MANAGEMENT OF PATIENTS AFTER RENAL TRANSPLANTATION Introduction Patients














- Slides: 40

MANAGEMENT OF PATIENTS AFTER RENAL TRANSPLANTATION
• • Introduction Patients who undergo renal transplant require complex care Diligent, multidisciplinary approach Knowledge of patient’s history pre-, during and post-transplant Surgeons, Nephrologist, consultants, PCP and allied health professional all work to direct transplantation efforts and adminster extremely detailed care.
Selection Criteria • Two essential questions that must be answered upfront. • The first is to the potential recipient : Why does the patient want a transplant? • The second is to the referring physician: Is the patient an appropriate transplant candidate?
Selection Criteria • Crucial to all discussions is the fact that transplantation is a treatment not a cure • The process requires long life commitment from both physicians and patients • Patients need to be realize the trade-offs, which for the vast majority of patients are worth it
Selection Criteria • Prior adherence to the medical and dialysis regimens • Ability to afford expensive medications, laboratory evaluations, and clinic visits • The Above two are very essential for a Successful Transplant process
Selection Criteria • Inclusion Criteria are ESRD or irreversible and progressive CKD with an e. GFR of <20 m. L/Min/1. 73 m 2 • Progressive CKD should be referred when the e. GFR is <30 m. L/Min/1. 73 m 2 for several reasons

Selection Criteria • Graft and patient survival advantage to receiving a “pre-emptive transplant” • Time on the wait list is a major determinant for receiving a kidney transplant • Dialysis is associated with progressive complications that may lead to the exclusion of consideration for kidney transplantation Kaplan B. Waiting time on dialysis as the strongest modifiable risk factor for renal transplant. Transplantation 2002; 74: 1377 -1381
Selection Criteria • Exclusion criteria are complex and involve multifaceted medical, social and ethical consideration • Current half life of a deceased donor graft is roughly nine years and for a living donor graft is approximately 12 years Lamb KE: Long-term renal allograft survival in the US. AM J Transplant 2011; 11: 450 -462
Selection Criteria • WHO Ethics Statement on transplantation, which was accepted by UNOS recommends that a potential candidate should not be considered for organ transplantation unless five-year survival rate is greater than 50% General principles for allocating human organs and tissues. Transplant Proc 1992; 24: 2227 -2235
Selection Criteria • This 5 year 50% life expectancy seems lenient given current graft survival rates, DWGF and CVD • Among Diabetic patients, CVD accounts for DWGF in 81%, however DWGF occurs in only 26% of transplant patients without DM. • 5 year 50% life expectancy should be waived when there is a possibility of living donation Cosio FG: Patient survival and cardiovascular risk after kidney transplantation: the challenge of diabetes. Am J Transplant 2008; 8: 593 -599

Pre-Transplant Evaluation • Careful review of past medical history • Age, gender, , cause of ESRD, previous transplant history • Dialysis modalities • Anuria, history of hematuria or proteinuria Venkat KK: Rapid resolution of proteinuria of native kidney origin following live donor transplantation. Am J Transplant 2005; 5: 351 -355
Pre-Transplant Evaluation Comorbid conditions Recurrent dialysis access thrombosis History of DVT, miscarriages. Endemic, occupational and social infection risks are important (Coccidio, toxo, ehrlichiosis). • Comprehensive physical examination • •
Pre-Transplant Evaluation • CV exam: carotids, femoral and peripheral pulses. • Much of what is used to direct our evaluation and management comes from the laboratory assessment

Table 1. Pre-Transplant Studies Blood Type, HLA type DSA (monthly sample once listed) CBC, CMP, Phosphorus, uric acid, lipid profile, hemoglobin A 1 C, PTH Infections studies-CMV, EBV, HSV, HIV, VZV, RPR, Hepatitis serology Immunization- Hepatitis B, Pneumococcal Annual testing while listed Adjunctive Testing Panorex to rule out abscesses EKG, Echo, Stress test+/- cardiac catheterization Carotids Doppler, CT angio of the iliac vessels CXR, PFT PAP, mammogram over 40, PSA over 40, colonoscopy over 50
The Transplant Procedure • • • Donor age, HLA mismatch, CMV EBV serostatus Induction agent, dose Surgeon, placement of urinary stent DGF, Serum creatinine at discharge
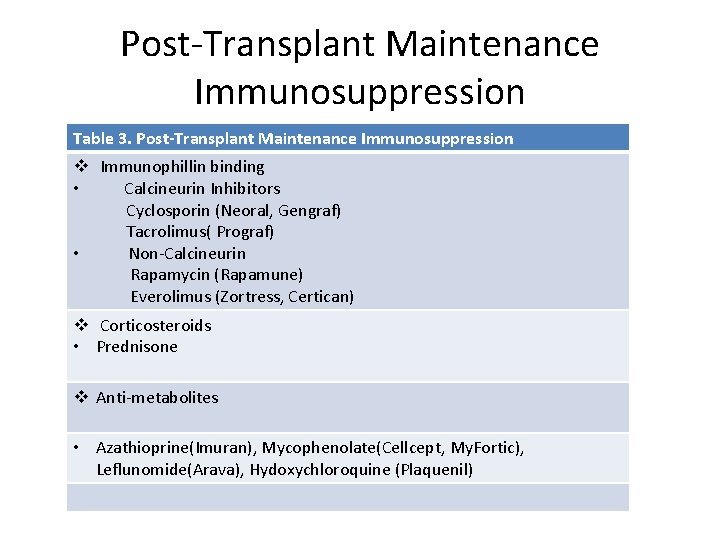
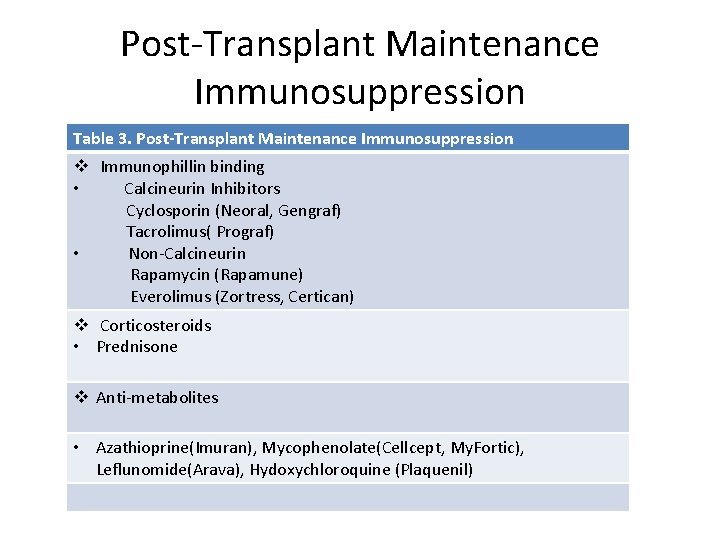
Post-Transplant Maintenance Immunosuppression Table 3. Post-Transplant Maintenance Immunosuppression v Immunophillin binding • Calcineurin Inhibitors Cyclosporin (Neoral, Gengraf) Tacrolimus( Prograf) • Non-Calcineurin Rapamycin (Rapamune) Everolimus (Zortress, Certican) v Corticosteroids • Prednisone v Anti-metabolites • Azathioprine(Imuran), Mycophenolate(Cellcept, My. Fortic), Leflunomide(Arava), Hydoxychloroquine (Plaquenil)
Post-Transplant Maintenance Immunosuppression v Controversies • Calcineurin inhibitors (CNI) or steroids withdrawal or avoidance • The use of mammalian targets of rapamycin(, TORs)
Post-Transplant Maintenance Immunosuppression • Induction – Thymo 5 mg/Kg total body weight IV with the first dose 1 mg/kg begun intraoperative followed by 2 mg/kg/d for two days – Dose is rounded to the nearest 25 mg, not adjusted to ideal body weight, no maximum dose

Post-Transplant Maintenance Immunosuppression • Tacrolimus – Begun on Postoperative day 1 or 2 even when DGF is present – Delayed introduction and failure to achieve a therapeutic CNI level by day 7 is associated with more rejection and no decrease in DGF – Target for a trough 7 -10 ng/m. L in the first 3 months and 3 -7 ng/m. L thereafter
Post-Transplant Maintenance Immunosuppression • Cyclosporine – Monitor peak (90 minutes levels) – C 2 levels are also interpretable – 800 -1200 ng/m. L in the first month then 400600 ng/m. L thereafter – Literature studies showing a level of 1000 ng/m. L provides 90% inhibition of lymphocytes and C 2 level of 400 with less rejection and less nephrotoxicity in cardiac transplant patients Varennes B: Clinical benefit of neoral dose monitoring with Cyclosporin 2 -hr post dose monitoring level compared with trough levels in stable heart transplant patients. Transplantation 1999; 68: 1839 -1842
Post-Transplant Maintenance Immunosuppression • MPA – 760 mg BID and reduce to 360 BID by postoperative day 5 – Drug-Drug interaction with Tacrolimus, Cyclosporine and PPI
Post-Transplant Maintenance Immunosuppression • Steroids – Methylprednisolone 7 mg /Kg intraoperatively followed by prednisone 1 mg/kg to a max of 80 mg on postoperative day 1, 2 – Then 20 mg per day during the first week, tapered by 5 mg/week to 5 mg/day by week 4 -5.

Post-Transplant Maintenance Immunosuppression • ELITE-Symphony trial – Compared cyclosporine, tacrolimus and rapamune – Best overall maintenance is the one using low dose tacrolimus, MMF and low dose steroids Ekberg H: Reduced exposure to calcineurin inhibitors in renal transplantation. N engl J Med 2007; 357: 2562 -2575
Post-Transplant Maintenance Immunosuppression • MYSS and MYSS following trials – Compared Imuran and MMF – NO difference in rejection, patient or graft survival – GFR was better long term with Imuran Remuzzi G: mycophenolate versus azathioprine for prevention of acute rejection in renal transplantation. Lancet 2004; 364: 503512

Post-Transplant Maintenance Immunosuppression • The current literature and available trials and regimens do not support steroid avoidance – Early withdrawal in a randomized, double blinded, placebo controlled trial with 5 year follow up comparing early withdrawal and low dose steroid showed no major differences in side effects but doubling of acute and chronic rejection rates in the early steroid withdrawal group
Post-Transplant Clinic Visits They are not routine care State the ‘Chief complaint’ Diagnostic code V 42. 0, V 58. 69 and V 58. 44 Historically, twice a week for the first month, monthly for six months, and then every 3 -4 months • That is no longer necessary or feasible • •
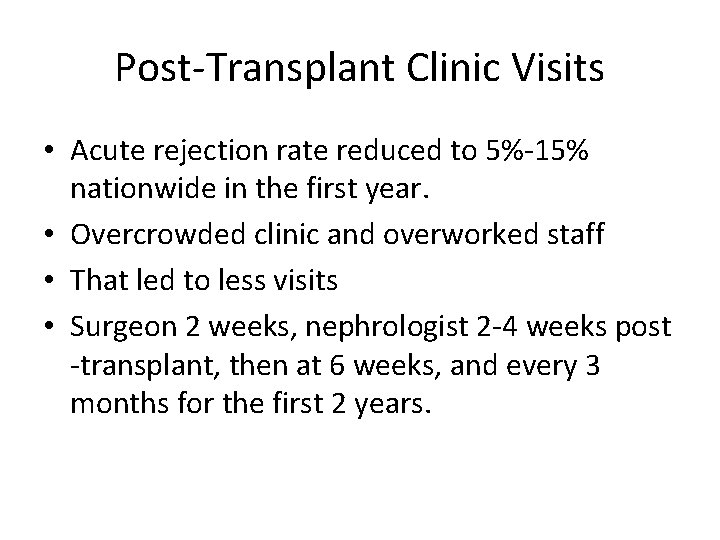
Post-Transplant Clinic Visits • Acute rejection rate reduced to 5%-15% nationwide in the first year. • Overcrowded clinic and overworked staff • That led to less visits • Surgeon 2 weeks, nephrologist 2 -4 weeks post -transplant, then at 6 weeks, and every 3 months for the first 2 years.

Post-Transplant Clinic Visits • Coordinate care with PCP and referring nephrologist so that the patients are seen every 3 -6 months

Post-Transplant Clinic Visits • Monitor for symptoms that might dictate a change in IS regimen beyond what might have been suggested by laboratory monitoring – HTN, insomnia, tremor, GI complications, etc. – Detailed drug history every visit
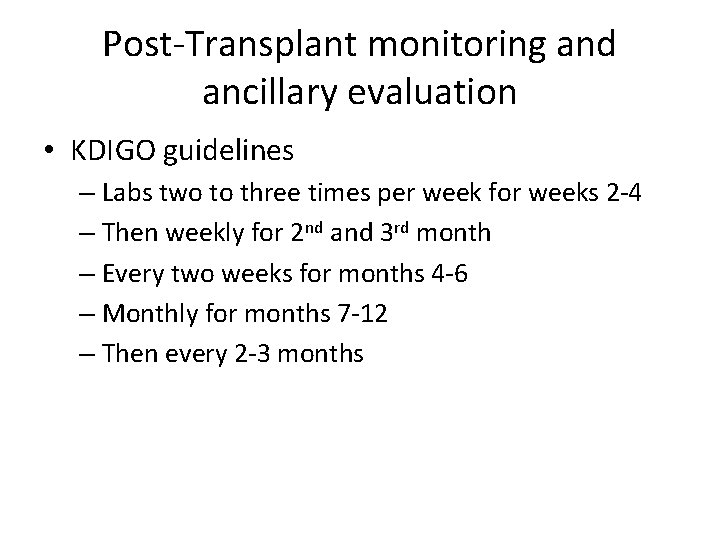
Post-Transplant monitoring and ancillary evaluation • KDIGO guidelines – Labs two to three times per week for weeks 2 -4 – Then weekly for 2 nd and 3 rd month – Every two weeks for months 4 -6 – Monthly for months 7 -12 – Then every 2 -3 months
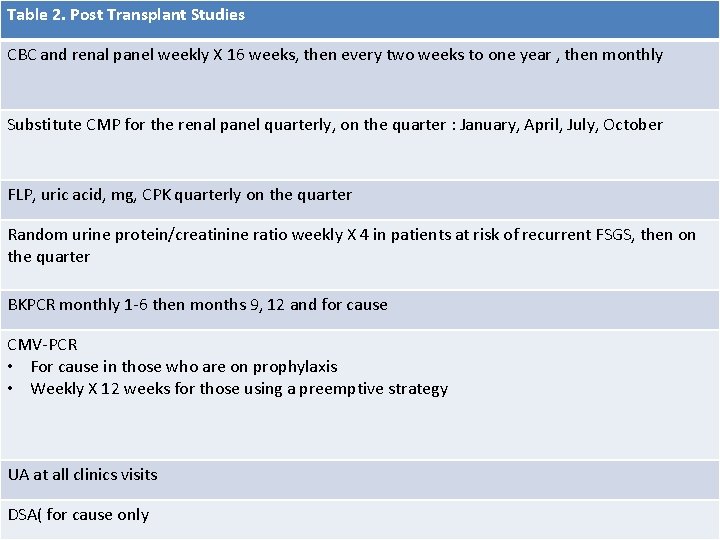
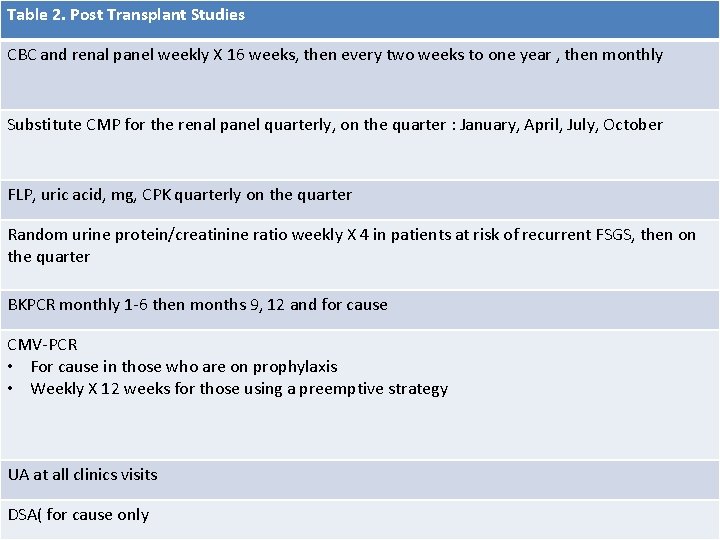
Table 2. Post Transplant Studies CBC and renal panel weekly X 16 weeks, then every two weeks to one year , then monthly Substitute CMP for the renal panel quarterly, on the quarter : January, April, July, October FLP, uric acid, mg, CPK quarterly on the quarter Random urine protein/creatinine ratio weekly X 4 in patients at risk of recurrent FSGS, then on the quarter BKPCR monthly 1 -6 then months 9, 12 and for cause CMV-PCR • For cause in those who are on prophylaxis • Weekly X 12 weeks for those using a preemptive strategy UA at all clinics visits DSA( for cause only

Virological Monitoring • CMV – Unnecessary during prophylaxis period with valganciclovir – Affordability/preemptive treatment: Weekly CMVPCR for the first 12 weeks – CMV infection mostly in the first 3 months – Diligent preemptive approach has been shown to be as cost-effective as prophylaxis

Virological Monitoring • EBV – Not recommended and no consensus – Interpretation , sensitivity and specificity are complicated for PTLD or EBV-associated disease

Virological Monitoring • BK virus – Serum PCR monthly for 6 months – At month 9, 12 – For cause – Viruria is very uncommon in the absence of viremia – Incidence increases by post transplant 3 rd month, plateaus by 6 th month
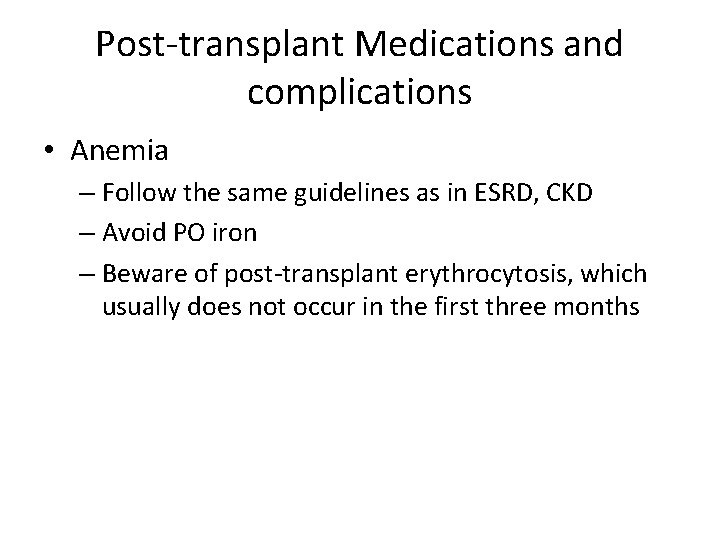
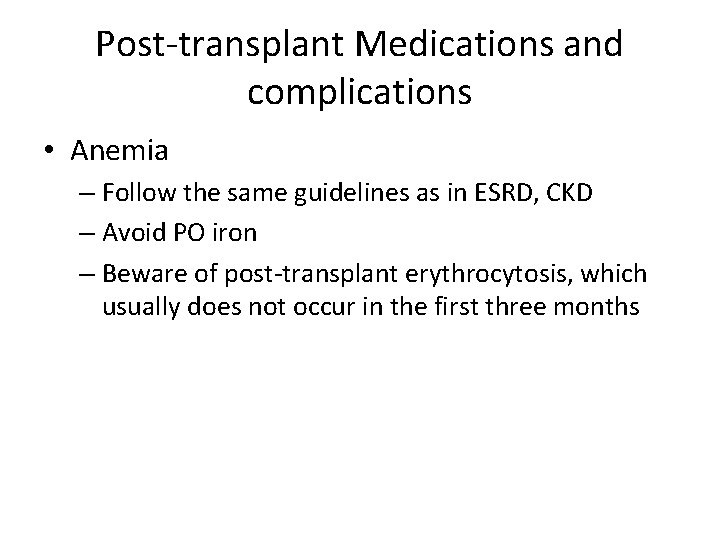
Post-transplant Medications and complications • Anemia – Follow the same guidelines as in ESRD, CKD – Avoid PO iron – Beware of post-transplant erythrocytosis, which usually does not occur in the first three months
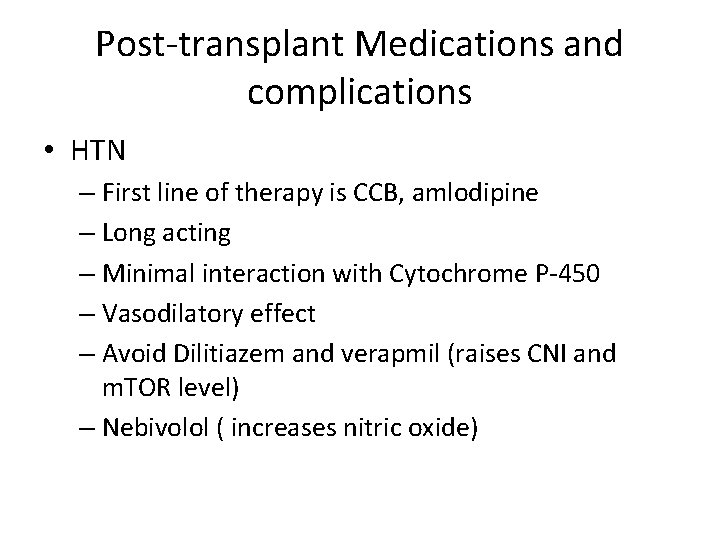
Post-transplant Medications and complications • HTN – First line of therapy is CCB, amlodipine – Long acting – Minimal interaction with Cytochrome P-450 – Vasodilatory effect – Avoid Dilitiazem and verapmil (raises CNI and m. TOR level) – Nebivolol ( increases nitric oxide)
Post-transplant Medications and complications • HTN – ACE I or ARB if LVH +/- CAD – Delay until after the third month
Post-transplant Medications and complications • Dyslipidemia – Fluvastatin is preferred – Less MACE – FDA warning, contraindicating the use of simvastatin with cyclosporin but not tacrolimus and not to exceed 20 mg dose with concomitant amlodipine

Post-transplant Medications and complications • Fever – Mostly of bacterial origin, UTI, pneumonia – Admission for fever >102 F – Pan culture, CMV-PCR, BK-PCR – Cipro/Azithromycin – Bacterial infection, no change in IS regimen unless life threatening – Stop antimetabolites for CMV or BK

Conclusion • Transplant management is complex • It requires diligence and communication among the patient, the transplant center, and other treating physicians and allied health care personnel • It is hard work that is necessary but very rewarding
 Res extra commercium
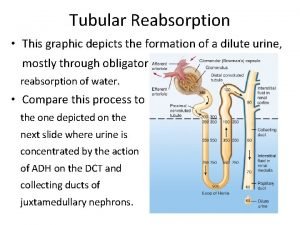
Res extra commercium Teoria do nefron intacto
Teoria do nefron intacto Vasa recta vs peritubular capillaries
Vasa recta vs peritubular capillaries After me after me after me
After me after me after me John 14:1
John 14:1 Bone marrow transplantation sri lanka
Bone marrow transplantation sri lanka Law of transplantation
Law of transplantation Patrick evrard mont godinne
Patrick evrard mont godinne Cultural transposition
Cultural transposition Transplant
Transplant Stem cell phuket
Stem cell phuket Introduction of lifting and transferring of patients
Introduction of lifting and transferring of patients Lippincott williams
Lippincott williams Management of patients with neurologic trauma
Management of patients with neurologic trauma Periodontal treatment of medically compromised patients
Periodontal treatment of medically compromised patients After the introduction
After the introduction Apple objectives
Apple objectives Renal medulla
Renal medulla Pacr course uwe
Pacr course uwe Renal angle
Renal angle Filtration fraction
Filtration fraction Urolith
Urolith Signo de puño percusion
Signo de puño percusion Naphthylamine
Naphthylamine اعادة الامتصاص في الكلية
اعادة الامتصاص في الكلية Lamivudine renal dose
Lamivudine renal dose What is the vasa recta
What is the vasa recta Earthy look in chronic renal failure
Earthy look in chronic renal failure Posicion de naegeli
Posicion de naegeli Causes of secondary hyperparathyroidism
Causes of secondary hyperparathyroidism First order drug elimination
First order drug elimination Clearance equation renal
Clearance equation renal Renal
Renal Lovenox renal dosing
Lovenox renal dosing Urinalysis
Urinalysis Fosa iliaca derecha
Fosa iliaca derecha Respiratory alkalosis renal compensation
Respiratory alkalosis renal compensation Kidney lobule
Kidney lobule Glitol
Glitol Acidosis metabolica y acidosis respiratoria
Acidosis metabolica y acidosis respiratoria Respiratory alkalosis renal compensation
Respiratory alkalosis renal compensation