Schizophrenia and dementia Chris Perkins Alzheimers NZ Conference




- Slides: 18
Schizophrenia and dementia Chris Perkins Alzheimers NZ Conference 04/11/16
• Increased life expectancy • Challenge of diagnosing dementia • Risk reduction • Management
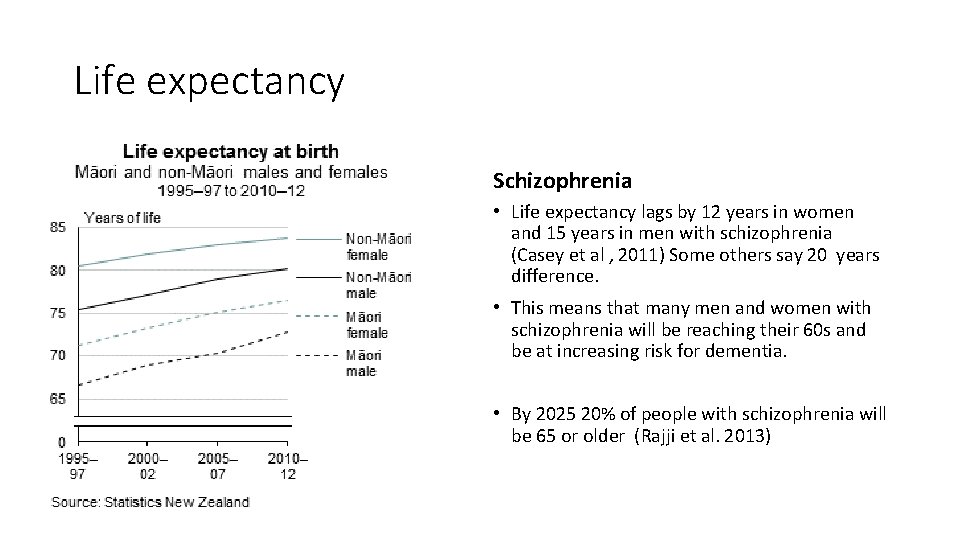
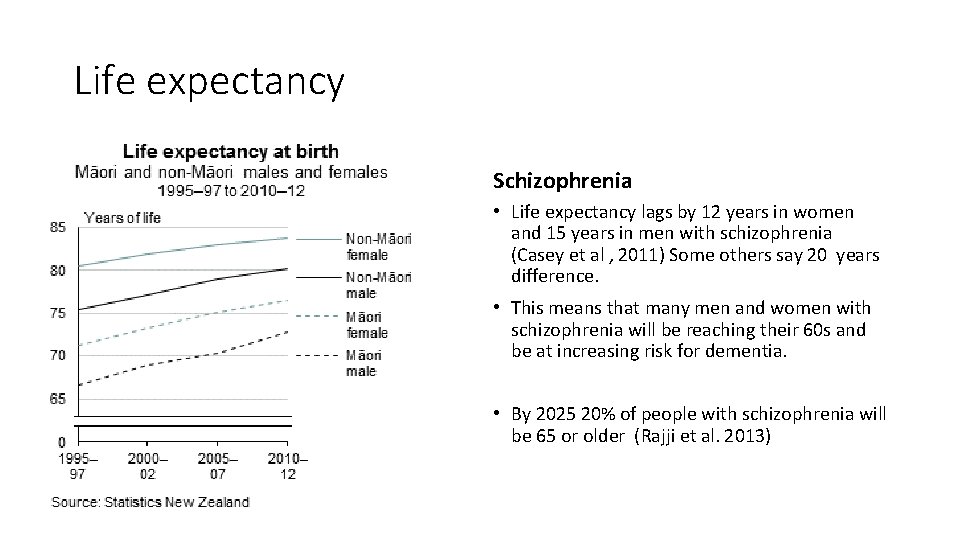
Life expectancy Schizophrenia • Life expectancy lags by 12 years in women and 15 years in men with schizophrenia (Casey et al , 2011) Some others say 20 years difference. • This means that many men and women with schizophrenia will be reaching their 60 s and be at increasing risk for dementia. • By 2025 20% of people with schizophrenia will be 65 or older (Rajji et al. 2013)
Danish cohort study: Ribe et al ( 2015) Risk of dementia > 2 x greater in people with schizophrenia “Individuals with schizophrenia, especially those younger than 65 years, had a markedly increased relative risk of dementia that could not be explained by established dementia risk factors”
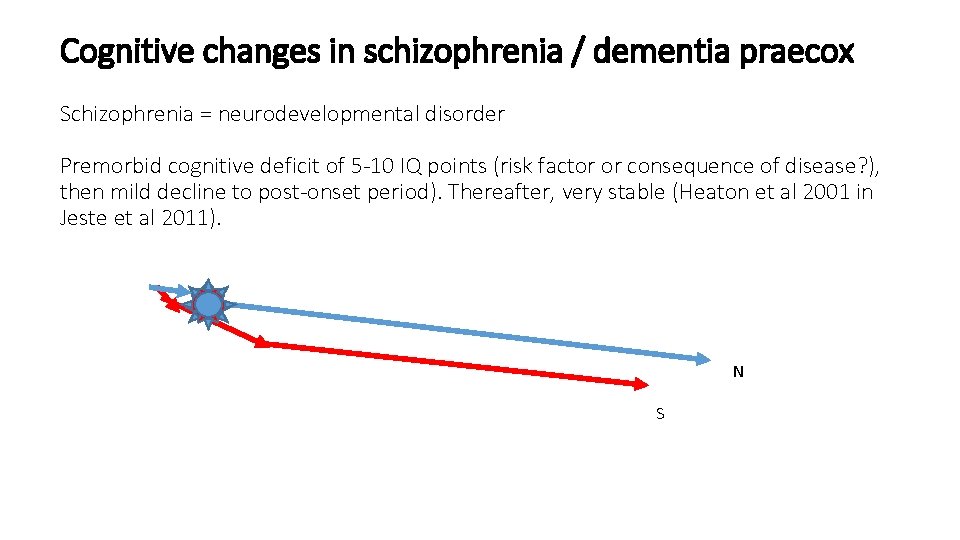
Cognitive changes in schizophrenia / dementia praecox Schizophrenia = neurodevelopmental disorder Premorbid cognitive deficit of 5 -10 IQ points (risk factor or consequence of disease? ), then mild decline to post-onset period). Thereafter, very stable (Heaton et al 2001 in Jeste et al 2011). N S
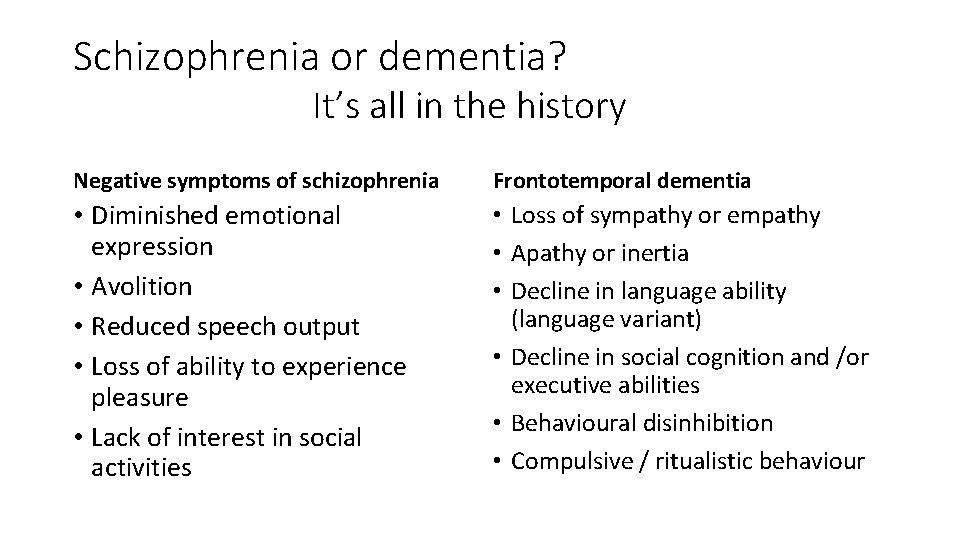
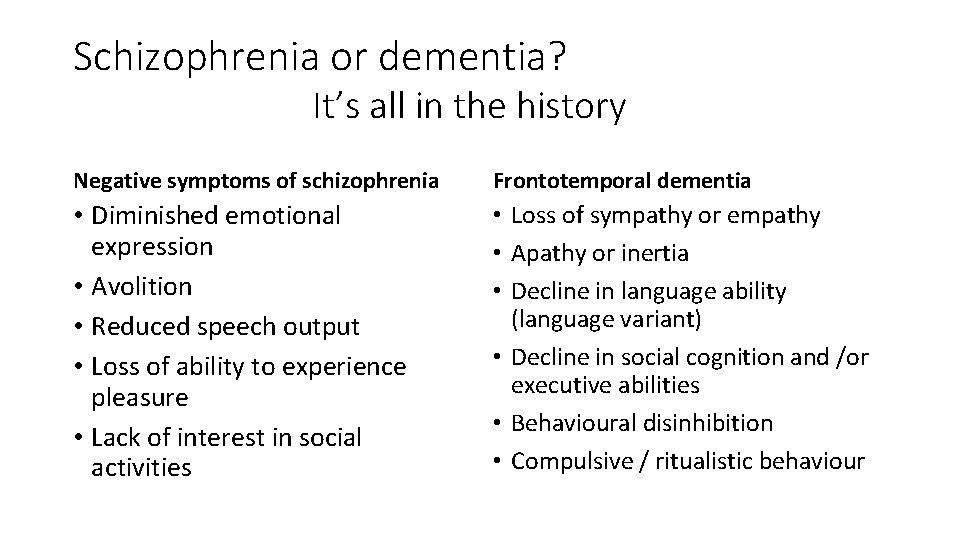
Schizophrenia or dementia? It’s all in the history Negative symptoms of schizophrenia Frontotemporal dementia • Diminished emotional expression • Avolition • Reduced speech output • Loss of ability to experience pleasure • Lack of interest in social activities • Loss of sympathy or empathy • Apathy or inertia • Decline in language ability (language variant) • Decline in social cognition and /or executive abilities • Behavioural disinhibition • Compulsive / ritualistic behaviour
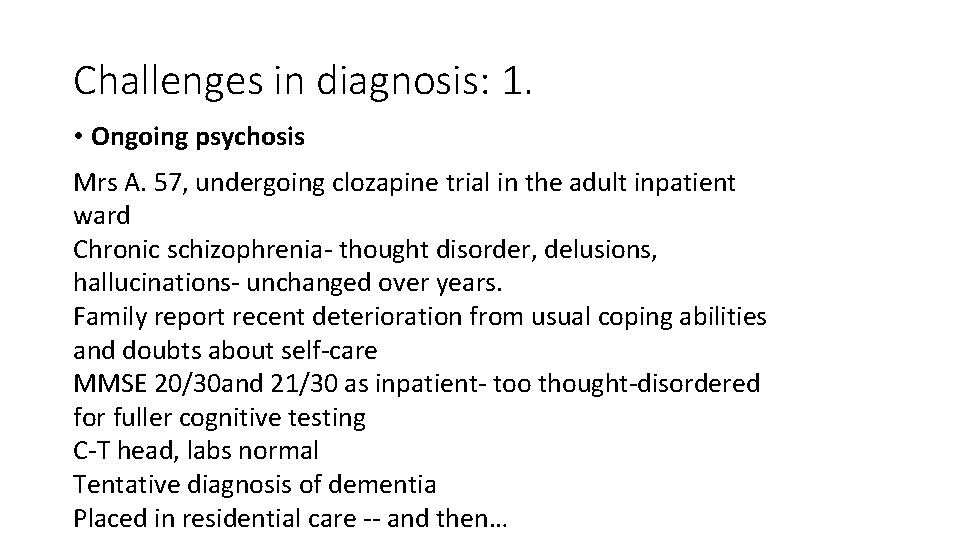
Challenges in diagnosis: 1. • Ongoing psychosis Mrs A. 57, undergoing clozapine trial in the adult inpatient ward Chronic schizophrenia- thought disorder, delusions, hallucinations- unchanged over years. Family report recent deterioration from usual coping abilities and doubts about self-care MMSE 20/30 and 21/30 as inpatient- too thought-disordered for fuller cognitive testing C-T head, labs normal Tentative diagnosis of dementia Placed in residential care -- and then…
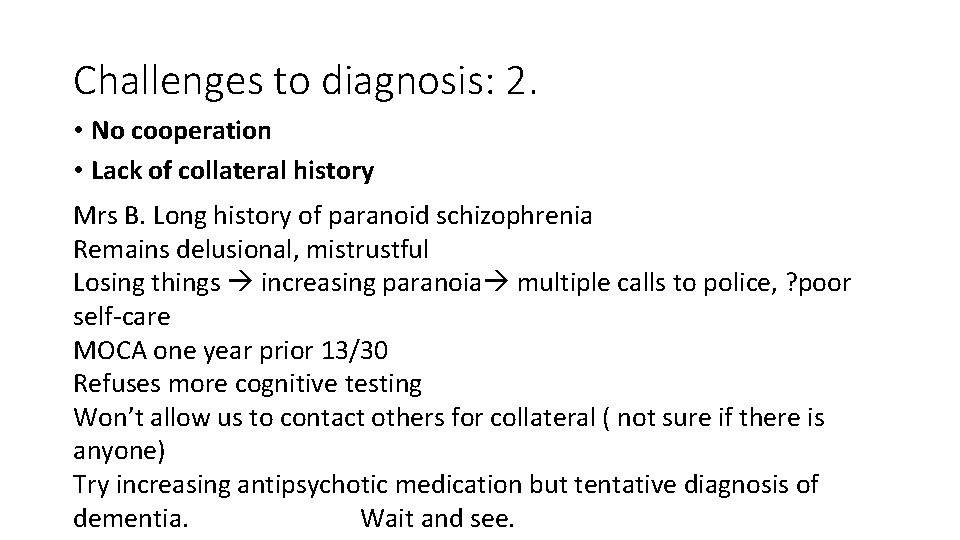
Challenges to diagnosis: 2. • No cooperation • Lack of collateral history Mrs B. Long history of paranoid schizophrenia Remains delusional, mistrustful Losing things increasing paranoia multiple calls to police, ? poor self-care MOCA one year prior 13/30 Refuses more cognitive testing Won’t allow us to contact others for collateral ( not sure if there is anyone) Try increasing antipsychotic medication but tentative diagnosis of dementia. Wait and see.
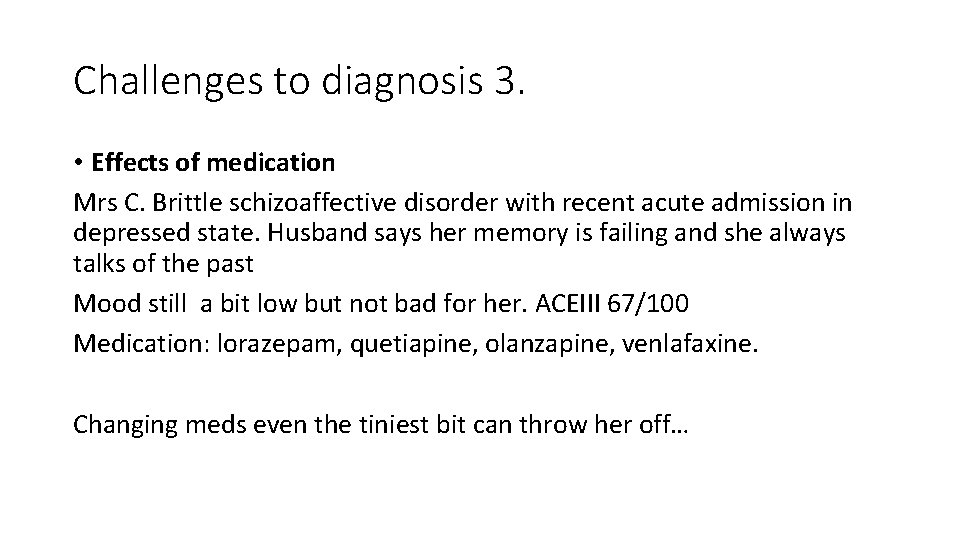
Challenges to diagnosis 3. • Effects of medication Mrs C. Brittle schizoaffective disorder with recent acute admission in depressed state. Husband says her memory is failing and she always talks of the past Mood still a bit low but not bad for her. ACEIII 67/100 Medication: lorazepam, quetiapine, olanzapine, venlafaxine. Changing meds even the tiniest bit can throw her off…
Dementia risk factors in L-T mental illness • Brain damage – reduced cognitive reserve from illness • Smoking and other substance use • Physical inactivity • Reduced socialisation • Poorly educated (often)- little cognitive stimulation • Poor physical health –metabolic syndrome(obesity, diabetes, hyperlipidaemia) often related to medication. • Reduced GP contact • Poverty: cost of medication and GP (Care Plus)
• • Keeping Body and Mind Together: Improving the physical health and life expectancy of people with serious mental illness • RANZCP (2015)

Management MH Old age ID

Summary • There will be more people with schizophrenia ageing and getting dementia • This is not a straightforward diagnosis to make • Our adult colleagues are aware of the need to attend to the physical health of their patients • We need to work together to ensure the best care for people ageing with schizophrenia

References • Casey, D. , Rodriguez, M. , Northcott, C. Vickar, G & Shihabuddin, L. (2011) Schizophrenia – Medical illness, mortality and aging INT’L. J. PSYCHIATRY IN MEDICINE, Vol. 41(3) 245 -251, • Vasilis P. Bozikas , Christina Andreou (2011) Longitudinal studies of cognition in first episode psychosis: a systematic review of the literature Australian and New Zealand Journal of Psychiatry 2011; 45: 93– 108 • Harvey, P. (2001) Cognitive and functional Impairments in Elderly Patients with Schizophrenia: A Review of the recent Literature Harvard Rev Psychiatry, 9, 2 , 59 -68 • Jeste, D. , Wolkowitz, M. &Palmer, B. (2011) Divergent trajectories of Physical, Cognitive and Psychosocial Aging in Schizophrenia Bulletin 37, 3: 451 -455 • RANZCP (2015) Keeping Body and Mind Together: Improving the physical health and life expectancy of people with serious mental illness • Ribe et al ( 2015) Long-term risk of dementia in persons with schizophrenia: a Danish population-based cohort study. JAMA Psychiatry 72 (11): 1095 -01 • Yucel, M. , Bora 1, E. , Lubman D. et al. (2012) Impact of Cannabis Use on Cognitive Functioning in Patients With. Schizophrenia: A Meta-analysis of Existing Findings and New Data in a First-Episode Sample. Schizophrenia Bulletin vol. 38 no. 2 pp. 316– 330 doi: 10. 1093/schbul/sbq 079 • ,

 Alzheimers society contented dementia
Alzheimers society contented dementia Alzheimers nz conference 2020
Alzheimers nz conference 2020 Chris perkins physio
Chris perkins physio Sirs conference 2021
Sirs conference 2021 Georgia alzheimers planning
Georgia alzheimers planning Fast scale dementia
Fast scale dementia Alzheimers sjukdom
Alzheimers sjukdom Alzheimers society citrix
Alzheimers society citrix Alzheimers eye test joke
Alzheimers eye test joke Charles perkins and the freedom rides
Charles perkins and the freedom rides Positive physical approach
Positive physical approach Confusion dementia and alzheimer disease chapter 19
Confusion dementia and alzheimer disease chapter 19 Chapter 49 confusion and dementia
Chapter 49 confusion and dementia Confusion dementia and alzheimer disease chapter 19
Confusion dementia and alzheimer disease chapter 19 Confusion dementia and alzheimer's disease
Confusion dementia and alzheimer's disease If a resident with ad shows violent behavior the na should
If a resident with ad shows violent behavior the na should Difference between dementia and delirium
Difference between dementia and delirium Moving and handling dementia patients
Moving and handling dementia patients Difference between delirium and dementia ppt
Difference between delirium and dementia ppt