About Dementia What is Dementia Dementia is a
About Dementia
What is Dementia? Dementia is a general term for the loss of memory and other intellectual abilities serious enough to interfere with daily life.
What is the Difference Between Dementia and Alzheimer’s Disease? ü Dementia is an umbrella term - like cancer. ü Just as there are different types of cancer, there are different types of dementia. ü There are over 70 types of dementia, with Alzheimer’s disease the most common type. ü Alzheimer’s disease accounts for about 70% of all dementia cases.
How The Brain Works q There are 100 billion nerve cells, or neurons, creating a branching network q Signals traveling through the neuron forest form memories, thoughts and feelings q Alzheimer’s disease destroys neurons
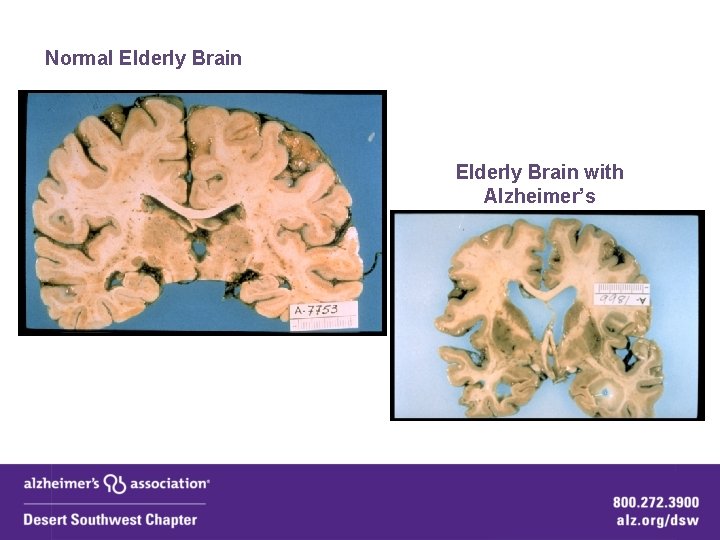
Normal Elderly Brain with Alzheimer’s
Effects of Dementia q Loss of cognitive functioning serious enough to interfere with daily functioning q Causes changes in: ü Memory ü Language ü Thought ü Navigation ü Behavior ü Personality/Mood ü Planning and organizing
Risk Factors: q The primary risk factor is age q Dementia is not a normal part of aging q Physical health: ü ü ü heart disease Diabetes high cholesterol high blood pressure lack of social engagement q Higher in women due to women living longer.
Body & Brain Connection: q Brain health comes from a healthy body and active social life. q Risk for AD or Vascular dementia is increased by a damaged heart or blood vessels. q Diabetes is mid-life can lead to AD decades later. q There is a strong link between serious head injury and risk for dementia.
Warning Signs: 1. Memory loss 2. Difficulty performing familiar tasks 3. Problems with language 4. Disorientation to time and place 5. Poor or decreased judgment 6. Problems with abstract thinking 7. Misplacing things 8. Changes in mood or behavior 9. Changes in personality 10. Loss of initiative
Quick Facts
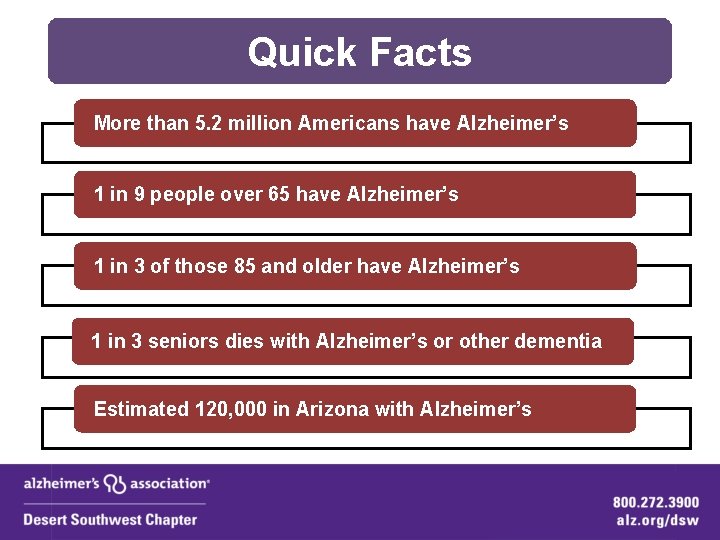
Quick Facts More than 5. 2 million Americans have Alzheimer’s 1 in 9 people over 65 have Alzheimer’s 1 in 3 of those 85 and older have Alzheimer’s 1 in 3 seniors dies with Alzheimer’s or other dementia Estimated 120, 000 in Arizona with Alzheimer’s

Quick Facts Alzheimer’s disease is the 6 th leading cause of death in the United States for those 65 and older By 2050, the number of people age 65 and older with Alzheimer’s disease may triple, from 5. 2 million to a projected 11 to 16 million. Alzheimer’s is the only leading cause of death that has no way to prevent, stop or cure it.
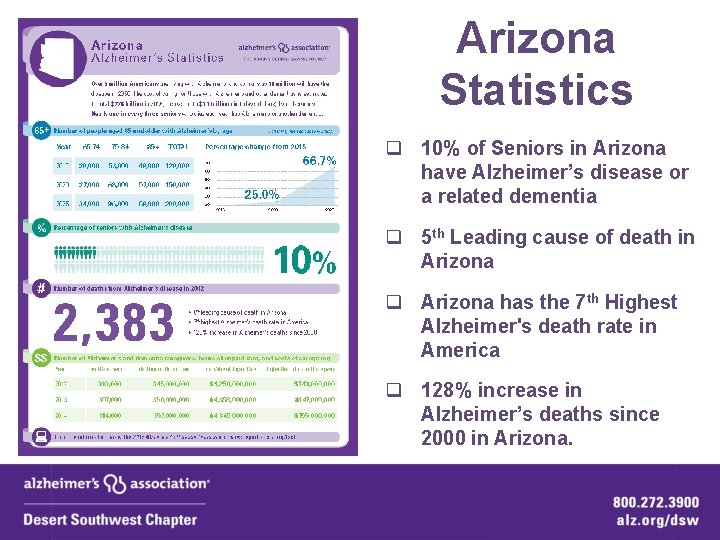
Arizona Statistics q 10% of Seniors in Arizona have Alzheimer’s disease or a related dementia q 5 th Leading cause of death in Arizona q Arizona has the 7 th Highest Alzheimer's death rate in America q 128% increase in Alzheimer’s deaths since 2000 in Arizona.
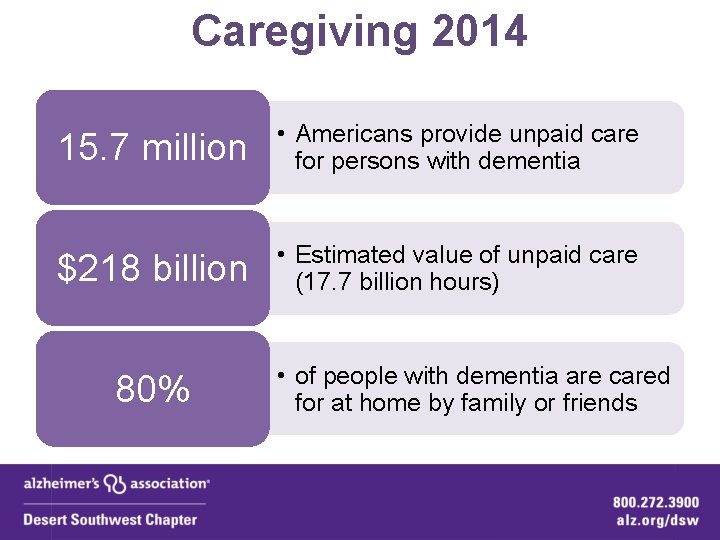
Caregiving 2014 15. 7 million • Americans provide unpaid care for persons with dementia $218 billion • Estimated value of unpaid care (17. 7 billion hours) 80% • of people with dementia are cared for at home by family or friends

Video
Stages
Early Stages q Short Term Memory - Forgetfulness q Difficulty with language: ü Word finding ü Repeated questions ü Slower processing time q Poor judgment q Losing things q Eyesight problems q Depression q Driving problems q Medication errors q May try to “hide it”
Middle Stages q Speech problems q Disorientation q Driving impairment q Wandering q Difficult Behaviors
Late Stages q Total Care q Incontinence q Extreme problems with: ü Mood ü Behavior ü Delirium q Severe communication problems q Loss of verbal & mobility skills

Middle or Late Stage Caregivers What You Might Observe q Signs of elder abuse or neglect q Calls for assistance q Caregiver stress q Caregiver burnout q Caregiver depression

Behaviors
Understanding Behaviors: The Brain q Dementia affects areas in the brain that control emotion and behavior. q The person’s ability for insight and judgment are impaired.
Understanding Behaviors q 80% will have some type of behavioral disturbance q Most occur in the moderate stages q Usually worsen as the day progresses (Sundowners) q A main reason for placement
Common Types of Behaviors q Common Types of Behaviors: ü Repetitive questioning ü Yelling or calling out ü Sleep disturbances ü Wandering ü Agitation/Anger ü Physical/Verbal Aggression ü Hypersexual Behavior/Disrobing

There is ALWAYS a Reason q All Behaviors have a purpose q Way to communicate Needs ü ü ü Bathroom Something to eat or drink Stimulation Companionship Pain
Infections q Susceptible to infections. q Common Infections In Older Adults: ü Urinary tract infection ü Pneumonia q Signs of Infection: ü Rapid changes in mood, cognition, and behaviors
Physical Pain q May be in physical pain and be unable to express it. q Often pain is expressed through behavior. q Often pain goes untreated.
Understanding Environment Behavioral Concerns q An over-stimulating (noisy) environment q A change in environment (a move or travel) q People with dementia require a calm yet structured setting q Structure and activity daily is critical
Boredom q Lack of Meaningful Activities: ü Cause Depression ü Cause Behaviors q TV Is Rarely An Activity: ü Unable to understand ü Unable to keep interest ü Frightened by what they see q Reading: ü Often have lost the ability

Communicating with Someone Who is Repetitive: q Use repetition to respond even when it feels frustrating q Give brief or short answers to respond to the request. q It isn’t useful to go into explanations
Hints to Prevent Agitation q Create a Calm Environment ü Move person to a quieter place ü Avoid background distraction - TV ü Overstimulation can make agitation worse q Verbal Aggression: ü Consider hard candy to keep the mouth engaged. q Monitor Personal Comfort ü ü ü Check for pain, hunger, thirst Constipation, full bladder, fatigue, infections (UTI) 2 Hour Toileting Schedule Be sensitive to frustration with trying to communicate There may be limited ability to understand direction
Bathing Common: ü ü ü Many people with dementia do not want to bathe Caregivers are often at a loss to get person to bathe As a result, person may appear unclean or have body odor You Have Memory loss: ü You are being told you need to bathe but you know you just had a bath this morning Impaired Judgment: ü The water looks dangerous and you think it feels cold Privacy issues: ü You don’t want to take off your clothes in front of other people, you feel ashamed ü Previous abuse issues may resurface
Approaching Dementia
Contact People with dementia often come in contact with first responders when: ü Become lost ü Unknowingly break the law ü Due to agitation – put selves & others at risk.
TALK Take it slow Ask simple questions Limit reality checks Keep eye contact
Take it Slow q Approach Slowly: ü They may be overwhelmed ü May feel things are happening faster than they are q Approach From the Front: ü Easily Startled q Speak Slowly & In Calm, Low Voice: ü Low voice helps de-escalate
Ask Simple Questions q Avoid multipart questions q Be patient, give time to process – 10 Second Rule q Rephrase if person confused q KISS – Keep it Short & Simple

Limit Reality Checks q Enter “their world” q Avoid correcting q Redirect q Talk about their past
Keep Eye Contact q Non-Verbal Communication Important q React Strongly to your body language & facial expressions q Give nods & keep open posture

Communication
Alzheimer’s & Communication As the disease progresses: ü lose ability to communicate thoughts and feeling through words ü lose the ability to understand words that others speak to them
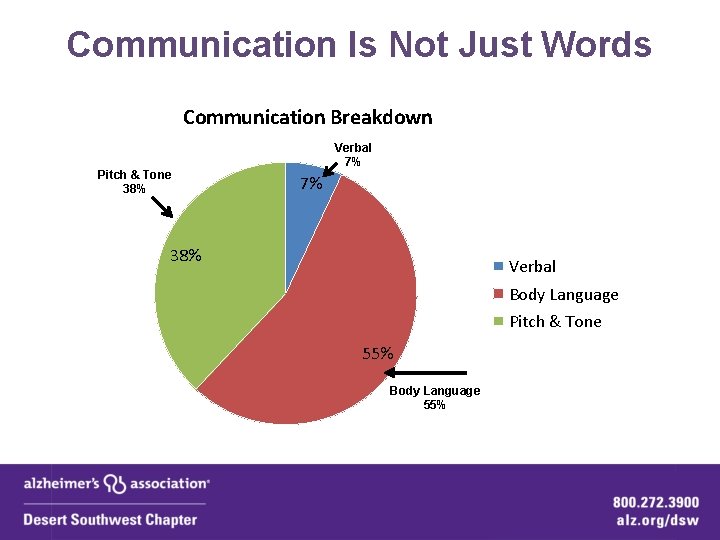
Communication Is Not Just Words Communication Breakdown Pitch & Tone 38% Verbal 7% 7% 38% Verbal Body Language Pitch & Tone 55% Body Language 55%
Mirror Effect q Your emotions & reactions influence the Person with dementia: q The person with dementia is often like a mirror: ü Any frustration & negative reactions/energy are often projected out and reflected back to you. ü The more calm and reassuring you are is also often reflected back to you.

Reassurance q 3 Main Strategies To Reassure: ü Don’t reason – usually increases frustration and anger. ü Ongoing reassurance – “You are safe here” or “I am here to help” ü Validate feelings – “I can see this is hard for you”.
Agitation
Hints During an Episode of Agitation q Do Not: ü ü ü ü Raise voice Rush Confront Argue Reason Shame Overly Explain

Hints During an Episode of Agitation q Do: ü Introduce Yourself ü Ask Questions ü Take to ER if Person Cannot Be Calmed Down ü Tell the Person You Are There to Help ü Refer Caregiver to the Alzheimer’s ü Open Posture Association ü Calm Voice ü Establish Your Authority

Therapeutic Fibbing q Goal ü Calm the person down q Deceased Parents ü On vacation, will be back next week q Wanting to “go home” ü Desire to feel safe, may be talking about childhood home ü “I will make sure you get home”
Types of Calls
Wandering q Can wander by foot or vehicle q If someone with dementia wanders they will do it again q Will often attempt to go to familiar places like work or school q Wandering is still a concern in placement q Usually follow dominate hand
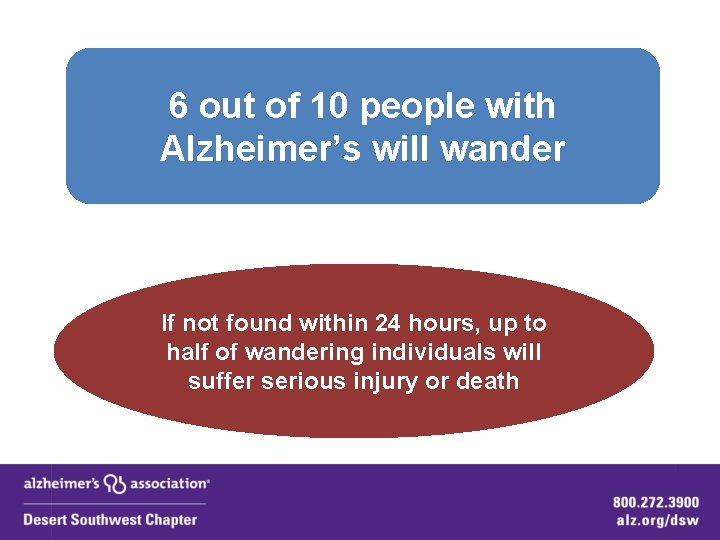
6 out of 10 people with Alzheimer’s will wander If not found within 24 hours, up to half of wandering individuals will suffer serious injury or death
Misconceptions of Wandering “My mother has never wandered before. ” q If a person with dementia is able to walk, wandering can happen at any time. q If wandering has already occurred, it will happen again.
Misconceptions of Wandering “We’ve explained to my dad why he should not go out by himself. ” q It is unlikely he’ll remember he has been told not to go out alone. q Will increasingly lose his ability to make good judgments and think logically.
Violence or Threat of Violence q De-Esculate - Apologize q Pain? UTI? q Body language q Encourage caregiver to call the Alzheimer’s Association q Reassurance q State who you are and that you are there to help
Paranoia/Delusions/ Hallucinations q Paranoia or Unrealistic Fears are Common ü Accusations of people stealing from them ü Accusations of family poisoning them ü May refuse meds or food q Delusions or false beliefs are also common ü Being “Kidnapped” and forced to be in the home against his or her will q Hallucinations are less common but do occur ü Seeing burglar ü Seeing children – common

Hypersexual Behavior or Indecent Exposure q Distraction more effective than scolding or lectures. q Confrontation does not work and may make it worse. q Behavior is not intentional q Get to caregiver/family member right away q If they can’t be found, take to ER.
Shoplifting q Person may not remember it when you arrive q De-escalate – speak calmly & be supportive q Resolve – work with the merchant

Abuse & Neglect
Types of Abuse q Physical: ü causing physical pain or injury q Emotional: ü verbal assaults, threats of abuse, harassment and intimidation q Neglect: ü failure to provide necessities, including food, clothing, shelter, medical care or a safe environment q Confinement: ü Restraining or isolating the person – Locking them in rooms
Types of Abuse q Financial: ü misuse or withholding of the person's financial resources (money, property) to his or her disadvantage or the advantage of someone else q Sexual abuse: ü sexual activity when the person is unable to understand, unwilling to consent, threatened or physically forced q Willful deprivation: ü denying medication, medical care, food, shelter or physical assistance, exposing the individual to the risk of physical, mental or emotional harm
Abuse & Neglect By Caregiver q Generally from lack of support rather than malice q Possible causes: ü ü ü Stress Social Isolation Depression Lack of Respite Verbal or Physical Abuse by Person with Dementia
Report To Adult Protective Services (APS) q By Phone: ü (877) SOS-ADULT or (877) 767 -2385 ü Available Monday-Friday 7 a. m. - 7 p. m. / Sat-Sun 10 a. m. - 6 p. m. q Online: 24 hours: ü https: //www. azdes. gov/landing. aspx? id=7307
Language to Use in APS Reports: q Do not state as Fact – Describe Your Observations: Use Key Words: ü Appeared ü Officer Observed ü Possible Vulnerable Adult ü As Evidenced by ü Officer Concerned By (Of)

Firearms

Firearms q Extreme Reactions to Common Events ü May not recognize family – see a burglar instead q Misinterpretation of Surroundings ü See something on TV – think it is real q Over-Reaction to Surrounding Events ü May pull firearm on loud children, ect.
Firearms q Encourage Caregiver to remove all firearms and bullets from home. q Do not just hide them – they can be found q Encourage Caregiver to Call the Alzheimer’s Association

q Call the Alzheimer’s Association for Help q Social Service Agency q Free Programs & Services to Support Caregivers q Award Winning Website: www. alz. org We Can Help!
Chapter Programs & Services

Serve All Types of Dementia Full name of organization is: Alzheimer’s Disease and Related Disorders Association Serve all people with Alzheimer’s and related dementias and Mild Cognitive Impairment (MCI)
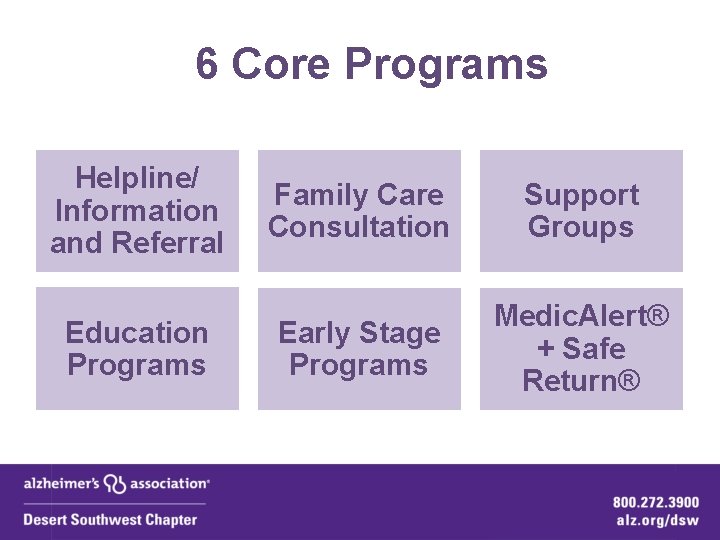
6 Core Programs Helpline/ Information and Referral Education Programs Family Care Consultation Support Groups Early Stage Programs Medic. Alert® + Safe Return®
Helpline Information and Referral

24 -Hour Helpline/Information & Referral 1 -800 -272 -3900 q Trained specialists provide information, support & referrals. q Confidential & Free. q Between 8 am - 5 pm, Monday - Friday, answered by staff. q After hours, calls are answered by professional staff at the National Call Center in Chicago. 24/7 365
Family Care Consultation
Family Care Consultation q Master’s level staff provide individualized guidance on: q care options q interventions q resources q Provide emotional support and coping strategies q Address immediate needs & planning for the future q Confidential q Free q Staff available by phone and scheduled office visits q Home visits available when needed

Support Groups

Support Groups q Trained facilitators lead groups of caregivers to: ü share information ü share experiences ü build new skills ü get support ü get ideas We have more than 30 support groups!

Education
Education q Designed to increase awareness and knowledge about dementia q Free q 1 to 2 hour classes q Half day conferences q Workshop series q Held in various locations in service area
Early Stage
Early Stage Programs ü ü Support Groups for Early Stage: q For people with memory loss and their care partner. q For people with memory loss with no care partner. q For people with Younger Onset dementia and their care partners. Early Stage Coordinator: q Dedicated staff member to work with individuals with memory loss and their care partners. q Provides support, information, and education. Quarterly Social Engagement Activities
Medic Alert® + Safe Return®

Medic. Alert® + Safe Return® q Bracelet or necklace. q If lost, a community support network will be activated, including local Alzheimer’s Association chapters and law enforcement agencies. q Scholarships are available to cover the cost of jewelry for the person with memory loss. 99% of those enrolled in Medic. Alert + Safe Return are returned safely, compared to less than 50% of those not enrolled.

q Web-based - GPS q Location device (such as a pager) or mounts a device to the car. q Family can monitor the location of the person via internet or phone. q Includes the 'back up' of Medic. Alert + Safe Return jewelry and program. q Includes live 24/7 operator support in the event of an emergency or location assistance. q Scholarships Not Available for This Program

Advocacy
Advocacy: q Advocates work on a local and national level to: ü Improve dementia care and services; ü Improve access to community-based care; ü Improve quality care in residential settings; and ü Expand funding for research and public programs serving people with dementia.

What We Don’t Do: ü Emergency Services ü Medical Services – Diagnosing ü Give Medical or Legal Advice ü Recommending one service or provider over another ü Provide Ongoing Respite
Alzheimer’s Association Free Online 1 st Responder Training
Online Training q Free q Anytime of day, or night, accommodating for shift work and new hires. q Quiz at the end q Certificate of Completion by the Alzheimer’s Association q http: //www. alz. org/care/alzheimers-firstresponder. asp
Thank You!
- Slides: 92