostic Evaluation: Liver Function Tests n Liver Biopsy n Other Diagnostic Tests - X-Ray - Ultrasonography - Computed Tomography (CT) - Magnatic Resonance Imaging - ERCP - Laproscopy - A radio-Isotop Liver scan (Liver size and hepatic flow) n

Common Liver Function Tests Serum Bilirubin Test (Direct, Total) n Serum Albumin Test n n Prothrombin Time (PT) Test: Serum Alkaline Phosphatase Test: Elevation indicate an obstruction of bile flow (more sensitive than others), liver injury, or certain liver cancer n Serum Aminotransferases (transaminases): Released from damaged liver cells n
Cont…. n n Alanin Transaminase (ALT) Test, (SGPT): Released from damaged Liver cells. It is good indicator for the progress or worsening of the Liver Aspartate Transaminase (AST): (SGOT): Released from damaged liver, heart, muscle, or brain cell 5’ Nucleotidase Test: Released by the liver when the liver is injured due to bile duct obstruction or impaired bile flow. Lactic Dehydrogenase Test: Released when organs such as the liver, heart , lung, or brain injured.

Cont………. n Gamma Glutamyl Transferase or Transpeptidase (GGT) (GGTP): Are elevated in alcohol abuse and markers for biliary cholestasis n Serum Ammonia

• Liver Biopsy n n Needle Aspiration of liver tissue to examine liver cells ( An Invasive Procedure) - Location 6 th intercostal space, Mid Axillary Line Preparation: - Check PT, PTT, And platelet count, and check for compatible donor blood. - consent form signed. - Vital signs (base line reading) - Patient education is essential for preperation
During Procedure Nursing Care: - Expose the Rt side of the patient’s upper ` abdomen (Rt hypochondriac region) - Instruct the patient to inhale and exhale several time then exhale and hold.
• Post-Procedure Nursing Care: n Turn the patient on to the Rt side, place the pillow under the costal margin for several hours ( Recumbent and immobile) - Assess vital signs q 10 -15 min for 1 hr - observe puncture site for hemorrhage after test - if the patient discharge ask him to avoid heavy lifting and strenuous activity for 1 week - Major complications are liver injury, bleeding, and peritonitis, and Pneumothorax.
Hepatic Dysfunction: Due to damage to the Liver’s Cells: - from primary liver disease: infection and cancer - Or Secondary causes such as biliary obstruction, anoxia, metabolic disorder, toxins and medications, nutritional deficiencies. - may be acute or chronic n S/S of impaired liver function: malaise, anorexia, indigestion, nausea, weigt loss, diarrhea or constipation, and aching RUQ pain n
Hepatic Dysfunction • Clinical Manifestations of Liver Dysfunction (Complications): I. Jaundice: Increase concentration of Bilirubin II. Portal Hypertension 1. Ascites (leads to hepatorenal Syndrome) 2. Esophageal Varices
. . Cont III. Hepatic Encephalopathy or coma: Due to accumulation of ammonia in the serum due to impaired protein metabolism. IV. Other Manifestations: - Edema - Bleeding - Vitamin Deficiency - Metabolic abnormalities - Pruritus (Due to bile salts retention) and other skin changes.
Hepatic Disorders: 1. • • Jaundice: Bilirubin is (more than 2. 5 mg/dl). Yellow- or green-tinged body tissues, sclera, and skin due to increased serum bilirubin levels
Types and causes: • 1. Pre-hepatic (Hemolytic) Jaundice: Result of excess breakdown of RBC’s and liver is presented with more bilirubin than it’s capable of excretion - Hemolytic transfusion reaction or other hemolytic diseases - Significant increase in unconjucated or free bilirubin - Fecal and urine urobilinogen increased. 2. Intra-hepatic (Hepatocellular): Decreased bilirubin uptake by damaged liver cells - Hepatitis - Cirrhosis - Cancer of the liver
Cont……. . 3. Post-hepatic ( Obstructive) Jaundice: due to occlusion of the bile ducts - Gallstone ( cholelithiasis). - Inflammatory process - Tumor - pressure from enlarged organ 4. Hereditary Hyperbilirubinemia: due to several inherited disorders. - Gilbert’s syndrome - Dubin-Johnson syndrome • 1. 2. 3. Causes Impaired Hepatic intake Conjugation of bilirubin Excretion of bilirubin into biliary system
Continue: n Hepatocellular and obstructive jaundice types are most associated with liver disease. n Signs and Symptoms Associated with Hepatocellular and Obstructive Jaundice Hepatocellular n ¨ ¨ n Patient may appear mildly or severely ill. Lack of appetite, nausea, weight loss Malaise, fatigue, weakness Headache, chills, and fever if infectious in origin Obstructive ¨ ¨ Dark orange-brown urine and light clay-colored stools Dyspepsia and intolerance of fats, impaired digestion Pruritus Dyspepsia and intolerance of fatty foods
Clinical Manifestations n n n n Yellow Sclera Yellowish-orange Skin Clay-colored feces Tea-colored urin Pruritus Fatique Anorexia Laboratory diagnostic tests: Increased serum bilirubin, alkaline phosphatase, cholesterol, serum bile salts, prolonged PT.

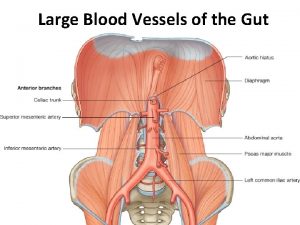
II. Portal Hypertension: n Obstructed blood flow through damaged liver results in increased BP through the portal Venous system n Consequences: 1. The formation of esophageal, gastric, and hemorrhoidal varices: Rupture cause massive bleeding Ascites: Accumulation of fluid in the abdominal cavity 2.
1. Ascites: n Ascites: Fluid in Peritoneal Cavity Due To: n Portal hypertension resulting in increased capillary pressure and obstruction of venous blood flow Vasodilatation of splanchnic circulation (blood flow to the major abdominal organs) Changes in the ability to metabolize aldosterone, increasing fluid retention Decreased synthesis of albumin, decreasing serum osmotic pressure Movement of albumin into the peritoneal cavity n n

Pathogenesis of Ascites
Manifestation 1. 2. 3. 4. 5. 6. 7. Increased abdominal girth Bulging flanks Striae Distended veins Rapid weight gain SOB Fluid and electrolyte imbalance

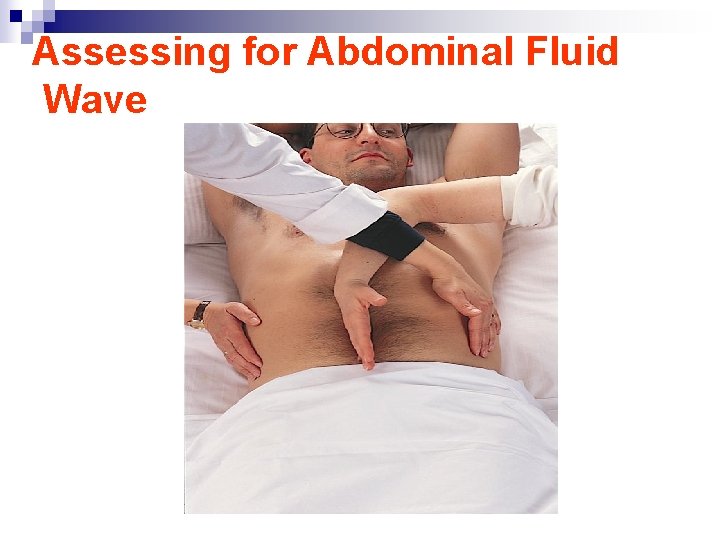
• Assessment of Ascites n n Record abdominal girth and weight daily. Paient may have striae, distended veins, and umbilical hernia. Assess for fluid in abdominal cavity by percussion for shifting dullness or by fluid wave. Monitor for potential fluid and electrolyte imbalances.
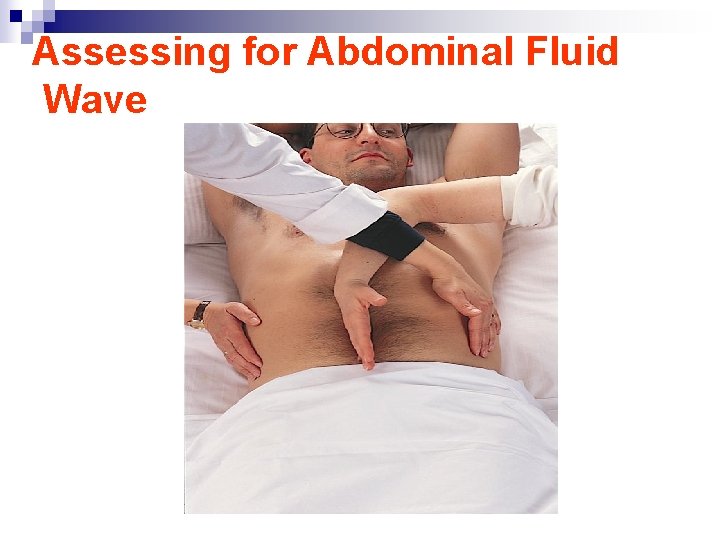
Assessing for Abdominal Fluid Wave

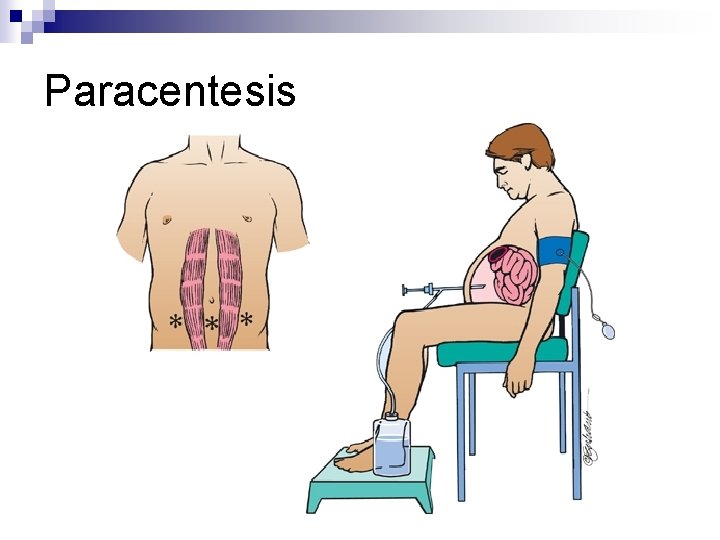
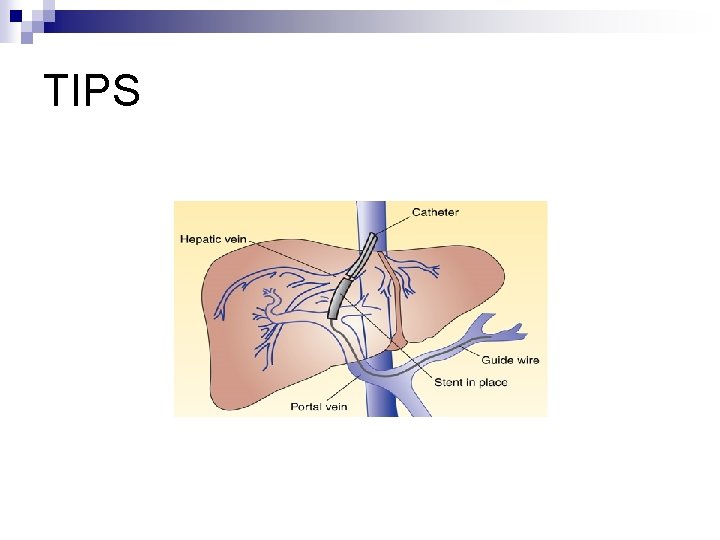
• Management Of Ascites n n n n Modify diet (reduced Sodium intake) Diuretics: Such as aldactone (aldosterone blocking agent) first line therapy. Lasix may be added with precaution because may result in: - fluid an electrolyte imbalance - Depletin of potassium result in rise of ammonia levels and result in encephalopathy Paracentesis Low-sodium diet Bed rest Administration of salt-poor albumin Transjugular intrahepatic portosystemic shunt (TIPS)
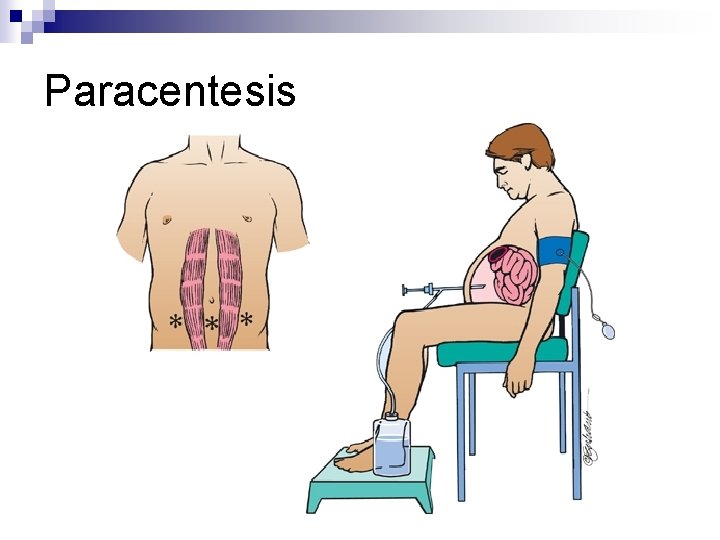
Paracentesis
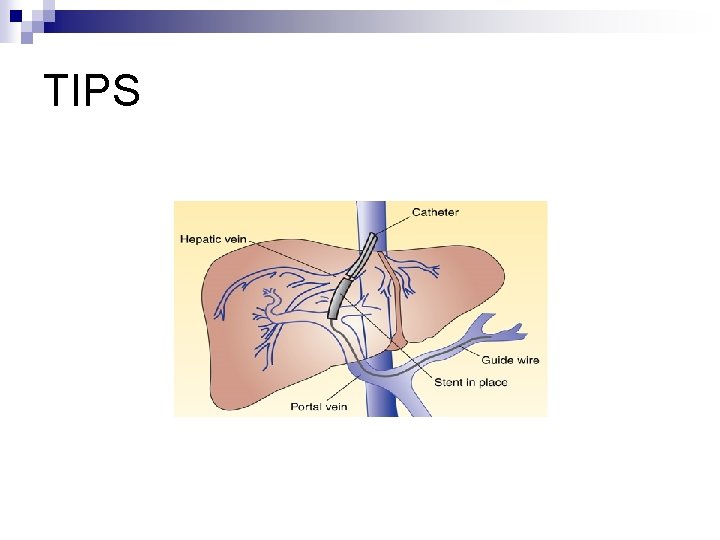
TIPS
Nursing Interventions: n Monitor I/O, Nutritional status Monitor and prevent edema: Daily Wt and measurements of abd girth Promotion of breathing Monitor serum ammonia level Monitor electrolyte leve Monitor cognitive status Monitor and promote skin integrity Promote comfort n Nursing care of paracentesis (chart 39 -2 (p. 1084) n n n n
2. Esophageal Varices: n n n Are dilated tortuous veins found on the submucosa of lower esophagus Caused by portal hypertension which is due to portal venous circulation obstruction Bleeding Esophageal varices can lead to hemorrhagic shock, decreased cerebral, hepatic, and renal perfusion Encephalopathy risk is increased due to increased nitrogen load in GI tract from bleeding and increased serum ammonia levels Hemorrhage may result from: Lifting heavy objects, straining at stool, coughing, Vomiting, poorly chewed food, irritating fluids, reflux of stomach contents, and medication
Cont…… n Clinical Manifestation 1. Hematemesis Melena General deterioration in mental or physical status History of alcohol abuse Cold clammy skin Hypotension Tachycardia 2. 3. 4. 5. 6. 7.
Cont…. . n Assessment and diagnostic Findings: Endoscopy: to identify the bleeding site 2. Barium swallow 3. Ultrasonography 4. CT 5. Angiography 6. Portal hypertension measures: indirect insertion of fluid-filled ballone catheter into the antecubital or femoral vein to the hepatic vein 7. Laboratory tests such as liver function test, blood flow and clearance studies to assess cardiac output and hepatic bld flow Managing Esophageal Varices: - monitor V/S, monitor signs of hypovolemia, O 2 administration, Pharmacological therapy to decrease portal pressure ( Vasopressin and Beta Blockers), Balloon Tamponade: Sengstaken-Blakemore tube 1.

Medical Management of Bleeding Esophageal Varices 1. Control Bleeding By applying pressure on the cardiac portion of the stomach and against the bleeding varices by a double-balloon tamponade (Sengstaken-Blakemore tube) - Has four opening: Gastric Aspiration, Esophageal aspiration, inflating of the gastric balloon, and inflating of the esophageal balloon - The pressure in the balloon should be 25 -40 mm. Hg and to be checked q 24 hrs - Overinfalting and leaving balloon for long time may cause injury from ulceration and necrosis of the mouth nose or stomach mucosa - Displacement of tube may result in obstruction of airway and asphyxia from aspiration - Overinfalting may result in sudden rupture and aspiration of gastric content into the lung. - Frequent assessment for bleeding and inflation of balloons are neede in order to minimize the complications.
Esophageal varices : nursing action • Continuous monitoring of physical, emotional & mental status • Assess vital signs & nutritional status • GI bleeding-elevated serum ammonia causing drowsiness to profound coma • Parenteral nutrition if complete rest of esophagus is indicated • Gastric suctioning to prevent straining & vomiting • Frequent oral hygiene & moist sponge to the lips to prevent thirst feeling • blood transfusions & Vit K therapy • Quiet environment & reassurance to relieve anxiety • Delirium secondary to alcohol withdrawal may occur; anxiety • Provide support & explanation about medical therapies
3. Hepatic Encephalopathy and Coma n n Results from accumulation of Ammonia and other toxic metabolites in the blood. Hepatic Coma represents most advanced stages of hepatic encephalopathy. (See stages in table 39 -3) Ammonia is a result of enzyme and bacterial digestion of dietary and blood protein in the GI tract. GI bleeding in Esophageal Varices increases ammonia.
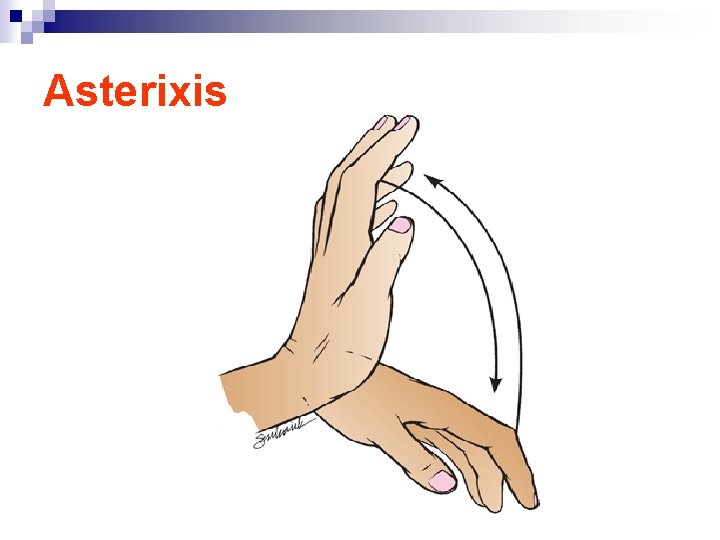
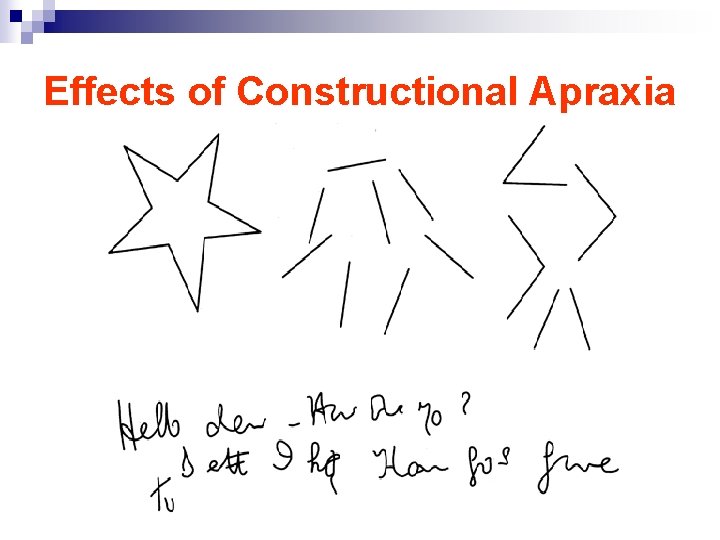
Clinical manifestation Mental changes n Motor disturbances n Alteration in mood n Changes in personality n Altered sleep pattern ( day and night reversal) n Asterixis( Flapping tremor of hands) - impaired writing and in ability to draw line or figures ( This way used to assess the improvement of the patient) - Constructional apraxia ( in ability to draw simple figures) n EEG slowing of brain Waves n Potential seizures n Fetor Hepaticas: Sweet slightly fecal odor to the breath of intestinal origin n
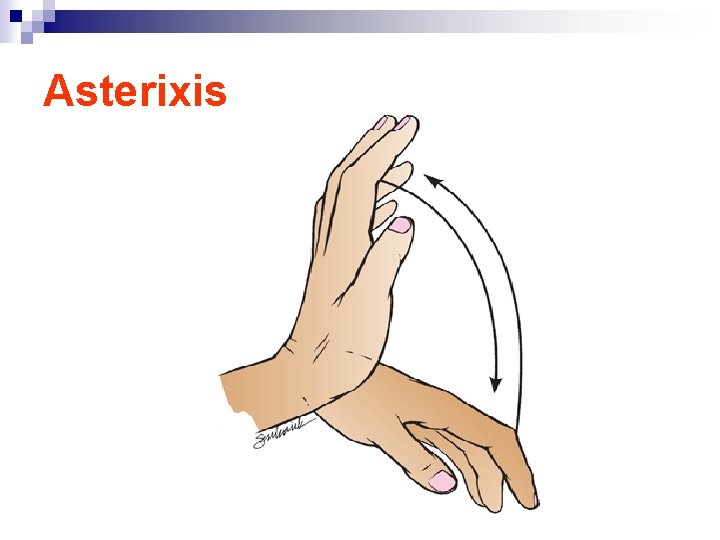
Asterixis
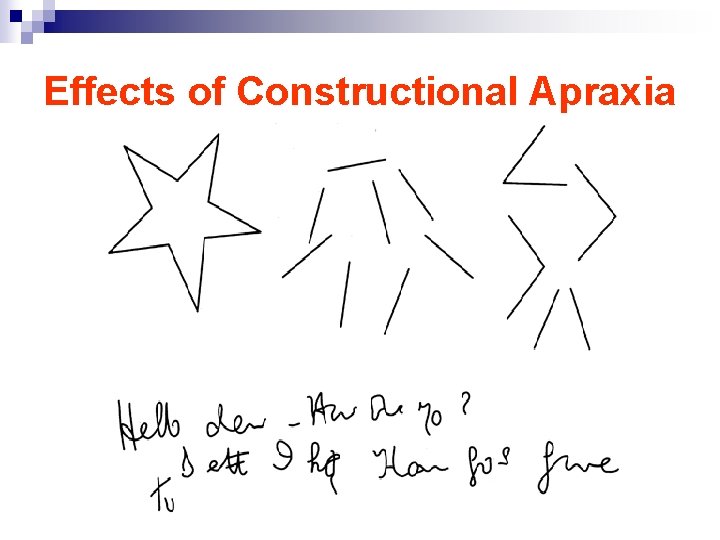
Effects of Constructional Apraxia
Medical Management: n Lactulose: promotes excretion of ammonia through stool to reduce serum ammonia levels - Causes intestinal bloating and cramps - Monitor for hypokalemia and dehydration - For comatose pt give through NG tube or enema n IV administration of glucose to minimize protein breakdown n Administration of vitamins to correct deficiency n Correct electrolyte imbalance
Cont. . n n n We don’t restrict protein completely ( at least. 5 g/kg usually 1 g/kg-1. 5 g/kg) Small frequent meals and complex CHO Substitute vegetable protein for animal protein Reduction of ammonia from GI tract by gastric suction, enemas, oral antibiotics Discontinue sedatives, analgesics, and tranquilizers. Monitor for and promptly treat complications and infections.
Viral Hepatitis: n n Hepatitis A, B, C, D, E Self study Compare and contrast the four types of Hepatitis in regards to: - Etiology - Mood of transmission - Incubation - Immunization - Patient teaching guide lines Use reference, Table 39 -4
Hepatic Cirrhosis n n Is a chronic disease characterized by replacement of normal liver tissue with diffuse fibrosis that disrupt the structure and function of the liver. Irreversible process
Type of Hepatic cirrhosis: 1. 2. 3. • • Alcoholic cirrhosis: The scar tissue surrounds the portal areas and is the most common type. Postnecrotic cirrhosis: There are broad bands of scar tissue as a late result of acute viral hepatitis Biliary cirrhosis: Scarring occurs in the liver around the bile ducts. Usually is the result of chronic biliary obstruction and infection (Cholangitis). Less common type. The portion of the liver involved in cirrhosis consist of portal and periportal spaces where the bile canaliculi communicated to form the liver bile ducts These portions become inflamed and the bile duct become occluded with thickened bile an pus.
Pathophysiology ( Causes of Hepatic cirrhosis): . 1. Nutritional deficiency with reduced protein intake 2. Excessive alcohol intake ( Most common cause) 3. Exposure to certain chemecals ( carbon tetrachloride, chlorinated naphthalene, arsenic, or phosphorus) or exposure to infection n Twice as many men as women are affected n Most patients are between 40 and 60 years of age.
Clinical Manifestation: 1. 2. 3. 4. 5. 6. 7. Liver enlargement: Early symptoms, liver loaded with fatty tissue (firm and has sharp edge, producing abd pain, later the liver decreases in the size due to contraction of scar tissue and the edges become nodular. Portal obstruction and ascites Infection and peritonitis Gastrointestinal varices Edema Vitamin deficiency and anemia Mental deterioration
Cont…. n Clinical manifestation: n Compensated Intermittent mild fever Vascular spider Palmer erythema Unexplained epistaxis ankle edema Vague morning indigestion Flatulent dyspepsia Abdominal pain Firm, enlarged liver splenomegaly n Decompensated Ascites Jaundice weakness Muscle wasting weight loss Continuous mild fever purpora spontaneous bruising Epistaxis Hypotension spares body hair white nails Gonadal atrophy Diagnostic Tests: LFT, CT, MRI, Ultrasound scanning and then confirmed by liver biopsy
Medical Management: n n n Based on presenting symptoms Monitor for complications Maximize liver function - Antiacids to decrease gastric distress and minimize the possibility of gastric bleeding - Adequate rest, Vitamins and nutritional support to promote healing of damaged liver cells -Potassium sparing diuretics - Avoidance of alcohol - adequate calories and protein ( unless if there is encephalopathy) - Fluid and elect. Restriction - Colchicine
Nursing Process: The Care of the Patient with Cirrhosis of the Liver: Assessment n n n n Focus on onset of symptoms and history of precipitating factors. Alcohol use/abuse Dietary intake and nutritional status Exposure to toxic agents and drugs Assess mental status. Abilities to carry out ADL/IADLs, maintain a job, and maintain social relationships Monitor for signs and symptoms related to the disease, including indicators for bleeding, fluid volume changes, and lab data.
Diagnosis Activity intolerance n Imbalanced nutrition n Impaired skin integrity n Risk for injury and bleeding n
Collaborative Problems/Potential Complications Bleeding and hemorrhage n Hepatic encephalopathy n Fluid volume excess n
Planning n Goals may include increased participation in activities, improvement of nutritional status, improvement of skin integrity, decreased potential for injury, improvement of mental status, and absence of complications.
Activity Intolerance Rest and supportive measures n Positioning for respiratory efficiency n Oxygen n Planned mild exercise and rest periods n Address nutritional status to improve strength. n Measures to prevent hazards of immobility n
Imbalanced Nutrition n n n n I&O Encourage patient to eat. Small, frequent meals may be better tolerated. Consider patient preferences. Supplemental vitamins and minerals, especially B complex; provide water-soluble forms of fat-soluble vitamins if patient has steatorrhea High-calorie diet, sodium restriction for ascites Protein is modified to patient needs. Protein is restricted if patient is at risk for encephalopathy.
Other Interventions n Impaired skin integrity ¨ Frequent position changes ¨ Gentle skin care ¨ Measures to reduce scratching n by the patient Risk for injury ¨ Measures to prevent falls to prevent trauma related to risk for bleeding ¨ Careful evaluation of any injury related to potential for bleeding
Nursing Management of Cirrhosis: 1. Adequate Nutrition n n 2000 -3000 cal/day High protein to help liver regenerate unless encephalopathy is there High CHO - Fat restriction is not necessary Restrict F/E intake if Ascites or edema presents Rest frequently Control tempreture Antiemetic, antiacids, antidiarrheal as ordered Vitamins supplements (Fat soluble) 2. Removal all hepatotoxic drugs 3. Avoid alcohol, and give antibiotic if ordered n n n
Cancer of the liver: n n n 1. 2. 3. n May be malignant or Benign (uncommon) Primary liver cancer are associated with - Chronic liver disease - Hepatitis B, and C infection - Cirrhosis Type of primary Liver cancer: (few) Hepatocellular carcinoma (HCC): Most common type. nonresectable Cholangiocellular carcinoma: Resectable ( early detection) Hepatocellular and cholangiocellular carcinoma: resectable Most of liver cancers are metastasized from other organs( Secondary)
Clinical Manifestation: n Pain, continuous dull ache in the right upper Quadrant, epigastrium or back Wt loss Loss of strength Anorexia Anemia may occur Enlarged liver and irregular in palpation Jaundice and Ascites n Assessment and Diagnostic tests n n n
Medical Management: 1. Nonsurgical Management: n Radiation therapy Chemotherapy Percutaneous Biliary drainage: are used to reestablish biliary drainage, relieve pressure and pain and decrease pruritus and jaundice. (Catheter inserted through the abd wall pass the obstruction then to DU after days the catheter is opened to external drainage to assess the bile amount, color and content). Laser hyperthermia: Using heat and direct it to tumor Immunotherapy: under investigation n n
Cont…. . 2. n n n Surgical Management: Lobectomy: Surgical resection of part of the liver up to 90%(Most common surgical procedure Cryosurgery (Cryoablation): Tumor destroyed by using liquid Nitrogen at 196 C. Liver transplantation: Replacement the liver with healthy donor organ. Recurrence of primary tumor is 70 -80% after transplantation.

Liver, Biliary System, and Pancreas
Biliary Conditions: n Definition of terms: Biliary (chart 40 -1) n Cholecystitis: Inflamation of the gallbladder Cholelithiasis: the presence of calculi in the gallbladder Cholecystectomy: removal of the gallbaldder Cholecystostomy: opening and drainage of the gallbladder Choledochotomy: opening into the common duct Choledocholethiasis: stone in the common duct n n n
Cont…. . n n n Choledochlithotomy: incision of common bile duct for removal of stones Choledochoduodenostomy: anastomosis of common duct to DU Choledochojejunostomy: anastomosis of CD to jejunom Lithotripsy: disintegration of gallstones by shock waves Laparoscopic chlecystectomy: removal of gallbladder by endoscopic procedure Laser Cholecystectomy: Removal of gallbladder using laser.

Cholecystitis: n Acute infection of the gallbladder causes pain, tenderness, and rigidity of the upper Rt abd and associated with nausea and vomitting and positive Murphy’s sign.
Types: 1. Calculous: gallbladder stone obstruct bile outflow causing back up of the bile in the gallbladder leading to autolysis and edema. Vascular supply is compromised and leads to gangrene and perforation 2. Acalculous: Acute gallbladder inflammation in the absence of obstruction by gallstones (major surgical procedure, trauma, or burns, cystic duct obstruction, primary bacterial infection, multiple blood transfusion

Cholithiasis n Calculi, or gallstone usually formed in the gallbladder from the solid constituent of the bile and vary in size, shape and composition 1. Pigment stone: precipitating of unconjugated pigment in the bile to form stones represent one third of cases. Causes cirrhosis, hemolysis and infection of the biliary tree 2. Cholesterol stones: Cholesterol is insoluble in water, solubility depend on bile acid and lecithin (phospholipid) in bile. Decreased bile acid and increase cholesterol synthesis in liver cause bile supersaturation with cholesterol which precipitate and form stone
Cont… n n n Four time more women than men develop cholelesterol stones and gallbladder disease (due to estrogen and contraceptive use which increase cholesterol saturation) Risk factors : Obesity, multi parous, Frequent changes in Wt, Rapid Wt loss, oral contraceptive, estrogens, cystic fibrosis, DM, and increases with age due to more cholesterol synthesis and decreased bile acid synthesis
Clinical Manifestations: n Silent, producing no pain and only mild GI symptoms( detected accidentally). Two type of Symptoms ( which may be acute or chronic) 1. From disease of the gallbladder itself: epigastric distress following fatty meal( fullness, abdominal distention) vague pain in the RUQ 2. From Obstruction of the bile passage by gallstone fever palpable mass Colicky pain ( Rt abdominal pain radiated to the back or Rt shoulder) Nausea and vomiting Murphy’s sign (inspiratory pain): Positive Jaundice (commonly occurs with obstruction of common bile duct) Changes in Urine color (dark color) and stool color ( clay-colored) Vitamin deficiency ( fat-soluble vitamins n
Diagnostic Tests: n n n Abdominal X-ray U/S Radionuclide imaging: IV radioactive agent Cholecystography: oral iodine contrast agent used 10 -12 hrs before X-ray, NPO Endoscopic retrograde cholengiopancretography (ERCP): Direct observation through fiberoptic scope inserted through esophagus into DU ( Discuss nursing implication). Percutaneous transhepatic Cholengiography: inject the dye directly into the biliary tree.

Cont……… n Medical management: Treatment of acute symptoms n Nutritional and supportive treatment: Lowfat, liquid diet, rest, IV fluids, nasogastric suction, analgesia and antibiotics n Pharmacological therapy to dissolve small, radiolucent gallstones composed primarily of cholesterol (ursodeoxycholic acid and chenodeoxycholic acid) n
Nonsurgical removal of gallstones n n Dissolving gall stone: infusion of solvent into the gallbladder Extracorporeal shockwave lithotripsy (through water bath): Pt should have < 4 stones, < 3 cm in diameter, and no liver or pancreas disease. Contraindicated inflammatory disease of the biliary system Intracorporeal lithotripsy: by ultrasound, pulsed laser By Instrumentation: such as ERCP
Surgical Management: n n n Laparoscopic Cholecystectomy Mini-Cholecystectomy Choledochostomy Surgical Cholecystostomy: opening the gallbladder to remove the stone or the pus by drainage when severely inflamed before removal. Percutaneous Cholycystostomy.

Nursing Process: Undergoing Surgery for Gallbladder Disease: Assessment n n n Patient history Knowledge and teaching needs Respiratory status and risk factors for postop respiratory complications Nutritional status Monitor for potential bleeding. GI symptoms: after laparoscopic surgery, assess for loss of appetite, vomiting, pain, distention, fever--potential infection or disruption of GI tract.
Diagnosis: Acute pain n Impaired gas exchange n Impaired skin integrity n Imbalanced nutrition n Deficient knowledge n

Collaborative Problems/Potential Complications n n n Bleeding Gastrointestinal symptoms Complications as related to surgery in general: atelectasis, thrombophlebitis n Planning n Goals may include relief of pain, adequate ventilation, intact skin, improved biliary drainage, optimal nutritional intake, absence of complications, and understanding of self-care routines.
Postoperative Care Interventions n n n n Low Fowler’s position May have NG tube NPO until bowel sounds return, then a soft, lowfat, high-carbohydrate diet postoperatively Care of biliary drainage system Administer analgesics as ordered and medicate to promote/permit ambulation and activities, including deep breathing. Turn, and encourage coughing and deep breathing, splinting to reduce pain. Ambulation
Patient Teaching (See Chart 40 -3) n n n Medications Diet: at discharge, maintain a nutritious diet and avoid excess fat. Fat restriction is usually lifted in 4 -6 weeks. Instruct in wound care, dressing changes, care of T-tube. Activity Instruct patient and family to report signs of gastrointestinal complications, changes in color of stool or urine, fever, unrelieved or increased pain, nausea, vomiting, and redness/edema/signs of infection at incision site.
Pancreatitis n n n A severe disorder that can lead to death. Acute pancreatitis does not usually lead to chronic pancreatitis. Acute pancreatitis: pancreatic duct becomes obstructed and enzymes back up into the pancreatic duct, causing autodigestion and inflammation of the pancreas Chronic pancreatitis: a progressive inflammatory disorder with destruction of the pancreas. Cells are replaced by fibrous tissue, and pressure within the pancreas increases. Mechanical obstruction of the pancreatic and common bile ducts and destruction of the secreting cells of the pancreas occur.
Causes: n n n n Biliary tract disease: Stones Long term use of alcohol Bacterial or viral infection Blunt abd trauma, peptic ulcer, ischemic vascular disease Hyperlipidemia, hypercalcemia Use of corticosteriods, thiazide diuretics, and oralcontraceptivr ERCP or surgeries near to pancreas.
Assessment and diagnostic findings n n n n History of Abd pain Serum amylase and Lipase Increase WBC’s X-Ray studies Ultrasound Abd CT-Scan ERCP rarely used because patient is acutely ill.
Manifestations n Acute: n Severe abdominal pain Patient appears acutely ill. Abdominal guarding Nausea and vomiting Fever, jaundice, confusion, and agitation may occur. Ecchymosis in the flank or umbilical area may occur. Patient may develop respiratory distress, hypoxia, renal failure, hypovolemia, and shock. n n n n Chronic: n Recurrent attacks of severe upper abdominal and back pain accompanied by vomiting Weight loss Steatorrhea n n

Nursing Process: Assessment n n n n Focus on abdominal pain and discomfort. Fluid and electrolyte status Medications Alcohol use GI assessment and nutritional status Respiratory status Emotional and psychological status of patient and family; anxiety and coping
Diagnosis: n n Acute pain Ineffective breathing pattern Imbalanced nutrition Impaired skin integrity n Collaborative Problems/Potential Complications: n n Fluid and electrolyte disturbances Necrosis of the pancreas Shock Multiple organ dysfunction syndrome DIC n Planning: n n Major goals include relief of pain and discomfort, improved respiratory function, improved nutritional status, maintenance of skin integrity, and absence of complications.
Relieving Pain and Discomfort Use of analgesics n Nasogastric suction to relieve nausea and distention n Frequent oral care n Bed rest n Measures to promote comfort and relieve anxiety n
 What causes hepatic encephalopathy
What causes hepatic encephalopathy Management of patients with neurologic trauma
Management of patients with neurologic trauma Management of patients with neurologic trauma
Management of patients with neurologic trauma Periodontal treatment of medically compromised patients
Periodontal treatment of medically compromised patients Post hepatic jaundice
Post hepatic jaundice Post hepatic jaundice
Post hepatic jaundice Dose adjustment in renal and hepatic disease
Dose adjustment in renal and hepatic disease Prehepatic hepatic and posthepatic jaundice
Prehepatic hepatic and posthepatic jaundice Hepatic encephalopathy pathophysiology
Hepatic encephalopathy pathophysiology Hepatic extraction ratio
Hepatic extraction ratio Hepatic facies
Hepatic facies Exceptions to courvoisier law
Exceptions to courvoisier law Hepatic blood flow
Hepatic blood flow Tips hepatic
Tips hepatic Hepatic toxicity
Hepatic toxicity Ligamentum liver
Ligamentum liver Portal venule of the liver lobule
Portal venule of the liver lobule Half life of ast
Half life of ast Mild hepatic steatosis
Mild hepatic steatosis Encephalopathy stages
Encephalopathy stages Hepatic extraction ratio
Hepatic extraction ratio Zones of liver
Zones of liver Superior rectal artery is a branch of
Superior rectal artery is a branch of Type of jaundice
Type of jaundice Loading dose calculation example
Loading dose calculation example Portal vein
Portal vein Hepatic encephalopathy symptoms
Hepatic encephalopathy symptoms Encephalopathy stages
Encephalopathy stages Hepatic encaph
Hepatic encaph Anatomie cai biliare
Anatomie cai biliare Hepatic extraction ratio formula
Hepatic extraction ratio formula Hepatic s terre
Hepatic s terre Fissura interlobularis
Fissura interlobularis Diet hepatic encephalopathy
Diet hepatic encephalopathy Chronic liver desease
Chronic liver desease Types of venules
Types of venules Hepatic extraction ratio formula
Hepatic extraction ratio formula Adventicea
Adventicea Figure 11-7 veins labeled
Figure 11-7 veins labeled Chapter 11 the cardiovascular system figure 11-3
Chapter 11 the cardiovascular system figure 11-3 Post hepatic jaundice
Post hepatic jaundice Choledochlithotomy
Choledochlithotomy Transaminitis definition
Transaminitis definition Asterixis in hepatic encephalopathy
Asterixis in hepatic encephalopathy S.terre hepatic
S.terre hepatic Hepatic encephalopathy stages
Hepatic encephalopathy stages Right hepatic vein
Right hepatic vein Portal space liver
Portal space liver Hepatic blood flow
Hepatic blood flow Liver zone
Liver zone Intrahepatic biliary apparatus
Intrahepatic biliary apparatus Hepatic clearance formula
Hepatic clearance formula Figure 11-9 is a diagram of the hepatic portal circulation
Figure 11-9 is a diagram of the hepatic portal circulation Hepatic portal system
Hepatic portal system Hepatic blood flow
Hepatic blood flow Hepatic encephalopathy staging
Hepatic encephalopathy staging Encephalopathy stages
Encephalopathy stages S.terre hepatic
S.terre hepatic Dd jaundice
Dd jaundice S.terre hepatic
S.terre hepatic Pre-hepatic jaundice
Pre-hepatic jaundice Fructose
Fructose Hepatic portal vein.
Hepatic portal vein. Coelic plexus
Coelic plexus Ch 14 the digestive system and body metabolism
Ch 14 the digestive system and body metabolism The hepatic portal vein transports blood
The hepatic portal vein transports blood Hepatic flexure
Hepatic flexure Protoscolex
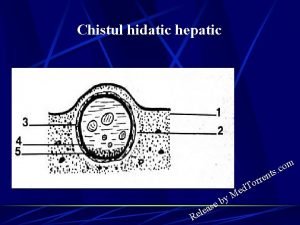
Protoscolex Hepatic veins
Hepatic veins Hepatic plexus
Hepatic plexus Lance uradomo
Lance uradomo Hepatopancreatic ampulla.
Hepatopancreatic ampulla. Cystic duct
Cystic duct Interior trunk
Interior trunk First pass effect drugs
First pass effect drugs S.terre hepatic
S.terre hepatic Lesser omentum
Lesser omentum Portal vein
Portal vein Capillaries function
Capillaries function Defecation
Defecation Figure 11-11 is a diagram of the hepatic portal circulation
Figure 11-11 is a diagram of the hepatic portal circulation Figure 11-8 arteries labeled
Figure 11-8 arteries labeled Hepatic impairment classification
Hepatic impairment classification Rosuvastatin tabletta
Rosuvastatin tabletta Liver cirrhosis stages
Liver cirrhosis stages Pancreatic juice
Pancreatic juice