Acute Liver Failure Sara Karjoo MD Kathleen Loomes






- Slides: 26

Acute Liver Failure Sara Karjoo, MD Kathleen Loomes, MD Children’s Hospital of Philadelphia 2013 Resident Education Series Reviewed by John Stutts, MD of the Professional Education Committee
What you need to know for the boards • 2011 AAP Pediatric Gastroenterology Content Guideline: – Formulate a management plan for a patient with acute hepatic failure – Know the prognostic features of acute hepatic failure in children – Know the differential diagnosis of acute hepatic failure – Understand manage the various complications associated with acute hepatic failure

Introduction • Adult definition: – Rapid deterioration of liver function AND – Evidence of coagulation abnormality (INR ≥ 1. 5) AND – Results in any degree of mental alteration/encephalopathy – No pre-existing liver disease – Illness < 26 weeks duration • Pediatric definition: – No evidence of chronic liver disease – Biochemical evidence of acute liver injury – Hepatic coagulopathy defined as INR ≥ 1. 5 not corrected by Vitamin K in the setting of hepatic encephalopathy OR INR ≥ 2. 0 regardless of presence or absence of hepatic encephalopathy
Signs and symptoms • May or may not include all of the following: – Prodrome of malaise and lethargy – Jaundice (often but not always seen) – Excess bleeding or bruising – Right upper quadrant tenderness (variably seen) – Inability to palpate or percuss the liver (decreased liver volume) – Hepatomegaly (viruses, malignancy, Budd-Chiari syndrome, etc) – Altered mental status, or progression to encephalopathy…

Hepatic encephalopathy (Adult definition) Stage • I Clinical Manifestation Asterixis Slight EEG Findings Minimal Present Generalized slowing Present Grossly abnorma Slowness of mentation. Disturbed sleep-wake • III • IV Drowsiness, confusion, disorientation Sleepy but arousable, stupor, unresponsive to commands, hyperreflexia, + Babinski Unconscious, absent reflexes, decerebrate and decorticate to pain Absent Delta waves HARD TO ASSESS IN CHILDREN
Epidemiology • 2000 cases yearly • Very rare • Acute liver failure accounts for 10% of pediatric liver transplantation
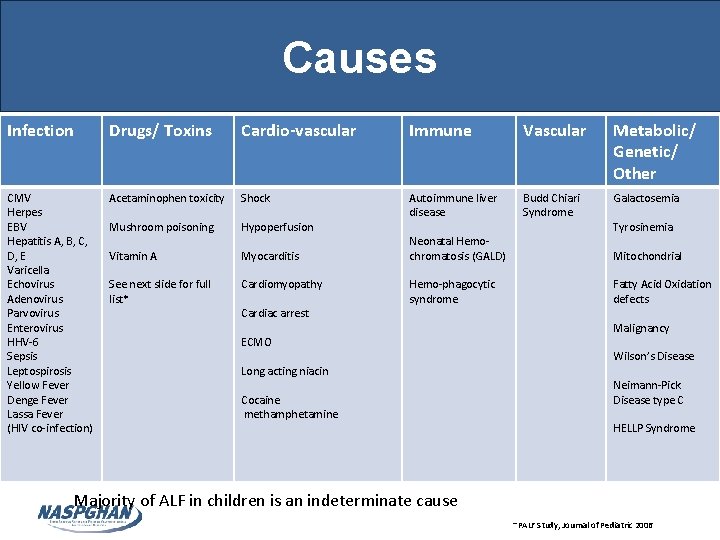
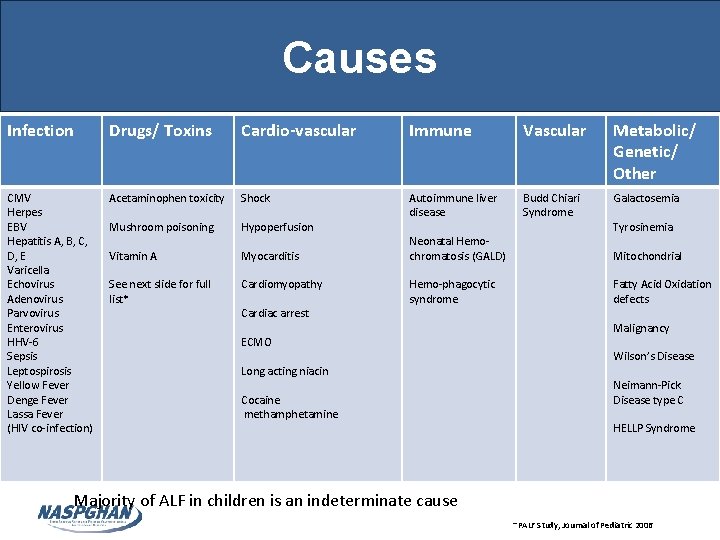
Causes Infection Drugs/ Toxins Cardio-vascular Immune Vascular Metabolic/ Genetic/ Other CMV Herpes EBV Hepatitis A, B, C, D, E Varicella Echovirus Adenovirus Parvovirus Enterovirus HHV-6 Sepsis Leptospirosis Yellow Fever Denge Fever Lassa Fever (HIV co-infection) Acetaminophen toxicity Shock Hypoperfusion Budd Chiari Syndrome Galactosemia Mushroom poisoning Autoimmune liver disease Vitamin A Myocarditis See next slide for full list* Cardiomyopathy Cardiac arrest Neonatal Hemochromatosis (GALD) Hemo-phagocytic syndrome ECMO Long acting niacin Cocaine methamphetamine Majority of ALF in children is an indeterminate cause Tyrosinemia Mitochondrial Fatty Acid Oxidation defects Malignancy Wilson’s Disease Neimann-Pick Disease type C HELLP Syndrome -PALF Study, Journal of Pediatric 2006
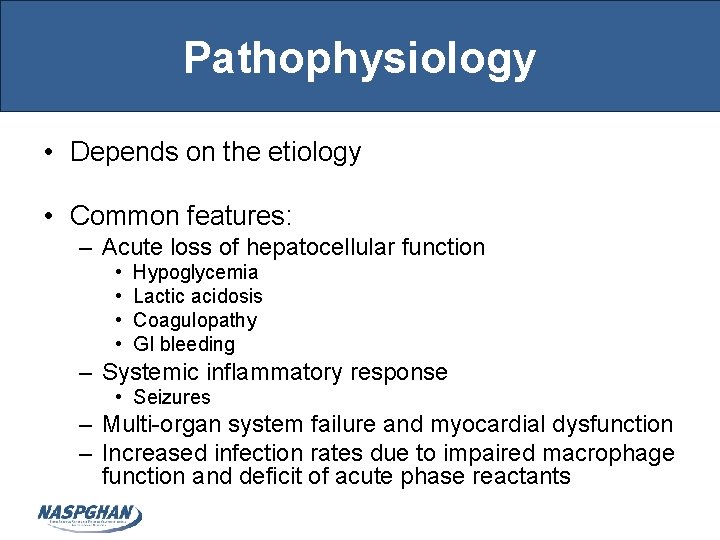
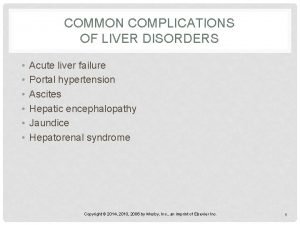
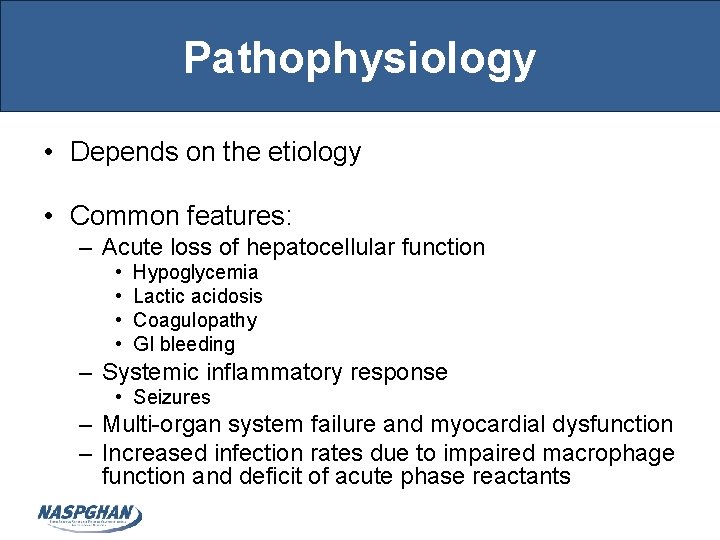
Pathophysiology • Depends on the etiology • Common features: – Acute loss of hepatocellular function • • Hypoglycemia Lactic acidosis Coagulopathy GI bleeding – Systemic inflammatory response • Seizures – Multi-organ system failure and myocardial dysfunction – Increased infection rates due to impaired macrophage function and deficit of acute phase reactants
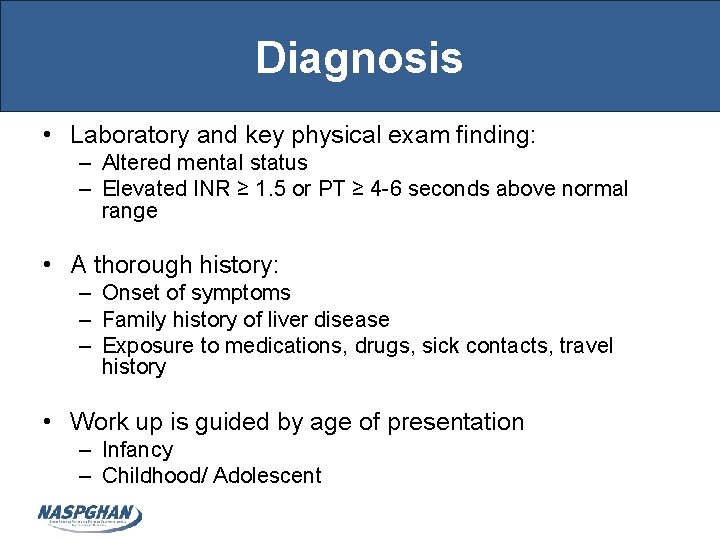
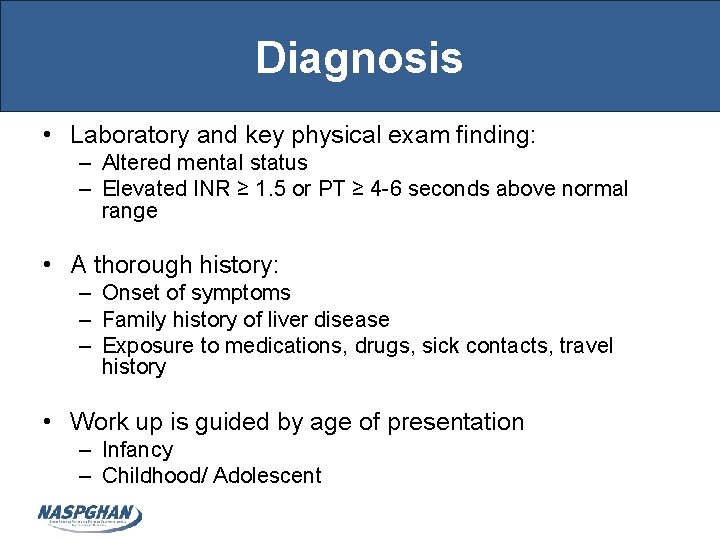
Diagnosis • Laboratory and key physical exam finding: – Altered mental status – Elevated INR ≥ 1. 5 or PT ≥ 4 -6 seconds above normal range • A thorough history: – Onset of symptoms – Family history of liver disease – Exposure to medications, drugs, sick contacts, travel history • Work up is guided by age of presentation – Infancy – Childhood/ Adolescent
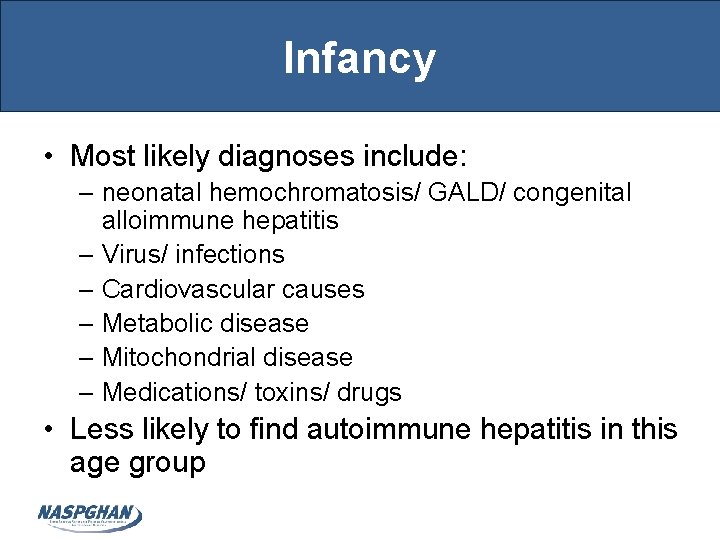
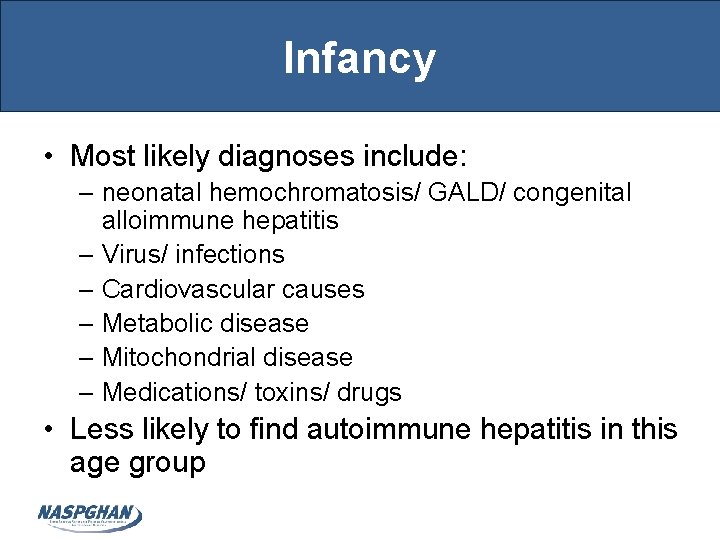
Infancy • Most likely diagnoses include: – neonatal hemochromatosis/ GALD/ congenital alloimmune hepatitis – Virus/ infections – Cardiovascular causes – Metabolic disease – Mitochondrial disease – Medications/ toxins/ drugs • Less likely to find autoimmune hepatitis in this age group

Work up during infancy • Drug testing – Acetaminophen level, drug screening • Viral serologies and PCRs • Metabolic work up: – – – – Plasma ammonia (arterial draw) Lactate/ pyruvate Acylcarnitine profile Urine succinylacetone Urine organic acids (UOA) Serum amnino acids (SAA) Liver biopsy • Cardiac etiologies – Echo – BNP
Childhood/ Adolescence • More likely to be caused by: – HELLP syndrome – Toxins/Drugs – Wilson’s Disease – Autoimmune – Malignancy – Budd-Chiari syndrome – Infections
Work up during childhood/ adolescence • General labs/workup: – – Chemistries Arterial blood gas measurement CBC and type and screen Pregnancy test (HELLP Syndrome) • Jaundice, coagulopathy, low platelets associated with hypoglycemia, hypertention, protienuria, with steatosis on imaging and liver biopsy – Liver biopsy • Drug screening – Acetaminophen level, drug screening • Infectious work up – Viral serologies and PCRs

Work up during childhood/ adolescence • Autoimmune Hepatitis work up – Auto-antibodies (ANA, ASMA, anti-LKM, anti-SLA, Ig. G) • Wilson’s Disease – – Slit lamp examination Urine copper and serum ceruloplasmin Total bilirubin and alkaline phospatase ratio Plasma ammonia • Vascular etiology/ Budd-Chiari – US abdomen with doppler • Malignancy – LDH, AFP, Uric acid, blood smear
Management • Admission to ICU and transfer to center that specializes in liver transplantation • Supportive care vs. monitoring for progression needing liver transplantation • Surveillance of co-morbitities and complications: – – – Sepsis Neurological changes (encephalopathy, seizures) Circulatory failure Renal failure Monitor and treat reduced serum glucose
Management: Coagulopathy • Patients with coagulopathy should be treated with vitamin K subcutaneously (age dependent doses) • Transfusion of platelet and FFP prior to invasive procedures, and in the setting of hemorrhage
Management: Neurological Symptoms • Cerebral edema, uncal herniation, and intracranial hypertension are the most serious complications • May contribute to hypoxic brain injury • AVOID CEREBRAL DEPRESSANTS – More beneficial to control seizures because they increase ICP with very short acting benzodiazepine then phenytoin
Management: Neurological Symptoms • Grade 1 -2 encephalophathy – Can be managed on ward in quiet environment with frequent neurologic checks – ICU transfer and CT head if consciousness declines – Avoid sedation if possible – Can consider treatment with lactulose to decrease ammonia levels
Management: Neurological Symptoms • Grade 3 -4 encephalopathy – Intubation and mechanical ventilation are mandatory – Cisatracurium is preferred because it does not increase ICP • Propofol decreases cerebral blood flow – ICU frequent blood and neurologic monitoring
Management: Infections • Treat acquired infections aggressively because they can progress to encephalopathy and cerebral edema • Infection is a major cause of mortality in acute liver failure • Role for prophylactic antibiotics
Management: GI Bleeding and Nutrition • Patients with ALF in ICU should receive prophylaxis with H 2 blocker or PPI for acid related gastrointestinal bleeding associated with stress • Enteral and parental nutrition decrease the risk of GI bleeding due to stress ulceration • Enteral nutrition is best, and do not need severe restriction of protein • Use higher dextrose fluid to combat hypoglycemia • Monitor and replace deficiency in phosphate, potassium, magnesium

Management: Renal and Cardiovascular • • • Renal dysfunction seen in severe disease Hemodynamic alterations lead to renal failure May need dialysis May see both azotemia or oliguria May need to treat hypotension with pressors Search for etiology of cardiomyopathy or myocarditis • Treat causes of alkylosis
Management: Other Concepts • Low level of aminotransferases may not reflect recovery, actually may be a sign of severe liver destruction • Steroids are helpful in setting of autoimmune disease, but not universally recommended in all causes of ALF • Limit sodium in fluids • Start diuretics to treat ascites
Indications for Liver transplant in ALF • Difficult decision because of inadequate predictors of prognosis, and depends on etiology – Liver failure from APAP ingestion more likely to recover vs. liver failure from Wilson’s disease • MELD scores, KCH criteria, and others are not good predictors of prognosis • Liver transplantation is considered if there is progression of liver disease with expected hepatic failure
Prognosis • Carries a high morbidity and mortality • However many patients recover • Short-term survival (1 year) including those undergoing transplantation is greater than 65% • The children who had an indeterminate cause have a poorer outcome
References • • • Lee, W. M. ; Larson, A. M. ; Straviz, R. T. AASLD Position Paper: The Management of Acute Liver Failure: Update 2011. Hepatology: 2011, 1 -22. http: //www. palfstudy. org/information. asp Acute Liver Failure Lecture by Kathy Loomes August 31, 2012. Dhawan, A. ; Cheeseman, P. ; Mieli-Vergani, G. Approches to acute liver failure in children. Pediatric Transplantation, 2004: 8, 584 -588. Squires, R. H. Acute liver failure in children. Seminars in liver disease, 2008: 28, 153 -166. SQUIRES, R. H. ; et al. ACUTE LIVER FAILURE IN CHILDREN: THE FIRST 348 PATIENTS IN THE PEDIATRIC ACUTE LIVER FAILURE STUDY GROUP. The Journal of Pediatrics, 2006; 148: 652 -8.
 Acute liver failure criteria
Acute liver failure criteria Paracetamol overdose stages
Paracetamol overdose stages Liver failure criteria
Liver failure criteria Acute fatty liver of pregnancy
Acute fatty liver of pregnancy Lchad deficiency
Lchad deficiency Acute fatty liver of pregnancy
Acute fatty liver of pregnancy Portal hypertension definition
Portal hypertension definition Hepatic encephalopathy staging
Hepatic encephalopathy staging Treatments for acute renal failure
Treatments for acute renal failure Acute vs chronic heart failure
Acute vs chronic heart failure Acute brain failure
Acute brain failure Ventricular escape rhythm
Ventricular escape rhythm Pacer failure to sense
Pacer failure to sense Brittle failure vs ductile failure
Brittle failure vs ductile failure Kathleen peterson forensic evidence
Kathleen peterson forensic evidence Merv grazinski
Merv grazinski Kathleen maddox
Kathleen maddox Kathleen merikangas
Kathleen merikangas Kathleen lynch ucd
Kathleen lynch ucd Kathleen jerchel
Kathleen jerchel Kathleen
Kathleen Kathleen durant
Kathleen durant Kathleen stassen berger
Kathleen stassen berger Kathleen quinlan smoking
Kathleen quinlan smoking Kathleen lynch ucd
Kathleen lynch ucd Kathleen berry md
Kathleen berry md Mary kathleen heneghan
Mary kathleen heneghan