2007 Guidelines for the management of arterial hypertension



































- Slides: 58
2007 Guidelines for the management of arterial hypertension Диагностические критерии артериальной гипертензии
2007 Guidelines for the management of arterial hypertension The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC)






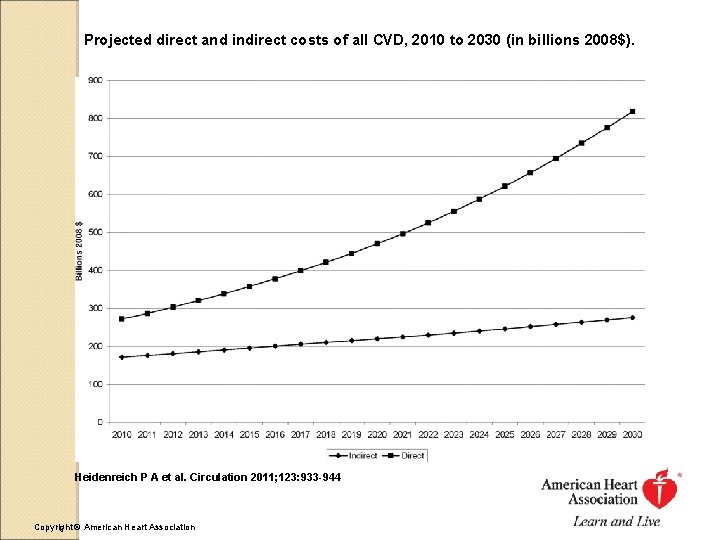
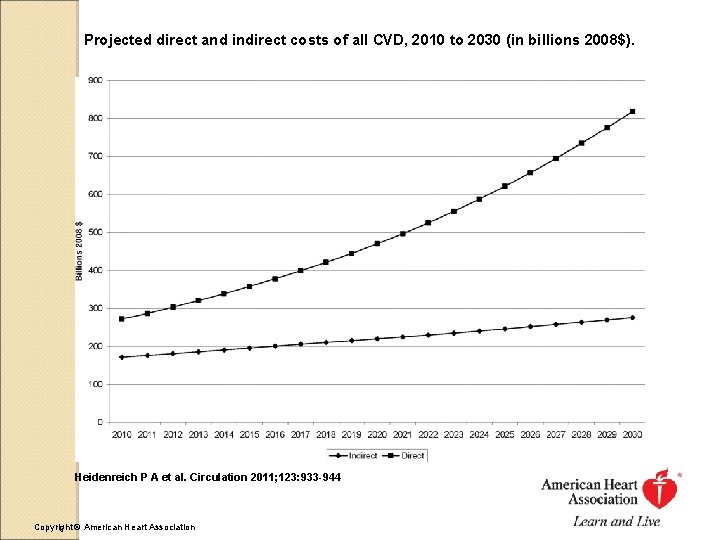
Projected direct and indirect costs of all CVD, 2010 to 2030 (in billions 2008$). Heidenreich P A et al. Circulation 2011; 123: 933 -944 Copyright © American Heart Association


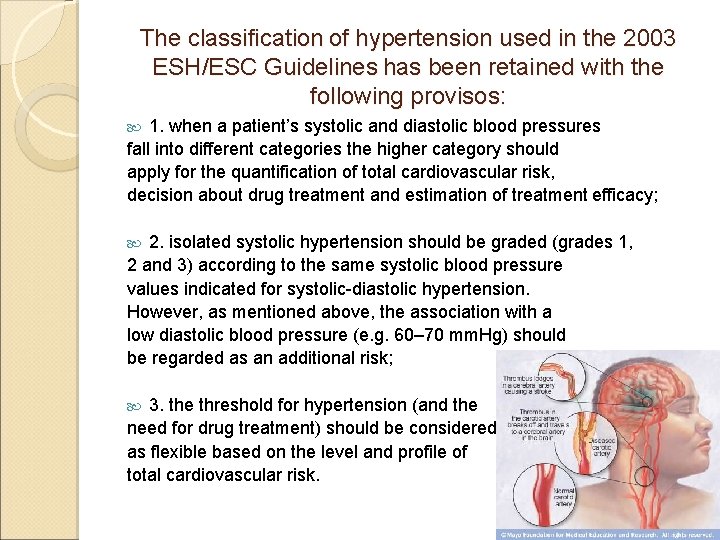
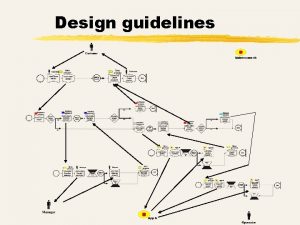
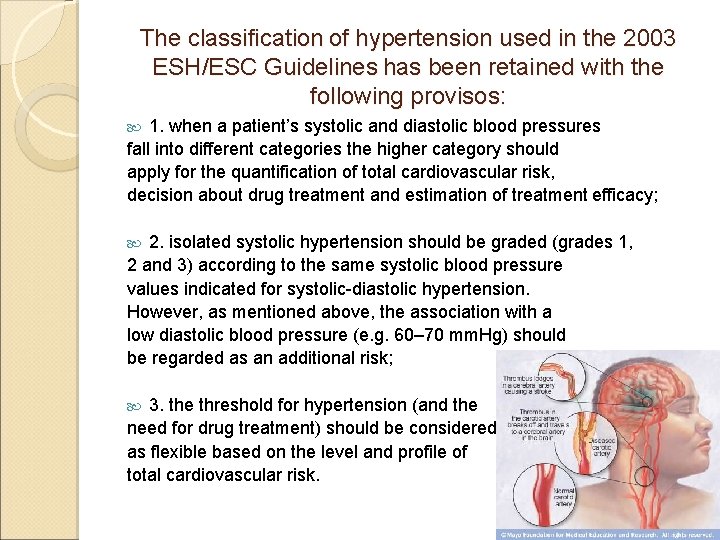
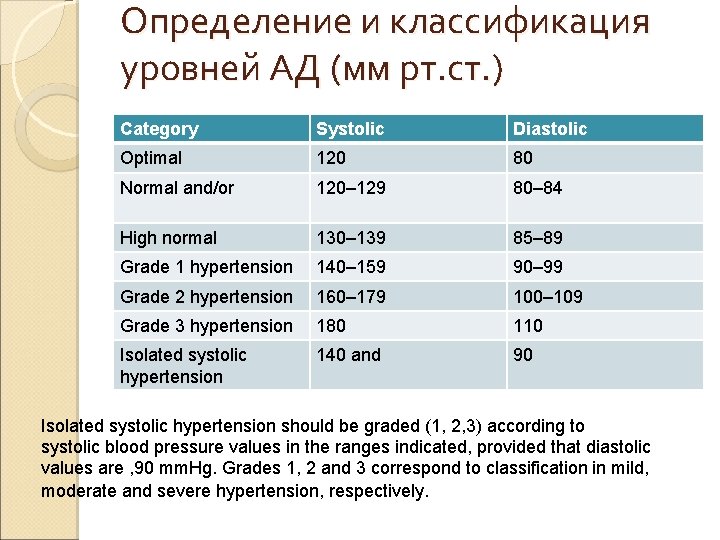
The classification of hypertension used in the 2003 ESH/ESC Guidelines has been retained with the following provisos: 1. when a patient’s systolic and diastolic blood pressures fall into different categories the higher category should apply for the quantification of total cardiovascular risk, decision about drug treatment and estimation of treatment efficacy; 2. isolated systolic hypertension should be graded (grades 1, 2 and 3) according to the same systolic blood pressure values indicated for systolic-diastolic hypertension. However, as mentioned above, the association with a low diastolic blood pressure (e. g. 60– 70 mm. Hg) should be regarded as an additional risk; 3. the threshold for hypertension (and the need for drug treatment) should be considered as flexible based on the level and profile of total cardiovascular risk.

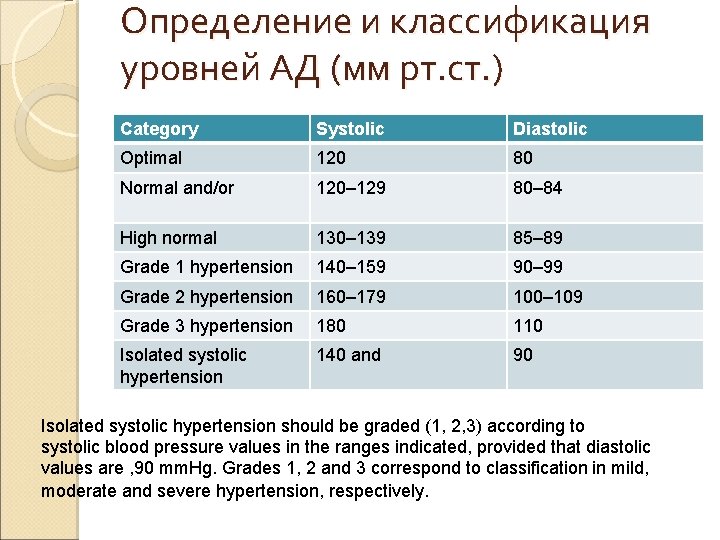
Определение и классификация уровней АД (мм рт. ст. ) Category Systolic Diastolic Optimal 120 80 Normal and/or 120– 129 80– 84 High normal 130– 139 85– 89 Grade 1 hypertension 140– 159 90– 99 Grade 2 hypertension 160– 179 100– 109 Grade 3 hypertension 180 110 Isolated systolic hypertension 140 and 90 Isolated systolic hypertension should be graded (1, 2, 3) according to systolic blood pressure values in the ranges indicated, provided that diastolic values are , 90 mm. Hg. Grades 1, 2 and 3 correspond to classification in mild, moderate and severe hypertension, respectively.



Total cardiovascular risk Dysmetabolic risk factors and subclinical organ damage are common in hypertensive patients. All patients should be classified not only in relation to the grades of hypertension but also in terms of the total cardiovascular risk resulting from the coexistence of different risk factors, organ damage and disease. Decisions on treatment strategies (initiation of drug treatment, BP threshold and target for treatment, use of combination treatment, need of a statin and other non-antihypertensive drugs) all importantly depend on the initial level of risk.
Total cardiovascular risk There are several methods by which total cardiovascular risk can be assessed, all with advantages and limitations. Categorization of total risk as low, moderate, high, and very high added risk has the merit of simplicity and can therefore be recommended. The term ‘added risk’ refers to the risk additional to the average one. Total risk is usually expressed as the absolute risk of having a cardiovascular event within 10 years.
Risk factors Systolic and diastolic BP levels Levels of pulse pressure (in the elderly) Age (M. 55 years; W. 65 years) Smoking Dyslipidaemia TC. 5. 0 mmol/l (190 mg/dl) or: - LDL-C. 3. 0 mmol/l (115 mg/dl) or: - HDL-C: M , 1. 0 mmol/l (40 mg/dl), W , 1. 2 mmol/l (46 mg/dl) or: - TG. 1. 7 mmol/l (150 mg/dl) Fasting plasma glucose 5. 6– 6. 9 mmol/L (102– 125 mg/dl) Abnormal glucose tolerance test Abdominal obesity (Waist circumference. 102 cm (M), . 88 cm (W)) † Family history of premature CV disease (M at age , 55 years; W at age , 65 years)
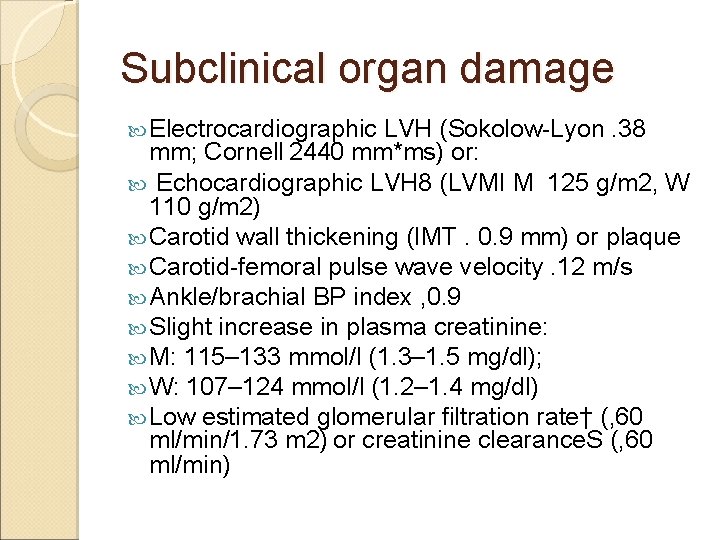
Subclinical organ damage Electrocardiographic LVH (Sokolow-Lyon. 38 mm; Cornell 2440 mm*ms) or: Echocardiographic LVH 8 (LVMI M 125 g/m 2, W 110 g/m 2) Carotid wall thickening (IMT. 0. 9 mm) or plaque Carotid-femoral pulse wave velocity. 12 m/s Ankle/brachial BP index , 0. 9 Slight increase in plasma creatinine: M: 115– 133 mmol/l (1. 3– 1. 5 mg/dl); W: 107– 124 mmol/l (1. 2– 1. 4 mg/dl) Low estimated glomerular filtration rate† (, 60 ml/min/1. 73 m 2) or creatinine clearance. S (, 60 ml/min)
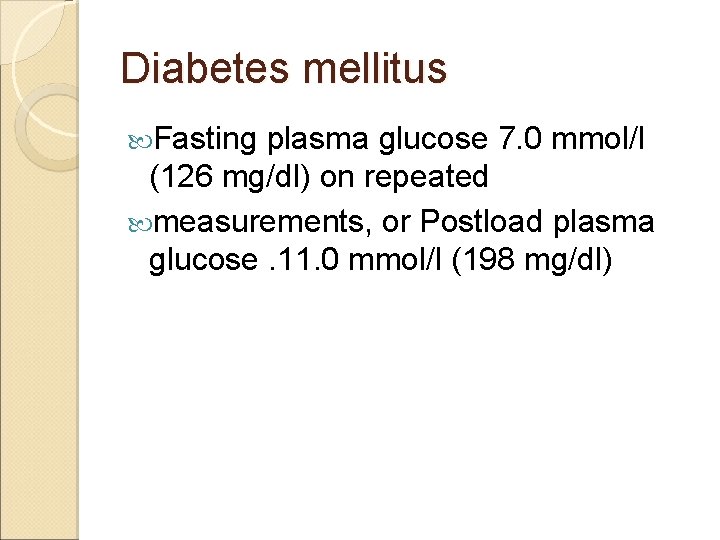
Diabetes mellitus Fasting plasma glucose 7. 0 mmol/l (126 mg/dl) on repeated measurements, or Postload plasma glucose. 11. 0 mmol/l (198 mg/dl)
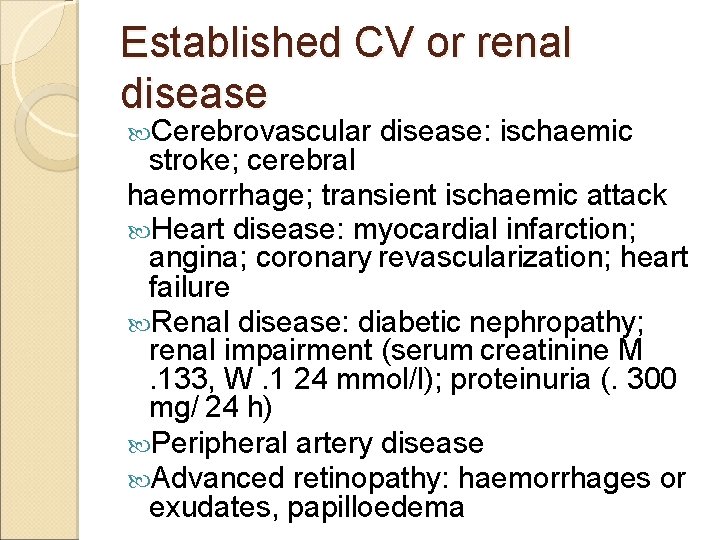
Established CV or renal disease Cerebrovascular disease: ischaemic stroke; cerebral haemorrhage; transient ischaemic attack Heart disease: myocardial infarction; angina; coronary revascularization; heart failure Renal disease: diabetic nephropathy; renal impairment (serum creatinine M. 133, W. 1 24 mmol/l); proteinuria (. 300 mg/ 24 h) Peripheral artery disease Advanced retinopathy: haemorrhages or exudates, papilloedema
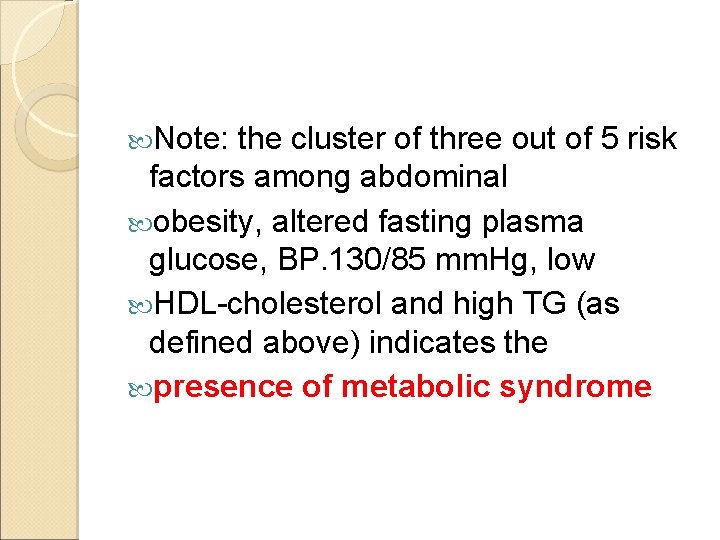
Note: the cluster of three out of 5 risk factors among abdominal obesity, altered fasting plasma glucose, BP. 130/85 mm. Hg, low HDL-cholesterol and high TG (as defined above) indicates the presence of metabolic syndrome
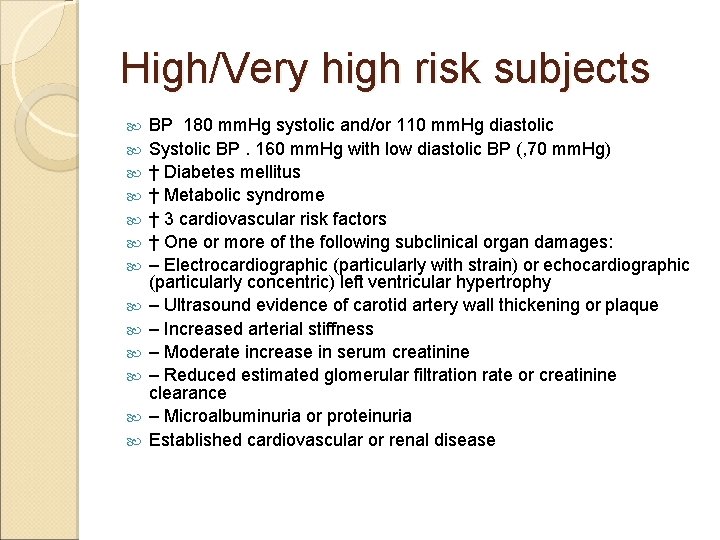
High/Very high risk subjects BP 180 mm. Hg systolic and/or 110 mm. Hg diastolic Systolic BP. 160 mm. Hg with low diastolic BP (, 70 mm. Hg) † Diabetes mellitus † Metabolic syndrome † 3 cardiovascular risk factors † One or more of the following subclinical organ damages: – Electrocardiographic (particularly with strain) or echocardiographic (particularly concentric) left ventricular hypertrophy – Ultrasound evidence of carotid artery wall thickening or plaque – Increased arterial stiffness – Moderate increase in serum creatinine – Reduced estimated glomerular filtration rate or creatinine clearance – Microalbuminuria or proteinuria Established cardiovascular or renal disease
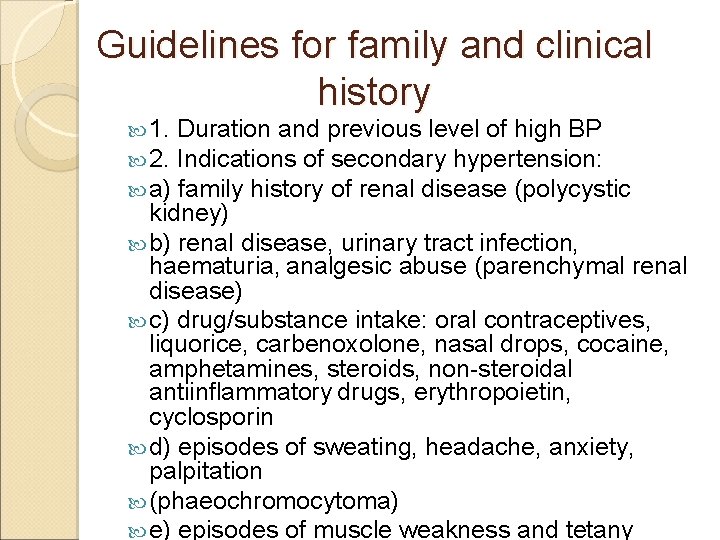
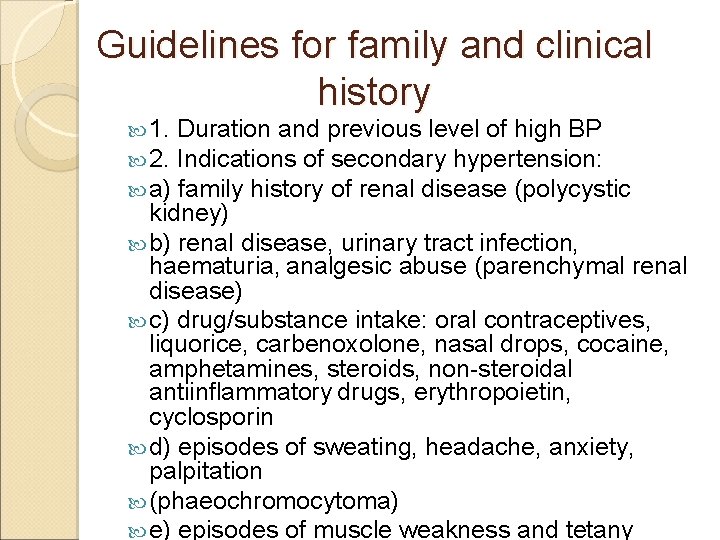
Guidelines for family and clinical history 1. Duration and previous level of high BP 2. Indications of secondary hypertension: a) family history of renal disease (polycystic kidney) b) renal disease, urinary tract infection, haematuria, analgesic abuse (parenchymal renal disease) c) drug/substance intake: oral contraceptives, liquorice, carbenoxolone, nasal drops, cocaine, amphetamines, steroids, non-steroidal antiinflammatory drugs, erythropoietin, cyclosporin d) episodes of sweating, headache, anxiety, palpitation (phaeochromocytoma) e) episodes of muscle weakness and tetany
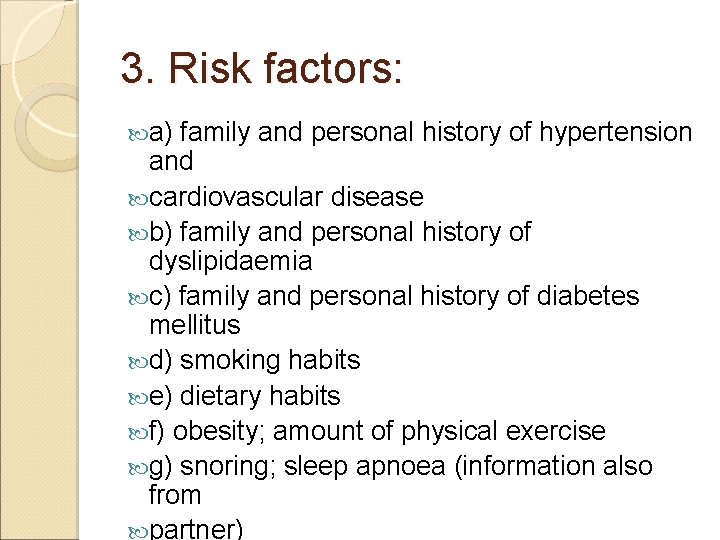
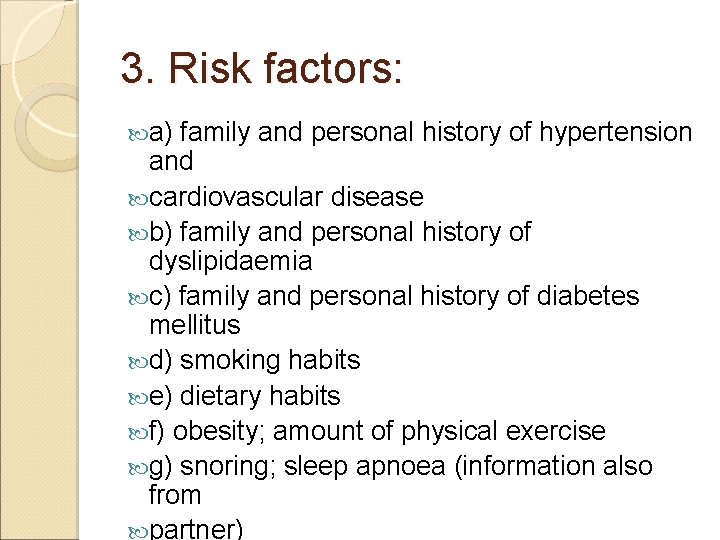
3. Risk factors: a) family and personal history of hypertension and cardiovascular disease b) family and personal history of dyslipidaemia c) family and personal history of diabetes mellitus d) smoking habits e) dietary habits f) obesity; amount of physical exercise g) snoring; sleep apnoea (information also from partner)
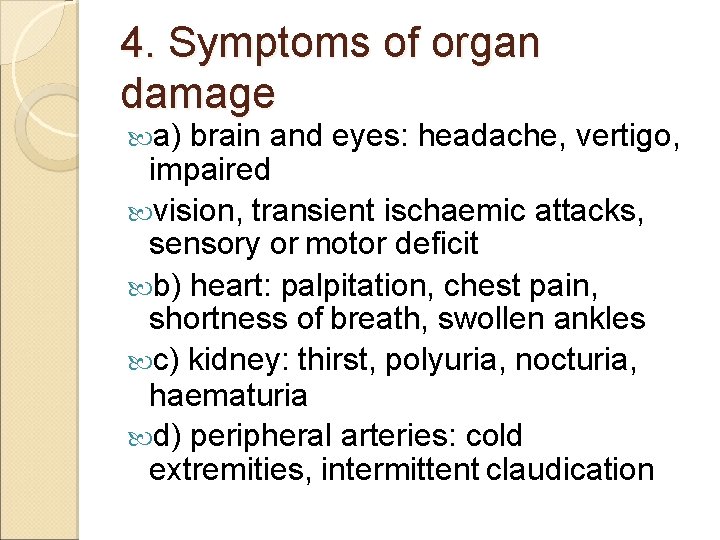
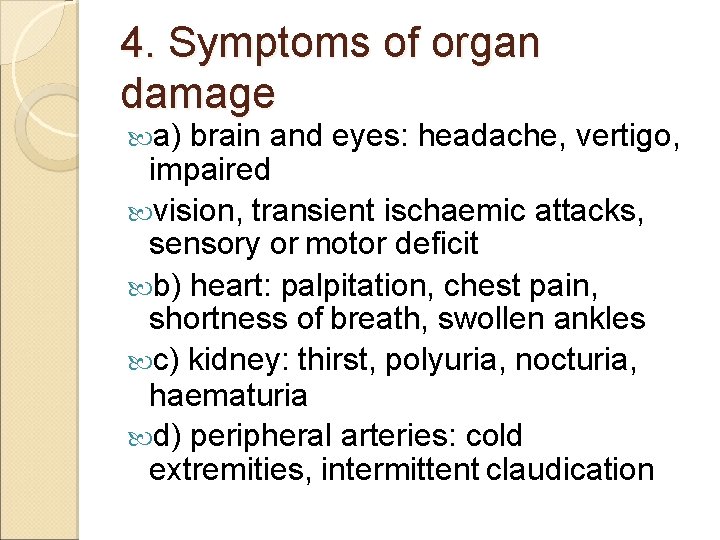
4. Symptoms of organ damage a) brain and eyes: headache, vertigo, impaired vision, transient ischaemic attacks, sensory or motor deficit b) heart: palpitation, chest pain, shortness of breath, swollen ankles c) kidney: thirst, polyuria, nocturia, haematuria d) peripheral arteries: cold extremities, intermittent claudication
5. Previous antihypertensive therapy: a) Drug(s) used, efficacy and adverse effects 6. Personal, family and environmental factors
Signs suggesting secondary hypertension and organ damage Features of Cushing syndrome Skin stigmata of neurofibromatosis (phaeochromocytoma) Palpation of enlarged kidneys (polycystic kidney) Auscultation of abdominal murmurs (renovascular hypertension) Auscultation of precordial or chest murmurs (aortic coarctation or aortic disease) Diminished and delayed femoral pulses and reduced femoral BP (aortic coarctation, aortic disease)
Signs of organ damage Brain: murmurs over neck arteries, motor or sensory Defects Retina: fundoscopic abnormalities Heart: location and characteristics of apical impulse, abnormal cardiac rhythms, ventricular gallop, pulmonary rales, peripheral oedema Peripheral arteries: absence, reduction, or asymmetry of pulses, cold extremities, ischaemic skin lesions Carotid arteries: systolic murmurs
Evidence of visceral obesity Body weight Increased waist circumference (standing position) M: . 102 cm; F: . 88 cm Increased body mass index [body weight (kg)/height (m)2] Overweight 25 kg/m 2; Obesity 30 kg/m 2
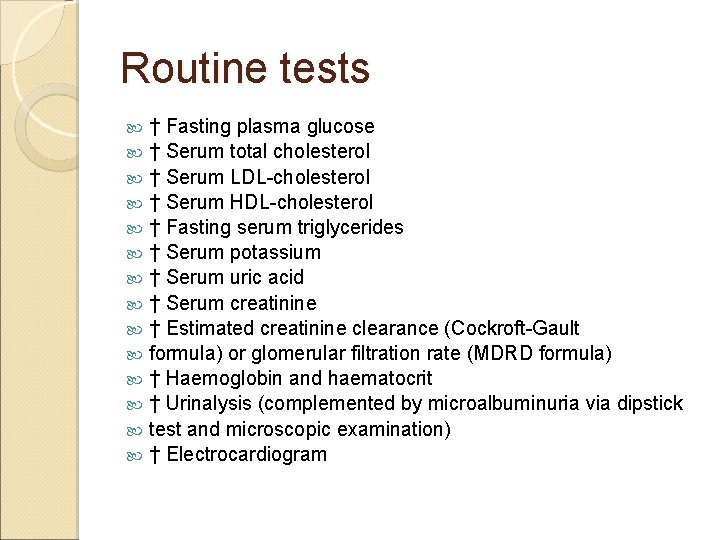
Routine tests † Fasting plasma glucose † Serum total cholesterol † Serum LDL-cholesterol † Serum HDL-cholesterol † Fasting serum triglycerides † Serum potassium † Serum uric acid † Serum creatinine † Estimated creatinine clearance (Cockroft-Gault formula) or glomerular filtration rate (MDRD formula) † Haemoglobin and haematocrit † Urinalysis (complemented by microalbuminuria via dipstick test and microscopic examination) † Electrocardiogram
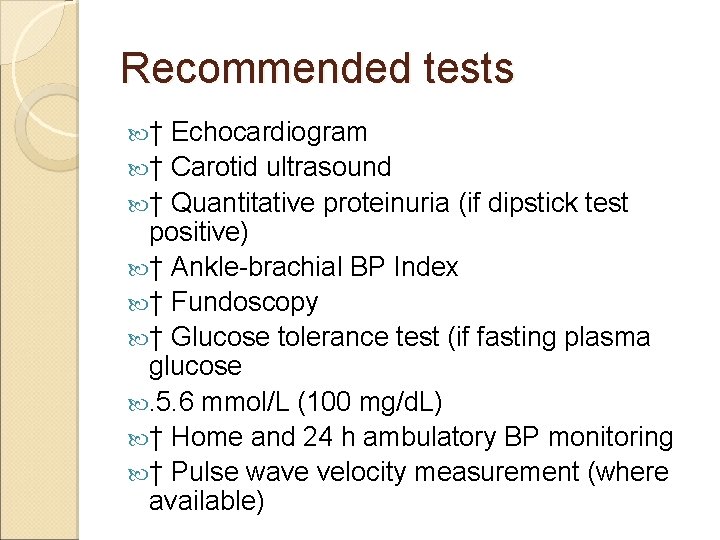
Recommended tests † Echocardiogram † Carotid ultrasound † Quantitative proteinuria (if dipstick test positive) † Ankle-brachial BP Index † Fundoscopy † Glucose tolerance test (if fasting plasma glucose . 5. 6 mmol/L (100 mg/d. L) † Home and 24 h ambulatory BP monitoring † Pulse wave velocity measurement (where available)
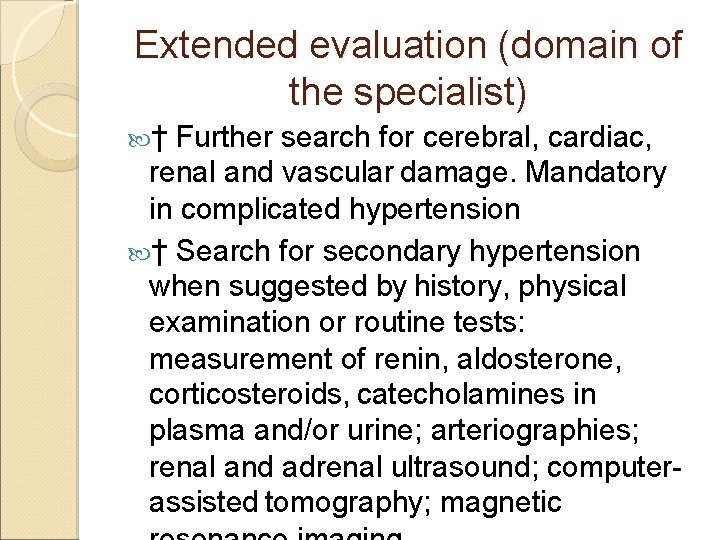
Extended evaluation (domain of the specialist) † Further search for cerebral, cardiac, renal and vascular damage. Mandatory in complicated hypertension † Search for secondary hypertension when suggested by history, physical examination or routine tests: measurement of renin, aldosterone, corticosteroids, catecholamines in plasma and/or urine; arteriographies; renal and adrenal ultrasound; computerassisted tomography; magnetic























 Hypertension
Hypertension Stage 1 hypertension
Stage 1 hypertension Malignant hypertension management
Malignant hypertension management Nursing management of portal hypertension
Nursing management of portal hypertension Diueritique
Diueritique Hypertension vs hypotension
Hypertension vs hypotension Hypertension
Hypertension Jnc7
Jnc7 Hypertension intracrânienne
Hypertension intracrânienne Med
Med Hypertension
Hypertension Diagnosis hypertension
Diagnosis hypertension Endorine
Endorine Jnc 7 hypertension
Jnc 7 hypertension Tête de méduse cirrhose
Tête de méduse cirrhose Modifiable risk factors for hypertension
Modifiable risk factors for hypertension Bp = co x svr
Bp = co x svr Definition of hypertension
Definition of hypertension Masked hypertension
Masked hypertension Definition of pulmonary hypertension
Definition of pulmonary hypertension Causes of secondary hypertension
Causes of secondary hypertension Cld vs dcld
Cld vs dcld Hypertension vs hypotension
Hypertension vs hypotension Nt pro brain natriuretic peptide
Nt pro brain natriuretic peptide Portal hypertension signs
Portal hypertension signs Missed some points on the visual field test for dvla
Missed some points on the visual field test for dvla Hypertension urgency vs emergency
Hypertension urgency vs emergency Veretigo
Veretigo What is the dash diet
What is the dash diet What is office blood pressure
What is office blood pressure Conclusion of hypertension
Conclusion of hypertension Pulmonary hypertension definition
Pulmonary hypertension definition Bmpr gene
Bmpr gene Mitral stenosis pulmonary hypertension
Mitral stenosis pulmonary hypertension Hypokalemia
Hypokalemia Pico question examples labor and delivery
Pico question examples labor and delivery Conclusion of hypertension
Conclusion of hypertension Sohil rangwala
Sohil rangwala Hypertensive crisis
Hypertensive crisis Presenting complaints of hypertension
Presenting complaints of hypertension Conclusion of hypertension
Conclusion of hypertension Medical nutrition therapy for hypertension
Medical nutrition therapy for hypertension Hypertensive crisis classification
Hypertensive crisis classification Phlebography
Phlebography Intracranial hypertension
Intracranial hypertension Decerebrate posturing
Decerebrate posturing Complications of cirrhosis
Complications of cirrhosis Health coaches for hypertension control
Health coaches for hypertension control Rules of halves in hypertension
Rules of halves in hypertension Dyslipidemia pathophysiology
Dyslipidemia pathophysiology Dianne zwicke
Dianne zwicke Chd pulmonary hypertension
Chd pulmonary hypertension Hypertension
Hypertension Pneumotrieste
Pneumotrieste Isolated systolic hypertension
Isolated systolic hypertension Traitement hypertension
Traitement hypertension Stages of pulmonary hypertension
Stages of pulmonary hypertension Presinusoidal portal hypertension
Presinusoidal portal hypertension Jnc 8 hypertension classification
Jnc 8 hypertension classification