Hepatic encephalopathy Portalsystemic encephalopathy hepatic coma 1 Hepatic
- Slides: 15
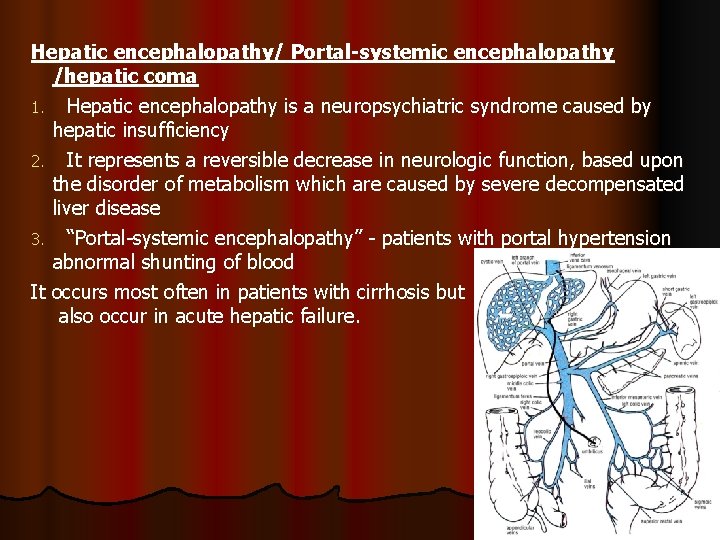
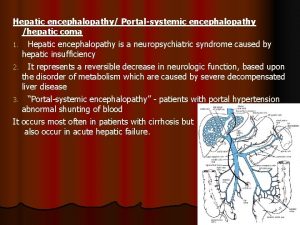
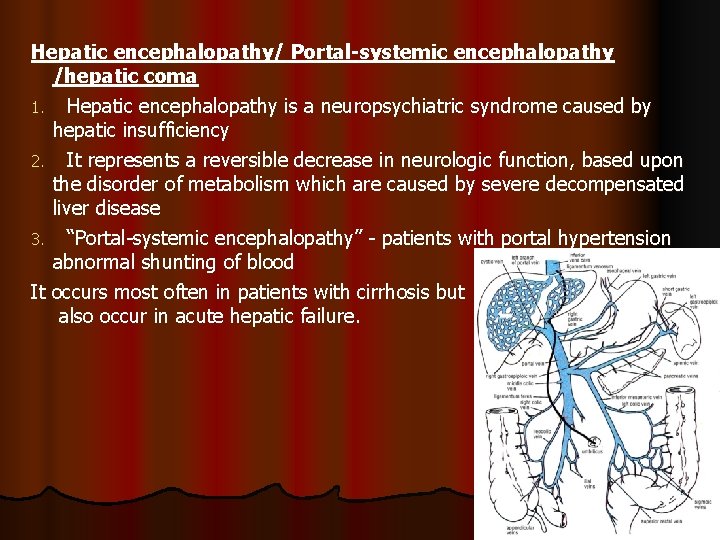
Hepatic encephalopathy/ Portal-systemic encephalopathy /hepatic coma 1. Hepatic encephalopathy is a neuropsychiatric syndrome caused by hepatic insufficiency 2. It represents a reversible decrease in neurologic function, based upon the disorder of metabolism which are caused by severe decompensated liver disease 3. “Portal-systemic encephalopathy” - patients with portal hypertension abnormal shunting of blood It occurs most often in patients with cirrhosis but also occur in acute hepatic failure.
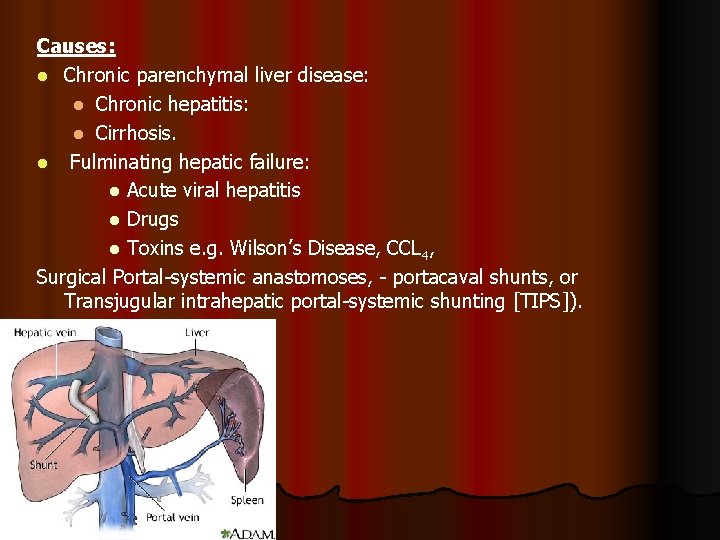
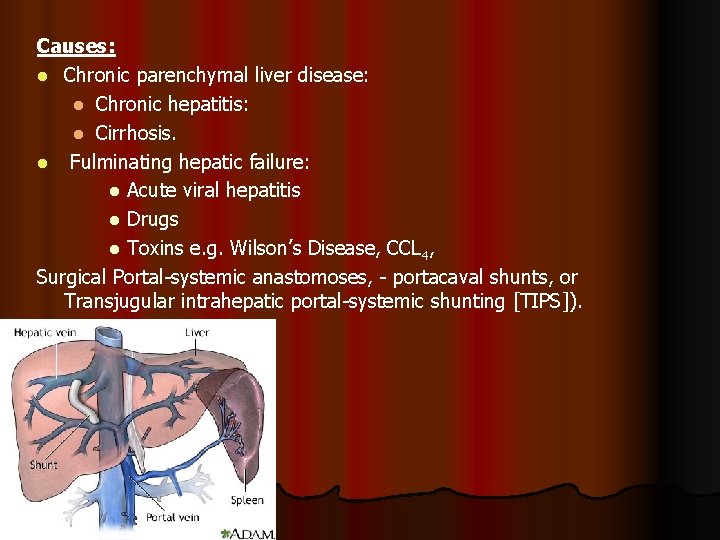
Causes: l Chronic parenchymal liver disease: l Chronic hepatitis: l Cirrhosis. l Fulminating hepatic failure: l Acute viral hepatitis l Drugs l Toxins e. g. Wilson’s Disease, CCL 4, Surgical Portal-systemic anastomoses, - portacaval shunts, or Transjugular intrahepatic portal-systemic shunting [TIPS]).
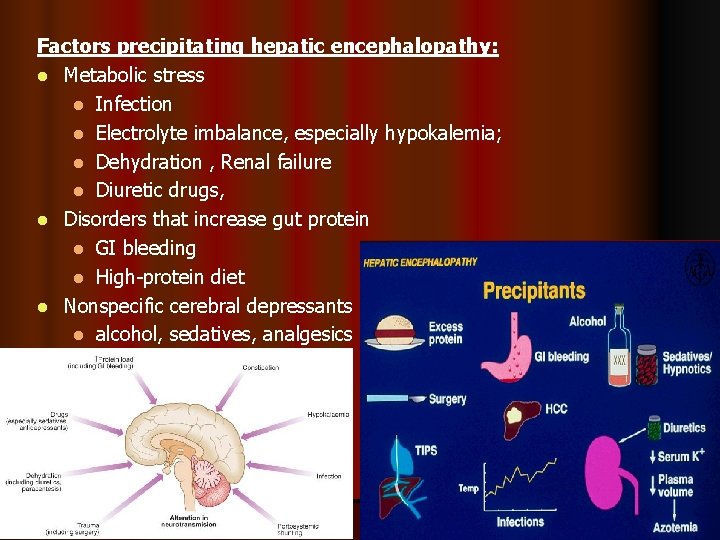
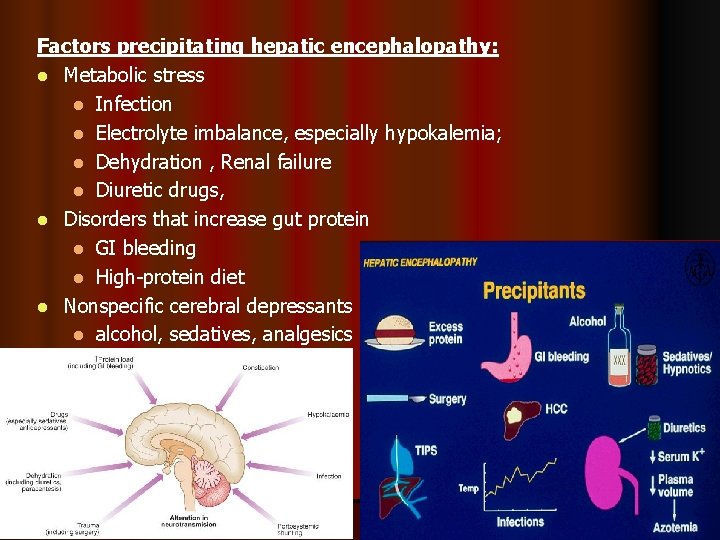
Factors precipitating hepatic encephalopathy: l Metabolic stress l Infection l Electrolyte imbalance, especially hypokalemia; l Dehydration , Renal failure l Diuretic drugs, l Disorders that increase gut protein l GI bleeding l High-protein diet l Nonspecific cerebral depressants l alcohol, sedatives, analgesics
Pathogenesis l Absorbed products – detoxified in Liver l PSS – toxic substances enter systemic circulation - Which are toxic to brain Other factors l Increase sensitivity to GABA (inhibitory neurotransmitter) l Increase circulating levels of endogenous benzodiazepines
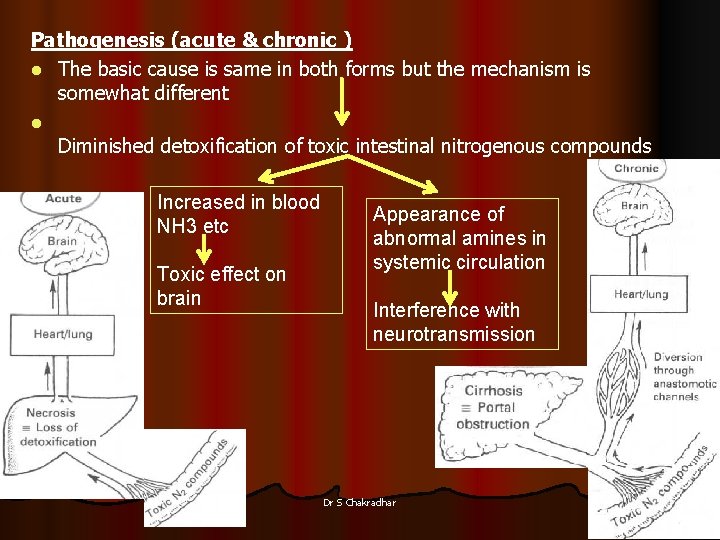
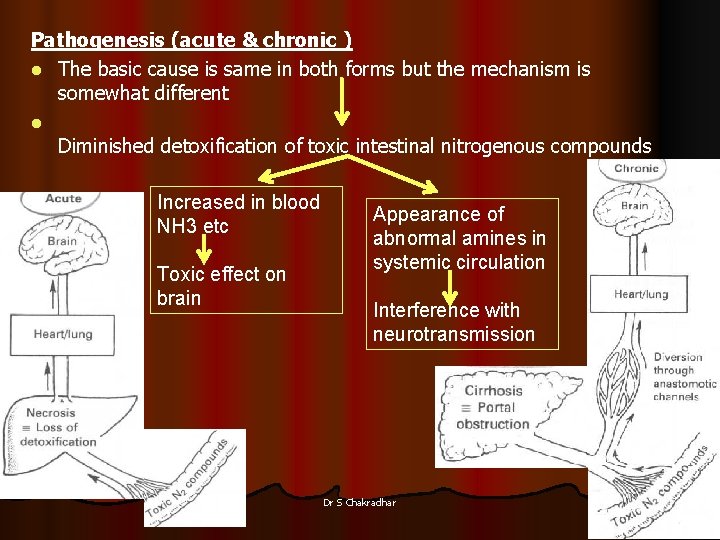
Pathogenesis (acute & chronic ) l The basic cause is same in both forms but the mechanism is somewhat different l Diminished detoxification of toxic intestinal nitrogenous compounds Increased in blood NH 3 etc Toxic effect on brain Appearance of abnormal amines in systemic circulation Interference with neurotransmission Dr S Chakradhar 5
Endotoxins of HE l Ammonia • Mercaptans - degradation of methionine in the gut l Phenols l Free fatty acids
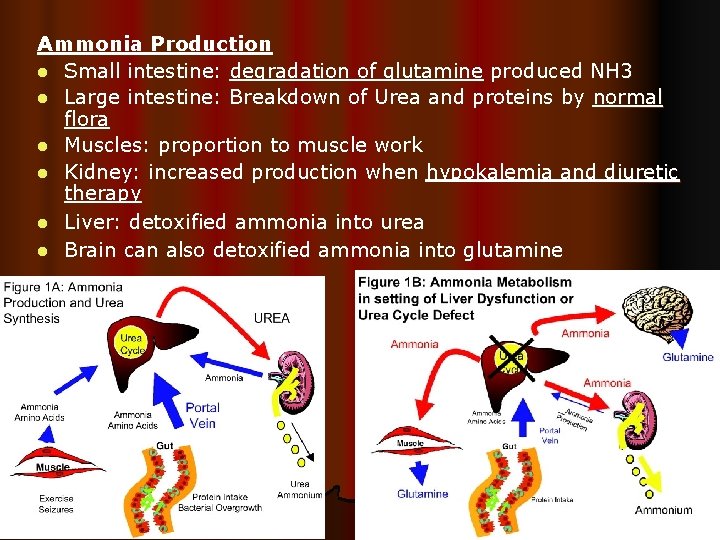
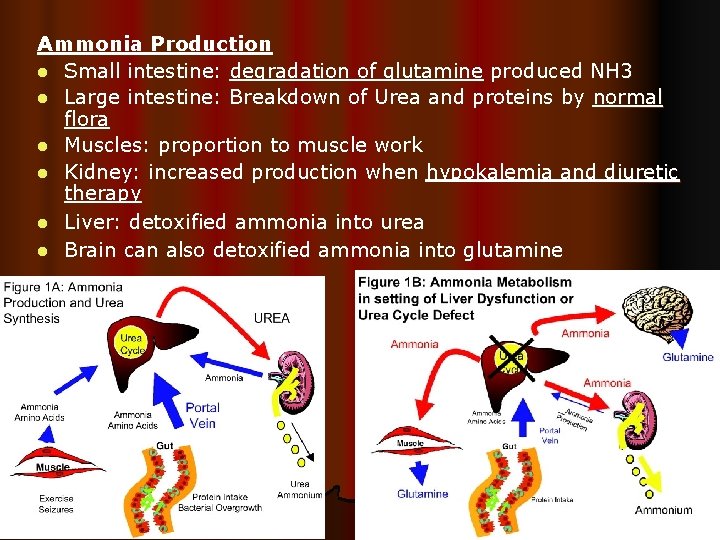
Ammonia Production l Small intestine: degradation of glutamine produced NH 3 l Large intestine: Breakdown of Urea and proteins by normal flora l Muscles: proportion to muscle work l Kidney: increased production when hypokalemia and diuretic therapy l Liver: detoxified ammonia into urea l Brain can also detoxified ammonia into glutamine
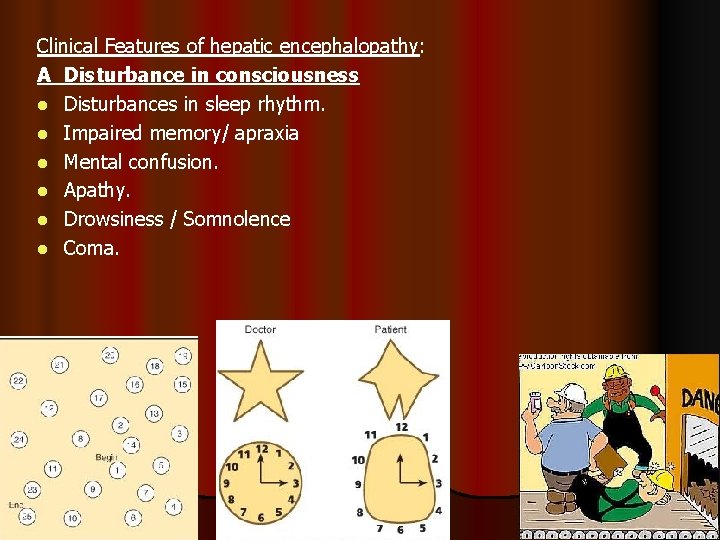
Clinical Features of hepatic encephalopathy: A Disturbance in consciousness l Disturbances in sleep rhythm. l Impaired memory/ apraxia l Mental confusion. l Apathy. l Drowsiness / Somnolence l Coma.
B. Changes Personality l Childish behavior. l May be aggressive out burst. l Euphoric. l Foetor hepaticus – Foul–smelling breath associated with liver disease due to mercaptans
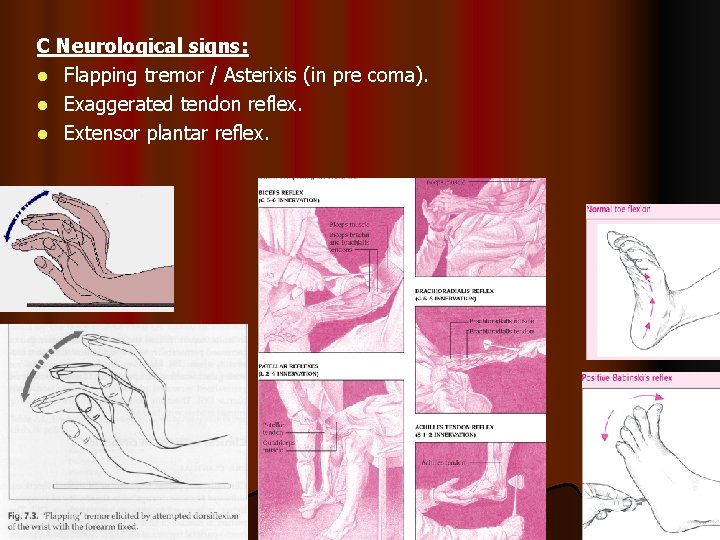
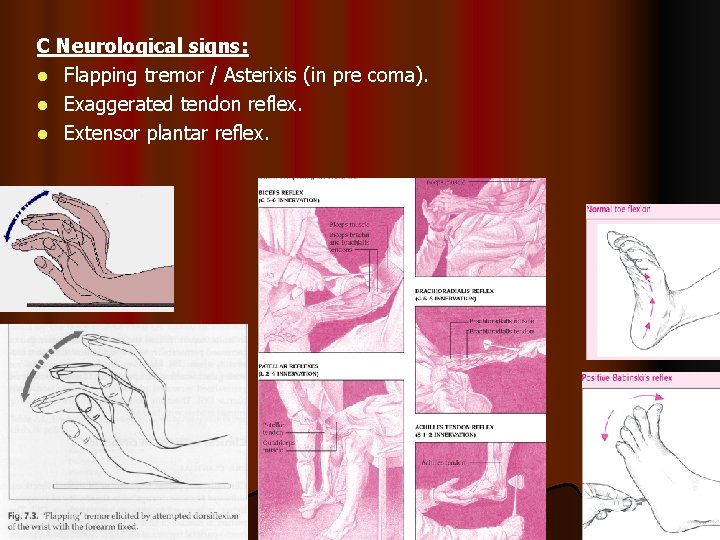
C Neurological signs: l Flapping tremor / Asterixis (in pre coma). l Exaggerated tendon reflex. l Extensor plantar reflex.
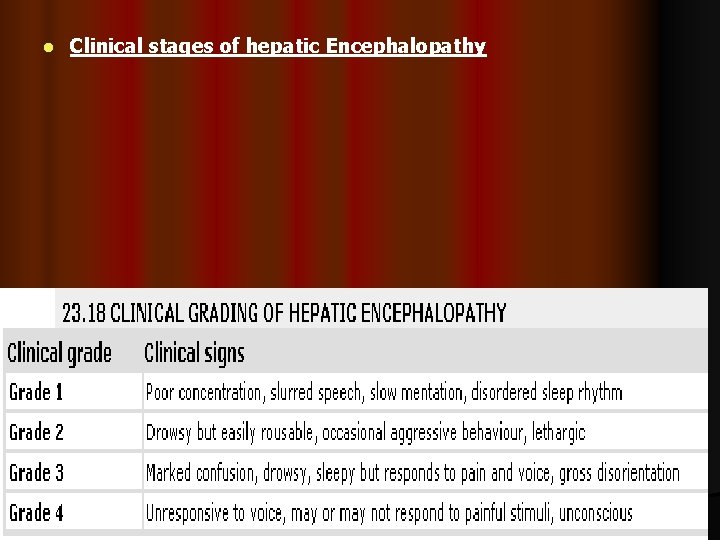
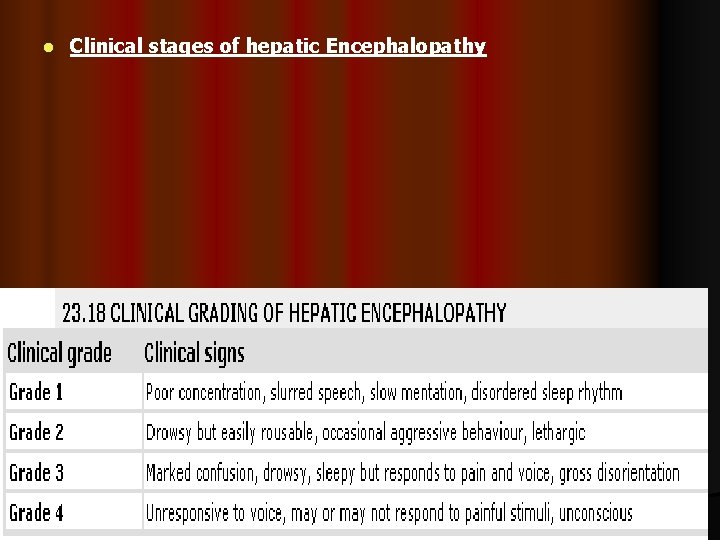
l Clinical stages of hepatic Encephalopathy
Investigations Diagnosis is usually made clinically l No Pathognomonic liver function abnormality l Elevation of blood ammonia l Hypokalaemia l EEG (Electroencephalogram) l CSF & CT Scan – Normal l Other Routine Investigations - TC, DC, ESR, Hb, Na, k, Urea, Creatinine, Prothrombin time
Differential Diagnosis l Subdural Haematoma l Drug or Alcohol intoxication l Wernicke’s encephalopathy l Hypoglycaemia
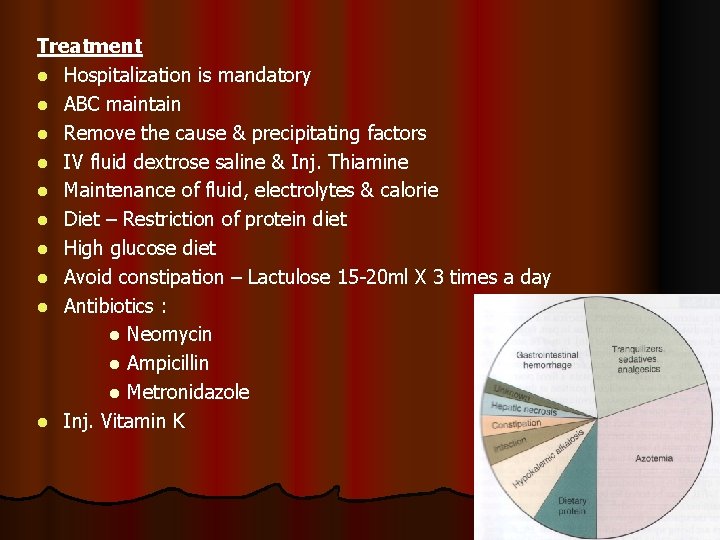
Treatment l Hospitalization is mandatory l ABC maintain l Remove the cause & precipitating factors l IV fluid dextrose saline & Inj. Thiamine l Maintenance of fluid, electrolytes & calorie l Diet – Restriction of protein diet l High glucose diet l Avoid constipation – Lactulose 15 -20 ml X 3 times a day l Antibiotics : l Neomycin l Ampicillin l Metronidazole l Inj. Vitamin K
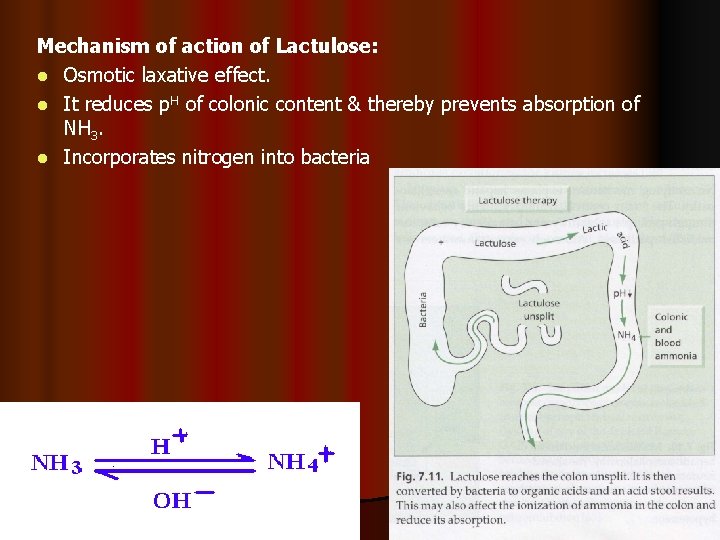
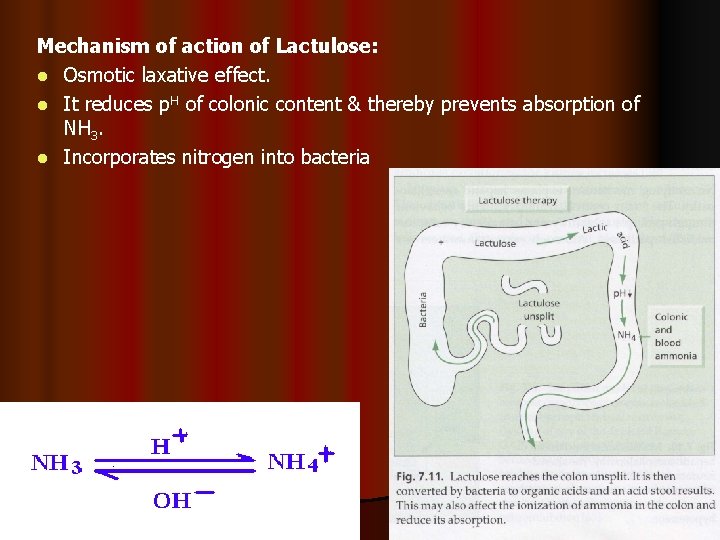
Mechanism of action of Lactulose: l Osmotic laxative effect. l It reduces p. H of colonic content & thereby prevents absorption of NH 3. l Incorporates nitrogen into bacteria
 Encephalopathy stages
Encephalopathy stages Fhf
Fhf Posology formula
Posology formula Diet hepatic encephalopathy
Diet hepatic encephalopathy Asterixis in hepatic encephalopathy
Asterixis in hepatic encephalopathy Hepatic encephalopathy pathophysiology
Hepatic encephalopathy pathophysiology Hepatic encephalopathy staging
Hepatic encephalopathy staging Encephalopathy stages
Encephalopathy stages Hepatic encephalopathy stages
Hepatic encephalopathy stages Hepatic encephalopathy grading
Hepatic encephalopathy grading Diet for hepatitis c
Diet for hepatitis c Constructional apraxia
Constructional apraxia Funcion de los puntos suspensivos
Funcion de los puntos suspensivos Netfrumur
Netfrumur Malignant hypertension treatment
Malignant hypertension treatment Acute toxic encephalopathy icd 10
Acute toxic encephalopathy icd 10