Chapter 17 Cardiac Function Elsevier items and derived
- Slides: 66
Chapter 17 Cardiac Function Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 1
Cardiovascular Anatomy Primary function of the heart is to reduce the driving force that propels blood through the vessels of the circulatory system Cardiac dysfunction can lead to abnormal function or death of cells throughout the body Cardiovascular disease is the leading cause of mortality in the United States Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 2
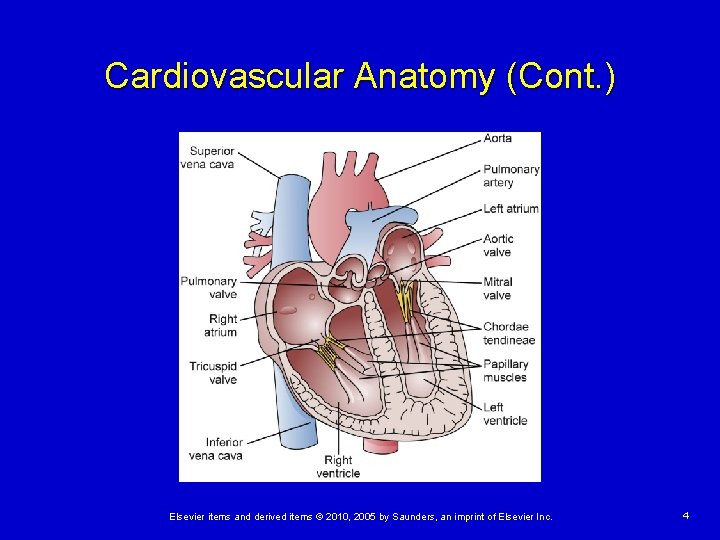
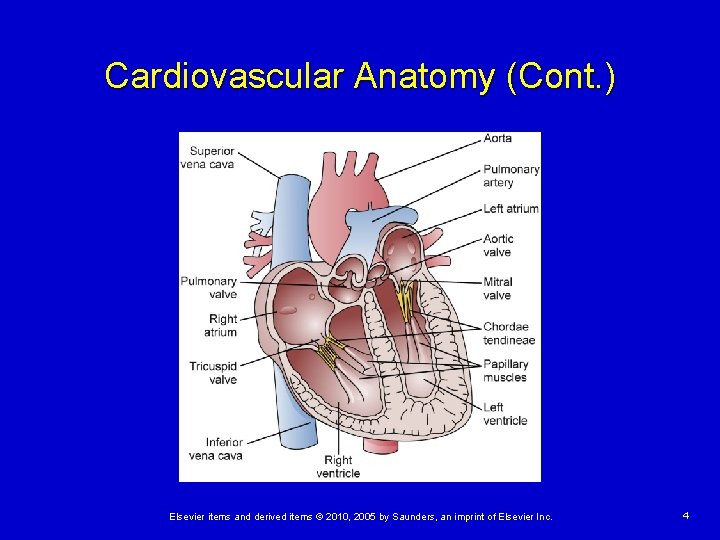
Cardiovascular Anatomy (Cont. ) Heart Located in the mediastinum Ø Ø Base Apex Cardiac valves control the direction of blood flow through the heart Ø Ø Mitral Tricuspid Pulmonic Aortic Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 3
Cardiovascular Anatomy (Cont. ) Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 4
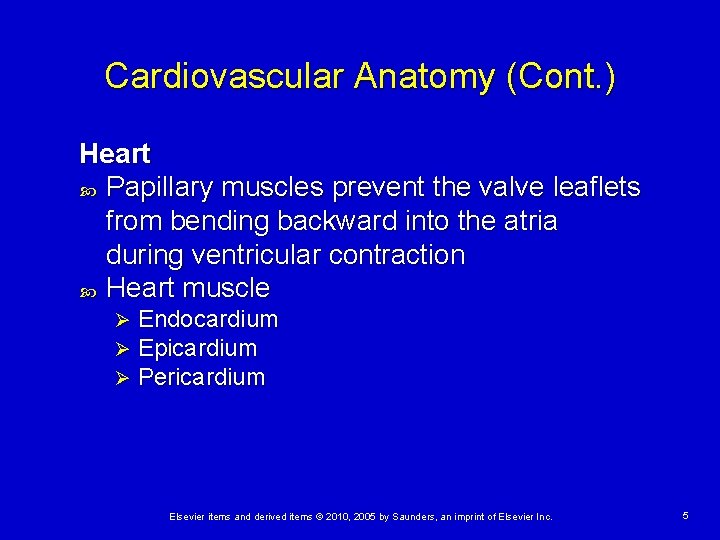
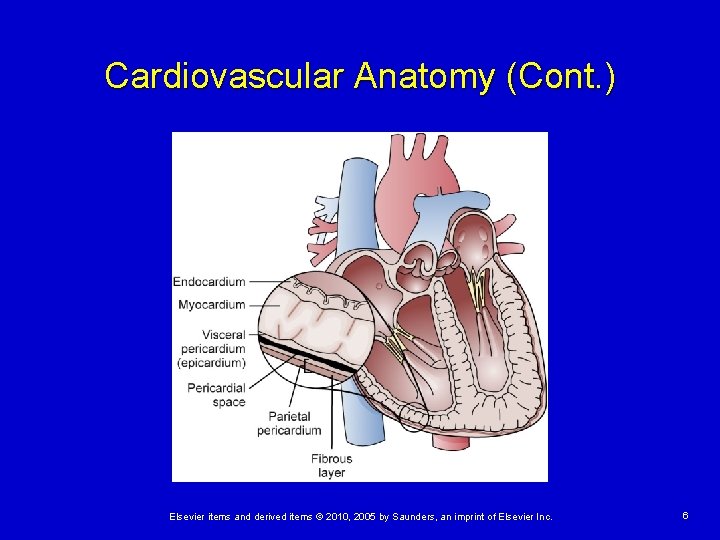
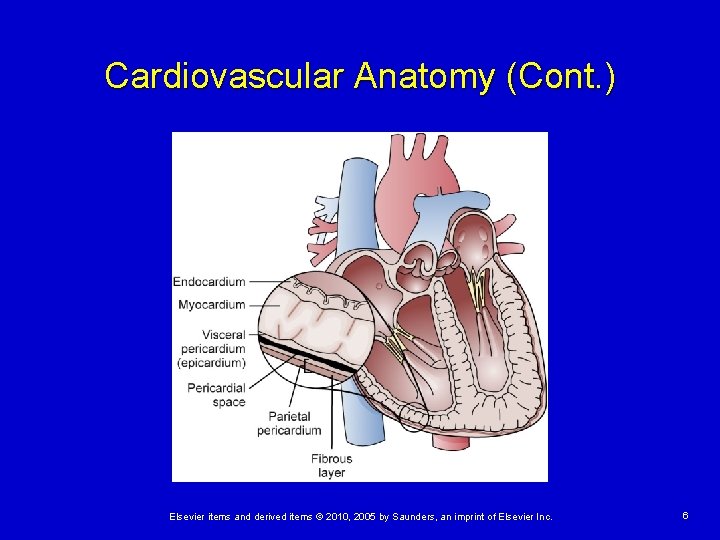
Cardiovascular Anatomy (Cont. ) Heart Papillary muscles prevent the valve leaflets from bending backward into the atria during ventricular contraction Heart muscle Ø Ø Ø Endocardium Epicardium Pericardium Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 5
Cardiovascular Anatomy (Cont. ) Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 6
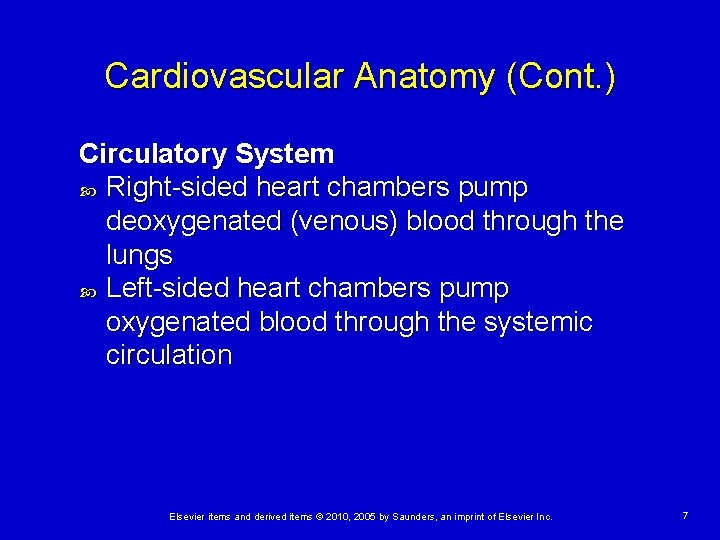
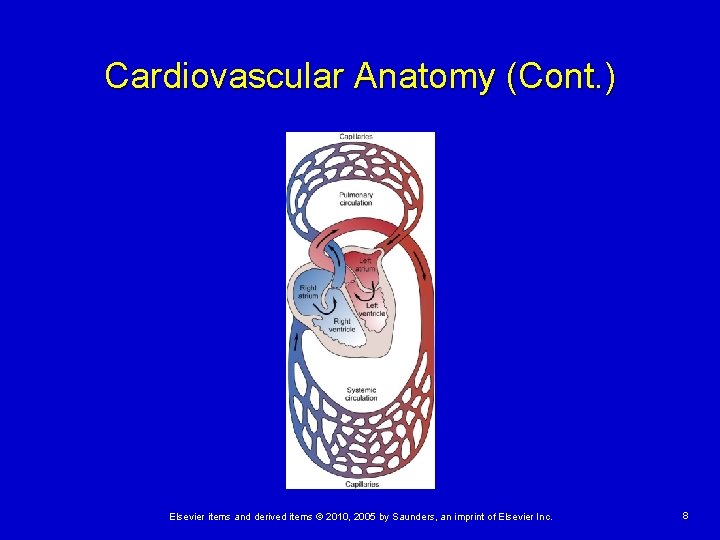
Cardiovascular Anatomy (Cont. ) Circulatory System Right-sided heart chambers pump deoxygenated (venous) blood through the lungs Left-sided heart chambers pump oxygenated blood through the systemic circulation Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 7
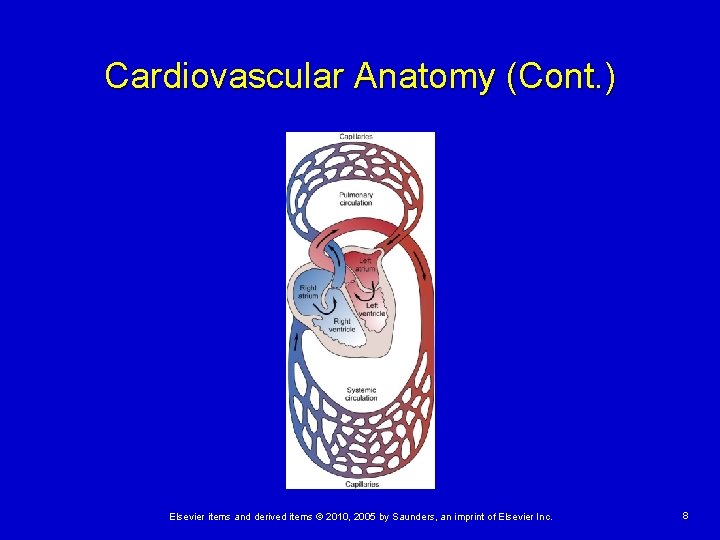
Cardiovascular Anatomy (Cont. ) Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 8
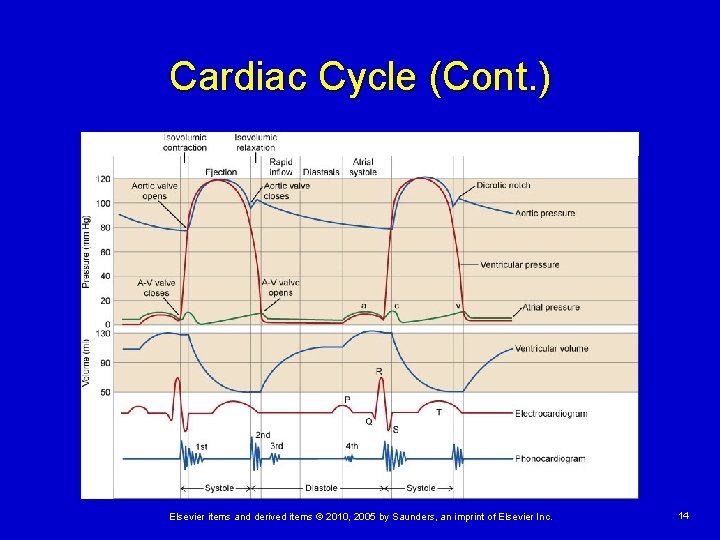
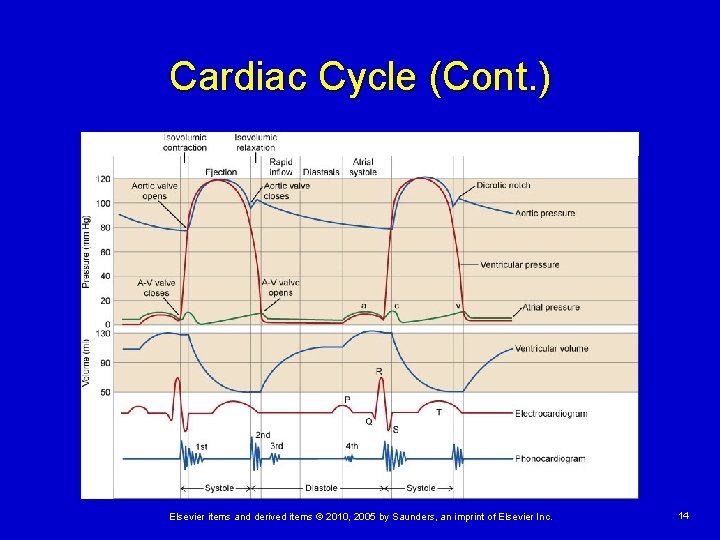
Cardiac Cycle Each heartbeat is composed of a period of ventricular contraction (systole) followed by a period of relaxation (diastole) Closure of the AV valves causes the first heart sound, S 1 Closure of the semilunar valves causes the second heart sound, S 2 Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 9
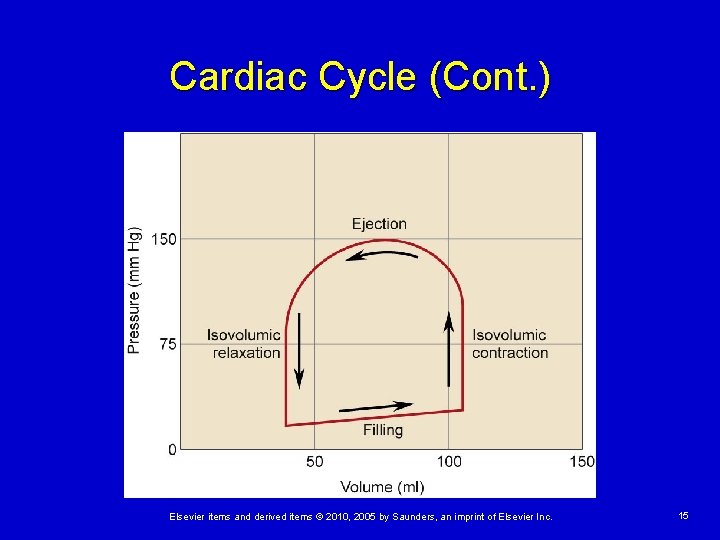
Cardiac Cycle (Cont. ) Isovolumic Contraction Following atrial systole the ventricles contract, causing intraventricular pressure to rise and the AV valves to close (S 1) Volume remains constant during this phase Rate of rise in pressure is an indication of contractility Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 10
Cardiac Cycle (Cont. ) Ventricular Ejection Contraction results in a rapid rise in ventricular pressure > aortic pressure, forcing the aortic valve to open with rapid ejection of blood from the ventricle Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 11
Cardiac Cycle (Cont. ) Stroke volume (SV) is the amount of blood ejected with each contraction of the ventricle (SV = EDV – ESV) End-diastolic volume is the volume of blood in the ventricle prior to ejection End-systolic volume is the amount of blood that remains in the ventricle after ejection Ejection fraction = SV/EDV Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 12
Cardiac Cycle (Cont. ) Isovolumic Relaxation Begins with semilunar valve closure in response to falling ventricular pressures and ends when the AV valves open to allow ventricular filling Ventricular blood volume remains constant during this phase Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 13
Cardiac Cycle (Cont. ) Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 14
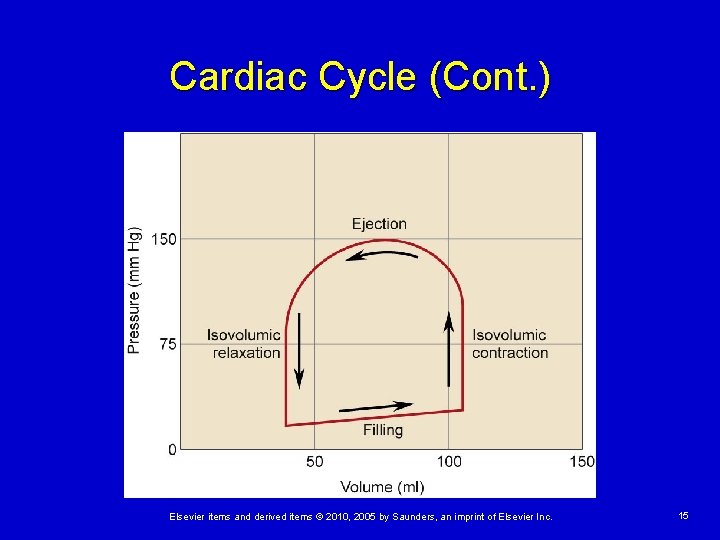
Cardiac Cycle (Cont. ) Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 15
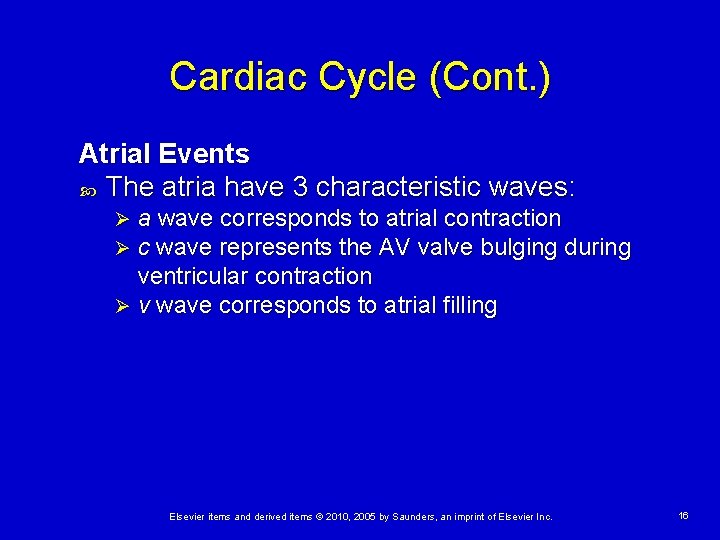
Cardiac Cycle (Cont. ) Atrial Events The atria have 3 characteristic waves: a wave corresponds to atrial contraction c wave represents the AV valve bulging during ventricular contraction Ø v wave corresponds to atrial filling Ø Ø Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 16
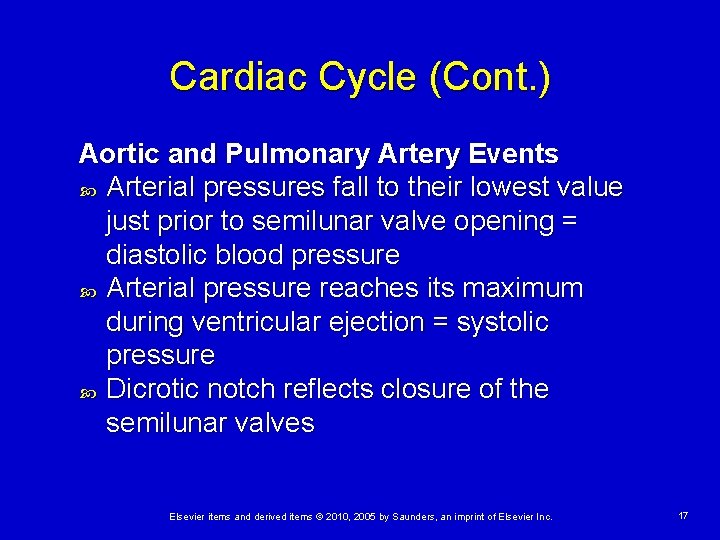
Cardiac Cycle (Cont. ) Aortic and Pulmonary Artery Events Arterial pressures fall to their lowest value just prior to semilunar valve opening = diastolic blood pressure Arterial pressure reaches its maximum during ventricular ejection = systolic pressure Dicrotic notch reflects closure of the semilunar valves Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 17
Coronary Circulation Coronary arteries supply blood to the heart muscle Right and left coronary arteries are located in the sinuses of Valsalva Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 18
Coronary Circulation (Cont. ) Anatomy of the Coronary Vessels Left main coronary artery divides into left anterior descending and circumflex branches Left anterior descending supplies the septal, anterior, and apical areas Ø Circumflex supplies the lateral and posterior left ventricles Ø Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 19
Coronary Circulation (Cont. ) Regulation of Coronary Blood Flow Driving pressure and vascular resistance to flow Ohm’s law—an increase in driving pressure increases flow, whereas an increase in resistance reduces flow Coronary driving pressure equals aortic blood pressure (ABP) minus right atrial pressure (RAP) (P) = ABP – RAP Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 20
Coronary Circulation (Cont. ) Coronary Vascular Resistance Two major determinants: Coronary artery diameter adjusted by autoregulation, ATP-sensitive potassium channels, nitric oxide levels, and autonomic nervous system Ø Varying degree of external compression due to myocardial contraction/relaxation (most coronary blood flow occurs during diastole) Ø Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 21
Cardiac Myocytes Two general types Working cells with mechanical pumping functions Ø Electrical cells that transmit electrical impulses Ø Both produce and transmit action potentials Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 22
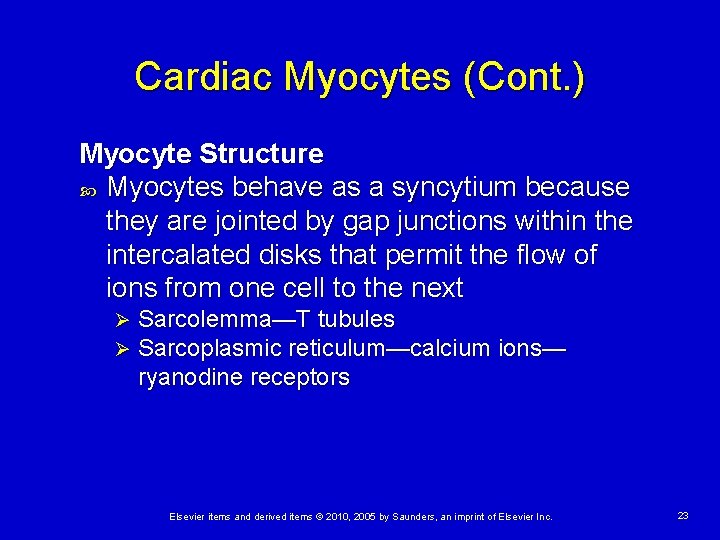
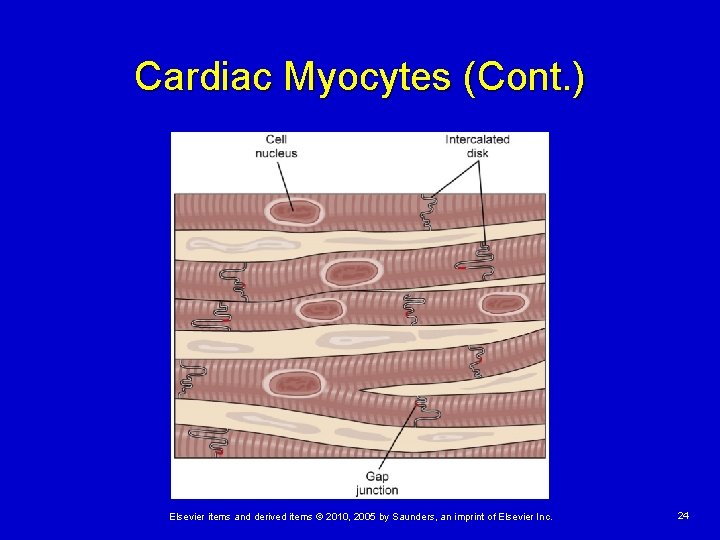
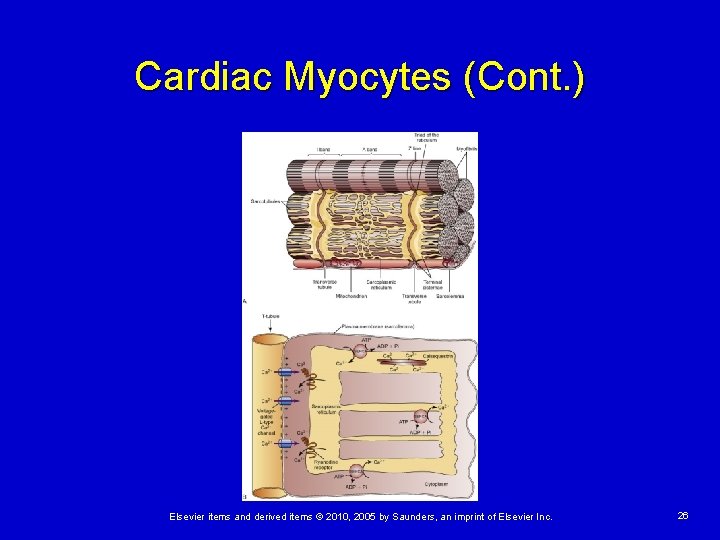
Cardiac Myocytes (Cont. ) Myocyte Structure Myocytes behave as a syncytium because they are jointed by gap junctions within the intercalated disks that permit the flow of ions from one cell to the next Ø Ø Sarcolemma—T tubules Sarcoplasmic reticulum—calcium ions— ryanodine receptors Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 23
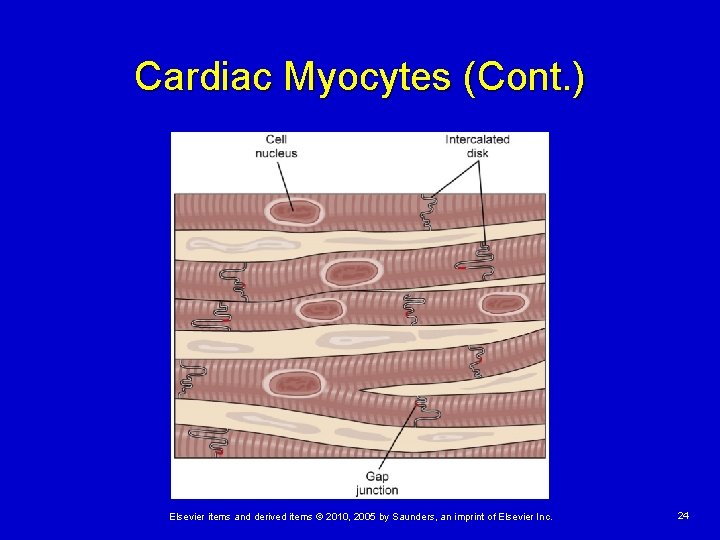
Cardiac Myocytes (Cont. ) Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 24
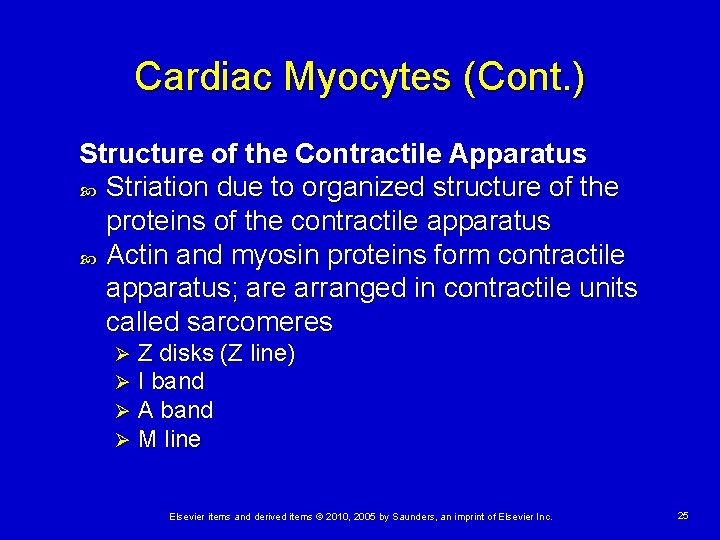
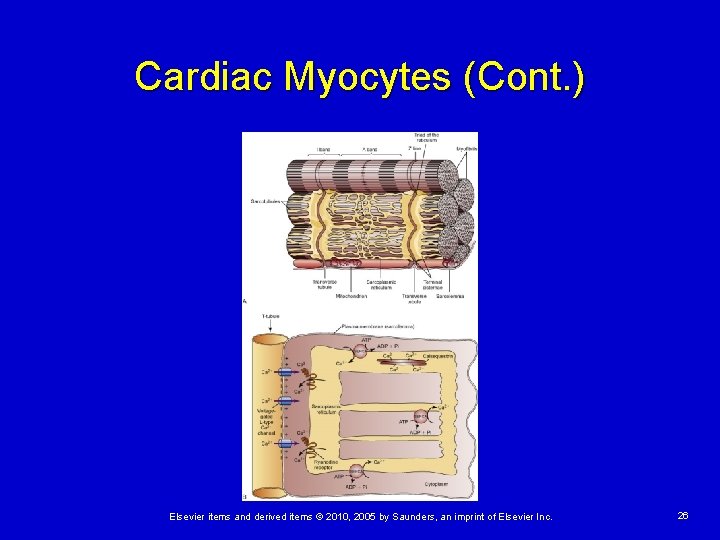
Cardiac Myocytes (Cont. ) Structure of the Contractile Apparatus Striation due to organized structure of the proteins of the contractile apparatus Actin and myosin proteins form contractile apparatus; are arranged in contractile units called sarcomeres Ø Ø Z disks (Z line) I band A band M line Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 25
Cardiac Myocytes (Cont. ) Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 26
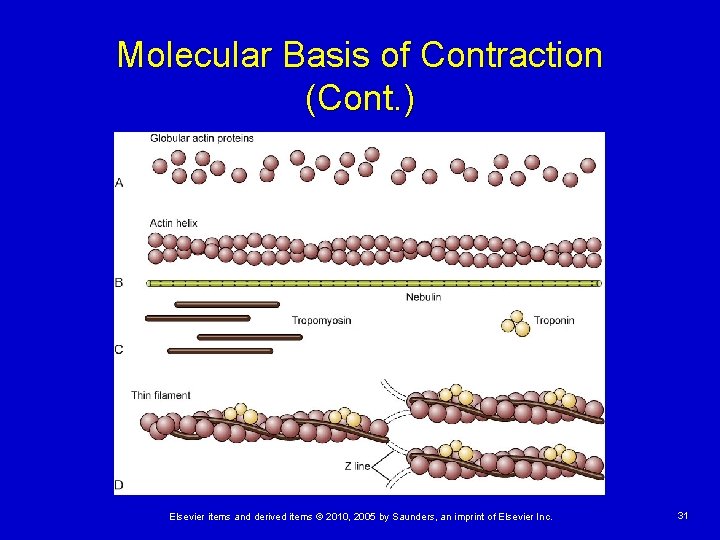
Cardiac Myocytes (Cont. ) Characteristics of Contractile Filaments Thick filaments Ø Myosin • Enzymatic activity and splits ATP • Titin Thin filaments Ø Actin • Tropomyosin • Troponin Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 27
Molecular Basis of Contraction All myocytes of the chamber must shorten simultaneously to produce a forceful contraction Specialized cells of the conduction system coordinate myocardial contraction Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 28
Molecular Basis of Contraction (Cont. ) Overview of Contraction Excitation-contraction coupling: Depolarization causes ion channels of the plasma membrane and T tubules to open allowing sodium and calcium entry and release of calcium from the SR. Presence of free calcium in the sarcoplasm results in contraction. Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 29
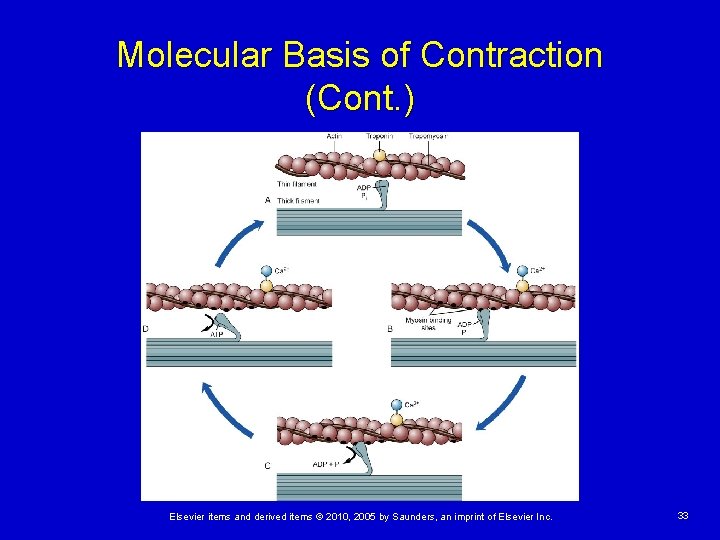
Molecular Basis of Contraction (Cont. ) Sliding Filament/Cross-Bridge Theory of Muscle Contraction of cardiac muscle by shortening of individual sarcomeres due to increased overlap of actin and myosin filaments Myosin heads bind to specific sites on actin and pull the thin filaments toward the center of the sarcomere Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 30
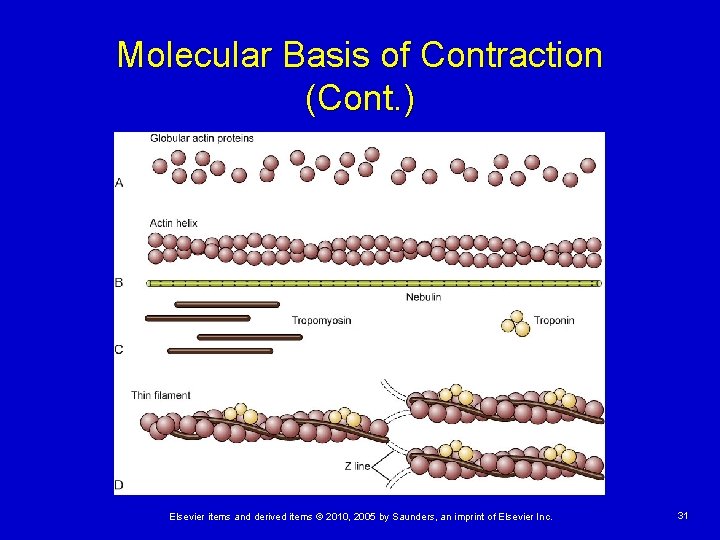
Molecular Basis of Contraction (Cont. ) Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 31
Molecular Basis of Contraction (Cont. ) Sliding Filament/Cross-Bridge Theory of Muscle Contraction ATP hydrolysis provides the energy for crossbridging and affects affinity of myosin for actin Myosin has high affinity for actin when ADP and Pi are bound; low affinity when ATP is bound Myosin cycles between high- and low-affinity states, making and breaking cross-bridges with the actin filament Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 32
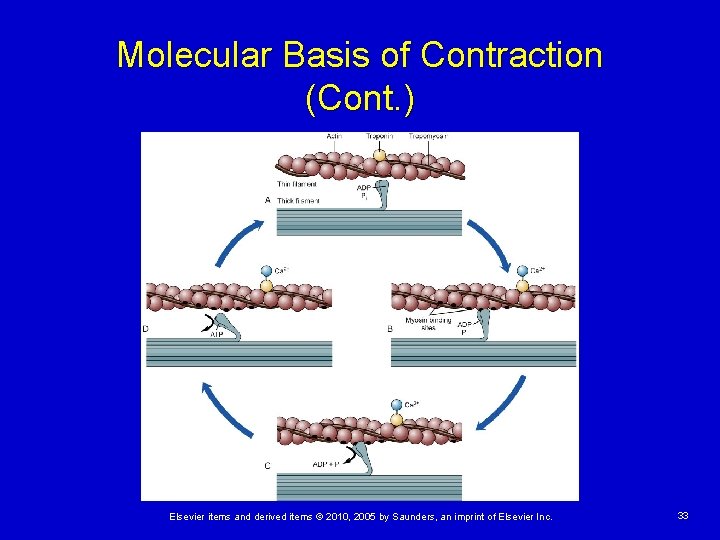
Molecular Basis of Contraction (Cont. ) Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 33
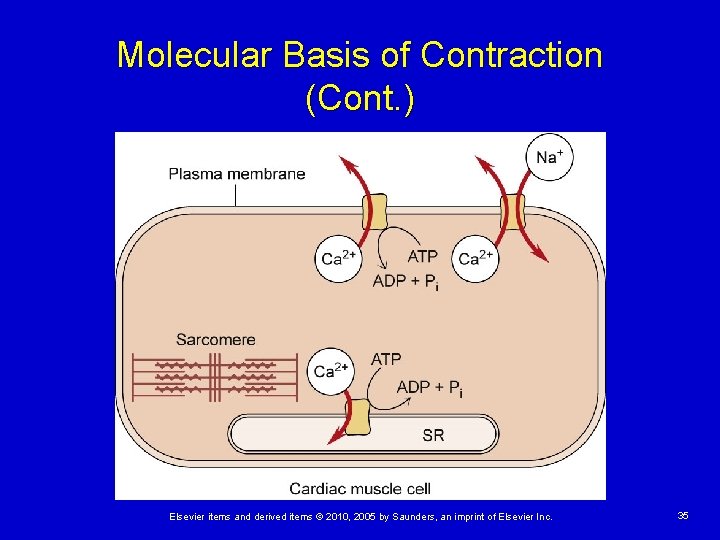
Molecular Basis of Contraction (Cont. ) Role of Calcium in Muscle Contraction is dependent on adequate calcium ions in the cytoplasm Muscle relaxation (lusitropy) is due to removal of calcium from the cytoplasm This is an energy-requiring process Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 34
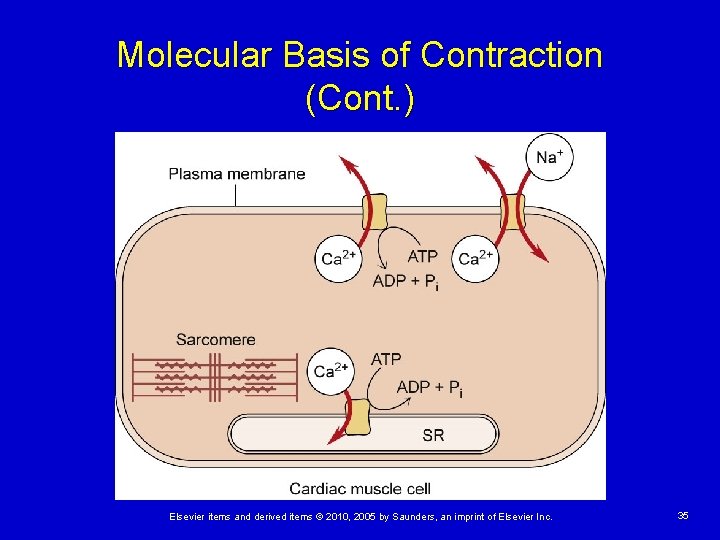
Molecular Basis of Contraction (Cont. ) Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 35
Molecular Basis of Contraction (Cont. ) Energy of Muscle Relaxation Significant energy required to pump calcium ions out of the cytoplasm Membrane pumps in the sarcolemma and SR actively move calcium out of the sarcoplasm against a concentration gradient Sarcolemma has 2 different calcium pumps Ø Ø One that requires ATP One that uses the potential energy of the sodium gradient to remove calcium SR calcium pumps (SERCAs) require ATP Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 36
Cardiac Energy Metabolism Uses energy from ATP hydrolysis to drive energy-requiring functions Accomplished by glycolytic and oxidative reactions Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 37
Cardiac Energy Metabolism (Cont. ) Oxygen Utilization Creatine phosphate (CP)—storage form of ATP CP an immediately available source of energy Under conditions of low ATP availability, CP is converted to ATP by the enzyme CK Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 38
Cardiac Energy Metabolism (Cont. ) Substrate Utilization Primary energy substrates are fatty acids and glucose Able to use lactate and ketones when they accumulate in the circulation Able to use a variety of substrates to produce ATP under varying metabolic conditions Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 39
Cardiac Electrophysiology Heart is rhythmically activated by action potentials Action potentials are generated and transmitted by a specialized conduction system Many cardiac disorders result from disturbances in electrical function that produce abnormal conduction pathways, dysrhythmias, and conduction blocks Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 40
Cardiac Electrophysiology (Cont. ) Cardiac Resting Potential Resting cardiac cells are negatively charged on the inside Difference in potassium ion concentration across the cell membrane determines resting membrane potential Increase in extracellular potassium hypopolarizes the cell while a decrease hyperpolarizes the cell Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 41
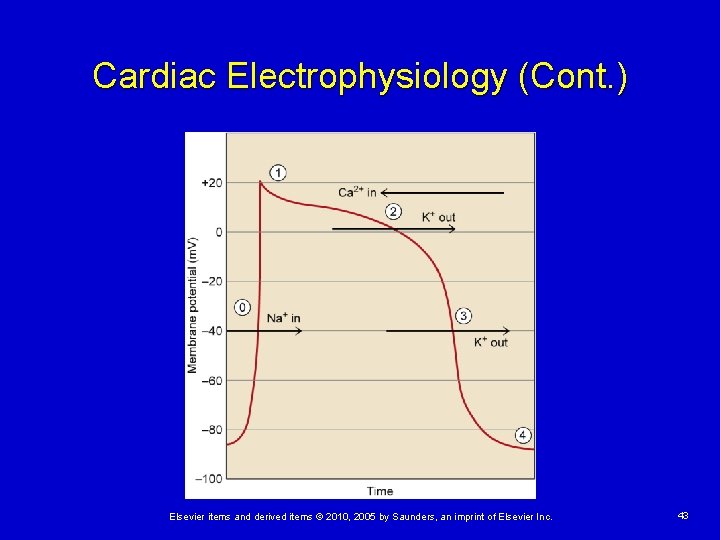
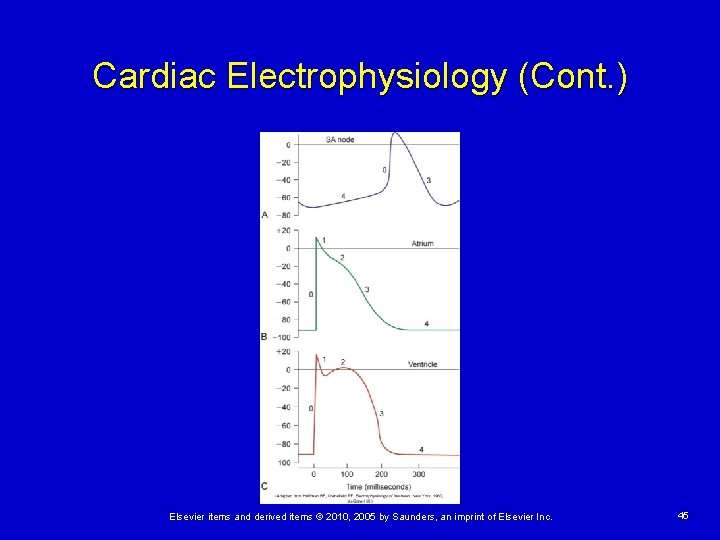
Cardiac Electrophysiology (Cont. ) Cardiac Action Potential Depolarization of cardiac cells to a threshold point results in activation of voltage-sensitive ion channels in the membrane Action potential in atrial and ventricular cells has 5 characteristic phases Atrial action potentials are shorter due to reduced phase 2 Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 42
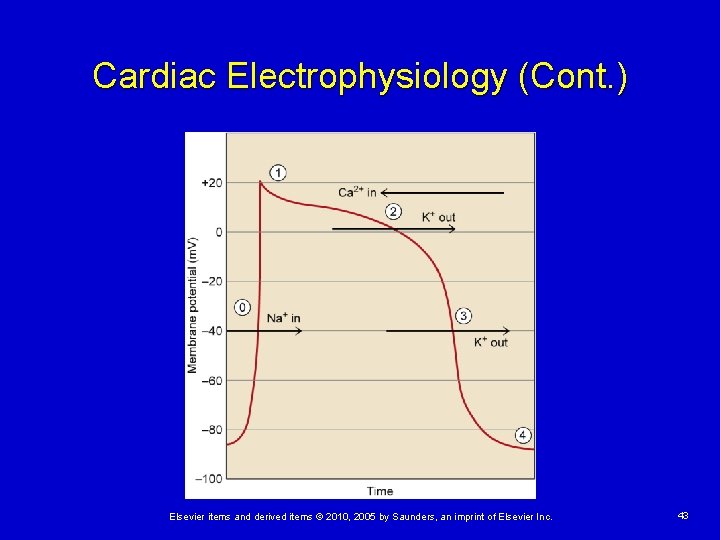
Cardiac Electrophysiology (Cont. ) Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 43
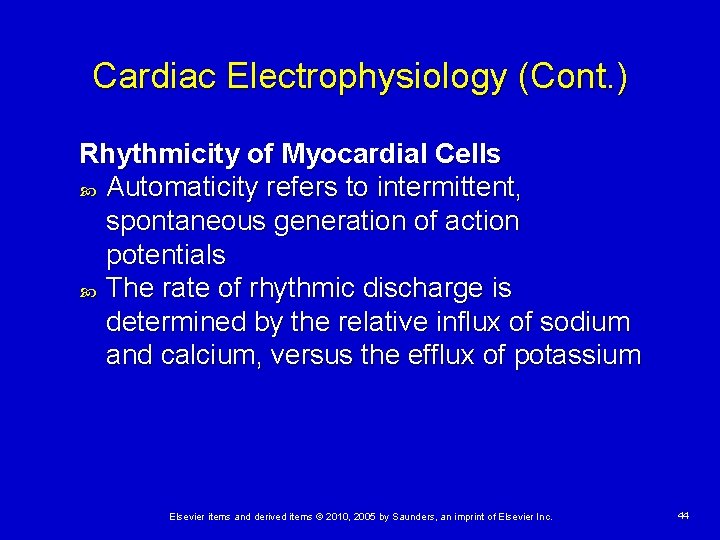
Cardiac Electrophysiology (Cont. ) Rhythmicity of Myocardial Cells Automaticity refers to intermittent, spontaneous generation of action potentials The rate of rhythmic discharge is determined by the relative influx of sodium and calcium, versus the efflux of potassium Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 44
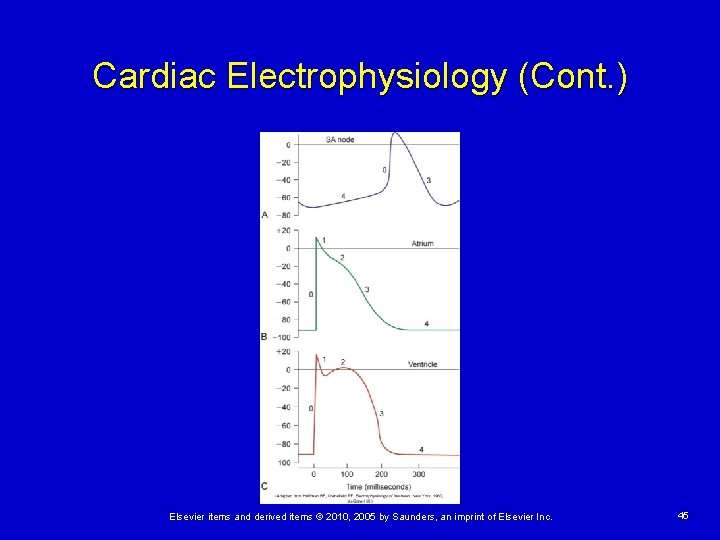
Cardiac Electrophysiology (Cont. ) Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 45
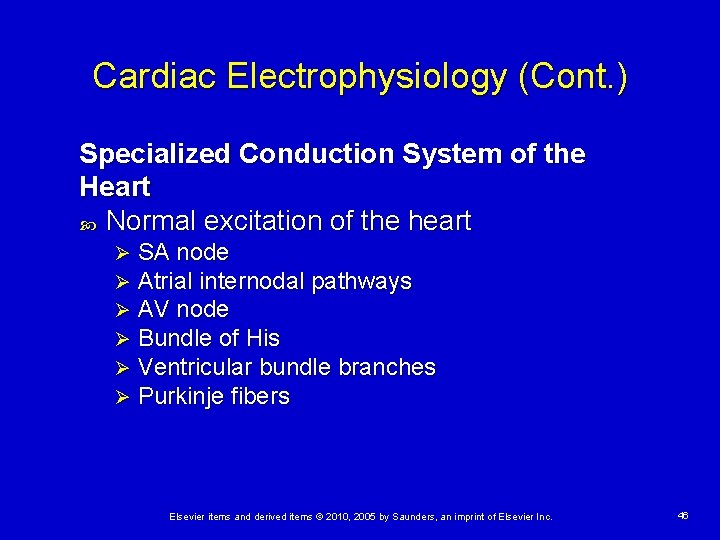
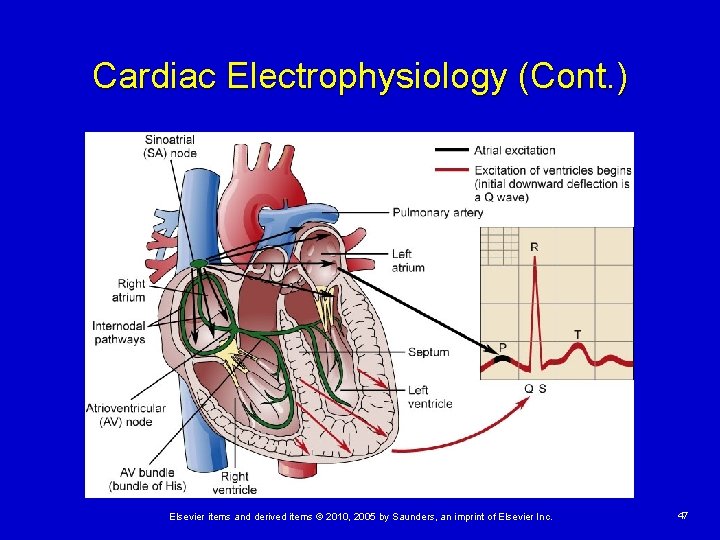
Cardiac Electrophysiology (Cont. ) Specialized Conduction System of the Heart Normal excitation of the heart Ø Ø Ø SA node Atrial internodal pathways AV node Bundle of His Ventricular bundle branches Purkinje fibers Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 46
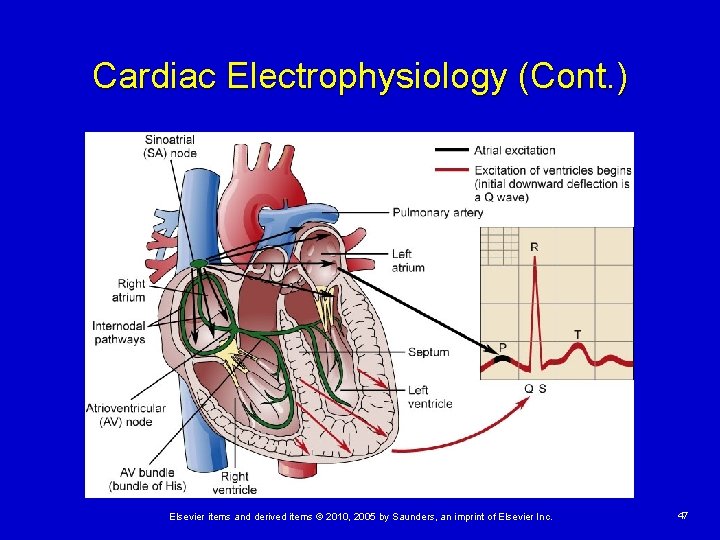
Cardiac Electrophysiology (Cont. ) Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 47
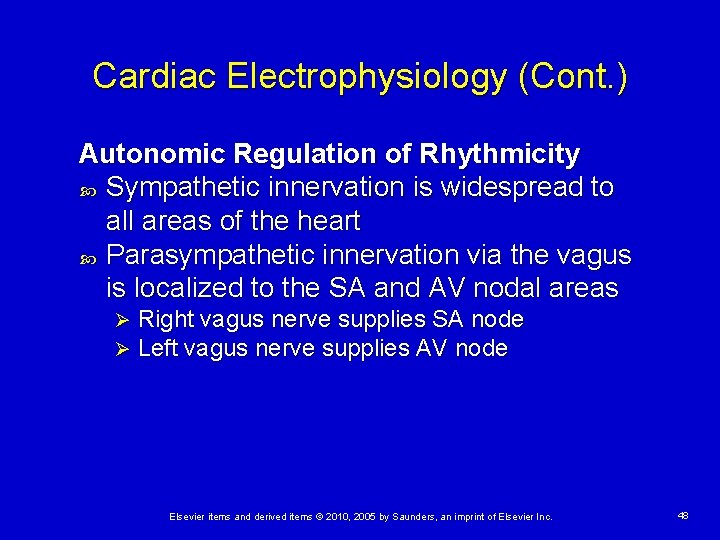
Cardiac Electrophysiology (Cont. ) Autonomic Regulation of Rhythmicity Sympathetic innervation is widespread to all areas of the heart Parasympathetic innervation via the vagus is localized to the SA and AV nodal areas Ø Ø Right vagus nerve supplies SA node Left vagus nerve supplies AV node Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 48
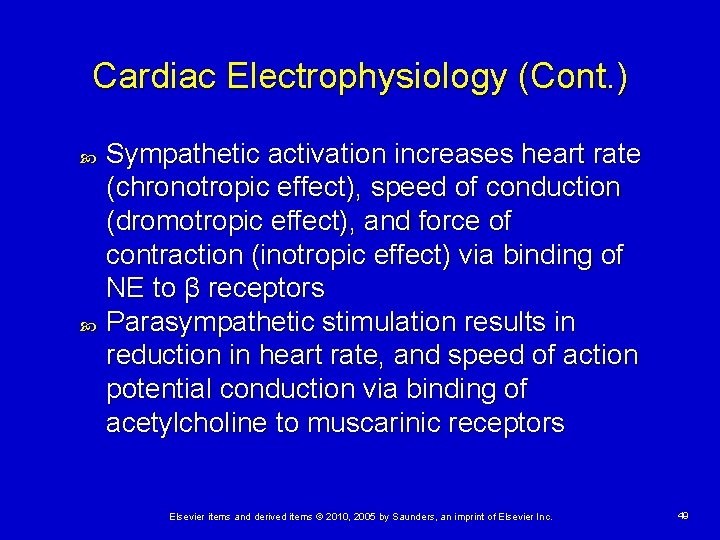
Cardiac Electrophysiology (Cont. ) Sympathetic activation increases heart rate (chronotropic effect), speed of conduction (dromotropic effect), and force of contraction (inotropic effect) via binding of NE to β receptors Parasympathetic stimulation results in reduction in heart rate, and speed of action potential conduction via binding of acetylcholine to muscarinic receptors Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 49
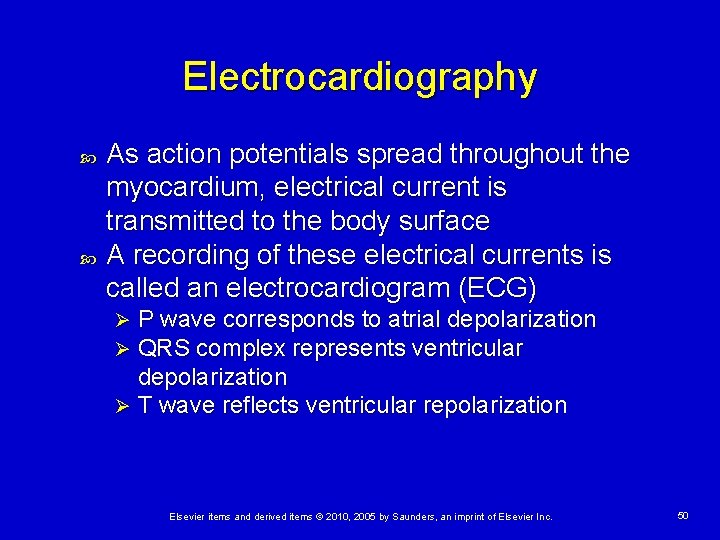
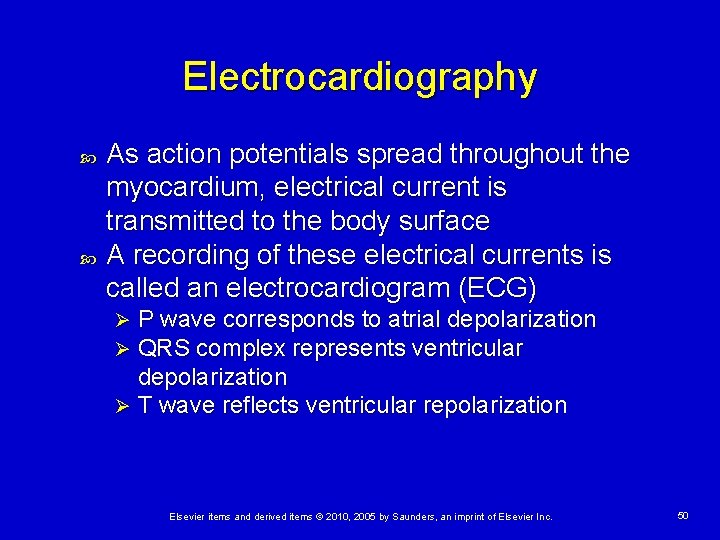
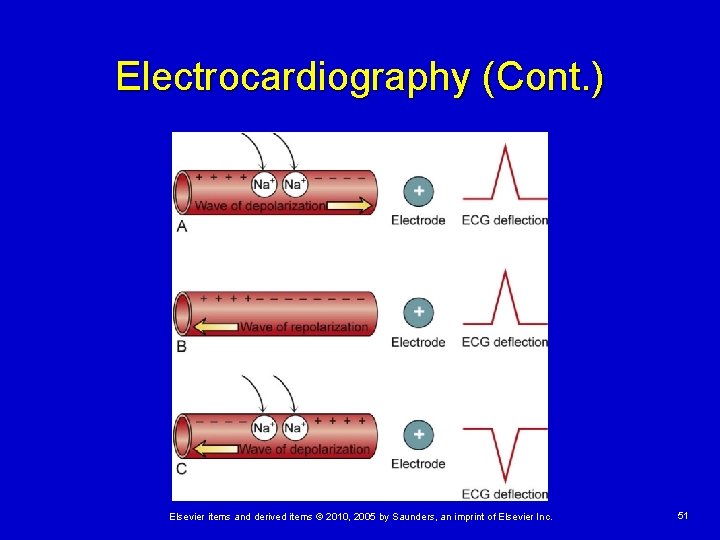
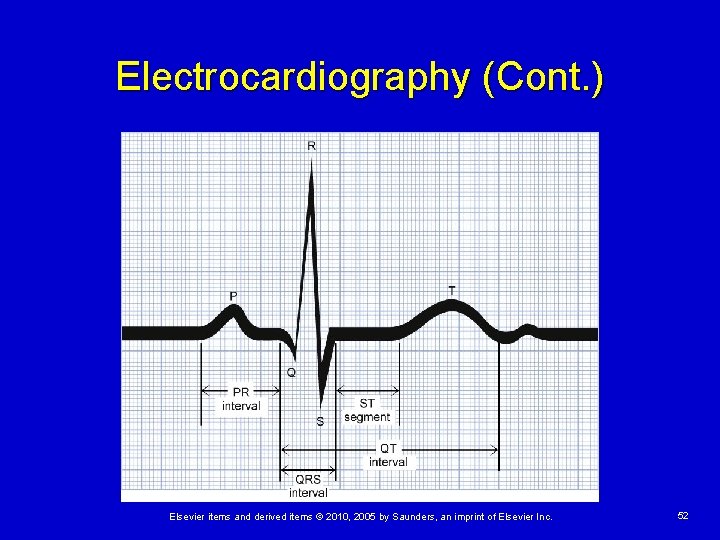
Electrocardiography As action potentials spread throughout the myocardium, electrical current is transmitted to the body surface A recording of these electrical currents is called an electrocardiogram (ECG) P wave corresponds to atrial depolarization QRS complex represents ventricular depolarization Ø T wave reflects ventricular repolarization Ø Ø Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 50
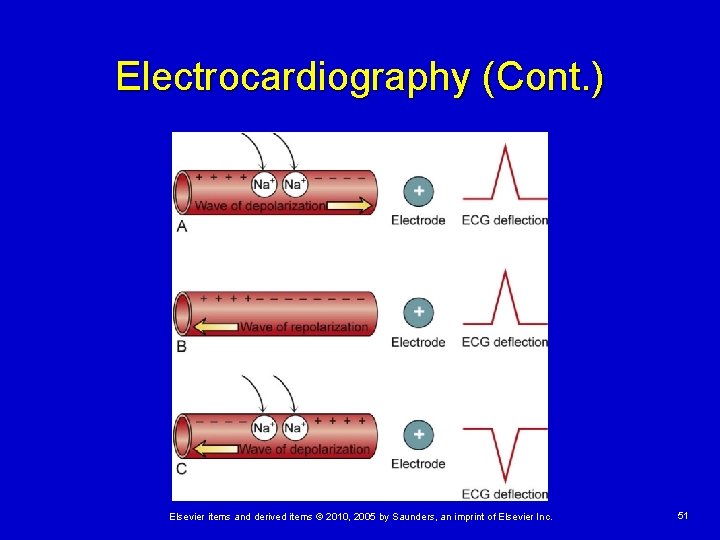
Electrocardiography (Cont. ) Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 51
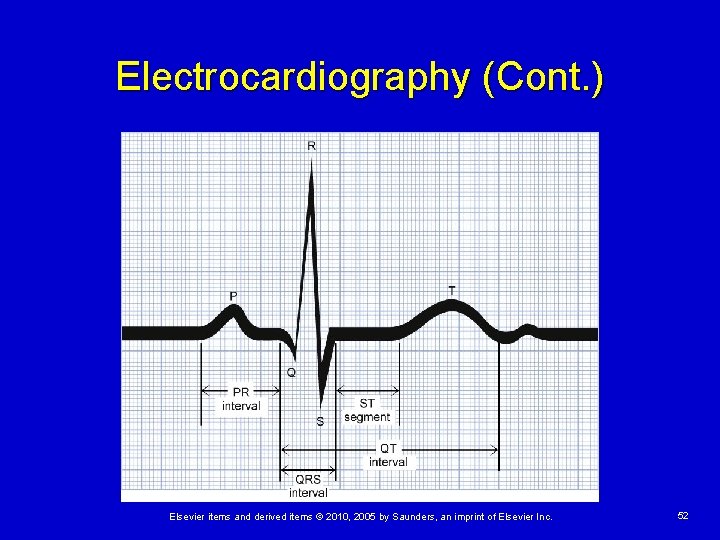
Electrocardiography (Cont. ) Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 52
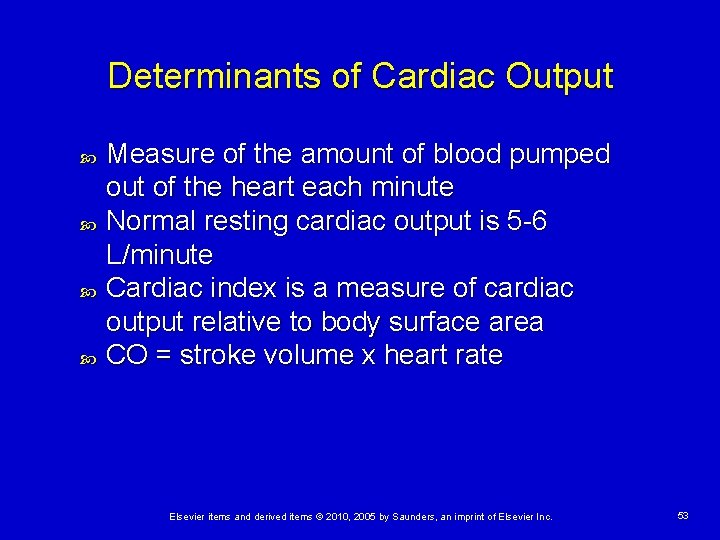
Determinants of Cardiac Output Measure of the amount of blood pumped out of the heart each minute Normal resting cardiac output is 5 -6 L/minute Cardiac index is a measure of cardiac output relative to body surface area CO = stroke volume x heart rate Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 53
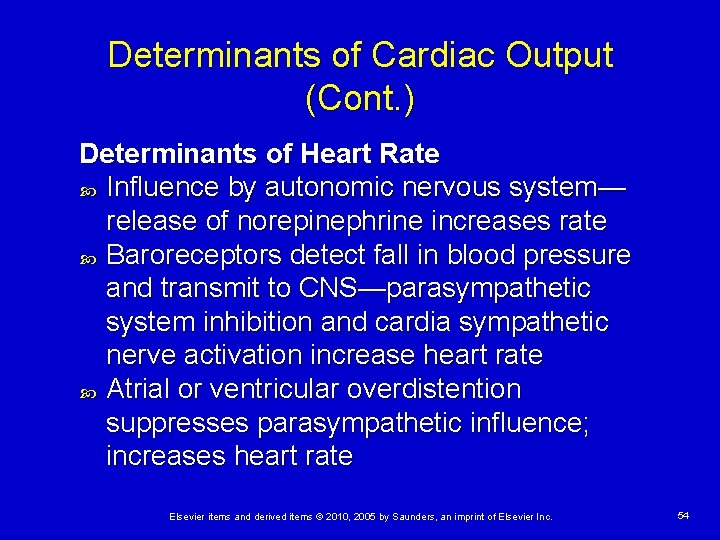
Determinants of Cardiac Output (Cont. ) Determinants of Heart Rate Influence by autonomic nervous system— release of norepinephrine increases rate Baroreceptors detect fall in blood pressure and transmit to CNS—parasympathetic system inhibition and cardia sympathetic nerve activation increase heart rate Atrial or ventricular overdistention suppresses parasympathetic influence; increases heart rate Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 54
Determinants of Cardiac Output (Cont. ) Determinants of Stroke Volume The volume of blood in the heart (preload) The contractile capabilities (contractility) Impedance opposing ejection of blood from the ventricle (afterload) Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 55
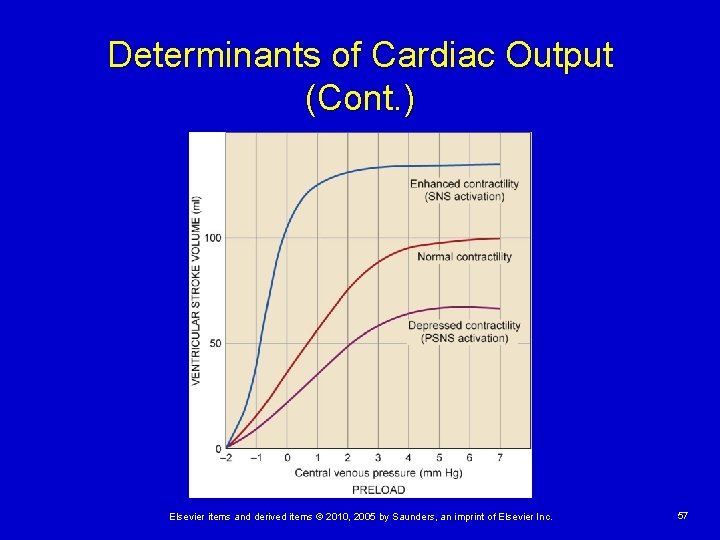
Determinants of Cardiac Output (Cont. ) Volume of Blood in the Heart (Preload) Frank-Starling law: increased preload stretches the sarcomere, resulting in more forceful contraction There are limits to the improvement in SV with increased diastolic filling Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 56
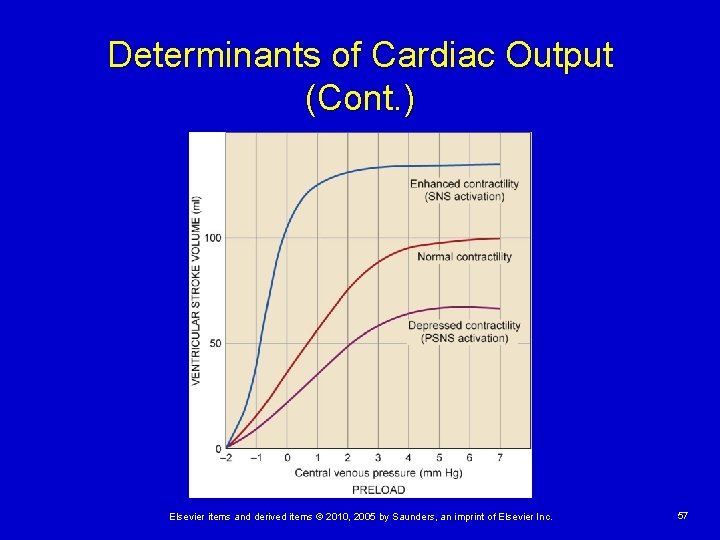
Determinants of Cardiac Output (Cont. ) Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 57
Determinants of Cardiac Output (Cont. ) Contractile Capabilities of the Heart (Contractility) The amount of contractile proteins in the muscle cells Availability of ATP Availability of free calcium ions in the cytoplasm Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 58
Determinants of Cardiac Output (Cont. ) Impedance to Ejection from the Ventricle (Afterload) Aortic valve narrowing can significantly increase afterload Increase in afterload increases pressure work and requires greater tension development within the walls of the chamber (wall stress) Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 59
Determinants of Cardiac Output (Cont. ) Cardiac Workload Oxygen requirements of the heart are determined by amount of energy (ATP) exerted to perform its pumping function Increases in the 4 determinants of CO are the major determinants of energy needs High afterload is most detrimental because it increases cardiac workload without increasing CO Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 60
Endocrine Function of the Heart Secretion of Natriuretic Peptides Atrial natriuretic peptide synthesized by myocytes and released in response to atrial stretch B-type natriuretic peptide produced and released by ventricles in response to chronic overdistention ANP and BNP cause enhanced excretion of sodium and water by the kidneys Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 61
Tests of Cardiac Function Electrocardiography Provides graphic illustration of the electrical currents generated by cardiac cells Ø Ø Ø Standard bipolar limb leads I, III Unipolar augmented leads a. VR, a. VL, a. VF 12 -lead ECGs Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 62
Tests of Cardiac Function (Cont. ) Magnetic Resonance Imaging and Computed Tomography Useful for imaging cardiac structures May identify: Ø Ø Ø Myocardial thickening Pericardial sac disease Valvular structures Congenital malformations Coronary plaque burden Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 63
Tests of Cardiac Function (Cont. ) Echocardiography Uses reflected sound waves to provide an image of cardiac structure and motion within the chest Useful in diagnosis of heart enlargement, valvular disorders, collections of fluid in the pericardial space, cardiac tumors, and abnormalities in left ventricular motion Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 64
Tests of Cardiac Function (Cont. ) Nuclear Cardiography Radioactive substances injected into the bloodstream are used to trace the patterns of blood flow in the heart Assesses the adequacy of blood flow to cardiac tissues Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 65
Tests of Cardiac Function (Cont. ) Cardiac Catheterization/Coronary Angiography A catheter is passed from the femoral or brachial artery into the aorta Used to directly measure pressures within cardiac chambers; visualize chamber size, shape, and movement; sample for blood oxygen content in various heart regions; measure CO and EF; and visualize and manage coronary artery obstructions Elsevier items and derived items © 2010, 2005 by Saunders, an imprint of Elsevier Inc. 66