Dueling Hypertension Guidelines Focus on ACCAHA Guidelines John
- Slides: 16
(Dueling) Hypertension Guidelines: Focus on ACC/AHA Guidelines John M. Flack, M. D. , M. P. H. , F. A. H. A, F. A. S. H, M. A. C. P Professor and Chair, Department of Medicine, Southern Illinois University Specialist in Clinical Hypertension (ASH) President, American Hypertension Specialist Certification Program
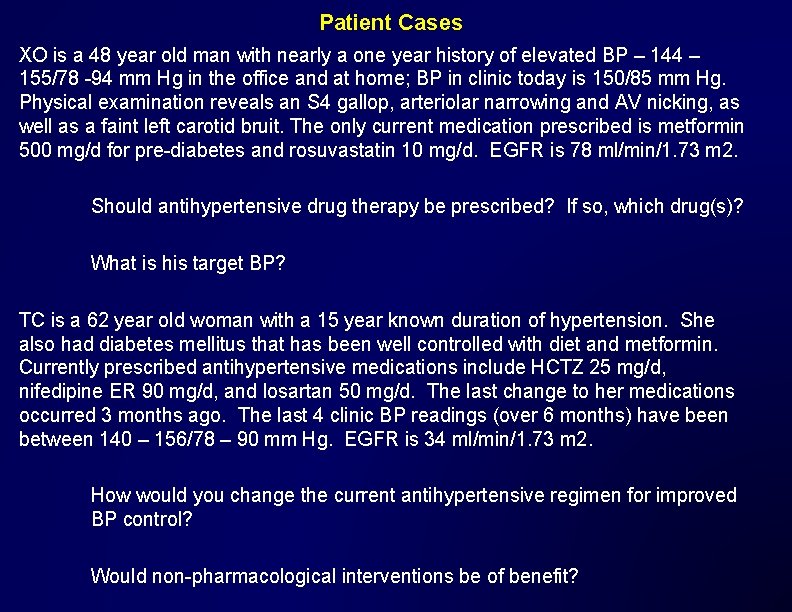
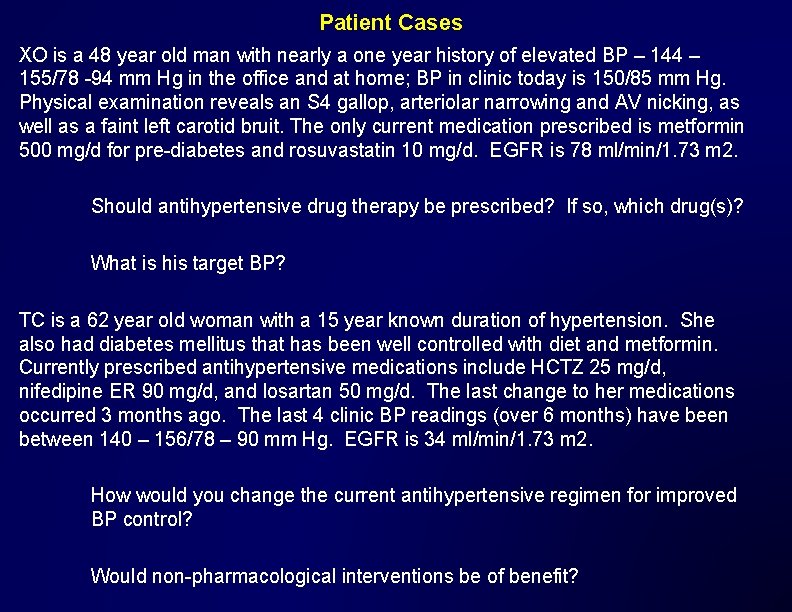
Patient Cases XO is a 48 year old man with nearly a one year history of elevated BP – 144 – 155/78 -94 mm Hg in the office and at home; BP in clinic today is 150/85 mm Hg. Physical examination reveals an S 4 gallop, arteriolar narrowing and AV nicking, as well as a faint left carotid bruit. The only current medication prescribed is metformin 500 mg/d for pre-diabetes and rosuvastatin 10 mg/d. EGFR is 78 ml/min/1. 73 m 2. Should antihypertensive drug therapy be prescribed? If so, which drug(s)? What is his target BP? TC is a 62 year old woman with a 15 year known duration of hypertension. She also had diabetes mellitus that has been well controlled with diet and metformin. Currently prescribed antihypertensive medications include HCTZ 25 mg/d, nifedipine ER 90 mg/d, and losartan 50 mg/d. The last change to her medications occurred 3 months ago. The last 4 clinic BP readings (over 6 months) have been between 140 – 156/78 – 90 mm Hg. EGFR is 34 ml/min/1. 73 m 2. How would you change the current antihypertensive regimen for improved BP control? Would non-pharmacological interventions be of benefit?
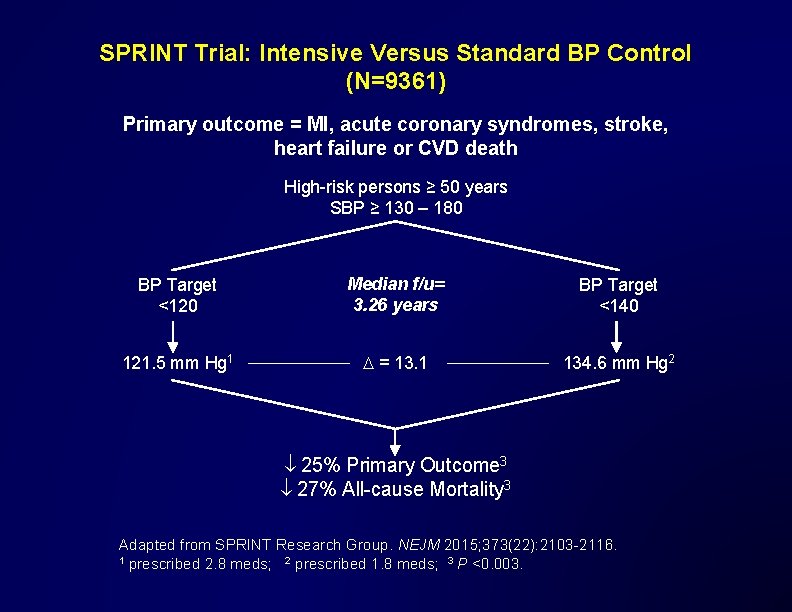
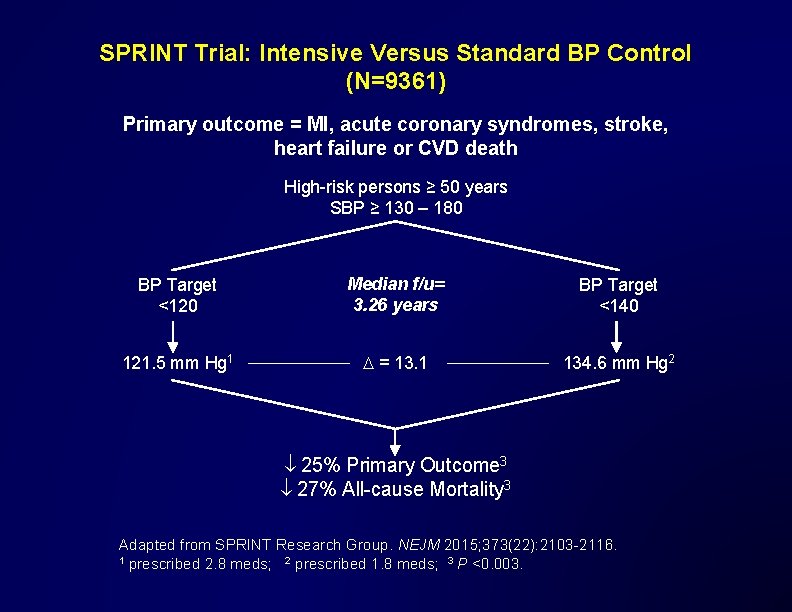
SPRINT Trial: Intensive Versus Standard BP Control (N=9361) Primary outcome = MI, acute coronary syndromes, stroke, heart failure or CVD death High-risk persons ≥ 50 years SBP ≥ 130 – 180 BP Target <120 Median f/u= 3. 26 years BP Target <140 121. 5 mm Hg 1 D = 13. 1 134. 6 mm Hg 2 25% Primary Outcome 3 27% All-cause Mortality 3 Adapted from SPRINT Research Group. NEJM 2015; 373(22): 2103 -2116. 1 prescribed 2. 8 meds; 2 prescribed 1. 8 meds; 3 P <0. 003.
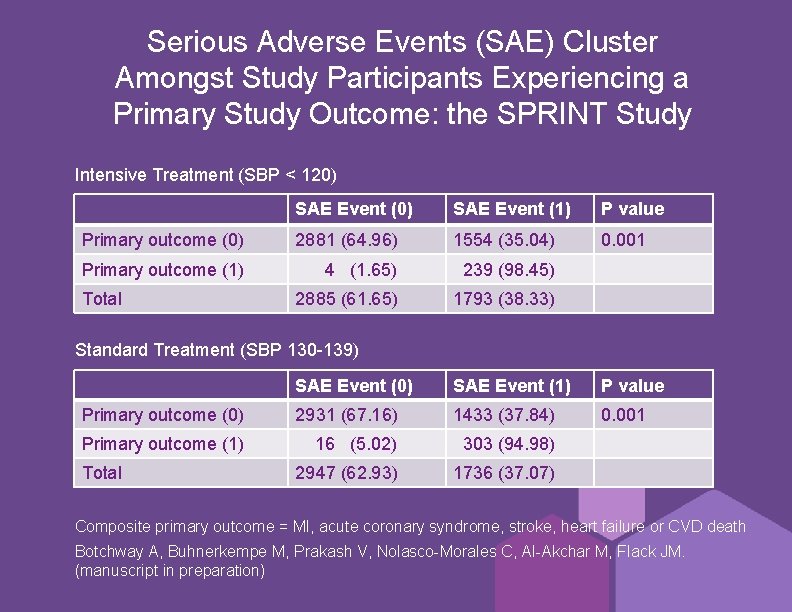
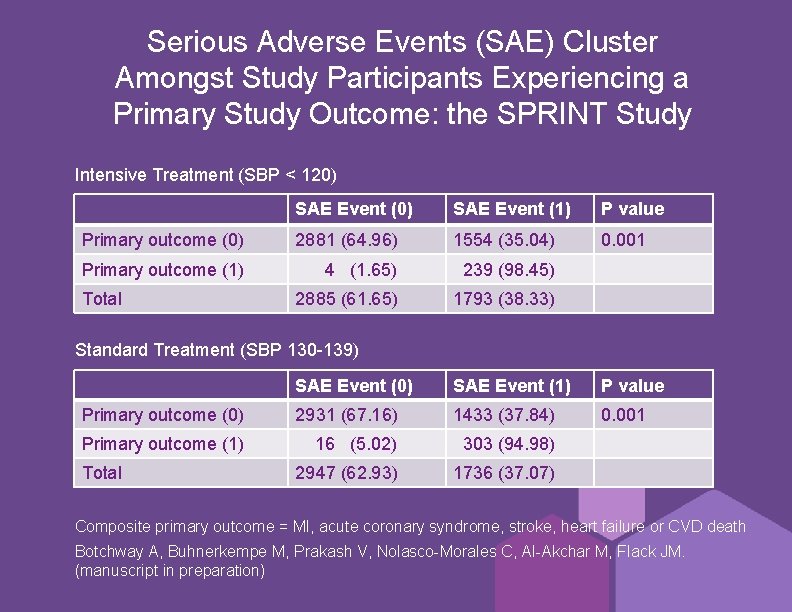
Serious Adverse Events (SAE) Cluster Amongst Study Participants Experiencing a Primary Study Outcome: the SPRINT Study Intensive Treatment (SBP ˂ 120) SAE Event (1) P value Primary outcome (0) 2881 (64. 96) 1554 (35. 04) 0. 001 Primary outcome (1) 4 (1. 65) 239 (98. 45) 2885 (61. 65) 1793 (38. 33) Total Standard Treatment (SBP 130 -139) SAE Event (0) SAE Event (1) P value Primary outcome (0) 2931 (67. 16) 1433 (37. 84) 0. 001 Primary outcome (1) 16 (5. 02) 303 (94. 98) 2947 (62. 93) 1736 (37. 07) Total Composite primary outcome = MI, acute coronary syndrome, stroke, heart failure or CVD death Botchway A, Buhnerkempe M, Prakash V, Nolasco-Morales C, Al-Akchar M, Flack JM. (manuscript in preparation)
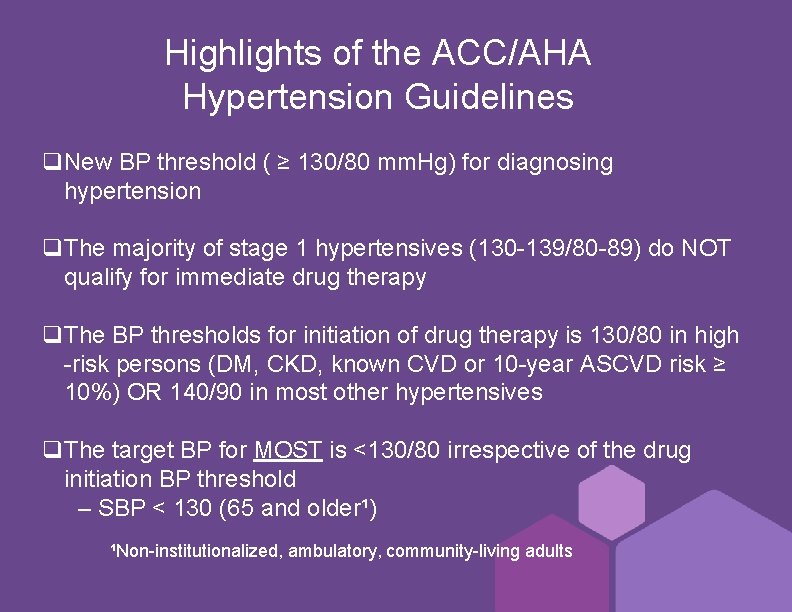
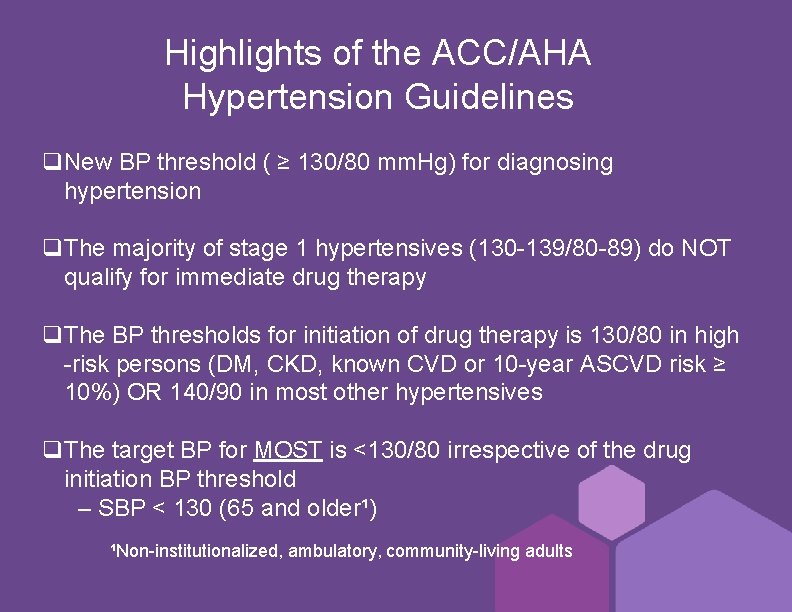
Highlights of the ACC/AHA Hypertension Guidelines q. New BP threshold ( ≥ 130/80 mm. Hg) for diagnosing hypertension q. The majority of stage 1 hypertensives (130 -139/80 -89) do NOT qualify for immediate drug therapy q. The BP thresholds for initiation of drug therapy is 130/80 in high -risk persons (DM, CKD, known CVD or 10 -year ASCVD risk ≥ 10%) OR 140/90 in most other hypertensives q. The target BP for MOST is ˂130/80 irrespective of the drug initiation BP threshold – SBP ˂ 130 (65 and older¹) ¹Non-institutionalized, ambulatory, community-living adults
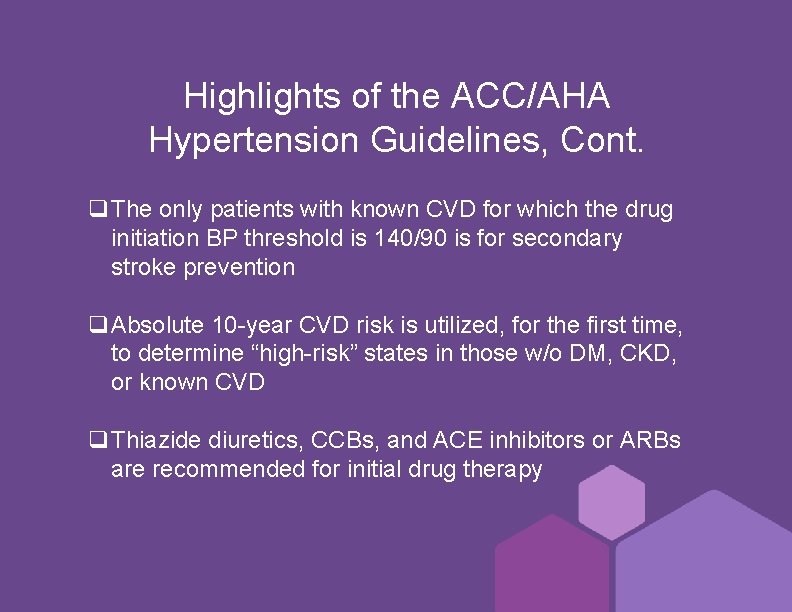
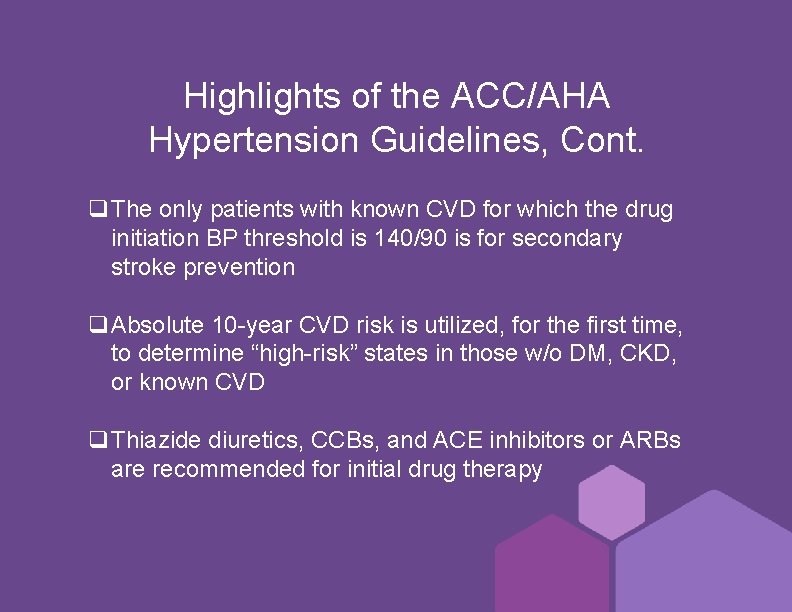
Highlights of the ACC/AHA Hypertension Guidelines, Cont. q. The only patients with known CVD for which the drug initiation BP threshold is 140/90 is for secondary stroke prevention q. Absolute 10 -year CVD risk is utilized, for the first time, to determine “high-risk” states in those w/o DM, CKD, or known CVD q. Thiazide diuretics, CCBs, and ACE inhibitors or ARBs are recommended for initial drug therapy
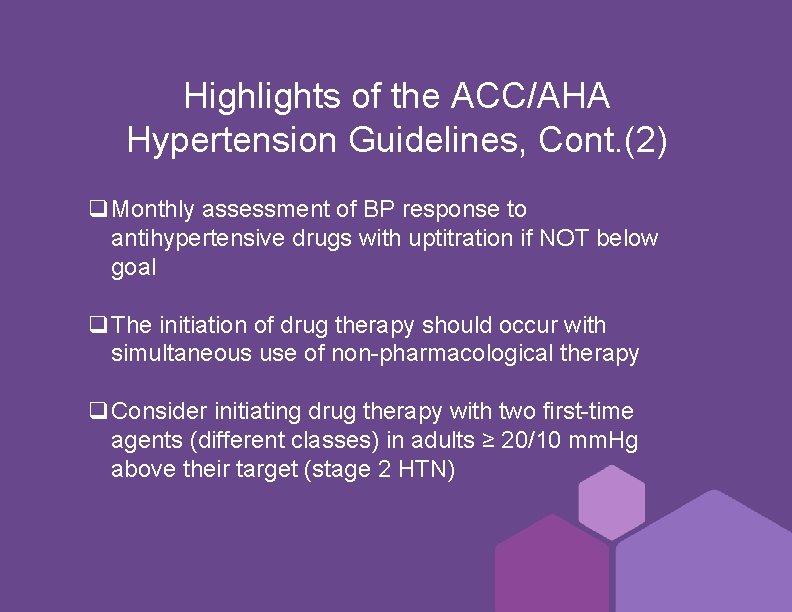
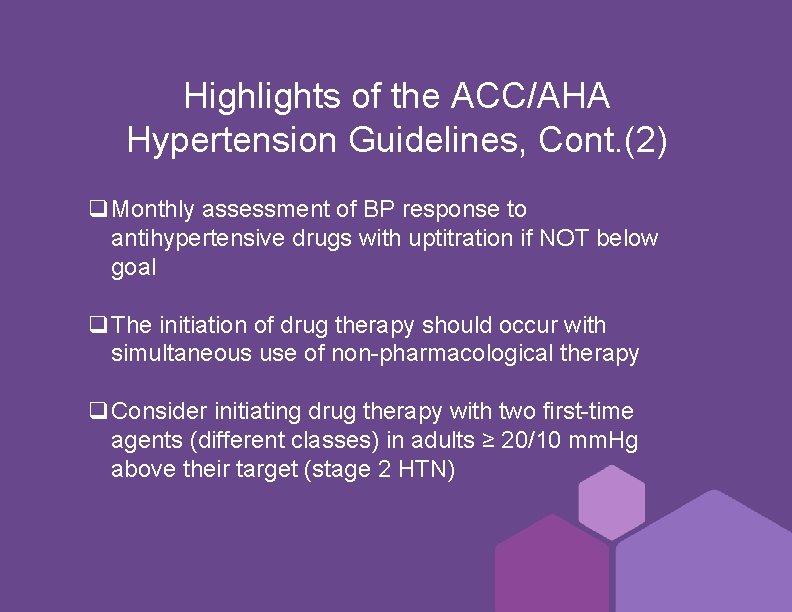
Highlights of the ACC/AHA Hypertension Guidelines, Cont. (2) q. Monthly assessment of BP response to antihypertensive drugs with uptitration if NOT below goal q. The initiation of drug therapy should occur with simultaneous use of non-pharmacological therapy q. Consider initiating drug therapy with two first-time agents (different classes) in adults ≥ 20/10 mm. Hg above their target (stage 2 HTN)
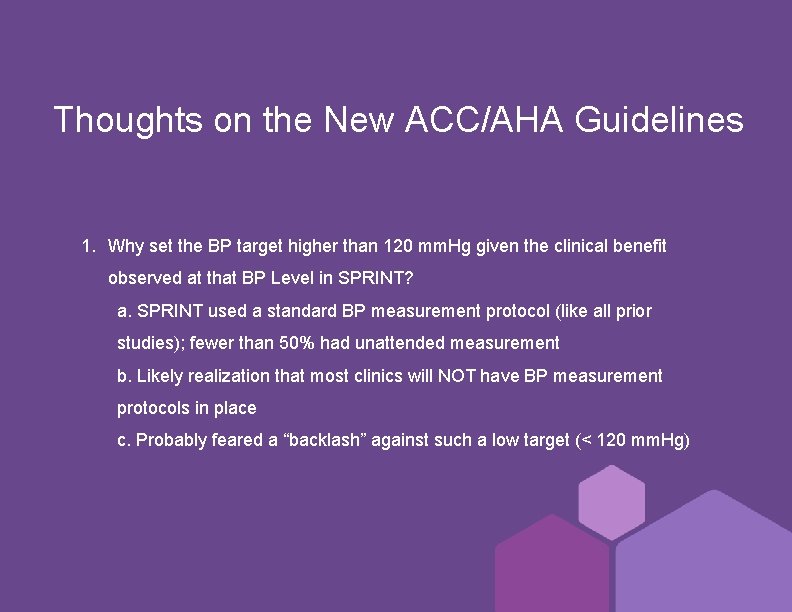
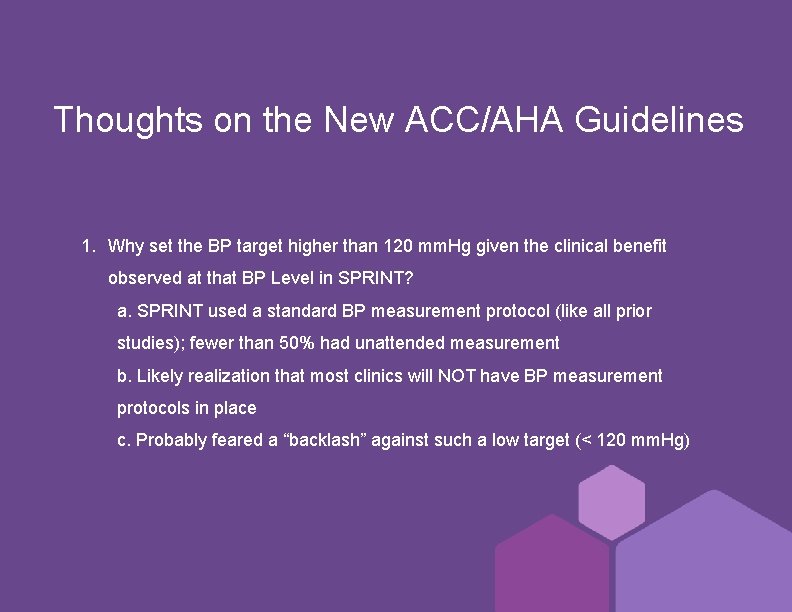
Thoughts on the New ACC/AHA Guidelines 1. Why set the BP target higher than 120 mm. Hg given the clinical benefit observed at that BP Level in SPRINT? a. SPRINT used a standard BP measurement protocol (like all prior studies); fewer than 50% had unattended measurement b. Likely realization that most clinics will NOT have BP measurement protocols in place c. Probably feared a “backlash” against such a low target (˂ 120 mm. Hg)
Thoughts on the New ACC/AHA Guidelines, Contd. 1. The BP treatment thresholds for “high risk” patients is 130/80 mm. Hg – even for such groups without clinical trial outcomes data to support the recommendation. Why? a. This is a flashpoint area of contention for those who synthesize the data across the vast hypertension outcomes database versus those who are absolutists b. The relative risk reduction for CVD events varies little across a broad range of BP’s and high-risk comorbid conditions c. The absolute risk reduction for CVD events is directly related to the pretreatment risk level
ACP/AAFP Recommend Systolic BP Targets Based on History and Risk Level in Adults ≥ 60 years old 1. SBP persistently ≥ 150 mm. Hg, initiate treatment to lower SBP to ˂ 150 mm. Hg (strong recommendation, high quality evidence) 2. In patients with prior stroke or TIA, initiate or intensify drug therapy to achieve SBP ˂ 140 mm. Hg (weak recommendation, moderate quality evidence) 3. In some patients with high cardiovascular (CV) risk, consider initiating or intensifying drug treatment to achieve SBP ˂ 140 mm. Hg (weak recommendation, low quality evidence) Qaseem A et al. Ann Intern Med 2017; 166: 430 -7.
Accurate BP Measurement The 3 Necessary Pillars Validated Device Measurement Techniques Measurement Conditions The above is true irrespective of the location of BP measurement (clinic, home)
Listings of Validated Home and Office BP Monitors https: //bihsoc. org/bp-monitors/ British and Irish Hypertension Society
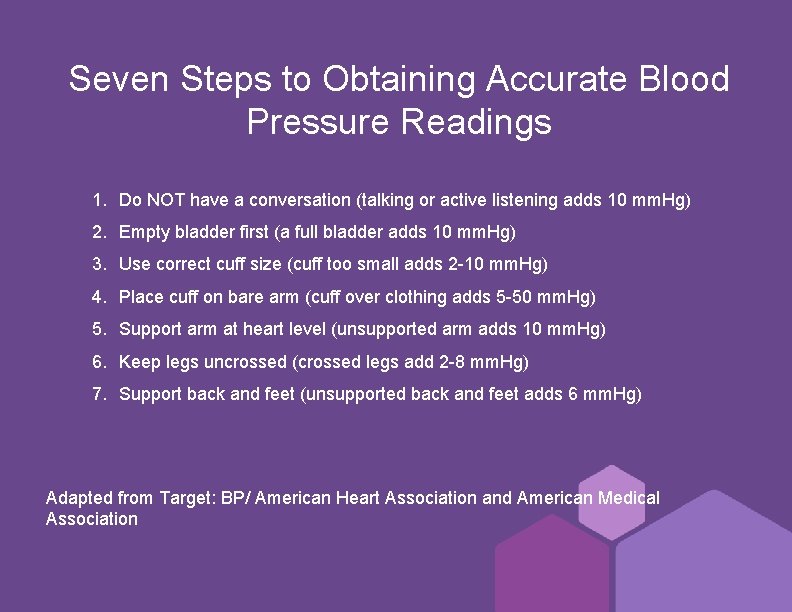
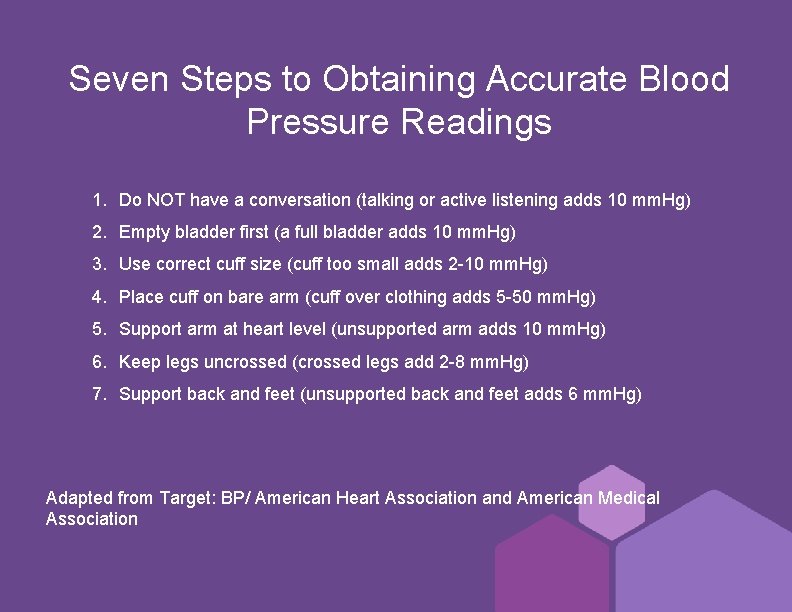
Seven Steps to Obtaining Accurate Blood Pressure Readings 1. Do NOT have a conversation (talking or active listening adds 10 mm. Hg) 2. Empty bladder first (a full bladder adds 10 mm. Hg) 3. Use correct cuff size (cuff too small adds 2 -10 mm. Hg) 4. Place cuff on bare arm (cuff over clothing adds 5 -50 mm. Hg) 5. Support arm at heart level (unsupported arm adds 10 mm. Hg) 6. Keep legs uncrossed (crossed legs add 2 -8 mm. Hg) 7. Support back and feet (unsupported back and feet adds 6 mm. Hg) Adapted from Target: BP/ American Heart Association and American Medical Association
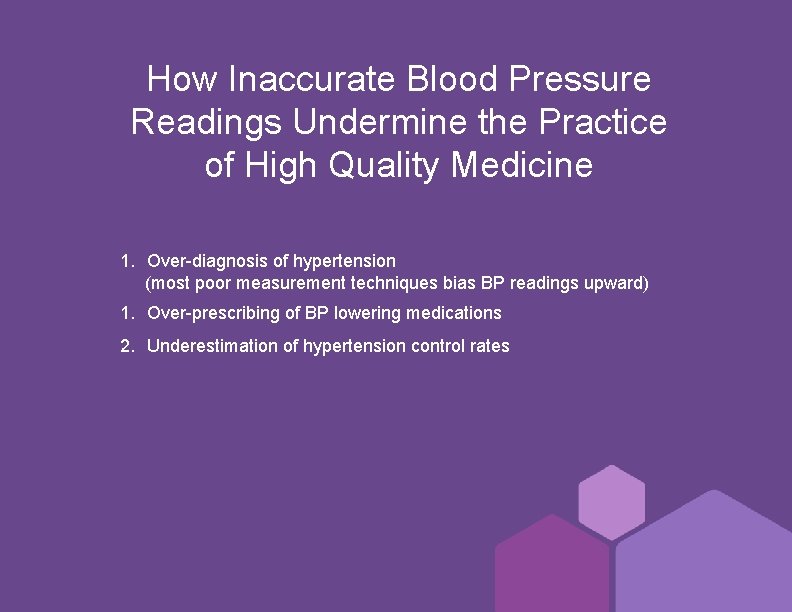
How Inaccurate Blood Pressure Readings Undermine the Practice of High Quality Medicine 1. Over-diagnosis of hypertension (most poor measurement techniques bias BP readings upward) 1. Over-prescribing of BP lowering medications 2. Underestimation of hypertension control rates
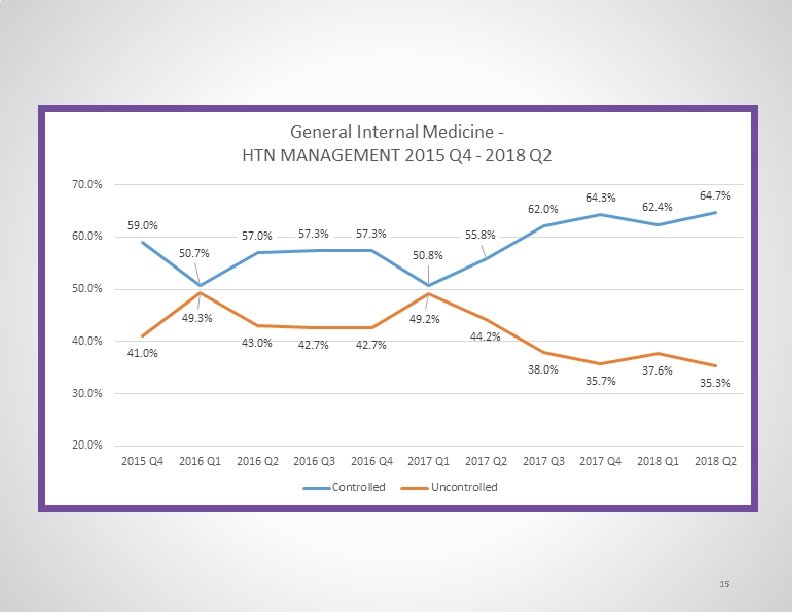
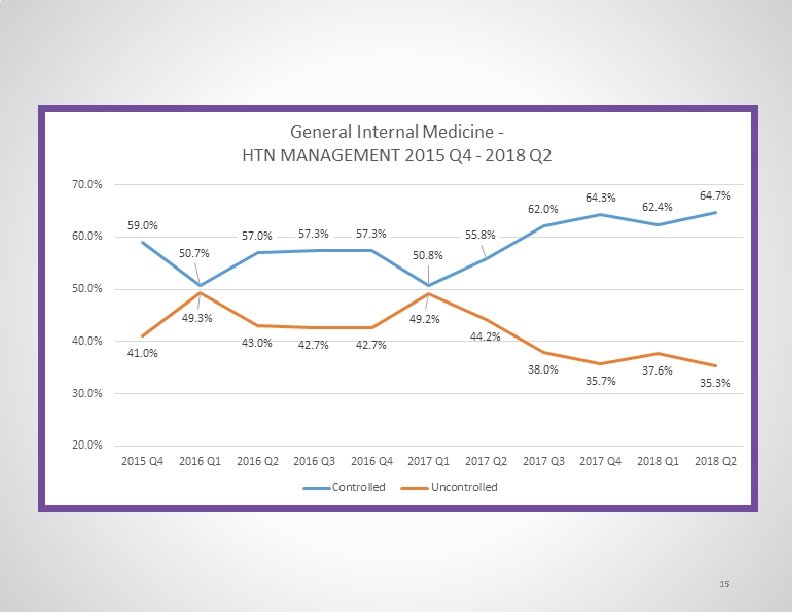
15
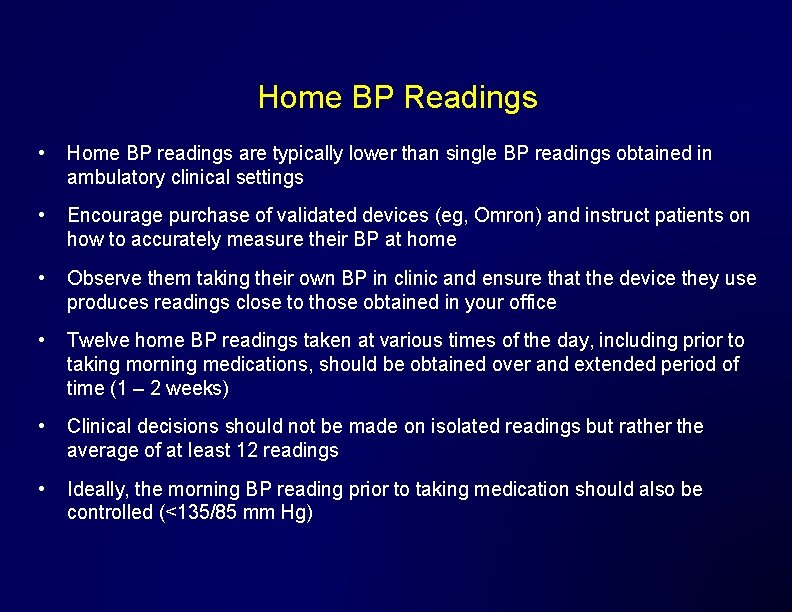
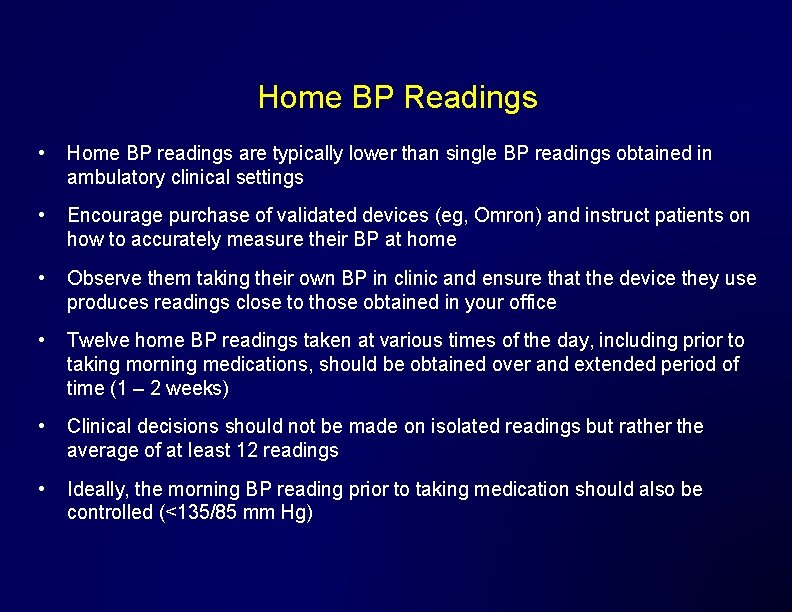
Home BP Readings • Home BP readings are typically lower than single BP readings obtained in ambulatory clinical settings • Encourage purchase of validated devices (eg, Omron) and instruct patients on how to accurately measure their BP at home • Observe them taking their own BP in clinic and ensure that the device they use produces readings close to those obtained in your office • Twelve home BP readings taken at various times of the day, including prior to taking morning medications, should be obtained over and extended period of time (1 – 2 weeks) • Clinical decisions should not be made on isolated readings but rather the average of at least 12 readings • Ideally, the morning BP reading prior to taking medication should also be controlled (<135/85 mm Hg)