ACUTE LIVER FAILURE Fulminant hepatic failure acute liver


- Slides: 27
ACUTE LIVER FAILURE
Fulminant hepatic failure (acute liver failure) is a clinical syndrome resulting from massive necrosis of hepatocytes or from severe functional impairment of hepatocytes. Synthetic, excretory, metabolic, protective and detoxifying functions of the liver are all severely impaired. .
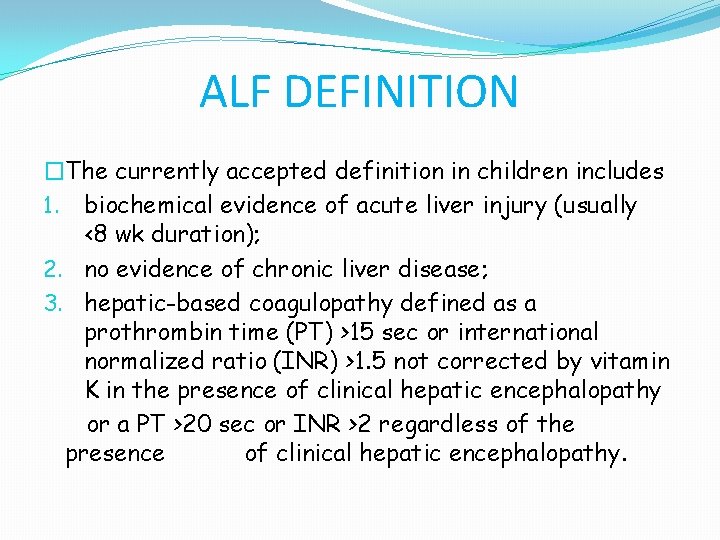
ALF DEFINITION �The currently accepted definition in children includes 1. biochemical evidence of acute liver injury (usually <8 wk duration); 2. no evidence of chronic liver disease; 3. hepatic-based coagulopathy
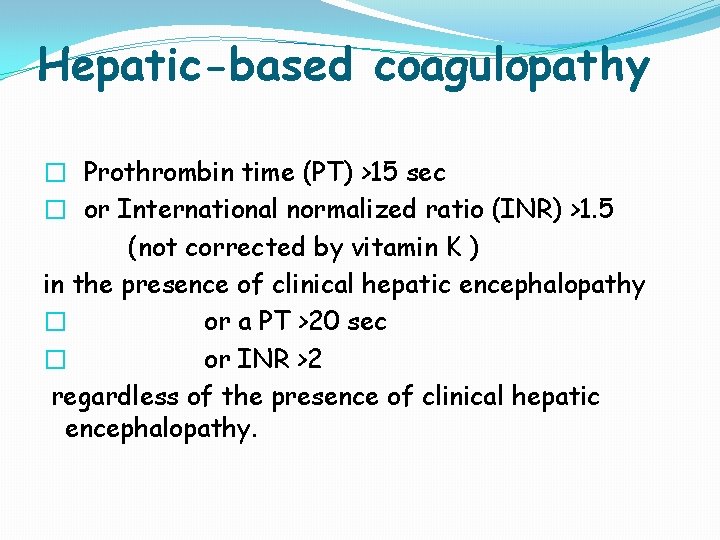
Hepatic-based coagulopathy � Prothrombin time (PT) >15 sec � or International normalized ratio (INR) >1. 5 (not corrected by vitamin K ) in the presence of clinical hepatic encephalopathy � or a PT >20 sec � or INR >2 regardless of the presence of clinical hepatic encephalopathy.
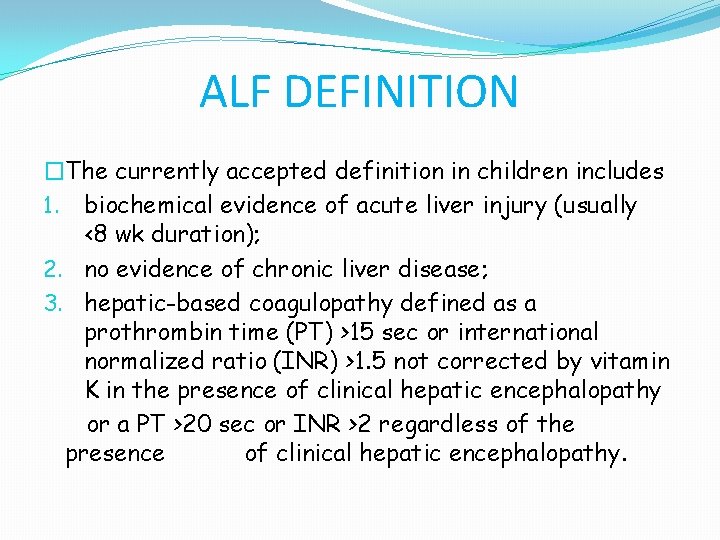
ALF DEFINITION �The currently accepted definition in children includes 1. biochemical evidence of acute liver injury (usually <8 wk duration); 2. no evidence of chronic liver disease; 3. hepatic-based coagulopathy defined as a prothrombin time (PT) >15 sec or international normalized ratio (INR) >1. 5 not corrected by vitamin K in the presence of clinical hepatic encephalopathy or a PT >20 sec or INR >2 regardless of the presence of clinical hepatic encephalopathy.
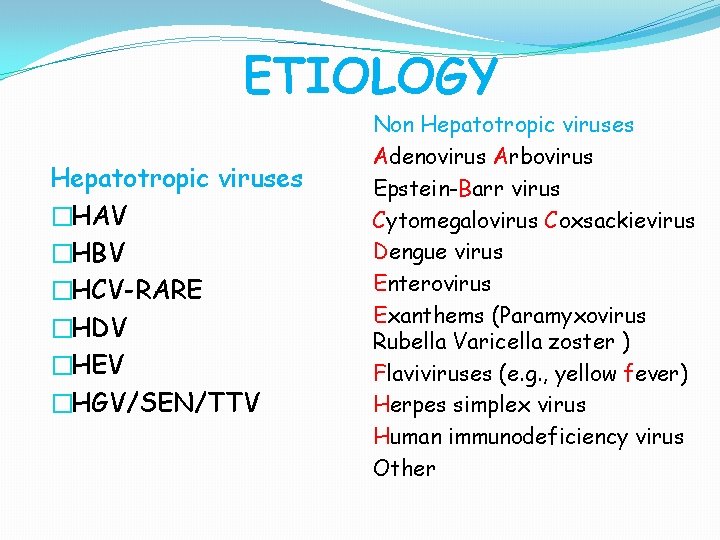
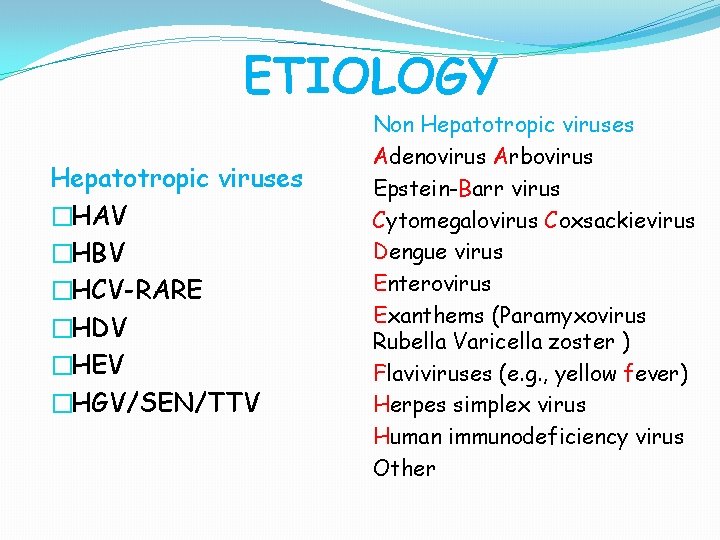
ETIOLOGY Hepatotropic viruses �HAV �HBV �HCV-RARE �HDV �HEV �HGV/SEN/TTV Non Hepatotropic viruses Adenovirus Arbovirus Epstein-Barr virus Cytomegalovirus Coxsackievirus Dengue virus Enterovirus Exanthems (Paramyxovirus Rubella Varicella zoster ) Flaviviruses (e. g. , yellow fever) Herpes simplex virus Human immunodeficiency virus Other
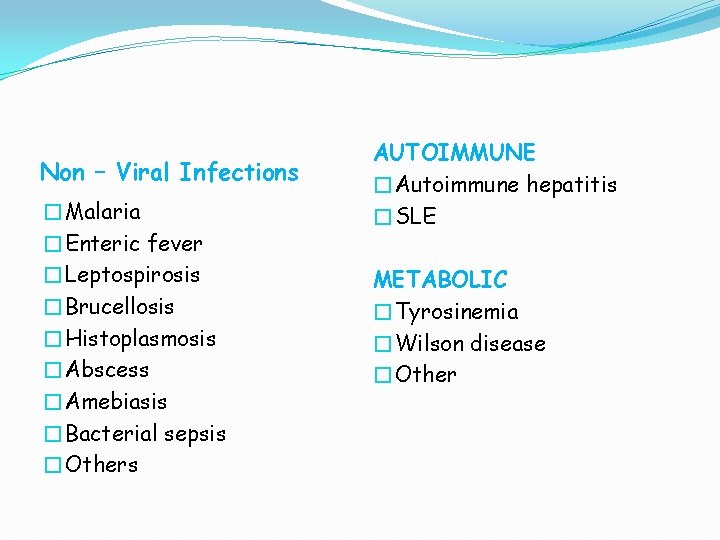
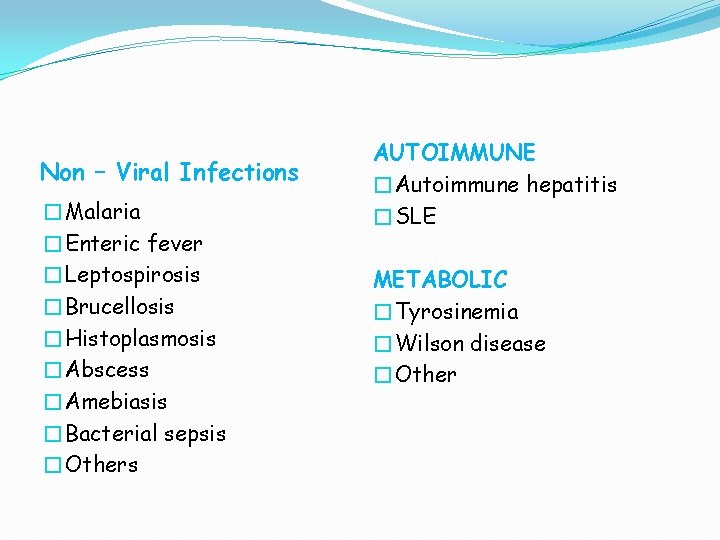
Non – Viral Infections �Malaria �Enteric fever �Leptospirosis �Brucellosis �Histoplasmosis �Abscess �Amebiasis �Bacterial sepsis �Others AUTOIMMUNE �Autoimmune hepatitis �SLE METABOLIC �Tyrosinemia �Wilson disease �Other
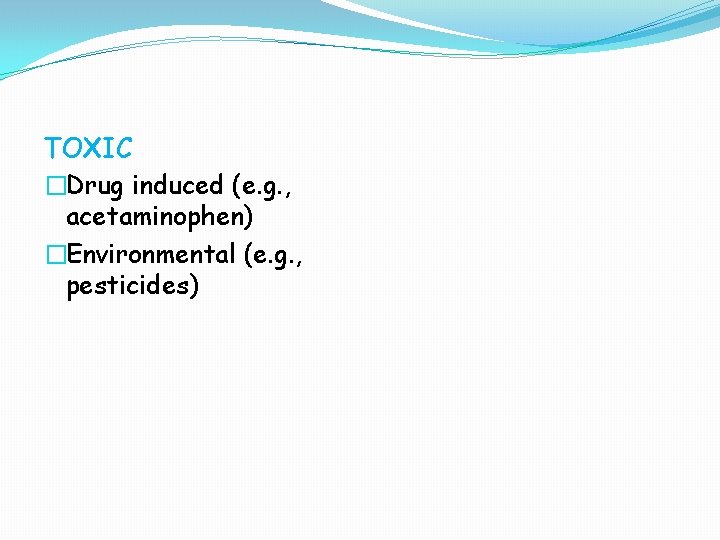
TOXIC �Drug induced (e. g. , acetaminophen) �Environmental (e. g. , pesticides)
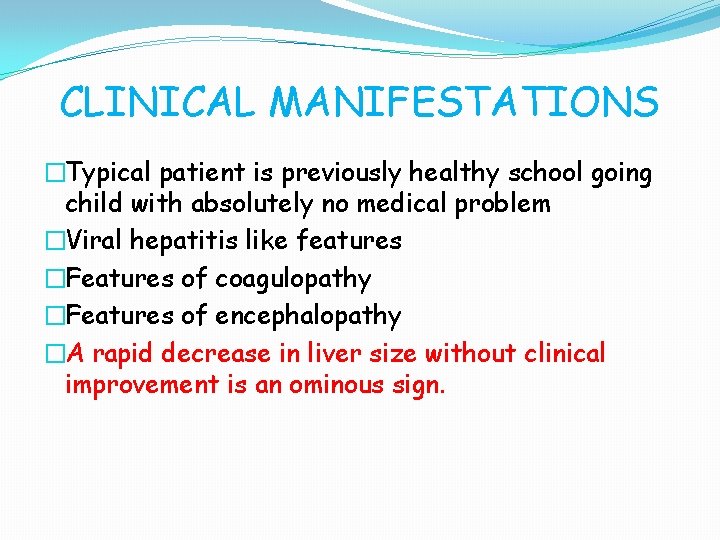
CLINICAL MANIFESTATIONS �Typical patient is previously healthy school going child with absolutely no medical problem �Viral hepatitis like features �Features of coagulopathy �Features of encephalopathy �A rapid decrease in liver size without clinical improvement is an ominous sign.
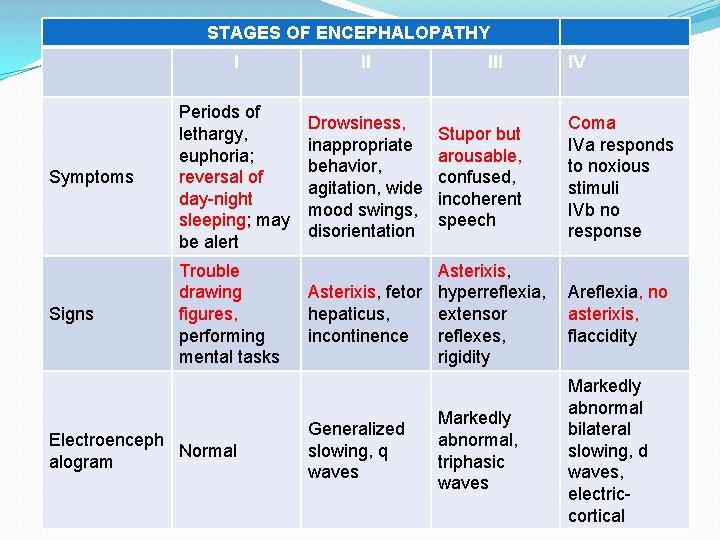
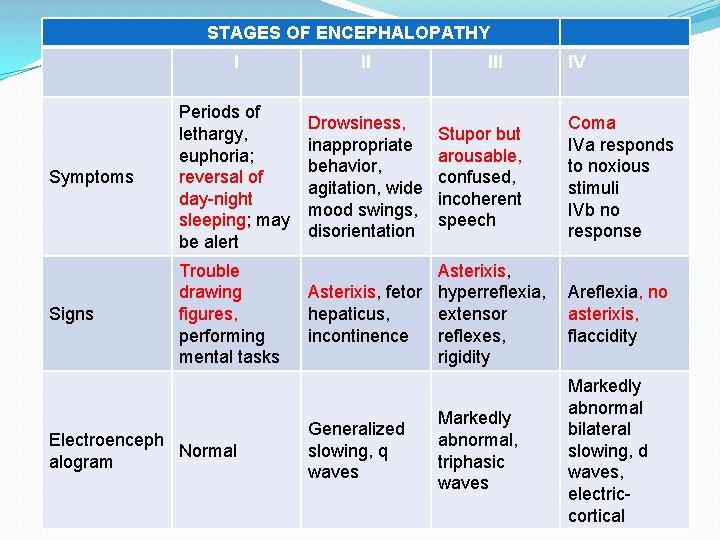
STAGES OF ENCEPHALOPATHY I II Symptoms Periods of lethargy, euphoria; reversal of day-night sleeping; may be alert Drowsiness, inappropriate behavior, agitation, wide mood swings, disorientation Signs Trouble drawing figures, performing mental tasks Asterixis, fetor hyperreflexia, Areflexia, no extensor hepaticus, asterixis, incontinence reflexes, flaccidity rigidity Electroenceph Normal alogram Generalized slowing, q waves III Stupor but arousable, confused, incoherent speech Markedly abnormal, triphasic waves IV Coma IVa responds to noxious stimuli IVb no response Markedly abnormal bilateral slowing, d waves, electriccortical

When to suspect ALF �Persistent anorexia �Persistent vomiting �Deepening jaundice �Decreasing liver span �Development of ascites �Bleeding manifestations �Neuropsychiatric symptoms
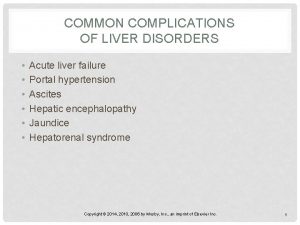
COMPLICATIONS �Hepatic encephalopathy �Cerebral edema �Coagulopathy �Electrolyte imbalance �Metabolic acidosis �Hypoglycemia �Infections
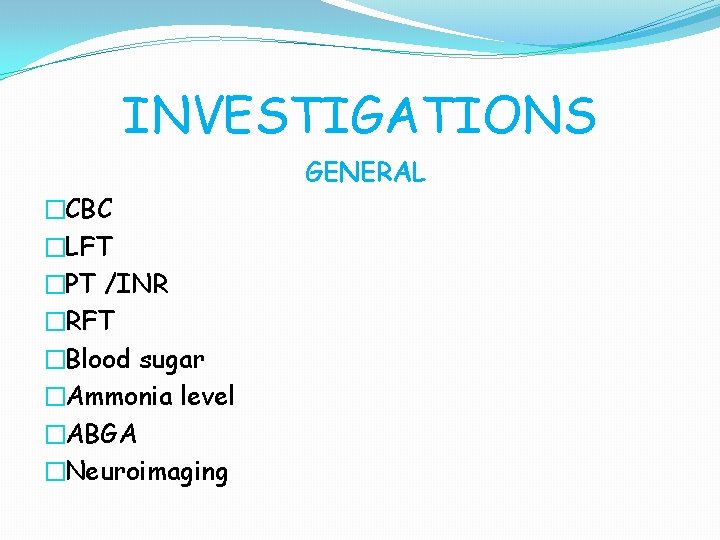
INVESTIGATIONS GENERAL �CBC �LFT �PT /INR �RFT �Blood sugar �Ammonia level �ABGA �Neuroimaging
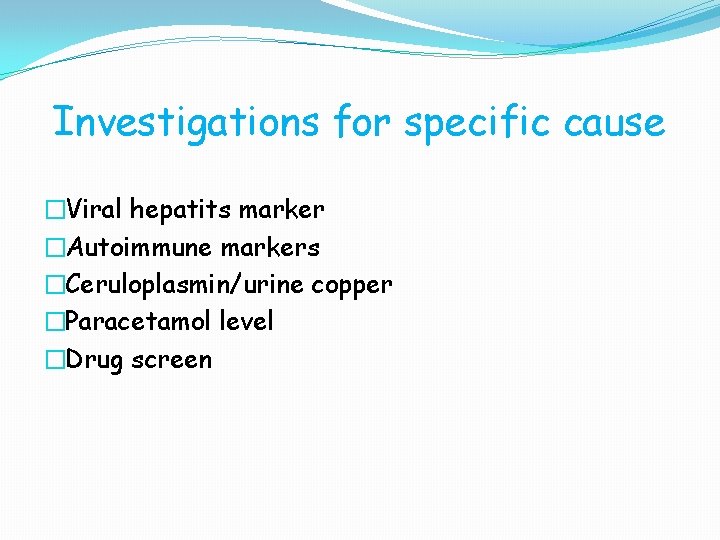
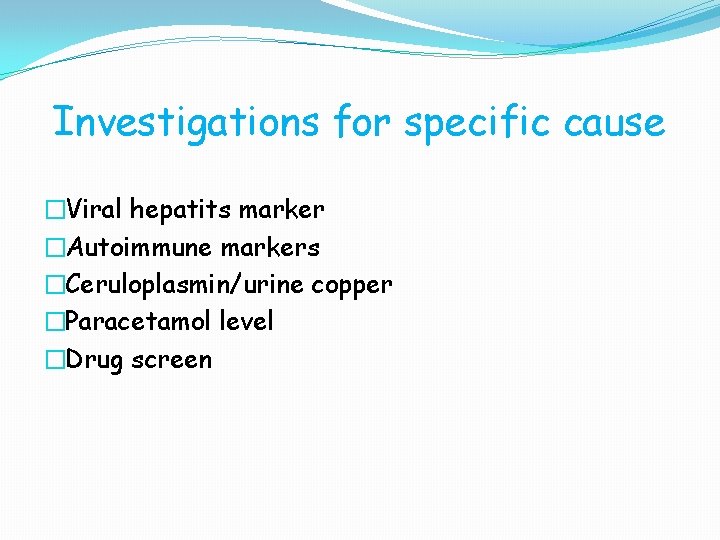
Investigations for specific cause �Viral hepatits marker �Autoimmune markers �Ceruloplasmin/urine copper �Paracetamol level �Drug screen
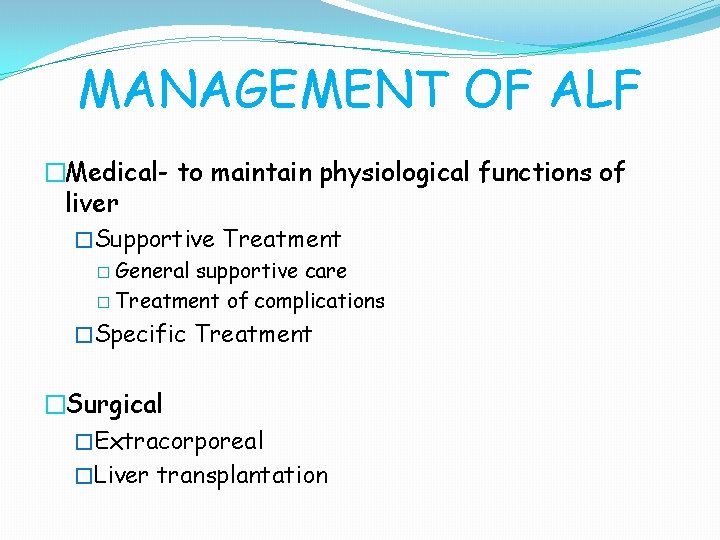
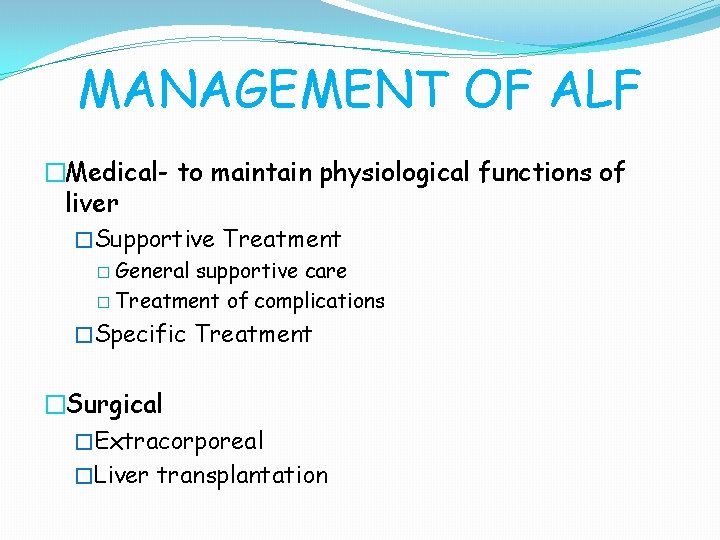
MANAGEMENT OF ALF �Medical- to maintain physiological functions of liver �Supportive Treatment � General supportive care � Treatment of complications �Specific Treatment �Surgical �Extracorporeal �Liver transplantation
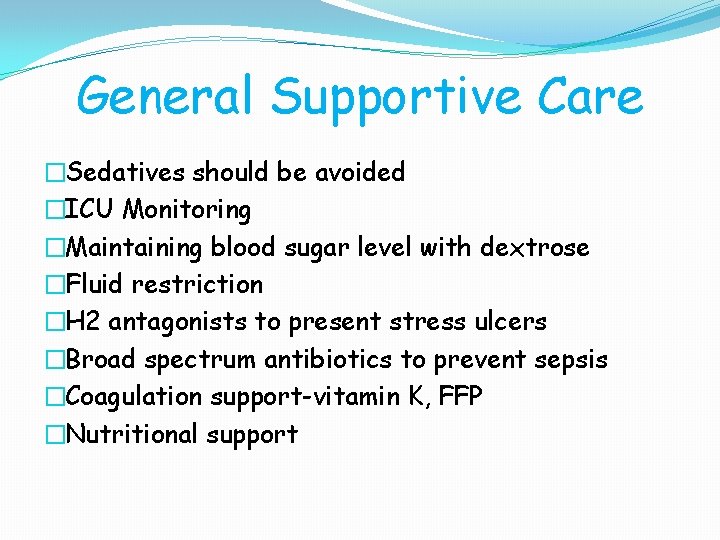
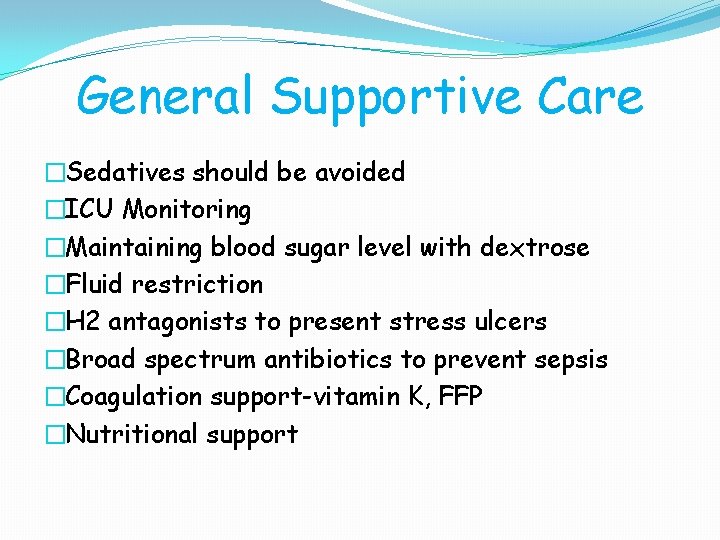
General Supportive Care �Sedatives should be avoided �ICU Monitoring �Maintaining blood sugar level with dextrose �Fluid restriction �H 2 antagonists to present stress ulcers �Broad spectrum antibiotics to prevent sepsis �Coagulation support-vitamin K, FFP �Nutritional support

Prevention and treatment of complications
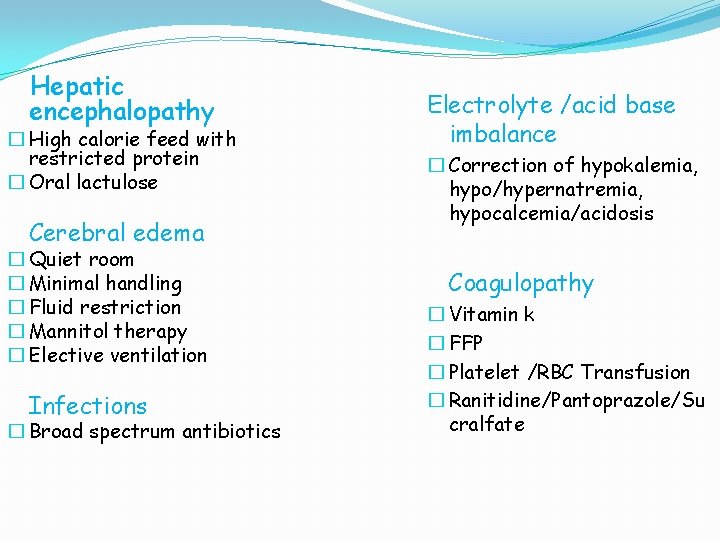
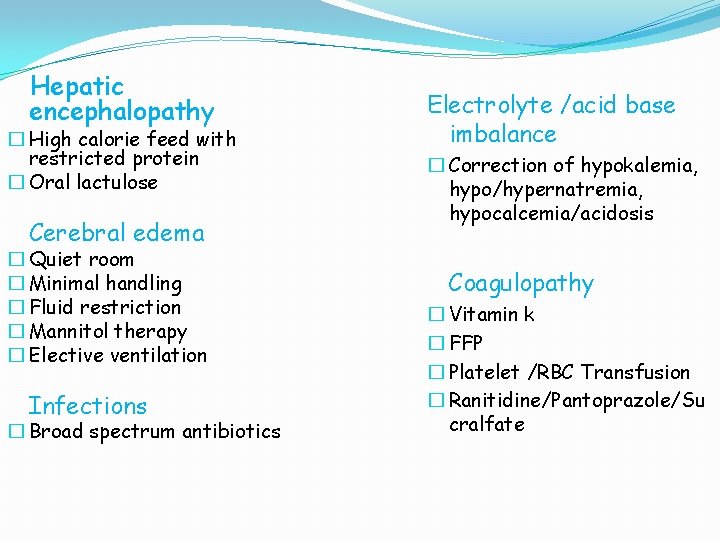
Hepatic encephalopathy � High calorie feed with restricted protein � Oral lactulose Cerebral edema � Quiet room � Minimal handling � Fluid restriction � Mannitol therapy � Elective ventilation Infections � Broad spectrum antibiotics Electrolyte /acid base imbalance � Correction of hypokalemia, hypo/hypernatremia, hypocalcemia/acidosis Coagulopathy � Vitamin k � FFP � Platelet /RBC Transfusion � Ranitidine/Pantoprazole/Su cralfate
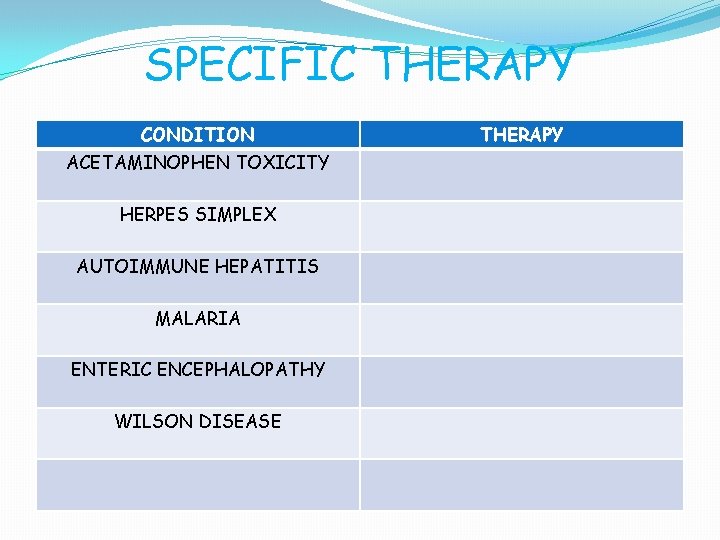
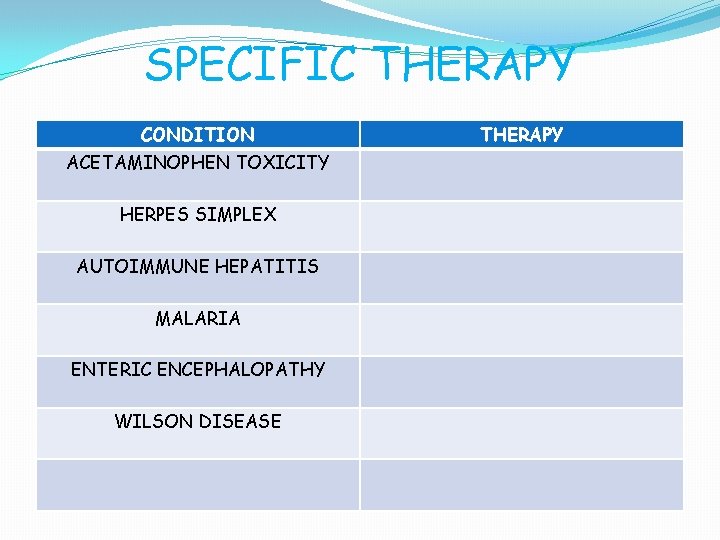
SPECIFIC THERAPY CONDITION ACETAMINOPHEN TOXICITY HERPES SIMPLEX AUTOIMMUNE HEPATITIS MALARIA ENTERIC ENCEPHALOPATHY WILSON DISEASE THERAPY
SURGICAL �Biologic liver support devices �Liver transplantation
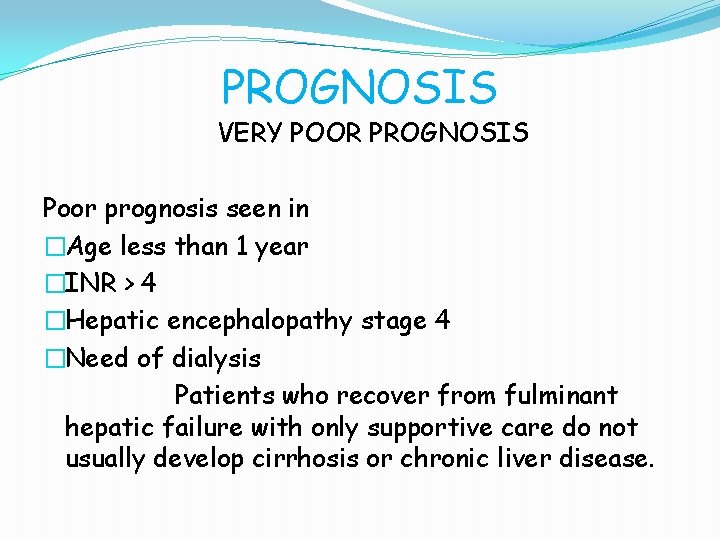
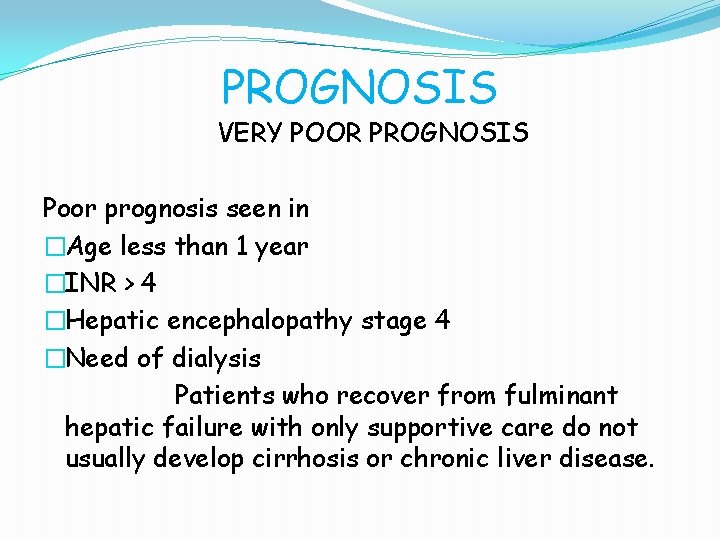
PROGNOSIS VERY POOR PROGNOSIS Poor prognosis seen in �Age less than 1 year �INR > 4 �Hepatic encephalopathy stage 4 �Need of dialysis Patients who recover from fulminant hepatic failure with only supportive care do not usually develop cirrhosis or chronic liver disease.
�Hepatic encephalopathy is aggravated by all except �HYPERKALEMIA �ANEMIA �HYPOTHYROIDISM �BARBITURATES
�NAME OF CELLS IN BRAIN SEEN IN HEPATIC ENCEPHALOPATHY
�WHICH ONE IS NOT ADVOCATED IN MANAGEMENT OF HEPATIC ENCEPHALOPATHY �ORAL LACTULOSE �I. V. GLUCOSE �HIGH PROTEIN DIET �COLONIC WASHOUT
�NUMBER CONNECTION TEST
�Liver failure in the perinatal period can be associated with prenatal liver injury and even cirrhosis. Examples include neonatal iron storage (hemochromatosis) disease, tyrosinemia, and some cases of congenital viral infection. Liver disease may be noticed at birth or after several days of apparent well-being. �Fulminant Wilson disease also occurs in older children who were previously asymptomatic but, by definition, have pre-existing liver disease. �In some cases of liver failure, particularly in the idiopathic form of acute hepatic failure, the onset of encephalopathy occurs later, from 8 to 28 wk after the onset of jaundice.
 Fulminant hepatit
Fulminant hepatit Transaminitis definition
Transaminitis definition Acute liver failure criteria
Acute liver failure criteria Alain sauvage
Alain sauvage Mink digestive system
Mink digestive system Liversoc
Liversoc Acg pregnancy
Acg pregnancy Acute fatty liver of pregnancy
Acute fatty liver of pregnancy Ascites veins
Ascites veins Hepatic encephalopathy treatment guidelines
Hepatic encephalopathy treatment guidelines Acute vs chronic heart failure
Acute vs chronic heart failure Acute brain failure
Acute brain failure Urinalysis
Urinalysis Cup and cone fracture ductile or brittle
Cup and cone fracture ductile or brittle Failure to sense
Failure to sense Capture beat
Capture beat S.terre hepatic
S.terre hepatic Function of ruminant stomach
Function of ruminant stomach Hepatic extraction ratio formula
Hepatic extraction ratio formula Foramen of winslow boundaries
Foramen of winslow boundaries Diet for hepatitis c
Diet for hepatitis c Rennin
Rennin Hepatic veins
Hepatic veins Encephalopathy stages
Encephalopathy stages Obstructive jaundice lab diagnosis
Obstructive jaundice lab diagnosis Half life of ast
Half life of ast Hepatic clearance formula
Hepatic clearance formula Obstructive jaundice bilirubin
Obstructive jaundice bilirubin