Approach to the poisoned patient Domina Petric MD




- Slides: 65
Approach to the poisoned patient Domina Petric, MD
Death causes in poisoning • Many toxins depress the central nervous system. • Comatose patients lose their airway protective reflexes and their respiratory drive. These patients may die as a result of airway obstruction by: • flaccid tongue • aspiration of gastric contents into the tracheobronchial tree • respiratory arrest These are the most common causes of death due to overdoses of narcotics and sedative-hypnotic drugs (for example barbiturates combined with alcohol).
Death causes in poisoning • Cardiovascular toxicity is also common in poisoning. • Hypotension may be due to depression of cardiac contractility. • Hypovolemia may be result of vomiting, diarrhea or fluid sequestration. • Peripheral vascular collapse may be due to blockade of α-adrenoreceptor-mediated vascular tone. • Hypothermia or hyperthermia, due to exposure to temperature-dysregulating effects of many drugs, can produce hypotension.

Death causes in poisoning Lethal arrhythmias (ventricular tachycardia, ventricular fibrillation) can occur as a result of overdose with: • ephedrine • amphetamines • cocaine • digitalis • theophylline • tricyclic antidepressants • antihistamines • some opioid analogs
Death causes in poisoning Cellular hypoxia, in spite of adequate ventilation and oxygen administration, may occur in case of poisoning with: • cyanide • hydrogen sulfide • carbon monoxide • other poisons that interfere with transport of utilization of oxygen
Death causes in poisoning Cellular hypoxia is evident by the development of: • tachycardia • hypotension • severe lactic acidosis • signs of ischemia on the ECG These patients may not be cyanotic.
Death causes in poisoning Seizures, muscular hyperactivity and rigidity may cause death in patients poisoned with: • antidepressants • isoniazid (INH) • diphenhydramine • cocaine • amphetamines
Death causes in poisoning • Seizures may cause pulmonary aspiration, hypoxia and brain damage. • Hyperthermia may result from sustained muscular hyperactivity and can lead to muscle breakdown, myoglobinuria, renal failure, lactic acidosis and hyperkalemia.
Death causes in poisoning Paraquat attacks lung tissue, resulting in pulmonary fibrosis that begins several days after ingestion. Massive hepatic necrosis due to poisoning by acetaminophen or certain mushrooms results in hepatic encephalopathy and death 48 -72 hours or longer after ingestion.
Death causes in poisoning Intoxication with alcohol and other sedative-hypnotic drugs is common contributing factor to motor vehicle accidents. Patients under the influence of hallucinogens (PCP, LSD) may suffer trauma in state of good or bad trip (for example, fall from a height).

INITIAL MANAGEMENT OF THE POISONED PATIENT
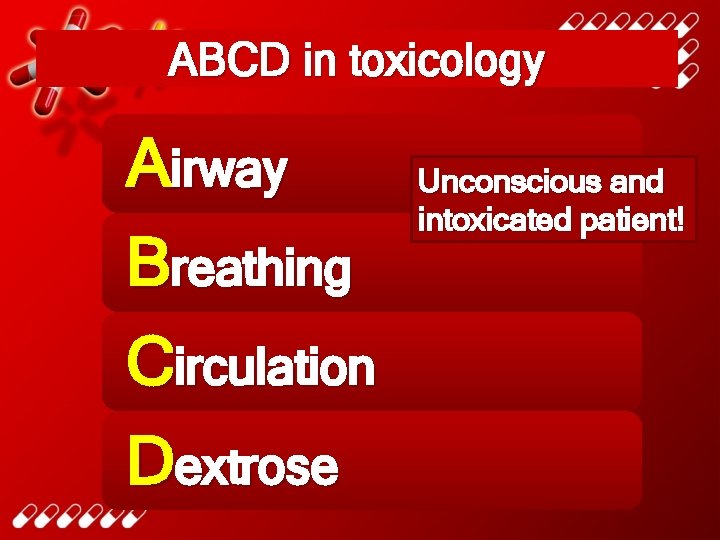
ABCD in toxicology Airway Breathing Circulation Dextrose Unconscious and intoxicated patient!
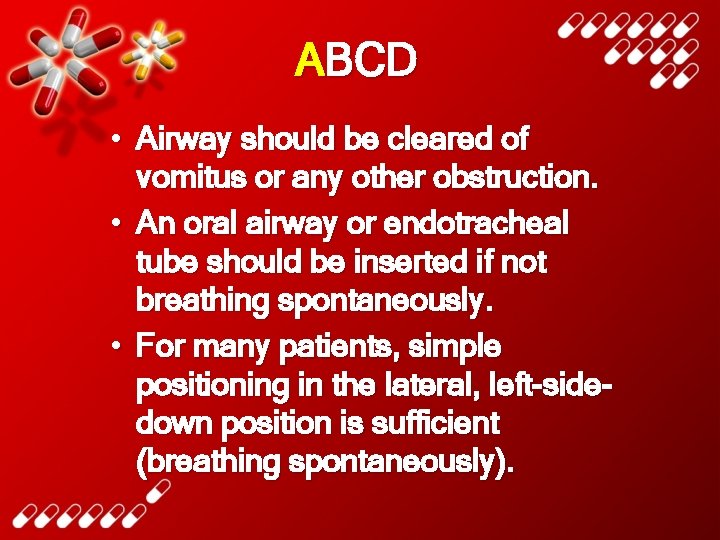
ABCD • Airway should be cleared of vomitus or any other obstruction. • An oral airway or endotracheal tube should be inserted if not breathing spontaneously. • For many patients, simple positioning in the lateral, left-sidedown position is sufficient (breathing spontaneously).
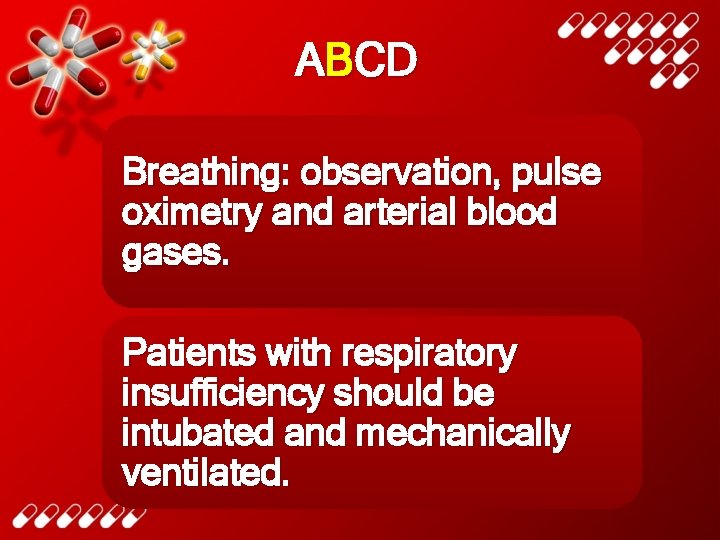
ABCD Breathing: observation, pulse oximetry and arterial blood gases. Patients with respiratory insufficiency should be intubated and mechanically ventilated.
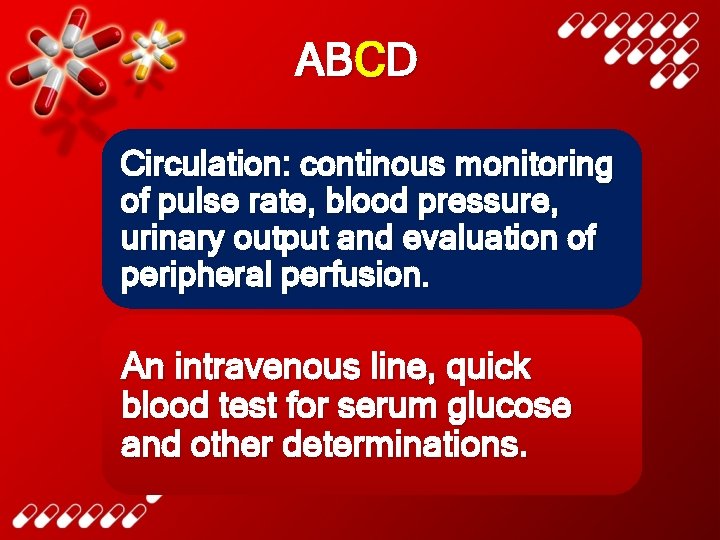
ABCD Circulation: continous monitoring of pulse rate, blood pressure, urinary output and evaluation of peripheral perfusion. An intravenous line, quick blood test for serum glucose and other determinations.
ABCD • Every patient with altered mental status should receive concentrated dextrose, unless a rapid blood glucose test demonstrates that the patient is not hypoglycemic. • Adults: 50 m. L of 40 -50% dextrose solution iv. • Children: 5 m. L/kg of 10% glucose or 2 m. L/kg of 25% dextrose iv.
ABCD Alcoholic or malnourished patients should receive 100 mg of thiamine im. or in the iv. infusion solution together with glucose/dextrose to prevent Wernicke´s syndrome.
ABCD • The opioid antagonist is naloxone, dose is 0, 4 -2 mg iv. • Naloxone reverses respiratory and CNS depression. • Larger doses of naloxone may be needed for patients with overdose involving propoxyphene, codeine and some other opioids.
ABCD • The benzodiazepine antagonist is flumazenil. • It should not be used if there is a history of tricyclic antidepressant overdose or a seizure disorder because it can induce convulsions in such patients.
HISTORY AND PHYSICAL EXAMINATION
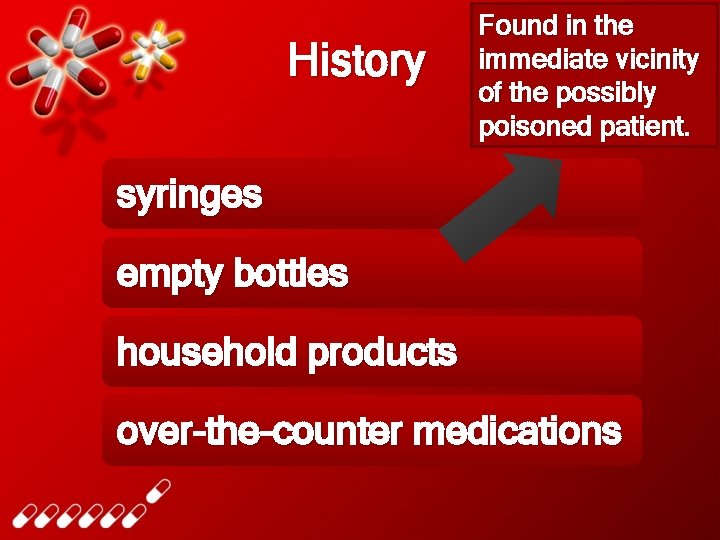
History Found in the immediate vicinity of the possibly poisoned patient. syringes empty bottles household products over-the-counter medications
Physical examination Brief examination with emphasizing important areas for the toxicologic diagnosis: • vital signs • eyes • mouth • skin • abdomen • nervous system
Vital signs • Blood pressure, pulse, respiration and temperature! • Hypertension and tachycardia are typical with amphetamines, cocaine and antimuscarinic (anticholinergic) drugs.
Vital signs Hypotension and bradycardia: overdose with calcium channel blockers, β blockers, clonidine and sedative hypnotics.
Vital signs Hypotension with tachycardia: tricyclic antidepressants, trazodone, quetiapine, vasodilators and β agonists.
Vital signs Rapid respirations: salicylates, carbon monoxide and other toxins that produce metabolic acidosis or cellular asphyxia.
Vital signs Hyperthermia: sympathomimetics, anticholinergics, salicylates and drugs producing seizures or muscular rigidity. Hypothermia: CNSdepressant drugs, especially when accompanied by exposure to a cold environment.
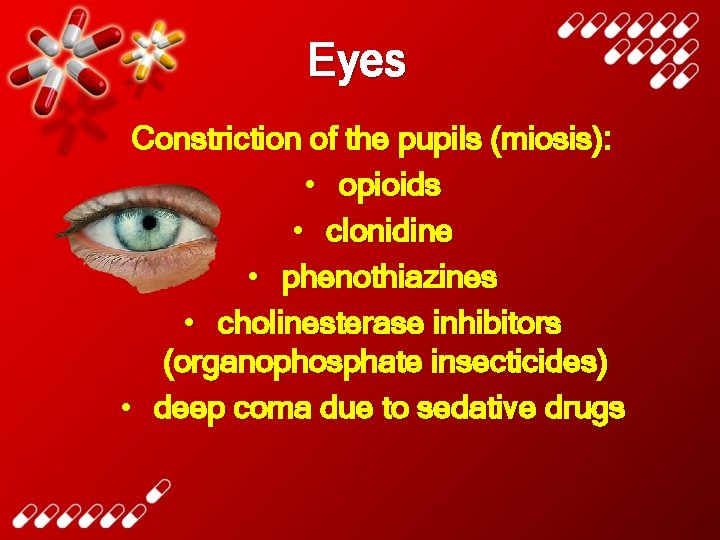
Eyes Constriction of the pupils (miosis): • opioids • clonidine • phenothiazines • cholinesterase inhibitors (organophosphate insecticides) • deep coma due to sedative drugs
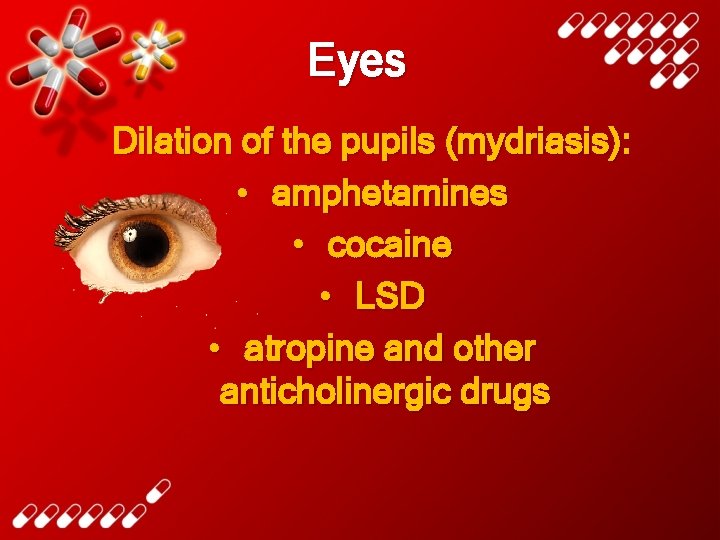
Eyes Dilation of the pupils (mydriasis): • amphetamines • cocaine • LSD • atropine and other anticholinergic drugs
Eyes Horizontal nystagmus is characteristic of intoxication with: • phenytoin • alcohol • barbiturates • other sedative drugs
Eyes Both vertical and horizontal nystagmus is strongly suggestive of phencyclidine poisoning.
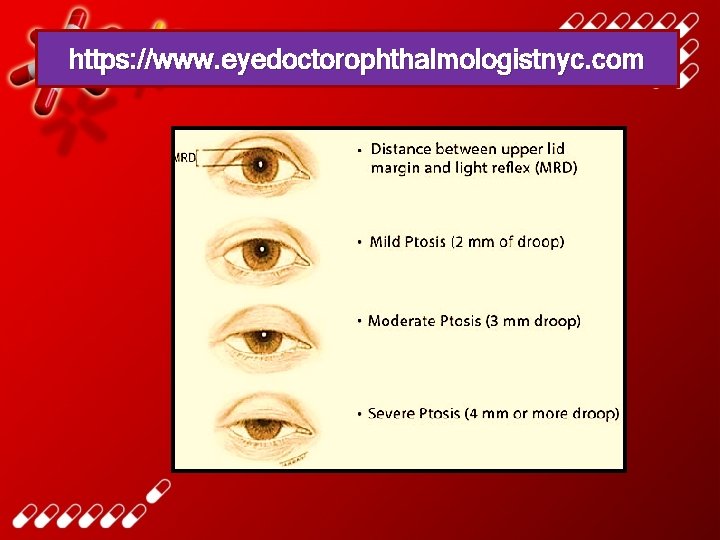
Eyes Ptosis and ophthalmoplegia are characteristic features of botulism.
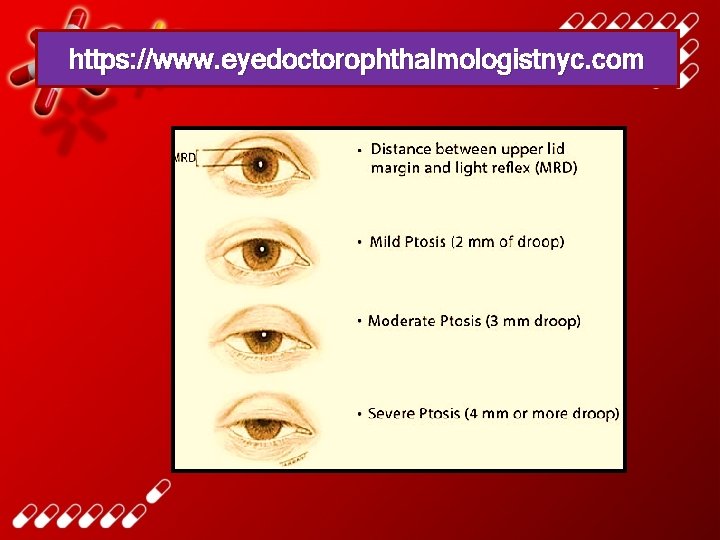
https: //www. eyedoctorophthalmologistnyc. com
Mouth Signs of burns due to corrosive substances. Soot from smoke inhalation. Typical odors of alcohol, hydrocarbon solvents or ammonia. Cyanide: odor like bitter almonds.

Caustic burns of tongue Medscape. com
Skin • Poisoning with atropine and other antimuscarinics: flushed, hot and dry skin. • Excessive sweating: organophosphates, nicotine and sympathomimetics.
Skin • Cyanosis may be caused by hypoxemia or by methemoglobinemia. • Icterus may suggest hepatic necrosis due to acetaminophen or Amanita phalloides mushroom poisoning.
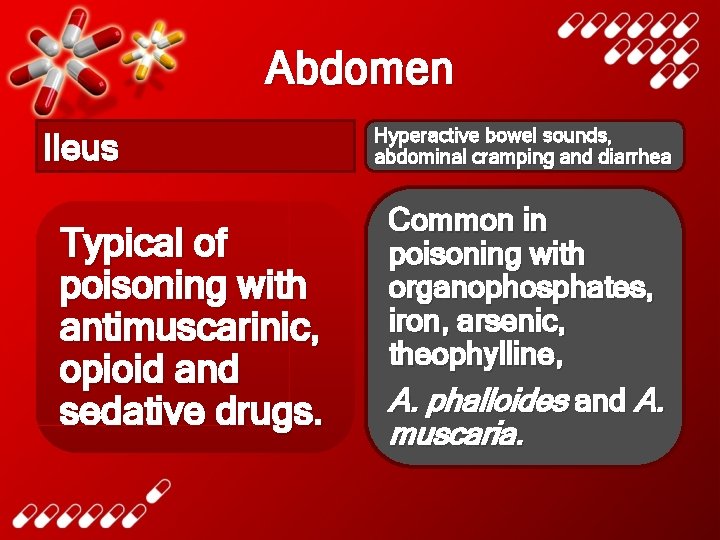
Abdomen Ileus Typical of poisoning with antimuscarinic, opioid and sedative drugs. Hyperactive bowel sounds, abdominal cramping and diarrhea Common in poisoning with organophosphates, iron, arsenic, theophylline, A. phalloides and A. muscaria.
Nervous system Focal seizures or motor deficits suggest a structural lesion (intracranial hemorrhage due to trauma) rather than toxic or metabolic encephalopathy.
Nervous system Nystagmus, dysarthria and ataxia are typical of phenytoin, carbamazepine, alcohol and other sedative intoxication.
Nervous system Twiching and muscular hyperactivity are common with atropine and other anticholinergic agents, also with cocaine and other sympathomimetic drugs.
Nervous system Muscular rigidity can be caused by haloperidol and other antipsychotic agents, also by strychnine or by tetanus.
Nervous system Serotonin syndrome: generalized hypertonicity of muscles and lower extremity clonus.
Nervous system Seizures are often caused by overdose with: • antidepressants (especially tricyclic antidepressants and bupropion) • cocaine • amphetamines • theopylline • isoniazid • diphenhydramine
Nervous system • Flaccid coma with absent reflexes and even an isoelectric electroencephalogram may be seen with deep coma due to sedative-hypnotic or other CNS depressant intoxication. • This should not be mistaken for brain death!

LABORATORY AND IMAGING PROCEDURES
Arterial blood gases • Hypoventilation results in hypercapnia (elevated p. CO 2) and hypoxia (low p. O 2). • Hypoxia may be present in a patient with aspiration pneumonia or druginduced pulmonary edema. • Poor tissue oxygenation due to hypoxia, hypotension or cyanide poisoning results in metabolic acidosis.
Arterial blood gases • The p. O 2 measures only oxygen dissolved in the plasma and not total blood oxygen content or oxyhemoglobin saturation. • It may appear normal in patients with severe CO poisoning. • Pulse oximetry may also give falsely normal results in CO intoxication.
Electrolytes • Sodium, potassium, chloride and bicarbonate are measured anion gap is then calculated. Anion gap=(Na++K+)-(HCO 3 - +Cl-) • Normally, the sum of the cations exceeds the sum of the anions by no more than 12 -16 mmol/L.
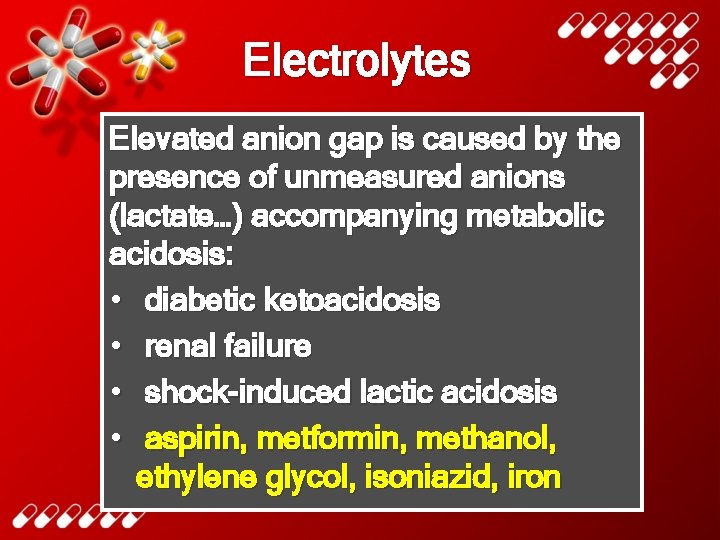
Electrolytes Elevated anion gap is caused by the presence of unmeasured anions (lactate…) accompanying metabolic acidosis: • diabetic ketoacidosis • renal failure • shock-induced lactic acidosis • aspirin, metformin, methanol, ethylene glycol, isoniazid, iron
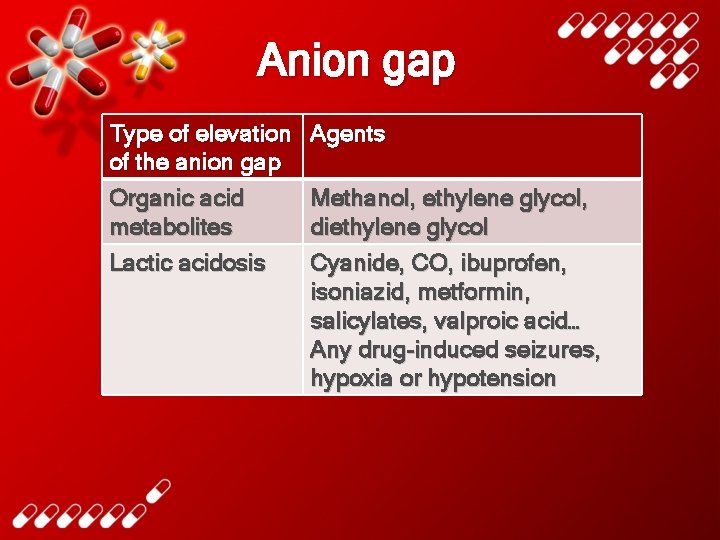
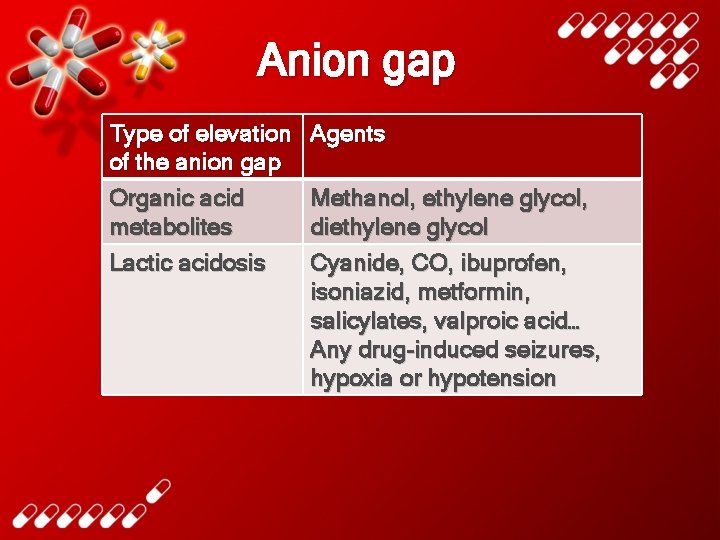
Anion gap Type of elevation of the anion gap Organic acid metabolites Lactic acidosis Agents Methanol, ethylene glycol, diethylene glycol Cyanide, CO, ibuprofen, isoniazid, metformin, salicylates, valproic acid… Any drug-induced seizures, hypoxia or hypotension
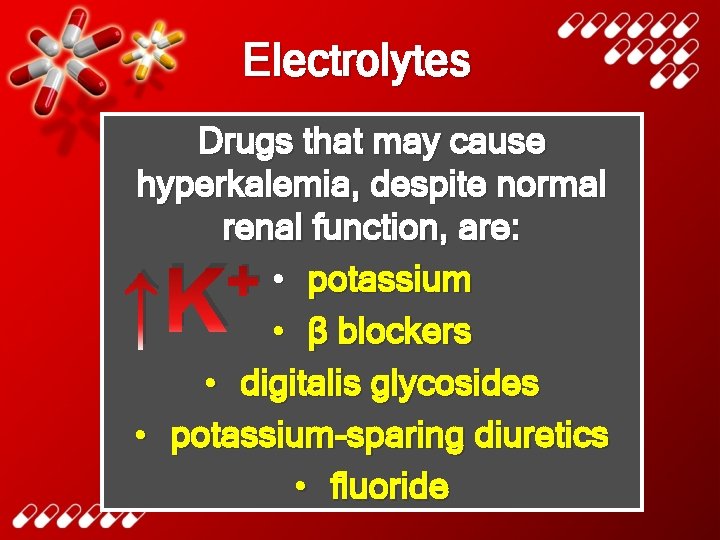
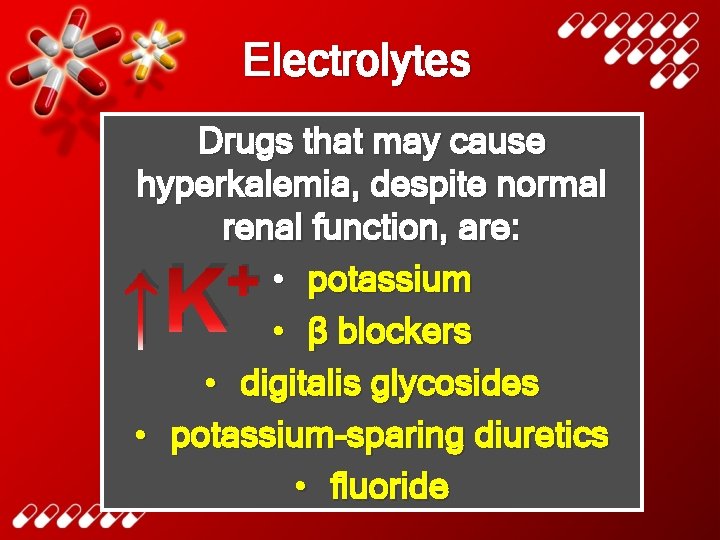
Electrolytes Drugs that may cause hyperkalemia, despite normal renal function, are: • potassium • β blockers • digitalis glycosides • potassium-sparing diuretics • fluoride + ↑K
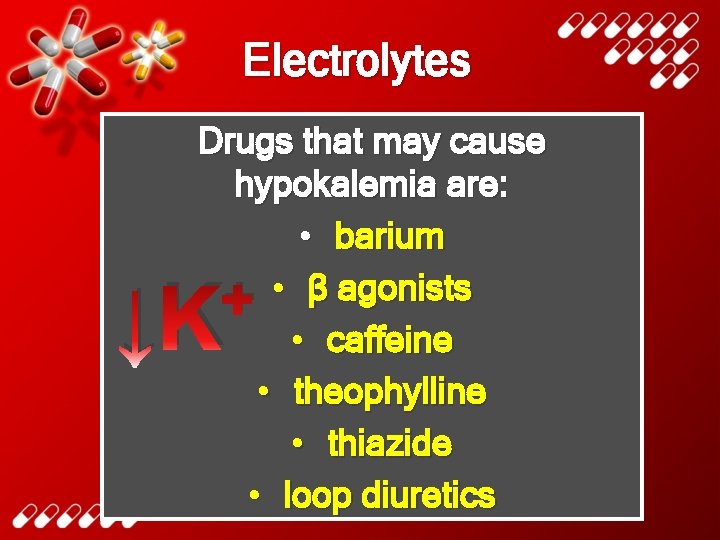
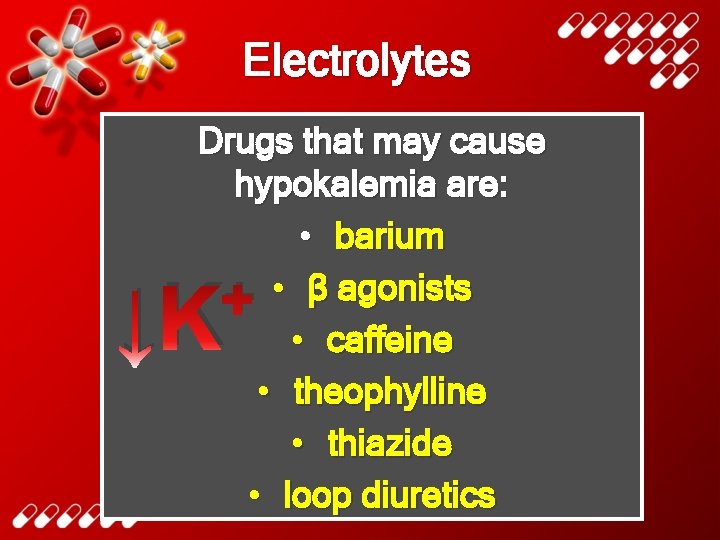
Electrolytes Drugs that may cause hypokalemia are: • barium • β agonists • caffeine • theophylline • thiazide • loop diuretics + ↓K
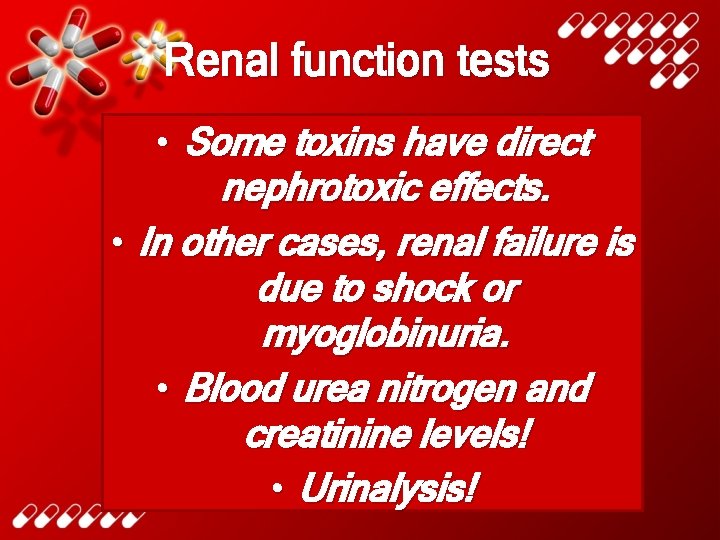
Renal function tests • Some toxins have direct nephrotoxic effects. • In other cases, renal failure is due to shock or myoglobinuria. • Blood urea nitrogen and creatinine levels! • Urinalysis!
Renal function tests • Elevated serum creatine kinase (CK) and myoglobin in the urine suggest muscle necrosis due to seizures or muscular rigidity. • Oxalate crystals in large numbers in the urine suggest ethylene glycol poisoning.
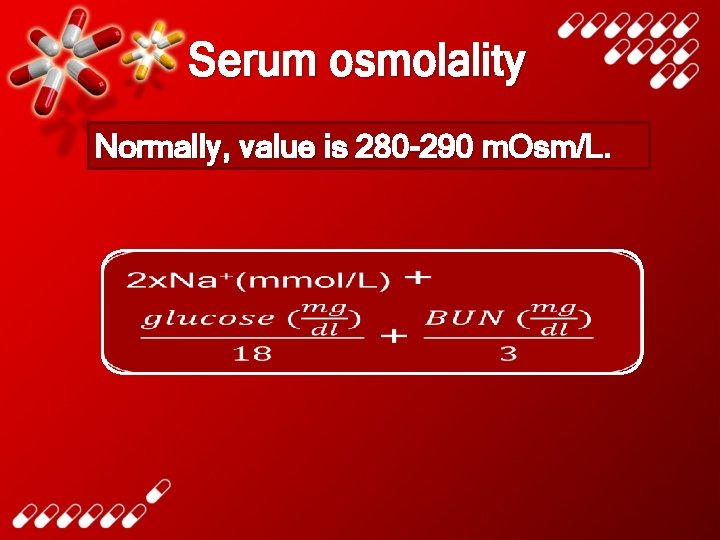
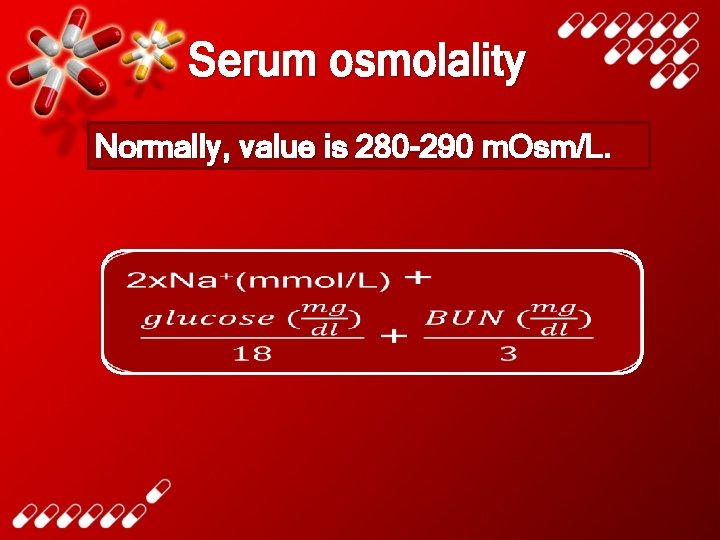
Serum osmolality Normally, value is 280 -290 m. Osm/L.
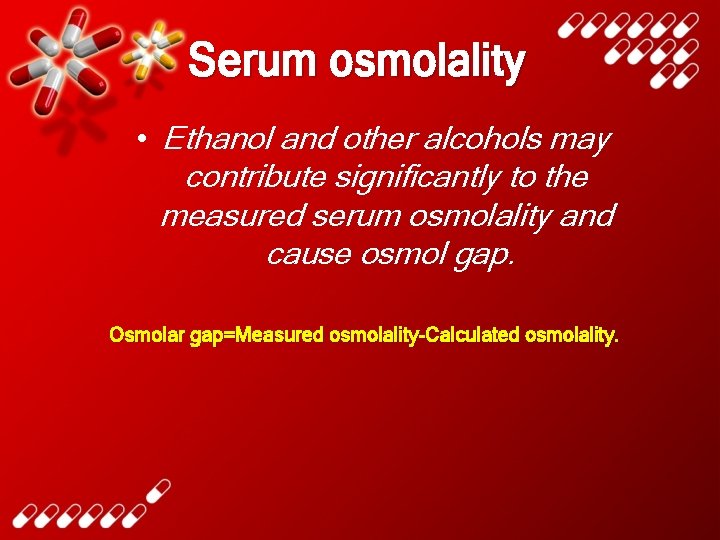
Serum osmolality • Ethanol and other alcohols may contribute significantly to the measured serum osmolality and cause osmol gap. Osmolar gap=Measured osmolality-Calculated osmolality.
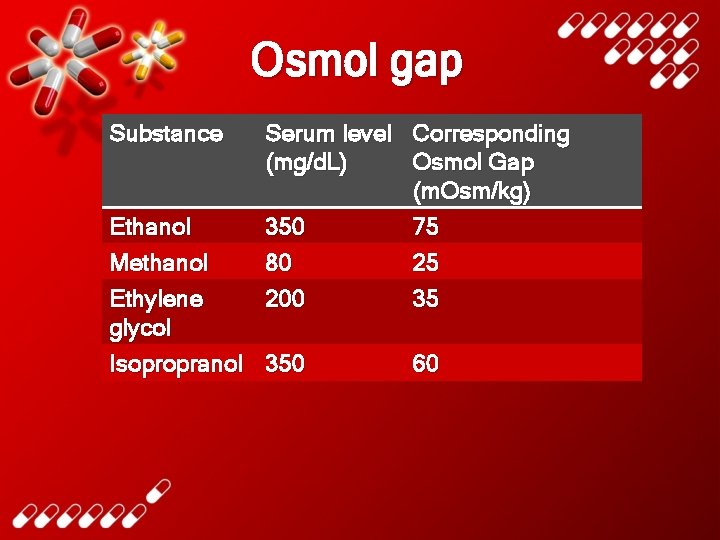
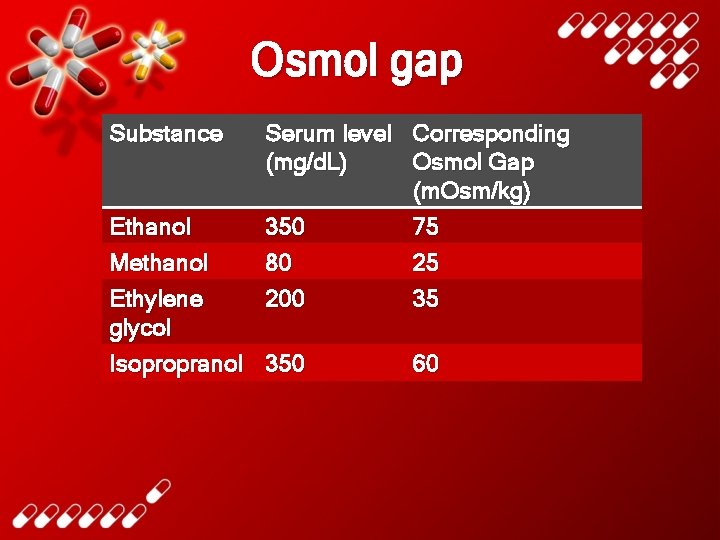
Osmol gap Substance Serum level Corresponding (mg/d. L) Osmol Gap (m. Osm/kg) 350 75 80 25 200 35 Ethanol Methanol Ethylene glycol Isopropranol 350 60
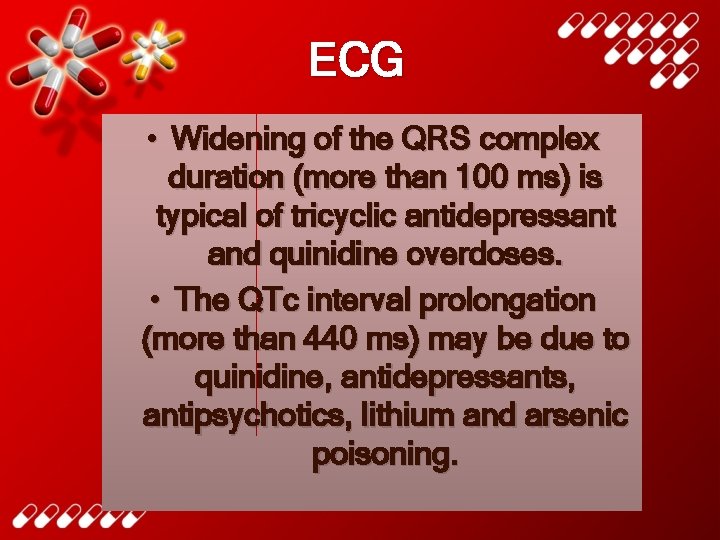
ECG • Widening of the QRS complex duration (more than 100 ms) is typical of tricyclic antidepressant and quinidine overdoses. • The QTc interval prolongation (more than 440 ms) may be due to quinidine, antidepressants, antipsychotics, lithium and arsenic poisoning.
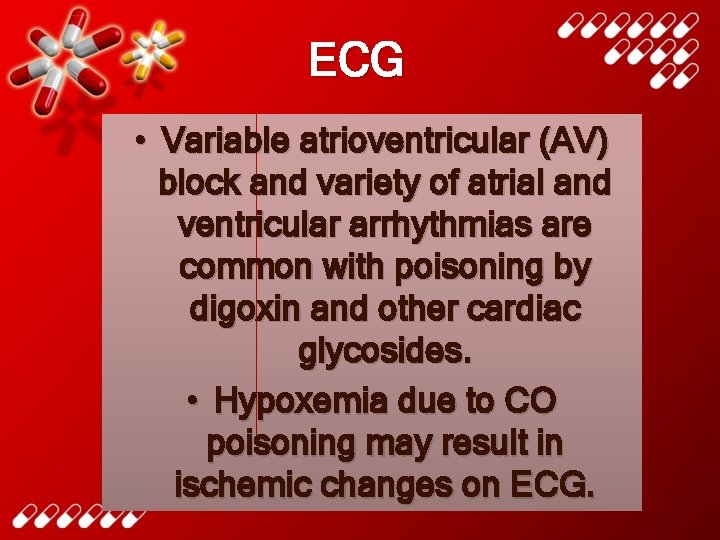
ECG • Variable atrioventricular (AV) block and variety of atrial and ventricular arrhythmias are common with poisoning by digoxin and other cardiac glycosides. • Hypoxemia due to CO poisoning may result in ischemic changes on ECG.
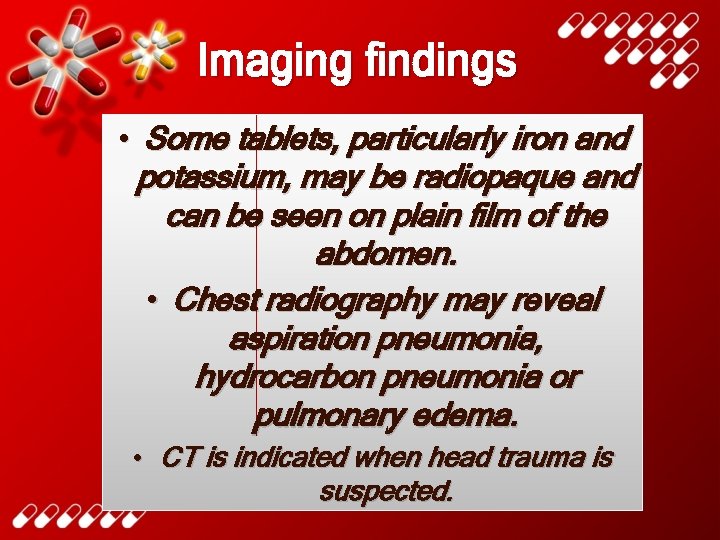
Imaging findings • Some tablets, particularly iron and potassium, may be radiopaque and can be seen on plain film of the abdomen. • Chest radiography may reveal aspiration pneumonia, hydrocarbon pneumonia or pulmonary edema. • CT is indicated when head trauma is suspected.
Toxicology screening tests When a specific antidote or other treatment is under consideration, quantitative laboratory testing may be indicated.
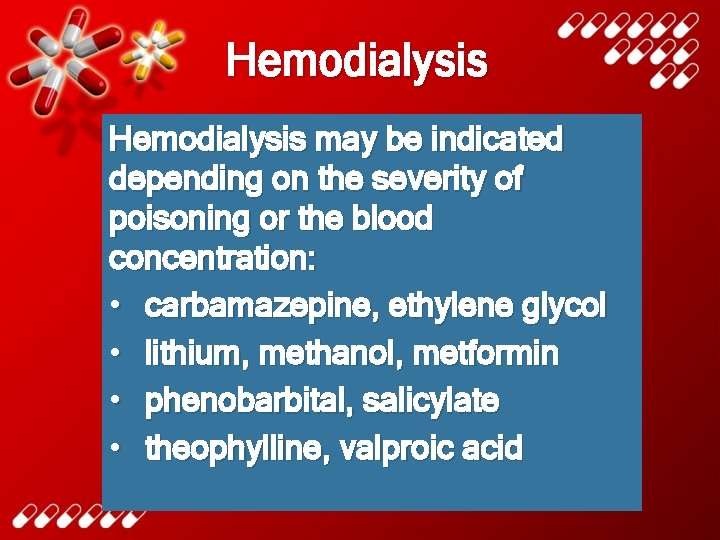
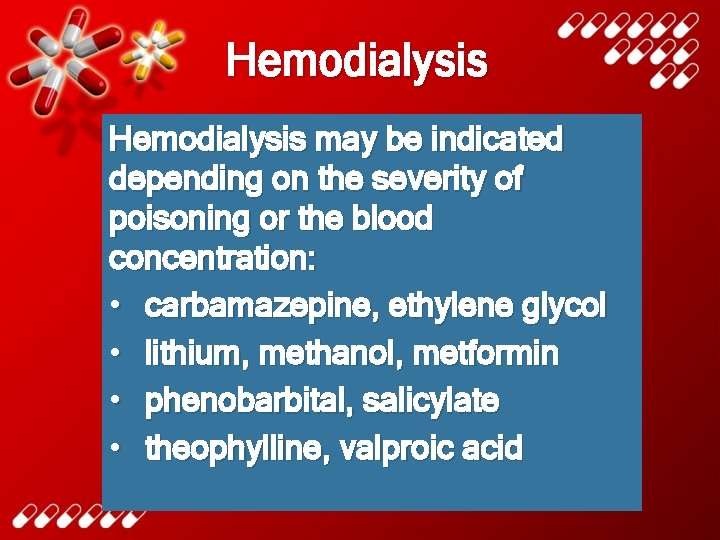
Hemodialysis may be indicated depending on the severity of poisoning or the blood concentration: • carbamazepine, ethylene glycol • lithium, methanol, metformin • phenobarbital, salicylate • theophylline, valproic acid
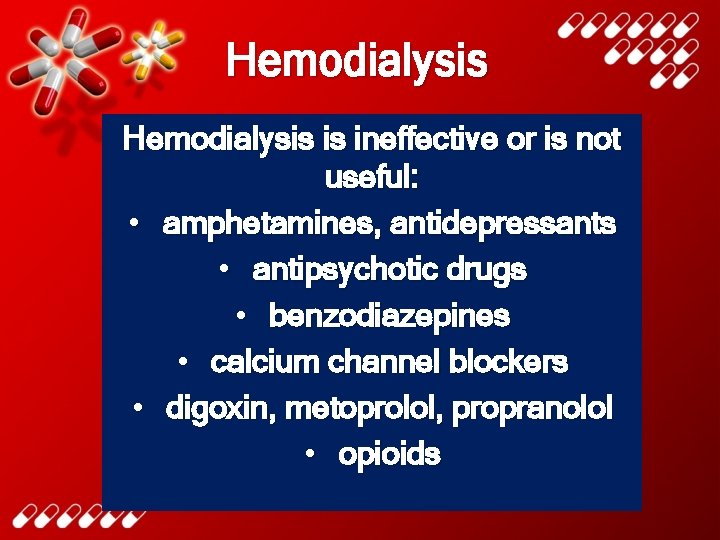
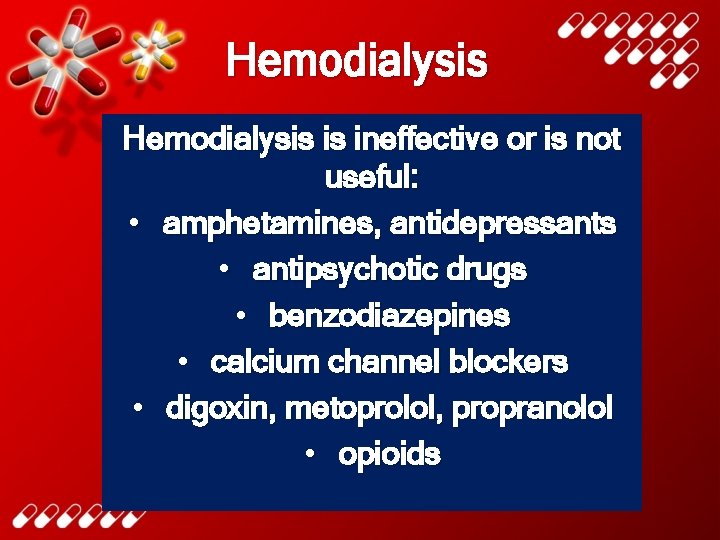
Hemodialysis is ineffective or is not useful: • amphetamines, antidepressants • antipsychotic drugs • benzodiazepines • calcium channel blockers • digoxin, metoprolol, propranolol • opioids
Literature • Katzung, Masters, Trevor. Basic and clinical pharmacology. • Medscape. com • Healthtap. com • Eyedoctorophthalmologistnyc. com • Web. MD. com • Lab. CE. com
 Domina petric
Domina petric Domina petric
Domina petric Domina petric
Domina petric Inr check
Inr check Domina petric
Domina petric Domina petric
Domina petric Domina petric
Domina petric La jin
La jin The curse of the poisoned pretzel
The curse of the poisoned pretzel Jure petric
Jure petric Dobriša cesarić pjesme lektira za 7 razred
Dobriša cesarić pjesme lektira za 7 razred Patient 2 patient
Patient 2 patient Kitzler witze
Kitzler witze 8 atitudes vencedoras
8 atitudes vencedoras Domina epistulam
Domina epistulam Domina los aprendizajes requeridos
Domina los aprendizajes requeridos Domina severe
Domina severe Cada miembro domina una parcela determinada del proyecto.
Cada miembro domina una parcela determinada del proyecto. Research approaches definition
Research approaches definition Waterfall strategy marketing
Waterfall strategy marketing Approach to system development
Approach to system development Multiple approach-avoidance conflict
Multiple approach-avoidance conflict Deep learning approach and surface learning approach
Deep learning approach and surface learning approach Comparison between virtual circuit and datagram network
Comparison between virtual circuit and datagram network Bandura's reciprocal determinism
Bandura's reciprocal determinism Theoretical models of counseling
Theoretical models of counseling Phản ứng thế ankan
Phản ứng thế ankan Các môn thể thao bắt đầu bằng tiếng bóng
Các môn thể thao bắt đầu bằng tiếng bóng Khi nào hổ mẹ dạy hổ con săn mồi
Khi nào hổ mẹ dạy hổ con săn mồi điện thế nghỉ
điện thế nghỉ Biện pháp chống mỏi cơ
Biện pháp chống mỏi cơ Một số thể thơ truyền thống
Một số thể thơ truyền thống Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Chó sói
Chó sói Ng-html
Ng-html Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan Số nguyên tố là
Số nguyên tố là Fecboak
Fecboak Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Hệ hô hấp
Hệ hô hấp Tư thế ngồi viết
Tư thế ngồi viết đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Tư thế worms-breton
Tư thế worms-breton Bổ thể
Bổ thể Tư thế ngồi viết
Tư thế ngồi viết ưu thế lai là gì
ưu thế lai là gì Thẻ vin
Thẻ vin Bàn tay mà dây bẩn
Bàn tay mà dây bẩn Thể thơ truyền thống
Thể thơ truyền thống Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Diễn thế sinh thái là
Diễn thế sinh thái là Thứ tự các dấu thăng giáng ở hóa biểu
Thứ tự các dấu thăng giáng ở hóa biểu Phép trừ bù
Phép trừ bù Chúa sống lại
Chúa sống lại Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập đại từ thay thế
đại từ thay thế Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Công thức tiính động năng
Công thức tiính động năng Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Lời thề hippocrates
Lời thề hippocrates