Alterations of Hormonal Regulation Chapter 19 Elsevier items
- Slides: 102
Alterations of Hormonal Regulation Chapter 19 Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
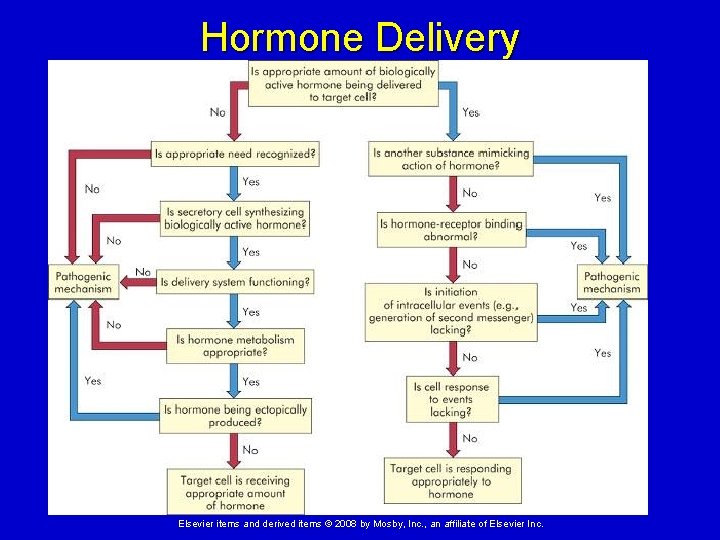
Mechanisms of Hormonal Alterations Elevated or depressed hormone levels can arise from: Dysfunctions of endocrine secreting tissues Target cell failure Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
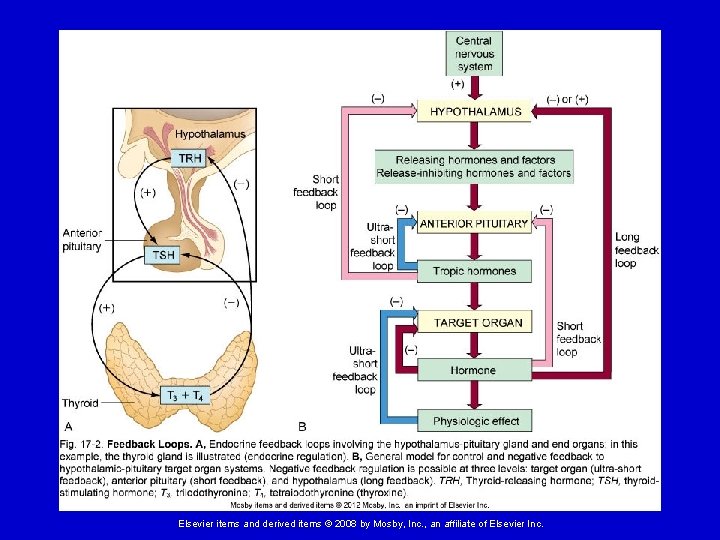
Dysfunctions of Endocrine Secreting Tissues Mechanisms that can cause this include: 1. Faulty feedback systems Gland is not receiving signals for release of appropriate levels of hormone Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
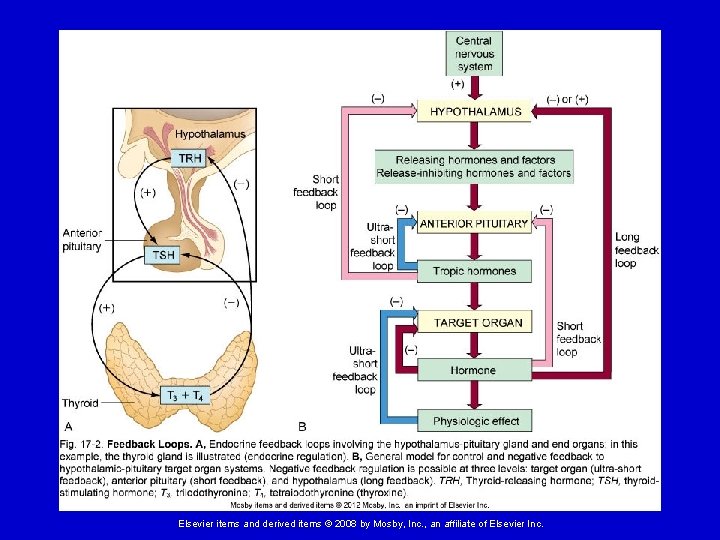
Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Dysfunctions of Endocrine Secreting Tissues 2. Dysfunction of the gland Secretory cells are unable to produce, obtain, or convert hormone precursors Gland synthesizes or releases excessive amounts of hormone Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Dysfunctions of Endocrine Secreting Tissues 3. Altered metabolism of hormones Increased hormone degradation or inactivation 4. Production of hormones from nonendocrine tissues Ectopic hormone release Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
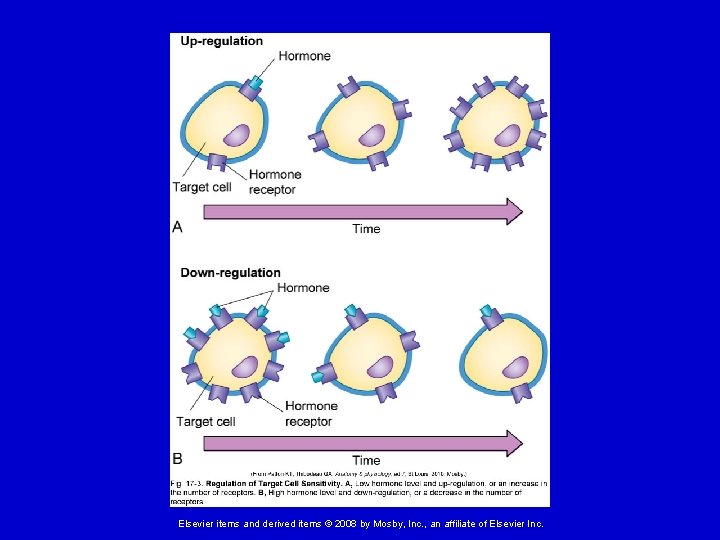
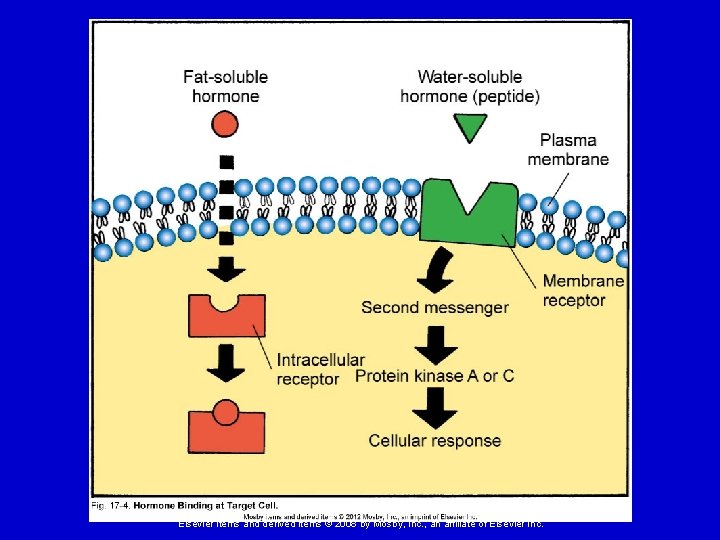
Target Cell Failure Mechanisms that can cause target cells to fail to respond to hormones include: 1. Cell surface receptor-associated disorders Decrease in number of receptors Impaired receptor function Presence of antibodies against specific receptors Antibodies that mimic hormone action Unusual expression of receptor function, for example on tumor cells Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Target Cell Failure 2. Intracellular disorders in messenger systems within the target tissue 3. Circulating inhibitors - generally antibodies that bind to the hormone and prevent binding Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
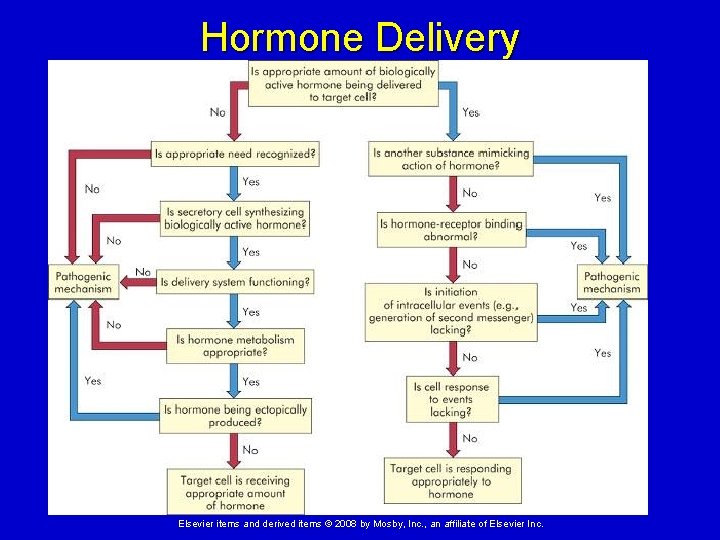
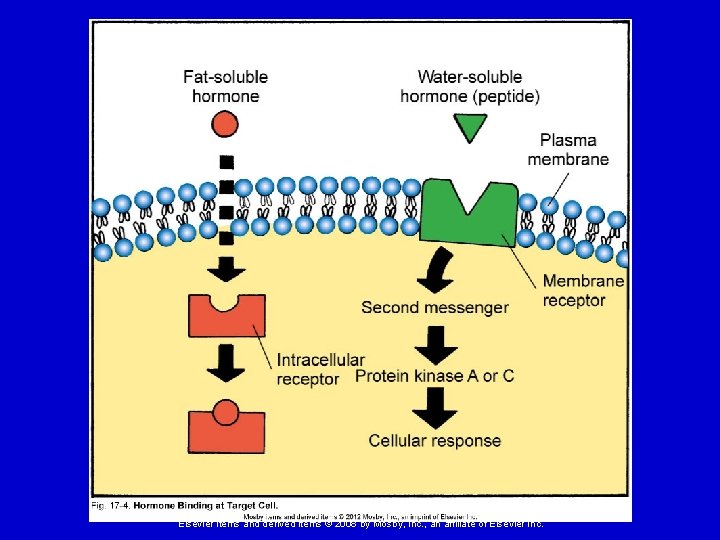
Hormone Delivery Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
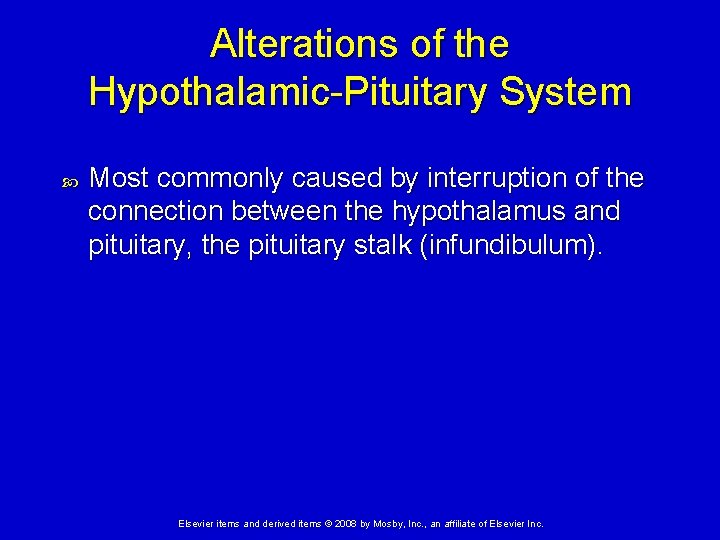
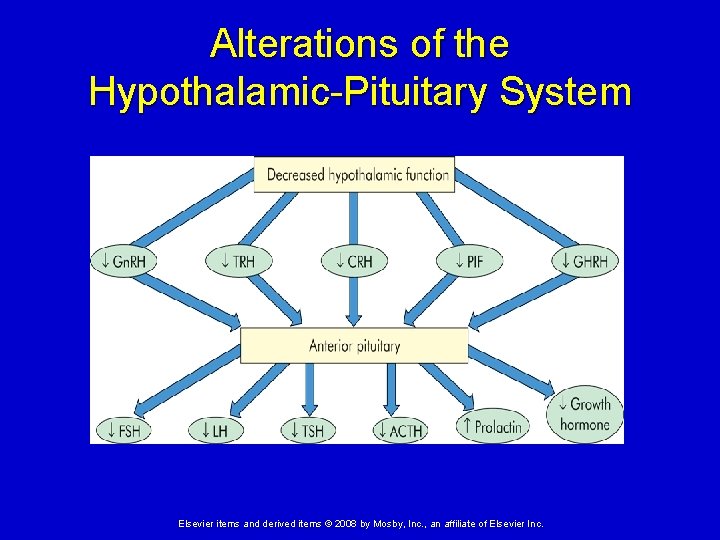
Alterations of the Hypothalamic-Pituitary System Most commonly caused by interruption of the connection between the hypothalamus and pituitary, the pituitary stalk (infundibulum). Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
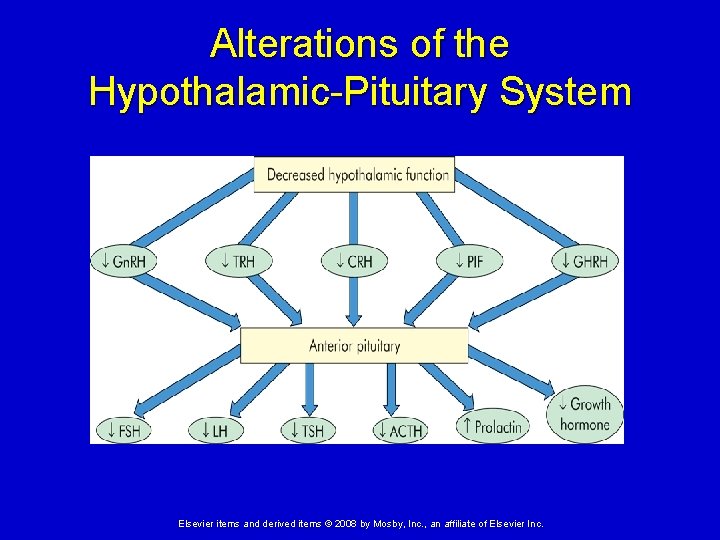
Alterations of the Hypothalamic-Pituitary System Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
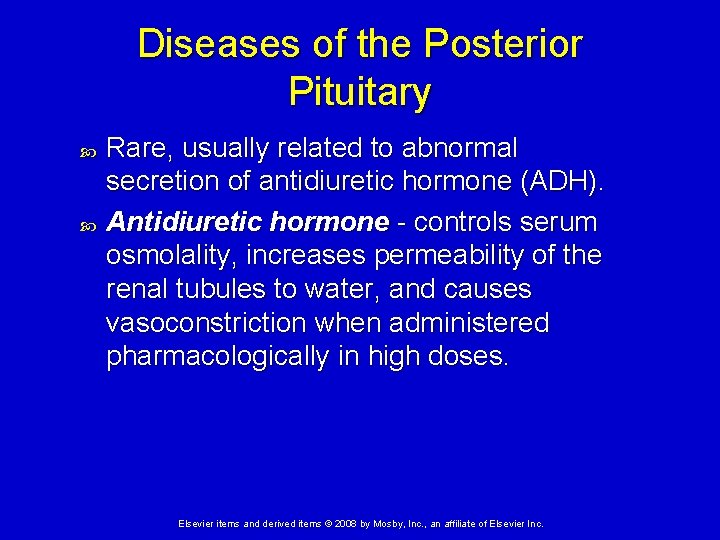
Diseases of the Posterior Pituitary Rare, usually related to abnormal secretion of antidiuretic hormone (ADH). Antidiuretic hormone - controls serum osmolality, increases permeability of the renal tubules to water, and causes vasoconstriction when administered pharmacologically in high doses. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Diseases of the Posterior Pituitary Syndrome of inappropriate antidiuretic hormone secretion (SIADH) Hypersecretion of ADH High ADH levels interfere with renal free water clearance, leading to abnormally concentrated urine, and dilute blood plasma (hypoosmolality), especially sodium (hyponatremic). Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Diseases of the Posterior Pituitary Etiology – SIADH can be caused by: Ø Cancer cells ectopically secreting ADH (Ex. small cell carcinoma) - most common Ø Brain trauma or infection Ø Infectious pulmonary diseases Symptoms are due to the hyponatremia (low serum sodium). Ø This can cause irreversible neurological damage. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Diseases of the Posterior Pituitary Diabetes insipidus Insufficiency of ADH Causes partial or total inability to concentrate the urine Low ADH levels cause formation of large quantities of dilute urine, and increased plasma concentration (hyperosmolality). Dehydration results. Symptoms - polyuria (excessive urination), thirst and polydipsia (excessive drinking) Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Diseases of the Posterior Pituitary Three types of diabetes insipidus: 1. Neurogenic - caused by insufficient amounts of ADH Ø Due to damage to the hypothalamus or pituitary. 2. Nephrogenic - caused by an inadequate response to ADH Ø Due to diseases that damage renal tubules (example – pyelonephritis) or drugs such as methoxyflurane anesthesia, lithium, or demeclocycline. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Diseases of the Posterior Pituitary Types of diabetes insipidis (cont. ) 3. Psychogenic (primary polydipsia) – caused by excessive intake of fluids Ø Due to psychological disorders Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Diseases of the Anterior Pituitary Hypopituitarism – insufficient secretion of one or more pituitary hormones. Etiology – pituitary infarction, head trauma, infections, and tumors Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
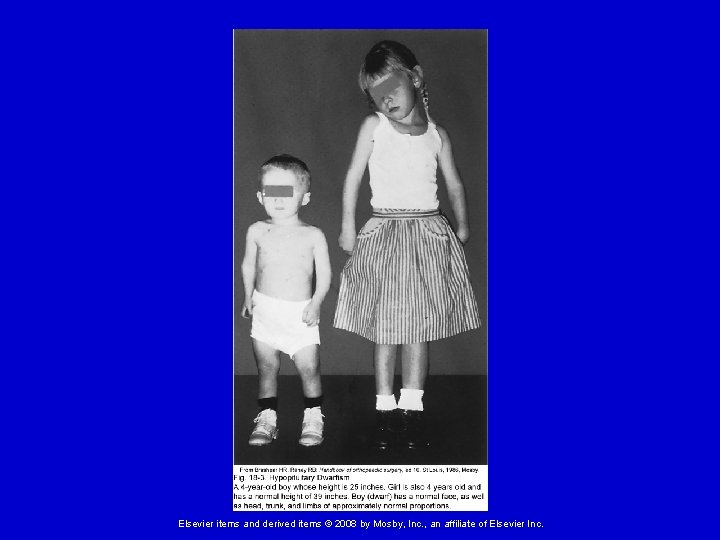
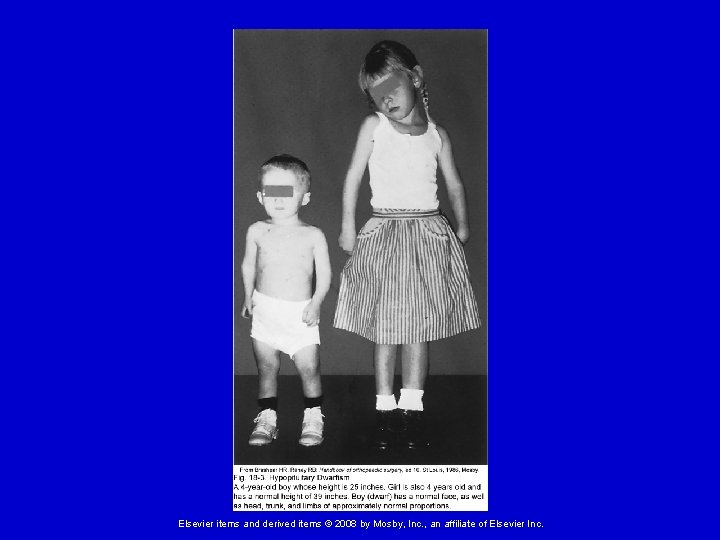
Diseases of the Anterior Pituitary Panhypopituitarism – decreased or absent secretion of all pituitary hormones. Ø ACTH deficiency – causes cortisol deficiency (life- threatening). Ø TSH deficiency – causes thyroid hormone deficiency. Ø FSH and LH deficiency – causes gonadal failure and loss of secondary sex characteristics. Ø GH deficiency – causes pituitary dwarfism. Ø ADH deficiency – causes diabetes insipidus. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Diseases of the Anterior Pituitary Hyperpituitarism Etiology – commonly caused by a benign slow-growing pituitary adenoma. Ø Hypersecretes the hormone of the cell type from which it arose, independent of regulation. Manifestations: Headache and fatigue Ø Visual changes Ø Hyposecretion of neighboring anterior pituitary hormones due to pressure atrophy Ø Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
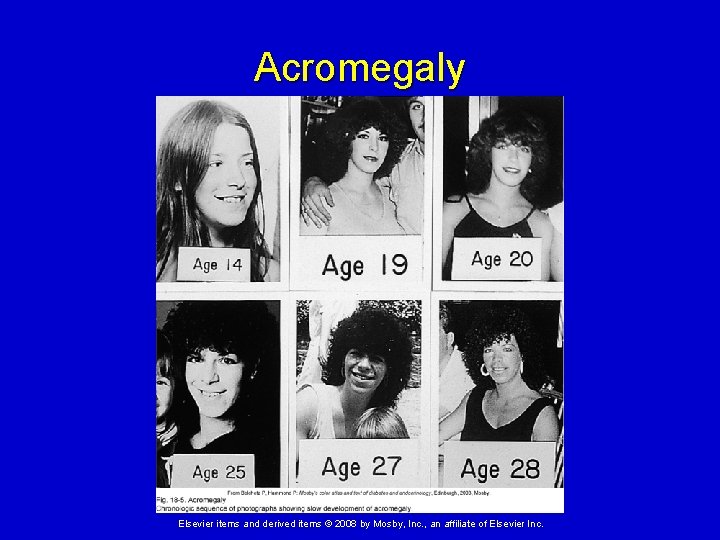
Diseases of the Anterior Pituitary Hypersecretion of growth hormone (GH) Acromegaly - hypersecretion of GH during adulthood (after closure of epiphyseal plates) Ø Proliferation of connective tissue and bony matrix creates course facial features, large hands and feet, etc. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
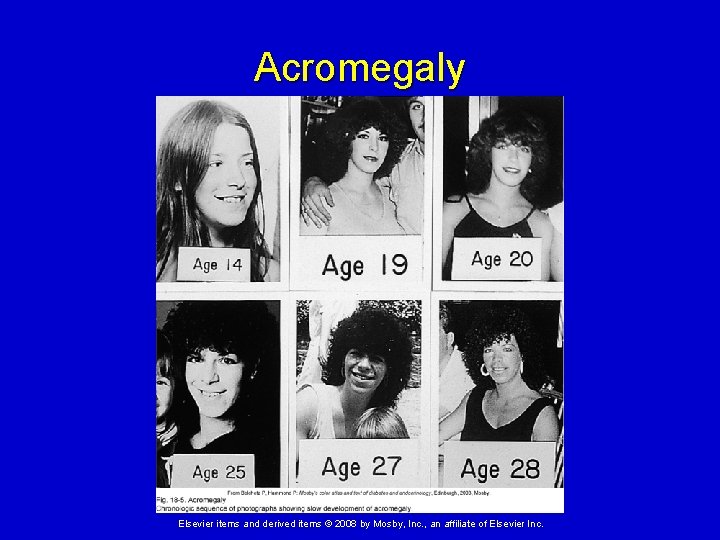
Acromegaly Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
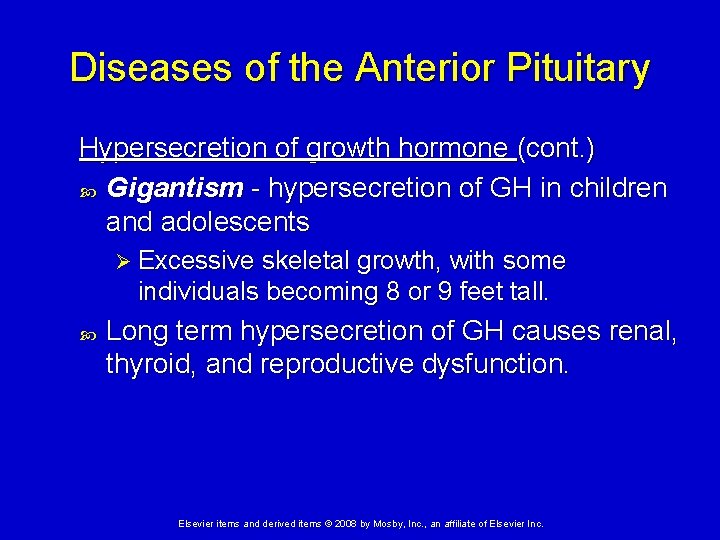
Diseases of the Anterior Pituitary Hypersecretion of growth hormone (cont. ) Gigantism - hypersecretion of GH in children and adolescents Ø Excessive skeletal growth, with some individuals becoming 8 or 9 feet tall. Long term hypersecretion of GH causes renal, thyroid, and reproductive dysfunction. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
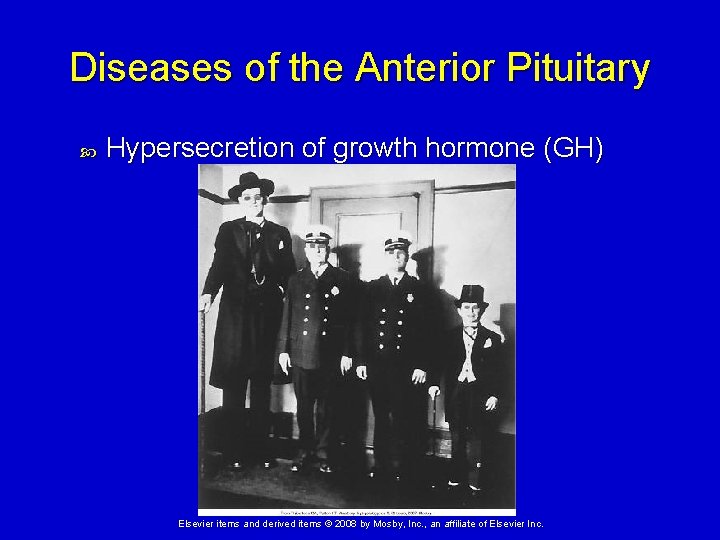
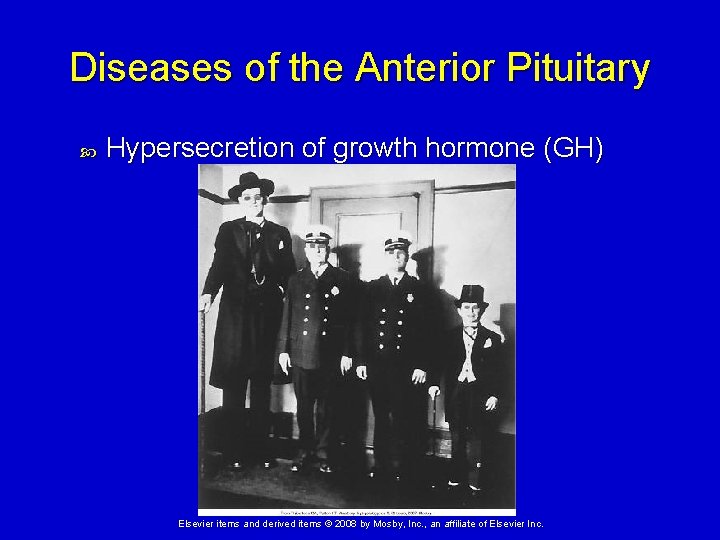
Diseases of the Anterior Pituitary Hypersecretion of growth hormone (GH) Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Diseases of the Anterior Pituitary Hypersecretion of prolactin Caused by prolactinomas – most common hormone-secreting pituitary tumor Manifestations: Ø In females - amenorrhea, galactorrhea (milk production without pregnancy), hirsutism, and osteopenia Ø In males - hypogonadism, erectile dysfunction, impaired libido, oligospermia, and diminished ejaculate volume Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
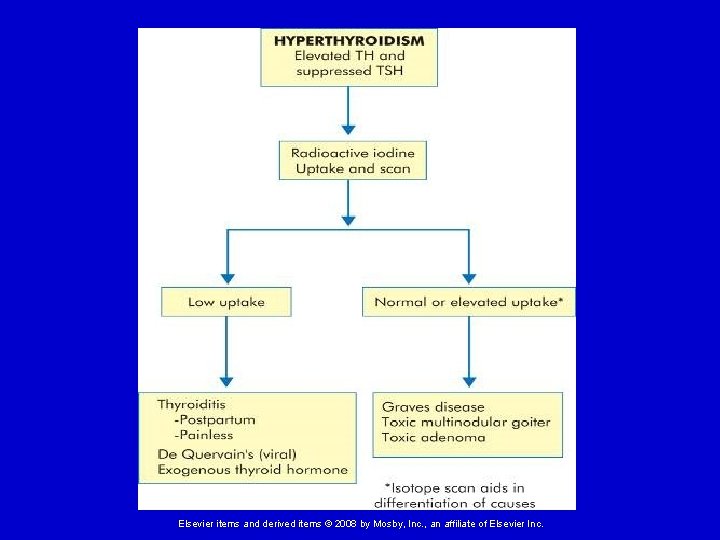
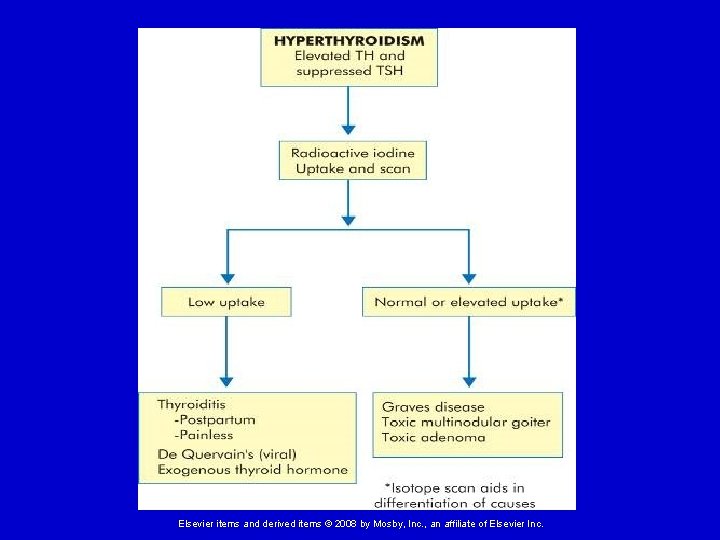
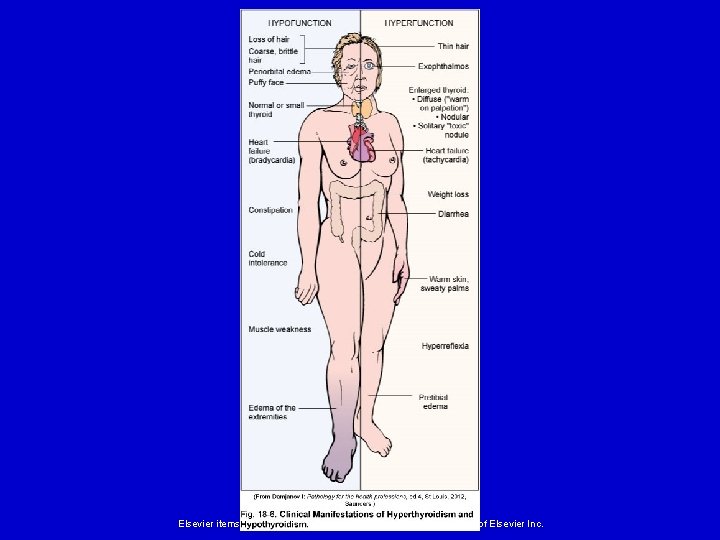
Alterations of Thyroid Function Hyperthyroidism Thyrotoxicosis - general condition in which elevated thyroid hormone (TH; T 3 and T 4) levels cause greater than normal physiologic responses. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
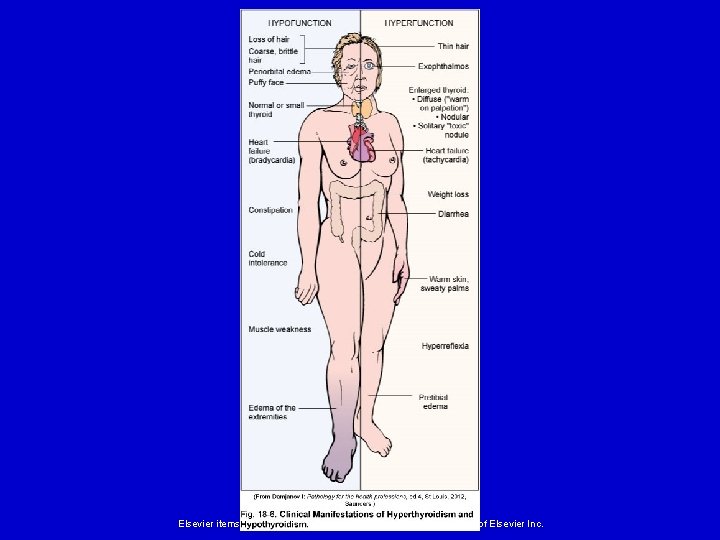
Alterations of Thyroid Function Hyperthyroidism (cont. ) Manifestations of thyroid hormone excess: Enlarged thyroid gland Ø Increase in metabolic rate and heat production (causes flushed skin and perspiration) Ø Nervous excitability and insomnia Ø Increased heart rate and cardiac dysrhythmias; heart failure (in extreme cases) Ø Weight loss Ø GI hyperactivity, diarrhea & vitamin deficiencies Ø Thinning of hair and skin Ø Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
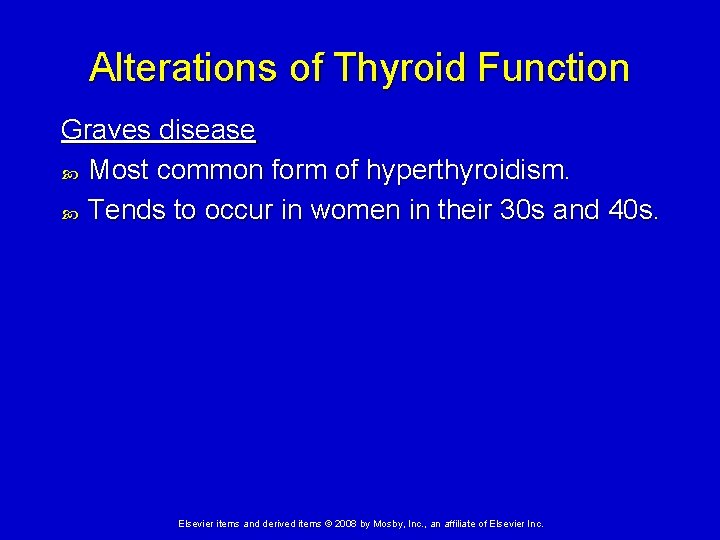
Alterations of Thyroid Function Graves disease Most common form of hyperthyroidism. Tends to occur in women in their 30 s and 40 s. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
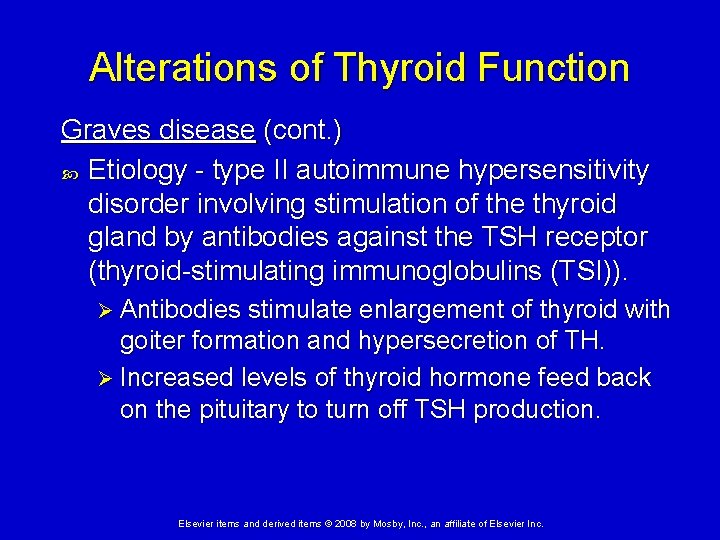
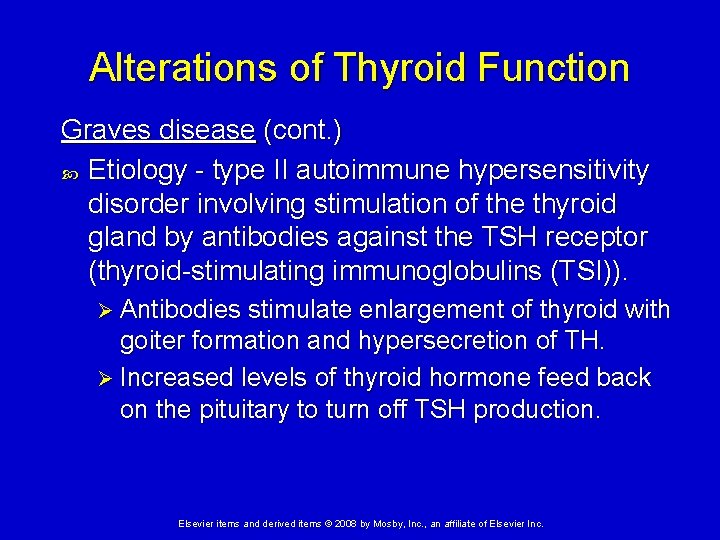
Alterations of Thyroid Function Graves disease (cont. ) Etiology - type II autoimmune hypersensitivity disorder involving stimulation of the thyroid gland by antibodies against the TSH receptor (thyroid-stimulating immunoglobulins (TSI)). Ø Antibodies stimulate enlargement of thyroid with goiter formation and hypersecretion of TH. Ø Increased levels of thyroid hormone feed back on the pituitary to turn off TSH production. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
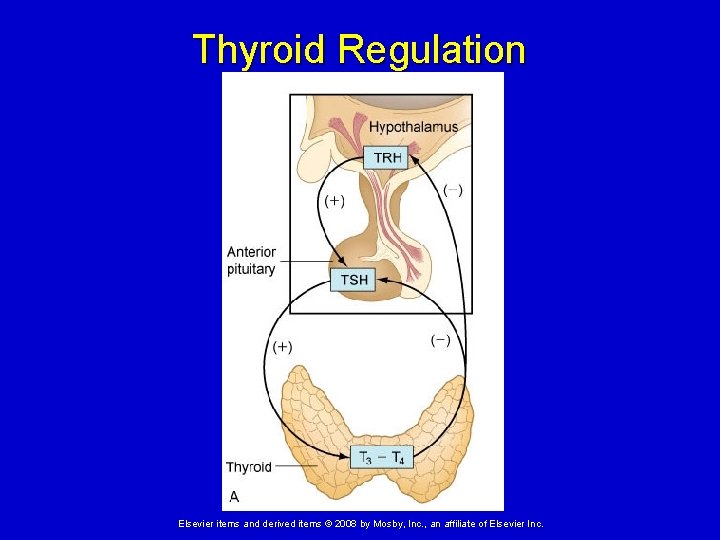
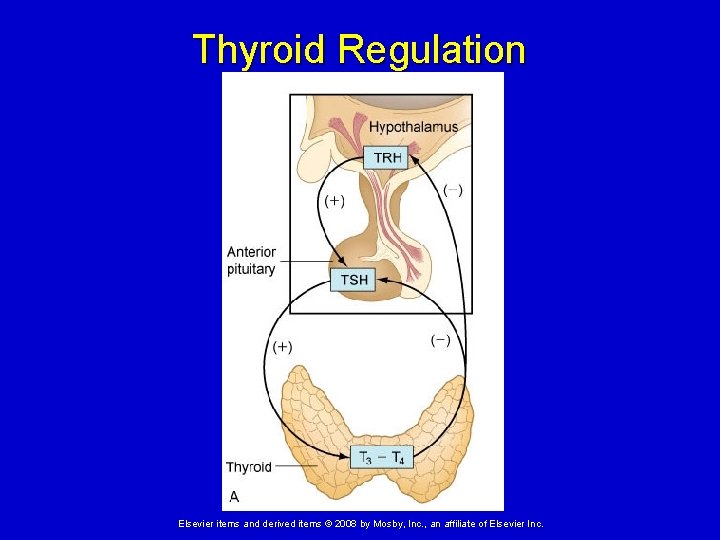
Thyroid Regulation Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
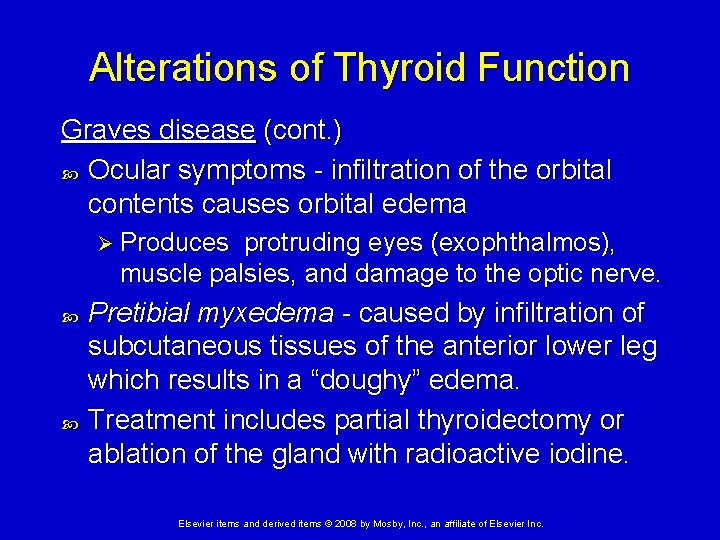
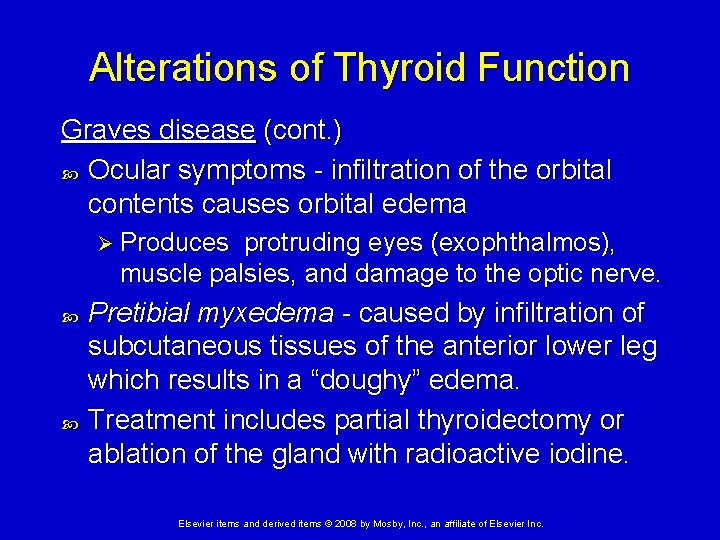
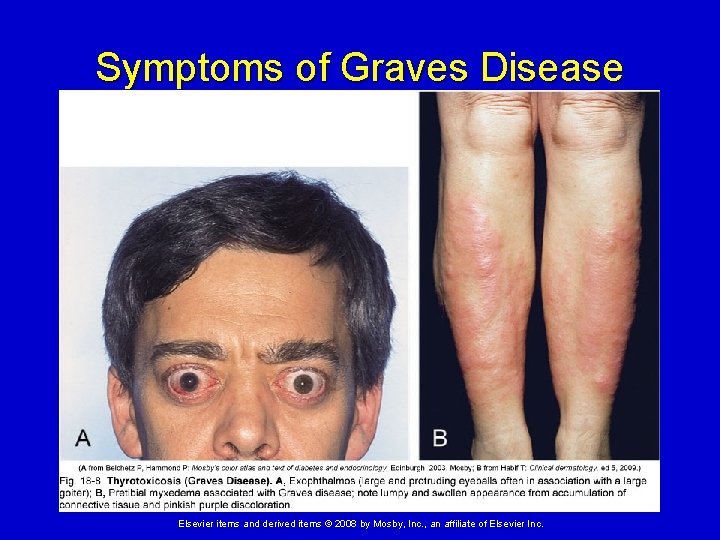
Alterations of Thyroid Function Graves disease (cont. ) Ocular symptoms - infiltration of the orbital contents causes orbital edema Ø Produces protruding eyes (exophthalmos), muscle palsies, and damage to the optic nerve. Pretibial myxedema - caused by infiltration of subcutaneous tissues of the anterior lower leg which results in a “doughy” edema. Treatment includes partial thyroidectomy or ablation of the gland with radioactive iodine. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
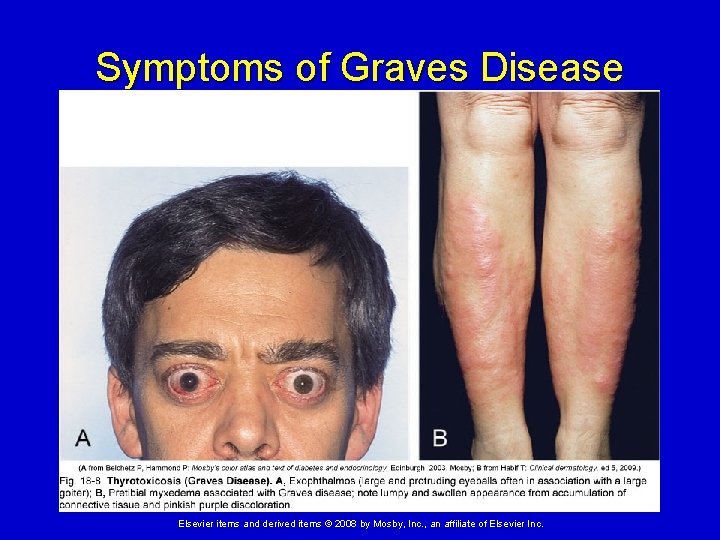
Symptoms of Graves Disease Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
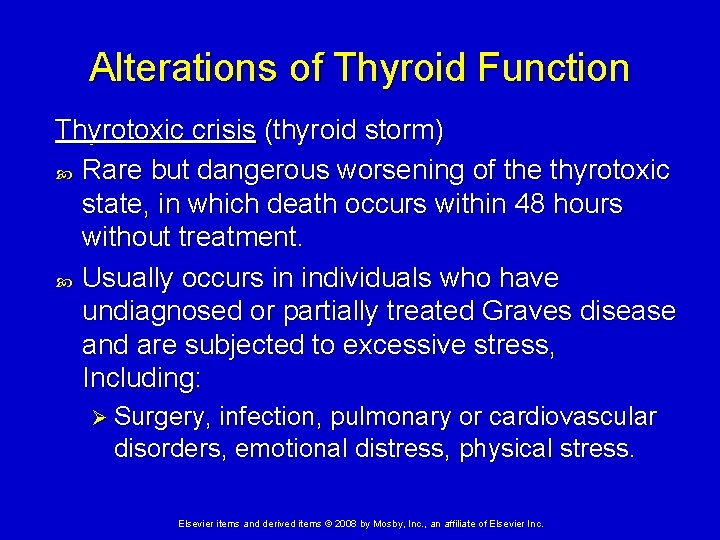
Alterations of Thyroid Function Thyrotoxic crisis (thyroid storm) Rare but dangerous worsening of the thyrotoxic state, in which death occurs within 48 hours without treatment. Usually occurs in individuals who have undiagnosed or partially treated Graves disease and are subjected to excessive stress, Including: Ø Surgery, infection, pulmonary or cardiovascular disorders, emotional distress, physical stress. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
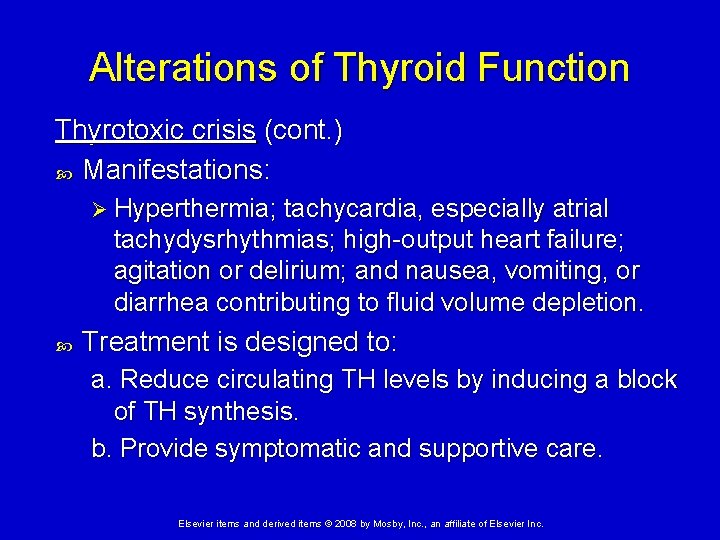
Alterations of Thyroid Function Thyrotoxic crisis (cont. ) Manifestations: Ø Hyperthermia; tachycardia, especially atrial tachydysrhythmias; high-output heart failure; agitation or delirium; and nausea, vomiting, or diarrhea contributing to fluid volume depletion. Treatment is designed to: a. Reduce circulating TH levels by inducing a block of TH synthesis. b. Provide symptomatic and supportive care. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Alterations of Thyroid Function Hypothyroidism Insufficient secretion of TH by the thyroid gland. Manifestations of thyroid hormone deficiency: Size of thyroid gland varies, depending on cause; may be small, normal or enlarged. Ø Decreased metabolic rate and body temperature; cold intolerance. Ø Weaker, more sluggish muscle contractions, which cause constipation and decreased cardiac contractility Ø Slow heart rate and decreased cardiac output Ø Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Alterations of Thyroid Function Hypothyroidism Manifestations of thyroid hormone deficiency (cont. ): Increased body weight Ø Rise in blood cholesterol levels (contributes to atherosclerosis) Ø Decreased sex drive, and menstrual irregularities Ø Depression of mental functioning and sleepiness Ø Course, brittle hair and hair loss Ø Severity is proportional to degree of hyposecretion. Ø Myxedema Ø Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
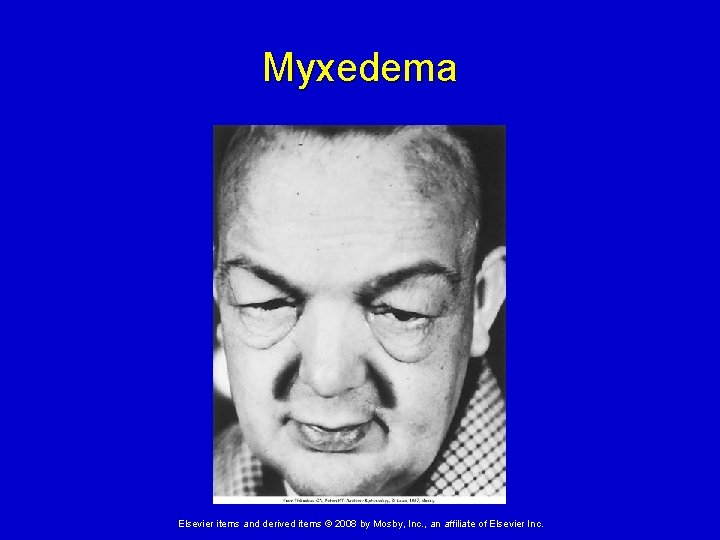
Alterations of Thyroid Function Hypothyroidism Myxedema Ø Characteristic sign of severe of long-standing hypothyroidism. Ø Altered composition of the dermis and other tissues. Ø Produces a nonpitting, boggy edema, especially around the eyes, hands, and feet. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
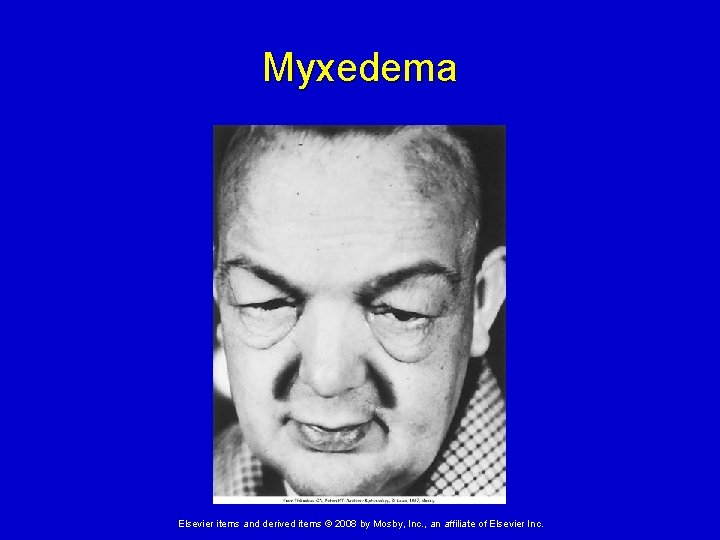
Myxedema Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
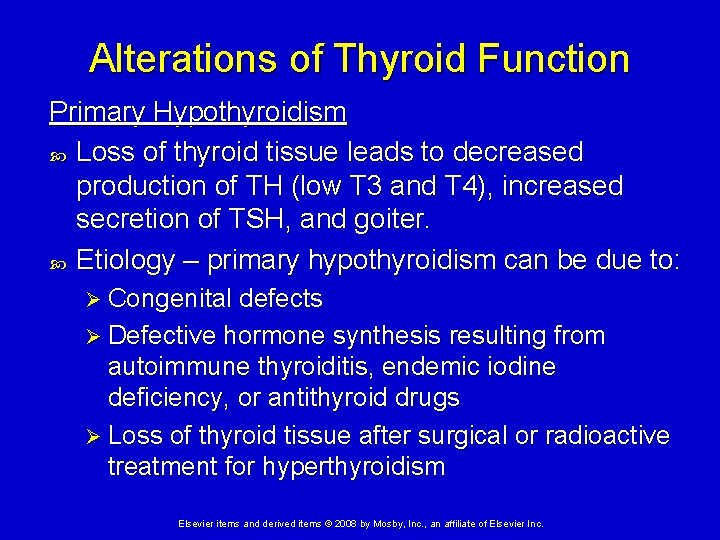
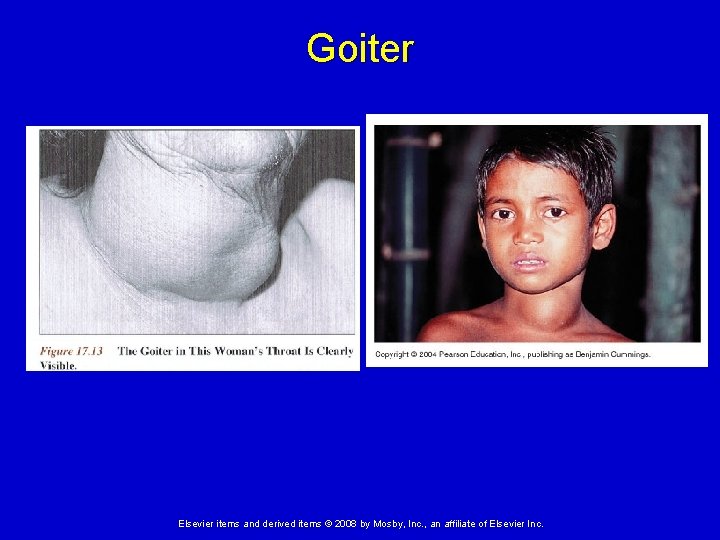
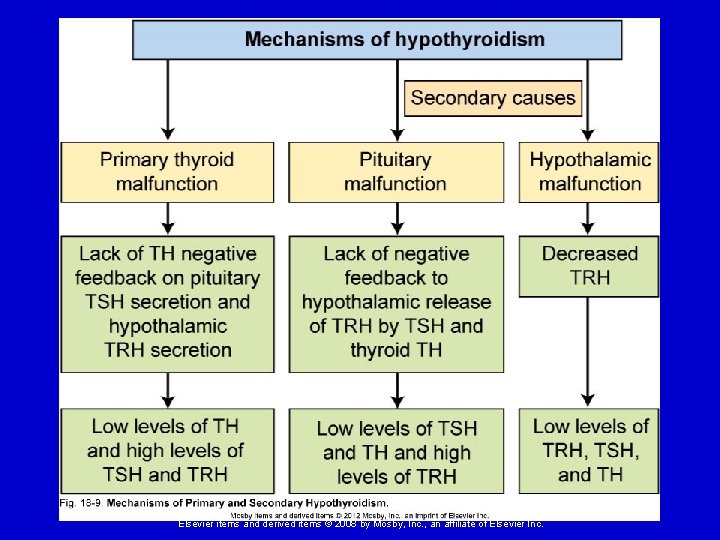
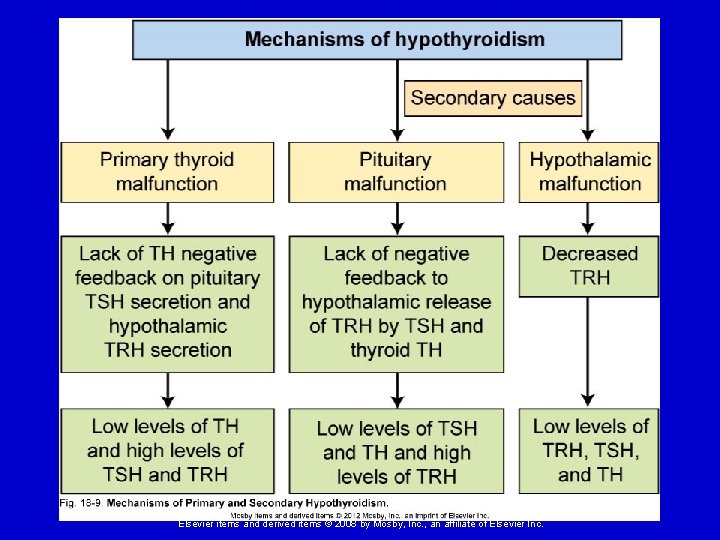
Alterations of Thyroid Function Primary Hypothyroidism Loss of thyroid tissue leads to decreased production of TH (low T 3 and T 4), increased secretion of TSH, and goiter. Etiology – primary hypothyroidism can be due to: Ø Congenital defects Ø Defective hormone synthesis resulting from autoimmune thyroiditis, endemic iodine deficiency, or antithyroid drugs Ø Loss of thyroid tissue after surgical or radioactive treatment for hyperthyroidism Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
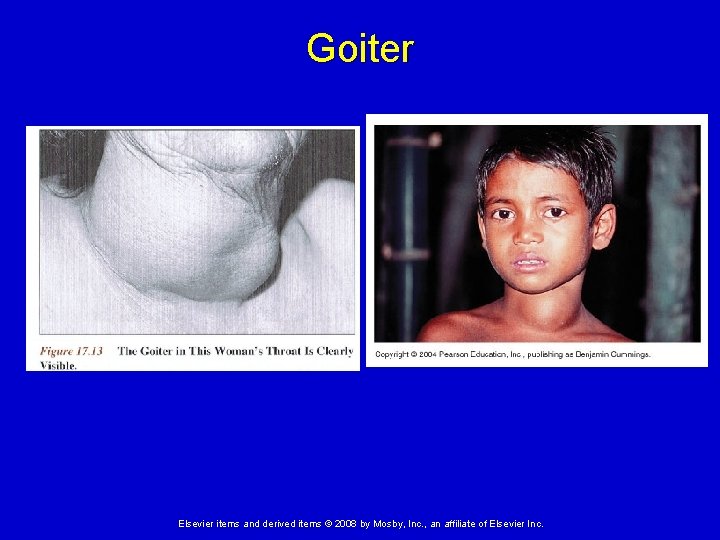
Goiter Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
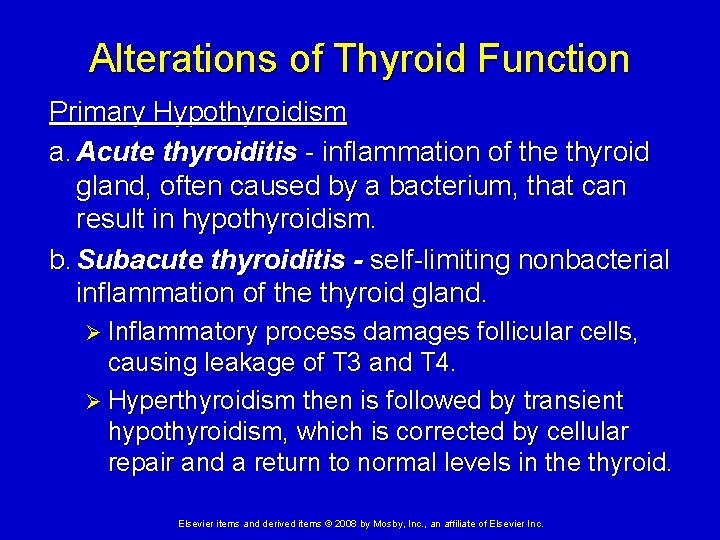
Alterations of Thyroid Function Primary Hypothyroidism a. Acute thyroiditis - inflammation of the thyroid gland, often caused by a bacterium, that can result in hypothyroidism. b. Subacute thyroiditis - self-limiting nonbacterial inflammation of the thyroid gland. Ø Inflammatory process damages follicular cells, causing leakage of T 3 and T 4. Ø Hyperthyroidism then is followed by transient hypothyroidism, which is corrected by cellular repair and a return to normal levels in the thyroid. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
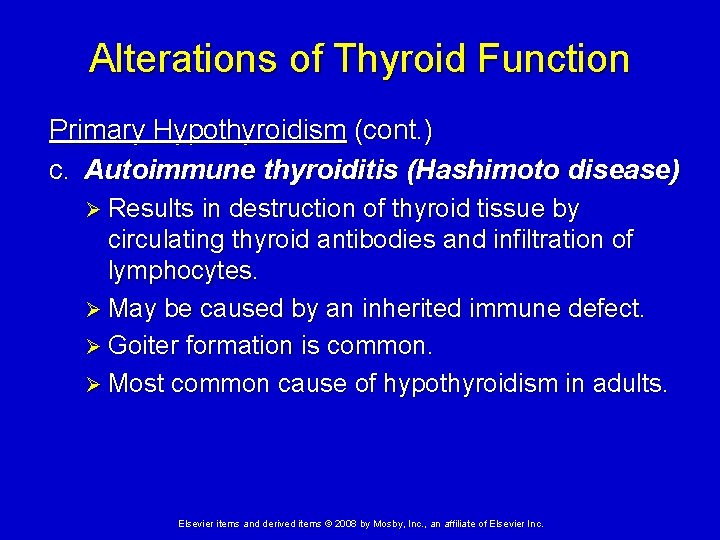
Alterations of Thyroid Function Primary Hypothyroidism (cont. ) c. Autoimmune thyroiditis (Hashimoto disease) Ø Results in destruction of thyroid tissue by circulating thyroid antibodies and infiltration of lymphocytes. Ø May be caused by an inherited immune defect. Ø Goiter formation is common. Ø Most common cause of hypothyroidism in adults. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
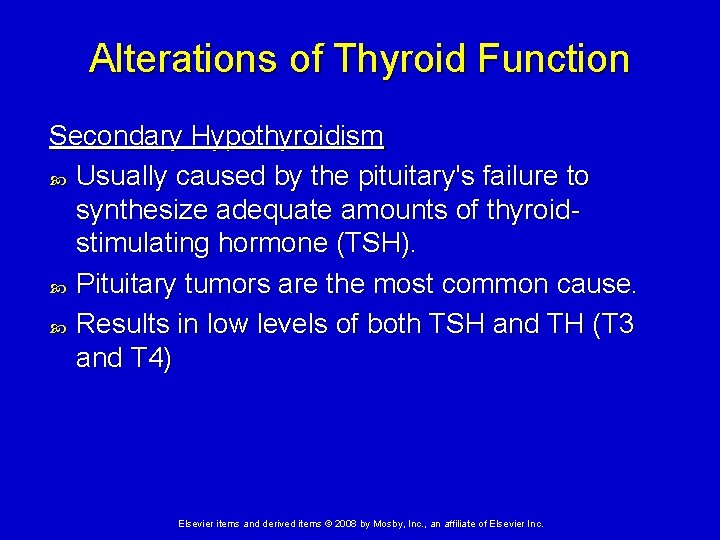
Alterations of Thyroid Function Secondary Hypothyroidism Usually caused by the pituitary's failure to synthesize adequate amounts of thyroidstimulating hormone (TSH). Pituitary tumors are the most common cause. Results in low levels of both TSH and TH (T 3 and T 4) Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
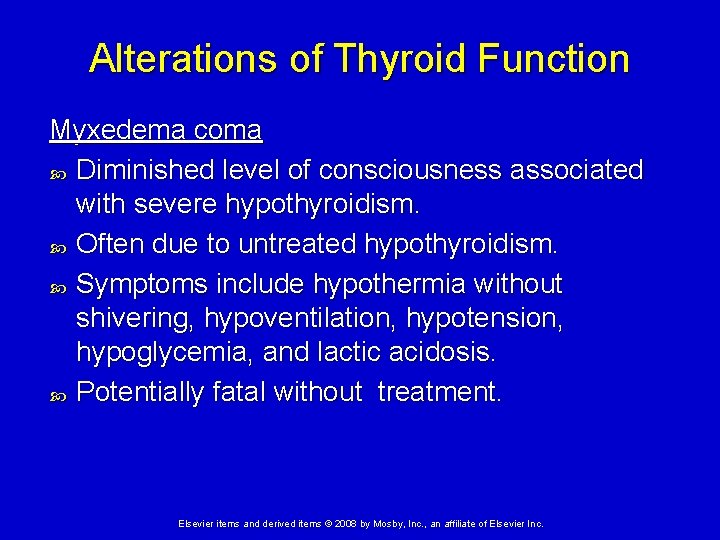
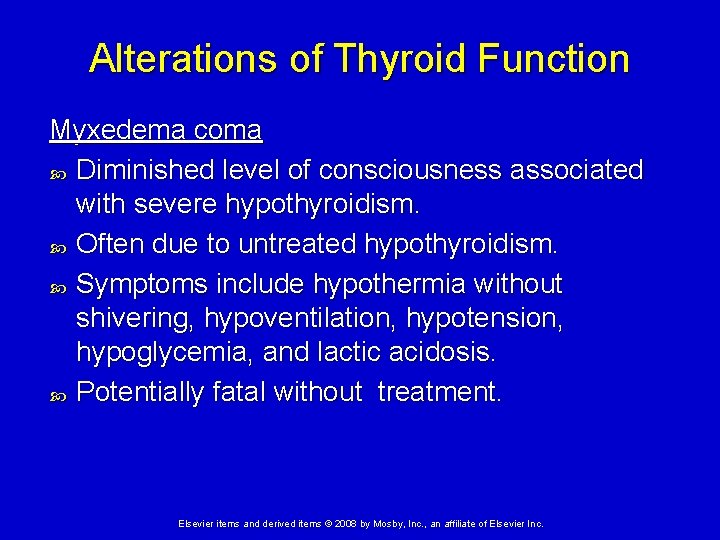
Alterations of Thyroid Function Myxedema coma Diminished level of consciousness associated with severe hypothyroidism. Often due to untreated hypothyroidism. Symptoms include hypothermia without shivering, hypoventilation, hypotension, hypoglycemia, and lactic acidosis. Potentially fatal without treatment. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
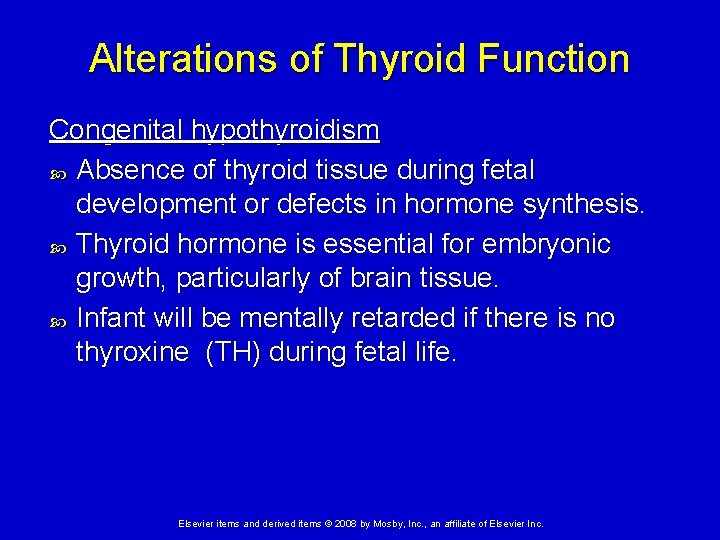
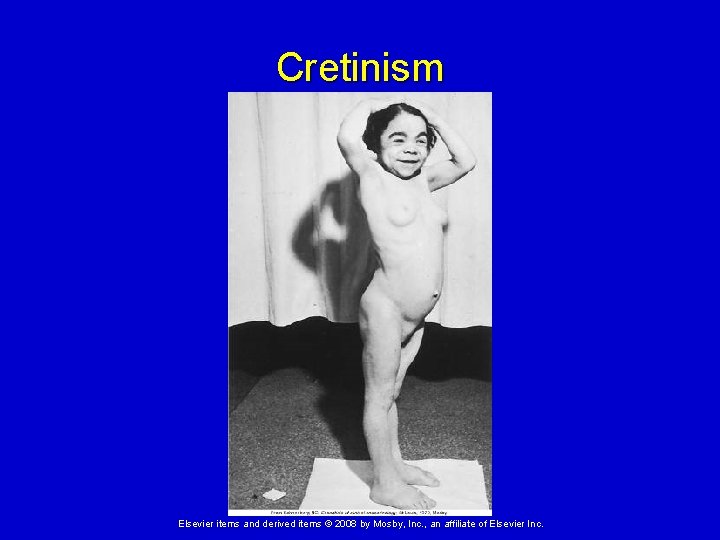
Alterations of Thyroid Function Congenital hypothyroidism Absence of thyroid tissue during fetal development or defects in hormone synthesis. Thyroid hormone is essential for embryonic growth, particularly of brain tissue. Infant will be mentally retarded if there is no thyroxine (TH) during fetal life. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
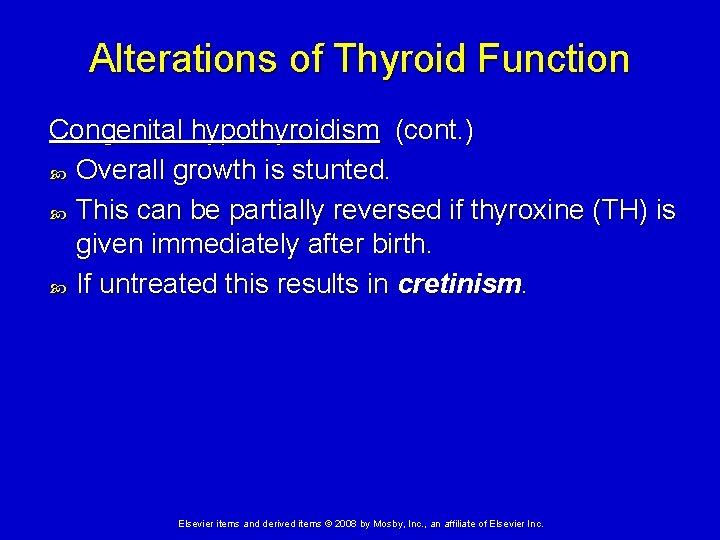
Alterations of Thyroid Function Congenital hypothyroidism (cont. ) Overall growth is stunted. This can be partially reversed if thyroxine (TH) is given immediately after birth. If untreated this results in cretinism. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
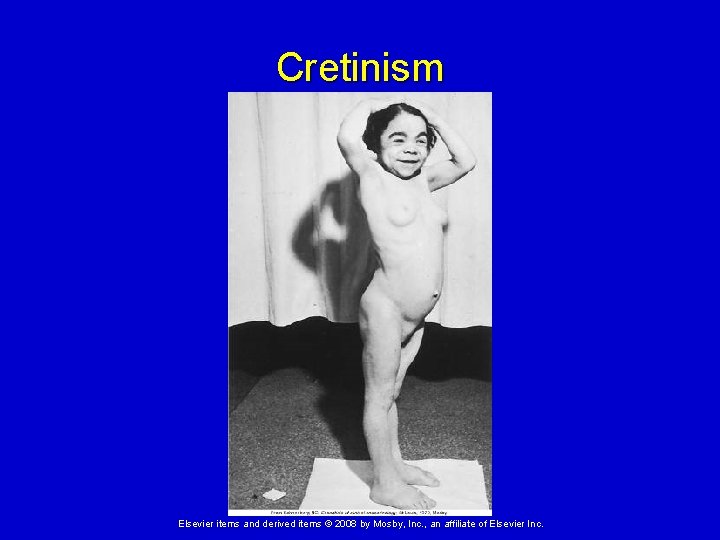
Cretinism Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
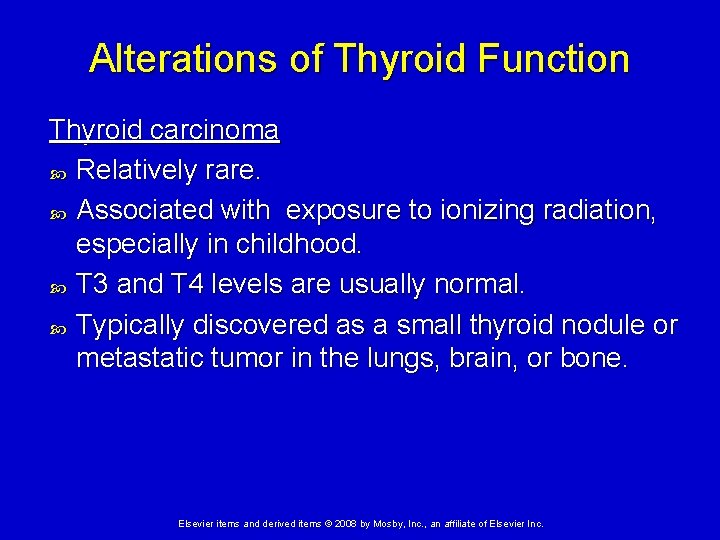
Alterations of Thyroid Function Thyroid carcinoma Relatively rare. Associated with exposure to ionizing radiation, especially in childhood. T 3 and T 4 levels are usually normal. Typically discovered as a small thyroid nodule or metastatic tumor in the lungs, brain, or bone. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Alterations of Parathyroid Function Cause profound effects on calcium homeostasis and bone health. Parathyroid hormone (PTH) helps to maintain normal serum calcium levels by stimulating the breakdown of bone and by increasing renal and gastric absorption of calcium. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Alterations of Parathyroid Function Hyperparathyroidism Excess secretion of PTH causes hypercalcemia and bone destruction. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Alterations of Parathyroid Function Primary hyperparathyroidism Excess secretion of PTH from one or more parathyroid glands Usually caused by an adenoma of the chief cells in the parathyroid gland. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Alterations of Parathyroid Function Primary hyperparathyroidism (cont. ) Manifestations: Ø Very high serum levels of calcium cause neurologic, gastric, and muscular dysfunction. Ø Bone resorption leads to osteopenia, osteoporosis, bone fragility, and pathologic fractures. Ø Hypercalcemia and hypercalciuria can contribute to the formation of renal calculi. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Alterations of Parathyroid Function Secondary hyperparathyroidism (cont. ) Increase in PTH secondary to a chronic disease. Usually a result of chronic renal failure. Ø Kidney cannot activate vitamin D and cannot adequately reabsorb calcium from tubules. Ø Persistent hypocalcemia results in increased PTH secretion, causing osteopenia Ø They exhibit bone fragility but without the signs and symptoms of hypercalcemia. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Alterations of Parathyroid Function Hypoparathyroidism Abnormally low PTH level causes inability to maintain normal serum calcium levels. Usually caused by parathyroid injury or removal during thyroid surgery Lack of PTH causes depressed serum calcium levels, increased serum phosphate levels, decreased bone resorption, and eventual hypocalciuria. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Alterations of Parathyroid Function Hypoparathyroidism (cont. ) Manifestations are primarily those of hypocalcemia: Ø Lowered threshold for nerve and muscle excitation, causing muscle spasms, hyperreflexia, clonic-tonic convulsions, laryngeal spasms, and, in severe cases, death by asphyxiation. Ø Also dry skin, alopecia, poor dentition, skeletal deformity. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Dysfunction of the Endocrine Pancreas Types of Diabetes Mellitus: Diabetes mellitus is a group of disorders characterized by glucose intolerance, chronic hyperglycemia, and disturbances of carbohydrate, protein, and fat metabolism. Classic signs and symptoms are often present as well (polyuria, polydipsia, polyphagia). Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Type 1 Diabetes Mellitus Insulin dependent diabetes mellitus (IDDM) Results from a severe, absolute lack of insulin caused by loss of pancreatic beta cells. Usually occurs in younger people. About 10% of DM cases. Type 1 A – immune-mediated (about 9%) Ø Type 1 B – idiopathic (about 1%) Ø Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
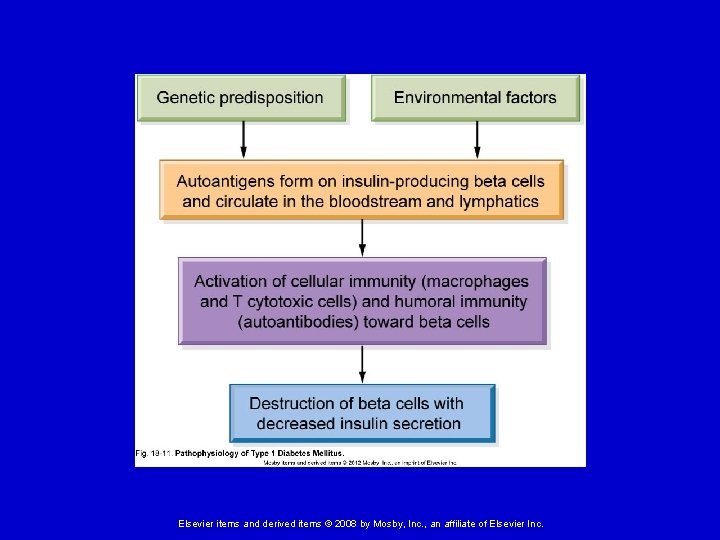
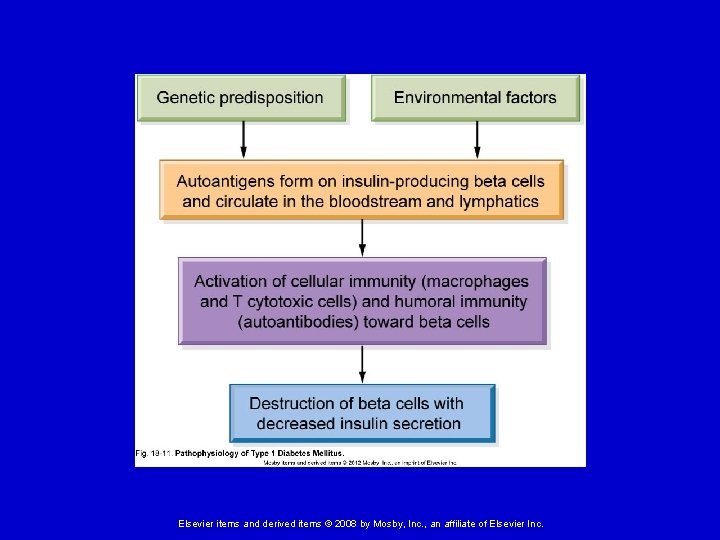
Type 1 Diabetes Mellitus Pathophysiology of Type 1 A: Ø In genetically vulnerable individuals an environmental trigger causes: • Production of autoantibodies against beta cells and insulin. • Cellular and cytokine-mediated injury (type IV hypersensitivity) • Destruction of insulin-secreting beta cells Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
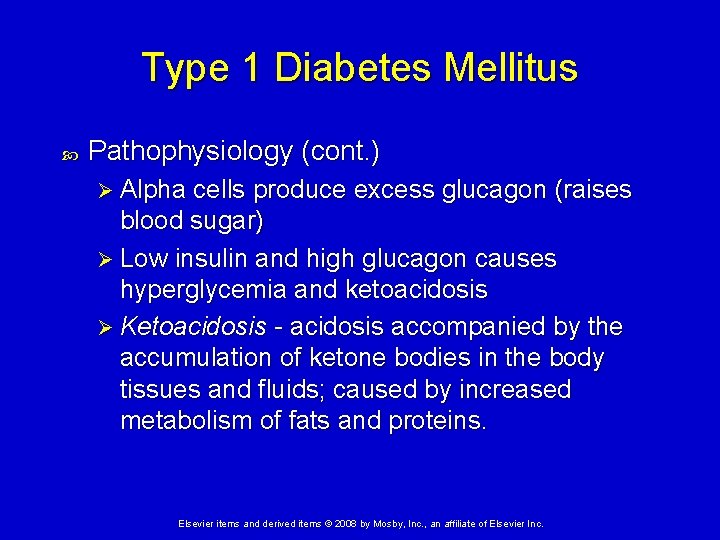
Type 1 Diabetes Mellitus Pathophysiology (cont. ) Ø Alpha cells produce excess glucagon (raises blood sugar) Ø Low insulin and high glucagon causes hyperglycemia and ketoacidosis Ø Ketoacidosis - acidosis accompanied by the accumulation of ketone bodies in the body tissues and fluids; caused by increased metabolism of fats and proteins. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
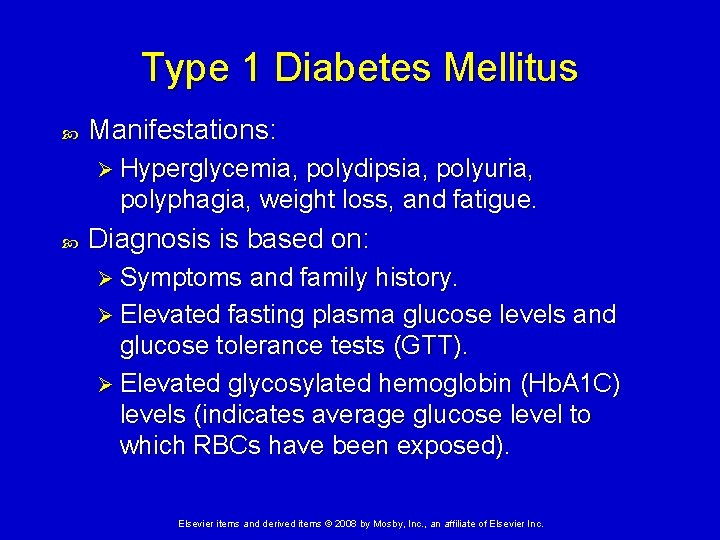
Type 1 Diabetes Mellitus Manifestations: Ø Hyperglycemia, polydipsia, polyuria, polyphagia, weight loss, and fatigue. Diagnosis is based on: Ø Symptoms and family history. Ø Elevated fasting plasma glucose levels and glucose tolerance tests (GTT). Ø Elevated glycosylated hemoglobin (Hb. A 1 C) levels (indicates average glucose level to which RBCs have been exposed). Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Type 1 Diabetes Mellitus Exercise allows uptake of glucose without insulin, so can cause hypoglycemia or reduce insulin requirement. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
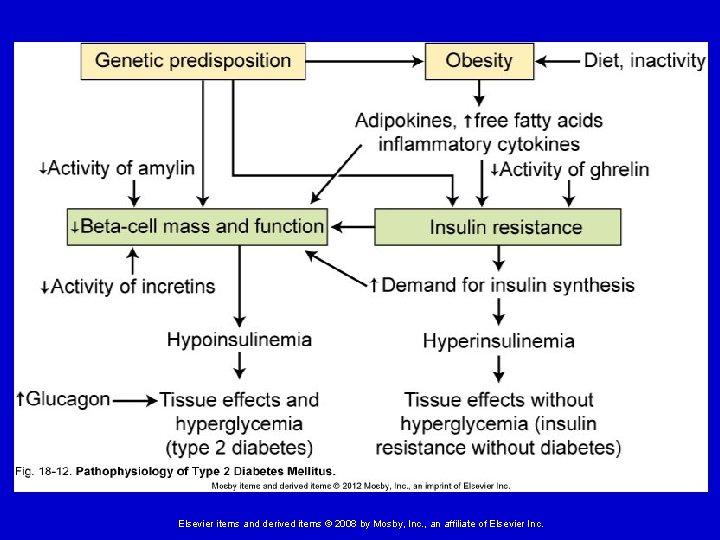
Type 2 Diabetes Mellitus Non-insulin dependent diabetes mellitus (NIDDM) Results from a combination of insulin resistance and declining insulin secretion. About 90% of DM cases. Usually diagnosed later in life, although increasing in younger groups. Strong genetic component; very common in certain ethnic groups. Triggered by environmental factors, including obesity, poor diet, and lack of exercise. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
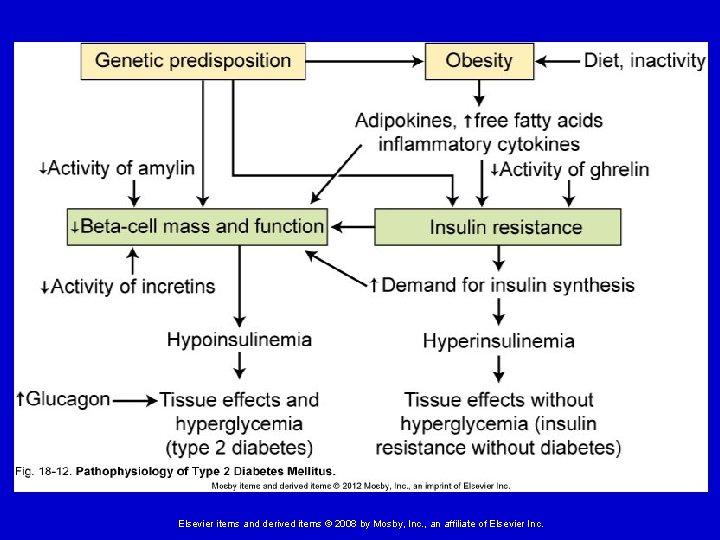
Type 2 Diabetes Mellitus Pathophysiology: Ø In the obese, insulin has a diminished ability to influence glucose uptake and metabolism (insulin resistance of target tissues). Ø Some insulin production continues in type 2 diabetes mellitus, but the size and number of beta cells decrease. Initially insulin secretion may be high, but it declines with time. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
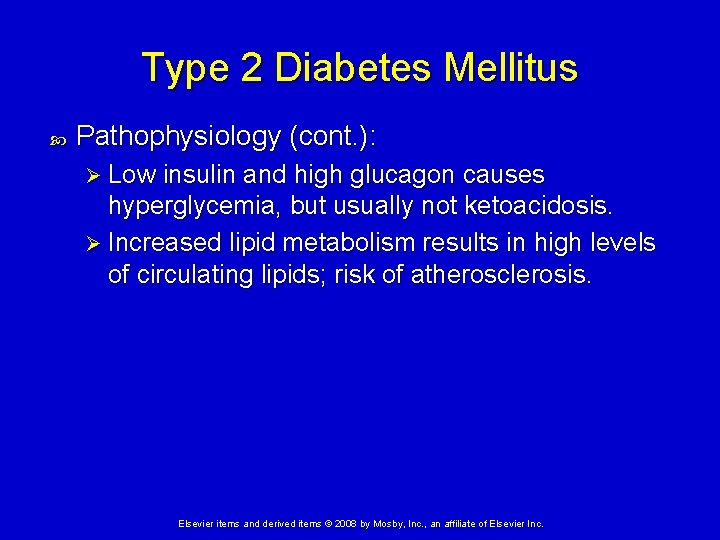
Type 2 Diabetes Mellitus Pathophysiology (cont. ): Ø Low insulin and high glucagon causes hyperglycemia, but usually not ketoacidosis. Ø Increased lipid metabolism results in high levels of circulating lipids; risk of atherosclerosis. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Gestational Diabetes Occurs when a woman not previously diagnosed with diabetes shows glucose intolerance during pregnancy. Can cause potentially life threatening complications for both mother and fetus. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
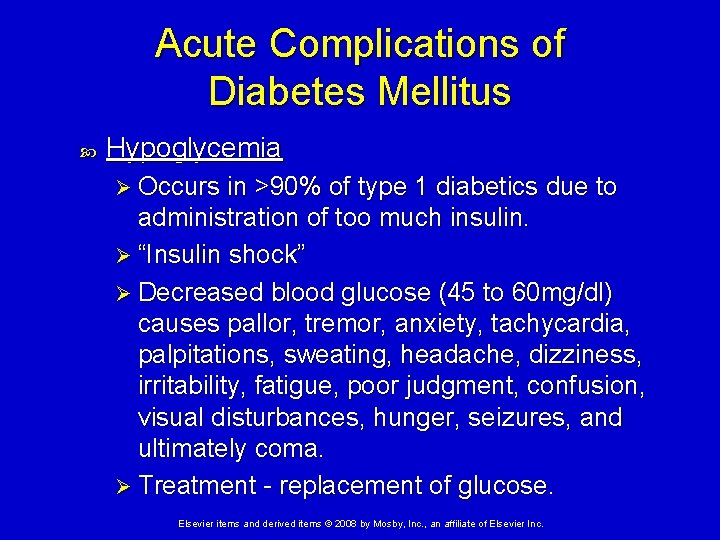
Acute Complications of Diabetes Mellitus Hypoglycemia Ø Occurs in >90% of type 1 diabetics due to administration of too much insulin. Ø “Insulin shock” Ø Decreased blood glucose (45 to 60 mg/dl) causes pallor, tremor, anxiety, tachycardia, palpitations, sweating, headache, dizziness, irritability, fatigue, poor judgment, confusion, visual disturbances, hunger, seizures, and ultimately coma. Ø Treatment - replacement of glucose. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
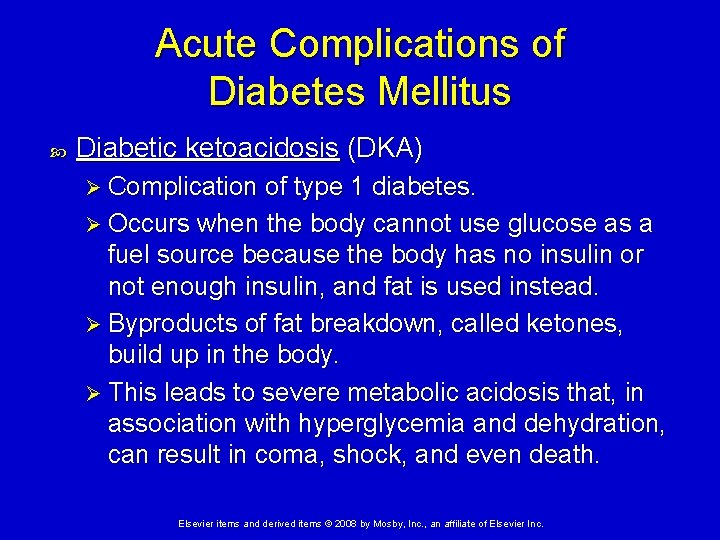
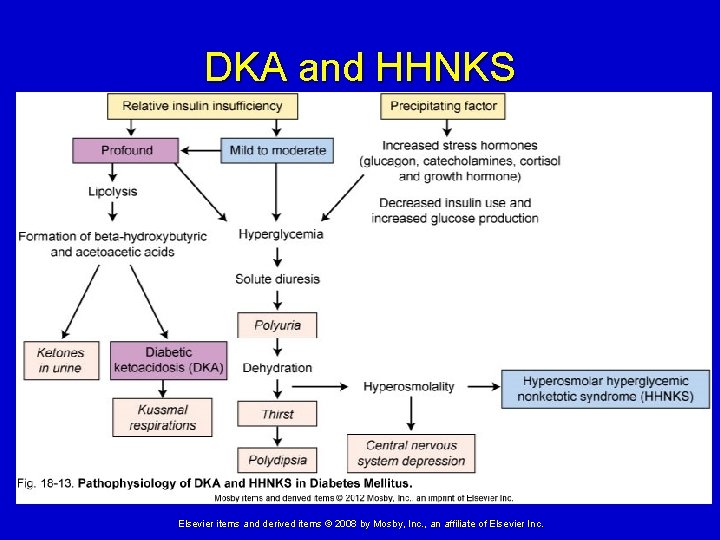
Acute Complications of Diabetes Mellitus Diabetic ketoacidosis (DKA) Ø Complication of type 1 diabetes. Ø Occurs when the body cannot use glucose as a fuel source because the body has no insulin or not enough insulin, and fat is used instead. Ø Byproducts of fat breakdown, called ketones, build up in the body. Ø This leads to severe metabolic acidosis that, in association with hyperglycemia and dehydration, can result in coma, shock, and even death. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
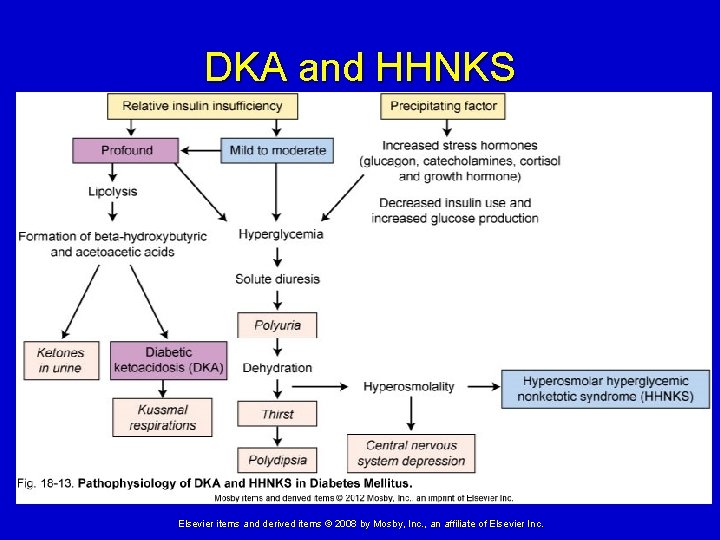
DKA and HHNKS Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
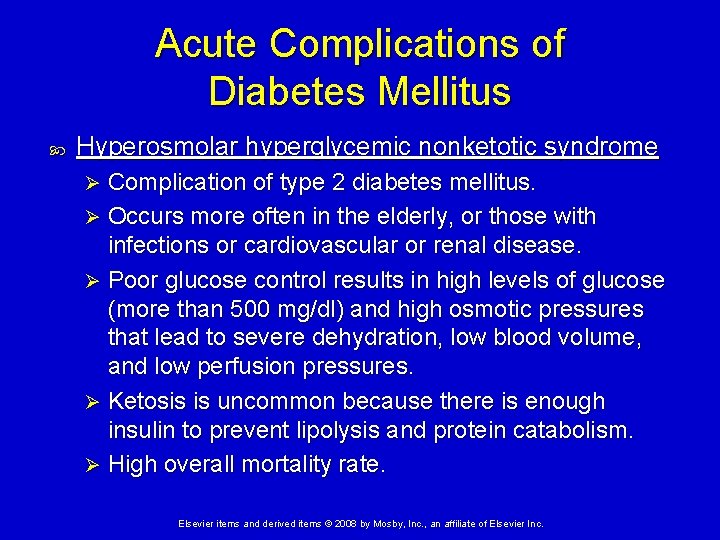
Acute Complications of Diabetes Mellitus Hyperosmolar hyperglycemic nonketotic syndrome Complication of type 2 diabetes mellitus. Ø Occurs more often in the elderly, or those with infections or cardiovascular or renal disease. Ø Poor glucose control results in high levels of glucose (more than 500 mg/dl) and high osmotic pressures that lead to severe dehydration, low blood volume, and low perfusion pressures. Ø Ketosis is uncommon because there is enough insulin to prevent lipolysis and protein catabolism. Ø High overall mortality rate. Ø Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Chronic Complications of Diabetes Mellitus Mechanisms of damage - alterations in carbohydrate, protein, and lipid metabolism (primarily hyperglycemia) adversely affects tissue in three ways: a. Glycation b. Induction of the polyol pathway c. Activation of protein kinase C Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Chronic Complications of Diabetes Mellitus a. Glycation - attachment of glucose to proteins, lipids, and nucleic acids in blood vessels, nerves, lenses, and other tissues, forming advanced glycation end products (AGEs). Ø AGEs stimulate cellular injury, inflammation, oxidation of lipoproteins, dysfunction of the endothelium (decreased vasodilators and anticoagulants) and thickening of the basement membrane. Ø Contributes to immunologic deficiencies and autoimmunity. Ø Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Chronic Complications of Diabetes Mellitus b. Induction of the polyol pathway Ø Causes conversion of glucose to sorbitol (and then slowly to fructose). Ø Sorbitol increases intracellular osmotic pressure, causing cellular edema and tissue dysfunction. Ø This process is especially important in renal cells, red blood cells, eye lens, and nerves. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Chronic Complications of Diabetes Mellitus c. Activation of protein kinase C Ø Protein kinase C (PKC) - a family of different intracellular signaling proteins. Ø Inappropriately activated by hyperglycemia. Ø Contributes to insulin resistance, tissue inflammation and edema, and production of mitogens and degradative enzymes. Ø These effects contribute to tissue remodeling and vascular dysfunction. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Sequelae of Chronic Diabetes Mellitus a. Diabetic neuropathies – nerve degeneration and delayed conduction. b. Microvascular disease – thickening and damage to the capillary wall. Ø Retinopathy – ischemia causes damage to retina. Ø Diabetic nephropathy – including end-stage renal disease; caused by damage to glomeruli. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Sequelae of Chronic Diabetes Mellitus c. Macrovascular disease – diabetes increases severity of atherosclerosis. Ø Coronary artery disease – high rate of CAD and myocardial infarction. Ø Stroke – twice as common for diabetics. Ø Peripheral arterial disease – results in gangrene and amputation. d. Infection - increased risk due to poor circulation and immune deficiencies. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
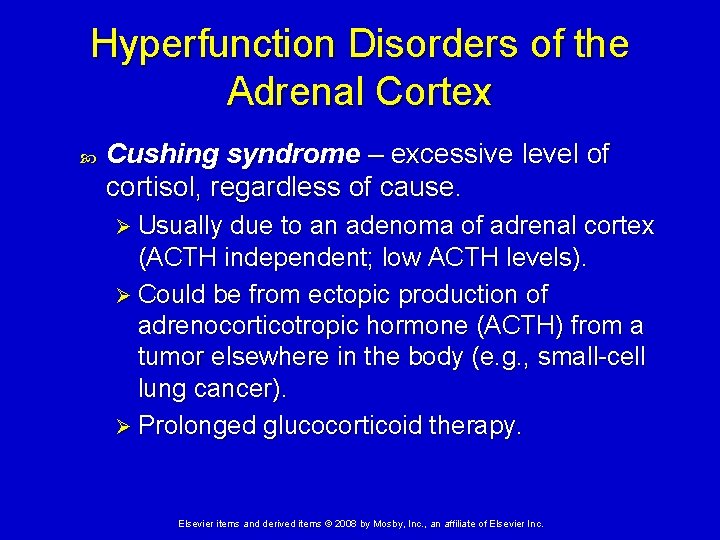
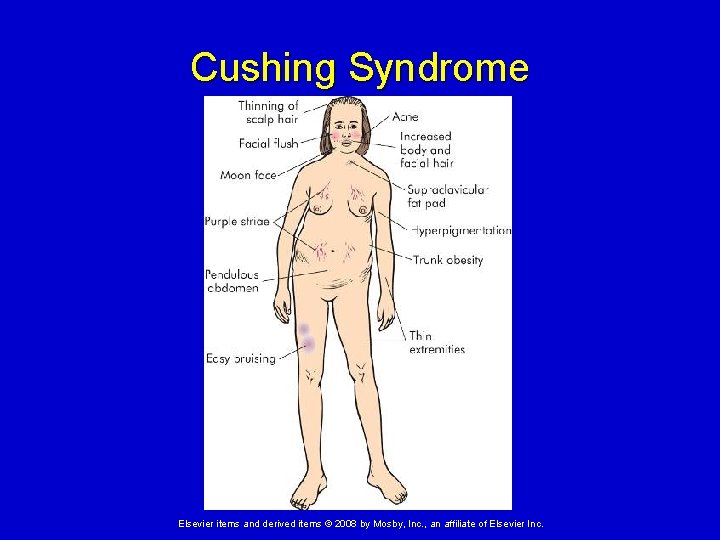
Hyperfunction Disorders of the Adrenal Cortex Hypercortisolism – disorders that result from high levels of cortisol secretion. Cushing disease – excessive anterior pituitary secretion of ACTH. Ø Usually due to a pituitary adenoma. Cushing syndrome – excessive level of cortisol, regardless of cause. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Hyperfunction Disorders of the Adrenal Cortex Cushing syndrome – excessive level of cortisol, regardless of cause. Ø Usually due to an adenoma of adrenal cortex (ACTH independent; low ACTH levels). Ø Could be from ectopic production of adrenocorticotropic hormone (ACTH) from a tumor elsewhere in the body (e. g. , small-cell lung cancer). Ø Prolonged glucocorticoid therapy. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
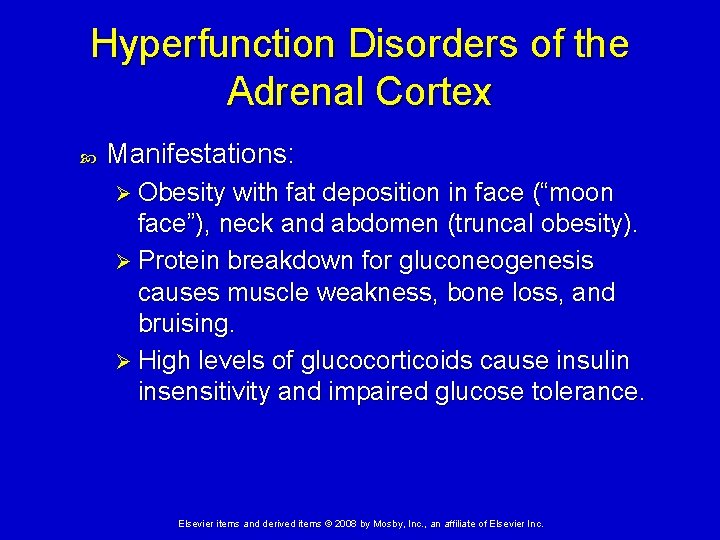
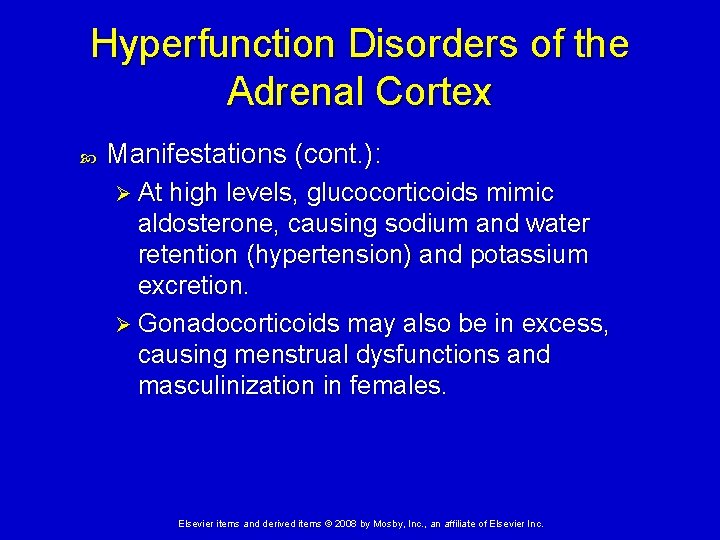
Hyperfunction Disorders of the Adrenal Cortex Manifestations: Ø Obesity with fat deposition in face (“moon face”), neck and abdomen (truncal obesity). Ø Protein breakdown for gluconeogenesis causes muscle weakness, bone loss, and bruising. Ø High levels of glucocorticoids cause insulin insensitivity and impaired glucose tolerance. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
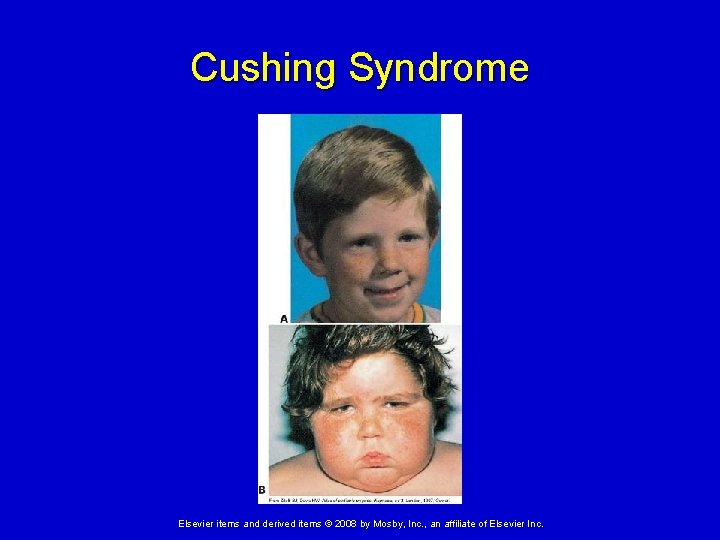
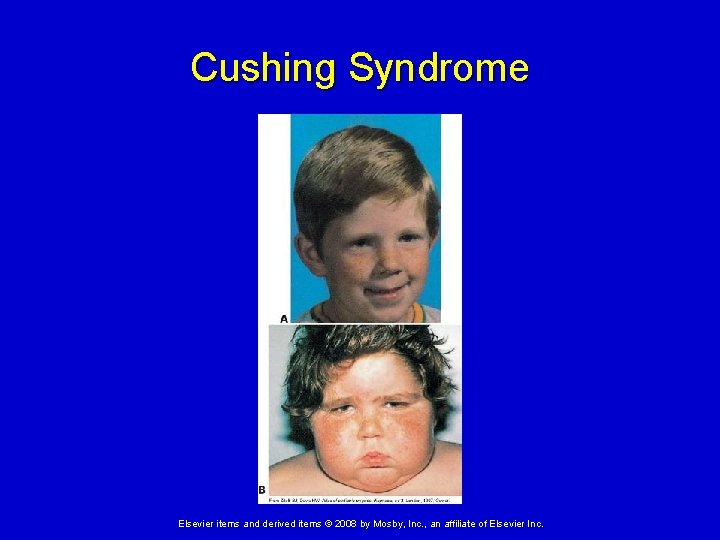
Cushing Syndrome Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
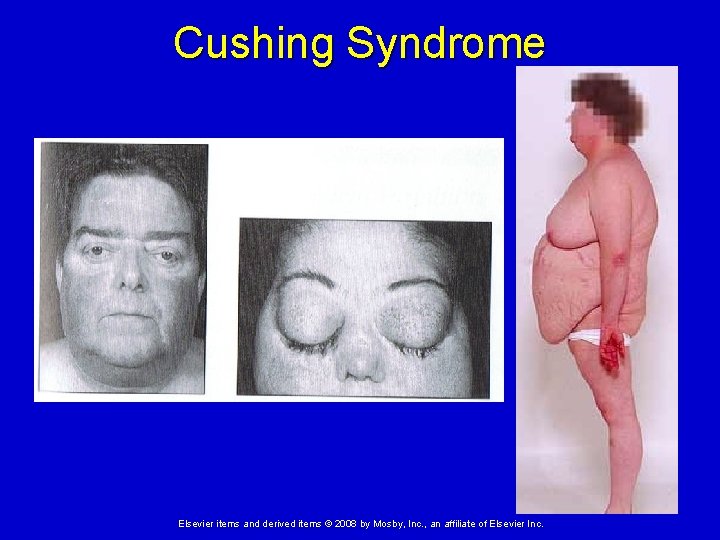
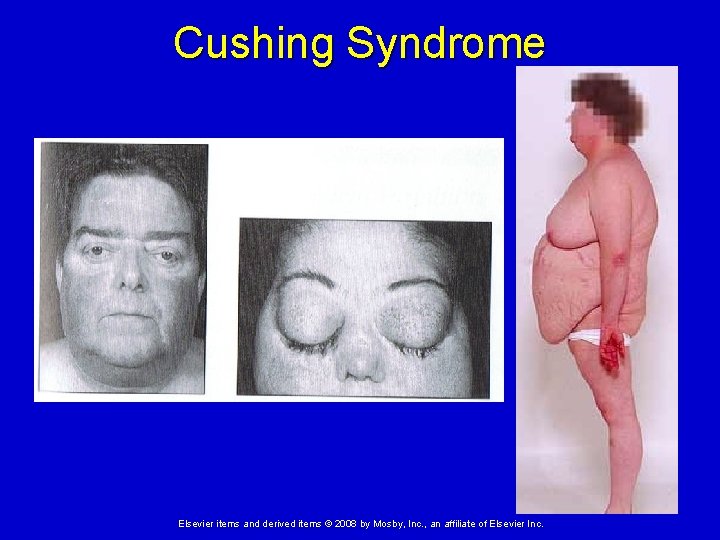
Cushing Syndrome Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
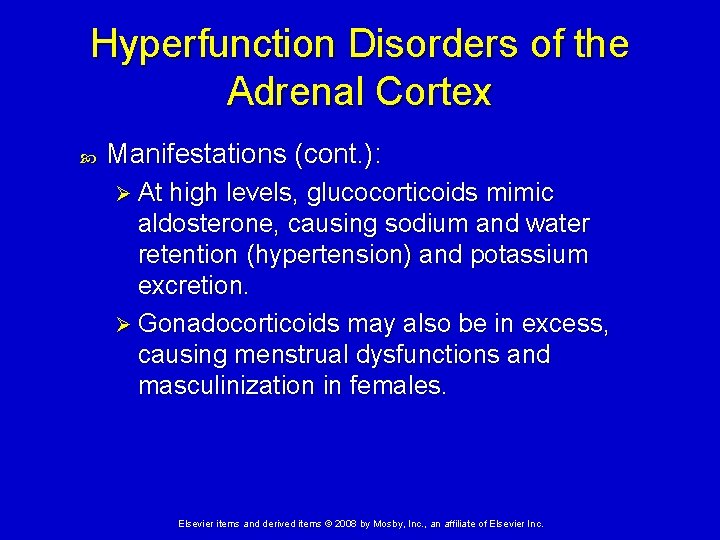
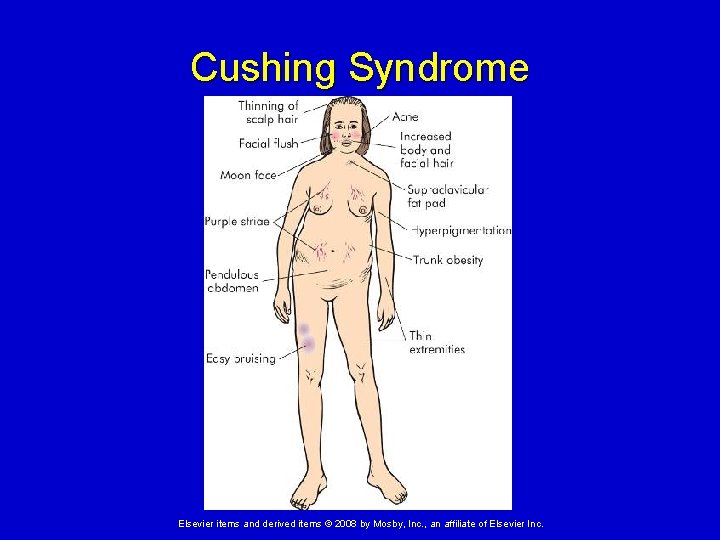
Hyperfunction Disorders of the Adrenal Cortex Manifestations (cont. ): Ø At high levels, glucocorticoids mimic aldosterone, causing sodium and water retention (hypertension) and potassium excretion. Ø Gonadocorticoids may also be in excess, causing menstrual dysfunctions and masculinization in females. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Cushing Syndrome Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
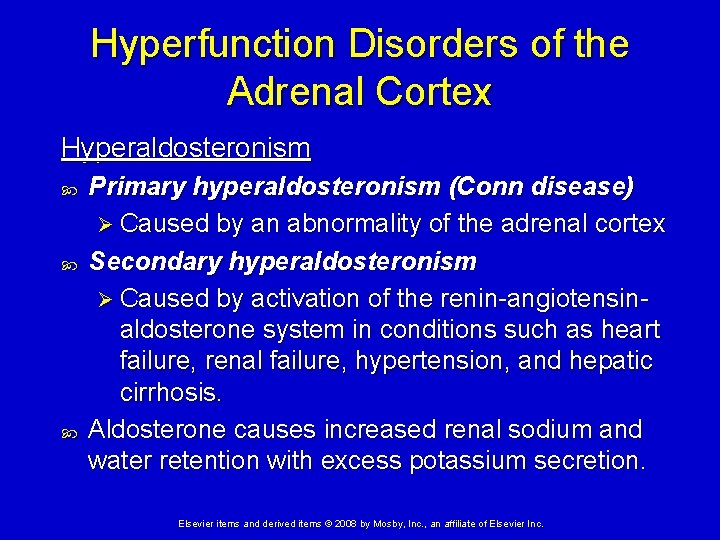
Hyperfunction Disorders of the Adrenal Cortex Hyperaldosteronism Primary hyperaldosteronism (Conn disease) Ø Caused by an abnormality of the adrenal cortex Secondary hyperaldosteronism Ø Caused by activation of the renin-angiotensinaldosterone system in conditions such as heart failure, renal failure, hypertension, and hepatic cirrhosis. Aldosterone causes increased renal sodium and water retention with excess potassium secretion. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
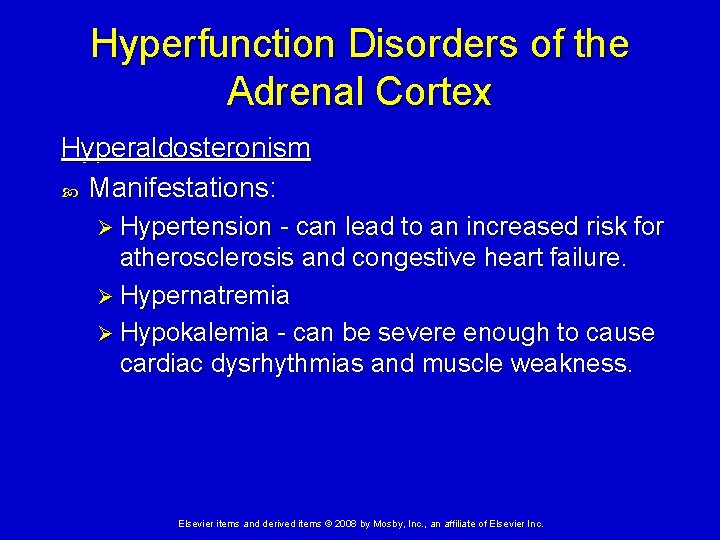
Hyperfunction Disorders of the Adrenal Cortex Hyperaldosteronism Manifestations: Ø Hypertension - can lead to an increased risk for atherosclerosis and congestive heart failure. Ø Hypernatremia Ø Hypokalemia - can be severe enough to cause cardiac dysrhythmias and muscle weakness. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
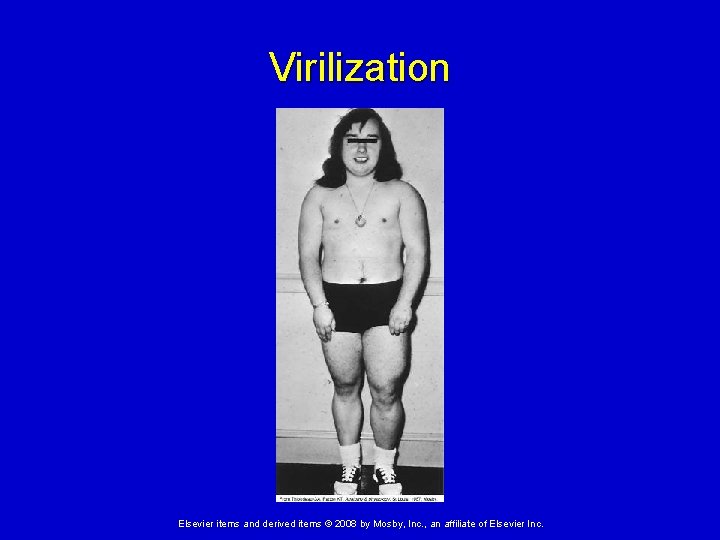
Hyperfunction Disorders of the Adrenal Cortex Hypersecretion of adrenal androgens and estrogens Usually due to an adrenal tumor. Feminization – can result in males. Virilization – development of male characteristics can result in females. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
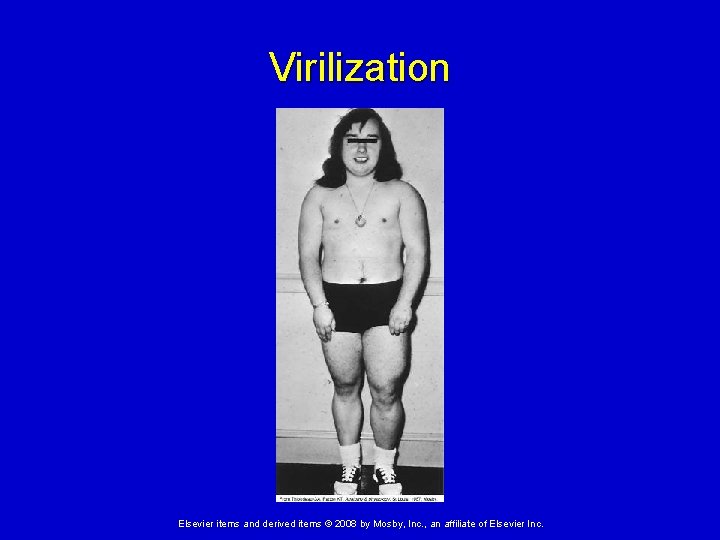
Virilization Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Hypofunction Disorders of the Adrenal Cortex Hypocortisolism - low levels of cortisol secretion. Due to either: Ø Inadequate stimulation of the adrenal glands by ACTH Ø Primary adrenal insufficiency - inability of the adrenals to produce and secrete the adrenocortical hormones. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Hypofunction Disorders of the Adrenal Cortex Hypocortisolism (cont. ) May be partial dysfunction so only synthesis of aldosterone or androgens is affected. May affect glucocorticoid or mineralocorticoid secretion or both. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Hypofunction Disorders of the Adrenal Cortex Primary adrenal insufficiency (Addison disease) Inadequate production of cortisol and aldosterone Caused by autoantibodies and cell-mediated immunity cause destruction of the adrenal cortex. Associated with other autoimmune diseases such as Hashimoto thyroiditis and pernicious anemia. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Hypofunction Disorders of the Adrenal Cortex Primary adrenal insufficiency (Addison disease) Manifestations: Ø Metabolic abnormalities (e. g. , hypoglycemia, hyponatremia, and hyperkalemia) Ø Hypovolemia and hypotension (can be lifethreatening) Ø Orthostatic dizziness, weakness and fatigue Ø Anorexia, nausea, abdominal pain Ø Changes in mental status like confusion and apathy due to hypoglycemia Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Hypofunction Disorders of the Adrenal Cortex Addisonian crisis – in response to an acute stressor, the patient experiences fever, nausea, vomiting, hyponatremia, hyperkalemia, hypotension, and dehydration, which could result in circulatory shock. In individuals with primary Addison disease, the lack of feedback on the pituitary results in increased compensatory secretion of ACTH which can cause hyperpigmentation of the skin. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Disorders of the Adrenal Medulla Adrenal medulla hyperfunction - usually caused by a: Pheochromocytoma – a catecholamineproducing tumor of the adrenal medulla. Most are benign, although 10% are malignant and may metastasize. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Disorders of the Adrenal Medulla Symptoms of catecholamine excess are related to their sympathetic nervous system effects: Ø Hypertension Ø Tachycardia, palpitations Ø Glucose intolerance Ø Excessive sweating Ø Constipation Ø Weight loss Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.
Disorders of the Adrenal Medulla With exposure to certain foods (containing tyrosine) or excessive physiologic stress (e. g. , surgery), episodes of extreme hypertension can occur with potential for cerebral and cardiovascular complications. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc.