Alzheimers and dementia research Associate Professor Michael Woodward






















- Slides: 84

Alzheimer’s and dementia research Associate Professor Michael Woodward AM Port Lincoln April 2017
Scope of talk 1. 2. 3. 4. 5. 6. The progression of Alzheimer’s disease New diagnostic approaches Prevention Treatment Other research Conclusions

AD Histopathology cerebral cortex Biel Senile plaques & neurofibrillary tangles
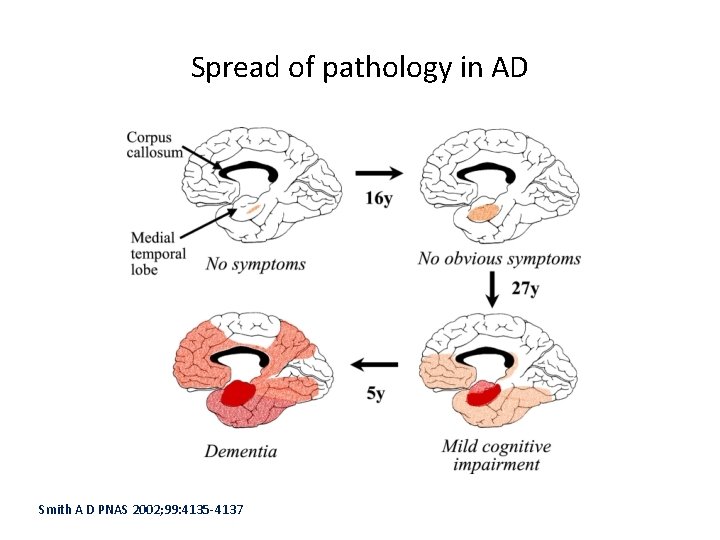
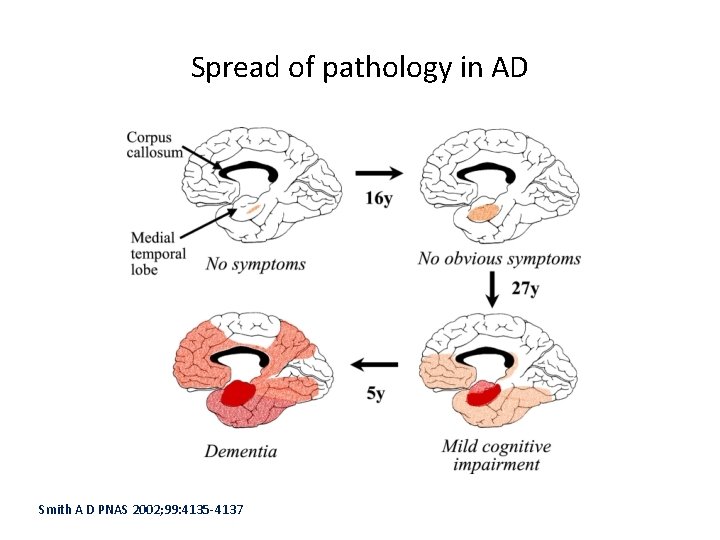
Spread of pathology in AD Smith A D PNAS 2002; 99: 4135 -4137
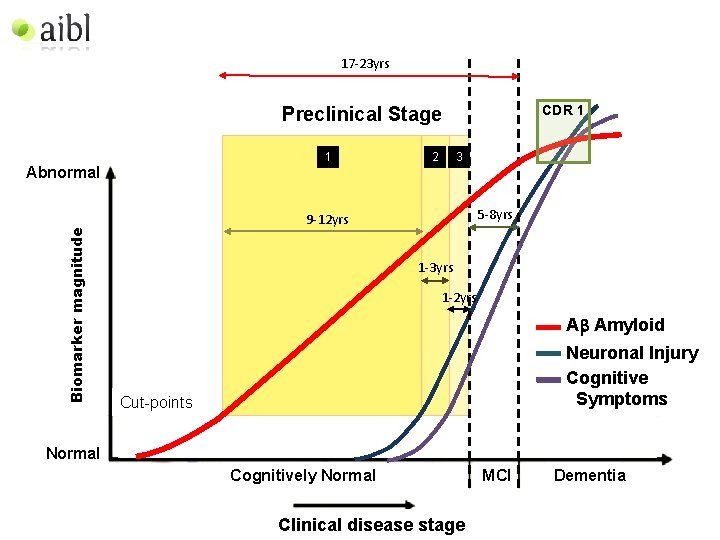
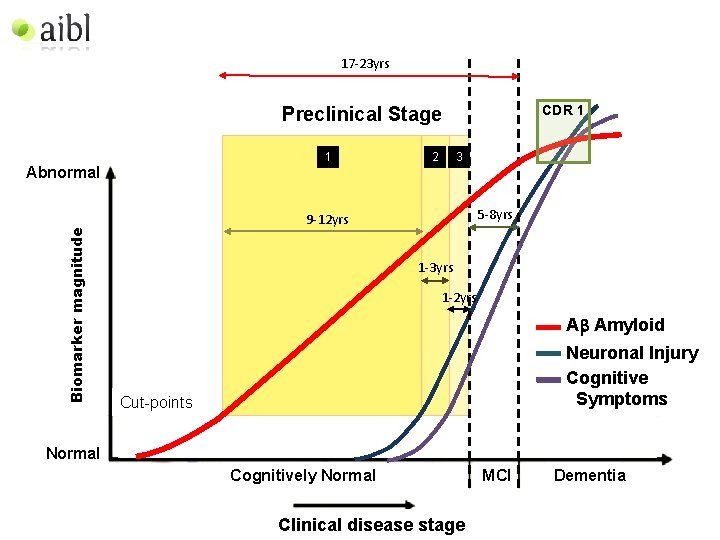
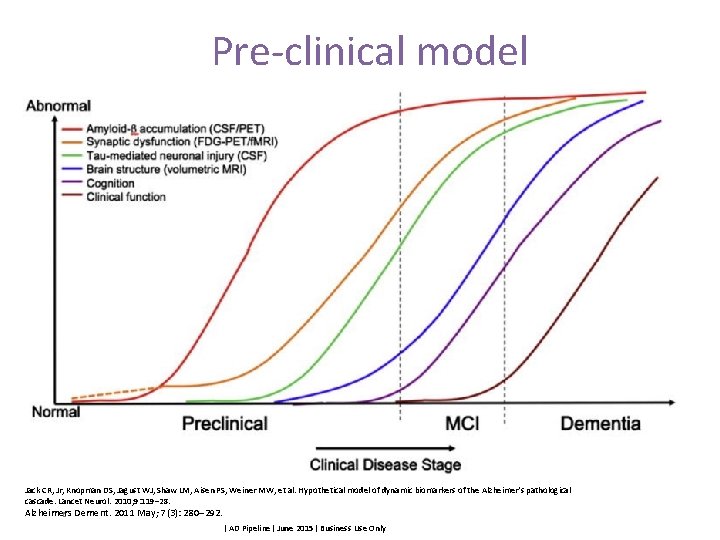
17 -23 yrs CDR 1 Preclinical Stage 1 Biomarker magnitude Abnormal 2 3 5 -8 yrs 9 -12 yrs 1 -3 yrs 1 -2 yrs Ab Amyloid Neuronal Injury Cognitive Symptoms Cut-points Normal Cognitively Normal Clinical disease stage MCI Dementia
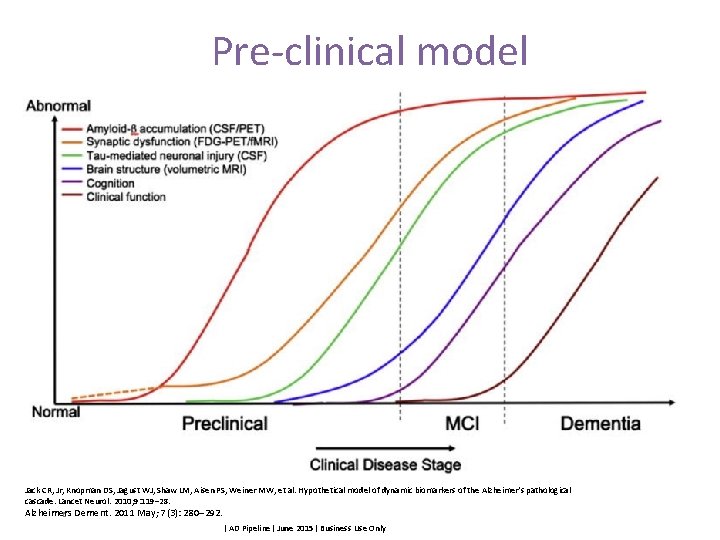
Pre-clinical model Jack CR, Jr, Knopman DS, Jagust WJ, Shaw LM, Aisen PS, Weiner MW, et al. Hypothetical model of dynamic biomarkers of the Alzheimer's pathological cascade. Lancet Neurol. 2010; 9: 119– 28. Alzheimers Dement. 2011 May; 7(3): 280– 292. 6 | AD Pipeline| June 2015| Business Use Only
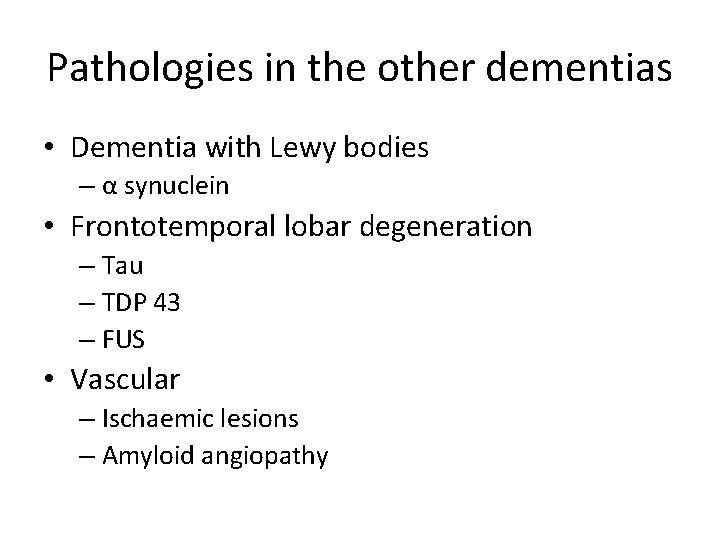
Pathologies in the other dementias • Dementia with Lewy bodies – α synuclein • Frontotemporal lobar degeneration – Tau – TDP 43 – FUS • Vascular – Ischaemic lesions – Amyloid angiopathy
New diagnostic paradigms • Preclinical AD • MCI due to AD • Other MCI – Prodromal DLB – Prodromal FTLD – Non-specified • AD – – Amnestic (limbic) Frontal variant Logopenic aphasia Posterior cortical atrophy
New diagnostic paradigms • FTLD – behavioural – language • Semantic aphasia • Primary progressive non-fluent aphasia – Motor • Lewy Body Disorders – Dementia with Lewy Bodies – Parkinson’s Disease with Dementia • Vascular Cognitive Impairment – Vascular Dementia – Mixed dementias – Incidental comorbidity
DIAGNOSTIC ADVANCES § Neuroimaging § MRI § PET § FDG § PIB / other amyloid ligands § Tau imaging § Biomarkers § CSF § Plasma § Other diagnostic advances

Lancet Neurol 2002

Lancet Neur 2002 Lancet Neurol 2002
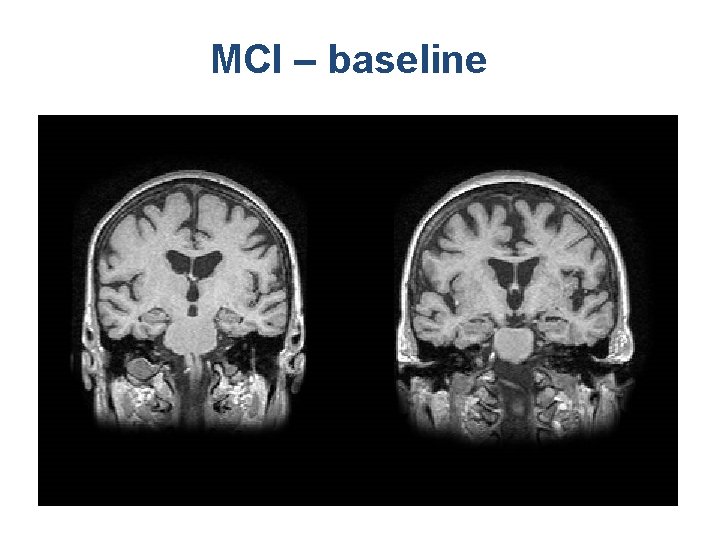
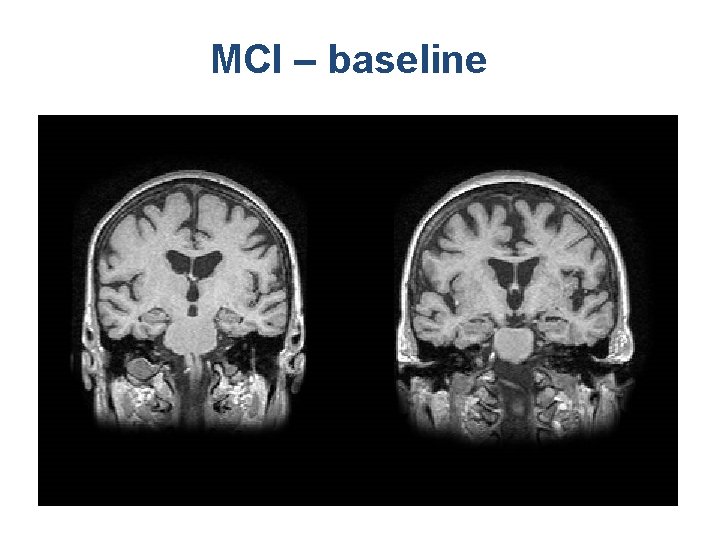
MCI – baseline
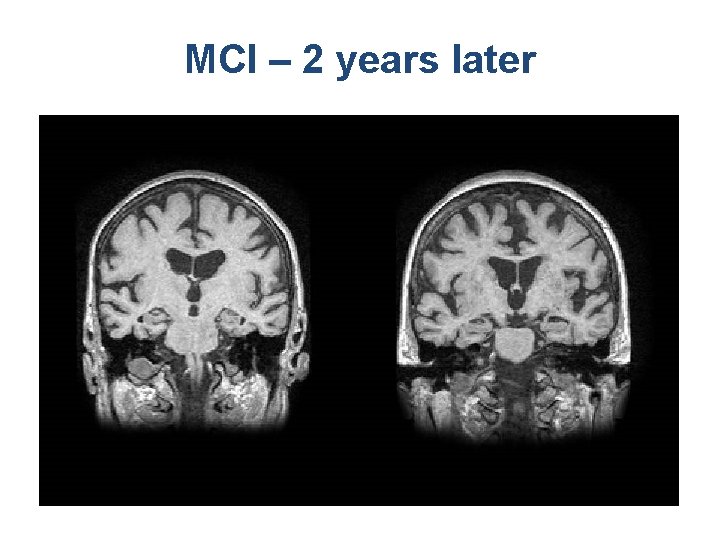
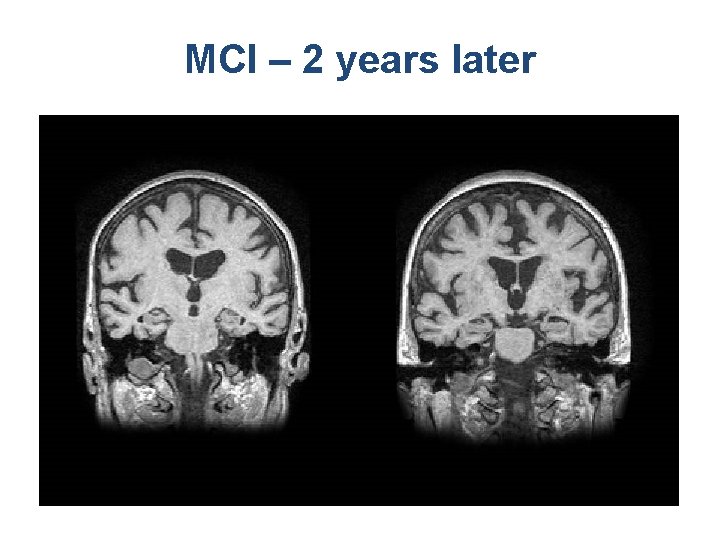
MCI – 2 years later

Small vessel disease

ARWMC predicts disability Change on IADL scale (> 1 item) at 1 yr by ARWMC grade Inzitari, Arch Internal Med 2007
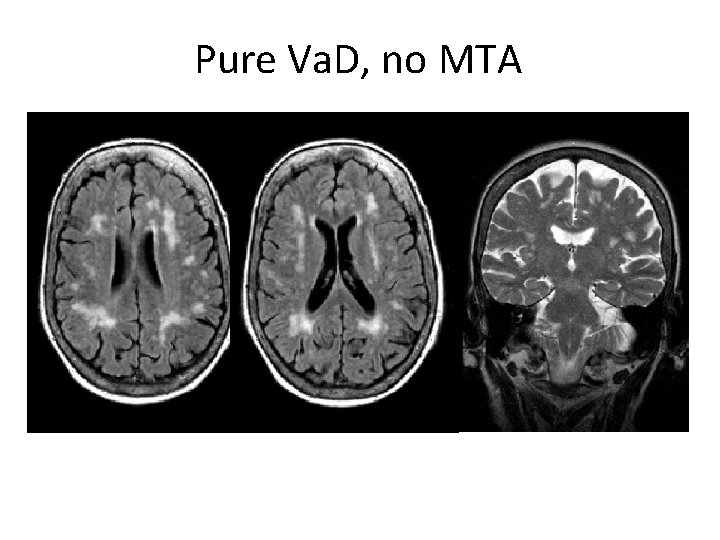
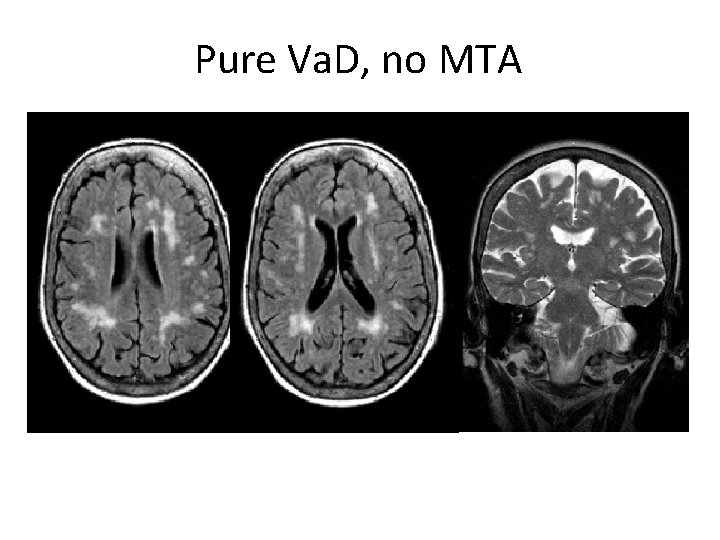
Pure Va. D, no MTA
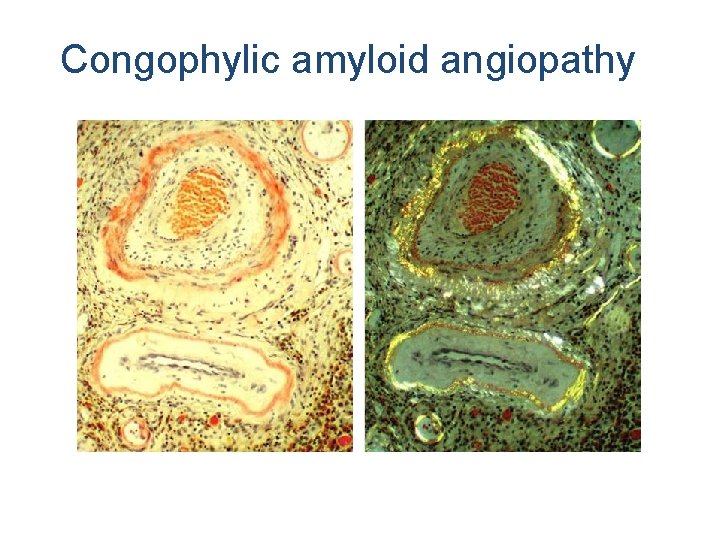
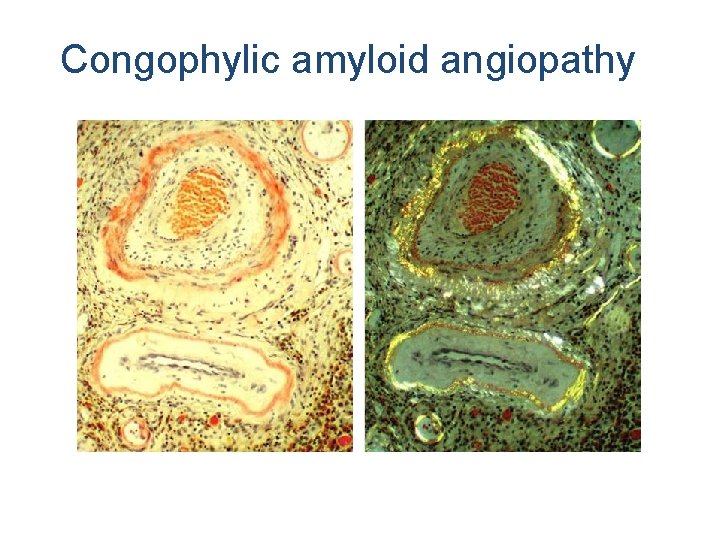
Congophylic amyloid angiopathy
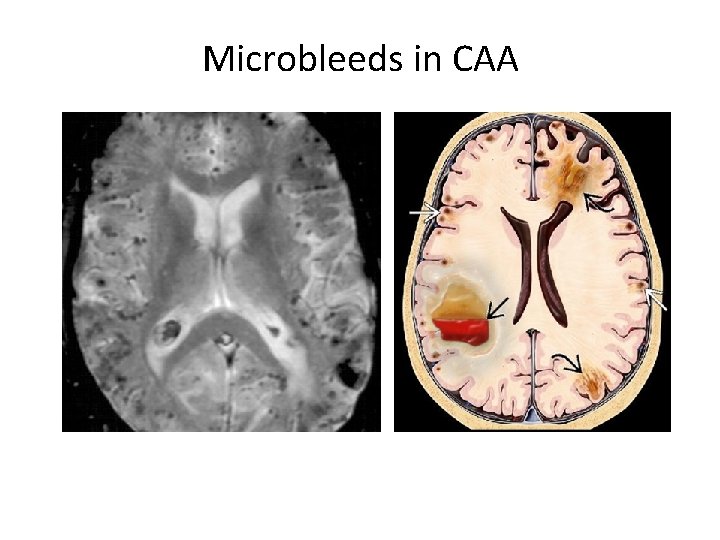
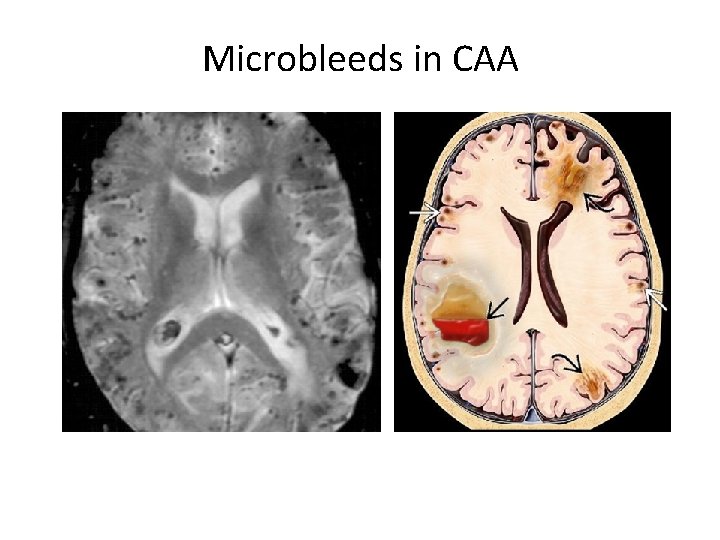
Microbleeds in CAA
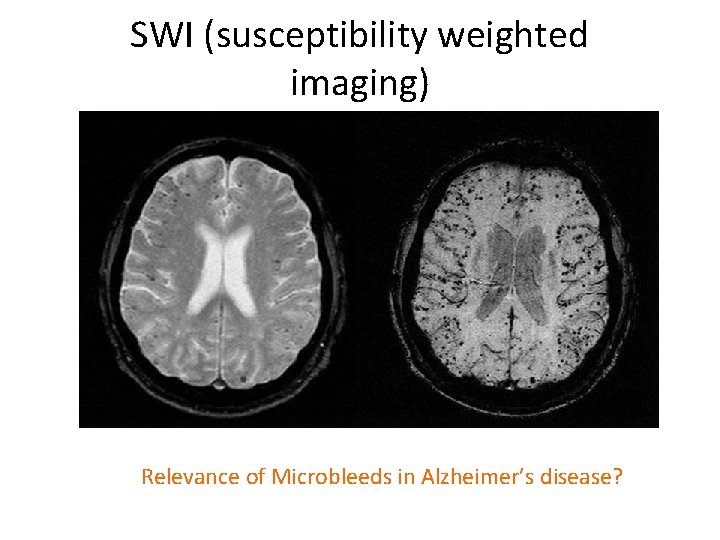
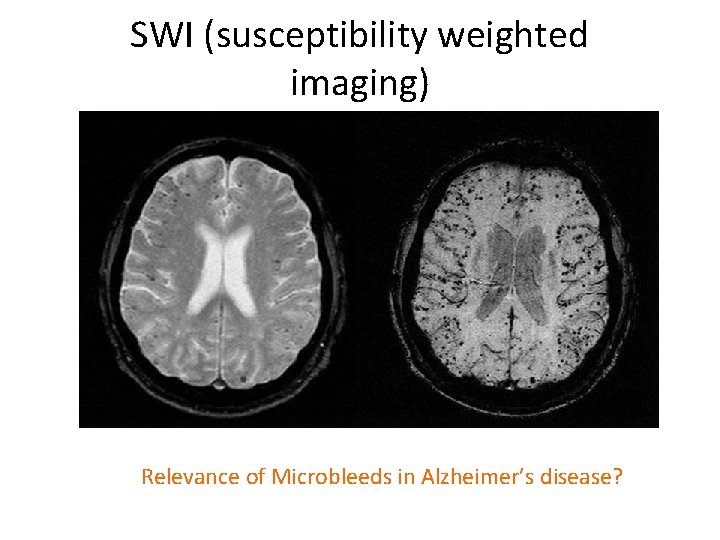
SWI (susceptibility weighted imaging) Relevance of Microbleeds in Alzheimer’s disease?
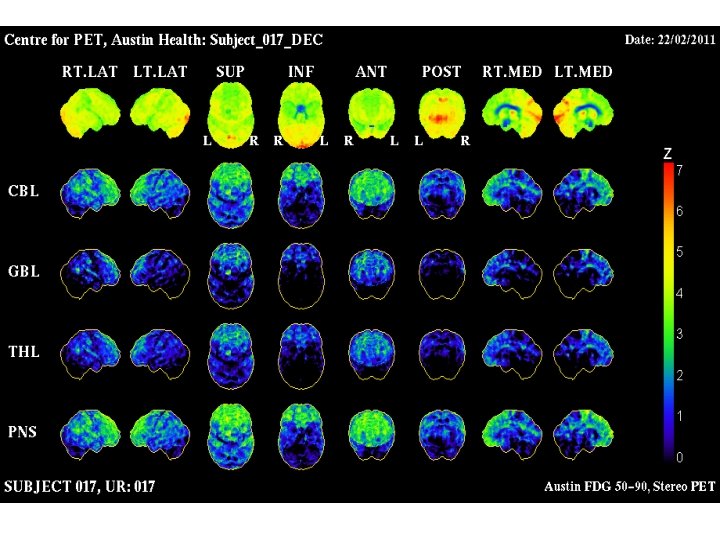
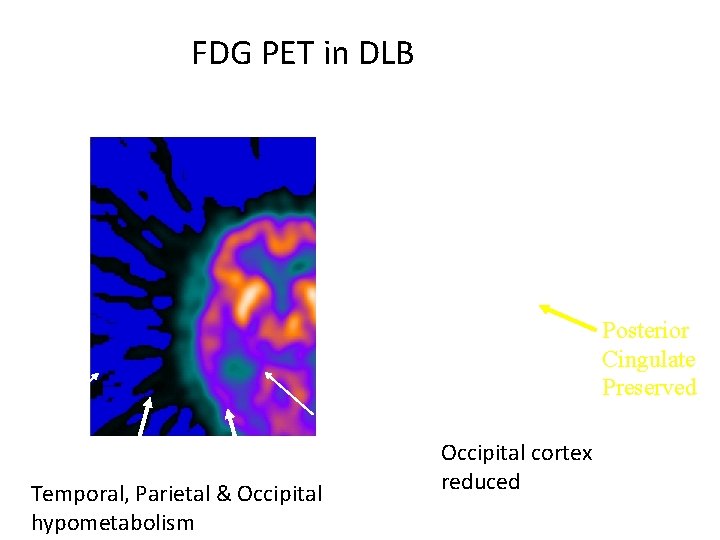
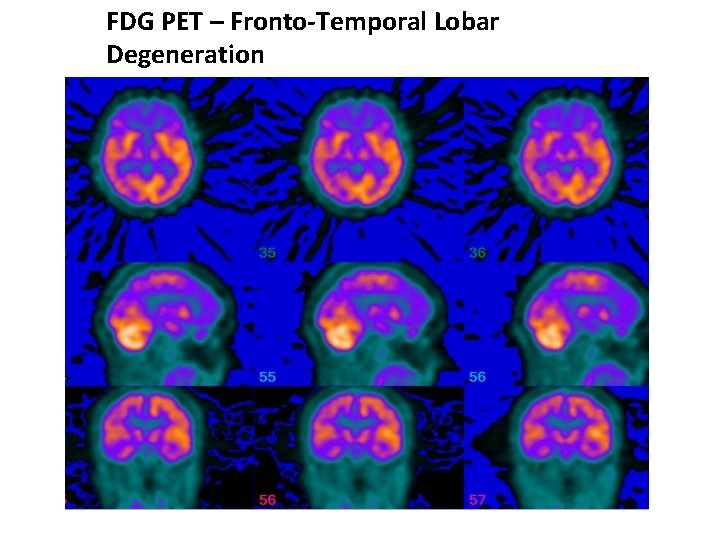
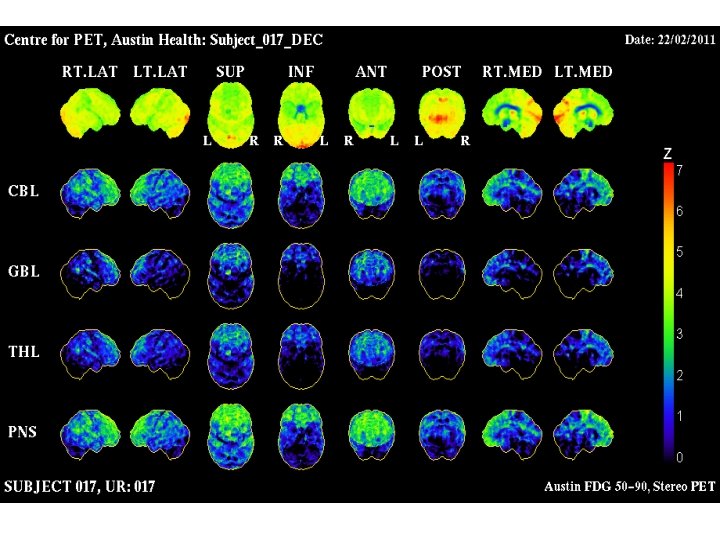
PET scanning • SPECT has only limited value • More sites now offering PET – Fluro Deoxy Glucose (FDG)-PET – Amyloid imaging • Pittsburg Compound B (Pi. B) • New fluorinated compounds have half life that allows them to shipped to sites without cyclotron – You need a cyclotron for 11 C Pi. B – Tau imaging
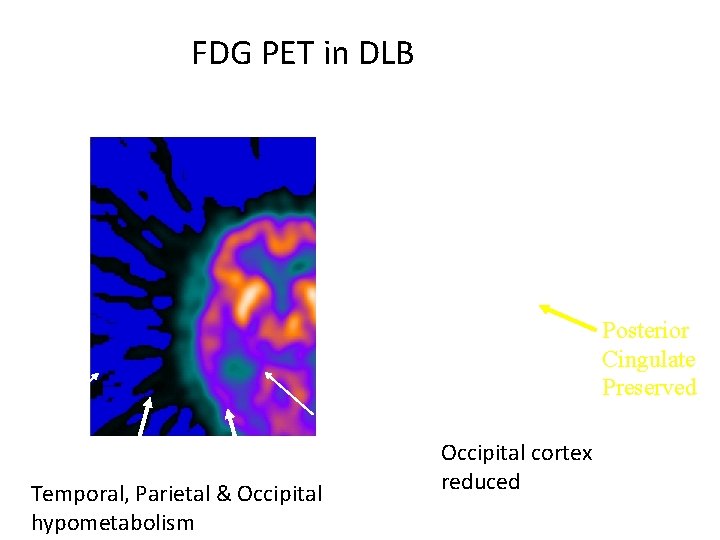
FDG PET in DLB Posterior Cingulate Preserved Temporal, Parietal & Occipital hypometabolism Occipital cortex reduced
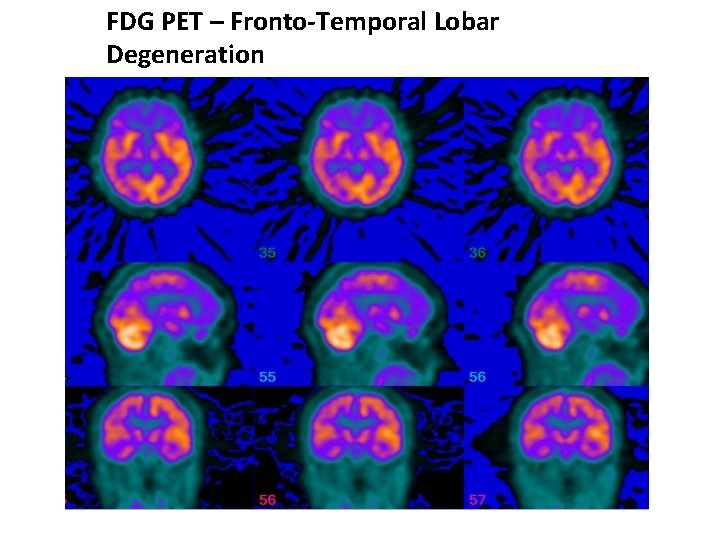
FDG PET – Fronto-Temporal Lobar Degeneration
POTENTIAL ROLES FOR AMYLOID IMAGING • Accurate diagnosis of AD • Early diagnosis and intervention when minimally impaired • Subject selection for anti-Aβ trials • Monitor the effectiveness of anti-Aβ therapy
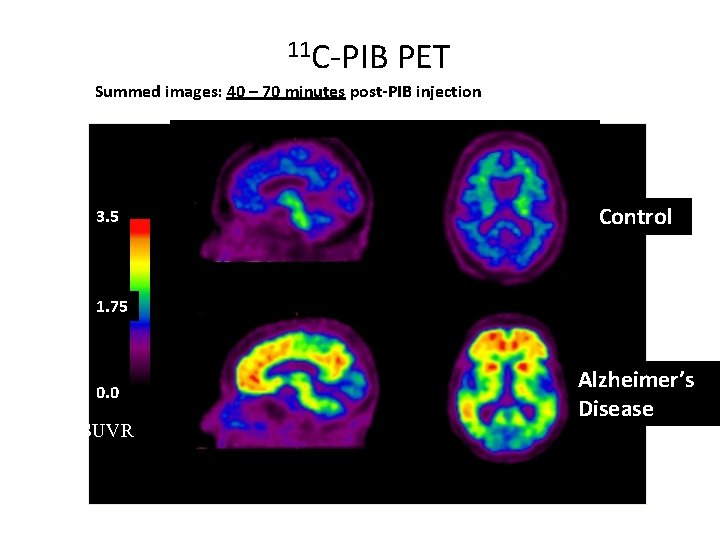
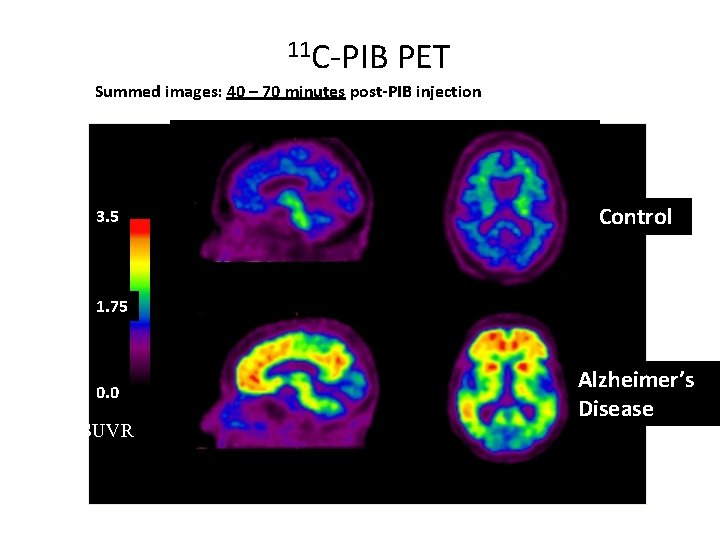
11 C-PIB PET Summed images: 40 – 70 minutes post-PIB injection 3. 5 Control 1. 75 0. 0 SUVR Alzheimer’s Disease
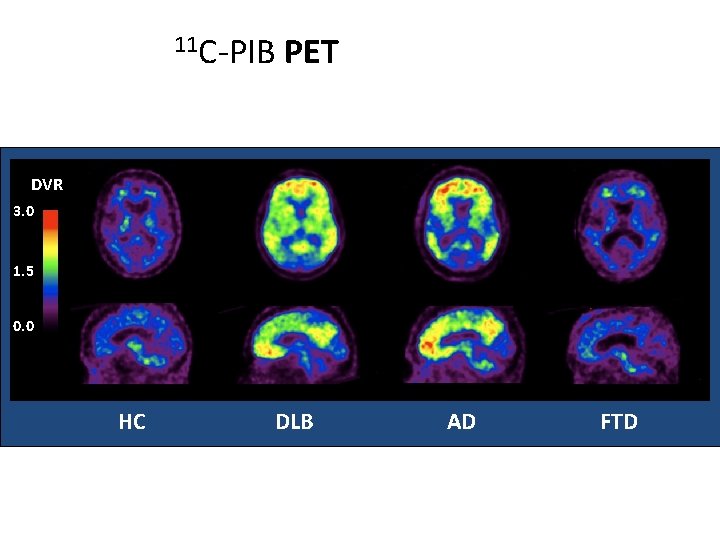
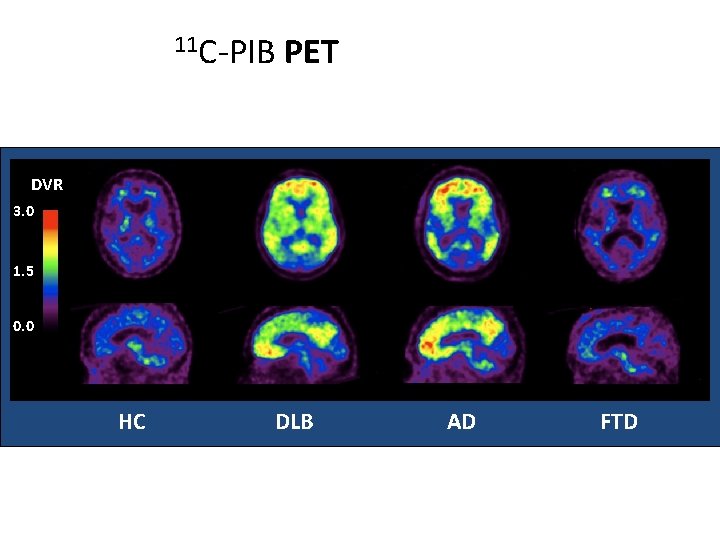
11 C-PIB PET DVR 3. 0 1. 5 0. 0 HC DLB AD FTD
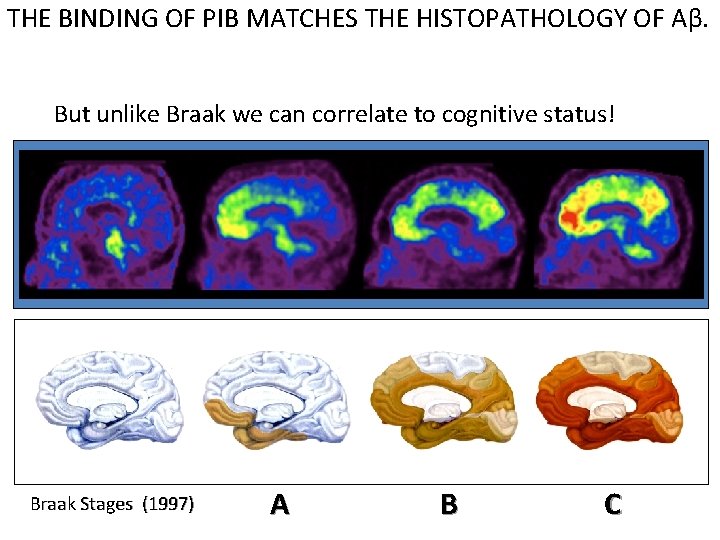
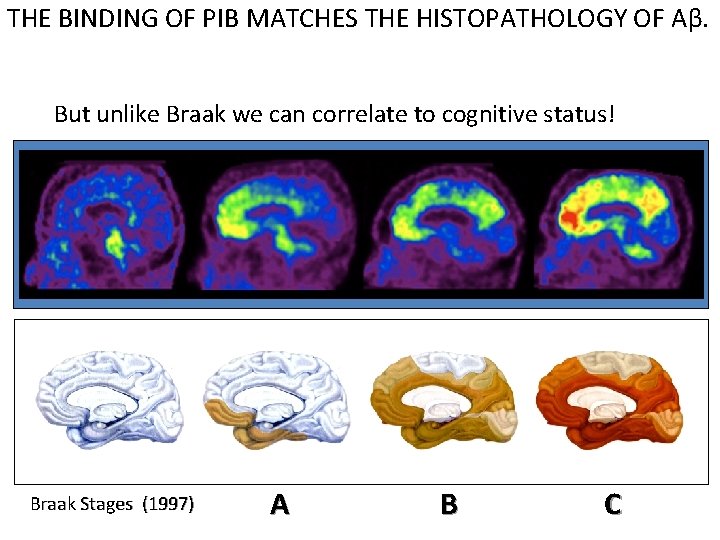
THE BINDING OF PIB MATCHES THE HISTOPATHOLOGY OF Aβ. But unlike Braak we can correlate to cognitive status! Braak Stages (1997) A B C
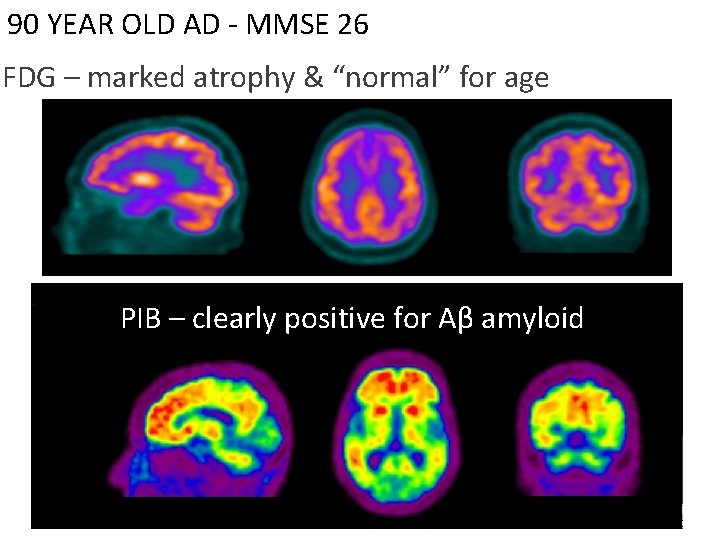
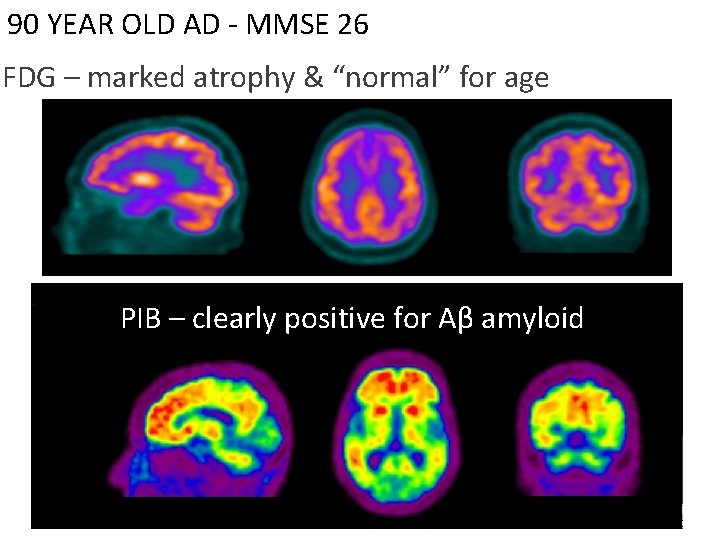
90 YEAR OLD AD - MMSE 26 FDG – marked atrophy & “normal” for age PIB – clearly positive for Aβ amyloid
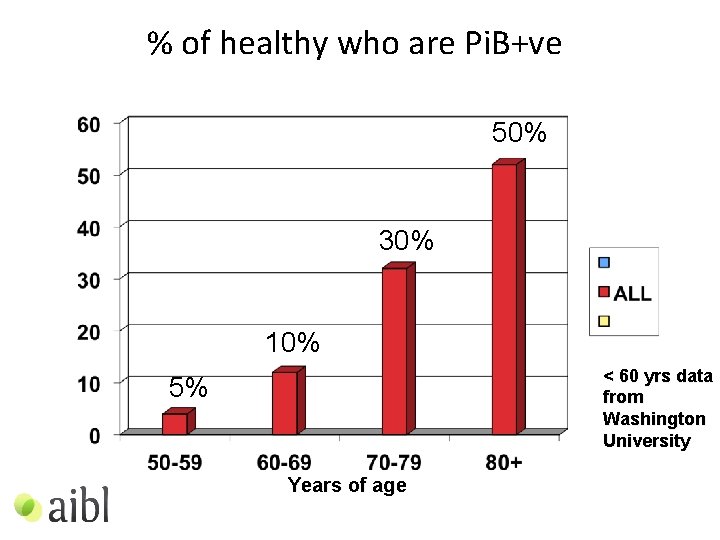
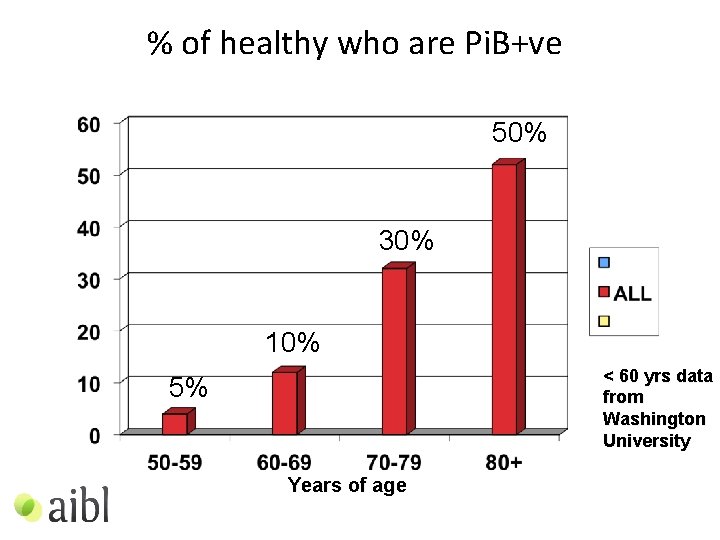
% of healthy who are Pi. B+ve 50% 30% 10% < 60 yrs data from Washington University 5% Years of age
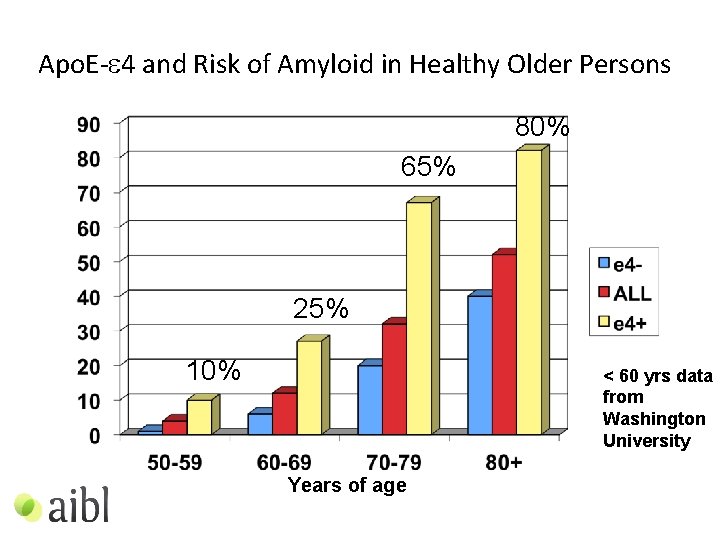
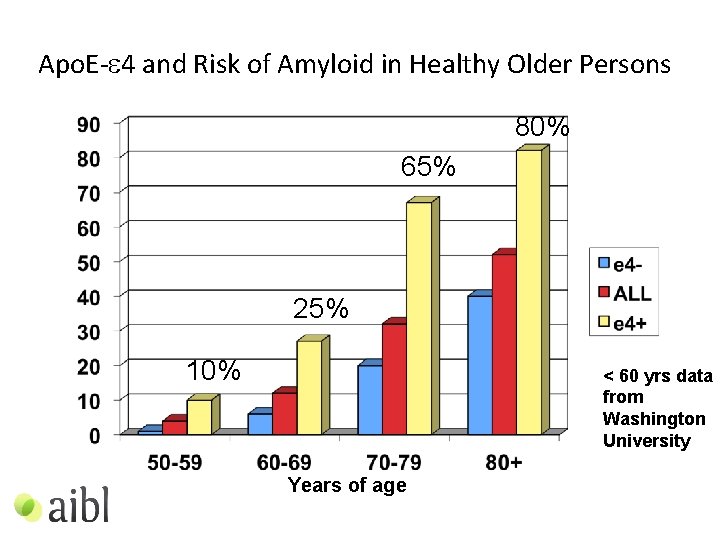
Apo. E-e 4 and Risk of Amyloid in Healthy Older Persons 80% 65% 25% 10% < 60 yrs data from Washington University Years of age
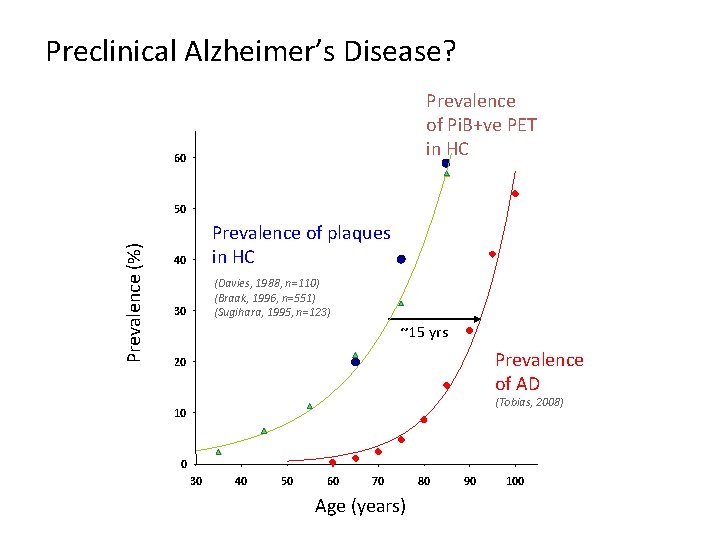
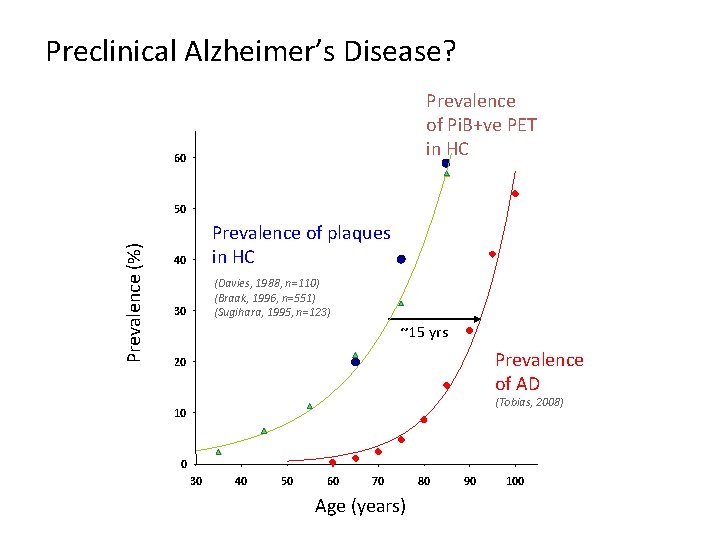
Preclinical Alzheimer’s Disease? Prevalence of Pi. B+ve PET in HC 60 Prevalence (%) 50 40 Prevalence of plaques in HC 30 (Davies, 1988, n=110) (Braak, 1996, n=551) (Sugihara, 1995, n=123) ~15 yrs Prevalence of AD 20 (Tobias, 2008) 10 0 30 40 50 60 70 Age (years) 80 90 100
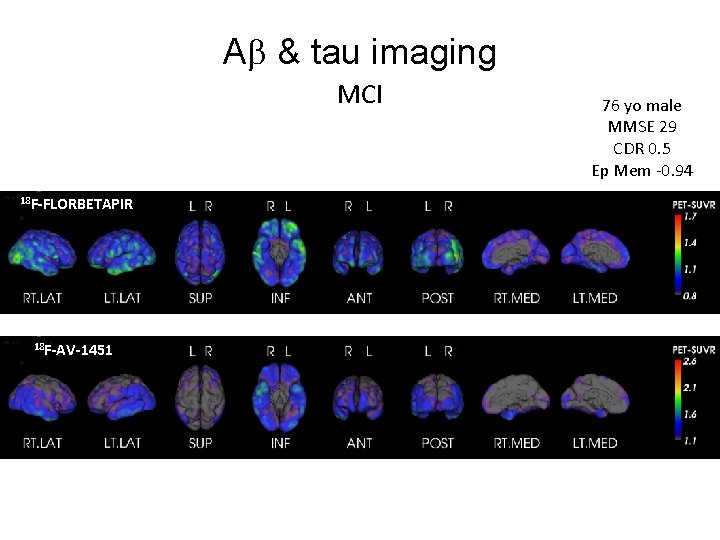
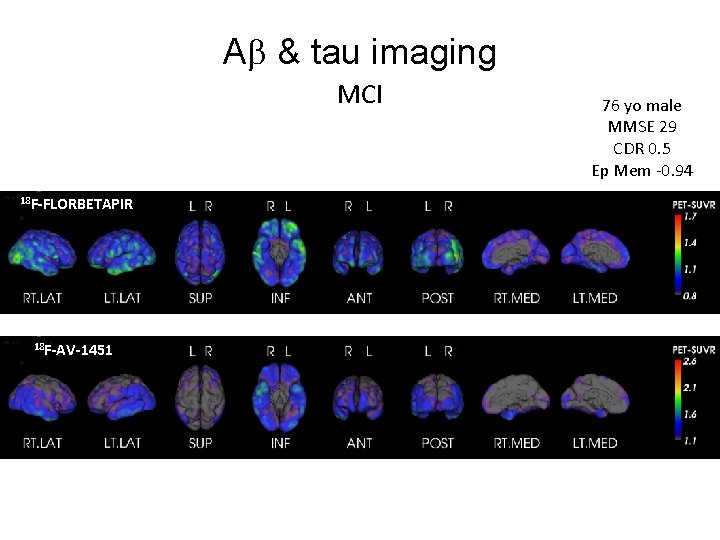
A & tau imaging MCI 18 F-FLORBETAPIR 18 F-AV-1451 76 yo male MMSE 29 CDR 0. 5 Ep Mem -0. 94
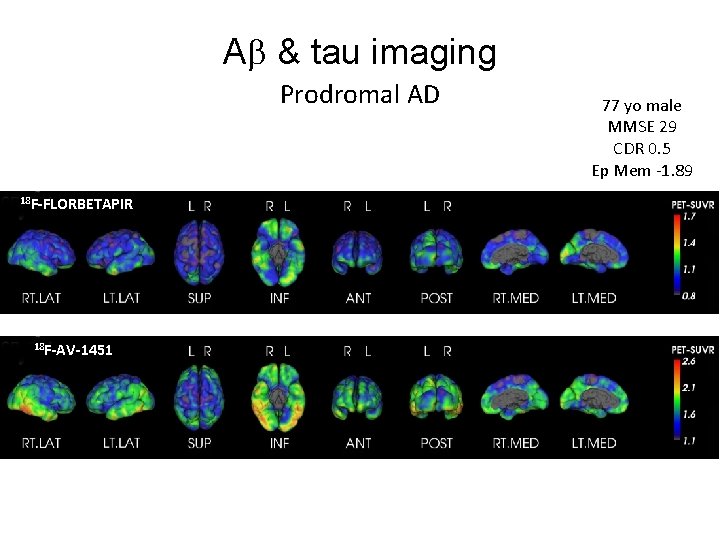
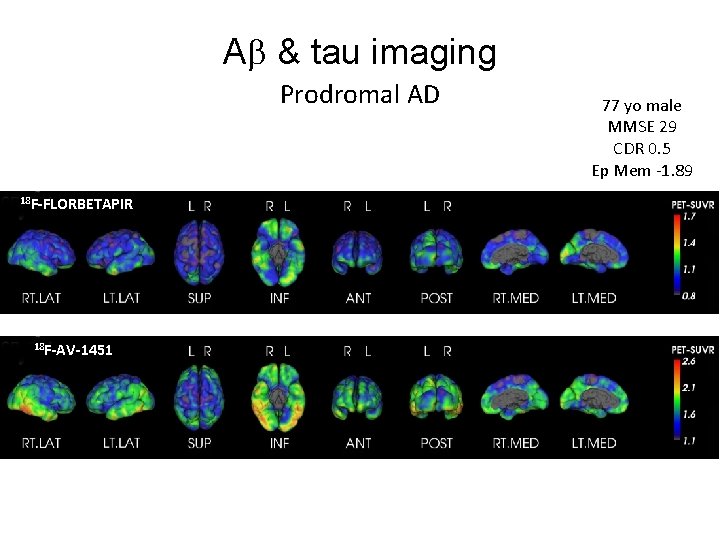
A & tau imaging MCI Prodromal AD 18 F-FLORBETAPIR 18 F-AV-1451 77 yo male MMSE 29 CDR 0. 5 Ep Mem -1. 89

A and tau imaging in the diagnosis of dementia 74 yo male e 4/e 3 MMSE=27; CDR=1; CDR So. B=3. 0 Composite memory = -3. 92; Composite non-memory = -2. 34 HADS-D = 3; HADS-A = 5 18 F-FLUTEMETAMOL 18 F-THK 5351 AD
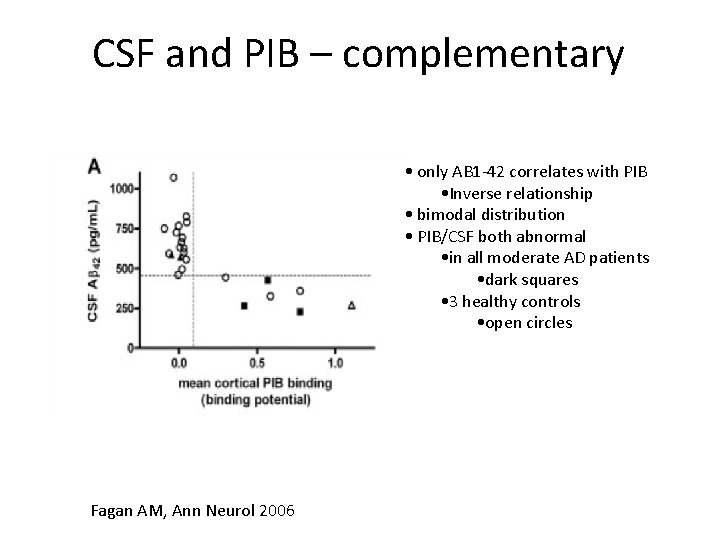
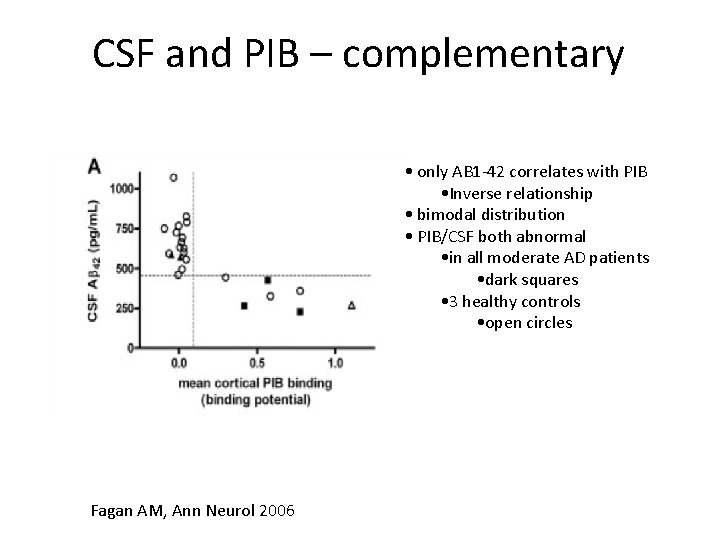
CSF and PIB – complementary • only AB 1 -42 correlates with PIB • Inverse relationship • bimodal distribution • PIB/CSF both abnormal • in all moderate AD patients • dark squares • 3 healthy controls • open circles Fagan AM, Ann Neurol 2006
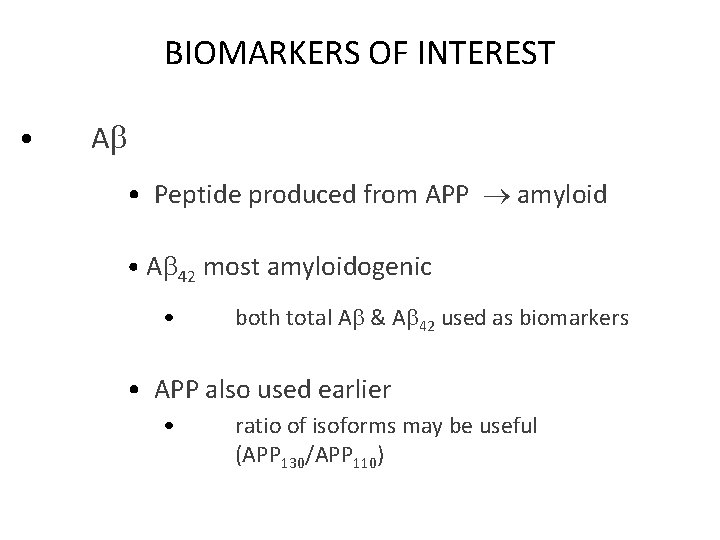
BIOMARKERS OF INTEREST • A • Peptide produced from APP amyloid • A 42 most amyloidogenic • both total A & A 42 used as biomarkers • APP also used earlier • ratio of isoforms may be useful (APP 130/APP 110)

BIOMARKERS OF INTEREST • Tau • main protein in neurofibrillary tangles • in healthy neurones, tau stabilises axonal microtubules • when abnormally hyperphosphorylated, tau dissociated from microtubules and self assembles into paired helical filaments • two forms used as biomarkers • total tau (T-tau) • (hyper) phospho tau (P-tau) • • phosphorylation at threonine 181 usually used 199 & 231 also studied
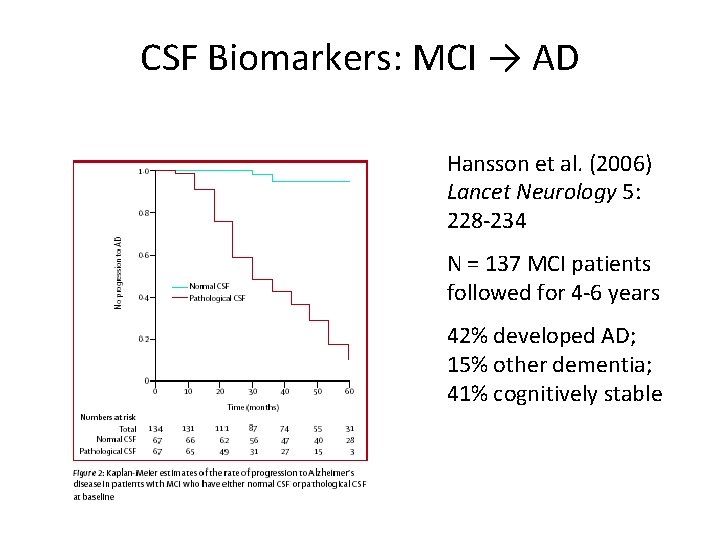
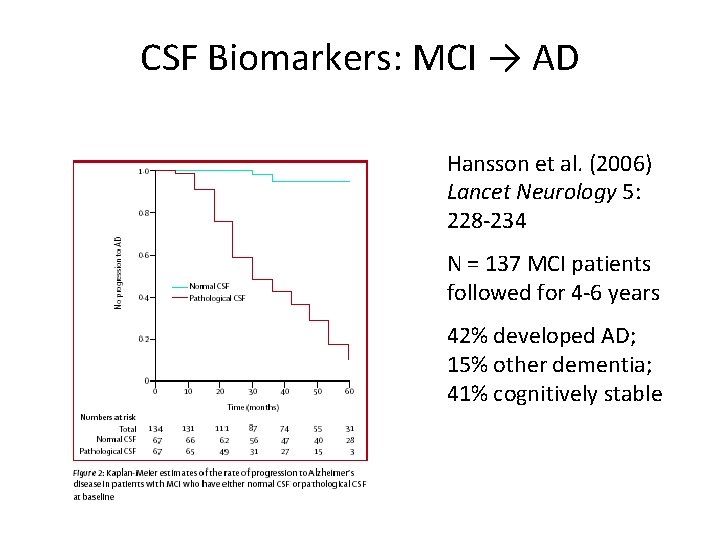
CSF Biomarkers: MCI → AD Hansson et al. (2006) Lancet Neurology 5: 228 -234 N = 137 MCI patients followed for 4 -6 years 42% developed AD; 15% other dementia; 41% cognitively stable
CSF BIOMARKERS IN OTHER DEMENTIAS • Aβ 42/tau useful in differentiating FTLD from AD 1. • Alpha-synuclein initially thought not useful in differentiating DLB from AD 2 – 1. 2. 3. more recently, found useful 3 Bian et al. Neurology 2008: 70: 1827 -35 Noguchi-Shinohars. Brain Research 2008 Nov 28 (Epub) Lancet Neurology 2011
BIOMARKERS - BLOOD • Aβ and tau being evaluated in diagnosis of AD - eg in AIBL study - but marked fluctuations in individuals • Others promising - eg heat shock protein 70 in vascular MCI combinations look more promising • Proteomics being used to develop more plasma biomarkers • May be also useful in predicting conversion from non demented to demented - eg total plasma amyloid 1. , 2. - eg plasma Aβ 3. 42 1. Lopez et al. Neurology 2008: 70: 1664 -71 2. Sundelöf J et al. Arch Neurol 2008; 65: 256 -63 3. Ringman et al. Neurology 2008; 71: 85 -92
Other research techniques for early diagnosis • • Retinal amyloid Other retinal techniques EEG Assessment of smell
Approaches to preventing dementia • • • Physical activity Mental stimulation Social interaction Diet Modify cardiovascular risk factors

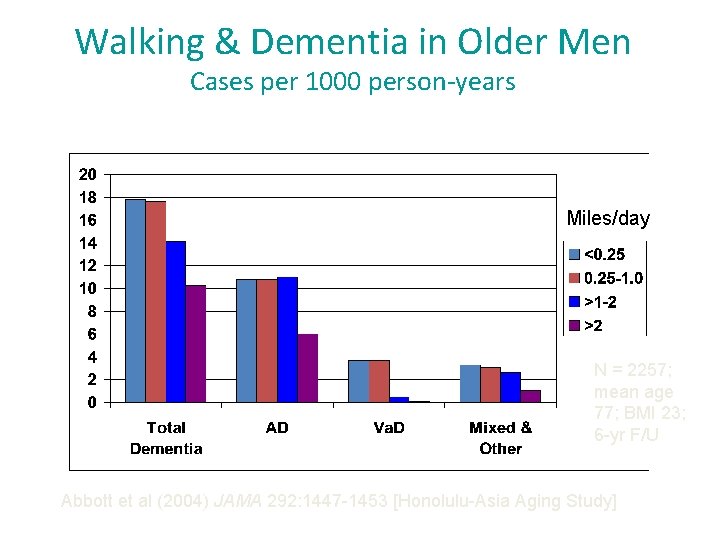
Physical Activity Some studies have shown that greater physical activity preserves cognitive function - eg Women Who Walk project 1 5, 925 woman over age 65 no cognitive impairment at baseline follow up 6 -8 years NEW COGNITIVE IMPAIRMENT (%) ACTIVITY LEVEL 1. Yaffe et al. Arch Intern Med 2001; 161: 1703 -8
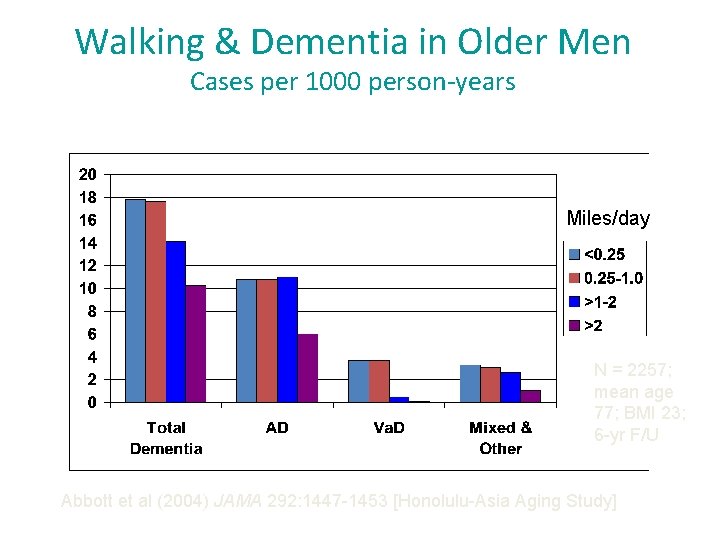
Walking & Dementia in Older Men Cases per 1000 person-years Miles/day N = 2257; mean age 77; BMI 23; 6 -yr F/U Abbott et al (2004) JAMA 292: 1447 -1453 [Honolulu-Asia Aging Study]

Lifestyle Factors for Prevention of Dementia • Great interest in population measures to reduce or delay onset of dementia – Delaying onset of dementia by 1 year could lead reduce global prevalence by 9. 2 million individuals by 2050 (Brookmeyer 2007) – An estimated 1/3 of AD cases worldwide attributable to seven potentially-modificable Risk Factors (Norton 2014) – Diabetes, Midlife Hypertension, Midlife Obesity, Physical Inactivity, Depression, Smoking and Low Educational Attainment – Worldwide – low educational attainment greatest populationattributable risk (PAR) = 19% – USA – physical inactivity greatest PAR = 21%
Are we already winning? • Age-specific prevalence of dementia reported to be falling in some populations – 2005 Duke, USA – prevalence of severe cognitive impairment fell between 1982 and 1999 – 2013 Cognitive Function and Ageing Study (CFAS, UK) • 2 cohorts of >65 year-olds assessed 20 years apart (1990 -93, 2008 -11) • 24% decrease in prevalence of dementia (Odds Ratio 0. 7 [95% C. I. 0. 6 -0. 9, p=0. 003) in the later cohort – 2013 Christensen et al (Denmark) • Compared individuals born in 1905 (at age 93, n=2262), to those born in 1915 (at age 95, n=1584). • More recent (1915) cohort scored higher on cognitive tasks and ADL scores (plus more lived longer) Manton 2005, Matthews 2013, Christensen 2013
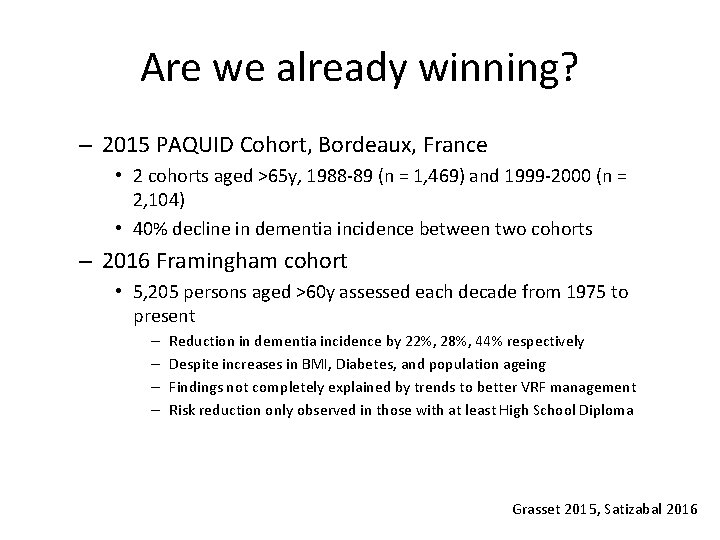
Are we already winning? – 2015 PAQUID Cohort, Bordeaux, France • 2 cohorts aged >65 y, 1988 -89 (n = 1, 469) and 1999 -2000 (n = 2, 104) • 40% decline in dementia incidence between two cohorts – 2016 Framingham cohort • 5, 205 persons aged >60 y assessed each decade from 1975 to present – – Reduction in dementia incidence by 22%, 28%, 44% respectively Despite increases in BMI, Diabetes, and population ageing Findings not completely explained by trends to better VRF management Risk reduction only observed in those with at least High School Diploma Grasset 2015, Satizabal 2016
Why is it so? • • • Better education? Early childhood factors? Sanitation/primary care? Treatment of vascular risk factors? Smoking? – Statins – Antihypertensive medications • Other factors? N. B. HOWEVER – global prevalence still predicted to increase over coming decades • Greatest burden of dementia in lower socioeconomic countries

INCLUSION CRITERIA: persons at risk of dementia/cognitive decline Ø Dementia Risk score > 6 points Based on risk factors assessed in earlier population surveys: Age, Education, Sex, Blood pressure, Cholesterol, BMI, Physical Activity (Kivipelto et al. , Lancet Neurology 2006) AND Ø Cognitive performance at mean level or slightly lower than expected for age (based on CERAD test battery) Kivipelto et al. , Alzheimer & Dementia 2013

Ngandu 2015
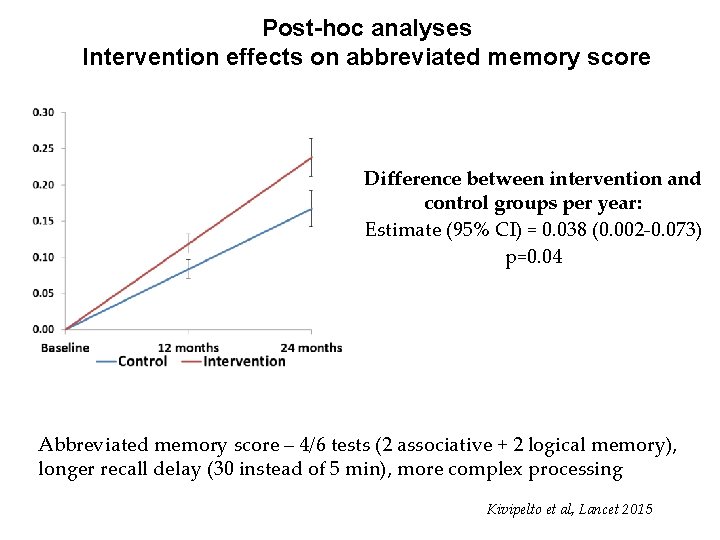
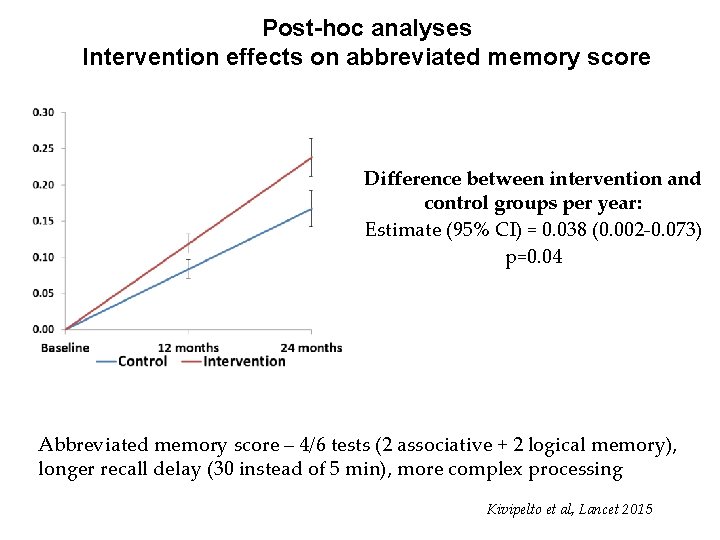
Post-hoc analyses Intervention effects on abbreviated memory score Difference between intervention and control groups per year: Estimate (95% CI) = 0. 038 (0. 002 -0. 073) p=0. 04 Abbreviated memory score – 4/6 tests (2 associative + 2 logical memory), longer recall delay (30 instead of 5 min), more complex processing Kivipelto et al, Lancet 2015
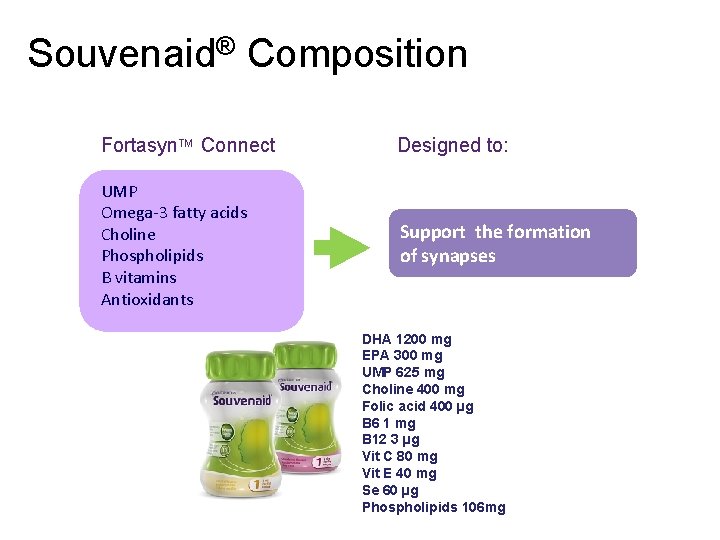
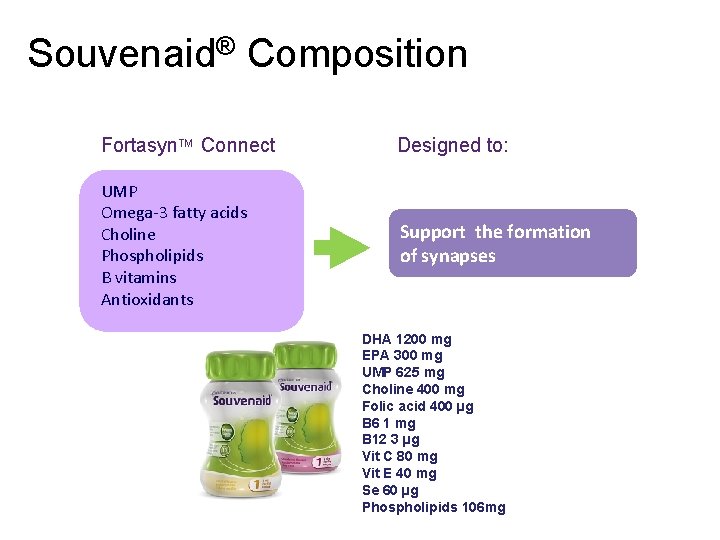
Souvenaid® Composition Fortasyn. TM Connect Designed to: UMP Omega-3 fatty acids Choline Phospholipids B vitamins Antioxidants Support the formation of synapses DHA 1200 mg EPA 300 mg UMP 625 mg Choline 400 mg Folic acid 400 µg B 6 1 mg B 12 3 µg Vit C 80 mg Vit E 40 mg Se 60 µg Phospholipids 106 mg

Souvenir II: Primary endpoint Significant effect on NTB memory domain over 24 weeks (whole period trajectory; p=0. 023) p = 0. 006 Statistical analysis re-run by Rush Alzheimer’s Disease Center ITT, Mixed Model for Repeated Measures (trajectory, mean ± SE)

Study design Lipi. Diet Clinical Trial: Study Design Objective: To investigate the effects of a medical food in prodromal AD in a double-blind, placebo-controlled study on cognition, biomarkers in plasma, CSF and atrophy rate on MRIs • • • E. U. funded project run by 16 centre independent consortium 24 -month randomised, controlled, double-blind, parallel-group, multicentre multi-country study with three optional 12 -month double-blind extension studies 300 subjects with prodromal AD (criteria of Dubois et al. 2007) Contact: www. lipididiet. eu Dubois et al. Lancet Neurol. 2007.
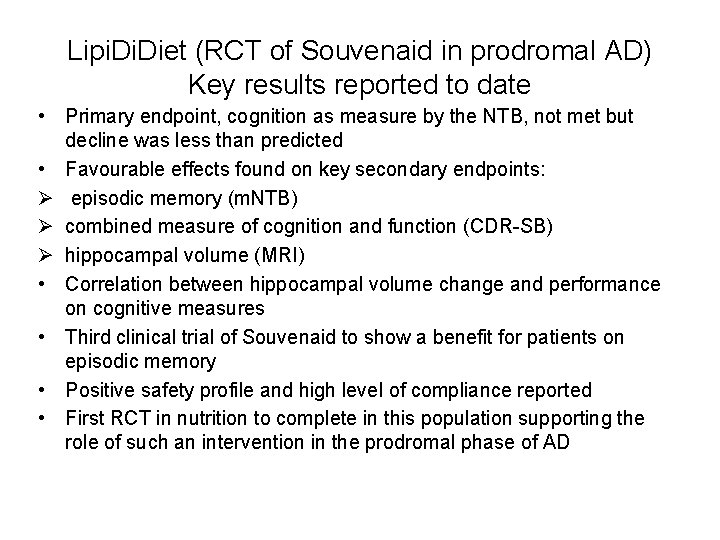
Lipi. Diet (RCT of Souvenaid in prodromal AD) Key results reported to date • Primary endpoint, cognition as measure by the NTB, not met but decline was less than predicted • Favourable effects found on key secondary endpoints: Ø episodic memory (m. NTB) Ø combined measure of cognition and function (CDR-SB) Ø hippocampal volume (MRI) • Correlation between hippocampal volume change and performance on cognitive measures • Third clinical trial of Souvenaid to show a benefit for patients on episodic memory • Positive safety profile and high level of compliance reported • First RCT in nutrition to complete in this population supporting the role of such an intervention in the prodromal phase of AD
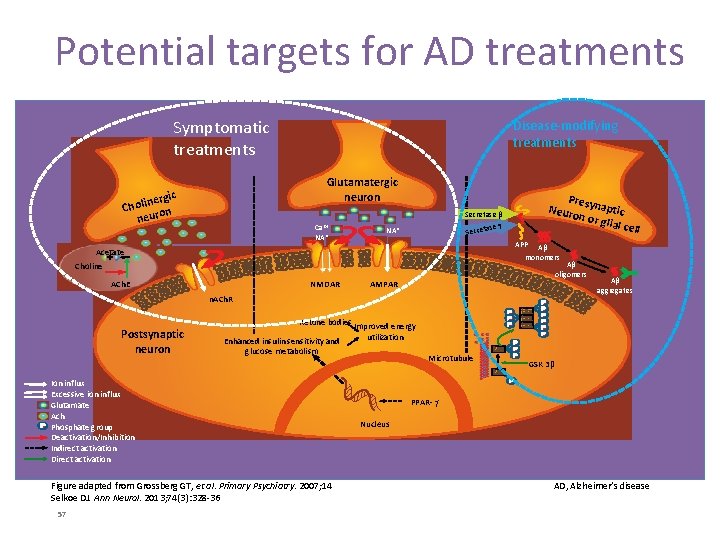
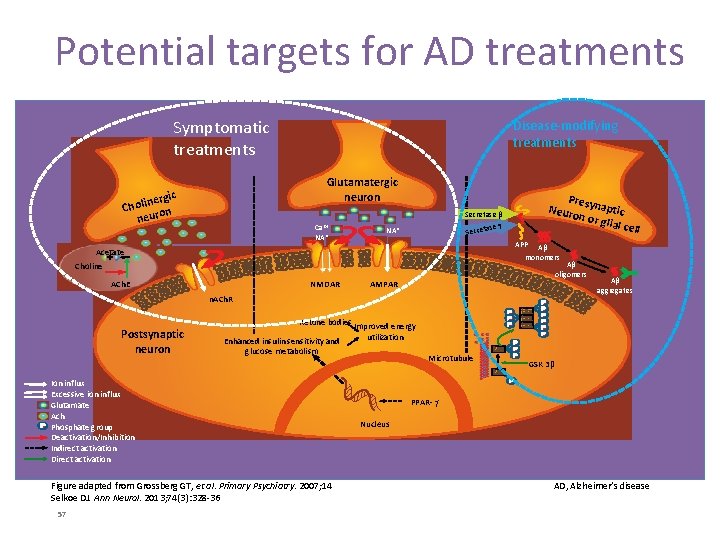
Potential targets for AD treatments Symptomatic treatments Disease-modifying treatments Glutamatergic neuron c nergi i l o h C on neur Ca 2+ NA* Pres Neuro ynaptic n or g lial ce ll Secretase β ase Secret NA* APP Aβ monomers Acetate Aβ oligomers Choline ACh. E NMDAR AMPAR n. ACh. R Postsynaptic neuron Ketone bodies Improved energy Enhanced insulin sensitivity and glucose metabolism Ion influx Excessive ion influx Glutamate Ach Phosphate group Deactivation/Inhibition Indirect activation Direct activation Figure adapted from Grossberg GT, et al. Primary Psychiatry. 2007; 14 Selkoe DJ. Ann Neurol. 2013; 74(3): 328 -36 57 Aβ aggregates utilization Microtubule GSK 3β PPAR- Nucleus AD, Alzheimer’s disease
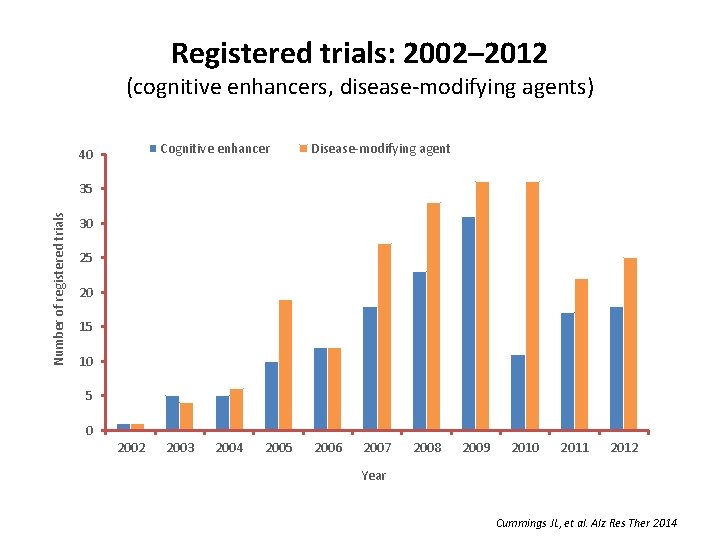
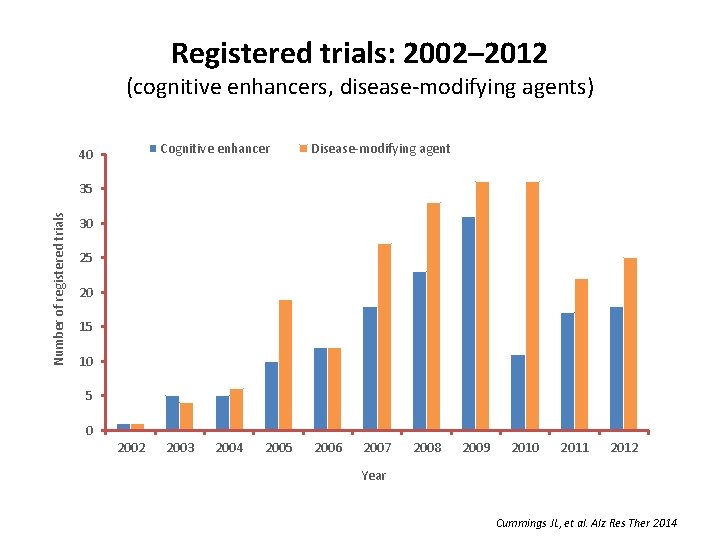
Registered trials: 2002– 2012 (cognitive enhancers, disease-modifying agents) Cognitive enhancer 40 Disease-modifying agent Number of registered trials 35 30 25 20 15 10 5 0 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 Year Cummings JL, et al. Alz Res Ther 2014
Symptomatic Therapies • 5 HT 6 antagonists – Lundbeck • Negative results recently – AXOVANT – Pfizer, sold on to an Indian company • Histamine 3 receptor antagonists – All trials failed • Others – AZT (sodium chromolyn + NSAID) – Buck (tropisotron)
Disease Modifying Approaches • Target Amyloid – Reduce production • BACE inhibition – Remove or reduce toxicity • m. Ab • Active immunization – Reduce membrane trafficking of aβ • RAGE inhibitors – Prevent aggregation • Target Tau – m. Ab – Reduce hyperphoshorylation • Sodium selenate (recent negative study) – Other • LMTX (prevents tau aggregation- but recent negative study)
Monoclonal Ab’s from Reverse Translational Medicine -the development of aducanumab • From sera of a cohort of individuals with mild cognitive impairment (MCI) that had improved on cognitive testing over time Hock’s Geneva team isolated anti Aβ antibodies – selected ones that bound to aggregated Aβ – using RTM created monoclonal Abs –in transgenic (Tg) mice (genetically changed to overexpress Aβ) these human m. Abs reduced Aβ levels by 50% through activation of microglia –seem to be acting against a conformational epitope of these Aβ aggregates rather than a linear sequence on the monomers –most encouragingly, there was increased dendritic branching and neuronal connectivity, along with neurogenesis. –memory also improved
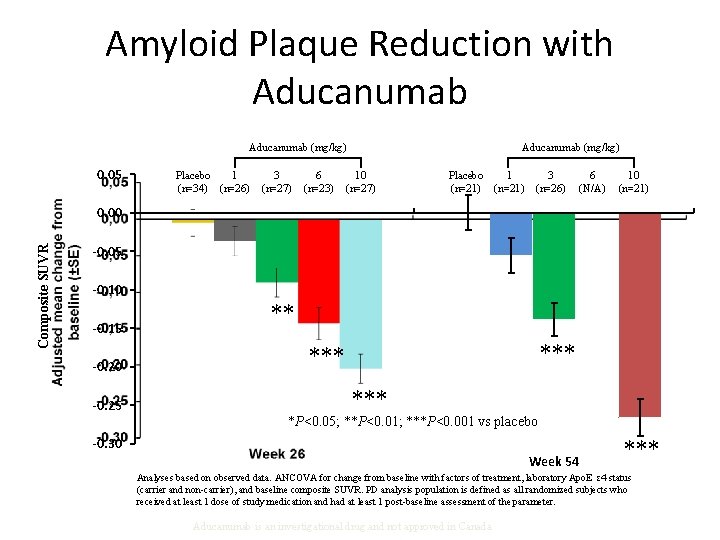
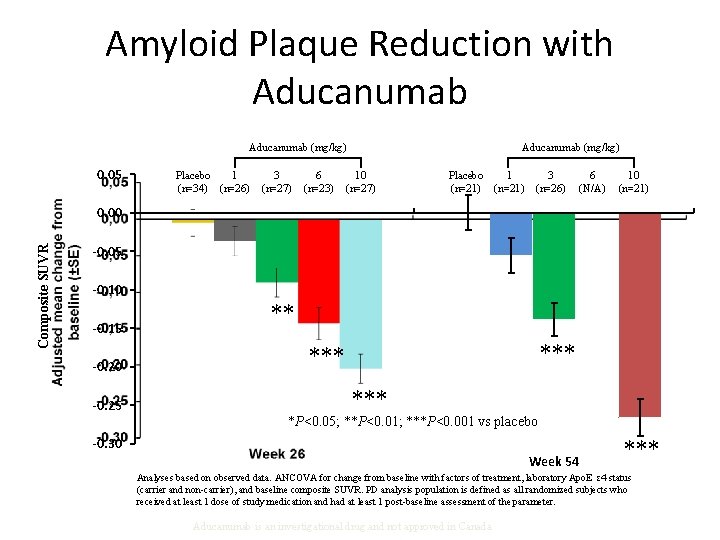
Amyloid Plaque Reduction with Aducanumab (mg/kg) 0. 05 Placebo 1 (n=34) (n=26) 3 (n=27) 6 (n=23) Aducanumab (mg/kg) 10 (n=27) 1 Placebo (n=21) 3 (n=26) 6 (N/A) 10 (n=21) Composite SUVR 0. 00 -0. 05 -0. 10 -0. 15 -0. 20 -0. 25 ** *** *P<0. 05; **P<0. 01; ***P<0. 001 vs placebo -0. 30 Week 54 *** Analyses based on observed data. ANCOVA for change from baseline with factors of treatment, laboratory Apo. E ε 4 status (carrier and non-carrier), and baseline composite SUVR. PD analysis population is defined as all randomized subjects who received at least 1 dose of study medication and had at least 1 post-baseline assessment of the parameter. Aducanumab is an investigational drug and not approved in Canada
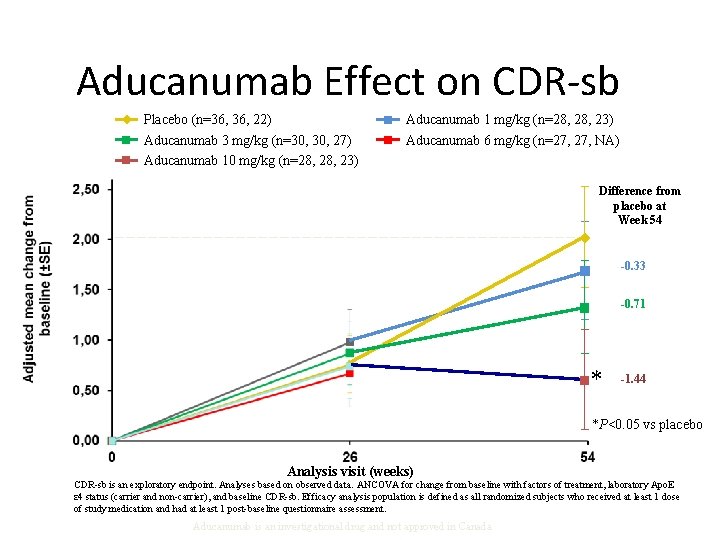
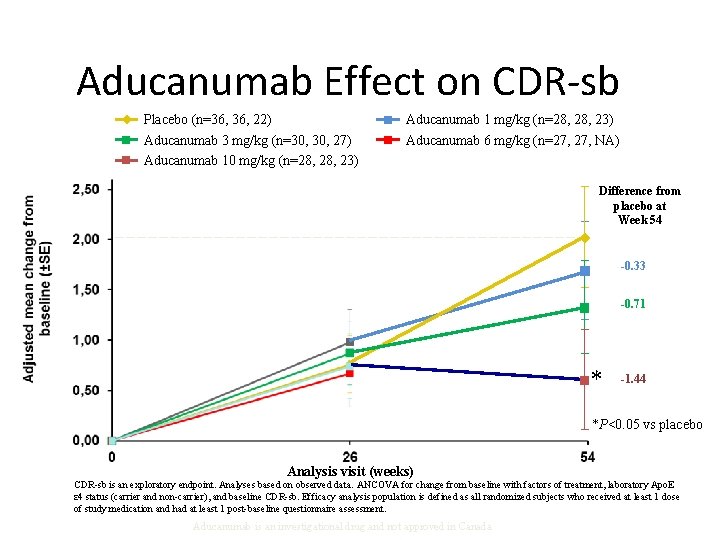
Aducanumab Effect on CDR-sb Placebo (n=36, 22) Aducanumab 3 mg/kg (n=30, 27) Aducanumab 10 mg/kg (n=28, 23) Aducanumab 1 mg/kg (n=28, 23) Aducanumab 6 mg/kg (n=27, NA) Difference from placebo at Week 54 -0. 33 -0. 71 * -1. 44 *P<0. 05 vs placebo Analysis visit (weeks) CDR-sb is an exploratory endpoint. Analyses based on observed data. ANCOVA for change from baseline with factors of treatment, laboratory Apo. E ε 4 status (carrier and non-carrier), and baseline CDR-sb. Efficacy analysis population is defined as all randomized subjects who received at least 1 dose of study medication and had at least 1 post-baseline questionnaire assessment. Aducanumab is an investigational drug and not approved in Canada
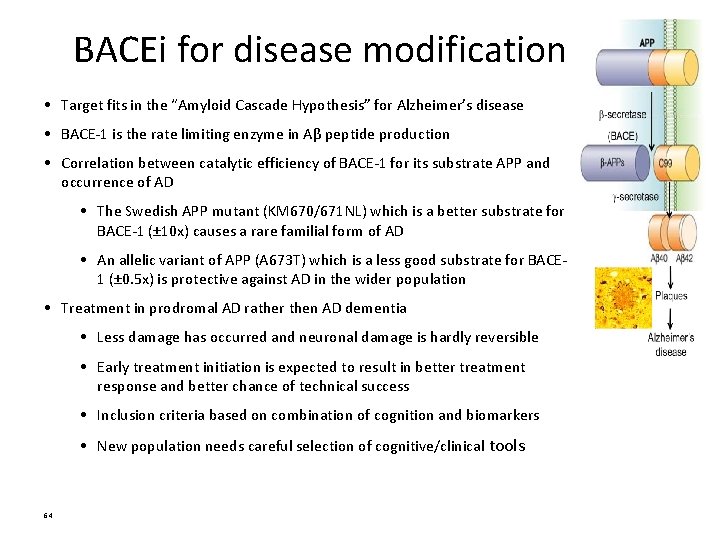
BACEi for disease modification • Target fits in the “Amyloid Cascade Hypothesis” for Alzheimer’s disease • BACE-1 is the rate limiting enzyme in Aβ peptide production • Correlation between catalytic efficiency of BACE-1 for its substrate APP and occurrence of AD • The Swedish APP mutant (KM 670/671 NL) which is a better substrate for BACE-1 (± 10 x) causes a rare familial form of AD • An allelic variant of APP (A 673 T) which is a less good substrate for BACE 1 (± 0. 5 x) is protective against AD in the wider population • Treatment in prodromal AD rather then AD dementia • Less damage has occurred and neuronal damage is hardly reversible • Early treatment initiation is expected to result in better treatment response and better chance of technical success • Inclusion criteria based on combination of cognition and biomarkers • New population needs careful selection of cognitive/clinical tools 64
MK 8931 for a. MCI due to Alzheimer’s disease Protocol Overview

Cog. Rx’s CT 1812: Changing Views About the Cause of Alzheimer’s Disease Leads to Hope for Patients OLD VIEW of Alzheimer’s: Beta-amyloid fibrils and plaques are the culprit NEW VIEW of Alzheimer’s: Beta-amyloid oligomers are the culprit = failed clinical trials ü ü = the first drugs to halt the disease science isbbased this Discoveries described in two publications: Cog. Rx NJ Izzo et al 2014 a, (PMID: on 25390368, 25390692) view Freely accessible from this link: http: //www. alzforum. org/news/conferencecoverage/meet-sigma 2 -new-av-receptor Cognition Therapeutics, Inc. 66

Treatment of non-AD dementias • DLB/PDD – Some evidence for ACh. EIs • FTLD – No specific therapies yet – Tau-directed therapies may be effective in FTLD-tau (40% of FTLD) – Therapies targetting TDP-43 and fus will be examined • Va. D – Modification of vascular risk factors – Beware antiplatelets/anticoagulants if microhaemorrhages • Probably we should target the pathology, not clinical diagnosis.
Will we cure /prevent AD? • It seems we may already be preventing it • In the next 5 years we will – Role out primary prevention strategies • We already have! – Identify those at risk • Apo. E 4, FHx, amyloid positive – Commence therapy before any memory loss (preclinical stage) • The earlier, the safer it needs to be • Likely a cocktail, from start or sequentially – BACE inhibitor – m. Ab against amyloid – Anti-tau therapies? – Similar approach to prodromal AD • But may also use symptomatic therapies – In dementia due to AD • Still likely to use disease modifying drugs – But can tolerate greater toxicity (eg more ARIA) • Major role for symptomatic therapies

BOARD MEMBERS • Associate Professor Michael Woodward AM (Chair) • Ian Knight (Treasurer) • Dr Amy Brodtmann • Graeme Samuel AC • Neil Samuel Alzheimer’s Australia Dementia Research Foundation – Victoria
THE FOUNDATION • Priority is given to projects focusing on psychosocial aspects of dementia, rather than drug therapy • Over 12 grants totalling just under $1, 000 previously awarded • 6 grants of $50, 000 each to be awarded for projects in 2017 • Annually around $300, 000 received in donations and bequests, helping to grow the grants program Alzheimer’s Australia Dementia Research Foundation – Victoria
ROBOTS FOR SUPPORTING DEMENTIA CARE Affective communication robots for supporting carers and people with dementia in home-based care • Prof Rajiv Khosla and colleagues, La Trobe University • The researchers developed and embedded various services in assistive robots used in the home • E. g. providing reminders, games and quizzes, relaying news and weather, singing and dancing • 9 couples took part in Victoria • Found increased social engagement and respite for carers

STUDY PARTICIPANTS WITH LUCY

DRIVING AND SOCIAL SKILLS • Prof Carolyn Unsworth and colleagues at La Trobe University are examining how location of assessment and the opportunity to undertake a second test affect the outcome of driver assessments for people with dementia • Dr Michelle Kelly and colleagues at University of NSW are developing and evaluating the Brief Assessment of Social Skills (BASS) screening tool for people with Alzheimer’s disease or frontotemporal dementia Alzheimer’s Australia Dementia Research Foundation – Victoria
WORKING WITH GPs ON DRIVING • Dr Jacqueline Liddle and colleagues at University of Queensland were awarded the Cecilia Margaret Hudson Dementia Research Grant • They will evaluate an education and support program for driving cessation for people with dementia implemented within GP clinics, assessing the impact of the program for people with dementia, their carers and GPs Alzheimer’s Australia Dementia Research Foundation – Victoria
MEMORY AND COGNITION • Dr Celia Harris and colleagues at Macquarie University are investigating the systems of memory support that people use to compensate for declining memory, and how effective they are • Dr Bridget Regan and colleagues at Monash University are evaluating the MAXCOG program that aims to give people strategies to help cope with their cognitive problems in daily life Alzheimer’s Australia Dementia Research Foundation – Victoria
REDUCING COGNITIVE DECLINE • Dr Michele Callisaya and colleagues at Monash University are evaluating a 6 month exercise program for people with diabetes to test whether physical activity can reduce their risk of cognitive decline • Dr Alex Bahar-Fuchs and colleagues at the Australian National University are evaluating a cognitive training program for people with mild cognitive impairment, with and without neuropsychiatric symptoms Alzheimer’s Australia Dementia Research Foundation – Victoria
DIAGNOSIS AND COMMUNICATION • Dr Hamid Sohrabi and colleagues at the Mc. Cusker Alzheimer’s Research Centre will investigate a new imaging technique to detect Alzheimer’s pathology in the eye, as a potential diagnostic test • Dr Janet Beilby and colleagues at Curtin University will trial a visual learning environment for communication skills training for professional and family carers Alzheimer’s Australia Dementia Research Foundation – Victoria
OXYTOCIN FOR SOCIAL SKILLS • Dr Donna Mc. Cade and colleagues at the Brain and Mind Research Institute will trial a new therapy, intranasal administration of oxytocin, to improve emotion recognition, social interactions and neuropsychiatric symptoms in people with Alzheimer’s disease Alzheimer’s Australia Dementia Research Foundation – Victoria

Associate Professor Muireann Irish “Beauty and the Brain” – A novel approach to anhedonia in dementia Dementia is typically associated with the loss of memory for one’s past. Mounting evidence suggests, however, that individuals with dementia experience changes in their capacity to derive pleasure, leading to apathy and social withdrawal. This study examines the extent to which loss of pleasure is present in different dementia subtypes and whether art and music stimuli offer promise to improve patient wellbeing.

Dr Nasser Bagheri Hotspots of dementia risk in Australian communities: an approach to better targeting preventive interventions We predicted future dementia risk for a sample of 17, 178 individuals over the age of 65 years with no history of dementia in the western Adelaide. The dementia risk score was computed for each individual using the Australian National University Alzheimer's Disease Risk Index (ANU-ADRI). This included seven risk factors (age, sex, body mass index, blood cholesterol, smoking, diabetes mellitus and depression), and two protective factors (physical activity and social engagement). The individual dementia risk scores were aggregated and visualised at a regional level for the study area. Our research finding showed there is a great deal of geographical variation in dementia risk across the communities in western Adelaide. Further geospatial analysis identified communities with significant high risk (hotspots) of dementia. Furthermore, the association between built environment and lifestyle factors is underway.

Dr Michelle Kelly The neural correlates of memory improvement following transcranial direct current stimulation combined with cognitive training (t. DCS + CT) in patients with amnestic mild cognitive impairment. Our research aim was to recruit 12 participants to conduct MRI and f. MRI scans before and after a 5 week intervention for improving memory, involving the administration of active or placebo brain stimulation during cognitive training administered 3 x week (15 treatment sessions total). So far we have recruited 13
Dr Michelle Kelly Our preliminary analysis conducted in 2015 with N = 28 indicated large sized memory improvements in both groups at the 3 month follow-up time point (i. e. , lasting effects). The average improvement was large enough to bring people’s memory from “mild impairment” back to within the normal range. When our final participant has completed the study, we will conduct the final analysis of the clinical trial data and neuroimaging data (i. e. , the currently funded study by AADR). The neuroimaging data will determine whether our intervention restored functioning of memory centers within the brain.
Conclusions • Dementia research is an increasingly rich landscape • And vital! – Soon to be the most common cause of death – 900, 000 Australians affected by 2050 – At least twice that many at risk • ie preclinical and prodromal stages • We are making progress in diagnosis, prevention and cure – But still a long way to go
 Promotion from assistant to associate professor
Promotion from assistant to associate professor Prof michael woodward
Prof michael woodward Alzheimers society contented dementia
Alzheimers society contented dementia Georgia alzheimers planning
Georgia alzheimers planning Fast scale dementia
Fast scale dementia Vaskulär demens
Vaskulär demens Alzheimers nz conference 2020
Alzheimers nz conference 2020 Historical research
Historical research Alzheimers eye test joke
Alzheimers eye test joke Professor michael bagshaw
Professor michael bagshaw Professor michael bagshaw
Professor michael bagshaw Prof. dr. michael nagel
Prof. dr. michael nagel Professor michael arthur
Professor michael arthur Professor michael quinlan
Professor michael quinlan Michael porter harvard professor
Michael porter harvard professor Positive physical approach
Positive physical approach Confusion dementia and alzheimer disease chapter 19
Confusion dementia and alzheimer disease chapter 19 Chapter 49 confusion and dementia
Chapter 49 confusion and dementia Chapter 19 confusion dementia and alzheimer's disease
Chapter 19 confusion dementia and alzheimer's disease Confusion dementia and alzheimer's disease
Confusion dementia and alzheimer's disease A helpful way for an na to respond to hallucinations is to
A helpful way for an na to respond to hallucinations is to Difference between dementia and delirium
Difference between dementia and delirium Moving and handling dementia patients
Moving and handling dementia patients Francisco fernandez md
Francisco fernandez md Amnesia
Amnesia Dementia treatments and interventions near patterson
Dementia treatments and interventions near patterson Woodward araştırması
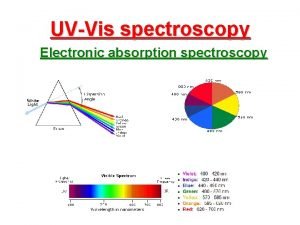
Woodward araştırması Lambert beer law and its limitations
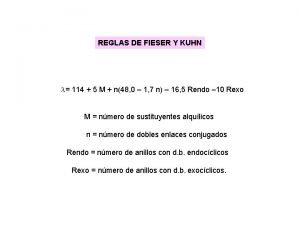
Lambert beer law and its limitations Règles de woodward-fieser
Règles de woodward-fieser Application of woodward fieser rule
Application of woodward fieser rule Woodward gs16
Woodward gs16 Reglas de woodward fieser
Reglas de woodward fieser John r. woodward
John r. woodward Waration certificate
Waration certificate R b woodward
R b woodward Regla de woodward fieser
Regla de woodward fieser Joan woodward technology
Joan woodward technology Woodward lawson method
Woodward lawson method Adhocracia
Adhocracia Lawrence ve lorsch araştırması
Lawrence ve lorsch araştırması William hilton explorer
William hilton explorer Richard b woodward
Richard b woodward Dementia bookcase analogy
Dementia bookcase analogy Dementia pugilistica
Dementia pugilistica Enriched model of care social psychology
Enriched model of care social psychology Fast dementia scale
Fast dementia scale Dementia 2015
Dementia 2015 Tom kitwood enriched model of dementia care
Tom kitwood enriched model of dementia care Reversible dementia
Reversible dementia Reversible dementia
Reversible dementia Barbara's story dementia
Barbara's story dementia Risk factor dementia
Risk factor dementia Fast score hospice
Fast score hospice Life story work dementia
Life story work dementia Trasodone
Trasodone Dementia friendly nevada
Dementia friendly nevada Promoting excellence in dementia care
Promoting excellence in dementia care Rarly signs of dementia
Rarly signs of dementia Dementia capable care
Dementia capable care Narritive text
Narritive text Pool activity levels
Pool activity levels Symptoms of dementia
Symptoms of dementia Positive risk-taking dementia
Positive risk-taking dementia Receptive language
Receptive language Dementia
Dementia Frontotemporal dementia
Frontotemporal dementia Unit 40 health and social care
Unit 40 health and social care Enriched model of dementia care
Enriched model of dementia care Rocking chair therapy for dementia patients
Rocking chair therapy for dementia patients Responsive
Responsive Lewry body dementia
Lewry body dementia Living well with dementia scotland
Living well with dementia scotland Dementia
Dementia Dementia pictures
Dementia pictures Dcm methode
Dcm methode 850 000 steps for dementia
850 000 steps for dementia Dementia is a condition characterized by
Dementia is a condition characterized by Bath city forum
Bath city forum Chartered it professional
Chartered it professional Tecniche associate al pensiero computazionale
Tecniche associate al pensiero computazionale The pyramid at chichen itza is most closely associate with
The pyramid at chichen itza is most closely associate with Lonestar nursing application
Lonestar nursing application Certified systems engineering professional
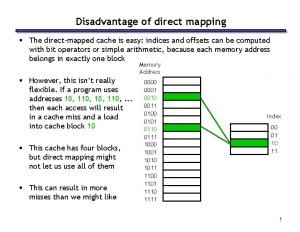
Certified systems engineering professional Disadvantages of direct mapped cache
Disadvantages of direct mapped cache Pjas cern
Pjas cern